Identifying and Addressing the
Needs of Adolescents and
Young Adults with Cancer
A LIVESTRONG and Institute of Medicine Workshop
Cancer is the leading disease-related cause of death in adolescents and young adults (AYAs). Each year almost 70,000 AYAs between the ages of 15 and 39 are diagnosed with cancer, approximately eight times more than children under age 15. This population faces many short- and long-term health and psychosocial issues, such as difficulty reentering school, the workforce, or the dating scene; problems with infertility; cardiac, pulmonary, or other treatment repercussions; and secondary malignancies. Survivors of AYA cancers are also at increased risk for psychiatric conditions such as anxiety, depression, substance abuse, and suicide. In addition, they may have difficulty acquiring health insurance and paying for needed care.
Many programs for cancer treatment, survivorship care, and psychosocial support do not focus on the specific needs and risks of AYA cancer patients. Recognizing this health disparity, in 2006 the National Cancer Institute (NCI) appointed a progress review group (PRG) to produce a report outlining recommendations for improving the care and outcomes for adolescents and young adults with cancer (HHS and LIVESTRONG Young Adult Alliance, 2006). A plan outlining strategies for implementation of these recommendations was developed in 2007 (LIVESTRONG Young Adult Alliance, 2007). Since that time, progress has been made in bringing attention to the special needs of AYAs with cancer. However, many challenges remain in providing optimal care for this population.
To facilitate discussion about gaps and challenges in caring for AYA cancer patients and potential strategies and actions to improve the quality of their care, the Institute of Medicine’s (IOM’s) National Cancer Policy Forum (NCPF) collaborated with the LIVESTRONG Foundation to convene a workshop, Addressing the Needs of Adolescents and Young Adults with Cancer, on July 15–16, 2013, in Washington, DC.1 The workshop featured discussion panels as well as invited presentations from clinicians, researchers, AYA cancer survivors, and health advocates working to improve the care and outcomes for this population. Participants discussed a variety of topics important to AYA patients with cancer, including
• the ways in which cancers affecting AYAs differ from cancers in other age groups and what that implies about the best treatments for AYA cancer patients;
• the unique psychosocial needs of AYA cancer patients;
• behavioral health and lifestyle management;
• fertility preservation;
• adequate cancer screening and surveillance for AYA cancer patients;
• challenges in acquiring health insurance and paying for appropriate treatment and survivorship care;
• long-term medical and psychosocial needs for AYA cancer survivors;
• palliative care; and
• end-of-life care needs.
Participants also discussed research gaps and the challenges to developing an evidence base to guide the care of AYAs with cancer. Because of the dearth of data on the AYA population, a number of speakers presented data from studies of childhood cancer survivors who have since entered the AYA age range. Although it may be reasonable to extrapolate some findings from that data to patients diagnosed as AYAs, caution is needed in drawing
________________
1 This workshop was organized by an independent planning committee whose role was limited to the identification of topics and speakers. This workshop summary was prepared by the rapporteurs as a factual summary of the presentations and discussions that took place at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants; are not necessarily endorsed or verified by the Institute of Medicine, the National Cancer Policy Forum, or the LIVESTRONG Foundation; and should not be construed as reflecting any group consensus.
conclusions for the AYA population. Workshop participants also suggested policy strategies that could be pursued to improve the care of and outcomes for this population.
This report is a summary of the workshop. A summary of suggestions from individual participants is provided in Box 1. The workshop agenda and statement of task can be found in the Appendix. The speakers’ biographies and presentations (as PDF and audio files) have been archived at http://www.iom.edu/Activities/Disease/NCPF/2013-JUL-15.aspx.
Adolescents and young adults are more susceptible to certain types of cancers, including leukemia, lymphoma, melanoma, and cancers of the central nervous system, germ cells, connective tissue, and thyroid. This group of cancers differs from the cancers that commonly afflict children or older adults. Consequently, “pediatric oncologists and adult-treating physicians and medical oncologists are not as familiar with this group of cancers as they are with the other cancers that affect their patients,” said Archie Bleyer, clinical research professor at the Knight Cancer Institute of the Oregon Health & Science University (OHSU) (see Figure 1). Brandon Hayes-Lattin, associate professor of medicine, hematology, and medical oncology and the medical director of the Adolescent and Young Adult Oncology Program at OHSU Knight Cancer Institute, said that AYAs are also more likely to be diagnosed with different subtypes of cancers than other groups, which affects what treatments are most likely to be effective for them. For example, one study found that AYAs are more likely to be diagnosed with melanomas that have BRAF2 mutations and thus are more likely to respond to BRAF inhibitor drugs (Menzies et al., 2012). Similarly, AYAs diagnosed with acute lymphoblastic leukemia (ALL) tend to have genetic defects in their tumors that are associated with better prognosis. “This might explain why younger people, even if given the same therapy [as older adults] tend to do better,” he said. However, he also presented data showing that AYA patients who received a pediatric treatment regimen for ALL had a 63 percent event-free survival at 7 years versus 34 percent with the adult treatment regimen (Stock et al., 2008). He added that a recent meta analysis found that patients under the age of 35 with a matched sibling had significantly better survival with an allogeneic bone marrow transplant (Gupta et al., 2013).
________________
2 Human homolog B of v-raf (rapidly accelerated fibrosarcoma viral oncogene).
BOX 1
Suggestions Made by Individual Workshop Participants
Address the care needs of Adolescent and Young Adult (AYA) patients diagnosed with cancer
• Provide a clearinghouse for programs focused on AYA patients with cancer
• Implement care models that promote timely referral, timely initiation of treatment, and attention to treatment-protocol adherence
• Establish multidisciplinary care teams with training in the unique needs and developmental stages of AYA patients
• Integrate information about palliative care into new patient orientation packets and programs and incorporate proactive palliative care across the cancer care continuum
• Discuss fertility at the time of diagnosis and have in place an established referral mechanism for fertility preservation
• Design stress-management programs for cancer patients
• Design lifestyle intervention programs to match the developmental stage and interests of AYA patients
• Provide guidance on how to maintain effective access to health care and insurance, including follow-up cancer care, survivorship care, and routine primary care
Improve cancer survivorship care for AYA patients
• Develop new models for transitioning AYAs into survivorship care and provide tiered care to AYA cancer survivors based on their particular long-term risks and psychosocial needs
• Develop evidence-based guidelines for surveillance of cancer recurrence and screening for new cancers
Bleyer noted that the incidence of melanoma, cervical cancer, and lung cancer has declined among AYAs during the past 10 years, probably due to prevention efforts, including anti-smoking and pro-sunscreen campaigns, restrictions on indoor tanning devices, and use of human papillomavirus (HPV) vaccines. Bleyer said that although the incidence of most of the cancers that AYAs are prone to develop has declined or has not increased in the past 10 years, some types of cancer have become more common in this age group, including kidney, thyroid, breast, colorectal, and testicular
• Use an exposure-based approach to risk-reduction strategies for late effects and secondary cancers among AYA cancer survivors
• Increase efforts to identify patients with genetic syndromes that predispose AYAs to cancer and to implement evidence-based risk-reduction strategies for those patients
• Foster more collaboration between oncologists and primary care providers
• Consider fertility preservation post treatment if desired
Improve training, education, and research
• Provide more specialty training programs and fellowships and continuing medical education programs focused on the care of AYA patients and establish standards for training
• Address research gaps in psychosocial care, late treatment effects, fertility, lifestyle interventions, access to care, and socioeconomic consequences of cancer diagnosis (such as education, employment, and career)
• Measure patient outcomes following psychosocial care to ensure that care is informed by evidence
• Foster more collaboration among various organizations, institutions, and federal agencies
• Educate the AYA population about new options to obtain and maintain health insurance through the Affordable Care Act (ACA)
• Use existing data to better understand the patterns of health care utilization and unique burdens of AYA cancer survivors, particularly in relation to the impact of the ACA
• Develop and leverage online resources to communicate with AYA patients and to facilitate research
• Tailor communications about research for the AYA population
cancer and ALL. He said that the increase in colorectal cancer incidence might be due to an increase in HPV-associated rectal cancer combined with an increased likelihood of detection now that colonoscopies are being applied more widely.
He added that although the incidence of both kidney and thyroid cancer has substantially increased among AYAs, this is likely due to increased detection by ultrasound and other diagnostic imaging. “Both are examples of overdiagnosis in which our diagnostic testing has become so advanced
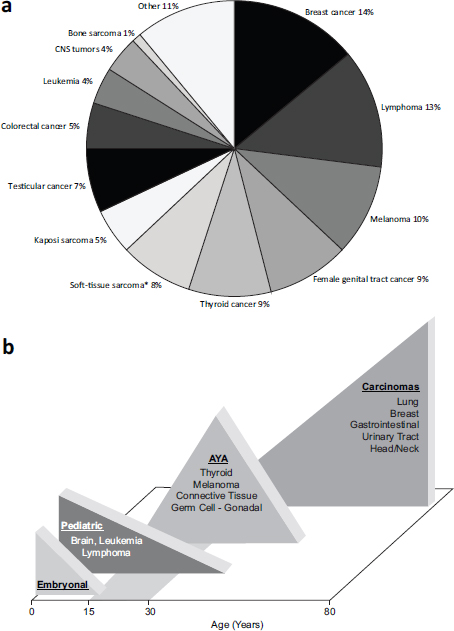
FIGURE 1 (A) Relative frequency of the common types of cancers in adolescents and young adults, aged 15–39, 1992–2002, and (B) the prevalence of cancer histology by age. The cancers that peak in incidence within each age range are listed in each triangle.
*Excluding Kaposi sarcoma.
NOTE: AYA = adolescent and young adult; CNS = central nervous system.
SOURCES: (A) Bleyer presentation; Bleyer et al. (2008). Reprinted by permission from Macmillan Publishers Ltd: Nature Reviews Cancer (Bleyer et al., 2008), copyright 2008. (B) Hudson presentation; Bleyer et al. (2006).
and widely available that we are now detecting indolent lesions of epithelial origin (IDLE) that do not need to be fixed. We are diagnosing more than we need to, and we are subsequently overtreating,” Bleyer said.
A new finding of uncertain significance is the proportion of cancer in AYAs that is not considered malignant, such as ductal carcinoma in situ (DCIS) of the breast and low-grade brain tumors (gliomas, craniopharyngioma, meningioma). Data from the Surveillance, Epidemiology and End Results (SEER) program indicate that about 15 percent of AYA cancers—one in every six to seven patients—are reported as non-malignant, the highest proportion of all age groups. Some of these non-malignant cancers are nonetheless lethal. “We need to look into this problem,” Bleyer said.
Melissa Hudson, director of cancer survivorship and division coleader for the cancer prevention and control program at St. Jude Children’s Research Hospital, showed that survival improved for those diagnosed with cancer in their 20s in the period 1993–1998 compared to those diagnosed during 1975–1980 (Veal et al., 2010). Survival decreased during the same time span for those diagnosed in their 30s.
More recent trends in cancer incidence, survival, and mortality among AYA patients are currently being assessed. The NCI held a meeting in September 2013, to examine current science and research gaps in AYA oncology. The workshop utilized five working groups that reviewed the available data on the epidemiology (incidence, survival, mortality) of select AYA cancers, as well as evidence related to basic biology, clinical trial enrollment, models of care, and health-related quality of life/symptom management for this population.
PROGRESS SINCE THE NCI PROGRESS REVIEW GROUP REPORT AND IMPLEMENTATION PLAN
The NCI PRG report made recommendations in five broad categories, shown in Box 2. The LIVESTRONG Foundation then convened the LIVESTRONG Young Adult Alliance, which has since evolved into an independent organization called Critical Mass: The Young Adult Cancer Alliance, to implement the report. Hayes-Lattin reported on the progress that has been made since the report came out in 2006.
BOX 2
NCI Progress Review Group Recommendations
1. Identify the characteristics that distinguish the unique cancer burden in the AYA oncology patient.
2. Provide education, training, and communication to improve awareness, prevention, access, and high-quality cancer care for AYAs.
3. Create the tools to study the AYA cancer problem.
4. Ensure excellence in service delivery across the cancer control continuum.
5. Strengthen and promote advocacy and support of the AYA cancer patient.
SOURCES: Hayes-Lattin presentation; HHS and LIVESTRONG Young Adult Alliance, 2006.
Identifying the Unique Cancer Burden in the AYA Population
A number of retrospective analyses have provided evidence for the biological distinctiveness of some of the cancers diagnoses in AYA patients, including osteosarcoma, colorectal cancer, ALL, breast cancer, testicular cancer, and thyroid cancer (Tricoli et al., 2011). Reports have also documented the unique characteristics of AYAs with cancer, including characteristics related to health-related quality of life (Smith et al., 2013), epidemiology trends (Johnson et al., 2013), toxicity (Gupta et al., 2012), and AYAs’ experience of psychological distress (Kwak et al., 2013).
Education, Training, and Communication
Efforts have been made to raise awareness of AYA cancer issues as a first step toward increasing the national focus on and resource allocation to the AYA cancer problem. The LIVESTRONG Young Adult Alliance has provided targeted education to patients, families and caregivers, and the public about AYA cancer issues and fostered the education of multidisciplinary care providers who work with AYAs in order to improve referrals and services for this population. Professional educational programs focused on AYAs with cancer now include the American Society of Clinical Oncology’s
Focus Under Forty3 online curriculum and the nurse oncology education program At the Crossroads.4 In addition, the LIVESTRONG Young Adult Alliance published a position statement on the necessary components for AYA oncology training for health professionals (Hayes-Lattin et al., 2010). There also now is a National Young Adult Cancer Awareness Week and associated media outreach activities.
“The field,” Hayes-Lattin said, “really is at a turning point of evolving from the notion of raising awareness as the principal target to formalizing some of those components, whether that would be requirements in educational curricula or certification standards.”
The NCI PRG report made a number of recommendations regarding research tool development, including recommendations to create a large prospective database of AYA cancer patients to facilitate research on this age group, to increase the number of annotated patient specimens to support research progress, and to improve grant coding and search term standardization to enable the evaluation of research efforts and progress. Since the report came out, there have been improved search tools in PubMed and other research databases that enable targeting of AYA-specific studies. But Hayes-Lattin noted a lack of available annotated biological specimens from AYA patients that researchers can prospectively link to treatments and patient outcomes. There is also still a need for a large prospective database of AYA cancer patients to facilitate research on this age group.
Much work remains to be done in this arena, Hayes-Lattin stressed, but he did point to progress made in other research-related areas. Efforts have been made to amend clinical trial eligibility requirements relating to age so that more adolescents and young adults with cancer can participate. A treatment regimen based on a pediatric protocol was recently applied in a clinical trial setting across multiple adult cooperative trial groups.5 The Alliance for Clinical Trials in Oncology also funded an adolescent and young adult cohort study that showed the feasibility of prospectively following adolescents and young adults from the time of their cancer diagnosis. Hayes-
________________
3 See http://university.asco.org/focus-under-forty (accessed October 8, 2013).
4 See http://www.noep.org/nursing-cne/preview/40-at-the-crossroads-cancer-in-ages-15-39 (accessed October 8, 2013).
5 See http://clinicaltrials.gov/show/NCT00558519 (accessed October 8, 2013).
Lattin also noted the newly created AYA-specific committees that are now a part of the NCI-supported National Clinical Trials Network. He called on the NCI and the Centers for Disease Control and Prevention (CDC) to formalize and coordinate their internal efforts to study AYAs with cancer.
To improve the standards and quality of cancer care provided to AYAs, the Alliance for Clinical Trials in Oncology published a position statement on elements of such quality cancer care (Zebrack et al., 2010). In addition, the National Comprehensive Cancer Network recently published its recommended guidelines for the care of AYAs. There have also been efforts to recognize and support excellence in service delivery, including the Fertile Hope Centers of Excellence Program, which recognizes fertility preservation efforts. But there is a lack of coordination among these efforts, Hayes-Lattin stressed. There also is still a great need to define outcome measures of high-quality care for AYA patients and then study how the various models for AYA care are or are not facilitating those outcomes, he added.
Both the Alliance for Clinical Trials in Oncology and Critical Mass continue to expand their AYA work and to hold annual meetings aimed at fostering advocacy and support for AYAs with cancer. There have also been efforts among other medical and advocacy organizations, including a number of charities that have combined forces to develop the International Charter of Rights for Young People with Cancer.6
“Since 2006,” Hayes-Lattin said, “we have amassed a really impressive array of medical institutions and advocacy groups that focus on at least some components of the adolescent and young adult cancer issue. The next opportunity is for us to map in a detailed way what that network looks like to increase the reach of organizations that have a part and to also find what gaps exist.” Hayes-Lattin added that Critical Mass is currently attempting to fill that mapping and coordination role.
________________
6 See http://cancercharter.org (accessed October 8, 2013).
PSYCHOSOCIAL ASPECTS OF AYA CANCER DIAGNOSIS AND TREATMENT
As several speakers pointed out, young adults are at a unique stage in their emotional, cognitive, and social development, which cancer often disrupts. The attempts by these young adults to establish independence from their parents, to complete school, to enter the workforce with a desired career, to find a life partner, and to raise a family often are temporarily, or sometimes permanently, derailed (see Figure 2).
Bradley Zebrack, associate professor at the University of Michigan School of Social Work, said that a young person’s experience with cancer is often the first time that he or she has confronted mortality in general. “Many of them have not even experienced a grandparent who has died or
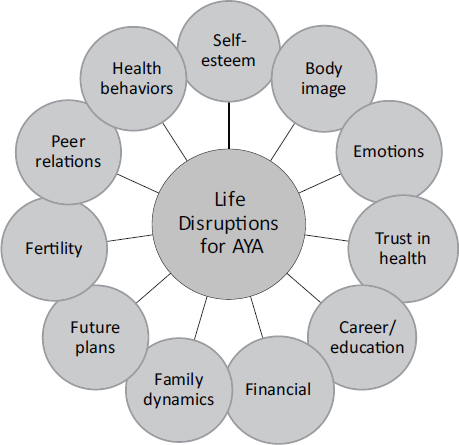
FIGURE 2 Possible life disruptions for AYA patients with cancer.
SOURCE: Fasciano presentation.
have been to a funeral,” he said. “These challenges to mortality come totally out of the blue, and they have limited experience in how to cope with these issues.”
Karen Fasciano, a clinical psychologist at the Harvard Medical School and director of the Young Adult Program at the Dana-Farber Cancer Institute, said that it is often the case that the demands of the young adults’ life-cycle stages go directly counter to the demands of their illness:
• When they want more intimacy with their peers and independence from their parents, and they want to feel like they are in control and invulnerable, the demands of their cancer make them feel isolated, vulnerable, dependent, and uncertain.
• When they want to feel part of a peer group and fit in, they feel isolated by the uniqueness of what they are experiencing.
• When they are developing their sexual identity, cancer treatment can influence sexual health and feelings of attractiveness.
• During a period focused on development of executive functions (i.e., planning, organization, mental flexibility, reasoning skills), cancer treatment can disrupt this development, and can impact educational and vocational attainment as well as decision making.
• When they are trying to make future plans, the future can seem elusive.
“Young people are really challenged with balancing the demands of illness with the demands of the life cycle,” Fasciano said, “and there can be some regression in development.” But she made a point of quoting a young adult cancer patient who gave this advice to fellow patients: “Don’t compare the beginning of your journey to the middle of someone else’s, and don’t feel like you are behind on anything or set back, because you haven’t taken a step back. You have moved onto a different path. Your life is different now.”
Patricia Ganz, Distinguished University Professor at the University of California, Los Angeles, Fielding School of Public Health and the David Geffen School of Medicine, and director of cancer prevention and control research at the Jonsson Comprehensive Cancer Center, stressed that young cancer survivors vary as to what their psychosocial needs are and that it is important to assess this in every patient rather than to treat the patients in cookbook fashion based on age assumptions.
Several participants pointed out that cancer disrupts family dynamics for AYAs. Often, a newly independent young adult may return home to live with his or her parents during cancer treatment. Although family support and cohesiveness is important in the adjustment to a cancer diagnosis and the associated life disruptions, Fasciano said, the different perspectives and expectations that family members can have may contribute to some distress. Many younger AYA patients may depend on parents for decision making, but for patients over 18 years of age, issues regarding guardianship and/or legal decision making may arise. Providers can help AYA patients and their families determine the role of the family in the patient’s care. “Providers can assess and help them define who is responsible for their care and discuss the responsibility of the family,” she said.
Zebrack said that not only are AYAs often concerned about parents being overprotective of them, but they may also be overprotective of their parents. “Maybe they have moved to completely different cities and go through the experience of cancer therapy on their own because they do not want to call Mom and Dad who are three time zones away and get them worried about it,” he said.
For AYA patients who already have children of their own, a cancer diagnosis and the burdens of treatment can be very disruptive to their family life and psychologically challenging for their children.
Disruption of School, Work, or Career Plans
Ruth Rechis, vice president of programs at the LIVESTRONG Foundation, described the results from an online survey7 conducted by LIVESTRONG in 2012, which found that most participants had to make some changes in their work life following a cancer diagnosis. Those changes
________________
7 Each of the surveys presented has strengths and limitations for assessing the experience of AYA patients with cancer, and each provides information on a different subset of the AYA population. For example, in the studies using large population based data (Medical Expenditure Panel Survey and Behavioral Risk Factors and Surveillance System), survivors were defined as those with a history of cancer diagnosed at ages 15~$@~8211;39 and the majority were longer-term cancer survivors. Other studies focused on individuals who are currently ages 15~$@~8211;39, and were recently diagnosed (including some with poorer prognosis and less likely to become longer-term cancer survivors). This is particularly relevant when considering differences in study results.
included taking time off, switching from full-time to part-time work, and changing to a less demanding job or to one with a more flexible work schedule. About three-quarters of the respondents also reported that their ability to perform mental or physical tasks and their overall productivity at work were affected by their cancer diagnosis. The percentage of respondents who reported these effects on their work was greater among AYA cancer survivors than among other cancer survivors.
In the same survey, more than one-quarter of respondents reported leaving school, about one-third reported that they had difficulty keeping up with school work, and a nearly equal number reported missing a large amount of school. Fifteen percent did not have any special services while they were in school, and many reported feeling that their classmates and teachers did not know how to support them.
The Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) Study focused more on what happened to AYA cancer survivors once they completed treatment (Parsons et al., 2012). This study surveyed AYAs who were in school or working when they were diagnosed with cancer and assessed how many were able to return to school or work between 15 and 35 months post diagnosis. The survey found that although most respondents felt cancer had an adverse impact on their schooling or work, most were able to resume school or work. Their employment rates were comparable to those of older adults diagnosed with cancer, although slightly less than the employment rates for their age group, reported Helen Parsons, assistant professor in the Department of Epidemiology and Biostatistics in the School of Medicine at the University of Texas Health Science Center at San Antonio. Those who quit working completely directly after their diagnosis were the least likely to return to work.
Another study based on the Behavioral Risk Factors and Surveillance System (BRFSS) sponsored by CDC compared AYA cancer survivors to same-age peers who had not had cancer (Tai et al., 2012). A significantly lower proportion of AYA cancer survivors reported being employed for wages, and a significantly higher proportion of AYA cancer survivors reported being out of work, said Eric Tai, medical officer for the Comprehensive Cancer Control Branch at CDC.
In addition, a study based on a large national survey, the Medical Expenditure Panel Survey (MEPS) sponsored by the Agency for Healthcare Research and Quality, evaluated employment and medical expenditures and found that the mean annual lost productivity for survivors of AYA cancers is more than double that of individuals without a cancer history (Guy et al.,
2013). These individuals were more likely to experience greater health-related unemployment and productivity losses, reported Robin Yabroff, an epidemiologist in the Health Services and Economics Branch of the Division of Cancer Control and Population Sciences at the NCI.
Others reported on what they called “job lock,” or the inability of cancer survivors to pursue a career of choice, often because of the need to keep their jobs and not go back to school in order to maintain employee benefits, including health insurance. “Although the data look good in that a large number of cancer survivors are working,” Ganz said, “they may not be working up to their potential and may have lost opportunities because of their cancer.” Yabroff concurred, adding, “It’s really important to not just think about whether they are currently employed but whether they would have had the same career trajectory if they hadn’t had cancer.”
The open-ended comments section of the AYA HOPE Study revealed a number of psychological stresses experienced by AYAs with cancer, including a fear of recurrence, concerns about managing their own distress and emotions as well as those of their parents and friends, and feeling burdened by the emotional responses of friends and family members when they told them they had cancer. Thirty-five percent of the AYAs indicated some kind of clinically significant distress at some point during the first 12 months after diagnosis. But Zebrack said that some respondents also noted positive life changes following their cancer diagnosis. For example, one person wrote, “It was a devastating experience, but it changed my life. I became more positive, more health conscious. I exercise more. But every day I think about it, and I seem very scared that it may return and I may not be strong enough to fight again.” Zebrack called this “the two faces of the cancer experience—both the elements of desperation and fear, but also of celebration and hope” and said it was reflected in a lot of the comments gathered in the study.
Zebrack described one study that found that the prevalence of psychological distress among AYAs with cancer varied over time following diagnosis (from 6 to 41 percent) but did not vary by the type of cancer or the prognosis (Kwak et al., 2013). The AYA HOPE Study found that 12 months after their cancer diagnoses, 41 percent of AYA cancer survivors reported an unmet need for counseling and other forms of psychosocial support.
AYAs frequently experience isolation along with their cancer diagnosis and treatment. Zebrack reported that the AYA HOPE Study found that many AYAs with cancer talked about their friends no longer calling them or dropping by or reported not having energy for those friends and maintaining their relationships. Sexual relationships are also difficult to maintain if cancer treatment affects an individual’s feelings of attractiveness or leads to sexual dysfunction. One cancer survivor who spoke at the conference said that her surgical scar and lack of hair made it hard for her to socialize. “I was so ashamed, and no one was there to help me figure out how to navigate that,” she said.
Zebrack added that social activity among younger AYAs often involves drinking alcohol, which is problematic for someone undergoing cancer treatment. Dating can be especially challenging, with many young cancer survivors struggling with decisions about when to reveal to potential romantic partners their health histories and how those might impact their long-term survival or ability to have children. “They have a fear of rejection,” Zebrack said. The Childhood Cancer Survivor survey (for those diagnosed between the ages of 0 and 21 years) found that cancer survivors were less likely to be married than their siblings who had never had cancer. Long-term, committed relationships can also be challenged following a cancer diagnosis.
The uniqueness of their cancer experience also can make AYAs feel as if they do not fit into their peer groups, which can contribute to their sense of isolation. As one AYA cancer survivor at the workshop said, “Now, when I go to a bar and people share their stories, they often seem kind of the same to me, and mine is a little different. It makes me stand out.” Another survivor said, “At 25 you are thinking about getting a job and getting married and having kids and buying a house. But when you are 25 and have cancer, you are not thinking about any of that. You are thinking, ‘I’m going to die, and this is going to suck, and how am I going to pay for this, and what am I going to tell my parents?’”
LATE AND LONG-TERM SIDE EFFECTS OF TREATMENT
Studies show that, because of their cancer treatments, many AYA cancer survivors are more likely to develop various chronic health problems than their peers without cancer. Many of these health problems develop
long after treatment has ended (see Table 1). Using data collected by its Behavioral Risk Factor System, the CDC found that, compared to people who have never had cancer, AYA cancer survivors have about double the prevalence of cardiovascular disease and are also at increased risk for diabetes, asthma, and hypertension. Furthermore, the prevalence of disability was twice as high in AYA cancer survivors as among those without cancer. Twenty-four percent of AYA cancer survivors reported having had 14 or more days of poor physical health in the previous month, which was double that seen among people without cancer.
The Childhood Cancer Survivor Study (CCSS) found that the age at diagnosis does not predict the degree of health conditions developed by a cancer survivor, reported Kevin Oeffinger, director of the Adult Long-Term Follow-Up Program in the Department of Pediatrics at Memorial Sloan-Kettering Cancer Center. This study found that almost half of childhood cancer survivors experience a serious or life-threatening condition or death between 5 and 30 years after diagnosis and that almost three-quarters develop at least one chronic condition (Oeffinger et al., 2006). Another study of adult survivors of childhood cancers found that by age 45, 96 percent of them had developed a chronic health condition and 81 percent had a severe or life-threatening condition, Oeffinger said (Hudson et al., 2013). The risk of developing a health condition increased over time.
Metabolic syndrome and cardiovascular disease are two common late effects of cancer treatment. Compared to healthy controls, survivors of testicular cancer are twice as likely to develop metabolic syndrome, even among those who are still relatively young men, Oeffinger reported. Studies suggest that the increased risk might stem from having received cisplatin and bleomycin chemotherapy, which can damage the lining of blood vessels and start an inflammatory reaction that results in cardiovascular disease. Patients who have had brain tumors also have metabolic disturbances that increase their risk of both cardiac disease and strokes. Cardiac disease risk is also increased in patients who have been treated with anthracyclines, such as doxorubicin. According to Oeffinger, almost all women who undergo total body irradiation prior to a stem cell transplant during adolescence or the young adult years will develop metabolic syndrome and have a higher risk of developing heart disease, despite often being thin. These women often lose their subcutaneous fat but have increased visceral fat.
Bernard Fuemmeler, associate professor of community and family medicine, psychiatry and behavioral science, and psychology and neuroscience at the Duke University Medical Center, also reported on studies that
TABLE 1 Potential Late Effects of Cancer Treatment, by System and Exposure
| System | Exposures | Potential Late Effects |
| Cardiovascular | Radiation therapy | Myocardial infarction or stroke |
| Anthracyclines | Congestive heart failure | |
| Platinums | Valvular disease | |
| Hypertension | ||
| Pulmonary | Radiation therapy | Restrictive lung disease |
| Bleomycin | Pulmonary fibrosis | |
| Carmustine/Lomustine | Exercise intolerance | |
| Renal/urological | Radiation therapy | Renal insufficiency or failure |
| Platinums | Hemorrhagic cystitis | |
| Ifosfamide/Cyclophosphamide | ||
| Endocrine | Radiation therapy | Obesity |
| Alkylating agents |
Infertility and gonadal dysfunction |
|
| Dyslipidemia | ||
| Insulin resistance and diabetes | ||
| Central nervous | Radiation therapy | Learning disabilities |
| system | Intrathecal chemotherapy | Cognitive dysfunction |
| Psychosocial | Cancer diagnosis |
Affective disorders (anxiety, depression) |
| Posttraumatic stress | ||
| Sexual dysfunction | ||
| Relationship problems | ||
|
Employment and educational problems |
||
| Insurance discrimination | ||
|
Adaptation and problem solving |
||
| Second | Radiation therapy | Solid tumors |
| malignancies | Alkylating agents | Leukemia |
| Epipodophyllotoxins | Lymphoma | |
SOURCE: Adapted from Oeffinger presentation.
showed survivors of childhood cancers, especially those with leukemia, or those treated with high-dose radiation, were more likely to be obese (Meacham et al., 2005; Oeffinger et al., 2003; Tai et al., 2012). The CCSS found that having cranial radiation therapy, being diagnosed at a younger age, or being female boosted the risk of developing obesity. One study of children with ALL found that 23 percent were obese by the end of their treatment, compared to 14 percent who were obese at diagnosis (Withycombe et al., 2009). Another study found that male survivors of childhood cancers had body mass indices similar to those of their siblings but that they had greater trunk fat and total body fat (Miller et al., 2010). “These studies cause concern that during that year of treatment, children are not being as active as they usually are and so are losing the opportunity to gain lean muscle mass,” Fuemmeler said. Unfortunately, there are few data regarding these late effects among survivors of AYA cancer.
Cancer survivors are also at risk for secondary malignancies (see Table 1). Survivors of Hodgkin’s lymphoma (HL) have a particularly high risk of developing another cancer, Hayes-Lattin said. A study by Hodgson (2011) found that the risk of developing another malignancy increased by more than 1 percent per year (see Figure 3). The risk varied depending on what age the HL diagnosis was made. “Although many of our Hodgkin’s lymphoma patients have little morbidity at the end of their treatment, about 16 percent that we follow have gone on to develop three or more major primary cancers,” Oeffinger said. Because of that, oncologists are now frequently opting to treat HL patients with a chemotherapy that goes by the acronym ABVD (containing adriamycin, bleomycin, vinblastin, and dacarbazine) instead of an older chemotherapy regimen called MOPP (containing mustragen, oncovin [aka vincristine], procarbazine, and prednisone) because the former has a reduced risk of morbidity and late effects.
Breast cancer is particularly prevalent among survivors of childhood HL who were treated with chest radiation. One study found that 35 percent of women with HL who received chest radiation developed breast cancer by age 50, compared to 31 percent of women with mutations in the BRCA genes and 4 percent of controls. The younger the women were when they received the radiation therapy and the higher the dose of radiation they received, the more likely they were to develop breast cancer. Risk tapers off in those who were 35 years or older when they received the treatment. The interval between chest radiation and the development of breast cancer is usually between 10 and 20 years. Bilateral breast cancer is also more common in women who received chest radiation. “It is overwhelming how fre-
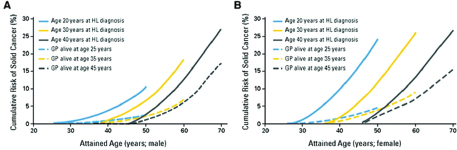
FIGURE 3 Cumulative incidence of solid cancers among 5-year survivors of Hodgkin’s lymphoma (HL) compared with controls of the same age in the general population (GP).
NOTE: A = males, B = females.
SOURCES: Hayes-Lattin Presentation; Hodgson et al.: Journal of Clinical Oncology 25(12), 2007:1489–1497. Reprinted with permission. © 2007 American Society of Clinical Oncology. All rights reserved.
quently we see bilateral disease, and we need to be very proactive with that,” said Oeffinger. He added that survival following a breast cancer diagnosis is linked to the stage of the cancer at diagnosis, just as it would be for someone without a prior cancer diagnosis, and that the hormone receptor status of the breast tumors in HL survivors is similar to that among the general population. By contrast, radiation to the ovaries lowers breast cancer risk, presumably by lowering estrogen exposure.
INFERTILITY AND EFFORTS TO PRESERVE FERTILITY
Now that so many cancers diagnosed in children and AYAs are curable, there has been growing concern about how cancer treatment might affect their fertility and about ways to preserve that fertility. Jennifer Levine, assistant professor of clinical pediatrics and director of the Center for Survivor Wellness in the Division of Pediatric Oncology at Columbia University Medical Center, said that the American Society of Clinical Oncology (ASCO), the American Society of Reproductive Medicine, and the National Comprehensive Cancer Network have all developed guidelines that state that fertility preservation should be an integral part of cancer treatment for AYAs. One participant said, “I think it has gone from ‘I hope my doctor thinks about my fertility’ to a mandate, and hospitals like mine have policies
in place so they provide information about the risk of infertility and offer potential preservation options.”
The 2010 AYA LIVESTRONG survey found that about one-quarter of AYAs took steps to preserve their fertility before their cancer treatment began. The most common steps taken were sperm banking for men and preserving eggs and embryos for women. Sixty-five percent of males who tried to father a pregnancy after treatment were successful, while 58 percent of females who tried to become pregnant after treatment were successful. The majority of those with successful pregnancies used natural means to become pregnant, Rechis reported.
The survey also assessed the reasons for not using fertility preservation and found that although some people were not interested in having children, many did not know their fertility was at risk, did not have enough time to pursue fertility preservation options, or thought the costs of such preservation were too prohibitive. “These are all things we can affect and make a change for AYA survivors,” Rechis said. Oeffinger agreed and said that there are psychological reasons to preserve fertility. “Infertility is the number one issue of our patient population because it ties into their body image, their sense of self-worth,” he said.
Levine provided some background information on the biology of fertility and then outlined the causes of infertility in cancer patients. In males, the germ cells start maturing into sperm cells at puberty, and in a healthy male, who is generally fertile from puberty until time of death, they continuously self-renew. Cancer treatment can deplete these germ cells. Levine said that it is very common for males to experience a temporary lack of sperm during or after radiation or chemotherapy because of both the destruction of maturing sperm cells and a relative depletion of germ cells. The maturation process can resume post-therapy, and the amount of time that a male is infertile after treatment varies from months to years. Ultimately, males usually become fertile again, but permanent infertility can occur if there is such a sufficient depletion of germ cells that there is no possibility of the maturation process resuming.
Cancer treatment or surgery can also cause infertility by damaging the pituitary gland, the pelvic nerves, or the ductal system, which can interfere with ejaculation. Sometimes it is the cancer itself and not necessarily the treatment that affects male fertility. Men with testicular cancer or HL will
sometimes lack viable sperm prior to treatment because of the effects of the disease process itself, Levine said.
Sperm banking is a well-established means to preserve male fertility. If viable sperm are produced, those sperm are frozen and stored for future use. It is generally recommended that men produce several specimens over the course of a number of days in order to maximize the volume of the sperm that can be stored. But it is possible that just one specimen will be sufficient for future fertility, Levine said. “There often is a lot of pressure to begin therapy, and people feel uncomfortable delaying the start of therapy to allow sperm banking,” she said. “But if sperm banking is thought of at the time of diagnosis, there may be time to produce multiple specimens before treatment starts.”
The cost of sperm banking can be a challenge for some patients. It costs between $500 and $700 to do a semen analysis, and annual storage costs range between $200 and $400. Fertile Hope’s Sharing Hope Program8 enables cancer patients to get discounted rates for sperm banking, Levine said. However, some patients may be too sick or too young to bank sperm at the time of diagnosis, and some may decline due to religious beliefs, she said.
If producing an ejaculate is a problem, sperm can be collected under anesthesia. This outpatient procedure is becoming more common, Levine said. Another option is to remove testicular sperm tissue and freeze it or to freeze an entire testicular specimen that includes germ cells which will be matured at a later point in time. Such testicular extraction can also be attempted post therapy as a more targeted means of acquiring viable sperm for assisted reproduction. In males receiving radiation therapy, gonadal shielding is also a common procedure to help preserve their fertility.
“Almost any post-pubertal male who is willing or interested in sperm banking should do it because it is really not so invasive,” Levine said. The earlier that men bank their sperm the better, she stressed, because even men with a lower risk for infertility might relapse in a period of time in which they are not producing sperm due to their previous therapy, so they won’t be able to bank sperm at that point. Levine said that although many patients may not require sperm banking, for the 10 or 15 percent of men who end up using banked sperm, “that is how they are going to start their biologic family.” She added that men can undergo a semen analysis for viable sperm
________________
8 See http://www.fertilehope.org/financial-assistance/index.cfm (accessed October 8, 2013).
post treatment to aid their decision about whether to continue to pay for sperm storage.
A woman’s fertility can be affected by a number of actions related to cancer treatment. Removing a woman’s ovaries or her uterus will render her infertile. Uterine surgery can cause scar tissue that may prevent implantation of the embryo. And cancer treatments, including treatments that affect the pituitary, can cause infertility by disrupting normal hormonal regulation. Unlike men, women are born with all the eggs they will ever have, and there is no self-renewal of germ cells. At menarche, women start to lose their egg follicles, and by their mid- to late 30s, their fertility begins to decline. By their late 40s or early 50s, most women reach menopause and can no longer become pregnant.
Cancer treatment can cause acute ovarian failure, in which the number of follicles drops down to levels that impede fertility, and it can hasten menopause. Oeffinger presented a study that found that the older a woman is when she is diagnosed with cancer, the more likely it is that she will experience infertility from her cancer treatment (Letourneau et al., 2012). Nearly half of women treated at age 35 for cancer experience infertility. “In our country, with so many women moving the timing of their family to later years, this obviously is quite an important issue,” he said. Cancer treatments lead some women, especially those treated with high-dose alkylating-agent chemotherapy and those who undergo a stem cell transplant, to experience early menopause. Even women who resume menstruation after chemotherapy can experience infertility. Premature menopause can also lead to sexual dysfunction.
Embryo freezing is the most common method for preserving the fertility of women undergoing cancer treatment, Levine said. This technique requires ovarian hyperstimulation in order to create multiple follicles in the ovaries. The follicles are retrieved prior to ovulation and fertilized to create embryos that are then frozen. The older a woman is when she has the procedure, the less likely is it to be successful. Embryo preservation requires a partner or donor sperm, and is very expensive, costing between $10,000 and $15,000, not including implantation costs. Embryo preservation takes a minimum of 2 weeks.
Oocyte cryopreservation is similar to embryo preservation except that it does not require fertilizing the egg and thus does not require a partner
or donor sperm. Last fall, the American Society of Reproductive Medicine deemed that this approach is no longer an experimental procedure. “It really is something that in general we are thinking more about for our patients,” Levine said, but she noted that oocytes are more susceptible to being damaged by the freeze-thaw cycle than embryos, so the success rate for this procedure is somewhat lower than for embryo preservation. It is just as expensive and requires just as much time, she added.
Another option is to remove ovarian strips, freeze them, and reimplant them later or use them for in vitro fertilization. This procedure can be done immediately and it is the only option for pre-pubertal females. But it is controversial because of the concern that cancer cells, particularly leukemia cells, might be reintroduced with the re-implanted tissue. There also is not much experience reported in the literature, with only about a dozen pregnancies known to have resulted from it, Levine said.
Some patients with cervical cancer are now being treated by removing only part of the uterus and cervix, Levine said; it is possible for these women to carry a pregnancy. In patients who receive radiation therapy, the ovaries can be protected with gonadal shielding and ovarian transposition, in which the ovaries are moved outside of the radiation field. Gonadotropin-releasing hormone agonists and antagonists are also commonly used to try to preserve female fertility, Levine said, although there is very little evidence to support that approach, and some studies suggest it may actually be detrimental to fertility.
Women may also want to consider pursuing similar actions to preserve fertility after their cancer treatment if they are not ready to have children at that time. Although there are tests that could potentially assess a woman’s fertility, these are not yet adequate or fully validated, Levine said. The CCSS generated promising data indicating that survivors are able to become pregnant, although it appeared that they took longer than their sibling controls.
Once a woman has completed her cancer treatment, she can pursue natural, assisted, or surrogate reproduction, although the possibility of a cancer relapse occurring during the pregnancy must be taken into account, as the pregnancy will limit the treatment options and timing. It is also possible that various late effects of treatment, such as cardiovascular or pulmonary impairments, could affect a pregnancy; these, too, must be taken into account. As Levine noted, such impairments can pose problems during pregnancy, when there is increased blood volume, and their presence may indicate the need to be seen by an obstetrician who specializes in high-risk pregnancies.
There are no data to suggest that children of cancer survivors have any increased risk of congenital abnormalities compared to the general population. But cancer survivors might have a genetic disposition to cancer that could be screened for with pre-implantation genetic diagnosis. Such a procedure can identify, for example, embryos that carry a mutated BRCA gene, Levine pointed out.
Levine suggested that providers discuss fertility with AYA patients at the time of their cancer diagnosis and give them a referral to have a more in-depth consultation with a reproductive endocrinologist if they wish. Fertility preservation should also be considered post treatment if it was not considered before treatment. Levine also suggested having an established referral mechanism in place related to fertility preservation. “If someone comes in saying they want a sperm bank, and you do not know where there is one or what kind of specimen jar to give them, fertility preservation is not likely to happen,” she noted.
Insurance Coverage of Fertility Preservation and Treatments
Not all insurance plans will cover the cost of fertility preservation or infertility treatment for cancer patients. One AYA cancer survivor who spoke at the workshop said that such coverage is critical. After her treatment, she said, she stopped menstruating and sought treatment with testosterone pellets, which cost $500 and were not covered by her insurance. Due to a flexible spending program at her job, she was able to pay for the treatment and subsequently started having normal menstrual cycles. “For 5 years,” she said, “I was menopausal and thought I would never have kids, which is a big emotional toll for a female at the age of 25, and if I hadn’t had money to pay for the testosterone treatment, I never would have tried it.”
Levine noted that LIVESTRONG has been encouraging insurance companies to cover the cost of fertility preservation for cancer patients and that the American Medical Association recently stated that insurance companies should cover fertility preservation in cases where the infertility is expected to occur as a result of cancer treatment. In addition, the California legislature recently introduced a bill to require insurance companies to cover fertility preservation. “If coverage can be obtained, this is going to make a tremendous difference for cancer survivors,” she said.
ONCOLOGY CARE ISSUES UNIQUE TO AYAs
As several speakers pointed out, there are a variety of oncology care issues unique to AYAs, including whether the patients should receive care from pediatric or adult oncologists, how they should transition from pediatric care to adult care, and how extensively their families should be involved in their care. There are also unique biological developmental issues that come into play in adolescents with cancer, and Melissa Hudson stressed that these issues must be considered when devising the patients’ treatment and follow-up care plans. She noted that these individuals are experiencing changes in body composition and rapid periods of growth in which their height and weight are increasing. AYAs also have various health behaviors and needs that are different from children or older adults with cancer, such as use of contraceptives, that may affect cancer treatment. “All these factors present to us unique biologic differences that may affect outcomes that should be considered in the evaluation of these patients,” she said.
Depending on age and specific diagnosis, AYA patients with cancer may be treated at either a pediatric cancer center or an adult cancer center, but often, these patients do not clearly fit into either treatment setting. The majority of patients are treated at an adult cancer center. The AYA HOPE Study found that only 2 percent of AYAs surveyed were treated at a pediatric hospital and only 5 percent saw any pediatric specialists. When only AYAs under the age of 25 were considered and those with early-stage male germ cell cancers were excluded from analyses, only one-quarter of the remaining patients saw a pediatric specialist for their cancer, reported Lynn Harlan, epidemiologist in the Health Services and Economics Branch of the Division of Cancer Control and Population Sciences at the NCI. If care is provided in an adult community oncology practice setting, patients may not have access to specific AYA-focused programs, and care providers may be less knowledgeable about the unique AYA developmental, psychosocial, and treatment needs, as the majority of cancer patients in the United States are over the age of 65.
One study compared Ewing’s sarcoma AYA patients who received the same treatment but in different settings (Albritton et al., 2004; Paulussen et al., 2003). This study found that patients were likely to survive longer if they were treated in a pediatric setting than if they were treated in an adult
setting, Hayes-Lattin reported, although no reasons were given to explain the findings.
Several AYA cancer survivors at the workshop spoke about how they decided whether to seek pediatric or adult care for their cancers. Hollie Farrish was diagnosed with Wilms’ tumor at the age of 25 after submission of pathology samples for a clinical trial revealed that the tumor, originally thought to be a renal cell cancer, had been misdiagnosed. Her oncologist had no experience with Wilms’ tumors but agreed to care for Farrish in consultation with a nearby children’s hospital. The oncologist made slight adjustments to the Children’s Oncology Group (COG) protocol to take into account the fact that children are more resilient than young adults. The treatment was successful, and Farrish said she appreciated the care she received. “I really liked my adult oncologist and wanted to be cared for by someone I trusted and liked rather than getting punted to a children’s oncologist at the age of 25.” She added, however, that neither a pediatric nor an adult oncology setting was quite appropriate for her. “It was either Dora the Explorer or AARP Travel and Leisure in the waiting room,” she said. “At 25, you are trying to go to Key West for spring break; you don’t want to be going for chemo at Children’s Hospital.” Benjamin Rubenstein, another AYA cancer survivor, decided to continue in the care of the pediatric oncologist who had started treating him when he was 16 because he trusted her and wanted to continue their relationship. “I am very loyal to my doctor because she understands all the treatment we did that affects me in so many different ways. I am going to stick with her until I get tired of playing with puzzles in the waiting room. I may be the first 50-year-old to still be in a pediatric center,” he said.
David Freyer, director of the Long-Term Information, Follow-Up and Evaluation (LIFE) Cancer Survivorship and Transition Program at Children’s Hospital Los Angeles (CHLA) and professor of clinical pediatrics in the Keck School of Medicine at the University of Southern California, explained that the transition from pediatric to adult care is especially critical for AYA cancer survivors because not only do they need to have more developmentally appropriate care, but they also need extensive follow-up and cancer surveillance by a physician who is aware of the likely chronic conditions and other late effects they are likely to develop from treatment and the risk-based monitoring they need to have.
Unfortunately, studies suggest that this transition is not as seamless as it should be and that many AYA cancer survivors are not receiving adequate follow-up care. The CCSS found that although most respondents had had a general exam within the previous 2 years, less than half had had a cancer-related visit, and 30 percent or less had had a visit at a cancer center (Oeffinger et al., 2004). Another study of the same survivors found that only 14 percent were undergoing general survivorship assessments and only 18 percent were getting the recommended risk-based assessments (Nathan et al., 2008). In addition, in a subpopulation of patients at risk for cardiomyopathy because of anthracycline exposure, within the previous 2 years only 28 percent had had echocardiograms. Only 41 percent of the women at risk for breast cancer had had mammograms.
Freyer listed a number of barriers to health care transitions for patients, providers, family members, and health care systems. Focus groups and small studies find that these survivors often do not seek out appropriate followup, in part due to their geographic mobility or to being unaware of what care is needed. One barrier often cited by these patients, Freyer said, is that they do not know their new providers and do not have a relationship with them as they did with the pediatric oncologists who initially treated them. Parents of adolescent cancer survivors tend to be overprotective and are used to navigating their children’s health care. These family caregivers may also be hesitant to have their children switch to new providers with whom they do not have a prior relationship.
Among primary care providers, Freyer said, studies find a lack of relevant knowledge and experience or comfort level with the AYA cancer patient population and sometimes even an unwillingness to take care of these individuals. “There is some reluctance on the part of these primary care providers in particular to take on the care of these medically complicated patients who they do not know and in the context of a very busy primary care practice that may have difficulty accommodating them.”
Oncologists have their own set of barriers to providing the appropriate transition to survivorship care. Brenda Nevidjon, clinical professor and specialty director of nursing and health care leadership at the Duke University School of Nursing, said that medical oncologists often do not refer their patients to survivorship clinics because they have developed a bond with these patients and want to have the positive experience of seeing them do well. Freyer agreed and added that this behavior does not serve the best interests of the survivors if it interferes with them getting appropriate survivorship care. One study found that pediatric oncologists had low levels
of knowledge of appropriate risk-based screening and survivorship care for a hypothetical female HL patient who had received radiation therapy and anthracyclines. Freyer suggested that as the new generation of oncologists in training become more familiar with survivorship programs, they will be more likely to refer their patients to them.
On the health care system level, there are a variety of impediments to effective care transitions. Cancer patients often lose health insurance coverage, for example, which is a major impediment to follow-up care. There are few seamless referral networks linking treatment centers with survivorship care providers that could aid in care transitions, and medical training generally has little coverage of survivorship care. Another barrier to making the health care transition is a lack of trust on the part of providers. “Pediatric providers need to trust that our adult colleagues will be able to care for these patients appropriately,” Freyer said, “but there is also a need for converse acceptance of responsibility.”
Freyer said that there are currently three basic models for the health care transition: continued care at the original cancer center, care transferred to a primary care community physician, and hybrid care in which care is transferred to community care but with support from the cancer center. For the model in which care is transferred to the community, Rechis said, there is an excellent resource to support primary care physicians providing followup care to AYA cancer patients. The educational program Focus Under 409 has a survivorship module that was created by a partnership between ASCO University and the LIVESTRONG Foundation.
Hudson noted that St. Jude’s Children’s Cancer Center uses another type of hybrid survivorship program in which the original treating physician often consults with physicians in their survivorship care program. Freyer noted that the same type of shared care occurs at CHLA. “The model we use in our institution does not require complete referral and loss of the patient to the cancer survivor program,” he said, adding that many patients are transferred to the survivor program within 2 years of ending therapy rather than the traditional period of 5 years from diagnosis. Consequently, many of these patients in the survivorship program are still on disease-directed follow-up and need scans for disease monitoring, which is not done in the survivorship program. “And if there is an oncologist who really feels it is essential to keep seeing the patient once a year, they are perfectly free to
________________
9 See http://university.asco.org/focus-under-forty (accessed October 8, 2013).
do so and we encourage it if that is what the patient and physician both want,” he said.
Freyer suggested that additional models are needed for transitioning adolescents into adult survivorship care, and he proposed providing tiered care to AYA cancer survivors based on their long-term risks, with the type and intensity of required follow-up differing by group because some patients are at higher risk than others. In the United Kingdom, for example, cancer survivors are subdivided into three different risk groups based on their treatment exposures. These groups are followed by a specialized center, by a primary care physician, or by mail (Eiser et al., 2006). At CHLA, patients are divided into two risk groups based on their treatment exposures and transition to appropriate care at age 21 (see Figure 4). Those with the lowest risk are assessed each year in person by their primary care physicians and virtually by CHLA’s LIFE Cancer Survivorship and Transition Program. Those in the high-risk group are assessed annually at the LIFE Clinic for Adult Survivors. This pilot program will also accept patients from the University of Southern California Comprehensive Cancer Center’s AYA and
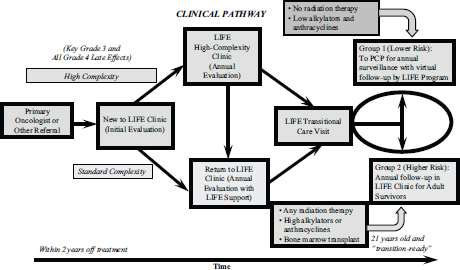
FIGURE 4 LIFE Cancer Survivorship and Transition Program at Children’s Hospital Los Angeles.
NOTE: LIFE = Long-Term Information, Follow-Up and Evaluation; PCP = primary care physician.
SOURCE: Freyer presentation.
adult survivor programs. “This will offer a lot of opportunity for clinical efficiency and resource sharing as well as research,” Freyer said.
Unlike caregivers for older patients with cancer, most caregivers for AYA cancer patients are parents. The LIVESTRONG online survey found that 82 percent of respondents reported that their parents were their primary caregivers; by contrast, 36 percent of those between 40 and 59 and 3 percent of those older than 60 report their parents as their primary caretakers. About half of the AYAs surveyed reported that their caregivers had to make changes to accommodate their care for a period of at least 2 months; the changes included taking time off of work, switching between full-time and part-time work, and retiring early. “These family members are making changes in their careers and may be the ones that are lending money to pay for the care, so they are definitely being impacted by this cancer diagnosis as well,” Rechis said. “We need to be cognizant of these family members that are supporting AYA cancer patients.”
Communications with AYA Patients
Jacqueline Casillas, director of the University of California, Los Angelese (UCLA) Pediatric Cancer Survivorship Program, Medical Director the UCLA Daltrey/Towshend Teen and Young Adult Oncology Program, and associate professor of pediatric hematology and oncology, spoke about the various factors that health care professionals need to be cognizant of when communicating with AYA patients. For example, health care professionals need to be cognizant that their communication style is AYA age appropriate and emphasizes patient empowerment. Use of diverse channels of communication, such as videos or text messaging, is also important for consideration in this age group. The inclusion of parents and other family members or care givers in the communication channels may be important cultural considerations for diverse groups of AYA cancer patients. Casillas stressed that because a cancer diagnosis often disrupts independence and leads to a young adult living with his or her parents while receiving their cancer care, the traditional patient-doctor dyad may not always be the best way to think about communications. Rather, a patient-doctor-parent triad may be necessary. “The parent may need to be involved in those discussions
about what should be done to promote the health of the AYA patient,” she said.
The degree of involvement of family members in patient communications may differ among ethnicities, Casillas added. For example, her study found that Latino AYAs are more likely to report the need to talk about their cancer care with their families. “Even people who were 35 said they still go back to their family members to help guide them on the type of care that they need,” she said. A major conclusion from her study was that it is critical to include the Latino nuclear family in survivorship care discussions. The study also found that it is critical to include information about health insurance options in a discussion about survivorship care. “The community felt that if we’re not telling them how they can get access to survivorship care, then we shouldn’t be trying to educate them about it,” Casillas said.
Justin Baker, chief of the Division of Quality of Life and Palliative Care at St. Jude Children’s Research Hospital, said that AYA compliance with medications and procedures can become a battleground as the young patients assert their independence. The proper response, he suggested, is not rigid discipline but rather flexibility with firmness, which builds trust and confidence. In other words, he said, the health care provider should think in terms of partnering, not paternalism.
Casillas described an in-depth qualitative focus group study conducted by Bradley Zebrack in young adults with cancer. This study indicated that patients found it helpful when the provider answered questions, but they considered it hurtful if the provider delivered information in a patronizing manner. This study also found that many AYAs want positive attention and support for feeling more like a normal person again. Consequently, when they are told in a survivorship clinic that they need to maintain a healthy body weight and exercise regularly, they may ask why they are being singled out for healthy behavior that everyone should follow. To respond appropriately, Casillas suggested that care providers put things in context by saying something like, “Yes, we all need to do a good job at this, but there may have been specific treatment exposures that may put you at greater risk, so having a strong healthy heart through regular exercise and healthy eating can be even more important.”
Both written and oral communications are important in fostering appropriate survivorship care, Casillas said. One study that she conducted found that having a written survivorship care plan was associated with AYA cancer survivors being more likely to report that they could actively manage their survivorship care. “Having such a care plan somehow prepares
survivors to be more self-assured about being their own health advocates,” she said. Given how mobile AYAs tend to be and how they tend to get treatment in different health care settings, a written care plan that they can pass on to new providers is especially helpful, Casillas said. “Survivors often say that it is exhausting to have to tell their story over and over again,” she said. Her study also found that ethnic minorities were more likely to report a lack of confidence in managing their survivorship care, and she stressed the importance of addressing language barriers and low levels of literacy among cancer survivors and their families.
Online outreach can also be a valuable way of providing peer social support to AYAs with cancer. “Social media has great potential for enhancing psychosocial support for AYAs,” Zebrack said. Farrish added, “As far as how to reach out to the AYA population, social networking is really a giant—Facebook, Twitter, YouTube, etc.” For example, she recently posted on Facebook that she got good results on her annual check-up and celebrated 8 years of being cancer-free. “That opened up a lot of doors for a lot of friends,” she said, as friends and friends of friends responded to her post, including those who were recently diagnosed with cancer themselves, and asked if they could speak with her. “It is amazing how far-reaching Facebook and Twitter are,” she added. “I became friends with people I did not really know that well just because they have cancer and I have cancer. It is very beneficial.” She and another AYA cancer survivor also noted that meeting people with cancer through social media sites paved the way for them to form or participate in an in-person cancer support group. Another participant noted that that the Dana-Farber Cancer Institute has a website for young adult patients that fosters peer support and that could be emulated by other centers across the country.
UNMET NEEDS OF AYAs WITH CANCER
Several workshop participants stressed that in addition to their unique medical care needs, AYAs with cancer have a number of informational and psychosocial needs that programs aimed at pediatric cancer patients or older adults with cancer often do not address. These needs include information about their disease, support groups for their age group, preventive health care and fertility preservation, and health insurance. AYAs with cancer also often need financial, practical, and peer support as well as counseling and coping strategies.
Harlan reported that more than one-third of the participants in the
AYA HOPE Study reported an unmet need for service; 16 percent said they needed help with financial planning related to health care; 15 percent needed mental health counseling to address a need that was not met; and 14 percent said they had unmet needs for a support group. More than half of these patients reported six or more unmet information needs, the most common being the need for information about how to handle their concern about getting another cancer. Similarly, in a study using the national MEPS survey data, survivors of AYA cancer were more likely to be unable to get or delayed getting necessary medical care than similar individuals without a cancer history (17.0 percent vs. 12.7 percent).
The CCSS and others have documented “a serious lack of important knowledge that is health related and includes what the previous diagnosis was as well as elements of cancer treatment they have received, what their current state of health and health risks are, and what disease prevention and wellness practices they should follow,” Freyer said. “Many of these survivors really crave knowledge about what their health risks are, what is likely to happen to them, and what they can do to help themselves. If they are not accessing that information by follow-up, they are missing out.”
Zebrack’s unpublished study of AYAs with cancer found that at 12 months after diagnosis, 57 percent indicated that they wanted or needed information not just about their cancer but also about long-term followup, including information about diet and nutrition and fertility. Forty-one percent reported an unmet need for counseling, and 39 percent reported unmet practical support needs such as assistance with health insurance, transportation, and child care. Zebrack noted that a 2010 National Health Interview Survey of 1,177 survivors of adult-onset cancer found that 90 percent reported the reason they were not getting their psychosocial care needs met was because they did not know what services were available to provide them (Forsythe et al., 2013).
“It’s important to pay attention to these psychosocial needs,” Zebrack said, “because they may influence outcomes by affecting adherence to treatment, completion of therapy, and quality of care received.”
Zebrack also stressed the importance of providing peer support to AYAs with cancer. Although people of all ages with cancer need peer support, such peer support is especially critical for AYAs, he said, because of their developmental stage. AYA cancer survivor Chris Prestano concurred, saying, “It’s different for young adults. In my first support group for people with head and neck cancer, I was the same age as these people’s grandkids and great grandkids and half the age of the facilitator.” She finally found a young
adult support group on her own via an Internet networking site called Stupid Cancer.10 “Stupid Cancer focuses more on socializing,” she said. “They do not meet in hospital settings but in restaurants or movie theaters, and sometimes cancer is talked about, but sometimes not.”
Farrish said that the nurses caring for her who were her age provided the peer support she needed. “They turned out to be a bigger support group than the support group I had to attend,” she said. “It is extremely important at our age of diagnosis to have somebody to turn to, to talk about things that are difficult to talk about with your 60-year-old oncologist.”
Rubinstein added, “I seek support in unique ways. I just do not call it support. Social gatherings are the way to do it, or adventure trips, like those offered by First Descents,11 an organization that sends young survivors on free trips. If I had been offered the opportunity to hang out with other cancer survivors at a Redskins game or the movies, I think I would have done it.”
AYAs with cancer also need information on health insurance and other financial support mechanisms. The CCSS found that many insured survivors had difficulty both obtaining health insurance and using it. Most had a lack of knowledge about what their insurance would cover and expressed a willingness to attend an educational program to learn about their health insurance coverage and rights, reported Elyse Park, associate professor of psychiatry at the Harvard Medical School Mongan Institute for Health Policy.
Farrish said that she was working at the time of her cancer diagnosis and went on short-term disability because her treatment plan was so intense. But in order to acquire the long-term disability she needed, she was told she had to file for Social Security disability by filling out an onerous amount of paperwork. “It was exhausting, and it took two-and-a-half months just to get my application submitted, and then they asked for more information,” she said. It took 3 or 4 months of filling out and filing forms until she received Social Security, and then she had it for only a couple of months. “Having a financial counselor would have helped greatly and probably saved me a month in trying to fill out this paperwork and provide the required documentation,” Farrish said. “Young people do not know what Social Security is and how you ask for it, so it is important that somebody help them with this.”
________________
10 See http://stupidcancer.org (accessed October 8, 2013).
11 See http://firstdescents.org (accessed October 8, 2013).
Screening/Surveillance for Cancer in AYA Survivors
There was much discussion about the appropriate screening and surveillance for cancer in AYA cancer survivors. Patricia Ganz stressed the importance of this aspect of care, noting that because the survivors are relatively young, early detection of recurrence or secondary cancers can save AYAs many years of life. “This is a group of individuals who have a long life ahead of them,” she said, “and cancer and these other chronic conditions are their main threats—they have very few competing causes of death. So detecting and treating recurrence and secondary cancers will have a high value in this group.”
Ganz and other speakers suggested tailoring surveillance for cancer recurrence based on each patient’s risk factors. Rapidly growing tumors require more frequent monitoring than more slowly growing tumors, Ganz said, and tumors more likely to recur locally will require a different type of monitoring than those more likely to recur systemically. “The surveillance strategy should be tailored to the type of tumor and its pattern of relapse and recurrence,” she said.
Ganz also stressed, however, that there is a paucity of research findings that can help guide practitioners concerning what surveillance for cancer is appropriate. Two reviews of the evidence concerning breast cancer surveillance found no difference in survival outcomes for women who had routine clinical office visits and mammograms versus women who had more intensive monitoring with blood work and imaging tests (Khatcheressian et al., 2013; Rojas et al., 2005). In her own practice, Ganz said, recurrences of breast cancer have rarely occurred without the patient being symptomatic.
Despite numerous doctors ordering tests for tumor markers in breast cancer, randomized controlled trial data indicate that such tests provide no value in follow-up care, Ganz said. “The rate of false-negative or false-positive findings is not known,” she said. In addition, normal or abnormal tumor marker results can contribute to false reassurance or increased anxiety for patients and can lead to unnecessary medical evaluations. “All you need to do is get a little rise in one of these tests, and a woman is on a tailspin of having positron emission tomography (PET)/computed tomography (CT) scans, magnetic resonance imaging (MRI), etc., and somebody will see a little something on the CT or MRI and say we need to follow that up when it is really nothing,” she said.
Data on the value of imaging tests for breast cancer recurrence is also sparse, Ganz said. Chest and abdominal CT scans or whole body PET
scans have not been evaluated as surveillance strategies for the follow-up of early-stage breast cancer. With the low prevalence of distant recurrence in early-stage breast cancer and the high risk of false-positive and incidental findings, there is no evidence to support the use of routine imaging tests, she said. She pointed to a recent recommendation from ASCO for the Choosing Wisely initiative that states that screening with biomarkers, PET, CT, or bone scans is not appropriate for asymptomatic patients who have been treated for breast cancer with curative intent (Schnipper et al., 2012).
Based on current evidence, clinical breast examinations and annual mammographic screening are recommended after curative treatment of breast cancer in order to detect local recurrence and new primaries. Because of a high rate of false-positives, breast MRI screening is recommended only in very high-risk women, such as those with BRCA1/2 mutations. Ganz stressed the need to encourage adherence to mammography surveillance, which has not been adequate in breast cancer survivors.
For other cancers to which AYAs are prone, Ganz said, the appropriate post-treatment surveillance is not as clearly defined. But she noted that “people are beginning to back away from recommending these surveillance tests for which we do not have evidence of value and [which] might cause harm.”
AYA cancer survivors are not only at risk for a recurrence of their original cancer, but they are also at higher risk for developing a new type of cancer. Sixteen percent of new cancers are diagnosed in people who have had cancer before, Ganz noted. There are a number of hereditary mutations that increase the likelihood of developing multiple cancers at a young age, including
• Li-Fraumeni syndrome (p53 mutations), which increases the risk of developing childhood leukemia, sarcoma, brain and breast cancers, and adrenal cortical carcinomas
• Lynch syndrome, which is linked to a greater risk of developing colon, uterine, ovarian, and urinary tract cancer
• Familial Adenomatous Polyposis syndrome, which heightens susceptibility to colon cancer
• BRCA1/2 mutations, which increase the risk of developing breast, ovarian, pancreatic, and prostate cancers, and melanoma
As Ganz noted, all of these conditions are associated with early-onset cancers in the AYA population, and recognizing these syndromes is critical
for secondary prevention. “Taking a family history and identifying that this person is in a family where there is a predisposition to these cancers may be very important in terms of discovering the mutation and then screening them for the risk of these other cancers,” Ganz said. “Get to know your geneticist and other people who are working on these genetic susceptibility syndromes.” She added that risk-reducing surgery and intensive surveillance for most of these predisposition syndromes are well established and are recommended in guidelines.
As had been noted earlier, AYA cancer survivors are also at greater risk for developing secondary cancers because of the cancer treatments they received. Radiation treatment is one of the most important risk factors for secondary cancers, Ganz said, and these cancers often do not arise until 10 to 20 years after initial exposure. Screening should be directed to affected areas in the radiation field, i.e., monitoring for breast cancer after chest radiation therapy, monitoring for thyroid cancer after neck radiation therapy, monitoring for gastrointestinal tract tumors after abdominal radiation therapy or after receiving radioactive iodine for thyroid cancer, and monitoring for basal cell cancer in exposed skin fields.
Radiation treatment exposure history is critical. Practitioners should be aware of the dose, field, and type of radiation that their patients received. Age at exposure is also important. For example, Ganz said, breast tissue is most at risk in women receiving radiation therapy between the ages of 10 and 30 years. Chemotherapy also poses risks of secondary cancers, including hematological malignancies such as acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin’s lymphoma. In addition, patients who received cyclophosphamide or ifosfamide are at greater risk of developing bladder cancer, Ganz said.
Ganz also noted that some of the imaging tests that cancer survivors undergo can themselves increase the risk of cancer, and survivors generally undergo many such tests. One study found that 5-year recurrence-free survivors had received a mean dose of 24 mSv of radiation, or the equivalent of about 1,300 chest X-rays (Daly et al., 2012). These survivors had received a 4.6-fold higher dose of radiation than controls. “Why are these disease-free, long-term AYA survivors having so many imaging studies?” Ganz asked. “How can we reduce the number of these unnecessary procedures and decrease radiation exposure?”
She noted that an IOM report on survivorship care for all ages found that such care is often poorly coordinated and she said that it is probably
even worse for AYA survivors who are at a very mobile life stage (IOM, 2005). “They may have gone off to college and moved away from their family and are nowhere near where they got treated,” she said. “We need care plans and better care coordination to avoid the unnecessary imaging and radiation exposure these survivors are getting. We need to do followup care with good, clear guidelines.” Ganz added, “We do not necessarily have to have rigid guidelines, but certainly guidance statements on recurrence surveillance for the most common AYA cancers could be a real step forward as well as standardized approaches for screening for second malignancies.” She suggested an exposure-based approach, using guidelines from the Children’s Oncology Group as a model.12 Conducting retrospective analyses of clinical trials to assess whether intensive surveillance was any more effective than less intensive efforts could be helpful in determining those surveillance guidelines, Ganz suggested. “This is essentially what people did for lymphoma—they looked back to see if those scans actually did any good.”
Ganz called on health care professionals to actively pursue risk reduction strategies, including chemoprevention and surgical prophylaxis. Ganz suggested implementing strategies such as
• avoiding additional environmental exposures such as tobacco, alcohol, and sun exposure or use of indoor tanning devices;
• considering use of anti-estrogen therapies such as tamoxifen after chest radiation exposure in women, because level 1 evidence is unlikely to be available, and patient risks of breast cancer exceed those necessary for consideration of this intervention;
• managing energy balance to reduce the risk of obesity; and
• increasing physical activity.
Ganz also called for providing counseling for AYA cancer survivors who are at a particularly high risk of recurrence or of developing secondary cancers and for more collaboration with primary care providers. Freyer stressed the importance of collaborating with primary care providers to address what he called the “follow-up gap” in AYA cancer survivors. “We need to use primary care providers whenever possible for long-term care because that is who these patients are seeing,” he said.
________________
12 See http://www.survivorshipguidelines.org (accessed October 8, 2013).
Lifestyle Challenges and Interventions
As is true for all cancer survivors, AYA cancer survivors can pursue various lifestyle changes and interventions to lower their risk of cancer recurrence, new cancers, or various chronic conditions for which their cancer treatments might make them especially prone. These measures include an appropriate diet, regular physical activity, and stress and substance abuse reduction programs.
Bernard Fuemeller, associate professor of Community and Family Medicine, Psychiatry and Behavioral Science, and Psychology and Neuroscience at the Duke University School of Medicine, said that there is little evidence to suggest that the quality or quantity of food intake of AYA survivors is different from that of healthy peers in most cases. However, there are a few exceptions. For some young cancer patients, for example, a caloric-dense diet may be promoted to prevent weight loss, and glucocorticoid therapy during maintenance therapy for ALL has been shown to increase calorie intake (Reilly et al., 2001). There is also some evidence that the diet quality and quantity of AYA cancer survivors is suboptimal. Studies find that only between 16 and 54 percent of such survivors have the recommended amount of fat in their diets (Badr et al., 2011; Demark-Wahnefried et al., 2005; Rabin and Politi, 2010; Robien et al., 2008); 86 percent are consuming more than the recommended daily intake of sugar (Robien et al., 2008); and a low percentage are eating five or more fruits and vegetables per day (Badr et al., 2011; Demark-Wahnefried et al., 2005; Rabin and Politi, 2010; Tai et al., 2012). “Although this is not that different from the general population,” Fuemeller said, “it’s still not good, given the risk factors that may occur later on for these patient populations.”
Fuemeller said that there is some evidence to suggest that AYA cancer survivors have lower levels of physical activity and greater sedentary activity than their healthy peers; this could be due to impairments in physical functioning that affect their ability to exercise. In addition, there may be developmental times during treatment when they are not acquiring the normal lean mass that they need for playing and growing up healthy, Fuemeller
said. Studies also find that survivors are less likely to meet physical activity guidelines than people in the general population and that they are less active and more sedentary than their siblings (Badr et al., 2011; Belanger et al., 2011; Castellino et al., 2005; Demark-Wahnefried et al., 2005; Florin et al., 2007; Ness et al., 2009; Rabin and Politi, 2010; Tai et al., 2012).
The causes of the reduced physical activity among AYA cancer survivors have not been firmly documented. “There may be cancer-specific things we need to be aware of,” Fuemeller said, “like fear of injury and fatigue and pain, or the belief that you can’t be active after treatment.” But he noted there is a high demand for survivorship programs that focus on how to manage weight and get back into good physical shape, including programs that teach about healthy eating. “Unfortunately, there are very few interventions available that we can begin to disseminate to this patient population that have been tailored for survivors,” he added.
Wendy Demark-Wahnefried, the associate director for cancer prevention and control at the University of Alabama at Birmingham Comprehensive Cancer Center, reported that there is increasing clinical evidence that physical activity has antineoplastic effects—that is, it not only improves quality of life, but is also associated with prolonged survival in observational studies of patients with breast, ovarian, colorectal, or prostate cancer. There are multiple biologically plausible mechanisms that could explain this phenomenon, she said, adding. “There’s some really good evidence that physical activity not only improves quality of life but quantity of life in cancer patients.”
Lifestyle Intervention Programs
Fuemeller noted that lifestyle intervention programs for cancer survivors tend to have high attrition rates and that cancer survivors tend to prefer distance-based delivery channels, such as the Internet, over in-person sessions. In one pilot study of an Internet-based physical activity program for young adult cancer survivors, participants in the intervention group reported maintaining a level of activity that was as great as or greater than the level of activity reported by those in a control group, and the program was considered highly acceptable by the participants. Another study used Facebook to recruit participants into an online exercise program called FITNET.13 Modules about physical activity were delivered via Facebook to
_____________
13 See http://www.fitnethealth.com (accessed October 29, 2013).
the intervention group. The control group had access to the Facebook page but not to the specialized physical activity modules, and they also had access to an Internet-based site for tracking and monitoring physical activity. Both groups increased their level of moderate to vigorous physical activity, and there were no significant group effects. “They liked the idea of having this available on Facebook, which is a site that they use a lot,” Fuemeller said.
Fuemeller developed a mobile phone app for teenagers that engages them in choices about diet and physical activity and includes a decision-support tool that a health coach can use to intervene with the patients. It was developed as a game for participants, who advance through a series of fantasy expeditions to save the world. The proper diet and activity level, which is tracked with various devices and apps, earns them points in the game and enables them to progress through a series of adventures.
Fuemeller suggested that lifestyle intervention programs be designed to match the developmental stage and interests of participants. “We can’t expect something that’s going to appeal to someone in their upper 20s or 30s is also going to appeal to the 16-year-old,” he said.
Ganz emphasized the need for stress management in young cancer survivors. “We started a stress reduction intervention because they were telling us they are exercising and eating well but they needed someone to help them manage their stress,” she said. She also noted that, despite the special needs of AYA cancer survivors, the programs that can help them will have to be aimed at a more general population of cancer patients “because we’re never going to have all these specialized programs to meet everyone’s needs.”
Karen Emmons, professor in the Department of Society, Human Development, and Health at the Harvard School of Public Health and deputy director of the Center for Community Based Research at the Dana-Farber Cancer Institute, reported that AYA cancer patients are at an increased risk of substance abuse. Several speakers suggested that this is due, in part, to the ages of the AYA cancer patients, with the peak of substance abuse occurring in individuals who are between 18 and 25 years of age (SAMHSA, 2009, 2010).
Emmons noted several reasons to be concerned about substance abuse in AYAs with cancer, including the following (Clarke and Eiser, 2007; Day et al., 1994; WCRF and AICR, 1997):
• Tobacco may exacerbate the treatment-related risk of cardiac and pulmonary toxicities and increase the risk of lung cancer.
• Alcohol is associated with an increased risk of aerodigestive cancers in adult survivors and may increase the risk of myocardial dysfunction, liver damage, osteoporosis, and breast cancer.
• Drug use can induce or exacerbate depression, anxiety, posttraumatic stress disorder, impacts of traumatic brain injury, and insomnia.
Emmons noted that tobacco use rates in childhood cancer survivors range from about 16 percent to about 37 percent. In the general population, there is a great deal of variability in smoking prevalence across states, likely due to variable state laws on tobacco use, she said. The lowest prevalence by state is about 9 percent, and the highest is about 27 percent. Most studies show that childhood cancer survivors smoke at a rate that is equal to or lower than the rates of smoking among their siblings or the general population, although the Behavioral Risk Factor Survey found a twofold increase in smoking among survivors. Emmons stressed that even if survivors smoke just as much but no more than their peers, “it’s a real problem for their health, especially in the context of all the late effects they are likely to develop,” she said. Moreover, cancer patients who continue to use tobacco after diagnosis have poorer treatment outcomes, higher rates of recurrence and second primary cancers, and poorer overall survival (IOM, 2013).
About three-quarters of AYA cancer survivors use alcohol, which is about the same as age-matched controls in the general population. There are few non-biased data about drug use in AYA cancer survivors, Emmons said, but about 12 percent of participants in the Childhood Cancer Survivor Survey reported using marijuana. She said that many lifestyle risk behaviors cluster together, with one study dividing up risk behavior into four groups (Rebholz et al., 2012):
1. Risk-avoiding individuals who did not engage, or engaged only to a minor extent, in risk behaviors and who reported health-protective behaviors
2. Moderate risk-avoiders, who engaged more frequently in physical activity and also consumed alcohol
3. Individuals who have a low engagement in health-protective behaviors and are likely to smoke, but not to drink
4. Risk-takers who engage in many of the assessed risk behaviors, such as smoking, marijuana consumption, and alcohol use, including binge drinking, and who have a lower engagement in health-protective behaviors
The factors linked to substance use in cancer survivors include less education, lower income, white race, being networked with people who smoke, and greater stress and lower mental health scores, Emmons said, noting that these are the same factors that are linked to substance abuse in the general population. “It is theorized that in the general population people engage in substance use to cope with life stressors, and data suggest that poor daily coping has been reported among childhood cancer survivors and that worry is linked to substance use. So, helping address some of these life stressors may help with reducing substance use,” Emmons said.
She suggested that educational and other efforts aimed at preventing substance abuse in young cancer survivors are warranted, citing a study that found that among non-smokers, 57 percent of survivors aged 10 to 18 years old were uncertain about whether they would smoke in the future and that having less knowledge about tobacco-related health risks was tied to greater intentions to smoke (Clarke and Eiser, 2007). Another study found that an intensive risk counseling intervention increased perceived vulnerability and reduced intentions to smoke (Tyc et al., 2003).
Emmons said that her research group has developed a peer counseling intervention for tobacco use that is effective when used in combination with nicotine replacement therapy. This intervention doubled the quit rates in childhood cancer survivors who smoked (Emmons et al., 2009). She has also developed Web- and print-based interventions that show similar quit rates. “In tobacco, we have some effective risk-reduction tools, but not so much for other behaviors,” Emmons said. She noted that a survey of 140 childhood cancer survivor programs that were part of the COG found that only 3 percent delivered optimal tobacco cessation treatment (de Moor et al., 2007). “We have a very long way to go,” she said.
Justin Baker of St. Jude Children’s Research Hospital said that the NCI defines palliative care as being “comfort care for a patient who has a serious disease” (NCI, 2010). He explained that, unlike end-of-life care, palliative care starts at diagnosis and continues throughout the illness. A palliative
care specialist team works alongside the patient’s primary cancer care team and provides care in multiple venues, including the hospital, clinic, and the home. This care is aimed at improving the patients’ and family members’ quality of life by addressing emotional, physical, practical, and spiritual issues. “When I talk about palliative care,” Baker said, “I do not talk about it as comfort care, but as anti-suffering care. Comfort care people traditionally think of palliative care as mostly symptom-based support, but suffering comes in all shapes and sizes, and that is what we need to be addressing.” Baker emphasized that palliative care should not be viewed as just end-oflife care.
Studies are beginning to document the benefits of palliative care. One study found that adding palliative care to standard care for metastatic lung cancer patients resulted in better quality of life, less anxiety and depression, the use of fewer hospital resources and chemotherapy, and longer life compared to standard care alone (Temel et al., 2010). “If you were going to create a drug that did all this for this patient population, it would be a billion-dollar drug,” Baker said. He stressed that palliative care improves patients’ well-being and also saves resources, “so early integration of palliative care makes an awful lot of sense.”
Based on this study of palliative care for lung cancer patients and seven other studies, ASCO has developed a provisional clinical opinion stating that combining standard oncology care and palliative care should be considered early in the course of illness for any patient with metastatic cancer or cancer with a high symptom burden. The clinical opinion also recommended more research on such combined care, Baker said.
Most facilities offer one of three approaches to palliative care, Baker said. One is the on-demand approach, which typically is a consult service. Another approach is trigger-based and targets specific patient populations likely to benefit from palliative care, such as those in intensive care, those with brain or other high-risk tumors, or those with relapsed disease. The third approach is institutional and integrates palliative care for every single patient. For example, an institution might have a pain policy in which a patient who receives a pain intervention automatically has a palliative care assessment afterward that is documented and tracked longitudinally. Another institutional approach is to devote specific resources to providing palliative care and tracking it as a quality indicator.
Most cancer treatment facilities do not find it feasible to provide palliative care from the time of diagnosis for every cancer patient, Baker said. Nonetheless, he continued,
Palliative care has to be proactive and cannot be reactive. When you have a palliative care oncology service that is devoted only to the consult-based approach, it turns into end-of-life care teams. Whereas when you have a proactive approach, you are dealing with symptoms and psychosocial distress on the front end, and you are giving these patients more resources, more time that can be devoted to these issues. So, I really encourage institutions to have an embedded expert model in which you have somebody with palliative care expertise doing these kinds of assessments in a routine and regular manner.
Baker suggested integrating education about palliative care into new patient orientation packets and programs and applying routine distress assessment tools that, in addition to ascertaining pain and other symptoms, also assess psychosocial distress.
Baker said that the integrative model at St. Jude uses standard operating procedures to address advanced care planning, ethical considerations, symptom control, emotional, social and spiritual care, care coordination and care continuity, care of the imminently dying patient, and bereavement care (see Figure 5). He stressed the importance of building trust with patients and maintaining a therapeutic relationship with them over the entire extent of their treatment. “This patient population does not deal well with transitions from provider to provider,” he said, “so different care teams
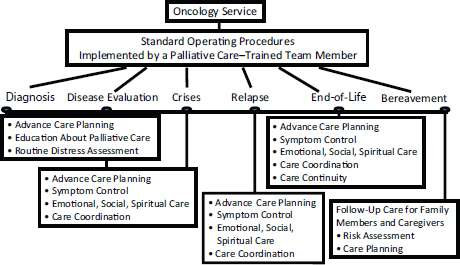
FIGURE 5 Embedded expert model of palliative care integration across the care continuum.
SOURCE: Baker presentation.
on the in-patient, out-patient, and home-based settings are not an effective way to help them. Interactions may be lengthy and may require innovative therapeutic compromises.”
Baker suggested that an AYA palliative care team should include a nurse, a social worker, a psychologist, a palliative care physician, and an oncologist. He added that a flexible, multidisciplinary palliative care team with extra training in the needs of the AYA patient could provide support within both pediatric and the adult facilities as well as support for home care.
Baker stressed that advance care planning is a critical part of cancer care. Such planning involves talking to patients and family members about what to do if the cancer for which the patient is currently being treated returns and becomes incurable. One study found that when this discussion took place and adolescents were significantly better informed about possible end-of-life decisions, there was better congruity between what the adolescents wanted and what the families thought the adolescents would want (Lyon et al., 2013). “In this case,” Baker said, “advance care planning enabled families to better understand and honor their adolescents’ wishes.”
Baker suggested having an integrated approach toward palliative care assessments and having those advance care planning discussion at several points during the care continuum, including at diagnosis, at disease evaluation, at disease crises or relapses, and at the end of life. “That does not necessarily mean that you talk about end-of-life planning at the very first meeting, but it does mean that you talk about the resources that may be available for palliative care in your institution,” he said. For example, when patients with brain tumors get good news about MRI results, a palliative specialist will talk about how it is excellent news but also give them the option to discuss what might happen if the tumor comes back.
The symptoms that AYA patients experience at the end of life are largely determined by the types of cancer they have. Eighty-nine percent of patients experience distressing symptoms, Baker said, with more than half experiencing three or more symptoms. Pain, dyspnea, and fatigue are the most prevalent symptoms. Baker noted there are also significant rehab
concerns for the AYA patient population. “Even as they are approaching the end of life,” he said, “it has been my experience that people want to be working to optimize their rehab issues.” Thus, St. Jude’s end-of-life care program provides physical, occupational, and speech therapy.
AYA patients with an incurable disease also have numerous psychological symptoms, especially during the last month of life. In one survey that Baker conducted, all AYA patients approaching the end of their lives reported experiencing sadness, anxiety, and the fear of being alone, of pain, and of death. “There is a significant psychological component to progressive cancer,” Baker stressed.
As noted previously, the psychological needs of AYAs with cancer are complex and vary considerably, but most AYAs with cancer are similar in reporting the need for peer support. Baker found that many AYAs with cancer reported feeling isolated from their regular peers at school or work because of their illness and finding that other AYA oncology patients provide an important support network. But, as Baker noted, the process of transitioning to end-of-life care may isolate AYA patients from their new peers, who are still on a curative path. The death of peers in a support group can also create psychological stress. “One patient stopped going to her support group once she found out that somebody in the group died,” Baker said. “There is almost a secondary isolation once a patient is no longer able to be cured. This psychological isolation is debilitating, and we really need to try to help facilitate this peer support.”
Death anxiety is commonly experienced by adolescents and young adults as they are going through their cancer treatment. Baker’s study at St. Jude found that nearly one-quarter of those cancer patients between 15 and 21 had lost a close friend in the previous year, with most of the friends who died being other oncology patients. “This grief experience can increase their death anxiety,” Baker said. Patients in the study reported that the loss of such friends led to grief and bereavement, shock, depression, fear, loneliness, and being upset with a lack of parent support in dealing with their grief. “This age group is very uncomfortable talking with their parents about their feelings anyway and seemed to expect more support from their parents when talking to them about the death of a friend,” Baker said. “They felt their parents were frequently changing the subject and trying to get away from that particular topic.”
Baker described a study he conducted that revealed the diverse ways that AYAs with cancer deal with death anxiety. The most common coping strategies cited by the patients were talking about their anxiety, seeking
distraction, and relying on religious beliefs (see Table 2). Given the diversity of coping strategies, Baker said it is important to individualize support for AYAs with cancer as they deal with their psychological stresses.
Baker also provided some quotes from AYAs with cancer who participated in his study. One wrote about his concern about the devastating effect a peer’s death had on his family. Another wrote about how the death of a fellow AYA with cancer provoked his own anxiety, especially given that the peer had died despite doctors reassuring him that he was going to be fine. One respondent wrote, “Sometimes his mother posted really depressing things about her grief on Facebook.” As Baker stressed, “These are things that our adolescent and young adult patients are dealing with on a day-today basis and that we have to be addressing proactively.”
Karen Fasciano noted that AYA patients who are approaching death have unique psychological issues, not shared by older adults, concerning how to come to terms with the meaning of their shortened lives and what their legacy will be in addition to the grief tied to dying young. AYA patients who have children have the additional challenge of preparing their children for the loss of a parent.
Baker added, “Don’t just assume that because an adolescent or young adult does not talk about death that they are not thinking about it. Give them an opportunity to talk about it.” Baker stressed that the AYA population cognitively understands that death is permanent and irreversible, although they may have a sense of immortality that may act as a defense mechanism. Eventually, acceptance of their own death develops in response to the fatigue of the overall disease journey. “I’ve seen this time and again where they have this mentality that ‘I’m going to beat this cancer,’ but then eventually the reality and just being tired makes them not want to come to
TABLE 2 Coping Strategies Employed by AYAs (n=98) for Death Anxiety and Grief
| Strategy | # | % |
| Talking about it | 23 | 23% |
| Don’t know/remember | 23 | 23% |
| Distraction (hobbies, school, work, being with people) | 15 | 15% |
| Religious beliefs/prayer | 9 | 9% |
| Time passing | 8 | 8% |
| Not thinking about it | 5 | 5% |
| Other | 15 | 13% |
SOURCE: Baker presentation.
the hospital any longer,” Baker said. “We have to provide possibilities for them to get that care they need at home.”
Baker added, however, that many patients receiving end-of-life care still also want to receive care in the clinic. “They want to be able to come back to the clinic when they are able,” he said, “but they also want to have clinic-based services provided in the home when they do not want to go to the clinic.” Baker noted that new provisions in the ACA enable patients to have both hospice care at home and concurrent oncology care at a facility.
Baker recommended working toward providing a “good death,” which he defined as one in which there is
• management of symptoms;
• spiritual and personal growth;
• care in a familiar setting surrounded by loved ones;
• provision of understandable evidence to guide decision making and planning;
• confidence that there will not be financial, emotional, or physical burden to family members; and
• right of self-determination and control of treatment.
HEALTH CARE INSURANCE CHALLENGES
Health insurance is a major issue for many AYAs with cancer, who often fall between the cracks in terms of being too old to be covered on their parents’ insurance, but not yet having a job that provides health insurance. Young adults in general are at risk of being uninsured, Park said, noting that one study in 2009 found that almost one-third of young adults aged 19 to 29 years old did not have coverage, with half of those without coverage earning less than 133 percent of the federal poverty level (Collins et al., 2011). Almost half of young adults reported forgoing medical care because of cost.
The CCSS showed that cancer survivors were at greater risk than their siblings for being uninsured (Park et al., 2005). One-third of them had difficulty obtaining coverage, compared to only 3 percent of their sibling controls, Park reported. Eleven percent were uninsured, which is similar to the approximately 15 percent uninsured rate in the general population. But, as Park noted, these cancer survivors need so much medical care that “it is a huge problem to address.” She described one study that found that nearly three-quarters of uninsured AYA cancer survivors had had no routine medical visits during the previous year and had had to forego medical care
because of cost—a significantly greater percentage than among uninsured people who had not had cancer (Kirchhoff et al., 2012).
AYAs without health insurance may also face delays in cancer diagnosis. One study of cancer patients between the ages of 15 and 29 found that lag times between symptom onset and cancer diagnosis were tied to the type of the patient’s health insurance (Martin et al., 2007). The longest lag times were associated with having public insurance rather than private health insurance and with self-payment for medical bills. Delays between symptom onset and diagnosis were associated with being diagnosed at an advanced stage of disease. “This is a population that is struggling with either achieving or maintaining their insurance access, so these are very pertinent results,” Melissa Hudson said.
Robin Yabroff reported that a study using the nationally representative MEPS data showed a mean annual medical expenditure for survivors of AYA cancers of about $8,300, which is about double that for similar individuals without a cancer history. Kevin Oeffinger pointed out that many of those medical expenditures go toward treating the multiple conditions that AYA cancer survivors are likely to develop due to their cancer treatment. “They are having multiple visits for multiple conditions and paying for multiple medications at a young age when most young adults are not paying for any type of medication, much less even going to the doctor,” he said.
In contrast to the CCSS, the study based on the BRFSS found no significant differences between AYA survivors and persons without cancer in terms of health insurance access. But there was a significantly higher proportion of AYA cancer survivors who reported that they could not see a doctor because of cost compared to persons without cancer, Eric Tai noted. These differences may be due to the different age ranges included in the studies and the different comparison group used in the CCSS (siblings) versus the state population-based BRFSS (sampled individuals). Distributions of health insurance were also different in the nationally representative, population-based MEPS (sampled individuals).
The type of health insurance also has an impact on access to care. In a study using the nationally representative MEPS data, Robin Yabroff reported that survivors of AYA cancers were more likely to be unable to get, or delayed necessary medical care, dental care, or prescription medications, compared to similar individuals without a cancer history (17 percent vs. 13 percent). This disparity in access to care between cancer survivors and similar individuals without a cancer history was greater among those with public health insurance (26 percent vs. 19 percent) and the uninsured (31
percent vs. 22 percent) than those with private insurance (11 percent vs. 9 percent). Similar patterns of access to care for cancer survivors and individuals without a cancer history by type of health insurance were observed for other preventive services (Yabroff et al., 2013).
Even when AYAs are insured, their health insurance may not adequately cover their medical care. Park said. She and her colleagues surveyed a subset of participants in the CCSS and found that more than half reported annual out-of-pocket costs of more than $2,000. “Even though they said they were satisfied with their insurance,” she said, “they were admittedly dissatisfied about costs, which seemed crippling in some cases.”
The 2010 LIVESTRONG survey found that 22 percent of respondents had an insurance provider refuse to cover a visit to the doctor or facility of their choice, 12 percent were denied insurance coverage because of their cancer, and 11 percent had insurance refuse to pay for a second opinion. Those who were 5 years or more post treatment were more likely to have been denied coverage because of their cancer. “The longer they were [past their cancer diagnosis], the more likely they were to experience that,” Ruth Rechis said. Thirty-nine percent reported that they or their family had to borrow money or go into debt because of their cancer, and 7 percent indicated that they had filed for bankruptcy, with 83 percent reporting that they were worried about having to pay large medical bills. “This idea of debt was much higher for the AYAs than it was for the others in our survey,” Rechis said.
A number of participants spoke about how provisions in the ACA are increasing the percentage of AYAs with medical coverage and how that should foster earlier diagnoses, better cancer care and survivorship care, and better surveillance for AYAs with cancer. Bleyer estimated that during the first 2 years after passage of the ACA, which raised the age at which children could be covered by their parents’ insurance to 26 years, about 6 million 19- to 25-year-olds became insured who previously were not able to be covered by their parent’s insurance. He estimated that almost 10,000 of these individuals have been diagnosed with new invasive cancers (Bleyer et al., 2012).
Park described other provisions of the ACA that should help AYAs diagnosed with cancer, including those that prohibit preventive care copays and promote primary care as well as those that ban exclusions for
pre-existing conditions. The ACA also calls for expansion of Medicaid eligibility to people whose income is up to 133 percent of the federal poverty level, which is significant because childhood and AYA cancer survivors are disproportionately likely to be covered by Medicaid. However, many states are opting out of that expansion. People whose income falls between 133 and 400 percent of the federal poverty level can receive subsidies on a sliding scale to cover part of the cost of health insurance under the ACA.
The ACA also requires coverage for recommended preventive care and promotes primary care through patient-centered medical homes, which in turn facilitates coordinated care between primary care physicians and other providers. But Park stressed that much of the preventive care that the ACA stipulates, such as recommendations by the U.S. Preventive Services Task Force for breast cancer screening starting at age 40 in average-risk women, are not applicable to AYA cancer survivors who might need to begin such breast cancer screening at an earlier age. “It’s great to have more of a focus on prevention,” Park said, “but it is not going to meet all of the needs [of cancer survivors].”
Other ACA provisions require insurance companies to cover the costs of routine medical care provided within clinical trials and prevent health plans from imposing lifetime limits on health care reimbursements. “People with medical difficulties are protected from having a cap on their elevated medical costs,” Park said.
But she stressed that AYA patients will need both advocacy and education to help them use these health care reform benefits. Her study found that more than half of childhood cancer survivors did not even know whether to feel concerned or hopeful about the benefits and protections under the ACA (Park et al., 2012). Both survivors and siblings demonstrated a lack of familiarity with the ACA and health-related legislation.
Park also noted that even with the ACA, insurance may still be financially prohibitive for some childhood cancer survivors. A single person who earns $46,000, which is just above 400 percent of the federal poverty level and thus does not qualify for a federal subsidy, may still view insurance as unaffordable, she said.
Recognizing the prevalence of unmet needs among AYAs diagnosed with cancer and the lack of standards for the care of AYA patients, several speakers provided “wish lists” for what models of care and support should
include for this population. The characteristics that Hudson suggested for optimal quality care included
• assistance with managing disease and treatment effects;
• cognizance among providers of the unique psychosocial context for AYA growth and development;
• assessment of and attention to the cognitive, psychiatric, and psychosocial needs of AYA;
• referral to available age-appropriate resources during treatment; and
• facilitation of transition to survivorship care.
Ideally, the team providing care to AYAs would include someone with expertise in AYA oncology as well as expertise in AYA developmental issues, Hudson said. She noted that although different care models are available, including those for cancer center-based care, community-based care, or a hybrid of these two types of care, “it is not only the fabric of an environment that matters, it is the ethos of care” (quoting from a journal article [Morgan et al., 2010]).
Hudson suggested that in addition to providing symptom management, addressing cancer-related health problems, and promoting a healthy lifestyle, a model program for AYAs with cancer should also be attentive to their specific needs regarding fertility, sexuality, and contraception. Mental health issues should also be addressed, including how the AYAs’ cancer experience is affecting their ability to develop intimate interpersonal relationships and attain their educational, career, or other life goals. Health education is also critical, particularly about cancer-related health risks and the types of self-management and monitoring that should be pursued. A model care system should also provide guidance on how to maintain effective access to health care and insurance, Hudson added. Finally, she suggested that care models should promote timely referral and initiation of treatment, attention to treatment protocol adherence, and smooth transitions from active cancer therapy to survivorship care. Ganz suggested that providing spiritual resources as part of care for AYAs with cancer might also be of benefit, given that studies indicate that they can help boost the psychological resiliency of cancer patients.
Participants noted examples of programs for AYA patients with cancer throughout the workshop (see Box 3). Rebecca Block, AYA psychosocial research leader and assistant professor of medicine at the Knight Cancer
Institute at OHSU, studied the psychosocial components in programs available to this population with cancer and found that the programs provided a range of services, including patient/peer navigation, physical therapy, genetic counseling, palliative care, peer support, chaplaincy, and nutritional counseling and partnerships with community-based organizations. However, many programs lacked some of the key components identified by Hudson as being critical. None provided legal services. Most assessed the psychosocial needs of their AYA patients only when the need for such assessment was identified. “These assessments aren’t happening unless someone’s noticing or saying something,” Block commented, and she added that other related issues that might be problematic are not assessed. Only one program did a comprehensive assessment on every single AYA who participated. “It’s great to do what we think patients need,” she said, “but it’d be even better to do what we know each patient needs. This requires consistent and comprehensive assessment.”
There are few service delivery standards or standard of care guidelines for AYAs with cancer, Block said, and this has led to a situation in which there are many different models for providing care for these individuals. Even models providing a specific service that is stipulated by treatment guidelines, such as peer support, vary in how they provide that peer support, she said, “and, maybe most importantly, we have no idea what they’re actually doing for people.” Most programs measure their effectiveness by such metrics as the number of patients participating in their programs and patient satisfaction. “The outcomes evaluated are extremely limited,” Block said, and she called for psychosocial care to be informed by evidence. As she noted, “Measuring satisfaction is not a substitute for measuring psychosocial outcomes.”
Block also noted that most psychosocial programs for AYAs with cancer are philanthropically funded, with a few programs acquiring grants to support the development and testing of a specific intervention. She said that sustaining such funding is a challenge for most programs.
EDUCATION NEEDS FOR HEALTH CARE PROFESSIONALS
Several workshop participants identified a lack of education for health care professionals on the special needs of AYA patients with cancer as a gap that needs to be closed, through AYA-focused specialty training programs or fellowships in oncology or hematology, support tools, or other initiatives.
BOX 3
Examples of Care Programs for AYA Patients with Cancer
Thriving After Cancer
The George Washington Cancer Institute in Washington, DC, offers Thriving After Cancer (TAC)a clinics that specialize in follow-up care for survivors who have completed active treatment for cancer. For adult survivors of pediatric cancer, TAC provides care in an appropriate adult setting. The TAC clinic also provides comprehensive services to survivors of adult-onset cancers. TAC takes a multidisciplinary approach and coordinates care with primary care providers to address the health risks and late effects of treatment. TAC provides not only medical care but also psychosocial services, and its care team includes psychiatrists, nutritionists, legal experts, and social workers. Preventive health care services are also provided, including a comprehensive fitness assessment with customized exercise plan as well as nutrition workshops. In addition, TAC provides career and vocational counseling, help with financial assistance and using health insurance, and free legal advice.
Life with Cancer Young Adult Program
Offered by Inova Cancer Services, the Life with Cancer Young Adult Programb targets cancer patients between the ages of 18 and 39 by offering group meetings co-facilitated by an oncology social worker and an oncology nurse educator. These meetings address such issues as fertility, isolation, insurance, dating and sexuality, financial assistance, education, employment, and age-appropriate peer support, including social networking. The members of the group also meet on their own for happy hours and volunteer opportunities.
Planet Cancer
Planet Cancerc is an online community of young adults in their 20s and 30s with cancer that offers a place to share insights and explore fears and other emotions. It offers online support groups and forums.
_____________
a See http://smhs.gwu.edu/gwci/patient-care/survivors/tac (accessed October 24, 2013).
b See http://www.lifewithcancer.org/young_adults.php (accessed October 24, 2013).
c See http://myplanet.planetcancer.org (accessed October 24, 2013).
Teen Impact Program at Children’s Hospital Los Angeles
Teen Impactd is a group-based psychological, emotional, and social support program of the Children’s Center for Cancer and Blood Diseases at Children’s Hospital Los Angeles. The primary service of the Teen Impact program is the support group meeting, but the program also offers a 3-day retreat and sponsors various special activities and events throughout the year, including art workshops, parties and celebrations, field trips, and music and cultural events. Teen Impact’s 3-day retreats for teens and young adults with cancer include outings to amusement parks and time to socialize with peers. Special group activities are planned each day to promote diversity, individuality, and group cohesion and bonding and to focus on identified themes and issues of survivorship. A physician and nurse attend all retreats to provide care for teens who are still receiving treatment or who have special medical needs.
Teen Cancer America
Teen Cancer Americae has a number of activities aimed at improving the care of teens and young adults with cancer, including
• Partnering with hospitals to create youth-oriented centers that provide peer support and interaction for those receiving treatment
• Funding analysis and documentation of U.S. best practices in the treatment of teens and young adults with cancer
• Developing, circulating, and administering ongoing training for doctors and other personnel who work with teens and young adults with cancer to help them deal with their unique needs
• Developing materials and programming to help students, teachers, administrators, educators, and employers understand how they can best support teens and young adults with cancer when they return to school and work
Change It Back
The Health Care Rights Initiative sponsors the Change It Backf Centers of Excellence Program, which is dedicated to facilitating the
_____________
d See http://www.chla.org/site/c.ipINKTOAJsG/b.3768089/#.UmGbRhb Cmio (accessed October 24, 2013).
e See http://www.teencanceramerica.org (accessed October 24, 2013).
f See http://hcri.org/programs/change-it-back (accessed October 24, 2013).
expansion of needed services to the AYA cancer population and increasing awareness about the services that are available to patients and their families. To receive a center of excellence designation, a cancer center, hospital, or clinic must directly provide or facilitate the following:
• Fertility counseling
• Health insurance and financial counseling
• Clinical trial education and facilitation
• Psychosocial support
• Transition to surveillance and survivorship care services
One participant suggested that standards and levels of training should also be developed for providers of psychosocial support for this population.
Freyer suggested additional medical training in survivorship care at the undergraduate level and at the graduate level in pediatric medical oncology fellowships. He also suggested establishing primary care residencies to provide training opportunities in caring for AYAs with cancer. He noted that CHLA requires fellows in pediatric hematology and oncology at the University of Southern California to have a rotation in cancer survivorship care in their second and third years. He also noted the availability of Webbased support tools for primary care providers, such as the Passport for Care14 developed by COG, and he suggested that there should be greater development and use of clinical guidelines and continuing medical education programs that focus on the AYA cancer patient.
Several workshop participants noted research gaps that exist for AYAs with cancer, including a lack of research on
14 See http://www.passportforcare.org (accessed October 8, 2013).
• psychosocial and developmental issues and the best ways to address them;
• late treatment effects, including secondary cancers and how to prevent and monitor for them;
• factors that enhance resilience among AYA cancer survivors and the influence of social networks on outcomes;
• ways to preserve or restore fertility;
• the socioeconomic consequences of AYA cancer, broken down by cancer type and treatment, and how the cancer experience affects career choices and trajectories;
• the best institutional practices or delivery models for treating AYAs with cancer and fostering transitions into survivorship care;
• access to care and the influence of the ACA and other measures aimed at addressing health care disparities; and
• substance use patterns and effective interventions.
There are several challenges involved in studying AYAs with cancer, including the heterogeneity of the population, the difficulty of recruiting AYAs for research projects, and bias in survey responses. As many workshop participants pointed out, the AYA category covers a large range of ages with a great deal of biological and developmental variability. Determining the best way to divide AYAs into subgroups for analysis can be challenging, Rechis said. Furthermore, differences among ethnic, educational, and treatment subgroups can influence research outcomes and make it difficult to apply results from a particular subgroup to the group as a whole.
AYAs traditionally have a low participation rate in clinical research. Hudson reported that SEER data from patients diagnosed in 2006 indicate that only 14 percent of cancer patients aged 15 to 39 were enrolled in clinical trials (Parsons et al., 2011), compared to about 60 percent of pediatric cancer patients. Thirty-four percent of those of ages 15 to 19 were enrolled in clinical research, while only 3 percent of those from 35 to 39 were enrolled, similar to the rate for older adults with cancer. The AYA HOPE Study found that only 7 percent of the survey respondents participated in a clinical trial. The top reason respondents gave for not participating in a trial was concern that the treatment they might receive would not have been sufficiently tested.
To encourage more AYA participation in survey research, some participants suggested offering financial incentives, such as paying participants $25 for completing a study. Benjamin Rubenstein noted that such financial incentives would prompt him personally to participate in research. “Money would incentivize me, or just an Amazon gift card,” he said. “It does not even have to be for that much.” Another participant agreed that “money talks” for the younger population but said “a 39-year-old is not going to be as impressed with a $25 gift card to Amazon as an 18-year-old.” Farrish suggested, “If the medical community takes better care of us, we are going to want to give back and take better care of the next person to get diagnosed” by participating in research. Rubenstein suggested that one way to improve AYA participation in research would be to tailor communications about such research to this population. “If you want young adults to be more responsive, word it the way that we talk,” he said. “Remember who your audience is and relate to us.”
Some researchers have used online tools to recruit AYA participants for their studies, but these online surveys may be subject to bias, with women being more likely to respond than men, for example. One participant noted, “We do lots of surveys that get us good information, but specific information from specific populations. We need to look at other methods for gathering data, including analyzing online conversations.”
Surveys available only in English can preclude the participation of non-English speakers, Brenda Nevidjon pointed out. Increasingly, however, surveys are being administered in multiple languages, as one participant noted. MEPS and the MEPS Experiences with Cancer survey, for example, were offered in English and Spanish, and the California Health Interview Survey was administered in six languages. In addition to being administered in appropriate languages, surveys must be sensitive to the needs of the community being studied, another participant suggested. “You need to address the questions the community finds relevant and work in partnerships so they can be answered,” he said. But engaging the community in research requires additional resources, which grants should provide, Casillas said. “There has to be a lot of groundwork with community-based participatory research,” which is important to gain the trust of the community partners she said. “This is an additional cost within research studies that is often thought about after the fact and I would encourage us to think about it early on in our grant planning process.”
In addition to research challenges, there are new research opportunities for those studying the AYA population with cancer, including novel online databases and data linkages. In particular, Yabroff mentioned the Cancer Research Network, which is a group of managed care organizations that can address research questions collectively (Nekhlyudov et al., 2013). The Cancer Research Network has health care delivery information about individuals with and without cancer of all ages, she noted. Much of the work exploring longitudinal patterns of care is done exclusively in the population aged 65 and older, she said. “More work with patterns of care and health care delivery in this younger population using existing data resources will be important.” Yabroff added that hospital and ambulatory care discharge data are increasingly linked to state-based cancer registry data. Such linkages can enable certain types of research that were previously not possible. ASCO also recently launched a large database for patient treatment data collected by ASCO physicians.
Several speakers stressed that AYAs are part of a wired generation that relies on the Internet for much of its information gathering and for interacting with others. Thus, researchers and those who provide care for this population need to be aware of and leverage online opportunities. One researcher reported that in a study of resilience, he is assessing AYAs with cancer through online surveys. “They are easy to do, the kids don’t mind doing them, and they are remotely available for multiple institutions,” he said, and he suggested embedding such assessments in all cooperative group studies in which AYAs participate. “Think of the outcomes we could collect, including longitudinal data,” he said. “We have the infrastructure for this.” Karen Emmons agreed that the time is right for online assessments, and Ganz said that the logistics for such assessments would not be too costly, given nearly universal access to computers and the Internet in this population. Others suggested reaching out to AYAs with cancer via email and social networks in order to encourage them to participate in clinical research. Rubenstein said that he tends to fill out cancer surveys that he receives through Twitter. Sharon Murphy, scholar in residence at the IOM, suggested establishing an online platform akin to PatientsLikeMe15 for gathering information about AYAs with cancer, including what treatments they have had, how they responded, the toxic effects they experienced, and so on. This continually
_____________
15 See http://www.patientslikeme.com (accessed October 8, 2013).
updated database could collect outcomes that could inform patient care in real time, she said. Another participant noted that the Teenage Cancer Trust has developed an app for smartphones that follows such a model. Leonard Sender, director of clinical oncology services at the Chao Family Comprehensive Cancer Center of the University of California, Irvine, added that this could be another tool for engaging patients in crowd source research. “The concept is that the patient is also the researcher,” he said. In addition, researchers are starting to analyze the online conversations at Planet Cancer and other websites as a way of assessing the concerns of AYAs.
Several speakers suggested specific policy measures that could improve care for AYAs with cancer, such as fostering more collaboration among various organizations and institutions and providing a clearinghouse for programs focused on AYAs with cancer. Bleyer said, “We need a central place where we can learn from each other on how to put together AYA programs.” Fasciano added, “To have some central place where we could disseminate programmatic issues that were studied and evidence-based for this population would be a really big step.” Sender pointed out that the Journal of Adolescent and Young Adult Oncology has been publishing a series of articles about models of care, including those in Canada, Italy, and other countries.
Hayes-Lattin and Bleyer suggested more collaboration between the NCI and CDC working groups focused on AYAs with cancer as well as between government agencies and nonprofit organizations, such as the LIVESTRONG Foundation, and various medical institutions. “We can’t do it alone, and obviously we are going to need to work together,” Hayes-Lattin said. Ashley Smith, a behavioral scientist in the Outcomes Research Branch of the Applied Research Program at the NCI, responded, “Each of us in our own institutes have our own priorities and areas of emphasis. But we recognize there is important work happening in different institutions and are working to make sure we are in line about those things.” Nita Seibel, head of pediatric solid tumors in the Clinical Investigations Branch of the Cancer Treatment and Evaluation Program at the NCI, added that public-private collaborations are especially important in the current era in which government funds are often not sufficient.
At the close of the workshop, Tom Kean, president and chief executive officer of C-Change, provided a brief overview of the themes of the workshop and the suggestions for actions that he asked participants to contemplate. Kean said that the primary focus throughout the workshop was on the patients, with frequent emphasis on fostering engaged patients and patient-centric programs. There were also many calls for better care coordination and integration. He added that numerous AYA-specific programs have been developed, but they vary a great deal, and there is a need to share information about those programs. “Let’s look at what we can learn from each other,” he said. Many programs also face sustainability challenges.
Another overarching theme was the need for better information on the AYA population with cancer. He noted the challenge of the tremendous variability across the 15-to-39 age range of AYA patients—where they are in the developmental life cycle and the very different needs that they have—which can make it difficult to extrapolate research results to different segments of the population. “We ought to start looking at them by the blocks of age groups within that broad 15-to-39 age range,” he said, “and also start to drill down and look at them by cancer type and by treatment in studies.” Other factors that may influence the care and outcomes for AYA patients include differences in lifestyle and culture, differences in family support and other personal connections, and the highly mobile nature of this population, he added. He also said that those working in the field need to outline research priorities, develop better research tools, foster clinical trial accrual, and make better use of existing data.
Kean reiterated the need to incorporate palliative care across the cancer care continuum. He also reviewed the challenges in survivorship care, including transitions to new care providers and care settings, surveillance for recurrences, screening for secondary cancers, and managing the risk of late effects of treatment. There were calls for more training opportunities for a range of health care professionals in order to ensure an adequate and competent health care workforce to meet the needs of AYA patients with cancer.
Kean also stressed that a cancer diagnosis is a life-altering event, which, especially among the AYA population, can alter many hopes and dreams. AYAs with cancer face many challenges in work and school. Relationships may be strained, and many patients are concerned about whether they will be able to have children in the future. These patients also often experience financial hardship as a result of their diagnosis, and many struggle to main-
tain adequate health care coverage and access to care. The provisions of the ACA could help address those coverage and access challenges, he said, but they are not sufficient on their own. “We need to be speaking out on these issues,” he said. “We have low public knowledge of what is in the ACA. People still do not understand what is there, and we need to do a better job as a collective community to spread the word.”
Another common theme was the need for better ways to communicate with AYA patients. Kean said that it will be important to develop communication strategies and tools that are tailored to the way AYAs communicate among themselves, for example, via social networks and online tools.
Kean also stressed the idea of giving back. AYA cancer survivors at the workshop said that patients who have had a positive experience with their care are more likely to be willing to give back and participate in research. But, Kean said, investigators also need to give back to the participants by providing information about what they are doing with the data and what the results may mean to patients like them. “This is what happens in community participatory research all the time,” he said. “It is very important for us to help people understand what we are doing when we want to [engage them in] research, especially for those who do not have a lot of experience [with clinical research].
Noting the progress made since the 2006 NCI PRG report, Kean said it was encouraging to see momentum for making improvements in the care of AYA patients with cancer, and he urged the workshop participants to build on that momentum for further progress.
































































