9
The HIV/AIDS Epidemic in New York City
The panel planned to study in some detail the impact of the HIV/AIDS epidemic in several locales as part of an effort to understand the localized dimensions of the epidemic. Our plan had been to focus on three cities, New York, Miami, and Sacramento, to determine the epidemic's impacts in places with quite different social, cultural, and demographic characteristics. Unfortunately, it proved logistically and financially difficult to carry out this plan. Fortunately, however, since several members of the panel lived or worked in New York and had convened for regular discussions over the several years of the panel's life a group of experienced observers of the epidemic, the panel was able to complete one of its planned empirical studies, that of New York City.
"Completed" is not quite accurate: many aspects of the epidemic in New York City are not included in this chapter and much more needs to be done before a picture that is in any way complete can be presented. We refrain from calling this chapter a case study in the proper sense, since such a study, being only one and thus lacking comparisons with similar studies, would require much more detail and depth before either causal connections between the complex phenomena can be discerned or even tentative generalizations can be suggested. Still, the panel believes that the New York City study, as it stands, offers a vivid portrait of the epidemic in a particular place and illustrates with particular force the principal conclusions of this report: namely, the epidemic is not spreading uniformly throughout the population but is highly localized, and the epidemic is now progressing in
such a way that a convergence of social ills creates a nidus in which it can flourish. It is our belief that New York City, special though it may be, exemplifies these conclusions. In New York City, as in the United States, the epidemic is highly localized and is flourishing in social settings where there is a ''synergism of plagues" (Wallace, 1988).
Much of the attention given to the epidemic has focused on national estimates and national needs. Although these are perfectly appropriate concerns, it must be understood that ultimately the epidemic, its impacts, and the responses to the impacts are experienced in specific locales. The United States, unlike many European countries, is composed of states and other political subunits that can and do pursue quasi-independent policies in many aspects of social life. For instance, all states, counties, and most large cities have their own public health agencies, which have differing traditions and varying levels of quality. In addition, these subnational, geopolitical units often have different political, economic, welfare, and crime control practices, all of which are involved in dealing with HIV/AIDS.
Although these subnational jurisdictions are smaller in size and population than the country, they are not homogeneous social and cultural units. Affluent people live in some parts of a city, and poor people live in others; individuals of European descent live in some communities, and African Americans and persons of Latin descent live in others. In some cities there are residential communities of gay men and lesbians, but in many there are not. Because HIV is not spread through casual contact, the structure of social networks in different localities and the geographical mobility of persons engaging in risky behavior shape the transmission of the virus. Sexual relationships and the sharing of drug injection paraphernalia are not random activities, but are embedded in other patterns of social interaction. HIV/AIDS is thus a disease of neighborhoods and communities, of high-prevalence localities and low-prevalence localities. Even a cursory look at the patterns of CDC-defined AIDS cases suggests distinct patterns in different cities. For example, many cities have few intravenous drug users who are infected and hence few women and infants who are HIV positive, while others have many intravenous drug users and so many infected women and infants.
New York has always been described as "special," meaning that it is unlike any other city in the United States. This view has considerable truth in it: New York City is an unruly, chaotic urban place, which regularly seems to verge on being economically and politically unmanageable. Its residents are the children of old immigrants who came by boat and new arrivals just off an airliner. New York City is actually a large number of collaborating and competing communities with disparate levels of power and resources. Many of these communities have no direct contact with other communities and compete with each other over resources and entitlements
in distant arenas, while others directly confront each other on the streets of the city over specific pieces of turf.
This study only partly confronts the complexity of the city and its response to the HIV/AIDS epidemic. It does not, as it might, list all of the people who took leadership positions and made the limited institutional reforms that characterized the city's best efforts. It is therefore a somewhat gloomy and admittedly partial vision. There is little discussion about the local media and its responses and nonresponses to the epidemic. We have used articles in the local press to track various controversies. A number of commissions and committees have attempted to analyze the epidemic in New York and plan for the future. We have read and quoted from their studies, even though we do not describe their special efforts (e.g., Citizens Commission on AIDS for New York City and Northern New Jersey, 1991).
Other local studies of the epidemic are needed (see Andrews et al., 1989). We hope there are researchers who will attempt to find out what happened in Los Angeles, San Francisco, Miami, Houston, Dallas, and Atlanta, as well as in Chicago, Detroit, and Denver. We believe the research community needs to discover the stories of the epidemic from the perspectives of the streets of the South Bronx and the apartments of Chelsea, the emergency rooms and pediatric units of Harlem, Bronx Lebanon, Woodhull, and St. Vincent's Hospitals, and the offices of the Gay Men's Health Crisis (GMHC), AIDS Coalition to Unleash Power (ACT-UP), Association for Drug Abuse Prevention and Treatment (ADAPT), and God's Love We Deliver, as well as providing the epidemiological models and health cost estimates that are the accounting frames that are only mere summaries of the realities of human action.
COURSE OF THE EPIDEMIC
Current Situation
By March 1992, 37,952 cases of AIDS had been reported to the Centers for Disease Control (CDC) for the New York City metropolitan statistical area (MSA)—the five boroughs of New York City and the immediate suburban counties of Putnam, Rockland, and Westchester (Centers for Disease Control, 1992); the five boroughs account for more than 95 percent of the cases. Those cases comprised 37,062 adults and 890 children less than 13 years old: 17.6 percent of all adult and 24.7 percent of all child cases of AIDS reported to the CDC by health departments in the United States. The proportion of the national epidemic represented by the New York City MSA has declined somewhat over the course of the epidemic. For cases reported from March 1990 to February 1991, the proportion from the New York City
MAS was 15.6 percent; from March 1991 to February 1992, it was 14.8 percent
All these figures, however, are an underestimation of the numbers of actual AIDS cases. There are four sources of this underestimation, which mirror the undercount problems on a national level. The first is the lag in the reporting of cases from the local site in which the disease is diagnosed to the local health department; the next lag is from then until the cases are reported to CDC and entered into the AIDS Case Registry. In New York City, one-third of AIDS cases are reported to the city health department within 1 month of diagnosis, about 85 percent are reported by 6 months, and the count is as nearly complete as it is likely to be after about 15 months (New York City Department of Health, 1989a). According to the U.S. General Accounting Office (1989), the lag time between diagnosis and reporting is growing longer rather than shorter.
A second source of underestimation is the extent of undercounting, that is, the number of cases that, if diagnosed and reported, would meet the current CDC case definition. These are cases that are lost to the system by inadvertence and overwork, failures of paperwork, deliberate decision, or by death from other causes among individuals whose AIDS was not diagnosed because they were not in contact with the health care system. The proportion of undercounted cases varies by geographical location and by risk group (U.S. General Accounting Office, 1989; Buehler, Berkelman, and Stehr-Green, 1992).
A third source of underestimation of the dimensions of the epidemic is HIV-infected people who die from complications of the disease prior to a diagnosis of AIDS. This may be a very significant factor in New York City.
The final source of underestimation is the occurrence of either new opportunistic infections that are the result of HIV infection or infections specific to particular populations that do not conform to the CDC case definitions. These are viewed by some as indications of the changing natural history of the disease or as symptoms of HIV/AIDS among less studied populations.
Of the 26,336 cases of AIDS reported in the state by December 1989, 87 percent were from the five boroughs of New York City, and an additional 7.8 percent were from the four counties with the most intimate social and economic connections with the city (Nassau, Suffolk, Westchester, and Rockland)—in all, 95 percent of all cases reported in New York State (AIDS in New York State, 1989).
Whatever the precise number of cases of AIDS, deaths from the opportunistic infections that are associated with end-stage HIV disease accounted for a very large proportion of the total mortality among young men and women in New York City in 1989. Among men aged 25 to 44, AIDS was the leading cause of death: 31.6 percent of deaths of men aged 25 to 34 and
35.2 percent of deaths of men aged 35 to 44. Among women aged 25 to 34, AIDS accounted for 26.1 percent of all deaths; in addition, 10 percent of the mortality among women aged 15 to 24 and 17 percent of the mortality among women aged 35 to 44 was also directly attributable to AIDS.
Localization of the Epidemic
One of the most striking features of the HIV/AIDS epidemic is its concentration in and within large urban centers. This is manifested across the United States, and New York is no exception. As noted above, 87 percent of all cases in New York State are concentrated in the five boroughs of the city. But that is only the first level of concentration of the epidemic. Within the city itself, AIDS cases are concentrated both in individual boroughs and in neighborhoods within the boroughs. Data on various characteristics of AIDS cases by 41 neighborhoods in the five boroughs have been published by the New York City Department of Health (1990a,b,c,d,e). Although there are other ways to define neighborhoods, these 41 areas—10 each in Manhattan, Queens, and Brooklyn, 7 in the Bronx, and 4 in Staten Island—have the virtue of being used for a wide variety of other epidemiologic, health care, and planning purposes.
The incidence rates vary as much within New York City as they do across the counties of New York State. Table 9-1 presents data on the number of adult persons with AIDS by selected demographic characteristic or risk categories and ethnic groups, reflecting the intense concentration of the epidemic in certain city neighborhoods. The variation in Manhattan, which is the hardest hit of the boroughs, remains quite large (from 341 to 1,802 per 100,000 persons). A more precise pattern is evident when the cumulative AIDS case data for the city are plotted using zip codes; see Figure 9-1. Within the larger geographical units, as defined by the United Hospital Fund's community health areas, one can observe the zip code areas with the highest concentrations of cumulative AIDS cases. In vast areas of the city, cumulative AIDS cases are fewer than 175 per 100,000, but in a small set of zip code areas, the rates are more than 700 per 100,000.
A similar geographical pattern can be found in the data on rates of HIV antibody seropositivity among women bearing children in New York City. Since 1987 all infants born in New York State have been tested for antibodies to HIV in anonymous serologic surveys of blood routinely taken (from the heel) for testing for inherited metabolic disorders. Such surveys are indirect measures of the rate of HIV infection among newborns, since only a fraction of babies born to HIV-infected mothers are themselves infected and since an infant may carry antibodies from its mother but not in fact be infected. They are, however, accurate indicators of the serostatus of the mother. Of 359,470 babies tested in New York City between November 1987 and September 1990, 4,453 women were determined to be infected
TABLE 9-1 AIDS Cases by Neighborhoods in New York City, Cumulative Incidence from 1981 to June 1990
|
|
|
Percentagea |
|||||
|
Borough and Neighborhood |
Number of Cases |
Rate per 100,000 |
Women |
Gay Menb |
IVDU |
African American |
Hispanic American |
|
Manhattan |
10,523 |
— |
9 |
67 |
29 |
25 |
21 |
|
Washington Heights/Inwood |
487 |
348 |
10 |
59 |
32 |
39 |
36 |
|
Central Harlem/Morningside Heights |
1,107 |
722 |
22 |
32 |
59 |
81 |
11 |
|
East Harlem |
873 |
1,125 |
21 |
26 |
65 |
50 |
41 |
|
Upper West Side |
1,807 |
925 |
6 |
78 |
20 |
18 |
21 |
|
Upper East Side |
597 |
341 |
5 |
86 |
10 |
9 |
14 |
|
Chelsea/Clinton |
1,986 |
1,802 |
3 |
84 |
14 |
11 |
15 |
|
Gramercy Park/Murray Hill |
979 |
852 |
4 |
79 |
18 |
13 |
16 |
|
Greenwich Village/Soho |
1,175 |
1,524 |
2 |
81 |
17 |
10 |
13 |
|
Union Square/Lower East Side |
1,434 |
960 |
12 |
57 |
39 |
16 |
32 |
|
Lower Manhattan |
96 |
748 |
16 |
58 |
36 |
23 |
25 |
|
Bronx |
3,855 |
— |
22 |
23 |
64 |
37 |
53 |
|
Kingsbridge/Riverside Dr. |
114 |
163 |
14 |
44 |
39 |
26 |
36 |
|
Northeast Bronx |
269 |
174 |
16 |
34 |
47 |
53 |
28 |
|
Fordham/Bronx Park |
699 |
420 |
22 |
25 |
61 |
29 |
56 |
|
Pelham/Throgs Neck |
611 |
268 |
22 |
22 |
62 |
32 |
50 |
|
Crotona/Tremont |
748 |
730 |
24 |
21 |
64 |
41 |
55 |
|
Highbridge/Morrisania |
866 |
795 |
24 |
21 |
68 |
48 |
49 |
|
Hunts Point/Mott Haven |
548 |
1,047 |
22 |
16 |
73 |
27 |
70 |
|
Brooklyn |
5,297 |
— |
20 |
31 |
51 |
50 |
26 |
|
Greenpoint/Williamsburg |
700 |
450 |
22 |
19 |
67 |
32 |
56 |
|
Bensonhurst/Bay Ridge |
207 |
128 |
14 |
39 |
50 |
9 |
16 |
|
Downtown, Heights, Park Slope |
907 |
523 |
12 |
56 |
37 |
33 |
25 |
|
Bedford Stuyvesant/Crown Heights |
1,516 |
523 |
24 |
24 |
57 |
78 |
14 |
|
East New York |
406 |
361 |
22 |
20 |
65 |
57 |
33 |
|
Sunset Park |
207 |
296 |
19 |
27 |
57 |
10 |
64 |
|
Borough Park |
218 |
140 |
19 |
35 |
49 |
15 |
27 |
|
East Flatbush/Flatbush |
716 |
293 |
23 |
28 |
34c |
73 |
14 |
|
Canarsie/Flatlands |
147 |
110 |
24 |
35 |
41 |
31 |
14 |
|
Coney Island/Sheepshead Bay |
273 |
120 |
21 |
34 |
51 |
25 |
23 |
|
Queens |
2,916 |
— |
15 |
41 |
45 |
39 |
26 |
|
Long Island City/Astoria |
279 |
158 |
12 |
51 |
41 |
25 |
24 |
|
West Queens |
852 |
309 |
8 |
52 |
40 |
19 |
47 |
|
Flushing/Clearview |
160 |
88 |
14 |
50 |
32 |
20 |
25 |
|
Bayside/Littleneck |
42 |
65 |
14 |
29 |
33d |
14 |
17 |
|
Bridgewood/Forest Hills |
206 |
110 |
7 |
48 |
40 |
6 |
23 |
|
Fresh Meadows |
65 |
82 |
13 |
46 |
42 |
22 |
18 |
|
Southwest Queens |
257 |
147 |
14 |
45 |
44 |
25 |
25 |
|
Jamaica |
665 |
334 |
21 |
26 |
58 |
81 |
10 |
|
Southeast Queens |
252 |
172 |
22 |
36 |
41 |
62 |
12 |
|
Rockaway |
138 |
177 |
30 |
20 |
65 |
63 |
16 |
|
|
|
Percentagea |
|||||
|
Borough and Neighborhood |
Number of Cases |
Rate per 100,000 |
Women |
Gay Menb |
IVDU |
African American |
Hispanic American |
|
Staten Island |
357 |
— |
17 |
33 |
52 |
22 |
16 |
|
Port Richmond |
70 |
153 |
24 |
16 |
57 |
31 |
11 |
|
Stapleton/St. George |
188 |
188 |
19 |
40 |
45 |
24 |
19 |
|
Willowbrook |
38 |
47 |
8 |
39 |
45 |
3 |
13 |
|
South Beach/Tottenville |
61 |
43 |
8 |
18 |
71 |
18 |
15 |
|
Total Borough |
25,260e |
|
|
|
|
|
|
|
Total Neighborhood |
22,948f |
|
|
|
|
|
|
|
a Does not equal 100 percent because a person can be counted in more than one category. b More broadly, men who have sex with men. c Thirty-two percent of cases defined as other. d Twenty-six percent of cases defined as other. e 186 unknown addresses. f 2,126 cases without zip code. SOURCE: Data from New York City Department of Health (1990a,b,c,d,e). |
|||||||
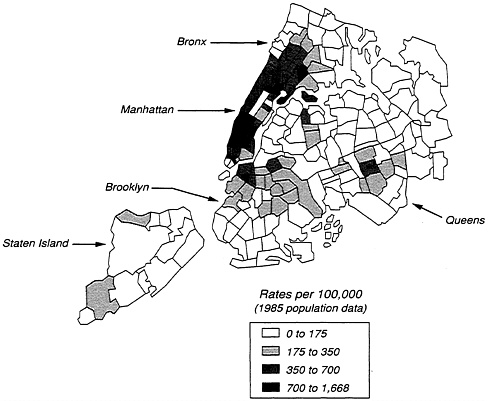
FIGURE 9-1 AIDS case rates in New York City, by zip code, as of April 1989.
SOURCE: Data from New York City Department of Health (1990a,b,c,d,e).
with HIV—a citywide seropositivity rate of 1.24 percent (Novick et al., 1991); see Table 9-2. This proportion has not changed substantially since testing of infants began, indicating there have not been rapid increases in seropositivity among women who are having children. This seroprevalence measure does not estimate the rates of HIV infection among all women of childbearing age: it excludes women who are not having children because of contraceptive use, infertility, celibacy, or spontaneous or induced abortion.
These data for childbearing women show a pattern similar to the AIDS data for women. Rates are high among African American (2.21 percent positive) and Hispanic women (1.41 percent positive) and particularly high for women aged 25 to 34. However, the rates vary substantially for both African American and Hispanic women by borough of the city; again, the highest rates are found in Manhattan and the Bronx. Since there is evidence of higher rates of sexually transmitted diseases among African American women than other women, there may be some consequent reduction in
TABLE 9-2 Seroprevalence Among Mothers of Newborns in New York City, November 1987-September 1990, by Borough and Neighborhood
|
Borough and Neighborhood |
Number Tested |
Number Positive |
Percent Positive |
|
Manhattan Total |
44,141 |
697 |
1.58 |
|
Washington Heights/Inwood |
8,808 |
57 |
0.65 |
|
Central Harlem/Morningside Heights |
7,907 |
213 |
2.69 |
|
East Harlem |
5,057 |
163 |
3.22 |
|
Upper West Side |
5,239 |
39 |
0.74 |
|
Upper East Side |
4,352 |
16 |
0.37 |
|
Chelsea/Clinton |
2,894 |
61 |
2.11 |
|
Gramercy Park/Murray Hill |
2,461 |
36 |
1.46 |
|
Greenwich Village/Soho |
1,500 |
4 |
0.27 |
|
Union Square/Lower East Side |
5,071 |
95 |
1.87 |
|
Lower Manhattan |
852 |
13 |
1.53 |
|
Bronx Total |
50,512 |
853 |
1.69 |
|
Kingsbridge/Riverside Dr. |
2,091 |
7 |
0.33 |
|
Northeast Bronx |
5,165 |
63 |
1.22 |
|
Fordham/Bronx Park |
10,128 |
125 |
1.23 |
|
Pelham/Throgs Neck |
8,655 |
95 |
1.10 |
|
Crotona/Tremont |
9,805 |
183 |
1.87 |
|
Highbridge/Morrisania |
9,093 |
225 |
2.47 |
|
Hunts Point/Mott Haven |
5,575 |
155 |
2.78 |
|
Brooklyn Total |
89,240 |
1,169 |
1.31 |
|
Greenpoint/Williamsburg |
10,782 |
148 |
1.37 |
|
Bensonhurst/Bay Ridge |
4,343 |
16 |
0.37 |
|
Downtown, Heights, Park Slope |
7,509 |
127 |
1.69 |
|
Bedford Stuyvesant/Crown Heights |
21,134 |
452 |
2.14 |
|
East New York |
7,838 |
119 |
1.52 |
|
Sunset Park |
4,670 |
46 |
0.99 |
|
Borough Park |
7,677 |
29 |
0.38 |
|
East Flatbush/Flatbush |
13,710 |
155 |
1.13 |
|
Canarsie/Flatlands |
4,367 |
24 |
0.55 |
|
Coney Island/Sheepshead Bay |
7,210 |
53 |
0.74 |
|
Queens Total |
59,550 |
376 |
0.63 |
|
Long Island City/Astoria |
5,337 |
42 |
0.79 |
|
West Queens |
13,010 |
70 |
0.54 |
|
Flushing/Clearview |
6,441 |
15 |
0.23 |
|
Bayside/Littleneck |
1,828 |
1 |
0.05 |
|
Bridgewood/Forest Hills |
5,269 |
20 |
0.38 |
|
Fresh Meadows |
2,239 |
4 |
0.18 |
|
Jamaica |
9,468 |
113 |
1.19 |
|
Borough and Neighborhood |
Number Tested |
Number Positive |
Percent Positive |
|
Southwest Queens |
6,953 |
36 |
0.52 |
|
Southeast Queens |
5,212 |
36 |
0.69 |
|
Rockaway |
3,793 |
39 |
1.03 |
|
Staten Island Total |
11,835 |
68 |
0.57 |
|
Port Richmond |
1,881 |
25 |
1.33 |
|
Stapleton/St. George |
3,200 |
27 |
0.84 |
|
Willowbrook |
2,306 |
6 |
0.26 |
|
South Beach/Tottenville |
4,448 |
10 |
0.22 |
|
New York City Total |
255,278 |
3,163 |
1.24 |
|
SOURCE: Data from New York City Department of Health (1990a,b,c,d,e). |
|||
childbearing capacity that would result in an underestimation of the seropositivity rate among this group (Aral and Holmes, 1990).
HIV seropositivity for women of childbearing age follows the general geographical pattern of AIDS cases for women and intravenous drug users in the city. The rates of highest seropositivity can be seen in the band extending from the northern edge of Manhattan into the central Bronx, across Manhattan below midtown, and in a solid band across the northern edge of Brooklyn. The scattered nature of the areas of high seropositivity suggests the decentralized and local nature of the epidemic in large portions of the city.
Predicting the Future of the Epidemic
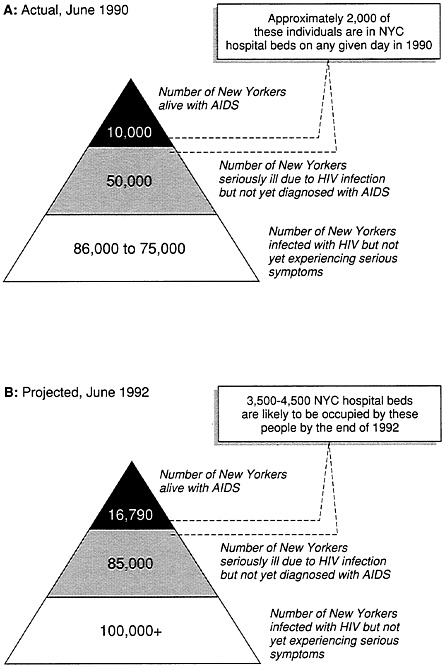
As the AIDS epidemic evolves, the proportion of persons at various stages of the disease has also been changing. If a major surge in infections in New York City occurred in the late 1970s and early 1980s, the early to mid-1990s should be the period, in the absence of effective therapies, when a majority of those who were infected will begin to show the symptoms of "frank" AIDS. Although the distributions in Figure 9-2 reflect substantial errors of measurement, they offer some numerical guidance as to what the future has in store for the city. The number at the apex of each pyramid is an indicator of the impact on the acute-care components of the health care system. The numbers in the two lower strata of each pyramid indicate people in the early stages of disease who could benefit from prophylactic measures to prevent or delay the onset of opportunistic infections. Those in the middle strata of the pyramid will require increased levels of outpatient care.
The New York City Department of Health estimates that the incidence of new HIV infections is about 2 percent per year, which would add about 4,000 new cases to the total each year at the present time (Carey, 1990). If this incidence figure remains stable and there is substantial future mortality (which would reduce the numbers of persons with HIV/AIDS), the prevalence of persons with HIV/AIDS in the city should decline substantially by the end of the 1990s.
Estimating the size of a present or future epidemic is not, however, as it might seem superficially, a neutral scientific act. It is a complex calculation that works with uncertain numbers, and they can be manipulated for many purposes. The results often have political reverberations. A July 1988 report by former health commissioner Dr. Stephen Joseph reduced by one-half the estimated number of HIV-infected individuals (Bayer, 1991; Lambert, 1988a,b); the original estimate of 400,000-500,000 was revised to a range of 149,000 to 225,000, provoking a confrontation with AIDS organizations. The suddenness of the change created an outcry within the larger AIDS community that garnered considerable press attention (Lambert, 1988a,b,c,d; Trafford, 1988; Loomis, 1989a,b,). The revised estimate was part of a general rethinking of the dimensions of the epidemic (Centers for Disease Control, 1990), but in New York City it seemed to presage a decline of interest in those who were ill or would become ill in the near future. Despite this initial reaction, however, the reduced numbers have become the accepted figures.
In the most recent report of the New York State Department of Health (1990), three different modeling methods were used to estimate the future course of the statewide epidemic by risk group, producing three substantially different estimates. All are included in the report to show the significant difficulties in generating ''precise" estimates of the future course of the epidemic. Indeed the estimates in 1990 vary considerably from those made in 1989. Of particular interest are the differences in the estimates of the future course of the epidemic among women. Modifications in the program used to estimate the logistic growth curve, which assumed very high rates of sexual partnering of intravenous drug users with nonuser partners, resulted in estimates of women infected through sexual contacts with men that are about three times higher by 1996 than are estimates produced by other methods. Studies of the actual sexual partnering patterns of women in New York City do not support such a high estimate (Fordyce et al., 1991). In the absence of additional systematic studies of sexual partnering and sexual behaviors in the general population, estimates will inevitably be very imprecise (see below).
If the projected decline in expected number of AIDS cases among all groups at risk is correct, it may be explained by a number of possible factors, including:
-
overestimation of the size of risk groups. There may have been fewer people in the identified risk groups (men who have sex with men or intravenous drug users) than was originally estimated in the mid-1980s.
-
overestimation of the proportion of people who are HIV positive. There may have been fewer persons in the identified risk groups who were infected because those who fell into the seroprevalence studies were not a representative sample of the social groups to which they belonged. This would mean that fewer persons have HIV/AIDS than expected.
-
reductions in high-risk behaviors early in the epidemic. Changes in sexual practices among gay men may have occurred sufficiently early in the epidemic so that the number of men who might have been expected to become infected in the period between 1982 and 1986 was dramatically reduced. This argument is supported by the rapid decline in rectal gonorrhea rates observed in New York City by Fordyce and Stoneburner (1990) during this period and by other studies of rectal gonorrhea reported by CDC for other cities (Centers for Disease Control, 1990:16). Similar changes in risk behaviors may have also occurred among intravenous drug users, although these changes are less well substantiated.
-
impact of the use of prophylactic medications on the onset of HIV-associated infections. The decline in the diagnoses of new AIDS cases may reflect the longer period between HIV infection and the appearance of opportunistic infections of those persons who are being treated with antiviral drugs and the early prophylactic treatment of Pneumocystis carinii pneumonia.
-
increase in outpatient treatment of persons with HIV before and after the onset of opportunistic infections with delays in reporting. Anecdotal evidence and a few studies suggest that many physicians do not report AIDS diagnoses among outpatients in a timely fashion (indeed, the majority of AIDS case reports come from hospitals). This produces an unmeasured delay in reporting as well as the loss of some cases to the record-keeping system (Greenberg et al., 1990). This is more likely to occur among those populations with access to private health care, and it interacts with the effects of prophylactic care.
-
undercounting of the morbidity and mortality that is associated with HIV infection as well as the failure to count persons who would have met the criteria for an AIDS diagnosis. This factor is of particular importance in New York City, where intravenous drug users make up a large proportion of the infected population. Using a variety of data sources, Stoneburner and his colleagues estimated that instead of the 2,440 narcotics-related AIDS deaths that were expected (on the basis of historical experience in the period studied) (Stoneburner et al., 1988:918):
[there was] a cumulative number of 6,157 narcotics-related deaths, 1,197
of which were reported as AIDS cases. Subtracting the expected 2,440 deaths and the 1,197 deaths reported as AIDS cases from the 6,157 actual deaths leaves 2,520 excess deaths that we suggest are HIV-related, but not yet recognized as AIDS.
Adding those deaths to the total number of deaths among intravenous drug users officially attributed to AIDS would increase the total number of HIV-related deaths of intravenous drug users in the official case registry by 35 percent. Such an undercount has dramatic consequences for public-and private-sector responses to the epidemic in New York City, where intravenous drug users comprise one-half of the recognized AIDS cases.
The number of women with HIV/AIDS, their rates of morbidity and mortality, the misfit between their symptoms and CDC-defined AIDS, and their access to health and welfare entitlements associated with an AIDS diagnosis are also deeply controversial issues and are especially important in New York City, where women represent approximately one-fifth of new AIDS cases. In 1988-1990, women accounted for nearly 20 percent of new AIDS cases in the Northeast as a whole (Miller, Turner, and Moses, 1990). Using data from New York State, the Newborn HIV Seroprevalence Study (Lessner, 1991) reports that an estimated 25,196 women aged 15 to 44 were infected with HIV during the period of 1981-1988. From these data, Lessner estimates that there will be 8,295 new cases of AIDS among women in that age group between 1989 and 1993 and about 2,000 new cases in 1993. Using sexual behavior data from a probability sample survey of women in New York City, Fordyce et al. (1991) modeled the number of women in New York City infected with HIV as the result of sexual contact with intravenous drug users. According to their model, new infections for women aged 15 to 44 in 1988 ranged between 867 and 1,668, and the total number of women infected by this mode of transmission for the 1977-1988 period ranges from 5,390 to 10,230 (the midpoint is 7,810). These data suggest that there will be substantial growth in the number of HIV-infected women in the 1990s and, as a consequence, an increase in the number of children born with HIV.
THE TWO EPIDEMICS
From the beginning, New York has had at least two socially, and therefore epidemiologically, separate epidemics. The first involves two linked, but not overlapping, populations of men who have sex with men. One comprises the gay community, which is primarily white but includes men from all ethnic groups. The other includes men of African or Hispanic descent whose sexual contracts are in semi-independent, ethnically homogeneous sexual communities that are only somewhat identified as gay.
The second HIV/AIDS epidemic is composed of intravenous drug users,
their sexual partners, and their children, who largely reside in the impoverished, ethnically segregated communities of the inner city. In recent years, the ratio of AIDS cases between men who have sex with men and male intravenous drug users has reached parity, and there has been a significant increase in HIV/AIDS among women and children.
For the period from 1982 to 1985, the proportion of women diagnosed with AIDS in New York City hovered around 10 percent. Since 1985 it has increased steadily each year: 12.4 percent in 1986, 15.8 percent in 1987, 16.4 percent in 1988, and 21.7 percent in 1989 (based on incomplete data for the year) (AIDS in New York State, 1989:60). Of the total number of female AIDS cases reported in New York State by December 31, 1989, approximately 57 percent were reported to have been infected through their own drug use and about 23 percent were infected through sexual contact with a drug user. There is no difference by ethnicity in these proportions (New York State Department of Health, 1989).
Epidemic #1: Men Who Have Sex with Men
In June 1981 the Centers for Disease Control reported that between October 1980 and May 1981, five young gay men had been diagnosed with Pneumocystis carinii pneumonia, an illness that would soon be so common that it would become known by its initials, PCP. The next month CDC reported that 26 cases of the formerly very rare Kaposi's sarcoma (KS) had been diagnosed among gay men in the prior 30 months. These reports provided the first intimations of an epidemic that would infect very large numbers of men who had sex with men. A decade later, the HIV/AIDS epidemic has passed through the stage of being regarded as the "gay plague" or being referred to as a "gay-related immune disorder."
Today, the epidemic has manifested itself in other populations, and the rapid spread in new infections in the gay community has slowed somewhat. However, it must be noted that of the approximately 1 million persons infected with HIV in the United States by the end of 1989, between one-half and two-thirds are men who had sex with men. Although gay men responded rapidly with preventive education, patterns of safer sex are not constant across groups and regions, and there is still concern that micro-epidemics may flare up again in the gay community (Stall et al., 1990).
In the period between 1981 and 1991, large numbers of gay men became ill and many died. Many others can be expected to become ill over the next 4 years. This is nowhere more true than in New York State, where it is estimated that by 1996 between 36,000 and 47,000 men will have been diagnosed with AIDS (using the current case definition) (New York State Department of Health, 1990). Between 75 and 80 percent of those men will
have died at the end of 1996 if there is no substantial advance in available treatments.
Scholars have noted that plagues and natural disasters have similar psychological consequences (Erikson, 1976). Both shatter the sociocultural order of a community and cause massive emotional reactions among the survivors, which typically appear in the form of collective and individual traumas. Collective trauma denotes the loss of communality—the loss of a network of relationships and shared meanings that provide intimacy, support, and a sense of self that ties individuals to the social order. Individual trauma refers to the emotional responses to death or devastation, which are shock, numbness, disorientation, guilt, and emotional depletion.
The HIV/AIDS epidemic has had many of these consequences for the gay community and the individuals who are part of it. Of particular importance is the epidemic's impact on a youthful cohort among gay men (those between 25 and 45 in 1980). Death in the United States is usually the province of the elderly, and its incursion into a youthful community means that social and psychological issues that are normally allocated to the end of the life course have to be dealt with at an early age.
An appreciation of the impact of the epidemic in the gay communities requires more than calculation of the numbers of persons infected, ill, or dead. The HIV virus and the emerging gay and lesbian community cultures in New York interacted in ways that profoundly influenced the course of the epidemic, the general public response to it, and the institutional structures and social identity of the gay community.
Evolution of the Gay and Lesbian Community
The pre-HIV/AIDS gay and lesbian community in New York City developed out of the stigmatized social conditions that existed prior to mid-1960s. From World War II until the end of the 1960s, persons identified as "homosexuals" by the medical profession and "dykes," "queens," "fags," and ''degenerates" by the public (Levine, 1979) sought to establish identities free of social marginalization and stigma and the harsh social sanctions they fostered (Weinberg and Williams, 1974). New York State criminalized same-sex contact and solicitation, which exposed lesbians and gay men to police harassment, imprisonment, and blackmail. Most mental health professionals considered both female and male homosexuality as a curable form of mental illness, which left these individuals open to mandatory psychotherapy and psychiatric hospitalization. Ridicule, ostracism, and even physical violence from family, friends, and strangers were common (Weinberg and Williams, 1974). Stigmatization thus shaped the structure of New York's lesbian and gay community. The threat of sanctions led to the formation of isolated social networks that functioned as surrogate kin structures and included
friendship cliques providing companionship, emotional support, and material aid (Helmer, 1963).
During the 1950s the homosexual community was discreetly clustered within several Manhattan and Brooklyn neighborhoods and entertainment zones (Weinberg and Williams, 1974). Middle-or upper-class lesbians and gay men filled the apartment buildings and townhouses of the East Side, Greenwich Village, and Brooklyn Heights (Helmer, 1963). Most of these men and women were white; only a handful were black or Puerto Rican. Working-class lesbians and gay men, who were predominantly white except for a sizable Puerto Rican contingent on the West Side, lived in tenements and rooming houses of Times Square, the seedy parts of Greenwich Village, and the Upper West Side. These neighborhoods also contained clandestine concentrations of lesbian and gay gathering places (Weinberg and Williams, 1974).
Stigma and oppression were the most important features of the pre-1960s homosexual community and the individuals who constituted its membership. The constant dangers associated with same-gender erotic desire produced a secret world that has been called the "closet culture." The belief that same-sex desires constituted immorality or pathology blocked some lesbians and gay men from having erotic contacts. The threat of exposure, entrapment, or involvement with police raids forced some lesbians and gay men to shun the opportunities for sexual or emotional relations. Thus, the homosexual community in New York City prior to the 1950s and 1960s was relatively fragmented, secretive, and constantly under threat. Some individuals were entirely socially isolated from the community, others used it only as a sexual marketplace, and still others lived in small friendship cliques. Most concealed their sexual desires to family, friends, coworkers, as well as their religious counselors.
The lesbian and gay liberation movement of the 1960s and early 1970s significantly reduced the stigma placed on female and male homosexuality (Marotta, 1981). The decision to embrace the names "lesbian" and "gay" was similar to the decision by "Negroes" to rename themselves "blacks,'' to claim a name that was formerly an epithet. The gay liberation movement partook in the same spirit that energized the feminist, countercultural, antiwar, and civil rights movements. Its activists strove to eradicate the stigma attached to same-gender sex and, within the sphere of sexual preference, to promote personal autonomy and the right to live within the larger society in accord with one's own values and choices (Adam, 1987). In addition, activists promoted values of self-expression and personal liberation, especially in regard to the use of drugs and to sexual behavior (Marotta, 1981). Political and legal protests were used to counter antigay and antilesbian discrimination in New York City. In response to these activities and general cultural changes, the New York State sodomy statute was declared
unconstitutional, and mental health professionals officially ceased treating same-sex love as a psychological disorder (Bayer, 1981).
Destigmatization of same-sex desires within the gay and lesbian and gay community during the 1970s allowed many gay men and lesbians to regard themselves as normal, healthy, and sexual. The parallel increase in social tolerance and modest decline in discrimination from the larger community allowed lesbians and gay men to "come out" before a wide range of audiences. Thousands of white, middle-class New Yorkers stopped passing as heterosexual and publicly expressed their gay identity. This identity took on the tones of an "ethnic" self-conception and fostered a massive expansion of the community's territorial, institutional, and cultural base.
The creation of a visible community with a wide range of services had wealth-creating consequences. Businesses that were owned by and that employed gay men and lesbians gained patronage. The community acquired many features of traditional ethnic groups that trade preferentially within their community group. Such practices enabled gay men to buy housing in the local community, and it increased discretionary funds for community service and political activities.
Gay liberation involved both changes and continuities in the sexual styles of gay men and lesbians. The visibility of the community and its members meant that gay sexuality did not necessarily involve personal secrecy. Changes in gender codes meant that many gay men began to adopt entirely masculine styles of personal presentation.
Some elements of prior practice continued for men whose sexual lives had been heavily secretive and repressed by social conditions of the past. This was particularly so in the maintenance of the tradition of "tricking" (having casual sex) with large numbers of partners. The increased visibility, size, and density of the gay community and the public emergence of institutions that were designed to promote easy congregation (baths, bars, discos) made meeting other men in anonymous and erotic circumstances far easier than it had been. There is limited evidence from interviews conducted by Kinsey in the 1940s that even under historically restricted conditions men who were part of the "homosexual" community accumulated large numbers of partners. Under the more open circumstances of the 1970s there were substantial increases in numbers of sexual partners by men in the community (Blumstein and Schwartz, 1983).
Levine has identified the visible world that emerged in these circumstances as dominated by the "clone culture" (Levine, 1989). The term clone emerged from the similarity in look and life-style among a large number of men that set them apart from other groups in the gay world. Levine's point is that not all gay men were clones, but that this culture represented the gay world in popular culture (in the same way that "queen" culture, "drag," and ''camp" had done so in earlier eras). Four features distinguished clones:
(1) strongly masculine dress and deportment; (2) uninhibited recreational sex with multiple partners, often in sex clubs and baths; (3) the use of alcohol and other recreational drugs; and (4) frequent attendance at discotheques and other gay meeting places. Clone culture with its pattern of sexual availability, erotic apparel, multiple partners, and reciprocity in sexual technique became an important organizing feature of gay male life during the 1970s. It also became a seedbed for high rates of sexually transmitted diseases as well as frequent transmission of the hepatitis B virus. Many treated sexually transmitted diseases as a price that had to be paid for a life style of erotic liberation.
Initial Response to the Epidemic
The response of the gay community to the beginning intimations of an epidemic were complex. The historical evidence is that the first response of afflicted communities and individuals to epidemics is denial and minimization. Gay men and the communities in which they lived were no exception. The accumulating evidence that the new disease (which was not yet called AIDS) was probably transmitted by sexual contact and that people with many sexual partners who were living in "the fast lane" were either already infected or likely to become infected was met with some disbelief. Some of the disbelief was in the form of "not me," but other responses were more ideological. In the minds of some, the liberation of gay life was identical with the expression of open and free sexuality: gay identity was focused on sexual freedom, and the denial of sexual expression seemed to be a denial of much that the gay movement had struggled for.
Those whose life-styles were not centered around the sexual aspects of gay life were more receptive to the first messages of changing behavior. Some were in the health professions, others were in conventional paired relationships, others had work that took them outside of the recreational life of the gay community, and still others who simply disapproved of what they saw as the sexual excess of some gay male life. Nevertheless, all gay groups urged voluntary behavior changes rather than public health intrusions into the civil rights of those at risk.
The early days of the epidemic in New York saw deep conflicts in the gay community. On one side were those who did not see the small number of cases as evidence for the need to change their sexual conduct and those who felt that the urging to change was coming from the medical profession that so recently condemned them as perverse and neurotic. The message and the messenger seemed untrustworthy. However, as early as mid-1982, community members were beginning to respond to the epidemic in an organizational way by the formation of Gay Men's Health Crisis (GMHC) (officially founded in November 1981) with planning meetings and fund raisers
that occurred earlier that summer (Chambre, 1991). As the number of ill and dying rose, it was clear that the community could not, by itself, care for them and that there was a serious need for governmental intervention. From 1981 to 1983 there was increasing community pressure on local and state governments to respond to what was beginning to be recognized as a profound health crisis.
In comparison with the rapid mobilization of public resources in San Francisco, where the gay community was a powerful political voice, the New York public health system moved slowly in response to the epidemic. In contrast to San Francisco, the New York gay community was a much smaller political constituency (San Francisco has a population of approximately 750,000, New York City, approximately 11 million) and had a much more complex political structure. GMHC and other volunteer agencies helped fill an institutional vacuum, focusing on the epidemic among gay men that was happening in their own community. The openly active gay community was willing to recognize it as their own. This contrasted with other similarly afflicted communities. As late as 1987 the major institutions of the African American and Hispanic communities had made only minimal formal responses and there was little evidence of AIDS-related organizations.
Substantial behavioral changes in sexual practices were documented in the gay community—the reduction of unsafe sex, particularly anal intercourse, and numbers of sexual partners. These changes antedated the initiation of formal educational programs to promote behavior change. Studies both in San Francisco and New York indicated that changes in behavior had begun by 1982-1983. By 1986 there had been dramatic declines in risky behavior in all age groups among gay white men (Hansfield, 1986). In New York, studies of the rectal gonorrhea rate (a proxy for risk of HIV transmission) showed about a 10 percent drop between 1981 and 1983 and a drop of close to 80 percent between 1983 and 1986. Similar declines are believed to have occurred among African American and Hispanic men, although lagging behind changes among white men). Martin, Garcia, and Beatrice (1989) reported that the gay-identified men in a nonrandom sample of 745 individuals had reduced their numbers of partners and incidents of anal intercourse by three-quarters (see also Siegel and Glassman). This change appears to have occurred as a result of informal feedback into the community from community-based organizations rather than from formal education programs sponsored by specific health agencies.
Evolution and Role of Volunteer Organizations
By the late 1980s the rate of new HIV infections among gay-identified men began to fall—partly because those at highest risk had already been
infected, but also because those still at risk had modified their behaviors. Young gay men were not getting infected at the rates that characterized the age cohort that came of age between 1975 and 1985. This period marked a major transition in the New York gay community. The volunteer agencies had emerged as a potent political force. Voluntary efforts had been the primary force in staying the epidemic of transmissions within the gay community and had also supplied most of the social support resources of those who were ill. The reduction in new infections and steady increase in the numbers of persons needing health care and other services caused the major volunteer agencies to turn their attention to issues of treatment and care. This attention extended to both the delivery of care and attempts to mobilize the governmental sector.
The Gay Men's Health Crisis (GMHC) is probably the largest central volunteer agency in New York providing supportive care to the gay community in New York City. Their activities included buddies; crisis intervention; support in securing and preventing discrimination in housing, health care, and employment; and providing educational services. By June of 1991, it had served 11,362 clients and had a current caseload of 3,266 persons. GMHC has taken stands on most of the major issues facing the gay community and attempted to extend its outreach to nongay-identified and other men who had sex with men throughout the city.
Although recognizing GMHC achievements, some within the gay community thought its political strategies were too moderate. The perceived need for a more radical political effort gave birth to ACT-UP (AIDS Coalition to Unleash Power). ACT-UP was created as a nonhierarchical direct action organization that made decisions concerning demonstrations ("actions" or "zaps") or policies on the basis of an open democratic forum. Although a committee structure developed around specific issues, the town meeting format has sustained itself in the face of substantial increases in membership. There are now ACT-UP groups in many cities across the country, and there is still no central office.
ACT-UP/New York has been an important player in conflicts within the city in a variety of areas and has extended its interests well beyond the gay-identified community. ACT-UP has been visible in a number of New York City conflicts, including those over the reduction in estimates of numbers of persons with HIV in New York City (Bayer, 1991); the appointment of Woodrow Meyers as Health Commissioner (Purdum, 1990; Bayer, 1991); the dispute about condoms in the schools; a continuing conflict with Cardinal John O'Connor about various positions of the Roman Catholic Archdiocese of New York related to AIDS and gay life; and attempts to improve police practices in dealing with the gay and lesbian community (ACT-UP/New York, 1991). On the national scene, ACT-UP/New York has played both an insider's and outsider's role in putting pressure on the National
Institutes of Health, the Food and Drug Administration, and the major pharmaceutical houses to speed the development and release of new drugs (Bryant, 1991; Taylor, 1990).
The tactics of ACT-UP, while often compelling and sometimes effective, have also generated strong criticism, and some gay activists believe them to be counterproductive. Events such as the disruption of U.S. Health and Human Services Secretary Louis Sullivan's speech at the International AIDS conference in 1991 and the zaps at St. Patrick's and Holy Cross cathedrals aroused considerable criticism, leading observers to wonder whether they were, on balance, more harmful than helpful.
Volunteer efforts on AIDS have been critical elements in delivering services and reducing the financial impact of the disease, and they have characterized New York's response from the very first moments of the epidemic. Volunteering in a systematic way, however, has been primarily a characteristic of the gay community (Chambre, 1991). This is not to say all volunteers are AIDS-infected gay men. They include the uninfected, women, persons who are not themselves gay, as well as a large number of professionals from a variety of fields.
Agencies and organizations that serve the gay community have attempted to reach other groups of men who have sex with men, intravenous drug users, and women, with mixed results. Of particular importance has been outreach to men who have sex with men in communities that have limited links to the organized gay community. Many African American, Hispanic, and Asian American men have strong contacts with the largely white gay community that is centered in Manhattan. However, these men find themselves caught between their identities as gay men and their bonds with their own ethnic communities that have negative attitudes toward men who have sex with men in general and toward gay men in particular. In addition, the white gay community also exhibits racism, which limits outreach efforts.
Men Outside Identified Gay Communities
Men who have sex with men are found not only in the predominantly white gay community, but also among men of African and Hispanic descent who are only somewhat identified as gay. At the onset of the epidemic little was known about men who had sex with men in various communities of the city. What has been learned about African American men and Hispanic men has largely emerged from research concerning the rates of HIV infection in these groups and ways of preventing further infection. Of all African American men who have been reported with AIDS in New York State, 33 percent are reported to be men who had sex with men; 49 percent are intravenous drug users; and 5 percent have both risk factors. Of all Hispanic men who have been diagnosed with AIDS, 33 percent are reported
to be men who have sex with men; 55 percent are intravenous drug users; and 5 percent have both risk factors (New York State Department of Health, 1990). Nationally, the majority of racial and ethnic minority men diagnosed with AIDS have contacted the disease as a result of having sex with men. However, because of the stigma of being known as someone who has sex with men, it is believed that there have been some false reports by African American men that their risk behavior is intravenous drug use.
A number of social networks in the African American community of men who have sex with men are epidemiologically separate from the gay community and show markedly different patterns of infection. A study of 57 African American gay men (who did not self-identify with the predominantly white gay community), raised in stable middle-or working-class, two-parent families showed that this discrete population was not HIV-infected. They did not observe safe sex (at the time of the interviews in 1988, none was using condoms), and sexual encounters often followed drinking in bars, at parties, and in private homes, but they selected partners from a neighborhood pool that was as yet uninfected (Hawkeswood, 1991). Other subgroups of men who have sex with men in the African American community appear to be at very high risk for infection because of involvement in street prostitution and "hustling." What little is known about these groups through anecdotes and informal reports suggests relatively high rates of unprotected sex as well as a considerable risk of arrest and imprisonment.
The Hispanic communities in New York City are enormously complex, and many have not been studied at all. An estimated 400,000 Dominican immigrants live in New York City, and Cubans and others from the Caribbean and Central America are also represented, but the major Hispanic community in New York City is Puerto Rican. All share a common cultural perspective on sexuality that is vastly different from prevalent American beliefs. Researchers have found that men who have sex with men in these cultures are divided roughly into two groups, "passivos" and "activos." Activos insert their penis into another man, either orally or anally, and the passivos receive a penis: these are usually, though not always, exclusive roles. Activos are defined as men since they insert, which is what men do to women, and passivos are defined as women since they receive the penis. The inserter is not viewed as homosexual: thus, the distinction between ''heterosexuality" and "homosexuality" as commonly understood does not fit this group. (Similar distinctions are found among prisoners and other groups of men who do not view the inserter as homosexual.)
The strength of this pattern depends on the level of acculturation of Hispanic populations into the culture of the United States. Carrier (1989) reports that the active/passive pattern is common among men in Mexico and among recent Mexican immigrants to the United States. Acculturation produces sexual styles more equivalent to those of white gay-identified men.
The pattern appears similar among New York Hispanic men. The continuing belief that the passive homosexual male is a woman has consequences for "coming out" in this community. There remains a tendency for some young men to offer an effeminate self-presentation; cross dressing is common, and some engage in prostitution as women. Such belief structures have important implications for public health practices directed to these communities.
There are few volunteer organizations that work solely with minority men who have sex with men. A general denial of the existence of HIV/AIDS characterizes many Hispanic communities in the city, accompanied by specific denials regarding men who have sex with men who have HIV/AIDS. In part this is a denial by the larger community that there are such men, but another element is the denial by the men themselves. Men who do not self-identify as gay may have some difficulty accepting services directed at those who are identified as gay or homosexual (Russell, 1990). The higher rates of morbidity and mortality in these populations and their lack of access to medical services may result in part from these cultural norms.
Individual Impacts: Discrimination and Impoverishment
For the reasons noted above—recognized rates of infection, a willingness to accept the reality of the epidemic, and active community-based groups monitoring its evolution—the impact of the epidemic has been best recorded in the gay-identified community. The impact on other infected communities is not well documented, and when their histories are better understood they may differ in important respects from the New York gay community. Nonetheless, many features of the experience are common.
HIV/AIDS is a disease that increases the likelihood of discrimination and reduces the economic prospects of individuals even if they do not lose their jobs. It is impoverishing, eliminating opportunities and destroying social networks. The new social networks it creates are often linked to dealing with illness and death.
A major portion of the work of various community-based organizations is providing assistance for gay men with HIV who have encountered discrimination. For example, GMHC provides free legal service to all persons in the New York City area diagnosed as HIV positive. In 6 years they have served 4,000 clients with problems in housing, insurance, health care, and employment. A survey of 60 persons with AIDS and of AIDS service organizations by the New York City Commission on Human Rights (1989) reported cases of discrimination, noting the social impact of discrimination
on costs of and access to health care, social services, education, and prevention must be factored into all programs and policy planning.
As previously noted, one of the results of the gay liberation movement was an increase in income and assets of the gay community. Much of the wealth consists of salary and wages, rather than savings. A prolonged illness of any type can impoverish even the solidly middle-class and professional segments of the population (Hansell, 1990); AIDS, however, can be particularly quick in producing financial ruin. Many gay men have been fired when their HIV disease was discovered. Most find it difficult to continue working full time as the disease progresses, yet they hesitate to stop work because of the almost inevitable loss of health insurance coverage. Many who are able to continue working discover that they are occupationally immobile because of health insurance considerations.
Those who are ill find themselves caught in a cycle of high treatment costs and inadequate insurance coverage. To avoid workplace discrimination, men sometimes pay for their own health care rather than submit bills to health care insurers (Oppenheimer and Padgug, 1991). An important share of the costs of HIV/AIDS treatment is the expense of drugs, and typical insurance restrictions on the coverage of prescription drugs (including exclusion of experimental drugs) results in high, out-of-pocket costs. The decline in the costs of AZT, the primary drug of treatment, from $10,000 to between $2,000 and $3,000 a year has been a help, but the costs of other drugs remain high.
The declining ability to work and the daunting costs of health care for HIV disease results in the phenomena of individuals' "spending down" into Medicaid. While only 10 percent of GMHC clients are Medicaid eligible when they first contact GMHC, within 1 year nearly 60 percent have become eligible. GMHC staff estimates that it takes 1 year, on average, for a middle-class, self-supporting individual with HIV to become at least partly dependent on public resources (Hansell, 1990).
Limited public resources have been supplemented by the volunteer community, both in terms of money and services. Productive working people who might have spent more time earning money are now instead involved in volunteer caretaking. Money that would have been saved or invested is spent on charity. Some have described the gay community as an economic colony of the health-care professions, the hospitals, and the pharmaceutical houses (Oppenheimer and Padgug, 1991).
Epidemic #2: Drug Users
In the opening stages of the epidemic it became apparent that sharing of drug injection paraphernalia among heroin addicts was a critical element in HIV transmission (Drucker, 1986). New York City, which had experienced
an epidemic of heroin use from the late 1960s into the middle 1970s, is thought to have an aging population (people aged 30 to 40) of some 200,000 heroin users. Experts believe the actual numbers could vary by as much as 50 percent, but 200,000 remains the best estimate possible given the illegal status of drug use and the limitations of any drug-user surveillance system (Turner et al., 1989). However, it was clear that a very large community existed at high risk for infections with a blood-borne viral disease. Indeed, early studies of HIV seropositivity among intravenous drug users showed a rapidly increasing rate. By 1985 it was estimated that intravenous drug users had a seropositivity rate that exceeded 50 percent (Des Jarlais, 1985; Drucker, 1986). Annual incidence rates for the same period were estimated to be between 1 and 11 percent.
Estimating the effect of the HIV/AIDS epidemic on the already existing population of older heroin addicts was complicated by the emergence of cocaine as a readily available street drug. Researchers reported that the majority of methadone patients reported injecting cocaine in the period from 1978 to 1985 (Selwyn and Schoenbaum, personal communication reported in Drucker, 1986). The short-acting effects of cocaine, when injected, increased the frequency of injections and the likelihood of contact with an infected needle.
The dynamic potential for rapid change in the social ecology of drug use was demonstrated by the introduction of crack cocaine in the mid-1980s in response to interruptions in previously plentiful supplies of marijuana. Retrospective analyses suggest that smokeable cocaine in the form now called crack was becoming available on the street in a number of cities (principally, Los Angeles, Miami, and New York) as early as mid-1984 (Hamid, 1990). Beginning in 1987 it became clear that crack added a variety of new complications. In its smokeable form, a nearly immediate, but extremely transitory "high" is experienced, leading to relatively frequent use. The drug was cheap in comparison with either high-quality cocaine or heroin, and the price fell as markets expanded. Since polydrug use has always been common—for example, many, if not most, users of heroin also used other drugs, including alcohol and marijuana—the addition of crack to the drug-use repertoire was not surprising.
Crack was inexpensive enough to be used by young people without much money, and it requires little preparation, creating a new class of youthful users and dealers. The drug was attractive to women, in part because its route of administration did not require injection. Ethnographic research among crack users in Harlem in 1989 found, in addition, that women with a chronic dependency felt crack changed the nature of their relations with men, making them feel powerful and in control of sexual interactions (Clatts, 1992). Unlike heroin or alcohol, which are sedatives, crack cocaine is a stimulant. Because it appears to act as a defense against
feelings of low self-esteem and depression, crack became the drug of choice among homeless youths and women who traded sex for drugs (Clatts et al., 1990a,b).
The explosion in crack use during the late 1980s deepened social problems in the areas of New York City that were already most affected by HIV/AIDS. In the opening phase of the crack epidemic, individuals who first began to use the drug exhibited acute signs of personal and social disorganization. Some individuals reported a nearly immediate loss of control and rapid escalations in use and an equally rapid collapse in the stability of personal relations. During this period, the behavior of crack users was thought to be entirely a function of the power of the drug and its impact on the brain, and a number of clinicians thought that such users were not amendable to treatment. The mass media struggled with how to interpret the problem, reporting in early 1989 that crack was "a disaster of historic proportions" (New York Times, 1989: E14). The police responded with concentrated surveillance and arrests in areas overrun by crack dealers, but dealers and buyers simply moved to other sites. Surges in arrests clogged the court dockets and the jails, but they did not appear to produce significant reductions in drug use. Indeed, the police commented that they could arrest four to five times more offenders if there were greater capacity to process them.
A variety of extremely serious second-order problems followed. Crack increased the likelihood of high-risk sexual behavior among female users of all ages. The emergence of "crack prostitutes" was widely reported—a pattern of sexual conduct that involved the exchange of sex by crack-addicted women for money or drugs (Tierney, 1990; Inciardi, 1991). In the most extreme cases, women were reported to be staying in crack houses and exchanging sex for drugs on an indiscriminate basis with many sexual partners, at least some of whom were infected with HIV (Williams et al., 1988).
Exchanges of sex for drugs also involved an increased risk of sexually transmitted diseases that might act as cofactors for HIV transmission. Crack use was identified in one New York City study as a significant behavioral cofactor reported by HIV-positive women visiting a municipal sexually transmitted diseases clinic (Chaisson et al., 1990). Three factors were thought to increase risk of transmission: (1) an increase in sexual partners; (2) the fact that men on cocaine maintain erections for longer, thereby increasing risk of vaginal dryness, leading to abrasions that provide access for the virus; and (3) oral lesions due to blisters caused by hot crack pipes, which increase the likelihood of transmission during oral sex.
In addition to increased risks of transmission, crack use significantly modified patterns of personal and social behavior. Although there is a strongly skewed sex ratio in traditional drug-use patterns (many more men than women), reports confirm that many more women than men have become
addicted to crack (see e.g., Hamid, 1990). A variety of experts in New York City commented on the disordering effects that crack use had on women, noting that women had become violent property offenders to an unprecedented degree (Hamid, 1990). A substantial increase in child neglect, abuse, and abandonment affected the workings of the family court and foster care systems, which were already under severe stress. In addition, there was a rise in the number of babies born in the city who showed evidence of maternal cocaine use, and some of those babies required many days of intensive care at very high cost. The "crack babies" added to the problems caused by the number of babies born who were HIV positive. The impact of crack on women was especially serious in minority communities, where women are often the only stable caretakers for children.
PUBLIC HEALTH AND HEALTH CARE
The concentration of the epidemic, both socially and geographically, has differentially affected the component agencies and services of the health care and social welfare systems of New York City. For example, municipal hospitals serving areas with large numbers of people with HIV/AIDS who do not have health care insurance usually have a very large number of patients in various stages of HIV disease. These municipal hospitals are already underfunded, understaffed, and threatened with further budgetary cuts, all of which affect their ability to provide care (Gage et al., 1991).
The lack of private care physicians in the inner-city communities enhances the importance of municipal hospitals. For instance, in the Mott Haven/Hunts Point section of the Bronx there are only 34 office-based primary care physicians for every 100,000 people, in contrast to 1,451 per 100,000 in the Upper East Side of Manhattan (Carey, 1990). Moreover, the few community-based physicians who are available have limited practices. In a recent study of 701 primary care providers in nine low-income communities, only 28 (3.9 percent) were able to provide "accessible, comprehensive and coordinated primary care," and only a quarter had admitting privileges to hospitals to which the poor have access. Those without such privileges must refer patients to the closest emergency room for hospital-level care (Carey, 1990). In such areas of the city, the emergency rooms of the municipal hospitals often serve as the health care providers of the first resort.
Of the 72 hospitals in New York City, 13 serve over one-half of the AIDS patients in the city: 3 are operated by the Roman Catholic Archdiocese and 10 by the New York City Health and Hospitals Corporation. The United Hospital Fund estimates that by 1993, 15 to 25 percent of beds in university hospitals and 50 percent of beds in municipal hospitals will be occupied by persons with diseases related to HIV/AIDS. This will be in a
hospital system with close to 90 percent occupancy rates and for which no expansion in beds is expected (Carey, 1990). The concentration of people with HIV/AIDS in certain facilities results from a variety of factors, including: the disease prevalence in community areas served by those hospitals; the expertise developed by institutions with significant concentrations of HIV/AIDS patients; reimbursements available for AIDS care; and resistance of some hospitals to caring for people with HIV disease or people without health insurance. This phenomenon is not restricted to New York City: national data indicate that in 1987, 20 percent of the hospitals in the nation provided 77 percent of the care for persons with HIV/AIDS, and 4 percent of the hospitals provided 32 percent of the care (Rothman et al., 1990).
Within the service areas of the hospitals that provide the largest amount of health care for persons with HIV/AIDS, there is evidence that some specific local areas (as defined by zip code) have a disproportionate number of AIDS cases. Of 542 recent AIDS-related discharges by Bronx Lebanon Hospital, for example, more than one-half had addresses in only two zip code areas. Bronx Lebanon provides a dramatic example of the way in which the HIV/AIDS epidemic can dominate a hospital's health care activities. In 1991 the hospital's average daily census of inpatients with HIV/AIDS ranged from 100 to 120, about four-fifths of whom were housed outside the specialized AIDS unit of 22 beds. Overall, the hospital estimates that one-third of its inpatients are HIV-infected. And during 1990, approximately 10,000 visits were made by persons with HIV/AIDS to the outpatient AIDS unit.
The high concentrations of HIV disease in New York City can be documented to the level of clusters of city blocks. HIV/AIDS in impoverished populations in the inner city is transmitted by behaviors that imply a common residential pattern. For example, intravenous drugs users appear to be a relatively immobile population that depends on a strong network of neighborhood residential and social ties to maintain contacts with "running buddies" and drug suppliers. This population's sexual partners are also relatively immobile, and often they and their children share common households with the drug users. Such factors increase the concentration of persons with HIV/AIDS within narrow boundaries and focus the impact of the epidemic in those communities.
A similar process of geographical concentration had occurred with gay men, but for quite different reasons. The areas in New York City with the highest concentrations of people with HIV/AIDS are those that are home to large numbers of gay men (United Hospital Fund areas Chelsea/Clinton and Greenwich Village-Soho), and within those two areas, the majority of persons living with HIV/AIDS reside in two (of nine) zip code areas. The construction of these quasi-ethnic communities, which provide a wide range of social and cultural services, also created an environment in which there
were high rates of sexual interaction, which resulted in transmission of HIV and other sexually transmitted diseases among some men. These residential communities now contain substantial numbers of men who are living with HIV/AIDS and who are users of the services provided by local hospitals and physicians (often gay themselves), as well as by the voluntary organizations that have been created in response to the AIDS epidemic. The everyday fact of living with the epidemic is thus concentrated in a small number of communities, which are in large measure insulated from the rest of the city.
The social concentration of the epidemic in some neighborhoods also has limiting effects on the proportion of health care professionals and facilities that come in contact with persons living with HIV/AIDS. Patients with HIV disease are concentrated within the catchment areas of specific hospitals. In addition, African Americans and Hispanics with HIV/AIDS (as well as those white gay men who are impoverished by HIV/AIDS) are more likely to be treated in municipal rather than private hospitals. During the week of January 21, 1990, for example, municipal hospitals in New York City had 16 percent of the beds but 37 percent of the AIDS patients (Carey, 1990).
Within some hospitals in New York State, specialized facilities have been developed to handle persons with HIV/AIDS, and a number of hospitals in the city have been designated AIDS centers by the state. (To be so designated hospitals must meet 14 standards of care; in return, they receive a higher level of reimbursement.) As of October 12, 1990, 13 hospitals in New York City were designated as AIDS centers. As of the same date, no municipal hospital had met the standards for center status, even though municipal hospitals have the largest proportions of HIV/AIDS patients in the city (except for three voluntary hospitals administered by the Archdiocese of New York and Bronx Lebanon).
The concentration of persons with HIV/AIDS in various locations does not necessarily mean that only physicians who maintain practices in those areas, either community-or hospital-based, are likely to see patients in any stage of HIV disease. In a 1988 telephone survey in New York City of a probability sample of 473 primary care physicians (internists, family care practitioners, general practitioners, and obstetricians-gynecologists), 61 percent said that they had "ever" had a person with HIV in their practice, and those physicians had accumulated an average of six patients who had AIDS. About one-third of the physicians said that they were currently treating patients who were HIV positive, and on average, those physicians had 15 such patients in their practice. Another one-third, however, said they would refer an asymptomatic HIV-positive patient elsewhere rather than treat the patient (Gemson et al., 1989). The data in this survey suggest that many primary care physicians in New York City have had some contact with
persons with HIV/AIDS. The physicians who reported having such patients were more often younger, better trained, less averse to or fearful of homosexuality, and more likely to know someone other than a patient who has AIDS. These findings suggest that some experience with persons with HIV/AIDS is relatively widely distributed among physicians.
The survey data do not necessarily conflict with data on concentrations of patients in hospitals, data on the neighborhood concentrations of AIDS cases, or the evidence from AIDS voluntary organizations that many physicians do not treat patients with HIV/AIDS. Although many physicians in private practice may have a small number of patients with HIV/AIDS (particularly middle-class men), the majority of persons with HIV are treated by a smaller number of health care professionals and agencies. The Gay Men's Health Crisis has a referral list of only 45 AIDS specialists in Manhattan (Lambert, 1990b). Even though there is evidence for some contact between many physicians and persons with HIV/AIDS, there is other evidence, even in New York City, that only a modest number of medical professionals in private or hospital practice regularly come into contact with persons with HIV/AIDS. Given the concentration of HIV/AIDS in specific neighborhoods and social communities, a substantial proportion of that number are professionals working in public-sector hospitals and physicians in private practice in gay areas of the city.
Despite the recommendations of various AIDS commissions and task forces that the burden of HIV/AIDS be dealt with on a citywide basis (New York City Department of Health, 1989a,b; Rothman et al., 1990), the epidemic is disproportionately felt in limited areas of the city. Indeed, although there are no single-disease hospitals for HIV, some hospitals and medical practices are in fact dominated by HIV/AIDS (Navarro, 1991). This is, in some measure, a result of the geographical concentration of the epidemic, which limits which health care providers and hospitals will be in the neighborhoods of AIDS patients. Another factor that has considerable influence is the limited health care resources that exist in the areas in which economically impoverished members of ethnic minorities live—poverty reduces physician availability and concentrates patients in the municipal hospitals. HIV/AIDS in this sense is not a citywide disease.
Public Health Effects of HIV/AIDS Concentration
The concentration of HIV/AIDS in particular neighborhoods of New York City reveals a chilling epidemiological fact: HIV/AIDS is but one in an overlapping cluster of epidemics. The affected neighborhoods, marked by poverty, poor access to health care, drug addiction, and social disintegration are beset with co-epidemics of disease. The most striking lesson to be learned from the concentration of AIDS in particular neighborhoods is that
AIDS cannot be viewed in isolation. The map of HIV disease in New York City is also a map of the epidemic spread of other diseases, including sexually transmitted viral and bacterial diseases, as well as some nonsexually transmitted diseases, particularly tuberculosis. AIDS cases are also concentrated in zones of urban poverty, poor health care, drug addiction, and social disintegration.
Gonorrhea, syphilis, and chancroid—the three classic venereal diseases that had nearly disappeared except for momentary and treatable recurrences—are increasing at epidemic rates among urban minority populations in the United States (Aral and Holmes, 1991). Syphilis and herpes have been associated with HIV infection in heterosexual men and women and homosexual men in the United States. HIV infection leads to altered manifestations of sexually transmitted diseases (STDs) and is thought to promote their spread. Thus, it has been suggested that HIV and other STDs interact to facilitate the sexual transmission of HIV (Aral and Holmes, 1991:66).
The recent spread of nonsexually transmitted infectious diseases is also occurring in neighborhoods already suffering from a high concentration of AIDS and other STDs. Certain parts of urban centers of the United States have become "islands of illness" (Rosenthal, 1990:1) as their residents experience a resurgence of measles, mumps, rubella, and whooping cough—all of which are diseases that can be prevented with vaccines. In addition, during the 1980s (following almost two decades of decline), New York City experienced a 132 percent increase in the incidence of tuberculosis (New York City Department of Health, 1991). New cases rose by more than 38 percent in the city in 1989-1990, almost four times the rate of increase in the previous year. The highest rate was found in central Harlem, where there were 233.4 cases per 100,000, more than 23 times the national average. Although African Americans made up 28.7 percent of the city's population in the 1990 census, they accounted for 58 percent of the tuberculosis cases. The association between tuberculosis and HIV disease has been documented in a number of studies (see, e.g., Barnes et al., 1991).
The rise of tuberculosis in impoverished communities is in part linked to the movement of people in and out of prison and jail systems in which crowded conditions, inadequate health care, and the presence of HIV/AIDS facilitate the transmission of the bacillus. The annual incidence of tuberculosis in the New York State correctional system increased from 15.4 cases per 100,000 in 1976-1978 to 132.2 cases in 1988. African Americans and Hispanics aged 30 to 39 who had used intravenous drugs were those usually infected, as one might expect. There is no evidence for a common source of the epidemic within the institutions, a finding that would confirm the view that the epidemics in New York City and in the prisons are part of a common epidemiologic community (Hammett et al., 1989).
The increase of tuberculosis in New York City was accompanied by an
epidemic of homelessness during the same period. In the late 1960s, homelessness in New York City meant ''skid row,"—large numbers of predominantly white men (often employed) living in an area called the Bowery. In marked contrast, today's homeless are more likely to be young (late 20s and early 30s), minorities, and, increasingly, mothers and children who are members of single-parent families (Hopper, 1990). By 1989, 69 percent of men living in the streets were African American, 17 percent were white, and 12 percent were Hispanic; of those regularly using city shelters, 72 percent were African American, 7 percent white, and 16 percent Hispanic (Hopper, 1990).
Recent research suggests that homelessness and the social disorder associated with it are critical factors in the increase of tuberculosis (Brudney and Dobkin, 1991). In research conducted at Harlem Hospital, which serves the area of the city with the highest tuberculosis rate, 224 consecutive patients with tuberculosis were studied during the first 9 months of 1988: percent of those patients had HIV/AIDS, 68 percent were homeless, 64 percent used crack cocaine or injected drugs, and 50 percent had high rates of alcohol use. Of the 178 who were discharged, 89 percent were lost to follow-up and did not complete treatment. The situation of many people with tuberculosis is so compromised by unemployment, poverty, and drug and alcohol use that even when they are diagnosed and prescribed a treatment regimen, they often fail to comply.
According to the same study, there has been a substantial disinvestment in tuberculosis control in both New York City and New York State. Traditional programs of inpatient tuberculosis care had been eliminated in the 1970s, but there was also a dramatic decline in funding outpatient treatment of tuberculosis. The fiscal crisis of the city in the 1970s led to reduced funds for tuberculosis control, and the state terminated its support for all city tuberculosis control activities in 1979. At the same time, the Public Health Service was also decreasing its support for tuberculosis control (Brudney and Dobkin, 1991). Yet even before the HIV/AIDS epidemic began, tuberculosis was resurgent. The dramatic increases in homelessness and in the use of shelters have created the seedbed for transmission and for noncompliance with treatment routines.
More recently, there has been a major surge of interest in the dangers of a tuberculosis outbreak as the dire predictions of the tuberculosis control workers have come true. A disturbing aspect of the resurgence of tuberculosis involves small outbreaks of a strain of the bacillus that is resistant to conventional treatments, representing a particular danger to individuals whose immune systems are compromised by HIV infection. Multiple drug-resistant tuberculosis (MDR-TB) is both more expensive and more complex to treat than non-drug-resistant varieties of tuberculosis. Following a November 1991 outbreak of MDR-TB in which 12 HIV-infected inmates and a
guard died, the Department of Corrections announced it will put in place programs of screening inmates and employees and isolating those inmates with tuberculosis in quarantine units in remodeled infirmaries (McFadden, 1992).
The problem of adherence to tuberculosis treatment routines has become especially important as the disease has become common among those with the most disorderly lives in the society: the homeless, the drug addicted, and those in these groups who have lost hope as a result of their infection with HIV. Inadequate support for the machinery of tuberculosis control compounds these problems. A recent request for $13 million from the federal government (to add to the $8 million budget for the city's Tuberculosis Bureau's) resulted in two grants totaling only $1.4 million (Belkin, 1991). In December 1991 an allocation of $8 million was promised from city, state, and federal funds to invest in "sweeping health measures to limit the spread of TB" (Altman, 1991), although there was no specification of how much of these funds was new money. The new program involved increased personnel and incentives for compliance, as well as the requirement that hospital rooms have better ventilation and ultraviolet lamps. In recent months there have been anecdotal reports that persons with HIV/AIDS may be avoiding hospitals because they are afraid of being infected with tuberculosis (Navarro, 1992).
Ethnicity and Residence: Data Collection and Other Public Health Issues
There is some evidence to suggest that the impact of HIV/AIDS differs among ethnic groups in New York City, although the way in which AIDS data are currently collected provides only limited insight into the situation. The CDC method of data collection (identifying only black/white/Hispanic and, more recently, Asian-Pacific) does not allow researchers or health care practitioners to trace the impact of the epidemic in particular ethnic communities, reducing opportunities to devise culturally appropriate prevention and treatment programs. The absence of data on income, education, or occupation invites the fallacy of attributing to skin color effects that are in fact the result of poverty and racism and of further stigmatizing disadvantaged communities.
Puerto Ricans are the ethnic group most severely affected by the HIV/AIDS epidemic in New York City. This fact has been determined despite the absence of incidence data for those born in Puerto Rico and the difficulty of determining ethnicity among those classified as Hispanic in AIDS mortality data (Menendez-Bergad et al., 1990). Between 1982 and 1987, AIDS accounted for a steadily increasing proportion of deaths among Puerto Rican born males, reaching 12 percent among Hispanics, compared with 6
percent for African American, and 2 percent for whites in 1987 (Menendez-Bergad et al., 1990).
The Puerto Rican incidence data provide important insights into the epidemic, suggesting that culturally distinctive patterns of behavior and residential segregation play a role in the spread of HIV disease. For example, all Puerto Ricans have U.S. citizenship and thus have no need to marry U.S. citizens to ensure continued residence (unlike other Hispanics born outside the United States). Indeed, Puerto Ricans marry each other in greater proportions than other Hispanic-origin groups in New York City, and they are also more likely to have sexual contact with other Puerto Ricans than with individuals from any other groups. In addition, needle-sharing networks among intravenous drug users are often racially or ethnically homogeneous (Schoenbaum et al., 1989), which further concentrates the virus. Puerto Ricans also maintain close links with family and friends, and many Puerto Ricans diagnosed with HIV disease in New York City return to Puerto Rico following diagnosis, underlining the idea that the Puerto Rican communities in New York City and San Juan can be thought of as a single social and epidemiologic "neighborhood" (Lambert, 1990a).
Women's ability to observe safe sex practices—specifically to persuade their partners to use condoms—is heavily influenced by cultural expectations. A study of 304 African American and Hispanic women of childbearing age at two inner-city health facilities showed that Hispanic women were more likely than African American women to believe that there was nothing they could do if their partners did not want to use condoms. Moreover, foreign-born women were more likely than native-born women to hold that view and also to know less about AIDS and safer sex practices (Worth, 1989; Ricardo, 1990). Thus, significant differences of epidemiologic relevance stem from distinctive cultural patterns of social and sexual contact, differences in national origin, in migration history, and in the prevalence of HIV in particular communities (Menendez-Bergad et al., 1990).
Very little is currently known about these important cultural and social differences for the many ethnic groups in New York City. Knowledge is particularly wanting for Hispanics. Prior to 1965, for example, Puerto Ricans accounted for the largest proportion of Hispanic immigrants to New York City. Since that time, immigration from Puerto Rico has declined and that from other locations has increased, especially from the Dominican Republic. Dominicans are now the second largest Hispanic group in New York City, approximately 50 percent of whom are thought to be illegal residents (Wasserman et al., 1990). The implications for health behavior and health care remain largely unexplored.
The Crisis of Infant Health
The impact of the AIDS epidemic among children in the city is now well known, but the epidemic is only one indication of the problematic status of child health among the minority poor in the city. Data from as early as 1985 suggested a growing health crisis for infants and children in the most impoverished sections of the city, including a leveling off in the previous long-term decline in infant mortality rates.
Data on low birthweight infants (less that 2,500 grams), a phenomenon highly associated with infant mortality as well as a precursor of a variety of problems for a child who survives the first year of life, are highly variable across the city. Gager (1988) have identified health center districts in the city with much higher than average rates of low birthweight infants. The four areas characterized by the largest proportion of low birthweight infants in 1985 (1 infant in 8 in contrast to 1 in 12 in the city at large) in Upper Manhattan and the South Central Bronx (Central Harlem, Morrisania, Mott Haven, and Tremont) had nearly 70 percent of all births paid for by Medicaid, 40 percent with late or no prenatal care, and 20 percent of all births to teenage mothers. The districts with a high prevalence of low birthweight infants have a familiar ring when compared with the neighborhoods that have been the sites for the highest rates of reported AIDS cases among poor adults and children. They are again those areas in the city where HIV/AIDS is interactive with other social and health crises.
The low-weight births are also concentrated in the same hospitals that serve the largest number of AIDS cases among minority adults and children. The largest number of low-weight births in Central Harlem occurred at Harlem Hospital: 50 percent of those births were to women who had late or no prenatal care and 80 percent were paid for by Medicaid. In East Harlem, most low-weight births occur at Metropolitan Hospital, and they too are largely paid for by Medicaid, although there is evidence of more prenatal care: only one in four mothers had late or no prenatal care. The data are similar for some hospitals in the Bronx, such as Lincoln (two-thirds late or no prenatal care and two-thirds supported by Medicaid). Similar patterns occur for the remainder of the city, with the voluntary hospitals reporting lower proportions of women who have late or no prenatal care.
The complex association among infant health, drugs, HIV seropositivity, and measures of socioeconomic status remains. Data that present the ecological correlation among HIV seropositive births, low birthweight infants, drug-related discharges from hospitals, and proportion of births to mothers with less than 12 years of education show a remarkable overlap by city area (Morse et al., 1991).
CORRECTIONAL SYSTEMS
The concentration of intravenous drug users in the impoverished inner-city communities of New York and the intimate association between drug use and criminality have led to a steady flow of drugs users in and out of the criminal justice system. The criminalized status of drug use and the crimes that are often committed by drug users involve a cycle of addiction, arrest, imprisonment, release, and relapse to addition. This revolving-door pattern has been characteristic of the life of the users of illegal drugs in the United States—particularly those using opiates and opiate derivatives—since the late 1920s (Musto, 1987). Since World War II, the cycle of addiction and criminalization has been disproportionately centered in minority communities, even though there is evidence of widespread illegal drug use in other communities.
When the federal war on drugs was declared in the 1980s, increased numbers of low-level drug users and sellers (who are often users themselves) were arrested, resulting in larger numbers of people at high risk for HIV infection being processed by criminal justice institutions. Of all correctional institutions, prisons are probably the most severely affected since they hold people for the longest periods of time and have responsibility for the health of their inmates.
Of the 130,000 people who are processed through New York City's correctional system each year (daily censuses are about 20,000 people), it is estimated that more than one-half have histories of drug use (though not all are intravenous drug users). Of the 50,000 or more intravenous drug users, it is estimated that between 20 and 25 percent are HIV positive. Thus, between 10,000 and 15,000 people with HIV disease were in the city's correctional system during 1988 alone (Association of the Bar of the City of New York, 1989). Approximately 54,000 people are held in state prisons, 60 to 70 percent of whom have histories of drug use (although not all are intravenous drug users); about 75 percent of the total are from New York City.
Women with HIV/AIDS are a particularly serious problem for the city (and state) correctional systems. About 5 percent of the prisoners in the state system are women; the midyear 1990 count was 2,721 prisoners. About 19 percent of female prisoners are HIV positive, and 57 women have died in prison from AIDS (Smith et al., 1991). Women are more likely to be committed to the state prison system for drug offenses than for crimes of violence, and many have been recently imprisoned as the result of crack cocaine use. In the city system, about 10 percent of the prisoners are women, and about one in five is HIV positive. Female inmates with HIV/AIDS require special services including drug treatment, frequent medical attention to the gynecological needs, pregnancy testing, and access to information
about infection control between mother and child (New York State Department of Health/New York AIDS Institute, 1989).
The inmates who flow through the correctional institutions of the city and the state are not drawn equally from every community in the city. The city is itself residentially segregated along ethnic lines, and although data do not exist on the residential distribution of those who enter the criminal justice system, it is not unreasonable to argue, given their ethnic distribution, that they are drawn from the areas that house the poor of the city. Currently, on any given day, 23 percent of all African American men in New York State aged 20 to 29 are in some form of control by criminal justice authorities—prison, jail, probation, or parole (see Table 9-3). Of those young men, 48 percent are in jail or prison. It is important to note that these are lower-bound numbers because they represent the count on a single day. Across an entire year, the proportions are somewhat higher. The proportion under the control of the criminal justice system is smaller for Hispanic men of the same age (14 percent), but the proportion of those in custody who are in prison or jail is the same—48 percent. In contrast, only 3 percent of whites in the same age range are in custody of any kind (Gangi and Murphy, 1990). More than 80 percent of all of the Department of Corrections Services prisoners in New York State are African American or Hispanic. The proportions in the jails of the city of New York are similar.
HIV/AIDS makes a special contribution to the bleak situation of many of these men and the women. The number of minority men in New York City who will die from HIV/AIDS (largely in their 30s and early 40s) will be substantial; estimates range between 50,000 and 100,000 (although the actual number will never be known precisely). Many of these men will pass through the criminal justice system, challenging its ability and willingness to deal humanely with HIV-infected inmates. The system's success in meeting that challenge will be felt not only by the inmates, but by the poor and minority communities from which they come and to which they may return.
Currently, 41 states plus the District of Columbia, Puerto Rico, and the Virgin Islands are under a court order or consent decree to improve conditions of confinement or limit the prison populations either for their entire prison systems or for specific institutions (Cade, 1990). Neither the New York City nor the New York State correctional systems are under such court orders or consent decrees, but both have had to expand rapidly to accommodate the rapid rise in prisoners over the past decades. In 1973, New York State had 12,500 persons in the state prison system; by September 1990, that number was more than 54,000 (Gangi and Murphy, 1990). In December 1991 it was reported that this number had reached 57,000 and that the state would add from 3,000 to 6,000 new beds through double bunking in the medium-security prisons (Raab, 1991). Similarly, the number
TABLE 9-3 Criminal Justice Custody Rates for Males Aged 20-29, by Ethnicity or Race, New York State
|
|
Under Custody |
|||||||
|
Group |
State Prisons |
County Jails |
Misdemeanor Probation |
Felony Probation |
Parole |
Total Population |
Number |
Percent |
|
White |
3,613 |
2,092 |
15,459 |
10,944 |
2,000 |
1,243,189 |
34,108 |
2.7 |
|
Black |
13,123 |
8,354 |
7,186 |
11,004 |
5,092 |
193,222 |
44,759 |
23.2 |
|
Hispanic |
5,641 |
3,813 |
2,052 |
5,511 |
2,704 |
164,575 |
19,721 |
12.0 |
|
Total |
22,377 |
14,259 |
24,697 |
27,459 |
9,796 |
1,600,986 |
98,588 |
6.2 |
|
SOURCE: Adapted from Gangi and Murphy (1990). |
||||||||
of prisoners in the New York City correctional system has increased—from 7,000 per day in 1980 to 20,000 per day in 1990 (Gangi and Murphy, 1990).
The state was expected to spend $3 billion in 1990 to cover the cost of operations and construction of the prison system. It costs approximately $58,000 a year to keep an inmate in a city jail; the cost of constructing a new jail cell is close to $200,000 (Gangi and Murphy, 1990). Not only are these costs high, resources used for prisons become unavailable for alternatives to imprisonment, for drug treatment, or for the health care system at large. This trade-off has raised questions about the wisdom of incarcerating drug offenders (Gangi and Murphy, 1990).
The focus on law enforcement solutions to drug problems, particularly in the visible communities of drug users in minority populations where the epidemic of HIV disease has centered, has created a major crisis in the criminal justice system, especially in prisons and jails (Association of the Bar of the City of New York, 1989). People with HIV disease, including those with AIDS, come in contact with the full gamut of the agencies of the criminal justice system—police, court officers, correctional officers, and probation and parole officers, as well as lawyers and judges. They find themselves at the double disadvantage of being accused or convicted offenders and ill with a disease that creates fear in many of the officials with whom they come in contact. Recent reports suggest that although some workers in the system have been particularly helpful to people with HIV/AIDS, there are many incidents of prejudice and discrimination that are harmful to the health and legal cause of persons with HIV/AIDS (Association of the Bar of the City of New York, 1989). There is evidence of trial delays and limitations on court access because of HIV status, problems with the behavior of court officers (e.g., wearing gloves and protective masks), problems with the transportation of HIV-infected accused and convicted people, and failures of confidentiality of HIV status (Association of the Bar of the City of New York, 1989).
Correctional System's Response to Inmates with AIDS
The New York City Department of Corrections has tried to be responsive to the AIDS crisis. In 1987, for example, a 40-bed infirmary unit was established on Rikers Island, a New York City jail, to house inmates who were diagnosed with AIDS. (The unit replaced the very inadequate facilities that had existed since 1984.) In 1989 prisoners with AIDS were moved to an expanded 66-bed annex to the infirmary. These improvements were taken under threat of court action by inmates with HIV/AIDS and concerned nongovernmental organizations. The new facility at Rikers Island is considered to be a model of efficient and humane care, but it is a segregated
unit, and all of the men in the unit know they have a fatal disease. The extended report on the situation in Rikers Island by Dobie (1990) indicates that the fear of dying in prison is widespread among the men in the unit and that there are difficulties in arranging compassionate release even for seriously ill men.
The policy of segregating inmates with "recognizable" AIDS (most inmates with "unrecognized" HIV disease are in the general prison population) was justified on a number of bases, including the risks to those infected if their status were known to other inmates. However, the segregation appears to be based on management considerations relating to institutional efficiency and movement in the institution and to and from court, as well as for health care and public health considerations. Actual medical care in the institution is now provided under contract by Montefiore Hospital (located in the Bronx), and acute care takes place in a number of municipal hospitals with secure units when beds are available; in 1989 there were a total of 66 such beds in two hospitals, Bellevue and Kings County. When beds are not available or specialized care is needed, prisoners, including those with HIV disease, are placed in wards meant for the general population. The prisoners are usually shackled 24 hours a day, although there are some circumstances in which manacles are not used. (For a detailed discussion of the use of manacles, see Association of the Bar of the City of New York, 1989:201.)
The New York State Department of Corrections Services has, for a variety of reasons, been less responsive to the issue of HIV/AIDS. In part this has been the result of a policy decision at the highest administrative levels. In 1988, Thomas A. Coughlin III, the commissioner of the department, stressed that their primary mission is not one of health care (quoted in Association of the Bar of the City of New York, 1989:207):
As Commissioner I would resist any attempts to redefine our mission to include primary responsibility for health care. Our system is predicated on the use of community health resources … AIDS is a devastating personal and societal problem; prison should not be the place to treat that problem. Any attempt to replicate in prison services that should be provided in the community to treat this problem is, in my opinion, bad public policy.
Although this position is understandable given the limited resources of the Department of Corrections Services, some 3,500 persons with HIV/AIDS are estimated to be in the state prison system. The sentences of state offenders are longer than those of inmates in the city correctional system. As a consequence, state inmates are more likely to find themselves in the end stages of their disease while imprisoned. State prison facilities are far flung, often in rural counties, far from the concentrated health care resources of the urban regions. Prior to the epidemic the state prison system
depended on limited-care infirmaries within the institutions, a few dedicated acute care beds in outside hospitals, and a case-by-case arrangement with community hospitals. Since the epidemic, problems have increased, but the response of the department has been modest—special needs units have been established in three institutions and a dormitory in a fourth. According to various external reports, the department's health-care facilities are currently inadequate for the needs of the inmates with HIV/AIDS (see New York State Department of Health, 1988). Furthermore, although the department has "mainstreamed" many of its prisoners with HIV/AIDS, it has also attempted to create specialized segregated facilities, which was halted by court order (Association of the Bar of the City of New York, 1989:219).1
There is evidence that the survival rate for prisoners in state custody who have histories of intravenous drug use and who have HIV/AIDS is far shorter than for people with similar characteristics in New York City who are not incarcerated: the latter survive 318 days from diagnosis to death; the former survive 159 days. There is also evidence that 25 percent of inmates who die in prison of HIV/AIDS are diagnosed only after autopsy; this percentage appears to be lower than that for people who die undiagnosed in the community (Potler, 1988; Stoneburner et al., 1988).) The differential in survival time may have a number of causes, including delays in identifying those who are infected and show signs of illness, inadequate care as a result of limited staff training, and understaffing (Potler, 1988). One might add to these causes the relative lack of treatment drugs available to prisoners (especially to those who are asymptomatic) and the stressful conditions of life for prisoners.
The failure of attempts to remediate the current health care crisis in state institutions is signaled by the fact that this most recent report of the Correctional Association now focuses on early release and clemency for the terminally ill while treating a major improvement in the health care facilities of the prison system as desirable goal. Medical parole for terminally ill inmates has been urged by a number of legislators, inmate groups, citizen groups, and correctional officials. According to recent press reports, there are now between 8,000 (the correctional systems estimate) and 12,000 inmates (citizens' groups estimate) with HIV/AIDS in the state prison system, and 2,600 prisoners are now being treated for HIV disease (Dao, 1992). A clemency program might increase contacts between terminally ill inmates and their families and would prevent prisoners from dying alone. In addition, it would save the prison system money by transferring the costs of treating terminally ill prisoners to the budgets of nonprison institutions.
IMPACT OF HIV/AIDS ON WOMEN, CHILDREN, AND FAMILIES
Women make up a growing proportion of persons with HIV/AIDS, particularly in New York City and northern New Jersey, which already lead the nation in the cumulative number of CDC-defined AIDS cases among women. They are nearly almost all poor and from African American or Hispanic communities. The highest rates of HIV-infected women occur in the South Bronx, Chelsea/Clinton, and Central and East Harlem in Manhattan and in Bedford Stuyvesant in Brooklyn (see Table 9-1 above). As noted above, researchers modeling HIV/AIDS among women in New York predict as many as 2,000 new cases in 1993 and a related increase in the number of babies born with HIV/AIDS.
A number of investigators have noted the importance of distinguishing between women with HIV/AIDS, children with HIV/AIDS as a result of perinatal transmission, and the interactive relationship between women and children, one or both of whom may have HIV/AIDS. Women are often viewed only in terms of their ''reproductive function," and an invidious distinction is drawn between "guilty" women infected by drug use or sex and "innocent" children (Chavkin, 1990).
The distinction between innocent and guilty sufferers has serious consequences for resource allocation. Funds are more readily devoted to babies and children with AIDS than to women who need drug treatment, housing, or other social resources. In addition, such a distinction between guilty and innocent affects interactions between women with HIV/AIDS and the traditional systems of care and caretakers. Ethnographic studies document numerous negative experiences on the part of poor African American and Hispanic women in their interactions with the health care system. These have the effect of disempowering women, reducing their sense of control over their own lives, and preventing them from seeking health care or complying with instructions given to them (Kenny et al., 1990).
Finally, the division of the world into guilty mothers and innocent children focuses the health care debate for women around the issues of childbearing, the prevention of reproduction, and decisions that women "ought to make" about whether to have children. Such debates generally do not result in the practical programs that are required to give women the resources with which to manage their own choices about sexuality and reproduction.
Research activity is also skewed toward women in their relation to their children or to children rather than to women themselves. The scientific reasons offered for the exclusion of women from clinical trials for drugs for HIV disease are complex. A number of feminists have pointed out, however, that women were previously excluded from other trials (e.g., those
related to heart disease), for which the specific complexities of HIV/AIDS did not obtain.
There has been widespread support for specialized health training and facilities for the care of women with HIV/AIDS; Bronx Lebanon Hospital has such a clinic for women (Citizens Commission on AIDS for New York City and Northern New Jersey, 1991). Such clinics, as planned, would focus on the social, economic, political, and psychological situation of women, factors that are often at the center of dealing with the nonmedical cofactors that affect the transmission and management of HIV disease.
As rates of HIV infection among women have increased, a number of medical investigators have begun to question earlier findings about the effects of HIV infection on the outcome of pregnancies. Asymptomatic HIV-infected female intravenous drug users in a New York City methadone program were not found to have decreased pregnancy rates or increased risk of adverse pregnancy outcomes. Moreover, acceleration in HIV disease during pregnancy was not found to be common (Selwyn et al., 1989b).
Data suggest that HIV-positive women are giving birth at rates normal for their age. Knowledge of their own HIV infection does not necessarily deter women from bearing children. Medical investigators associated with Montefiore Medical Center in the Bronx found that knowledge of HIV antibody status was not the overriding factor in decisions to terminate pregnancies; matters related to pregnancy—such as experience with a prior elective abortion, a negative emotional reaction to pregnancy, and whether the pregnancy had been unplanned—were more important (Selwyn et al., 1989a). Research conducted by anthropologist Anitra Pivnick among the same community of women explored the notion of reproductive choice in a broader context of family and social relations, economic circumstances, and cultural influences (see Pivnick et al., 1991). The 120 women in the study population—62 percent Hispanic (predominantly Puerto Rican), 30 percent African American, and 8 percent white—had a mean age of 34.9 years. Three factors distinguished HIV-positive women who chose to bear children from those who chose to terminate their pregnancy: prior abortion experience, the duration of knowledge of serostatus, and history of the mother's residence with existing children. Women who elected to continue with their pregnancies had a significantly lower lifetime abortion rate than women who chose abortions. They had also known of their serostatus for a significantly longer period of time, which presumably enabled them to consider decisions about childbearing without the pressures of pregnancy. Finally, women who had not lived with any child for 100 percent of the child's life were more likely to choose to bear a child than women who had that experience. (Many women in the study had themselves been "given away" by their own mothers and had confessed to life-long feelings of sadness and reproach.) Women who had managed to keep at least one of their own
children felt a profound sense of accomplishment. The study suggests that drug treatment options and family services, the first steps in keeping families together, could relieve many women of the need to replace lost offspring by giving birth to infants who face an unpromising future (Pivnick et al., 1991).
HIV positive women have difficulty obtaining abortions. In one study, test calls were placed to 25 abortion clinics. After the appointment was made, the caller revealed that she was HIV positive: 16 clinics (64 percent) canceled the appointment and refused to perform the procedure; others charged higher rates (Franke, 1989).
Data from a national, population-based survey to measure the prevalence of HIV infection in women giving birth to infants indicate that an estimated 1.5 of every 1,000 women giving birth to infants in 1989 were infected. The highest HIV seroprevalence rates were observed in New York (5.8 per 1,000) the District of Columbia (5.5 per 1,000), New Jersey (4.9 per 1,000), and Florida (4.5 per 1,000). Assuming a perinatal transmission rate of 30 percent, the authors estimate that approximately 1,800 newborns acquired HIV infection during one 12-month period (Gwinn et al., 1991). In another study, blood specimens collected from parturients in a recent New York City study indicate that as many as 2 percent of live births occur among women with HIV infection (Barbacci et al., 1990).
Further evidence of the high rates of HIV infection in childbearing women in New York is provided by the New York State Department of Health's newborn seroprevalence study. On the basis of the testing of blood specimens obtained from all infants born in the state between November 30, 1987, and March 31, 1990, the study found an overall seropositivity rate of 0.66 percent for childbearing women. The magnitude of the health problem was most striking in New York City, where in some zip code areas as many as 1 of every 22 childbearing women were found to be HIV-infected (Novick et al., 1991). The rates were highest in the Bronx, followed by Manhattan and then Brooklyn. The rates for Queens and Staten Island were more than twice the rates for the two New York State regions adjacent to New York City (New York City Suburban and Mid-Hudson Valley) (Novick et al., 1991). The lower overall seropositivity rate for New York State exclusive of New York City (0.17 percent) is deceptive, however, since zip code analyses revealed small areas with rates approaching those in New York City. This underscores the need for small-area information in assessing large geographic areas: apparently low seropositivity may mask communities with rates that are a serious public health concern (Novick et al., 1991).
The New York State study also showed the mothers of black and Hispanic newborns with the highest (0.87 percent) seropositivity rate. The rate of 0.12 percent for whites and for other racial and ethnic groups, however,
confirms a significant incursion of HIV infection in these populations as well (Novick et al., 1991). Moreover, newborn seropositivity increased with maternal age: an especially sharp rise in the infection rate was seen for women in New York City—from 1 in 624 at age 14 to 1 in 71 at age 24. Although racial/ethnic and maternal age patterns are needed for projections and resource allocation, race and age are not as such risk factors. Identifying the patterns offers insight into the environmental factors that determine prevalence and that allow for the targeting of preventive measures. Furthermore, as the rate of HIV infection among heterosexuals increases, current policies of offering HIV testing only to women with currently acknowledged risk factors will become even more inadequate (Barbacci et al., 1990).
Women with HIV/AIDS in poor urban neighborhoods also have special needs. Women in single-parent households must deal not only with the impact of their illness, but with their concerns about the children they will be leaving behind when they die (Indyk et al., 1990). It is expected that 20,000 children will be orphaned by AIDS in New York City by 1993 and that over the next few years 60,000-70,000 children will lose one parent to AIDS (Citizens Commission on AIDS for New York City and Northern New Jersey, 1991). Children of a mother who has died of AIDS are likely to confront stigma in school and in the community). Ignorance and prejudice about AIDS still undermine the intervention efforts of community-based health organizations attempting to deal with the special educational needs of those children.
Caring for Infected Children: Examples in Harlem
Pediatric HIV infection is a family disease: more than 80 percent of pediatric AIDS cases reported to the CDC identify perinatal exposure as the mode of transmission. Thus, a child with HIV disease is often the index case that leads to the identification of infected parents and siblings previously considered healthy. Extended kin often assist in the care of these children, providing support or acting as foster parents, and uninfected siblings are left to witness the deterioration and destruction of their family. Few diseases of childhood affect an entire family with such clarity (Abrams and Nicholas, 1990).
The situation at Harlem Hospital was described for the panel by pediatrician Elaine Abrams. The Pediatric AIDS Unit at Harlem aims to provide high-quality care for HIV-infected children largely in the context of highly disenfranchised families. Only one-half of the children are accompanied by their natural parents; many are in alternative or foster care settings. Extended kin—aunts, uncles, and especially grandmothers—often provide care for the children. The grandmothers, who may be suffering from the loss of their natural children, also face the burdens of failing health, limited financial
resources, and multiple responsibilities, which further complicate the medical management of a sick child (Abrams and Nicholas, 1990).
The care program at Harlem Hospital is supported to a significant degree with research funds. Although supporting clinical care through research grants is a strategy born of necessity, participation in a research protocol can enhance overall care. A research protocol enforces thoroughness and follow-up in cases for which medical and social data on patients may be hard to locate. The program's focus on integrated medical and social services for mothers and children allows research to be carried out in an otherwise chaotic milieu. The provision of primary care that focuses on the needs of families permits mothers, caretakers, and children to comply with the requirements of a research protocol. The reverse is also true: in the absence of integrated care, research would not be possible.
The benefits of this approach are clear, but difficulties are also present. The continuity of research funds cannot be guaranteed. Balancing the needs of mothers and children may cause conflicts. Some hospital staff, patients, and child welfare professionals tend to mistrust or fear scientific research. Many HIV-positive children are in foster custody, and social workers and others who care for those children understandably wish to protect their rights. The staff at Harlem Hospital, however, work closely with the foster care system, acknowledging the disadvantages as well as the advantages of experimental protocols. The Child Welfare Administration of New York City has developed a medical advisory board to evaluate protocols and now advises that the "best potential treatment option" may be experimental therapy. In such cases, a child's natural parents are approached for their consent. If the parents are deceased or cannot be found after diligent effort, the commissioner may grant consent for the child's entry into an experimental protocol.
In 1986 and 1987 few alternatives existed for the care of HIV-positive children outside of the households of their natural parents. Many children who were medically ready for discharge but whose natural parents could not care for them thus spent much of their lives as "boarder babies," hospitalized for want of a less institutional setting for care (Hegarty et al., 1988). Since 1988 several options have been developed. Resources have been made available to recruit foster care families willing to care for children at risk for HIV infection. New York City established the Incarnation Children's Center (ICC), a transitional unit that offers medical care and nurturing in a home-like environment. Children remain at ICC until an appropriate foster home is identified.
In contrast to the widespread assumption that HIV-positive children are often "abandoned," experience at ICC shows that only 20 percent of children come to ICC through abandonment at time of admission: 80 per cent of the children admitted to Incarnation Center during the past 2-1/2 years do
have some involvement with family members. About one-third have frequent weekly visits from parents or immediate extended kin, and about one-third have occasional visits (every 2 to 4 weeks) from both male and female family members. Fathers visit children at the Center (which is located at the edge of Harlem) more often than they do at Harlem Hospital. The homelike atmosphere at ICC perhaps encourages more frequent visits, especially by older fathers who work and who have relationships with drug-addicted mothers.
A total of 190 children have so far been cared for at ICC, of whom 162 children are now in homes: 85 percent are in foster homes with nonrelatives, and 15 percent have been returned to their natural families, although they were originally slated for transfer to foster homes. As the number of infected children continues to rise, the need for additional alternate care facilities will also increase. The experience at ICC shows that the length of the children's stays in hospital can be reduced and that children and their families can be offered nurturing care that is difficult to provide in hospital settings.
There are now a number of children with HIV/AIDS in the local Harlem schools. Some were infected through blood products; others became infected through perinatal transmission. The availability of medical treatments has increased the expected lifespan of infected children, and HIV-infected children as old as 10, 11, and 12 years of age are in school. In addition to HIV-related health problems, some children manifest behavior disorders related to factors other than HIV. Fetal alcohol syndrome may be evident, as well as the long-term effects of low birthweight, lack of prenatal care, and maternal drug use during pregnancy. And some children may live with mothers who continue to take drugs or who live with men who do.
At school, HIV-infected children often face a staff that lacks the knowledge or means to confront the many problems associated with their condition. At home, for complex reasons that include fear of community reaction or the desire to protect the child from full knowledge about the illness, parents or caretakers may also avoid discussing the full dimensions of the disease. However, with earlier diagnosis and treatment that can now prolong life, there are stronger incentives to deal with the fear and prejudice that HIV infection arouses. Some experts argue that the concept of long-term, complex medical therapy should be presented to educators, caretakers, and medical staff (including physicians) and reinforced over time (Abrams and Nicholas, 1990).
RELIGION: CONFLICT OVER CONDOMS AND AIDS EDUCATION FOR YOUNG PEOPLE
From the beginning of the HIV/AIDS epidemic, there has been a continuous conflict over the role of education about safer sex and condoms in preventing the transmission of HIV. This debate has been particularly sharp when the targets of the educational and condom distribution programs have been young people of high school age, although there has been strong resistance in the national government to condom education for persons of all ages (Specter, 1989).
The proponents of safer sex education and condom provision to youths point out that they do not necessarily approve of early sexual experimentation on the part of young people, but that large numbers of young persons are sexually active under conditions of relative ignorance about the consequences of their conduct. The decision not to provide safer sex education or condoms to young people places them in danger of the transmission of HIV and other STDs that increase the likelihood of HIV transmission. The arguments of the proponents are short term, pragmatic, and health oriented: young people are sexually active; it is unlikely that they will abstain regardless of how often they are exhorted, and they are in danger of contracting a fatal disease. The logical consequence of this position is the provision of age-appropriate sex education that includes information about same-gender sex, modes of HIV transmission and methods of prevention, as well as the provision of condoms without either mandatory counseling or parental consent.
The opponents of safer sex education and the provision of condoms stress the long term, the role of the parent and church versus the school and the state, and issues of morality. In their view, the control of the sexuality of young people properly resides with parents and the religious institutions to which parents and children belong, which emphasize chastity before marriage and fidelity afterward. The provision of safer sex education and condoms threaten these goals and appear to condone sexual experimentation. For some religious groups, such as the Roman Catholic church, condoms are a completely forbidden form of birth control.
The antagonists in New York City have been locked in a debate largely directed not at each other, but at the relatively uncommitted wider community. The immediate targets of the arguments are such decision makers, such as school board members and school administrators or those who appoint them.
When condom provision in the public senior high schools was proposed in 1986, an active coalition of religious groups, spearheaded by the Archdioceses of New York and Brooklyn, persuaded the school board to reject the proposal. In the fall of 1990 the new school chancellor asked that the
members of the newly appointed school board support a plan for condom distribution (Berger, 1990b). He noted the many AIDS cases among young people and reported that 80 percent of New York City's 261,000 public high school students were having intercourse. Four of the five new members of the seven-member board reported that they favored such distribution. The plan was opposed by one board member, who said, "It sends a message to young people that we expect them to have sex" (Berger, 1990b:B4). The officials of the Roman Catholic church made their position clear by pointing out that condom provision "says that the universal value that places sexual activity as acceptable only within the context of marriage can neither be taught by our schools nor accepted by our students" (Berger, 1990b:B4).
In December 1990 the Board of Education received the chancellor's plan to distribute condoms to all students who requested them. All public high schools were to be included, and counseling or parental consent was not required (Berger, 1990d). Opponents remained adamant, and some potential supporters wanted counseling to be provided, including information on condom use and how to persuade a partner to use one. In addition, they wanted all students to be told that sexual abstinence before marriage is the best method of prevention (Berger, 1990a). Proponents of the program wished to dissociate it from pregnancy prevention—the issues were simply those of HIV disease and health. They hoped to avoid further conflict with the Roman Catholic church over birth control.
The role of the Roman Catholic church in AIDS education and prevention had already produced conflict regarding church obligations in AIDS prevention education when receiving state funds for health care services. The New York State Public Health Council voted to exempt Catholic-operated nursing homes and hospitals from the requirement that HIV/AIDS patients receive condoms, safer sex counseling, contraceptives, and abortion services. AIDS activists opposed receipt of public funds by Catholic-operated institutions unless they agreed to provide prevention information (e.g., the role of condoms in AIDS prevention), which they declined to do because it is contrary to church doctrine. The church stated that such information violates its "institutional conscience" and can be received elsewhere. In another dispute, the Archdiocese refused to lease to the Board of Education unused Catholic parochial school space for special education classes on AIDS prevention. The leases were barred unless the board waived its sex education curriculum, which includes information on forms of contraception not approved by the church. The decision was based on the evaluation of the 1984 sex education curriculum that, according to the evaluation "makes no mention of modesty, chastity, premarital sexual abstinence or even marital fidelity" (Goldman, 1991:30).
The Board of Education itself was divided on the condom plan. The four African American and Hispanic members favored it (in varying degrees),
and the three white members opposed it, again in varying degrees. One of the opponents objected to the board's citation in its curriculum of literature from a gay and lesbian organization that had published a booklet that one board member considered particularly offensive, although that booklet was not used in school education (Berger, 1990c).
An open meeting conducted by the board in February 1991 attracted 277 speakers and ran from 10 a.m. until late in the evening. The division between the proponents and opponents was clear: on one side were religious groups and those whose allegiance was to traditional values; on the other side were health professionals, AIDS workers, persons with AIDS, and activist groups. The disagreements among African Americans mirrored the larger debate, with distortions born of racial discrimination: Did the provision of condoms to African American youths signal a racist lack of faith in their ability to be sexually abstinent? (This same subtext framed the needle-exchange debate: the conflict between health promotion and the danger that needle provision would simply support or expand the use of drugs in already afflicted communities.) Actual research about the utility of condoms, either in preventing HIV transmission or in influencing the sexual activity of young people, was rarely cited in the debate over condom use. The actual experiences of school districts across the country that had implemented condom programs were rarely discussed (Lewin, 1991). The complexity of the studies and the mixed results they presented seemed to limit their usefulness in public debate (Dreyfoos, 1991). A few weeks after the public meeting Mayor David Dinkins backed the condom plan without counseling or parental consent (Berger, 1991a). The board approved the plan for condom provision without parental consent by a vote of four to three, divided along racial and ethnic lines, with some discussion of a future provision for a parental option to exclude their children from the program (Berger, 1991b).
The ideological structure of the conflict and the social composition of the opposing groups were predictable and similar to conflicts over HIV/AIDS and sexuality in other communities and at the national level. Although the specific outcome in any community is unpredictable, there are constants: the relative inadequacy of scientific evidence on those questions for which science is important (e.g., if the presence of a condom provision program increases or decreases sexual activity among the young) and the irrelevance of scientific findings in settling what are ultimately conflicts between different religious and secular perspectives on the solution of social problems.
CONCLUSIONS
The panel's findings on the HIV/AIDS epidemic among gay men, intravenous drug users, and women and children in New York City reflect a highly localized epidemic that is increasingly concentrated among poor people and racial and ethnic minorities. Responding to the problem of HIV requires knowledge of the local communities and an understanding of the cultural realities of those who live there. The inner-city poor may live in New York City, but they do not live in the same New York City as those who are more affluent and better protected from the epidemic (and many other risks) by regular employment, health care insurance, and lower crime rates. Those with HIV/AIDS among the inner-city poor often live and die in invisible neighborhoods within the segregated communities of the city.
The February 1991 end of the Citizens Commission on AIDS for New York City and Northern New Jersey was an important signal of the changed political and economic context at the beginning of the second decade of the HIV/AIDS epidemic. The commission was a major example of a foundation-supported volunteer attempt to provide private-sector leadership and offer a nonpartisan influence on public policy in dealing with HIV/AIDS. Its demise, after somewhat less than 4 years of life, can be attributed to the normal processes of wear and tear on volunteer efforts, the completion of some of the original tasks set by the organization, and the declining interest of the private funding sector in supporting organizations dealing with the HIV/AIDS epidemic. Indeed, in its final report, the commission reflected on the unfinished task and what lies ahead in what may yet be the most devastating phase of the epidemic (Citizens Commission on AIDS for New York City and Northern New Jersey, 1991):
The AIDS epidemic continues its relentless course, with no end in sight. But AIDS is fading from public concern. When the Citizens Commission on AIDS was created three and a half years ago, AIDS was an unpopular cause. It is now rapidly becoming a "post-popular" cause, without ever having truly engaged widespread public support.
Such a conclusion after the first decade of an epidemic that has taken a minimum of 30,000 lives in New York City requires an attempt to understand a catastrophe that may ultimately take nearly 200,000 lives in New York City, cost billions of dollars, and leave untold numbers of shattered lives, but will have passed through the city without fundamental impacts on the overall life of the city.
Epidemics appear to have much in common. They share a common dramaturgical form of progressive acknowledgment, collective agreement on an explanatory framework, and a negotiated public response (Rosenberg, 1989). They differ, however, according to the particular social and biological environments in which they take place. HIV disease in New York City
occurs increasingly in the context of socioeconomic and ethnic deprivation, as well as among populations already suffering high levels of morbidity and mortality. The New York City epidemic is thus exceptional in certain ways, but it is not exceptional in that it is embedded in the ongoing life of the city (to some extent, in the life of Northern New Jersey and San Juan, Puerto Rico, as well). The particular impact of the HIV/AIDS epidemic can only be appreciated when one examines the complex of social and biological problems with which it constantly interacts.
Such an examination, even though only partially covered in this report, has revealed that the synergism of plagues that converges on certain areas of New York City and the people who dwell in them creates the seedbed for an epidemic that will devastate those people far more seriously than HIV/AIDS will devastate the nation at large. In those areas—as in similar areas in cities throughout the country—the social institutions that might control the spread of the disease and provide care for those who suffer from it are already overburdened or nonexistent. The panel does not believe one can generalize from New York City to the United States; at the same time, the panel suggests that monitoring the impact of HIV/AIDS, that is, attempting to see the epidemic's course in light of the social context in which it moves, will show similar patterns elsewhere.
NOTE
REFERENCES
ACT-UP/New York (1991) ACT-UP New York: Capsule History. New York: ACT-UP.
Abrams, E.J., and S.W. Nicholas (1990) Pediatric HIV infection. Pediatric Annals 19(8):482-487.
Adam, B.D. (1987) The Rise of a Gay and Lesbian Movement. Boston: Twayne Publishers.
Altman, L.K. (1991) New York moving to limit TB spread. New York Times December 8:A1.
Andrews, R., B. Preston, E. Howell, and M. Keyes (1989) A Comparative Analysis of AIDS Service Demonstration Projects in Los Angeles, Miami, New York, and San Francisco. Washington, D.C.: SysteMetrics/McGraw Hill, Inc.
Aral, S., and K. Holmes (1990) Epidemiology of personal behavior and sexually transmitted diseases. In K. Holmes, et al., Sexually Transmitted Diseases. New York: McGraw Hill.
Aral, S.O., and K.K. Holmes (1991) Sexually transmitted diseases in the AIDS era. Scientific American 264:62-69.
Association of the Bar of the City of New York/Joint Subcommittee on AIDS in the Criminal
Justice System (1989) AIDS and the Criminal Justice System: A Final Report and Recommendations. New York: Association of the Bar of the City of New York.
Barbacci, M.B., G.A. Dalabetta, J.T. Repke, B.L. Talbot, P. Charache, et al. (1990) Human immunodeficiency virus infection in women attending an inner-city prenatal clinic: ineffectiveness of targeted screening. Sexually Transmitted Diseases 17:122-126.
Barnes, P.F., A.B. Bloch, P.T. Davidson, and D.E. Snider (1991) Tuberculosis in patients with human immunodeficiency virus infection. New England Journal of Medicine 324:1644-1649.
Bayer, R. (1981) Homosexuality and American Psychiatry: The Politics of Diagnosis. New York: Basic Books, Inc.
Bayer, R. (1991) The dependent center: the first decade of the AIDS epidemic in New York City. Unpublished manuscript, Department of Sociological Medical Sciences, Columbia University.
Belkin, L. (1991) Top TB peril: not taking medicine. New York Times November 18:B1.
Berger, J. (1990a) Condom plan for schools draws criticism. New York Times December 6:B1.
Berger, J. (1990b) Five out of seven ask condoms in the schools: New York's chancellor backed on distribution. New York Times September 27:B1.
Berger, J. (1990c) New York city school board members clash on condom proposal. New York Times December 20:B4.
Berger, J. (1990d) Opposition to condom plan by some principals is seen. New York Times December 5:B3.
Berger, J. (1991a) Dinkins backs condom plan: some board members work on a compromise. New York Times February 26:B1.
Berger, J. (1991b) School board approves plan for condoms: rejects any provision for parental consent. New York Times February 28:B1.
Blumstein, P., and P. Schwartz (1983) American Couples. New York: William Morrow.
Brudney, K., and J. Dobkin (1991) Resurgent tuberculosis in New York City: HIV, homelessness, and the decline of tuberculosis control programs. American Review of Respiratory Disease 144:745-749.
Bryant, M. (1991) ACT-UP: playing the inside and the outside. Medicine and Health Perspectives April 1.
Buehler, J.W., R.L. Berkelman, and J.K. Stehr-Green (1992) The completeness of AIDS surveillance. Journal of Acquired Immune Deficiency Syndromes 5(3):257-264.
Cade, J. (1990) Status report: state prisons and the courts. National Prison Project Journal 22(Winter):7-8.
Carey, J.M. (1990) AIDS in New York City. New York: American Council on Science and Health.
Carrier, J.M. (1989) Sexual behavior and the spread of AIDS in Mexico. Medical Anthropology 10:129-142.
Centers for Disease Control (CDC) (1990) HIV/AIDS Surveillance Report . December:1-8. Atlanta, Ga.: Centers for Disease Control.
Centers for Disease Control (CDC) (1992) HIV/AIDS Surveillance Report . Atlanta, Ga.: Centers for Disease Control.
Chaisson, M.A., R.L. Stoneburner, D.S. Hildebrandt, W.E. Ewing, E.E. Telzak, et al. (1990) Heterosexual Transmission of HIV-1 With the Use of Smokeable Freebase Cocaine Crack. Paper presented at the Sixth International Conference on AIDS, San Francisco.
Chambre, S.M. (1991) The volunteer response to the AIDS epidemic in New York City: implications for research on voluntarism. Nonprofit and Voluntary Sector Quarterly 20:267-288.
Chavkin, W. (1990) Drug addiction and pregnancy: policy crossroads. American Journal of Public Health 80:483-487.
Citizens Commission on AIDS for New York City and Northern New Jersey (1991) AIDS: Is There a Will to Meet the Challenge? New York: Citizens Commission on AIDS for New York City and Northern New Jersey.
Clatts, M.C. (1992) Poverty, drug use, and AIDS: converging lines in the life stories of women in Harlem. In Minority Women and Health: Gender and the Experience of Illness. (In Press).
Clatts, M.C., E. Springer, and M. Washburn (1990a) Outreach to Homeless Youth in New York City: Implications for Planning and Practice in Social Services. Paper presented at the annual meeting of the American Public Health Association, New York.
Clatts, M.C., W.R. Davis, S. Deren, and S. Tortu (1990b) 1990: Sex for Crack: The Many Faces of Risk Within the Street Economy of Harlem. Paper presented at the 2nd Annual Demonstration Conference, Bethesda, Maryland,
Dao, J. (1992) New York's prisoners with AIDS ask for dignity during last days. New York Times March 22:A1.
Des Jarlais, D.C. (1985) AIDS Among Intravenous Drug Users: Overview and Update. Paper presented at the International Conference on AIDS, Atlanta, Georgia.
Dobie, K. (1990) Stick men and giants: inside the Rikers Island AIDS ward. Village Voice December 4:28-37.
Dreyfoos, J. (1991) Condoms can decrease teen-age pregnancy and AIDS risks. New York Times February 11:A18.
Drucker, E. (1986) AIDS and addiction in New York City. American Journal of Drug and Alcohol Abuse 12:165-181.
Erikson, K.T. (1976) Everything in Its Path: Destruction of Community in the Buffalo Creek Flood. New York: Simon and Schuster.
Fordyce, E.J., and R. Stoneburner (1990) Patterns of High Risk Sexual Behavior Among Gay and Bisexual Clients at New York City STD Clinics, 1981-1989, and Associated AIDS Morbidity Trends. Paper presented at the annual meeting of the American Public Health Association, New York.
Fordyce, E.J., S. Blum, A. Balanon, and R.L. Stoneburner (1991) A method for estimating HIV transmission rates among female sex partners of male intravenous drug users. American Journal of Epidemiology 130:590-598.
Franke, K.M. (1989) Discrimination Against HIV Positive Women by Abortion Clinics in New York City. Paper presented at the Fifth International Conference on AIDS, Montreal.
Gage, L.S., V.S. Weslowski, D.P. Andrulis, E. Hintz, and A.B. Campter (1991) America's Safety Net Hospitals: The Foundation of Our Nation's Health System. Washington, D.C.: National Association of Public Hospitals.
Gager, C.T. (1988) Twelve Health Center Districts in Need: A Birth Atlas. New York: Community Service Society of New York.
Gangi, R., and J. Murphy (1990) Imprisoned Generation: Young Men Under Criminal Custody in New York State. New York: Correctional Association of New York.
Gemson, D.H., J. Colombotos, J. Elinson, E.J. Fordyce, and R. Stoneburner (1989) The Role of the Physician in AIDS Prevention: A Survey of Primary Care Physicians in New York City. Final Report to the New York City Department of Health.
Goldman, A.L. (1991) Citing sex classes, bishop bars school leases. New York Times January 12:30.
Greenberg, A.B., R. Evans, E. Bryan, E. Lopez, and P. Thomas (1990) Completeness of AIDS Case Reporting and the Spectrum of HIV Disease Among Outpatients in New York City. Paper presented at the Sixth International Conference on AIDS, San Francisco.
Gwinn, M., M. Pappaioanou, J.R. George, W.H. Hannon, S.C. Wasser, M.A. Redus, R. Hoff,
F.G. Grady, A. Willoughby, A.C. Novello, L.R. Peterson, T.J. Dondero, and J.W. Curran (1991) Prevalence of HIV infection in childbearing women in the United States. Journal of the American Medical Association 265(13):1704-1708.
Hamid, A. (1990) The political economy of crack-related violence. Contemporary Drug Problems Spring:31-78.
Hammett, T.M., S. Moini, L. Harrold, and M. Weissberg (1989) 1988 Update: AIDS in Correctional Facilities. Issues and Practices in Criminal Justice. Washington, D.C.: National Institute of Justice.
Hansfield, H.H. (1986) Totally safe sex or AIDS response. American Journal of Pubic Health 76(5):588-589.
Hansell, D. (1990) Presentation to NAS Panel on Monitory Social Impact of the AIDS Epidemic New York Study Group. April 2, 1990.
Hawkeswood, W.G. (1991) One of the Children: An Ethnography of Identity and Gay Black Men. Ph.D. dissertation. Anthropology Department, Columbia University.
Hegarty, J.D., E.J. Abrams, V.E. Hutchinson, S.W. Nicholas, M.S. Suarez et al. (1988) The medical care costs of human immunodeficiency virus-infected children in Harlem. Journal of the American Medical Association 260:1901-1905.
Holmes, K.K., J.M. Karon, and J. Kreiss (1990) The increasing frequency of heterosexually acquired AIDS in the United States, 1983-1988. American Journal of Public Health 80:858-863.
Hopper, K. (1990) The new urban niche of homelessness: New York city in the late 1980s. Bulletin of the New York Academy of Medicine 66:435-50.
Inciardi, J.A. (1991) King rats, chicken heads, slow necks, freaks and bloodsuckers: a glimpse at the Miami sex for drugs market. Unpublished manuscript, Department of Criminal Justice, University of Delaware.
Kenny, M., J. Mantel, N. Cortez, V. Gonzalez, and L.S. Brown (1990) HIV Prevention Among Women at Risk: An Ethnographic Analysis. Paper presented at the annual meeting of the American Public Health Association, New York.
Lambert, B. (1988a) The cool reaction to New York's ''good news" on AIDS, dissent and distrust. New York Times July 21:B1,B2.
Lambert, B. (1988b) Halving of estimate on AIDS is raising doubts in New York. New York Times July 20:A1.
Lambert, B. (1988c) Number of AIDS cases in New York still varies. New York Times September 23:B3.
Lambert, B. (1988d) Puzzling questions are raised on statistics on AIDS epidemic. New York Times July 24:B4.
Lambert, B. (1990a) AIDS travels New York-Puerto Rico "air bridge." New York Times June 15:B1.
Lambert, B. (1990b) AIDS war shunned by many doctors. New York Times April 23:A1.
Lessner, L. (1991) Projection of AIDS incidence in women in New York. American Journal of Public Health 81(Suppl.: The New York State HIV Seroprevalence Project):30-34.
Levine, M.P. (1979) Gay ghetto. Journal of Homosexuality 4:363-377.
Levine, M.P. (1989) The Impact of AIDS on the Homosexual Clone Community in New York City. Paper presented at the Fifth International Conference on AIDS, Montreal.
Lewin, T. (1991) Studies on teen age sex cloud condom issue. New York Times February 8:A14.
Loomis, K. (1989a) AIDS: The numbers game. New York March 6:44-49.
Loomis, K. (1989b) Voodoo statistics: the health department's mess. Village Voice April 4:33-34.
Marotta, T. (1981) The Politics of Homosexuality. Boston, Mass.: Houghton Mifflin Co.
Martin, J.L., M.A. Garcia, and S. T. Beatrice (1989) Sexual behavior changes and HIV antibody
in a cohort of New York City gay men. American Journal of Public Health 79(4):501-503.
McFadden, R.D. (1992) A drug-resistant TB results in 13 deaths in New York prisons. New York Times November 16:A1.
Menendez-Bergad, S., E. Drucker, S.H. Vermund, R.R. Castano, R.R. Perez-Agosto, et al. (1990) AIDS mortality among Puerto Ricans and other Hispanics in New York City, 1981-1987. Journal of Acquired Immune Deficiency Syndromes 3:644-648.
Miller, H.G., C.F. Turner, and L.E. Moses (1990) AIDS: The Second Decade. Committee on AIDS Research and the Behavioral, Social, and Statistical Sciences, National Research Council. Washington, D.C.: National Academy Press.
Morse, D.L., L. Lessner, M.G. Medvesky, D.M. Glebatis, and L.F. Novick (1991) Geographic distribution of newborn HIV seroprevalence in relation to four sociodemographic variables. American Journal of Public Health 81(Suppl.: The New York State HIV Seroprevalence Project):25-29.
Musto, D. (1987) The American Disease: Origins of Narcotic Control. New York: Oxford University Press.
Navarro, M. (1991) Dated AIDS definition keeps benefits from many patients. New York Times July 8:A1,B5.
Navarro, M. (1992) AIDS patients, facing TB, now fear even the hospital. New York Times March 15:A1.
New York City Commission on Human Rights (1989) The Extent and Impact of HIV-Related Discrimination in New York City—A Survey of PWAS and Service Providers. Unpublished draft report, AIDS Division, New York City Commission on Human Rights.
New York City Department of Health (1989a) City Health Information 8(4).
New York City Department of Health (1989b) City Health Information 8(7).
New York City Department of Health (1990a) Cases of AIDS in Your Neighborhood: The Bronx. Cumulative Adult AIDS Case by Race, Gender, Age and Risk Factor. August 1990. AIDS Program Services, New York City Department of Health.
New York City Department of Health (1990b) Cases of AIDS in Your Neighborhood: Brooklyn. Cumulative Adult AIDS Case by Race, Gender, Age and Risk Factor. August 1990. AIDS Program Services, New York City Department of Health.
New York City Department of Health (1990c) Cases of AIDS in Your Neighborhood: Manhattan. Cumulative Adult AIDS Case by Race, Gender, Age and Risk Factor. August 1990. AIDS Program Services, New York City Department of Health.
New York City Department of Health (1990d) Cases of AIDS in Your Neighborhood: Queens. Cumulative Adult AIDS Case by Race, Gender, Age and Risk Factor. August 1990. AIDS Program Services, New York City Department of Health.
New York City Department of Health (1990e) Cases of AIDS in Your Neighborhood: Staten Island. Cumulative Adult AIDS Case by Race, Gender, Age and Risk Factor. August 1990. AIDS Program Services, New York City Department of Health.
New York City Department of Health (1991) City Health Information 10(3).
New York State Department of Health (1988) AIDS in New York State. Albany: New York State Department of Health.
New York State Department of Health (1989) AIDS in New York State. Albany: New York State Department of Health.
New York State Department of Health, New York AIDS Institute (1989) Management of HIV Infection in New York State Prisons.
New York State Department of Health (1990) AIDS in New York State. Albany: New York State Department of Health.
New York Times (1989) Crack: a disaster of historic dimension, still growing. New York Times May 28:E14.
Novick, L.F., D.M. Glebatis, R.L. Stricof, P.A. MacCubbin, L. Lessner, et al. (1991) Newborn seroprevalence study: methods and results. American Journal of Public Health 81(suppl.):15-21.
Oppenheimer, G.M., and R.A. Padgug (1991) AIDS and the crisis of health insurance. In F. Reamer, ed., AIDS and Ethics. New York: Columbia University Press.
Pivnick, A., A. Jacobson, K. Eric, M. Hsu, M. Mulvihill, and E. Drucker (1991) Reproductive decisions among HIV-infected, drug-using women: the importance of mother-child coresidence. Medical Anthropology Quarterly 5(2):153-169.
Potler, C. (1988) AIDS in Prison: A Crisis in New York State Corrections . New York: The Correctional Association of New York.
Purdum, T.S. (1990) Nominee for health commissioner loses vital backing. New York Times January 19:B1.
Raab, S. (1991) New York State to install 3000 more prison beds. New York Times December 8:52.
Ricardo, M. (1990) Differences in AIDS-Related Knowledge and Beliefs About Condom Use Among Black and Hispanic Women of U.S. and Non-U.S. Origin. Paper presented at the IV International Conference on AIDS Education, San Juan, Puerto Rico.
Rosenberg, C.E. (1989) What is an epidemic—AIDS in historical perspective. Daedalus 118(2):1-17.
Rosenthal, E. (1990) Health problems of inner city poor reach crisis point. New York Times December 24:1.
Rothman, D.J., E.A. Tynan, and the New York City Task Force on Single-Disease Hospitals (1990) Advantages and disadvantages of special hospitals for patients with HIV infection: a report by the New York City Task Force on Single-Disease Hospitals. New England Journal of Medicine 323:764-768.
Russell, M. (1990) Impediments to Accessing Services for Black Gay and Bisexual Men Who Choose Not to be "Gay Identified." Paper presented at the Sixth International AIDS Conference, San Francisco.
Schoenbaum, E.E., D. Hartel, P.A. Selwyn, R.S. Klein, K. Davenny, et al. (1989) Risk factors for human immunodeficiency virus infection in intravenous drug users. New England Journal of Medicine 321:874-879.
Selwyn, P.A., R.J. Carter, E.E. Schoenbaum, V.J. Robertson, R.S. Klein, et al. (1989a) Knowledge of HIV antibody status and decisions to continue or terminate pregnancy among intravenous drug users. Journal of the American Medical Association 261:3567-3571.
Selwyn, P.A., E.E. Schoenbaum, K. Davenny, V.J. Robertson, A.R. Feingold et al. (1989b) Prospective study of human immunodeficiency virus infection and pregnancy outcomes in intravenous drug users. Journal of the American Medical Association 261:1289-1294.
Siegel, K., and M. Glassman (1989) Individual and aggregate level change in sexual behavior among gay men at risk for AIDS. Archives of Sexual Behavior 18(4):335-348.
Smith, P.F., J. Mikl, B.I. Truman, L. Lessner, J.S. Lehman, et al. (1991) HIV infection among women entering the New York state correctional system. American Journal of Public Health 81(Suppl.: The New York State HIV Seroprevalence Project):35-40.
Specter, M. (1989) HHS aide blocks publication of pamphlet on condom use: action on AIDS-education brochure angers officials. Washington Post October 7:A2.
Stall, R., M. Ekstrand, L. Pollack, L. McKusick, and T.J. Coates (1990) Relapse from safer sex: the next challenge for AIDS prevention efforts. Journal of Acquired Immune Deficiency Syndrome 3:1181-1187.
Stoneburner, R.L., D.C. DesJarlais, D. Benezra, L. Gorelkin, J.L. Sotheran, et al. (1988) A larger spectrum of severe HIV-1-related disease in intravenous drug users in New York City. Science 242:916-919.
Taylor (1990) AIDS guerrillas. New York Magazine November 12:62-73.
Tierney, J. (1990) Newark's spiral of drugs and AIDS. New York Times December 16:A1, A23.
Trafford, A. (1988) The AIDS numbers game: body counts, on paper, are the latest political battleground. Washington Post (health section) July 26:WH6.
Turner, B., T. Fanning, M. Keyes, and L. Markson (1989) New York Medicaid AIDS Patients: Trends in Hospital Use and Mortality Rates. Paper presented at the Fifth International AIDS Conference, Montreal.
U.S. General Accounting Office (1989) AIDS Forecasting: Undercount of Cases and Lack of Key Data Weaken Estimates. GAO/FMED-89-13. Washington, D.C.: U.S. General Accounting Office.
Verhovek, S.H. (1991) Spouse visits for inmates with HIV. New York Times August 5:B1.
Wallace, R. (1988) A synergism of plagues: "planned shrinkage," contagious housing destruction and AIDS in the Bronx. Environmental Research 47:1-33.
Wasserman, G.A., V.A. Rauh, S.A. Brunelli, M. Garcia-Castro, and B. Necos (1990) Psychosocial attributes and life experiences of disadvantaged minority mothers: age and ethnic variations. Child Development 61(2):566-580.
Weinberg, M.S., and C.J. Williams (1974) Male Homosexuals. New York: Oxford University Press.
Williams, T.M., C.E. Sterk, S.R. Friedman, C.E. Dozier, and J.L. Sotheran (1988) Crack Use Puts Women at Risk for Heterosexual Transmission of AIDS. Paper presented at Fourth International Conference on AIDS, Stockholm, Sweden.
Worth, D. (1989) Sexual decision-making and AIDS: Why condom promotion among vulnerable women is likely to fail. Studies in Family Planning 20:297-307.