Summary
Beyond the oft-quoted figures about how many Americans are without health insurance, policymakers and the public have few regularly reported indicators to characterize concretely the problems of access to health care services. The images and case stories that appear in the news media give life to the problems of those who cannot obtain the services they need. Yet individual stories cannot systematically reveal the size and changing nature of access problems, their causes, and their effects. The need for this information has been heightened by growing national interest in health care reform, one objective of which is improved access. Whether this objective of federal reform efforts is being achieved cannot be assessed adequately without better health-related indicators.
The mandate of the Institute of Medicine (IOM) to a 17-member committee of experts chosen for the Access Monitoring Project was to develop a set of indicators for monitoring access to personal health care services at the national level over time. It was envisioned that these indicators would be akin to national economic indicators—the unemployment rate, new housing starts, the inflation rate, consumer confidence surveys—which provide a picture of the state of the economy and how it might be changing. Similarly, access indicators would allow us to track whether conditions for obtaining care, particularly among vulnerable groups in society, were improving or getting worse. In addition, like economic indicators, the expectation of routinely available reports would stimulate national debate about needed policy actions and the consequences of actions taken.
The focus of this report, like the committee's deliberations, is on access to personal health services—the one-on-one interaction of provider and patient. The committee chose five objectives of personal health care to organize its indicators: successful birth outcomes, reducing the incidence of preventable diseases, early detection and diagnosis of treatable diseases, reducing the effect of chronic diseases and prolonging life, and reducing morbidity and pain through timely and appropriate treatment. This specific focus on personal health care does not gainsay the important investments society can make in population-based strategies in such areas as the environment, pollutants, health education, occupational health, and injury control. Policies in these fields could potentially save more lives and have a greater impact on quality of life than programs to extend health services. Nonetheless, the large proportion of the nation's resources being devoted to personal health care has provoked considerable interest in monitoring those investments from the standpoint of equity of access.
The IOM committee's approach to developing indicators was to find measures that would track the use of services known to have measurable effects—for example, prenatal care. An outcome of using these effective services—fewer low birthweight infants—is also an indicator of access to services that can be monitored. Analysis of these indicators would provide information on the effects of health policies; the data could be used in turn in making choices with regard to the three major concerns of health care policymaking: access, quality, and cost.
This study had two key objectives: first, to propose an initial set of indicators that lays the groundwork for the evolution of a monitoring system and, second, to use those indicators to assess the current state of access at the national level. The first objective entailed clarifying what is really meant by saying we want to improve access and translating concerns about who cannot get what type of care into a limited and cohesive set of indicators that can offer reliable and valid measurements. Applying these indicators to produce an assessment about access, the second objective, involved obtaining a decade's worth of data, analyzing the data, and interpreting the meaning of trends.
Although the state of the art of monitoring access is still at an elementary stage, there is sufficient information available to draw some important conclusions. In most instances the basic data bases exist to measure the indicators chosen, but crucial modifications in how and when data are collected are necessary to make them more useful for monitoring. The committee offers numerous recommendations in this report for the data collection and research needed to push the evolution of monitoring forward at a faster, surer pace.
GENERAL CONCLUSIONS ON THE STATE OF ACCESS
As a whole, indicators of access to personal health care services provide little encouraging evidence of progress over the past decade. Stagnation is the single best word to characterize our current state. Successes like improvements in breast cancer screening are counterbalanced by the return of diseases that can be avoided, like tuberculosis and congenital syphilis. Underlying most of the indicators is a growing division between the haves and the have-nots in our society.
A large group of citizens in this country make contact with medical providers only a little more than half as often as their fellows. This group lacks health care coverage and is generally at the low end of the income scale. Indicators that measure health outcomes suggest that at least for people from low-income neighborhoods the difference in health care use has a profound impact on their health and well-being. Admission rates to hospitals for conditions that should be controlled with appropriate ambulatory care are on average four times higher for residents of low-income than for high-income neighborhoods. The committee believes that evidence is building to demonstrate that no or inadequate health care coverage is the reason many of these people fail to obtain the timely and appropriate care that would make a difference in the state of their health. Further work is required, however, to establish solid causal linkages between the access barriers of lack of health insurance, low-income, and nonfinancial factors such as culture and geographic isolation and measures of outcome such as premature death, sickness, disability, and avoidable hospitalization.
Compared with other groups in society, blacks and some ethnic minorities are more likely to have low-incomes and inadequate health insurance. The effects of these burdens are borne out by utilization and outcome indicators virtually across the board. There is evidence of inequity in the timely receipt of ambulatory care, immunizations, dental visits, and some sophisticated procedures. Even in instances in which general improvement can be seen that spans the U.S. population, improvement is slower for these groups—especially blacks.
Some of the most striking differences can be found in mortality rates by race. After controlling for a number of behavioral risk factors, a wide gap persists between mortality rates of middle-aged black men and women and their white counterparts. A reasonable estimate is that one-third to one-half of the gap may be attributable to access problems. In 1970 black infants were 85 percent more likely than whites to die during the first year of life; by 1988 black infants were more than twice as likely as whites to die during their first year. A related measure is the slow but steadily growing disparity in low birthweights for blacks and whites during the past 20 years.
DEFINING ACCESS
Access is a shorthand term for a broad set of concerns that center on the degree to which individuals and groups are able to obtain needed services from the medical care system. Often because of difficulties in defining and measuring the concept, people equate access with insurance coverage or with having enough doctors and hospitals in the geographic area in which they live. But having insurance or nearby health care providers is no guarantee that people who need services will get them. Conversely, many who lack coverage or live in areas that appear to have shortages of health care resources do, indeed, receive services.
For the purposes of its work the committee defined access as follows: the timely use of personal health services to achieve the best possible health outcomes. An important characteristic of this definition is that it relies on both the use of health services and health outcomes as yardsticks for judging whether access has been achieved. The test of equity of access involves determining whether there are systematic differences in use and outcomes among groups in U.S. society and whether these differences result from financial or other barriers to care.
In applying its definition of access, the committee sought to occupy a practical middle ground between all care that people might want or need and the belief that medical care can make an important difference in people's lives. The definition forces us to identify those areas of medical care in which services can be shown to influence health status and then to ask whether the relatively poorer outcomes of some population groups can be explained by problems related to access. The definition also emphasizes the need to move beyond standard approaches that rely mainly on enumerating health care providers, the uninsured, or encounters with health care providers to detect access problems.
No matter how generally efficacious a particular health service may be, a good health outcome cannot always be guaranteed. The most important consideration is whether people have the opportunity for a good outcome—especially in those instances in which medical care can make a difference. When those opportunities are systematically denied to groups in society, there is an access problem that needs to be addressed.
The access monitoring indicators recommended by the committee are intended to detect when and where access problems occur in the personal health care system. They do not explain the exact causes of these problems, but they can provide a better basis for generating theories about why differences in access exist among populations. Although they are only proxies for complicated phenomena, over time the indicators give important information about the direction and speed of change. They also provide clues about the relative status of groups of people at the same moment in time. Indicators will not always move in the same direction. Some may increase,
some may decline, and others may show no change. Although this makes overall assessments more complicated, it can be useful to highlight problems and gains in specific areas.
The committee focused on access problems that it believed, if corrected, were most likely to lead to improved health outcomes across the age spectrum. It identified indicators that could be used to measure changes in the degree of access to specific types of personal health care (defined as the one-on-one interaction of provider and patient). The committee's deliberations resulted in a list of 15 indicators that were grouped into several distinct categories. These categories define a set of national objectives (see above) for the personal health care system; each set of indicators provides a means for assessing progress toward a specific objective.
THE COMMITTEE'S INDICATORS AND PROGRESS TOWARD ACCESS OBJECTIVES
Objective 1: Promoting Successful Birth Outcomes
Numerous studies have shown links between the early initiation, amount, and content of prenatal care and birth outcomes. Outcomes that indicate problems in access include infant mortality, low birthweight, and incidence of congenital syphilis.
For all races slightly less than 70 percent of all women received adequate prenatal care in each year from 1986 to 1988. The percentage of women receiving early care increased steadily during the 1970s (from 67.9 percent for all races in 1970 to 75.9 percent in 1979) but remained static between 1980 and 1988. There is a striking difference between whites and blacks in receiving adequate prenatal care (73.5 and 50.7 percent, respectively) (Figure 1).
The U.S. infant mortality rate dropped 7 percentage points between 1989 and 1990, a significantly greater decline than occurred during previous years of the decade when the average annual decline was less than 3 percentage points. The average rate of decline during the 1980s was well below the annual average of 4.7 percentage points. However, the greatest portion of the decrease during the past two decades was in neonatal deaths, which probably reflects improvements in medical technology rather than better prenatal care. With respect to low birthweight, some decline in rates occurred during the 1970s, but no improvement was apparent during the 1980s.
Each case of congenital syphilis indicates either a lack of any prenatal care (even one prenatal care visit should alert a health care provider to the need for treatment) or a lack of adequate care (a prenatal visit at which an infected mother is not diagnosed is inadequate). Treatment of syphilis at least 30 days prior to delivery should prevent infection in the infant.
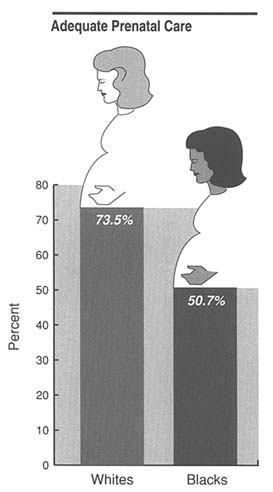
FIGURE 1 Percentage of 1988 births, by race, for which the mother received what is considered adequate prenatal care. The data on which this figure is based come from 49 states and the District of Columbia, as reported by the National Center for Health Statistics.
The recent rise in U.S. congenital syphilis rates—they tripled from 1989 to 1990 (Figure 2)—is thought to be due in part to the increase in cocaine use (particularly ''crack" cocaine), with its attendant transmission of sexually transmitted diseases. Rates of congenital syphilis therefore may also indicate a lack of available, acceptable, and effective drug treatment services for pregnant women.
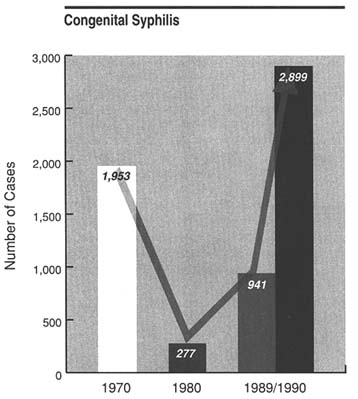
FIGURE 2 Number of cases of congenital syphilis (i.e., among infants up to age 1) for selected years, according to data from the Centers for Diseases Control.
Objective 2: Reducing the Incidence of Vaccine-Preventable Childhood Diseases
There are few instances in which personal health care can virtually prevent a disease from occurring. Access to immunization for childhood diseases provides the best current example of this potential of health care services. Figure 3 shows that less than half of nonwhite preschoolers in 1985 were immunized for measles and less than two-thirds of white preschoolers were so immunized.
Although surveys of immunization have been infrequent and plagued with methodological problems, those that have been conducted indicate declines since 1970 in the vaccination levels for diphtheria-pertussis-tetanus (DPT) and polio for preschool children. There are no clear trends in the
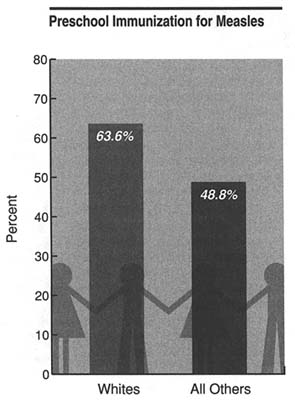
FIGURE 3 Percentage of preschool (children ages 1–4) immunizations for measles in 1985 for whites and all other ethnic groups. This figure is based on data from the U.S. Immunization Survey, conducted by the Centers for Disease Control.
vaccination rates for other diseases, particularly during 1983–1985. Because disease occurrence is cyclical in nature, caution must be exercised in interpreting trends from year to year. Nonetheless, in theory no child should contract these diseases if most are immunized. Recent outbreaks of measles and DPT are particularly disturbing sentinel events in this regard.
Objective 3: Early Detection and Diagnosis of Treatable Diseases
There are a number of diseases for which early detection is important enough to justify screening large segments of the population. For screening to be worthwhile, an effective medical intervention must be available for treating the disease of interest at an early stage. The committee focused on screening for breast and cervical cancer. Although public health education efforts are critical for creating awareness of screening tests, the personal
health care system must ensure that providers follow through with periodic testing and provide appropriate treatment when disease is identified.
As of 1987 only about two-thirds of U.S. women over the age of 18 had had a Pap smear in the previous three years to detect cervical cancer. Hispanic women are less likely to have had the procedure than black or white women. In addition to problems of access to these services for minority women in general, the elderly are of special concern. Elderly white women were more than twice as likely as younger white women never to have had the procedure (22.6 percent of elderly white women had not had the test). About twice this proportion (43 percent) of older minority women reported never having had a Pap smear. Figure 4 shows the percentages of women who have never had a Pap smear.
Recent studies seem to indicate a dramatic increase in mammography
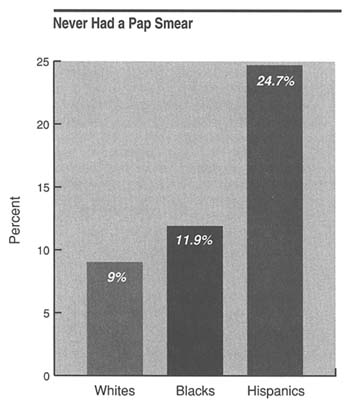
FIGURE 4 Percentage of white, black, and Hispanic women in 1987 who were 18 years of age and older and had never had a Pap smear. The percentages were derived from National Health Interview Survey data for 1987.
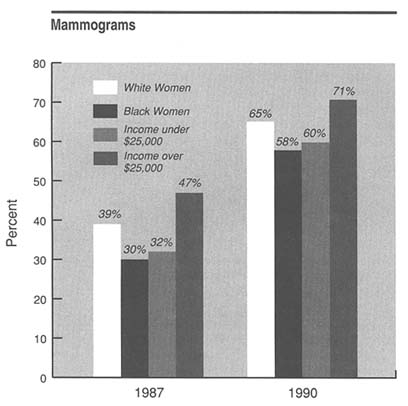
FIGURE 5 This figure shows changes between 1987 and 1990 in (1) the percentages of black and white women age 40 and older who reported ever having had a mammogram and (2) the percentages of women of that age reporting mammography who had incomes over $25,000 and under $25,000. The 1987 percentages are based on data from the National Health Interview Survey of that year; the 1990 percentages were calculated from data collected by the Mammography Attitudes and Usage Study conducted by the Jacobs Institute of Women's Health with technical assistance from the National Cancer Institute.
screening, although differences persist by age, race, and income (Figure 5). Mammogram screening increased between 1987 and 1990 probably as a result of media coverage and enhanced public health promotion efforts. By 1990, among women over age 40, 64 percent reported having ever had a mammogram, nearly twice the proportion reporting mammography three years earlier.
The progression of cancer can occur despite appropriate therapy, but discovery of late-stage cancers may also indicate underuse of an effective
screening test. Alternatively, or in addition, late-stage cancer may also reflect inappropriate medical follow-up of a diagnosed disease. Either or both of these explanations may apply to findings showing that individuals living in high-income areas had about 10 percent fewer cases of late-stage breast cancers in the mid-1980s compared with an earlier time period in the mid-1970s. Low-income areas improved only about half as much over the same time period.
Among whites the proportion of cases of late-stage cervical cancer remained approximately the same in the 1970s and 1980s. In contrast, the proportion of late-stage diagnoses for blacks, which had been approximately the same as for whites in the mid-1970s, nearly doubled by the mid-1980s. With respect to income levels, only a small difference persists over time, and that gap appears to be narrowing.
Objective 4: Reducing the Effects of Chronic Disease and Prolonging Life
Many of the reasons people use medical care are related to the treatment of chronic conditions. These diseases usually are not self-limiting but are ongoing over an extended period of time. Adverse consequences of chronic conditions can occur with or without regular medical care, but negative consequences are more common when regular care is absent. Even when life cannot be extended, health care can contribute to improved functioning for individuals with chronic disease and can minimize discomfort. The committee chose to track chronic disease follow-up care by examining patterns of physician use and use of high-cost discretionary procedures. The two outcome indicators focus on states of illness that require hospital admission and an experimental measure of access-related excess mortality to detect racial differences (described above in the general conclusions).
Having health care coverage makes a major difference in whether people who believe themselves to be in poor health have at least one physician contact within a year. In 1989 the uninsured were more than twice as likely to go without physician contact as those with private health insurance, Medicaid, or Medicare. Figure 6 shows the proportion of persons with no physician visits in the past year, among those who rated themselves as being in poor or fair health in 1989 (the committee's indirect indicator of an underlying chronic disease).
As an indicator, referral-sensitive surgeries reach beyond entry into the personal health care system to assess a second level of access—expensive discretionary procedures. That this is a problem worth monitoring emerges from the medical literature, which contains examples of medical and surgical procedures for which there are differences in utilization according to patient health insurance status, race, and other sociodemographic factors. If
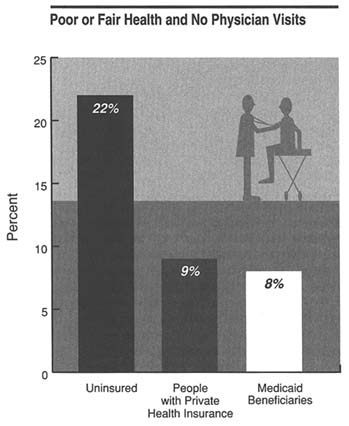
FIGURE 6 Percentage of people in 1989 who were in poor or fair health (by their own report) and who did not contact a physician. The figure, which is based on data from the 1989 National Health Interview Survey, shows the percentages by health insurance status.
one considers ratios of low-income to high-income area admission rates for all referral-sensitive procedures combined, people from poor areas appear to be about two-thirds as likely to obtain the services. The most marked differences in rates of use of procedures were for breast reconstruction, coronary artery bypass grafts, and coronary angiography.
Ongoing medical management can effectively control the severity and progression of a number of chronic diseases, even if the diseases themselves cannot be prevented. An advanced stage of a chronic disease requiring hospitalization may indicate the existence of one or more access barriers to personal health care services. Thus, hospital admissions for certain
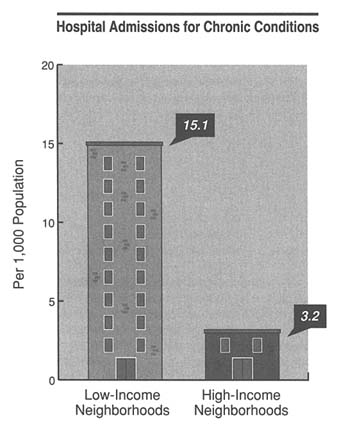
FIGURE 7 Number of hospital admissions for relatively controllable chronic conditions per 1,000 people from low- and high-income neighborhoods. (The low-and high-income designations were developed by using zip codes and Census Bureau information). The figures are a joint product of the Codman Research Group, the Ambulatory Care Access Project (United Hospital Fund of New York), and the IOM Access Monitoring Committee.
conditions are a potentially useful indicator of the performance of the ambulatory health care system. High rates of admissions for conditions related to treatable chronic diseases, in particular, may provide indirect evidence of serious patient access problems or deficiencies in outpatient management (see Figure 7).
In comparisons of hospital admission rates for people from low-and high-income zip codes, all of the ambulatory-care-sensitive admission rates were substantially higher for low-income areas. The overall average ratio was 4.65. The greatest differences—ranging from six-to sevenfold—were
related to admissions for congestive heart failure, hypertension, and asthma. Yet even the lowest ratio, for the diagnosis of angina, showed income differences almost threefold in magnitude.
Objective 5: Reducing Morbidity and Pain through Timely and Appropriate Treatment
The primary medical concern of the 90 percent of people who see themselves as being in good health is, Will I be able to see a doctor if I become sick? One utilization indicator for this objective attempts to measure this concern by singling out healthy people who suddenly become so sick that they must reduce their normal activities. The question is whether such characteristics as insurance status, income, and race have an effect on whether medical attention is obtained. A related outcome indicator looks at the effects of delayed or inappropriate outpatient treatment for acute disease by relying on analysis of admission rates by zip code for a select group of diagnoses.
A second utilization indicator moves from medical care to dental care, a set of services that have limited insurance coverage and thus the potential for being highly income sensitive. Dental services also represent an area of personal health care in which treatment, although usually not life saving, contributes to general well-being and social functioning.
People without insurance and Medicare recipients without supplementary policies were more likely than those with private insurance to refrain from seeking medical care or advice when sick. The differences for both groups compared with those with private insurance are about 10 percentage points. The likelihood of contacting a physician decreases by about 5 percentage points at the lowest income levels for the uninsured and the privately insured. Presumably, anticipated out-of-pocket costs are deterring some of the insured from obtaining services.
People who see themselves as being in good to excellent health—the population of interest in this objective—may seek medical attention for any number of reasons. The personal health care system in some cases provides only symptomatic relief to patients for conditions that would resolve independent of any medical intervention. In other situations, however, symptoms that are not addressed in a timely fashion can evolve into acute medical problems requiring hospitalization. Mild cases of such infections as bacterial pneumonia, cellulitis, kidney diseases, and precursor conditions leading to pelvic inflammatory disease can often be managed with antibiotics in outpatient settings, preventing the disease from becoming more severe. For most of the diagnoses used in this indicator, admissions from low-income zip codes were two to five times higher than admissions from high-income zip codes.
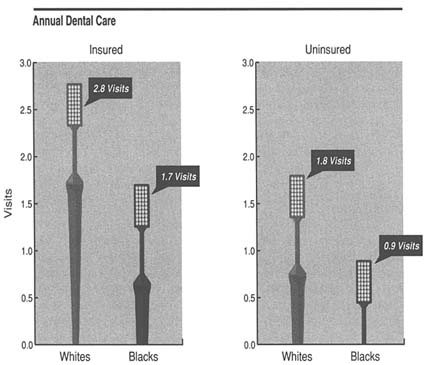
FIGURE 8 Number of annual dental visits by whites and blacks (according to data from the 1989 National Health Interview Survey) for those with and without private insurance.
In general, the use of dental care has been increasing, but there are serious inequities in use based on insurance, race, and income differences. Between 1983 and 1989 the number of dental visits per person in the United States increased 17 percent, from 1.8 to 2.1. During the same period the proportion of those who had never visited a dentist fell from 7.7 percent to 6.4 percent.
In 1989 those with dental insurance made an average of about one more visit to the dentist than those without insurance (2.7 in comparison to 1.7). Consistent differences between whites and blacks persisted despite insurance coverage (Figure 8). As income increases, the difference between the number of visits by those with insurance and those without decreases.
RECOMMENDATIONS
A major aim of the IOM Access Monitoring Project was to improve the state of the art in measuring access problems by determining what indicators can be identified now, what important access problems do not have indicators, and what steps need to be taken over the long term to institutionalize a monitoring system based on valid, reliable data. The purpose of these activities was to create a basis by which decisionmakers could determine how the nation is faring with respect to access over time. Toward this end, the committee has formulated a set of recommendations arising out of its general review of the indicators, trends in the data, and problems in measurement and methodology encountered in the course of its analyses. By way of summary, some overarching themes from the recommendations are worth highlighting.
• Federal Role The committee recommends that there be a federal organization responsible for monitoring access to personal health services. This ongoing function should include the central collection, analysis, improvement, and dissemination of information on changes in access. The same organization should have the responsibility to provide technical assistance and consultation to local organizations that conduct their own analyses of access indicators. These efforts should include activities to encourage improved technical capacity and to promote, where appropriate, consistent definitions and analytic approaches.
• State and Local Monitoring States and local communities would benefit from a national access monitoring process. At the national level, the utilization and outcome indicators selected for this report are intended to be sensitive to the direction and extent of change in structural, financial, and personal barriers. At the state and local levels, these barriers are increasingly definable in terms of a specific set of Medicaid benefits, institutional providers, population demographics, and physical features of the environment. Thus, the advantage of proximity is being able to relate changes to more concrete circumstances. The problem is that either local data are incomplete or there are insufficient resources to analyze the local data that do exist. To address this problem, it is necessary first to identify clearly what data are needed (i.e., develop a monitoring framework) and how the data might be interpreted; a cost-effective strategy for obtaining missing data should then be devised and implemented.
The committee has proposed a framework for monitoring access and has analyzed specific indicators, demonstrating how they might be related to barriers. As a first step, in areas for which local data are available, states and localities can compare themselves with the national averages. They can also use additional data (e.g., from surveys intended to determine which physicians accept Medicaid) and their general familiarity with the contours
of the local health care system—knowledge that is not available at the national level—to draw conclusions about access problems faced by their vulnerable populations. In addition, decisions about whether to invest in new data collection can be helped by the knowledge of what can be done with the data. Understanding the potential payoffs, and the extent to which emerging national trends apply to local circumstances, will allow communities to determine their data collection needs.
The committee recognizes that constrained state and local public health budgets are likely to limit investments in major new surveys, hospital discharge data collection systems, and cancer registries. To the extent that upfront research and development costs can be borne by the federal government or foundations, the cost of implementing enhanced data systems could be reduced for local jurisdictions.
• Racial and Ethnic Differences Anyone who reads this report will be struck by the persistent and in some cases widening disparities in access between blacks and whites. Studies of health care access that compare the experience of whites with that of racial and ethnic minorities other than blacks frequently reveal similar disparities. When certain factors, such as insurance status and income, are taken into account, some of these disparities diminish. There continues to be a need to oversample minorities in national surveys as well as to conduct specialized surveys focused on minorities. To understand the roles that income and insurance play, all surveys should include questions that elicit such information.
Because it is not always feasible to improve the utility of national data bases—that is, by recording the race or ethnicity of patients—it will be necessary to mount studies that more fully characterize unexplained problems of access.
• Directions for Health Services Research In its analysis the committee has reaffirmed that lack of health care coverage is, to a great extent, a good proxy for access. Evidence is mounting about the role insurance plays in influencing not only health care use but outcomes as well. Much work remains to be done in fleshing out these relationships.
Nonetheless, the committee is convinced that other factors play an important role in explaining differences in access to care. This sense is illustrated by the experience of other industrialized nations in which financial barriers to services have been removed but serious inequities among various population groups still occur. Many believe that these inequities would be diminished by changes in the way the delivery of care is organized and by greater responsiveness of providers to the personal and cultural characteristics of their clients. Thus, the committee has concluded that, even if the United States were to adopt universal entitlement, achieving the objectives around which its indicators are organized is likely to remain a great challenge. Further research into these aspects of access is clearly needed.
The limitations of confining measures of equity of access to financial variables are nowhere better illustrated than by those health services that must be combined with effective social services and public health planning for good results. Good prenatal care, for example, must be concerned with how the nutritional needs of the pregnant woman will be met. This service-integration feature, generally acknowledged for prenatal care, is also present in a set of topics that the committee identified for further development as access indicators. These topics represent access problems that may be amenable to solutions requiring close linkages among personal health care services, public health, and social services. In other words, the access problems of homeless people, migrants, people with disabilities, patients with the acquired immune deficiency syndrome (AIDS), and victims of domestic violence will not be solved with an insurance card alone. The complexity of the problems these people face taxes our current understanding of how to measure access barriers. Their problems require organizational solutions that include continuity of care, integration of services, and other subtle characteristics. Tracking these access problems will require measurement skills and methodologies that lie beyond our current capabilities.


















