4
Mechanisms of Immune Function
For some years after the discovery of antibodies, the immune response was thought to be purely protective. It was soon discovered, however, that the same mechanism that protected against infectious microbes also could be activated by innocuous substances, such as milk proteins, to cause immune responses that were potentially dangerous.
When studying the toxicity of extracts of sea anemones, early twentieth-century investigators observed that dogs given a second injection, several weeks after the first, often became acutely ill and died within a few minutes. This response was called anaphylaxis (Gr., ana = against; phylaxis = protection), implying incorrectly that it represented an increase in susceptibility to a toxic substance rather than the expected increase in resistance. (Earlier discoveries of anaphylaxis were overlooked, unfortunately, as sometimes happens when valid observations are ignored until they can be accommodated within a conceptual framework.) Almost simultaneously, other observers noted similar responses in guinea pigs to widely spaced injections of nontoxic protein antigens. With the increasing use of horse and rabbit antisera to treat various infectious diseases in man, various adverse reactions due to the immune response soon became commonplace.
In an attempt to organize a chaotic set of observations, the term allergy (Gr., "altered action") was introduced to cover any altered response to a substance induced by a previous exposure to it. Increased resistance, called immunity, and increased susceptibility to reactions were called hypersensitivity or allergy and were then regarded as opposite forms of immunizations. Through usage, however, "allergy" and "hypersensitivity" have become
synonymous; both terms refer to the altered state induced by an antigen, in which pathological reactions can be subsequently elicited by that antigen or by a structurally similar substance. Within the context of the allergic response the antigen is usually referred to as the "allergen," and the immunized individual, previously called immune, is called sensitive, hypersensitive, or allergic.
Allergic responses were originally divided into two classes, immediate and delayed, on the basis of the lag in their appearance—several minutes after the administration of antigen in the former, and several hours or even a few days in the latter. These terms are still used, but they are now endowed with a different meaning. Not only the reactions that appear within minutes, but also some of the more slowly evolving ones, are mediated by freely diffusible antibody molecules. To emphasize this common feature, both are now called immediate type responses (although "immediate" is not to be taken literally). In contrast, the delayed type are those slowly evolving responses that are mediated by specifically reactive ("sensitized") T lymphocytes rather than by freely diffusible antibody molecules; hence they are also called cell-mediated hypersensitivity. They constitute part of a larger group of reactions, called cell-mediated immunity, in which similar mechanisms are also involved in resistance to many infectious agents and to neoplastic cells.
Chapters 1 and 2 of this report provide general descriptions of concepts and definitions related to sensitization, hypersensitivity, and IgE-mediated allergy. To recapitulate in summary, allergic disease occurs when a susceptible individual is exposed to an allergen and becomes sensitized. Additional exposure to the sensitizing allergen leads to the development of an allergic reaction through the release of histamine and other chemicals from mast cells. Exposure to other substances (e.g., environmental tobacco smoke) may serve to promote the development of allergic reactions and disease.
The typical allergic reaction such as hay fever begins when allergenic proteins from substances such as grass pollen, are inhaled by a sensitive individual and pass through the nasal mucosa. The inhaled allergens then interact with IgE antibodies on the surface of mast cells in the mucosa to cause the release of histamine and other bioactive mediators. These mediators, in turn, cause vasodilation of blood vessels and stimulate secretory cells. The result is the clinical symptomatology and manifestations of nasal congestion, rhinorrhea, and conjunctivitis commonly associated with allergies.
As discussed previously in this report, nearly 20 percent of the population suffer to a greater or lesser degree with allergies involving localized anaphylactic reactions to extrinsic allergens such as grass pollen, animal dander, mites in house dust, and so on. Contact of the allergen with cell-bound IgE in the bronchial tree results in asthma, in the nasal mucosa results in hay fever, and in the conjunctival tissues results in allergic conjunctivitis.
The past 10 to 15 years have brought increased recognition of the importance of indoor allergens—in particular, of protein allergens—in generating allergic responses and asthma (Burge and Platts-Mills, 1991a; Burrows et al., 1989; Platts-Mills et al., 1991a). In part, this recognition is based on an awareness of the clinical significance of the increased time spent by modern humans indoors (Spengler and Sexton, 1983). This increased exposure has led to assessments of the potential contribution of proteins inhaled in the indoor environment to the pathogenesis of several allergic conditions, including allergic rhinitis, sinusitis, allergic conjunctivitis, asthma, and hypersensitivity pneumonitis. This chapter addresses the basic mechanisms of cellular, tissue, and airway responses to inhaled proteins. It seeks to use these responses as a framework to plan control strategies based on patterns of exposure and epidemiology.
RESPONSE OF AIRWAY CELLS AND TISSUES TO INDOOR ALLERGENS
This section discusses the resident cells and tissues that are involved in airway host responses; the discussion is organized on the basis of the structure of the upper and lower airways. A second topic is the function of immune and inflammatory cells that may infiltrate resident cells and tissues of these airways in response to an immune reaction directed against inhaled protein allergens. Table 4-1 identifies the cells of the airway and highlights their effector function (i.e., the action they take against a target cell). The
TABLE 4-1 Structural and Inflammatory Characteristics of Cells of the Airway
final portion of this section discusses the various mediators of inflammation and hyperreactivity in airways and the ways in which these mediators may influence the airway response to inhaled allergens.
Epithelium and Other Airway Structural Tissues and Cells
EPITHELIAL CELLS
The resident cells and tissues of the upper and lower airways include the epithelial covering of the upper airways as well as the lining of the bifurcations of the bronchi and extending to the respiratory bronchioles. The epithelial cells that cover these structures are ciliated and known as epithelial brush-like cells (or type III epithelial cells). These bronchial brush cells have surface cilia that beat material and proteins caught in mucus toward the upper airway and out of the lower and upper airway system. A similar cell is the alveolar brush cell, which is found in the alveolar space (Hunninghake et al., 1979).
In addition to the type III alveolar epithelial or brush cells, two other types of epithelial cells line the bronchial mucosa or overlay the alveolar structure. Known as type I and type II alveolar epithelial cells, these have various and diverse functions. Both the bronchial brush cell with columnar epithelium (the type III epithelial cell noted above) and type I epithelial cells are end-stage differentiated cells that cover the vast majority of the respiratory epithelium. Type II alveolar epithelial cells are capable of dividing and may give rise to both type I and type III cells through their proliferative activity (Hunninghake et al., 1979). They are the source of phospholipid-rich surfactant, which maintains the integrity of the alveolar spaces; in addition, they may produce factors that are involved in nonspecific host defense (Hunninghake et al., 1979). Goblet cells or mucus-producing cells found in the bronchi are also prominent; such cells can produce materials, in particular, mucus, that blanket the bronchial brush cells and enhance their functioning.
SUBEPITHELIAL STRUCTURES
Below the overlay of epithelial cells in the respiratory mucosa is a rich network of subepithelial structures. Obviously, blood vessels are present, which contain both endothelium and smooth muscle; also to be found are other resident cells that are involved in maintaining ground structure. These include fibroblasts; mast cells in a resting or basal, nonactivated state; nerve cells; and a rich biochemical network of ground substances including collagen, fibronectin, and other structural proteins and proteoglycans that contribute to the integrity of the airways. Within the bronchi, structural integrity
is further maintained by bronchial smooth muscle; the larger bronchi and the trachea are supported as well by cartilaginous rings. All of the cells that make up the tissues of the upper and lower airway—epithelial cells, fibroblasts, cartilage cells, smooth muscle cells, blood vessels comprising endothelial and vascular smooth muscle cells, nervous tissue, and resident nonactivated inflammatory cells, such as mast cells—can and do respond to inhaled materials with nonspecific host defense (Hunninghake et al., 1979). Moreover, once such a response has been evoked, there may be a further influx of immune and inflammatory cells to the airway.
Immune and Inflammatory Cells in the Airway
A wide variety of immune and inflammatory cells are involved in airway responses to inhaled proteins in the bronchi as well as in the upper and lower airways. Specific responses are initiated by interacting sets of cells composed of macrophages and other significant antigen-presenting cells, as well as lymphocytes—in particular, T helper lymphocytes (although other forms of T lymphocytes and B cells are also involved in this response). Figure 4-1 shows the interaction of allergen with relevant immune and inflammatory
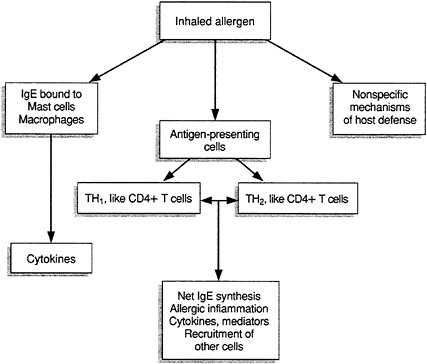
FIGURE 4-1 Immune cells and their interactions with allergens.
cells in the airway. The discussion below of the response to inhaled protein first deals with the role of macrophages and T and B cells and then describes mast cells, eosinophils, and neutrophils, other cells that are significant in airway host defense.
MACROPHAGES
In terms of number and presumably function, the alveolar and airway macrophages are the predominant airway inflammatory and immune effector cells. Airway macrophages are derived from precursor blood monocytes that migrate to the airways and differentiate there (Unanue and Cerottini, 1989). (The precursors of blood monocytes are monoblasts and promonocytes, which are found in bone marrow.) There are other cells in body tissue that are similar to airway and/or alveolar macrophages in distribution and differentiation—for example, Kupffer cells in the liver and osteoclasts of bone.
FUNCTION
The function of macrophages is to provide nonspecific as well as specific host defense in various tissues; these tissue macrophages can be resting or activated, depending on local conditions. The ability of macrophages to "process" extracellular proteins, including inhaled proteins taken from ambient inspired air and leached from particles, makes them primary airway defenders; they not only eliminate inhaled proteins but also act as allergen-presenting and allergen-processing cells (Unanue and Cerottini, 1989). In addition, macrophages secrete diverse bioactive molecules that influence the physiology of many tissues; in the upper and lower airways they are critical to physiologic function. The nature of these proteins and of other host defense factors involved in the generation of responses by macrophages will be covered in more detail elsewhere in this chapter; macrophages are important in the maintenance of airway tissue.
ANTIGEN-PRESENTING CELL FUNCTIONS
The antigen-presenting cell (APC) is involved in immune and inflammatory reactions in the airway. Antigen presentation is mediated by the expression of specific proteins on the surface of the airway macrophage, which functions in the actual presentation and recognition of protein allergens and other APC antigens—by helper T cells in particular. The response to both inhaled and soluble proteins clearly depends on the CD4+ subtype of helper T cells (see the discussion below); thus, the role of the class II major histocompatibility complex (MHC) macrophages in presenting protein fragments to these T cells is critical (Unanue and Cerottini, 1989).
ANTIGEN PROCESSING
Over the past few years a great deal has been learned about the actual molecular configuration and mechanism of protein processing, which occurs through the subcellular organelles of antigen-presenting macrophages, and its role in generating immunogenic complexes composed of fragments of protein allergens and class II MHC molecules. The identification in 1987 of a crystalline structure for MHC molecules included an antigen fragment-binding pocket within the three-dimensional structure of the molecules (Brown et al., 1988). This discovery led to the postulation of a new model for the recognition by T cells of protein fragments derived from whole allergens or proteins (Brown et al., 1988).
In this process, protein allergens are taken up by the plasma membranes of antigen-presenting macrophages into a phagocytic vacuole that eventually fuses with endosomes. Next, enzymes associated with a nine-subunit subcellular organelle called a proteosome degrade these foreign proteins to peptides. These peptides can then associate with the binding groove of class II MHC that are molecules expressed on the inner membrane of the endocytic vacuole (Martin and Goodman, 1990). The process thus generates a complex composed of a fragment of protein anywhere between 9 and 20 amino acids in length; the complex is bound to the binding groove of a class II MHC molecule. This complex, when redisplayed on the surface plasma membrane of the antigen-presenting macrophage, allows a specific T cell receptor with binding specificity for this particular antigenic fragment (or T cell epitope) to bind to the APC and initiate an immune response.
In addition to this critical protein-processing/antigen-presenting function of macrophages and other APCs, these cells also generate a number of important substances critical to host defense in a nonspecific manner. These substances include cytokines such as interleukin-1 (IL-1), tumor necrosis factor, interferons of the alpha and gamma categories, protein-derived regulatory mediators such as fibronectin, transforming growth factor β, and platelet-derived growth factor (Martin and Goodman, 1990). A number of bioactive lipids are also synthesized by macrophages and APCs, including leukotrienes (LTB4 and LTC4), prostaglandin (PG) E2, and other arachidonic acid metabolites including PGI2, and hydroxyeicosatetraenoic acids (HETES) and other products of cellular arachidonate (Rosenwasser, 1986). Another bioactive lipid produced by macrophages is platelet-activating factor (PAF). Complement proteins and enzymes including collagenase, elastase, and cathepsins are also major secretory products of airway macrophages and play a significant role in host airway defense (Borish et al., 1991).
OTHER APCS IN THE AIRWAY
In addition to alveolar macrophages, other subsets of cells within the airway can perform some of the major immunological and host defense functions of macrophages. These other classes of antigen-presenting cells include dendritic cells (Borish et al., 1991), which are found in lymphoid tissue and in the subepithelial areas of normal and asthmatic airways; activated B lymphocytes; epithelial cells; fibroblasts; smooth muscle cells; and endothelium. Under the proper conditions, these cells function in vitro as APCs, similar to macrophages. Whether that is their primary role in vivo, however, has not been adequately established.
T LYMPHOCYTES
The major cell type with which antigen-presenting macrophages and other APCs interact in the airway is the CD4+ subset of T cells. Table 4-2 lists the major classes and subpopulations of T cells and notes their major functions and the immune complexes to which they bind (i.e., their specificity). T lymphocytes are prominent among the various populations of airway cells; their importance lies in their major role in the recognition of inhaled proteins (Robinson et al., 1992). T lymphocytes arise from bone marrow-derived precursors selected by thymic maturation through a complicated selection and deletion process that occurs during T cell maturation. The T cells that emerge during this process populate peripheral lymphoid tissues. The majority of such cells display unique combinations of cell surface proteins; it is these proteins that differentiate and function within the mature T cell compartment. Most mature T cells—in fact, the vast majority of T cells that have been selected through the thymus—express on their surface the protein markers CD2 and CD3.
T CELL RECEPTORS
On allergen-specific T cells, the presence of the CD3 marker is associated with coexpression of specific T cell receptors that are developed through molecular recombination events. These events can encompass the association and recombination of various gene segments involved in specific recognition of protein antigens in conjunction with self class II MHC molecules. Hence, the vast majority of CD3+ T cells coexpress an α and a β chain for a T cell receptor. Two or three distinct genetic segments encode these chains, which confer on the cell the specific capability to bind to a protein antigen and class II MHC molecule complex on APCs.
The T cell receptor α chain comprises a variable region, a joining region, and a constant region; the β chain is composed of a variable region, a
TABLE 4-2 Classification of T Lymphocytes
diversity region, a joining region, and a constant region. These seven genetic segments make up the two proteins that are involved directly in recognizing inhaled foreign proteins in the airway. The CD2-CD3+ T cells can be further divided into subcategories on the basis of other cell surface proteins, which indicate the differentiation of these cells according to specific functions. For example, the ability of a particular subset of T cells to help B cells produce antibodies or to help macrophages and other accessory cells express delayed-type hypersensitivity is critically dependent on the coexpression of the CD4 marker on the T cell in conjunction with the CD2 and CD3 markers for T cell delineation.
THE CD4 SUBPOPULATION
The CD4 marker has received a great deal of attention because it is the major receptor for the human immunodeficiency virus (HIV), whose coprotein, gp120, binds to the CD4 protein. The CD4 protein is therefore an important biological marker of T cells, and it makes T cells a target for retroviral infection and eventual destruction in HIV disease. The CD4 marker is important in another regard as well: it acts as a cofactor in recognizing immunogenic complexes of protein antigens in conjunction with class II MHC molecules. Thus, the subset of CD4+ T cells is the helper cells involved in the response to inhaled protein and, in particular, to inhaled allergens, triggering an allergic response (Robinson et al., 1992).
CYTOKINES OF T CELL SUBPOPULATIONS
There has been much research in the past few years to further subdivide the ab T cell receptor-positive CD2/CD3/CD4+ population into two groups. One group, known as the TH1 subpopulation of CD4+ T helper cells, is involved in the mediation of delayed-type hypersensitivity; these cells have a unique protein profile that is secreted at activation. Known as cytokines, these proteins are one of the effector molecules generated by T cells that contribute to host defense. Therefore, for example, infection with an intracellular parasite with a preference for infecting macrophages leads (in both murine and human systems) to generation of a T cell response characterized by the production of gamma interferon and lymphotoxin (Mossmann and Coffman, 1989). IL-4 and IL-5, the T cell cytokines involved in antibody production, and the immunoglobulin E (IgE) and IgA isotype switch are not utilized.
By contrast, the other group of ab T cells, the TH2 subpopulation of CD4+ T helper cells, is quite prominent in responses to allergens in the airway, both in vitro and in vivo (Wierenga et al., 1990). These CD4+ TH2 cells have an enhanced capability for producing IL-4, IL-5, IL-9, and IL-10, cytokines that are involved in the generation of allergic antibody responses and allergic inflammation. The next section discusses the potential role of these TH1 and TH2 CD4+ T cells in greater detail, describing the role of cell-mediated immunity in T cells and macrophages in the regulation of IgE-mediated disease and in hypersensitivity responses to inhaled proteins.
THE CD8 SUBPOPULATION
In addition to CD4+ populations in the airway, researchers have identified CD8+ T cell subsets. Known as cytolytic T lymphocytes (CTLs), these cells perform a cytotoxic function and are restricted to a set of targets different from those of CD4+ T cells. These CTL targets are protein antigens expressed on the surface of antigen-presenting cells in the context of class I MHC molecules. (Class I MHC molecules are ubiquitously expressed and play a prominent role in recognizing viral antigens after viral infection of all sorts of target cells, including B lymphocytes, macrophages, and epithelial cells.) The potential role of CD8+ T cells in regulating the response in the airway to inhaled proteins and allergens is not yet clear, but it is reasonable to assume that it involves limiting viral infection. In particular, it may involve limiting the potential damage that might result from inhaled allergenic proteins mediated by CD4+ TH2-type cells. CD8+ cells may also contribute to other regulatory phenomena, especially given that, early on, these cells were thought to act as suppressor cells in the regulation of antibody synthesis. Although antigen-specific suppressor cells have been
quite difficult to identify in terms of cloning and structure, it is entirely possible that cells with a cytotoxic function bearing the CD8 marker may play some role in the regulating of CD4+ responses to inhaled proteins and allergens.
One potential role function of CD8+ T cells may be in the regulation and mediation of airway responses in patients with hypersensitivity pneumonitis (HP). While precipitating IgG to the offending antigen in HP is often an important diagnostic and possibly pathogenetic marker, recent studies have identified an enhanced utilization of CD8+ T cells in the bronchoalveolar lavage (BAL) of patients with HP. The function of these CD8+ BAL T cells is unknown, but their potential role as regulators or cytotoxic effectors for HP pathogenesis is intriguing.
OTHER T CELL SUBPOPULATIONS
Subpopulations of CD4+ and CD8+ T cells can also be differentiated according to whether they express the CD45 RA or CD45 RO molecule on their surfaces. CD45 RA and CD45 RO are protein molecules that are expressed as the cells undergo differentiation. One gene codes for each of CD45 RA and CD45 RO; and alternative gene splicing of messenger RNA yields either product as the T cells differentiate. For example, CD45 RA is expressed primarily on naive cells that have not yet been selected for their antigen specificity. The expression of CD45 RO on CD4+ or CD8+ cells is associated with a memory phenotype; it indicates that the cell has been stimulated previously through its antigen receptor. CD45 RA and CD45 RO both participate in the activation of T cells through enzymatic activities related to intracellular signaling.
B LYMPHOCYTES
B lymphocytes, the other major population of lymphocytes, are also involved in the immune and inflammatory reaction that occurs in the airways. B lymphocytes are derived from bone marrow precursors that mature through development in the bone marrow and by exposure to microenvironmental milieus that include a number of growth- and development-related cytokines. The process begins with the selection of B cells for their antigen-specific binding capabilities; these are reflected in membrane IgM on antigen-specific but immature cells. Following selection, the sequential effect of various T cell-derived cytokines, including IL-4, IL-5, and IL-6, drives the undifferentiated but antigen-specific B cells to differentiate further into antibody-secreting plasma cells. This process is accompanied by the specific selection of immunoglobulin isotypes different from the original surface IgM.
The products of B cells (i.e., secreted immunoglobulins) can be divided into five major isotypes depending on the heavy-chain structure of the immunoglobulins. These isotypes have different functions; of particular interest for inhaled indoor allergens are the isotypes associated with IgE, the major allergenic (or reaginic or atopic) antibody marker, and IgA, a mucosa-derived isotype involved in host defense. Therefore, in the airway, the generation of both IgE and IgA is extremely important, and the ability of CD4+ TH2 cells to produce the cytokines IL-4 and IL-5, factors involved in the specific selection of these reaginic and respiratory antibody isotypes, is critical (Wierenga et al., 1990).
In addition to their antibody-synthesizing capabilities, B lymphocytes are also of great interest because of several other immunological functions. These include the processing of antigens and proteins and the expression of both MHC class II- and class I-associated protein antigens for recognition by T lymphocytes.
MAST CELLS
Mast cells are important immune effector and inflammatory cells in the airway. Like the T and B lymphocytes and macrophages, mast cells are derived from bone marrow precursors that generate mature airway tissue cells with significant host defense capability. Mast cell development is influenced by various cytokines including granulocyte macrophage colony-stimulating factor (GM CSF), IL-3, IL-4, IL-9, and IL-10; these substances seem to induce and drive the ability of precursors of mast cells to be selected for mature mast cell growth. Mast cells are of major importance in host defense because, other than basophils, these cells are the only cells that bear high-affinity Fc receptors for IgE. Bridging of IgE antibody and IgE Fc receptors by allergen on the surfaces of mast cells activates the cells to release the contents of their granules and other newly synthesized mediators. This cross-linking event and biochemical activation, utilizing subcellular and suborganelle activation molecules within the structure of the mast cell, lead to the release of both preformed mediators from the mast cell and granule-associated materials. These materials include proteoglycans, enzymes such as tryptase and chymase, and other kinds of mediators that can have proinflammatory effects. In addition to these preformed, granule-associated mediators, mast cells can generate newly synthesized mediators, including bioactive lipids such as PAF, prostaglandins (PG), and leukotrienes (LT) of the C, D, and E categories (Rankin et al., 1982). These mediators are also generated by stimulation of the allergen cross-linking of IgE Fc-receptor type I molecules on the surface of the mast cell. Recent studies have proposed an even greater role for the mast cell in allergic inflammation and long-term inflammation in response to allergens (Plaut et al., 1989).
Moreover, findings show that mast cells also have the capacity to synthesize cytokines in a manner akin to that of TH2 type CD4+ T helper cells (Robinson et al., 1992). Thus, the role of mast cells in the response to inhaled protein allergens is not a trivial one.
EOSINOPHILS
The eosinophil is another effector cell in the airway that can play a significant role in reducing the inflammation associated with responses to inhaled protein antigens. Eosinophils are derived from bone marrow precursors; production of mature eosinophils is stimulated by the action of cytokines, such as GM CSF, IL-3, and IL-5. GM CSF and IL-3 are also involved in ensuring eosinophil survival, both in vitro and in vivo; IL-5 is involved in activation, another aspect of eosinophil biology. The eosinophil can express an activated profile, the so-called hypodense profile, which is generally associated with eosinophils that have released their granules (Clutterbuck et al., 1989).
The eosinophils have a number of toxic capabilities—for example, they generate toxic oxygen-derived species and enzymes that can digest ground substances such as proteases and elastases. Another toxic capability is their expression of a family of proteins that are highly toxic to epithelia; these proteins include highly toxic basic proteins, such as major basic protein, the eosinophil-derived cationic protein, and eosinophil-derived neurotoxin (Sher et al., 1990). Through their unique structure and highly basic nature, these proteins are positively charged at a physiologic pH, permitting their generation of several toxic responses, including epithelial damage and antiproliferative effects. The fact that eosinophils are associated with reversible airway disease and airway damage clearly demonstrates their importance in the effector phase of airway responses to inhaled allergen; nevertheless, they depend on specific mechanisms for their recruitment. In particular, the activation by an allergen of T lymphocytes, and possibly mast cells, will generate the cytokines required to evoke a strong eosinophil response in airway inflammation.
NEUTROPHILS
At one time, neutrophils were thought to be extremely important in stimulating the asthmatic, destructive airway response that is found in patients with asthma. Now, however, the role of neutrophils appears to be less essential than was once thought, primarily because research has shown that eosinophils, mast cells, macrophages, and T cells are more central to the type of inflammation seen in this response. A number of factors, including cytokines, leukotrienes, and lipids, act to recruit neutrophils into the airways
in an inflammatory and immune response. Once there and activated, the neutrophils have the same capabilities as eosinophils to generate toxic oxygen-derived species as well as to mediate tissue damage by generating elastases and other enzymes. Therefore, the contribution of neutrophils to airway inflammation and response to inhaled protein allergens should not be discounted (Boey et al., 1989).
MEDIATORS
Various kinds of mediators are derived from the immune and inflammatory cells discussed in the previous section and are important in the inflammatory response in the airways. These mediators include chemicals and autocoids such as histamine, serotonin, and adenosine; proteins such as secreted cytokines including tumor necrosis factor, IL-1, IL-8, and IL-6; enzymes and other toxic proteins such as collagenase, elastase, cathepsins, and the major basic protein; related cationic proteins; and neuropeptides. Table 4-3 shows the cytokine families involved in inflammation, and Table 4-4 lists other nonspecific mediators of host defense.
Under appropriate conditions, all of these mediators can stimulate enhanced mast cell and eosinophil-dependent inflammatory reactions in the airway. For example, substance P, neurotensin, and other factors made by stimulating C-type fibers in the airways can be associated with enhanced airway reactivity and inflammation. The actual interaction between the generation of substance P in the form of noncholinergic neurotransmitters and the hyperresponsiveness to cholinergic and α-adrenergic stimuli observed in patients with asthma appears to be well established.
Lipid mediators and bioactive lipids are also important in the inflammatory
TABLE 4-3 Cytokine Families
|
Family |
Classification |
|
Interferons (IFN) |
IFNα, IFNβ, IFNγ |
|
Interleukins (IL) |
IL-1 through IL-12 |
|
Colony-stimulating factors (CSF) |
Granulocyte CSF, granulocyte macrophage CSF, macrophage CSF, multi-CSF erythropoietin, IL-3, IL-5 |
|
Growth differentiative, reparative, and proliferative factors |
Platelet derived growth factor, fibroblast growth factor, nerve growth factor, epidermal growth factor, insulin-like growth factor |
|
Tumor necrosis factors (TNF) |
TNFα, TNFβ |
|
Histamine-releasing factors |
Connective tissue activating peptide III, macrophage chemotactic activating factor |
TABLE 4-4 Nonspecific Mediators of Inflammation and Host Defense
|
Mediator |
Source |
Function |
|
Complement proteins C5α , C3α , membrane attack complex |
Serum, liver, reticuloendothelial system |
Amplify immunoglobulin-mediated tissue damage |
|
Enzymes Cathepsin, trypsin elastase, chymase neutrol proteases |
Polymorphonuclear leukocytes, macrophages |
Tissue damage |
|
Cationic proteins Major basic protein, eosinophil derived neurotoxin, eosinophil cationic protein |
Eosinophils |
Tissue damage, antiproliferative activity |
|
Leukotrienes Leukotrienes, hydroxyeicosatetraenoic acids, etc. |
Mast cells, neutrophils, eosinophils, macrophages |
Smooth muscle contraction, edema and tissue swelling |
|
Prostaglandins Prostaglandin F, prostaglandin D, prostaglandin E |
Same as for leukotrienes |
Immunosuppression, edema |
|
Platelet-activating factor |
Same as for leukotrienes, endothelium |
Cellular influx and edema |
response. Products of arachidonate metabolism, including both lipoxygenase and cyclooxygenase products, can be proinflammatory; such products may be mediators in activating other inflammatory cells at a site of inhaled protein antigen deposition. Reactive oxygen metabolites, which are products made by activated macrophages, neutrophils, and eosinophils, are another significant type of mediator, as are superoxide, peroxide, and hypochlorous acid—all of these substances may contribute to an inflammatory response to inhaled allergens. There is also evidence indicating that the production of nitrites, nitrates, and nitric acid by the endothelium and macrophages may have a profound effect on both T and B cells as well as on smooth muscle function in blood vessels and in the airway. These nitrogen-based mediators and/or their abrogation may have an effect on muscle tone in the airways during an inflammatory response.
Recent evidence has identified important new mechanisms for the recruitment of inflammatory cells in the airways. An integral aspect of these mechanisms is the ability of inflammatory cells (such as those discussed earlier in this chapter) to express on their surface families of proteins known as adhesion molecules. These molecules and their ligands allow polymorphonuclear leukocytes (PMNs), for example, to bind to endothelial cells and
to initiate migration of these cells into inflamed tissues. The adhesion molecules are upregulated by cytokines and can be inhibited by anti-inflammatory drugs such as steroids. The identification of IL-8 and other cytokines as chemotactic factors combined with our new understanding of cell adhesion and movement provides a useful framework for potential models of airway inflammatory cell recruitment in response to inhaled allergens.
GENERATION OF IMMUNE RESPONSE AND HOST DEFENSE TO INDOOR ALLERGENS
Nonspecific Mechanisms of Airway Host Defense
Several significant nonspecific mechanisms of airway host defense may play a role in the response of the upper and lower airways to inhaled protein antigens, allergens, and/or particles (see Tables 4-3 and 4-4). These mechanisms include cough and glottic functions in the upper airway and mucociliary clearance (i.e., through the production of mucus and the function of cilia); this second mechanism works to clear larger particles in the upper airway and in the upper respiratory tree of the lower respiratory tract. As mentioned earlier, the effectiveness of epithelial clearing mechanisms is tied to the ability of type III epithelial cells to generate proper ciliary motion; this serves to eliminate inhaled particles by beating particulate matter, caught in the bed of mucus, out of the airway.
In addition to this mechanism, goblet cells and submucosal cells contribute to airway host defense. These cells include many of the immune, inflammatory, and respiratory structure cells highlighted previously; they produce multiple soluble proteins in addition to mucus. A number of these proteins include enzymes such as collagenase and elastase, complement fragments, cytokines, fibroblasts, and other ground substance regulatory mediators such as platelet-derived growth factors. Antiproteases are also present in both the upper and lower respiratory tract and are derived either from serum or from respiratory cells themselves. These antiproteases include alpha-1-antitrypsin, alpha-2-macroglobulin, alpha-1-antichymotrypsin, and bronchial mucus inhibitors derived from airway cells. Liver cells are also involved in limiting the damage mediated by proteases such as elastase, collagenase, and cathepsins.
A number of cells whose functions were outlined earlier are involved in clearance in a nonspecific way; these cells act on particles and proteins that reach the upper and lower airways. Cells in this category include alveolar macrophages, bronchial macrophages, neutrophils, dendritic cells, and natural killer cells, a form of lymphocyte involved in nonspecific host defense against defined targets.
Allergen-Specific Mechanisms of Airway Responses
The generation of specific IgE and IgG against inhaled indoor allergens has been well established in both experimental animals and humans with allergic disease. Obviously, biological inhalant proteins carried into the airways on particles that range in size from 0.1 to 50 μm in diameter are most likely to generate an immune and allergic response in both the upper and lower airways. Little is known about the exact kinetics and concentration of inhaled allergen necessary to generate a response of this sort either in animals or in human subjects. It is enough to say that the airways and lungs can be an important portal of sensitization to foreign proteins and in particular to certain allergens found indoors. The kinetics of antibody formation and recognition are not well established because standardized methods of identifying allergen exposure on inhalation in the natural environment or under experimental conditions have not been developed. Nonetheless, one may be sure that the cells of the airways are interacting in such a way as to generate the appropriate phenotype of an allergic response in subjects who inhale protein allergens. Table 4-5 lists potential immunologic hypersensitivity reaction mechanisms in the allergic diseases associated with inhaled allergen exposure.
The potential role of T cells and cytokines in the regulation of IgE-mediated and hypersensitivity pneumonitis responses to inhaled proteins is of great interest. Ongoing research has found that inhaled protein allergens are processed by bronchial macrophages and other antigen-presenting cells in such a manner that allergenic peptides are then recognized by CD4+ T helper cells in the airway. These allergen epitope-specific T cells in the airways of atopic asthmatic individuals are critically involved in the generation of proinflammatory mediators; these mediators, which include the whole panoply of cells outlined in the previous section, subsequently recruit the various kinds of factors and cells related to and associated with airway inflammation and hyperreactivity. In particular, the CD4+ TH2 subset of T lymphocytes, when activated by allergen presented in the context of class II MHC molecules on an antigen-presenting cell, stimulates the generation of cytokines such as IL-3, IL-4, IL-5, and GM CSF. Cytokine production leads to the activation and recruitment of other allergy accessory cells in the airway (e.g., mast cells, eosinophils, basophils, and neutrophils). In fact, recent data suggest that the TH2 population of cells in humans is preferentially activated in response to the unique structures associated with allergens, and it has been shown that these kinds of cells produce these cytokines in response to allergen in the airways. An allergic proinflammatory process thus can be set up on the basis of recognition of an inhaled protein allergen. Other trigger factors may also play a role in this inflammatory milieu. An example is the potential action of a viral infection. When activated in a
TABLE 4-5 Immunologic Hypersensitivity Reaction, Types I to IV
|
Type of Reaction* |
Onset |
Antibody |
Principal Cell/Effector |
Airway Syndrome |
Effector Molecule |
|
Antibody dependent: anaphylactic (atopic reaginic)—type 1 |
Rapid (seconds to minutes) |
IgE |
Mast cells/basophils |
Allergic rhinitis, asthma |
Histamine, leukotrienes, platelet activating factor, prostaglandins, cytokines |
|
Complement-mediated immune adherence (phagocytic reaction)—type II |
Intermediate (minutes to hours) |
IgM/IgG |
Neutrophils, reticuloendothelial cells |
Immunologic pulmonary hemorrhagic syndrome |
Imunoglobulins, complement fragments, enzymes |
|
Immunocomplex (or tissue reactive antibody)—type III |
Intermediate (30 minutes to 2 hours) |
IgM/IgG |
Neutrophils, reticuloendothelial cells |
Hypersensitivity pneumonitis |
Complement fragments, enzymes |
|
T-cell reactions: cell-mediated immune response—type IV |
Prolonged (delayed 18–24 hours) |
None |
Responder T cell and monocyte/macrophage/antigen-presenting cells |
Asthma, hypersensitivity pneumonitis |
Cytokines, mediators |
|
* Gell and Coombs (Gell et al., 1975) classification of Types I to IV. SOURCE: Adapted from NRC, 1992a. |
|||||
virus-specific manner, other populations of T cells, such as the CD8+ T cell, may spur the generation of GM CSF, IL-3, and gamma interferon (IFNα, all of which can lead to a proinflammatory milieu and the generation of factors related to allergic inflammation. Tables 4-6 and 4-7 summarize the mechanisms by which immune cells and cytokines induce airway reactions.
In addition to these mechanisms for pulmonary reactions to inhaled allergens, there are similar mechanisms for reactions at other tissue sites including the nose, the conjunctivae, and the skin. There are even data to suggest that indoor allergens may play some role in generating allergic inflammation of the skin resembling atopic dermatitis. Presumably, the skin has the same immunological mechanisms for allergy reactivity, except that there is also the possibility that epidermal and dermal cells, including Langerhans, cells, keratinocytes, and fibroblasts, will be involved in allergen-induced reactivity.
It is worth noting that the allergen response at all of these tissue sites adheres to a specialized pattern of kinetics after challenge. In the airways and nose, an initial immediate response is seen within the first 20 minutes to 1 hour after challenge. Beginning at 6-8 hours after challenge and continuing for 24-28 hours, a delayed response is seen; this response has been attributed to recruitment of inflammatory cells to the site of allergic reaction. This so-called late-phase response has become an important model for, or window into, the potential mechanisms of allergic inflammation.
TABLE 4-6 Sources of Cytokines in Allergen Induced-Airway Inflammation
TABLE 4-7 Cytokine-Induced Airways and Allergic Inflammation
Adjuvant Effects
Inhaled contaminants within the airways can serve as adjuvants and may have a costimulatory effect on airway function. This includes the ability of endotoxin and endotoxin-related proteins derived from bacteria to act as macrophage-activating factors in association with inhaled protein antigens. Considerable evidence has accrued, both from animal models and human subjects, to suggest that the adjuvant effects associated with macrophage
activation are related to lipid A of endotoxin. Other relevant substances such as synthetic and water-soluble adjuvants are primarily macrophage activators involved in generating, from macrophages, proinflammatory cytokines such as IL-1, IL-6, and tumor necrosis factor. When administered with protein antigens, these proinflammatory cytokines can have an effect similar to that of standard endotoxin—or of any of the other water-soluble adjuvants and other materials that have adjuvant effects. It is entirely possible that inhaled contaminants, endotoxins, and endotoxin-like proteins, as well as fungal proteins and other irritants such as tobacco smoke, may activate macrophages and generate a proinflammatory milieu. Such a milieu will enhance the basic immunogenicity and allergenicity of inhaled proteins, which act as stimulants of the CD4+ T cell populations in a more standard immunological model.
CONCLUSIONS AND RECOMMENDATIONS
A great deal of knowledge has accumulated in the past 15 years concerning the role of inhaled proteins (including allergens) in airway inflammation. The prospects for the future are bright. Newer techniques of immunological science include the use of sophisticated methods for the detection of proteins. Indeed, such methods as monoclonal antibody-based radioimmunoassays and enzyme-linked immunosorbent assays as well as the potential use and recognition of the actual protein sequences of the allergens involved in inducing allergic responses have led us to consider a whole new approach to detection. Use of these reagents to enhance and better control environmental stimuli is a logical goal, as is the potential use of molecule-based products, including allergen fragments, cytokines, and cytokine inhibitors, to produce immune modulation in the host. Such promising approaches permit considerable optimism regarding the potential interruption of the immune system- and inflammatory-based circuits triggered by inhalation of proteins and allergens and long-term exposure to inhaled indoor allergens.
Evidence suggests that the adjuvant effects associated with macrophage activation are related to endotoxin. Additional research is necessary, however, to clarify this phenomenon.
Research Agenda Item: Determine whether bacterial products (such as endotoxin) or fungal products may act as adjuvants in the immune responses to indoor allergens.
As discussed in earlier chapters of this report, the magnitude of allergen exposure appears to be related to the risk of sensitization. Allergen exposure is also related to the risk of developing asthma and the age at which asthma develops. Genetic and other local host factors are also important in
atopy and asthma. Understanding the relative importance of each of these individual factors and their interaction with each other is essential to understanding the mechanisms of immune function.
Research Agenda Item: Conduct research to identify risk factors other than exposure, and clarify their potential significance relative to indoor allergy. This effort should include an evaluation of the role of genetic and local host factors in allergen sensitization.






















