2
Magnitude and Dimensions of Sensitization and Disease Caused by Indoor Allergens
The magnitude and dimensions of a disease or its antecedents can be measured and described in several ways (Table 2-1). The prevalence of a disease, for example, is a measure of its frequency in a population at some specified point in time. The incidence of a disease is the number of new cases of the disease that occur during a specified period of time. Exploration of disease incidence can focus public health attention on critical time periods in the development of disease. For example, the observation that allergy often develops by age 5 suggests that interventions are needed for infants and young children.
Incidence and prevalence rates can be determined for the entire population, or they can be specified by gender, age, ethnic group, socioeconomic class, geographical region, or time of year. The increased mortality from asthma among African Americans (Sly, 1988; NHLBI, 1991), for instance, has focused attention on the disease in this segment of the population. Community-based epidemiological studies and national health surveys provide the best available estimates of the overall prevalence of immunologic sensitization and of specific diseases.
Disease severity—a measure of the impact of a disease on a patient's life, the intensity of medical care required, and the ultimate outcome—is another indicator of the magnitude and dimensions of a particular disease. Measures of disease severity are often derived from national mortality data and hospital discharge statistics. They are used to evaluate the effectiveness of therapeutic regimens, environmental control strategies, and educational and behavior modification self-management programs.
TABLE 2-1 How Diseases Can Be Measured
|
Question |
Appropriate Measure |
|
How many people have asthma sometime in their life? |
Cumulative prevalence |
|
How many people have asthma in the United States today? |
Current prevalence |
|
How many people get asthma when they are children? |
Age-specific incidence rates |
|
Do children have more asthma than adults? |
Comparison of prevalence rates for specific age ranges |
|
Does allergy have a role in asthma? |
Comparison of the probability of developing asthma among people with and without skin test reactivity |
|
What proportion of asthma is attributable to allergy? |
Attributable fraction |
|
What proportion of asthma in children is attributable to house dust mite exposure? |
Attributable fraction |
Generally speaking, mild disease causes symptoms but only intermittently requires medication and infrequently alters life activities. Moderately severe disease may require regular physician visits, regular medication, and lost time from work or school. Severe illness may require admission to an intensive care unit, to a regular medical floor, or to a hospital emergency room (in decreasing order of intensity). In the case of allergic disease, death occurs relatively infrequently. Other measures that can be used to indicate the magnitude and dimensions of a particular disease (such as allergy) include quality of life, trends over time, and economic and psychosocial impact.
This chapter uses these and other measures to discuss the magnitude and dimensions of two aspects of allergic disease: sensitization and the specific allergic diseases themselves. Immunologic sensitization is important because it is an indicator of the population at greatest risk of developing allergic disease. The remainder of this chapter discusses the public health significance of immunologic sensitization and allergic disease in these terms.
IMMUNOLOGIC SENSITIZATION
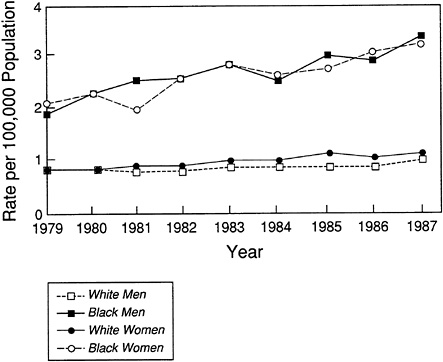
Allergic disease develops through a series of steps that are becoming more clearly understood (Figure 2-1). As described briefly in Chapter 1, allergic disease occurs when a genetically predisposed or susceptible individual is exposed to an allergen and becomes immunologically sensitized. The occurrence of different types of sensitization can be ascertained by skin
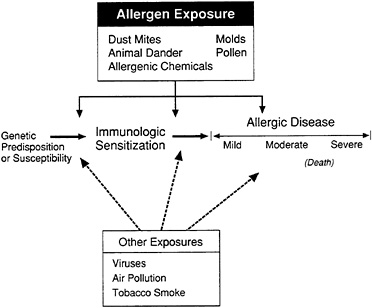
FIGURE 2-1 Development of allergic disease, illustrated schematically. A genetically susceptible individual is exposed to an allergen and becomes immunologically sensitized. At this stage the person is asymptomatic, but the sensitization may be detected by skin tests or laboratory tests. Over time, a proportion of sensitized individuals will develop one of a group of allergic diseases. Exposure to allergen is understood to be a major factor at each stage of the pathogenesis of these diseases.
tests, serologic measurements, or tests of cell function. In the early stages of sensitization, people who are sensitized have not developed symptoms of disease. The magnitude of this group within the population is of interest, however, because it reflects the proportion of the population at greatest risk of developing allergic disease. Additional exposure to the sensitizing allergen leads to the development of an allergic reaction (disease) that can be mild, moderate, or severe, depending on the amount of exposure. Exposure to other substances that might irritate the respiratory tract (e.g., environmental tobacco smoke) can serve to promote the development of allergic reactions and disease.
Skin testing has been the primary diagnostic tool for allergy for over 100 years. Skin test reactivity (i.e., a positive skin test, also known as atopy) indicates that an individual has been immunologically sensitized and now has specific immunoglobulin E (IgE) antibody against one or more common allergens. The presence of skin test reactivity indicates an increased risk for one of several diseases including allergic rhinitis and asthma, but at the time skin test reactivity is detected, disease may or may not be present. Table 2-2 shows results from several studies that measured sensitization
prevalence in various populations. The results indicate a range from a low of 20 percent to a high of 51 percent in different studies. It is estimated that about 40 percent of people in the United States have been immunologically sensitized as indicated by skin test reactivity to a panel of currently available allergens. The recent International Consensus Report (NHLBI, 1992) claims that about 30 percent of all populations are skin test positive.
Early childhood is a common time for sensitization. Barbee and others (1987) showed that 22 percent of a cohort of children less than 5 years old had skin test reactivity to one or more allergens. During an 8-year follow-up, the prevalence increased to 44 percent. Gergen and coworkers showed that 18 percent of Caucasian and 28 percent of African American children showed skin test reactivity when tested between the ages of 6 and 11 (Gergen et al., 1987). In a cohort of genetically susceptible children, 20 percent developed skin test reactivity by age 5; another 20 percent became reactive between ages 5 and 11 (Sporik et al., 1990).
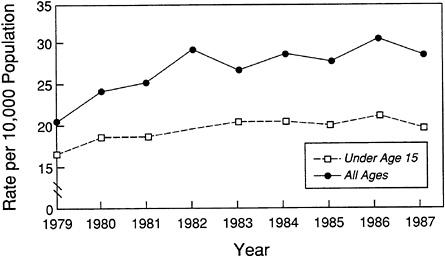
Skin test reactivity increases in prevalence until age 20–45 and then decreases (Figure 2-2; Barbee et al., 1976, 1987; Gergen et al., 1987). In most studies, skin test reactivity is similar for both sexes, although men have more total IgE (Barbee et al., 1976; Burrows et al., 1980; Klink et al., 1990). Although immunologic sensitization is generally stable over time, small seasonal variations have been observed (Peat et al., 1987). Prevalence rates of sensitization also increase somewhat with the use of a greater number of allergens during testing (Barbee et al., 1987).
Table 2-3 and Figure 2-3 show estimates of the prevalence of sensitization in certain population samples to specific allergens as determined by skin test reactivity. Among Australian schoolchildren, for example, sensitization to house dust mite was shown to be most common, followed by grass and weeds, animal danders, and molds (Peat et al., 1987). Similar rates of sensitization have recently been found in middle-class American children. The prevalence of cockroach allergy shown in Figure 2-3 may well be higher in selected populations, such as among residents in cities in which cockroach infestations are widespread. A study of patients visiting an emergency room in Virginia showed that 5 percent of nonasthmatics were sensitized to cockroaches, compared to 33 percent of asthmatics (Pollart et al., 1989). Fifty-four percent of patients referred to a Kansas City clinic for possible allergic disease were sensitized to cockroach allergen (Hulett and Dockhorn, 1979).
Risk Factors
In keeping with a public health approach to prevention and control of allergic disease and the need to improve the understanding of the etiology,
TABLE 2-2 Partial Listing of Published Data on the Prevalence of Skin Test Reactivity
|
Source |
Population |
%a |
Notes |
|
United States |
|||
|
Barbee et al., 1987 |
Community sample (N = 1,333; Arizona) |
39 51 |
Ages 8–60 Rates with retesting 8 years later |
|
Gergen et al., 1987 |
Nationwide sample (N = 16,204; NHANESb) |
20.2 |
Some people with disease were excluded; the skin test flare was used as the response |
|
Freidhoff et al., 1981 |
Workplace study (N = 174; Maryland) |
24 |
Lower rates are seen in other workplace studies |
|
Barbee et al., 1976 |
Community sample (N = 3,012; Arizona) |
34 |
Ages 5–55 |
|
Hagy and Settipane, 1969 |
College freshmen (N = 1,243) |
30.9 |
|
|
Henderson, 1993 (personal communication 1-26-93) |
Schoolchildren (N = 225; North Carolina) |
40 |
|
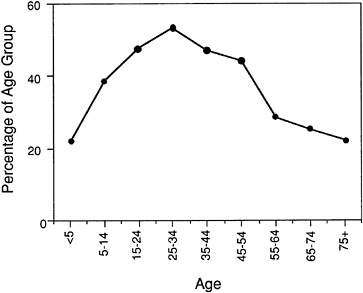
FIGURE 2-2 Changes in skin test reactivity with age. By age 5, approximately 20 percent of children will be sensitized to common aeroallergens. Skin test reactivity increases with age until ages 25–34 and then declines. Source: Barbee et al., 1987.
it is important to identify potential risk factors associated with allergic disease. Risk factors are biological, environmental, and behavioral characteristics that are causally associated with health-related conditions (Lalonde, 1974; Last, 1986). Heredity, for example, is an important biological risk factor in the development of immunologic sensitization and allergy. Infants of parents with allergic disease develop positive skin tests at higher rates than infants in population-based studies. Skin prick test reactivity during the first year of life has been reported as ranging between 30 and 70 percent of at-risk infants—i.e., those who have one or both parents with allergic disease (Zeiger, 1988). In general, if one parent has allergies and the other does not, then the chances are one in three that each of their children will have allergies. If both parents have allergies, it is much more likely (seven in ten) that each of their children will have some manifestation of allergic disease.
Exposure to allergens is an example of an environmental risk factor related to the prevalence of sensitization. Household exposure to elevated levels of dust mite allergen (see Chapter 3) in infancy, for example, has been associated by age 5 with an increased prevalence of positive dust mite skin tests and an increased concentration of dust mite IgE antibody (Zeiger, 1988). Another example is found among people living at high altitudes in Briançon, France, where significantly lower rates of sensitization to house
TABLE 2-3 Partial Listing of Published Prevalence Data on Sensitization (per 100 population) to Some of the Common Aeroallergens
|
Source |
Population |
House Dust Mite |
Grasses and/or Weed Pollen |
Animal Danders |
Molds |
Notes |
|
Barbee et al., 1976 |
Community (N = 3,101; United States) |
ND |
17–24 |
NDa |
8 |
Crude house dust: 9b |
|
Peat et al., 1987 |
Schoolchildren (N = 2,363; Australia) |
19–31 |
18–29 |
20–25 |
10–20 |
|
|
Sears et al., 1989 |
Birth cohort to age 13 (N = 714; New Zealand) |
30.1 |
32.5 |
13.3 |
|
|
|
D. Charpin et al., 1988a |
Adults (France) |
|
|
|
|
|
|
|
Marseille (N = 4,008; low altitude) |
44.5 |
|
|
|
|
|
|
Briançon (N = 1,055; high altitude) |
10 |
|
|
|
|
|
D. Charpin et al., 1991 |
Schoolchildren (France) |
|
|
|
|
|
|
|
Martigues (N = 693; low altitude) |
16.7 |
8.5 |
5.6 |
|
|
|
|
Briançon (N = 240; high altitude) |
4.1 |
21.7 |
3.3 |
|
|
|
Henderson, 1992 (personal communication) |
Schoolchildren (North Carolina) |
27 |
Pending |
Pending |
|
|
|
Godfrey and Griffiths, 1976 |
Schoolchildren (N = 303; Southampton, England) |
26 |
24 |
|
|
|
|
a ND, no data. b Crude house dust is a skin test reagent that contains unpredictable amounts of antigens such as dust mite, animal dander, and molds. Its use has been largely replaced by purified allergen extracts. |
||||||
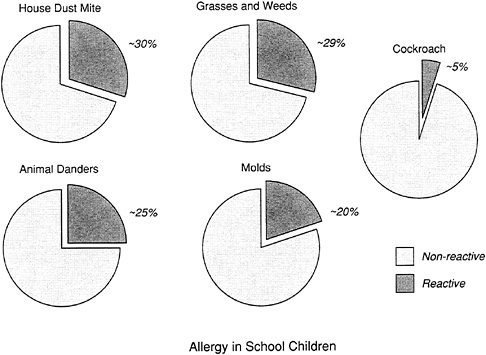
FIGURE 2-3 Estimated prevalence of skin test reactivity to selected aeroallergens among schoolchildren. The presence of skin test reactivity indicates that the child has been sensitized to that aeroallergen by an IgE mechanism. Henderson found lower rates of skin test reactivity to animal danders and molds in their population. (Table 2-3 shows results from additional epidemiological studies.) Sources: Henderson, 1993; Peat et al., 1987; Sears et al., 1989.
dust mite occur than in comparison populations at lower altitudes (Martigues for children and Marseilles for adults) (D. Charpin et al., 1988a, 1991; Vervloet et al., 1979). Analyses of house dust from Briançon found lower levels of house dust mite compared with the levels in dust from low-altitude homes (see Table 2-3). In addition, Sporik and colleagues (1990) demonstrated a trend toward an increasing degree of sensitization among children at age 11 with greater dust mite exposure at age 1. Chapter 6 analyzes these and other studies and suggests that there may be an exposure-response relationship between dust mite exposure and the prevalence of skin test reactivity (sensitization).
Exposure to environmental tobacco smoke is another example of an environmental risk factor in that it appears to be associated with increased skin test reactivity in children (Burrows and Martinez, 1989) and a twofold increase in serum IgE in infants (Zeiger, 1988). Zeiger also discussed the possible effects of exposure to ingestants and microbial agents on the risk
of sensitization. Animal studies have shown an increased rate of new IgE sensitization when allergen exposure is interspersed with ozone, nitrogen dioxide, or sulfur dioxide inhalation (Matsumura, 1970a–c; Riedel et al., 1988; Sheppard, 1988b). Diesel fumes have also been shown to act as an adjuvant for IgE sensitization (Muranaka et al., 1986).
The effect of active smoking—a possible behavioral risk factor—on the prevalence of skin test reactivity in adults is uncertain, given the existence of conflicting data. Barbee and colleagues (1987) found lower rates of skin test reactivity among current smokers than either nonsmokers or ex-smokers; ex-smokers had higher rates of skin test reactivity than nonsmokers. The study team interpreted this finding as demonstrating a self-selection process; that is, smokers with skin test reactivity would stop smoking. In contrast, Gergen and coworkers (1987) did not find a relationship between skin test reactivity and smoking status.
Other Types of Sensitization
Immunologic sensitization may also occur through non-IgE mechanisms. Specific IgG in the serum, for example, is a marker of sensitization to allergens known to cause hypersensitivity pneumonitis. Tests of lymphocyte proliferation can indicate sensitization through cellular immune mechanisms (see Chapter 4).
Exposure to allergens in the workplace may result in immunologic sensitization and occupational disease. Table 2-4 lists agents that are associated with causing asthma in occupational settings. The prevalence of sensitization among workers ranges from less than 10 percent for some agents to as much as 80 percent for platinum. Exposures may occur in an industrial or office setting. Although many of the protein allergens have long been recognized, a lengthening list of newly recognized allergenic chemicals is developing (see Chapter 3).
The prevalence of exposure and sensitization to defined, reactive, allergenic chemicals has led to a relatively new but growing category of chemical allergens. Most of these chemicals were initially developed for use in specific industrial processes, but their commercially useful reactive properties often make them react with human proteins as well, a feature that is thought to contribute to their allergenicity. As with other allergens, immunologic sensitization to these chemicals may occur in the absence of symptoms of allergic disease.
DISEASES
Although some people remain asymptomatic despite being immunologically sensitized, many develop one of several diseases including asthma,
TABLE 2-4 Selected Agents Causing Asthma in Selected Occupations
|
Occupation or Occupational Field |
Agent |
|
Animal-related |
|
|
Laboratory animal workers, veterinarians |
Dander, urine proteins |
|
Food processing |
Shellfish, egg proteins, pancreatic enzymes, papain, amylase |
|
Dairy farmers |
Storage mites |
|
Poultry farmers |
Poultry mites, droppings, feathers |
|
Granary workers |
Storage mites, aspergillus, indoor ragweed, grass pollen |
|
Research workers |
Locusts |
|
Fish food manufacturing |
Midges |
|
Detergent manufacturing |
Bacillus subtilis enzymes |
|
Silk workers |
Silkworm moths and larvae |
|
Plant proteins |
|
|
Bakers |
Flour |
|
Food processing |
Coffee bean dust, meat tenderizer (papain), tea |
|
Farmers |
Soybean dust |
|
Shipping workers |
Grain dust (molds, insects, grain) |
|
Laxative manufacturing |
Ispaghula, psyllium |
|
Sawmill workers, carpenters |
Wood dust (western red cedar, oak, mahogany, zebrawood, redwood, Lebanon cedar, African maple, eastern white cedar) |
|
Electric soldering |
Colophony (pine resin) |
|
Cotton textile workers |
Cotton dust |
|
Nurses |
Psyllium, latex |
|
Inorganic chemicals |
|
|
Refining |
Platinum salts |
|
Plating |
Nickel salts |
|
Diamond polishing |
Cobalt salts |
|
Stainless steel welding |
Chromium salts |
|
Manufacturing |
Aluminum fluoride |
|
Beauty shop |
Persulfate |
|
Refinery workers |
Vanadium |
|
Welding |
Stainless steel fumes |
|
Organic chemicals |
|
|
Manufacturing |
Antibiotics, piperazine, methyldopa, salbutanol, cimetidine |
|
Hospital workers |
Disinfectants (sulfathiazole, chloramine, formaldehyde, psyllium, glutaraldehyde) |
|
Anesthesiology |
Enflurane |
|
Poultry workers |
Aprolium |
|
Fur dyeing |
Paraphenylene diamine |
|
Rubber processing |
Formaldehyde, ethylenediamine, phthalic anhydride |
|
Occupation or Occupational Field |
Agent |
|
Organic chemicals |
|
|
Plastics industry |
Toluene diisocyanate, hexamethyl diisocyanate, diphenylmethyl isocyanate, phthalic anhydride, triethylene tetraamines, trimellitic anhydride, hexamethyl tetramine |
|
Automobile painting |
Dimethyl ethanolamine toluene diisocyanate |
|
Foundry workers |
Furfuryl alcohol resin |
|
SOURCE: NHLBI, 1991 |
|
rhinitis, eczema, hypersensitivity pneumonitis, and allergic bronchopulmonary aspergillosis. Figure 2-4 shows the generally accepted range of prevalence for these diseases in the population. Estimates of the magnitude of these diseases are affected by the diagnostic criteria used, as well as different study and data collection methods. Individual diseases are discussed in further detail below and are grouped as follows: first, common diseases clearly related to allergy, then less common diseases clearly related to allergy, and finally, common diseases possibly related to allergy.
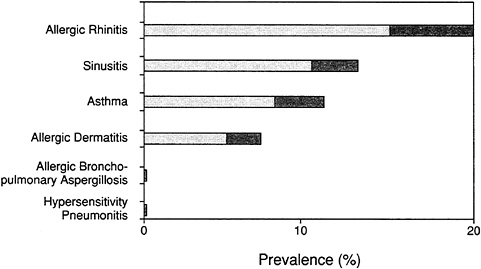
FIGURE 2-4 Estimated range of prevalence of diseases in total U.S. population that are commonly, although not invariably, related to allergy. Darker screen indicates the range in published data.
Source: NHLBI, 1991.
Common Diseases Clearly Related to Allergy and IgE Antibody
Three common diseases are clearly related to exposure to indoor allergens: asthma, rhinitis (hay fever), and allergic skin conditions (i.e., eczema and urticaria). Although specific causal genes have not been identified, the genetic predisposition for these diseases is well established. If neither parent has a history of allergy or atopy, a child has only a 0–19 percent chance of having a childhood allergic disease. If one parent has atopy, the risk rises to 31–58 percent; if both parents have atopy, the risk rises still further to 60–100 percent (Zeiger, 1988; Table 2-5). In addition, an earlier age of onset of allergic disease is related to a family history of atopy (Figure 2-5; Smith, 1988). Examples of the effects of these diseases on quality of life are provided in Box 2-1. The economic impact of these conditions was discussed briefly in Chapter 1.
TABLE 2-5 Prediction of Development of Sensitization or Allergic Disease in Childhood Based on Parameters Present During Infancy
|
Factor |
Likelihood of Allergic Disease (%) |
|
Parental atopy history |
|
|
Both parents |
60–100 |
|
One parent |
31–58 |
|
Neither parent |
0–19 |
|
Aeroallergen exposure assessed at age 1* |
|
|
<10 µg Der p I/g of dust |
6 |
|
>10 µg Der p I/g of dust |
28 |
|
Serum IgE during infancy |
|
|
Increased >1 standard deviation above geometric mean |
75 |
|
Normal |
5 |
|
Illness during infancy |
|
|
Recurrent croup |
58 |
|
Recurrent wheezing |
36 |
|
Wheezing and blood eosinophilia |
75 |
|
Wheezing and positive radioallergosorbent test |
44 |
|
None of these illnesses |
13 |
|
SOURCE: Zeiger (1988) and Sporik et al. (1990). * The data on aeroallergen exposure, which were derived from Sporik and colleagues, were obtained from a cohort of newborns, each of whom had one parent with allergic disease. Asthma was defined as active wheezing and bronchial hyperreactivity. The numbers in parentheses show the percentage of all subjects who reported a history of wheezing. The relative risk of active asthma was 4.8 times greater if the child had been exposed to more than 10 µg of Der p I/g of dust in infancy. The percentage of sensitization for children exposed to less than 10 µg Der p I/g of dust was 31 percent; the percentage for children exposed to more than 10 µg was 56 percent. |
|

FIGURE 2-5 Relationship between a family history of allergic disease and the time of onset of allergic disease in children. Family history is an extremely important determinant of the risk of allergic disease in children.
Source: Smith, 1988.
ALLERGIC ASTHMA
Definition and Diagnosis
Asthma is a lung disease characterized by (1) airway obstruction that is reversible (but not completely so in some patients) either spontaneously or with treatment, (2) airway inflammation, and (3) increased airway responsiveness to a variety of stimuli (NHLBI, 1991). Lung inflammation is often present even when symptoms are absent. People with asthma often experience intermittent wheezing, coughing, chest tightness, and shortness of breath.
The diagnosis of asthma for an individual patient is usually made during a physician office visit, emergency room visit, or hospitalization. The diagnosis is based on one or more of the following: history of episodic symptoms, signs of asthma on physical examination (chiefly wheezing), or pulmonary function test results demonstrating reversible airflow obstruction and bronchial hyperreactivity (see Chapter 5). Bronchial hyperreactivity may be quantified by determining the concentration of methacholine or histamine required to induce a transient drop in lung function. In asthmatics, the concentration of methacholine required to induce a drop in lung function is usually lower than in nonasthmatics.
|
BOX 2-1 Impact of Allergic Disease on Quality of Life Allergic diseases can disrupt childhood education and family life and have a negative effect on quality of life.
|
Once a diagnosis of asthma is made, the contribution of allergy to asthma is of great interest. Allergy may be confirmed through either skin testing or measurement of specific IgE antibodies in blood samples, or both. The causal relationship between allergy and asthma is established by the individual's history (see Chapter 5). For example, asthma that occurs in the spring may be due to allergens from tree pollen. People with perennial asthma are often unaware of the allergens that trigger their disease. Current recommendations include environmental modification as an early step in asthma management (NHLBI, 1991).
The diagnosis of asthma in population-based studies has been made in a variety of ways. Diagnostic criteria may be influenced by the local language, customs, and definitions and by physician habits, questionnaires, and study objectives (Kryzanowski et al., 1990). Examples of the epidemiologic definition of asthma include a history of episodic or persistent wheezing, a physician diagnosis of asthma, evidence of reversible airflow obstruction on pulmonary function tests, evidence of bronchial hyperreactivity, or a combination
of the above. Airway inflammation, a cardinal feature of asthma, cannot practically be determined in population studies. Differences in diagnostic criteria may explain variable rates of disease. Another source of variation is diagnostic overlap with conditions such as bronchitis (Gregg, 1983; Lebowitz et al., 1990) which can occur in children or adults. Forty to 50 percent of children with asthma also have chronic bronchitis. In adults, 50 to 80 percent of smokers have chronic bronchitis, and only a minority of these have asthma (Snider, 1988).
Research indicates that of those persons with asthma, 90 percent of children, 70 percent of young adults, and 50 percent of older adults also have allergy (Lehrer et al., 1986; Peat et al., 1987; Platts-Mills et al., 1992). These data strongly suggest a role for allergy in the pathogenesis of asthma, particularly in childhood.
Attributable Fraction
Public health officials are often asked to estimate the fraction of asthma in the population that could be attributed to allergy or to exposure to a specific allergen. Several conceptual issues must be understood before making these calculations. Last (1986) states that attributable fractions in the population cannot be estimated from prevalence data but must be calculated from incidence data obtained in cohort studies. This is particularly true for conditions such as cancer where the case-fatality rate is high, and the prevalence in a population grossly underestimates the cumulative incidence rate. It is also true for brief, self-limited illnesses such as influenza where the point prevalence would underestimate cumulative incidence. By contrast, asthma is a chronic disease with a low case-fatality rate, and therefore the prevalence and the cumulative incidence rates are similar. The prevalence of asthma is a reasonable measure of the burden of the disease in a society. Estimates of the fraction of asthma attributable to allergy or to a specific allergen may, therefore, utilize cumulative incidence or prevalence data.
Last (1986) also states that attributable fractions should not be obtained from the distribution of risk ratios obtained in case control studies. Approaches have been developed that use data from case control studies (Schlesselman, 1982), but these should be verified with population-based data. The essential limitation in using case control data to estimate population attributable risk is that it is difficult to know whether the control group is representative of the general population. This concern lessens when the outcome of interest is similar in multiple control groups.
Another problem with calculating attributable fractions is the issue of competing risks. Individuals may be exposed simultaneously to several risk factors, such as house dust mite, cockroach, and cat allergens. The assumption is generally made that exposure to competing risks is uniform in the
population, and that the calculations listed below are fairly robust to competing risks. It is possible that the attributable fractions for several risks will sum to more than 1 (i.e., more than 100 percent).
Finally, the risk estimates should not be generalized to the entire population when they are calculated based on studies of a segment of the population, such as children. The reason for this is that measures of risk may systematically change over time. As noted above, the prevalence of skin test reactivity is lower in school children than in young adults.
Studies that are used to calculate attributable fractions should meet several criteria. For example, the exposed and unexposed populations should be alike with respect to demographic variables that could affect disease rates. The study instruments that are used should be the same, and preferably the exposed and unexposed populations should have been studied by the same team.
Finally, calculation of attributable fractions should be specified as referring to the entire population or to only the exposed population.
According to Last (1986) the population attributable risk is calculated as:
where AFp, the attributable fraction (population), also called the population attributable risk, is the proportion of the disease that can be attributed to exposure to the risk factor; Ip is the incidence in the population; and Iu is the incidence in the unexposed population.
The attributable fraction in the exposed population is calculated as:
where AFe is the attributable fraction (exposed), i.e., the proportion of cases among the exposed population that can be attributed to exposure to the risk factor of interest; Ie is the incidence rate among the exposed group; and Iu is the incidence rate among the unexposed group.
Table 2-6 presents some estimates of attributable fraction using data from several published studies.
Prevalence
Recent surveys have found prevalence rates of asthma of 8 to 12 percent in the U.S. population—an estimated 20–30 million people (Burrows et al., 1989; Mak et al., 1982; Pattemore et al., 1990; Weiss et al., 1992a). As yet unpublished data suggest that 10 percent of children had been prescribed an inhaler for the treatment of asthma (Platts-Mills, personal communication; Sporik et al., in press). The National Asthma Education Program
has estimated that 10 million people in the United States currently have asthma (NHLBI, 1991). Figure 2-6 shows how the definition of asthma can affect estimates of prevalence in epidemiological studies. Additional work is needed to clarify the relationship between asthma and the various definitions of allergy phenotype.
Incidence
About half of the cases of childhood asthma develop before age 5, and most of the rest develop before adolescence. Incident cases are uncommon between ages 20 and 40, with a gradual increase in incidence beginning in the fifth decade of life. Overall, cases of asthma have increased in the past few decades. During the 1920s and 1930s, incident cases were uncommon; a gradual increase began in the 1940s, however, and has continued up to the present. The overall annual incidence of asthma in a Tucson study was 0.46 percent (Lebowitz, 1989).
Impact
Asthma is generally treated in outpatient settings. In 1985, of the 640 million total ambulatory care visits estimated by the National Ambulatory Medical Care Survey (NHLBI, 1991), 6.5 million (1 percent) had asthma as a first-listed diagnosis. From 1970 to 1987, hospital discharge rates for asthma increased nearly threefold. African Americans were more than twice as likely as Caucasians to be hospitalized.
Most recently K. B. Weiss and colleagues (1992b) estimated that 1.8 million people required emergency room services for asthma in 1985, and 48 percent of the visits involved children under age 18. There were an estimated 1.5 million hospital outpatient visits to treat asthma. K. B. Weiss and colleagues (1992b) also estimated the cost of illness related to asthma in 1990 to be $6.2 billion.
Another measure of impact is absenteeism. A WHO/EURO report (1990) reported that a substantial portion of absenteeism from work or school is associated with infectious and allergic episodes caused by exposure to indoor air. Similarly, a 1979 report (NIAID, 1979) stated that asthma was among the leading causes of physician visits, hospitalizations, and workdays lost.
Trends Over Time
Figures 2-7, 2-8, and 2-9 show recent trends over time in asthma prevalence, mortality, and hospitalization rates, respectively. The prevalence rate of asthma in the first half of the century was about 1-2 percent in Caucasian populations in industrialized countries (Gregg, 1989). The first estimate of the prevalence rate of asthma in the United States—in 1928—was less than 1 percent in both children and adults; a 1930 survey reported a prevalence
TABLE 2-6 Some Estimates of Attributable Fractions
|
Study |
Population |
Definition of Exposure |
Ie |
Iu |
Attributable Fraction |
|
The attribution of skin test reactivity to allergen exposure |
|||||
|
House dust mites |
|||||
|
Murray et al., 1985 |
Children visiting allergy clinic (Canada) |
u = residence in dry areas (N = 60) e = residence in humid areas (N = 714) |
0.4 |
0.02 |
0.95 |
|
D. Charpin et al., 1991 |
Schoolchildren (France) |
u = residence in low mite region (N = 240) e = residence in high mite region (N = 693) |
0.167 |
0.041 |
0.75 |
|
D. Charpin et al., 1988a |
Adults (France) |
u = residence in low mite region (N = 1,055) e = high mite region (N = 4,008) |
0.275 |
0.102 |
0.63 |
|
Sporik et al., 1990 |
Children of an atopic parent (England) |
u = exposure to <10 µg/g of mite (N = 17) e = exposure to >10 µg/g of mite (N = 43) |
0.47 |
0.31 |
0.34 |
|
Grass pollen |
|
|
|
|
|
|
D. Charpin et al., 1991 |
Schoolchildren (France) |
u = residence in low grass region (N = 693) e = residence in high grass region (N = 240) |
0.217 |
0.085 |
0.61 |
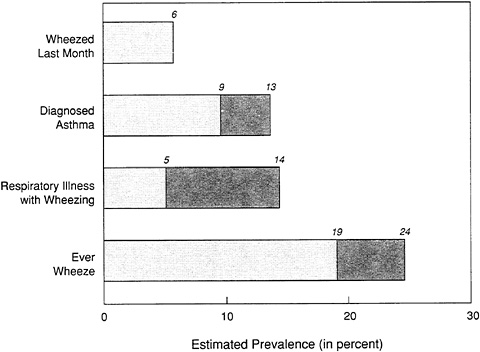
FIGURE 2-6 Effect of case definition on estimates of the prevalence of asthma. Shaded area indicates the range of data. Sources: Barbee et al., 1985; Britton et al., 1986; Peat et al., 1987.
rate of about 0.5 percent (Barbee et al., 1985). Over the past 20 years, much higher current and cumulative prevalence rates have been reported from surveys of both children and adults; Figure 2-7 shows the rise in rates for 1980–1987 alone. Mortality epidemics occurred in Britain and Australasia around 1960 and in Britain and New Zealand in the 1970s. U.S. surveys in the 1970s showed prevalence rates of between 4 and 6.7 percent (Barbee et al., 1985; NCHS, 1986). In 1983 Sharma and Balchum stated that 9 million Americans had asthma, 3 million of whom were children.
Recent data also suggest a possible increase in the severity of asthma, using mortality and hospitalization rates as indices of severity (Figures 2-8 and 2-9, respectively; Barbee et al., 1985; Gergen and Weiss, 1992; Gregg, 1983, 1989). Hospital admissions appear to have increased remarkably in Great Britain and the United States, paralleling the increase in prevalence. The hospital discharge rate with asthma as the first-listed diagnosis rose 43 percent among children less than age 15 from 19.8 to 28.4 discharges per 10,000 population (NHLBI, 1991). A 5 percent increase in total hospitalizations for asthma occurred between 1987 and 1990 (NCHS, 1992). These data could reflect changes in the course of the disease or changes in medical
practice, including shifting diagnostic criteria or methods (Gregg, 1983, 1989; Newacheck et al., 1986). It should also be noted, however, that except for an increase in mild asthma among older Caucasian children, a significant increase in prevalence rates has not been seen in the National Health Interview Survey (Weitzman et al., 1992).
Asthma death rates have increased substantially in this country over the past 10 years. In 1988, 4,580 people died from asthma in the United States (NHLBI, 1991). During 1979–1984, the death rate for asthma rose from 1.2 per 100,000 people (in 1979) to 1.5 per 100,000 (in 1983 and 1984). Asthma was reported as the underlying cause of 1,674 deaths in the United States in 1977; this statistic increased to 3,564 in 1984 (Sly, 1988), a trend that runs counter to the decreasing death rates seen between 1950 and 1978 (Sly, 1988). Although the first observed rise was concomitant with a change in coding procedures by the National Center for Health Statistics, the rising trend has persisted during a period of uniformity in coding. The increase in death rates has been seen across ages and races but is particularly notable among African Americans (NHLBI, 1991; Sly, 1988). Increases in asthma mortality have been variously attributed to inadequate medical management (especially among minority patients of low socioeconomic status), underutilization of available health care, neglect of personal health, changes in prescribing practices, inappropriate use of medications, and altered environmental factors,
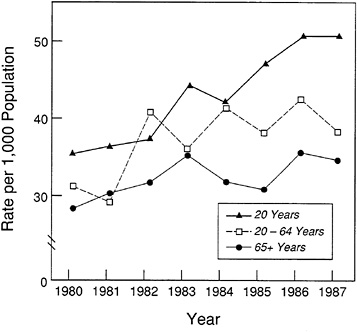
FIGURE 2-7 Trends in Asthma Prevalence. Source: NHLBI, 1991.
including exposure to new allergens. The New Zealand experience (Sears et al., 1989) indicates that several of these factors are likely to contribute to increased mortality and that broad intervention can reduce these rates (Burrows and Lebowitz, 1992; Lofdahl and Svedmyr, 1991).
Risk factors
Genetic Factors Genetic factors are important in asthma and atopy (Gregg, 1983; Horwood et al., 1985; Lebowitz et al., 1984; Sibbald, 1980; Sibbald et al., 1980). The highest prevalence of asthma occurs among children whose parents have evidence of allergic disease (see Table 2-5; Barbee et al., 1985; Luoma, 1984; Sporik et al., 1990). In addition, the symptom of ''persistent wheeze" has been shown to have a familial component. Theoretically, familial aggregation of cases of asthma could be explained either by genetic factors or by common exposure to increased environmental risks. The low prevalence of asthma (as well as low rates of smoking-related lung disease) among Native Americans has been attributed to unspecified genetic factors.
Bronchial Hyperreactivity Bronchial hyperreactivity is both a feature of asthma and a risk factor for its development. The risk of bronchial hyperreactivity increases with increasing skin test reactivity (Burrows and Lebowitz, 1992; Lofdahl and Svedmyr, 1991).
Skin Test Reactivity The presence of skin test reactivity is clearly a strong risk factor for asthma. This relationship has been shown using a variety of definitions of asthma and different study designs. New asthma that develops before age 40 is likely to be associated with allergen skin test reactivity, high total serum IgE, a family history of atopy, and prior symptomatology. Total IgE is still strongly related to asthma prevalence and incidence above age 60 (Burrows et al., 1991). Overall, half of existing cases of asthma have been attributed to allergenic factors.
Recently, the risk of asthma has been related to skin test reactivity to specific allergens. Gergen and Turkeltaub (1992), using data from the second National Health and Nutrition Examination Survey (NHANES II), demonstrated an independent association of asthma with reactivity to an extract of crude house dust (odds ratio, 2.9) and to alternaria (odds ratio, 2.3). In a birth cohort of New Zealand children that was monitored up to age 13, sensitivities to house dust mite (odds ratio, 6.7) and to cat dander (odds ratio, 4.2) were highly significant independent risk factors associated with the development of asthma (Sears et al., 1989). Grass sensitivity, although common, was not an independent risk factor (odds ratio, 1.33). Aspergillus fumigatus was uncommon (skin test positivity in only 2.4 percent of the sample) but was significantly correlated with asthma (odds ratio, 13.8).
Allergen Exposure As outlined above, the magnitude of allergen exposure appears to be related to the risk of sensitization. Allergen exposure is also related to the risk of developing asthma and the age at which asthma develops. Sporik and colleagues (1990) demonstrated that exposure to more than 10 µg of dust mite allergen (Der p I) per gram of dust was associated with a 4.8 relative risk of asthma by age 11.1 These investigators also showed that the age at which the first episode of wheezing occurred was inversely related to the level of dust mite exposure assessed when the subject was 1 year old.
Allergen exposure has also been related to disease severity. Voorhorst and coworkers (1967) showed that allergic and atopic asthmatics with sensitivity to house dust mite had clinic visits that correlated well with mite growth curves in their homes, a finding that has been confirmed by others (Andersen and Korsgaard, 1986; Tovey et al., 1981a). Clark and colleagues (1976) found a reduction in peak flows 2 of children with asthma that they associated with house dust when housecleaning increased particle concentrations in the air. O'Hallaren et al., (1991) provided evidence that exposure to the aeroallergen Alternaria is a risk factor for sudden respiratory arrest in asthmatics. The O'Hallaren team found that alternaria skin test reactivity was associated with a 200-fold risk of respiratory arrest, the timing of which corresponded uniformly with the alternaria season in that region.
It has been shown that prolonged allergen avoidance reduces the severity of asthma as indicated by tests of bronchial hyperreactivity (Platts-Mills et al., 1982). For example, asthmatic children who stayed in a sanitorium in Davos, Switzerland, for 1 year showed progressive reductions in bronchial hyperreactivity. It has also been demonstrated that patients with seasonal asthma will lose their bronchial reactivity to histamine after the pollen season.
Hospital emergency room studies have demonstrated an increased risk of allergen sensitization among asthmatics compared with patients being treated for other conditions. The content of allergen in reservoir dust samples from the homes of asthmatics compared with patients with other conditions is also reported to be larger. These studies are covered in detail in Chapter 3.
Geographic location Rates of asthma in other populations around the world appear to be highly variable (Barbee et al., 1985; Gregg, 1983). Charpin and coworkers (1988b) found no urban–rural difference in asthma
|
1 |
That is, a person exposed to this level of dust mite allergen is 4.8 times more likely to develop asthma than a person who has not been so exposed. |
|
2 |
Peak flow is a measure of lung function. See the Glossary and Chapter 5 for definition and details. |
prevalence rates. Sly found no difference in urban versus rural asthma mortality rates and no variation by geographic region (Sly, 1988). K. B. Weiss and colleagues (1992a), however, found that inner-city asthma was more prevalent than asthma in suburban areas. Moreover, in a comparison of asthmatics being treated at two Delaware hospitals, cat allergy and cat allergen exposure were more common among patients who were treated in a suburban Wilmington hospital, and cockroach allergy and allergen exposure were more common among patients being treated in an urban Wilmington hospital (Gelber et al., in press). This suggests that similarities in urban and rural asthma prevalence rates may mask significant differences in relevant allergen exposures and sensitivities.
Demographics
Age Asthma prevalence rates are highest in earliest childhood, declining to a low at around age 20 and then slowly increasing with age (Barbee et al., 1985; Mak et al., 1982). Between 5 and 14 percent of children will have a respiratory illness with wheezing at some time (Barbee et al., 1985). All wheezing in children is not asthma, however; an infectious disease, bronchiolitis, is also associated with wheezing.
Hospitalization rates for asthma vary with age. NCHS data (1992) indicate that from birth to age 14, 169,000 hospitalizations occurred due to asthma (30.8 hospitalizations per 10,000 population); from age 15 to 44, 86,000 hospitalizations occurred (19.1 per 10,000 population); from age 45 to 64, 86,000 occurred (18.2 per 10,000); and for age 65 and older, 102,000 occurred (32.4 per 10,000 population).
Gender Most studies report a greater prevalence of asthma among boys than among girls, usually by a ratio of 1.5–2 to 1. However, studies in Sweden, Finland, and Arizona have not demonstrated this predominance in males. The increased prevalence of asthma among boys does not appear to be related to genetic or familial factors (Sibbald et al., 1980), but it has been associated with males' greater predilection for infections, especially wheezing lower respiratory infections (Gregg, 1983). S. Weiss and colleagues (1992) report apparent sex differences in the relationship between asthma and lung function development, with males more likely to have asthma but with females experiencing a greater deficit in pulmonary function.
In adults over age 40, new cases of asthma are more likely to occur among women. If the asthma is associated with airflow obstruction (at the time of diagnosis or later), incidence is greater among adult males than among adult females (0.44 percent per year versus 0.39 percent per year; Lebowitz, 1989). Increased rates later in life reflect overlap with "wheezy bronchitis," which is most commonly due to smoking.
Race and Ethnic Group Several studies have reported racial differences in the prevalence and severity of asthma in the United States, but such results are inconsistent. Schwartz and colleagues (1990) reported an asthma prevalence rate of 7.2 percent among African American children compared with 3 percent among Caucasian children. For adolescents, prevalence is higher among Caucasians (5–6 percent) than among African Americans (3–4 percent); rates for Native Americans are close to zero, and rates among Asians are unknown (Barbee et al., 1985). A study of adults by Di Pede and coworkers (1991) found a prevalence of diagnosed asthma of 4.9 percent among Caucasians (non-Mexican Americans) and a prevalence of 0.9 percent among Mexican Americans. In the same study, Caucasians reported more respiratory symptoms (even within smoking groups) than Mexican Americans. The apparent difference in Caucasian/Mexican American rates may reflect cultural differences in reporting, since the lung function of the two groups is similar for comparable ages, heights, and genders.
Asthma mortality rates are significantly higher among African Americans than among Caucasians (NHLBI, 1991; Sly, 1988). Overall, the death rate from asthma rose from 1.2 per 100,000 population in 1979 to 1.5 in 1983 and 1984. Overall mortality rates among African Americans are two- to threefold higher than among Caucasians and fivefold higher among children. Between 1979 and 1984, the mortality rate rose from 1.8 to 2.5 per 100,000 population among African Americans and from 1.1 to 1.4 per 100,000 among Caucasians.
Socioeconomic Status Socioeconomic status seems to contribute significantly to asthma prevalence rates and to indices of disease severity. Studies have shown that asthma prevalence rates among children are inversely related to socioeconomic status and residential mobility and are directly related to crowding (Lebowitz, 1977, 1989). Schwartz and colleagues (1990) found that both residence in central cities and low income significantly contributed to asthma prevalence rates. Poverty has also been associated with increased hospitalizations for asthma (NHLBI, 1991). A study of inner-city children in the United States demonstrated a cumulative prevalence rate of asthma of 10.6 percent (Mak et al., 1982). (Inner-city asthma death rates in Chicago were two times greater than those for the United States; in New York City they were three times greater than those for the United States [Evans, 1992; K. B. Weiss et al., 1992a].) The criterion for diagnosis in that study was a positive response to the following question: Have you ever had a condition that causes difficulty in breathing, with wheezing noises in the chest?
Air Pollution Recent human challenge studies showed a twofold increased sensitivity to allergen in allergic asthmatics following a 1-hour exposure to ozone under conditions typical of summer smog (0.12 parts per
million [ppm], 1 hour, at rest; Molfino et al., 1991). However, ozone did not alter the acute response to nasal challenge with allergen when higher ozone exposure levels were used (0.5 ppm ozone, 4 hours, at rest; Bascom et al., 1990). Epidemiological studies point to a contribution by outdoor air pollution to asthma exacerbations. Bates and Sitzo (1987) related increased hospitalizations for asthma to increases in air pollution in the Toronto region. Other studies are well summarized in a recent chapter (Bresnitz and Rest, 1988). Prevalence rates of bronchial responsiveness were associated with specific indoor pollutant exposures only among groups of people of lower socioeconomic status (Quackenboss et al., 1989b).
In summary, asthma is a prevalent disease whose magnitude includes a significant socioeconomic component. Indoor allergens are important at all phases of the disease process, from sensitization to disease onset and severity and prognosis. There is evidence that environmental control strategies can affect the severity of the disease. Nonallergic factors may modify the role of allergens in the disease process.
ALLERGIC RHINITIS
Rhinitis is inflammation of the mucosa (surface cells) of the nose; it causes such symptoms as sneezing, runny nose (rhinorrhea), postnasal drip, and congestion. Allergic rhinitis ("hay fever") is rhinitis caused by IgE-mediated inflammation. The contribution of allergy to this condition is assessed through the individual's medical and environmental history and by skin testing or blood serology to seek specific IgE against suspected allergens.
Other types of rhinitis that can cause similar symptoms include nonallergic rhinitis, vasomotor rhinitis, and infectious rhinitis. These diagnoses are made by the physician on the basis of clinical presentation and are considered when skin testing fails to show evidence for an allergic cause of the rhinitis or when symptom patterns suggest other diagnoses.
Prevalence and Incidence
The prevalence rate of allergic rhinitis is 15–20 percent, although estimated prevalence rates range from 8 to 43 percent (Hagy and Settipane, 1969). Some evidence suggests that the prevalence of allergic rhinitis is rising (Barbee et al., 1987). Incidence rates are highly variable, and are considered untrustworthy at present. Absenteeism and other impacts have not been adequately assessed.
Risk Factors
Allergy A high degree of skin test reactivity to common allergens correlates well with the rate of allergic rhinitis in population studies (Burrows
et al., 1976). For example, in the study by Burrows et al. (1976), the fraction of the population with the lowest rate of skin test reactivity had a prevalence of allergic rhinitis of 2 percent; those with intermediate reactivity had a prevalence of 53 percent; and those with the highest skin test reactivity had an 89–100 percent prevalence of allergic rhinitis. In a study conducted in Tucson, allergic rhinitis was similar whether skin test reactivity was positive for perennial allergens (such as house dust mites) or seasonal allergens. Nationwide surveys—specifically, the National Health and Nutrition Examination Survey (NHANES)—also relate seasonal rhinitis symptoms to positive skin tests for seasonal allergens (Gergen and Turkeltaub, 1991). A similar relationship was not demonstrated with perennial rhinitis and dust allergy; however, the NHANES was limited because it did not use now-available allergen extracts that allow for improved sensitivity and specificity. Allergic rhinitis was independently associated with allergy to rye grass, ragweed, and house dust. Another nationwide survey is in progress using additional allergens.
A study in six U.S. cities (Brunekreef et al., 1989) found significant relationships between rates of hay fever and "mold" or "dampness" in homes (odds ratios of 1.57 and 1.26, respectively), although neither finding could be correlated with fungal counts (Su et al., 1989; 1990).
Age The prevalence of allergic rhinitis increases with age, up to the middle years, and then decreases. This same age-related pattern has been seen in studies with widely varying prevalence rates. For children, the National Health Interview Survey (NHIS) developed a prevalence rate of allergic rhinitis without asthma of 5.3 percent for those under age 18. A community-based study of non-Hispanic Caucasians in Tucson showed a prevalence of allergic rhinitis of 29.4 percent in children ages 3–14 (Lebowitz et al., 1975). Rates in other studies have been reported as between 3 and 19 percent (Arbeiter, 1967; Broder et al., 1962; Freeman and Johnson, 1964; Smith and Knowles, 1965). For adults, the NHIS study elicited a rate of 11.2 percent for ages 18–44, whereas the Tucson study found a prevalence of 42.6 percent in those over age 15. This rate was thought to be due in part to the migration of allergic subjects to Tucson. The NHIS study showed a prevalence of 9 percent for ages 45–64 and 5.2 percent for ages 65 and older (NCHS, 1986).
ECZEMA
Eczema (eczematous dermatitis) is a characteristic inflammatory response of the skin to multiple stimuli. There is usually a primary elicitor of the response (such as an allergen) after which many factors may contribute. The unifying feature of eczematous dermatitis is the occurrence of vesicular
eruptions, that is, small blisters within the rash. The initial diagnosis is based on the individual's history and the appearance of the skin; occasionally, skin biopsy is used.
Immunologic sensitization is the primary mechanism for two of the major types of eczema, atopic dermatitis and allergic contact dermatitis. These conditions are discussed below.
Atopic Dermatitis
Atopic dermatitis is associated with IgE allergy and, often, with a family history of atopy. The striking feature of the disease is severe, spasmodic itching; it results in "constant and vigorous rubbing, scratching, and even tearing and pounding which many of the tortured patients carry out by day and particularly by night, for periods of months to years" (Sulzberger, 1971, p. 687). The condition is diagnosed through the individual's medical history and physical examination and by identification of IgE allergy using skin tests for specific antibody in the sera.
Prevalence, Incidence, and Natural History Few estimates of prevalence exist for atopic dermatitis. Prevalence rates of 7.7 and 4.8 percent have been reported for children and adults, respectively (Lebowitz, 1975). The incidence of atopic dermatitis varies dramatically with age. Of all people with atopic dermatitis, 60 percent develop the condition before age 1; 30 percent develop it between ages 1 and 5; 10 percent develop it between ages 6 and 20. Of all people with atopic dermatitis, 58 percent have persistent disease for more than 15 years, but most heal by age 60 (NIAID, 1979).
Risk Factors The prevalence of eczema was not related to skin test reactivity in one population-based study (Burrows et al., 1976), but other studies have shown a relationship (Platts-Mills et al., 1991b). Infant eczema is related to cord blood IgE (Halonen et al., 1992).
Allergic Contact Dermatitis
Allergic contact dermatitis is a common skin condition unrelated to IgE allergy that is associated with the cellular immune response. The agents causing this disease are usually molecules that possess one or several reactive chemicals capable of forming stable bonds with tissue proteins and other tissue elements. The agent must penetrate the skin to induce the disease, and it is recognized that primary irritation of the skin favors sensitization.
The mechanism of this dermatitis is delayed-type hypersensitivity, which means that it is an allergic state that is not due to circulating antibodies but to specifically sensitized T-cells. The disease is diagnosed by patch testing, which consists of applying a small quantity of the suspected agent to the
surface of the skin and inspecting the site for inflammation 48–72 hours later.
The treatment of contact dermatitis follows three key principles: (1) continued contact with the specific allergen must be avoided by all means, (2) local irritation should be avoided, and (3) local therapy should be employed. (Steroid creams are generally prescribed, with oral steroids used in the most severe cases.)
Prevalence Contact dermatitis accounts for 20–30 percent of all patients treated in dermatology clinics. Seasonal factors such as the growth of poison ivy alter the rates of dermatitis cases. Most of the allergens associated with contact dermatitis are not aeroallergens; however, there have been instances in which airborne contact allergens have produced contact dermatitis.
Less Common Diseases Clearly Related to Allergy
Allergic bronchopulmonary aspergillosis, hypersensitivity pneumonitis, and humidifier fever are conditions that appear to be less common in the United States than the diseases discussed previously in this chapter. Nevertheless, they merit attention because of their potential severity.
ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS
Allergic bronchopulmonary aspergillosis (ABPA) is an intriguing condition characterized by the development of a specific immune response to the Aspergillus species of fungi that colonize the central airways. A related disease is allergic Aspergillus sinusitis. The diagnostic features of the disease include (1) asthma, (2) a history of infiltrates found by chest radiograph, (3) immediate skin test reactivity to Aspergillus, (4) elevated total serum IgE, (5) precipitating antibodies to Aspergillus fumigatus, (6) peripheral blood eosinophilia (expected at the time of radiographic infiltrates), (7) elevated serum IgE and IgG to A. fumigatus, and (8) proximal (central) bronchiectasis (Greenberger, 1988).
Prevalence
An estimated 10,000 cases of ABPA were prevalent in the United States in 1977; it is thought to be more common in the United Kingdom (NIAID, 1979). Approximately 25 percent of patients with asthma have IgE antibody to Aspergillus flavus, and 10 percent have IgG antibody; yet ABPA occurs in only 4 percent of Aspergillus skin test-positive individuals (Schwartz et al., 1978). ABPA also occurs in 10 percent of patients with cystic fibrosis (Greenberger, 1988).
HYPERSENSITIVITY PNEUMONITIS
Hypersensitivity pneumonitis is a specific immunologic lung disease characterized by inflammation of the lung parenchyma. The causative agents are numerous and diverse, and the immune pathogenesis includes formation of specific IgG antibody and formation of lung granulomas. The clinical spectrum is also diverse and ranges from recurrent, acute flu-like illnesses to a gradually increasing breathlessness. Hypersensitivity pneumonitis sometimes occurs in sporadic outbreaks, for example, when a building's ventilation system becomes contaminated. Diagnosis is often difficult because it requires a high index of suspicion, and the appropriate laboratory studies (i.e., precipitins) are sometimes unfamiliar to many physicians (see Chapter 5). Table 2-7 lists various causes of hypersensitivity pneumonitis that have been reported in nonindustrial indoor environments.
Prevalence
No prevalence rates are available for the general population. Clinical assessments of the type recommended by Solomon (1990) have not been utilized to obtain rate estimates or population impacts.
Disease Severity
In 1977, it was estimated that 2,000 hospitalizations occurred in the United States in which hypersensitivity pneumonitis was the primary (50 percent) or secondary (50 percent) diagnosis. Treatment consists of corticosteroid therapy and removal from exposure. Failure to institute these measures can result in disease or disability resulting from irreversible fibrosis and respiratory failure (EPA, 1991b).
Risk Factors
Indoor Environment Exposure to allergenic bioaerosols in residential or commercial heating, ventilation, and air-conditioning (HVAC) systems can cause hypersensitivity pneumonitis. Causative agents include thermophilic actinomycetes, Aspergillus species, Aureobasidium species, and other proteins.
Occupation/Hobby The risk of hypersensitivity pneumonitis increases markedly with exposure to allergens through hobbies and occupations, ranging from 0.5 to 10 percent of exposed populations. For example, the prevalence of hypersensitivity pneumonitis among pigeon breeders ranges from 6 to 15 percent (NIAID, 1979). Farmer's lung, a hypersensitivity pneumonitis that usually arises from exposure to thermophilic actinomycetes, probably occurs in 3–4 percent of exposed populations, with estimates ranging from 0.5 to 10 percent of farmers (NHLBI, 1982; NIAID, 1979). Occurrences among
TABLE 2-7 Hypersensitivity Pneumonitis in Indoor Environments
|
Disease |
Source of Antigen |
Probable Allergen |
|
Familial hypersensitivity pneumonitis |
Contaminated wood dust in walls |
Bacillus subtilis |
|
Humidifier lung |
Contaminated humidifiers, dehumidifiers, air conditioners |
Thermophilic actinomycetes: Micropolyspora faeni, T. candidus, T. vulgaris, Penicillium spp., Cephalosporium spp. Amebae: Naegleria gruberi and Acanthamoeba castellani |
|
Cephalosporium hypersensitivity pneumonitis |
Contaminated basement (sewage) |
Cephalosporium spp. |
|
Pigeon breeder's disease |
Pigeon droppings |
Altered pigeon serum |
|
Laboratory worker's hypersensitivity pneumonitis |
Rat fur |
Male rat urine |
|
Summer type hypersensitivity pneumonitis |
House dust |
Trichosporon cutaneum |
|
SOURCES: Fink, 1988; Lopez and Salvaggio, 1988; Rose, 1992. |
||
farmers have decreased markedly with changes in methods of harvesting and baling hay.
Other occupations also present opportunities for development of hypersensitivity pneumonitis. Office workers are estimated to develop hypersensitivity pneumonitis at rates of from 1.2 to 4 percent (EPA, 1991b). Banaszak and colleagues (1970) reported that 15 percent of workers in one office displayed pulmonary disease from thermophilic actinomycetes; their exposure had occurred through a contaminated air-conditioning system. Sauna takers disease (caused by Aureobasidium pullulans) occurs infrequently. However, lifeguards at an indoor swimming pool reportedly experienced an extremely high rate of attack of a hypersensitivity pneumonitis-like condition; the causative agent of the disease remains unidentified (Rose and King, 1992).
Climate/Season In Japan, 74 percent of the cases of hypersensitivity pneumonitis reported by hospitals (a total of 835 cases) were associated with predominantly hot, humid climates and occurred in the summer. These cases were attributed to Trichosporon cutaneum on the basis of detection of antibody in the blood.
Immunologic Sensitization In some studies, up to 20 percent of exposed populations will have IgG against the allergen in their serum. Because more than 90 percent of affected individuals will have a specific antibody, these individuals are thought to constitute a subset of the exposed population who are at increased risk of developing the disease. These general figures, however, may vary markedly across individual circumstances.
HUMIDIFIER FEVER
Humidifier fever is an illness with influenza-like symptoms that develops shortly after exposure to aerosols from microbiologically contaminated humidifiers. Recovery can occur within days, even with continuing exposure. It often recurs on the first day of reexposure following a period of no exposure.
Inhalation challenge with extracts from contaminated water can produce symptoms of humidifier fever, but the causative agent is still unknown. Experimental exposure of symptomatic workers to humidifier allergens can induce headache, rhinitis, and lethargy as well as asthma and alveolitis; similar exposure does not cause symptoms in previously unexposed individuals. These findings have led to a presumption that a specific immunologic mechanism is operative. A World Health Organization report, for example, listed endotoxin as the leading suspect (WHO, 1990). Finnegan and others (1987) identified allergens of amebae in contaminated humidifiers but failed to correlate their presence with humidifier fever or with work-related
symptoms in a group of 25 workers with humidifier fever and 90 workmate controls.
Prevalence
In general, published estimates are only educated guesses. The U.S. Environmental Protection Agency (EPA, 1991b) states that epidemics in the workplace are rare but that when they do occur, ''attack rates are high (30–75 percent)." Based on symptoms, Finnegan and coworkers (1984) estimated a rate of occurrence of 2–3 percent in Great Britain in office buildings with mechanical ventilation. Prevalence rates in the home, however, have not been evaluated (EPA, 1991b).
Common Diseases Possibly Related to Allergy
There are several syndromes in which a role for indoor allergens is possible or suspected but largely undefined. These include chronic sinusitis and bronchitis, sick building syndrome and other nonspecific syndromes, and acute respiratory illnesses.
SINUSITIS
Sinusitis is defined as inflammation of the sinuses, which are four pairs of hollow structures that surround the nasal cavity. Chronic sinusitis is defined by physicians as persistent inflammation of the mucosa of the sinuses lasting for more than 3 months (Slavin, 1989). Symptoms may include facial pressure, nasal stuffiness, hyposmia, prurulent nasal secretions, sore throat, fetid breath, and malaise. Coughing and wheezing occasionally occur.
Prevalence and Severity
Sinusitis is an important cause of morbidity (Slavin, 1989). In 1981, statistics from the U.S. Department of Health and Human Services indicated that 31 million people had chronic sinusitis; data from the National Center for Health Statistics (NCHS, 1986) are similar (13.9 percent, more than 30 million people). Sinusitis is thus more prevalent than arthritis (27 million) and hypertension (25.5 million). In Great Britain, the Department of Health and Social Security estimates that a half million working days are lost in that country each year due to sinusitis (Slavin, 1989).
In 1975, the rate of physician-confirmed sinusitis in Tucson adults was reported to be 29.4 percent (Lebowitz et al., 1975). The difference between this rate and the figures listed above does not reflect decreasing prevalence over time but rather variable case definitions.
Risk Factors
Age The prevalence of chronic sinusitis varies with age. According to estimates from the National Center for Health Statistics, it occurs in 6 percent of people under age 18, 16.4 percent of those between ages 18 and 44, 18.5 percent of those age 45–64, and 15.4 percent of those over age 65 (NCHS, 1986). A similar age pattern was reported in Tucson (Lebowitz et al., 1975).
Allergy Allergic rhinitis is considered a common risk factor for both acute and chronic sinusitis (Slavin, 1989), but the proportion of chronic sinusitis for which it is the dominant factor is unknown. The NHANES data, analyzed by Gergen and Turkeltaub (1992), did not show a relationship between reported sinusitis and skin test reactivity.
Nonallergic factors that predispose an individual to sinusitis are upper respiratory infection, overuse of topical decongestants, hypertrophied adenoids, deviated nasal septum, nasal polys, nasal tumors, foreign bodies, cigarette smoke, swimming and diving, barotrauma, and dental extractions. Immunodeficiency syndromes, cystic fibrosis, bronchiectasis, and the immotile cilia syndrome can also be associated with chronic sinusitis.
CHRONIC BRONCHITIS
Chronic bronchitis is commonly defined by clinicians as a chronic productive cough, without a medically discernible cause, that is present more than half the time for 2 years (Snider, 1988). Epidemiologists define chronic bronchitis more precisely as a cough productive of phlegm for a total of 3 months per year for at least 2 years in a patient in whom other causes of chronic cough have been excluded (e.g., infection with Mycobacterium tuberculosis, carcinoma of the lung, chronic congestive heart failure; Snider, 1988). The major risk factor for chronic bronchitis is cigarette smoking. The prevalence of chronic bronchitis among nonsmokers rises from age 15 to 60, increasing from 7 to 18 percent; prevalence among smokers rises from 40 to 82 percent (Snider, 1988).
Figure 2-10 illustrates the overlap between asthma, chronic bronchitis, and emphysema (Snider, 1988). Asthma, by definition, is characterized by reversible airflow obstruction, although a few patients may develop unremitting airflow obstruction. Patients with chronic bronchitis may have partially reversible airflow obstruction (Snider, 1988). The term chronic obstructive pulmonary disease (COPD) is often used by doctors when adult patients have evidence of one or more of three diseases: chronic bronchitis, emphysema, and asthma.
The nonproportional Venn diagram in Figure 2-10 shows subsets of patients with chronic bronchitis, emphysema, and asthma in three overlapping
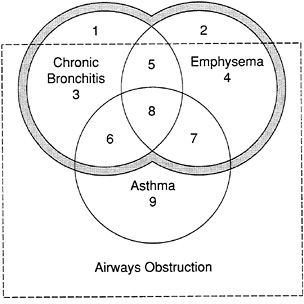
FIGURE 2-10 Relationship between asthma, chronic bronchitis, emphysema, and allergy. Numbers refer to subsets described in text.
Source: Snider, 1988.
circles. Subsets of patients lying within the rectangle have obstruction of their airways. Patients with asthma, subset 9, are defined as having completely reversible airways obstruction and lie entirely within the rectangle; their diagnosis is unequivocal. Patients in subsets 6 and 7 have reversible airways obstruction with chronic productive cough or emphysema, respectively. Patients in subset 8 have features of all three disorders. It may be difficult to be certain whether patients in subsets 6 and 8 indeed have asthma or whether they have developed bronchial hyperreactivity as a complication of chronic bronchitis or emphysema; the history helps. Patients in subset 3 have chronic productive cough with airways obstruction but no emphysema; it is not known how large this subset is, since data from epidemiologic studies using the computer tomography scan, the most sensitive in vivo imaging technique for diagnosing or excluding emphysema, are not available. It is much easier to identify in the chest radiography patients with emphysema who do not have chronic bronchitis (subset 4). Most patients in subsets 1 and 2 do not have airways obstruction as determined by the FEV1 (forced expiratory volume exhaled in 1 second) but have clinical or radiographic features of chronic bronchitis or emphysema, respectively. Because COPD, when defined as a process, does not have airways obstruction as a defining characteristic, and because pure asthma is not included in the term COPD, patient subsets 1–8 are included within the area outlined by the shaded band that denotes COPD (Snider, 1988).
There is a recognized association between bronchial hyperresponsiveness, atopy (skin test reactivity), and COPD. Studies have demonstrated that the risk of bronchial hyperresponsiveness is related to skin test reactivity (Cockroft et al., 1984; Lebowitz et al., 1991, Peat et al., 1987; Sears et al., 1989). The index rises with the number of positive skin tests and the magnitude of the skin test reaction to each allergen. Therefore, an individual with many strongly positive skin tests to many allergens is much more likely to show bronchial hyperresponsiveness than an individual with no skin test reactivity. The association between atopy, bronchial hyperresponsiveness, and COPD may be explained by three alternative models (Sparrow et al., 1988). First, cigarette smoke may cause inflammation and mucosal damage, resulting in three unrelated by-products: atopy, bronchial hyperresponsiveness, and COPD. Second, when a person has atopy and therefore bronchial hyperresponsiveness, exposure to cigarette smoke leads to COPD. Third, cigarette smoke, atopy, and bronchial hyperresponsiveness are independent factors that contribute to the development of COPD.
SICK BUILDING SYNDROME
Sick building syndrome (also known as tight building syndrome, closed building syndrome, and new building syndrome) is a term given to nonspecific building-related illness. Figure 2-11 shows the relationship between these and other diseases and conditions that may occur in indoor environments and the general approach to their evaluation and management. Sick building syndrome describes a constellation of symptoms including mucosal irritation, fatigue, headache, and occasionally, lower respiratory symptoms and nausea. Patients or workers report that symptoms increase with the amount of time spent in certain buildings and tend to improve when they leave that building. Symptom prevalence rates associated with indoor environments vary tremendously, from less than 5 percent to as much as 50 percent.
For the majority of cases of sick building syndrome, the cause is unknown. A contribution by allergy has been considered unlikely since atopy or specific sensitivity to indoor allergens often is not found. Nevertheless, people with allergic disease frequently are the individuals who are most affected when an indoor air quality problem is occurring. A definitive conclusion that indoor allergens are not related to sick building syndrome awaits further study, particularly with respect to fungal allergens.
SPECIFIC BUILDING-RELATED ILLNESS
Specific building-related illness is defined as illness caused by identifiable toxic, infectious, or allergenic agents, which can be detected by appropriate
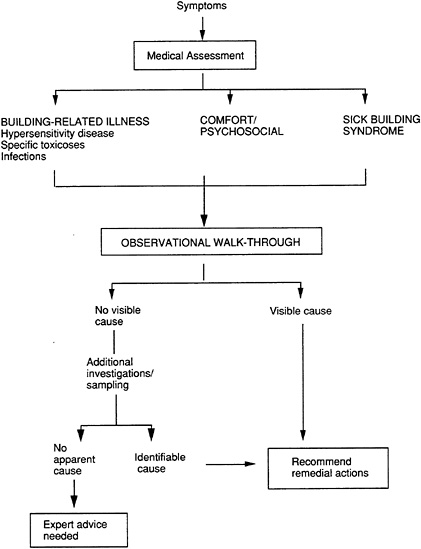
FIGURE 2-11 Approach to the evaluation of symptoms occurring in indoor environments.
clinical laboratory tests in patients or by identification of the source in the building (Samet, 1990). Hypersensitivity pneumonitis, humidifier fever (see above), and infection with Legionella species are included in this category of illness. Prevalence rates for specific syndromes are largely unknown and estimates vary tremendously among buildings.
Some researchers believe that there is a set of nonspecific symptoms that are distinguishable, that are different from the other conditions described above, and that are due to indoor allergens (Burge, 1990). Fungus-related
illnesses, for example, have been identified or suggested in some instances (Anderson and Korsgaard, 1986; Finnegan et al., 1984; Morey, 1988). Further information can be obtained from a review and an editorial by Kreiss (1988, 1990).
ACUTE RESPIRATORY ILLNESSES
Assessments of disease magnitude often depend on a subject's recalling the occurrence of a disease and recognizing its relationship to allergy. For example, questionnaires will ask, "Have you had hay fever?" For an affirmative answer, the subject must recognize that his or her recurrent nasal symptoms are in fact due to an allergic nasal condition. Diary studies, that ask subjects to record symptoms on a daily basis, are another way of assessing the burden of respiratory symptoms in the population. In general, they suggest that respiratory symptoms are quite common, more so than recall studies would indicate. In a diary study of Manhattan (New York) residents, it was determined that the rates of symptoms were much greater when diaries were used than when subjects were asked to recall their health status over the past several years (Lebowitz et al., 1972a,b). The study of 1,707 residents assessed respiratory symptoms for 1,168 person-years of observation. One or more symptoms occurred at least one-quarter of the time among 22 percent of subjects in the study and at least half the time among 6.5 percent. The symptoms that were most often reported included common cold and rhinitis (8 percent of all person-days each), cough (5 percent), headache (2.45 percent), eye irritation (1.8 percent), and chest whistling/wheezing (0.77 percent). The investigator in this study has speculated that reported colds and other infections could have been mislabeled and that an unknown portion of these symptoms could be attributable to allergic diseases.
Data from the NHIS (NCHS, 1986) indicate that in 1985 there were 87.1 acute respiratory conditions per 100 persons. Of these, 46.4 percent were categorized as influenza, 35 percent as common colds, and 11.7 percent as other acute respiratory illnesses. The remainder were labeled as acute bronchitis (3 percent), pneumonia (1 percent), and other (2 percent).
CONCLUSIONS AND RECOMMENDATIONS
As outlined in this chapter, allergic disease constitutes a substantial public health problem in the United States. Data on its exact magnitude and dimensions, however, are incomplete, or lacking, in many cases. Better data regarding the incidence, prevalence, attributable fraction, and cost of allergic diseases are essential to the development of effective programs of prevention and control. Accurate determinations of the magnitude and dimensions
of sensitization and disease caused by regional and local indoor allergens would be useful in this regard. The following recommendations for research and data collection will be useful in accurately determining the magnitude and dimensions of sensitization and disease caused by indoor allergens.
Research Agenda Item: Determine prevalence rates of sensitization, allergic diseases, and respiratory morbidity caused by regionally and locally relevant indoor allergens and assess the contributions of different allergens to these conditions.
Socioeconomic status seems to contribute to asthma prevalence rates and to indices of disease severity. Similarly, several studies have reported racial differences in the prevalence and severity of asthma in the United States, but such results are inconsistent. In order that these differentials can be translated into effectively targeted public health interventions, additional research is needed to clarify these relationships.
Research Agenda Item: Conduct studies to clarify the relationships that exist between socio- economic status, race, and cultural environment and the incidence, prevalence, severity, and mortality associated with allergic disease including asthma.
The annual costs (direct and indirect) associated with asthma have been estimated at more than $6.2 billion—an increase of 39 percent since 1985. The size of these costs and the trend towards even greater costs argue for careful attention not only to the effects of allergy in causing asthma but also to the litany of other conditions that are more commonly thought to be associated with "allergies." Accurate assessments of the costs associated with asthma and other allergic diseases would be useful in the development of health policy initiatives and the implementation of appropriate and cost effective interventions.
Research Agenda Item: Determine the economic impact of asthma and other allergic diseases.
Allergic disease occurs when a genetically predisposed or susceptible individual is exposed to an allergen and becomes immunologically sensitized. In the early stages of sensitization, people who are sensitized have not developed symptoms of disease. The magnitude of this group within the population is of interest, however, because it reflects the proportion of the population at greatest risk of developing allergic disease. Additional exposure to the sensitizing allergen leads to the development of an allergic reaction (disease) that can be mild, moderate, or severe, depending on the amount of exposure.
The relationship between exposure, sensitization, and disease, and the
potential for a threshold level of exposure below which the risk of sensitization is reduced, is of critical importance in the prevention and control of allergic disease. Epidemiological data would be useful in determining these relationships and in developing and evaluating public health and medical intervention strategies.
Research Agenda Item: Conduct appropriate epidemiological studies of exposure-response relationships of important defined indoor allergens that induce sensitization in humans. Such studies should include a focus on identifying threshold exposures.
Indoor allergens are associated with a wide variety of particles in a broad size range, only some of which are microscopically identifiable, culturable, or detectable with existing immunoassays. Evaluation of indoor allergens requires both air and source sampling, and several different analytical techniques (including microscopy, culture, and immunoassays) must be used to characterize even the well-known allergens. Because of the complexity of the assessment problem, indoor allergens, with a few exceptions, have not been identified and studied.
Research Agenda Item: Encourage and conduct additional research to identify and characterize indoor allergens. The new information should be used to advise patients about avoiding specific allergenic agents.