7
Illustrative Preventive Intervention Research Programs
Although preventive intervention research is still a relatively young field and formidable tasks lie ahead, the past decade has brought encouraging progress. At present, there are many intervention programs that rest on sound conceptual and empirical foundations, and a substantial number are rigorously designed and evaluated. From a mental health perspective, these interventions are consistent with—even though they do not prove—the hypothesis that serious psychological problems can be avoided by preventive action before the onset of a diagnosable disorder.
In this chapter the committee selects a limited number of these interventions to illustrate a range of promising program approaches to achieving diverse prevention goals. This review of preventive interventions is based on three principles presented in earlier chapters in this report: (1) Prevention of the initial onset of mental disorders can be accomplished through intervention programs aimed at risk reduction, which can include both reduction of causal risk factors and enhancement of protective factors. The goal is to address malleable, or modifiable, risk and protective factors related to the onset of disorders, including precursor symptoms, to reduce the incidence of mental disorders or at least to delay their onset. However, even if the interventions fail to prevent a disorder, they may have some effect on reducing the severity or duration of the disorder. (2) Preventive intervention programs can be successfully implemented at all three levels—universal, selective, and indicated—described in Chapter 2. (3) Preventive intervention programs can be initiated throughout the life span.
The committee-reviewed numerous prevention programs that were supported by federal agencies and private foundations. A wide net was cast in soliciting nominations, but the search could not be exhaustive. A majority of the prevention programs that currently exist are service programs and demonstrations that have not incorporated rigorous research methodologies. Even those that have an evaluation component usually have not used rigorous standards for assessment of effectiveness. Thus the nation is spending billions of dollars on programs whose effectiveness is not known. Most of the prevention programs discussed in this chapter meet the criteria listed below, including the use of a randomized controlled trial design. Such a high standard lends credence to the results of these studies. These program illustrations demonstrate that rigorous protocols can be applied to complex interventions, yielding tangible outcomes.
Many of the prevention programs that were reviewed used quasi-experimental designs. Where their findings provide some confirmatory evidence for a study with a randomized controlled trial design, or where their findings provide new leads in areas where there have been no randomized controlled studies, the information is briefly discussed in the chapter. Also, three well-known service projects that have not been rigorously evaluated are presented to highlight the potential for applying experimental designs to preventive interventions created by practitioners. All prevention program titles are in italics. Titles of programs that met the criteria for use as full illustrations are preceded by an asterisk. These illustrative programs are also listed in Table 7.1 and are abstracted in more detail in the background materials (program abstracts are available as indicated in Appendix D).
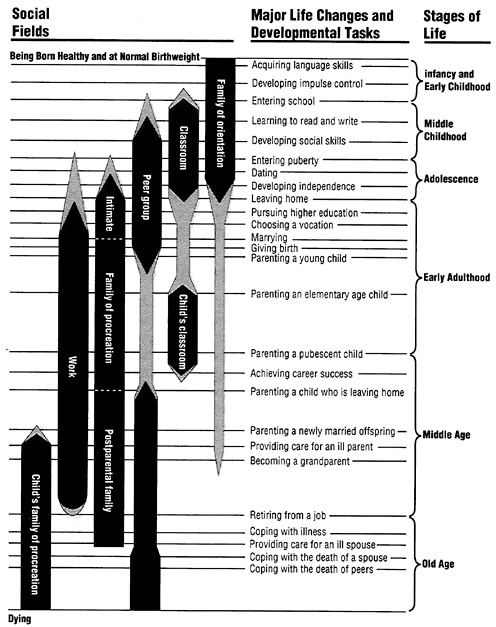
The programs target different age groups and are arranged here in developmental sequence from gestation through old age. As individuals move from one stage to the next, the developmental tasks facing them change, as does the nature of the risk and protective factors. This life course presentation serves to emphasize the importance of continuity and integration of interventions across the entire life span. Prevention programs that lasted for several years and bridged successive developmental phases or had effects on more than one generation are presented in this chapter at the earliest developmental phase. At the end of each section, several findings and leads that emerged from the review of programs addressing that age group are listed. The order of the points does not imply priority, and the list is not meant to be comprehensive but rather to illustrate the sorts of patterns, problems, and directions for future work that can be learned from such a perspective.
CRITERIA FOR EXAMINING PREVENTIVE INTERVENTION PROGRAMS DESCRIBED IN THE LITERATURE
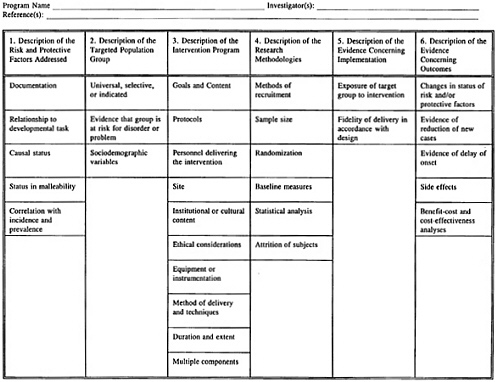
As a basis for selecting the illustrative preventive intervention research programs, the committee formulated six criteria. The criteria pertain to (1) the risk and protective factors addressed, (2) the targeted population group, (3) the intervention itself, (4) the research design, (5) evidence concerning the implementation, and (6) evidence concerning the outcomes. Each of these criteria is described in detail below. In addition, Figure 7.1 displays these criteria in a format that may be useful to the reader in future examinations of published prevention programs.
Description of the Risk and Protective Factors Addressed
A well-documented description of the risk and protective factors addressed in the preventive intervention and how they relate to developmental tasks of the targeted group is a critical scientific first step. Without such specification, the rationale for identifying any group for intervention will be difficult to provide. Furthermore, the accumulation of data about well-documented risk and protective factors is essential to the design of preventive interventions, and the identification of malleable, or modifiable, risk factors is crucial to the success of prevention efforts built on the risk reduction model.
In identifying risk and protective factors, the causal status of the risk or protective factor is crucial. Some risk factors may not be causal but are nevertheless useful for identifying and targeting high-risk populations. The risk factors used to target the population may not always be the risk factors that one is attempting to modify through an intervention.
Although definitive scientific evidence of the causal role that a risk or protective factor plays in the development of mental disorder is seldom available until an intervention is tried, certain critical pieces of evidence should be in place. For example, there should be epidemiological evidence to suggest that the risk or protective factor is statistically correlated with the incidence or prevalence of the disorder itself. Furthermore, evidence that the risk or protective factor precedes the disorder is an important indication that the factor has at least a potential role in causation. Also, there may be a dosage effect, that is, the stronger the risk factor, the more disorder. In addition, the mechanism or process through which the risk or protective factor potentially operates should be specified. For example, a protective factor may affect risk either directly by operating on the antecedent risk factor itself or indirectly by affecting the strength of the relationship between the risk factor and
some mental health outcome. A protective factor may also operate by affecting some mediating mechanism that stands causally between the risk factor and the development of mental disorder.
Ultimately, it is important that the risk and protective factors addressed in the prevention program be explicitly identified and established as risk and protective factors in rigorous scientific studies. As scientific evidence converges on particular sets of risk and protective factors, interventions addressing them become more plausible and more likely to succeed.
Description of the Targeted Population Group
A description of the characteristics of the targeted group is another critical ingredient. As described in Chapter 2, universal preventive interventions are provided to entire populations; selective preventive interventions are targeted toward groups or individuals with high lifetime or high imminent risk; and indicated preventive interventions are targeted toward high-risk individuals on the basis of the individual's minimal, but detectable, behavioral symptoms that could later develop into a full-blown mental disorder, or the individual's biological markers that identify him or her as being at especially high risk.
Because our knowledge of precursor signs and symptoms of mental disorders is only preliminary (for example, no standardized lists of these exist), it is often difficult in practice to distinguish between selective and indicated interventions. We are just beginning to understand which risk factors contribute in a general way to multiple disorders and which are actually precursor symptoms for a single disorder. For example, in the causal chain leading to conduct disorder, aggressive behaviors at ages 4 to 6 are stable predictors of later problems and could be used to trigger an indicated intervention. Farther along the chain, at ages 9 to 11, academic difficulties also begin to stabilize as predictors of later conduct disorder and substance abuse. At this point the academic problems are not just a general risk factor for multiple disorders; they are also a precursor symptom for conduct disorder and can also be used to target an indicated population. The committee believes that the exercise in distinguishing between selective and indicated targeted populations is a useful one—and has attempted to do it for the illustrations given here—for it allows us to see more clearly where past efforts have been directed and how successful they have been. In addition, the distinction provides clues as to what degree of specification of targeted group tends to produce the best outcomes.
Specifying the targeted group is important for evaluating the degree
to which the group actually displays the purported risk factors, for evaluating the actual and potential impact of the intervention, and for replicating the intervention. For example, scientific evidence should be provided to indicate that the group targeted actually is a group at risk for a particular disorder, cluster of disorders, or problem, and, if known, the degree to which the group is at risk should also be provided.
The targeted group should be described not only in terms of its risk and protective factors but also in terms of a combination of sociodemographic variables, including such characteristics as gender, age, race, socioeconomic status, living conditions, exposure to major life transitions, and family configuration. The number of participants and the distribution of sociodemographic characteristics in various experimental and control conditions should also be specified. Finally, because of potential effects on outcomes, there should be a description of the recruitment process and the consent process.
Description of the Intervention Program
All too often, treatment interventions as well as preventive interventions lack adequate description. This lack of specification is sometimes due to restrictions imposed by journal publication formats. In other cases, adequate descriptions of intervention protocols, including documents such as intervention manuals and training programs for delivery of the intervention, are simply missing. This is a danger signal, impeding evaluation.
Adequate descriptions of the goals and content of the intervention, and of the personnel delivering the intervention, including their professional qualifications and/or training for the delivery of the intervention, are needed. Detailed descriptions of the intervention site, including information on physical surroundings; the institutional and cultural context; special ethical considerations; and special physical aspects of the environment, including equipment or instrumentation, are other elements.
The actual methods of delivery must also be described, including the use of any special techniques, such as media devices and learning exercises. In addition, there must be a clear indication of the duration and extent of the intervention, including the prescribed length of exposure to the intervention by individuals or groups, whether booster sessions after the main intervention are required, and if so, at what intervals.
Finally, many preventive interventions have multiple components that are designed to work in an additive, sequential, or interactive
fashion. Each of the components, modules, or stages ought to be described in enough detail that replication is possible.
Description of the Research Methodologies
The choice of research methodologies is a major issue in examining preventive interventions and the research trials designed to determine their outcomes. It heavily determines whether evidence is compelling that a preventive intervention could have produced its intended effect.
The ideal research design in a preventive trial is a randomized controlled trial of adequate size embedded in a longitudinal study. However, a variety of other designs, including group comparisons such as pretest-posttest, and quasi-experimental designs such as interrupted time series and regression discontinuity, are often employed. Such designs may be particularly necessary for large-scale community interventions. Although such designs have the potential for yielding useful data, they are less desirable than true randomized experimental designs. Such designs also require detailed descriptions of comparison groups, including methods of recruitment and any other information that might allow evaluation of comparison groups.
The research design should include appropriate use of statistical methods and account for attrition of participants through appropriate use of weighting procedures, statistical modeling of attrition effects, or the conservative use of full randomized designs even where attrition has taken place (Kraemer, 1992; Cohen, 1988; see also commissioned paper by Kraemer and Kraemer in the background materials, available as indicated in Appendix D).
Even when randomized assignment is possible, attrition is still a threat. It is frequently still necessary to confirm that randomized assignment has had its intended effects by comparing experimental and control groups on sociodemographic characteristics and other characteristics in addition to the outcomes. Furthermore, designs that employ appropriate and sufficient baseline measures, such as data on intelligence, personality, and physical health, are highly desirable because variables that appear extraneous are potentially significant. Inclusion of such measures has become standard practice for the evaluation of most randomized trials.
Description of the Evidence Concerning the Implementation
How well the intended objectives and processes of the intervention were actually implemented needs to be examined even when an
adequate, detailed description of the intervention program is available. The critical issue is whether the intervention was delivered in accordance with its design. It is important to assess the degree to which targeted participants actually were exposed to the intervention and, wherever possible, the degree to which there were variations in exposure or dosage. The degree to which the intervention was delivered with fidelity can be determined if evidence is provided through various program data collected by external observers, through detailed program archives documenting contacts with participants, or through knowledge obtained from participants who were targets of the intervention.
Description of the Evidence Concerning the Outcomes
The final element to be examined is the outcomes. Most fundamentally, evidence should be provided that risk or protective factors have been changed. Without at least preliminary evidence that the intervention was successful in reducing risk factors or increasing protective factors, or in showing that protective factors reduced the strength of the relationship between risk factors and outcomes or affected some hypothesized mediating process, the claim that the intervention had an effect on some aspect of the causal chain leading to disorder becomes less convincing.
Other obvious sources of evidence of preventive effects would be an actual reduction in the observed rate of new cases of disorder or a delayed onset of disorder in the experimental group. It is entirely possible for a trial to provide evidence that the incidence of a particular disorder was reduced or the onset was delayed without clearly showing the mechanism of action by which the effect occurred. Accordingly, trials should, if possible, identify evidence not only on rates and age of onset of disorder but also on effects on risk or protective factors.
Still other outcomes are important to assess. These include the identification of unanticipated side effects, data regarding the costs and benefits of the intervention, and any benefit-cost or cost-effectiveness analyses conducted as part of the intervention evaluation. However, information on side effects and benefits and costs rarely has been included in published reports. Increasingly, it should become a standard part of the evidence on outcomes.
A DEVELOPMENTAL PERSPECTIVE
With these criteria in mind, the committee reviewed the preventive intervention research using, as an organizing conceptual framework, an
understanding of human development throughout the life span. As mentioned above, each developmental phase brings new tasks to be accomplished; each is accompanied by potential biopsychosocial risk factors as well as opportunities for growth. Just as each individual is continually changing and evolving, risk and protective factors emerge and disappear over time or, if present for a long time, may express themselves differently. Likewise, outcome variables may need to vary through developmental stages. Figure 7.2 illustrates the conceptual framework of the life course of human development, with developmental tasks and corresponding social relationships and settings, such as family of orientation and peer group, which are the appropriate targets and contexts for preventive interventions. (See Table 7.1 for a summary of research programs corresponding to this life course framework.)
INTERVENTIONS FOR INFANTS
In infancy, the biopsychosocial risk factors that can hinder development include, but are not limited to, preventable infections, disease, or injuries that can cause brain damage, neurodevelopmental disorders, or behavioral disorders; problems of parent-infant attachment or parenting; deprivation of cognitive and language stimulation; economic deprivation; and child maltreatment. The corresponding protective factors of robust health and “good-enough” parenting—coupled with adequate nutrition and shelter—encourage the physical, intellectual, and emotional growth of the child.
In recent years, there have been notable increases in infants and children at risk for developmental impairments, and in infants and children already showing such problems (Rickel and Allen, 1987). Unemployment, deteriorating neighborhoods, increased violence, and lack of access to medical care have all contributed to this problem (see Chapter 6 on risk and protective factors). The Center for the Study of Social Policy (1992) concluded that our nation has failed to keep pace with the needs of its youngest citizens: over the 1980s child poverty expanded, births to unmarried teens climbed, more children were living in families with only one parent, and more babies were being born at risk because they were underweight.
Although the larger societal and structural issues will require societal and macroeconomic solutions, a number of creative and comprehensive programs have shown that it is possible to address the adverse effects on mothers and children of the heightened risks caused by these social changes. Preventive intervention strategies that have been used during infancy to target babies and their parents include high-quality prenatal
and perinatal care, childhood immunization, regular home visitation, parenting education, promotion of healthy parent-infant interaction, appropriate cognitive and language stimulation, well-baby health care, family support, and center-based infant day care.
Physical Health Interventions with Applications to Mental Health
High-Quality Prenatal and Perinatal Care
Prenatal and perinatal care provide examples of universal preventive interventions directed at the entire population of pregnant women for the protection of the developing fetus and the newborn baby. There is a strong general health promotion and wellness aspect to prenatal care, but such care is also known to prevent prematurity and low birthweight, as well as specific disabilities and disorders in newborns.
There is general agreement that all pregnant women should receive early, regular, and comprehensive prenatal care. In Healthy People 2000: National Health Promotion and Disease Prevention Objectives (DHHS, 1991), the U.S. Public Health Service affirmed that ensuring all infants a healthy start in life and enhancing the health of their mothers must be a top priority in the 1990s if we are to ensure the future health of the nation. Despite this consensus, however, there continue to be large numbers of women in the United States who do not receive prenatal care. Teenage mothers, mothers who are members of disadvantaged minorities, and unmarried mothers all tend to receive prenatal care that is late or inadequate, or they receive no prenatal care at all (IOM, 1985). Well-established medical guidelines define the timing and protocol for appropriate prenatal care, but frequently these are not followed for these high-risk groups (IOM, 1985).
Lack of prenatal care has important implications for mental disorders. Inadequate or absent prenatal care is the main cause of a mixed group of preventable disorders that appear in low-birthweight babies. In the United States, there are disproportionately high rates of low-birthweight babies in some racial and ethnic groups, particularly among African-Americans (Center for the Study of Social Policy, 1992). Low-birthweight babies constitute about 60 percent of all infant deaths. Those babies that survive often do so with major lifelong disorders, such as mental retardation and cerebral palsy, as well as behavioral, emotional, and learning problems (IOM, 1985). There is also some preliminary limited evidence that pregnancy and birth complications may play a role in later development of schizophrenia (see Chapter 6). Improving prenatal and perinatal care and delivering this care to all pregnant
TABLE 7.1 Illustrative Preventive Intervention Programs Using Randomized Controlled Trial Design
|
Targeted Population Group/Sample Size When Project Began |
Risk Factors Addressed |
Outcomes (for total intervention group or subgroups) |
Principal Investigator(s) and Year(s) |
|
|
Infants |
||||
|
Prenatal/Early Infancy Project |
Selective/N=394 |
Economic deprivation, maternal prenatal health and damaging behaviors, poor family management practices |
Improved maternal diet and reduced smoking during pregnancy, fewer preterm deliveries, higher-birthweight babies, less child abuse |
Olds, 1988, 1986 |
|
Tactile/Kinesthetic Stimulation |
Selective/N=40 |
Preterm delivery, low birthweight |
Better physical and mental development of infants |
Field, 1986 |
|
Early Intervention for Preterm Infants |
Selective/N=60 |
Teenage parenthood, low socioeconomic status, preterm delivery |
Better parenting behaviors and attitudes of mothers, better cognitive competence, better physical development, better temperament of infants |
Field, 1980 |
|
Infant Health and Development Program |
Selective/N=985 |
Low birthweight, poor family management practices, academic failure, early behavior problems |
Better cognitive competence, fewer behavior problems |
Ramey, 1990 |
|
Carolina Abecedarian Project |
Selective/N=107 |
Academic failure, lack of readiness for school, economic deprivation, low commitment to school |
Better cognitive competence, lower rates of retention in grade in school |
Horacek and Ramey, 1987 |
|
Solving Program |
||||
|
Houston Parent-Child Development Center |
Selective/N=~700 |
Economic deprivation, academic failure, early behavior problems, poor family management practices |
Better family management practices, fewer behavior problems |
Johnson, 1991, 1990 |
|
Mother-Child Home Program of Verbal Interaction Project |
Selective/N=156 |
Academic failure, economic deprivation, poor family management practices, early behavior problems |
Better family management practices, better cognitive competence |
Levenstein, 1992, 1984 |
|
Parent-Child Interaction Training |
Indicated/N=105 |
Economic deprivation, early behavior problems, poor family management practices, depressive Solving Program symptoms |
Lower rates of attention deficits and conduct problems |
Strayhorn, 1991 |
|
High/Scope Preschool Curriculum Comparison Study (including Distar) |
Selective/N=68 |
Academic failure, early behavior problems, economic deprivation |
Better cognitive competence |
Weikart and Schweinhart, 1992, 1986 |
|
Perry Preschool Program (using high/Scope curriculum) |
Selective/N=123 |
Academic failure, economic deprivation, early behavior problems, low commitment to school |
Better cognitive competence, greater achievement and school completion, better vocational outcomes, fewer conduct problems and arrests |
Weikart and Schweinhart, 1987, 1984 |
|
I Can Problem Solve: Interpersonal Cognitive Problem-Solving Program |
Selective/N=219 (N=60 in pilot study) |
Economic deprivation, poor impulse control, early behavior problems |
Better cognitive problem-solving skills, fewer behavior problems |
Shure and Spivack, 1982, 1979 |
|
Elementary-Age Children |
||||
|
Assertiveness Training Program (program 1) |
Universal/N=343 |
Early behavior problems, academic failure |
Improved social assertiveness, improved academic performance |
Rotheram, 1982 |
|
Assertiveness Training Program (program 2) |
Indicated/N=101 |
Early behavior problems, academic failure |
More assertive behavior, better school achievement, fewer behavior problems |
Rotheram, 1982 |
|
Children of Divorce Intervention Program |
Selective/N=75 |
Marital conflict and separation, early conduct problems |
Lower anxiety, fewer learning problems, better adjustment |
Pedro-Carroll and Cowen, 1989, 1986, 1985 |
|
Family Bereavement Program |
Selective/N=72 |
Child bereavement, poor family management practices, early behavior problems |
Lower levels of symptoms of depression and conduct disorder |
Sandler, 1992 |
|
Social Skills Training |
Selective/N=28 |
Peer rejection, early conduct problems |
Less peer rejection, better interpersonal skills |
Bierman, 1986 |
|
Social Relations Intervention Program |
Indicated/N=86 |
Early behavior problems (aggression), peer rejection, impulsivity |
Less aggression, less peer rejection, more prosocial behavior |
Lochman, in press |
|
Montreal Longitudinal-Experimental Study |
Indicated/N=172 |
Poor family management practices, peer rejection, academic failure, early behavior problems, violence on television |
Less aggressive behavior, less delinquent behavior, better school achievement |
Tremblay, 1992, 1991 |
|
Community Epidemiological Preventive Intervention: Mastery Learning and Good Behavior Game |
Universal/N=2314 |
Academic failure, aggressive and antisocial behavior, concentration problems, depressive symptoms, shy behavior |
Less aggressive and shy behavior, better cognitive competence—especially among those with early depressive symptoms |
Kellam and Rebock, 1992 |
|
Academic Tutoring and Social Skills Training |
Selective/N=40 |
Academic failure, peer rejection, early behavior problems, early depressive symptoms |
Better cognitive competence, less peer rejection |
Coie and Krehbiel, 1984 |
|
Seattle Social Development Project |
Universal/N=908 |
Poor family management practices, early behavior problems, low commitment to school, academic failure |
Better family management practices and family bonding, greater attachment to school, lower rates of delinquency and drug use initiation |
Hawkins and Catalano, 1988 |
|
Adolescents |
||||
|
Changing Teaching Practices |
Selective/N=1166 |
Low commitment to education, academic failure, behavior problems |
Greater attachment and commitment to school, lower rates of school suspension for misbehavior |
Hawkins, 1988 |
|
Positive Youth Development Program |
Universal/N=282 |
Early drug use onset, favorable attitudes toward drugs, social influences to use |
Better coping skills, better stress management strategies, better conflict resolution and impulse control, less excessive alcohol use |
Caplan and Weissberg, 1992 |
|
Adolescent Alcohol Prevention Trial |
Universal/N=3011 |
Attitudes favorable to the use of drugs, social influences to use, early onset of drug use |
Lower rates of tobacco, alcohol, and marijuana use, lower prevalence of problem alcohol use and drunkenness |
Hansen and Graham, 1991 |
|
ALERT Drug Prevention |
Universal/N=6527 |
Social influences to use, early onset of drug use, attitudes favorable to the use of drugs |
Lower rates of tobacco, alcohol, and marijuana use |
Ellickson and Bell, 1990 |
|
Alcohol Education Project |
Universal/N=2536 |
Favorable attitudes toward alcohol consumption, early onset of alcohol use, association with alcohol-consuming friends, community norms favorable toward alcohol use |
Less initiation of alcohol use, increased knowledge about alcohol, decreased use among those drinking prior to study |
Perry et al., 1989 |
|
Midwestern Prevention Project |
Universal/N=5065 |
Social influences to use, early onset of drug use, attitudes favorable to the use of drugs |
Lower rates of tobacco, alcohol, and marijuana use |
Pentz, 1989 |
|
Behaviorally Based Preventive Intervention |
Indicated/N=80 |
Academic failure, early behavior problems, alienation from family, low commitment to school |
Less conduct problems and delinquency |
Bry, 1992 |
|
Intervention Campaign Against Bully-Victim Problems |
Universal/N=2400 |
Aggressive behavior, poor family management practices, favorable attitudes toward bullying/aggression |
Less bullying, less delinquent behavior, more attachment to school |
Olweus, 1991 |
|
Adults |
||||
|
Prevention and Relationship Enhancement Program (PREP):An Empirically Based Preventive Intervention Program for Couples |
Universal/N=135 |
Couple relationship problems |
Better marital adjustment, less divorce, less physical violence |
Markman, 1992 |
|
University of Colorado Separation and Divorce Program |
Selective/N=153 |
Marital separation/divorce, anxiety, depression, childrearing problems, economic problems |
Fewer symptoms of anxiety and depression, better vocational outcomes |
Bloom and Hodges, 1985, 1982 |
|
Perceived Personal Control Preventive Intervention for a Caesarean Birth Population |
Selective/N=70 |
Caesarean delivery, depressive symptoms |
Lower levels of postpartum depression, more rapid physical and psychological recovery |
Tadmor and Brandes, 1988, 1984 |
|
Prenatal/Early Infancy Project |
Selective/N=394 |
Single parent status, school dropout, economic hardships, joblessness, subsequent pregnancy |
Better vocational adjustment, fewer second pregnancies, better educational achievement |
Olds, 1988 |
|
Caregiver Support Program for Coping with Occupational Stress |
Selective/N=247 |
Occupational stress, distress, anxiety, depression |
Lower psychological distress, better job satisfaction |
Heaney, 1992 |
|
JOBS Project for the Unemployed: Michigan Prevention Research Center |
Selective/N=928 |
Involuntary job loss, anxiety, depression, alcohol abuse, marital stress |
Fewer depressive symptoms, higher pay, cost-effective outcomes |
Vinokur, Price, Caplan, and van Ryn, 1992, 1991 |
|
San Francisco Depression Prevention Research Project: A Randomized Trial with Medical Outpatients |
Selective/N=150 |
Depressive symptoms, medical problems, low income, minority status in public primary care setting |
Lower levels of depressive symptoms |
Muñoz, 1993, 1990, 1987 |
|
Projecto Bienestar: An Intervention for Preventing Depression in Hispanic Immigrant Women in the Community |
Selective/N=399 |
Low income, immigrant minority status, distress, depressive symptoms |
Fewer depressive symptoms |
Vega, 1990, 1987 |
|
Peer- and Professionally-Led Groups to Support Family Caregivers |
Selective/N=56 |
Caregiver burden, anxiety, depression |
Lower levels of psychiatric symptoms, including anxiety and depression, better coping skills |
Toseland, 1990, 1989 |
|
Elderly |
||||
|
Widow-to-Widow: A Mutual Help Program for the Widowed |
Selective/N=162 |
Widowhood, bereavement, depression, anxiety, social isolation |
Fewer depressive symptoms, less social withdrawal |
Vachon, 1982, 1980, 1979 |
women may decrease developmental risks associated with the later
Interventions with high-risk groups should use the broad definition of prenatal care recommended by the U.S. Public Health Service Expert Panel on the Content of Prenatal Care (USPHS, 1989). Going beyond the traditional guidelines for prenatal care, the panel argued that all pregnant women, as a minimum, should receive general information about the physiological and emotional changes of pregnancy as well as fetal growth and development. In addition, they should receive education regarding positive maternal health behaviors and habits, psychosocial preparation for childbirth, and education and support for effective parenting and family behaviors (USPHS, 1989). There was specific emphasis on the identification of and intervention for behavior disorders likely to produce child maltreatment and/or family violence.
In 1988 the Institute of Medicine assessed the barriers to adequate prenatal care and reviewed 31 intervention programs nationwide, all of which were selective programs directed at high-risk groups (IOM, 1988). Programs studied were categorized according to one of five areas of major emphasis: (1) reducing financial obstacles, (2) increasing the basic capacity of the prenatal care system, (3) improving institutional practices to make services more accessible and acceptable, (4) casefinding, and (5) providing social support. Few of these programs used randomization techniques or other strong research designs to assess program effects. Selection bias, in particular, flawed most evaluations. Moreover, because many of the programs were complex, it was difficult to distinguish the specific impact of individual elements. The IOM committee concluded that although several types of programs can succeed in bringing women into prenatal care and maintaining their participation, the success of many programs has been modest, often because they have become embedded in a complicated, fragmented network of maternity services characterized by pervasive financial and institutional obstacles to care (IOM, 1988). Access barriers were identified in all five categories. A significant finding was that casefinding and social support are the most effective means of increasing early and continuing use of prenatal care and compliance with health recommendations among mothers most at risk of absent or inadequate prenatal care (IOM, 1988).
Immunization
Childhood immunization, like prenatal care, is an example of a universal preventive intervention directed at the entire population even though it is given to individuals. Immunization is an example of the
traditional public health model—in which each vaccine can confer long-lasting, often lifetime, protection against a specific physical disease. Currently, infants and children can and should be immunized against poliomyelitis, diphtheria, pertussis, tetanus, measles, mumps, rubella, Haemophilus influenzae type b (Hib) to protect children from meningitis, and hepatitis B. For example, when children are not immunized for Hib and meningitis occurs, there is the possibility of long-term negative effects on the brain, resulting in neurodevelopmental problems, mental retardation, learning disability, and psychological and behavioral disorders (Plotkin and Mortimer, 1988).
In the United States, widespread vaccination on appropriate schedules has produced a dramatic drop in the number of cases of the previously common childhood diseases, and their associated high mortality, morbidity, and sequelae. These declines are reported at 97 percent or more since the year the maximum number of cases for each disease was reported (Peter, 1992).
The cost-effectiveness of vaccination is well documented (Hinman, 1988). In 1983 the measles-mumps-rubella vaccine program had a cost-benefit ratio of 14:1, leading to a total saving of $1.4 billion (White, Koplan, and Orenstein, 1985). A study of pertussis vaccine showed that $2.10 is saved for each $1.00 spent on pertussis vaccination (Hinman and Koplan, 1985).
Currently, there is an immunization crisis in the United States, signaled by recurrent measles epidemics. Because measles is the most contagious of the vaccine-preventable diseases, its resurgence acts as a sentinel that warns of a breakdown in the overall immunization rates for other diseases. Epidemiological studies find that the source of the problem lies in the failure to achieve adequate immunization rates among children in the first two years of life. Rates are well below the 1990 national objective of 90 percent of children with completed immunizations by the second birthday (Cutts, Zell, Mason, Bernier, Dini, and Orestein, 1992; CDC, 1991). The failures of preschool immunization are most notable in inner-city and minority populations. In the inner-city areas, typically, fewer than 50 percent of the two-year-olds have been appropriately vaccinated, and African-American and Hispanic children are at highest risk (CDC, 1992, 1991, 1990).
In 1991 the National Vaccine Advisory Committee identified four major reasons for the low immunization rates among preschool children: (1) missed opportunities for vaccination, (2) deficiencies in the public health care delivery system, (3) lack of access to care, and (4) inadequate public awareness of the importance of immunizations. To ensure that immunizations reach all high-risk groups, specially de-
signed selective interventions may be needed. These interventions should take the above problems of access into account.
Programs aimed at improving Parenting and Reducing Risks for Infants
In addition to the universal, widely implemented programs just discussed, there are some specific, experimentally designed preventive interventions targeted at infants and their families. The *Prenatal/Early Infancy Project is an example of a comprehensive program intended to prevent a wide range of maternal and child problems often associated with poverty (Olds, Henderson, Tatelbaum, and Chamberlin, 1988, 1986). It is a selective program targeted to a high-risk geographical area, with high rates of poverty and child maltreatment, in the semirural Appalachian region of New York. The sample consisted of 394 women, most of whom were white, who entered the program at no later than 25 weeks of pregnancy. At registration, 47 percent were 19 years old or younger, 62 percent were unmarried, and 61 percent were from the lowest socioeconomic group. Violence, drug abuse, and alcoholism were common. Many women reported having been abused as children.
The specific goals were to reduce the mothers' prenatal health-damaging behaviors, enhance parenting skills, give social support to mothers, encourage the use of existing community resources, help the mothers achieve desired educational and occupational goals, and reduce unwanted or inappropriate additional pregnancies. Olds expected that these objectives for the mothers could be attained through a home nurse visitation program. He also expected highly desirable outcomes for the children, including reduction in prematurity and low birthweight, decreases in accidents and infectious diseases, improvement in cognition and language development, decreases in psychological and behavioral problems, reduction in child abuse and neglect, and facilitation of healthy growth and nutrition.
The intercorrelated nature of the biological and psychosocial factors were also recognized. As previously stated, unwed and teenage mothers are at greater risk of having low-birthweight and premature babies. There is increasing understanding that the established higher likelihood of adverse developmental, learning, and behavioral outcomes for low-birthweight and premature babies is largely mediated by adverse childrearing factors, such as poorly educated parents, poverty, isolation of the family, and a stressful environment (Rose, Feldman, Rose, Wallace, and McCarton, 1992; Sameroff and Chandler, 1975).
The intervention was a randomized clinical trial. Women were ran-
domly assigned to one of four groups: (1) developmental screening of the children at one and two years of age and referral for services, (2) developmental screening and transportation to well-child care clinics, (3) home nurse visitation during pregnancy, and (4) home nurse visitation during pregnancy and until children were two years old.
The program design was conceptually based on the “ecological” model (Bronfenbrenner, 1979), which posits interdependence among social systems that operate simultaneously at the level of the marital and parent-child dyads, the family as a whole, and the larger socioeconomic influences of the community. The intervention strategy relied on home nurse visitation during critical phases of the life cycle of a family—pregnancy and the first two years of the infant's life. The home visits, which the mother's primary support person was encouraged to attend, were biweekly at first and tapered off to every six weeks by two years of age.
The design of the program permitted evaluation of the relative effects of specific elements of intervention for both the whole sample and those subsets defined as being at risk. For the evaluation of the postnatal outcomes, groups 1 and 2 were combined into one control group for purposes of analysis and compared with group 4 as the experimental condition, referred to here as “nurse-visited.” It was found that during pregnancy, nurse-visited mothers made better use of medical and other formal services than the control group. The nurse-visited mothers experienced greater social support, improved their diets more, and reduced their cigarette smoking. The greatest impact on infant's birthweight and mother's length of pregnancy was for nurse-visited young teenagers. They had a 75 percent reduction in preterm delivery. For the women who were at highest risk (poor, unmarried, and teenage), there was a reduction in the incidence of verified cases of child abuse, a drop from 19 to 4 percent among those who were nurse-visited (Olds and Kitzman, 1990). (For outcomes with the mothers, see the discussion in the section below on interventions for adults.)
Unfortunately, community-level implementation of the Prenatal/Early Infancy Project by one public health department was unsuccessful (see Box 11.1 in Chapter 11). The program is now, however, being replicated by Olds in an urban area in another part of the country with a different high-risk group, minority mothers, to test the generalizability of the intervention.
In an intense 10-day selective preventive intervention program, the *Tactile/Kinesthetic Stimulation study, Field and colleagues demonstrated positive outcomes for preterm, low-birthweight babies (Field, Schanberg, Scafidi, Bauer, Vega-Lahr, Garcia et al., 1986). In a randomized
controlled trial, the infants who received tactile, kinesthetic stimulation gained significantly more weight—47 percent more per day—than infants in the control group. The infants in the intervention group also were alert and awake more during the awake/sleep behavioral observation, scored significantly higher on the Brazelton subscales of mature habituation, orientation, motor, and range of scale behavior, and were hospitalized significantly fewer days after the onset of the intervention period. This last outcome has positive implications for benefit-cost analyses.
In the *Early Intervention for Preterm Infants study, Field and colleagues had targeted preterm neonates whose mothers were African-American, unmarried, less than 19 years of age, and of low socioeconomic status based on education and occupation (Field, Widmayer, Stringer, and Ingatoff, 1980). The selective preventive intervention, which consisted of home visits by a two-person team —a trained interventionist and a teenage African-American work study student—aimed to prevent developmental delays in the infants by teaching mothers about caretaking practices and enhancing parent-infant interactions. At four months, the infants who had been randomly assigned to the intervention group had significantly better weight and length and higher scores on the Denver Developmental Screening test. At eight months the results still held, with the intervention infants exhibiting significantly higher mental scores on the Bayley Scales of Infant Development. Additionally, these infants had significantly lower blood pressures.
The *Infant Health and Development Program is a selective preventive intervention focused on preventing or reducing the health problems, developmental disabilities, and learning and behavioral problems associated with low birthweight (Infant Health and Development Program, 1990; Kraemer and Fendt, 1990). This eight-site randomized clinical trial was designed to evaluate the efficacy of a multicomponent program consisting of pediatric care, child development activities, and family support services. It is a good example of the use of a multicenter clinical trial design applied to research in human development. It is also a well-designed prospective study that illustrates the feasibility of applying a standard comprehensive intervention in diverse community sites.
This kind of ambitious multisite design was desirable and ready to be tested because a number of previous small studies had demonstrated the efficacy of early intervention for improving the developmental, cognitive, and behavioral outcomes for low-birthweight babies. These previous studies, however, were limited by small numbers of subjects at single sites and lack of long-term follow-up. There was, nevertheless, sufficient relevant experience with home visitation programs for parent
education and with high-quality center-based infant day care to adopt those materials as curricula for the multisite program. Thus, building on the previous studies, the multisite intervention was designed as the first intervention for low-birthweight babies to include both home visitation and center-based components.
A total of 985 infants, each with a birthweight of 5½ pounds (2,500 grams) or less and a gestational age of 37 weeks or less, participated in the study. Two birthweight groups of the 985 infants were defined to assess possible differential responses: heavier babies (weighing 2,001 to 2,500 grams) and lighter babies (weighing less than 2,000 grams). Within each weight group, one third of the subjects were randomly assigned to an experimental group, and two thirds to a control group. The experimental and control groups both received the same high-quality pediatric surveillance, which included periodic medical, developmental, and social (family) assessments, with referrals for services as needed. The experimental group received two additional components: (1) Home visits by educators to teach parents about the specialized, curriculum-based child development activities they were to administer, and also to supervise curriculum-based problem solving by the parents for self-identified problems. The home visits were weekly during the baby's first year and biweekly until 36 months. (2) Participation by the children in a center-based child development program from the ages of 12 to 36 months for teacher-administered, curriculum-based developmental activities five days per week. Transportation to and from the center was provided. In addition, parenting groups met bimonthly for education and support.
The major finding was that the experimental group achieved significantly higher cognitive scores than the control group at 36 months of age (correcting for prematurity). There was also a marked difference in the response of the heavier and the lighter babies to the intervention. For the heavier babies, the IQ scores in the experimental group were, on average, 13.2 points higher than in the control group. For the lighter babies, results were also positive and significant, but not as great. The IQ scores were 6.6 points higher in the lighter-weight experimental group than for their control counterparts.
For the total control group, both heavier and lighter babies, over 18 percent had IQ scores below 70 (the mental retardation range), and almost 50 percent were below 85. The intervention was not effective for any of the study infants with birthweights of 1,500 grams or less. In this lowest-weight group (used only for analysis purposes), there was virtually no difference between the experimental and the control groups in the proportion who tested at IQ of 70 or below.
There were small but significant intervention effects at age 36 months in behavioral competence. The intervention had a positive effect, especially with infants of mothers with low education levels. Mothers in the intervention group reported that there were fewer serious behavior problems but more minor problems.
Longer-term follow-ups have been planned, and results pertaining to academic achievement and behavioral problems in school will be available soon as a measure of the durability of the effects of this infancy and early childhood intervention. This carefully designed program will soon be scaled up into larger field trials by the Centers for Disease Control and Prevention, with support from The Robert Wood Johnson Foundation. The issue of program effectiveness will be a high priority.
Horacek and co-workers demonstrated the utility of early and continued intervention to prevent developmental delays and promote academic success among children at risk by virtue of economic and social deprivation (Horacek, Ramey, Campbell, Hoffman, and Fletcher, 1987). In the * Carolina Abecedarian Project, they randomly assigned socially and economically deprived children at infancy to experimental or control groups. A composite of risk indicators, including low level of family education, low family income, low parental and sibling IQ, and evidence of family psychopathology or social maladaptation, was used to identify children at risk for school failure. The intervention included (1) year-round, center-based full-day care for children beginning at 8 to 12 weeks of age and continuing until kindergarten entry, (2) a toy-lending library to permit continuity of learning from center to home, (3) a home visitation program, and (4) parent group meetings. At kindergarten entry, 96 of the original 111 subjects were randomly assigned again to school-age experimental and control conditions, which continued for three years. This design allowed comparison of the effects of early versus late versus combined intervention on children's cognitive and social development. Some children received both the preschool and the school-age intervention, some received only the preschool or the school-age intervention, and some received no intervention.
The intervention significantly reduced the number of children repeating a grade in school, and it improved the children's test scores in reading and math. Effects were greatest for children who received both the early and the school-age intervention phases. In spite of the fact that the children came from environments predictive of academic failure, they achieved a rate of advancement to the next grade nearly equal to that of an average-risk comparison group constituted for the study. For children who received only one intervention phase, those who received
the preschool intervention performed better than those who received the school-age intervention.
Evidence from a Quasi-Experimental Study
The Family Development Research Program served a poor, predominantly African-American sample of 108 families with incomes of less than $5,000 in which mothers had less than a high school education and a history of semiskilled or unpaid work (Lally, Mangione, and Honig, 1988). Over 85 percent of the participating families were single-parent, female-headed households. This selective study retained a large proportion of families; thus differential attrition was not a major threat to its conclusions.
The multicomponent intervention was provided from the last trimester of the mother's pregnancy through age five for the child. The intervention included a weekly home visit by a “child development trainer” who sought to serve as a friend and advisor on important family issues. The home visitor sought to foster a positive, supportive mother-child relationship, encouraged the family to take an active role in the child's development, and helped the family make contacts with local service agencies. In addition, child care and early educational enrichment were provided in a community center for children from six months to five years of age.
A 10-year follow-up study revealed that children who participated in the intervention had less involvement with the juvenile justice system than did the comparison group (6 percent versus 22 percent), and when they were involved with juvenile justice, their delinquent behavior was less serious. In addition, there were positive effects on school achievement, but these were for girls only (Lally, Mangione, Honig, and Wittner, 1988).
Unfortunately, the study used a quasi-experimental design. The matched comparison group was constituted when subjects were three years old, so obviously there was no random assignment to groups. Such a design prevents the elimination of many alternative hypotheses regarding sources of observed group differences.
An Example from Prevention Services
Healthy Start in Hawaii, a selective intervention program for families at risk of child abuse, is similar in concept and content to the Prenatal/Early Infancy Project described above. Healthy Start, however, was initiated by the Maternal and Child Health Branch of the Hawaii Health Depart-
ment in 1985 not as a research project but as a statewide service project. In 1990 the U.S. Advisory Board on Child Abuse described the program as “clearly the star” of U.S. home visitation programs (U.S. Advisory Board on Child Abuse and Neglect, 1990).
Healthy Start registers pregnant women and mothers with babies up to three months old and serves them until the child is five years old. It uses 15 selection factors to screen for at-risk status. In 1992, Healthy Start was screening 55 percent of the population, and by 1995 it expects to screen 90 percent. About 20 percent of those screened are found to be at risk.
Program elements include early identification of at-risk families, community-based home visiting by laypersons (not nurses as in the Prenatal/Early Infancy Project), linkage to primary health care services and a “medical home,” and linkage and coordination with community services. The goals of the program are to provide (1) adequate prenatal and primary well-child health care; (2) quality child care in infancy and early childhood; (3) parental competence and promotion of child development through parent education, infant stimulation, home visitors, and social support; (4) links to medical and community services and (5) continuity of funding so that clients and providers both experience reliability of service provision.
Since the inception of the program, the rates of child abuse and neglect in Hawaii have been slowly decreasing, but it is impossible to determine how much of this is due to the program. A rigorous evaluation is needed. Such an evaluation should provide a detailed analysis of the screening factors that best detect high risk, the implementation, cost-effectiveness, and the child outcomes, including developmental progress, language proficiency, school readiness, and an array of behavioral outcomes, as well as data on rates of child abuse and neglect. However, the ideal way of determining program effectiveness would be a randomized controlled trial with multiple outcome measures.
Findings and Leads
On the basis of the review of interventions for infants, the following points emerge:
-
Infants born to high-risk mothers and children at high risk of not being immunized could benefit from preventive interventions that reduce financial, institutional, and other access barriers.
-
Home nurse visitation can be an effective means of influencing
-
maternal and child outcomes. In some programs, it may be most effective with the at-risk mothers who are the hardest to reach and most distrustful and may have relatively little effect on mothers who are not at risk.
-
Provision of intensive and prolonged center-based early childhood education, combined with home visitation to families, can prevent cognitive developmental delays and academic failure in children at risk.
-
It is possible to adhere to a rigorous protocol for a complex, comprehensive human development study across several sites that show great diversity in their characteristics. Even with rigorous protocols, appropriate care in implementation can lead to low attrition rates and positive responses from the participants.
-
Highly regarded service programs, such as Healthy Start in Hawaii, can be mined for useful leads on which to base more rigorously designed research studies. Such studies could provide more powerful evidence regarding the outcomes of the programs and could improve the effectiveness of these preventive services.
INTERVENTIONS FOR YOUNG CHILDREN
During early childhood, two examples of important developmental tasks that must be achieved to lower risk for adverse mental health outcomes are (1) the acquisition of language skills to prepare the child to read and write and (2) the development of impulse control (Hawkins and Catalano, 1992). Achieving these tasks has a significant benefit for the ongoing social and cognitive development of the child. Failure at these tasks has been associated with later behavioral and school maladjustment, as well as with the development of mental health problems (Hawkins and Catalano, 1992).
Recent preschool preventive interventions have addressed several risk factors that are related to these developmental tasks, as well as to the development of mental and behavior problems. Risk factors and precursor symptoms that have been addressed in promising interventions during childhood include economic deprivation, poor family management practices, cognitive or developmental delays, school failure, and early behavior problems.
Prevention efforts that address these risk factors during early childhood have adopted a number of approaches, including (1) center-based early childhood education, in which preschool programs are designed to enhance social competence and cognitive development; (2) home visitation to provide a variety of support and educational services; (3) parenting training and education to teach skills in caregiving and
effective behavior management; (4) family support services, which provide survival-focused support; and (5) policy initiatives that address issues of child safety, health, and education. Most programs have combined two or more of these approaches in multicomponent interventions.
Dramatic increases in the proportion of children living in poverty have stimulated research on the developmental outcomes associated with growing up in poverty. As mentioned above, children from poor families are at heightened risk for mental health problems, as well as other problem behaviors (Farrington, Loeber, Elliott, Hawkins, Kandel, Klein et al., 1990). The risk poor children face has been addressed in two ways. First, poverty has been used as a selection criterion in choosing target populations for early childhood intervention. Second, some programs have directly addressed the financial, housing, and other economic needs of poor families in addition to addressing the child's risk for later problems (e.g., Infant Health and Development Program, 1990; Lally, Mangione, and Honig, 1988; Lally, Mangione, Honig, and Wittner, 1988; Andrews, Blumenthal, Johnson, Kahn, Ferguson, Lasater et al., 1982). Virtually all the programs reviewed in this section have focused on reducing risk for children raised in poverty.
Programs Aimed at Improving Parenting and Enhancing Child Development
Multicomponent programs that add center-based child care and early education to their parenting components can be introduced at this phase of development as well as during infancy. The *Houston Parent-Child Development Center program provides another example of the effectiveness of these augmented approaches (Johnson, 1991, 1990; Johnson and Walker, 1987). The Houston Parent-Child Development Center recruited Mexican-American families in poverty who had one-year-old children with no neurological impairments or chronic illnesses. Because mothers were required to participate extensively, the project did not include families whose mother's employment might interfere with their participation. Eligible volunteers recruited from door-to-door surveys were randomly assigned to experimental or control conditions.
The two-year selective preventive intervention included 20 to 30 home visits of 1½ hours duration during the first year, which focused on mother-child interaction, recognized the child's developmental status, and used the home as an environment for learning. In addition, four weekend workshops were offered on special topics to ensure participation of fathers, 90 percent of whom were present in participating families.
During the second year, children attended nursery school four mornings per week, and mothers attended three-hour classes at the center four mornings per week for eight months. Class topics included home management (including health and budgeting) and child development and management issues. Monthly evening sessions for mothers and fathers were offered on special topics, including sex education, family planning, and driver education. The center explicitly sought to serve as a support system for participating mothers and families. Cultural relevance and bilingual format were included in the program design.
At 36 months, mothers showed significantly positive effects of the program. They used more praise and less criticism, and there was more positive mother-child interaction. Few differences were observed in children's behavior during the preschool period, but at follow-up, when children were aged 8 to 11 (in grades 2 to 5), intervention children were rated by teachers as more prosocial and engaging in less acting out and problem behavior, including less impulsive and disruptive behavior and less fighting. The program did not affect measured intelligence.
Overall, this intervention made extensive time demands on mothers. Approximately 550 hours of family participation was expected. Unfortunately, about half of the intervention participants had left by the end of the program, in part because of the high mobility of the Mexican-American families in the sample and also perhaps because full participation consumed so many hours that it almost completely prevented the mother from having a job. This high attrition rate presents a major difficulty in evaluating program effectiveness, which perhaps could have been avoided had these cultural and logistic issues been considered.
The *Mother-Child Home Program of Verbal Interaction Project targeted economically disadvantaged, single mothers of low educational attainment who had two-year-old children (Levenstein, 1992; Madden, O'Hara, and Levenstein, 1984). The selective preventive intervention design involved trained home visitors (either paid paraprofessionals or unpaid volunteers), who visited mothers and their children twice per week for 30 minutes when the child was aged two to four. Home visitors followed cognitive curricula that employed books and toys. They played with the child and mother together, modeling the verbal curriculum and helping the mother to improve her skills to enhance the child's development. Visitors were trained to involve the mother and to pull gradually away from the interaction, allowing the mother and child to play together. On average, more than 35 visits were made each year to intervention families.
Compared with evaluation-only and control groups, the experimental group of children improved significantly in IQ at two-year follow-up
and scored significantly better on achievement and IQ tests in grades 5 and 8. The investigators found evidence of improvement in maternal childrearing behavior, including verbal interaction, following the intervention. Improvements in the mother's childrearing behavior by the time the child reached age four were linked to the child' s later positive classroom attitudes and behavior as rated by first-grade teachers. Moreover, younger siblings of intervention children entering the program in later years had significantly higher IQ scores (by eight points), suggesting the possibility that what the mother learned about parenting enhanced the cognitive development of her younger children also.
As in many field studies, influences other than the intervention affected the outcomes. For example, 94 percent of the parents in the experimental group and 75 percent of the parents in the control group reported that their children attended preschool programs after the intervention. These programs may have affected performance in grades 5 and 8. A low rate of acceptance (52 percent) by those who were offered an opportunity to be in the study may have introduced self-selection. In addition, the subject randomization process used in later years of the study also may have introduced self-selection of more highly educated and intelligent mothers into the study sample. Nonetheless, this multiyear intervention study indicates the promise of a home-delivered curriculum focused on improving maternal skills to facilitate the cognitive development of the child.
Parent-child interaction has also been targeted during early childhood through indicated preventive interventions. Strayhorn and Weidman (1991) reported the results of a study, *Parent-Child Interaction Training, in which low-income parents who identified one or more behavioral problems in their children were recruited from Head Start and other sources. They were randomly assigned to the experimental or the control group. Participants were 64 percent African-American, and a majority were single female heads of household. Over 41 percent of the mothers evidenced mild or greater depression on the Beck Depression Inventory. Parents in the experimental group were offered four to five two-hour group sessions with instruction and role playing on parenting skills, including behavioral management. They were also trained in play and conducted individual play sessions with their children, attending sessions until they reached “criterion.”
Although parental participation in the intervention varied, group comparisons at one-year follow-up revealed significant improvements in experimental subjects when compared with controls on teacher-rated attention deficit/hyperactivity and on behavior as rated by teachers on the Behar behavior questionnaire. Again, analyses suggested that im-
proved parenting practices following intervention predicted better child outcomes one year later. Conclusions are limited by attrition, the absence of baseline data for the experimental and control children, and some changes in patterns of significant findings from posttest to one-year follow-up. Nevertheless, these results suggest the promise of interventions aimed at enhancing parents' skills in behavioral management and in verbal interaction with their children during prosocial play when such interventions are offered to economically deprived parents of children evidencing early behavior problems in the home.
Other programs have aimed at helping children develop the skills to meet the demands of schooling. Many of these center-based programs have also included parent-focused components such as home visitation. In the *High/Scope Preschool Curriculum Comparison Program (Weikart, Schweinhart, and Larner, 1986), the highly structured Distar model (a programmed learning approach wherein the teacher initiates activities and the children respond (Carnine, Carnine, Karp, and Weissberg, 1988)), the child-directed experiential approach of the High/Scope Cognitive Curriculum (Hohmann, Banet, and Weikart, 1979), and the nursery school program based on psychoanalytic theory produced similar improvement in cognitive performance through age 10 when combined with educational home visits by teachers. Differences in long-term effects on behavior were found as a function of the curriculum approach that was adopted (Schweinhart and Weikart, 1992). Subjects exposed to the Distar teacher-led, programmed-learning approach were twice as likely as subjects in other early childhood education groups (p < .05) to report involvement in delinquent acts (e.g., violence, drug abuse, and status offenses) at 10-year follow-up (when they were age 15). The effect size for the overall delinquency score ranged from 0.48 to 0.60. This difference was attributed by the investigators to the fact that the Distar program, which was primarily academic, gave little attention to the social behavior of the children, whereas the two other curriculum approaches did.
The *Perry Preschool Program used the High/Scope curriculum and focused on enhancing the intellectual and social development of three-and four-year-old African-American children from backgrounds of extreme poverty. The selective preventive intervention, begun in 1962, consisted of daily participation in preschool over a one- to two-year period and weekly home visits by trained teachers. The experimental intervention was associated with positive effects on academic performance and social adjustment when randomly assigned experimental and control subjects were followed up and compared at age 19 (Berrueta-Clement, Schweinhart, Barnett, Epstein, and Weikart, 1984). Atten-
dance in the Perry-Preschool Program was associated with a lower rate of deviant behavior and greater social competence in adolescence and early adulthood (Schweinhart, 1987). In primary school the Perry Preschool children demonstrated lower rates of aggression, disobedience, disruptive behavior, lying, stealing, and profanity (an average of 2.3 offenses per person, compared with 3.2 for the no-preschool group). At age 15 the Perry Preschool group reported fewer acts of misconduct, and at age 19 they reported fewer violent acts and less police contact (an average of 1.2 arrests per person, compared with 2.3 for the no-preschool group). Only 31 percent of the preschool group had been arrested at least once by age 19, compared with 51 percent of the no-preschool group. By age 19, experimental preschool participants had lower arrest rates and fewer lifetime arrests, as well as lower rates of self-reported fighting, than control subjects. They also had higher rates of secondary school completion, lower rates of placement in special education classes, and higher grade point averages than their control counterparts (Berrueta-Clement et al., 1984).
Programs Aimed at Enhancing Social Competence
The evidence linking aggression and other behavior problems in childhood with increased risk of later mental disorders has led to the development of educational strategies designed to enhance the social competence of youngsters. These interventions are based, in part, on the hypothesis that aggressive and disruptive children are deficient in basic, teachable, interpersonal skills (Spivack and Shure, 1974) and that acquiring these skills can reduce the risk of childhood psychopathology and later mental disorders.
Social competence interventions seek to enhance children's capacities to coordinate cognition, affect, and behavior so that they can respond adaptively to social tasks and challenges (Weissberg, Caplan, and Sivo, 1989). These interventions have focused on four skill areas: (1) self-management or self-control, (2) communication, (3) decision making and problem solving, and (4) resisting negative and limiting social influences.
One of the original programs to enhance social competence, Shure and Spivack's *I Can Problem Solve: An Interpersonal Cognitive Problem-Solving (ICPS) Program, was targeted to economically disadvantaged four- and five-year-old African-American children from federally funded Head Start day care centers and kindergarten classrooms in inner-city Philadelphia. The curriculum includes a manual of scripted lessons of games and interpersonal dialogues provided daily for 20 minutes over a
three- to four-month period. It also includes 10 to 12 lessons that introduce the language and basic concepts for thinking about alternative solutions to problems and about the consequences of actions, approximately 20 lessons that teach children to recognize and be sensitive to the feelings of others, and approximately 15 lessons teaching problem-solving processes for generating several possible solutions in a social situation and thinking about the likely consequences of each solution. Each lesson is delivered to small groups of nursery school or kindergarten children by a classroom teacher trained in the curriculum. Teachers are taught an important informal communication method called “problem solving dialoguing” to provide children with opportunities to use their new skills in social situations arising in the classroom or on the playground.
In testing the curriculum, Shure and Spivack chose not to restrict the intervention to children who were already showing skills deficits, but rather to provide it to all urban children from families in poverty attending intervention day care centers and intervention kindergartens, thus making it a selective preventive intervention.
A complicated design, small numbers, and substantial attrition (39 percent lost in year two) hampered the study. Nevertheless, the results provided empirical support for the efficacy of enhancement of social competence through training in interpersonal problem-solving skills at ages four and five in urban day care and school settings. Shure and Spivack (1988, 1982, 1980) reported that social competence training produced durable effects on social behavior. Children trained in nursery school were rated as significantly better than untrained controls on measures of adjustment at the end of the intervention and again one year later when rated by kindergarten teachers. These effects were observed in those at highest risk. For children trained in kindergarten, 70 percent of those previously rated as impulsive were rated as adjusted, compared with 6 percent of the impulsive controls. The investigators showed that acquisition of skills to generate alternative solutions and consequential thinking skills predicted behavioral adjustment at post-test.
The results suggest that providing a social competence curriculum to inner-city disadvantaged children before first grade can help to reduce aggressive and socially inappropriate behaviors predictive of later mental health problems. By the spring of kindergarten, only 30 percent of children in control classrooms were rated by their teachers as normally adjusted, compared with 77 to 85 percent of the children in the three experimental groups exposed to different lengths and combinations of intervention at ages four and five.
The investigators had first conducted a pilot test of the use of the ICPS curriculum by inner-city African-American mothers in poverty (Shure and Spivack, 1982). Twenty mothers of four-year-old children who showed observable behavioral difficulties in nursery school and 20 matched controls were studied in an indicated preventive intervention. The findings demonstrated that mothers could be trained to teach their children ICPS lessons at home. Children in the experimental group improved significantly more than controls on measures of interpersonal skills and behavioral adjustment. Moreover, the improvement in behavior generalized to the classroom, as reflected in teacher ratings of behavioral adjustment.
Findings and Leads
-
Multicomponent interventions that address multiple risk factors have proved effective in improving the family management practices of low-income parents and in facilitating the cognitive and social development of children of low-income, low-birthweight, and low-education backgrounds, preparing them for successful entry into the primary grades. There is also some evidence that multicomponent early childhood interventions have shown effects in promoting prosocial behavior and preventing behavior problems.
-
Preventive interventions designed to enhance social competence through teaching interpersonal problem-solving skills at ages four and five in urban day care and school settings and through parents training their children in these skills at home have produced durable effects on conduct problems in children.
-
Early childhood interventions can have positive long-term effects on academic performance and social adjustment. Achieving enduring effects through adolescence, a period of great risk for onset of mental disorders, by intervening in early childhood is a noteworthy possibility.
-
All of these early childhood interventions are characterized by intensity. In most of the programs, services were provided daily over periods of several years, often involving frequent visits to families' homes. All of the effective early childhood programs reviewed here recognize the role of parents in the continuing development of children, and all involve parents on some level, whether through home visitation or center-based programs. All of the programs worked to involve parents in supporting the cognitive and behavioral development of their children. Some provided parents with supports for handling financial, housing, and other material problems as well. These successful interventions typically involved multiple intervention components focused on multiple risk factors for later disorders.
-
Early childhood interventions, delivered with fidelity and quality, clearly can reduce risks for later disorders in children from at-risk families. Data are not yet available regarding the effects of these early childhood interventions on the incidence of a wide range of diagnosable disorders, including, but not limited to, substance abuse disorders, conduct disorder, depressive disorders, and schizophrenia.
INTERVENTIONS FOR ELEMENTARY-AGE CHILDREN
Middle to late childhood (ages 5 to 12) is a period of rapid cognitive and social development. Most children learn to read and to interact in ways that gain social approval from peers during this period. Children who cannot perform academic tasks at grade level by grade 4 and/or who develop social incompetence, impulsivity, and aggressive behavior during this period are at high risk for developing mental disorders, especially substance abuse, conduct disorder, and depressive disorders.
In addition, the family environment may contribute to risk during this period. Poor parenting practices, high levels of conflict in the family, and a low degree of bonding between children and parents appear to increase the risk for mental disorders.
Preventive interventions at this period have focused on the children, with less attention to parents. The children, now developmentally more advanced, are capable of engaging in more verbal interventions. High-risk factors for children, including early behavior problems, have been addressed through enhancement of social competence and academic achievement. Intensive family preservation services have provided crisis intervention for families where children are at risk for out-of-home placement.
Programs Aimed at Enhancing Parenting Skills and Family Functioning
Universal interventions seeking to enhance parenting skills, such as courses on parenting complete with books and video tapes, have been popularized over the past two decades. Unfortunately, virtually no controlled studies have examined the effects of these relatively widely disseminated programs, either in terms of risk reduction or in terms of the prevention of mental disorders or related health and behavior problems. A number of experimental treatment studies, however, have demonstrated the effectiveness of parenting skills training during early and middle childhood to reduce antisocial behaviors in children meeting diagnostic criteria for disorder. (See Chapter 8; also see Dumas, 1989;
McMahon and Wells, 1989; Fraser, Hawkins, and Howard, 1988; Kazdin, 1987; for reviews.)
An Example from Prevention Services: Family Preservation Services
In a related but separate area, public and private providers of children 's services have initiated intensive family preservation services for families whose children are at risk for out-of-home placement. These short-term crisis interventions are delivered to families in their homes toward the goal of stabilizing the family—by improving family functioning and linking the family to sustaining sources of support—to the point that out-of-home placement of the child is not necessary. These programs are both a response to evidence that out-of-home placement is predictive of more negative social, health, and mental health outcomes and therefore is a risk factor for mental disorders and a response to the rising costs of foster care, congregate care, and institutional care for children removed from their families. Reducing the risk of out-of-home placement might reduce the subsequent onset of mental disorders.
The Homebuilders Program in Tacoma, Washington, pioneered the development of intensive family preservation services. In programs based on the Homebuilders model, workers deliver a variety of clinical and material services in the home setting. The services are of short duration (90 days or less) and intensive (a minimum of 8 to 10 hours of face-to-face client contact per week). The mental health status of the parents and children is not assessed.
Early uncontrolled evaluations of intensive family preservation services reported significant cost savings resulting from avoidance of out-of-home placements (Kinney, Madsen, Fleming, and Haapala, 1977), stimulating legislative and administrative interest in the intervention. Currently, intensive family preservation services are being implemented in child welfare, juvenile justice, and mental health systems.
The most rigorous evaluation of intensive family preservation services was a New Jersey study in which 214 eligible families were randomly assigned to family preservation services using the Homebuilders model or to a control group that received existing community services (Feldman, 1991a, b). In spite of an attempted random assignment, there was a significantly higher percentage of whites in the family preservation group (51.3 percent) than in the control group (33 percent). Excellent implementation data indicate that the intervention was conducted in accordance with the Homebuilders model. Both experimental and control groups were at risk for out-of-home placement; just under 20
percent had experienced a prior out-of-home placement. Over 86 percent were from poverty. Most were referred as a result of the child's out-of-control behavior; one quarter were referred because of abuse, neglect, or risk thereof.
At the termination of this intervention, children had entered placement in only 6 percent of experimental families, compared with 16.5 percent of control families. A series of comparisons suggest that families receiving preservation services functioned better than control families when the intervention ended, an indication that the services had improved social support systems for families, reduced family conflict, and strengthened family bonding. The difference in the percentages of children entering placement from experimental and control families persisted over time through multiple follow-ups to 12 months after termination, at which time placement rates were 42.7 percent for the experimental group and 56.7 percent for the control group. These results suggest that even though intensive family preservation services are effective in avoiding some out-of-home placements in the short-term, their long-term results are less impressive.
Programs Aimed at Enhancing Social Competence
In the *Assertiveness Training Program, a universal preventive intervention, Rotheram, Armstrong, and Booraem (1982) trained college students to lead assertiveness training sessions with a sample of 60 percent white, 35 percent Chicano, and 5 percent African-American fourth-, fifth-, and sixth-grade students from predominantly working-class homes in California. An experimental study comparing assertiveness training against a placebo control intervention demonstrated effects at one-year follow-up on both social competence and academic achievement. In addition to this universal program, an indicated preventive intervention study was done with 101 children targeting four groups: underachievers, disruptive students with conduct problems, children with multiple problems related to achievement and conduct, and exceptional children without major problems. In this study, effects appeared to be least strong among children evidencing multiple problems at baseline (Rotheram, 1982).
Social competence components also have been included in interventions designed for populations selected for intervention because of exposure to specific risk factors or stressors during childhood, including parental divorce, parental substance abuse, and parental depression.
Children from homes broken by marital discord are at risk for conduct disorder and substance abuse disorders (Baumrind, 1983; Penning and
Barnes, 1982; Robins, 1980). Pedro-Carroll and Cowen (1985), in their *Children of Divorce Intervention Program (CODIP), sought to reduce risk and enhance adaptation among children of divorce. They developed a curriculum of 10 one-hour weekly sessions for children in grades 4 through 6 whose parents had divorced. The curriculum included a component focused on understanding feelings about divorce and divorce-related anxieties, a cognitive skills-building component for resolving interpersonal conflicts, and a component dealing with skills for controlling anger. A team of two trained facilitators led the school-based intervention.
This selective preventive intervention was first tested with children from white middle-class families in four suburban schools. Participants were recruited through letters and phone calls to parents. Parental consent was necessary for participation. Parents of participants had been separated for an average of 23.6 months. Participants were matched by gender, grade, length of time since parental separation, and other preadjustment measures before being randomly assigned to the experimental group or control group that received a delayed intervention.
At posttest, two weeks following program completion, teachers rated experimental participants as being significantly better adjusted than control subjects on two measures of the Classroom Adjustment Rating Scale (CARS)—shy-anxious behaviors and learning problems. Teachers also rated participants as significantly more socially competent at posttest than controls on the Health Resources Inventory (HRI), which includes indicators of adaptive assertiveness, peer sociability, and frustration tolerance. Similarly, experimental children rated themselves as significantly less anxious than controls at posttest. Further, at posttest, parents of intervention children rated them as significantly less maladjusted than did parents of controls on a scale including items on peer relationships, school performance, and feelings about divorce. These findings were replicated in a less rigorously designed study by Pedro-Carroll and colleagues (Pedro-Carroll, Cowen, Hightower, and Guare, 1986).
Alpert-Gillis, Pedro-Carroll, and Cowen (1989) subsequently extended the program to 16 45-minute sessions and tested it with second-and third-grade children in an urban setting. About 31 percent of participating children were nonwhite. The curriculum was revised to reflect the sociocultural population of urban children targeted. Unfortunately, they used a quasi-experimental design; that is, the experimental group was recruited by a different procedure than the comparison group, and there was no random assignment to the two groups. Greater
emphasis was placed on teaching children ways to cope with the problem of infrequent contact with noncustodial parents and to seek support from extended family members and other caring adults. In addition, curriculum materials were selected to portray families of diverse ethnic backgrounds. The definition of divorce was also expanded to include the termination of a common-law relationship or a long-standing live-in partnership if the mother reported a separation. Participants ' parents had separated an average of 3.75 years before the intervention.
Pretest comparisons with a group of children from intact families showed both the experimental and the comparison groups of children of divorce were significantly less well adjusted. At posttest, one to four weeks following the intervention, experimental children evidenced significant improvements when compared with comparison groups on (1) self-ratings on the Children's Divorce Adjustment Scale, which assesses coping skills and attitudes toward family, parents, and self; (2) parent ratings of children's feelings, behaviors, and problem-solving skills; and (3) teacher ratings of children's competence, including assertiveness, frustration tolerance, and peer social skills.
The findings from the original study, receiving some support from the second study, suggest that a relatively brief social competence intervention can produce immediate reductions in anxiety, adjustment problems, and behavior problems among both middle-class white children and poor and working-class, urban, multiethnic children who have experienced parental divorce or separation. Longer-term effects of the intervention have not been investigated. The results to date suggest the promise of selective preventive interventions focusing on the enhancement of social competence during the elementary grades for children who have recently experienced parental separation.
Other investigators are also seeking to reduce risk and enhance adaptation of children of divorce (see Grych and Fincham, 1992, for a review; Gwynn and Brantley, 1987; Stolberg and Garrison, 1985; Kalter, Pickar, and Lesowitz, 1984). In addition, Sandler and colleagues, in the *Family Bereavement Program, sought to improve the mental health of children who had experienced the death of a parent within the past two years (Sandler, West, Baca, Pillow, Gersten, Rogosch et al., 1992). They did this by attempting to enhance the family environment. The intervention group received a three-session family grief workshop and 13 highly structured sessions from a family advisor who had personally experienced a bereavement similar to the deaths experienced by the families. Parent reports indicated that the intervention group improved on symptoms related to depression and conduct disorder, especially for
the older children. This finding suggests the need to target programs to children's different developmental needs.
More targeted social competence interventions have been designed for populations of children with risk factors for later disorders, such as peer rejection or early aggressive behavior. Bierman's (1986) program, *Social Skills Training, examined the impact of a social skills training program that involved role playing naturalistic interactions between a target child and peer partners. This selective intervention was targeted at 11-year-olds who had low peer acceptance and were deficient in conversation skills. Children were randomly paired with two same-gender peers and assigned to one of two experimental conditions: social skills training or peer experience. On short-term follow-up, the social skills training showed an overall positive effect on conversational skill acquisition and peer response.
Lochman and co-workers tested an expanded social competence curriculum, the *Social Relations Intervention Program, with a sample of 86 African-American fourth-grade children identified through sociometric ratings as the most socially rejected and physically aggressive in their classrooms and then randomly assigned to intervention and control groups (Lochman, Coie, Underwood, and Terry, in press). The indicated intervention, based on earlier quasi-experimental work (Lochman and Curry, 1986), consisted of positive social skills training to promote prosocial behaviors and cognitive-behavioral training to decrease anti-social reflexive responses and foster adaptive social problem solving. The curriculum included 26 30-minute individual sessions and 8 small-group sessions. It had four components: social problem-solving training, positive play training, group entry skills training, and training on coping with anger (including how to identify and reduce impulsive behavior and how to use self-talk to regulate behavior). Sessions were held twice weekly at school from early October to late April, for a total of 12 to 18 sessions, by a team of psychology graduate students and a university psychologist.
Small samples, nonequivalent comparison groups, and substantial attrition posed threats to this study, but teacher-rated aggression and rejection were significantly lower among a subgroup of rejected-aggressive children who had received the intervention than among rejected-aggressive children in schools not offered the intervention. One year later, for those remaining in the study, significantly lower teacher ratings of aggression and higher teacher ratings of prosocial behavior were observed in the aggressive-rejected subsample. The intervention appeared to have little effect on the behaviors or ratings of rejected children not also identified as aggressive.
Lochman (1992) followed up several of these aggressive boys in a quasi-experimental study of the longer-term effects of the anger-coping curriculum. Thirty-one boys rated by their teachers as aggressive and disruptive in grades 4, 5, and 6 were compared with 52 boys in other schools rated by either teachers or peers as aggressive. The intervention was followed by significant short-term improvements in rates of substance use, general behavioral deviance, and classroom behavior as measured by observational data and self-reports from the two groups. Three years following the intervention, boys exposed to the school-based intervention had lower rates of drug and alcohol involvement and higher levels of social problem-solving skills, although not lower rates of delinquency or classroom behavior problems. However, a subset of 12 who received booster sessions in the year following the original intervention, combined with five parent training workshops, also showed enduring effects on passive off-task classroom behavior three years after the intervention.
Building explicitly on the treatment interventions developed by Patterson and colleagues (Patterson, Reid, Jones, and Conger, 1975), Tremblay and colleagues at the University of Montreal designed a two-year indicated intervention program for disruptive seven-year-old boys, the *Montreal Longitudinal-Experimental Study (Tremblay, McCord, Boileau, Charlebois, Gagnon, LeBlanc, and Lariveet, 1991). It combined home-based training for parents in family management skills, offered once every two weeks for a two-year period, with social skills training delivered in schools to disruptive boys within small groups of prosocial male peers. Parents received an average of 17 parenting sessions over the two-year period, and 19 training sessions were provided to the children over the same time. Sessions for the children focused on initiating social interaction, improving interpersonal skills, making verbal requests, following rules, handling anger, and mastering “look and listen” techniques for regaining self-control.
A field experiment tested the intervention with a sample of 172 boys from low-socioeconomic areas of Montreal who were assessed by their teachers at the end of kindergarten as highly disruptive. Boys were randomly assigned to one of three groups: experimental (received intervention); observational (received attention but no intervention); and control. Teacher ratings indicated that boys in the experimental group became significantly less aggressive than boys who did not receive the intervention. This difference lasted through the most recently reported follow-up at age 12, three years following intervention. Further, significantly more control boys were retained in a lower school grade or placed in special classes, schools, or institutions. Twice as many control boys (44 percent) as boys in the experimental group (22
percent) were rated as having serious adjustment problems at age 12. Moreover, significantly more control boys had initiated minor delinquency by age 12 (Tremblay, Vitaro, Bertrand, LeBlanc, Beauchesne, Boileau, and David, 1992; Tremblay et al., 1991).
Programs Aimed at Enhancing Academic Achievement
Apparently reciprocal relationships between achievement and early depression have led some researchers to explore interventions focused on the promotion of academic achievement as a preventive intervention (Kellam and Rebok, 1992). Similarly, the evidence that poor academic achievement predicts both later drug abuse and delinquency (Hawkins, Catalano, and Miller, 1992) has led to the investigation of enhancement of academic competence as a component of preventive interventions.
Several intervention studies have focused on the enhancement of academic competence during the elementary grades. The use of certain methods of instruction in classrooms has been shown in experimental studies to improve achievement. Several studies have linked achievement gains to the amount of active instruction and direct supervision of learning provided by teachers (Brophy and Good, 1986). Some intervention trials have trained teachers in the use of effective instructional methods, including the use of interactive and “mastery” teaching methods, in which teachers frequently monitor students' performance. Teachers are trained to use the results of these frequent assessments to adjust instruction or provide more intensive support, such as tutoring or cooperative learning groups, to increase the academic and cognitive development of all students, including those at risk of poor achievement.
An experimental community-based study, *Community Epidemiological Preventive Intervention: Mastery Learning and Good Behavior Game, of mastery learning methods in first grade in 19 ethnically and sociodemographically mixed public schools in Baltimore, Maryland, found positive effects on reading achievement (Kellam and Rebok, 1992). Moreover, virtually all of the reading gains occurred among students initially showing depressive symptoms and among those with initially low reading scores, suggesting that this universal intervention may have greater benefits for those at risk for depressive disorders. In addition, the Good Behavior Game program had positive effects on aggressive and shy behavior, with the largest effects found for the most aggressive children.
Learning and achievement problems have also been addressed in tandem with peer rejection through selective interventions targeted at children with both risk factors. Individual tutoring has been shown to produce significant improvements in reading and math achievement
among low-achieving, socially rejected fourth graders in *Academic Tutoring and Social Skills Training, and effects on reading scores remained at one-year follow-up (Coie and Krehbiel, 1984).
Hawkins, Catalano, and their colleagues implemented the *Seattle Social Development Project with first graders in eight Seattle, Washington, public schools (Hawkins, Catalano, Morrison, O'Donnell, Abbott, and Day, 1992). The initial universal preventive intervention program lasted four years, from the first through the fourth grade. It was a multicomponent intervention and sought to reduce risks in family, school, and peer environments. Although participating schools were chosen on the basis of high crime in their catchment areas (and therefore the intervention might be designated as selective), the program focused on all children rather than on identified at-risk children. One school implemented the program with all students, and one school served as a full control school. The students in the remaining six schools were randomly assigned to experimental and control classrooms. The intervention included teacher training and supervision to modify classroom instruction and classroom management practices in grades 1 through 4, training and supervision of first-grade teachers in the use of Shure and Spivack 's (1988) Interpersonal Cognitive Problem Solving Curriculum (see the section above on early childhood), and parent training in grades 1, 2, and 3. Teachers were trained in proactive classroom management, effective instructional methods, and cooperative learning (Hawkins, Doueck, and Lishner, 1988; Hawkins and Lam, 1987). Parents were offered two programs. The first, offered when children were in first grade, was a skills-training program focused on management of children' s behavior (Hawkins, Catalano, Jones, and Fine, 1987). The second, “How to Help Your Child Succeed in School,” offered when children were in second and third grades, focused on providing parental support for academic development (Hawkins et al., 1987).
Results of assessments were reported shortly after the children entered fifth grade (Hawkins et al., 1992). Fewer children in the experimental group than in the control group reported having initiated delinquent behavior and alcohol use. Children from the experimental group also reported more positive results than control group children for parent management, family communication, family involvement, attachment to family, school rewards, school attachment, school commitment, and achievement tests.
An Example from Prevention Services: School Reorganization
Academic achievement can also be enhanced through a preventive intervention aimed at altering the organization of a school. The School
Development Program was created by Comer and colleagues at the Yale Child Study Center as a demonstration of a prevention service that was evaluated initially by quasi-experimental methods and only later by a randomized controlled trial (Comer, 1985). The organizational development model that was used focuses on broadening the involvement of those who have a stake in the school. It creates a school management team, a mental health team, and a program to encourage and support parent involvement. Parents, teachers, and administrators play active and meaningful roles in all these groups, and the result is an enhanced sense of “ownership” of the school's programs.
The School Development Program was first applied in two inner-city elementary schools serving predominantly low-income African-Americans in New Haven, Connecticut, beginning in 1968. Comer (1988) reported positive gains in student academic achievement and in standardized reading and math tests compared with national norms over a 12-year period after implementation of the program. A follow-up study of children from intervention schools and a matched comparison group found higher reading and math scores, school grades, and social competence scores among the children in the intervention schools (Cauce, Comer, and Schwartz, 1987). After further testing with increasingly more rigorous design, the School Development Program is now being used in more than 100 schools throughout the country, and The Rockefeller Foundation has awarded funding for national dissemination of the intervention. A randomized controlled study of the intervention, supported by the MacArthur Foundation, is currently under way in Prince Georges County, Maryland (Jessor, 1993). Such a rigorous design is especially difficult in community intervention of this scale, but the study may yield valuable information regarding the efficacy of the intervention.
Evidence from Quasi-Experimental Studies
Elias and colleagues extended and elaborated on Shure and Spivack 's (1988) Interpersonal Cognitive Problem Solving Curriculum for use with children in grades 4 and 5 to prepare them to handle the transition to middle school more effectively (Elias, Gara, Ubrlaca, Rothbaum, Clabby, and Schuyler, 1986). Quasi-experimental analyses with a sample of white children from predominantly working-class homes suggested some small but lasting effects on indicators of psychopathology six years later (Elias, Gara, Schuyler, Brandon-Muller, and Sayette, 1991).
Interventions to enhance social competence have been included in programs offered in settings beyond the school, including after-school programs for latchkey children (Ross, Saavedra, Shur, Winters, and
Felner, 1992), after-school programs for children in public housing (Jones and Offord, 1989), and programs offered through Boys and Girls Clubs in public housing (Schinke, Orlandi, and Cole, 1992). Nonexperimental results suggest that providing well-designed opportunities for active learning and practice of cognitive, interpersonal, and problem-solving skills to children from economically deprived backgrounds during late childhood and early adolescence in after-school programs might contribute to the development of social competence and reduce behavior problems.
Alterations in teaching methods have been combined with other intervention elements to increase achievement among students at risk by virtue of extreme economic deprivation. In a predominantly African-American school in which 76 percent of the children were eligible for federally funded free lunch, Slavin and colleagues in the Success for All program, which had a quasi-experimental design, sought to bring all students up to grade level in reading by the end of third grade (Slavin, Madden, Karweit, Livermon, and Dolan, 1990). The project provided half-day preschool and full-day kindergarten focused on language development, academic readiness, and improved self-concept. In grades 1 through 3, pull-out programs and special education programs were replaced with an intensive interactive reading program supplemented by reading tutoring for students needing extra assistance. In addition, a team of two social workers provided family support, and a parent liaison worker provided parent education and encouraged parents to become involved in the child's education. Two inner-city schools serving predominantly African-American and low-income children were matched. Matched pairs of students from each school at grade levels K through 3 were compared. At the end of one year of intervention, children in the intervention school had higher scores on reading tests, with greatest effects found for students with the lowest 15 percent at baseline. The results were hampered by lack of clarification about how schools were assigned to the experimental and control groups.
Findings and Leads
-
Intensive family preservation services appear to be an effective short-term mechanism for reducing risk of out-of-home placement, stabilizing families in crisis, and developing family competences and supports. However, long-term results are less impressive, and outcome data related to mental health for children and their parents are not available. More rigorous research designs of service programs such as this one could yield valuable information.
-
Preventive interventions to enhance social competence for children of elementary age can be effective in reducing early behavior problems predictive of risk for several mental disorders. Whether delivered to whole classrooms of high-risk children or targeted to individual children referred for early behavior problems, social competence curricula have produced significant reductions in early risk factors associated with later onset of conduct disorder, depressive disorders, and substance abuse disorders. Although the evidence is not conclusive, these interventions appear to produce larger and more consistent effects on behavior when begun in the early elementary grades, when followed by booster sessions or offered continuously for more than a year, and when combined with parent training interventions that enlist adult caretakers in more effectively managing child behavior.
-
The use of specific instructional methods in classrooms and individual tutoring interventions for low achievers holds promise for reducing academic failure among those at risk for mental disorders. Some selective interventions focused on enhancing academic achievement appear to have the greatest effects with those at greatest risk when subgroups have been analyzed separately (Kellam and Rebok, 1992; Slavin et al., 1990). It is plausible that ensuring the academic success of all children through the use of effective instructional methods in the classroom will reduce academic failure as a risk factor for depressive disorders, conduct disorder, and substance abuse. Unfortunately, few studies have moved beyond short-term follow-ups of effects on risk factors for these disorders.
-
Because multiple risk factors have been implicated in the etiology of most, if not all individual disorders, including conduct disorder, substance abuse disorders, and mood disorders, investigators have designed multicomponent interventions focused on reducing risks in several domains (including family, school, and peer environments) by using efficacious risk reduction components. Program results suggest that such designs are highly promising. For example, when guided by a common theory that specifies common aims and principles for a preventive intervention in different domains, teacher and parent training programs offered together can strengthen prosocial involvements and reduce early-appearing health and behavior problems.
-
Current preventive intervention research designs, such as those for children of divorce, could be applied to other groups of high-risk children. For example, work has begun in designing and fielding interventions for children of alcoholics (e.g., Springer, Phillips, Phillips, Cannady, and Derst-Harris, 1992; Emshoff, 1990), but these have not yet been well evaluated. Work has also begun with children whose parents
-
are depressed. Parental depression itself is among the strongest predictors of depression in offspring (Petersen, Compas, Brooks-Gunn, Stemmler, Ey, and Grant, 1993; see Box 6.3 in Chapter 6). Clinical and education interventions for multiple family members based on etiological studies of resilient adolescents exposed to parental depression have been developed (Beardslee, Salt, Porterfield, Rothberg, van de Velde, Swatling et al., 1993; Beardslee, Hoke, Wheelock, Rothberg, van de Velde, and Swatling, 1992; Beardslee, 1990), and rigorous testing of the effects of these interventions on children's behaviors and psychopathology is currently under way.
INTERVENTIONS FOR ADOLESCENTS
Biological events associated with puberty have come to symbolize the transition from childhood to adolescence. This period between childhood and adulthood has become more prolonged as the age of puberty has decreased in industrialized nations (now beginning for girls on average at age 12½ years) and the entry into full-time productive adult roles has been delayed by educational decisions. Hamburg (1992) has described the developmental risk factors that are associated with adolescence, including the exploratory behavior that is central to early adolescence. For example, children today appear to be at greatest risk for the initiation of substance use and delinquent behaviors indicative of conduct disorder from ages 12 to 15.
The early initiation of delinquent behaviors or substance use has been shown to be strongly predictive of antisocial personality or substance abuse disorders. Thus efforts to prevent conduct disorder and substance abuse disorders during adolescence have focused largely on reducing the incidence of disorders by preventing early onset. Even though the co-morbidity of numerous disorders, including substance abuse, conduct, and mood disorders, has been well established (Elliott, Huizinga, and Menard, 1989; Jessor and Jessor, 1977), the preponderance of research on preventive interventions for adolescents has been disorder-specific, focusing for the most part on the prevention of substance abuse, or to a lesser extent, on the prevention of conduct disorder. Virtually no prevention programs during adolescence have focused on the prevention of depressive disorders or depressive symptoms (Muñoz, 1993a) or schizophrenia, in spite of the fact that the incidence of depressive disorders increases during this period (Petersen et al., 1993) and the initial onset of schizophrenia often occurs in late adolescence. Few prevention studies targeting adolescents have measured the effects of intervention on the incidence of multiple disorders.
Prevention efforts during adolescence have received less attention than have efforts to treat individuals who already have these disorders. Given the disorder-specific nature of much prevention research during this period, it is useful to review interventions that have focused specifically on the prevention of substance abuse or conduct disorder. First, however, a program is presented that focused on academic performance and behaviors more generally.
Program Aimed at Enhancing Academic Achievement and School Behavior
There is some evidence from the Seattle Social Development Project (discussed in the section on the elementary period above) that, when implemented in middle-school classrooms in grade 7, the selective interventions of teacher and parent training are particularly effective in changing the school behavior of adolescents who are at elevated risk by virtue of low achievement. Hawkins, Doueck, and Lishner (1988), in their study *Changing Teaching Practices, conducted a selective preventive intervention research program in which seventh-grade students in three schools were randomly assigned to one of 15 experimental or 18 control classrooms. Teachers were also randomly assigned to experimental or control classrooms. One additional school was assigned to be a full control school, and another to be a full experimental school. The intervention included teacher training in proactive classroom management, effective instructional methods, and cooperative learning methods. After one year, the full experimental and control groups were compared (Hawkins and Lam, 1987). A separate investigation focused on intervention effects on low achievers, defined as those students who received a math achievement score in the lower three stanines (bottom 23 percent) on the California Achievement Test in the spring of sixth grade. Although the students from the experimental group did not report different rates of delinquency or drug use, low achievers in experimental classrooms were significantly more attached and committed to school and significantly less likely to have been suspended from school than their control counterparts. This effect was significant only among low achievers, and not in the general population.
Programs Aimed at Preventing Substance Abuse
The evidence that early first use of substances is predictive of later substance abuse disorder (Kandel, Yamaguchi, and Chen, 1992; Robins and Przybeck, 1985) suggests the goal of preventing, or at least delaying,
initiation in hopes of preventing later abuse. Substance abuse prevention research has focused largely on preventing the initiation of substance use or reducing use among those who have initiated use early. To accomplish this goal, prevention researchers have tested school curricula focusing on enhancing social competence, providing social influence resistance training, and promoting norms against drug use. The risk factors addressed by these programs include the early age of onset, social influences to use drugs, including drug-using peers, and norms and attitudes favorable to alcohol or other drug use. In addition, interventions to change laws and norms regulating alcohol and other drug behaviors have also been assessed for effects on adolescents.
Enhancing Social Competence
Social competence curricula have been developed that include specific content on prevention of substance use. The *Positive Youth Development Program combined training in general social competence with information on substance abuse and on how to apply the skills to situations involving alcohol and drug use (Caplan, Weissberg, Grober, Sivo, Grady, and Jacoby, 1992). Participants were students in an urban middle school (90 percent African-American, 8 percent Hispanic, 2 percent mixed race) and in a suburban middle school (99 percent white, 1 percent Hispanic). The 20-session curriculum was provided in two 50-minute sessions per week by university-based health educators who worked with teachers in classrooms randomly assigned to the intervention training.
Regardless of setting, exposure to the curriculum was associated with better impulse control and conflict resolution skills, as rated by teachers, and with lower scores on a self-reported measure of intent to use alcohol. It was also associated with lower rates of self-reported heavy alcohol use among intervention students than among control students, although no significant differences between groups were found in the incidence (rates of initiation) of alcohol, marijuana, or tobacco use.
Providing Social Influence Resistance Training and Promoting Norms Against Drug Use
Many approaches to drug abuse prevention in the schools have been tried. To date, consistently effective interventions have included at least two components: (1) classroom-based training in skills to identify and resist influences to use drugs and (2) encouragement to adopt norms against drug use during adolescence. Social influence resistance training (Ellickson and Bell, 1990; Hansen, Johnson, Flay, Graham, and Sobel,
1988) provides instruction, modeling, and role play for students to learn to identify and resist influences to use drugs. Curricula promoting norms against drug use (Hansen and Graham, 1991; Ellickson and Bell, 1990; Perry, 1986) have included portrayals of drug use as socially unacceptable, identification of short-term negative consequences of drug use, provision of evidence that drug use is less prevalent among peers than children may think, encouragement for children to make public commitments to remain drug free, and in some cases the use of peer leaders to teach the curriculum.
Nearly all curricula include information on the prevalence and effects of alcohol and other drug use. However, this component alone does not appear sufficient to change the drug and alcohol behavior of youth (Hansen, 1992; Schinke, Botvin, and Orlandi, 1991; Stuart, 1974; Weaver and Tennant, 1973).
The combination of social influence resistance and normative change content in school curricula has produced modest significant reductions during early adolescence in the onset and prevalence of cigarette smoking, alcohol, and marijuana use across a number of experimental studies conducted by a variety of investigators (Ellickson and Bell, 1990; Hansen et al., 1988; McAlister, Perry, Killen, Slinkard, and Maccoby, 1980; see Hansen, 1992, for a recent review.)
Hansen and Graham (1991) have examined the relative contribution of the two components in a universal four-condition experimental study, the *Adolescent Alcohol Prevention Trial, of 3,011 seventh-grade students at 12 junior high schools. The study population was 44 percent white and 54 percent minority (e.g., African-American, Hispanic, and Asian-Americans). Schools were stratified by size, test scores, and ethnic composition, and randomized to the following conditions: (1) an information program about the social and health consequences of alcohol and drug use; (2) a resistance training program on how to identify and resist peer and advertising pressure to use alcohol and drugs; (3) a normative education program geared toward remedying students' false perceptions about the prevalence and acceptability of alcohol and drug use among their same-age peers (methods used included discussing topics in class, completing and reviewing interviews with nondrinkers, developing positive friendships, establishing nondrinking as a positive quality, and writing and videotaping antialcohol rap songs); and (4) a shortened combination of information, resistance training, and normative education.
Results, which were analyzed at the classroom level on data collected in the year following intervention, suggested that normative change was the active ingredient in the curricula. Overall, those classrooms that
received the normative education program had significantly reduced rates of alcohol consumption (p < .001), marijuana use (p < .001), and cigarette smoking (p < .05), compared with classrooms that did not (groups 1 and 2). Analyses were conducted of program effects on prevalence and incidence using dichotomous measures of alcohol, cigarette, and marijuana use. For alcohol use, the greatest effect was on the delay in the age of onset of ever being drunk; the incidence of drunkenness in classrooms not exposed to the normative change component increased 11 percent, compared with an increase of 4 percent for those exposed to that component. There was also a greater increase in prevalence of problem alcohol use in the groups not exposed to the component (an increase of 2.4 percent) than in the normative education groups (which increased 0.3 percent).
Exposure to the normative change component had a similar effect on the use of marijuana. Classrooms that did not receive that component demonstrated an increased prevalence of marijuana use, compared with the normative education classrooms (an increase of 6.2 versus 2.2 percent). Hansen and Graham (1991) have suggested that previously reported positive effects of peer resistance skills-training programs may have been due to the normative education components included in these programs. It appears that the enhancement of social norms against tobacco, alcohol, and marijuana use in adolescence is an essential component of school curricula seeking to prevent the early onset of alcohol and other drug use as a strategy for preventing substance abuse disorders.
Ellickson and Bell (1990) reached a similar conclusion in another universal program, when, at one-year follow-up, the initial effects on alcohol use from their social influence resistance training, * ALERT Drug Prevention, had disappeared. They speculated that social influence training is less effective in preventing alcohol use than tobacco and marijuana use because a normative consensus has not been established around the use of alcohol.
There is some evidence that the use of peer leaders from the student population to share in the teaching of the substance abuse prevention curriculum is more effective than teacher-led conditions (Botvin, Baker, Filazzola, and Botvin, 1990a; Klepp, Halper, and Perry, 1986; Murray, Johnson, Luepker, and Mittelmark, 1984; McAlister, 1983). Peer leaders may be effective in stimulating classroom norms antithetical to drug use.
Perry and colleagues, in a four-country pilot study conducted under the auspices of the World Health Organization, attempted to delay the onset of alcohol use in eighth and ninth graders and to reduce the use of alcohol by those already involved with it (Perry, Grant, Ernberg,
Florenzano, Langdon, Myeni et al., 1989). Twenty-five schools were randomly assigned to one of three conditions: peer-led education, teacher-led education, or control. The teacher-led and peer-led curricula (five sessions) were identical in content, except for the fact that the peer-led program took place in small groups, whereas the teacher-led program was conducted with the classroom as a whole. Self-report data at one-month follow-up showed that peer-led programs for teenage drinkers and nondrinkers were significantly more effective in preventing or reducing alcohol use than programs taught by teachers.
Although attention to the establishment of a clear consensus regarding norms is apparently an important component of substance abuse prevention programs, this strategy has some limitations and risks. For example, Ellickson and Bell (1990) found that although their curriculum was effective in preventing tobacco use among those who were not tobacco users in grade 7, the program had counterproductive effects on those already smoking. Smokers at baseline who were exposed to the curriculum actually smoked more at posttest than their control counterparts. It is plausible that explicit campaigns to show drug use as nonnormative behavior isolate or alienate those who already engage in that behavior. Ellickson and Bell found that these individuals were already at risk for mental health problems by virtue of high levels of family conflict, problems in parent-child communication, early delinquency, low achievement, and low commitment to school (truancy).
Multicomponent Interventions
The establishment through public policy of clear normative standards regarding alcohol and other drugs appears important in preventing or at least delaying the onset of drug use. Peers, family members, the community, and the media all influence the development of an adolescent's norms and attitudes regarding behavior. Some drug abuse prevention programs have combined school-based curriculum interventions with interventions focused on parents, community leaders, and the media to promote greater normative clarity and consistency in the adolescent's social environment.
Pentz and colleagues tested a multicomponent communitywide program, The *Midwestern Prevention Project, involving a curriculum of social influence resistance skills training and normative change content for students in grades 6 and 7 (Pentz, Dwyer, MacKinnon, Flay, Hansen, Wang, and Johnson, 1989). A 10-session school-based universal intervention provided information on the health consequences and prevalence of substance use and taught assertiveness and social resistance
skills. This was combined with homework assignments to be conducted with parents; booster sessions in the year after the initial intervention; organizational and training opportunities for parents in positive parent-child communication and in reviewing school policies; training of community leaders to organize drug abuse prevention task forces; and news coverage via newspaper articles, short television clips, and a press conference. The multicomponent program produced lower rates of weekly cigarette smoking (down 8 percent), alcohol use (down 4 percent), and marijuana use (down 3 percent) after the second year of intervention, and significantly lower prevalence of monthly cigarette (down 6 percent) and marijuana (down 3 percent) use three years after the initial school intervention, although the prevalence of alcohol use was not significantly reduced at this measurement point (Johnson, Pentz, Weber, Dwyer, Baer, MacKinnon, Hansen, and Flay, 1989). The comprehensive intervention appears to have been effective in lowering tobacco and marijuana use prevalence among those at risk because of exposure to parental drug use, drug-using peers, and early initiation of use.
This study's conclusions are tempered by methodological considerations. Only 8 of the 42 participating schools were randomly assigned to experimental and control conditions. In the other 34 schools, the assignment was based on the flexibility of the principal and his or her willingness to reschedule classes to accommodate the intervention. Additionally, students in different grades were compared in the quasi-experimental nonequivalent comparison group design. The results of a more controlled trial of the multicomponent intervention conducted by Pentz and her colleagues in Indiana have not been reported in full. Nevertheless, the results reported to date indicate multiple drug use behaviors were reduced by the combination of curriculum and mobilization of parents, community members, and the media to promote norms consistent with those provided in the curriculum.
Policy Initiatives
Substance abuse disorders depend on the availability of substances and on the prevalence of substance use in the population. Current policy-focused prevention strategies seek to limit the availability of drugs through prohibition of drugs such as marijuana and cocaine, taxation on alcohol at purchase (Levy and Sheflin, 1985), raising the minimum drinking age (Joksch, 1988; Saffer and Grossman, 1987; Cook and Tauchen, 1984; Kreig, 1982), and restrictions on how alcohol is sold (Holder and Blose, 1987). The legal status of a substance is associated
with the prevalence of its use in the population. Alcohol, an intoxicant legal for adults to purchase and use, is the substance most widely used by both adults and adolescents. Alcohol abuse and alcoholism are, in turn, the most prevalent substance abuse disorders.
With respect to alcohol, increases in taxes on alcohol at purchase have been shown to produce immediate and sharp decreases in liquor consumption rates and cirrhosis mortality (Cook and Tauchen, 1982). Similarly, increased alcohol availability resulting from the privatization of wine sales has been shown to result in at least short-term increases in alcohol consumption (Wagenaar and Holder, 1991). However, longer time series analyses conducted by Mulford, Ledolter, and Fitzgerald (1992) have suggested that the increased consumption following privatization of sales is only temporary. Long-term sales trends in one state tracked for 10 years were unaffected by the change in distribution system approximately midway through the period.
Increasing the legal age for drinking alcohol to 21 years has been shown to be associated with lower levels of alcohol use among high school seniors and recent high school graduates, and with lowered involvement in alcohol-related fatal crashes among drivers under 21 (O'Malley and Wagenaar, 1991). Lower levels of alcohol use persisted into the early twenties, beyond the legal drinking age.
Investigation of another policy measure to limit alcohol availability, restricting how alcohol is sold, has shown that allowing patrons to purchase distilled spirits by the drink increased the consumption of distilled spirits and the frequency of alcohol-related car accidents (Holder and Blose, 1987).
Evidence from a Quasi-Experimental Study
As noted above, components on alcohol and other drugs have been included in some social competence curricula (Caplan et al., 1992). Conversely, the work of Botvin and colleagues in substance abuse prevention has combined (1) training in skills to resist social influences to use drugs with (2) a focus on the development of general social competences, including verbal and nonverbal communication skills, skills for social interaction with same- and opposite-sex peers, assertiveness skills, and skills for coping with anxiety (Botvin et al., 1990a; Botvin, Baker, Tortu, and Botvin, 1990b). A recent evaluation suggested the promise of this approach when led by peers, but the evaluation highlighted the importance of the fidelity or integrity of implementation of curricula-based interventions (Botvin et al., 1990a). Only about 62 percent of the trained experimental teachers in their study implemented
60 percent or more of the curriculum content. This finding has clear implications for the dissemination of preventive interventions.
Programs Aimed at Preventing Conduct Disorder
Conduct disorder involves frequent, persistent, and patterned antisocial behaviors, including delinquent behaviors, whether against property (e.g., burglary, fire-starting) or persons (e.g., fighting, violent behavior, rape), as well as other problem behaviors (e.g., lying, running away). (For more detailed descriptions of conduct disorder, see Chapter 5 and Chapter 6.) During adolescence, conduct disorder increases in prevalence and affects current functioning. Conduct-disordered behaviors that become integrated into the behavior patterns of the individual during adolescence predict antisocial personality in adulthood, indicate risk for other disorders (including mood disorders and schizophrenia), and affect adult functioning and opportunities.
Risk factors associated with the development and diagnosis of conduct disorder include early aggressive behavior, school failure, criminal and alcoholic behavior of parents, poor family management practices (e.g., inconsistent discipline, poor monitoring), and family conflict (Kazdin, 1990). These factors are often well established before the onset of adolescence. During early adolescence, as with substance use, peer influences and norms conducive to antisocial behaviors increasingly and strongly predict involvement in delinquent and other problem behaviors (Elliott et al., 1989).
In contrast to substance abuse prevention, the preponderance of the evaluated efforts to prevent conduct disorder have focused on individuals at risk rather than on community or school populations. For example, preventive interventions effective in preventing conduct disorder during adolescence have focused on 12- to 15-year-olds at risk by virtue of academic or behavioral problems and by virtue of an older sibling's involvement in status offenses.
A family-focused treatment intervention in an experimental study demonstrated positive effects in preventing delinquent behaviors in siblings of 13- to 16-year-olds who had committed minor delinquent offenses or had been declared ungovernable by the juvenile court (Alexander and Parsons, 1980, 1973). The intervention combined behavior management skills training techniques for parents with communications skills training. The brief family systems intervention significantly altered patterns of communication within experimental families and resulted in statistically significant preventive effects on younger siblings. A 2½- to 3½-year follow-up of the juvenile court records of the younger
siblings of the originally targeted participants found that 20 percent of the younger siblings in families that received the short-term family systems intervention were referred to court, compared with 43 to 63 percent of the younger siblings in families that received other experimental or control conditions (Klein, Alexander, and Parsons, 1977).
Some indicated preventive interventions that have shown positive effects in preventing delinquency have involved both family and school intervention. Bry's (1982) three-year indicated preventive intervention, *Behaviorally Based Preventive Intervention, targeted adolescents with academic and behavior problems at school. Samples of seventh-grade students with low academic motivation, alienation from family, and several school discipline referrals were identified in a low-income urban school and a middle-income suburban school. Within schools, participants were placed in matched pairs on the basis of sixth-grade academic records and randomly assigned to receive the intervention or serve as controls. The intervention consisted of the use of positive reinforcements for desirable school behavior. Weekly report cards were used to monitor student behavior in the classroom as reported by teachers. Program staff met weekly with intervention students to discuss report cards. Positive reports elicited praise and approval from staff, and negative reports elicited discussions of how to win more approval from teachers. Parents were routinely informed of students' progress through phone calls, letters, and home visits. Booster sessions were also provided every two weeks over a period of two years following the initial intervention, although attendance at booster sessions was low. Nevertheless, the intervention appeared to prevent later delinquency as measured both by self-reports of criminal behavior at one-year follow-up and by court records at five-year follow-up. Ten percent from the intervention group, compared with 30 percent from the control group, had accumulated a court file.
Evidence from Quasi-Experimental Studies: Altering School Organization and Social Environments
School transitions represent a time of risk for increased symptoms of psychological problems. Both substance use and antisocial behaviors increase in prevalence following transitions from elementary to middle or junior high school and from middle school to high school. There is evidence that the structure of schooling itself may affect these changes in behavior following school transitions (Hamburg, 1992). Comprehensive recommendations for changing the structure of education, especially in middle schools, have been made (Carnegie Council on Adolescent Development, 1989).
Gottfredson and Gottfredson (1992) also have focused on changes in school organization and management in testing interventions to prevent delinquency and substance abuse in secondary schools. (See similar work by Comer in the section on interventions in the elementary period.) An important ingredient in the Gottfredsons' work is a focus on providing a method for school stake-holders to reorganize the school to make it more effective in the social and cognitive development of all students. The method involves a systematic assessment of school problems carried out by a school improvement team of teachers, parents, school administrators, community agencies, students, and district-level staff. The team reviews school policy, climate, instruction, and organization and plans and implements changes. The intervention is called the Program Development Evaluation method (Gottfredson, 1984).
Gottfredson (1986) evaluated an intervention that included the establishment of an organizational structure to facilitate shared decision making and management in schools, the use of curriculum and specialists trained to respond to student concerns, academic innovations including cooperative learning, reading and test taking programs, and career exploration. In addition, direct services were provided to a randomly assigned subsample of high-risk students in participating schools. After three years, students in experimental schools reported lower rates of drug use, delinquent behavior, and alienation, and higher rates of attachment to school, higher educational expectations, and a greater belief in school rules than students in comparison schools. However, although the direct services for selected high-risk students improved their school achievement (promotion and graduation rates), these services did not produce significant effects on the delinquent behaviors of the high-risk students over and above the effects of the organizational intervention in the school (Gottfredson and Gottfredson, 1992; Gottfredson, 1986).
Gottfredson has evaluated the method in inner-city Baltimore, Maryland, and in Charleston, South Carolina. The Baltimore study showed significant decreases in rebellious behavior and negative student attitudes toward school following use of the method (Gottfredson, 1988). An evaluation of the method in six Charleston schools found that, in comparison with control schools, those using the method improved significantly in classroom order, classroom organization, and clarity of rules (Gottfredson, Karweit, and Gottfredson, 1989).
Another broad intervention targeted the school environment at a particular developmental phase. Felner and colleagues focused on the restructuring of schools through the School Transitional Environmental Project (STEP) designed to address the risks associated with the transi-
tion from middle-school to high school, including academic failure and low commitment to school (Felner, Ginter, and Primavera, 1982; Felner and Adan, 1988). The intervention had two components: (1) reorganizing the school environment to alleviate stressors associated with the transition and (2) redefining the role of homeroom teachers to give them more central roles as counselors and mediators between students and the school administration. The goal of STEP was to enhance adjustment through a school restructuring program that assigned project students to one of four experimental homerooms. The homeroom teachers were given more responsibility to meet the administrative, counseling, and guidance needs of their students. The students in the experimental groups were assigned to take their core academic courses (math, English, social studies, and science) together, and all the experimental classrooms were in close proximity to enhance feelings of belonging and social support among a more stable cohort of peers. The underlying hypothesis was that by changing the role of school personnel and the overall social ecology of the high school environment to increase levels of social support available to students and reduce the confusion and complexity of the new school environment, both academic and personal adjustment would be enhanced.
The effectiveness of STEP, a selective preventive intervention, was examined with a sample of 185 ninth graders (65 in the experimental group and 120 in the control group) from a primarily minority, lower-income high school. The experimental sample was selected randomly from the entering ninth-grade population who had met all requirements for the eighth grade and who had not been identified as needing special mental health services. The control group was matched on age, gender, and race with the experimental group, but there was no random assignment to the groups. Three-year follow-up data collected at the end of high school revealed lower school dropout rates for the students in the experimental group (21 versus 43 percent of controls) (Felner and Adan, 1988). Positive effects on two indexes of school adjustment, namely, grade point average (p < .05) and absenteeism (p < .05), were observed following the intervention and were maintained through grade 10. In addition, project students rated the school environment as demonstrating greater order, rule clarity, teacher control, and innovation (p < .01), suggesting that reported changes in behavior and academic performance reflected changes in the school environment associated with the intervention. These results show the promise of interventions aimed at the risk factors associated with school transitions. They also suggest that throughout primary and secondary school, having a close relationship with a supportive teacher may be a signifi-
cant protective factor against academic and mental health problems. Felner has now combined the school restructuring components of STEP with curriculum changes suggested by the Carnegie Council and applied the program in 50 schools with 22,000 children (R. Felner, personal communication, 1993).
Others have taken a more comprehensive approach by targeting the broader social environments of the school, family, and community, seeking to spread the prevention message throughout the social environments affecting the adolescent. Olweus's *Intervention Campaign Against Bully-Victim Problems was designed to prevent bullying among children and adolescents in Norway (Olweus, 1991). The primary emphasis of the multicomponent prevention program was to educate the community, families, and school personnel on the scope of the bully-victim problem, and potential solutions. The intervention program was implemented as a nationwide campaign. The components of the program included (1) an educational booklet on the bullying problem distributed to all schools, (2) parent education (in the form of a booklet) on the bullying problem and possible solutions, (3) a 25-minute video with stories about the lives of “bullied children,” which was available for rent or sale, and (4) a self-report questionnaire to be completed by the children in the program.
The universal preventive intervention was evaluated by using a quasi-experimental cohort sequential design, and time-lagged comparisons were made between age-equivalent groups. The sample consisted of 2,400 students in grades 4 through 7 from 42 primary and secondary schools. Using self-reports of “being bullied” and “bullying others,” the findings indicated a 50 percent reduction in the levels of bully-victim problems at both the 8-month and the 20-month follow-up assessments. Youths also reported a reduction in reports of antisocial behavior (e.g., vandalism, theft, truancy) and an increased satisfaction with school life. Although the design does not rule out potential sources of influence, the fact that children reported a reduction in bullying, victimization, and other antisocial behavior following the intervention suggests the potential benefit of interventions seeking to reduce violence by establishing commonly shared concerns regarding antisocial behavior and discouraging such behavior in the media, schools, and homes.
Evidence from a Quasi-Experimental Study: Programs Aimed at Violence Prevention
The emergence of concern with violence as a major public health problem (Rosenberg and Mercy, 1991; Sullivan, 1991; see also Chapter 3)
has led to the development of interventions focused on preventing violent behaviors included in the diagnostic criteria for conduct disorder. In this area the emerging prevention strategies bear some resemblance to prevention programs targeting substance abuse. That is, the preventive interventions focus on changing norms regarding violent behavior and providing skills to solve problems without violence. Social competence promotion in problem solving and developmentally appropriate social interaction have been included in school-based curricula seeking to prevent violence. However, the committee is aware of no published controlled studies of classroom-based prevention curricula focused explicitly on preventing violence, although some studies are under way.
To date, methodological problems, including quasi-experimental designs, have thwarted a clear assessment of the effectiveness of community-based intervention programs to prevent violence in the United States. For example, the Violence Prevention Project (VPP), a comprehensive prevention program using a community-based model for the prevention of youth violence, recently reported data from an evaluation study of the intervention (Hausman, Spivak, Prothrow-Stith, and Roeber, 1992). The curriculum included a 10-session community-based “Violence Prevention Curriculum for Adolescents” and a mass media normative change campaign involving television, posters, T-shirts, and brochures. The results indicated little difference in exposure to the intervention between youths in control neighborhoods and youths in experimental neighborhoods. About 55 percent of both experimental and control youths self-reported exposure to the intervention. The results underscore the importance of monitoring implementation and program exposure in evaluating preventive interventions. They also leave open the question of whether combined interventions focused on establishing norms opposed to violence are effective in actually preventing it.
Findings and Leads
-
Prevention of early substance use has been shown to be a logical and effective strategy for the prevention of substance abuse disorders. There is evidence that the incidence of substance use can be reduced by school curricula that promote norms antithetical to substance use and teach skills to resist social influences to use drugs. The promotion of clear norms against use appears to be a key component of these interventions. There is also evidence that promoting explicit norms against use in family, school, and community settings through multi-component communitywide interventions holds promise for preventing
-
early substance use. However, normative change strategies may be counterproductive with some of those at highest risk by virtue of their exposure to multiple biopsychosocial risk factors. For example, adolescents who have been exposed to parental alcoholism and violence and who have already initiated use of alcohol themselves may react to normative change campaigns by increasing their substance use. This possibility suggests that combining risk reduction interventions introduced earlier in development with norm-focused interventions during adolescence might be a useful approach.
-
There is also evidence that preventive interventions that seek to restrict the availability of alcohol and other substances through higher taxation, raising the legal age of drinking, or limiting how liquor is distributed may reduce both the rates of alcohol consumption and the adverse consequences associated with alcohol use, including alcohol-related accidents.
-
During adolescence, initiatives focused on the nature and structure of schooling and school experiences themselves may have mental health promotion or disorder prevention potential. Few of these interventions have been evaluated for effects on conduct or other mental disorders, but a number have shown effects in reducing risk factors. Examples include efforts to promote broader academic success during adolescence.
-
The concept of school reorganization and the leads from Comer's and the Gottfredsons' studies suggest the promise of efforts to empower school communities at both the elementary and the secondary levels to regain control of the cognitive and social development agenda of their schools. Intervention trials that focus on identifying how the school and its community can be more effective in reducing risks for and enhancing protective processes against the development of psychopathology may be particularly useful.
-
There is some evidence from Norway that preventive interventions can change community norms regarding aggression. The extent to which such a normative consensus can be created regarding the prevention of violence in this country, given the diversity of race, culture, and class, remains to be demonstrated.
-
Attention to fidelity and integrity of implementation is critical to the success of a prevention program.
INTERVENTIONS FOR ADULTS
Movement from adolescence to adulthood changes the developmental tasks facing the individual as well as the nature of the risk and protective factors. As various life domains in adulthood, such as family and work
life, begin to exert their separate influences, developmental tasks become more differentiated (see Figure 7.2). These tasks include establishing and maintaining committed relationships as well as successful childbearing and effective parenting. Assuming and maintaining occupational roles are also crucial, not only because work can provide a sense of mastery and satisfaction, but also because paid employment provides material support for the developing adult and his or her family. For some adults—particularly poor, single parents—coping with chronic stressors such as financial hardship and lack of emotional support for their parental role also complicates their efforts to perform these tasks successfully and places them at increased risk.
In adulthood, psychosocial risk factors that increase the likelihood of mental health problems correspond closely to these developmental tasks. Marital conflict and divorce, unsupported childbirth and childrearing, stressful work roles and occupations, involuntary job loss, chronic poverty, and discrimination all constitute critical risk factors in adulthood, particularly among those with psychosocial or biological vulnerabilities.
However, there are corresponding protective factors that, when incorporated into systematic preventive intervention efforts, can help to reduce the likelihood of mental disorder. These include problem-solving skills, the availability of responsive social and medical services, and social, material, and emotional support from friends, family, and others. Work supervisors, health personnel, teachers, spouses, and others can be potent sources of either support or stress or both. In addition, a variety of social skills, including the ability to cope with one's emotions, to control the demands of work and mobilize supportive co-workers, to use job seeking skills, and to nurture spouse and family support, all are protective factors that can help safeguard mental health.
The following review of a number of prevention programs focuses on five major areas of adult life where preventive trials have reduced risk factors and enhanced protective factors in the course of adult development. These include programs aimed at (1) the development and maintenance of marital relationships, as well as programs for coping with marital separation; (2) the special stresses of childbearing and childrearing; (3) occupational stress and job loss; (4) preventing depressive disorders among adults at risk because of poverty and minority status; and (5) supporting adult children who provide care for ill parents.
Programs Aimed at the Marital Relationship
The marital relationship can be a major protective factor or stressor, especially for vulnerable individuals. Two preventive programs are
described below. One is aimed at enhancing marital relationships, and the other is intended to cope with the risks associated with separation and divorce.
Enhancing Marital Relationships
Destructive marital conflict and marital distress are major risk factors for many forms of interpersonal and psychological dysfunction and psychopathology (Coie, Hawkins, Ramsey, and Watt, 1991). Specifically, marital distress has been associated with higher rates of depression in adults and also related to the development of conduct disorder in children (see Chapter 6). Markman (1984) has argued that destructive conflict among spouses, marital distress, and the effects of divorce constitute a major social problem that costs billions of dollars per year.
Markman and colleagues have developed the *Prevention and Relationship Enhancement Program (PREP), designed to prevent distress and divorce in couples who are already married or planning marriage (Renick, Blumberg, and Markman, 1992). PREP, a universal preventive intervention, is based on the identification of and intervention with variables that are most predictive of later distress and relationship satisfaction. Couples who are not currently experiencing relationship difficulties are taught skills identified by research as predicting satisfying and healthy relationships. They are also taught how to thwart those behaviors that predict later marital distress. The central principle underlying the program is that the constructive handling of disagreements can prevent later distress. Furthermore, PREP assumes that opportunities in a relationship should be created to control conflicts and handle problems before they get too large.
Earlier research on which PREP is based (Markman, 1984, 1981, 1979; Gottman, Markman, and Notarius, 1977) suggested that distressed and nondistressed couples communicate differently. Distressed couples were found to engage in negative escalation during discussions, whereas nondistressed couples exited at the beginning stages of negative interaction cycles (Gottman et al., 1977). Furthermore, longitudinal studies (Markman, 1984, 1981, 1979) indicate that the quality of communication before marriage and before the development of distress in the relationship is one of the best predictors of future marital distress.
The PREP intervention takes one of two formats. In the extended version, couples attend six 2- to 2½-hour weekly sessions in groups of four to eight couples. They hear lectures on communication skills and then privately practice their new communication skills to discuss issues in their relationship. The communications consultant acts as a coach to
help the couple master these new skills. In the second format, groups of 20 to 40 couples hear the same lectures at a weekend retreat and then use their private rooms to practice their skills on their own.
At the 1½-year follow-up, PREP couples report greater relationship satisfaction and fewer relationship problems. At three years, they report fewer sexual difficulties and less problem intensity. At four years, PREP husbands report better relationship satisfaction than controls and show less dominance, conflict, and overall negative communication. At five years, husbands report greater relationship satisfaction, show less denial and negative escalation, and use more problem-solving behaviors. In addition, at five years, 19 percent of control couples had divorced, whereas only 8 percent of PREP couples had done so. Furthermore, PREP couples reported fewer instances of physical violence with their spouse than did control couples across the three-, four-, and five-year follow-ups (Markman, Renick, Floyd, Stanley, and Clements, 1993).
Most of the evaluation findings for the PREP program have focused on reduction of risk factors rather than specific mental health outcomes, and an improved version of this study would also assess mental health outcomes. This program has been disseminated both in Europe and in the United States and has been adopted for use by clergy, who often provide premarital counseling.
Coping with Separation and Divorce
The epidemiology of divorce as well as stressful life events theory (Bloom, 1985) suggests that marital separation and divorce constitute major stressful life events with major impacts on health and mental health. Epidemiological research conducted in Pueblo, Colorado, as well as a review of the research literature (Bloom, Asher, and White, 1978), indicates that marital separation is associated with higher levels of distress, anxiety, and depression and higher rates of admission to psychiatric inpatient facilities.
Five specific categories of risk can be identified in the literature associated with marital separation and divorce. They include (1) weakened support systems, (2) problems with childrearing and single parenting, (3) legal and financial issues, (4) housing and homemaking problems, and (5) education and occupational problems, particularly for the female spouse in joining or rejoining the labor force.
Bloom and Hodges developed the *University of Colorado Separation and Divorce Program specifically to address these risk factors and to enhance protective factors (Bloom, Hodges, Kern, and McFaddin, 1985; Bloom,
Hodges, and Caldwell, 1982). This intervention is aimed at newly separated persons who are engaged in the task of negotiating the transition to single life with new occupational and childrearing responsibilities. It is not aimed at improving preexisting marital relationships. Participants had separated because of marital discord and had been separated no longer than 6 months. Bloom and Hodges (1988) followed a number of guidelines in designing the selective program. Principles included the use of a clear program rationale, focus on newly separated persons, specified duration and eligibility requirements, use of a university site so as to avoid defining marital separation as an illness, economical program delivery, a goal of education and competence enhancement, and attempts to be comprehensive in the range of services.
The Separation and Divorce Program was coordinated by a number of program representatives, each of whom worked with 15 newly separated persons. Information in coping with a wide variety of life domains was provided by subject matter specialists, who provided two-hour workshops with groups of participants. Program areas included socialization, childrearing and single parenting, housing and homemaking, employment and education, and legal and financial issues, all designed to enhance coping skills and mobilization of support.
After four years of follow-up in a well-designed and well-executed randomized trial, a number of positive impacts on mental health could be observed. Experimental group members were significantly higher in adjustment, had fewer separation-related problems, and reported significantly greater separation-related benefits than controls. Positive program effects, including lower levels of psychiatric symptoms, were still evident after four years. Preventive effects included reductions in maritally related sources of distress as well as in symptoms of anxiety and depression (Bloom et al., 1985).
The Separation and Divorce Program has been documented with a series of research papers and also a clear and well-documented program manual, which includes details of rationale, design, data collection, and examples from the point of view of participants and staff members.
Programs Aimed at the Challenges of Childbearing and Childrearing
Childbearing and childrearing present major challenges that can affect the well-being of women and their children. Below are two prevention programs that promise to reduce risks associated with insufficiently supported childbearing and childrearing.
Coping with the Stresses of Caesarean Childbirth
Women who deliver children by caesarean section are more likely than control populations to develop postnatal depressive symptoms (Kendell, Rennie, Clark, and Dean, 1981). In addition, the emotional difficulties encountered by women delivering by caesarean birth (CB) are accentuated by hospital practices and attitudes of the hospital staff (Cohen, 1977; Donovan, 1977). Tadmor (1988) reported that CB mothers were not usually well prepared for the event and were cast into the role of surgical patient rather than mother. They were also often separated for longer periods from their children and their new babies, and they may not have received adequate support from their spouse.
The specific psychological and developmental tasks confronted by the CB mother include acquiring a realistic appraisal of the reasons for the caesarean birth and a share in the decision-making process. In addition, she faces the task of dealing with the loss of the natural childbirth process and with the negative feelings associated with caesarean birth. Other psychological tasks include establishing an attachment to the baby and dealing with the physiological limitations imposed by the caesarean birth.
Tadmor and Brandes developed the *Perceived Personal Control (PPC) Preventive Intervention for a Caesarean Birth Population, a selective prevention program, to enable the CB mother to accomplish the specific psychological tasks associated with caesarean births and to enhance her coping skills so that she can ensure a positive outcome and deal successfully with any future caesarean births (Tadmor, Brandes, and Hofman, 1988; Tadmor and Brandes, 1984). The underlying theoretical framework of the intervention is the perceived personal control crisis model developed most specifically by Caplan (1977) and Caplan and Killilean (1976). The premise of this model was that the availability of a coping response that mediates between the individual's appraisal of some event and his or her responses to it is a critical protective factor that will produce a generalized measure of resistance to stressors.
The intervention begins with an anticipatory guidance session, which helps to familiarize the CB couple with the medical environment and the sequence of steps through which they will pass. They receive detailed information with respect to the course, safety, and duration of the caesarean birth, anesthesia, and the physiological and emotional reactions they can anticipate. During the birth itself, the father actively provides emotional support to the mother. A variety of efforts to enhance the possibility of immediate bonding between infant and
parents are engaged. After delivery, the mother and father are given full care of the baby under supervision.
The program was evaluated in a randomized controlled trial. Mothers completed questionnaires on the fourth or fifth postpartum day, and there were follow-ups at 6 and 12 months after the caesarean birth to assess physiological and psychological recovery and to document the implementation of the intervention model, beneficial effects of the model, duration of full breast-feeding, and response to crises.
Results indicated that the program had a number of impacts. Experimental mothers were released from the hospital sooner than controls, initiated independent care of the baby sooner, and continued nursing longer. After day one, experimental mothers requested less medication than controls, and experimental fathers showed closer attachment to the babies than control fathers. Experimental mothers also had a more rapid psychological recovery from the caesarean birth, and distress was reduced.
The PPC intervention is designed to be implemented only in a community institution such as a general hospital. Resistance in the hospital by medical and nursing staff is a major potential limitation. Implementation requires dealing with a complex network of interlocking events and may impose additional burdens on the staff as well as on the mental health worker who implements the program. Furthermore, continuous training has to be provided for new physicians and nurses who join the department.
Enhancing Personal Development of New Mothers
The *Prenatal/Early Infancy Project is a comprehensive selective preventive intervention designed to prevent a wide range of maternal and child problems often associated with poverty (Olds et al., 1988; Olds et al., 1986). It is a unique program in that it targeted both children and mothers and measured outcomes for both generations. The design of the study and the outcomes related to improved parenting and reducing risks for the children were presented in the section “Interventions for Infants” earlier in this chapter. Discussion here is limited to intervention strategies and outcomes related to the mothers' personal development.
The Prenatal/Early Infancy Project was based on the assumption that nurse home visitors are in an ideal position to identify and change factors in the family environment that interfere with maternal health habits and personal accomplishments in the area of work, education, and family planning. Beginning during pregnancy, nurses attempted to form effective and supportive relationships with the women by emphasizing the women's personal strengths. Nurses encouraged the women
to clarify plans for completing education, returning to work, and bearing additional children. Nurses stressed that the decision to return to school and seek employment after delivery should be made after full consideration of the women's own best interests as well as the babies'. Nurses helped interested women find appropriate jobs or job placement services and plan for child care. They also advised them about job interviews and showed them and their partners birth control devices, discussing the advantages of different methods of family planning.
Results of a randomized controlled trial evaluating the effect of the nurse visiting program on outcomes for the mothers showed reduction in a number of risk factors. Among women who had not graduated from high school when registered for the study, 59 percent of the nurse-visited and 27 percent of the comparison group had either graduated or enrolled in an educational program by six months postpartum.
Between birth and the 22-month follow-up, the nurse-visited, poor, unmarried older women had worked 2½ times longer than their counterparts in the control group, who were not nurse-visited. Qualitative analysis of the employment data indicated that by the 46-month interview, most of the women who worked held unskilled labor and service positions; some held semiskilled jobs; and a few were in clerical or sales positions. Nurse-visited, poor, unmarried older women reported that they received more help from other families with child care and were on public assistance 157 fewer days than the poor, unmarried older women in the control group, a 40 percent reduction. This effect, however, did not extend into the two-year period following the end of the intervention at 24 months postpartum. Subsequent pregnancies were reduced in the nurse-visited, poor, unmarried group, with the women having one third fewer subsequent pregnancies than the poor, unmarried women in the control group.
Programs Aimed at Occupational Stress and Job Loss
Work and unemployment represent areas of risk for adults. Occupational stress on the one hand and job loss on the other represent critical points for preventive intervention. Two preventive programs are described below, one aimed at a stressful work role, the other at vulnerable persons who have recently experienced job loss.
Occupational Stress and Coping
In work life and more generally, the beneficial and protective factors of social support on health are well documented (Israel and Rounds,
1987; Cohen and Wills, 1985; Berkman, 1984; House, 1981). Social support has been associated with longer life (Berkman, 1984), compliance with health regimens, higher levels of psychological well-being, decreased morbidity (Cohen and Wills, 1985; House, 1981), and more rapid recovery from serious physical illness and injury. In addition, a variety of studies have shown that social support can buffer the adverse consequences of stress. Although the mechanisms are not yet entirely understood, low levels of social support have been firmly established as a risk factor for poor mental and physical health (Berkman, 1984).
House (1981) and Thoits (1986) have suggested that social support can protect employees from the deleterious effects of exposure to unmodifiable or unavoidable work place stressors. Mechanisms through which social support may provide its positive effects include helping employees to modify stressful situations, develop new appraisals of stressful situations, and decrease the emotional upset associated with problematic situations.
The *Caregiver Support Program (Heaney, 1992) is a selective prevention program designed to help one particular occupational group, house managers and direct caregivers of the mentally ill and developmentally disabled in group homes. Caregivers work long hours on multiple and rotating shifts, with mental patients who are sometimes assaultive. Their job responsibilities include helping clients with activities for daily living, carrying out behavioral programming, accompanying clients on community outings, and coping with a variety of unscheduled demands and tasks, sometimes in relative social isolation. The low levels of social support, high levels of burden and work demands, and inadequate material and informational resources for coping with the task of caregiving all constitute risk factors for psychological distress (Heaney, 1992).
The Caregiver Support Program was designed to train house managers and caregivers to cope more effectively in their stressful work environment. Six weekly or biweekly training sessions, involving analysis and strengthening of social networks, developing effective staff training skills, and work group problem solving, as well as maintaining new skills and occupational self-esteem, were delivered to house managers and at least one other member of each group home support team. Training sessions were facilitated by a pair of trainers, and training protocols were highly specified and delivered with high reliability.
A randomized controlled trial evaluating the Caregiver Support Program showed changes in risk factors, with the strongest effects occurring as improvements in supervisor support, reductions in supervisor undermining, and higher levels of contact with and positive feedback from supervisors in the experimental group. In addition, the program
reduced depressive symptoms and somatization among employees most at risk for leaving their jobs.
As with many work place interventions where participation is voluntary, there is likely to be substantial variation in exposure to the actual intervention, even in a randomized experiment. Statistical models can estimate the interaction between characteristics associated with participation and actual exposure to the intervention to estimate experimental effects, but differential selection into or out of exposure to the intervention remains an issue. The effects of the intervention were probably reduced by the incomplete implementation associated with the “train-the-trainer” approach, in which only house managers and one direct care staff person per home were primarily exposed to the training intervention. Thus the effects of exposure to the Caregiver Support Program represent a lower-bound estimate of the program's impact.
Coping with Job Loss and Reemployment
There is substantial epidemiological evidence that unemployment is associated with higher levels of mental health problems, particularly symptoms of depressive and anxiety disorders (Kessler, Turner, and House, 1988). Furthermore, involuntary job loss is a stressful life event that produces a range of subsequent crises, including financial hardship and family conflict. Some epidemiological evidence suggests that in addition to higher levels of anxiety and depressive disorders, unemployment rates are associated with higher levels of alcohol abuse, child abuse, marital conflict, and a variety of other related mental health problems (Gordus, 1984). These data are of mixed quality, but more recent, community-based epidemiological studies by Kessler and colleagues indicate a higher relative risk of high levels of symptoms of depressive disorders and anxiety disorder in unemployed groups than in steadily employed groups (Kessler et al., 1988; Kessler, House, and Turner, 1987).
The process of job seeking itself is stressful, but the process can be enhanced by protective factors that reduce the likelihood of lowered motivation, discouragement, and prolonged unemployment. Such protective factors include the acquisition of effective job-seeking skills and strong social support during the job-seeking process.
The *JOBS Project for the Unemployed was a selective preventive intervention designed to help job losers cope with the stresses of job loss and setbacks in the job search process, as well as seek social support and develop and use job-searching skills leading to more rapid reemployment in high-quality jobs (Price, van Ryn, and Vinokur, 1992; Vinokur,
Schul, and Price, 1992; Caplan, Vinokur, Price, and van Ryn, 1989; Vinokur, van Ryn, Gramlich, and Price, 1991).
The intervention was based on the theory of self-efficacy; that is, the knowledge that one can succeed is a motivational force for attempting difficult behaviors. The target group for the JOBS intervention was recent job losers who had applied for unemployment insurance from the various offices of the Michigan Employment Security Commission. It was delivered to groups of 18 to 20 persons in the form of a training program with eight three-hour sessions over two weeks. Trainers were trained intensively before program delivery, and the intervention was monitored closely by observers during delivery. Pairs of trainers delivered a standard curriculum to job losers, including components on (1) skills training and support for dealing with obstacles to reemployment, (2) identifying sources of job leads, (3) finding job leads and social networks, (4) conducting an information interview, (5) handling emotions related to unemployment, (6) practicing and rehearsing interviews, (7) thinking like an employer, and (8) evaluating a job offer.
The impact of the JOBS project was evaluated in a randomized controlled trial. Two and one-half years after the completion of the randomized trial, people in the experimental group showed significant reductions in depressive symptoms (Price et al., 1992). Furthermore, participants obtained higher-paying jobs and higher-quality jobs, which resulted in higher income, and therefore higher tax revenues. The benefit-cost analysis results indicated that the cost of the intervention (approximately $300 per person) was rapidly offset by these increased tax revenues (Vinokur, van Ryn, Gramlich, and Price, 1991). Other analyses indicated that women in general and people with less education, who were at higher levels of disadvantage, benefited more from the JOBS intervention (Vinokur et al., 1992). Additional analyses indicated that the JOBS intervention was most successful with those people who were at highest risk for subsequent episodes of depressive symptoms.
The primary limitation of the JOBS project is that it was explicitly designed for and has been tested only on job losers in the context of the unemployment insurance offices. It is unclear whether the JOBS intervention can have similar impacts on other groups of unemployed persons who are not recent job losers, such as persons reentering the job market after long periods of time or for the first time or discouraged workers who are no longer seeking employment. A second limitation arises from the attempts to disseminate the intervention on a broad scale to assess how easily it can be adopted by other social service systems. It remains unclear whether it can be delivered with integrity in less well controlled circumstances.
A detailed intervention manual for the JOBS program is available. A more extensive replication of the research evaluating the impact of the JOBS program is currently under way, and a training manual for replicating the JOBS intervention and copies of research reports are also available.
Programs Aimed at Preventing Depressive Disorders Among Adults at Risk Because of Poverty and Minority Status
Depressive disorders, referred to here as depression, are a major health problem (see Chapter 5 and Chapter 6). Not only is depression one of the most common of the serious mental disorders, but, partly because of stigma and partly because of lack of knowledge regarding its symptoms and the availability of effective treatments, most persons who have the disorder do not receive treatment. This is especially true for certain ethnic minorities and those in poverty. How to reach and support these populations in effective ways represents a major challenge for prevention research and practice. Two pioneering efforts in this area are described below.
The prevalence of clinical depression is between 9 and 14 percent in the general population. Shapiro and colleagues indicated that only 20 percent of individuals meeting criteria for major depression get treatment from mental health specialists (Shapiro, Skinner, Kessler, Von Korff, German, Tischler et al., 1984). This major underutilization of services is even worse for certain groups, such as Hispanics. For example, in the UCLA Epidemiologic Catchment Area (ECA) sample, only 11 percent of Mexican Americans meeting diagnostic criteria for DSM-III disorders had sought mental health services, compared with 22 percent of similarly diagnosed non-Hispanic whites at the same site (Hough, Landsverk, Karno, Burnam, Timbers, Escobar, and Regier, 1987). Not only do certain minority groups underutilize services much more than others, but they also show higher levels of stressful life events and higher levels of depressive symptoms (Roberts, 1987).
Two of the earliest randomized trials investigating prevention of depression in adults included minorities as major segments of their samples. The *San Francisco Depression Prevention Research Project focused on public sector primary health care facilities as an ideal site for identifying individuals at risk for depression (Muñoz, Ying, Armas, Chan, and Gurza, 1987). Shapiro et al. (1984) found that although only 20 percent of depressed individuals sought mental health care, 75 percent sought other types of health care. Thus the prevalence of depression in primary care populations is much higher than in the
general population. It made sense, then, that persons who were at risk for depression would also seek help there. Given their medical and economic problems, some proportion of those seeking help would be nonsymptomatic but at risk, and others symptomatic but not yet over the threshold into a clinical episode of depression. This randomized controlled preventive trial screened primary care low-income medical patients, the majority of whom were members of ethnic minority groups, identified those who already met criteria for major depression or other mental disorders, and referred them for treatment. Those who did not meet DIS/DSM-III criteria, were not receiving mental health treatment, had been enrolled in the primary care clinic for at least six months, and spoke either English or Spanish were invited to participate in the randomized trial of this selective intervention.
The intervention consisted of a course in cognitive behavioral methods to gain greater control of mood. Doctoral-level psychologists were the instructors, and they followed a protocol (Muñoz and Ying, 1993a). A Spanish-language version was also used. Topics focused on (1) the nature of depression and social learning theory; (2) self-control approaches; (3) how thoughts, activities, and interpersonal interactions affect mood; and (4) how to identify and change those behaviors. The course was conducted in a small-group format with no more than 10 participants per group. The class intervention consisted of eight weekly two-hour sessions.
To date, this is the only randomized controlled prevention trial intended to test whether an intervention could prevent new clinical episodes of major depression. The impact of the prevention project was evaluated in a randomized trial comparing experimental and control group members at 6- and 12-month follow-up periods. Participants in the experimental group had significantly fewer depressive symptoms at both time points. At 12-month follow-up, 4 of the 72 control participants and 2 of the 67 experimental participants met DIS/DSM-III criteria for major depression. The low incidence did not allow sufficient statistical power to test whether the rate of new cases was significantly reduced.
Participants assigned to the experimental group showed the intended changes in the cognitions and behaviors hypothesized to be risk factors for depressive symptoms. Compared with the control group, those assigned to receive the depression prevention course became less pessimistic, had more positive (self-rewarding) and fewer negative (self-punishing) thoughts, and engaged in more pleasant and social activities at one or more follow-up assessment periods. In addition, reductions in negative thoughts and increases in levels of pleasant activity were shown to lead to reductions in depressive symptoms.
Prevention of depression might have additional benefits in terms of reducing utilization of unnecessary medical services. The Depression Prevention Research Project did not find significant differences in medical service utilization between the experimental and the control groups. Further analyses revealed that patients with higher levels of somatization had a greater number of medical visits as stressful life events increased than did nonsomatizers (Miranda and Pérez-Stable, 1993). This suggests that attempts to reduce medical service costs ought to focus on teaching somatizers to cope better with stress. Like most studies of depression, this project relied heavily on self-report data, and outcomes could be made more powerful by adding other sources of data, particularly on the relationship between mood changes and other domains of functioning, such as work or interpersonal relationships. A manual is available for this intervention (Muñoz, 1993a).
Vega and colleagues identified low-income immigrant women of Mexican heritage at consistently high risk for distress and depressive symptomatology (Vega, Valle, and Kolody, in press; Vega and Murphy, 1990; Vega, Valle, Kolody, and Hough, 1987). Ethnographic research identified natural support systems as critical to the well-being of this group. Specifically, the profile of risk that emerged involved both household and extrahousehold factors. Women in the target group typically were experiencing increased burdens and diminished resources, low control, and a sense of personal powerlessness because of chronic economic and social marginality. Their living conditions in families with husbands having unsteady employment or physical handicaps, and the responsibility of caring for large families, placed these women under substantial stress. In addition, most spoke only Spanish, and their social roles were limited to housekeeping.
Counterbalancing protective factors could be mobilized, however. Vega et al. (in press) indicated that emotional and material support, including resource redistribution, transportation, and translation assistance, are all key forms of social support in scarce supply for this population.
*Projecto Bienestar was aimed at reaching women who were at high risk for depression but currently had mild or no depressive symptomatology (Vega and Murphy, 1990; Vega, Valle, Kolody, and Hough, 1987). The rationale for the selective intervention (Roskin, 1982) argued that attempts to modify the environment by providing opportunities to strengthen individual capacities for coping with critical developmental tasks and unanticipated stressful circumstances could have preventive effects regarding the onset of depression.
Two types of interventions were provided. The first replicated the cultural style of natural helpers (Servidoras) found in low-income com-
munities of Southern California and was a one-to-one intervention carried out by these helpers in the community. These natural helpers were trained and supervised by project staff. The second intervention (Merienda educativa) was a peer group intervention organized and led by a Servidora. Each type of intervention consisted of 12 contacts, but actual exposure varied depending on the group.
Projecto Bienestar was evaluated in a randomized trial comparing the one-on-one and group interventions with a control group over the course of one year. In general, the Merienda group intervention showed significant effects that were nonlinear. The one-on-one intervention showed no effects. The results for the group intervention indicated no significant differences between women with low and high baseline levels of symptoms of depression and those in the control group. On the other hand, for women in the middle range of depression scores, the group intervention had clear positive effects, suggesting that there are strong and complex interactions between baseline depression levels and the effect of the preventive intervention. Nevertheless, for women whose baseline depression scores are at midlevel, the group intervention appears to be effective in preventing subsequent depressive symptoms.
The complexity of the findings suggests that this intervention should be tailored carefully, through screening or other means, to particular subpopulations of the general population in question. In addition, these results suggest that further analyses may reveal interesting and informative relationships between baseline depressive symptoms and preventive interventions.
Program Aimed at Supporting Adult Children Providing Care for Ill Parents
The stressful role of caregiving has been reported to have negative effects on physical (Golodetz, Evans, Heinritz, and Gibson, 1969), social (Cantor, 1983), and psychological well-being (Lawton and Maddox, 1985; Klein et al., 1977; Busse, 1976). Toseland (1990) has reviewed evidence suggesting that various supportive interventions for children of parents needing caregiving can have protective effects against the stresses associated with caregiving for chronic disorders. A variety of research suggests that both peer-led and professional-led support groups may be of value in reducing the stressors associated with chronic caregiving. The target group for these interventions consisted of the adult daughters and daughters-in-law who were the primary caregivers for their parents.
In Toseland, Rossiter, and Labrecque's (1989) preventive intervention, *Peer- and Professionally-Led Groups to Support Family Caregivers, groups of caregivers met for a total of eight weekly two-hour sessions. Both peer and professional leaders relied heavily on supportive interventions, including ventilation of stressful experiences, expressions of support, and understanding and affirmation of members' ability to cope.
The professional-led sessions followed a two-part protocol including education and discussion as well as problem-solving training. Topics in the education and discussion section included introduction to the support group, caregiver emotions, care receivers' reaction to illness, taking care of oneself, communication between caregivers and care receivers, community resources, medical needs, pharmacology, nursing home placement processes, and managing within the home. A problem solving component involved a six-step model including (1) identifying the problem, (2) anticipating its consequences, (3) identifying its antecedents, (4) generating alternative solutions, (5) evaluating the solutions, and (6) carrying out a plan. Peer-led sessions were less structured and used a self-help approach that emphasized mutual support, the sharing of common concerns, and free exchange of information.
The interventions were evaluated in a three-group randomized trial: (1) peer-led sessions, (2) professional-led sessions, and (3) control group. Both peer- and professional-led experimental groups produced increases in psychological well-being compared with the control condition. Participants in the experimental conditions also reported statistically significant differences with controls in their levels of psychiatric symptoms on the global severity index and the positive symptom index (Toseland, 1990). In addition, results favored the experimental groups in the areas of somatization, obsessive-compulsiveness, and phobic anxiety. Furthermore, participants in the experimental groups differed significantly from those in the control group in social support and in social support network size. Both peer-and professional-led experimental groups also showed higher levels of knowledge of community resources. The patterns of improvement did reflect, to some degree, the nature of the intervention. Peer-led groups spent more time socializing and sharing personal experiences and experienced higher levels of informal social support, whereas professional-led groups tended to focus more on highly structured skills and knowledge.
Follow-up after one year (Toseland, 1990) showed that both peer-led and professional-led experimental groups were more effective than the control group in helping caregivers of frail, older persons reduce the stress of pressing problems, increase formal and informal social supports, and make more personal changes in their caregiving role. The
experimental groups also reported higher levels of interpersonal competence, but the initial differences in mental health symptoms were not observed one year later, indicating that improvements in coping and competence may not be enough to prevent psychiatric symptoms.
Toseland (1990) and colleagues suggested several possibilities for improving the effectiveness of interventions for caregivers. For example, for those already experiencing debilitating psychiatric symptoms, psychotherapeutically oriented treatment interventions may be more appropriate. On the other hand, short-term improvements in social support could be sustained for caregivers without serious psychiatric symptoms if preventive interventions were incorporated by either extending weekly group sessions or making periodic booster sessions available. Local chapters of the Alzheimer's Disease and Related Disorders Association could sponsor such groups.
Findings and Leads
-
The Caregivers Support Program and the JOBS project both found that the interventions were most successful with people who were at highest risk. Projecto Bienestar was most effective, however, with women with midlevel depressive symptom scores. Interventions should be carefully tailored to groups in which they will have the most impact.
-
A practical implication of the findings on the JOBS project is that a preventive intervention that both reduces mental health problems and is cost-effective could be implemented at a relatively low cost. In addition, the benefit-cost analyses suggest that the intervention could pay for itself in higher levels of tax revenues in a relatively short period, clearly under one year.
-
As a general intervention for those at risk for depressive symptoms, the San Francisco Depression Prevention Project shows the key role of thoughts and activities, thus reinforcing a broad range of research on the relationship between cognitions, behaviors, and mood. The project demonstrates that randomized controlled trials with low-income, public sector primary care populations are feasible, these trials may include non-English-speaking persons, the prevalence of depressive symptoms is very high, and preventive interventions can reduce depressive symptoms. The next step is to carry out a randomized controlled trial with sufficient statistical power (see Muñoz, 1993b, Table 1) to adequately test whether onset of first episode of major depressive disorder can be prevented. Once a clinical episode has occurred, the probability of relapse is very high (see Chapter 5). Therefore research programs should concentrate on the prevention of the first episode.
-
The Perceived Personal Control Preventive Intervention Model (Caplan, 1977) is potentially applicable to a wide range of community institutions, including the general hospital. This model could be adapted to a variety of developmental transitions in which the enhancement of coping skills and personal control is important.
-
The Caregiver Support Program has been shown to increase coping resources and reduce stress-related symptoms in social service workers. Modifications in the Caregiver Support Program might include providing training to all members of work teams and developing organizational-level reward structures for successfully implementing the program concepts and skills.
-
When outcome data are limited to self-report measures, the full impact of the preventive program may not be known. Adding other sources of outcome data, such as from standardized tests or from family members or teachers of the participant, can increase the validity of the findings.
INTERVENTIONS FOR THE ELDERLY
Old age brings important changes in the social and biological life of the individual, including its own developmental tasks, risk factors, and a need for compensating protective factors. In older persons, work diminishes as a major source of stress and satisfaction, and new challenges emerge. Offspring leave the family, and for some older people the role of grandparent emerges. Retirement becomes a milestone for persons who earned their living outside the home. Perhaps most important, illness in oneself or in one's family or the death of a spouse or other loved ones may produce major life changes for the aging individual.
Developmental challenges that emerge in this period include caring for others, particularly a spouse, coping with severe and incapacitating illness in oneself or in loved ones, as well as coping with loss and death. In addition, maintaining meaningful roles and finding new social roles that give life meaning constitute an important but often ignored developmental task.
Accordingly, risk factors for the elderly include relationship loss and bereavement, chronic illness and caregiver burden, social isolation, and loss of meaningful social roles. On the other hand, protective factors include social support in a wide variety of forms—family, peers, informal relationships, more formal support groups, responsive health and social services such as respite care, and opportunities for new productive social roles.
The prevention programs reviewed in this section address (1) caregiver burden, an important potential risk factor for the elderly and (2) loss of a loved one or spouse, a risk factor that is almost inevitable for the elderly.
Evidence from a Quasi-Experimental Study: Relieving Caregiver Burden
Elderly caregivers of profoundly disabled elderly spouses and parents face major stressful burdens. Demographic trends make it clear that this burden will increase dramatically as we enter the twenty-first century. (For further discussion of caregiver burden, see the sections on Alzheimer's disease in Chapter 5 and Chapter 6.)
Caregivers are more likely than others to experience problems in the areas of social participation and psychological distress. Furthermore, the relationship between the patient and the caregiver, living arrangements, the caregiver's perceived adequacy of social support, and the caregiver 's gender are related to the probability of experiencing lower levels of well-being. As George and Gwyther (1988) observed, “there are no data suggesting that the stresses of caregiving place one at risk for psychiatric disorder as defined by conventional diagnostic criteria. Nonetheless, our research results suggest that caregivers are a group at risk for substantial psychological distress” (p. 317).
No randomized controlled trial data are available; most studies in this area have used quasi-experimental design. The Duke University Family Support Program (George and Gwyther, 1988; Gwyther and Brooks, 1983) is described here as an illustration of the work that currently exists. It is a quasi-experimental design in a longitudinal survey context. The program consisted of community support groups for the family caregivers and memory-impaired older adults. Three basic functions of support groups were identified: (1) Persons sharing a common problem frequently report the need for more information. Support groups are a potentially useful mechanism for information transfer and exchange. (2) In addition, support groups provide neutral support based on the fact that persons have experienced a specific problem and feel psychologically isolated. They can share experiences, coping strategies, and perhaps a sense of mutual understanding and validation. (3) Finally, support groups in some cases perform an advocacy function, mobilizing community support for their problem, and/or educating the community. This advocacy role can, itself, present therapeutic opportunities by augmenting the range of choices for self-efficacy.
Each family support program group had co-facilitators consisting of
one family caregiver and one professional service provider, who provided access to local agencies with physical and material resources as well as professional expertise. In addition, the development of one-to-one networks was specifically recommended by the family support program, consisting of dyadic relationships between caregivers with common interests.
In evaluating the intervention, George and Gwyther (1988) explicitly focused only on risk factors; they did not measure psychological well-being as an outcome of their intervention. They focused specifically on knowledge of Alzheimer's disease and related disorders, knowledge of available community-based services, use of the services, and feelings of being misunderstood and/or lonely. In addition, the study examined membership in the support group versus no membership.
The intervention had a strong effect on knowledge of Alzheimer's disease and knowledge of community services, but little effect on use of community services. Nevertheless, it also had strong effects on reduction of feelings of loneliness and feelings that no one understands the caregiver's situation. Longitudinal analyses of results substantially confirmed these initial cross-sectional findings with few exceptions. Future studies would benefit from more rigorous methodological design and inclusion of psychological measures of outcomes. A manual for this program is available (Gwyther and Brooks, 1983). In North Carolina, the manual has been supplemented by training sessions for the support group leaders, called support group facilitators.
Other forms of assistance are also needed to ease caregiver burden. Respite care is the service that caregivers desire most but is least available. Respite care involves temporary relief from the responsibility of caregiving and can be delivered as an in-home, day center, or institutional service for periods of time ranging from a few hours to a few days.
Programs Aimed at Enhancement of Coping with Widowhood and Bereavement
Bereavement is a life event that deserves serious attention in understanding the mental health of persons of all ages (IOM, 1984). Widowhood and bereavement will affect increasingly large groups of the elderly in the coming years. Widows and widowers experience grief, including feelings of sadness, despair, anger, and guilt. They also experience feelings of profound disruption as well as the role loss associated with losing a spouse. After the immediate needs following the death of a spouse have been met, including funeral arrangements,
legal arrangements, immediate social service arrangements, and the initial support from loved ones, the widow or widower is often left alone and is expected by others to recover rapidly. This period of transition, from six weeks to two months after the death, appears to be more difficult than the period immediately following the death.
Many bereaved people will live many more years after their loss, and some are at risk for a variety of problems. Bereavement has been studied extensively as a risk factor, and Marris's (1958) and Parkes 's (1965) early epidemiological work suggests that bereavement reactions can increase the risk of depression. Epidemiological research also indicates that conjugal bereavement is associated with higher risk for elevated levels of physical deterioration and death (Lieberman and Videka-Sherman, 1986). In addition, widows and widowers are more likely than single or married peers to be socially isolated, to live in poverty, to be emotionally troubled, and to have fewer meaningful social activities (IOM, 1984).
Protective factors for the bereaved include emotional and social support, higher levels of social engagement and interaction, formation of meaningful new social roles, as well as the opportunity in mutual-help groups for the catharsis and interaction that can lead to personal insight.
*Widow-to-Widow: A Mutual Help Program for the Widowed, developed by Silverman (1988) as a service program, involves recruiting widowed aides who have some perspective on their own grief and who are in a position to reach out to other widowed persons in their transition state. Widowed helpers were recruited by word of mouth and through local community action programs. Identification of the newly widowed was done through funeral directors, who became involved in Widow-to-Widow programs as sponsors and served on advisory boards. Outreach typically began with a first contact two months after the death. Initial contact was by mail, and the initial social visits later evolved into group discussions.
Vachon and colleagues evaluated the Widow-to-Widow program in a research trial in Toronto (Vachon, Sheldon, Lancee, Lyall, Roger, and Freeman, 1982, 1980; Vachon, 1979). They randomly assigned 162 newly widowed women to control and experimental groups. The intervention consisted of one-to-one support by another widow, practical help in locating community resources, and small group meetings. The intervention was not limited to any predefined duration or phase of bereavement.
Widows who participated in the program were more apt to have begun new relationships and activities and did so more quickly. They also experienced fewer depressive symptoms on a psychiatric screening
instrument than women in the control group. This was particularly true for women who experienced high stress immediately after the death of their spouse. Over the two years of the randomized trial, most women recovered with or without help; however, those receiving the intervention recovered more quickly (Vachon et al., 1980).
The Widow-to-Widow program focused almost exclusively on widowed women. Presumably, such a mutual support program could also be useful for widowed men. Randomized trials of this form of support would provide information about the range of impact of the program and about subgroups at higher risk who could be more likely to benefit from the intervention, but few have been conducted.
The Widow-to-Widow program model seems already to have been widely disseminated through such organizations as the American Association of Retired Persons (AARP). Careful trials to assess which program models would be particularly well suited for dissemination, which individuals would be most likely to benefit, and whether depressive disorders are prevented would be important next steps in the development of these programs.
Evidence from a Quasi-Experimental Study: Mutual-Help Groups for Widowed Persons
THEOS, a national network of self-help groups that aid widowed persons, was the vehicle used to reach widows and widowers in a preventive program addressing issues of bereavement (Lieberman and Videka-Sherman, 1986). The research design, which was complex but quasi-experimental, compared participants in the mutual-help program (experimental group) to a probability sample of widowed persons in a longitudinal data set (comparison group). The experimental group showed improved mental health status over a one-year period, whereas the control group showed deterioration on all mental health measures except depression.
In addition, experimental group members who made strong social linkages in THEOS showed more positive changes on six of the eight mental health measures (depression, anxiety, somatic symptoms, well-being, self-esteem, and mastery) than those who attended meetings but did not develop other social linkages within THEOS.
These results were checked by examining whether high-participation experimental group members were different in other important ways, including having special aptitudes and skills that would account for the establishment of their new social linkages. No important differences were found, with the possible exception that low meeting attenders had
somewhat lower need-for-affiliation scores. In short, a variety of risk factors associated with social isolation appeared to have been reduced by participation in THEOS mutual-help intervention, and a number of measures of precursor symptoms of mental disorders showed improvement in comparison with a control group.
Lieberman and Videka-Sherman (1986) pointed out that their analyses strongly suggest that the mere passage of time could not account for the positive changes observed in the high-participation experimental members. Nor did improvements in mental health scores appear to be simply the result of attendance. Instead, a particular type of high-intensity mutual support involvement appeared to be the active mechanism of the intervention.
Findings and Leads
-
The Widow-to-Widow program was most successful with those women who experienced high stress immediately after the death of their spouse. This result suggests increased targeting of this high-risk group. Trials are needed to determine whether depressive disorders can be prevented.
-
A variety of naturally occurring mutual-help groups could be rigorously evaluated to assess their preventive potential, particularly when the mutual-help groups are aimed at aiding persons in coping with major life transitions, losses, illnesses, or stigmatizing experiences.
A NEW GENERATION OF DEVELOPMENTAL STUDIES
Recently, a new generation of preventive intervention research studies have been designed and supported by federal, state, and private sources. These studies have adhered to high methodological standards and hold great promise for identifying causality and malleability of individual and combined risk factors, demonstrating efficacy and effectiveness of single- or multiple-component interventions, and assessing not only reduction of risk factors but also reduction of incidence of mental disorders. Because this work is still in progress, the programs are not reviewed here, but the project titles and investigators are included in the reference list. Some of the research to note over the next decade will come from investigators such as D. Cicchetti, whose work focuses on preventing developmental problems in children with depressed mothers; B. Egeland, whose work is with children of high-risk mothers; D. Olds, who is replicating the Prenatal/Early Infancy Project in Memphis with a different high-risk sample; J. Coie and N. Guerra, whose
prevention demonstration projects to prevent conduct disorder point the way for combining research methodologies with service programs; T. Field, whose work with high-risk mothers and their babies is showing psychological and physiological benefits from the therapeutic use of touch; W. Beardslee, whose aim is to prevent depression in children and adolescents who have been exposed to parental depression; J. Reid and C. Webster-Stratton, who in separate indicated prevention programs are pushing the boundaries with children who have precursor symptoms of conduct disorder through the application of techniques that have proved successful in treatment settings; and G. Clarke, whose school-based interventions are yielding the first data on prevention of major depressive disorders among adolescents at high risk for depression.
MAJOR FINDINGS AND PROMISING LEADS
-
Although their numbers are relatively small, some excellent illustrations of preventive interventions are available. These illustrations point the way toward further work by highlighting successes as well as problems. The design of new prevention programs should consider such illustrations and adapt methodologies and strategies for intervention accordingly.
-
There are data that clearly show that preventive interventions can reduce risk factors that are associated with the onset of many mental disorders. However, as yet, there is no evidence that preventive interventions reduce the incidence of mental disorders. Risk reduction findings are encouraging about the eventual prevention of the initial onset of some disorders, such as major depressive disorder and alcohol abuse.
-
The criteria presented here for the assessment of prevention programs that have been completed and published can be a guide for researchers, practitioners, and policymakers as they make critical decisions for this field.
-
Although there are numerous prevention service programs throughout the life span, most prevention research programs are targeted to the needs of infants, preschoolers, elementary-age children, and adolescents. There is a nationwide and unfortunate lack of prevention research programs targeted to the needs of adults, especially the elderly.
-
Although there are excellent reasons to target an intervention for a specific age or stage of life, and for a particular disorder or problem, there is usually no single intervention at a single point in time that accomplishes comprehensive goals of prevention for a lifetime. The
-
ultimate goal to achieve optimal prevention should be to build the principles of prevention into the ordinary activities of everyday life and into community structures to enhance development over the entire life span. This would include promoting consensual community values and norms.
-
Attention should be given to the potential risks of short-term interventions that are beneficial but are then curtailed or terminated.
-
Many prevention programs clearly demonstrate that education, physical health care, employment, and mental health care are not separable. Improvements in one area can affect other areas. A logical extension of this finding is support for collaboration among the agencies and institutions in these domains.
-
Risk factors can occur in single or multiple domains, such as home, school, peer group, neighborhood, or work site. When risk factors occur in multiple domains, interventions are required in all of them. Prevention programs from infancy to adolescence have clearly demonstrated the feasibility of multidomain interventions.
-
Risk factors can also occur across generations in the same family. The Prenatal/Early Infancy Project has clearly shown that positive outcomes can be secured for both infants and their mothers from a single comprehensive interaction. Prevention programs should take advantage of opportunities to reduce risks, assess outcomes, and compare benefits and costs for members of different generations within a household, such as adult children serving as caregivers for disabled parents.
-
Many prevention research programs have similar methodological complications: difficulty in adhering to a strict randomized controlled trial design; high attrition of participants; lack of documentation of fidelity in delivering the intervention; lack of multiple measures of outcomes from multiple sources; and insufficient long-term follow-up, which can prevent the collection of outcome data on incidence of multiple disorders.
-
Some prevention programs get scaled up into field trials or quickly become translated into service programs. Others that have positive outcomes and seem to be equally well designed, however, do not. One factor that contributes to the difference is marketing, such as encouraging a school or an agency to use a new program.
-
Social competence enhancement has been shown to be a successful intervention with young children. Social competence programs have extended the basic social competence curriculum of Shure and Spivack to address stressors and interpersonal challenges of different developmental periods. Social competence interventions should probably be
-
included in risk reduction interventions seeking to strengthen resilience in populations at risk for early behavior problems. Again, however, it is important to note that to date, the long-term preventive effects of such interventions on the incidence of most mental disorders is unknown and follow-up studies are needed.
-
Prevention research suggests the importance of using interventions beginning in the preschool and elementary age periods to create normative consensual behavior regarding substance use and bullying. With such early intervention, those at risk might be hypothesized to be more committed to the normative standards of the larger community and to be less likely to violate widely shared community standards for behavior.
-
The combined evidence suggests that some proportion of conduct disorder may be preventable. Developmentally adjusted interventions in early childhood, during the elementary grades, and in adolescence have been tested and have, in isolated experiments and with some confirmatory data from quasi-experimental studies, shown modest but statistically significant effects in preventing later delinquent behaviors and related indicators of conduct disorder during adolescence. Few of these preventive interventions have used diagnostic criteria to ascertain effects on the incidence of the disorder. Nevertheless, there is promise in several components, including early childhood education, parent training, enhancement of social and academic competence, and school curricula promoting consensual norms antithetical to risk behavior for disorder, such as substance use.
-
Interventions that have been highly successful at certain developmental stages, such as home visiting with families with infants and preschoolers, might also be useful at other stages of the life span, such as with the elderly, who may be homebound, and single parents or dual-career parents who cannot work another scheduled event into their lives.
-
Service programs can provide good leads regarding intervention, community context, and exchange of ideas. Such programs can also be brought into the preventive intervention research cycle and tested for their effectiveness in reducing psychological symptoms and mental disorders. For example, Healthy Start in Hawaii and Homebuilders provide excellent ideas.
-
The combined evidence suggests that a number of programs have successfully focused on prevention of depressive symptoms in adults and the elderly, but data on the prevention of the first episode of major depressive disorder are not yet available, in part because of inadequate sample sizes in preventive trials.
-
In general, research on preventive interventions that emphasize an ecological perspective has been neglected. As yet, there are no communitywide prevention research programs that target multiple age groups and attempt to change community norms. Such research has special issues, such as difficulty in randomization. However, for some problems, it may be necessary to foster new consensual values and norms in neighborhoods and communities. Beginning work in the areas of substance abuse and alcohol prevention and in Olweus's program to reduce bullying shows promise.
-
Even though biological risk factors have a significant role in the onset of mental disorders, there are few prevention programs other than prenatal care and childhood immunizations that address these factors. As knowledge grows in this area over the next decade, growth in the number of programs addressing these factors is expected.
-
Changes in laws and pricing have affected the availability of alcohol and appear to be successful in the prevention of alcohol use. There are also some data to suggest that peer-led didactic curricula can reduce and prevent alcohol use.
-
Many prevention research programs are most successful with the individuals within the sample who are at highest risk, but there are many exceptions. Much remains to be learned about tailoring interventions to groups in which they will have the most impact. Consideration will need to be given to benefit-cost issues as well as the potential harmful effects of screening and labeling individuals as being at risk.
REFERENCES
Alexander, J. F.; Parsons, B. V.( 1980) Functional Family Therapy. Monterey, CA: Brooks/Cole Publishing.
Alexander, J. F.; Parsons, B. V.( 1973) Short-term behavioral intervention with delinquent families: Impact on family process and recidivism. Journal of Abnormal Psychology; 18: 219–225.
Alpert-Gillis, L. J.; Pedro-Carroll, J. L.; Cowen, E. L.( 1989) The Children of Divorce Intervention Program: Development, implementation, and evaluation of a program for young urban children. Journal of Counseling and Clinical Psychology; 57: 583–589.
Andrews, S. R.; Blumenthal, J. B.; Johnson, D. L.; Kahn, A. J.; Ferguson, C. J.; Lasater, T. M.; Malone, P. E.; Wallace, D. B.( 1982) The skills of mothering: A study of Parent-Child Development Centers . Monographs of the Society for Research in Child Development, 47; 6, Serial No. 198.
Baumrind, D.( 1983) Why adolescents take chances—and why they don't. Paper presented at the National Institute for Child Health and Human Development, Bethesda, MD.
Beardslee, W. R. (Judge Baker Children's Center, Boston, MA). “Prevention for Families with Affective Disorder.” National Institute of Mental Health Grant No. RO1 MH48696.
Beardslee, W. R.; Hoke, L.; Wheelock, I.; Rothberg, P. C.; van de Velde, P.; Swatling, S.( 1992) Preventive intervention for families with parental affective disorders: Initial findings. American Journal of Psychiatry; 149(10): 1335–1340.
Beardslee, W. R.( 1990) Development of a clinician-based preventive intervention for families with affective disorders. Journal of Preventive Psychiatry and Allied Disciplines; 4: 39–61.
Beardslee, W. R.; Salt, P.; Porterfield, K.; Rothberg, P. C.; van de Velde, P.; Swatling, S.; Hoke, L.; Moilanen, D. L.; Wheelock, I.( 1993) Comparison of preventive interventions for families with parental affective disorder. Journal of the American Academy of Child and Adolescent Psychiatry ; 32(2): 254–263.
Berkman, L. F.( 1984) Assessing the physical health effects of social networks and social support. Annual Review of Public Health; 5: 413–432.
Berrueta-Clement, J. R.; Schweinhart, L. J.; Barnett, W. S.; Epstein, A. S.; Weikart, D. P.( 1984) Changed Lives: The Effects of the Perry Preschool Program on Youths Through Age 19 (High/Scope Educational Research Foundation, Monograph 8). Ypsilanti, MI: High/Scope Press.
Bierman, K. L.( 1986) Process of change during social skills training with preadolescents and its relation to treatment outcomes. Child Development; 57: 230–240.
Bloom, B. L.( 1985) University of Colorado Separation and Divorce Program: A program manual. Washington, DC: Government Printing Office; DHHS Pub. No. (ADM) 88–1556.
Bloom, B. L.; Asher, S. J.; White, S. W.( 1978) Marital disruption as a stressor: A review and analysis. Psychological Bulletin; 85: 867–894.
Bloom, B. L.; Hodges, W. F.( 1988) The Colorado Separation and Divorce Program: A preventive intervention program for newly separated persons. In: R. H. Price, E. L. Cowen, R. P. Lorion, and J. Ramos-McKay, Eds. Fourteen Ounces of Prevention: A Casebook for Practitioners. Washington, DC: American Psychological Association.
Bloom, B. L.; Hodges, W. F.; Caldwell, R. A.( 1982) A preventive program for the newly separated: Initial evaluation. American Journal of Community Psychology; 10(3): 251–264.
Bloom, B. L.; Hodges, W. F.; Kern, M. B.; McFaddin, S. C.( 1985) A preventive intervention program for the newly separated. American Journal of Orthopsychiatry; 55: 9–26.
Botvin, G. J.; Baker, E.; Filazzola, A. D.; Botvin, E. M.( 1990a) A cognitive-behavioral approach to substance abuse prevention: One-year follow-up. Addictive Behaviors; 15: 47–63.
Botvin, G. J.; Baker, E.; Tortu, S.; Botvin, E. M.( 1990b) Preventing adolescent drug abuse through a multimodal cognitive-behavioral approach: Results of a 3-year study. Journal of Consulting and Clinical Psychology; 58: 437–446.
Bronfenbrenner, U.( 1979) The Ecology of Human Development: Experiments by Nature and Design . Cambridge, MA: Harvard University Press.
Brophy, J.; Good, T. L.( 1986) Teacher behavior and student achievement. In: M. C. Wittrock, Ed. Handbook of Research on Training. 3rd ed. New York, NY: Macmillan Press; 328–375.
Bry, B. H.( 1982) Reducing the incidence of adolescent problems through preventive intervention: One- and five-year follow-up. American Journal of Community Psychology; 10: 265–276.
Busse, E. W.( 1976) Hypochondriasis in the elderly: A reaction to stress. Journal of American Geriatrics Society; 24: 145–149.
Cantor, M.( 1983) Strain among caregivers: A study of experience in the U.S. The Gerontologist; 23: 556–561.
Caplan, G.( 1977) Support systems and community mental health. Paper presented at a seminar at Harvard University: Boston, MA.
Caplan, G.; Killilean, M.( 1976) Support Systems and Mutual Help: Multidisciplinary Explorations. New York, NY: Grune & Stratton.
Caplan, M.; Weissberg, R. P.; Grober, J. S.; Sivo, P. J.; Grady, K.; Jacoby, C.( 1992) Social competence promotion with inner-city and suburban young adolescents: Effects on social adjustment and alcohol use. Journal of Consulting and Clinical Psychology; 60: 56–63.
Caplan, R. D.; Vinokur, A. D.; Price, R. H.; van Ryn, M.( 1989) Job seeking, reemployment and mental health: A randomized field experiment in coping with job loss. Journal of Applied Psychology; 74(5): 759–769.
Carnegie Council on Adolescent Development.( 1989) Turning Points: Preparing American Youth for the 21st Century. Washington, DC: Carnegie Corporation.
Carnine, D.; Carnine, L.; Karp, J.; Weissberg, P.( 1988) Kindergarten for economically disadvantaged children: The direct instruction component. In: C. Warger, Ed. A Resource Guide to Public School Early Childhood Programs. Alexandria, VA: Association for Supervision and Curriculum Development; 73–78.
Cauce, A. M.; Comer, J. P.; Schwartz, D.( 1987) Long-term effects of a systems-oriented school prevention program . American Journal of Orthopsychiatry; 57: 127–131.
CDC (Centers for Disease Control).( 1992) Early childhood vaccination levels among urban children—Connecticut 1990 and 1991. Mortality & Morbidity Weekly Report; 40: 888–891.
CDC (Centers for Disease Control).( 1991) Measles vaccination among selected groups of pre-school children—United States. Mortality & Morbidity Weekly Report; 40: 36–39.
CDC (Centers for Disease Control).( 1990) 1989 Update: Measles outbreak, Chicago, 1989. Mortality & Morbidity Weekly Report; 39(319): 325–326.
Center for the Study of Social Policy with The Annie E. Casey Foundation .( 1992) Kids Count Data Book. Washington, DC: Center for the Study of Social Policy.
Cicchetti, D. (University of Rochester, Rochester, NY). “Preventive Intervention for Toddlers of Depressed Mothers.” National Institute of Mental Health Grant No. RO1 MH45027.
Clarke, G. (Oregon Health Sciences University, Eugene, OR). “School Based Prevention of Adolescent Depression.” National Institute of Mental Health Grant No. RO3 MH48118–02.
Cohen, J.( 1988) Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates.
Cohen, N. W.( 1977) Minimizing emotional sequelae of caesarean childbirth. Birth and Family Journal; 4: 114–119.
Cohen, S.; Wills, T. A.( 1985) Stress, social support, and the buffering hypothesis. Psychological Bulletin; 98: 310–357.
Coie, J. (Duke University, Durham, NC). “Multi-Site Prevention of Conduct Disorder.” National Institute of Mental Health Grant No. RO1 MH48043.
Coie, J.; Krehbiel, G.( 1984) Effects of academic tutoring on the social status of low-achieving, socially rejected children. Child Development; 55: 1465–1478.
Coie, J.; Hawkins, J. D.; Ramsey, S.; Watt, N.( 1991) Prevention research: Conceptual model of strategies and procedures . Paper presented at the National Prevention Conference, June 1991, Washington, DC.
Comer, J. P.( 1988) Educating poor minority children. Scientific American; 259(5): 42–48.
Comer, J. P.( 1985) The Yale-New Haven Primary Prevention Project: A follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry ; 24(2): 154–160.
Cook, P. J.; Tauchen, G.( 1984) The effect of minimum drinking age legislation on youthful auto fatalities, 1970–1977. Journal of Legal Studies; 13: 169–190.
Cook, P. J.; Tauchen, G.( 1982) The effect of liquor taxes on heavy drinking. Bell Journal of Economics; 13: 379–390.
Cutts, F. T.; Zell, E. R.; Mason, D.; Bernier, R. H.; Dini, E. F.; Orenstein, W. A.( 1992) Monitoring progress toward U.S. preschool immunization goals. Journal of the American Medical Association; 267: 1952–1955.
DHHS (Department of Health and Human Services).( 1991) Healthy People 2000: National Health Promotion and Disease Prevention Objectives. Washington, DC: Government Printing Office; DHHS Pub. No. (PHS) 91–50212.
Donovan, B.( 1977) The Caesarean Birth Experience: A Practical, Comprehensive and Reassuring Guide for Parents and Professionals. Boston, MA: Beacon Press.
Dumas, J. D.( 1989) Treating antisocial behavior in children: Child and family approaches . Clinical Psychology Review; 1: 197–222.
Egeland, B. (University of Minnesota, Minneapolis, MN). “An Evaluation of STEEP: A Program for High-Risk Mothers.” National Institute of Mental Health Grant No. RO1 MH41879.
Elias, M. J.; Gara, M.; Schuyler, T.; Brandon-Muller, L. R.; Sayette, M. A.( 1991) The promotion of social competence: Longitudinal study of a preventive school-based program. American Journal of Orthopsychiatry; 61: 409–417.
Elias, M. J.; Gara, M.; Ubrlaca, M.; Rothbaum, P. A.; Clabby, J. F.; Schuyler, T.( 1986) Impact of a preventive social problem intervention on children's coping with middle-school stressors. American Journal of Community Psychology; 14: 259–275.
Ellickson, P. L.; Bell, R. M.( 1990) Drug prevention in junior high: A multi-site longitudinal test. Science; 247: 1299–1305.
Elliott, D. S.; Huizinga, D.; Menard, S.( 1989) Multiple Problem Youth: Delinquency, Substance Use and Mental Health Problems. New York, NY: Springer-Verlag.
Emshoff, J. G.( 1990) A preventive intervention with children of alcoholics. Prevention in Human Services; 7(1): 225–254.
Farrington, D. P.; Loeber, R.; Elliott, D. S.; Hawkins, J. D.; Kandel, D. B.; Klein, M. W.; McCord, J.; Rowe, D. C.; Tremblay, R. E.( 1990) Advancing knowledge about the onset of delinquency and crime. In: B. B. Lahey and A. E. Kazdin, Eds. Advances in Clinical Child Psychology. Vol. 13. New York, NY: Plenum Press; 283–342.
Feldman, L. H.( 1991a) Assessing the effectiveness of family preservation services in New Jersey within an ecological context. New Jersey Division of Youth and Family Services: Bureau of Research, Evaluation and Quality Assurance.
Feldman, L. H.( 1991b) Evaluating the impact of intensive family preservation services in New Jersey. In: D. E. Biegel and K. Wells, Eds. Family Preservation Services: Research and Evaluation. Newbury Park, CA: Sage Publications; 47–71.
Felner, R. D.; Adan, A. M.( 1988) The School Transitional Environment Project: An Ecological Intervention and Evaluation. In: R. Price, E. L. Cowen, R. P. Lorion, and J. Ramos-McKay, Eds. Fourteen Ounces of Prevention: A Casebook for Practitioners. Washington, DC: American Psychological Association; 111–122.
Felner, R. D.; Ginter, M.; Primavera, J.( 1982) Primary prevention during school transitions: Social support and environmental structure. American Journal of Community Psychology; 10: 277–290.
Field, T. (University of Miami, Miami, FL). “Preventing Depression in Infants of Depressed Mothers.” National Institute of Mental Health Grant No. R37 MH46586.
Field, T. M.; Schanberg, S. M.; Scafidi, F.; Bauer, C. R.; Vega-Lahr, N.; Garcia, R.; Nystrom, J.; Kuhn, C. M.( 1986) Tactile/kinesthetic stimulation effects on preterm neonates. Pediatrics; 77(5): 654–658.
Field, T. M.; Widmayer, S. M.; Stringer, S.; Ignatoff, E.( 1980) Teenage, lower-class, black mothers and their preterm infants: An intervention and developmental follow-up. Child Development; 51(2): 426–436.
Fraser, M. W.; Hawkins, J. D.; Howard, M. O.( 1988) Parent training for delinquency prevention. Child and Youth Services; 11: 93–125.
George, L. K.; Gwyther, L. P.( 1988) Support group for caregivers of memory-impaired elderly: Easing caregiver burden. In: L. A. Bond and B. M. Wagner, Eds. Families in Transition: Primary Prevention Programs That Work. Newbury Park, CA: Sage Publications; 309–331.
Golodetz, A.; Evans, R.; Heinritz, G.; Gibson, C.( 1969) The care of chronic illness: The responsor role. Medical Care; 7: 385–394.
Gordus, J. P.( 1984) Coping with unemployment: I. The trainers' guide. Industrial Development Division, Institute of Science and Technology, The University of Michigan. Unpublished paper.
Gottfredson, D. C.( 1988) An evaluation of an organization development approach to reducing school disorder. Evaluation Review; 11: 739–763.
Gottfredson, D. C.( 1986) An empirical test of school-based environmental and individual interventions to reduce the risk of delinquent behavior. Criminology; 24: 705–731.
Gottfredson, D. C.; Gottfredson, G. D.( 1992) Theory-guided investigation: Three field experiments. In: J. McCord and R. E. Tremblay, Eds. Preventing Antisocial Behavior: Interventions from Birth Through Adolescence. New York, NY: Guilford Press; 311–329.
Gottfredson, D. C.; Karweit, N. L.; Gottfredson, G. D.( 1989) Reducing Disorderly Behavior in Middle Schools. Baltimore, MD: Center for Research on Elementary and Middle Schools.
Gottfredson, G. D.( 1984) A theory-ridden approach to program evaluation. American Psychologist; 39: 1101–1112.
Gottman, J. G.; Markman, H. J.; Notarius, C. I.( 1977) The topography of marital conflict: A sequential analysis of verbal and nonverbal behavior. Journal of Marriage and the Family; 46: 461–478.
Grych, J. H.; Fincham, F. D.( 1992) Interventions for children of divorce: Toward greater integration of research and action. Psychological Bulletin; 111: 434–454.
Guerra, N. (University of Illinois at Chicago). “Preventing the Emergence of Anti-Social Behavior in High-Risk Children. ” National Institute of Mental Health Grant No. R18 MH48034.
Gwynn, C.; Brantley, H.( 1987) Effects of a divorce group intervention for elementary school children . Psychology in the Schools; 24: 161–164.
Gwyther, L. P.; Brooks, B.( 1983) Mobilizing networks of mutual support: How to develop Alzheimer caregivers ' support groups. Durham, NC: Duke University Center of the Study of Aging and Human Development .
Hamburg, D. A.( 1992) Today's Children: Creating a Future for a Generation in Crisis. New York, NY: Times Books.
Hansen, W. B.( 1992) School-based substance abuse prevention: A review of the state of the art in curriculum, 1980–1990. Health Education Research; 7: 403–430.
Hansen, W. B.; Graham, J. W.( 1991) Preventing alcohol, marijuana, and cigarette use among adolescents: Peer pressure resistance training versus establishing conservative norms. Preventive Medicine; 20: 414–430.
Hansen, W. B.; Johnson, C. A.; Flay, B. R.; Graham, J. W.; Sobel, J.( 1988) Affective and social influence approaches to the prevention of multiple substance abuse among seventh grade students: Results from Project SMART. Preventive Medicine; 17: 135–154.
Hausman, A. J.; Spivak, H.; Prothrow-Stith, D.; Roeber, J.( 1992) Patterns of teen exposure to a community-based violence prevention project. Journal of Adolescent Health; 13: 668–675.
Hawkins, J. D.; Catalano, R. F.( 1992) Communities That Care: Action for Drug Abuse Prevention. San Francisco, CA: Jossey-Bass Publications.
Hawkins, J. D.; Catalano, R. F.; Jones, G.; Fine, D.( 1987) Delinquency prevention through parent training: Results and issues from work in progress. In: J. Wilson and G. Loury, Eds. Children to Citizens: Families, Schools, and Delinquency Prevention . Vol. 3. New York, NY: Springer-Verlag; 186–204.
Hawkins, J. D.; Catalano, R. F.; Miller, J. R.( 1992) Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin; 112(1): 64–105.
Hawkins, J. D.; Catalano, R. F.; Morrison, D. M.; O'Donnell, J.; Abbott, R. D.; Day, L. E.( 1992) The Seattle Social Development Project: Effects of the first four years on protective factors and problem behaviors. In: J. McCord and R. Tremblay, Eds. The Prevention of Antisocial Behavior in Children. New York, NY: Guilford Press.
Hawkins, J. D.; Doueck, H. J.; Lishner, D. M.( 1988) Changing teaching practices in mainstream classrooms to improve bonding and behavior of low achievers. American Educational Research Journal; 25: 31–50.
Hawkins, J. D.; Lam, T.( 1987) Teacher practices, social development, and delinquency. In: J. D. Burchard and S. N. Burchard, Eds. Prevention of Delinquent Behavior. Newbury Park, CA: Sage Publications; 241–274.
Heaney, C. A.( 1992) Enhancing social support at the workplace: Assessing the effects of the Caregiver Support Program. Health Education Quarterly; 18(4): 477–494.
Hinman, A. R.( 1988) Public health considerations. In: S. A. Plotkin and E. A. Mortimer Jr., Eds. Vaccines. Philadelphia, PA: W. B. Saunders; 587–611.
Hinman, A. R.; Koplan, J. R.( 1985) Pertussis and pertussis vaccine: Further analysis of benefits, risks and costs. Developmental Biology Standards; 61: 429–437.
Hohmann, M.; Banet, B.; Weikart, D. P.( 1979) Young Children in Action: A Manual for Preschool Educators. Ypsilanti, MI: High/Scope.
Holder, H. D.; Blose, J. O. (1987) Impact of changes in distilled spirits availability on apparent consumption; A time series analysis of liquor-by-the-drink. British Journal of Addiction; 82: 623–631.
Horacek, H. J.; Ramey, C. T.; Campbell, F. A.; Hoffman, K. P.; Fletcher, R. H.( 1987) Predicting school failure and assessing early intervention with high-risk children. Journal of the American Academy of Child and Adolescent Psychiatry ; 26: 758–763.
Hough, R. L.; Landsverk, J. A.; Karno, M.; Burnam, M. A.; Timbers, D. M.; Escobar, J. I.; Regier, D. A.( 1987) Utilization of health and mental health services by Los Angeles Mexican Americans and non-Hispanic whites. Archives of General Psychiatry; 44: 702–709.
House, J. S.( 1981) Work Stress and Social Support. Reading, MA: Addison-Wesley.
Infant Health and Development Program.( 1990) Enhancing the outcomes of low birthweight premature infants: A multi-site randomized trial. Journal of the American Medical Association; 263: 3035–3042.
IOM (Institute of Medicine).( 1988) Prenatal Care: Reaching Mothers, Reaching Infants. Washington, DC: National Academy Press.
IOM (Institute of Medicine).( 1985) Preventing Low Birthweight. Washington, DC: National Academy Press.
IOM (Institute of Medicine).( 1984) Bereavement: Reactions, Consequences and Care. Washington, DC: National Academy Press.
Israel, B. I.; Rounds, K. A.( 1987) Social networks and social support: A synthesis for health educators . Advances in Health Education and Promotion; 2: 311–351.
Jessor, R.( 1993) Successful adolescent development among youth in high-risk settings . American Psychologist; 48(2): 117–126.
Jessor, R.; Jessor, S. L.( 1977) Problem Behavior and Psychosocial Development: A Longitudinal Study of Youth. New York, NY: Academic Press.
Johnson, C. A.; Pentz, M. A.; Weber, M. D.; Dwyer, J. H.; Baer, N. A.; MacKinnon, D. P.; Hansen, W. B.; Flay, B. R.( 1989) Relative effectiveness of comprehensive community programming for drug abuse prevention with high-risk and low-risk adolescents. Journal of Consulting and Clinical Psychology; 58: 447–456.
Johnson, D. L.( 1991) Primary prevention of behavior problems in young children: The Houston Parent-Child Development Center. In: R. Price, E. L. Cowen, R. P. Lorion, and J. Ramos-McKay, Eds. Fourteen Ounces of Prevention: A Casebook for Practitioners. Washington, DC: American Psychological Association; 44–52.
Johnson, D. L.( 1990) The Houston Parent-Child Development Center Project: Disseminating a viable program for enhancing at-risk families. Prevention in Human Services; 7: 89–108.
Johnson, D. L.; Walker, T.( 1987) Primary prevention of behavior problems in Mexican-American children . American Journal of Community Psychology; 15: 375–385.
Joksch, H. C.( 1988) The impact of severe penalties on drinking and driving. Washington, DC: AAA Foundation for Traffic Safety.
Jones, M. B.; Offord, D. R.( 1989) Reduction of antisocial behavior in poor children by nonschool skill development. Journal of Child Psychology and Psychiatry and Allied Disciplines ; 30: 737–750.
Kalter, N.; Pickar, J.; Lesowitz, M.( 1984) School-based developmental facilitation groups for children of divorce: A preventive intervention. American Journal of Orthopsychiatry; 54: 613–623.
Kandel, D. B.; Yamaguchi, K.; Chen, K.( 1992) Stages of progression in drug involvement from adolescence to adulthood: Further evidence for the gateway theory. Journal of Studies on Alcohol; 53: 447–457.
Kazdin, A. E.( 1990) Prevention of conduct disorder. Paper presented to the National Conference on Prevention Research, National Institute of Mental Health, Bethesda, MD.
Kazdin, A. E.( 1987) Treatment of antisocial behavior in children: Current status and future directions. Psychological Bulletin; 102: 187–203.
Kellam, S. G.; Branch, J. D.; Agrawal, K. C.; Ensminger, M. E.( 1975) Mental Health and Going to School. Chicago, IL: University of Chicago Press.
Kellam, S. G.; Rebok, G. W.( 1992) Building developmental and etiological theory through epidemiologically based preventive intervention trials. In: J. McCord and R. E. Tremblay, Eds. Preventing Antisocial Behavior: Interventions from Birth Through Adolescence. New York, NY: Guilford Press; 162–195.
Kendell, R. E.; Rennie, D.; Clark, J. D.; Dean, C.( 1981) The social and obstetric correlates of psychiatric admission in the puerperium. Psychological Medicine; 11: 341–351.
Kessler, R. C.; House, J. S.; Turner, J. B.( 1987) Unemployment and health in a community sample. Journal of Health and Social Behavior; 28: 51–59.
Kessler, R. C.; Turner, J. B.; House, J. S.( 1988) Effects of unemployment on health in a
community survey: Main, modifying, and mediating effects. Journal of Social Issues; 44(4): 69–85.
Kinney, J. M.; Madsen, B.; Fleming, T.; Haapala, D. A.( 1977) Homebuilders: Keeping families together. Journal of Consulting and Clinical Psychology; 45: 667–673.
Klein, N. C.; Alexander, J. F.; Parsons, B. V.( 1977) Impact of family systems intervention on recidivism and sibling delinquency: A model of primary prevention and program evaluation. Journal of Consulting and Clinical Psychology; 45: 469–474.
Klepp, K. I.; Halper, A.; Perry, C. L.( 1986) The efficacy of peer leaders in drug abuse prevention. Journal of School Health; 56(9): 407–411.
Kraemer, H. C.( 1992) Reporting the size of effects in research studies to facilitate assessment of practical or clinical significance. Psychoneuroendocrinology; 17(6): 527–536.
Kraemer, H. C.; Fendt, K. H.( 1990) Random assignment in clinical trials: Issues in planning (Infant Health and Development Program). Journal of Clinical Epidemiology; 43: 1157–1167.
Kreig, T. L.( 1982) Is raising the legal drinking age warranted? The Police Chief; 32–34.
Lally, J. R.; Mangione, P. L.; Honig, A. S.( 1988) The Syracuse University Family Development Research Program: Long-range impact on an early intervention with low-income children and their families. In: D. Powell, Ed. Advances in Applied Developmental Psychology: Parent Education as Early Childhood Intervention, Vol. 3. Norwood, NJ: Ablex Publishing.
Lally, J. R.; Mangione, P. L.; Honig, A. S.; Wittner, D. S.( 1988) More pride, less delinquency: Findings from the ten-year follow-up study of the Syracuse University Family Development Research Program . Zero to Three; 8(4): 13–18.
Lawton, M. P.; Maddox, G. L.( 1985) Annual Review of Gerontology and Geriatrics. New York, NY: Springer.
Levenstein, P.( 1992) The Mother-Child Home Program: Research methodology and the real world. In: J. McCord and R. E. Tremblay, Eds. Preventing Antisocial Behavior: Interventions from Birth Through Adolescence. New York, NY: Guilford Press; 43–66.
Levy, D.; Sheflin, N.( 1985) The demand for alcoholic beverages: An aggregate time-series analysis . Journal of Public Policy and Marketing; 4: 47–54.
Lieberman, M. A.; Videka-Sherman, L.( 1986) The impact of self-help groups on the mental health of widows and widowers. American Journal of Orthopsychiatry; 56(3): 435–449.
Lochman, J. E.( 1992) Cognitive-behavioral intervention with aggressive boys: Three-year follow-up and preventive effects. Journal of Consulting and Clinical Psychology; 60: 426–432.
Lochman, J. E.; Coie, J. D.; Underwood, M. K.; Terry, R. (in press) Effectiveness of a social relations intervention program for aggressive and nonaggressive rejected children. Journal of Consulting and Clinical Psychology.
Lochman, J. E.; Curry, J. F.( 1986) Effects of social problem-solving training and self-instruction training with aggressive boys. Journal of Clinical Child Psychology; 15: 159–164.
McAlister, A. L.( 1983) Social-psychological approaches. In: T. J. Glynn, C. G. Leukefeld, and J. P. Ludford, Eds. Preventing Adolescent Drug Abuse: Intervention Strategies. NIDA Research Monograph No. 47; Washington, DC: Government Printing Office; 36–50.
McAlister, A. L.; Perry, C.; Killen, J.; Slinkard, L. A.; Maccoby, N.( 1980) Pilot study of smoking, alcohol, and drug abuse prevention. American Journal of Public Health; 70: 719–721.
McMahon, R. J.; Wells, K. C.( 1989) Conduct disorders. In: E. J. Mach and R. A. Barkley, Eds. Treatment of Childhood Disorders. New York, NY: Guilford Press; 73–132.
Madden, J.; O'Hara, J.; Levenstein, P.( 1984) Home again: Effects of the Mother-Child Home Program on mother and child. Child Development; 55: 636–647.
Markman, H. J.( 1984) The longitudinal study of couples' interactions: Implications for understanding and predicting the development of marital distress. K. Hahlweg and N. Jacobson, Eds. Marital Interactions: Analysis and Modification. New York, NY: Guilford Press; 253–281.
Markman, H. J.( 1981) Prediction of marital distress: A 5-year follow-up. Journal of Consulting and Clinical Psychology; 49(5): 760–762.
Markman, H. J.( 1979) Application of a behavioral model of marriage in predicting relationship satisfaction of couples planning marriage. Journal of Consulting and Clinical Psychology; 47(4): 743–749.
Markman, H. J.; Renick, M. J.; Floyd, F.; Stanley, S. M.; Clements, M.( 1993) Preventing marital distress through effective communication and conflict management: A 4- and 5-year follow-up. Journal of Consulting and Clinical Psychology; 61(1): 70–77.
Marris, P.( 1958) Widows and Their Families. London, England: Routledge and Kegan Paul.
Miranda, J.; Pérez-Stable, E. J.( 1993) The effects of preventive intervention on the use of medical services . In: R. F. Muñoz and Y. W. Ying, Eds. The Prevention of Depression: Research and Practice. Baltimore, MD: Johns Hopkins University Press.
Mulford, H. A.; Ledolter, J.; Fitzgerald, J. L.( 1992) Alcohol availability and consumption: Iowa sales data revisited. Journal of Studies on Alcohol; 53: 487–494.
Muñoz, R. F.( 1993a) The depression prevention course. In: R. F. Muñoz and Y. W. Ying, Eds. The Prevention of Depression: Research and Practice. Baltimore, MD: Johns Hopkins University Press.
Muñoz, R. F.( 1993b) The prevention of depression: Current research and practice. Applied and Preventive Psychology; 2: 21–33.
Muñoz, R. F.; Ying, Y. W.( 1993) The Prevention of Depression: Research and Practice. Baltimore, MD: Johns Hopkins University Press.
Muñoz, R. F.; Ying, Y.; Armas, R.; Chan, F.; Gurza, R.( 1987) The San Francisco depression prevention research project: A randomized trial with medical outpatients. In: R. F. Muñoz, Ed. Depression Prevention: Research Directions. Washington, DC: Hemisphere Press; 199–215.
Murray, D. M.; Johnson, C. A.; Luepker, R. V.; Mittelmark, M. B.( 1984) The prevention of cigarette smoking in children: A comparison of four strategies. Journal of Applied Social Psychology; 14: 274–288.
National Vaccine Advisory Committee.( 1991) The measles epidemic: The problems, barriers, and recommendations . Journal of the American Medical Association; 266: 1547–1552.
Olds, D. (University of Colorado, Denver, CO). “Study of Home Visitation for Mothers and Children.” Maternal and Child Health Bureau Grant No. MCJ-360579.
Olds, D. L.; Henderson, C. R.; Tatelbaum, R.; Chamberlin, R.( 1988) Improving the life-course development of socially disadvantaged mothers: A randomized trial of nurse home visitation. American Journal of Public Health; 78(11): 1436–1444.
Olds, D. L.; Henderson, C.; Tatelbaum, R.; Chamberlin, R.( 1986) Preventing child abuse and neglect: A randomized trial of nurse home visitation. Pediatrics; 78(1): 65–78.
Olds, D. L.; Kitzman, H.( 1990) Can home visitation improve the health of women and children at environmental risk? Pediatrics; 86(1): 108–116.
Olweus, D.( 1991) Bully/victim problems among schoolchildren: Basic facts and effects of
an intervention program. In: K. Rubin and D. Pepler, Eds. The Development and Treatment of Childhood Aggression. Hillsdale, NJ: Lawrence Erlbaum Associates.
O'Malley, P. M.; Wagenaar, A. C.( 1991) Effects of minimum drinking age laws on alcohol use, related behaviors and traffic crash involvement among American youth: 1976–1987. Journal of Studies on Alcohol; 52: 478–491.
Parkes, C. M.( 1965) Bereavement and mental illness: Part 2. A classification of bereavement reactions. British Journal of Medical Psychology; 33: 14–15.
Patterson, G. R.; Reid, J. B.; Jones, R. R.; Conger, R. E.( 1975) Families with Aggressive Children, Vol. I. Eugene, OR: Castalia.
Pedro-Carroll, J. L.; Cowen, E. L.( 1985) The Children of Divorce Intervention Program: An investigation of the efficacy of a school-based prevention program. Journal of Counseling and Clinical Psychology; 53: 603–611.
Pedro-Carroll, J. L.; Cowen, E. L.; Hightower, A. D.; Guare, J. C.( 1986) Preventive intervention with latency-aged children of divorce: A replication study. American Journal of Community Psychology; 14: 277–289.
Penning, M.; Barnes, G. E.( 1982) Adolescent marijuana use review. International Journal of the Addictions; 17: 749–791.
Pentz, M. A.; Dwyer, J. H.; MacKinnon, D. P.; Flay, B.; Hansen, W. B.; Wang, E. Y. I.; Johnson, C. A.( 1989) A multicommunity trial for primary prevention of adolescent drug abuse. Journal of the American Medical Association; 261: 3259–3266.
Perry, C. L.( 1986) Community-wide health promotion and drug abuse prevention. Journal of the School of Health; 56: 359–363.
Perry, C. L.; Grant, M.; Ernberg, G.; Florenzano, R. U.; Langdon, M. C.; Myeni, A. D.; Waahlberg, R.; Berg, S.; Andersson, K.; Fisher, K. J.; Blaze-Temple, D.; Cross, D.; Saunders, B.; Jacobs, D. R.; Schmid, T.( 1989) WHO Collaborative Study on Alcohol Education and Young People: Outcomes of a four-country pilot study. The International Journal of the Addictions; 24: 1145–1171.
Peter, G.( 1992) Childhood immunizations. New England Journal of Medicine; 327(25): 1794–1800.
Petersen, A. C.; Compas, B. E.; Brooks-Gunn, J.; Stemmler, M.; Ey, S.; Grant, K. E.( 1993) Depression in adolescence. American Psychologist; 48: 155–168.
Plotkin, S. A.; Mortimer, E. A.( 1988) Vaccines. Philadelphia, PA: Harcourt Brace Jovanovich, Inc.; 302.
Price, R. H.; van Ryn, M.; Vinokur, A.( 1992) Impact of a preventive job search intervention on the likelihood of depression among the unemployed. Journal of Health and Social Behavior; 33: 158–167.
Reid, J. (Oregon Social Learning Center, Eugene, OR). “Oregon Prevention Research Center.” National Institute of Mental Health Grant No. P50 MH46690.
Renick, M. J.; Blumberg, S. L.; Markman, H. J.( 1992) The Prevention and Relationship Enhancement Program (PREP): An empirically based preventive intervention program for couples. Family Relations; 41: 141–147.
Rickel, A. U.; Allen, L.( 1987) Preventing Maladjustment from Infancy through Adolescence. Newbury Park, CA: Sage Publications.
Roberts, R. E.( 1987) Epidemiological issues in measuring preventive effects. In: R. F. Muñoz, Ed. Depression Prevention: Research Directions. Washington, DC: Hemisphere Press; 45–75.
Robins, L. N.( 1980) The natural history of drug abuse. Acta Psychiatrica Scandinavica; 62(Suppl. 284): 7–20.
Robins, L. N.; Przybeck, T. R.( 1985) Age of onset of drug use as a factor in drug and other disorders. In: C. L. Jones and R. J. Battjes, Eds. Etiology of Drug Abuse: Implications
for Prevention. NIDA Research Monograph No. 56. Washington, DC: Government Printing Office; DHHS Pub. No. ADM 85–1335: 178–192.
Rose, S. A.; Feldman, J. F.; Rose, S. L.; Wallace, I. F.; McCarton, C.( 1992) Behavior problems at 3 and 6 years: Prevalence and continuity in full-terms and preterms. Development and Psychopathology; 4: 361–374.
Rosenberg, M. L.; Mercy, J. A.( 1991) Assaultive violence. In: M. L. Rosenberg and M. A. Fenley, Eds. Violence in America: A Public Health Approach. New York, NY: Oxford University Press; 14–50.
Roskin, M.( 1982) Coping with life changes: A preventive social work approach. American Journal of Community Psychology; 10: 331–340.
Ross, J. G.; Saavedra, P. J.; Shur, G. H.; Winters, F.; Felner, R. D.( 1992) After-school program for primary grade latchkey students on precursors of substance abuse. Journal of Community Psychology; Office of Substance Abuse Prevention Special Issue: 22–38.
Rotheram, M. J.( 1982) Social skill training with underachievers, disruptive, and exceptional children. Psychology in the Schools; 19: 532–539.
Rotheram, M. J.; Armstrong, M.; Booraem, C.( 1982) Assertiveness training in fourth and fifth grade children. American Journal of Community Psychology; 10(5): 567–582.
Saffer, H.; Grossman, M.( 1987) Beer taxes, the legal drinking age, and youth motor vehicle fatalities . Journal of Legal Studies; 16: 351–374.
Sameroff, A. J.; Chandler, M. J.( 1975) Reproductive risk and the continuum of caretaking casualty. In: F. D. Horowitz, M. Hetherington, and S. Scarr-Salopatek, Eds. Review of Child Development Research. Vol. 4. Chicago, IL: University of Chicago Press; 187–244.
Sandler, I. N.; West, S. G.; Baca, L.; Pillow, D. R.; Gersten, J. C.; Rogosch, F.; Virdin, L.; Beals, J.; Reynolds, K. D.; Kallgren, C.; Tein, J. Y.; Kreige, G.; Cole, E.; Ramirez, R.( 1992) Linking empirically-based theory and evaluation: The Family Bereavement Program. American Journal of Community Psychology; 20(4): 491–523.
Schinke, S. P.; Botvin, G. J.; Orlandi, M. A.( 1991) Substance Abuse in Children and Adolescents: Evaluation and Intervention . Newbury Park, CA: Sage Publications.
Schinke, S. P.; Orlandi, M. A.; Cole, K. C.( 1992) Boys and Girls clubs in public housing developments: Prevention services for youths at risk. Journal of Community Psychology; 118–128.
Schweinhart, L. J.( 1987) Can preschool programs help prevent delinquency? In: J. Q. Wilson and G. C. Loury, Eds. From Children to Citizens: Families, Schools, and Delinquency Prevention . New York, NY: Springer-Verlag; 13–53.
Schweinhart, L. J.; Weikart, D. P.( 1992) High/Scope Perry Preschool Program outcomes. In: J. McCord and R. E. Tremblay, Eds. Preventing Antisocial Behavior: Interventions from Birth Through Adolescence. New York, NY: Guilford Press; 67–86.
Shapiro, S.; Skinner, E. A.; Kessler, L. G.; Von Korff, M.; German, P. S.; Tischler, G. L.; Leaf, P. J.; Benham, L.; Cottler, L.; Regier, D. A.( 1984) Utilization of health and mental health services: Three epidemiological catchment area sites. Archives of General Psychiatry; 41: 971–978.
Shure, M. B.; Spivack, G.( 1988) Interpersonal cognitive problem solving. In: R. H. Price, E. L. Cowen, R. P. Lorion, and J. Ramos-McKay, Eds. Fourteen Ounces of Prevention: A Casebook for Practitioners. Washington, DC: American Psychological Association; 69–82.
Shure, M. B.; Spivack, G.( 1982) Interpersonal problem-solving in young children: A cognitive approach to prevention. American Journal of Community Psychology; 10: 341–356.
Shure, M. D.; Spivack, G.( 1980) Interpersonal problem solving as a mediator of behavioral adjustment in preschool and kindergarten children. Journal of Applied Developmental Psychology; 1: 29–44.
Silverman, P. R.( 1988) Widow-to-widow: A mutual help program for the widowed. In: R. Price, E. Cowen, R. P. Lorion, and J. Ramos-McKay, Eds. Fourteen Ounces of Prevention: A Casebook for Practitioners. Washington, DC: American Psychological Association; 175–186.
Slavin, R. E.; Madden, N. A.; Karweit, N. L.; Livermon, B. J.; Dolan, L.( 1990) Success for All: First year outcomes of a comprehensive plan for reforming urban education. American Educational Research Journal; 27: 255–278.
Spivack, G.; Shure, M. B.( 1974) Social Adjustment of Young Children. San Francisco, CA: Jossey-Bass Publications.
Springer, F.; Phillips, J.; Phillips, L.; Cannady, L. P.; Derst-Harris, E.( 1992) CODA: A creative therapy program for children in families affected by abuse of alcohol or other drugs. Journal of Community Psychology; OSAP Special Issue: 55–74.
Stolberg, A. L.; Garrison, K. M.( 1985) Evaluating a primary prevention program for children of divorce. American Journal of Community Psychology; 13: 111–124.
Strayhorn, J. M.; Weidman, C. S.( 1991) Follow-up one year after parent-child interaction training: Effects on behavior of preschool children. Journal of the American Academy of Child and Adolescent Psychiatry ; 30: 138–143.
Stuart, R. B.( 1974) Teaching facts about drugs: Pushing or preventing? Journal of Educational Psychology; 66: 189–201.
Sullivan, L. W.( 1991) The prevention of violence: A top HHS priority. Public Health Reports; 106: 268–269.
Tadmor, C. S.( 1988) The Perceived Personal Control preventive intervention for a caesarean birth population. In: R. H. Price, E. L. Cowen, R. P. Lorion, and J. Ramos-McKay. Fourteen Ounces of Prevention: A Casebook for Practitioners. Washington, DC: American Psychological Association; 141–152.
Tadmor, C. S.; Brandes, J. M.( 1984) The perceived personal control crisis intervention model in the prevention of emotional dysfunction for a high risk population of caesarean birth. The Journal of Primary Prevention; 6: 244–255.
Tadmor, C. S.; Brandes, J. M.; Hofman, J. E.( 1988) Preventive intervention for a caesarean birth population. Journal of Preventive Psychiatry; 3(4):
Thoits, P.( 1986) Social support as coping assistance. Journal of Consulting and Clinical Psychology; 54: 416–423.
Toseland, R. W.( 1990) Long-term effectiveness of peer-led and professionally-led support groups for caregivers. Social Service Review; 64: 308–327.
Toseland, R. W.; Rossiter, C. M.; Labrecque, M. S.( 1989) The effectiveness of peer-led and professionally-led groups to support family caregivers. The Gerontologist; 29(4): 465–471.
Tremblay, R. E.; McCord, J.; Bioleau, H.; Charlebois, P. I.; Gagnon, C.; LeBlanc, M.; Larivee, S.( 1991) Can disruptive boys be helped to become competent? Psychiatry; 54: 148–161.
Tremblay, R. E.; Vitaro, F.; Bertrand, L.; LeBlanc, M.; Beauchesne, H.; Boileau, H.; David, L.( 1992) Parent and child training to prevent early onset of delinquency: The Montreal Longitudinal-Experimental Study. In: J. McCord and R. Tremblay, Eds. Preventing Antisocial Behavior: Interventions from Birth Through Adolescence. New York, NY: Guilford Press; 117–138.
U.S. Advisory Board on Child Abuse and Neglect.( 1990) Child Abuse and Neglect: Critical
First Steps in Response to a National Emergency. Washington, DC: Government Printing Office.
USPHS (U.S. Public Health Service) Expert Panel on the Content of Prenatal Care.( 1989) Caring for Our Future: The Content of Prenatal Care. Report of the Public Health Service Expert Panel on the Content of Prenatal Care. Washington, DC: Department of Health and Human Services.
Vachon, M. L. S.( 1979) Identity change over the first two years of bereavement: Social relationships and social support in widowhood. York University, Toronto, Canada: Unpublished doctoral dissertation .
Vachon, M. L. S.; Sheldon, A. R.; Lancee, W. J.; Lyall, W. A. L.; Roger, J.; Freeman, S. J. J.( 1982) Correlates of enduring distress patterns following bereavement: Social network, life situations and personality. Psychological Medicine; 12: 783–788.
Vachon, M. L. S.; Sheldon, A. R.; Lancee, W. J.; Lyall, W. A. L.; Roger, J.; Freeman, S. J. J.( 1980) A controlled study of self-help intervention for widows. American Journal of Psychiatry; 137: 1380–1384.
Vega, W. A.; Murphy, J.( 1990) Projecto Bienestar: An example of a community-based intervention. In: Culture and the Restructuring of Community Mental Health: Contributions in Psychology. Series No. 16; Westport, CT: Greenwood Press; 103–122.
Vega, W. A.; Valle, R.; Kolody, B. (submitted for publication) Preventing depression in the Hispanic community: An outcome evaluation of Projecto Bienestar.
Vega, W. A.; Valle, R.; Kolody, B.; Hough, R.( 1987) The Hispanic social network prevention intervention study: A community-based randomized trial. In: R. F. Muñoz, Ed. Depression Prevention: Research Directions. Washington, DC: Hemisphere Publishing; 217–231.
Vinokur, A. D.; Schul, Y.; Price, R. H.( 1992) Demographic assets and psychological resources in the reemployment process: Who benefits from the JOBS intervention for the unemployed? Michigan Prevention Research Center Working Paper, Institute for Social Research, University of Michigan.
Vinokur, A. D.; van Ryn, M.; Gramlich, E. M.; Price, R. H.( 1991) Long-term follow-up and benefit/cost analysis of the JOBS Project . Journal of Applied Psychology; 76(2): 213–219.
Wagenaar, A. C.; Holder, H. D. (1991) A change from public to private sale of wine: Results from natural experiments in Iowa and West Virginia. Journal of Studies on Alcohol; 52: 162–173.
Weaver, S. C.; Tennant, F. S.( 1973) Effectiveness of drug education programs for secondary school students . American Journal of Psychiatry; 130: 812–814.
Webster-Stratton, C. (University of Washington, Seattle, WA). “Preventing Conduct Disorders in Head Start Children.” Administration for Children and Families Grant No. 93–600 (90CD0949/01) and “Parent Training Models for Anti-social Children.” Institute for Nursing (National Center for Nursing Research) Grant No. NR 01 075–09.
Weikart, D. P.; Schweinhart, L. J.; Larner, M. B.( 1986) A report on the High/Scope preschool curriculum comparison study: Consequences of three preschool curriculum models through age 15 . Early Childhood Research Quarterly; 1: 15–45.
Weissberg, R. P.; Caplan, M. Z.; Sivo, P. J.( 1989) A new conceptual framework for establishing school-based competence promotion programs. In: L. A. Bond and B. E. Compas, Eds. Primary Prevention and Promotion in the Schools: Primary Prevention of Psychopathology, Vol. 12. Newbury Park, CA: Sage Publications: 255–296.
White, C. C.; Koplan, J. P.; Orenstein, W. A.( 1985) Benefits, risks, and costs of immunization for measles, mumps, and rubella. American Journal of Public Health; 75(7): 739–744.