Summary
The United States is experiencing an epidemic of obesity among both adults and children. Approximately 35 percent of women and 31 percent of men age 20 and older are considered obese, as are about one-quarter of children and adolescents. While government health goals for the year 2000 call for no more than 20 percent of adults and 15 percent of adolescents to be obese, the prevalence of this often disabling disease is increasing rather than decreasing.
Obesity, of course, is not increasing because people are consciously trying to gain weight. In fact, tens of millions of people in this country are dieting at any one time; they and many others are struggling to manage their weight to improve their appearance, feel better, and be healthier. Many programs and services exist to help individuals achieve weight control. But the limited studies paint a grim picture: those who complete weight-loss programs lose approximately 10 percent of their body weight, only to regain two-thirds of it back within 1 year and almost all of it back within 5 years.
These figures point to the fact that obesity is one of the most pervasive public health problems in this country, a complex, multifactorial disease of appetite regulation and energy metabolism involving genetics, physiology, biochemistry, and the neurosciences, as well as environmental, psychosocial, and cultural factors. Unfortunately, the lay public and health-care providers, as well as insurance companies, often view it simply as a problem of willful misconduct—eating too much and exercising too little. Obesity is a remarkable disease in terms of the effort required
by an individual for its management and the extent of discrimination its victims suffer.
While people often wish to lose weight for the sake of their appearance, public health concerns about obesity relate to this disease's link to numerous chronic diseases that can lead to premature illness and death. The scientific evidence summarized in Chapter 2 suggests strongly that obese individuals who lose even relatively small amounts of weight are likely to decrease their blood pressure (and thereby the risk of hypertension), reduce abnormally high levels of blood glucose (associated with diabetes), bring blood concentrations of cholesterol and triglycerides (associated with cardiovascular disease) down to more desirable levels, reduce sleep apnea, decrease their risk of osteoarthritis of the weight-bearing joints and depression, and increase self-esteem. In many cases, the obese person who loses weight finds that an accompanying comorbidity is improved, its progression is slowed, or the symptoms disappear.
Healthy weights are generally associated with a body mass index (BMI; a measure of whether weight is appropriate for height, measured in kg/m2) of 19–25 in those 19–34 years of age and 21–27 in those 35 years of age and older. Beyond these ranges, health risks increase as BMI increases. Health risks also increase with excess abdominal/visceral fat (as estimated by a waist-hip ratio [WHR] >1.0 for males and >0.8 for females), high blood pressure (>140/90), dyslipidemias (total cholesterol and triglyceride concentrations of >200 and >225 mg/dl, respectively), non-insulin-dependent diabetes mellitus, and a family history of premature death due to cardiovascular disease (e.g., parent, grandparent, sibling, uncle, or aunt dying before age 50). Weight loss usually improves the management of obesity-related comorbidities or decreases the risks of their development.
The high prevalence of obesity in the United States together with its link to numerous chronic diseases leads to the conclusion that this disease is responsible for a substantial proportion of total health-care costs. We estimate that today's health-care costs of obesity exceed $70 billion per year. To this figure can be added the more than $33 billion spent yearly on weight-reduction products (including diet foods and drinks) and services, for an estimated total of more than $100 billion per year as the economic costs of obesity. Such an estimate cannot include the psychosocial costs of obesity, which range from lowered self-esteem to the more serious binge-eating disorders and clinical depression.
Given the huge economic and personal costs of obesity, research must continue to identify the fundamental biological defects that underlie obesity and discover how to manage and ultimately treat them. At the same time, however, it is important to improve the success of obesity treatments available now. This report is directed to the latter purpose. Treatment
cannot cure obesity, of course, but it can provide assistance, information, and reinforcement for the long-term management of this disease.
It is important to note that this report focuses on adult obesity. Given the relatively few data on evaluating and managing obesity in children and adolescents, as well as the time constraints under which we operated, little attention was paid to the subject. However, pediatric obesity is an important public health problem, and we have included a background paper on the subject in Appendix C of this report.
TYPES OF PROGRAMS AND APPROACHES TO TREAT OBESITY
The wide variety of weight-loss programs can be placed along a continuum on the basis of many factors, including intensity of treatment, cost, the nature of the intervention(s), and degree of involvement of health-care providers. We chose to organize the plethora of programs into three major categories: do-it-yourself programs, nonclinical programs, and clinical programs:
-
Do-it-yourself programs are individually formulated and therefore extraordinarily varied. This category includes any effort by an individual to lose weight by himself or herself or with a group of like-minded others through programs such as Overeaters Anonymous and TOPS (Take Off Pounds Sensibly) and community-based and work-site programs. Individual judgment, books, products, and group therapy may dispense good or bad advice. The common denominator of programs in this category is that outside resources are not used in a personalized or individualized manner.
-
Nonclinical programs are popular and are often commercially franchised. They typically have a structure created by a parent company and often use instructional and guidance materials that are prepared in consultation with health-care providers. The qualifying characteristic of these programs is that they rely substantially on variably trained counselors (who are not health-care providers) to provide services to clients.
-
Clinical programs are those in which services are provided by a licensed professional who may or may not have received special training to treat obese patients. The programs may or may not be part of a commercial franchise system. In some clinical programs, an individual professional provider works alone; in others, a multidisciplinary group of professional providers works together and systematically coordinates their efforts, records, and patient base. Clinical programs include such services as nutrition, medical care, behavior therapy, exercise, and psychological
-
counseling, and they may utilize very-low-calorie diets, medications, and surgery.
We have identified five broad approaches to treatment used by the do-it-yourself, nonclinical, and clinical programs: diet, physical activity, behavior modification, drug therapy, and gastric surgery. Not all approaches are used by, or available to, each category of programs. However, each program category uses one or more of these approaches.
Special attention is due drugs and surgery, because these options may offer help to individuals who have failed with other approaches. Data show that anti-obesity drugs help some people to lose weight and maintain weight loss. However, relatively few such drugs are available for this purpose, and their use is generally limited to several months. Standards for use of anti-obesity drugs should be liberalized so that these medications are treated similarly to those used for the treatment of other medical problems such as hypertension, where the presumption is that medication may be required for long periods of time and beneficial results are maintained only as long as the drug is taken. Such a change should stimulate research and development on new, more effective, medications. In regard to surgery, there is compelling evidence that comorbidities are reduced or delayed in severely obese patients who have lost weight as a result of gastric surgery. Therefore, it is puzzling that this treatment is not more widely used for severely obese individuals (BMI ≥ 35) at very high risk for obesity-related morbidity and mortality.
It is important to state that our recommendations are meant to apply to the weight-management programs that use data or testimonials in their advertising and promotional activities to suggest that weight loss is likely to be successful with them or that they are more effective than competing programs. Programs that engage in these activities should be held to some level of proof of their claims, so they must be encouraged to collect certain types of information in standardized ways and provide certain kinds of information to potential clients. Potential clients, in turn, should be encouraged to expect this information from programs, so that programs that do not comply may be put at a competitive disadvantage and thereby become motivated to rethink their position. This information is needed so that consumers can make informed choices and there can be reasonable oversight of programs by regulatory agencies such as the Federal Trade Commission, the Food and Drug Administration, and state agencies, as well as by interested biomedical scientists. Weight-management programs that do not make claims of success—such as classes provided by a community YMCA or YWCA, counseling by dietitians at a local hospital, or meetings of a local chapter of Overeaters Anonymous—should
not be required to assume the data-collection burdens and expense of meeting our recommendations, but should endeavor to do so if resources permit. Given that the loss of even a small amount of weight may benefit health, we want interested clients to have many options in their communities to receive help in achieving a healthful lifestyle.
EVOLVING FROM WEIGHT LOSS TO WEIGHT MANAGEMENT
The facts summarized above provide compelling evidence of the need for a new perspective on obesity-treatment outcomes. This report has been developed in response to that need. We recommend that the definition of success that is applied in evaluating weight-loss programs be broadened and made more realistic based on the research findings that small weight losses can reduce the risks of developing chronic diseases. Specifically, the goal of obesity treatment should be refocused from weight loss alone, which is often aimed at appearance, to weight management, achieving the best weight possible in the context of overall health. In contrast to weight loss, the primary purpose of weight management is to achieve and maintain good health. This concept includes weight loss but is not limited to it. We recommend that weight-loss programs evolve into weight-management programs and be judged more by their effects on the overall health of participants than by their effects on weight alone. The recommendations set forth in this report are framed around weight management.
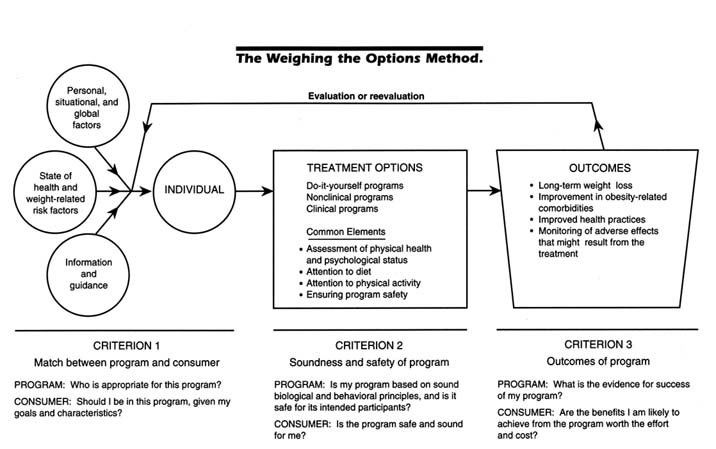
This report is organized around a simple conceptual overview of decisionmaking—an individual making a decision about an option and then experiencing an outcome and evaluating it—that we adapted and expanded and from which we developed criteria and a model for evaluating obesity-treatment programs. Our Weighing the Options model (see Figure 1) provides a framework for the conduct of programs and behavior of individuals that should help consumers choose more wisely from among available programs. Its health-based approach to weight management should also help them to be more successful at weight loss.
Figure 1 illustrates the model in such a way that each of its major components is associated with a criterion, and each criterion is discussed as it pertains to both weight-management programs and consumers seeking such programs. Our discussion of this model and recommendations derived from it is organized by the three criteria: (1) match between program and consumer, (2) soundness and safety of the program, and (3) outcome of the program.
Weighing the Options Criterion 1: The Match Between Program and Consumer
Matching, which pertains to the first part of our model, has long been a key aspect of medical treatment. Chapter 5 reviews several schemes for matching in the obesity field, all of which we found useful although limited for our purposes. We approached the matching of individuals to treatments by identifying four sets of factors that may influence decision-making:
-
Personal, situational, and global factors: Personal factors include demographic ones, such as age and gender, that cannot be changed as well as psychosocial ones, such as motivation and readiness to change, that one can alter. Situational factors can be changed by the individual's actions; an example is using the stairs whenever appropriate rather than the elevator. Global factors are those that influence the environment in which an individual lives, such as culture and views about weight; they typically change slowly over time from the efforts of large numbers of people. The availability and cost of a weight-loss program are two global factors that often influence a person's decision about whether or not to undertake a particular weight-loss program.
-
Health status and weight-related risk factors are factors that, as they worsen, may become an individual's primary motivation for losing weight. These factors are described in the section on Criterion 2.
-
Information and guidance come from a variety of sources, including the media (information and advertising); family, friends, and acquaintances (who relay their opinions and experiences with the various options); and health-care providers. The information and guidance may be sound or unsound, well intentioned or intended to deceive, and empowering or provoking inaction. They may also be incomplete or biased toward a particular program or approach that may not be suitable.
-
Experiencing a successful, partially successful, or unsuccessful outcome from an obesity-treatment program: This factor applies to those who have already gone through a program and are deciding whether to continue with the same program or try another one.
In some cases, it is possible to identify mismatches of individuals with weight-loss programs, at least in the sense of excluding people from particular options. For example, a healthy young woman with a BMI of 28 is no candidate for gastric surgery, whereas a very obese male with a BMI of 40 and hypertension—who has not lost weight despite many attempts—is not likely to be helped by a do-it-yourself diet book or exercise video. However, for most people who wish to lose weight, there is
general agreement that it is not yet possible to match people with programs to significantly improve their chances of success. The complex interactions that occur between an individual and the many factors that influence program choice are beyond the current ability of biomedical science to explain, much less predict. Nevertheless, it is possible to make some prudent qualitative recommendations to increase the likelihood of a successful match. They are described below and summarized in Table 1.
Program's Perspective on Criterion 1: Who Is Appropriate for This Program?
Each program decides what types of clients are appropriate and inappropriate given its specific philosophies, protocols, and treatment approaches. Pregnant women and individuals who are underweight or anorectic are inappropriate candidates for any weight-loss program. Nonclinical programs should require (and do-it-yourself programs should advise) that lactating women, children, and adolescents, as well as those with bulimia; significant cardiovascular, renal, or psychiatric disease; diabetes; or other significant medical problems undertake weight loss only under medical supervision or in consultation or partnership with their health-care provider. Nonclinical programs should encourage clients with obesity-related comorbidities or other health problems to maintain contact with their health-care provider for the duration of the program. Both nonclinical and clinical programs should obtain some information on the state of health and weight-loss goals of potential clients to determine if they are appropriate for a specific program and what types of individualized attention they may require.
Do-it-yourself programs such as those provided in diet books, diet plans in magazines, or over-the-counter weight-loss devices or products should provide information in the text or other instructional materials on who should and who should not use the program. Since there is usually no legal obligation that this information be provided or that it be true and complete, the publisher or manufacturer of the program should be responsible for providing it voluntarily.
Consumer's Perspective on Criterion 1: Should I Be in This Program, Given My Goals and Characteristics?
Because consumers decide on their own or with the help of others whether to enter a weight-loss program and which one to choose, they must consider carefully their weight-loss goals and whether they are appropriate
TABLE 1 Summary of Recommendations Pertaining to Criterion 1
|
|
Program Perspective |
|||
|
|
Do-It-Yourself Program |
Nonclinical Program |
Clinical Program |
|
|
Decide what clients are appropriate for program |
Yes |
Yes |
Yes |
|
|
Provide information in text or other instructional materials on who can and who should not use program |
Publisher or manufacturer of program should provide information voluntarily |
Yes |
Yes |
|
|
Obtain information on state of health and weight-loss goals of potential clients |
Generally cannot do |
Yes |
Yes |
|
|
Weight loss for individuals with obesity-related comorbidities or other health problems |
Encourage contact with health-care provider for duration of program |
Yes |
||
|
Weight loss for lactating women, children, and adolescents; and those with bulimia, significant cardiovascular, renal, or psychiatric disease; diabetes; or other significant medical problems |
Advise against without medical supervision |
Require medical supervision as condition of entry |
May be appropriate |
|
|
Weight loss for pregnant women and individuals who are underweight or anorectic |
Discourage |
Discourage entry |
||
|
Consumer Perspective |
||||
|
Consider carefully your weight-loss goals and whether you are an appropriate candidate for weight loss. |
||||
|
Decide whether the time is right to be able to devote the considerable attention and effort required to succeed at weight loss. |
||||
|
Be evaluated by a health-care provider (or have been in recent past) before undertaking a do-it-yourself or nonclinical program. Discuss program or product with health-care provider. |
||||
|
Expect that programs will provide sufficient information so you can assess whether you are appropriate or inappropriate as a potential candidate. |
||||
candidates for weight loss, and decide whether the time is right for them to devote the considerable attention and effort required to succeed. Individuals should expect a program to provide them with sufficient information to help assess whether they are appropriate or inappropriate potential candidates. We recommend that those contemplating a do-it-yourself or nonclinical program be evaluated first by a health-care provider (or have been assessed in the recent past) before proceeding. They should discuss the program or product with a knowledgeable health-care provider to determine whether it is sound and appropriate.
Weighing the Options Criterion 2: The Soundness and Safety of the Program
The programs themselves and their characteristics constitute the center section of the Weighing the Options model. Earlier, we described the three types of programs into which all options were placed: do-it-yourself, nonclinical, and clinical programs. Insofar as the vast majority of dieters choose to join weight-loss services or select do-it-yourself options, there is an almost total absence of controls for the efficacy and safety of weight-loss methods as actually practiced throughout the population. Because health risks may attend obesity and the process of losing weight, we believe that all programs should meet some minimum expectations. Specifically, we recommend that four critical areas be addressed by all weight-loss and weight-management programs: (1) assessment of physical health and psychological status, (2) attention to diet, (3) attention to physical activity, and (4) ensuring program safety. These critical areas are discussed in detail in Chapter 6 and summarized below.
-
Assessment of physical health and psychological status: Individuals considering a do-it-yourself or nonclinical program to lose weight should have some basic knowledge about their overall state of health before they begin. This is important not only because we believe that all adults should assume some responsibility for their health care, but because this self-assessment should help them determine which programs might be best for them. Many nonclinical programs screen potential clients by measuring height and weight and asking questions about health status. Ideally, however, obese individuals should have a physician review their health history and provide a physical examination, with particular attention to obesity comorbidities, prior to beginning a program. Individuals are almost always assessed by physicians as part of a clinical program.
-
Diet: How much one eats (and, to some extent, what one eats) is a major determinant of body weight. Therefore, food intake should play a central role in all weight-management efforts. The overall goal in obesity
-
treatment is to obtain a negative energy balance by reducing energy intake (i.e., eating less), increasing energy expenditure (i.e., performing more physical activity), or preferably both. Programs that promise results without dieting and physical activity will surely be ineffective over the long term. Generally, weight loss requires decreasing total energy intake and utilizing, as much as possible, a variety of available foods. The federal government's dietary guidance plan, the Food Guide Pyramid, is a useful tool to help individuals meet dietary recommendations. Decreasing alcohol intake, foods of minimal nutritional value, and fats and simple sugars is a good strategy for reducing energy intake without eliminating essential nutrients. A weight-reduction diet should contain adequate protein to maintain nitrogen balance and limit the loss of lean body mass. Energy intakes of less than 1,200 kcal/day may not meet nutrient requirements, and a dietary supplement may be needed. Individuals consuming such low-calorie diets should seek the advice of a health-care provider (e.g., a physician or dietitian). Diets of less than 800 kcal/day should not be used except under a physician's supervision. A health-care provider knowledgeable about obesity and its treatment and about the physiology of weight loss can help an individual develop a nutritionally adequate diet plan tailored to his or her weight-loss goals and appropriate to factors such as gender, age, dietary preferences, and level of physical activity.
-
Physical activity: As with diet, activity level should play a central role in all weight-management efforts. Physical activity can lead to weight loss, may help prevent weight regain after a weight-loss program, and helps reduce some of the comorbidities associated with obesity (e.g., dyslipidemias and hyperglycemia). Because most obese persons are inactive, physical activity interventions in this group should be approached with low starting levels and slow progression to higher levels of activity. We recommend that a gradual reshaping of a participant's physical activity pattern over time be the focus of intervention, rather than providing a strict, regimented, and specific dose of activity in an exercise prescription. The most feasible mode of activity for most adults is walking. Each person should develop a realistic goal for increasing activity, perhaps with professional guidance, which can be modified over time as activity levels increase. It is reasonable to suggest a gradual progression up to 1 hour of moderate-intensity activity (e.g., brisk walking) each day, accumulated over the course of a day. As participants become more physically fit, they will be capable of more activity; they may ultimately engage in more vigorous activities such as cycling, jogging, or other vigorous sports and recreational activities and thereby achieve their caloric-expenditure goals in a shorter period of time. Selection of activity goals and the type of activities to be used are highly individualized matters.
-
Persons should be encouraged to find what works for them and should evaluate different approaches until a sustainable activity plan is developed.
-
Ensuring program safety: Generally, the more restrictive the diet, the greater are the risks of adverse effects associated with weight loss. Do-it-yourself and nonclinical programs must be relatively safe (i.e., carry minimal risk) for their clients. Clinical programs must also be as safe as reasonably possible, given that they are likely to be designed for the very obese with comorbidities and health problems. Programs must insist that clients with one or more obesity-related comorbidities be monitored. A client should expect a program to provide detailed information about any potential risks that could occur. Special attention must be paid to the safety of programs for children, pregnant women, and the elderly. There are a variety of minor and major risks associated with dieting. For example, there is an increase in the risk of gall bladder disease among people who lose weight rapidly on very-low-fat diets. Risks to health from weight loss vary with the individual and the type of program.
Our recommendations related to Criterion 2 are described below and summarized in Table 2.
Program's Perspective on Criterion 2: Is My Program Based on Sound Biological and Behavioral Principles, and Is It Safe for Its Intended Participants?
All providers should take steps to ensure that their programs are safe and sound. Nonclinical and clinical programs can provide information about the qualifications and training of staff, appropriate corporate managers, and, if desired, consultants involved in developing the program. Authors and other originators of do-it-yourself programs should cite their credentials, qualifications, and experiences in managing obesity.
Clinical programs should be able to assess the physical and psychological health of their patients. Nonclinical and do-it-yourself programs, in contrast, can only encourage clients to have such an assessment conducted by their health-care providers. All programs should encourage individuals to know their blood pressure and blood lipid concentrations; whether or not they have diabetes, osteoarthritis in weight-bearing joints, or sleep apnea; and whether a family member has died prematurely from coronary heart disease. Do-it-yourself and nonclinical programs should strongly encourage individuals who have one or more of these risk factors to be under the care of a health-care provider. These programs should develop simple checklists for clients to highlight the importance of routinely
TABLE 2 Summary of Recommendations Pertaining to Criterion 2
|
|
Program Perspective |
|
|
|
|
Do-It-Yourself Program |
Nonclinical Program |
Clinical Program |
|
Take steps to ensure that program is safe and sound |
Yes |
Yes |
Yes |
|
Encourage individuals to know their blood pressure and blood lipid concentrations; whether or not they have diabetes, osteoarthritis in weight-bearing joints, or sleep apnea; and whether a family member has died prematurely (before age 50) from coronary heart disease |
Yes |
Yes |
Yes |
|
Encourage individuals who have one or more risk factors (see above) to be under care of health-care provider |
Yes |
Yes |
NA (not applicable) |
|
Assess clients for risk factors (see above) |
NA |
NA |
Yes |
|
Develop simple checklists for clients to highlight importance of routinely monitoring health status |
Yes |
Yes |
NA |
|
Inform about the known and hypothetical risks of program |
Yes |
Yes |
Have special responsibilities to assess and manage potential risks, especially when special diets, drugs, or surgery are used |
|
Qualifications and training |
Cite credentials, qualifications, and experiences in managing obesity |
Provide this information about staff, appropriate corporate managers, and if desired, consultants involved in developing the program |
|
|
|
Program Perspective |
|
|
|
|
Do-It-Yourself Program |
Nonclinical Program |
Clinical Program |
|
Height and weight of clients and calculation of body mass index and waist-to-hip ratio |
Encourage clients to take these measurements and make calculations. Instruct how to do so and explain results. |
Make measurements and calculations; provide and interpret results |
|
|
Assessment of physical and psychological health of clients |
Encourage clients to have assessment performed by their health-care provider |
Perform assessment |
|
|
Psychological assessment |
Provide test such as Dieting Readiness Test; give explicit guidance how to use and score it |
Administer test such as Dieting Readiness Test |
Administer test such as Dieting Readiness Test along with the General Well-Being Schedule |
|
Diet and physical activity assessment |
Inform clients of importance of attention to these factors; give explicit guidance how to do so |
Clients should have these evaluated at the beginning and end of treatment phase of program and at least every 6 months during any maintenance phase |
|
|
Consumer Perspective |
|||
|
Have a good understanding of program and what to expect from it through treatment and any maintenance phase. |
|||
|
Monitor weight weekly and continue to assess (or have assessed) diet and physical activity patterns at 6-month intervals or more frequently after the weight-loss phase of program. |
|||
|
Expect that program will be a safe and sound one. |
|||
|
Expect that do-it-yourself programs will provide the credentials and qualifications of the author/originator. Nonclinical and clinical programs will make available information about the qualifications and training of staff. |
|||
monitoring health status. Clinical programs should assess all clients for these risk factors.
Nonclinical and clinical programs should measure the height and weight of clients and calculate their BMI and WHR, providing both the results and the information to interpret those results. Do-it-yourself programs should encourage their clients to take these measurements and make these calculations, instruct them how to do so, and explain the results.
Clients in nonclinical and clinical programs should have their diets and physical activity patterns evaluated at least at the beginning and end of the treatment phase of the program and every 6 months during any maintenance phase (various assessment tools are described in Appendix A). Nonclinical programs should assess the psychological status of clients with a questionnaire such as the Dieting Readiness Test; clinical programs should use this type of questionnaire along with a second questionnaire such as the General Well-Being Schedule (both questionnaires are provided in Appendix B). Do-it-yourself programs should inform clients about the importance of attention to diet, physical activity, and psychological assessment (by providing the Dieting Readiness Test or a similar questionnaire), and give explicit guidance in how to do so.
Since no weight-loss attempt is risk free, it is incumbent on each program to inform potential clients about the known and hypothetical risks of that program. Clinical programs have special responsibilities to assess and manage potential risks, especially when special diets (e.g., very-low-calorie diets), drugs, or surgery are used as part of the treatment.
Consumer's Perspective on Criterion 2: Is the Program Safe and Sound for Me?
Given the limitations of do-it-yourself and nonclinical programs to assess health compared to clinical programs, consumers choosing the former have a greater responsibility for self-monitoring their health. Consumers should have a good understanding of the program of interest and what they can expect from it throughout the treatment and any maintenance phase. They should have access to information about the qualifications and training of staff in nonclinical and clinical programs and the credentials and qualifications of the author/originator of a do-it-yourself program.
Clients should expect that the program of interest will be a safe and sound one (by meeting our recommendations for them as detailed above). We recommend that they monitor their weight weekly and continue to assess (or have assessed) their diet and physical-activity patterns at 6-month
intervals or more frequently after the weight-loss phase of a program. This will act as a useful periodic check on these two major influences of weight and will help to maintain weight loss.
Weighing the Options Criterion 3: Outcomes of the Program
The third portion of the model focuses on the outcomes of the program. We have identified four components of successful weight management: (1) long-term weight loss, (2) improvement in obesity-related comorbidities, (3) improved health practices, and (4) monitoring of adverse effects that might result from the program. We believe that weight-loss programs should be judged by how well individuals do in these four areas, and potential clients should expect that a high-quality program will attend to, or urge attention be paid to (since most of these components are not under the direct control of the program), each of these areas. We recommend that the following be used as guidelines to determine if these goals are met:
-
Long-term weight loss: Long-term means 1 year or more, and weight loss of any significance is the loss of ≥ 5 percent of body weight or a reduction in BMI by 1 or more units.
-
Improvement in obesity-related comorbidities: One or more associated risk factors (e.g., high blood pressure; elevated blood concentrations of cholesterol, triglycerides, or glucose; and non-insulin-dependent diabetes mellitus), if present, should be improved to a degree considered clinically significant.
-
Improved health practices: Obtaining health-related knowledge may be assessed indirectly by evaluating whether basic information about obesity is presented by the program and whether the individual reads or hears it. Engaging in good eating habits may be assessed by using a dietary assessment tool such as those cited in Appendix A or evidence that the individual meets the recommendations of the Food Guide Pyramid on at least 4 of 7 days. Engaging in regular physical activity involves one-half hour or more of moderate-intensity activity (e.g., brisk walking) four or more times a week and preferably daily. Obtaining regular medical attention includes seeing a physician at yearly intervals, particularly if the individual has not achieved a healthy weight. Regular screening of these individuals by a health-care provider will help to identify as early as possible the presence of comorbid conditions and lead to the initiation or continuation of appropriate treatment. Improved well-being can be assessed through questionnaires described in Appendix A. For all programs, we recommend a test such as the Dieting Readiness Test prior to
-
initiation and, in addition, for clinical programs only, a test such as the General Well-Being Schedule to screen for eating disorders and psychiatric pathologies (see Appendix B).
-
Monitoring adverse effects that might result from program: Clinical and nonclinical programs should question their clients periodically about any changes in health while on the program and should encourage them to volunteer such information if changes do occur. A do-it-yourself program should inform consumers that because the program may potentially have adverse health effects, they should be attentive to any changes in their health while on it.
As stated earlier, most people fail at weight management over the course of a year or more. Research shows that for the small numbers of people who do maintain their losses, the most important factors associated with long-term success include a regular habit of exercise, continued contact with the treatment program, normalization of eating patterns, continued self-monitoring of diet and exercise, and a positive, problem-solving attitude toward life's stressors. Family dysfunction and negative life events are associated strongly with weight rebound.
Our recommendations for Criterion 3 are described below and summarized in Table 3.
Program's Perspective on Criterion 3: What Is the Evidence for Success of My Program?
It is not cost effective or practical for most do-it-yourself programs to evaluate their outcomes. Nevertheless, they can make sure that they cover the importance of long-term weight loss and the reduction of obesity-related comorbidities, provide information and guidance on improving health behaviors, and discuss in detail the potential health risks from weight loss in general and their program in particular.
Because clients come physically to nonclinical and clinical programs, the programs can monitor and document their weight loss over time. Such programs should have quality control procedures in place to ensure that protocols are adhered to by staff and to modify those protocols as warranted given the experiences and feedback of clients. They should also have mechanisms to evaluate the success of their programs. If the company is organized as a franchise, mechanisms should be available to evaluate the program as a whole and at individual sites.
All programs should also provide information and guidance on improving health behaviors and should discuss the potential risks of dieting, including those from their programs. Do-it-yourself and nonclinical programs should encourage clients (and strongly encourage those with
TABLE 3 Summary of Recommendations Pertaining to Criterion 3
|
|
Program Perspective |
||
|
|
Do-It-Yourself Program |
Nonclinical Program |
Clinical Program |
|
Be judged primarily on success in achieving long-term weight loss, including small losses that are maintained |
Yes |
Yes |
Yes |
|
Be judged on ability to empower clients to eat a healthful diet and become more active, reduce obesity-related comorbidities, improve objective and subjective measures of quality of life, and make desired changes in health-related knowledge and attitudes |
Yes |
Yes |
Yes |
|
Provide information and guidance on improving health behaviors and discuss potential risks of dieting, including those from their programs |
Yes |
Yes |
Yes |
|
Contact with health-care provider for monitoring and disposition of any obesity-related comorbidities |
Encourage clients, especially those with obesity-related comorbidities |
Provide medical assessment and monitoring |
|
|
Evaluate outcomes |
Probably not cost effective or practical. Make sure to cover the importance of long-term weight loss and the reduction of obesity-related comorbidities, provide information and guidance on improving health behaviors, and discuss potential health risks from weight loss in general and their program in particular. |
Monitor and document weight loss of clients over time. Have quality control procedures in place to ensure that protocols are adhered to by staff, and modify protocols given the feedback and experiences of clients. Have mechanisms to evaluate success of program. |
|
|
Consumer Perspective |
|||
|
You and the program have joint responsibilities for your final outcome. |
|||
|
Have realistic expectations of program and be willing to devote the time and effort required. |
|||
|
Choose a program in light of your own short- and long-term goals for weight management. Reevaluate your goals every 3 to 6 months. |
|||
|
Choose programs that focus on long-term weight management; provide instruction in healthful eating, increasing activity, and improving self-esteem; and explain thoroughly the potential health risks from weight loss. |
|||
|
Look for programs that devote considerable effort to helping people change their behaviors through information, guidance, and skills training. |
|||
|
For do-it-yourself programs, look through program literature for information (beyond testimonials or other anecdotal evidence) that program is successful. |
|||
|
If you are in a do-it-yourself or nonclinical program, be in touch with a health-care provider who can monitor any changes in your health. |
|||
|
Expect that at 3- to 6-month intervals, a program will evaluate whether you are meeting your goals and whether the goals or treatment should be modified. |
obesity-related comorbidities) to have regular contact with a health-care provider throughout the treatment and maintenance phases of their weight loss so that their overall health can be monitored as well as the disposition of any comorbidities. Clinical programs should be expected to provide this medical assessment and monitoring.
It is appropriate that weight-management programs continue to be judged primarily on their success in achieving long-term weight loss (including small weight losses that are maintained). However, in addition, programs should be judged on their ability to empower their clients to eat a healthful diet and become more active, reduce obesity-related comorbidities, improve objective and subjective measures of quality of life, and make desired changes in health-related knowledge and attitudes.
Consumer's Perspective on Criterion 3: Are the Benefits I Am Likely to Achieve from the Program Worth the Effort and Cost?
When they begin a weight-management program, consumers must recognize that they and the program have responsibilities for the final outcome. To improve their chances for success, consumers should choose programs that focus on long-term weight management; provide instruction in healthful eating, increasing activity, and improving self-esteem; and explain thoroughly the potential health risks from weight loss. Individuals
interested in a specific do-it-yourself program should search in the program literature for evidence that the program is successful; if information on success is absent or consists primarily of testimonials or other anecdotal evidence (including, in the case of programs by health-care providers, only their own clients or patients), the program should be viewed with suspicion.
Consumers should look for programs that devote considerable effort to helping people change their behaviors through information, guidance, and skills training. To make the most of the weight-management effort, however, consumers should have realistic expectations of a program and be willing to devote the time and effort required. Those in do-it-yourself and nonclinical programs should be in touch with a health-care provider who can monitor the status of any obesity-related comorbidities and changes in health.
When individuals choose a program, it should be in light of their short- and long-term goals for weight management. Our Weighing the Options model (see Figure 1) is a dynamic one that incorporates periodic reevaluation by the client and program to assess whether an individual and a program are meeting these goals and whether the goals or the treatment should be modified. We recommend these evaluations every 3 to 6 months.
Truth and Full Disclosure
It is important to determine the nature and amount of information to be disclosed to individuals considering a weight-management program. Information on program disclosure should be sufficient to enable the client to make informed choices among the program options and, we hope, decrease unrealistic expectations. Our recommendations, if put into practice, should also lead to decreases in unsubstantiated claims and thus highlight any unethical behavior by the programs themselves. The background for these recommendations is the extensive literature on informed voluntary consent that has become a key element in research on human subjects and several sets of guidelines described in Chapter 1: the truth-in-dieting regulation in New York City, the weight-loss guidelines for Michigan, actions by the Federal Trade Commission to regulate deceptive claims by weight-loss programs, and National Institutes of Health guidelines for evaluating weight-loss programs and choosing a weight-loss program.
Any weight-management program has a responsibility to prospective clients to provide truthful and unambiguous information that is not misleading or subject to misinterpretation. This includes a written (and, for nonclinical and clinical programs, oral) description of the risks and
benefits of treatment and an opportunity to ask questions. To assist individuals in making informed choices from the many nonclinical and clinical programs, information made available should include the nature of a given program, its structure and management, and a description of its staff, including training; all costs, including effort and time; the type of client typically served by the program; and the short- and long-term treatment outcomes. Key elements of these recommendations are provided in Table 4. Obviously there can be no such standardization for do-it-yourself programs, given the nature of the individual's interaction with these programs, the wide variety of approaches that they encompass (e.g., books, devices, products, and dietary supplements), and their almost unlimited freedom to make statements and claims.
To facilitate comparisons between programs, we recommend that weight-management programs collect the data summarized in Table 5. At the current time, it is difficult to compare different programs, in part
TABLE 4 Program Disclosure of Information
|
All potential clients of weight-management programs should receive information such as the following: |
|
• A truthful, unambiguous, and nonmisleading statement of the approach and goals of the program. Part of such a statement might read, for example, ''We are a program that emphasizes changes in lifestyle, with group instruction in diet and physical activity." |
|
• A brief description of the credentials of staff, with more detailed information available on request. For example, "Our staff is composed of one physician (M.D.), two registered nurses (R.N.s), three registered dietitians (R.D.s), one master's-level exercise physiologist, and one Ph.D.-level psychologist. At your first visit, you will be seen by the physician. At each visit you will be seen by a dietitian and exercise physiologist and after every five visits by the psychologist. Résumés of our staff are available on request." |
|
• A statement of the client population and experiences over a period of 9 months or more. For example, "To date, we have seen 823 clients for at least three visits each. Although only 26 clients have participated in this program for more than 1 year, they have maintained an average weight loss of 12 pounds." |
|
• A full disclosure of costs. For example, "If you avail yourself of all our facilities with one weekly visit for a period of 1 year, the total cost to you will be between $2,000 and $2,500." Costs should include the initial cost; ongoing costs and additional cost of extra products, services, supplements, and laboratory tests; and costs paid by the average client. Programs may also wish to provide information on the experiences clients have had in recovering their costs from third-party payers. |
|
• A statement of procedures recommended for clients. For example, "We urge that each of our clients see a physician before joining our program. If you have high blood pressure or diabetes, you should see your physician at intervals of his or her choosing while with our program." |
TABLE 5 Collection of Data by Weight-Management Programs
|
1. The number of people attending the first treatment session. (This is the group of potential clients and those who will become actual clients.) |
|
2. Number of clients attending their first two treatment sessions (a gauge of those who have really begun a program) and percentage continuing to participate in the program at 1, 3, 6, and 12 months. (These timepoints seem reasonable but are selected somewhat arbitrarily, for while there is no set of ideal timepoints, it is important to have a set for standardization and comparison among programs. Programs may, of course, use additional timepoints.) |
|
3. Average weight, height, body mass index (BMI), and waist-to-hip ratio (WHR) of clients attending the first two sessions and average change in these variables at 1, 3, 6, and 12 months in the program. (These data should be assembled by gender and, if possible, by race, age, and starting weight or BMI.) |
|
4. The percentage of actual clients who complete each of the stages of the treatment program. This means either the number of clients that complete the program's prescribed number of sessions (e.g., 8 weeks for an 8-week program) or the number of clients in treatment at 3 months. |
|
5. The percentage of actual clients who re-enroll in the same program for further treatment. (This figure should not necessarily be interpreted as a measure of client failure in a program; it may indicate satisfaction with the program.) |
because of differences in the clients selected and in the data collected and reported.
If programs make claims for long-term maintenance of weight loss, the percentage of clients who have lost weight and maintained it for 1 and 2 years should be provided (along with the percentage of clients for whom the information is available) as well as the average weight loss. Many companies use testimonials, often from prominent people, to show a program's success at achieving weight loss. In these cases, they should also cite the experience of their clients in general (as noted above) or cite the general experience of similar dieters taken from reports in the scientific literature.
Implications of Our Recommendations
We are well aware that our recommendations will elicit a variety of reactions. Some will consider them to be overly general and not providing sufficiently detailed guidance to consumers for selecting a program and to programs for improving the quality of their services. Others will see the recommendations as being too prescriptive—too much like implicit standards of care that regulatory agencies or consumer-protection bodies at the national, state, or local levels might turn into regulations resulting in potentially onerous and expensive limitations on the conduct of major commercial weight-loss programs. We developed our recommendations
without engaging in this debate and based them on the scientific research available and the deliberative judgment of the committee. As one expert committee, we think it likely that implementing our recommendations will help more people to lose weight successfully and keep it off over the long term. How they are implemented, however, should be decided not by us but by broad constituencies through an interactive process of public discussion. Consumers, weight-management programs, researchers, and regulatory agencies should all find these recommendations of use in somewhat different ways.
Given the billions of dollars consumers currently spend on weight-loss programs, we believe strongly that these programs require special attention and evaluation. Unfortunately, our health-care system has not treated obesity as a chronic disease requiring long-term management, even as the prevalence of this disease continues to increase. We believe that a new concept of obesity treatment is needed, and this report represents a first effort by a group of biomedical experts convened by the Food and Nutrition Board of the Institute of Medicine to stimulate this process. This report provides clients, obesity-management programs, researchers, and policymakers with recommendations by which to evaluate programs and outcomes. Although there will undoubtedly be discussion about the specific details of our recommendations, we believe that consensus exists about the need for them.
THE FUTURE OF WEIGHT MANAGEMENT
Successful weight management ultimately includes preventing obesity from developing in the first place or delaying its onset and keeping somewhat overweight individuals from becoming obese, subjects addressed in Chapter 9. At this time, the tools are not available to prevent obesity, and most prevention programs to date have ended in failure. Programs to prevent obesity and encourage the adoption of healthier lifestyles among adults at work sites and in community programs produce modest results at best. Very few studies have investigated preventing obesity in children, for example, through school-based programs or by modeling healthy eating behaviors in the family. We recommend that money not be spent on large obesity prevention programs; smaller-scale research programs on prevention should be focused, perhaps according to stages of life at which obesity is more likely to occur, such as adolescence, or among high-risk groups, such as black females. Given the disappointing results of obesity prevention programs, more studies are needed on how to conduct large-scale intervention studies more effectively and to produce more desirable results.
Chapter 10 describes our research and policy recommendations. Continued
research to understand the fundamental causes of obesity, particularly at the molecular and genetic levels, is enormously important. In addition, the behavioral and environmental influences on the expression of obesity need to be much better understood. The genetic and environmental determinants of obesity and its associated comorbidities vary among population groups, and the variation and reasons for this variation are important areas of research. In addition, research is needed on cognitive-behavioral approaches to increase success at long-term weight loss and maintenance and to further understand the contributions of diet and physical activity in achieving successful weight management. Furthermore, it would be useful to determine the mechanisms by which antiobesity drugs and gastric surgery promote weight loss.
While research should eventually uncover the causes of obesity and lead to this disease being better managed, prevented, and treated, the application of scientific findings alone is rarely enough to resolve public health problems. Public policies are needed to translate the research findings to the lay public and to apply what is already known about successful weight management. We have three major public-policy recommendations:
-
Obesity should be acknowledged as one of this country's most important nutrition-related diseases, which has important consequences for the funding of research by government, foundations, and private agencies; for health-care reform; and for oversight of the weight-loss industry by regulatory agencies.
-
There must be increased recognition and support for obesity research at the genetic, molecular, and cellular levels that will aid our understanding of the causes of obesity and its associated comorbidities.
-
A more aggressive policy is required to inform the public and health-care providers about the nature of obesity, the difficulties inherent in treating this disease, and the need for susceptible individuals to take steps to prevent its occurrence or minimize its development. Health-care providers in particular should learn more about obesity and its treatment.
Because successful weight management has proven an elusive goal for most obese individuals in the United States, the marketplace has provided many legitimate as well as unfounded products and services. Improving the rate of success at weight management requires would-be dieters to understand that gimmicks, from weight-loss pills to esoteric diets, either are totally ineffectual or are no more than small countermeasures to an incompletely understood disorder of energy balance. Furthermore,
dieters should stay away from programs that claim more than they can substantiate or state that their unique methods ensure permanent weight loss. For its part, the scientific community must continue research to provide a fundamental understanding of the causes of obesity, leading to the design of maximally successful treatments and means to more effectively prevent this disease.