Effect of Human Ecology and Behavior on Sexually Transmitted Diseases, Including HIV Infection
JUDITH N. WASSERHEIT
There are few infectious diseases that crystallize as hauntingly as sexually transmitted diseases (STDs) the effects of changes in human ecology and behavior on disease patterns. Webster's unabridged dictionary defines ecology as "a branch of science concerned with the interrelationship of organisms and their environment, especially as manifested by natural cycles and rhythms, community development and structure, interactions between different kinds of organisms, geographic distributions, and population alterations" (1). The dismaying growth in the spectrum and rates of STDs experienced over the past two decades in most parts of the world, including the United States, is, indeed, a reflection of the complex interactions of these pathogens with at least three types of environments. In this brief overview, I will summarize six changes in STD patterns that have emerged during the past 20 years and discuss their links to changes in the physiological microenvironment, the behavioral personal environment, and the sociocultural macroenvironment. Finally, I will highlight the implications of these links for effective STD prevention programs.
CHANGING PATTERNS OF SEXUALLY TRANSMITTED DISEASES
The last 20 years have witnessed six striking changes in STD patterns: emergence of new STD organisms and etiologies, reemergence of old
Judith N. Wasserheit is director of the Division of STD/HIV Prevention, National Center for Prevention Services, Centers for Disease Control and Prevention, Atlanta, Georgia.
TABLE 1 Changing patterns of STDs
|
Pattern |
Examples |
|
Emergence of new organisms/etiologies Reemergence of old STDs Population shifts Etiology shifts Altered incidence of complications Increased antimicrobial resistance |
HIV, infertility, ectopic pregnancy, fetal death, low birth weight, prematurity, anogenital cancer, proctocolitis Syphilis HIV infection, syphilis, gonorrhea Urethritis, cervicitis, PID Perinatal HIV infection, congenital syphilis, PID, dysplasia Gonorrhea, chancroid |
|
PID, pelvic inflammatory disease. |
|
STDs, shifts in the populations in which STDs are concentrated, shifts in the etiological spectra of STD syndromes, alterations in the incidence of STD complications, and increases in antimicrobial resistance (Table 1). Many STDs represent examples of more than one of these trends.
Exciting insights into the pathophysiology and natural history of both bacterial and viral STDs have led to the discovery of sexually transmitted etiologies for such diverse syndromes as infertility, ectopic pregnancy, other adverse outcomes of pregnancy, anogenital cancers, and proctocolitis. However, human immunodeficiency virus (HIV) is clearly the archetype of a newly emerging STD pathogen, one that has devastated the world with a fatal pandemic involving an estimated 14 million people, of whom approximately 2.5 million have developed AIDS (2). In the United States alone, it is likely that as many as a million individuals are infected with HIV, and more than 361,000 AIDS cases have been reported since 1981, when the syndrome was first recognized (3).
Despite its recent emergence, AIDS is, in addition, a prime example of a disease that is shifting to affect new populations (Figure 1). In the United States, AIDS spread first among predominantly white homosexual and bisexual men, but AIDS incidence in this population began to plateau by the early 1990s (4, 5). The second wave of the AIDS epidemic emerged among injecting-drug users (IDUs) and was concentrated among racial and ethnic minority populations. At least since 1989, however, the greatest proportionate increase in reported AIDS cases has been due to heterosexual transmission, and the majority of these cases have occurred among women (4–7). Between 1991 and 1992, for example, a 17% increase in AIDS cases attributed to heterosexual transmission was observed, compared with a 1% decrease in cases due to homosexual or bisexual transmission, and a 1% increase in IDU-related cases among heterosexuals. In 1992, although half of all new AIDS cases
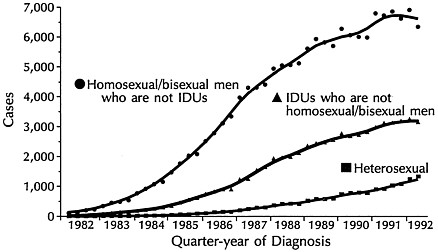
FIGURE 1 AIDS incidence by transmission category and quarter-year of diagnosis, January 1982 through June 1992, United States. Data are adjusted for delays in reporting but not for incomplete reporting.
occurred among homosexual or bisexual men, almost 60% of heterosexually transmitted AIDS cases occurred in women, and, for the first time, more women were reported with AIDS as a result of heterosexual transmission than as a result of injecting-drug use. Furthermore, among women, non-Hispanic Blacks experienced the most rapid increases in heterosexually acquired AIDS (5).
Syphilis offers a classic example of the reemergence of an easily diagnosed and readily treatable STD. Following World War II, with the widespread availability of penicillin, infectious (primary and secondary) syphilis rates in the United States fell almost 95%, from 66 cases per 100,000 persons in 1947 to 4 cases per 100,000 persons in 1956. However, this triumph was not sustained. The incidence of syphilis rose progressively after 1956 to reach a 40-year peak of 20 cases of infectious syphilis per 100,000 persons by 1990 (8).
Echoing some aspects of the sequential AIDS epidemics discussed above, syphilis also exemplifies a STD that has shifted its principal target from one population to another. The syphilis epidemic hit the United States in two distinct waves. The first, from about 1960 to 1980, was concentrated among homosexual men, and the second, over the latter half of the subsequent decade, had its greatest impact among minority heterosexuals. As is elegantly highlighted by Rolfs and Nakashima (8), this shift was reflected in striking changes in the male/female incidence rate ratio for infectious syphilis during this 30-year period (Figure 2).
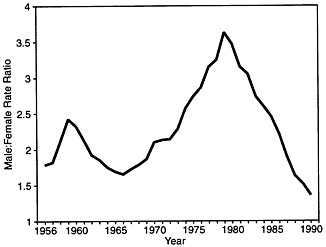
FIGURE 2 Primary and secondary syphilis in the United States, 1956–1990. Reprinted with permission from ref. 8 (copyright 1994, Blackwell Scientific Publications).
From 1966 to 1979, the ratio more than doubled, from 1.7 to 3.6, and then fell precipitously to 1.3 by 1991. Between 1985 and 1990, infectious syphilis rates also rose 165% among non-Hispanic Blacks, while they fell among persons of all other races and ethnicities. The 14-fold higher syphilis rates among Blacks than among Whites reported in 1985 exploded to a 60-fold differential by 1991 (9).
As the AIDS and syphilis epidemics penetrated heterosexual populations, the incidence of perinatal and congenital infections increased as well. AIDS cases resulting from perinatal transmission increased 13.4% between 1991 and 1992, an increase second only to that due to heterosexual transmission itself (5), and congenital syphilis rates increased at least 5-fold between 1985 and 1991, after adjustment for the new case definition that was instituted in 1989.
Gonorrhea trends in the United States present a sharp contrast to syphilis patterns and, again, highlight the protean nature of STDs. Despite the common mode of transmission shared by these STDs, gonorrhea and infectious syphilis trends have consistently diverged over the past 25 years (Figure 3). From 1965 to 1975, gonorrhea rates more than doubled, while infectious syphilis rates increased slightly. During the next 15 years, gonorrhea rates declined with increasing momentum as syphilis rates skyrocketed (10).
In addition to the population shifts characterized by sexual practices,
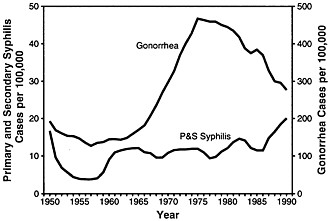
FIGURE 3 Rates of primary and secondary syphilis and gonorrhea in the United States, 1950–1990. Reprinted with permission from ref. 8 (copyright 1994, Blackwell Scientific Publications).
race, and gender observed with syphilis, age-related population shifts have been seen with gonorrhea. Over the last decade, gonorrhea rates have declined among both men and women in all age groups between 15 and 40 years of age except 15- to 19-year-olds (9). As a result, adolescents in this country now have the highest age-specific gonorrhea rates among women and the second highest age-specific rates among men. After adjustment for the proportion of the population which is sexually active, the gap between teenagers and older adults widens even more (11).
Gonorrhea also provides an excellent example of rapid and repeated emergence of new types of antimicrobial resistance. The recognition of penicillinase-producing Neisseria gonorrhoeae in 1976 has been followed by appreciation of an increasingly diverse array of resistance patterns and mechanisms, including both plasmid- and chromosomally mediated resistance to penicillins and tetracyclines, the two former mainstays of treatment (12). Between 1988 and 1991, national surveillance of gonococcal isolates conducted by the Centers for Disease Control and Prevention documented an increase in the proportion of resistant isolates from 21% to 32.4%, more than a 50% increase in only 3 years (9, 13, 14)!
In the United States, as gonorrhea rates have declined, chlamydia rates have climbed, shifting the apparent balance of etiologies of urethritis, cervicitis, and PID. Indeed, in 1991, reported chlamydia cases exceeded reported gonorrhea cases among women for the first time (9).
However, this reversal is probably an artifact of real changes in gonorrhea incidence superimposed upon improved chlamydia surveillance due to both diagnostic advances and more widespread legal requirements for chlamydia reporting. Nevertheless, a relative increase in chlamydial infection may have contributed to recent decreases in hospitalized cases of PID in the face of stable numbers of ambulatory PID cases because of the more indolent nature of chlamydial infection compared with gonococcal PID (15).
Human papillomavirus (HPV) infection provides a final example of changing patterns of STDs. HPV infection has repeatedly emerged as one of the most important risk factors for cervical dysplasia (16–18). Furthermore, several studies have documented an increased prevalence of dysplasia among HIV-infected women compared with HIV-uninfected subjects (19). In a recent New York City study, for example, HIV-infected women were almost 6 times as likely to have colposcopic evidence of cervical intraepithelial neoplasia as their HIV-uninfected counterparts, and the majority of cervical intraepithelial neoplasia was attributable to HPV infection in both groups (T. C. Wright, T. V. Ellerbrock, and M. A. Chiasson, personal communication).
ENVIRONMENTAL CHANGES AFFECTING STD PATTERNS
Why have all of these changes in STD patterns occurred? What environmental changes continue to drive the evolution of these disease patterns?
Let us consider three interrelated types of environments affecting STD patterns (Figure 4). The microbiologic, hormonal, and immunologic microenvironments most directly influence susceptibility, infectiousness, and development of sequelae. These microenvironments are shaped, in part, by the personal environments created by an individual's sexual, substance-use, and health-related behaviors.
The personal environments are also important determinants of acquisition of infection and development of sequelae but, in addition, they mediate risk of exposure to infection. These are, therefore, the environments that most directly affect changing disease patterns such as the emergence or reemergence of STDs, or the population shifts discussed above.
Finally, individuals' personal environments are, in turn, molded by powerful macroenvironmental forces, including socioeconomic, demographic, geographic, political, epidemiologic, and technological factors. Over the past 20 years, the profound changes that have occurred in many aspects of the personal environment and the macroenvironment have been reflected in new STD patterns.
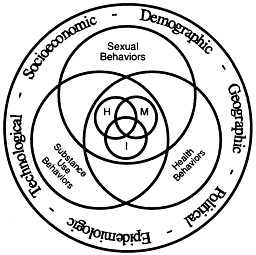
FIGURE 4 Environments affecting STD patterns. M, microbiological; H, hormonal; I, immunological.
The Physiological Microenvironment
Trend data are not available for most of the biological indices of the microenvironments affecting STD patterns (Table 2). For example, while we know that the vaginal flora and acidity (pH) of the microbiological microenvironment influence susceptibility to STDs, we do not know how these factors have changed over time among populations of women in the United States. Similarly, manifestations of the hormonal microenvironment, such as the size of the zone of cervical ectopy,* the penetrability of the cervical mucus, the patency of the cervical canal, the phase of the menstrual cycle, and possibly even the composition of seminal and prostatic fluids, may contribute to susceptibility to STDs or their sequelae (20), and we know little about population trends in these factors.
Trend data are, however, obtainable for a few of these microenvironmental parameters. By altering cervicovaginal ecology, modulating vaginal pH, transactivating other pathogens, or other mechanisms, one STD may increase susceptibility to other STDs or their complications (19, 21). Thus, recent increases in STDs may have fueled some of the
TABLE 2 Microenvironments affecting STD patterns
|
Microbiologic |
Hormonal |
Immunologic |
|
Vaginal flora and acidity (pH) |
Cervical ectopy |
Pregnancy |
|
STD coinfection |
Cervical mucus |
HIV infection |
|
|
Cervical patency |
Prior STD exposure |
|
|
Menses |
|
|
|
Seminal/prostatic fluid? |
|
changing disease patterns biologically as well as epidemiologically. Decreases in the age of menarche, a manifestation of the hormonal microenvironment, have been documented (22, 23). Finally, competing factors that influence the immunological microenvironment, such as pregnancy, HIV infection, and prior exposure to STDs, can also be traced over time in some populations.
The Behavioral Personal Environment
Changes in sexual behaviors have been one of the primary engines driving changing patterns of STDs, including HIV infection (Table 3). Steady decreases in age of first sexual intercourse and concomitant increases in premarital sexual activity have been documented repeatedly both in the United States and abroad (21, 24, 25). Data from the National Survey of Family Growth, for example, indicate that the percentage of 15- to 19-year-old American women reporting premarital intercourse almost doubled from 28.6% in 1970 to 51.5% in 1988 (26). Although increases were greatest among younger White adolescents, the proportion of Black women reporting premarital sexual activity was higher than the proportion of White women for each age group and year examined. This trend is particularly disturbing because early age of
TABLE 3 Personal environments affecting STD patterns
|
Sexual behaviors |
Substance-use behaviors |
Health behaviors |
|
Age at coital debut |
Intravenous drug use |
Condom use |
|
Number of sex partners |
Crack cocaine |
Pill and IUD use |
|
Commercial sex |
Exchange of sex for drugs |
Vaginal douching |
|
Sexual practices |
Alcohol use |
Circumcision |
|
|
|
Early health-care utilization |
|
|
|
Compliance with therapy |
|
|
|
Provider screening |
|
IUD, intrauterine device. |
||
coital debut appears to be associated with subsequent patterns of multiple sexual partners and sex with risky partners, such as bisexual, injecting-drug-using, or HIV-infected individuals (27). Furthermore, the hormonal microenvironment is age-dependent. Thus, for young adolescents, behavioral risk factors such as multiple, risky partners conspire with biological risk factors such as large zones of cervical ectopy to result in high STD rates.
Younger cohorts also report more sexual partners than older groups, and the proportion of young adults with multiple sexual partners appears to be increasing over time (24, 25, 28-31). In fact, between 1971 and 1988, the proportion of sexually active adolescent women reporting more than one sexual partner swelled from 39% to 62% (29). In part this may be due to the combined effect of trends toward younger age of coital debut and older age at first marriage. During the decade of the '80s, American women experienced an increase of approximately 30% in the median number of years that they spend in this relatively high risk stage of their reproductive lives (32). In addition, these increases were greatest for Black women and for women living in poverty.
Sonenstein and colleagues (33) have observed analogous trends among young men. Among 17- to 19-year-old American men, the average number of sexual partners in the previous year rose from 2.0 in 1988 to 2.6 in 1991, and the proportion reporting 5 or more partners increased from 6% to 11% over the same time period. Both this study and the 1991 National Survey of Men suggest that Black men report more sexual partners than White or Hispanic men; however, other national survey data indicate that these patterns vary substantially by gender and marital status (30-32, 34).
Both commercial sex (exchange of sex for money or drugs) and specific sexual practices such as anal intercourse, intercourse during menses, or ''dry sex"* have also been linked to increased risk of STDs or their sequelae (21, 35-37). However, few trend data are available on these sexual behaviors. Cross-sectional national survey data indicate that more White men than Black men reported anal intercourse (21% vs. 13.6%) or same-gender sexual activity during the past 10 years (2.4% vs. 1.3%) (30). In contrast, anecdotal information suggests that dry sex may be practiced more frequently by Black Americans than by Whites (31).
Over the past 25 years, dramatic changes in substance-use behaviors reinforced the impact of changes in sexual behaviors on STD and HIV patterns. Drug use promotes anonymous sex and exchange of sex for drugs or money. Both drug and alcohol use may also impair ability to practice safe sex. In this context, it is very disturbing that the National Institute on Drug Abuse estimates that illicit drug use increased from less than 5% of Americans ever using these substances in the early 1960s to over 10% by the early 1970s (38). By 1988, an estimated 36.6% of Americans 12 years of age or older had tried illicit drugs.
In terms of impact on STD and HIV trends, regular or recent use of illicit drugs is more important than previous experimentation. The National Household Survey of Drug Abuse indicates that use of most illicit drugs (including cocaine) at least once within the past year increased during the 1970s and peaked during the first half of the 1980s (39). Reported use of cocaine within the past year by high school seniors, for example, rose from 5.6% in 1975 to 13.1% in 1985, and subsequently declined to 3.5% by 1991.
Intravenous drug use and crack cocaine use have been particularly potent factors in the changing patterns of STDs, especially syphilis and HIV infection (21, 40). Both of these behaviors have been associated with low socioeconomic status and appear to be more common among Black and Hispanic Americans than among White Americans (31, 38).
Health-related behaviors are the third component of the personal environments affecting STD patterns (Table 3). Several of these behaviors, such as early health-care utilization, compliance with therapy, and provider screening, primarily affect the distribution of the curable STDs by reducing the duration of infectiousness of these diseases and by limiting the incidence of long-term complications.
Other health-related behaviors, such as contraceptive use, vaginal douching, and circumcision, may influence STD patterns more broadly (21). Correct and consistent condom use and male circumcision both decrease risk of STDs, including HIV infection (41). Oral contraceptive pill use, on the other hand, may augment risk of chlamydial and gonococcal cervicitis but seems to decrease risk of PID (41). Both of these effects are probably mediated by pill-induced changes in the hormonal microenvironment such as expanded zones of ectopy and decreased penetrability of cervical mucus. IUD use and vaginal douching have been linked with increased risk of PID—in the former case, principally during the first 3 months following device insertion (41, 42). These two behaviors also clearly alter the vaginal microenvironment. Finally, both pill and IUD use may increase STD risk by reducing the likelihood of condom use.
Contraceptive use trends have been a critical force in evolving STD
patterns. One of the key elements of the sexual revolution of the 1960s was the rapid diffusion of the pill, the first unobtrusive, female-controlled pregnancy prevention technology. National surveys of married women showed steady increases in pill use until 1973, a decline from 1973 to 1982, and stabilization in use rates between 1982 and 1988 (43). During the 1982-1988 period, pill use also remained unchanged among never-married and formerly married women but increased among women between the ages of 20 and 34, while IUD use declined in all groups. Condom use increased from 12% to 20% among never-married women, and from 21% to 33% among 15- to 19-year-olds during this period. Smaller gains were observed among women in their twenties. Contraceptive use at first intercourse grew from 47% of women in 1975-1979 to 66% of women in 1983-1988, with the increases entirely attributable to condom use among Whites and increases balanced between condom use and pill use among Blacks (44).
National longitudinal data on vaginal douching and on male circumcision are not available. However, national data collected in 1988 document that vaginal douching is strongly associated both with Black race and with poverty (31). Anecdotal information suggests that circumcision may be more common among White men than among other racial or ethnic groups.
Data on health-care utilization, compliance with therapy, and provider screening behaviors are also quite limited, and conflicting information on racial or ethnic differentials makes definitive interpretation difficult (31). Furthermore, a reporting bias may arise because racial/ethnic minority populations often seek care from publicly funded providers who are more likely to test for and report STDs than are private providers (21). Yet financial and social barriers to early and effective care clearly disproportionately affect adolescents and members of minority communities who live in poverty. Deterioration of the public health infrastructure in the United States during the 1980s has undoubtedly exacerbated these problems and may have contributed to the spread of HIV infection, the reemergence of adult and congenital syphilis, and the rapid evolution of gonococcal resistance.
The Sociocultural Macroenvironment
Perhaps the greatest challenge of STD and HIV prevention lies in developing strategies that acknowledge the powerful and interrelated macroenvironmental forces that shape many of the sexual, substance-use, and health-related behaviors of individuals' personal environments (Table 4). Factors such as poverty, low status of women, social up-heaval, urbanization, and migration or geographic mobility promote risk
TABLE 4 Macroenvironments affecting STD patterns
|
Socioeconomic |
Political |
Demographic |
|
Poverty |
Public health infrastructure |
Young age structures |
|
Status of women |
Social upheaveal |
Sex ratio imbalance |
|
Geographic |
Technological |
Epidemiologic |
|
Urbanization |
STD tests |
STD prevalence |
|
Domestic and international travel |
STD therapies |
|
|
Migrant labor |
Prevention technologies (e.g., female condom) |
|
behaviors because they destabilize societal norms by increasing inequality, anonymity, and marginalization (21, 45). These factors often cluster in and foster environments with fragile public health infrastructures, thus creating barriers to health-related behaviors among populations most in need of services. Communities of high STD and HIV prevalence result. Further social disintegration may ultimately precipitate extensive out-migration and spread of disease (46).
The demographic characteristics of these populations frequently compound the problem. Young age composition and sex ratio imbalance are linked with many of the factors mentioned above, as well as with STD and HIV risk behaviors. It is noteworthy that in the United States relatively large and growing segments of minority populations are sexually active adolescents and young adults, while the proportion of the White population in these groups has been declining since the mid-1980s (21, 45).
Poverty and deterioration of the public health infrastructure have been particularly important forces in shaping STD and HIV patterns in the United States. Poverty is associated with substance abuse, exchange of sex for drugs or money, poor access to health services, and young age at first intercourse. Both the poverty rate and income inequality increased in this country during the last 20 years. The poverty rate rose to 14.2% in 1991 from 11.4% in 1978 and disproportionately affected women, young people, and racial and ethnic minority populations, particularly in urban areas (31, 47, 48). For example, the proportions of White, Hispanic, and Black Americans living in poverty in 1991 were 11.3%, 28.7%, and 32.7%, respectively. The comparable figures for 1973 (the first year for which data on Hispanic origin were recorded) were 8.4%, 21.9%, and 31.4%. These data and shifts in race/ethnicity-specific ratios of actual income to poverty level income highlight both that the extent and depth of poverty are greatest among Black Americans and
that Hispanic Americans have experienced the largest increases in poverty over the last two decades.
These socioeconomic trends have been accompanied by changes in the political environment that further limited the access to STD care for those relying on public sector providers. At the same time that chlamydia, herpes, HPV infection, and AIDS emerged, and as syphilis rates climbed and treatment of gonorrhea required increasingly expensive antibiotics, support for STD services flagged and the public health infrastructure in the United States deteriorated. Many STD clinics across the country were unable to meet the demand for services and, increasingly, were forced to turn patients away without care. Frequently, those patients who did receive care had to wait many hours to be seen. A survey of public STD clinics conducted in 1989 revealed problems of this type in 19 of 23 sites (45). It is ironic that these trends occurred in the setting of tremendous advances in diagnostic and therapeutic technologies which should have made feasible highly effective STD prevention programs. Furthermore, increased knowledge about the effectiveness of condoms and other prevention technologies was offset by the development of a more conservative political environment.
IMPLICATIONS FOR EFFECTIVE STD PREVENTION PROGRAMS
STDs offer an outstanding "case study" of the synergistic effects of changes in human ecology and behavior on patterns of infectious diseases. The last 20 years have brought explosive growth in the spectrum, complexity, range of sequelae, and, in some cases, incidence of STDs. It is likely that complete eradication of STDs, including HIV infection, must await development of vaccines that can be delivered in conjunction with antimicrobial agents and behavioral interventions. However, even in the absence of effective vaccines, enormous progress can be made in prevention and control of these infections if we broaden our focus to include all three of the environments discussed above.
Traditional, clinic-based STD programs have emphasized interventions that target the physiological microenvironments and selected health behaviors. Programs developed with an appreciation of the role of risk behaviors and macroenvironmental forces in STD and HIV epidemiology will be likely to improve the effectiveness of these clinical interventions by focusing them on populations most in need of services and by addressing barriers to care that might otherwise be ignored.
The multiple environments affecting STD patterns highlight three other important principles. First, both clinic-based and community-based behavioral interventions are essential companions to diagnosis and treatment in effective prevention programs. Second, STD/HIV
prevention, substance-abuse prevention, and pregnancy prevention efforts are likely to reinforce each other. Finally, the community can play a pivotal role in modulating the impact of macroenvironmental factors on the personal environments that shape STD and HIV patterns.
SUMMARY
The last 20 years have witnessed six striking changes in patterns of sexually transmitted diseases (STDs): emergence of new STD organisms and etiologies, reemergence of old STDs, shifts in the populations in which STDs are concentrated, shifts in the etiological spectra of STD syndromes, alternations in the incidence of STD complications, and increases in antimicrobial resistance. For example, human immunodeficiency virus (HIV) emerged to devastate the United States with a fatal pandemic involving as many as 1 million people. The incidence of syphilis rose progressively after 1956 to reach a 40-year peak by 1990. In both cases, disease patterns shifted from homosexual men to include minority heterosexuals. Over the last decade, gonorrhea became increasingly concentrated among adolescents, and several new types of antimicrobial resistance appeared. Three interrelated types of environments affect STD patterns. The microbiologic, hormonal, and immunologic microenvironments most directly influence susceptibility, infectiousness, and development of sequelae. These microenvironments are shaped, in part, by the personal environments created by an individual's sexual, substance-use, and health-related behaviors. The personal environments are also important determinants of acquisition of infection and development of sequelae but, in addition, they mediate risk of exposure to infection. These are, therefore, the environments that most directly affect changing disease patterns. Finally, individuals' personal environments are, in turn, molded by powerful macroenvironmental forces, including socioeconomic, demographic, geographic, political, epidemiologic, and technological factors. Over the past 20 years, the profound changes that have occurred in many aspects of the personal environment and the macroenvironment have been reflected in new STD patterns.
I thank Sevgi Aral, Willard Cates, Jr., Ronald Fichtner, Allyn Nakashima, John Ward, and Linda Wright-DeAguero for their valuable input to this article, and Ed Johns and Diane Vitro for their excellent assistance with the figures and tables.
REFERENCES
1. Grove, P. B., et al., eds. (1966) Webster's Third New International Unabridged Dictionary (Merriam, Springfield, MA), p. 720.
2. Merson, M. H. (1993) IXth International Conference on AIDS, June 6–11, 1993, Berlin, pp. PS-01-1 (abstr.).
3. Centers for Disease Control and Prevention (1993) HIV/AIDS Surveill. Rep. 5, Vol. 4, p 5.
4. Centers for Disease Control and Prevention (1992) Morbid. Mortal. Wkly. Rep. 41, 463–468.
5. Centers for Disease Control and Prevention (1993) Morbid. Mortal. Wkly. Rep. 42, 547–557.
6. Centers for Disease Control and Prevention (1990) Morbid. Mortal. Wkly. Rep. 39, 81–86.
7. Centers for Disease Control and Prevention (1991) Morbid. Mortal. Wkly. Rep. 40, 358–369.
8. Rolfs, R. T. & Nakashima, A. K. (1994) Modern Epidemiology of Syphilis in the United States and Western Europe in Syphilis, eds. Hook, E. W., III, & Lukehart, S. A. (Blackwell, Cambridge, MA), in press.
9. Centers for Disease Control and Prevention (1993) Div. STD/HIV Prevent. Ann. Rep. (Cent. Dis. Contr., Atlanta), pp. 103–174.
10. Gershman, K. A. & Rolfs, R. T. (1991) Am. J. Public Health 81, 1263–1267.
11. Aral, S. O., Schaffer, J. E., Mosher, W. D. & Cates, W., Jr. (1988) Am. J. Public Health 78, 702–703.
12. Whittington, W. L. & Knapp, J. S. (1988) Sex. Transm. Dis. 15, 202–210.
13. Schwarcz, S. K., Zenilman, J. M., Schnell, D., Knapp, J. S., Hook, E. W., III, Thompson, S., Judson, F. N. & Holmes, K. K. (1990) J. Am. Med. Assoc. 264, 1413–1417.
14. Centers for Disease Control and Prevention (1993) Morbid. Mortal. Wkly. Rep. 42, 29–39.
15. Rolfs, R. T., Galaid, E. I. & Zaidi, A. A. (1992) Am. J. Obstet. Gynecol. 166, 983–990.
16. Oriel, J. D. (1990) Int. J. STD AIDS 1, 7–9.
17. Cancer Unit for Microbiology and Immunology, World Health Organization (1987) Bull. World Health Org. 65, 817–827.
18. International Agency for Research on Cancer (WHO) (1989) (Oxford Univ. Press, New York), IARC Sci. Publ. No. 94.
19. Wasserheit, J. N. (1992) Sex. Transm. Dis. 19, 61–77.
20. Ehrhardt, A. A. & Wasserheit, J. N. (1991) in Research Issues in Human Behavior and Sexually Transmitted Diseases in the AIDS Era, eds. Wasserheit, J. N., Aral, S. O., Holmes, K. K. & Hitchcock, P. J. (Am. Soc. Microbiol., Washington, DC), pp. 97–121.
21. Aral, S. O. & Holmes, K. K. (1990) in Sexually Transmitted Diseases, eds. Holmes, K. K., Mardh, P. A., Sparling, P. F., Wiesner, P. J., Cates, W., Jr., Lemon, S. M. & Stamm, W. E. (McGraw–Hill, New York), pp. 19–36.
22. Bullough, U. L. (1981) Science 213, 365–366.
23. Rees, M. (1993) Lancet 342, 1375–1376.
24. Biggar, R. J., Brinton, L. A. & Rosenthal, M. D. (1989) J. Acquired Immune Defic. Synd. 2, 497–502.
25. ACSF investigators (1992) Nature (London) 360, 407–409.
26. Centers for Disease Control and Prevention (1991) Morbid. Mortal. Wkly. Rep. 39, 929–932.
27. Greenberg, J., Magder, L. & Aral, S. O. (1992) Sex. Transm. Dis. 19, 331–334.
28. Johnson, A. M., Wadsworth, J., Wellings, K., Bradshaw, S. & Field, J. (1992) Nature (London) 360, 410–412.
29. Kost, K. & Forrest, J. D. (1992) Family Planning Perspectives 24, 244–254.
30. Billy, J. O. G., Tanfer, K., Grady, W. R. & Klepinger, D. H. (1993) Family Planning Perspectives 25, 52–60.
31. Aral, S. O. & Wasserheit, J. N. (1994) in African-Americans and Hispanics: The Role of Behavioral and Psychosocial Factors, eds. Johnson, E. H., Amaro, H., Antoni, M., Jemmot, J. & Szapocnik, J. (Praeger, New York).
32. Forrest, J. D. (1993) Obstet. Gynecol. 82, 105–111.
33. Ku, L., Sonenstein, F. & Pleck, J. (1993) Am. J. Public Health 83, 1609–1614.
34. Dolicini, M. M., Catania, J. A., Coates, T. J., Stall, R., Hudes, E. S., Gagnon, J. H. & Pollack, L. (1993) Family Planning Perspect. 25, 208–214.
35. Kingsley, L. A., Detels, R., Kaslow, R., Polk, B. F., Rinaldo, C. R., Chmiel, J., Detre, K., Kelsey, S. F., Odaka, N., Ostrow, D., VanRaden, M. & Visscher, B. (1987) Lancet i, 345–349.
36. European Study Group (1989) Br. Med. J. 298, 411–415.
37. Sweet, R. L., Blankfort-Doyle, M., Robbie, M. O. & Schachter, J. (1986) J. Am. Med. Assoc. 255, 2062–2064.
38. U.S. Department of Health and Human Services (1991) Third Triennial Report to Congress on Drug Abuse and Drug Abuse Research (Natl. Inst. Drug Abuse/Alcohol, Drug Abuse and Mental Health Admin., Bethesda, MD), DHHS Publ. No. (ADM)91-1704, pp. 13–29.
39. Drugs and Crime Data Center and Clearinghouse (1992) Fact Sheet: Drug Use Trends (U.S. Dept. of Justice, Bureau of Justice Statistics, Washington, DC), pp. 1–5.
40. Rolfs, R. T., Goldberg, M. & Sharrar, R. G. (1990) Am. J. Public Health 80, 853–857.
41. Cates, W., Jr., & Stone, K. M. (1992) in Reproductive Tract Infections, eds. Germain, A., Holmes, K. K., Piot, P. & Wasserheit, J. N. (Plenum, New York), pp. 93–129.
42. Scholes, D., Daling, J. R., Stergachis, A., Weiss, N. S., Wang, S. & Grayston, J. T. (1993) Obstet. Gynecol. 81, 601–606.
43. Mosher, W. D. (1990) Family Planning Perspectives 22, 198–205.
44. Mosher, W. D. & McNally, J. W. (1991) Family Planning Perspectives 23, 108–116.
45. Aral, S. O. & Holmes, K. K. (1991) Sci. Am. 264, 62–69.
46. Wallace, R. (1988) Environ. Res. 47, 1–33.
47. U.S. Department of Commerce (1992) Poverty in the United States: 1991 (Bureau of the Census, Washington, DC) Current Population Rep., Series P-60, No. 181.
48. U.S. Department of Commerce (1990) Household Wealth and Asset Ownership: 1988 (Bureau of the Census, Washington, DC) Current Population Rep., Series P-70, No. 22.
















