1 The Epidemiology of HIV and AIDS
The picture we can draw of the HIV/AIDS epidemic is limited by the data available. To date, the AIDS case reporting system of the Centers for Disease Control and Prevention (CDC) is the only complete national population-based data available to monitor the epidemic. Although data are useful in evaluating disease prevalence and incidence, reported AIDS cases are only the clinical tip of the iceberg of effects produced by HIV infection. HIV seroprevalence surveys are informative for their description of the magnitude of the epidemic, but they represent people whose date of infection is unknown; these surveys are thus limited in their ability to characterize the current direction of the epidemic. HIV incidence data are far more informative for monitoring the current course of the epidemic. Nevertheless, because HIV infection is not reportable in all states, and because most studies of HIV have not included representative samples, these data are of limited value for generalizing to other specific populations or to the entire U.S. population. HIV surveillance data also provide information that is of limited value in forecasting the future of the epidemic. To address this limitation, some have argued (e.g., Centers for Disease Control and Prevention, 1994a; Turner et al., 1989) that a broader monitoring system of the epidemic should include precursors to AIDS and HIV infection. Better-developed behavioral epidemiologic data on known risk behaviors (i.e., sexual behavior and drug use) could provide data on sites of potential transmission and future spread.
Despite these limitations, current epidemiologic data provide valuable
insights into the HIV/AIDS epidemic in the United States. This chapter reviews these data with particular emphasis on the role of injection drug users. However, before reviewing these data, the panel thought it critical to provide the reader with a brief review of current knowledge of the underlying biological mechanisms involved in the transmission of the virus. The details of these behaviors and processes are important to developing an appreciation for the complexity of the issues at hand.
BIOLOGICAL MECHANISMS OF TRANSMISSION
Although the consensus among the research community is that the development of an effective vaccine for the human immunodeficiency virus (HIV) is still years away, significant strides have been made in biomedical research. As Rogers (1992:522) stated, ''We now know quite precisely how the virus is transmitted and how it is not and what it does to human cells and the immune mechanism, and we know enough about its structure and life-cycle to have identified multiple potential points to get at it."
HIV transmission is limited to sharing of contaminated injection drug paraphernalia, sexual contact, transmission from infected mother to child, exposure to infected blood or blood products, and transplantation of infected organs or tissues. As of December 31, 1993, injection drug use and sexual contact accounted for approximately 92 percent of all adult and adolescent AIDS cases reported to CDC. We review here postulated mechanisms for transmission through activities associated with injection drug use, sexual, and perinatal transmission and detail the associated human behaviors.
Injection Drug Use Transmission
Injection drug use involves practices that facilitate the transmission of HIV infection. The primary category of such practices is direct needle sharing, which involves the reuse of needles and syringes that have been contaminated through prior use by an infected individual. Penetration of the needle through the skin is sufficient for contamination and subsequent transmission of HIV infection, as has been demonstrated in cases of needlestick injuries among health care workers (McCray, 1986). In instances of occupational exposure of health care workers, in which the amount of blood exposure frequently is small (Napoli and McGowan, 1987), the risk of transmission is about 3/1,000 exposures (Ippolito et al., 1994).
Direct Needle Sharing
The higher rates of HIV infection in injection drug users than in health
care workers are due to much more frequent injections (an average of one to two injections per day, according to some published surveys) and the practice of registering. Registering means that once a needle is inserted, the drug user will draw back the plunger of the syringe to examine for the presence of blood to ensure that the needle has been properly placed into a vein. Registering, then, involves contamination of both the needle itself and the hub, barrel, and plunger of the syringe. Although the syringe is typically rinsed before reuse, residual blood may adhere or remain, which may be released into the next person who uses the syringe by subsequent agitation (by drawing up and administrating the drug solution). Studies of the survivability of HIV in dried or aqueous states (Resnick et al., 1986) suggest that transmission may occur even if there is a delay of a day or more before the needle and syringe are reused by a different person.
A related practice of direct needle sharing has been termed booting (Inciardi, 1990; Ouellet et al., 1991), which involves additional steps in the basic injection pattern described above. Booting is the practice performed after registering and administering the drug solution. In this process, with the needle still in the vein, the injector draws back on the plunger of the syringe to fill the barrel with blood and then reinjects the blood, sometimes repeating this practice several times. More commonly reported with cocaine than with heroin injection, this practice allegedly enhances the euphoria associated with the drug's effects. Others, however, describe the motivation for engaging in this practice as economic, that is, to wash out all traces of the drug when administering it. The volume of blood that remains in the barrel of the syringe following booting is greater than that for the practice of registering and, at least theoretically, may be associated with a higher risk of transmission to anyone who subsequently uses a booted syringe. Empirical data on the risk of transmission for the practice of booting are sparse because few injection drug users can report reliably on whether previously used syringes were booted. Nevertheless, in one study, booting was associated with increased HIV seropositivity among injection drug users (Lamothe et al., 1993).
The setting in which drug injection takes place can also be related to direct sharing. A shooting gallery is a clandestine location where injection drug users go to rent needles and syringes. As used syringes are returned to a common container to be rented again, this process amounts to sequential anonymous sharing of needles and syringes (Friedland and Klein, 1987; Ouellet et al., 1991). Results of a study in which researchers tested used syringes collected from shooting galleries in Miami shed some light on the potential risk associated with injection drug use in the context of a shooting gallery. They showed that 20 percent of those syringes that had visible blood residue were positive for HIV, compared with 5.1 percent of those that had no visible blood residue (Chitwood et al., 1990). In a follow-up
study carried out 2 years later (McCoy et al., 1994), researchers reported that 52 percent of the syringes showing visible traces of blood tested positive for HIV.
Indirect Needle Sharing
A separate category of drug injection practices can be termed indirect needle sharing because they do not directly involve passing a contaminated needle and syringe between individuals. Instead, indirect sharing involves common use of other drug preparation or injection equipment that can become contaminated. Examples include cookers, cotton, rinse water, and the drug-sharing practices called frontloading and backloading.
The cooker is a small container, typically a spoon or a metal soda bottle cap, in which a drug in the form of powder is mixed with water and heated into a solution. The heat is applied only to the point of allowing the drug to become soluble; additional heating (which might have a sterilizing effect) is not applied, as this would require time to cool that a drug user in partial withdrawal is often unwilling to tolerate. Although two drug injectors might each possess their own needle and syringe (and therefore deny that they are needle sharing), a potential for cross-contamination of needles and syringes is possible if each dips and draws solution from the same cooker in the same, or possibly later, injection episodes.
Cotton—sometimes cotton balls and other times cigarette filters or other similar materials—is placed into a cooker. Injectors draw up drug solution into their needles and syringes through the cotton, which is used to filter out particulate matter from the cooker. Cotton, which is submerged into the drug solution, typically is not discarded after each use. Instead, it is saved in containers to be soaked later to release residual drugs during periods when their availability is scarce. If contaminated needles are submerged in cotton, there is at least a theoretical possibility of contamination with viable virus that might lead to transmission.
Rinse water refers to containers of water from which one injector will draw up and squirt out tap water between the use of needles and syringes by different individuals. As needles and syringes are dipped into this rinse water, the water becomes contaminated. Contamination increases with greater use, especially over protracted periods between water changes, and also if rinse water that has been drawn into a syringe is squirted back into the same container that is to be reused for additional rinses. Moreover, rinse water is commonly used not only for rinsing, but also for the mixing of the drug solution to be injected. With regard to sharing rinse water, it is the injection of this contaminated water that poses the greatest threat for HIV transmission, especially in the case of cocaine injection, because cocaine is water
soluble and does not always require heating in a cooker to be dissolved (depending on the dilutants and adulterants used).
Frontloading involves the parceling out of individual portions from a mixer/distributor's syringe to the other participants' syringes by removing the needles from the receiving syringes. Backloading involves transferring the drug from one syringe to another by removing the plunger from the receiving syringes. The drug solution can also be divided by having the mixer/distributor squirt all but his or her own portion back into the cooker for each participant to draw up his or her own agreed-on individual portion. These behaviors have been described in some detail in the professional literature (Inciardi and Page, 1991; Koester et al., 1990; Koester, 1994; Turner et al., 1989; Grund et al., 1990, 1991; Jose et al., 1993; McCoy et al., 1994; Samuels et al., 1991; Zule, 1992; Page et al., 1990; Auerbach et al., 1994).
Risk Behaviors and Interventions
Little attention has been given to these risk behaviors in most HIV/AIDS prevention interventions aimed at injection drug users. In an in-depth ethnographic study, Koester and Hoffer (1994) reported that only 7 percent of the injectors they interviewed in their study were aware that these behaviors represented any type of risk of becoming infected. These findings are disturbing, given that over 70 percent of their study participants were participating or had participated in an HIV/AIDS intervention program.
The distinction between direct and indirect needle sharing is not merely academic but reflects a dichotomy that must be considered when evaluating needle exchange and bleach distribution programs. These intervention programs are aimed at direct needle-sharing practices by providing new sterile needles or disinfectant for them. However, neither sterile needles nor their disinfection can be expected to prevent transmission due to sharing of cookers, cotton, rinse water, or frontloading/backloading. Any assessment of the reductions in HIV seroconversion rates for specific programs needs to consider these points. It would seem prudent for prevention programs to educate people about the potential dangers of indirect sharing methods and supply sterile equipment whenever possible.
Finally, it must be noted that infectious agents other than HIV can be transmitted by contaminated injection equipment. Other blood-borne pathogens that have been associated with injection drug use include malaria, syphilis, hepatitis B and C viruses, and human T-lymphotrophic virus type II, as well as other bacterial pathogens that cause sepsis and endocarditis (Cherubin, 1967; Sapira, 1968; Louria et al., 1967; Levine and Sobel, 1991; Stein, 1990; Haverkos and Lange, 1990; Cherubin and Sapira, 1993; Stimmel et al., 1975; Novick et al., 1988; Kreek, 1983; Esteban et al., 1989; Donahue
et al., 1991; Des Jarlais et al., 1992; Selwyn and Alcabes, 1994). The recognition of multiple pathogens that can be transmitted parenterally by injection drug users is important, because development and implementation of prevention programs directed at HIV infection can be viewed more broadly as prevention programs for blood-borne pathogens in general.
Sexual Transmission
Sexual intercourse was implicated as a primary mode of transmission of the virus even before the etiologic agent (HIV) had been identified (Jaffe et al., 1983a, 1983b; Centers for Disease Control, 1981, 1982). However, the sexual transmission of the virus is not highly efficient, and the risk of acquiring the infection as a result of a single sexual exposure is relatively low (Friedland and Klein, 1987; Institute of Medicine, 1988; Holmberg et al., 1989). That does not mean that documented evidence of people becoming infected after one or only a few sexual contacts does not exist (Padian et al., 1988). Sexual transmission depends on the type and frequency of sexual encounters, as well as the prevalence of other risk factors (e.g., condom use). Receptive anal intercourse is particularly dangerous regardless of the sexual orientation of the individuals (Kingsley et al., 1987; Winkelstein et al., 1987), and frequent sexual exposures (vaginal or anal) to an infected partner also increase the likelihood of transmission (Padian et al., 1990; Lazzarin et al., 1991).
With respect to heterosexual transmission, as with other sexually transmitted diseases, women are at higher risk than men (Aral, 1993). Nonetheless, as is also the case with other sexually transmitted diseases, transmission occurs in both directions (male-to-female and female-to-male). The differential efficiency of transmission between the sexes has led to some debate about whether current estimates of female-to-male transmission rates are accurate (Redfield et al., 1985; Haverkos and Edelman, 1985, 1988; Polk, 1985; Handsfield, 1988; Padian et al., 1991; Haverkos and Battjes, 1992; Haverkos and Needle, 1994; Haverkos, 1994).
Transmission rates may also vary depending on the risk group of the originally infected partner. The risk of transmission has been shown to be lower for female partners of hemophiliacs and bisexual men and for partners of transfusion-infected persons than it is for female or male partners of injection drug users (Padian, 1987; Padian et al., 1987; Curran et al., 1988; De Gruttola and Mayer, 1988; Johnson, 1988).
Delineation of the precise biological mechanisms involved in the heterosexual transmission of HIV has been complicated by the difficulty of identifying a potential series of sexual encounters in which exposure to HIV is known to have occurred each time. We know that cell-free virus is infectious for blood product recipients and that cell-associated virus can infect
cell lines in vitro. We simply do not know the relative contributions of cell-free and cell-associated HIV transmission in various at-risk circumstances, including drug injection and sexual contact. Furthermore, viral factors that may influence the efficiency of transmission are so far poorly understood, i.e., certain strains of HIV may be more easily transmitted than other strains. It is not yet known whether specific viral genotypic or phenotypic attributes influence the efficiency of viral transmission.
Transmission is known to be facilitated by a compromise of the integrity of mucosal surfaces and the presence of other sexually transmitted diseases, such as syphilis and chancroid, particularly in the recipient (Johnson and Laga, 1988). By increasing circulating lymphocytes and macrophages that may harbor HIV at the site of local infection, the presence of sexually transmitted diseases may potentially increase infectiousness as well. As a result, the prevalence of sexually transmitted diseases in a population of individuals at risk for HIV infection can significantly alter the efficiency of virus spread.
If a virus-transmitting donor has advanced HIV disease, the recipient may also be more likely to become infected. Furthermore, infection by an advanced-stage donor is associated with a higher incidence of acute viral syndrome in the recipient (Laga et al., 1989). These phenomena may be due to increased viral load in the transmitter or to increased virulence of the transmitted strains of HIV (which may be present after a long period of infection), or both. Infectiousness may also increase over time because plasma-associated and cell-associated viral load increases with disease progression, and studies show that the presence of HIV RNA is more likely to occur in the semen of men with lower CD4+ cell counts.
Perinatal Transmission
Female injection drug users or partners of male injection drug users represent the largest number of HIV-infected women of childbearing age, constituting a sizable threat for perinatal transmission of HIV. The transmission of HIV from an infected mother to her offspring may occur in utero, during the birth process (intrapartum), or at some time following birth (postpartum) by breast-feeding. The relative frequency of the different timings of infection has not been clearly defined and may vary among different populations and locales. Approximately 25 to 30 percent of neonates born to HIV-seropositive mothers become infected (Boylan and Stein, 1991; Vermund et al., 1992; Mofenson, 1992).
For infants born to HIV-seropositive mothers, the transplacental transfer of maternal anti-HIV antibodies complicates the accurate estimate of the number of infants infected in utero versus those infected during or after birth.1 Furthermore, because many HIV-infected pregnant women are unaware
of their infection, the opportunity for the early diagnosis and treatment of their infected infants frequently may be missed. Similarly, interventions to prevent postpartum transmission, such as avoidance of breast-feeding, are not available to women who do not know that they are infected with HIV. Such interventions may also not be recommended in regions of the world where risks of HIV transmission are overshadowed by risks for other adverse health outcomes (e.g., diarrheal disease) among infants who are not breast-fed.
In perinatal transmission, a variety of factors, usually associated with latter-stage disease, including the presence of maternal p24 antigenemia and low maternal CD4+ lymphocyte counts at the time of conception, correlate with the likelihood of infection of a neonate. Additional risk factors in perinatal transmission include high maternal CD8+ T-lymphocyte counts, placental membrane inflammation, and maternal fever. It is likely that many HIV infections in infants are acquired at birth through contact with contaminated blood or secretions. Among twins born to HIV-infected mothers, a higher risk of HIV infection is seen in the firstborn, even for twins delivered by cesarean section, suggesting that factors related to the delivery process affect the risk of infection.
The fact that both the virus donor and the recipient are known in the case of perinatal HIV infection provides potential opportunities for interventions to decrease the risk of viral transmission. Recent studies have shown that antiviral treatment of an HIV-infected mother with zidovudine (AZT) can significantly decrease the likelihood of HIV infection in her offspring (Connor et al., 1994). The availability of an effective intervention to decrease perinatal HIV transmission has increased interest in screening pregnant women for the presence of HIV infection so that perinatal HIV infection may be limited.
Conclusion
In summary, much is known about the various modes of HIV transmission. However, it is not possible to provide accurate estimates of their relative efficiency. It is difficult to identify accurate denominators for the numbers of individuals and encounters in which exposure has occurred; moreover, transmission of the virus depends on factors other than the mode of exposure. The dose of virus transferred (inoculum size), the frequency of exposure, differences in host susceptibility, variations in infectiousness of an infected person over time, and the differences in virulence among HIV isolates, as well as the presence of factors such as particular sexual practices and the presence of sexually transmitted diseases, may all influence the likelihood of transmission.
EPIDEMIOLOGIC DATA
In this section we first review general epidemiologic trends in HIV and AIDS and then review data particular to injection drug users.
HIV and AIDS Surveillance
As of June 1994, AIDS had claimed over 243,000 lives in the United States, and 401,749 cases of AIDS had been reported to CDC. On January 1, 1993, CDC revised its AIDS surveillance case definition for adolescents and adults to include three additional clinical conditions and one laboratory marker of immunosuppression.2 This expansion made for a broader case definition, resulting in a large increase in AIDS cases reported across all subpopulation groups. In 1993, 105,990 new adolescent and adult AIDS cases were reported, representing a 127 percent increase over the 46,791 cases reported in 1992.
There were 5,228 pediatric AIDS cases reported to CDC as of December 31, 1993. In 39 percent of cases, the mother was an injection drug user, and in an additional 17 percent of cases she had sex with an injection drug user. Thus, over half of all pediatric AIDS cases are associated with the HIV epidemic among injection drug users. This is likely to be a lower bound estimate because the risk factors for the mother were unknown for an additional 21 percent of pediatric cases.
In 1992, AIDS had become the eighth leading cause of death in the United States. Among women ages 25 to 44, AIDS was the fourth leading cause of death; for men in this age group, AIDS was the leading cause of death, surpassing unintentional injuries, heart disease, cancer, suicide, and homicide (Centers for Disease Control and Prevention, 1994b). Moreover, in New Jersey and New York, AIDS has been reported to be the leading killer among African American women between the ages of 20 and 40 (Kaplan, 1993). In addition to race, the risk to women also appears to be heavily skewed by social class (Epstein et al., 1993; Hu et al., 1993; Kaplan, 1993; Phillips et al., 1993; Fife and Mode, 1992). As discussed below, the largest recent increases in case reporting were observed for adolescents, women, racial/ethnic minorities, and individuals infected through injection drug use and heterosexual contact.
The dynamic nature of the epidemic is illustrated by the temporal changes in dissemination within the United States. In 1984, two cities—New York and San Francisco—reported half of all AIDS cases in this country; as of December 1993, those two cities accounted for 18 percent of new cases. These two cities have also differed in the distribution of AIDS cases by mode of exposure: in San Francisco the majority of cases are related to men who have sex with men; in New York the majority of cases are related
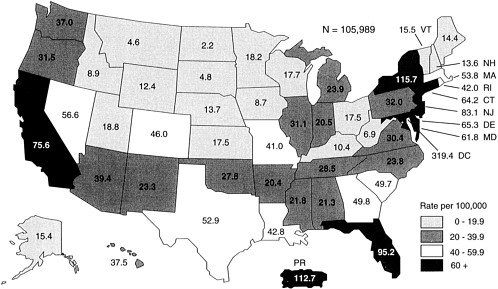
to injection drug use. Figure 1.1 illustrates the variation in AIDS incidence rates across states. Moreover, a closer look at selected metropolitan area AIDS cases reported in 1993 reveals some substantial variations within and across regions (Table 1.1).
In contrast to surveillance data on AIDS, precise estimates of HIV infection rates in the total U.S. population remain problematic. National estimates rely on mathematical models that back calculate HIV incidence from AIDS surveillance data as well as a composite of HIV seroprevalence data from numerous sources: states' reporting and screening of newborns, blood donors, armed forces recruits, Job Corps participants, persons attending alternative testing sites and sexually transmitted disease clinics, admissions to drug abuse treatment centers and prisons, and various other sentinel populations.3 Over the years, the Public Health Service (PHS) has estimated that there are between 600,000 and 1.2 million HIV-infected people in the United States and that approximately 40,000 new infections occur each year among adults and adolescents (U.S. Public Health Service, 1986; Centers for Disease Control, 1987, 1990a; MacQuillan et al., 1993). A discussion of the large observed variations in PHS estimates over the years is presented in Vermund (1991).
Mode of Acquisition of Infection
Important trends in the mode of acquisition of the HIV infection can be discerned. In this country and throughout the world, the majority of HIV infections are sexually transmitted (Roper et al., 1993). In most of the world, over 75 percent of HIV infections are due to heterosexual behavior, approximately 15 percent to homosexual behavior, and a relatively small proportion to injection drug use. However, in the United States, men who have sex with men account for the largest number of reported AIDS cases (54 percent of all reported cases, that is, 193,652 cases as of December 31, 1993). Yet a review of the percentage of annual AIDS cases (Figure 1.2), classified according to CDC's exposure categories, reveals that the proportion of cases of men who have sex with men has decreased steadily over the years (from 74 percent in 1981 to 47 percent in 1993), while the proportion of cases of exposure from injection drug use has steadily increased over the last 13 years (from 12 percent in 1981 to 28 percent in 1993).
In the United States, gay and bisexual men are still the largest risk group for HIV infection and disease. Drug users constitute the next-largest risk group, although there is a large overlap between these groups. Recent CDC estimates of HIV prevalence and incidence (Holmberg, 1993, 1994) indicate that the HIV/AIDS epidemic in the United States is being driven by three subepidemics: (1) injection drug users and their sexual partners and offspring (especially in the northeastern United States; Miami, Florida; and
TABLE 1.1 Newly Reported AIDS Cases by Select Metropolitan Areas, 1993
|
Metropolitan Area of Residence |
Number |
Percent of Total Cases |
Local Annual Rate per 100,000 Population |
|
Central United States |
|
|
|
|
Chicago, Illinois |
2,497 |
2.3 |
32.7 |
|
Cincinnati, Ohio |
273 |
0.3 |
17.3 |
|
Cleveland, Ohio |
454 |
0.4 |
20.4 |
|
Dayton, Ohio |
153 |
0.1 |
15.9 |
|
Denver, Colorado |
1,111 |
1.0 |
62.8 |
|
Detroit, Michigan |
1,272 |
1.2 |
29.5 |
|
Indianapolis, Indiana |
499 |
0.5 |
34.5 |
|
Kansas City, Missouri |
771 |
0.7 |
47.2 |
|
Milwaukee, Wisconsin |
369 |
0.3 |
25.3 |
|
Minneapolis-Saint Paul, Minnesota |
576 |
0.5 |
21.7 |
|
Saint Louis, Missouri |
886 |
0.8 |
35.0 |
|
Salt Lake City, Utah |
237 |
0.2 |
20.5 |
|
SUBTOTAL |
|
8.3 |
|
|
Northeastern United States |
|
|
|
|
Baltimore, Maryland |
1,780 |
1.7 |
72.7 |
|
Boston, Massachusetts |
2,426 |
2.3 |
42.6 |
|
Hartford, Connecticut |
632 |
0.6 |
56.4 |
|
Jersey City, New Jersey |
735 |
0.7 |
132.0 |
|
Nassau-Suffolk, New York |
992 |
0.9 |
37.3 |
|
New Haven, Connecticut |
974 |
0.9 |
59.8 |
|
New York, New York |
14,716 |
13.8 |
171.8 |
|
Newark, New Jersey |
2,109 |
2.0 |
109.3 |
|
Philadelphia, Pennsylvania |
2,656 |
2.5 |
53.6 |
|
Pittsburgh, Pennsylvania |
293 |
0.3 |
12.2 |
|
Providence, Rhode Island |
325 |
0.3 |
35.6 |
|
Washington, District of Columbia |
2,788 |
2.6 |
63.0 |
|
SUBTOTAL |
|
28.6 |
|
San Juan, Puerto Rico); (2) young and minority men who have sex with men; and (3) heterosexual women who use crack. Of these three subepidemics, two are directly linked with drug use, which underscores its catalytic role in the transmission of HIV infection.
Another noteworthy trend depicted in Figure 1.2 is the substantial increase in the proportion of new AIDs cases attributed to heterosexual transmission (from 1 percent in 1984 to 9 percent in 1993). The proportion of reported heterosexually acquired AIDS cases in women increased from 28 to 37 percent between 1987 and 1991, compared with an increase of 1.1 to 2.7 percent among men during the same years (Neal et al., 1993). Between 1991 and 1992, the annual reported AIDS cases among women increased
|
Metropolitan Area of Residence |
Number |
Percent of Total Cases |
Local Annual Rate Per 100,000 Population |
|
Southern United States |
|
|
|
|
Atlanta, Georgia |
1,912 |
1.8 |
59.1 |
|
Dallas, Texas |
1,880 |
1.8 |
65.9 |
|
Fort Lauderdale, Florida |
1,274 |
1.2 |
96.7 |
|
Fort Worth, Texas |
440 |
0.4 |
30.4 |
|
Jacksonville, Florida |
909 |
0.8 |
93.7 |
|
Miami, Florida |
3,514 |
3.3 |
172.9 |
|
New Orleans, Louisiana |
750 |
0.7 |
57.4 |
|
Orlando, Florida |
924 |
0.9 |
69.1 |
|
Phoenix, Arizona |
875 |
0.8 |
36.6 |
|
San Juan, Puerto Rico |
1,960 |
1.8 |
103.4 |
|
Tampa-Saint Petersburg, Florida |
1,437 |
1.3 |
67.9 |
|
West Palm Beach, Florida |
858 |
0.8 |
93.9 |
|
SUBTOTAL |
|
15.6 |
|
|
Western United States |
|
|
|
|
Honolulu, Hawaii |
276 |
0.3 |
31.7 |
|
Houston, Texas |
2,569 |
2.4 |
70.7 |
|
Los Angeles, California |
6,040 |
5.6 |
66.6 |
|
Oakland, California |
1,285 |
1.2 |
59.4 |
|
Orange County, California |
759 |
0.7 |
30.3 |
|
Portland, Oregon |
280 |
0.6 |
41.3 |
|
Riverside-San Bernardino, California |
1,201 |
1.1 |
41.2 |
|
Sacramento, California |
491 |
0.5 |
34.0 |
|
San Diego, California |
1,695 |
1.6 |
64.4 |
|
San Francisco, California |
4,670 |
4.4 |
287.5 |
|
San Jose, California |
555 |
0.5 |
36.2 |
|
Seattle, Washington |
1,116 |
1.0 |
51.7 |
|
SUBTOTAL |
|
19.9 |
|
|
Total AIDS Cases in 1993—106,949 |
|
|
|
|
SOURCE: HIV/AIDS Surveillance Report (Centers for Disease Control and Prevention, 1994b:5-7). |
|||
another 9.1 percent, compared with an observed increase of 2.5 percent among men during the same period (U.S. Public Health Service, 1994). During the latest time period for which annual data are available (1992 to 1993), the number of reported AIDS cases among women increased 167 percent (from 6,295 in 1992 to 16,824 in 1993), compared with a 120 percent increase among men (from 40,496 in 1992 to 89,165 in 1993).4
Whereas heterosexual contact accounted for 4 percent of reported AIDS cases among men in 1993, the figure was 37 percent among women. The majority of new AIDS cases among women occurred among African Americans
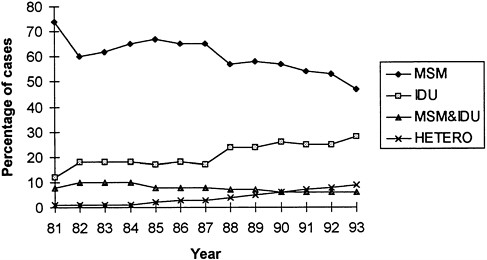
FIGURE 1.2. Annual percentage of new AIDS cases per mode of exposure, 1981 to 1993. NOTE: MSM = men who have sex with men; MSM & IDU = men have sex with men and inject drugs; IDU = injection drug use; HETERO = heterosexual contact. SOURCE: Unpublished data from the Centers for Disease Control and Prevention, National Center for Infectious Diseases, 1994.
(54 percent). Figure 1.3 illustrates that this ethnic/racial disparity also was observed in new pediatric cases (55 percent were African American). A closer examination of cases by exposure category reveals that 71 percent of the newly reported cases among African American women were related to injection drug use; 52 percent of African American women diagnosed with AIDS in 1993 injected drugs, and an additional 19 percent of those cases were attributed to ''sex with injecting drug user" (i.e., heterosexual contact). That same year, for other racial/ethnic categories of women diagnosed with AIDS linked with injection drug use, the corresponding proportions were 61 percent of white women (44 percent injected drugs and 17 percent reported sexual contact with an injection drug user) and 76 percent of Hispanic women (48 percent injected drugs and 28 percent reported sexual contact with an injection drug user). Among both male and female injection drug users, this ethnic disparity is greatest in the northeastern United States.
In sum, these epidemiologic data indicate that injection drug users are currently a major component of the HIV epidemic in the United States and a key bridge to the heterosexual populations. They underscore the critical importance of directing prevention efforts to injection drug users and their sexual partners.

FIGURE 1.3 Proportion of adult men, women, and pediatric AIDS cases by race.
SOURCE: Data from HIV/AIDS Surveillance Report (Centers for Disease Control and Prevention, 1994b).
HIV AND AIDS AMONG INJECTION DRUG USERS
Surveillance
Prevalence and incidence rates of HIV among injection drug users vary considerably by geographic location, so the experiences of different communities also vary. In a 1988 review of 92 studies of intravenous drug users in treatment, Hahn and colleagues (1989) reported HIV seroprevalence rates that range from 0 to 65 percent. Marked geographic differences were noted: HIV rates were highest in the Northeast (ranging from 10 to 65 percent), and lower in the West, the Midwest, and the South—5 percent or lower.
More recent information concerning the prevalence of HIV infection among injection drug users has been consistent with the findings reported by Hahn et al. (1989). In updates (Prevots et al., 1995) of CDC's HIV seroprevalence surveys of injection drug users entering drug treatment centers (most sites were methadone maintenance programs) from 1988 through 1993, seroprevalence rates of 27 percent in the Northeast, 12 percent in the South, 7 percent in the Midwest, and 3 percent in the West were reported for all years combined. Although seroprevalence rates were similar among women and men, observed rates among women were consistently higher than among men in all geographic areas. The South was the only region in
which seroprevalence rates among women were found to be statistically higher than among men (i.e., 18 percent and 10 percent, respectively). Moreover, in all regions, seroprevalence rates among African Americans were higher than among whites; African Americans had a two- to sixfold increased seroprevalence compared with whites (rates ranged from 8 percent among African Americans compared with 3 percent among whites in the Midwest to 38 percent compared with 21 percent, respectively, in the Northeast). Hispanics in the Northeast were found to have prevalence rates similar to those of African Americans in the same region, but they were found to have higher rates than African Americans in the Midwest. These same surveillance data indicate that HIV seroprevalence has stabilized in most U.S. metropolitan areas. Although a moderate decline in HIV seroprevalence among the young (<30) white injection drug users was observed in high-seroprevalence areas (>10 percent), trends in annual seroprevalence were found to be stable among age and racial/ethnic subgroups. Des Jarlais et al. (1994) have also reported such declines in a cross-sectional survey among young injection drug users entering a detoxification unit in a high-seroprevalence area.
Similar patterns of seroprevalence by geographic areas have been reported by researchers at the National Institute on Drug Abuse (Battjes et al., 1991) from data collected as part of a series on nonblind point-prevalence surveys among injection drug users admitted to methadone treatment in seven areas (New York City; Trenton and Asbury Park, New Jersey; Baltimore, Maryland; Chicago, Illinois; San Antonio, Texas; and Los Angeles, California) over a 2-year period (from late 1987 through early 1989). These researchers reported significant variations in seroprevalence across geographical locations. The highest rates were observed in the Northeast: New York City and Asbury Park had rates ranging from 28.6 to 58.6 percent. Los Angeles (West) had low prevalence rates ranging from 0.9 to 3.4 percent over the course of this 2-year study. With the exception of Chicago, the multiple data points across time revealed stable seroprevalence rates within geographic location. In a more recent look (i.e., 1987 through 1991) at the seroprevalence rates in five of those original cities (i.e., New York City, Asbury Park, Trenton, Baltimore, and Chicago), Battjes et al. (1994) reported similar seroprevalence rates by location.
This reported stabilization of seroprevalence rates within geographical areas is comparable to the results of mathematical modeling studies that indicate that HIV incidence among injection drug users has shown a slight to moderate decline since the mid-1980s (Brookmeyer, 1991). Moreover, Drucker and Vermund (1989) have provided a mathematical model that allows the estimation of prevalence rates for population subgroups and overcomes some of the limitations that are associated with large-scale national cross-sectional surveys. National seroprevalence surveys are expensive,
and they can mask significant variations and changes in small local population subgroups. However, the Drucker and Vermund model allows the use of local serosurvey data among various injection drug user subgroups to estimate seroprevalence among key population subgroups in a given geographic area.
Despite the wide variation by geographic location, evidence suggests that, even in areas in which prevalence is low among injection drug users, the risk of HIV infection should not be viewed with complacency. In Milan, Edinburgh, New York City, and Bangkok, once HIV became established in a community of injection drug users (i.e., a prevalence of less than 10 percent), prevalence subsequently rose dramatically within the next 2 to 4 years (Angarano et al., 1985; Robertson et al., 1986; Des Jarlais and Friedman, 1988a; Des Jarlais et al., 1994; Kitayaporn et al., 1994). Although this pattern has not been observed universally (some cities, such as Los Angeles, stabilize prevalence at lower levels), these examples suggest the need for HIV prevention programs not only when prevalence is moderate or high, but also when prevalence is low (especially when injection drug users frequently engage in high-risk behaviors). It is interesting to note, in a study of four cities with sustained low seroprevalence of HIV in injection drug users, all cities had extensive HIV prevention efforts (Des Jarlais, 1994).
Hahn and colleagues' review of injection drug users in treatment (Hahn et al., 1989) reported that the HIV seroincidence data available from some sites revealed rates of 0 to 14 percent per year, again, with the highest incidence reported in the Northeast, especially in New York City. Similar trends were observed among surveys conducted nationwide (again, in a variety of treatment settings) by CDC (Allen et al., 1992). Here, annual seroincidence rates ranged from 0 to 43 percent, the highest rates (ranging from 15 to 44 percent) again reported in the Northeast.
One study provided prevalence and incidence rates for HIV infection among intravenous drug users in and out of treatment in Philadelphia (Metzger et al., 1993). In 1989, prevalence was 10 percent among intravenous drug users in methadone treatment and 16 percent among those out of treatment. Eighteen months later, follow-up rates revealed incidence rates of 3.5 percent for those intravenous drug users in treatment, and 22 percent for those out of treatment. These data, although subject to possible selection bias, suggest that treatment for drug abuse is probably an important intervention for HIV prevention.
Efficiency of transmission among injection drug users varies according to many behavioral risk characteristics, which vary among individuals. They include: frequency of injection, sharing injection equipment, the number of needle-sharing partners, and risky sexual practices (discussed below). However, in most studies that have examined risk factors and seroconversion or prevalent
infection, the sharing of drug injection equipment, including needle sharing and the use of shooting galleries, was the most significant predictor of HIV (Marmor et al., 1987; Vlahov et al., 1990; Solomon et al., 1993; Schoenbaum et al., 1989; Nicolosi et al., 1992). The type of drug administered intravenously is also associated with HIV infection. After controlling for other known risk factors, intravenous drug users who inject cocaine are more likely to be infected than intravenous drug users who inject heroin (Anthony et al., 1991; Chaisson et al., 1989; Novick et al., 1989). This may be partly because cocaine injectors are known to inject more frequently than other injectors in any given drug session.
Certain demographic factors are also associated with infection. As mentioned above, there are dramatic geographic differences in the distribution of AIDS in general, and HIV infection among intravenous drug users in particular (Des Jarlais et al., 1991; Lange et al., 1988). In general, rates are also higher among minority intravenous drug users (Friedman et al., 1987; Schoenbaum et al., 1989), women (Nelson et al., 1991, in press), and younger users (Nicolosi et al., 1992; Solomon et al., 1993; Nelson et al., 1993). These factors highlight the importance of directing prevention activities to these groups. In addition to minority women, such at-risk individuals include young, recent initiates into drug use, many of whom may be excluded from programs in which evidence of chronic use is a criterion for participation.
Sexual Transmission Among Injection Drug Users
As mentioned above, gay and bisexual intravenous drug users are not rare, and bisexual intravenous drug users may act as a conduit for transmission from both the homosexual and the intravenous drug user communities to heterosexuals, particularly women. In a survey of intravenous drug users recruited in San Francisco from street outreach and drug treatment programs (Lewis and Watters, 1991), 12 percent (49/396) of intravenous drug-using men were bisexual, based on reports of female partners prior to entry into the study. However, fewer than half of these men identified themselves as being bisexual, highlighting the difficulties that female partners have in assessing their male sexual partner's risk history. This may be particularly important because, in at least one study (Mandell et al., 1994), bisexual men (along with homosexual men) were more likely to report needle sharing than their heterosexual counterparts. Bisexual men may also have been important by acting as a conduit for HIV infection between homosexual men and the injection drug user community, at least in some areas. For example, in Chicago (Lampinen, 1992), the first reported AIDS case from injection drug use occurred in a bisexual man, and large numbers of
cases involving users who were also gay and bisexual men continued for several years.
As discussed above, sexual transmission from intravenous drug users to their sexual partners may pose a greater risk for women than for men. The likelihood that an injection drug user has an injection drug-using partner is generally quite high, particularly among women (Mandell et al., 1994; Ross et al., 1992; Dwyer et al., 1994). As estimated, 75 to 90 percent of female injection drug users have a male injection drug-using partner compared with 20 to 50 percent of male users who have female drug-using partners (Cohen et al., 1989; Mondanaro, 1990; Donoghoe, 1992). In one survey in New York City (Fordyce et al., 1991), 2 percent of all currently sexually active women in 1990 reported that they knew they had a sexual partner who injected drugs. In another survey of risk factors for HIV infection among female injection drug users in methadone treatment (Schoenbaum et al., 1989), the number of male sexual partners who used drugs was strongly associated with HIV infection and was the only risk factor associated with acquisition of HIV for those women who had not used drugs since 1982.
Female sexual partners of male injection drug users may use sex as a way to obtain drugs (Donoghoe, 1992). They may also share needles with partners, thus exposing themselves to two sources of risk. Such women may be at even greater risk for sexual transmission of HIV than female partners of male injection drug users who do not themselves inject drugs—who may, in fact, be less likely to use condoms with male injection drug-using partners than with their partners who do not inject (Klee et al., 1990; Cohen, 1991; Worth, 1989).
Trading sex for drugs or money increases infection rates between injection drug users and the heterosexual community. Approximately 25 percent of female injection drug users engage in prostitution (Cohen et al., 1989; Donoghoe, 1992; Saxon et al., 1991). According to one survey in Baltimore (Astemborski et al., 1994), women who traded sex for drugs with more than 50 men over the 10 years prior to entry into the study were more likely to be infected with HIV than other female injection drug users. This finding remained significant after controlling for a range of risk factors for HIV.
In addition, women who use crack (whether or not they use injection drugs) may also trade sex for drugs and may also serve to bridge the gap between injection drug use and the heterosexual risk of HIV transmission (Des Jarlais and Friedman, 1988b; Edlin et al., 1994). Through acquisition of large numbers of partners, many of whom are also injection drug users, women who engage in this practice also expose themselves to HIV. This problem may be confounded by the profound disinhibition associated with cocaine use, resulting in little concern for safe sex or safe needle use (Donoghoe, 1992; Hartel et al., 1992). This may be due in part to the direct effects of
crack as a sexual stimulant (Grinspoon and Bakalar, 1985; Weiss and Mirin, 1987). However, the relative magnitude of the pharmacologic causal effect of crack (or cocaine) on increased sexual activity is still not well understood. Although there may be increased sexual activity associated with early stages of use, as use of the drug increases, sexual dysfunction follows. Even then, there may be heightened sexual activity—sex for crack exchanges—but at this more advanced stage of drug abuse, the increase in sexual activity appears to be driven by the compulsion to use the drug and tends to be devoid of pleasurable sensation. Hence, if infected by their injection drug-using partners, these noninjection drug-using sexual partners also constitute a conduit into the heterosexual community. Crack may also amplify the spread of HIV because of its strong association with syphilis. Trading sex for crack has resulted in a large increase in syphilis (Centers for Disease Control and Prevention, 1992; Greenberg et al., 1992), which may in turn facilitate HIV transmission by increasing either infectiousness or susceptibility.
Some of the increased rates of transmission from injection drug users to their sexual partners, compared with transmission rates from infected people from other risk groups to their sexual partners, may also be attributed to high-risk sexual practices. In one survey of injection drug users who were not in treatment but who were recruited and interviewed on the street in San Francisco (Lewis and Watters, 1991), 67 percent of the sample reported never using condoms, 15 percent had more than 10 partners, and approximately 35 percent engaged in prostitution or practiced anal sex (or both). In a similar nationwide survey, 70 percent of injection drug users reported never using condoms, and more than 25 percent practiced anal sex (Centers for Disease Control and Prevention, 1990b). In a survey of injection drug users in treatment taken in the Northeast, Texas, and California, only 14 percent reported using condoms (Battjes and Pickens, 1988). In another similar study in New York City, only 5 percent reported condom use at all (Primm et al., 1988); among those who did use condoms, fewer than half used them for all sexual encounters. In the San Francisco survey described above (Lewis and Watters, 1991), more than a third of both bisexual and heterosexual male injection drug users reported that they never used condoms.
In a variety of studies that attempted risk reduction programs among injection drug users, success was greater in influencing participants to change risky injection behavior than sexual behavior (Des Jarlais and Friedman, 1988b). Again, for women this may be particularly difficult because the change to safe sex practices requires the cooperation of the male partner, which may not always be a feasible proposition (Worth, 1988). An additional concern related to power dynamics in sexual partnerships is the disclosure of HIV status. In particular, women may fear disclosing their HIV
infection to male partners, thus increasing the likelihood of unsafe sexual practices (North and Rothenberg, 1993).
Part of the increase in transmission rates from injection drug users may be attributed to misclassification of modes of transmission. What is called sexual transmission may actually be transmission associated with injection drug use in the partner. Many noninjection drug-using partners of injection drug users report past injection drug use and recent use of noninjection drugs such as cocaine or crack (Centers for Disease Control and Prevention, 1991), and many of these partners also report having traded sex for drugs or money. Furthermore, as mentioned above, because female injection drug users are more likely to have a male injection drug-using partner, misclassification of female-to-male transmission is probably more severe than that for male-to-female transmission. Of course, what is labeled as transmission attributed to injection drug use may in fact be due to heterosexual contact; it is nearly impossible to separate these effects. The confluence of high-risk sexual practices with injection drug-using behavior may make it more difficult to intervene because of sources of uncertainty in the mechanisms of transmission. Nevertheless, simply acknowledging high transmission rates in areas characterized by injection drug use may be sufficient to justify proper allocation of health care resources and targeting of prevention messages.
Finally, it is possible that increased rates of transmission may also result from the fact that injection drug users may be more infectious than individuals from other risk groups or, conversely, their partners may be more susceptible. In one heterosexual partner study (Padian et al., 1994), rates of male-to-female transmission were higher from injection drug users to their partners compared with transmission from men in other risk groups, after controlling for all known risk factors in a multivariate model. An improved understanding of the postulated biological mechanisms for heterosexual transmission might shed light on this issue.
Perinatal Transmission from Injection Drug Users
Several studies have demonstrated an association between HIV infection in newborns and drug use in their mothers. Such studies have examined risk factors either using the individual as the unit of analysis (Hand et al., 1992) or in ecologic studies that correlate HIV incidence in neonates with drug use, as determined by either hospital discharge data (Morse et al., 1991) or drug-use rates by zip code (Novick et al., 1989).
Female injection drug users (regardless of their serostatus) may be more likely to become pregnant than their counterparts who do not inject drugs. Researchers (Caskey and Wathey, 1982) found that, in New York City, birth rates for addicted women were higher than those for nonaddicted women.
Female injection drug users may also be poorer users of contraception, as demonstrated in one study (Ralph and Spigner, 1986), in which female injection drug users were less likely to use condoms than a comparable group of women matched on age, ethnicity, and marital status.
In one study that was able to extricate the effects of injection drug use from HIV infection in association with pregnancy among a group of female injection drug users (all of whom were recruited at a methadone treatment clinic), 24 percent of the 70 who were seropositive and 22 percent of the 115 who were seronegative became pregnant during the course of follow-up (Selwyn et al., 1989). Similar numbers of infected and uninfected women chose to terminate their pregnancy. When comparing those who did elect to terminate with those who did not (among HIV-positive women), the reasons for termination were not unlike those reported for uninfected women, including lack of a planned pregnancy, negative feelings toward the pregnancy, and having a difficult time deciding whether to continue the pregnancy (Selwyn et al., 1989).
SUMMARY
In summary, an injection drug user infected with HIV can cause a cascade of new infections in many other individuals through needle sharing, sexual transmission, and perinatal transmission. In fact, HIV infection among injection drug users is driving the epidemic among women and among children (Des Jarlais et al., 1989; Des Jarlais and Friedman, 1988a; Fordyce et al., 1991; Turner et al., 1989). Obviously, then, any reduction in infection among injection drug users would also result in a reduction of infection among their sexual partners and future offspring. Each of these newly infected individuals can in turn cause a cascade of additional infections, again, through needle sharing, sexual transmission, and perinatal transmission. Each female of childbearing age who becomes infected is at risk of infecting a newborn. Thus, prevention of infections among injection drug users affects the growth rates of the epidemic not only among themselves, but also among adults and children in the community of noninjection drug users.
As this chapter notes, the sharing of contaminated needles is responsible for a substantial proportion of HIV infection among injection drug users. Provision of sterile needles and adequate disinfection of used needles would seem to have some merit as strategies to reduce the risk of HIV transmission in this population. However, other drug injection practices involving indirect sharing and sexual practices that are capable of transmitting HIV infection cannot be affected by the provision of sterile needles, syringes, and disinfectants.
As a result, evaluation of needle exchange and bleach distribution programs
that use HIV seroconversion as an outcome probably cannot be expected to find absolute or complete reductions in HIV seroincidence. Programs that are more comprehensive in orientation and that include components on the prevention of sexual transmission would seem to have greater impact in terms of HIV prevention. However, it must be kept in mind that injection drug users are at risk for a wide variety of blood-borne pathogens, including the hepatitis viruses. Strategies to prevent transmission of the HIV infection by injecting drugs in this population might have broader public health impact in terms of prevention of other blood-borne pathogens as well. In evaluating HIV prevention programs, it is important to consider whenever possible their impact on other infectious diseases.
Finally, in order to assess the needs of a community, better methods of monitoring epidemic spread and the potential for such spread must be developed. Consequently, the panel supports the creation of more active epidemiologic surveillance of HIV prevalence and incidence so that the current progress of the epidemic can be accurately monitored. We also strongly encourage development of surveillance for behavioral data on known risk behaviors (i.e., sexual behavior and drug use), as well as surrogate markers for HIV risk, such as incident sexually transmitted diseases. This is needed so that intervention programs can be appropriately selected and evaluated.
The panel's review of the available epidemiologic data lead to the following specific conclusions and recommendations.
Conclusions
-
The spread of HIV among injection drug users, their sexual partners, and offspring accounts for a major proportion of new HIV infections in the United States, and the resultant propagation of the AIDS epidemic.
-
Throughout the United States, the epidemiology of HIV and AIDS differs, depending on geography, inherent differences in the population at risk, and the distribution of risk behaviors associated with transmission.
-
Injection drug use with contaminated injecting equipment contributes significantly to the spread of HIV infection and thereby to the AIDS epidemic.
Recommendations
The panel recommends that:
-
The Assistant Secretary for Health should charge appropriate agencies to develop improved ways of monitoring and reporting the prevalence
-
of HIV in population subgroups of injection drug users (e.g., youth, women) in the United States.
-
Given the serious public health threat associated with HIV infection among injection drug users, their sexual partners and offspring, the Assistant Secretary for Health should ensure that AIDS prevention efforts targeted to injection drug users are expanded specifically to include behavioral interventions in order to limit the further spread of HIV infection.
-
AIDS behavioral prevention efforts need to target direct and indirect needle sharing and the sexual practices of injection drug users and their sex partners.
NOTES
REFERENCES
Allen, D.M., I.M. Onorato, and T.A. Green 1992 HIV infection in intravenous drug users entering drug treatment, United States, 1988 to 1989. American Journal of Public Health 82(4):541-545.
Angarano, G., G. Pastore, L. Monno, T. Santantonio, N. Luchena, and O. Schiraldi 1985 Rapid spread of HTLV-III infection among drug addicts in Italy. Lancet 2(8467):1302.
Anthony, J.C., D. Vlahov, K.E. Nelson, S. Cohn, J. Astemborski, and L. Solomon 1991 New evidence on intravenous cocaine use and the risk of infection with human immunodeficiency virus type 1. American Journal of Epidemiology 134(10):1175-1189.
Aral, S.O. 1993 Heterosexual transmission of HIV: The role of other sexually transmitted infections and behavior in its epidemiology, prevention and control. Annual Review of Public Health 14:451-467.
Astemborski, J., D. Vlahov, D. Warren, L. Solomon, and K.E. Nelson 1994 The trading of sex for drugs or money and HIV seropositivity among female intravenous drug users. American Journal of Public Health 84(3):382-387.
Auerbach, J.D., C. Wypijewska, and H.K.H. Brodie, eds. 1994 AIDS and Behavior: An Integrated Approach. Washington, DC: National Academy Press.
Battjes, R.J., and R. Pickens 1988 AIDS Transmission Risk Behaviors Among Intravenous Drug Abusers (IVDAs). Presented at the Fourth International AIDS Conference, Stockholm, June 12-16.
Battjes, R.J., R.W. Pickens, and Z. Amsel 1991 HIV infection and AIDS risk behaviors among intravenous drug users entering methadone treatment in selected U.S. cities. Journal of Acquired Immune Deficiency Syndromes 4:1148-1154.
Battjes, R.J., R.W. Pickens, H.W. Haverkos, and Z. Sloboda 1994 HIV risk factors among injecting drug users in five U.S. cities. AIDS 8:681-687.
Boylan, L., and Z.A. Stein 1991 The epidemiology of HIV infection in children and their mothers—Vertical transmission. Epidemiology Reviews 13:143-177.
Brookmeyer, R. 1991 Reconstruction and future trends of the AIDS epidemic in the United States. Science 253:37-42.
Caskey, W.R., and R.B. Wathey 1982 Female Addiction: A Longitudinal Study. Lexington, MA: Lexington Books.
Centers for Disease Control 1981 Kaposi's sarcoma and Pneumocystis pneumonia among homosexual men—New York City and California. Morbidity and Mortality Weekly Report 30:305-308.
1982 Persistent, generalized lymphadenopathy among homosexual males. Morbidity and Mortality Weekly Report 31:249-252.
1987 Human immunodeficiency virus infection in the United States: A review of current knowledge. Morbidity and Mortality Weekly Report 36(suppl. S-6):1-48.
1990a HIV prevalence estimates and AIDS case projections for the United States: Report based upon a workshop. Morbidity and Mortality Weekly Report 39(RR-16):1-31.
1990b Behaviors for HIV transmission among intravenous-drug users not in drug treatment—United States, 1987-1989. Morbidity and Mortality Weekly Report 39(16):273-276.
1991 Drug use and sexual behaviors among sex partners of injecting-drug users—United States, 1988-1990. Morbidity and Mortality Weekly Report 40(49):855-860.
1992 Update: Acquired immunodeficiency syndrome—United States, 1992. Morbidity and Mortality Weekly Report 42:547-551, 557.
1994a CDC HIV/AIDS Prevention 5(2).
1994b HIV/AIDS Surveillance Report 5(4).
Chaisson, R.E., P. Bacchetti, D. Osmond, B. Brodie, M.A. Sande, and A.R. Moss 1989 Cocaine use and HIV infection in intravenous drug users in San Francisco. Journal of the American Medical Association 261(4):561-565.
Cherubin, C. 1967 The medical sequelae of narcotic addiction. Archives of Internal Medicine 67:23-33.
Cherubin, C.E., and J.D. Sapira 1993 The medical complications of drug addiction and the medical assessment of the IV drug users: Twenty-five years later. Archives of Internal Medicine 119:1017-1028.
Chitwood, D.D., C.B. McCoy, J.A. Inciardi, D.C. McBride, M. Comerford, E. Trapido, H.V. McCoy, J.B. Page, J. Griffin, M.A. Fletcher, et al. 1990 HIV seropositivity of needles from shooting galleries in South Florida. American Journal of Public Health 80:150-152.
Cohen, J.B. 1991 Why women partners of drug users will continue to be at high risk for HIV infection. Journal of Addiction Diseases 10:99-110.
Cohen, J., L. Hauer, and C. Wofsy 1989 Women and intravenous drugs: Parenteral and heterosexual transmission of HIV. Journal of Drug Issues 19:39-56.
Connor, E.M., R.S. Sperling, R. Gelber, P. Kiselev, G. Scott, J.J. O'Sullivan, R. Van Dyke, M. Bey, W. Shearer, R.L. Jacobson, E. Jimenez, E. O'Neill, B. Bazin, J.-F. Delfraissy, M. Culnane, R. Coombs, M. Elkins, J. Moye, P. Stratton, and J. Balsley 1994 Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. New England Journal of Medicine 331(18):1173-1180.
Curran, J.W., H.W. Jaffe, A.M. Hardy, W.M. Morgan, R. M. Selik, and T.J. Dondero 1988 Epidemiology of HIV infection and AIDS in the United States. Science 239:610-616.
De Gruttola, V., and K.H. Mayer 1988 Assessing and modeling heterosexual spread of the human immunodeficiency virus in the United States. Review of Infectious Diseases 10:138-150.
Des Jarlais, D.C. 1994 Epidemiology of HIV Among Intravenous Drug Users. Presentation at the meeting of the Panel on Needle Exchange and Bleach Distribution Programs, January 7.
Des Jarlais, D.C., and S.R. Friedman 1988a HIV infection among persons who inject illicit drugs: Problems and prospects. Journal of Acquired Immune Deficiency Syndromes 1:267-273.
1988b HIV and intravenous drug use. AIDS 2(1):S65-S69.
Des Jarlais, D.C., S.R. Friedman, D.M. Novick, J.L. Sotheran, P. Thomas, S.R. Yancovitz, D. Mildvan, J. Weber, M.J. Kreek, and R. Maslansky 1989 HIV-1 infection among intravenous drug users in Manhattan, New York City, from 1977 through 1987. Journal of the American Medical Association 261(7):1008-1012.
Des Jarlais, D.C., S.R. Friedman, K. Choopanya, S. Vanichseni, and T.P. Ward 1992 International epidemiology of HIV and AIDS among injecting drug users. AIDS 6:1053-1068.
Des Jarlais, D.C., S.R. Friedman, J.L. Sotheran, J. Wenston, M. Marmor, S.R. Yancovitz, B. Frank, S. Beatrice, and D. Mildvan 1994 Continuity and change within an HIV epidemic. Injecting drug users in New York City, 1984 through 1992. Journal of the American Medical Association 271(2):121-127.
Donahue, J.G., K.E. Nelson, A. Muñoz, D. Vlahov, L.L. Rennie, E.L. Taylor , A.J. Saah, S. Cohn, N.J. Odaka, and H. Farzadegan 1991 Antibody to hepatitis C virus among cardiac surgery patients, homosexual men, and intravenous drug users in Baltimore, Maryland. American Journal of Epidemiology 134(10):1206-1211.
Donoghoe, M.C. 1992 Sex, HIV and the injecting drug user. British Journal of Addiction 87:405-416.
Drucker, E., and S.H. Vermund 1989 Estimating population prevalence of human immunodeficiency virus infection in urban areas with high rates of intravenous drug use: A model of the Bronx in 1988. American Journal of Epidemiology 130(1):133-142.
Dwyer, R., D. Richardson, M.W. Ross, A. Wodak, M.E. Miller, and J. Gold 1994 A comparison of HIV risk between women and men who inject drugs. AIDS Education and Prevention 6(5):379-389.
Edlin, B.R., K.L. Irwin, S. Faruque, et al. 1994 Intersecting epidemics: Crack cocaine use and HIV infection among inner-city young adults. Multicenter Crack Cocaine and HIV Infection Study Team. New England Journal of Medicine 331(21):1422-1427.
Epstein, M.R., G.A. Conway, C.R. Hayman, et al. 1993 Youth, Poverty and HIV: Trends in HIV Prevalence in a National Job Training Program, 1988-1992 . Paper presented at the 121st meeting of the American Public Health Association, San Francisco, CA.
Esteban, J.I., R. Esteban, Viladomiu, J.C. Talavera-Lupez, A. Gonzalez, J.M. Hernandez, M. Roget, V. Vargas, J. Genesca, M. Buti, et al. 1989 Hepatitis C antibodies among risk groups in Spain. Lancet 2(8658):294-297.
Fife, D., and C. Mode 1992 AIDS prevalence by income group in Philadelphia. Journal of Acquired Immune Deficiency Syndromes 6:1111-2225.
Fordyce, E.J., S. Blum, A. Balanon, and R.L. Stoneburner 1991 A method for estimating HIV transmission rates among female sex partners of male intravenous drug users. American Journal of Epidemiology 133(6):590-598.
Friedland, G.H., and R.S. Klein 1987 Transmission of the human immunodeficiency virus. New England Journal of Medicine 317(18):1125-1135.
Friedman, S.R., J.L. Sotheran, A. Abdul-Quader, B.J. Primm, D.C. Des Jarlais, P. Kleinman, C. Mauge, D.S. Goldsmith, W. el-Sadr, and R. Maslansky 1987 The AIDS epidemic among blacks and Hispanics. Millbank Quarterly 65(Suppl 2):455-499.
Greenberg, J., D. Schnell, and R. Colon 1992 Behavior of crack cocaine users and their impact on early syphilis intervention. Sexually Transmitted Diseases 19:346-350.
Grinspoon, L., and J. Bakalar 1985 Cocaine: A Drug and Its Social Evolution. New York, NY: Basic Books.
Grund, J.P., C.D. Kaplan, N.F. Adiraans, P. Blanken, and J. Huisman 1990 The limitations of the concept of needle sharing: The practice of frontloading. AIDS 4(8):819-821.
Grund, J.P. C.D. Kaplan, and N.F.P. Adriaans 1991 Needle sharing in the Netherlands: An ethnographic analysis. American Journal of Public Health 81(12):1602-1607.
Hahn, R.A., I.M. Onorato, S. Jones, and J. Dougherty 1989 Prevalence of HIV infection among intravenous drug users in the United States. Journal of the American Medical Association 261(18):2677-2684.
Hand, I..L, A. Wiznia, R.T. Checola, M.H. Kim, L.M. Noble, T.J. Daley, and J.J. Yoon 1992 Human immunodeficiency virus seropositivity in critically ill neonates in the South Bronx. Pediatric Infectious Disease Journal 11(1):39-42.
Handsfield, H.H. 1988 Heterosexual transmission of human immunodeficiency virus. Journal of the American Medical Association 260(13):1943-1944.
Hartel, D., E. Schoenbaum, P. Selwyn, I. Fleming, A. Gapuchin, and G. Friedland 1992 Gender Differences in Drug Use and AIDS Mortality Among Intravenous Drug Users. Eighth International Conference on AIDS, Amsterdam.
Haverkos, H. 1994 Reporting AIDS in New York City. Journal of the American Medical Association 271(4):273-274.
Haverkos, H, and R. Battjes 1992 Female-to-male transmission of HIV. Journal of the American Medical Association 268:1855.
Haverkos, H.W., and R. Edelman 1985 Female-to-male transmission of AIDS. Journal of the American Medical Association 254(8):1035-1036.
1988 The epidemiology of acquired immunodeficiency syndrome among heterosexuals. Journal of the American Medical Association 260(13):1922-1929.
Haverkos, H.W., and W.R. Lange 1990 Serious infections other than human immunodeficiency virus among intravenous drug users. Journal of Infectious Diseases 161:894-902.
Haverkos, H., and R. Needle 1994 Reporting AIDS in New York City. Journal of the American Medical Association 271(4):273-274.
Holmberg, S.D. 1993 Emerging epidemiological patterns in the USA. Presented at the Sixth Annual Meeting of the National Cooperative Vaccine Development Group for AIDS, Alexandria, Va., October 30-November 4.
1994 Panel on Injection Drug Users and the HIV Epidemic: Understanding the Regional Differences in Prevalence, Incidence, and Risk Factors for Transmission. Public Health and Diversity: Opportunities for Equity, American Public Health Association's 122nd Annual Meeting and Exhibition, Washington, D.C., November 2.
Holmberg, S.D., C.R. Horsburgh, Jr., J.W. Ward, and H.W. Jaffe 1989 Biologic factors in the sexual transmission of human immunodeficiency virus. Journal of Infectious Diseases 1601(1):116-125.
Hu, D.J., R. Frey, S. Costa, et al. 1993 AIDS Rates and Sociodemographic Variables in the Newark, New Jersey, Metropolitan Area . Paper presented at the Ninth International Conference on AIDS, Berlin, Germany.
Inciardi, J. 1990 AIDS—A strange disease of uncertain origins. American Behavioral Scientist 33:397-407.
Inciardi, J., and J. Page 1991 Drug sharing among intravenous drug users. AIDS 5(6):772-773.
Institute of Medicine 1988 Confronting AIDS: Update 1988. Washington, DC: National Academy Press.
Ippolito, G., G. DeCarli, V. Puro, N. Petrosillo, C. Arici, B. Bertucci, L. Bianciardi, L. Bonazzi, A. Cestrone, M. Daglio, et al. 1994 Device-specific risk of needlestick injury in health care workers. Journal of the American Medical Association 272(8):607-610.
Jaffe, H.W., D.J. Bregman, and R.M. Selik 1983a Acquired immune deficiency syndrome in the United States: The first 1,000 cases. Journal of Infectious Disease 48:339-345.
Jaffe, H.W., K. Choi, P.A. Thomas, H.W. Haverkos, D.M. Auerbach, M.E. Guinan, M.F.
Rogers, T.J. Spira, W.W. Darrow, M.A. Kramer, S.M. Friedman, J.M. Monroe, A.E. Friedman-Kien, L.J. Laubenstein, M. Marmor, B. Safai, S.K. Dritz, S.J. Crispi, S.L. Fannin, J.P. Orkwis, A. Kelter, W.R. Rushing, S.B. Thacker, and J.W. Curran 1983b National case-control study of Kaposi's sarcoma and Pneumocystis carinii pneumonia in homosexual men: Part I. Epidemiologic results. Annals of Internal Medicine 99:145-151.
Jaffe, H.W., W.W. Darrow, D.F. Echenberg, P.M. O'Malley, J.P. Getchell, V.S. Kalyanaraman, R.H. Byers, D.P. Drennan, E.H. Braff, J.W. Curran, and D.P. Francis 1985 The acquired immunodeficiency syndrome in a cohort of homosexual men. A six-year follow-up study. Annals of Internal Medicine 103:210-214.
Johnson, A.M. 1988 Heterosexual transmission of human immunodeficiency virus. British Medical Journal 296:1017-1020.
Johnson, A.M., and M. Laga 1988 Heterosexual transmission of HIV. AIDS Suppl 1:S49-S56.
Jose, B., S.R. Friedman, A. Neaigus, R. Curtis, J.P. Grund, M.F. Goldstein, T.P. Ward, and D.C. Des Jarlais 1993 Syringe-mediated drug-sharing (backloading): A new risk factor for HIV among injecting drug users. AIDS 7(12):1653-1660.
Kaplan, M.S. 1993 Women and AIDS: Toward a Feminist Conception of Social Prevention. Paper presented at the 121st annual meeting of the American Public Health Association, San Francisco, CA.
Kingsley, L.A., R. Detels, R. Kaslow, B.F. Polk, C.R. Rinaldo, Jr., J. Chmiel, K. Detre, S.F. Kelsey, N. Odaka, D. Ostrow, et al. 1987 Risk factors for seroconversion to human immunodeficiency virus among male homosexuals: Results from the Multicenter AIDS Cohort Study. Lancet 1(8529):345-349.
Kitayaporn, D., C. Uneklabh, B.G. Weninger, et al. 1994 Incidence determined retrospectively among drug users in Bangkok, Thailand. AIDS 1994:1443-1450.
Klee, H., J. Faugier, C. Hayes, T. Boulton, and J. Morris 1990 Factors associated with risk behavior among injecting drug users. AIDS 2:133-145.
Koester, S.K. 1994 Copping, running and paraphernalia laws: Contextual variables and needle risk behavior among injection drug users in Denver. Human Organization 53(3).
Koester, S.K., and L. Hoffer 1994 Indirect sharing: Additional HIV risks associated with drug injection. AIDS and Public Policy Journal Summer:100-105.
Koester, S.K., R. Booth, and W. Wiebel 1990 The risk of transmission from sharing water, drug mixing containers, and cotton filters among intravenous drug users. International Journal on Drug Policy 1(6):28-30.
Kreek, M.J. 1983 Health consequences associated with the use of methadone. Pp. 456-482 in Research on the Treatment of Narcotic Addiction, J.R. Cooper, F. Altman, B.S. Brown, and D. Czechowicz, eds. Rockville, MD: National Institute on Drug Abuse.
Laga, M., H. Taelman, P. Van der Stuyft, et al. 1989 Advanced immunodeficiency as a risk factor for heterosexual transmission of HIV. AIDS 3:361-366.
Lamothe, F., J. Bruneau, R. Coates, J.G. Rankin, J. Soto, R. Arshinoff, M. Brabant, J. Vincelette, and M. Fauvel 1993 Seroprevalence of and risk factors for HIV-1 infection in injection drug users in Montréal and Toronto: A collaborative study. Canadian Medical Association Journal 149(7):945-951.
Lampinen, T.M. 1992 Prevalence of Human Immunodeficiency Virus Type I Among Chicago Injecting Drug Users. Thesis submitted in partial fulfillment of the requirements of the Master of Science in Public Health Sciences in the Graduate College of the University of Illinois at Chicago School of Public Health, Chicago.
Lange, W.R., F.R. Snyder, D. Lozovsky, V. Kaistha, M.A. Kaczaniuk, and J.H. Jaffe 1988 Geographic distribution of human immunodeficiency virus markers in parenteral drug abusers. American Journal of Public Health 7(4):443-446.
Lazzarin, A., A. Saracco, M. Musicco, and A. Nicolosi 1991 Man-to-woman transmission of the human immunodeficiency virus. Risk factors related to sexual behavior, man's infectiousness, and woman's susceptibility. Italian Study Group on HIV Heterosexual Transmission (published erratum appears in Archives of Internal Medicine April 1992, 152[4]:876). Archives of Internal Medicine 151(12):2411-2416.
Levine, D.P., and J.D. Sobel, eds. 1991 Infections in Intravenous Drug Abusers. New York, NY: Oxford University Press.
Lewis, D.K., and J.K. Watters 1991 Sexual risk behavior among heterosexual intravenous drug users: Ethnic and gender variations. AIDS 5:77-83.
Louria, D.B., T. Hensle, and J. Rose 1967 The major medical complications of narcotic addition. Annals of Internal Medicine 67:1-32.
MacQuillan, G.M., M. Khare, T.M. Ezzati, et al. 1993 The seroepidemiology of human immunodeficiency virus in the United States household population: NHANES III, 1988-1991 [abstract 21]. P. 59 in Program and Abstracts: The First National Conference on Human Retroviruses and Related Infections. Washington, DC: National Foundation for Infectious Diseases, American Society for Microbiology.
Mandell, W., D. Vlahov, C. Latkin, M. Oziemkowska, and S. Cohn 1994 Correlates of needle sharing among injection drug users. American Journal of Public Health 84(6): 920-923.
Marmor, M., D.C. Des Jarlais, H. Cohen, S.R. Friedman, S.T. Beatrice, N. Dubin, W. El-Sadr, D. Mildvan, S. Yancovitz, U. Mathur, and R. Holzman 1987 Risk factors for infection with human immunodeficiency virus among drug abusers in New York City. AIDS 1:39-44.
McCoy, C.B., P. Shapshak, S.M. Shah, H.V. McCoy, J.E. Rivers, J.B. Page, D.D. Chitwood, N.L. Weatherby, J.A. Inciardi, D.C. McBride, D.C. Mash, and J.K. Watters 1994 HIV-1 Prevention: Interdisciplinary studies and reviews on efficacy of bleach and compliance to bleach prevention protocols. Pp. 255-283 in Proceedings, Workshop on Needle Exchange and Bleach Distribution Programs. Washington, DC: National Academy Press.
McCray, E. 1986 Occupational risk of the acquired immunodeficiency syndrome among health care workers. New England Journal of Medicine 314(17):1127-1132.
Metzger, D.S., G.E. Woody, A.T. McLellan, C.P. O'Brien, P. Druley, H. Navaline, D. DePhilippis, P. Stolley, and E. Abrutyn 1993 Human immunodeficiency virus seroconversion among intravenous drug users in-and out-of-treatment: An 18-month prospective follow-up. Journal of Acquired Immune Deficiency Syndromes 6:1049-1056.
Mofenson, L.M. 1992 Preventing mother to infant HIV transmission: What we know so far. The AIDS Reader March/April:42-51.
Mondanaro, J. 1990 Treatment of Women with Chemical Dependency Problems. Lexington, MA: Lexington Press.
Morse, D.L., L. Lessner, M.G. Medvesky, D.M. Glebatis, and L.F. Novick 1991 Geographic distribution of newborn HIV seroprevalence in relation to four sociodemographic variables. American Journal of Public Health 81(Suppl):25-29.
Napoli, V.M., and J.E. McGowan, Jr. 1987 How much blood is in a needlestick? [letter] Journal of Infectious Diseases 155(4):828.
Neal, J.J., C.A. Ciesielski, and P.L. Fleming 1993 Heterosexually Acquired AIDS in the United States: The Next Epidemic Wave. Paper presented at the 121st annual meeting of the American Public Health Associations, San Francisco, CA.
Nelson, K., D. Vlahov, and S. Cohn 1991 Sexually transmitted diseases in a population of intravenous drug users: Association with seropositivity to the human immunodeficiency virus (HIV). Journal of Infectious Diseases 164:457-463.
Nelson, K.E., D. Vlahov, L. Solomon, S. Cohn, and A. Muñoz in press Temporal trends of incident HIV infection in a cohort of injection drug users in Baltimore, Maryland. Archives of Internal Medicine.
Nicolosi, A., M.L. Correa Leite, M. Musicco, S. Molinari, and A. Lazzarin 1992 Parenteral and sexual transmission of human immunodeficiency virus in intravenous drug users: A study of seroconversion. American Journal of Epidemiology 135(3):225-233.
North, R.L., and K.H. Rothenberg 1993 Partner notification and the threat of domestic violence against women with HIV infection. New England Journal of Medicine 329:1194-1196.
Novick, D.M., P. Farci, T.S. Croxsan, M.B. Taylor, C.W. Schneebaum, M.E. Lai, N. Bach, R.T. Senie, A.M. Gelb, and M.J. Kreek 1988 Hepatitis D virus and human immunodeficiency virus antibodies in parenteral drug abusers who are hepatitis B surface antigen positive. Journal of Infectious Diseases 158(4):795-803.
Novick, D.M., H.L Trigg, D.C. Des Jarlais, S.R. Friedman, D. Vlahov, and M.J. Kreek 1989 Cocaine injection and ethnicity in parenteral drug users during the early years of the human immunodeficiency virus (HIV) epidemic in New York City. Journal of Medical Virology 29:181-185.
Ouellet, L., A. Jimenez, W. Johnson, et al. 1991 Shooting galleries and HIV disease: Variations in places for injecting illicit drugs. Crime and Delinquency 37:64-85.
Padian, N.S. 1987 Heterosexual transmission of acquired immunodeficiency syndrome: International perspectives and national projections. Review of Infectious Diseases 9:947-960.
Padian, N., L. Marquis, D.P. Francis, R.E. Anderson, G.W. Rutherford, P.M. O'Malley, and W. Winkelstein, Jr. 1987 Male-to-female transmission of human immunodeficiency virus. Journal of the American Medical Association 258(6):788-790.
Padian, N., J. Wiley, and S. Glass 1988 Anomalies of Infectivity in the Heterosexual Transmission of HIV. Paper presented at the Fourth International Conference on AIDS, Stockholm.
Padian, N., P.J. Hitchcock, R.E. Fullilove, 3d, V. Kohlstadt, and R. Burnham 1990 Report of the NIAID Study Group on Integrated Behavioral Research for Prevention and Control of Sexually Transmitted Diseases. Part I: Issues in defining behavioral risk factors and their distribution . Sexually Transmitted Diseases 17(4):200-204.
Padian, N.S., S.C. Shiboski, and N.P. Jewell 1991 Female-to-male transmission of human immunodeficiency virus. Journal of the American Medical Association 266(12):1664-1667.
Padian, N., S. Shiboski, E. Vittinghoff, and N. Hessol 1994 Heterosexual transmission of HIV in Northern California: 1984-1993. Presented at the Society for Epidemiologic Research, Miami.
Page, J.B., D. Chitwood, P. Smith, N. Kane, and D. McBride 1990 Intravenous drug use and HIV infection in Miami. Medical Anthropology Quarterly 4(4):56-71.
Phillips, R.K., N. Salem, and S.R. Novey 1993 Targeting HIV/AIDS Services to Meet Growing Needs of Underserved Populations in Los Angeles County. Paper presented at the 121st annual meeting of the American Public health Association, San Francisco, CA.
Polk, B.F. 1985 Female-to-male transmission of AIDS. Journal of the American Medical Association 254(22):3177-3178.
Prevots, D.R., D.M. Allen, J.S. Lehman, T.A. Green, L.R. Petersen, and M. Gwinn 1995 Trends in HIV Seroprevalence Among Injection Drug Users Entering Drug Treatment Centers, United States, 1988-1993. Paper presented at the Second National Conference on Human Retroviruses and Related Infections, Abstract 312. In press, American Journal of Epidemiology.
Primm, B.J., L.S. Brown, B.S. Gibson, and A. Chu 1988 The Range of Sexual Behaviors of Intravenous Drug Abusers. Presented at the Fourth International AIDS Conference, Stockholm, June 12-16.
Ralph, N., and C. Spigner 1986 Contraceptive practices among female heroin addicts. American Journal of Public Health 76:1016-1017.
Redfield, R.R., P.D. Markham, S.Z. Salahuddin, M.G. Sarngadharan, A.J. Bodner, T.M. Folks, W.R. Ballou, D.C. Wright, and R.C. Gallo 1985 Frequent transmission of HTLV-III among spouses of patients with AIDS-related complex and AIDS. Journal of the American Medical Association 253(11):1571-1573.
Resnick, L., K. Veren, S.Z. Salahuddin, et al. 1986 Stability and inactivation of HTLV-III/LAV under clinical and laboratory environments. Journal of the American Medical Association 255:53-68.
Robertson, J.R., A.B.V. Bucknall, P.D. Welsby, J.J. Roberts, J.M. Inglis, J.F. Peutherer, and R.P. Brettle 1986 Epidemic of AIDS-related virus (HTLV-III/LAV) infection among intravenous drug users. British Medical Journal 292(6519):527-529.
Rogers, D.E. 1992 Report card on our national response to the AIDS epidemic: Some A's, too many D's. American Journal of Public Health 82(4):522-524.
Roper, W. L., H. B. Peterson, and J. W. Curran 1993 Commentary: Condoms and HIV/STD prevention—Clarifying the message. American Journal of Public Health 83(4):501-503.
Ross, M.W., A. Wodak, and J. Gold 1992 Sexual behaviour in injecting drug users. Journal of Psychology and Human Sexuality 5:89-104.
Samuels, J.F., D. Vlahov, J.C. Anthony, L. Solomon, and D.D. Celentano 1991 The practice of ''frontloading" among intravenous drug users: Association with HIV-antibody. AIDS 5(3):343.
Sapira, J.D. 1968 The narcotic addict as a medical patient. American Journal of Medicine 45:555-588.
Saxon, A., D.A. Calsyn, S. Whittaker, and G. Freeman 1991 Sexual behavior of intravenous drug users in treatment. Journal of Acquired Immune Deficiency Syndromes 4:938-944
Schoenbaum, E.E., D. Hartel, P.A. Selwyn, R.S. Klein, K. Davenny, M. Rogers, C. Feiner, and G. Friedland 1989 Risk factors for human immunodeficiency virus infection in intravenous drug users. New England Journal of Medicine 321(13):874-879.
Selwyn, P.A., and P.A. Alcabes 1994 The Potential Impact of Needle Exchange Programs on Health Outcomes Other Than HIV and Drug Use. Paper commissioned by the Panel on Needle Exchange and Bleach Distribution Programs.
Selwyn, P.A., R.J. Carter, E.E. Schoenbaum, V.J. Robertson, R.S. Klein, and M.F. Rogers 1989 Knowledge of HIV antibody status and decisions to continue or terminate pregnancy among intravenous drug users. Journal of the American Medical Association 261(24):3567-3571.
Solomon, L., J. Astemborski, D. Warren, A. Muñoz, S. Cohn, D. Vlahov, and K. Nelson 1993 Difference in risk factors for human immunodeficiency virus type-1 seroconversion among male and female intravenous drug users. American Journal of Epidemiology 137(8):892-898.
Stein, M.D. 1990 Medical complications of intravenous drug use. Journal of General Internal Medicine 5:249-257.
Stimmel, B., S. Vernace, and F. Schaffner 1975 Hepatitis B surface antigen and antibody in asymptomatic drug users. Journal of the American Medical Association 243:1135-1138.
Turner, C., H. Miller, and L. Moses, eds. 1989 AIDS: Sexual Behavior and Intravenous Drug Use. National Research Council. Washington, DC: National Academy Press.
U.S. Public Health Service 1986 Coolfont report: A PHS plan for prevention and control of AIDS and the AIDS virus. Public Health Reports 101:341-348. 1994 Fight against HIV/AIDS moves to new fronts. Prevention Report, Office of Disease Prevention and Health Promotion. Washington, DC: U.S. Department of Health and Human Services.
Valdiserri, R. 1994 Presentation at HIV Prevention: Looking Back, Looking Ahead: Targeted and
Universal Approaches to Reducing the Risk of HIV Transmission, New York Academy of Medicine, September 20.
Vermund, S.H. 1991 Changing estimates of HIV-1 seroprevalence in the United States. Journal of NIH Research 3:77-81.
Vermund, S.H., M.A. Galbraith, S.C. Ebner, A.R. Sheon, and R.A. Kaslow 1992 Human immunodeficiency virus/acquired immunodeficiency syndrome in pregnant women. Annals of Epidemiology 2(6):773-803.
Vlahov, D., A. Muñoz, J.C. Anthony, S. Cohn, D.D. Celentano, and K.E. Nelson 1990 Association of drug injection patterns with antibody to human immunodeficiency virus type 1 among intravenous drug users in Baltimore, Maryland. New England Journal of Medicine 123(5):847-856.
Weiss, R., and S. Mirin 1987 Cocaine. Washington, DC: American Psychiatric Press.
Winkelstein, W., Jr., M. Samuel, N.S. Padian, J.A. Wiley, W. Lang, R.E. Anderson, and J.A. Levy 1987 The San Francisco Men's Health Study, III: Reduction in human immunodeficiency virus transmission among homosexual/bisexual men, 1982-86. American Journal of Public Health 77(6):685-689.
Worth, D. 1988 Self-Help Interventions with Women at High Risk of HIV Infection. Montefiore Medical Center, New York City.
1989 Sexual decision-making and AIDS: Why condom promotion among vulnerable women is likely to fail. Studies in Family Planning 20(6):297-307.
Zule, W.A. 1992 Risk and reciprocity: HIV and the injection drug user. Journal of Psychoactive Drugs 24(3):243-249.