2
U.S. Physician Supply and Requirements: Match or Mismatch?
Discussion of today's issues relating to the supply of and requirements for physicians in this nation requires some appreciation of policies and events affecting the physician workforce that date to World War II. This chapter briefly reviews those developments and then turns to a more detailed description of the current stock of physicians and expected trends in physician supply. Because any analysis of the match or mismatch between supply and requirements calls for complex forecasts of numbers, the chapter also briefly describes common approaches to estimating the present and future supply of physicians and the need or demand for physician services.1 That discussion is followed by a section on factors that will affect the future requirements for physicians. A short section provides some illustrative comparisons of physician-to-population ratios for the United States and selected other nations. The chapter ends with discussion of conclusions that can be drawn from research, the marketplace, and other evidence.
PHYSICIAN WORKFORCE ISSUES SINCE WORLD WAR II
General Issues
The aggregate supply, geographic distribution, and specialty mix of physicians in the United States have been topics of major national interest since the end of World War II because of the impact of the physician workforce on the cost, accessibility, and quality of health care. With respect to costs, although
direct outlays for physician services constitute only 20 percent of health care expenditures, some experts have estimated that decisions made by physicians are directly or indirectly responsible for 70 to 90 percent of all health care expenditures (Feil et al., 1993; Mullan et al., 1995). An inadequate physician supply or a maldistribution of physicians geographically or by specialty (or both) is widely believed to impair access to health care. With respect to quality of care, a physician shortage might make medical care unavailable, but a physician surplus might produce underemployed practitioners with poor technical skills or create incentives to recommend unnecessary diagnostic and therapeutic procedures.
Pre-1980s Era
Concerns about a physician shortage dominated national physician workforce policy during the 1950s, 1960s, and early 1970s. As given in government statistics of the time, the number of active nonfederal M.D. physicians per 100,000 population in 1950, for example, was 126.6; the figure rose to 127.4 in 1960 and 137.4 in 1970 (DHHS, 1993). At those levels, the consensus was that the United States needed more physicians to provide medical care to a growing population, to expand access to care in rural and inner-city areas, and to meet the increased demand for care that would result from the passage of Medicare and Medicaid legislation.
The response to these perceived needs was complex. Federal and state governments took steps to increase the domestic production of physicians and to enable more graduates of foreign medical schools—that is, international medical graduates, or IMGs—to train and practice in the United States. Federal initiatives included capitation and construction grants to medical schools; direct support for education and training in family medicine, general internal medicine, and pediatrics; and payments to hospitals through Medicare and some state Medicaid programs for the costs associated with residency training programs. Federal funding was also made available to support the education and training of nurse practitioners and physician assistants. Several service-linked programs were developed, including the National Health Service Corps and financial support for community health centers and area health education centers (Kindig et al., 1993; Schroeder, 1994a; Desmarais, 1995; Mullan, 1995). A variety of state initiatives—such as the opening of new medical schools, increases in medical school class size, and the development of loan and scholarship programs for medical students—supplemented the federal effort.
These efforts to increase the U.S. physician supply were spectacularly successful (Figure 2-1). Between 1970-1971 and 1991-1992 the annual number of graduates from allopathic medical schools (M.D.s) in this country increased from approximately 9,000 to more than 15,000;2 the analogous rise for graduates
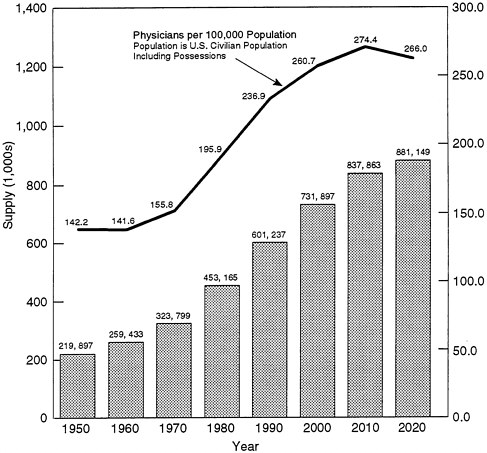
FIGURE 2-1. Basic format of figure adapted from Rivo and Satcher (1993, p. 1077).
SOURCE: Unpublished data from the Bureau of Health Professions (BHP) provided November 1, 1995. 1950 through 1990 data adjusted by BHP from American Medical Association Physician Masterfile and unpublished American Osteopathic Association data. Projections for 2000, 2010, and 2020 are from the BHP physician supply model.
of osteopathic medical schools (D.O.s) was from 500 to more than 1,500. As a result of these increases and federal policies that allowed more IMGs to practice in the United States, the number of physicians per 100,000 population increased dramatically.3 A rise in the ratio of active nonfederal M.D.s to population of 60 percent occurred in the 20-year period between 1970 and 1990: the increase was from 137.4 per 100,000 population in 1970 to 173.4 in 1980 and then to 219.5 in 1991. An even greater percentage increase (104 percent, but on a considerably smaller base) was posted in the ratio of active osteopathic physicians per 100,000 population: from 5.7 in 1970 to 7.5 in 1980 and then to 11.6 in 1991. In short,
by the mid-1970s the nation had 1 active physician for every 584 persons in the country (DHEW, 1977) and, by the early 1990s, 1 for every 398 persons.
A major change in thinking about the adequacy of the U.S. physician workforce came in 1980 with submission of the report of the Graduate Medical Education National Advisory Committee (GMENAC, 1981). GMENAC supply forecasts were for 536,000 professionally active physicians in 1990 and nearly 643,000 in 2000—for physician-to-population ratios of 220 and 247 per 100,000 persons, respectively. Based on an adjusted need-based forecast of the requirement for physicians (see below), GMENAC concluded that the nation could expect to have a surplus of physicians in the future (not a shortage) and that the surplus would grow from 70,000 physicians in 1990 to 145,000 by the year 2000.
Although controversial, the GMENAC report signaled the beginning of a change in federal physician workforce policy. It catalyzed the development of a widespread (but not universal) consensus that the nation either had or soon would have a physician supply that exceeded its requirements.4 This view, as well as pressure to reduce federal spending and the emphasis on a competitive market approach to health care that began with the election of President Reagan in 1980, had several effects. In particular, it caused the federal government to reduce greatly its effort to increase the aggregate physician supply and to focus more of its attention on problems associated with the geographic and specialty maldistribution of physicians. Even with these changes in emphasis, however, the U.S. physician supply could be characterized, from then to the present, as very large and growing.
Current Status
By no means did the numbers of physicians in this country stop rising in the 1980s. Using data from the masterfiles of the American Medical Association (AMA) and the American Osteopathic Association (AOA), Kindig (1994) estimated that, in 1992, the nation had more than 628,000 active allopathic and osteopathic physicians, or 245.0 physicians per 100,000 population. Of these, slightly more than 461,000 (74 percent) were engaged in patient care, yielding a rate of 180.1 per 100,000 population. An additional 99,000 physicians were providing some patient care as residents or fellows (38.7 per 100,000 population).
Table 2-1 presents the breakdown of all physician supply in more detail. Although these are 1992 data, 1994 figures would be higher in terms of both absolute numbers of physicians and population ratios. The instructive point is that the numbers for all active physicians exceed those that GMENAC forecast for 1990 and in fact approach the levels estimated for 2000.
Although the committee is not dealing directly with issues of specialty or geographic maldistribution, these matters remain significant to the broader questions of restructuring the health care system in this country. Of relevance to the specialty debate are the data that Kindig (1994) presents showing that, in 1992, slightly more than 182,000 active patient care physicians (not including residents and fellows) were in the primary care disciplines of family practice, general practice, general internal medicine, and general pediatrics. This translates into approximately 71 practitioners per 100,000 population, or about 39 percent of the patient care physicians not in training. Left to debate is whether this proportion of the physician workforce ostensibly involved in primary care is adequate or still reflects a small to moderate shortage in primary care.
Another controversial point about the U.S. physician supply concerns the country of origin of those clinicians. According to Mullan et al. (1995), in 1992 approximately 23 percent of M.D.s active in the United States (139,086 of 605,685) were graduates of foreign medical schools.5 Of these, just over 19,000 (14 percent) were native U.S. citizens (USIMGs); most received their undergraduate medical education in the Dominican Republic, Grenada, Mexico, or Montserrat. The remaining nearly 120,000 IMGs practicing in the United States that year were foreign born (FNIMGs). Since 1975, approximately 25 percent of IMGs have come from India, and considerable numbers have also come from Pakistan, the Philippines, the United Arab Republic, Israel, Italy, and the United Kingdom.
Physician Workforce Trends
Overall Trends in Supply
Numbers at any point in time do not tell the entire story about the nation's current or anticipated supply of physicians; trend lines are also important. For the past two decades the U.S. physician supply has been growing at one and one-half times the rate of growth of the general population (COGME, 1994). In 1970, depending on who is included, there were between 151 (see Table 2-1) and 157 active physicians (Schroeder, 1994b) per 100,000 population. As noted previously, by 1992 the active-physician-to-population ratio had grown to 245 per 100,000. The federal Council on Graduate Medical Education (COGME) has estimated that if current trends continue there will be 298 active U.S. physicians per 100,000 by the year 2020,6 after which the physician-to-population ratio is expected to remain constant or decline slightly. This projected "bulge" in the U.S. physician supply in the early part of the twenty-first century is considered inevitable inasmuch as most physicians who contribute to it are already in training or in practice (Cooper, 1994).
TABLE 2-1. Supply of Physicians in the United States, 1970, 1980, 1992, by Type of Activity
|
|
No. of Physiciansa |
No. of Physicians per 100,000 Populationa |
||||
|
Type of Activity |
1970 |
1980 |
1992 |
1970 |
1980 |
1992 |
|
Total |
328,020 |
462,276 |
685,291 |
160.9 |
203.5 |
267.5 |
|
Total Active Physiciansb |
308,487 |
436,667 |
627,723 |
151.4 |
192.2 |
245.0 |
|
Total active physicians in patient carec |
222,657 |
310,533 |
461,405 |
109.2 |
136.7 |
180.1 |
|
Total active physicians in other professional activity |
31,582 |
38,009 |
39,816 |
15.5 |
16.7 |
15.5 |
|
Teaching |
NA |
NA |
8,293 |
NA |
NA |
3.2 |
|
Research |
NA |
NA |
16,398 |
NA |
NA |
6.4 |
|
Administration |
NA |
NA |
15,125 |
NA |
NA |
5.9 |
|
Total physicians in training providing patient cared |
50,687 |
61,450 |
99,138 |
24.9 |
27.1 |
38.7 |
|
Not classifiede |
3,561 |
26,675 |
27,364 |
1.7 |
11.7 |
10.7 |
|
Total Inactive Physicians |
19,533 |
25,609 |
57,568 |
9.6 |
11.3 |
22.5 |
|
NOTE: NA = not available. a Data for 1970 and 1980 are for allopathic physicians (M.D.s) only; data for 1992 include both allopathic and osteopathic physicians. b Includes all physicians and physicians in training except those specifically identified as ''inactive." c Although physicians in training clearly provide considerable patient care, they are not included in this total; see their separate line item, below. d "Physicians in training" is defined for 1970 and 1980 as "interns and residents, all years"; for 1992 the term is defined as "residents and fellows." e "Not classified" includes, for 1970 and 1980, those physicians for whom an address is not known. SOURCES: Data for 1970 and 1980 adapted from National Center for Health Statistics (NCHS, 1983, Tables 1 and 55). Data for 1992 adapted from Kindig (1994, Table 1 and text). |
||||||
The increase in enrollment in the 126 U.S. allopathic and 16 osteopathic medical schools during the 1960s and 1970s contributed considerably to increases in the nation's physician supply. Since the 1980s, however, the number of M.D. and D.O. graduates from domestic schools has remained quite constant—about 17,500 per year. Nonetheless, the number could begin to rise in the years ahead if the four schools of osteopathic medicine now under development successfully put their plans into effect (Arnstein, 1995).
Trends in Graduate Medical Education
Despite this relative stability in the number of U.S. medical school graduates, the number of physicians in graduate medical education (GME) programs has been increasing steadily: about 4 percent per year. According to Shine (1995), more than 104,000 physicians were in GME training in 1993–1994 as compared to fewer than 85,000 in 1988–1989. This represents an increase of about 24 percent in just five years.
The rise in these GME figures is explained by three factors. One is the fact that physicians in residency training are a source of financial support for hospitals through the current incentives and mechanisms of GME payments from the federal government. A second is that, on average, residents remain in training longer than they once did.
Third, in large part the increasing numbers of residency positions are occupied by growing numbers of IMGs. Mullan et al. (1995), for example, provided data to show that the number of U.S. medical graduates (USMGs) in GME training has remained stable since the early 1980s but that, between 1988 and 1993, the number of IMGs in residency or fellowship training increased 80 percent (from 12,433 to 22,706). The number of IMGs in first-year residency positions grew by more than 3,200 between 1988 and 1993, whereas the number of USMGs declined by nearly 230 individuals (Fitzhugh Mullan, Director of the Bureau of Health Professions, data presented to the committee, July 19, 1995). In 1993–1994, more than one-quarter of first-year residency positions were filled by IMGs.
Green (1995) provided data from major academic medical centers in New York State showing that 24 percent of the residency positions were held by IMGs (slightly more than 6 percent USIMGs and 17 percent FNIMGs [respectively, U.S.-born and foreign-born]); the percentages by specialty ranged from 100 percent IMGs (pediatric nephrology) to 0 percent (allergy and immunology; radiation oncology). Whitcomb and Miller (1995) reported that of more than 20,000 first-year residents in six specialties (family practice, internal medicine, obstetrics/gynecology [OB/GYN], pediatrics, psychiatry, and surgery), nearly 32 percent were IMGs (ranging from about 7 percent in OB/GYN to 44 percent in psychiatry).
The increase in IMGs in GME programs is attributable directly to an increase in FNIMGs, not USIMGs (Mullan et al., 1995; Fitzhugh Mullan, Director of the Bureau of Health Professions, presentation to the committee, July 19, 1995). In fact, the latter have decreased in number, reflecting the lower number of U.S. students studying medicine outside the United States in the mid-to late-1980s. In 1993, for example, of the 22,706 IMG residents, 35 percent were in the United States on exchange visitor (J) visas; 31 percent were permanent U.S. residents; 12 percent were naturalized U.S. citizens, and 12 percent were in various other immigration categories (such as refugees); only 10 percent were native U.S. citizens.
The distribution across immigration categories is important, because it suggests that using immigration law, and particularly changing the J or exchange visa category, will not enable the United States to deal effectively with the large and growing pool of IMGs. For example, the large proportion of permanent U.S. residents represents those physicians who "have a green card" (often through family preference in the form of having a first-degree relative who is a U.S. citizen) and who are on their way to becoming naturalized citizens here. Although in the past the exchange visa was assumed to be a major policy instrument in this area, it has recently been liberalized and, in any case, has traditionally been exploited or circumvented. Thus, stiffening requirements in this visa category will still control only at best about one-third of IMG residents in terms of their movement into practice in this country.
At first glance, the relevance of the presence of IMGs, particularly FNIMGs, to the overall question of physician supply in this nation may be questioned. However, various experts have estimated that as many as 75 percent of the FNIMGs who take their residency training in the United States will remain in this country to practice (Mullan et al., 1995); in 1993 alone, about 60 percent of IMGs were in immigration categories that imply a high probability the individuals would remain permanently in the United States. Thus, the issue of the long-term match between the supply of physicians in this country and the expected requirements for physician services cannot, ultimately, be addressed without consideration of the role of and policies toward IMGs.
METHODS OF ESTIMATING PHYSICIAN SUPPLY, PRODUCTIVITY, AND REQUIREMENTS
Physician Supply
Most analyses of the U.S. physician supply utilize the databases compiled by the AMA and the AOA; some also rely on information from the American Board of Medical Specialties. Beginning with the current physician population, such analyses attempt to predict the future rate of entrance to and exit from the
profession. Entrants include graduates of U.S. allopathic and osteopathic medical schools and IMGs admitted to practice in the various states. Losses from the profession include those due to factors such as death, retirement, or change of career. Although this aspect of predicting the future physician supply is rather straightforward, Feil et al. (1993) have emphasized that apparently minor disagreements about entrance and exit rates can lead to large discrepancies in supply forecasts over time.
Physician Productivity
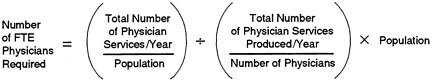
In considering the match between the supply of and requirements for physicians (or their services), assumptions about productivity can play a significant role in the calculations. In plain language, physician productivity is the total number of physician services produced in a year divided by the total number of active physicians in that year.7 The need or demand for physician services—or, more precisely, the number of the "full-time-equivalent" (FTE) physicians required to yield that number of physician services—is the product of the total population and the per capita use of physician services in a year divided by physician productivity.
The idea is captured in the following illustrative equation (adapted from Reinhardt, 1991):
Future productivity is, however, notoriously difficult to forecast. The growth of salaried compensation for physicians as a result of the growth of managed care and similar arrangements, the increasing number of women in medicine and osteopathy, the aging of the physician workforce, the uncertain but perhaps rising rates of retirement of older physicians, and the desire of some younger physicians to limit their work hours in order to spend more time with their families or to pursue other activities have led several experts to predict that the productivity of U.S. physicians will decrease in the years ahead (Kletke et al., 1990; Cooper, 1994). Reinhardt (1991) called attention in particular to the point that the average productivity of physicians at any given time is a significant factor in producing (estimated) physician surpluses or shortages; other relevant
factors are the state of medical technology at the time and the willingness of physicians to delegate tasks to nonphysician personnel.
Furthermore, an important distinction between "hourly productivity" and "total productivity" should be maintained. The former is essentially the number of physician services produced per physician-hour, and it may increase over time in some managed care arrangements (e.g., through delegation of tasks). The latter is the product of hourly productivity and the numbers of hours worked per year per physician; this figure might well decrease over time, owing to some of the factors noted above.
Physician Requirements
The term "requirement" is generally used as an umbrella term to encompasses all attempts to measure the need or the demand for physician services. Determining the requirement for physicians or their services involves more judgment and assumptions than does predicting the future physician supply. Not surprisingly, therefore, no single approach to forecasting physician requirements is universally accepted (Feil et al., 1993). Four methods of estimating the future requirement for physicians have been used in recent years: (1) demand-based forecasting, (2) need-based forecasting, (3) adjusted need-based forecasting, and (4) the extrapolation method.
Demand-based forecasts of physician requirements determine the number of physicians needed in the future based on current patterns of health service utilization and projected changes in those patterns over time. Demand-based forecasting measures what is likely to be rather than what should be. It forms the basis of the forecasts developed by the Bureau of Health Professions (BHP, of the Health Resources and Services Administration [HRSA], Department of Health and Human Services [DHHS]) and the AMA. Demand-based forecasts are seen as more pragmatic than those using a need-based approach, and they have been criticized for their tendency to carry current inequities into the future and for their failure to anticipate future trends (Schroeder, 1994a).
Pure need-based forecasts of physician requirements attempt to estimate the actual burden (incidence and prevalence) of illness and injury in the entire population and provide for an ideal level of medical care for that burden. They assume that all illness will be not only identified but also treated, and thus these models are based on what should be rather than what is or what will be. They are not widely used because they tend to inflate the amount of illness that will actually be seen by physicians and are based on the provision of care that would require amounts of resources well beyond those that are currently available or likely to be so in the future (Schroeder, 1994a).
The impractical nature of pure need-based forecasts of physician requirements has led to the development of an adjusted need-based approach.
GMENAC (1981), for example, made a downward adjustment in its need-based forecasts to recognize the reality that a certain amount of illness does not require the services of a physician and that only a fraction of illness within the population can realistically be expected to be identified and managed by health care providers. Although the adjusted need-based model is more realistic than the pure need-based variety, it too has been criticized as being logistically unwieldy and open to bias because it requires panels of experts to make judgments about the type and amount of health care needed (Schroeder, 1994a).
A variant of the demand-based forecasting model is the extrapolation method recently used by Weiner (1994) in a study commissioned for COGME. In this approach, current patterns of staffing within managed care plans are extrapolated to a reshaped health care system of the future. The extrapolation method (which has also been used by Schwartz et al., 1988, and Mulhausen and McGee, 1989) has many of the same strengths and weaknesses of other demand-based studies. It also has been criticized for assuming that the populations currently enrolled in managed care plans and their levels of utilization are representative of the population as a whole (Feil et al., 1993). Weiner (1993) has cautioned that "adopting HMO staffing levels as ideals may lead to an underestimate of the 'true need' within a general population" (p. 435).
In summary, no single method of predicting either the supply of or the requirements for physicians (or physician services) is widely accepted as best or completely accurate.8 All methods in current use require assumptions about the future that may or may not be correct, and relatively small variations in assumptions can lead to large discrepancies in forecasting that are magnified the farther into the future one attempts to extend the prediction. In view of this inherent weakness in any forecasting methodology, the fact that most studies of the physician workforce in the past 15 years have reached similar conclusions about the adequacy of the U.S. physician supply is perhaps surprising, but it lends credence to the basic judgment about existing and future oversupply.
THE FUTURE REQUIREMENT FOR PHYSICIANS
Factors That Could Increase Requirements
Several factors could result in an increased need or demand for physician services in the years ahead. Most important of these would be enactment of legislation to provide universal access to health care services for the estimated 40 million Americans who now lack health insurance. In view of both the failure of the Clinton administration to obtain passage of the Health Security Act and the more recent efforts to reduce federal spending by dramatic levels, the goal of universal access is very unlikely to be attained in the foreseeable future.
Other factors that could increase the demand for physician services include the emergence of new diseases such as acquired immunodeficiency syndrome (AIDS) or the reemergence of "old" diseases such as tuberculosis (IOM, 1992), the development of new health technologies to treat diseases for which no adequate treatment currently exists, and the again of the U.S. population. Yet other phenomena, such as changes in health care organization and in financing and reimbursement mechanisms, might dampen the demand for physician services while increasing the demand for related health care services.
For example, the growth in the number of elderly persons in this country (and the aging of that cohort) could increase the demand for long-term-care facilities, geriatric nurse practitioners, and other nursing personnel more than the demand for physician services. Furthermore, nearly a half century of biomedical research has yielded much knowledge now ready for clinical evaluation and perhaps application; this may prompt a greater use of physicians as clinical investigators as well as higher employment of physicians in the pharmaceutical and biotechnology industries, although the proportion of physicians in research or employment by such firms is tiny in comparison to the proportion in patient care. Putting a quantitative figure on the impact of all these factors on physician requirements is extremely difficult (Weiner, 1993).
Factors That Could Decrease Requirements
Managed Care
Most knowledgeable observers believe that in the absence of legislation to guarantee universal access to health care, future requirements for physician services will drop. A major factor in this assessment is the growth of managed care (see the appendix to this chapter). According to the Physician Payment Review Commission (PPRC, 1995), enrollment in health maintenance organizations (HMOs) in the United States more than doubled between 1985 and 1994, increasing to 17 percent in 1994; when a broader definition of managed care is used, data on insured persons in large firms suggest that as many as 65 percent are in some form of managed care. COGME (1994) has estimated that by the year 2000, two-thirds of the U.S. population will be enrolled in some type of managed care arrangement with strong utilization controls. The Prospective Payment Assessment Commission (ProPAC, 1995) has also cited figures indicating that only about one-third of insured people are in indemnity plans, and about two-thirds are in HMOs, preferred provider organizations (PPOs), or point-of-service (POS) arrangements; Davis et al. (1995) puts the figures at "more than half" of the employed, insured population in "forms of managed care that limit
enrollees' choice to a restricted network of physicians, hospitals, and other providers" (p. 100).
The net effect of managed care on requirements for physician services is driven by several factors, however. One is the proportion of the population actually in managed care organizations, which is large, as just noted, but unpredictable for the longer run. Another is the demographics of persons enrolled in such plans. Factors likely to reduce the effective demand for physician services (examples from Davis et al., 1995) include age (being younger), ethnic background (being of minority status), and income and education levels (being of lower income and less education).
A third variable is the ratio of physicians to population in those organizations. In general, managed care uses fewer physicians per unit of population served than does the traditional fee-for-service (FFS) sector. One report put the use by staff-and group-model HMOs at about 130 FTE patient care physicians per 100,000 enrollees, a use rate 28 percent below the current U.S. patient care physician supply of 180 per 100,000 (Kindig et al., 1993); Gamliel et al. (1995) cited current ratios in HMOs of 120 to 138 (as contrasted with prevailing ratios overall of 225 and 104 per 100,000 populations in metropolitan and nonmetropolitan areas, respectively). Other information, however, suggests that the ratio of patient care physicians to enrollees in "mature HMOs" comes closer to the FFS levels; Dial et al. (1995) put the figure at perhaps as high as 140 per 100,000 members.
These ratios also vary considerably by type of plan, region of the country, and other factors. For example, in one survey of HMOs belonging to the Group Health Association of America (GHAA), the interquartile range of full-time physicians per 100,000 members varied from 85 to 168 (Dial et al., 1995, citing Palsbo et al., 1993). Dial et al. (1995) reported the median ratio of 136 FTE physicians per 100,000 enrollees (weighted by various characteristics of the HMOs' enrollment) in a group of GHAA member HMOs. More detailed figures were 109 for staff-model HMOs and 142 for group-model HMOs; 284 for smaller HMOs (enrollments below 80,000) and 125 for larger HMOs. The authors note, however, that these figures can be low for managed care organizations overall because the sample excluded independent practice association (IPA) and network-type plans and because the data omit counts of hospital-based physicians.
Finally, data from a study conducted by the University Hospital Consortium (UHC) (Neal Vanselow, Tulane University, personal communication, 1995) show an HMO average of 137 physicians per 100,000 population but a range across five different HMOs of about 99 to 178 physicians. The UHC data suggest that managed care entities use 62 percent fewer physicians per capita, although the average masks the pattern of greater use of primary care physicians and lower use of specialists in the HMOs.
To be more specific, the UHC data indicate that the number of FTE physicians in cardiology in the nation as a whole is 4.5 per 100,000 persons but only 2.6 per 100,000 enrollees in five large HMOs. Large discrepancies exist in other medical specialties (e.g., gastroenterology, 3 and 1.6 per 100,000 persons; neurology, 3.7 and 1.6) and in some surgical specialties (OB/GYN, 13.5 and 9.1; ophthalmology, 6.5 and 2.5; orthopedics, 7.7 and 4.2; but interestingly, not in general surgery). The managed care world is moving to "carve out" mental health care, and some health care experts raise significant concerns about adequate access to the full range of mental health professionals as this phenomenon gains momentum. Thus, the committee found the UHC figures for psychiatry of interest. The U.S. average is now 14.1 psychiatrists per 100,000 population; the HMO average in the HUC data was 6.5 (with a range of 3.5 to 11.1 across the HMOs analyzed).
Managed care enrollees often represent a selected segment of the population that utilizes health care services less intensely than do persons with FFS insurance coverage, those eligible for Medicare and Medicaid, and uninsured populations. To correct for this phenomenon, COGME (1994) estimates have assumed that (1) the two-thirds of the population enrolled in managed care in the year 2000 will require 171 patient care physicians per 100,000 and (2) the one-third of the population remaining in the FFS sector will require a physician-to-population ratio of 174 per 100,000. Both of these figures are below the current U.S. patient care physician supply of 180 per 100,000.
In generalizing from all these data, it may not be unreasonable to conclude that physician-to-population ratios in a fairly tightly controlled managed care organization may be 40 physicians per 100,000 persons lower than the prevailing overall average in the nation today (i.e., 140 as contrasted with 180). This figure does not adequately take into account any large movement of Medicare or Medicaid beneficiaries into such HMOs in the future, nor does it consider the effect of increasing use of nonphysician primary care personnel (see below); these trends, however, may be offsetting in their effects on the demand for physician services and physicians.
Use of Nonphysician Personnel
Another important factor that is likely to decrease the requirement for physician services is the increase in numbers of midlevel personnel, such as advanced practice nurses (APNs) and physician assistants (PAs), who now perform many of the services that were previously the exclusive domain of physicians. There are now approximately 100,000 APNs in the United States; half are nurse practitioners or nurse-midwives; half, clinical nurse specialists (Mundinger, 1994). The number of nurse practitioners is expected to grow considerably in the years ahead as a result of the establishment of new education
and training programs (Cooper, 1994). Moreover, the supply of PAs practicing in this country in 1993 exceeded 23,300, and it will increase to between 36,000 and 40,000 by the turn of the century, depending on the assumptions made about support for PA educational programs and other factors (Advisory Group on Physician Assistants and the Workforce, 1994). Other work indicates that PAs and nurse practitioners are increasingly being substituted for medical and surgical residents in the nation's teaching hospitals (Riportella-Muller et al., 1995), although the cost-savings potential, if any, is debatable. For example, one analysis for New York City hospitals calculates that the cost of replacing physicians in residency positions with such mid-level personnel would be quite high (Green and Johnson, 1995).
The use of APNs and PAs in HMOs is considerable; about 65 percent of the GHAA HMOs surveyed by Dial et al. (1995) reported having APNs on staff, and a similar proportion also used PAs. The vast majority of the tasks of such personnel involve primary care, and they clearly substitute for primary care physicians in these plans; by and large, the higher the ratio of nonphysician personnel to primary care physicians, the lower is the ratio of primary care physicians to total membership (Dial et al., 1995).
During a site visit to Minneapolis/St. Paul and Rochester, Minnesota, in the fall of 1994, the Institute of Medicine (IOM) Committee on the Future of Primary Care observed another development that could have the effect of decreasing the requirement for physician services. Several managed care organizations in Minnesota are experimenting with a process known as "substitution" or "offloading." In an effort to increase efficiency and reduce health care costs, they are allowing health care personnel with lesser amounts of education or training to perform tasks and assume responsibilities traditionally reserved for physicians and other health professionals with longer periods of formal preparation. Registered nurses (RNs), for example, use protocols to monitor anticoagulant therapy in ambulatory patients and to manage by telephone a large percentage of uncomplicated urinary tract infections in women. Licensed practical nurses (LPNs) perform tasks previously reserved for RNs, and office assistants assume responsibilities that were previously the domain of the RN or the LPN. That IOM committee was also told that the role of physicians has changed considerably as a result of these experiments. For example, primary care physicians have more time to see patients with complex problems, thus reducing the need for referrals to specialists.
In a commentary on the restructuring and redeployment of America's health care workforce, Schwartz (1994) cautioned that the marketplace is rapidly implementing new forms of health care delivery involving broad workforce substitution without formal or rigorous evaluation of the safety or effectiveness of such interventions. He emphasized the need for studies that would delineate the specific circumstances under which one type of provider could be substituted for another and the ways in which such changes would affect patient outcomes
and costs. Should the type of substitution seen in Minnesota become the norm, however, it could markedly reduce the demand for physician services.
INTERNATIONAL COMPARISONS
Several studies have assessed the adequacy of the U.S. physician supply by comparing various measures, such as physicians per population, to the physician workforce in other countries. Comparisons must be made with caution, however, because the definitions of physician (e.g., active in patient care or not) may differ somewhat across countries and studies and because the structure and organization of health care systems may differ markedly as well. Whitcomb (1994), for example, raises ''serious questions" about using the experience of England, France, or Germany as guidance for physician workforce planning in this country.
Schroeder (1984) documented that in 1980, the U.S. supply of physicians per population was smaller than in Belgium and West Germany, about the same as in the Netherlands, and larger than in the United Kingdom. Both Belgium and the Netherlands had officially recognized a physician oversupply (evidence cited included falling physician incomes, physician underemployment or even unemployment, and low morale of those in training) and had taken steps to reduce medical school enrollment or restrict specialty training, or both. Schroeder also noted that the United States had a much higher ratio of specialists to generalists than any comparison country, and he concluded that the European experience indicated that the most pressing health manpower problem in the United States was an oversupply of specialists.
An analysis by Schieber et al. (1993) of the health care delivery systems of the late 1980s and early 1990s in the 24 industrialized countries that constituted the membership of the Organization for Economic Cooperation and Development (OECD) revealed a physician supply ranging from 90 per 100,000 population (Turkey) to 380 (Spain). The U.S. supply was 230 per 100,000 persons at that time, a figure close to the OECD average of 240. Again, the United States was found to have a much higher specialist-to-generalist ratio than the other OECD nations. The authors concluded that these differences in specialty mix tempered the utility of the comparisons.
In a study done for BHP/HRSA, Whitcomb (1994) found that the 1993 physician workforces in several western democracies (including the United States) ranged between 230 and 280 physicians per 100,000 persons. At 140, the United Kingdom had a recognized physician shortage. Data from France suggested both physician oversupply and physician unemployment.
BHP/HRSA concluded that a physician oversupply has been recognized in France, Germany, Belgium, the Netherlands, and Spain. For example, physician unemployment in Spain was said to have reached 20 percent in 1990, and both
unemployment and underemployment of physicians were recognized in several of the other nations. In Germany, for instance, an estimated 5,000 to 8,000 doctors are unemployed, mostly new graduates and women (George Sheldon, University of North Carolina, personal communication, 1995). All five countries are taking steps to control the physician supply.
Drawing firm conclusions about the appropriateness of the U.S. physician supply based on international comparisons is severely constrained by major differences among health care systems. In many of the countries used for comparison purposes, health care delivery is based on the principles of managed care. Often, these nations offer universal access to health care, and many may engage in extensive governmental regulation of the delivery system. Medical education and training programs differ from those in the United States as well, and the resultant distribution by specialty is quite different from the more than 2:1 specialist-to-generalist ratio found in this country. Even with these caveats, however, the notion that the United States has a very generous supply of physicians, especially of subspecialists, relative to the supply in other major Western democracies seems generally to be a defensible one.
MATCH OR MISMATCH?
Conclusions of Physician Workforce Studies
Most of the physician workforce studies appearing since 1980 have concluded that the U.S. physician supply will exceed requirements and will continue to get even further out of balance if nothing occurs to change these trends. As already noted, for instance, the seminal GMENAC study (1981) predicted that the aggregate U.S. physician supply would overshoot requirements by 70,000 in 1990 and by 145,000 in the year 2000. Its findings derived from an adjusted need-based approach for determining the requirement for physician services.
A decade later, PPRC (1992) reached a similar view. Although PPRC did not conduct an independent study of the adequacy of the U.S. physician workforce, its 1992 annual report to Congress concluded from available data that "the number of physicians exceeds, or soon will exceed, that required to meet national health care needs" (p. 284).
Feil et al. (1993) reviewed eight major forecasts of physician supply and requirements published between 1980 and 1990; they concluded that, with one exception, all suggested a physician surplus in the year 2000. The size of the predicted oversupply varied from fewer than 50,000 (Jacobsen and Rimm, 1987) to more than 300,000 (Mulhausen and McGee, 1989).
The exception to the studies reviewed by Feil and her coauthors was a study done by Schwartz et al. (1988), which predicted a near balance between
physician supply and demand by the turn of the century. The authors also concluded that if a slight surplus should occur it was likely to be largely erased by increased involvement of physicians in administrative activities and a variety of nontraditional clinical activities that currently occupied little of a physician's time.
Some of the assumptions in the Schwartz et al. study have been questioned, however. For example, the authors assumed that less than one-half (specifically, 44 percent) of the U.S. population would be enrolled in "competitive medical plans" by the year 2000, but more recent predictions are that perhaps two-thirds of the population will be enrolled in some form of managed care with tight utilization controls by that date (COGME, 1994). Perhaps more important was another assumption concerning GME—specifically, that the number of residents in training would remain constant at the 1983 level of 73,000. In fact, the number of resident physicians has increased each year since 1983; numbers between 104,000 (Shine, 1995) and 108,000 (COGME, 1995) have been cited for 1993–1994 (the differences stemming from data sources and which types of trainees are counted). Finally, the Schwartz study did not appear to take into account either the role played by increasing numbers of PAs and APNs or the effect of substitution on the need for physician services.
Using an extrapolation method and assuming that 40 to 65 percent of Americans would receive their health care from integrated managed care networks in the near future and that all citizens would be covered by some form of health insurance, Weiner (1994) predicted that, in the year 2000, the overall surplus of patient care physicians would reach 165,000, a figure representing about 30 percent of all physicians in the patient care category. He further estimated that in 2000 the supply of specialists would exceed requirements by 61 to 67 percent (depending on the assumptions used) and that the supply of primary care physicians would be in approximate balance with requirements.
In its fourth report to Congress and DHHS, COGME (1994) predicted an overall surplus of 80,000 patient care physicians in the year 2000, consisting of a shortage of 35,000 generalist physicians and a surplus of 115,000 specialists. Taking a longer view, it also predicted a net physician surplus of 120,000 by 2020, with a projected shortage of 80,000 generalists and a surplus of 200,000 specialists. COGME's projections resulted from a demand-based study that assumed no changes in the current training pipeline and a health care system dominated by managed care arrangements. In 1995, COGME revised the figures upwards to "a year 2000 surplus of 125,000 specialists and a modest shortage of 20,000 generalist physicians …" (p. 1), for a net oversupply of 105,000. By implication, the estimated overall surpluses in coming years are growing rapidly.
In yet another recent analysis, Gamliel et al. (1995) applied an extrapolation model similar to that of Weiner. With some different assumptions and the supposition that current trends would apply, these authors arrived at the following predictions: (1) an overall surplus of 73,000 patient care physicians
in 2000 (comprising a surplus of 111,000 specialists and a deficit of 38,000 generalists) and (2) a surplus of 111,000 physicians in 2020 (about 196,000 more specialists than needed and about 85,000 fewer generalists).
Evidence from the Marketplace
Physician Incomes
One market indicator of the adequacy of the physician supply might be changes in physician income. Other factors being equal in a reasonably perfect market (which health care is not), a physician shortage would be expected to result in increased incomes, whereas a surplus would have the opposite effect. Several surveys of U.S. physician income reported during the past two years give conflicting results.
Some reports appear to support the idea of balance (or at least no obvious surplus or shortage). Mitka (1994b), describing data from an AMA survey, showed that median physician income rose 5.4 percent in 1993, with larger increases for the primary care specialties and no changes for many nonprimary care specialties. Two surveys of physicians in group practice by the Medical Group Management Association (MGMA) showed that overall physician income rose 2.3 percent in 1993 and 2.2 percent in 1994 (Mitka, 1995b). In 1993, this involved an appreciable increase in the income of primary care physicians and a decline or, at best, only a small growth in the income of most specialists (Mitka, 1994a). Academic physicians responding to an MGMA survey indicated that faculty pay for primary care physicians increased 4.6 percent in 1994 and specialist pay decreased 1.8 percent; overall, academic physician pay increased 2.3 percent in 1994 compared with 4.2 percent in 1993 (Mitka, 1995a).
Two other surveys show an overall decrease in physician incomes, which might be thought to be more consistent with an oversupply. First, a survey by Medical Economics of the 1993 median net income of office-based physicians in private practice yielded information pointing to an overall drop of 8.3 percent (Goldberg, 1994). Incomes rose in family practice and internal medicine and declined for most other specialties. Second, William M. Mercer Inc. surveyed 191 organizations and developed data to indicate that, in 1994, the average total cash compensation of physicians employed by group practices, hospitals, and HMOs decreased by 2.3 percent (Borzo, 1995). This survey also demonstrated a rise in cash compensation for family practitioners, internists, and pediatricians.
A decade ago, Sloan and Schwartz (1983) indicated that physician supply and outlays for physician services grew in the 1970s; in addition, gross income of individual physicians increased about 1 percent annually, but real net income for physicians rose only about 1.7 percent over the entire period. Changes in
physician-to-population ratios (i.e., supply) explained only about one-fifth of the rise in expenditures. More important explanatory variables included growing population, aging of the population, and expanding insurance coverage; specialty mix had little impact then on spending. The authors noted that "some four fifths of the observed increase in expenditures would have taken place even if the physicians supply had not increased faster than the population" (p. 768). They predicted similar patterns of expenditures and physician incomes for the 1980s and, in particular, argued that the "contribution of an increased physician supply to the rise in expenditures will be relatively small" (p. 768) and that net income (in constant dollars) might stay about the same or even decline slightly because of factors such as practice expenses (e.g., malpractice insurance or medical equipment costs). Thus, information about physician supply and physician income does not lead to straightforward interpretations, and more systematic data on this point will be necessary to establish whether the growing number of physicians in the aggregate is leading to lower incomes across the board.
The impact of physician supply on physician income is more complex than just implied, however, because some experts believe that as physician supply increases, one may see a segmentation, or split, in the effect on incomes. Such a pattern would complicate any inferences to be drawn about the supply-income relationship. For the FFS sector, Frenk et al. (1991) offered the following illustration from Mexico: One group of physicians, who are older, established, and more specialized, continues to experience rising (or certainly stable) incomes; the growing number of less expert, younger, and/or less well established physicians, by contrast, finds it more difficult to maintain sufficient workloads, skills, and thus steady incomes. Conversely, however, younger physicians (certainly those coming from U.S. schools) might be thought to be trained in the latest techniques, cost-effective practice patterns, and willingness to innovate; thus, they may be able to attract appropriate patient loads, sustain existing or acquire new skills, and maintain incomes.
In the managed care sector, all of these issues are less clear. In some (but not all) arrangements, physicians may be employees of a capitated health care plan; when this is so, their personal incomes will be less directly connected to the size of their own patient load than would be true in the FFS arena. Another complicating factor is the effect that managed care's emphasis on generalist care might have on the ability of specialists and subspecialists to maintain their skills. A final unknown is whether older, more expert specialists would or would not be more attractive to managed care systems and what effects the employment or contracting practices of these networks would have on physician incomes.
In the end analysis, whether trends in physician income can tell us anything useful about the supply of physicians in generalist or specialist practices and about physician preferences for FFS or managed care practice remains unclear. The committee cautions against placing too much reliance on such information.
Other Evidence
Other market factors that might provide insights about the adequacy of the physician supply are changes in the number of unemployed physicians, the interest of college students in pursuing medical careers, and the number of physicians taking early retirement or relocating. PPRC (1995) concluded that none of these indicators has as yet produced evidence of a physician surplus. In its most recent annual report to Congress, PPRC (1995), stated that there is "little evidence, either anecdotal or more systematic, of physicians unable to secure work" (p. 312). In addition, it noted both the record number of applications to medical school in 1994 and the record levels of interest on the part of college freshmen in a career in medicine. Finally, the PPRC was unable to find good data sources by which to track the number of physicians relocating or taking early retirement. The 1995 PPRC report concluded that although some changes have occurred in the labor market for physicians, it is still too early to know whether they signal a departure from previous trends.
Information available to this IOM committee differs from that just summarized above. Committee members have received numerous anecdotal reports of early physician retirements, physician relocations, empty office calendars, and even physician bankruptcies. Most of these come from markets such as Minnesota and southern California in which the growth of managed care has been particularly rapid, and they involve mainly nonprimary care specialists. At least one recently published report confirms these trends (Page, 1994).
CONCLUSION
Most studies of the adequacy of the physician workforce for the past 15 years have concluded that the United States has an oversupply of physicians, generally characterized as a large surplus of most nonprimary care specialists and either a shortage or a relative balance in the supply of primary care physicians. Marketplace evidence supporting these findings is at present inconclusive.
The committee was not unanimous in labeling the current number or stock of physicians as an absolute oversupply or excess, for two reasons. First, on theoretical grounds, the need or demand for physicians is better understood as requirements for physician services. Second, the idea that a surplus exists (or does not) is best settled in the context of explicit assumptions about the goals and characteristics of the health care system now (and in the future) and about different ways in which those goals might be met.
Rather, the committee concluded that the nation clearly has at present an abundant supply of physicians—which some members of the committee were prepared to label a surplus—and that judgments about the implications of those
numbers must be made in the context of the overall U.S. health care system and the components of that system that are of greatest concern (e.g., the quality and costs of health care and access to services). It was certainly of the view that the growth in physicians training and entering practice each year is sufficient to cause concern that supply in the future will be excessive, regardless of the assumptions made about the structure of the health care system. Finally, the committee concluded that the steady rise in numbers of physicians coming into practice is attributable primarily to ever-increasing numbers of IMGs, about which it is very concerned.
Two major sets of questions remain, however. Will the current or anticipated numbers of physicians have, on balance, positive or negative consequences for costs, accessibility, and quality of health care in the nation? Will that supply have beneficial or harmful effects on such matters as the efficient use of human resources and the long-term future of the nation's academic health centers? Furthermore, will those judgments differ depending on where on a "tightly managed care" to "fully fee-for-service" spectrum the U.S. health care system settles? These topics are taken up in the next chapter.
NOTES
|
1. |
Figures for the supply of physicians in this country can diverge dramatically, depending on whether the data refer to all physicians, all active physicians, all active nonfederal physicians, patient care physicians, or some other grouping. By most accounts, active physicians are those who are neither retired nor working fewer than 20 hours per week. Different sources will use different classifications, so comparisons across sources may be invalid or at least require further examination. The committee has tried to be explicit about the groupings used in the text and in Table 2-1. |
|
2. |
By convention, allopathic schools are distinguished from osteopathic schools. Allopathic schools produce physicians with a "doctor of medicine" (M.D.) degree; osteopathic institutions graduate those with a "doctor of osteopathy" (D.O.) degree. The former greatly outnumber the latter, today by about 126 to 16 schools. |
|
3. |
Reporting of the number of physicians differs somewhat across the period 1970–1992. Sources include DHEW (1977), NCHS (1983), and DHHS (1993). |
|
4. |
Some observers (e.g., Sheldon, 1991; Jonasson et al., 1995) believe that, for some physician categories such as general surgery, the GMENAC (1981) report estimates were off the mark because it projected the training of more surgical residents than actually have been trained. COGME (1994) also comments on shortages in several specialties, including general surgery, psychiatry, preventive medicine, and geriatrics. Consequently, the question of a significant excess of surgeons (or at least general surgeons) may be more debatable than it is for certain other subspecialties. Apart from the issue of numbers, however, lies the question of whether existing methods for predicting supply or requirements are equally appropriate across all types of physician specialties (or, indeed, across all types of health care personnel). |
APPENDIX
A Brief Note on Managed Care
The IOM committee was not charged to examine issues relating to managed care. However, the transformation of the U.S. health care system and the rapid movement toward managed care structures are of signal importance in understanding the impact of physician supply in the future and in considering the impact of managed care on physician requirements. Thus, the committee was motivated to comment on the phenomenon, and this appendix provides a very brief overview of the factors the committee tried to take into account.
Experts disagree on the definition and inclusiveness of managed care. At its broadest, managed care plans might be considered to involve some or all of the following features: complex organizational arrangements (e.g., among institutions and clinicians); more explicit financial incentives for both providers and members or enrollees than is typical in a fee-for-service (FFS) arrangement; coordination and integration of services; defined access to the physician panel and/or services; strong controls on utilization, especially of specialists; and accountability for an enrolled population and for quality of care. One useful description is that of Iglehart (1994, p. 1393): managed care plans "… integrate the financing and delivery of medical care through contracts with selected physicians and hospitals that provide comprehensive health care services to enrolled members for a fixed predetermined fee."
In most people's minds, managed care can include traditional staff-and group-model HOMs, IPAs, and PPOs (which may involve tightly bound arrangements that render them exclusive provider organizations [EPOs]). Managed care also comprises a variety of so-called point-of-service (POS) plans, which offer incentives for patients to use the panel of physicians belonging to the plan but cover some fraction of the costs of use of out-of-plan physicians.
Whether physicians are salaried employees of the plans, or have capitated contractual arrangements with plans, or are reimbursed on a FFS basis, complicates the task of cleanly defining managed care. For example, HMOs and similar managed care entities might be classified into (at least) five levels of capitation, involving hospital care, primary care, hospital-based specialties (such as anesthesia or laboratory medicine), medical specialties, and surgical specialties. HMOs may capitate most frequently for the first two categories and then contract out, in a wide array of patterns, for the other types of specialty services, often on a volume-based adjusted FFS basis. Thus, in the words of one committee member: "If you have seen one HMO, you have seen one HMO."
Generally, the growth in managed care arrangements today appears to be in PPO- and POS-type networks. Reporting on findings from the 1993 Robert Wood Johnson Foundation Employer Health Insurance Survey (which covered
more than 20,000 employers in 10 states), Cantor et al. (1995) indicated that, among all employees of these firms, 54 percent were offered indemnity plans, 48 percent a PPO plan, and 45 percent an HMO. With respect to the firms themselves, the figures for types of plan offered were, respectively, 55, 38, and 25 percent across the states studied. Gabel (1995) indicated that in 1994, 25 percent of people insured were in HMOs, 25 percent in PPOs, 15 percent in POS plans, and only 35 percent in traditional indemnity plans; he also stated that among employed individuals who have a choice between managed care and traditional FFS insurance, the proportion choosing PPOs and POS plans increased between the mid-1980s and 1994.
Because cost constraints in PPOs and POS arrangements may be weaker than those in traditional HMOs and EPOs (i.e., they may more closely resemble those operating in the FFS sector), the otherwise expected effects of managed care on utilization and expenditures may be dampened. This factor complicates any analysis of the relationships between physician supply and costs of care in an increasingly managed care world. (For further discussions of these issues, readers are referred also to PPRC, 1995, and ProPAC, 1995.)


























