Appendix A
Demographic Overview and State of the Data
From a demographic standpoint, a study of the mortality and morbidity of females in Sub-Saharan Africa is a difficult task. The lack of data on cause-specific mortality and morbidity, particularly data disaggregated by gender, is a recurrent theme throughout this report. Although African countries have made considerable advances in expanding their demographic data bases, data of the kind needed for this book are scanty. Data are almost nonexistent for females of certain age groups, and for both males and females for a number of diseases and conditions. The data that do exist are from scattered sources, most of which are subject to underreporting or other sources of bias. In general, researchers are just beginning to construct a composite picture of mortality and morbidity of females over the course of their lifetime in Sub-Saharan Africa. This composite picture combines information from varying sources of data, but still suffers from large gaps; in addition, details of specific regional and local variations are rarely available.
This appendix reviews the nature of the evidence on female mortality and morbidity in Sub-Saharan Africa, while recognizing the limited sources and reliability of the available data. It presents current levels and trends in female mortality and morbidity and highlights gaps in the information. In view of the scarcity of available data, the appendix is also prescriptive, suggesting areas that require more data for a better understanding of female health.
DATA ON FEMALE MORTALITY AND MORBIDITY ACROSS THE LIFE SPAN
Data on Mortality
Sources and Measures
Demographers have long incorporated a life span perspective in data collection and analysis through either cohort measures or measures based on stable populations that reflect the fertility or mortality experience of a birth cohort as it ages. Most common is the use of a synthetic cohort, where fertility or mortality is expressed as the level that would be experienced by a cohort of males or females living through the age-specific rates prevailing at a given time. The key to this approach is the availability of age-specific rates. Life expectancy at birth is a measure that summarizes mortality experience throughout the life span.
Age-specific rates are traditionally based on vital registration data, providing numbers of deaths by age, sex,
and cause of death; and on census data, providing age and sex-specific ''denominator" data. Vital registration data in Africa are scanty, however. Sub-Saharan Africa lacks vital registration systems (with the exception of Mauritius and South Africa) that even approach the United Nations standards for completeness.
Another traditional source of information on mortality and morbidity is based on the health care services, but this information is of limited use in Sub-Saharan Africa. One reason for this is that the majority of deaths occur outside the health care system. Another is that health care service information is usually restricted to inpatients in tertiary facilities, and there are substantial selection biases among the populations that use these health services, reflecting, for example, differentials in access to health services according to age, gender, and geography or a higher level of risk among those utilizing the services. Access may be lower, for instance, in young teenage groups or in rural areas (Graham, 1991; Timaeus, 1991d). Only a small proportion of women at risk in Sub-Saharan Africa have access to hospitals (Graham, 1991). Much of the health care provided to the African population is through smaller, community-based primary health care services (Ewbank, 1988), and evidence suggests that deaths among patients in contact with these facilities tend to be omitted in health service statistics because of incomplete recordkeeping (Graham, 1991).
Since the 1960s, demographic data have improved substantially. Censuses and surveys, described below, have filled some of the statistical needs traditionally met through vital registration data. Most important to the current level of knowledge about African mortality, however, has been the development of survey instruments and methodologies to measure mortality through specific retrospective questions asked of a mother or other family member about births and deaths, which can be included in a census or survey. These questions, described below, result in estimates of mortality over a broad age group. Indicators most often used are the probability of survival from birth to exact age 5, and the conditional probability of survival from age 15 to age 50. The estimates thus reflect "partial lifetime" mortality over a substantial age period. The mortality measures refer to the time period over which the deaths occurred, although greater weight is generally given to the information from more recent deaths. Expert matching of these estimates with model schedules of mortality, developed on the basis of mortality experience over a broad range of countries and time periods, can be used to estimate life expectancy at birth.
The above methodology is most developed for the estimation of mortality among infants and children, which includes the majority of deaths in a developing country. Estimates are based on a mother's retrospective reporting of her fertility history, or a question on the number of children ever born and the number of children surviving to the time of the survey (UN, 1983). These measures also provide limited information on mortality over time. Information on survival between birth and age 5 within the two to three years immediately prior to the survey is generally considered the most accurate. Limitations of the method include probable understatement of birth and death events recalled from the past, inclusion of fostered and adopted children, and decreasing accuracy of reporting as overall numbers of births and childhood deaths decline. Whether there is a selective underreporting of female versus male deaths through use of these measures is uncertain.
Procedures to estimate adult mortality are still being developed and refined, spurred on by more recent recognition that child and adult mortality are not as closely associated as had been thought; thus, traditional methods of estimating adult mortality based on child mortality are no longer considered accurate. The most direct approach—to ask about deaths in a household in a fixed previous time period—has not proved very useful in developing countries, because it requires large sample sizes to yield sufficient numbers of observations. Indirect methods have been more successful. These methods include, for example, the widowhood and orphanhood methods (Timaeus, 1991a,b,c; UN, 1983) and the sisterhood method (Graham et al., 1988, 1989). Such methods are based on questions that ask the respondent about survival of close relatives. Estimates are converted to survival probabilities across an age span, often ages 15–60, based on assumptions about past age patterns and trends of fertility and mortality. Widowhood questions have not been as widely used in Africa as orphanhood questions, because the former require a greater number of respondents to obtain accurate estimates. Sisterhood methods are fairly recent developments and, as such, are still being evaluated, but early field trials are encouraging (Graham, 1991; Trussell and Rodriguez, 1990). Orphanhood questions may underestimate mortality for theoretical reasons, as well as because of adoption, where respondents may refer to surviving stepparents or foster parents, rather than to early mortality of the biological parents. The impact of the adoption effect is possibly greater on reporting about mothers than about fathers, which may underlie the relatively steep declines noted in female
compared with male adult mortality (Timaeus, 1991d). Mortality estimates may also be biased by other reporting errors, such as age misstatements or omissions.
During the 1960s, several of the English-speaking countries initiated efforts in census data collection, and a major impetus was provided by the African Census Program in the 1970s, when 22 countries undertook census activities. A majority of Sub-Saharan African countries also undertook censuses in a 1980s round (de Graft-Johnson, 1988). Many of these efforts, however, did not include the kinds of indirect mortality measures described above, which would allow for robust estimates of mortality.
A number of Sub-Saharan African countries have conducted national and subnational household demographic surveys under internationally sponsored programs in an attempt to gather reliable demographic data —for example, the World Fertility Surveys (WFS), Contraceptive Prevalence Surveys (CPS), Demographic and Health Surveys (DHS), and a socioeconomic survey, the Living Standards Measurement Studies (LSMS). Demographic Health Surveys have now been conducted in 25 countries in Sub-Saharan Africa. These surveys have provided the bulk of the information that allows for more accurate assessment of mortality rates.
In addition to these efforts, a limited number of small-scale community studies have been conducted in various sites of Sub-Saharan Africa that provide fairly high-quality information on mortality and selected aspects of morbidity. Such studies have been conducted in Kenya (Machakos), The Gambia (Keneba), Ghana (Danfa), Nigeria (Malumfashi), Senegal (Niakhar, Bandafassi, Mlomp), and Burkino Faso (Kongoussi) among other sites (Feachem et al., 1991; Gbenyon and Locoh, 1989). These studies generally utilize population-based surveillance systems or multiround surveys. Such frequent contacts with a household over a number of years substantially improve the accuracy of data collection, but the intensive effort required limits the total number of households that can be surveyed.
Even with these useful additions, however, the availability and quality of survey data on mortality in the region, particularly by gender, are limited, and they differ according to the age category and disease examined. In part, the information collected reflects the focus of concern in the region. For example, high fertility levels and high infant and child mortality levels—compared with the rest of the world —have long been predominant causes of concern in Sub-Saharan Africa. It is not surprising, therefore, that the WFS concentrated on women in the reproductive ages at the time of the survey, and thus provided substantial data primarily on marital fertility and infant and child mortality. The DHS, in turn, has an expanded focus on health-related behaviors related to child mortality, nutrition, and morbidity, but provides little or no information on adult mortality. The longitudinal surveys mentioned above have focused on specific diseases such as malaria, measles, or schistosomiasis, or on malnutrition, and their fairly small size requires years of surveillance before reliable adult mortality information is acquired.
Based on these sources, a partial picture of mortality and cause of death in Sub-Saharan Africa can be constructed, but significant gaps in the life span remain. For example, because of low mortality rates in the ages between 5 and 15 years, even in developing countries, virtually nothing is known about health conditions in these ages for either males or females. The focus on reproductive age women has provided little information on health conditions related to chronic and degenerative disease. The relative infrequency of a maternal death compared with child death has posed a serious obstacle to collection of accurate information on maternal deaths in a survey format.
For cause of death, data on children are more complete than those for adolescents and adults. One reason for this is that it is easier to collect on child mortality through surveys, given the large proportion of children in the population, their high mortality rates, and the characteristic clinical presentation of many childhood diseases. By far the largest proportion of infant and childhood deaths in Africa, for example, is caused by about a half-dozen infectious and parasitic diseases, including measles, diarrhea, respiratory infections, and malaria. These are acute conditions with relatively short durations that are relatively easy to diagnose, even by lay observers. Adult death,, in contrast, tend to be caused more often by chronic diseases with more obscure clinical manifestations and, as a result, are more difficult to diagnose accurately. Thus, data on cause of death in the older age categories are generally less complete and accurate.
In many studies, causes of death are assigned on the basis of retrospective reports from untrained observers, usually members of the deceased's family. These "verbal autopsy" methods are only reliable for the easily
recognized causes that form a large proportion of all deaths in a given age group (Ewbank and Gribble, 1993). There have not been any evaluations of these methods for estimating causes of adult mortality. It is unlikely, however, that these methods will prove reliable for most causes of death among adults, especially if attempts are made to disaggregate cardiovascular disease and cancers. A possible exception to this is the diagnosis of "maternal causes" related to pregnancy and childbirth.
As data sources in Sub-Saharan Africa expand, the variation in mortality levels, trends, and causes of death among countries is becoming more evident. As a result, the traditional composite picture of mortality in the region no longer holds.
Gender Differences in Mortality
There are few data available for Sub-Saharan Africa that permit age-specific comparisons of mortality rates by gender for anything less than very wide age groupings. Therefore, comparisons from Europe and North Africa are presented here because they may be broadly informative.
Henry (1989) reviewed the European historical evidence on gender differentials in mortality. Most of the life tables he examined showed higher rates in females than in males aged 25 to 44 years in populations where fertility rates were higher than average. This excess is largely explainable through maternal mortality. At younger ages, the picture is less clear. Excess female mortality was common in some or all age groups between 5 and 19 years of age in most European countries at some point in the nineteenth century. This pattern of excess mortality in female children and adolescents, however, is not as pronounced in life tables after the nineteenth century. The reasons for this shift remain unexplained.
Figures A-1 and A-2 demonstrate the gender differentials in mortality over age 1 in Algeria and Tunisia around 1970 and in the mid-1980s. In 1968–1969, there was excess mortality among females in Tunisia at ages 1–4 and 25–44 years. By 1984, there was only a small amount of excess female mortality at ages 10–14 years. In Algeria, there was excess female mortality at ages 1–24 years in 1970, but by 1988 there was only slight excess among female children at ages 1–4 and adult females aged 25–29 years. The excess mortality among females, where it exists, is often largest proportionally during the childbearing years. Mortality rates at these ages, however, are relatively low in all populations. Excess female mortality among infants and children is often less proportionally, but it can be large in absolute terms because of the relatively high mortality rates under age 5.
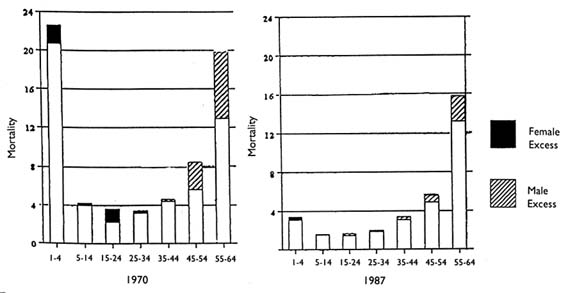
FIGURE A-1 Sex differentials in mortality by age, Algeria, 1970 and 1987.
SOURCE: Tabutin, 1992, p. 204.
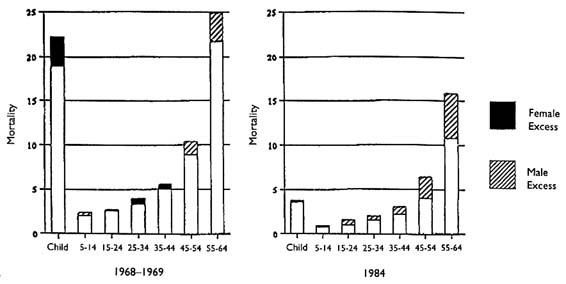
FIGURE A-2 Sex differentials in mortality by age, Tunisia, 1968–1969 and 1984.
SOURCE: Tabutin, 1992, p. 205.
The data on gender differences in mortality by age in Sub-Saharan Africa are available for only very broad age groupings, and these indicate that mortality differences are small, and in most cases favor girls (Rustein, 1984; Timaeus, 1993). Less is known about gender differentials in adolescent and adult mortality, although aggregate estimates for the ages 15 to 60 years suggest that the favorable mortality experience in the female child continues through adulthood. These limited findings, coupled with the evidence from Europe and North Africa cited above, suggest that if there is significant excess female mortality in Sub-Saharan Africa, it is likely concentrated in the reproductive years.
Levels of Mortality
Table A-1 presents estimates of mortality under age 5 for countries in Sub-Saharan Africa and for North Africa. The estimates in Sub-Saharan Africa range from 47 deaths age 5 per 1,000 live births (females in Botswana) to 281 per 1,000 (males in Mali). These estimates for Sub-Saharan Africa, with the exception of those for Togo, do not demonstrate the excess female child mortality observed for Egypt and Tunisia. If child mortality is broken down into specific age groups, however, significant differences are shown in the level of female advantage by age. Among infants, particularly among neonates, where death is largely determined by birthweight and congenital conditions, males are reported to have higher mortality rates than females, as is observed throughout the world. At ages above 1, however, where mortality is much more likely from infectious and parasitic disease, the levels are far more equal. Female, however, still enjoy a slight advantage in most Sub-Saharan countries (Gbenyon and Locoh, 1989).
Table A-2 presents estimates of adult survival for countries of Africa. Despite efforts to pull together all available data, these estimates are somewhat out of date, and describe only about 40 percent of Sub-Saharan Africa's population, excluding some major countries such as Nigeria, Ethiopia, and Zaire. The estimates are judged to be of very low to fair reliability, because they are based primarily on retrospective questions about adult deaths in censuses and surveys, and are subject to underreporting of deaths and to reporting biases, and often demonstrate inconsistency between sources when more than one source is available.
The estimates in the table demonstrate a wide range in levels of survival, although among sources judged to be of fair reliability, the data indicate that approximately 75 percent of 15-year-olds can expect to reach their 60th birthday under the level of mortality that prevailed in the 1970s and 1980s. In selected countries, the data indicate
TABLE A-1 Summary of Infant and Child Mortality Differences by Gender, African Countries, World Fertility Surveys and Demographic and Health Surveys
|
Region/Country |
Year |
Males |
Females |
Male Excess |
|
Sub-Saharan Africa |
||||
|
Benin |
1981 |
240 |
215 |
25 |
|
Botswana |
1988 |
65 |
47 |
18 |
|
Burundi |
1987 |
190 |
181 |
9 |
|
Cameroon |
1978 |
139 |
121 |
18 |
|
Côte d'Ivoire |
1980 |
219 |
184 |
35 |
|
Ghana |
1979 |
139 |
121 |
18 |
|
Ghana |
1988 |
160 |
147 |
13 |
|
Kenya |
1978 |
158 |
145 |
13 |
|
Kenya |
1989 |
96 |
85 |
11 |
|
Lesotho |
1977 |
188 |
169 |
20 |
|
Liberia |
1986 |
242 |
216 |
26 |
|
Mali |
1987 |
281 |
277 |
4 |
|
Mauritania |
1981 |
192 |
185 |
7 |
|
Namibiaa |
1992 |
94 |
89 |
5 |
|
Nigeriaa |
1981 |
170 |
156 |
14 |
|
Nigeriaa |
1990 |
200 |
182 |
19 |
|
Senegal |
1978 |
278 |
265 |
13 |
|
Senegal |
1986 |
215 |
202 |
13 |
|
Sudan |
1989 |
140 |
130 |
10 |
|
Tanzaniaa |
1991 |
160 |
147 |
14 |
|
Togo |
1988 |
156 |
162 |
-5 |
|
Uganda |
1988 |
197 |
179 |
18 |
|
Zambiaa |
1992 |
188 |
168 |
20 |
|
Zimbabwe |
1988 |
93 |
81 |
12 |
|
North Africa |
||||
|
Egypt |
1980 |
208 |
222 |
-14 |
|
Egypt |
1988 |
129 |
135 |
-5 |
|
Morocco |
1980 |
153 |
148 |
5 |
|
Morocco |
1987 |
118 |
117 |
1 |
|
Tunisia |
1978 |
119 |
120 |
-2 |
|
Tunisia |
1988 |
76 |
74 |
2 |
|
a Recent DH country report data. SOURCE: Calculated from Hill, 1991, and recent DHS country reports. |
||||
that less than 60 percent survive to their 60th year, a substantial differential from the above, but the quality of data for these countries is judged to be fairly low.
The data indicate somewhat more favorable levels of survival in adult women compared with adult men for most countries in the region. Only Mali and Malawi have estimates that suggest a female excess in the proportion dying between ages 15 and 60. As a comparison, estimates for the North African countries of Tunisia and Algeria for specific time periods in the 1960s through the 1980s do reveal excess female mortality at some ages. Nevertheless, overall mortality at ages 15 to 60 is higher for males in both countries at all time periods. Since mortality rises rapidly with age after age 40, any excess female mortality under age 40 may be counterbalanced in aggregate mortality measures by excess male mortality at ages 40–60, where the mortality rates are higher.
Socioeconomic Differences There is substantial evidence that factors such as education and, to a lesser extent, occupation and income have a potent influence on child mortality. Much less is known, however, about the
TABLE A-2 Survivorship from Age 15 to Age 60 by Sex, 1970s and 1980s
|
Region and Country |
Date |
45P15 Males |
Females |
Both Sexes |
Reliability |
Source |
|
Western |
||||||
|
Benin |
1978 |
749 |
779 |
764 |
Very low |
Orphanhood |
|
Côte d' Ivoire |
1978–1979 |
646 |
741 |
694 |
Fair |
Multiround survey |
|
The Gambia |
1978 |
773 |
812 |
793 |
Fair |
Intercensal orphanhood |
|
Ghana |
1982 |
778 |
880 |
830 |
Low |
Orphanhood since marriage |
|
Liberia |
1970–1971 |
550 |
584 |
567 |
Fair |
Multiround survey |
|
Mali |
1986 |
579 |
541 |
560 |
Low |
Recent deaths and orphanhood |
|
Mauritania |
1980 |
782 |
823 |
803 |
Fair |
Orphanhood and recent deaths |
|
Senegal |
1978 |
652 |
710 |
682 |
Fair |
Multiround surveys |
|
Sierra Leone |
1974 |
466 |
510 |
488 |
Very low |
Orphanhood |
|
Togo |
1981 |
704 |
760 |
733 |
Very low |
Recent deaths |
|
Middle |
||||||
|
Cameroon |
1976 |
644 |
666 |
654 |
Low |
Recent deaths and orphanhood |
|
Congo |
1984 |
656 |
703 |
680 |
Very low |
Recent deaths and orphanhood |
|
Eastern |
||||||
|
Burundi |
1981 |
622 |
699 |
661 |
Low |
Orphanhood since marriage |
|
Kenya |
1974 |
714 |
769 |
742 |
Fair |
Intercensal orphanhood |
|
Madagascar |
1974–1975 |
487 |
551 |
518 |
Very low |
Recent deaths |
|
Malawi |
1977 |
741 |
706 |
723 |
Low |
Intersurvey orphanhood |
|
Rwanda |
1978 |
584 |
629 |
607 |
Low |
Recent deaths |
|
Tanzania |
1988 |
656 |
675 |
666 |
Very low |
Recent deaths and orphanhood |
|
Zimbabwe |
1978 |
801 |
863 |
833 |
Very low |
Orphanhood |
|
Southern |
||||||
|
Botswana |
1980 |
555 |
732 |
646 |
Low |
Recent deaths |
|
Lesotho |
1976 |
503 |
749 |
627 |
Fair |
Recent deaths and orphanhood |
|
South Africa |
1985 |
638 |
766 |
702 |
Fair |
Vital registration |
|
Swaziland |
1981 |
561 |
761 |
663 |
Fair |
Intercensal orphanhood |
|
Northern |
||||||
|
Sudan (northern) |
1975 |
695 |
768 |
732 |
Fair |
Orphanhood and widowhood |
|
SOURCES: Data from Benin (Benin, n.d.); Côte d' Ivoire (Ahonzo et al., 1984); The Gambia (Blacker and Mukiza-Gapere,1988); Ghana and Senegal (Timæus, 1991d); Liberia, Madagascar, andRwanda (Waltisperger and Rabetsitonta, 1988); Mali (Mali, 1980 andprovisional 1987 census tables); Mauritania (Timæus, 1987); SierraLeone (Okoye, 1980); Togo (Togo, 1985); Cameroon (Cameroon, 1978,1983); Congo (Congo, 1978, 1987); Burundi (Timæus, 1991c); Kenya(Mukiza-Gapere, 1989); Malawi (Timæus, 1991b); northern Sudan (Sudan,1982); Tanzania (Tanzania, 1982 and provisional 1988 census tables);Zimbabwe (Zimbabwe, 1985); Botswana (Botswana, 1972, 1983); Lesotho(Timæus, 1984); South Africa (South Africa, 1988); Swaziland (Swaziland,1980 and unpublished 1986 census tables). Reprinted from Timæus, 1993, p.222, in Foote et al., 1993. |
||||||
relationship of socioeconomic factors to differentials in adult mortality. Timaeus (1993) cites data suggesting that adult female life expectancy in the Sub-Saharan African region in the mid-1970s was related to GNP per capita and secondary-school enrollment, although he notes that neither index alone is strongly predictive of adult survivorship.
Urban-Rural Differences Data suggest that adult mortality is lower in urban Africa than in rural Africa. This observed differential is larger in countries with high mortality rates, and this may indicate that the survival advantage of urban areas decreases as overall mortality declines. The generally lower mortality rates observed in urban Africa must, however, conceal pockets of poverty and high mortality among urban dwellers. In general, national and rural adult mortality estimates vary more among Sub-Saharan African countries than those of urban mortality (Timaeus, 1993). There are no available data on urban-rural differences in mortality disaggregated by gender.
Trends in Mortality over Time
Several studies have documented improvement in child mortality levels in Sub-Saharan Africa over the decades since World War II (see, for example, Hill, 1991; Hill and Pebley, 1989; Hill and Yazbeck, 1994). Sub-Saharan Africa has higher overall levels of child mortality than other regions, but shows similar absolute declines in these rates over time. Hill (1991) notes that in many African countries, during the 1950s, 30 to 40 percent of children died by the age of 5, and in only a few countries did less than 22 percent die. By the 1970s, few countries lost more than 27 percent, and many lost less than 22 percent of children under age 5. A breakdown of these figures by gender is not available.
Figure A-3 demonstrates the improvement in the life expectancy of adult females in a set of 15 mainland Sub-Saharan African countries (Timaeus, 1993). A comparison by region demonstrates that all western and middle African countries included in Figure A-3 experienced a rapid decline in adult female mortality for the time periods examined. Four countries—the two southern states for which data are available (Lesotho and Swaziland), northern Sudan, and Kenya —demonstrated only small gains in adult female survivorship in the 1960s and 1970s. These are also the four countries that had the lowest estimated mortality rates for females in the early 1960s. The other eastern African countries included in Figure A-3 had more rapid declines in female mortality (Timaeus, 1993). Although the methods of data collection and calculation underlying these estimates are subject to error, these data indicate a strikingly consistent improvement in female survivorship in the 1970s. Whether this trend has continued to date, and at what pace, is uncertain.
Cause-Specific Mortality Across the Life Span
Although sparse overall, much more evidence has accumulated on cause of death among children than among adults. This information is primarily available from population surveillance systems, hospital records, and vital registration. Although profiles of cause of death for the region as a whole have been published (for example, World Bank, 1993), these profiles are carefully constructed from the few small-scale studies that have been done in this region. The number of deaths in such studies is usually small, and the estimates are subject to many kinds of error and bias, so their results must be interpreted with caution.
Childhood Studies of cause of death among children culled from approximately 12 study sites in Sub-Saharan African are reviewed in two sources (Ewbank and Gribble, 1993; Feachem and Jamison, 1991). Infant and child mortality are dominated by a set of causes including acute respiratory infection (ARI), diarrhea, and measles, and in several areas, malaria. Low birthweight, tetanus, and birth trauma are important causes associated with neonatal mortality. Thus, the childhood mortality experience in Sub-Saharan Africa is similar to that in other countries in the predominance of ARI and diarrhea. What is unique to Africa, however, is the impact of malaria and measles. As noted earlier, gender differentials among all causes of death generally reveal a small advantage for female over male children. Malaria and measles are exceptions, however: fairly high-quality evidence from longitudinal studies indicates that young females have a greater likelihood than males of dying from either malaria or measles
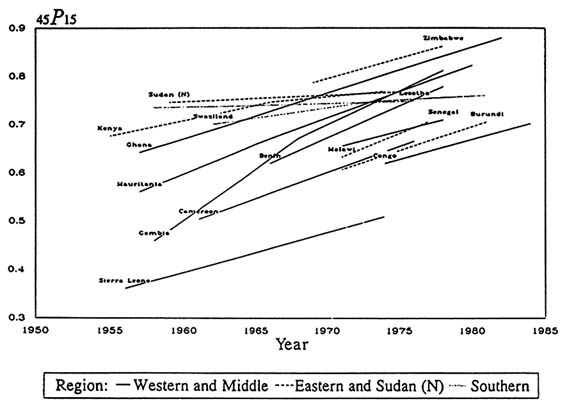
FIGURE A-3 Trends in female survivorship from age 15 to age 60.
SOURCES: Data from Benin (Benin, n.d.); Côte d'Ivoire (Ahonzo et al., 1984); The Gambia (Blacker and Mukiza-Gapere, 1988); Ghana and Senegal (Timaeus, 1991c); Liberia, Madagascar and Rwanda (Waltisperger and Rabetsitonta, 1988); Mali (Mali, 1980, and provisional 1987 census tables); Mauritania (Timaeus, 1987); Sierra Leone (Okoye, 1980); Togo (Togo, 1985); Cameroon (Cameroon, 1978, 1983); Congo (Congo, 1978, 1987); Burundi (Timaeus, 1991a); Kenya (Mukiza-Gapere, 1989); Malawi (Timaeus, 1991b); northern Sudan (Sudan, 1982); Tanzania, (Tanzania, 1982, and provisional 1988 census tables); Zimbabwe (Zimbabwe, 1985); Botswana (Botswana, 1972, 1983); Lesotho (Timaeus, 1984); South Africa (South Africa, 1988); Swaziland (Swaziland, 1980, and unpublished 1986 census tables). Reprinted from Timaeus, 1993, p. 231, in Foote et al., 1993.
(see, for example, Chapter 10, and Fargues and Nassour, 1988). Causes for this differential are still being investigated. Much of the information on cause of death is from small-scale community studies; although they provide high-quality information, they yield little information on the representativeness of the findings. Thus, further work to identify the causes of death among children over a wider geographic area would be useful.
Adulthood Timaeus (1993) presents cause-specific data for adults within broad age groups from four small studies in Cape Verde, Mali, western Sierra Leone, and South Africa. For females, the risk of death in the age group 15–44 from communicable and reproductive diseases ranges from 13 to 72 per 1,000, the highest risk being in western Sierra Leone. Risk from communicable and reproductive disease is about half to two-thirds the level of risk from noncommunicable disease (except in Sierra Leone, where they are equal). For both sexes, cardiovascular disease is the leading cause of death within the age group 45–64, followed by neoplasm and digestive disease. The risk of death from injury is fairly small compared with the other major categories, but varies from 5 to 26 per 1,000 across the four sites. Data suggest that gender differentials in cause-specific mortality are generally small, particularly in the age group 15–44 years and for noncommunicable diseases, because among younger adults, higher mortality among males from injury and digestive disease is offset by deaths from maternal causes among
females. It should be noted, however, that this information is, again, not representative of Sub-Saharan Africa. The widely varying profiles across sites suggest that much further work on identifying causes of death among adults is necessary to obtain a composite picture that inspires any degree of confidence.
Mortal Conditions of Special Note Two major causes of female mortality in Sub-Saharan Africa deserve special note because of their profound adverse impact on mortality trends, not only for females themselves, but also for the many others around them who depend on their care. These two causes are maternal mortality and HIV/AIDS. As documented in Chapter 4, maternal mortality rates in Africa are higher than anywhere else in the world. In Sub-Saharan Africa, 150,000 women a year die of maternal causes, about one every 3.5 minutes. If, on average, a woman in Africa has six children during her lifetime (World Bank, 1992), and women who die in their reproductive years leave an average of two or more children (Herz and Measham, 1987), such mortality would leave nearly a million children motherless each year.
Evidence presented in Chapter 4 indicates significant variability in maternal mortality ratios among countries of Sub-Saharan Africa, with a high of 2,900 deaths per 100,000 live births in Mali and a low of 77 deaths per 100,000 live births in Zimbabwe. Five of the 33 countries for which data are available have ratios of over 1,000 deaths per 100,000 live births, over a hundred times the mortality ratio in the United States (Rosenfield, 1989), and only 12 have ratios under 200 deaths per 100,000 live births.
Within countries, certain categories of females are at greater risk than others. A very early first birth increases a woman's risk of dying from pregnancy-related causes. Women ages 15–19 face a 20 to 200 percent greater risk of pregnancy-related death than older women, and the younger the adolescent, the higher the risk (WHO, 1989). In Nigeria, for example, women under 15 were found to be 4 to 8 times more likely to die of pregnancy-related conditions than those 15 –19 (Harrison and Rossiter, 1985); data from Ethiopia indicated that teenage women were twice as likely to die from pregnancy-related conditions than were women ages 20–24 (UN, 1989). In sum, pregnant adolescents have a higher likelihood of pregnancy-related complications and consequent risk of pregnancy-related mortality than women further along in their reproductive years; the risk rises again toward the end of those years.
Unlike maternal mortality, analyses of adult mortality, based on retrospective questions about adult survival, do not yet capture the growing role of HIV/AIDS in the mortality profile of Sub-Saharan Africa because of its long period from infection to death and its rapidly increasing incidence over the past decade. HIV may show an increasingly adverse effect on women in Sub-Saharan Africa because of its long incubation period, the rapid heterosexual spread of the virus, and the characteristics of the existing social structure in Sub-Saharan Africa, which may exacerbate the vulnerability of females to infection by HIV (see Chapters 2 and 11). Among young females, these problems may be even more important. Seroprevalence studies among STD clinic patients generally show higher overall HIV seroprevalence rates among men than among women, but this is far from universal. Rates are often higher among younger women (ages 15 to 34 years), and seroprevalence rates are rapidly increasing (CIR, 1993a,b; 1994a,b). The increase in seroprevalence rates is mirrored by a concomitant rise in HIV-related mortality. In a recent study in Rwanda, for example, approximately 90 percent of mortality among childbearing urban women was attributed to HIV infection (Linden et al., 1992).
Data on Morbidity
Sources and Quality
Data on morbidity in Sub-Saharan Africa are considerably scarcer and less accurate than those on mortality. Gender-specific morbidity data are available mainly from a few small-scale surveillance projects or from surveys conducted by nonmedical personnel trained to identify diseases with common and easily recognized symptoms.
As with mortality data, the quality of data on morbidity depend on the disease and age category examined. Estimates of the prevalence of observable and clinically distinct illnesses, such as a number of tropical infectious diseases or the childhood diseases, are more reliable than those for diseases that may require laboratory confirmation, such as malaria, or have less specific symptoms or subtle signs, such as most of the chronic diseases and
mental disorders. Estimates of the prevalence or incidence of the diseases in this last category are derived primarily from reviews of hospital-based case series (see Chapter 7), which are highly selective in nature and probably vastly underestimate the true magnitude of disease and disability in the population. This underestimation may have a particularly severe affect for females in Sub-Saharan Africa, because their pattern of accessing and utilizing medical care is generally limited (see Chapter 2).
Estimates of Morbidity
Because available mortality data suggest that females in the region have generally lower death rates than males at any given age—except for the reproductive ages, when women experience excessive mortality from pregnancy and childbirth—efforts to study or address female morbidity across the life span have been limited. Yet a number of studies have demonstrated that although female life expectancy usually exceeds that of males, females more frequently report suffering from chronic diseases that limit their productivity. Analysis of the LSMS for Ghana and Côte d'Ivoire showed, for example, that females had higher rates of self-reported morbidity and substantially higher rates of hospitalization than males (Murray et al., 1992). A prospective study of illness in Kenya also found higher rates of morbidity among females than among males. Murray and colleagues (1992) reported that over the study period 1984–1985, men were ill 20 percent of days, and women 33 to 50 percent of days. Men experienced reduced activity 4 percent of days, while women experienced reduced activity 9 to 13 percent of days.
Disability-Adjusted Life Years
In 1993, the journal Lancet wrote, "Every so often an important piece of new thinking about international public health appears. Investing in Health, from the World Bank, is such a document" (Lancet, 1993). One of the more important contributions of the 1993 World Development Report (WDR) was the estimate developed to measure the burden of disease in populations, that of the "disability-adjusted life year" (DALY) (World Bank, 1993).
It is broadly agreed that the DALYs presented in the World Development Report, particularly those for Sub-Saharan Africa, are subject to limitations, given the availability and quality of the epidemiologic data and the sensitivity of the underlying assumptions.1 DALY estimates, for example, were not available disaggregated by regions within Sub-Saharan Africa. Data available to derive estimates for Africa, in particular, were by necessity based on little more data than is described here. The chapters in this report, therefore, with one exception, use original data for comparisons rather than DALY estimates. The DALY construct, however, is strongly supported by the committee presenting this report, because it provides a global comparative means for estimating the lifetime burden of disease and disability and, as such, for better understanding how disease determinants and their outcomes influence health across the human life span and across continents. The contribution of the WDR in this respect is novel and important, and attempts to improve the estimation of DALYs and to identify other measures of lifetime disease burden are encouraged.
Understanding Mortality and Morbidity Across the Life Span
Demographic data collection in the past has yielded substantial information regarding infant and child mortality in Sub-Saharan Africa, and more recently it has begun to yield aggregate information about the probability of survival across the middle of the life span, ages 15 to 60. Morbidity data collection, however, with its focus on specific diseases, has not yet encompassed a life span perspective, except perhaps in early childhood, when the combined effect of infectious and parasitic disease and nutritional status have been examined together. Thus, a composite picture of disease and disability by stages of the life span remains limited to only pieces of the puzzle.
Available data indicate that males suffer more of a health disadvantage at infancy than females, but that by childhood ages, health risks are more equal. If there is an overall female disadvantage at this stage of the life span, it is very small.
A majority of health concerns in Africa begin to surface during the early school years, adolescence, and the teen years. Information on STDs and HIV, early pregnancy, and safe abortion, which have a lifelong impact on the health of females, is becoming more available, but a comprehensive and representative picture remains elusive. In the early adolescent and middle teen years, deleterious lifestyle behaviors begin and take hold, and many of these, such as cigarette smoking (see Chapter 7), are known to adversely affect adult health status. Information that characterizes this process and documents the adoption and prevalence of these behaviors in females in Sub-Saharan Africa, as in males, is not yet being systematically collected.
In the adult reproductive years, little is known about how diseases and disease determinants interact, or how they cumulatively or perhaps synergistically influence health status during the later adult years. Estimates of the proportion of female deaths attributable to maternal conditions compared with other health conditions, for example, often rely on a simple indicator of deaths within certain age groups (for example, the years of fertility), and these estimates vary widely among sites and data sources. The relationship among these diseases is thus poorly defined and reveals little about the relationship of reproductive health with overall female health (see Chapter 4). More recent emphasis on adult mortality is now producing estimates on aggregate risk of death during adulthood. Little is known, however, about major causes of death among older females or males in Sub-Saharan Africa that are known to predominate among adults in other regions of the world. Cancer registries are not well developed, and little information is available on either incidence or prevalence of cardiovascular diseases, chronic obstructive pulmonary diseases, or other noncommunicable diseases believed to affect women in the region (see Chapter 7).
Mortality rates, both cause-specific and in the aggregate, are imperfect indicators of morbidity, and data on morbidity for most age groups, as indicated above, remain limited. Information on the prevalence of disease determinants (risk factors) or on disease cofactors is also absent.
To achieve a life span perspective, the relationship among diseases, disabilities, and disease determinants at different ages must be better understood, both for females and for males. At this stage, basic representative information on mortality by cause and morbidity prevalence by age group for defined populations is still a necessity. Health service statistics will probably not yield this kind of information over time, given the selective nature of the populations utilizing health services and the uncertainty of available denominator data for comparisons. It is, therefore, more realistic to assume that data from demographic and epidemiologic surveys and studies will fill these gaps.
As noted above, morbidity information, currently collected on a disease-specific basis, cannot yield the information needed for a life span perspective. DALYs have partially circumvented this problem by incorporating dimensions of disability into an aggregate measure; the feasibility of measuring disability in a setting such as Sub-Saharan Africa, however, is an open question. Furthermore, the extent to which the DALY construct can be adapted to adequately reflect health conditions prevalent in developing countries, where the epidemiological transition is at a much earlier stage, is a question that deserves further attention. It is thus clear that further work in both the conceptual and methodological arenas is required for a life span perspective for males and females to come to maturity.
CONCLUSIONS
Although African countries have made considerable advances in expanding their demographic data bases, a composite picture of female (and male) health across the stages of the life span is limited to only pieces of the puzzle. The data that exist are rarely disaggregated by gender and are from scattered sources, most of which are subject to underreporting or other sources of bias. While past demographic data collection has provided substantial information on infant and child mortality, and current efforts have begun to yield aggregate information about the probability of survival across the middle of the life span, ages 15 to 60; morbidity data collection, with its past focus on specific disease conditions, has not yet encompassed a life span perspective. Further understanding of the interrelationships among diseases and disabilities and their longer-term sequelae—coupled with advances in the conceptual and methodologic means of data collection and analysis—will be required for a better understanding of health status and disease risk across the life span.
RESEARCH NEEDS
To obtain the kinds of data that will permit a better understanding of the relationship among diseases, disabilities, and disease determinants across the female (and male) life span, the following is recommended:
-
The continuation and expansion of internationally sponsored surveys to collect information on cause-specific mortality and morbidity is strongly encouraged. These surveys should ensure that all data collected are disaggregated by gender and age, and that methods of data collection and analysis are standardized to the extent possible across surveys to ensure consistent data quality and to permit valid comparisons of findings across regions, populations, and time.
-
Data on causes and prevalence of disabilities should also be collected, because they will allow for more accurate estimates of disease burdens in specific populations.
-
Survey efforts should focus, to the extent possible, on the tracking of defined cohorts of individuals over time, since such propective data can provide not only reliable measures of disease incidence and mortality, but also the best picture of how diseases, disabilities, and future disease determinants interact to influence health over the life span. The use of such ''population laboratories" in the past has provided important contributions to understanding mortality and morbidity dynamics in Sub-Saharan Africa, but the quality of these studies has been uneven. Careful weighing of the costs and benefits of the information to be gained in such surveys will be needed, and survey construction, data collection, and analysis should be more closely coordinated across surveys to maximize survey cost-effectiveness and the comparability and generalizability of survey results.
-
Possible use of sentinel disease surveillance systems as a cost-effective means to identify and monitor changing patterns in mortality and morbidity in populations in stable catchment areas should be investigated. Data from such sources would need to be interpreted with care given the selection biases inherent in the populations tracked, but these data would ideally be supplemented with information from other, more representative, data sources, such as national or subnational household surveys.
-
Development and refinement of health indexes that provide a useful means for evaluating the impact of disease and disability across the life span, such as the DALY, should be strongly encouraged. Efforts toward this end should consider the broad range of health measures used to estimate disease burden (such as DALYs), quality of life (QALYs, for example), and other health indexes currently used for the purposes of resource evaluation and allocation.
NOTE
1. To an extent, the committee shared this view and, as such, decided not to include DALYs in its report. The committee's decision, however, does not reflect a rejection of the methods or approach used by the World Bank to calculate DALYs, but rather a concern about the quality of the supporting evidentiary base for the Sub-Saharan African region.
REFERENCES
Ahonzo, E., B. Barrere, and P. Kopylov. 1984. Population de la Cote d'Ivoire. Abijan: Ministere de l'Economie et des Fiances.
Benin. No date. Enquete sur la Fecondite au Benin. Cotonou: Bureau Central de Recensement.
Blacker, J. G. C., and J. Mukiza-Gapere. 1988. The indirect measurement of adult mortality in Africa: Results and prospects. In African Population Conference, Dakar, 1988, Vol. 2. Liege: International Union for the Scientific Study of Population.
Botswana. 1972. Report on the Population Census, 1971. Gaborone: Central Statistics Office.
Botswana. 1983. 1981 Population and Housing Census: Administrative/Technical Report and National Statistical Tables. Gaborone: The Government Printer.
Cameroon. 1978. Recensement General de la Population et de l'Habitat d'Avril 1976, Tome 2. Yaounde: Direction de la Statistique et de la Compatibilite Nationale.
Cameroon. 1983. Enquete Nationale sur la Fecondite du Cameroun, 1978, Rapport Principal Yaounde: Direction de la Statistique et de la Compatibilite Nationale.
CIR (Center for International Research, U.S. Bureau of the Census) 1993a. Trends and Patterns of HIV/AIDS Infection in Selected Developing Countries. Research Note No. 10. Washington, D.C.: U.S. Bureau of the Census.
CIR (Center for International Research, U.S. Bureau of the Census) 1993b. Trends and Patterns of HIV/AIDS Infection in Selected Developing Countries. Research Note No. 12. Washington, D.C.: U.S. Bureau of the Census.
CIR (Center for International Research, U.S. Bureau of the Census) 1994a. Recent HIV Seroprevalence Levels by Country: June 1994. Research Note No. 13. Washington, D.C.: U.S. Bureau of the Census.
CIR (Center for International Research, U.S. Bureau of the Census) 1994b. Trends and Patterns of HIV/AIDS Infection in Selected Developing Countries. Research Note No. 14. Washington, D.C.: U.S. Bureau of the Census.
Congo. 1978. Recensement General de la Population du Congo, 1974, Tome 4. Brazzaville: Centre National de la Statistique et des Etudes Economiques.
Congo. 1987. Recensement General de la Population et de l'Habitat de 1984, Tome 3. Brazzaville: Bureau Central de Recensement. de Graft-Johnson, K. T. 1988. Demographic data collection in Africa. Pp. 13–28 in E. van de Walle, P. O. Ohadike and M. D. Saka-Diakanda, eds., The State of African Demography. Liege: International Union for the Scientific Study of Population.
DeCock, K. M., B. Barrere, L. Diaby, et al. 1990. AIDS—The leading cause of adult death in the West African City of Abidjan, Ivory Coast. Science 249:793–796.
Essex, M., S. Mboup, P. J. Kanki, M. R. Kalengayi, and P. J. Brewer. 1994. AIDS in Africa. New York: Raven.
Ewbank, D. C. 1988. Health in Africa. Pp. 85–102 in E. van de Walle, P. O. Ohadike, and M. D. Saka-Diakanda, eds., The State of African Demography. Liege: International Union for the Scientific Study of Population.
Ewbank, D. C., and J. N. Gribble, eds. 1993. Effects of Health Programs on Childhood Mortality in Sub-Saharan Africa. Working Group on the Effects of Child Survival and General Health Programs on Mortality, Committee on Population. Washington, D.C.: National Academy Press.
Fargues, P., and O. Nassour. 1988. Douze Ans de Mortalite Urbaine au Sahel. INED Travaux et Documents 123. Paris: Presses Universitaires de France.
Feachem, R. G., and D. T. Jamison, eds. 1991. Disease and Mortality in Sub-Saharan Africa. New York: Oxford University Press for The World Bank.
Feachem, R. G., D. T. Jamison, and E. R. Bos. 1991. Changing patterns of disease and mortality in Sub-Saharan Africa. Pp. 3–27 in R. G. Feachem and D. T. Jamison, eds., Disease and Mortality in Sub-Saharan Africa. New York: Oxford University Press for The World Bank.
Foote, K. A., K. H. Hill, and L. G. Martin. 1993. Demographic Change in Sub-Saharan Africa. Washington, D.C.: National Academy Press.
Gbenyon, K., and T. Locoh. 1989. Les Differences de Moralite entre garcon et filles [The Difference in Mortality Between Males and Females] in Mortalit et Societe en Afrique, G. Pison, E. van de Walle, and M. Sala-Diakanda, eds., Mortalite et Societe en Afriques au Sud du Sahara. Paris: INED.
Graham, W. J. 1991. Maternal mortality: Levels, trends, and data deficiencies. Pp. 101–116 in R. G. Feachem and D. T. Jamison, eds., Disease and Mortality in Sub-Saharan Africa. New York: Oxford University Press for The World Bank.
Graham, W., W. Brass, and R. W. Snow. 1988. Estimating maternal mortality in developing countries. Lancet 1:416–417.
Graham. W., W. Brass, and R. W. Snow. 1989. Estimating maternal mortality: The sisterhood method. Stud. Fam. Plan. 20(3):125–135.
Harrison, K. A., and C. E. Rossiter. 1985. Maternal mortality. Br. J. Obstet. Gyn. (Suppl. 5):110–115.
Henry, L. 1989. Men's and women's mortality in the past. Population (English Selection) 1:177–201.
Herz, B., and A. R. Measham. 1987. The Safe Motherhood Initiative: Proposals for Action. World Bank Discussion Paper 9. Washington, D.C.: World Bank.
Hill, A. 1991. Infant and child mortality: Levels, trends, and data deficiencies Pp. 37–74 in R. G. Feachem and D. T. Jamison, eds., Disease and Mortality in Sub-Saharan Africa. New York: Oxford University Press for The World Bank.
Hill, K., and A. R. Pebley. 1989. Child mortality in the developing world. Pop. Devel. Rev. 15(4):657–688.
Hill, K., and A. Yazbeck. 1994. Trends in Child Mortality, 1960–90: Estimates for 84 Developing Countries. Background Paper Number 6 for World Development Report, 1993: Investing in Health. New York: Oxford University Press.
Lancet. 1993. Editorial. World Bank's cure for donor fatigue. Lancet 342(8863):63–64.
Linden, C. P., S. Allen, A. Serufilira, et al. 1992. Predictors of mortality among HIV-infected women in Kigali, Rwanda. Ann. Intern. Med. 116:320–328.
Mali. 1980. Recensement General de la Population, Decembre 1976. Resultats Definitifs, Tome 1. Bamako: Bureau Central de Recensement.
Mukiza-Gapere, J. H. G. 1989. Biases and errors in the orphanhood method of estimating adult mortality: An empirical examination. Ph.D. thesis, University of London. Photocopy.
Murray, C. J. L., G. Yang, and X. Qiao. 1992. Adult mortality: levels, patterns, and causes. Pp. 23–111 in R. G. Feachem, T. Kjellstrom, C. J. L. Murray, M. Over, and M. A. Phillips, eds., The Health of Adults in the Developing World. New York: Oxford University Press for The World bank.
Okoye, C. S. 1980. Mortality Levels and Differentials in Sierra Leone, Vol. 2. Freetown: Central Statistics Office.
Rosenfield, A. 1989. Maternal mortality in developing countries: an ongoing but neglected epidemic. J. Am. Med. Soc. 262(3):376–379.
Rustein, S. O. 1984. Infant and Child Mortality Levels, Trends and Demographic Differentials. WFS Comparative Studies, 43. Voorburg, Netherlands: International Statistical Institute, Central Bureau of Statistics
Rutenberg, N., and J. Sullivan. 1991. Direct and indirect estimates of maternal mortality from the sisterhood method Pp. 1669–1696 in Proceedings, Demographic and Health Surveys World Conference, August 5–7, 1991, Vol. 3. Baltimore, Md.: Macro International.
South Africa. 1988. South African Statistics, 1988. Pretoria: Central Statistical Service.
Sudan. 1982. The Sudan Fertility Survey, 1979: Princiap Report, Vol. 1. Khartoum: Department of Statistics.
Swaziland. 1980. Report the 1976 Swaziland Population Census. Vol. 2. Mbabane: Central Statistical Office.
Tabetic, D. 1992. Excess female mortality in Northern Africa since 1965: a description Population (English Selection) 4:187–207.
Tanzania. 1982. 1978 Population Census, Vol. 5. Dar es Salaam: Bureau of Statistics.
Timaeus, I. M. 1984. Mortality in Lesotho: A Study of Levels, Trends and Differentials Based on Retrospective Survey Data. WFS Scientific Report 59. Voorburg, Netherlands: International Statistical Institute, Central Bureau of Statistics
Timaeus, I. M. 1987. Adult mortality in Mauritania. In Evaluation de l'Enquete Nationale Mauritanieanne sur la Fecondite. WFS Scientific Report 83 Voorburg, Netherlands: International Statistical Institute.
Timaeus, I. M. 1991a. Estimation of adult mortality from orphanhood before and since marriage Pop. Stud. 45(3):455–472.
Timaeus, I. M. 1991b. Estimation of mortality from orphanhood in adulthood. Demography 28(2):213–227.
Timaeus, I. M. 1991c. Measurement of adult mortality in less developed countries: A comparative review. Pop. Index 57:522–568.
Timaeus, I. M. 1991d. Adult mortality: Levels, trends, and data sources. Pp. 87–100 in R. G. Feachem and D. T. Jamison, eds., Disease and Mortality in Sub-Saharan Africa. New York: Oxford University Press for The World Bank.
Timaeus, I. M. 1993. Adult mortality. Pp. 218–255 in K. A. Foote, K. H. Hill, and L. G. Martin, Demographic Change in Sub-Saharan Africa. Washington, D.C.: National Academy Press.
Togo. 1985. Recensement General de la Population et de l'Habitat, 9–22 Novembre, 1981, Tome 4. Lome: Bureau Central de Recensement.
Trussell, J., and M. Rodriguez. 1990. A note on the sisterhood estimator of maternal mortality. Stud. Fam. Plan. 21(6): 344–346.
UN (United Nations, Department of International Economic and Social Affairs). 1983. Indirect Techniques for Demographic Estimation, E.83.XIII.2. New York.
UN (United Nations). 1989. Adolescent Reproductive Behavior: Evidence from Developing Countries Vol. 11. UN Population Studies No 109/Add.1. New York.
Waltisperger, D., and T. Rabetsitonta. 1988. Un bilan de trente ans de mesures directes de la mortalite adulte en Afrique. In African Population Conference, Dakar, 1988, Tome 2. Liege: International Union for the Scientific Study of Population.
World Bank. 1992. Better Health in Africa. World Bank, Africa Technical Department (AFTPN). (Draft unpublished tabulations, August 25). Washington, D.C.
World Bank. 1993. World Development Report 1993: Investing in Health. New York: Oxford University Press.
WHO (World Health Organization). 1989. The Health of Youth, Facts for Action. Youth and Sexually Transmitted Diseases. A42/Technical Discussions/10. Geneva.
Zimbabwe. 1985. Main Demographic Features of the Population of Zimbabwe. Harare: Central Statistics Office.
















