Nursing Staff and Quality of Care in Nursing Homes
Meridean Maas, Ph.D., R.N., F.A.A.N., Kathleen Buckwalter, Ph.D., F.A.A.N., and Janet Specht, M.A., R.N.
This paper focuses on a review of literature and research regarding nurse staffing and quality of care in nursing homes. Background information for this review was obtained through computerized literature searches, through solicited contributions and personal communications from nurse researchers and long-term-care scholars, and from presentations at a special panel session convened at the Gerontological Society of America meeting in Atlanta, Georgia, in November of 1994. The first section of the paper reviews the background and historical development of nursing homes in the United States, while the second section describes the current status of institutional long-term care. The next two sections discuss the future demand for nursing home care and some selected issues in long-term care. The fifth section presents a detailed review of research relevant to the linkage of staffing and quality of care. The final three sections outline research questions and areas that need to be studied, present a case study of staffing and quality in an exemplary nursing home, and set forth recommendations for policy initiatives.
Dr. Maas is professor, Dr. Buckwalter is distinguished professor, and Ms. Specht is research program assistant and doctoral candidate at the University of Iowa College of Nursing.
Background And Historical Development Of Nursing Homes In The United States
From Almshouses to Nursing Homes
Nursing home policy was developed from social welfare issues regarding care of the poor. A strategy known as ''indoor relief" was developed in Elizabethan England when social planners used almshouses to care for the poor, who were divided into the "deserving poor" (those who were unable to work) and the "undeserving poor" (those who were perceived as morally corrupt because they were able to work). The poor elderly were housed in almshouses and exempt from moral judgments because of their age and inability to work (Hall and Buckwalter, 1990).
In the United States in the 1920s, almshouses were funded by the states and were used to continue the policy of providing indoor relief for the deserving poor who were unable to be employed in the factories, as well as providing care for the blind, chronically ill, mentally ill, and frail and old individuals. In 1923, about half of the 78,000 residents of almshouses were elderly and infirm. Society began to protest the housing of the infirm elderly with the poor and insane and Congress, because of this public pressure, stipulated that persons in public institutions should not receive old age funds; people in boarding houses, however, were eligible. Not surprisingly, this legislation prompted a sharp increase in the number of boarding homes in which nurses were hired to care for the frail and chronically ill. Thus, many boarding homes became known as nursing homes (Kalisch and Kalisch, 1978; Vladeck, 1984). Also in the early 20th century, private care homes emerged for elderly widows of various ethnic or religious groups (e.g., Lutheran homes, Jewish homes), which served as the precursors for today's charitable and nonprofit nursing homes (Vladeck, 1984).
Nursing homes really began to develop following passage of the Social Security Act of 1935, which provided payment to individual beneficiaries and thus turned indoor relief into "outdoor relief." That is, community-based services began to emerge that prevented the need for almshouse placement (Kalisch and Kalisch, 1978; Vladeck, 1984). With passage of the Kerr-Mills Medical Assistance to the Aged Act in 1950, which allowed for direct payment to care providers, and with increases in the number of older adults in the population, the nursing home industry boomed.
In 1954, the American Nursing Home Association lobbied for and won the right for nonprofit nursing homes to be built in conjunction with hospitals using Hill-Burton funds. Thus, nonproprietary homes were moved into the medical-surgical domain where, after passage of the Medicaid and Medicare Acts in 1965, they were required to meet strict federal nursing standards, creating the skilled-level facilities of today. Standards of care relaxed somewhat during the Nixon administration, and proprietary homes could apply for small business develop-
ment loans, which excluded them from the strict federal nursing criteria and led to the creation of intermediate-level care facilities with criteria developed by individual states for reimbursement under Medicaid (Vladeck, 1984).
Altogether, between 1980 and 1990, there was a 24 percent increase in nursing home occupancy rates (McKnight's Long-term Care News, 1993). The percentage of residents requiring more hours of care, more services on a daily basis, and having higher acuity levels has also risen over the past few years. Indeed, 43 percent of all Americans who passed their 65th birthday in 1990 are expected to use a nursing home at least once in their lives (Murtaugh et al., 1990).
Development of Long-Term Care for the Mentally Ill Elderly
For the first half of the 20th century, the mentally ill elderly were systematically admitted to state hospitals, which provided them with custodial care (Kermis, 1987). By the late 1950s and early 1960s, however, the indoor relief policy regarding care of the mentally ill began to change as mental health programming was reoriented to a system of outpatient psychiatric treatment, rehabilitation, and prevention. Both the Kennedy and Johnson administrations supported deinstitutionalization of mental patients in the large state hospitals and the creation of community mental health centers to provide outpatient treatment. Thus, the population of the state mental hospitals, which included many elderly, decreased by as much as 66 percent (Kane, 1984), and those elderly who continued to require institutionalization were most often placed in nursing homes to receive care (Mechanic, 1980).
Unfortunately, the medical focus of most nursing home administrators and personnel left them unprepared to care for those elders with cognitive, behavioral and affective disorders, and nursing homes were faced with large numbers of residents who failed to respond to programming in a conventional manner, did not sleep at night, and became violent when confronted with other residents (Hall and Buckwalter, 1990). Research by Zimmer and colleagues (1984) found that 64 percent of elderly residents of skilled nursing homes had significant behavioral problems, of which nearly 23 percent were classified as "severe." Despite the fact that 58 percent of these patients were receiving psychoactive drugs, both psychiatric diagnoses and consultations were absent. Similarly high rates of mental illness and cognitive disorder (70 to 80 percent) in the absence of active treatment were reported by Roybal (1984) and Rovner and Rabins (1985). By and large, health planners and economists failed to recognize the additional staffing and financial burdens these mentally ill and cognitively impaired residents placed on the nursing home system (Vladick and Alfano, 1987). The current trend, however, is for integrated interdisciplinary treatment teams to provide psychiatric care in nursing homes, an approach that allows for the use of psychopharmacologic, psychoeducational, behavioral, and family or social interventions. Preliminary outcome data suggest, moreover, that this more comprehen-
sive approach results in the use of fewer psychotropic medications, more effective resolution of behavioral problems, and decreased costs related to the need for hospitalization (Dey, 1994).
Current Status Of Institutional Long-Term Care
Institutional long-term care can be viewed from several vantage points. This section presents data on the number and types of facilities and on the mix of residents cared for in those facilities. Federal and state regulations affecting long-term care and how those regulations affect reimbursement for care are discussed. Finally, staffing issues, including staffing requirements, staff mix and qualifications, the nature of nursing home work, and staff salaries, are described.
Numbers and Types of Homes
Long-term institutional care of elderly residents falls into two major categories: (1) traditional nursing homes, which primarily are facilities that provide either intermediate-level nursing care or skilled nursing care, but might also include "board-and-care" residential homes, and (2) recent alternatives to the traditional nursing homes, such as foster care homes, family homes, or assisted-living homes. Numbers of homes are presented to illustrate trends in the availability of institutional long-term-care options.
Traditional Nursing Homes
Today, the primary providers of institution-based care for dependent elders are the more than 20,000 intermediate and skilled nursing homes. Although the Omnibus Budget Reconciliation Act of 1987 (OBRA 87) eliminated the distinction between skilled and intermediate nursing homes, Title XIX continues to distinguish the two types for reimbursement. According to the 1985 National Nursing Home Survey (NCHS, 1987), 75 percent of nursing homes were proprietary, 20 percent voluntary nonprofit, and 5 percent government operated. Forty-one percent were operated by nursing home chains and about 50 percent were independently operated. Proprietary homes provided 69 percent of the nursing home beds, voluntary nonprofit homes provided 23 percent of the beds, and public homes 8 percent. Eighteen percent of the available beds were skilled nursing, 30 percent were skilled nursing and intermediate level, 28 percent were intermediate level only, and 25 percent were not certified. One-third of the nursing homes had fewer than 50 beds, about another third had between 50 and 99 beds, 28 percent had 100 to 199 beds, and only slightly more than 6 percent had 200 or more beds.
Another type of traditional nursing home is the board and care home. A board and care home differs from intermediate- or skilled-level nursing homes in
that continuous care provided by licensed nurses is not required. Board and care homes outnumber skilled and intermediate nursing homes by more than 2 to 1 in the United States and have an average size of 15 beds (Brown University Long-Term Care Quality Letter, 1994).
Both nursing homes and board and care homes have high occupancy rates, 91.5 percent and 85.6 percent respectively. However, the 1991 National Health Provider Inventory, mailed to providers and analyzed by the National Center for Health Statistics (NCHS), found wide geographic variations in the prevalence of nursing homes versus board and care homes or home care (Brown University Long-Term Care Quality Letter , 1994). The Midwest relied heavily on regular nursing homes, little on board and care, and moderately on home care. The Northeast relied heavily on all three, with much more home health care use than in the other regions. The South showed moderate usage of all three types of care, and the West relied on board and care more than any other region. Nationwide, the study counted 15,511 nursing homes, with 1.6 million beds and 1.5 million residents. While the number of free-standing nursing homes has dropped by 1,644 since 1986, the number of nursing home beds has increased by 60,000—meaning that existing nursing homes are becoming larger.
Recent Alternative Long-Term-Care Models
A number of residential care models have recently arisen in response to the need to develop alternatives to the medical model emphasis in most traditional long-term-care facilities. These alternatives include a range of state-licensed residential living environments such as foster care, family homes, residential care facilities, and assisted-living arrangements (Wilson, 1994).
These variations in facilities are possible because there are no federal guidelines standardizing long-term residential care, and state regulations vary widely regarding environmental, programming, and nursing care standards, with minimum staffing ratios ordinarily set quite low. Although residential care settings vary in size (ranging from small private homes accommodating up to 4 residents, to large congregate care facilities that may care for more than 100 residents), all offer assistance or care and share with the residents the responsibilities for activities of daily living. Ideally, the care provided is flexible, resident and family oriented, and intended to optimize individual dignity, functioning, health, and well-being. Because these alternative facilities also provide care for demented residents, the physical environment and design features of the facility should support the functioning of the impaired older adult and accommodate difficult behaviors and diminished abilities (Alzheimer's Association, 1994).
Assisted living, for example, is a model of supportive housing that is growing rapidly because of consumer preferences and lower costs than those associated with traditional models of long-term care (Wilson, 1994). The state of Oregon has been a leader in developing standards of assisted-living care for the
purposes of licensure and evaluating resident outcomes. Residents are entitled to a private apartment (shared only by choice) that includes a kitchen, a bath with roll-in shower, locking doors, and temperature control capability. Routine nursing services and case management for ancillary services are provided. Data show that residents in these Oregon assisted-living facilities have a remarkably high level of disability: 84 percent have some mobility impairment, 75 percent require assistance with medications, and 63 percent require assistance with bathing. Most importantly, the orientation of staff toward the residents is to empower them by sharing responsibilities, enhancing choices, and managing risks (Wilson, 1994). Because of the lack of regulations and standards, consumers need to question providers about all aspects of services, including the philosophy of care, number and type of staff, staff training, staff supervision, and costs, to determine if resident and family needs will be met.
The sub-acute unit is another alternative long-term-care model. With the advent of the Medicare prospective payment system and use of diagnosis-related groups (DRG) as the basis for payment in hospitals, older adults began to be discharged "quicker and sicker" to nursing homes. In the United States, this early discharge of older adults from hospitals has led to a movement to create sub-acute care units in nursing homes, discussed more fully below in "Future Demand for Institutional Long-term Care." These units do not necessarily focus on frail older adults in the latter stages of life, but are in response to the economic changes affecting hospitals and tend to reinforce a medical model of care (Lyles, 1986; Ganroth, 1988; Swan et al., 1990).
Case-Mix Data
According to Fries (1994), case-mix refers to distinctions of residents related to resource use where resource use is primarily defined as a ratio of nursing time to costs. Nursing home residents are a heterogeneous mix of vulnerable adults whose ages may span more than 50 years. Residents are also getting older; those over the age of 85 years constitute about 42 percent of nursing home residents, up from 34 percent in 1980. Despite the dramatic increase in the number of nursing home residents who are age 85 or older, there are more than 181,000 (12 percent) residents under the age of 65 in nursing homes (McKnight's Long-term Care News, 1993). As noted earlier, a high percentage (around 75 percent) of persons who reside in nursing homes are reported to suffer from a chronic dementing process or some form of mental health or behavioral alteration. Most of these residents also have medical and personal care needs that require ongoing staff intervention and support. For example, about half (51 percent) of residents are incontinent of urine. Physical care issues, low staff ratios, regulatory issues, and inadequate staff preparation and training often mean that residents with behavioral impairment are still poorly understood and tolerated in the long-term-care environment (Hall, 1995).
Regulations and Reimbursement
Over the past few years, a paradigm shift has occurred in long-term care—from a biomedical treatment orientation and custodial care approach to a more social-behavioral model of care with a rehabilitative focus (Burgio and Scilley, 1994). However, implementation of a social-behavioral model of care has been constrained by regulations and reimbursement that are still guided by a medical model and by tensions between federal and state jurisdictions for regulating and reimbursing nursing homes.
Issues of staffing and care policies in traditional long-term-care facilities are influenced by a combination of federal and state regulations. Because the federal government is the only payer for Medicare and shares the rapidly increasing payment with states for Medicaid, and because consumer concerns intensified, federal interest in regulation increased and resulted in the passage of OBRA 87. Yet state regulatory groups did not control the development of OBRA regulations and do not have the option to not implement them. The OBRA 87 regulations mandated higher standards for quality care, but federal and individual state reimbursement formulas have not necessarily changed to enable nursing homes to better meet the higher standards.
Enactment of OBRA 87 resulted in regulations that required nursing homes to adopt a more active social-behavioral treatment model for residents. In contrast to an earlier emphasis on facility cleanliness and the physical plant, the new regulations are more resident focused, emphasizing systematic assessment and individual plans of care that foster the highest achievable level of resident well-being. In addition to restricting the use of antipsychotic medications for the treatment of behavioral problems, OBRA also mandated more training for each nurse's aide (a minimum of 75 hours of initial training that addresses psychosocial as well and physical health care, and 12 hours of in-service education annually), as well as assurance of skill competency (Burgio and Scilley, 1994).
Thus, with OBRA 87 setting the standard for quality of care in long-term-care facilities, the nursing home industry today is among the most highly regulated businesses in America. Beset with regulations developed in response to perceived abuses and poor quality care, licensed nursing homes are charged with providing care that meets the vast needs of diverse residents, yet often they must try to meet that charge with only minimum reimbursement and inadequate staffing (Hall, 1995). Success or failure to meet the government mandates is evaluated by the facility's own quality assurance programs, as well as surveys conducted by multiple agencies, care review boards, and state ombudspersons who investigate complaints (Hall, 1995). A report by the Department of Health and Human Services Office of the Inspection General indicates that most states are doing an adequate job of carrying out their survey responsibilities as outlined under OBRA 87. However, survey staff issues, enforcement, and inspections remain problematic, and there is need for improved training of state surveyors
and better communication between state and federal surveyors in terms of consistent application of guidelines for quality of care (McKnight's Long-term Care News, 1993). In addition to the surveying difficulties, the lack of attention to how reimbursement affects the ability of homes to meet quality standards is a serious concern.
Nationally, there is some movement toward case-mix reimbursement for nursing home care, although most states continue currently to reimburse by capitated cost-based systems—systems that are limited by a cap regardless of the cost to provide the care. Use of this system tends to encourage nursing homes to preferentially accept private pay and minimal care persons, rather than persons whose care is reimbursed by Medicaid.
The lack of federal regulation coupled with wide variation in state regulations also affects alternative forms of long-term-care facilities and the level of reimbursement available to those facilities. Currently there are few regulations for assisted-living facilities, and reimbursement under Title XIX for assisted living is limited to a few states. Public expenditures for community-based services are relatively small compared to those for nursing home care (O'Shaunessy and Price, 1987). Medicaid, which is the principal source of funding of health care services for low income persons, finances mostly nursing home care and was not designed to support a full array of social and other long-term-care community-based services. A few states provide some reimbursement, but because of a lack of Medicaid reimbursement most deny persons who cannot privately pay for this option. Some, but not all, long-term-care insurance policies cover assisted living and other arrangements alternative to nursing home care. There also is some controversy surrounding reimbursement rates for special care units, because of a lack of data to support whether or not a higher cost of care is justified on these units.
Staffing, Staff-Mix, and Qualifications
Over 1.5 million residents are cared for in nursing homes by 1,200,000 full-time equivalent (FTE) employees each day, of whom 700,000 FTEs provide some form of nursing or personal care. Nursing aides (designated by the acronym NAs and also referred to in this paper as nurse aides, nurse assistants, and nursing assistants) and orderlies account for over 40 percent of a home's total FTEs. Registered nurses (RNs), on the other hand, make up less than 7 percent of a nursing home's total FTEs and less than 20 percent of a facility's total nursing staff. Of the estimated 1.5 million employed RNs in the United States, fewer than 100,000 are employed in nursing homes (NCHS, 1988). And yet nothing is more important than the characteristics of the nursing staff in terms of determining the residents' quality of life. Staff interaction with residents and the nature of the relationship that develops between them is what matters most to residents, far
more than the administrative philosophy or decor of the facility (Kayser-Jones, 1989).
Data from the 1985 National Nursing Home Survey (NCHS, 1988) indicated that nursing homes had an average of 71.4 FTE staff per 100 beds, with an average of 5.2 RN FTEs, 7.4 LPN FTEs, and 30.8 NA FTEs per 100 beds. Proprietary homes averaged 4.3 RN FTEs per 100 beds, while voluntary nonprofit homes averaged 6.7 RN FTE per 100 beds and government-operated homes 7.4 RN FTEs per 100 beds.
Regulations are such that very few nursing homes (5.6 percent) have an RN on duty 24 hours a day (Jones et al., 1987). Because available staff are distributed over a 24-hour period, for every 100 beds the average staffing is 1 RN, who is most likely to be the director of nursing, 1.5 LPNs, and 6.5 nurse aides, as compared to a ratio of 1 RN for every 4 patients in a hospital (Mezey, 1992). The median amount of RN time per resident, per day, across all nursing homes in 1985 was 12 minutes or less, and nearly 40 percent of nursing homes reported 6 minutes or less of RN time per resident per day (Jones et al., 1987).
Similarly, the American Nurses Association (ANA) found staffing ratios of nursing assistants to patients in intermediate-level care facilities to be 1:11, whereas the ratio for licensed nurses was 1:100 (ANA, 1991). Nursing assistants are the primary care givers in long-term care. Consequently, the care that they provide is an important determinant of the quality of life and quality of care for nursing home residents. The typical NA is a 20- to 40-year-old female; about half are members of a minority group, with low socioeconomic status and a high school education or less. Typically, they are paid little more than the minimum wage.
Nurse vacancy rates are higher in nursing homes than in other practice settings. Despite recent improvements (in 1993, 70 percent of state nursing home association executives indicated that vacancy rates in their states had dropped to 10 percent or less) (McKnight's Long-term Care News, 1993), nurses still find hospitals a more attractive setting in which to work. RN salaries in nursing homes are about 15 percent lower than salaries for hospital RNs (Maraldo, 1991). While this situation may have changed somewhat, due to greater concerns about hospital costs in recent years, nursing homes continue to compete poorly for RNs because of wages and working conditions. Unfortunately, caring for the elderly is still not considered prestigious or financially rewarding when compared to other areas of nursing practice.
The OBRA 87 regulations contain no staffing standards except that an RN is to be on duty for 8 of the 24 hours each day. Some homes have obtained waivers that permit them to substitute LPNs. Thus, staffing requirements for nursing homes vary from state to state. In Iowa, for example, two hours of nursing care hours per patient day are required for certified Medicaid residents. This breaks down to only about five minutes per hour, even though the average resident who is unable to feed him- or herself requires about one hour of assistance for each
meal provided. If these Medicaid residents who are dependent on receiving help to eat should lose weight continuously over a period of several months, the facility may receive a citation for poor quality care—a real "Catch 22." Some long-term-care providers have successfully sued to become eligible for staffing levels greater than those reimbursed by the Medicaid statute, as was the case with an Atlantic City, New Jersey, nursing home, which argued that the unusual configuration of the facility (three buildings connected by ramps and walkways) required additional Medicaid funds so it could provide adequate staff (McKnight's Long-term Care News, 1993).
According to the Select Committee on Aging (1992) in the U.S. House of Representatives, without changes in staffing regulations, the needs of the elderly will remain largely unmet through the year 2020. In their report to the chairman, the committee listed several reasons for a lack of health care personnel trained in geriatrics and gerontology: difficulty recruiting and retaining qualified personnel for direct care in nursing homes, poorly trained workers, little training of family and friend care givers, vague job descriptions, shortages of qualified faculty to teach the needed knowledge and skills to physicians, nurses, and other health professionals, and the lack of appropriate training sites. Clearly, low salaries for nursing home personnel contribute to recruitment and retention problems and low reimbursement rates affect nursing home providers' interest in paying higher salaries.
Nature of the Work in Nursing Homes
Nursing home work is often difficult, stressful, frustrating, and labor intensive, especially for NAs, who have the most direct contact with residents. Nursing home staff have to confront aging, disability, and dying. Much of the care of the elderly is not pleasant, such as caring for urinary and bowel incontinence or dealing with a cognitively impaired elder who is agitated and combative. Combined with low wages, minimal benefits, hard physical work, and the often progressively deteriorating abilities of the residents, the nature of the work for nursing staff is often characterized as tedious, unpleasant, and unrewarding. Furthermore, because concern for costs is likely to continue while resident acuity increases, the workload of NAs and nurses in nursing homes may very well get heavier.
Research related to the actual nature of the work role of NAs documents that the complexity level of most tasks is low (suggesting a routinized approach), and that even when NAs carry out direct care tasks, their attention is not always directed toward residents. The highest level of psychosocial quality interaction was found to occur in the process of socializing, an informal component of care, suggesting the need for alternative task structuring and more resident-centered models of care (Brannon et al., 1992). Other studies support the notion that staff-
to-staff interactions are much more frequent than staff-to-resident interactions (Burgio et al., 1990).
In general, RNs in nursing homes suffer from a lack of prestige within the total health care delivery system. They are not only victims of financial disparity, but they are also subjected to humiliation and professional degradation, and their work role is often tied up exclusively with administrative functions. While the reasons are many, the lack of respect for nurses who choose to care for the elderly in nursing homes is at least in part because nurses and other health professionals often share the negative attitudes of society toward the elderly (Harrington, 1984).
The work of nursing home personnel is not without rewards, however. These rewards are largely intrinsic and evolve from the relationships formed with the elderly residents and the satisfaction gained from feeling that one has contributed to the quality of their lives, if only in a small way. For some, there are also the rewards of personal development that come from learning about aging and the opportunity to gain clinical skills. Nonetheless, extrinsic rewards for nursing staff remain problematic and this is largely responsible for the frequent turnover of staff and inability to recruit and retain qualified staff.
Staff Salaries and Incentives
As already mentioned, salaries and other incentives are problematic for all nursing staff in long-term care. One of the major reasons for the dearth of RNs in nursing homes is economic, and retention rates among long-term-care staff have been shown to increase concurrently with increases in average weekly salary. In 1988 they received 88 percent of the typical acute care wage, and by 1990 the percentage had dropped to 86 percent. For RNs, the highest hourly rate was $18.91 in hospitals, followed by $16.82 for home care, and $15.26 for nursing home RNs (Hospital and Healthcare Compensation Service, 1994). Since 1990, there is some evidence that salaries for some staff in nursing homes may be increasing, although they continue to lag behind salaries in hospitals. Annual salaries for Directors of Nursing (DON) were recently reported to have increased by 6 percent to $41,200 (McKnight's Long-term Care News, 1995). The salaries and benefits of nursing assistants, however, provide little incentive and lag behind those for hospital aides and home care aides. The median hourly wage reported by hospital aides was $7.12 between 1987 and 1989, compared to $5.29 for nursing home aides and $4.22 for home care aides.
Noting that RNs are a critical component of the rural health care delivery system and in some areas the sole providers of care, the Select Committee on Aging (1992) reported a shortage of 45,382 FTE RNs in nonmetropolitan areas of the United States. The $3,000 discrepancy in annual salary between nurses employed in small hospitals and those employed in large hospitals probably played a role in the shortage (Movassaghi et al., 1992). According to Kayser-Jones (1981b), often the only nurses willing to work for the low wages offered
are those who cannot get employment in other types of health settings because of poor qualifications.
Selected Issues In Long-Term Care
Cultural Diversity Among Staff and Residents
Issues Regarding Minority Care Providers
Increasing the numbers of minority and disadvantaged persons in the health and allied health professions to care for the underserved, such as the elderly, is an important component of health care reform. Shortages of minority providers may adversely affect access, cost, and quality of care. At the same time, the background and characteristics of many nursing home staff may adversely affect their job performance (Burgio and Scilley, 1994). The lives of many nursing assistants, in particular, are beset with personal problems and tragedies that leave them with too few personal resources to respond effectively to residents and that interfere with their ability to provide quality care to the frail, dependent elderly (Tellis-Nayak and Tellis-Nayak, 1989). In their ethnographic study on quality of care, nursing homes, and nurse aides' cultures, Tellis-Nayak and Tellis-Nayak (1989, p. 312) concluded that the ''institutional culture of the average nursing home not only ignores the affective needs of the nurse's aides, but it even assaults their self-esteem." They also assert that out of a concern for quality, advocates and policymakers have inappropriately reduced a complex problem to one of staffing and training issues alone, failing to appreciate the important role social history can play in staff apathy and lack of concern for residents.
Every individual carries a cultural heritage, and older people generally have more ties to their heritage than do many in the younger generations. Elders of particular ethnic or racial minority groups may have customs and beliefs that are important to them, but are no longer remembered or respected by the young. Although it is important for staff to respect and attend to the cultures of Black, Hispanic, Native American, and Asian minorities, it also should be remembered that many Caucasian persons are also members of ethnic groups that have distinct cultures, such as Jews, Poles, or Irish persons (Snyder, 1982). While it is neither practical nor necessary for staff to share the same ethnicity or cultural heritage as the residents, staff do need to learn about the usual lifestyles and backgrounds of the elders for whom they are caring. Even staff who share a common culture with residents may find that differences between generations present obstacles to understanding and respect. A clash of beliefs about health and illness and about appropriate remedies and treatments may be disconcerting to both staff and residents. When staff have some knowledge about the usual practices and beliefs of residents, there is a basis for communication that can optimize care and the residents' compliance with recommended treatment. To promote adjustment in
the nursing home, staff need to know at least some of the basic vocabulary of the residents, and it is important that someone, either volunteer or staff, be available for translation when elders speak limited English (Snyder, 1982).
Problems related to cultural and racial diversity are particularly acute in urban nursing homes, where a majority of staff may belong to minority groups, whereas the residents are predominantly white. Preliminary findings from a study of ethnic and racial conflict between nursing home staff and residents in New York revealed a high prevalence of racially charged verbal abuse and name calling of aides by residents (Teresi et al., 1994).
Institutional Care Needs of Minority Elderly
There is a lack of research and thus an inadequate knowledge base about the long-term health care needs of minority elders and other age groups. The research that does exist strongly suggests some disparity of service use and inequity of access for ethnic and minority populations, despite increased need (Barresi and Stull, 1993). While the general growth of the elderly population in the United States is well known, the increase in racial and ethnic elderly populations is less well recognized. Yet the elderly population is increasing faster among ethnic and racial minorities populations (Hispanics, American Indians, African Americans, Asians, and Pacific Islanders) than among whites, and the total population of ethnic and minority elderly has doubled with each national census since 1960 (Harper and Alexander, 1990). In some parts of the country, these ethnic and minority elderly will soon be the majority among the population aged 65 years and older (Cuellar, 1990; Morioka-Douglas and Yeo, 1990; Richardson, 1990). In 1985, approximately 14 percent of the population 65 and over were persons of color (Elders of Color, 1991). A significant increase in the population 85 years of age and older and in the number of females is also occurring, and a substantial proportion of these elderly are of racial and ethnic minorities.
Despite having poorer health and less help from relatives than comparison groups of white elders, black elders are less likely to be institutionalized. At comparable rates of frailty, the likelihood of nursing home admission for blacks is less than half that of whites (Belgrave and Bradsher, 1994). Poverty, geographical isolation, and discrimination are now given more weight in this pattern than the previous characterization of personal preference.
Although the Indian Health Service (IHS) has a statutory responsibility to meet the health needs of American Indians, it tends to define its mission in terms of acute care. As a result, the rapidly increasing long-term-care needs of the growing numbers of aging tribal members are largely ignored. John (1991) points out that an additional problem confronting tribal elders is a policy of age discrimination in resource allocation within the IHS. Specifically, he notes that the IHS concentrates its resources on the health problems of younger tribal members through the Resource Allocation Method, which is based on a calculation of
potential years of productive life lost. This strategy virtually ignores health issues for elders over age 65. For example, there are only ten reservation-based nursing homes in the United States, and they currently house 435 residents (Manson, 1989). A National Indian Council on Aging (1981) report indicated that 46 percent of older tribal members are assisted by extended family members to accomplish one or more activities of daily living.
Data regarding long-term care of the minority population are particularly lacking in respect to Hispanic elderly people, especially given the fact that Hispanics make up about 4 percent of the elderly population in the United States (AARP, 1985a) and are the fastest growing subgroup of the elderly (Lopez-Aqueres et al., 1984). More than 600,000 Hispanics are over the age of 65 (AARP, 1985b). What data do exist show that Hispanic populations report greater utilization of informal support systems than of professional health care providers (Greene and Monohan, 1984). As with Asians and Pacific Islanders in the United States, elder Hispanics face hypertension, tuberculosis, and cancers as their major health concerns. These elderly are less likely to use formal health care services, including nursing homes, due to lack of knowledge of available services (Holmes et al., 1983), cultural and language differences, and reliance on traditional medicine (Espino et al., 1988; AARP Minority Affairs, 1990).
In a study of nine nursing homes in San Antonio, Texas, Chiodo and colleagues (1994) found strong evidence that Mexican American nursing home residents are more cognitively and functionally impaired, after controlling for age and education, than non-Hispanic white residents. They also were significantly more likely to be funded by Medicaid, and they were more likely to have lived with relatives prior to institutionalization.
Major differences between Puerto Rican Hispanics and non-Hispanics admitted to nursing homes were identified in a study by Espino and coworkers (1988). The Puerto Rican Hispanics were significantly younger and functionally more impaired, both physically and mentally, than their non-Hispanic counterparts and more similar to chronologically older non-Hispanic nursing home residents.
Some research documents the need for nurses to be aware of the implications of ethnicity in caring for the elderly. In a study of immigrant, Canadian-born, and Anglo-born elderly in long-term-care facilities, Jones and Van Amelsvoort Jones (1986) found significant differences in the observed interactions among the groups. Although the elderly as a whole had minimal verbal interaction directed to them during morning and evening care, overall, male residents were spoken to less than female residents, and ethnic females had the least number of commands, the fewest statements, and the least number of questions spoken to them by staff.
Violence, Abuse, and Conflict
"Granny battering" and "slow euthanasia" are heard about quite often by
nurses (Bahr, 1981), and it is usual to find daily reports in the news of elder abuse perpetrated by criminals, family members, or care givers. Because the numbers of dependent and vulnerable elderly in the population are increasing, abuse and crimes against the elderly will likely continue to occur in proportionate numbers in the future. Elder abuse is identified in the literature as rights violations, physical abuse, material abuse, and psychological abuse (Pollick, 1987). Rights violations are the denial of the basic rights of the elderly person as defined by the 1961 and 1971 White House Conferences on Aging (Beck and Ferguson, 1981). Material abuse is monetary or material theft or misuse (DHHS, 1980). Physical abuse includes acts of omission or commission that result in physical harm, with omission being the most common (Beck and Ferguson, 1981). Psychological abuse is behavior that demeans or diminishes the dignity or self-worth of the elderly person (Hickey and Douglass, 1981). Accurate documentation of elder abuse is problematic because the elderly are often unreliable witnesses or fear retaliation, and because observable physical signs are easily explained as caused by falls and injuries. Most professionals agree that elder abuse is a common and serious public health problem, with 1 study documenting 60 percent of 228 professionals (police officers, social workers, adult protection workers, mental health workers, legal services providers, clergy members, morticians, and coroners) reporting that they deal with elder abuse at least once per week (Hickey and Douglass, 1981). Typically, the abused elder is female, more than 70 years old, physically or mentally impaired or both, and living in the community with an adult child or some family member (DHHS, 1980).
Abuse also occurs, however, in institutional settings. Research conducted in one 200-bed nonprofit nursing home suggests that the majority of nursing assistants are kind and helpful most of the time, although abuse (primarily psychological abuse such as yelling, swearing, and being insulting) does occasionally occur. The investigator suggests that the stressful work role of NAs leads to exhaustion and burnout that may precipitate abuse, and argues that mechanisms are needed to help nonprofessional staff deal with their work-related stress (Foner, 1994). Others (Kayser-Jones, 1990) have characterized the behavior of NAs as rude, neglectful, uncaring, and sometimes verbally and physically abusive.
Although most nursing homes take care to observe residents' rights, no nursing home can guarantee that every right of every individual will be respected. Problems and conflicts are bound to occur occasionally. Usually complaints are equitably and amicably resolved within the facility. But when a problem cannot be resolved internally, a resident or family member may contact the local office of the long-term-care ombudsman program. Examples of problems and conflict between a family member and staff are feelings of being depreciated or belittled, perceptions that a loved one is not receiving all available services or treatments, concerns about financial matters that are not fully explained or accounted, feelings of discrimination, or concerns that the facility staff does not adequately discuss treatment, transfer, or discharge options.
Physical abuse resulting from poor care, such as skin breakdown, rough handling, or inattention to bowel and urinary elimination needs, is another serious problem that can occur in institutions. This type of physical abuse may be inflicted by health care personnel who are not well qualified (Baker, 1977). Citing the dearth of research regarding maltreatment of residents of nursing homes, Pillemer (1988) provides a theoretical model of maltreatment as the outcome of staff members' and patients' characteristics as these are influenced by aspects of the nursing home environment and by certain factors exogenous to the facility. As highlighted in the model and supported by a review of the literature, staff who are at more risk for abusive behaviors toward the institutionalized elderly are more likely to be young (Penner et al., 1984), have lower levels of education (Baltz and Turner, 1977; White, 1977), be male (U.S. Department of Justice, 1985; Straus, 1986), have the least experience (Penner et al., 1984), and be under more stress (Heine, 1986). More recently, Pillemer and Hudson (1993) report an evaluation of a model abuse prevention curriculum for nursing assistants, showing high satisfaction with the program and reduced conflict and abuse of residents. Cassell (1989) also suggests that physicians sometimes abuse their elderly patients when they employ their power in a manner they believe to be in the best interests of the sick.
Just as residents can suffer at the hands of staff, nursing staff are also subject to abuse by residents. Studies about the incidence of aggressive resident behavior in nursing homes are sparse, but the few available studies suggest that the presence of behavioral problems warrants concern (Zimmer et al., 1984; Beck et al., 1991). Sometimes aggressive resident behaviors are violent and may cause fear in nursing staff as well as harm. Management of aggressive resident behaviors presents difficult care problems for nursing staff. In a study of 101 nursing home and intermediate care residents in Veterans Administration (VA) facilities, Winger and colleagues (1987) found 9 percent of nursing home and 34 percent of intermediate care residents had no aggressive behaviors, while 84 percent of nursing home residents and 57 percent of intermediate care residents had behaviors that endangered themselves or others. A study by Everitt and coworkers (1991) documented that the three most distressing resident behaviors nursing staff encountered were physical abuse, verbal abuse, and wandering. Lusk (1992), in an exploratory study, found NAs reporting a variety of injuries (e.g., black eye, torn shoulder cuff requiring surgical repair) from residents' aggressive behaviors, while another study comparing physically aggressive behavior in two Department of Veterans Affairs nursing homes found more instances of aggressive behavior in the home with a greater percentage of neurologic and psychiatric patients (Rudman et al., 1993). Meddaugh (1987) reviewed chart and incident reports to investigate the aggressive behavior of 72 residents in a skilled nursing facility. Twenty-six staff members (27 percent) were abused by a resident 1 to 2 times in a 3-month period. In a study of 124 residents in 4 nursing homes, Ryden and colleagues (1991) found that 51 percent of aggressive behavior was physical,
48 percent was verbal, and 4 percent sexual. Aggression was correlated with functional dependence, although no category correlated with cognitive impairment.
Perhaps most difficult to deal with in nursing homes are the interactions among residents, some of which are positive and encourage friendships, while others are negative and involve violent arguments and even physical fights. Jones (1975) studied 441 residents in 10 intermediate care nursing homes and found that spatial proximity is an important consideration in the analysis of social interaction between residents. Arguments and fights occurred more frequently in fairly restricted spatial arrangements (e.g., 4-bed rooms), while friendship interactions were more likely to occur between residents who resided at least 2-rooms' distance from one another. The results suggest that in the limited environment of the nursing home both closeness and distance are needed for positive interactions among residents.
Access
It is estimated that 22 percent of the elderly long-term-care population live in nursing homes and other facilities, whereas 40 percent or more live at home with a spouse. The elderly are at higher risk for physical and mental health problems, impaired coping, functional decline, and premature institutionalization than the general population (Preston and Mansfield, 1984). These risks are even greater for the elderly who live alone and in poverty, particularly women (Krout, 1986).
Public expenditures for community-based services are relatively small compared to those for nursing home care (O'Shaunessy and Price, 1987). Medicaid, which is the principal source of funding of health care services for low income persons, finances mostly nursing home care. Expenditures for institutional long-term care in 1993 are estimated to be $74.9 billion. (Of that amount $36.9 billion were from Medicaid and $4.8 billion were from Medicare.) (DHHS, 1993).
Nevertheless, there is concern about underuse of nursing home care by some elderly, especially in areas where there are fewer nursing home beds per capita of elderly in the population. In general, rural areas have a higher concentration of the elderly and higher rates of chronic illness and disability. The growing number of older citizens in rural areas is especially pronounced in the Midwest and South. Yet the number of available nursing home beds—whether in traditional nursing homes or alternatives such as in-home care—is less per capita in these areas than in urban areas, and the shortage of RNs is greater in rural areas and in areas where the more impoverished elderly reside (Select Committee on Aging, 1992). Although Medicaid pays at least some of the costs of care for about 60 percent of nursing home patients, efforts by states to control costs of Medicaid have tended to limit the supply of nursing home beds. Further, the lack of Medicare reimbursement and the spend-down requirements to qualify for Medic-
aid assistance discourage some elderly from the use of nursing home care when it is needed (O'Shaunessy and Price, 1987).
Future Demand for Institutional Long-Term Care
Effect of Demographic Trends
As mentioned earlier, the population of older adults with complex and chronic conditions that require long-term care is growing. In 1985 there were about 1.4 million elders (people over age 65) residing in nursing homes; by the year 2050 this number is expected to increase fourfold (Andreoli and Musser, 1991). Current demographic predictions suggest that although the proportion of the U.S. population aged 65 and older will remain fairly constant, the proportion aged 85 and older will continue to rise in the next 30 years to about 2.1 percent of the population. With a stable population, these increases in proportion reflect the increase in the absolute numbers of elderly persons, particularly those 85 and older, who will increase in number from about 200,000 in 1951 to an estimated 1.2 million in 2011 (Bond and Bond, 1987). Over the next several decades, the proportion of nursing residents who are "old-old" (i.e., over age 85) is also expected to increase to somewhere around 50 percent.
Recent estimates indicate that one-half of the women and almost one-third of the men who turned 65 in 1990 will require nursing home care during their life. By the year 2010, an estimated 76 percent of the elderly are expected to be completely independent, but 24 percent of the elderly—about 7 million elderly persons—are projected to have some impairment that requires them to seek assistance with one or more activities of daily living (Scanlon, 1988; Kane and Kane, 1991). The number of dependent elders is expected to grow as the proportion of elderly in the population, especially those over age 75, increases (Griffin et al., 1989; Strumpf and Knibbe, 1990). Dependencies for assistance range from instrumental activities of daily living (IADL), such as cooking, shopping, and cleaning, to personal care activities of daily living (ADL), such as toileting, dressing, bathing, transfer and ambulation, and eating. Of the 7 million elderly needing long-term care by the year 2010, 1.75 million will be in nursing homes or other institutions; 1.4 million out of the total 7 million will need assistance with almost every ADL and IADL. Further, as a result of the aging population and increasing life expectancy, by the year 2020 the number of elderly residents in nursing homes could nearly double (Kemper and Murtaugh, 1991).
Trends in Case-Mix and Characteristics of Nursing Homes
By 2030, the elderly will comprise 20 percent of the population and use 30 percent of health care resources (Select Committee on Aging, 1992). The majority of residents in nursing homes will be 80 years and older, functionally depen-
dent in multiple ADLs, have multiple chronic illnesses, and be cognitively impaired. Because of continued short hospital stays for acute illnesses and increased use of home care services where possible, residents in nursing homes will tend to be sicker and more acute illnesses will be treated in the nursing home. At the same time, alternative settings, such as assisted living and group home facilities, will be more available and will house more of the younger elderly with fewer or less severe impairments (O'Connor, 1995). More emphasis in these facilities will be placed on rehabilitation to maintain and improve function. Convalescent nursing homes are also expected to be more prevalent, with many elderly discharged to their own home after a short stay for recovery and rehabilitation.
Nursing homes will also include greater numbers of residents with AIDS, more residents with infections like methacycline-resistant Staphylococcus aureus and tuberculosis, elderly who are developmentally disabled, residents requiring rehabilitation, and hospice residents. Special units devoted to the care of residents with these conditions, as well as residents on ventilators and with pressure sores, are expected to increase.
Although it is positive that more alternatives to nursing homes will be available for the elderly, the downside is that the majority, if not all, of the residents of nursing homes will require more complex and intensive nursing care, and most will be highly functionally debilitated both cognitively and physically. Logically, this changing case-mix has clear implications for the types and numbers of staff that will be required to deliver quality care. More professional nursing staff (registered nurses) with gerontological training and greater use of gerontological nurse practitioners will be needed, both to plan and provide care and to direct and supervise the care provided by assisting staff. The nature of the work with mostly "old old," highly debilitated residents will provide quality-of-care challenges for assisting staff that they will not be able to meet without professional leadership and direction, and it will exacerbate stress, burnout, and turnover problems that are already of great concern.
Subacute Care
As home- and community-based long-term-care options (e.g., assisted-living facilities, continuing care retirement communities) erode the market share served by traditional nursing homes, subacute medical and rehabilitation services are emerging as a viable discharge option for patients who are suffering from cardiac conditions and cancer, recovering from surgical procedures and transplants, who require wound management, or who are ventilator dependent. More than 50 percent of nursing home admissions currently come from hospitals, with most needing care for unstable medical conditions.
According to a report on a subacute care demonstration project in Illinois (McKnight's Long-term Care News, 1993), subacute care includes physician supervision and RN care and physiological monitoring on a continuous basis. Fa-
cilities will be responsible for developing for every admission a comprehensive plan of care that includes measurable objectives and timetables designed to meet a broad range (e.g., medical, psychosocial) of patient care needs. Rules related to quality assessment and quality improvement, personnel requirements, and admissions practices have been set forth by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), which has recently incorporated subacute care into its survey process. Increased staff levels will be necessary to accommodate patients receiving subacute medical, nursing, and rehabilitation services. Outcomes, physical plant, and physician credentials are three major areas addressed in JCAHO accreditation standards for subacute units (Stahl, 1995). It is noted that RN credentials are not included, a curiosity since RNs will obviously play a large role in the care of residents in subacute units in nursing homes. A further concern is that the medical focus will continue to compromise implementation of a social-behavioral model of care in nursing homes.
Special Care Units for Dementia
Special care units (SCU) emerged as an important environmental intervention for care of persons with dementia in the 1980s. Today more than 1 in 10 nursing homes has a special unit or program for people with dementia, with more than 1,500 SCUs providing in excess of 50,000 special care beds. Data indicate that the number of SCUs is continuing to grow rapidly, with more than 2,500 units projected to be in operation by 1995 (NIA, 1994). Although there is much diversity among SCUs, most incorporate some type of physical modification, including security measures to limit egress, specialized activity programming for residents, and special training for staff, who are often permanently assigned to the unit.
There are several reports of studies to evaluate the effects of SCUs; however, most have not employed designs with sufficient control to rule out competing explanations (Greene et al., 1985; Hall et al., 1986; Cleary et al., 1988; Matthew et al., 1988). Experimental research by Maas and Buckwalter (1990) is one exception. Analysis revealed no significant changes in cognitive or functional abilities over time and no significant differences in these abilities between Alzheimer's disease patients on the SCU and on traditional integrated nursing home units (Swanson et al., 1994). Patients on the special unit were restrained less than those living on traditional units, but the SCU patients fell significantly more, on the average. The total number of medications for each patient was not significantly different for SCU versus traditional unit patients, and the number per patient did not increase over the 1-year study period. A multicenter collaborative initiative, funded by the National Institute on Aging and designed to explore the effectiveness of SCUs, evaluate specific interventions and family involvement in care, and compare SCU outcomes to those of traditional nursing home care, is currently under way.
Projected Staffing Requirements
The projected demand for nursing home care has sparked debate over costs and the adequacy of homes to deliver quality care. The anticipated need for qualified care givers in nursing homes is expected to increase anywhere from two- to fivefold by the middle of the next century (DHHS, 1991). Projections of the number of FTE registered nurses needed to supervise care by the year 2000 range from 260,000 to slightly over 1 million (NIA, 1987). There were only 92,000 FTE RNs employed in nursing homes in 1984 (Sheridan et al., 1992). The House of Representatives Select Committee on Aging (1992) forecast that by 2030, at least 36,000 geriatricians and 1.1 million RNs will be required to provide adequate health care for the elderly population in 2020. According to the Select Committee's estimate, 223,900 RNs will be needed in nursing homes compared to 94,900 in 1990. Current RN-to-resident ratios for nursing homes are estimated to be 6.3 nurses per 100 residents, while the projected need for the decade of the 1990s, due to the anticipated changes in case-mix, is from 10.2 to 16.2 RNs per 100 residents. In addition, 671,100 NAs will be needed in nursing homes compared to 421,900 in 1990, and 167,000 licensed practical nurses (LPN) compared to 112,100 in 1990 (Select Committee on Aging, 1992). Although estimates of current and projected staffing vary according to time frame and perspectives on the appropriate staff mix in nursing homes, it is apparent that the demand for nursing staff in nursing homes is rising dramatically. The rising demand may influence recommendations for staffing numbers and staff-mix in nursing homes, despite a lack of research evidence directly linking quality and staffing.
Regulatory and Reimbursement Projections
There is no doubt that OBRA has done a great deal to improve the quality of care in nursing homes by placing new emphasis on outcomes evaluation, staff training, residents' rights and quality of life, and the decreased use of restraints and psychoactive drugs. In regard to RN staffing, OBRA requires a licensed nurse to be on duty at all times, and for 8 hours each day that nurse must be an RN. Further, OBRA requires a full-time director of nursing who must be an RN.
In our view, the OBRA regulations are minimal and do not go far enough in requiring 24-hour RN coverage with specific numbers of assisting staff for a specific number of residents to assure quality of care and reasonable work expectations for staff. The American Nurses Association has advocated for quality nursing home care by promoting RN coverage around the clock, nurse aide training and certification, and opposing waivers of OBRA licensed nurse requirements. The Institute of Medicine's Committee on Nursing Home Regulation recommended that "nursing homes should place their highest priority on the recruitment, retention, and support of adequate numbers of professional nurses who are trained in gerontology and geriatrics to ensure an adequate number and
appropriate mix of professional and nonprofessional nursing personnel to meet the needs of all types of residents in each facility'' (IOM, 1986). Despite such recommendations, the nursing home industry has sought waivers even of OBRA's minimal increases in staffing standards (Francese and Mohler, 1994). The industry cites a shortage of RNs and inadequate reimbursement to pay their salaries as reasons for not being able to meet the OBRA staffing standards. Thus the nation's ability to meet the future demand for long-term care will continue to be affected by government reimbursement policies that are not commensurate with government regulations regarding the quality of care.
Review of Research Relevant to Linkage of Staffing and Quality of Care
This section undertakes a review of the literature that investigates the quality of care provided in long-term-care facilities and examines linkages between quality of care and various aspects of nurse staffing. Following an initial discussion of definitions of quality and how it is measured, we discuss the relationship between cost and quality of care. Studies are then presented that focus on aspects of staffing (staff attitudes, level of training, level of stress and turnover rates, number of staff and staff mix) and that consider the effect of the variables on quality of care. Finally, we review research that examines the relationship between quality of care and environmental factors such as reimbursement policies, type of facilities, and management systems or organizational climate.
Definitions and Measurement of Quality
Few concepts have been more elusive, controversial, or politically volatile than nursing home quality of care. Perhaps this is because as individuals we all fear functional impairment, loss of independence, and impoverishment, but as citizens we do not have the will to provide the financing for quality of care in nursing homes. Quality of care in nursing homes is a complex concept confounded by regulations and debates about what should be measured to assess quality, case-mix, facility characteristics, and methods of measurement (Mezey, 1989; Mezey and Lynaugh, 1989). Moreover, quality of care has been defined both as an input measure and as an outcome (Kruzich et al., 1992). But perhaps most confounding has been the continued reliance upon a medical model in defining standards of care and reimbursement formulas. Quality in long-term care requires different strategies than in acute care. In long-term care the focus is on replacing the patient role with a self-care role, emphasizing the individual's abilities to function with remaining abilities despite chronic disease, impairment, or both. Nursing homes are "nursing" homes so, clearly, quality of care is dependent upon the quality of nursing. Yet professional RNs are so scant in nursing homes as to be almost a novelty (Maraldo, 1991).
Prior to OBRA 87, quality of care in nursing homes was largely evaluated and regulated according to structure and process standards rather than the achievement of patient outcomes. Traditional reliance on structural measures failed to capture the essence of nursing home quality (Braun, 1991), although Stein and colleagues (1986) found that resident perceptions of quality and level of satisfaction were strongly related to objective surveyor ratings of nursing home quality. In Kurowski and Shaughnessey's (1985) review of studies comparing quality of homes with regulator surveys, many aspects of quality were not sensitive to the surveys and adding observation to surveys did not adequately measure quality (Fackelmann, 1986). Davis (1991) reviewed a number of studies that have examined macro-organizational and structural variables and quality and noted the paucity of empirical evidence to support these linkages. Thus, research findings in general have shed little light on the characteristics of nursing homes (such as size, ægis, age, and rural or urban location) that inform our understanding of what factors contribute to quality care.
The Omnibus Budget Reconciliation Act of 1987 provided a starting point for a new definition of quality in long-term care and focused measurement of quality on patient outcomes (Wilging, 1992). According to OBRA, a nursing home's purpose is to "bring each resident to the highest practicable level of mental, physical, and psychosocial well-being, and to do so in an environment that emphasizes resident's rights" (Wilging, 1992, p. 22). Quality care begins with a standardized, comprehensive patient assessment coordinated by an RN, which requires that specific attention be given to activities of daily living, vision and hearing, pressure sores, urinary incontinence, range of motion, psychosocial functioning, use of nasogastric tubes, accidents, nutrition, hydration, antipsychotic and other drug use, and special services such as respiratory therapy. (Bowel elimination was ignored as an outcome to be monitored, but has been added in version 2.0 of the minimum data set.) The OBRA legislation proved to be the impetus for improving the quality of care in nursing homes. The requirement that specific fields be included in a minimum data set (MDS) on all residents in nursing homes provides a valuable source of data for evaluating quality on the basis of resident outcomes (Zimmerman, 1991). From the data on resident outcomes included in the MDS, quality indicators have been proposed and are being tested for how well they measure quality for aggregates of residents in nursing homes (Rantz and Miller, 1994).
The "highest practicable level of functioning," however, is in reality defined by what is fiscally appropriate within each facility. Whether or not adequate resources are available to provide quality care is still an issue, and many would agree that resources are often not adequate. For example, the study conducted by the Institute of Medicine's Committee on Nursing Home Regulation supported higher nursing staff standards as a major means for assuring quality of care in nursing homes, along with new staffing, training, and registry requirements for nursing staff (IOM, 1986). Unfortunately, the goal of requiring 24-hour RN
coverage in nursing homes was not achieved in OBRA because of political pressures touting a nursing shortage and higher costs. Although OBRA increased staffing requirements, the facts are that nursing assistants make up 85 percent of nursing staff in nursing homes and provide the majority of direct care to residents, with residents receiving on average only 12 minutes per day of care from RNs (Maraldo, 1991). As noted earlier, the issue of staff-to-resident ratios is also of concern. In acute care, there are an estimated 98 RNs for every 100 patients, while in nursing homes there are 5.2 RNs for every 100 residents (Wilging, 1992). This marked discrepancy is not likely due to a true corresponding difference in the needs of patients for nursing care in the two settings, but is rather due to how "highest practicable" is being defined by economic and political realities.
The concept of quality in the practice setting has, to date, included only limited attention to outcome assessments and public input (DHHS, 1993). Traditional paradigms of quality thus need redefinition to assure an excellence in health care that is responsive to the changing needs of the public. The movement to continuous quality improvement (CQI) is seen as one way of focusing on processes and systems, rather than individual efforts, in quality management applications (DHHS, 1993). When residents are asked what constitutes quality of care and what factors are most important in creating a good environment, they emphasize kindness, consideration, friendliness, and empathetic listening on the part of staff, suggesting that staff attitudes have a major impact on resident quality of life (Goodwin and Trocchio, 1987).
Although families continue to be involved in care following placement of their loved one in a nursing facility, relatively little is known about the relationships among families and nursing home staff, especially from the perspective of family members (Duncan and Morgan, 1994). What research has been conducted in this area indicates that families equate good quality nursing home care with care that is affectively appropriate, emotionally sensitive, respectful, and professional, and that emphasizes a personal relationship with the resident. Families tend to base their evaluations of care as much on social and emotional factors as they do technical competence in performing care tasks (Bowers, 1988; Duncan and Morgan, 1994), whereas staff often give priority to the smooth functioning of the organization. What this means is that nurse aides, in particular, often get caught between the desires of the organization and those of family members (Duncan and Morgan, 1994). To address these differences, Bowers (1988) proposed a collaborative approach to care that would encourage families to become more involved in technical aspects of care while facilitating staff's emotional involvement with residents. Interestingly, in those facilities where families found little respect for the work of the nonprofessional staff, they also enjoyed little support for their goal of having their loved one treated in a personal manner by the staff. As noted in a study using focus groups and interviews with families of patients with dementia, families concluded that "the demands and rewards of the nursing home as a system were often detrimental to quality care" (Duncan and
Morgan, 1994, p. 241). In another study, which examined the use of nasogastric feeding tubes in nursing homes, two themes of interest emerged in the family interviews. First, there was little or no communication among health care providers, patients, and their families regarding the use of nasogastric tubes. Second, some families perceived that the tubes were used for the convenience of the staff who did not want to take the time, or did not have the patience, to feed residents (Kayser-Jones, 1990).
Cost of Quality
The cost and financing of institutional long-term care to achieve the highest practicable functioning and well-being of patients is one of the biggest issues facing the assurance of quality care in nursing homes. Since OBRA, the average increase in reimbursement rate reported across the country has been about $1.50 per resident (Wilging, 1992). Few would argue that this is adequate to implement all that OBRA requires for assuring quality of care for nursing home residents, let alone to move beyond minimum standards. Without increased reimbursement, the nursing home industry will likely continue to seek ways to compromise OBRA standards, especially regarding RN staffing. "We get what we pay for" remains a truism that is no less applicable to nursing home quality of care than it is elsewhere.
As noted earlier, nursing homes are the major cost center for long-term care, with expenditures of more than $70 billion dollars in 1993 (DHHS, 1993). Data from the 1987 Medicare and Medicaid Automated Certification Survey (covering 14,000 nursing homes in 525 counties and 46 states) suggest that cost-saving decisions that lead to substituting less expensive staff and using more laborsaving techniques may lead to bad patient outcomes. That is, cost minimization may be achieved, but quality of care suffers. Where RN wages are high, nursing homes tend to use larger numbers of less expensive staff, whereas when LPN wages are higher, nursing homes use more RNs and NAs (Zinn, 1993). In addition, when the market price for nursing services is high, nursing homes use more laborsaving techniques such as catheterization, restraints, tube feedings, and nontoileting of residents, which may not necessarily represent good care strategies. However, where Medicaid per diem reimbursement rates are higher, and where there is more competition among facilities for patients, nursing homes use more licensed (RN and LPN) staff and have lower rates of catheterizations and nontoileting of residents. Spector and Takada (1991) also found that more RNs were employed when per capital income was higher, while more LPNs were used with higher Medicaid levels and in urban areas. When there was cost-based reimbursement, more RNs and LPNs were employed. These data suggest that nursing homes have not yet found consistent and effective ways to save money without sacrificing professional leadership and quality (Zinn, 1993).
Some have argued that families are a neglected resource for the delivery of
care in nursing homes. In a study to evaluate the effects of a special care unit for residents with Alzheimer's disease on resident, staff, and family member outcomes, Maas and colleagues (1991) found that family members were dissatisfied with their lack of involvement in the care of their relatives, with the activities provided for the residents, and with the amount of resources devoted to the provision of care. Based on these troubling results, Maas and colleagues (1994) are currently conducting a study funded by NINR. The study will test the effects on family and staff satisfaction and stress, as well as on resident outcomes, of an intervention designed to create a family-staff partnership for the care of institutionalized persons with Alzheimer's disease.
Factors that Influence Staff Performance
Job Satisfaction and Turnover
Staffing problems are expected to continue at least through the end of this century (Caudill and Patrick, 1991). In light of the growing demand for qualified personnel in long-term-care facilities and concern over the nursing shortage, however, surprisingly little research (aside from state and national surveys) has been conducted in the area of staff turnover, and the important other side of the coin, staff retention (Robertson et al., 1994).
Turnover in nursing staff is generally affected by a variety of factors leading to low job satisfaction, including low compensation and benefits, poor working conditions and quality of the nursing home, few opportunities for advancement, and problems with staff relationships (Birkenstock, 1991). Studies specifically focusing on NAs in long-term-care settings have cited numerous individual characteristics (e.g., age, education, background) as well as management factors (e.g., inadequate in-service education, supervision and orientation; few opportunities for advancement, performance appraisal, and compensation) as contributing to the high rate of turnover and dissatisfaction (Reagan, 1986; Wagnild and Manning, 1986). A study by Wagnild identified a "cycle of turnover" and found that NA turnover can be reduced by careful analysis of management practices, starting with the recruitment and selection of applicants and extending through orientation, staff development, supervisory skills, employee compensation, and involvement of aides in management decisions (Wagnild, 1988, p. 22).
Comparing levels of job satisfaction in social care homes, Willcocks and colleagues (1987) found the lowest levels in homes where the ratio of staff hours to residents was below the average. Low levels of staff satisfaction were particularly prevalent where staff had less autonomy and time constraints allowed only the essentials of care to be carried out. Although staff tended to rate their overall job satisfaction highly, negative elements noted were in regard to working conditions, staff shortages perceived to result in poor care, inadequate involvement in decisions, and inadequacies of training and consultation.
A recent study by Robertson and colleagues (1994) identified factors that affected RN retention in long-term care, focusing on what nurses reported as enhancing their job satisfaction and commitment to this area of practice. Briefly, the three highest rated factors related to satisfaction were recognition from patients, challenge of the work, and the authority to exercise judgment for patient care. The most important factors seen as contributing to retention were relationships with colleagues, available support staff, authority to exercise judgment in patient care, challenge of the work, adequate nurse-to-resident ratio, support from administration, and adequate supplies and equipment. The investigators also calculated mean difference scores for all items, indicating that importance was greater than satisfaction in these areas for the nurse respondents. The largest mean differences found were in the areas of paperwork, salary and benefits, and staffing. Further analysis and synthesis of the data revealed, consistent with previous findings in the literature, five main areas in which issues associated with retention of nurses in long-term care arise: (1) relationships, (2) patient care factors, (3) money and benefits, (4) levels of staffing and supplies, and (5) amount of paperwork. Difficulties in these areas represent serious problems in long-term care that threaten the quality of care provided in these settings (Robertson et al., 1994). Thus, to promote staff retention in long-term care and to make nursing homes a more attractive and satisfying practice setting, administrators must recognize both the importance to nurses of patient care factors and the authority to manage patient care issues and make clinical decisions, and the need to provide RNs with attractive compensation and benefits, recognition, training, and participation in decision making about their work.
Stress and Burnout
Nurses who work with the elderly confront many complex and potentially stressful care situations. Nowhere is this more true than for nursing home staff who work in highly demanding, labor- and client-intensive jobs. High stress at work can create morale problems that ultimately detract from the staff member's job performance (Sheridan et al., 1990). The causal model depicted below (see Figure 1), derived from research on work stress and morale among nursing home employees, highlights both antecedents and outcomes of work-related stress (Weiler et al., 1990, p. 321).
The antecedent conditions include objective organizational characteristics such as: (1) the variety of tasks in nursing positions, (2) the degree to which supervisory authority is delegated, (3) the closeness of supervision, (4) the degree of specialization, (5) the skill level of the work, (6) the quantity of the work, and (7) the pace of the work. Subjective organizational characteristics include: (1) task routinization, (2) communication, and (3) distributive justice. Social support includes perceived support from supervisors, coworkers, spouse, friends, and relatives. Personal characteristics refer to variables such as age, sex, educational
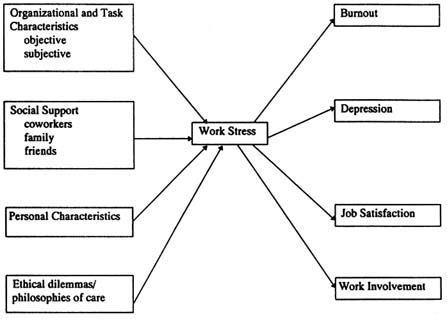
FIGURE 1 Causal model of work stress.
attainment, length of nursing service, occupational position or title, work status (e.g., full- or part-time), marital status, and number of relatives living nearby. Ethical dilemmas are situations in which no choice is clearly correct and the alternatives are equally unsatisfactory, while a philosophy of care incorporates ANA standards of care and the nurses' personal beliefs regarding the residents' right of autonomy, their role in the decision making process, and their right to respectful treatment (Weiler et al., 1990).
A large body of literature has examined the outcomes of work-related stress, revealing a strong link between stress and adverse physical and psychological consequences (LaRocco et al., 1980). There is equally compelling evidence, however, that social support serves to mitigate against these adverse effects and reduces burnout among nurses (Constable and Russell, 1986). Burnout, a phenomenon characterized by loss of concern for residents, and physical, emotional and spiritual exhaustion, may lead to indifference or negative feelings toward elderly residents, overuse of chemical or physical restraints, and heightened potential for abuse (Heine, 1986). Burnout has also been shown to result in administrative difficulties such as high rates of tardiness, absenteeism, and attrition (Goldin, 1985).
The outcomes of work-related stress, according to the above model, include: (1) burnout, defined as a syndrome of emotional exhaustion, depersonalization,
and lack of personal accomplishment; (2) depression, which is the degree of negative affect experienced by nursing personnel; (3) job satisfaction, which is the affective orientation of nursing personnel toward the work situation; and (4) work involvement, defined as the degree to which nursing personnel identify with the job (Weiler et al., 1990).
It has been suggested that nursing personnel who work with patients with Alzheimer's disease are especially vulnerable to the effects of stress and burnout. Alzheimer's disease patients present many difficult care and management problems because of their progressive cognitive, functional, and psychosocial deterioration, which can result in bizarre and combative behaviors, emotional outbursts, and wandering. Moreover, nursing home staff are often poorly trained to cope with the disruptive behaviors of residents, and they are therefore repeatedly frustrated by their inability to manage recurrent problems (Stolley et al., 1991). Many nursing homes are also not equipped with environmental structures or the support and service systems required to care appropriately for the person with Alzheimer's disease (Peppard, 1984). A recent study, using a quasi-experimental design with repeated measures, examined whether staff who cared for Alzheimer's disease patients on a special care unit were less stressed and less burned out than staff who cared for such patients on traditional (integrated) units. Findings revealed that the principal area of stress reduction for nursing personnel working on the SCU occurred with respect to staff knowledge, abilities, and resources. Subscale analysis indicated significantly less stress for staff who worked in the SCU with respect to residents' verbal and physical behavior. The SCU was designed specifically to provide the special environmental structures and support and service systems for the care of Alzheimer's disease patients that would enhance functioning and decrease associated behavioral problems. These may be important factors in reducing stress and burnout for staff caring for residents with Alzheimer's disease (Mobily et al., 1992). The investigators also recommended that whenever possible, staff who work with residents who have Alzheimer's should be carefully screened and selected for their ability to be sensitive to the needs of these residents, their flexibility, and their imagination, as well as ability to respond to persons with impaired communication and ever-changing moods (Coons, 1991). Specialized training in the care of residents with Alzheimer's disease is also a critical factor (see next section, "Education and Training").
In an effort to manage stress among nursing personnel in long-term-care facilities, it seems logical to examine those antecedent conditions in the model depicted above that are amenable to change. Research by Hare and Pratt (1988) has shown that higher levels of nursing burnout in both acute and long-term-care settings may be related to the nature of the physically and emotionally strenuous work tasks, low status in comparison to other positions in the health care system, limited training, low wages and benefits and, of interest to this report, poor staffing-to-patient ratios. Further, problems with support in the work environ-
ment, especially from peers and supervisors, have repeatedly been shown to be a primary source of stress among nurses (Cronin-Stubbs and Rooks, 1985). It has also been suggested that nursing personnel who elect to work with clients who have a poor chance of survival (as opposed to nursing personnel who do not work with these patients by choice) have reduced vulnerability to burnout because their work provides them with a sense of meaning (Hare and Pratt, 1988). The interventions summarized below have been set forth to address organizational sources of stress in the long-term-care setting (Weiler et al., 1990, pp. 333–334):
- Improved in-service training, especially in multidimensional problems of the elderly, that emphasizes psychosocial and behavioral problems common in this population.
- Increased variety in job tasks.
- Improved supervision.
- Implementation of a management style that allows for feedback, flexibility, and sensitivity.
- Clear and realistic objectives for resident care.
- Higher wages and better benefits for staff.
- Adequate staffing levels.
Although the latter two recommendations may be considered nonnegotiable by some administrators because of the cost implications associated with their implementation, it should be noted that the costs related to staff burnout, absenteeism, and turnover can far outweigh the costs associated with adequate staffing and compensation (Weiler et al., 1990).
Another source of work-related stress that may be amenable to change has to do with the effect of the physical environment and structural factors. Although very little research has been done in this area, work by Lyman (1987) suggests that physical and architectural features, such as adequate space, separate activity rooms, staff offices and toilet facilities, resident care facilities, barrier-free hallways, visible exits with amenities such as wide entry doors and ramps, and emergency exits, may decrease caregiver burden and stress. Enhancing social support networks is another important strategy that can serve as a buffer against the stresses inherent in working with the elderly. Interventions designed to strengthen supportive relationships among staff, staff training related to stress management, and work-related counseling and support groups have all been shown to reduce vulnerability to burnout, depression, and job dissatisfaction (Weiler et al., 1990).
Education and Training
Although previous research has provided inconclusive evidence of a strong relationship between the care provider's attitudes toward the elderly and the
quality of resident care (Wright, 1988), Storlie (1982) argued that dedicated and compassionate nursing staff are essential for maintaining high quality care on a day-to-day basis. Further, few would disagree that nurse aides need to be skilled in providing care, given that they make up about 85 percent of nursing home personnel and provide the majority of direct care. Yet many nurse aides are functionally illiterate, untrained, and inadequate to the tasks at hand (Maraldo, 1991). With the number of cognitively impaired and functionally dependent residents in nursing homes, sophisticated approaches for care are required that are beyond the knowledge and skill of persons with one year or less of training. The need for competent professionals who are caring, qualified, and compassionate caregivers has been documented by research on residents in long-term-care settings (NCCNHR, 1985). However, the reality is that the majority (96 percent) of directors of nursing in long-term-care facilities are not academically prepared for their positions (Bahr, 1991), having little or no specific education about the aging process, gerontological nursing principles, or managerial skills. The lack of educationally prepared RNs who understand the unique health and social needs of older adults and who are effective managers of assisting nursing staff is a critical problem. Combined with the small number of RNs employed in nursing homes and the reported vacancy rate of about 10 percent for RNs, the problem takes on gargantuan proportions (Bahr, 1991).
Much of the published literature on education in long-term care discusses the need for more training and adequate supervision of staff, especially for NAs. Methods most commonly used in staff training are didactic, using both verbal and written instruction, but there has been relatively little effort to study systematically the success of these methods with long-term-care staff, or to evaluate their ability to maintain therapeutic staff behaviors over time (Burgio and Burgio, 1990). In a review of the literature on this topic, Burgio and Burgio (1990, p. 289) urge the development of efficient training procedures "to teach nursing assistants basic therapeutic principles and skills," and argue that "management systems must be designed and implemented to assure that these skills will be performed appropriately and consistently in the natural environment." They also outline a number of strategies to overcome organizational resistance to staff-management interventions.
Burgio and Burgio (1990) suggest that an important step in motivating staff to perform patient-related tasks is effective in-service training, which should include: (1) didactic instruction presented both in verbal and written formats, (2) modeling of the procedure by a trainer, and (3) role playing by the trainees coupled with immediate trainer feedback regarding their performance. The attitudes of staff affect not only their own expectations about their working lives, but also the way in which they approach residents. Thus an important aspect of in-service training is to correct the tendencies to view residents as childlike, unreliable, and manipulative, and to reduce depersonalization of physical care and the neglect of psychosocial needs.
Assessment of training outcomes includes more than simple paper and pencil tests to determine knowledge of the procedure; rather, assessment should also include a checklist assessment of skill performance in a situation that permits immediate corrective feedback and praise, followed by assessment of the trainee's skill performance on the nursing unit. Burgio and Burgio (1990) argue that these assessments should take place immediately following the in-service training, as well as at regular intervals thereafter, with remedial training sessions required in the event of poor performance.
Consultation
As noted earlier in the section on staffing qualifications and preparation, most RNs employed by long-term-care facilities have associate degrees, that is, two years of training that includes little specialized training in gerontology or psychiatry. Thus, liaisons with advanced practice nurses (e.g., geriatric and psychiatric nurse practitioners) who possess skill in these areas can provide an invaluable resource to the long-term-care team, especially when dealing with behaviorally impaired residents. The liaisons can thus improve the quality of care for residents and the quality of life for visitors and staff (Hall, 1995).
Psychiatric nurses, in particular, can play a critical role in meeting the mental health and behavioral needs of nursing home residents through consultation and education efforts, which have been found to improve care through the reduction of symptoms and negative behaviors and the achievement of optimal resident functioning (Samter et al., 1994). Assessment and management of emotional problems require specialized knowledge, skill, and creativity (Stevens and Baldwin, 1988). Currently, the vast majority of nursing home personnel are nonprofessionals in whom these attributes are underdeveloped. The lack of skilled care givers and adequate resources to meet the mental, emotional, and behavioral problems of nursing home residents suggests that without specialized psychiatric interventions the mental health needs of the elderly residing in nursing homes will remain unmet or be treated inappropriately (Stevens and Baldwin, 1988).
Consultations with skilled mental health professionals is thus an important and effective intervention (Parsons et al., 1988; Smith et al., 1994). Effective psychiatric consultation can influence staff attitudes and behaviors toward residents by helping long-term-care staff to develop systematic approaches to the assessment and management of disturbed residents, and to focus on specific behaviors and plans of action related to those behaviors (Parsons et al., 1988). Such consultations are among the many vital factors that can ensure that the nursing homes of today will truly provide better quality of care to behaviorally impaired residents than did the almshouses and state mental hospitals of yesteryear.
Quality and Number of Staff
As noted above, the nursing shortage still exists in many long-term-care settings. Difficulty recruiting and retaining qualified personnel to provide direct care in nursing homes remains a crucial problem, although the number of staff per se may not be the whole answer to the provision of quality care in nursing homes. Research by Fries (1994) has documented that much of staffing is driven by the type of resident. Resident characteristics (case-mix) explained 55 percent of the variance in resource use, with facility characteristics (including staffing levels) adding another 13 percent. The remaining one-third of the variance in resource use was accounted for by differences in residents across days (e.g., number of baths per week). Case-mix also explained about 35 percent of the variance in RN costs.
According to Fries (1994), different states have different staffing levels, but the relative use for types of residents remains constant. Much of staffing is also driven by the type of resources and use of the available staff time is discretionary (Fries, 1994). Thus, adding additional staff may result in some more staff time for all residents and not more time for those who really need it. At the special panel session on ''Quality and Staffing in Nursing Homes" held at the 1994 Gerontological Society of America meeting, Fries argued the need, based on his data, to be more efficient in the use of current numbers of staff before it is assumed that higher staffing numbers are needed in nursing homes. He questioned whether some residents in nursing homes truly need that level of care, but rather are encouraged to be in nursing homes by flat rate reimbursement systems. Further, Fries (1994) suggested that higher quality may be possible by changing some staff practices in nursing homes without substantially greater resource investment. For example, use of fewer chemical and physical restraints was found to save staff time. Schnelle (1994) argued that despite the considerable experience of his research team in implementing highly specific protocols for managing incontinence, 100 percent compliance was never achieved. Thus, while nursing staff in nursing homes should have higher salaries and more help, just giving them more money and adding more staff is not the total answer. More specific protocol and management technologies also are needed in order to actually achieve higher quality care. Finally, consistent administrative support and RN leadership are also needed to guide staff performance so that it will result in quality outcomes.
Others also report that staffing shortages include insufficient numbers of NAs to provide the "hands on" care, as well as too few geriatrically prepared professional nurses to supervise care and provide leadership and guidance to the staff (Kayser-Jones, 1994). Current staffing patterns contribute to meeting resident needs through functional routines rather than individual care needs or resident preferences (Wright, 1988). Truly individualized care requires that a profes-
sional nurse, with specialized training, not only supervises the work of nonprofessional staff but also participates in and directs that care.
Although there are mixed results from research comparing quality to nursing hours, several studies have found nursing hours significantly related to quality indicators (Linn et al., 1977; Mech, 1980; Fottler et al., 1991). Disturbing data from a national survey conducted by the ANA suggest that those nursing homes with higher nurse vacancy rates experience more problems in areas such as medication errors and resident falls (McKibbin, 1990). Further, research by Kayser-Jones and colleagues (1989) indicated that insufficient and inadequately trained nursing staff was a contributing factor to the deterioration and eventual hospitalization of nursing home residents.
Other research supports the notion that staffing is an important variable that influences eating behavior (Kayser-Jones, 1994). The consequences of inadequate staffing can include: (1) the feeding of residents in a hurried manner that does not preserve their dignity (e.g., giving residents a large amount of food with each bite, feeding several residents at once, mixing food), and (2) inadequate nutritional intake, resulting in weight loss in residents and necessitating the use of liquid supplements and sometimes tube feedings. These finding are supported by research conducted by Blaum and colleagues (in press), which shows low nutrition of residents associated with their being fed by staff.
Willcocks and colleagues (1987) also found that staff-oriented rather than resident-oriented practices were strongest in homes with the lowest staffing levels. Staff shortages resulted in dispensing with flexibility for both residents and staff and opting for formalization of the care regime in order to complete what was regarded as essential work. Homes with higher ratios of staff-to-resident hours and a higher proportion of part-time staff rather than full-time staff were more likely to have resident-oriented practices as well as higher levels of agreement between staff and residents about what constitutes ideal environmental features.
Many gerontologists have proposed that ombudsman programs and other forms of community presence could improve nursing home quality of care. Cherry (1991) compared the effects of community presence programs on quality of nursing care with a random sample of 134 Medicare-and Medicaid-certified long-term-care facilities in Missouri. The presence of an ombudsman program was found to be the most important factor associated with quality for intermediate care facilities and also was significantly associated with quality for skilled nursing homes where there was ample staffing of RNs.
Quality and Staff-Mix
Type of staff may be more important than the available staff hours. Willcocks and colleagues (1987) found that management staff in homes with a social model of care, as opposed to a medical model of care, had more resident-oriented views
on features of residential life, while care staff were more likely to express views that spring from organizational needs for routine. Since ideas about the provision of quality care are likely to flow from management and professional staff, available hours and organizational practices that permit them to demonstrate skilled care and supervise nonprofessional staff are necessary. Otherwise, supervisory staff can only carry out inspections to ensure that the worst practices are avoided.
Some experts believe that nursing homes that rely on predominately unskilled nursing staff jeopardize the quality of nursing home care (Shields and Kick, 1982). In a landmark study by Linn and colleagues (1977), higher levels of RN hours per patient were associated with improved functional status, survival, and the discharge of residents to the community. Other variables, however, such as higher cost, professional staff-to-patient ratios, better meal service, physical plant, and patient records were also associated with positive outcomes. Braun (1991), in an historical cohort study in which 390 veterans discharged to 11 nursing homes were followed for 6 months, found the quality variable "RN hours" was significantly and inversely related to mortality, while the quality variable "use of nursing process" was significantly related to probability of discharge. Using data from reports of 455 Medicare-certified skilled nursing facilities, Munroe (1990) found a positive, significant relationship between nursing home quality and the ratio of RN hours to licensed vocational nurse (LVN) hours per resident day. For every 25 percent increase in the ratio of RN hours to LVN hours, there was a decrease of 0.53 in the number of health-related deficiencies in the facilities.
In an analysis of data from the National Medical Expenditure Survey, Spector (1994) and a colleague found that higher per capita income and urban location led to more RNs employed in nursing homes. They also found that compared to for-profit homes, hospital-based and government nursing homes had more RNs and LPNs, but nonprofit homes had more RNs and fewer LPNs. In terms of outcomes, having a greater number of RNs was associated with fewer deaths annually, having more LPNs was associated with an increase in ADLs, and having more nurse aides had no impact. Spector reported less variation in nurse aide numbers across nursing homes than in RNs and LPNs, which may explain the failure to observe a nurse aide staffing effect on quality. Spector also found that states with higher Medicaid reimbursement levels had more LPNs per 100 residents, adjusted for case-mix. Although these states also tended to have more RNs, the relationship was not significant. Further, Spector found that in states where reimbursement was cost-based, more RNs were used but at the expense of LPNs. The implications of these findings for quality, however, were not straightforward. In a study of nursing homes in Rhode Island, Spector and Takada (1991) found that low RN and LPN turnover was related to greater functional improvements among residents. Spector (1994) noted that his findings support the notion that consistent RN leadership leads to better resident outcomes.
Attempts have been made to establish staff requirements for particular groups
of residents (Senior, 1978) or in accordance with prescribed tasks (Rhys-Hearn, 1979), but without regard for the quality of care or resident outcomes. When staff were allocated in accordance with nurses' identification of patients' optimal nursing requirements, Rhys-Hearn (1979) found that in no case was the care given equivalent to the care prescribed. Norwich (1980) noted that when "extra" time was available, it was spent in physical care activities rather than psychosocial or therapeutic support, a finding supported in research by Savage and coworkers (1979) about psychogeriatric wards. In an observational study of staff behaviors in a nursing home, Burgio and colleagues (1990) found that LPNs displayed significantly more patient care behaviors and nurse aides significantly more nonwork behaviors than other nursing staff. RNs displayed the least nonwork behavior. Although all staff used most of their time for work, the study results may support the need for more licensed staff for greater productivity and for supervision of assisting staff. However, more than a decade ago Eliopoulos (1983) presented mathematically derived staff models to argue that higher RN staffing would be financially insupportable, in that the cost per patient would almost double with an all RN staff.
Staffing level and mix provide important information about the organizational climate of a nursing home and the way in which care is provided, and may help to explain agitated psychomotor behaviors of residents as related to environmental and personal variables (Kolanowski et al., 1994). Specifically, in a study conceptually grounded in Kayser-Jones' (1989) model of environment and quality of life in nursing homes, Kolanowski and colleagues (1994) found that the addition of staff mix as an organizational variable significantly increased the amount of variance explained, over and above that contributed by personal variables of the residents such as functional ability, cognitive and health status, mood, sensory deficits, and psychotropic drugs prescribed. Residents on those units with a higher ratio of licensed personnel had fewer instances of problematic behaviors, suggesting that staff who have the knowledge to care for frail elders are less likely to use restraints to manage behavior. Findings in a study by Bleismer (1994) of nursing homes in Minnesota also support the positive relationship between licensed nursing staff and quality of care and the idea that licensed nurse leadership needs to be doing more than completing paper work and assuring recorded compliance with regulations. The study found that in the first year after patient admission, higher licensed nursing hours were significantly related to improved functional ability in the patient, decreased probability of patient death, and increased probability of discharge home. Thus the data suggest that licensed nurse leadership needs to be directly involved with resident care and staff guidance.
Even among the licensed staff, research has shown that nurses' perceptions and attitudes about problem behaviors in residents vary according to educational background and preparation (e.g., LPNs vs. RNs) (Burgio et al., 1988). Most RNs employed by long-term-care facilities have associate degrees, that is, two
years of training that includes little specialized training in gerontology or psychiatry. As noted earlier, in contrast to hospitals, where is it rare that DONs have less than a bachelor's degree and more often are at least master's prepared, DONs in nursing homes are often graduates of associate degree and diploma programs. Leadership and management are not part of the basic preparation offered by these programs and these DONs rarely have advanced training in gerontology. Turnover among DONs is also high, amounting to over 30 percent annually in Minnesota (Ryden, 1994).
"Nursing homes are beginning to use advanced practice nurses (gerontological nurse practitioners and specialists) to deal with the complex and multiple care needs of older persons in nursing homes. Their expert knowledge and skill in gerontological nursing has had a positive impact on reducing admissions to hospitals and reducing emergency room visits. Researchers at the University of Minnesota School of Nursing are currently involved in a 4-year study to look at clinical and cost outcomes with using advanced practice nurses in nursing homes" (C. Heine, personal communication, 1995).
Studies of advanced practice nurses, such as clinical nurse specialists and geriatric nurse practitioners, in nursing homes have shown that they can improve resident outcomes and contribute to quality by changing the focus from custodial to rehabilitative care (Kane et al., 1976, 1988), and by increasing the ability of facilities to care for more complex and acutely ill patients (Mezey and Scanlon, 1988). Nurse practitioners (NP) can enhance care and revenues by developing specialty services (e.g., bowel and bladder training programs, diabetes and wound management centers) that can be staffed by the general nursing staff and members of interdisciplinary teams. NPs can also serve as nurse managers in Medicare skilled units so that those units can develop higher quality, more technologically advanced subacute programs, and increase Medicare skilled care occupancy rates (Knapp, 1994).
Research by Evans and Strumpf (1994), investigating the relative effects of two experimental interventions delivered by GNSs on the use of physical restraints and resident and staff outcomes, found that staff mix and resident personal competence were important factors in the occurrence of disturbing behaviors likely to be managed by restraint. These disturbing behaviors occurred more frequently in situations where the availability of licensed nurses was low and resident frailty high. Further, although staff increased their assessment and intervention skills, the investigators noted the need for a "consistent professional presence" by a clinician with geriatric expertise to maintain minimal restraint use in the facility. Findings suggest that quality outcomes (e.g., restraint reduction) do not necessarily require more staff, but do require staff who have the requisite knowledge base and access to gerontological expertise, education, resident-centered assessment, monitoring, care planning, evaluation, and support in their efforts to provide quality individualized care (Evans and Strumpf, 1994; Strumpf, 1994).
A number of demonstrations have provided convincing evidence that GNPs and GNSs are effective in nursing homes. The Health Care Financing Administration (HCFA) supported the evaluation of two demonstration projects, the Robert Wood Johnson Foundation Teaching Nursing Home Program and the Nursing Home Connection, while the Kellogg Foundation supported the Mountain States program to place GNPs in nursing homes. These evaluations confirmed that nurses with advanced preparation in care of the elderly decrease unnecessary hospitalizations and use of emergency rooms, improve admission and ongoing patient assessments, provide better illness prevention and case finding, decrease incontinence, lower the use of psychotropic drugs and physical restraints, and generally improve the overall management of chronic and acute health problems. These improvements in care occurred without incurring additional costs, and in some instances at a reduced cost.
The experience of the Teaching Nursing Homes (TNH) provides further evidence of the need for professional gerontological nurses in nursing homes (Mezey, 1994). In comparing the TNHs with matched nursing homes in the same state, with the only difference being the presence of an advanced practice nurse in the TNHs, the TNHs had significantly fewer hospitalizations than the comparison homes and fewer emergency room visits. There also were notable improvements on a variety of quality indicators, such as management of urinary incontinence, decreased use of psychotropic medications including long-acting benzodiazepines and other such medications related to poor quality outcomes in nursing homes, and less use of restraints. Mezey (1994) noted that quality in some of the nursing homes was improved by increasing the number of RN FTEs, an observation that is not at all counterintuitive to the relationship between increased professional staff and improved practice. Ryden (1994) supports the assertion that RN leadership is a key to achieving quality outcomes in nursing homes.
Other research that tests interventions in nursing homes also supports the need for a continuous professional nurse presence to provide leadership and direction for assisting staff (Evans and Strumpf, 1989). For example, several researchers (Schnelle, 1990; Schnelle et al., 1990; Hawkins et al., 1992) tested management systems for nursing assistants to carry out interventions for incontinence that have shown significant improvements in resident dryness. According to Schnelle (1994), the interventions had a positive effect until the controlled conditions were withdrawn, when staff reverted to previous practices. In a multisite study, after the controlled conditions ceased, the management system and incontinence protocol were continued in only one of the sites. In this site the DON was particularly interested and involved. Schnelle (1994) concluded that it was the interest and leadership of this RN that resulted in the sustained use of the management system and intervention. Fries (1994) suggests, however, that with staff being forced to use the National Resident Assessment Instrument on a regular basis, it is hard to believe that staff will regress from the use of such interventions.
Some facilities use level of care or case-mix systems to allocate numbers and type of staff, with clinical nurse specialists available throughout the facility (Morris, 1994). According to Morris (1994), this systems approach allows for better decisions regarding number and type of staff needed, produces a better match between patient's need for care and the care provided, and improves resident outcomes. Thus, different categories of residents (e.g., short stay convalescent or rehabilitation, hospice residents, long stayers who have severe chronic mental and physical impairments) require very different staff numbers and skills.
Quality, Staff Satisfaction, and Turnover
There is no simple relationship between how staff regard the quality of their working life, staff turnover, and the quality of resident care, although most agree that dissatisfied staff are more likely to produce poor quality of care (Bond and Bond, 1987).
The behavior and attitudes of NAs can play a critical role in the quality of life of nursing home residents, and yet high attrition rates and alienation have been reported by nursing assistants. Mor (1995) noted that if aides are treated like "replaceable parts," then they are more likely to treat the residents in their care as "objects" as well, whereas active NA involvement in the care planning process may be related to quality of care. Research has demonstrated that long-term-care facilities that have lower bed-to-aide ratios, include NAs as part of the care team, value NAs' opinions, and acknowledge their important role in the provision of quality care, have lower turnover rates (Mor, 1995). Factors not related to NA turnover were: case-mix severity, payer source mix, facility size and ownership, and hours of aide training.
Survey data examining staff turnover rates in nursing homes have documented rates ranging from 55 to 65 percent for RNs. Turnover rates for NAs go up to 400 percent, with an average of around 99 percent. According to the Institute of Medicine (IOM, 1986), 45 percent of NAs left their jobs within the first three months and another 30 percent left within the first year of employment. Munroe (1990) reported an average of 107 percent turnover for the entire staff of 455 California nursing homes, with turnover significantly greater in proprietary homes. Thus, nurse aides, who provide somewhere between 80 percent and 90 percent of personal care, have the highest turnover of any nursing home staff (IOM, 1986).
Kane (1994) has argued persuasively that the frontline workers, including NAs, who most directly affect the daily experiences of nursing home residents receive the "least social investment" in terms of job training, wages, benefits, and social support. Because they have little autonomy in terms of altering their daily routine, these frontline workers may tend to focus more on the tasks than on the resident for whom the tasks are being performed, resulting in poor quality care.
A review of the research literature finds several studies suggesting that an
adequate number of well prepared and stable personnel is essential for quality care. The reciprocal relationship between quality of care and levels of staff turnover has been referred to since Revans (1964) found that high turnover of nurses in acute hospitals was related to length of patient stay. Garibaldi and colleagues (1981) found that the physical care of nursing home residents in the United States deteriorated during periods of high staff turnover, while Stryker (1981) hypothesized that depression, disengagement, disorientation, and isolation among long-term-care residents is likely to increase when staff-resident relationships are disrupted by high turnover. Thus, staff hours available, the relationships between full-time and part-time staff, and staff turnover are likely to be relevant to the quality of care. Further, staff turnover may be related to other circumstances associated with quality care. Mor (1994) found, for example, that in facilities where value was placed on involvement of nurse aides in the care planning process, there was a substantially lower turnover rate after controlling for a number of other theoretically relevant factors.
Job turnover can be costly in terms of hiring, training, and facility productivity losses, but perhaps most importantly high attrition rates can adversely affect sensorially impaired residents who do not cope well with frequent changes in staff (McDonald, 1994). Further, the effect of high turnover rates among nonprofessional staff is such that they fail to be assimilated into a sociocultural environment that fosters positive attitudes toward quality of care (Wright, 1988). Because residents value the relationship between the nursing assistant and themselves and consistency in the persons who deliver their care, high turnover, heavy use of part-time staff, and use of float or agency staff negatively impact the quality of care (Erickson, 1987). High turnover of RN and LPN staff compromises the continuity of leadership and supervision of staff as well as the treatment and care of residents.
Quality, Reimbursement, and Staffing
The relationship between reimbursement and staffing is complex, and the implications for quality are not straightforward. Cost-based and case-mix-based are two types of reimbursement schemes used for nursing homes. In cost-based reimbursement, a facility may supply services as needed and submit the resulting cost to the state for reimbursement. To control expenditures, some states place advance limits on each facility's rate, based on the prior year's cost per resident. Some states even "cap" the number of staff hours or the number of dollars per resident day, regardless of differing care needs. Such reimbursement limits can put a chilling effect on a nursing home's willingness to change its mix of residents by admitting residents supported by Medicaid or residents who require much care. In case-mix-based reimbursement, each resident is categorized according to a classification system that reflects the staff time and costs required for care of the residents in each category. The state determines a reimbursement rate
for each facility based on the number of residents it serves in each category. Case-mix formulas deserve careful scrutiny and a number of questions warrant further investigation. For example, are staff values derived from valid counts of time for care of each category of resident? Was the timed care what the resident needed, and was it performed by appropriately qualified staff? Does the reimbursement formula also include realistic time for assessments, care planning, and documentation? Does it allow for professional observation and evaluation of care, decision making and planning of care, and coordination with families and other disciplines involved in the care? Are compensation factors for each kind of nursing personnel realistic?
When reimbursement does not fully provide for the cost of care, nursing homes respond in a number of ways. They may increase private pay rates or seek to cut costs by increasing efficiency or reducing expenditures for services, including nurse staffing. Some nursing homes have been known to cut nourishment or supplies for the care of incontinent residents (Harrington, 1984). Changes in staffing may take the form of fewer full-time personnel and a greater proportion of less qualified personnel. Either of these "solutions" can have negative effects on work conditions and the quality of resident care.
Spector (1994) reported results from analysis of data from the 1987 National Expenditure Survey. Spector noted that if a state had a higher Medicaid reimbursement level, the higher level was associated with more LPNs per 100 residents adjusted for case-mix, but it was not related to the number of nurse aides. There were more RNs with higher Medicaid reimbursement, but the relationship was not significant. As discussed earlier, in states where there was a cost-based reimbursement system the nursing homes had more RNs, but fewer LPNs. Overall, Spector (1994) reported that while no relationship was found between reimbursement and outcomes, reimbursement had an effect on staffing and staffing had an effect on outcomes.
Current institutional long-term-care classification systems, such as the Resource Utilization Groups System (RUGS), separate persons with severe behavioral problems from those with primarily physical problems (Fries and Cooney, 1985). The RUGS-II revision continued to assume that emotional and cognitive problems do not complicate the care of the elderly person's physical problems, or the care of persons who can independently perform ADLs, in a way that adds appreciably to their care requirements or consumption of nursing resources (Rohrer et al., 1989). This assumption is not in keeping with data indicating, based on time records, that nursing home staff spend 36 percent of their time caring for residents with cognitive impairment (Hu et al., 1986).
Thus, case-mix-based reimbursement systems may actually discourage the delivery of therapeutic care by failing to fully account for the impact of mental illness or cognitive impairments on requirements for care (Rohrer et al., 1989). A study of 285 nursing home residents found that their behavioral problems influenced the care they received. Lack of cognitive ability caused staff to spend more
time in the delivery of personal care and medications, even when extent of physical disability was controlled for. Negative affect was found to increase the quantity of psychosocial care received, while aggressive behaviors had no effect on the types of nursing time studied. This interesting latter finding may reflect the lack of mental health therapy provided by nursing staff at the time the study was conducted (pre-OBRA), many of whom relied on restraints and/or sedation to manage aggressive residents (Rohrer et al., 1989). These data, together with other supporting literature, indicate that mental health problems clearly affect the amount of nursing time that elderly long-term-care residents require. This suggests that nursing homes must be reimbursed in a way that permits and encourages mentally ill and cognitively impaired residents to receive needed psychosocial services.
In 1989, the Health Care Financing Administration formally began a project to develop and test the RUGS classification in nursing homes on a national level. The Multi-State Nursing Home Case-Mix and Quality Project involved the design of a resident-level resource use classifications system for the prospective payment of Medicare and Medicaid nursing facility services. Kansas, Maine, Mississippi, and South Dakota participated in the project, with additional data contributed by Nebraska and Texas. A total of 6,660 resident assessments were used in the study. The analysis resulted in a 43-group classification system called Resource Utilization Groups System, Version III (RUGS-III) (Fries et al., 1994). The classification model will be used for a Medicare prospective payment system across all six states and New York and as the basis for Medicaid reimbursement to nursing homes in the first four project states.
Like RUGS-I and -II, RUGS-III is a category-based classification system. Nursing home residents are classified into one of the mutually exclusive groups of the system. Placement into a group is done by evaluating the fit with a sequence of three hierarchically arranged levels. The first major dimension is five categories of resident type: rehabilitation, special care, clinically complex, "impaired cognitive/behavior problem," and "physical functioning (reduced)." The second level looks at either intensity of care, extensive and special needs, or activities of daily living. Bed mobility, eating, toileting, and transfer are activities of daily living that are measured. A third level evaluates and rates activities of daily living, treatment count, additional nursing attention required for depression, and nursing rehabilitation. For the first time, nursing rehabilitation has been added as the third level for "impaired cognitively/behavior problem" and "physical functioning (reduced)." A toileting program performed by nurses is added to rehabilitation measures. Categories are listed hierarchically in order of cost from the highest, rehabilitation, to the lowest, physical functioning (reduced). Thus RUGS-III expands the number of categories in the classification and included the need for nursing resources for rehabilitation and treating depression, both of which were frequent criticisms of RUGS-I and -II. With RUGS-III revisions, the RUGS case-mix system, which recognizes the differences in the costs of caring
for distinct residents, currently appears to offer the best compromise between appropriate resources for each resident's needs and administrative feasibility, providing appropriate incentives and equitable reimbursement.
Quality and Type of Facility
Most research on the relationship of nursing home characteristics to quality of care has targeted two main areas: (1) the interrelationships among organizational characteristics, and (2) the relationship of organizational characteristics to resident functioning (Kruzich et al., 1992).
Research relating type of ownership to quality of care is equivocal. Although Elwell (1984) found that nonprofit homes are more likely to spend more money on direct patient care and have higher staff-to-patient ratios than proprietary homes, Kosberg and Tobin (1972), and more recently Kruzich and colleagues (1992), found no relationship between facility ownership and quality of care. Spector (1994) was unable to link type of facility with quality of care.
Little relationship has been found between type of ownership (e.g., for-profit vs. nonprofit) and RN and LPN nurse staffing ratios in a recent Massachusetts study (Kaffenberger, 1994). That is, for-profit homes did not use more LPNs instead of more highly trained RNs. The investigators speculate that the limited effect of ownership type may be due to many factors, such as the demanding regulatory environment, cost-based public payment, and the importance of quality to the private market.
Quality, Management Systems, and Organizational Climate
Management Systems
Management procedures are noted to play a critical role in the maintenance of staff performance (Sheridan et al., 1992). Direction, delegation, assertiveness, recognition, reprimand, liaison, and sensitivity are leadership dimensions that have been found to have significant effects on the job attitudes and job performance of nursing staff in nursing homes and hospitals (Sheridan et al., 1984; Sheridan et al., 1990). Mor (1994), however, found huge variation in the degree to which the authority and the management perspective of the DON in nursing homes is actually implemented.
Clear guidelines and monitoring systems, including contingent, supervisory feedback and praise, have been shown to effectively maintain staff behavior change and diminish the need for disciplinary procedures (Burgio and Burgio, 1990). Most staff management systems employ some type of ongoing performance monitoring and feedback, although they vary in terms of incentives and consequences related to staff performance (Burgio and Scilley, 1994). A study by Burgio and colleagues (1990), which compared the use of individual staff
performance feedback and group staff performance feedback, showed significantly greater compliance with prompted voiding regimens when individual staff performance feedback was used.
Permanent assignment of staff to residents results in more quality outcomes for residents and more satisfaction and feelings of accountability for employees. Evaluation of a primary care model of delivery of nursing aide care (e.g., permanent aide assignment, a team approach, and enhanced communication) in nursing homes demonstrated increased quality-of-care indicators such as improved behavior, affect, and social activities among residents (Teresi et al., 1993).
The importance of a staff management system was illustrated in research by Schnelle and colleagues (1990) that evaluated a prompted voiding procedure for urinary incontinence. The investigators found that the staff did not maintain the prompted voiding program without the Industrial Quality Control procedure in place. This procedure had three components: (1) a performance standard; (2) staff monitoring (by self and supervisors), and (3) quality control sampling. As noted above, Schnelle (1994) reported only one site where the protocols were continued. This occurred at a site where the DON provided leadership and direction to staff.
The work of Tellis-Nayak and Tellis-Nayak (1989, p. 312) suggests that those nursing homes that successfully break the hopeless cycle of high staff attrition, low morale, and indifferent care have managed to ''create an institutional structure that remains sensitive to the nurse's aides needs, nurtures their idealism, and values their central role." The relationships between social climate, quality of care, and resident health and well-being are increasingly being recognized. Indeed, while the recreational and physical environments have been shown to be important, nothing is more central to determining quality of life for residents than the social contacts and human relationships that emerge in the long-term-care setting (Kayser-Jones, 1989). Research supports the notion that social-environmental factors such as cohesion (the degree to which staff are perceived as being supportive) are significantly related to life satisfaction in residents (Gould, 1992), and that the sociocultural environment shapes staff attitudes, which then get translated into actions (Wright, 1988).
Organizational Climate
A typology of social climates in group residential facilities for older adults was developed by Timko and Moos (1991). Six distinct types of social climate were identified, including: supportive, self-directed; supportive, well-organized; open conflict; suppressed conflict; emergent-positive; and unresponsive. Those facilities with social climates in the first two categories—supportive, self-directed and supportive, well-organized—had residents who rated higher in well-being and levels of self-initiated activities and who used fewer health services.
Sheridan and colleagues (1992) argued that the climate the administrator
builds is key to the delivery of quality care, and that OBRA will likely fail because it restricts management initiatives and emphasizes punitive consequences of staff shortcomings. A study by Kayser-Jones (1989) reported that rehospitalization rates were affected as much by social-structural factors as by clinical factors, although Booth (1986) found no relationship between restrictiveness of the environment and rates of mortality and functional dependency. In their study of 530 nursing staff working in 25 for-profit and nonprofit nursing homes, Sheridan and colleagues (1992) found that staff members' job attitudes, opinions regarding elderly residents, and perceptions of the organizational climate varied between successful for-profit and nonprofit homes, but the human relations-oriented organization and cohesion climate in the unsuccessful homes was significantly lower than the climate in either the successful for-profit or nonprofit homes. There is also some evidence that involvement of staff in an interdisciplinary process for assessing and planning care is related to the psychological well-being of residents (Mor, 1994).
Case Study: The Iowa Veterans' Home
The following case study is presented as additional evidence that a higher ratio of RNs with specific gerontological preparation to assisting staff is related to improved quality of care in nursing homes. The case study also illustrates the importance of professional nurse involvement in resident assessment, delivery of care, and the direction and supervision of care delivered by assisting staff (Maas, 1989). A key to the delivery of quality care is that each resident has a specific RN who has authority and accountability for his or her care, 24 hours each day, and over an extended period of time. Formal and continuing education in geriatric and gerontological nursing for all nursing staff is another key to the achievement of quality outcomes for residents.
A model of professional nursing practice in a nursing home is demonstrated at the Iowa Veterans Home (IVH) in Marshalltown, Iowa (Maas, 1989). This model was developed in the late 1960s and early 1970s and has been in the process of implementation since that time. The professional governance model includes an RN nurse organization that determines all standards for nursing practice, policies governing practice, and nursing clinical programming.
The IVH is a state-owned long-term-care facility that provides nursing care to more than 800 mostly elderly veterans and spouses. Three levels of care are provided: residential, intermediate, and skilled. In 1988, about 12 percent of the residents required residential care, with the remainder nearly equally divided between intermediate and skilled care. In 1988 there were 70 RNs, 330 ancillary personnel, and 50 other health professionals. From 1983 through 1988, the average annual turnover among RNs was 5 percent, and the average length of employment for nurses who were on staff for this period was 7.5 years. Furthermore, in 1988 at the height of the nurse shortage, 50 RN applications were on file.
In contrast, an average length of stay of 1 year for RNs in nursing homes has been reported (Kayser-Jones, 1981a).
An interdisciplinary model is used to plan, implement, and evaluate health services for each resident. Core members of each interdisciplinary team are the resident's primary RN, social worker, dietitian, physician, and recreation therapist. Each RN has 24-hour, seven-days-a-week authority and accountability for a caseload of residents.
Before the professional model of practice was implemented, the philosophy of care was mostly custodial in nature. Registered nurses were assigned to shifts and patient care units as supervisors of the care delivered by the assisting staff, with little authority to decide matters that affected the quality of the residents' lives or health.
As the RNs progressed in the conceptualization and implementation of the professional practice model, they were aware of the need for additional nursing knowledge. The nurses determined that practice should be data-based whenever possible, that each nurse should specialize in the treatment of one or more of the nursing diagnoses of the long-term-care residents, and that the knowledge needed for accountability should be organized by the nursing diagnoses of the residents. The incidence of nursing diagnoses and interventions for the elderly and long-term-care clients determines priorities for continuing education and research. One illustration of the nurses' emphasis on knowledge and continuing education was the number who were certified by the ANA. In 1989, 33 nurses had been certified by the ANA as gerontological nurses, 1 as a mental health nurse, and 1 in community health. Thirty of the certified nurses were employed at IVH; five more nurses were preparing for the 1989 certification test. Thirty-five nurses had continued formal education in baccalaureate and master's programs. Since 1989, between five and eight RNs have been certified as gerontological nurses each year and five or six are enrolled in advanced education programs at any given time.
The nurses discovered that the results of interventions for nursing diagnoses included increased patient welfare and favor from families, administrators, and other health disciplines. There are a number of indicators of increased quality of nursing care. For example, the number of indwelling catheters and decubiti was much lower after the model of practice was implemented, even though the proportion of residents with complex nursing care problems increased. The rates of monitors of poor quality care also were consistently below the average rates for comparable long-term-care institutions. A descriptive study, "Nurse Autonomy and Patient Welfare," funded by the Division of Nursing in the National Institutes of Health, was conducted from 1972 to 1976 to document the process whereby nurses collectively developed professional governance and the consequences of this for residents. Data for a number of patient welfare measures (self-care scale, nurse- and resident-rated; well-being scale, resident-rated; problems inventory, resident-rated; resident interviews) were collected at regular intervals throughout
the study period. The trend for all measures was that resident welfare increased throughout the study period. The discrepancy between actual self-care and capacity to perform self-care decreased as rated by both nurses and residents, total scores for the well-being scale increased, and the problems inventory total scores decreased. Results of the resident interviews were consistent with the findings using the standardized measures, with more residents reporting satisfaction with their care and increased control over their lives at the end of the study (Maas and Jacox, 1977).
In addition, the IVH Nursing Department reports show that in the late 1960s and early 1970s, the monthly rate of skilled care residents with Foley catheters averaged 25 percent, whereas in the 1980s the average monthly rate of indwelling catheters was 7 percent for a larger group of skilled-care patients. Similarly, the average monthly decubitus rate was 8 percent in the early 1970s but in the 1980s averaged 4 percent, despite an increase in the numbers of debilitated, at-risk residents. The 1987 Iowa Department of Health and Iowa Foundation for Medical Care reports contain statistics for quality-of-care indicators for intermediate care facilities in Iowa. These statistics support the improved quality-of-care indicators at the IVH in contrast to all other intermediate care facilities in Iowa. Measures of the quality of the residents' lives also reflect achievement of high standards; for example, in the extent to which residents' rights to determine their care and to control other circumstances of living are protected and enabled.
Priority Questions Needing Further Research
Who Should Be in a Nursing Home?
Some researchers question whether or not certain residents currently in nursing homes should really be there. Morris and coworkers (1990) found a number of light care residents, according to the National Resident Assessment Instrument, in their data base. These data suggest that perhaps a substantial number of residents should have been discharged. Analysis of residents in facilities reimbursed using a case-mix formula indicated that the percentage of light care residents is less under these incentives.
- There is still a critical need for research to examine the role that nursing homes should play in long-term care, including what residents are best served by what types of facilities.
How Can Quality Best Be Measured?
Schnelle (1994) suggests that there is a myth associated with chart-based review of quality. Because of high regulatory pressure and specific standards for documentation, but little specificity as to how to actually meet regulations, chart
documentation systems are created that are largely fictional. Technology that provides specific directions for nurse aide behaviors, so as to meet regulations regarding the management of restraint use, has been developed. In research testing the effects of this technology, the actual release of restraints was monitored unobtrusively. Findings revealed that, as opposed to the "release every 2 hours and exercise" regulation, 60 percent of the residents who were restrained actually stayed restrained for 6 hours or longer. Yet on the chart there was very consistent documentation of release every 2 hours (Schnelle, 1994). Because most of the effort is put into compliance on paper, Schnelle argues that this creates a situation where both policy researchers and nursing home providers avoid real problem solving. OBRA, however, has placed more emphasis on monitoring actual patient outcomes in conjunction with chart review.
Based on her research, Baldwin (1994) believes that some outcome measures, such as quality-of-life and quality assurance measures used in other settings, may have to either be modified or developed specifically for nursing homes. Baldwin further suggests that qualitative data may convey more information about quality outcomes than the more traditionally used quantitative measures.
There are concerns about the reliability and validity of MDS data because of emphasis on regulations and the use of chart review to assess quality. Correlations between direct observation of quality indicators and MDS rating have been found to range between 0 to 0.75 (Schnelle, 1994). The use of consultant RNs, who are hired by some nursing homes to come in specifically to fill out the MDS, adds to concern about the reliability and validity of the data for measuring quality of care.
- Investigations to assess the reliability and validity of MDS data and to test other strategies for assuring the reliability and validity of quality care data in nursing homes are needed.
Wright (1988) has argued that the attitudes of nursing home personnel have been measured inappropriately, with scales based on negative stereotypes and inaccurate knowledge about the aged. She recommends reconceptualizing attitudes from those toward older people in general to attitudes toward behavior that is essential to the care of residents in nursing homes, including concepts of individualized care, rehabilitation potential, and choice. Wright also sets forth a proposed research model for examining staff attitudes and quality of care.
According to Burgio (1994), there are good, reliable quantitative measures of quality being used with developmentally disabled populations that are not being used in nursing homes. In general, Burgio asserts that the quality of care in nursing homes has been measured poorly.
- Additional research efforts should focus on reconceptualizing and evalu-
- ating measures of quality and staff characteristics that are hypothesized to be related to quality outcomes.
What Are the Effects of Organization, Staff, and Staffing Characteristics on Quality?
Results from a recent survey conducted by Decision Data Collection, Inc., for the ANA (ANA, 1995) indicate that reduction of the RN work force by cutting nursing budgets in hospitals is causing unsafe conditions for patients and massive increases in the workload of the remaining RNs. The survey found more medication errors, accidents resulting in patient falls and fractures, and unnecessary inconveniences for patients. Concerns expressed were primarily in the areas of insufficient time to spend with patients and to monitor their conditions adequately. In light of 1990 data from the ANA, which indicated that 66 percent of nursing homes reported increased nurse workloads and more nurse hours worked (McKibbin, 1990), there is some cause for concern about increased workload having a similar impact on quality of care in the long-term-care industry. According to Close and colleagues (1994, p. 26), "Patterns of workload increases and staff turnover may indicate unintended and unanticipated responses in the long-term care labor arena to policies intended to control acute care costs and to improve the quality of care to long-term care recipients." Therefore, the following areas of research need to be addressed.
- There is a critical need to study causes and circumstances of employment, staff relations, and work that promote staff job satisfaction and retention, and to test strategies for retention of NAs, LPNs, RNs, and DONs in nursing homes.
- Additional needs are to systematically study the effects of different numbers of staff, staff mix, and staff-to-resident ratios on resident outcomes, including resident and staff abuse and controlling for case-mix and organization structure variables.
- More research also is needed to assess and test the effects of staff's abilities to manage patients with varying levels of professional nurse consultation, direction, and oversight.
- The advantages and disadvantages of part-time versus full-time staff for achieving quality outcomes should be systematically examined.
- Clearly, the etiology and appropriate management of aggressive behaviors of nursing home residents against staff, and vice versa, is an area deserving of more research.
- Further studies also are needed to better understand the specific causes of elder abuse and to test interventions for institutional staff and families that are designed to prevent instances of abuse.
- Experimental research focusing on relationships between nurses and resi-
- dents and on the effectiveness of interventions designed to control resident behavior, other than chemical and physical restraints, are especially needed.
Efforts to improve nursing home care through training and job redesign have had mixed results (Smyer et al., 1991). Job redesign was implemented by a team of Penn State investigators to enhance motivation and change the nature of the work itself by making it the focus of a guided staff process. Findings revealed that improvements in staff knowledge had little impact on NA job performance as reflected in the ratings of supervisors, suggesting that training alone will not dramatically improve the quality of care and quality of life in nursing homes (Smyer et al., 1991). - Research needs include: (1) descriptive studies of what licensed nurses and other staff do in nursing homes, distinguishing among advanced practice nurses (e.g., GNPs, GCNs, RNs, and LPNs); (2) studies that examine how DONs and RNs provide effective leadership and direction of staff; (3) studies that evaluate and compare the most effective use of RNs and LPNs in nursing home settings; (4) studies to test a variety of management interventions on staff satisfaction and performance and resident outcomes; and (5) studies to design and test technologies that specify clinical interventions and assist staff with their implementation.
Few studies have examined the relationship between macro-organizational and structural variables and quality; thus, there is a paucity of empirical evidence to support these linkages. To date, research findings have shed little light on the characteristics of nursing homes (such as size, ægis, age, and rural or urban location) that might inform our understanding of what results in quality care. - More research assessing the relationships among organization characteristics and quality outcomes should be conducted.
How Are Families Involved in Care and What Do They Understand About Quality and its Cost?
Questions about family member involvement in the care of their institutionalized relatives continue to be of interest. Some argue that there is the potential to augment staff resources and improve the quality of care in nursing homes by involving families more in the care of residents (Brubaker, 1987; Buckwalter and Hall, 1987; Bowers, 1988; Maas et al., 1994).
- Based on the current literature and research findings, more research is needed to document: (1) how families and nursing home staff can best work together to achieve quality care outcomes, (2) what families and the public under-
- stand about quality and its costs, and (3) at what level of quality are families and the public willing to assume costs?
What Are the Effects of Cultural Differences Among Residents and Staff in Nursing Homes and What Strategies Are Needed to Ensure Quality?
- Based on the review of cultural diversity issues in nursing homes, research is needed to describe: (1) the ability of racial and ethnic minority elderly and their families to mobilize community resources; (2) the access of these elderly to informal caregivers; (3) perceptions of alienation experienced by minority elderly residents and their families; and (4) minority families' perceptions of social, medical, and functional factors resulting in nursing home admission.
- More research related to ethnicity and race is needed to help determine the approach and perspective older persons take toward the problems they encounter in adapting to institutionalization.
- Research also is needed to describe cultural differences: (1) among elderly residents and staff who are members of the same ethnic and racial groups; (2) among staff who are members of different age, ethnic, and racial cultures; and (3) among residents of different racial and ethnic groups. In addition, strategies must be tested for: (1) educating staff and residents about cultural differences, and (2) incorporating the appropriate cultural practices into care and staff-resident relationships so that care is culturally competent.
Policy Recommendations
Long-term care must be part of any health care reform in order to ensure funds, care, and dignity for the elderly served. The predominance of chronic conditions requires the development and testing of new models of care that effectively bridge acute and long-term-care services. The relationship of staffing and quality of care is a primary concern in policy reforms. Based on the review of the historical background of nursing homes, the current status and future demand for nursing home care, and research relevant to the linkage of staffing and quality care, the following policy recommendations are set forth.
|
Recommendation 1: |
The minimum standards for the number of RNs in nursing homes should be increased. |
|
Recommendation 2: |
At least one RN for every 50 residents, in addition to the DON, should be required to be present daily over each 24-hour period of care. |
|
Recommendation 3: |
Every RN employed by a nursing home should be required to have specific formal education in gerontological nursing and in the management and supervision of assisting staff. At least 50 percent of continuing education credits for relicensure should be in these content areas as well. |
|
Recommendation 4: |
The minimum qualification for a DON in a nursing home should be a bachelor's degree in nursing. |
|
Recommendation 5: |
Every nursing home should be required to have at least one advanced gerontological nurse practitioner in their employ to provide both direct resident care and leadership for other nursing staff in caring for residents and monitoring quality outcomes. |
|
Recommendation 6: |
Compensation for qualified RNs and all nursing staff in nursing homes should be required to be more competitive with that provided by hospitals. |
|
Recommendation 7: |
Medicaid, Medicare, and other third party payers should be required to reimburse master's and doctorally prepared advanced practice nurses (GNPs and GCNs) for their clinical services. |
A recurrent theme throughout this review was the need for a consistent professional nurse (RN, NP) presence in nursing homes for the provision of quality care. This paper emphasized the need for RN leadership, direction, and supervision of assisting nursing staff because: (1) there is high turnover among assisting staff; (2) assisting staff have minimal training; (3) nurse aide work is difficult, often unpleasant, and rewards are few—circumstances that will likely worsen with the trend toward more acutely ill and frail future nursing home residents; (4) assisting staff need help coping with stress and maintaining quality, individualized care of residents; (5) salaries and benefits lag behind those in hospitals and home care, compromising the recruitment and retention of quality staff; (6) adding assisting staff without increased direction and supervision is likely to result in an inappropriate use of time and resources; (7) while mandated standardized assessment (e.g., MDS, RAI) does help to get resident problems identified, it does not provide for solutions to the problems or get the care provided; (8) there is some empirical evidence that the number of RNs in nursing homes is linked with positive resident outcomes; and (9) there is need for supportive and motivating systems to manage staff performance. Administrators also must recognize the importance to nurses of the authority to manage patient care issues and make clinical decisions.
|
Recommendation 8: |
Require case-mix reimbursement with higher levels of reimbursement and higher minimum staffing standards. |
To promote recruitment and retention of qualified staff in long-term care and to make nursing homes a more attractive and satisfying practice setting, salaries need to be more competitive with those for comparable positions in other settings. Nursing homes also must be reimbursed in a way that permits and encourages all residents, including the mentally ill and cognitively impaired, to receive needed physical and psychosocial services.
A goal in long-term care is to move from a custodial to a rehabilitative model
of care. With the majority of direct care provided by nurse aides, this cannot be accomplished when staff-to-patient ratios are high (e.g., 1 staff person to 20 residents). However, it is known that nursing homes can have low staff-to-resident ratios and still have poor quality care. Thus, greater staff numbers must be combined with the recommendations for increased staff training, strategies to decrease turnover rates, and more intensive supervision and direction of nurse aides by qualified RNs. One aspect of training that must be improved is that provided by effective role models who supervise and consult with staff, as well as unit delivering resident care, when they are on the unit.
|
Recommendation 9: |
Require improved training of nursing home surveyors as consultative overseers who interpret and apply standardized state and federal mandated guidelines for quality-of-care assessment. |
Because of the variation in the quality of surveyors and the interpretations of guidelines, combined with the increase in surveyors for different regulators, nursing homes deserve to be assured that all surveyors have comparable skills and are applying standards correctly, judiciously, and equitably toward the goal of improved resident care.
|
Recommendation 10: |
Require nursing homes to provide a minimum of three hours of didactic and three hours of supervised practicum education annually for staff and family members on techniques for managing and preventing disruptive and aggressive resident behaviors. |
|
Recommendation 11: |
Require nursing homes to educate families and staff, both at the time of resident admission and with periodic reinforcement, about how to interact with each other to be mutually supportive and to recognize quality care outcomes. |
Staff and family members need to have the knowledge and skills that best prepare them to understand and recognize quality resident outcomes, to be better able to establish cooperative relationships, and to share decisions so that the optimal resources of both staff and families are used to achieve quality outcomes. Staff and families need to recognize families as allies and resources in the care of elderly residents, and acknowledge the need for staff to involve family members in decisions about the care of their loved ones. Staff also should encourage the negotiation of family-staff partnerships in the care of residents, which may be an important aspect of delivering quality nursing home care.
|
Recommendation 12: |
Require nursing homes to provide education programs for staff on the cultural beliefs, values, and practices of ethnic and racial minority residents. |
|
Recommendation 13: |
Require nursing homes to attempt to hire staff representatives of ethnic and racial minority groups of which residents are members. |
With increasing cultural diversity among elderly residents and staff in nursing homes, the achievement of quality outcomes requires that staff have an understanding of the values and practices that are important to the quality of life of residents and to satisfying and effective work relationships among staff. Minority elders need available gerontological services that are affordable, accessible, and culturally competent.
|
Recommendation 14: |
More opportunities for formal educational preparation in gerontological nursing should be provided by: (1) enhancing opportunities for mid-career nursing faculty to continue learning and to obtain gerontological content through the provision of faculty development awards, fellowships, short term courses, certificate programs, continuing education, and opportunities to work with master teachers in gerontology; (2) development of gerontological nursing education related to special populations of the diverse elderly; (3) merging the categories of geriatric nurse clinical specialists and geriatric nurse practitioners, and preparing geriatric nurses in advanced practice roles to provide primary and comprehensive care to the elderly in nursing homes; (4) developing model geriatric nursing curricula that incorporate advanced information technologies at both undergraduate and graduate levels; (5) offering freestanding undergraduate gerontological nursing courses that are available to all undergraduate students; (6) mandating continuing education credits (a minimum of 1 credit per year in gerontological nursing for re-licensure); (7) providing traineeships for faculty and student training in gerontological nursing; (8) continuing to emphasize the need to increase numbers of minorities in gerontological nursing; and (9) promoting interdisciplinary training and consultation. |
Nursing faculty who have learned gerontological and geriatric content and skills are more likely to support the introduction of gerontological content in curricula and improve the quality of education in both undergraduate and advanced practice programs. Education in gerontology must recognize the specific characteristics and needs of various populations in America such as rural Americans, aging women, and older adults with mental health problems. Thus it is no longer relevant to discuss persons over 65 as a homogenous group. More advanced nurse practitioners are needed to meet the complex and growing future needs of the aging population, and to lead, teach, and provide patient care in nursing homes. For nursing to prepare sufficient numbers of expert gerontological clinicians, appropriate curricula must be implemented at all levels of the educational process and evaluated to ensure they meet minimum standards. Funding for enhanced training opportunities for faculty and graduate students will increase the knowledge base that supports geriatric nursing practice. There also is
a need to prepare more nurses with geriatric knowledge to meet the demands for the future, including an increased number of persons from minority groups. All gerontological and geriatric nurses, educators, and clinicians will need to regularly update their knowledge base in gerontology. Adequate compensation for nurses who work with the elderly needs to be assured to provide incentives for increased recruitment and retention of qualified nurses in nursing homes.
Advanced information technologies (i.e., fiber optic and digital networks) will increasingly be used in settings remote from educational institutions. Nurses will need to be proficient in the use of such technologies in order to provide care to elders and education to staff. Finally, because geriatric care in the next century will be increasingly interdisciplinary, students from a variety of disciplines should be exposed to interdisciplinary care in their training if they are to be expected to practice in a cooperative, collegial manner.
|
Recommendation 15: |
Increased funding for gerontological nursing research should be provided by: (1) increasing the number of postdoctoral opportunities in gerontological nursing to prepare future researchers, (2) increasing the level of funding to NINR for gerontological research, (3) encouraging GECs and Centers on Aging to hold geriatric nursing faculty training workshops in grantsmanship and proposal development, and (4) increasing funding for faculty and doctoral student training in gerontological research. |
Geriatric nursing research has benefited older persons by improving care practices and quality of life, and yet nurses have not fared well in terms of successfully competing for NIH monies in aging-related research. In some cases it is because the quality of the proposals submitted (especially with regard to methodological rigor) is not sufficient to merit consideration for funding. Those gerontological nurse researchers who are fully qualified and produce competitive research proposals are disadvantaged by the disproportionately low level of funding for NINR, which must fund all nursing research, and the competition for limited funds from other NIH agencies. This situation is particularly unfortunate in that the relationship between education, research, and practice should be a dynamic one, with research informing practice and teaching and with more curricula being research driven.
|
Recommendation 16: |
A provider number for the accountable RN and standardized nursing interventions should be added to the long-term-care minimum data set so that practice pattern variations and outcomes effectiveness can be assessed for specific interventions and nurse providers with MDS data. |
References
AARP (American Association of Retired Persons). A Portrait of Older Minorities. Washington, D.C.: AARP, 1985a.
AARP. A Profile of Older Americans 1985. Washington, D.C.: AARP, 1985b.
AARP Minority Affairs. A Portrait of Older Minorities. Washington, D.C.: AARP, 1990.
Alzheimer's Association. Residential Settings: An Examination of Alzheimer Issues. Chicago: Alzheimer's Association, 1994.
ANA (American Nurses Association). Report on Long-Term Care Staffing. Kansas City: ANA, 1991.
ANA. The Report of Survey Results: The 1994 ANA Layoffs Survey. The American Nurse (March):1 and 7, 1995.
Andreoli, K.G., and Musser, L.A. Trends That May Affect Nursing's Future. Pp. 71–80 in: B.W. Spradley, ed. Readings in Community Health Nursing, 4th ed. Boston: Little, Brown, 1991.
Bahr, R.T. The Battered Elderly: Physical and Psychological Abuse. Family and Community Health 4(2):61–69, 1981.
Bahr, R.T. Reaction to the Invitational Conference: ''Mechanisms of Quality in Long-Term Care: Service and Clinical Outcomes." Pp. 103–109 in: Mechanisms of Quality in Long-Term Care: Service and Clinical Outcomes. Pub. no. 41-2382. New York: National League for Nursing Press, 1991.
Baker, A. Granny Battering. Nursing Mirror 144:65–66, 1977.
Baldwin, B. Presentation at special session on staffing and quality care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Baltz, T.M., and Turner, J.G. Development and Analysis of a Nursing Home Aide Screening Device. The Gerontologist 17:66–69, 1977.
Barresi, C.M., and Stull, D.E., eds. Ethnic Elderly and Long-Term Care. New York: Springer Publishing, 1993.
Beck, C.M., and Ferguson, D. Aged Abuse. Journal of Gerontological Nursing 7(6):333–336, 1981.
Beck, C., Rossby, L., and Baldwin, B. Correlates of Disruptive Behavior in Cognitively Impaired Elderly Nursing Home Residents. Archives of Psychiatric Nursing 5(5):281–291, 1991.
Belgrave, L.L., and Bradsher, J.E. Health as a Factor in Institutionalization: Disparities Between African Americans and Whites. Research on Aging 16(2):115–141, 1994.
Birkenstock, M. From Turnover to Turnaround. Geriatric Nursing 12(4):194–196, 1991.
Blaum, C.S., Fries, B.E., and Fiatarone, M.A. Factors Associated with Low Body Mass Index and Weight Loss in Nursing Home Residents. Journals of Gerontology: Medical Sciences, in press.
Bleismer, M. Outcomes of Minnesota Nursing Home Residents and Their Relationship to Structural and Process-Related Attributes (Doctoral dissertation, Rush University, 1994). Dissertation Abstracts International, 1994.
Bond, J., and Bond, S. Developments in the Provision and Evaluation of Long-Term Care for Dependent Old People. Pp. 47–85, in: P. Fielding, ed. Research in The Nursing Care of Elderly People. New York: John Wiley and Sons, 1987.
Booth, T. Institutional Regimes and Induced Dependency in Homes for the Aged. The Gerontologist 26:418–423, 1986.
Bowers, B. Family Perceptions of Care in a Nursing Home. The Gerontologist 28:361–368, 1988.
Brannon, D., Streit, A., and Smyer, M. The Psychosocial Quality of Nursing Home Work. Journal of Aging and Health 4(3):369–389, 1992.
Braun, B.I. The Effect of Nursing Home Quality on Patient Outcome. Journal of American Geriatric Society 39:329–338, 1991.
Brown University Long-term Care Quality Letter. National Center for Health Statistics Studies Nursing, Board and Care Homes. 6(12):8, 1994.
Brubaker, T.H., ed. Aging, Health and Family. Newbury Park, Calif.: Sage Publications, 1987.
Buckwalter, K.C., and Hall, G.R. Families of the Institutionalized Older Adult: A Neglected Resource. In: T.H. Brubaker, ed. Aging, Health and Family. Newbury Park, Calif.: Sage Publications, 1987.
Burgio, L.D. Presentation at special session on staffing and quality care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Burgio, L.D., and Burgio, K.L. Institutional Staff Training and Management: A Review of the Literature and a Model for Geriatric, Long-term Care Facilities. International Journal of Aging and Human Development 30(4):287–302, 1990.
Burgio, L.D., and Scilley, K. Caregiver Performance in the Nursing Home: The Use of Staff Training and Management Procedures. Seminars In Speech and Language 15(4):313–322, 1994.
Burgio, L.D., Butler, F., and Engel, B. Nurses' Attitudes towards Geriatric Behavior Problems in Long-Term Care Settings. Clinical Gerontologist 7(3/4):23–34, 1988.
Burgio, L.D., Engel, G.T., Hawkins, A., McCormick, K., and Scheve, A. A Descriptive Analysis of Nursing Staff Behaviors in a Teaching Nursing Home: Differences Among NAs, LPNs, and RNs. The Gerontologist 30:107–112, 1990.
Cassell, E.J. Abuse of the Elderly: Misuses of Power. New York State Journal of Medicine (March):159–162, 1989.
Caudill, M.K., and Patrick, M. Costing Nurse Turnover in Nursing Homes. Nursing Management 22(11):61–64, 1991.
Cherry, R.L. Agents of Nursing Home Quality of Care: Ombudsmen and Staff Ratios Revisited. The Gerontologist 31:302–308, 1991.
Chiodo, L.K., Kanten, D.N., Gerety, M.B., Mulrow, C.D., and Cornell, J.E. Functional Status of Mexican American Nursing Home Residents. Journal of The American Geriatrics Society 42:293–296, 1994.
Cleary, T.A., Clamon, C., Price, M., and Shullaw, G. A Reduced Stimulation Unit: Effects on Patients with Alzheimer's Disease and Related Disorders. The Gerontologist 28:511–514, 1988.
Close, L., Estes, C.L., Linkins, K.W., and Binney, E.A. A Political Economy Perspective on Frontline Workers in Long-Term Care. Generations XVIII(3):23–27, 1994.
Constable, J.F., and Russell, D.W. The Effect of Social Support and the Work Environment upon Burnout Among Nurses. Journal of Human Stress 12:21–26, 1986.
Coons, D. Training Direct Service Staff Members to Work in Dementia Care Units. Pp. 126–143 in: D. Coons, ed. Specialized Dementia Care Units. Baltimore: The Johns Hopkins University Press, 1991.
Cronin-Stubbs, D., and Rooks, C. The Stress, Social Support, and Burnout of Critical Care Nurses: The Results of Research. Heart-Lung 14:31–39, 1985.
Cuellar, J. Aging and Health: American Indian/Alaska Native Elders. Stanford, Calif: Stanford Geriatric Education Center, 1990.
Davis, M.A. On Nursing Home Quality: A Review and Analysis. Medical Care Review 48(2):129–166, 1991.
Dey, S.E. The Shift from Nursing Homes to Care at Home. International Psychogeriatrics 21–22, 1994.
DHHS (U.S. Department of Health and Human Services). Elder Abuse. Washington, D.C., U.S. Government Printing Office, 1980.
DHHS. Health Personnel in the United States. Eighth Report to Congress. Washington, D.C.: U.S. Government Printing Office, 1991.
DHHS. An Agenda for Health Professions Reform. Rockville, Md.: Bureau of Health Professions, 1993.
Duncan, M.T., and Morgan, D.L. Sharing the Caring: Family Caregivers' Views of Their Relationships with Nursing Home Staff. The Gerontologist 34:235–244, 1994.
Elders of Color. Geriatric Care News 17(9):1732–1733, 1991.
Eliopoulos, C. Nurse Staffing in Long-Term Care Facilities: The Case Against a High Ratio of RNs. Journal of Nursing Administration 10:29–31, 1983.
Elwell, F. The Effects of Ownership on Institutional Services. The Gerontologist 24:77–83, 1984.
Erickson, J. Quality and the Nursing Assistant. Provider 13(4):4–6, 1987.
Espino, D.V., Neufeld, R.R., Mulvihill, M., and Libow, L.S. Hispanic and Non-Hispanic Elderly on Admission to the Nursing Home: A Pilot Study. The Gerontologist 28:821–824, 1988.
Evans, L.K., and Strumpf, N.E. Tying Down the Elderly. Journal of the American Geriatrics Society 37:65–74, 1989.
Evans, L.K., and Strumpf, N.E. Reducing Restraints in Nursing Homes: A Clinical Trial. Paper presented at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontology Society of America, Atlanta, Georgia, November 1994.
Everitt, D.E., Fields, D.R., Soumerai, S.S., and Avorn, J. Resident Behavior and Staff Distress in the Nursing Home. Journal of The American Geriatric Society 39:792–798, 1991.
Fackelmann, K.A. Critics Cite Flaws in HHS' New System for Inspection of Nursing Homes. Modern Healthcare 16(3):27, 1986.
Foner, N. Nursing Home Aides: Saints or Monsters? The Gerontologist 34:245–250, 1994.
Fottler, M., Smith, H., and James, W. Profits and Patient Care Quality in Nursing Homes: Are They Compatible? The Gerontologist 21:532–538, 1991.
Francese, T., and Mohler, M. Long-term Care Nurse Staffing Requirements: Has OBRA Really Helped? Geriatric Nursing 15(3):139–141, 1994.
Fries, B.E. Presentation at special panel session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Fries, B.E., and Cooney, L.M. Resource Utilization Groups: A Patient Classification System for Long-Term Care. Medical Care 23:110–122, 1985.
Fries, B.E., Schneider, D.P., Foley, W.J., et al. Refining a Case-Mix Measure for Nursing Homes: Resource Utilization Groups (RUG-III). Medical Care 32(7):668–685, 1994.
Ganroth, L. Long-term Care Resource Requirements Before and After the Prospective Payment System. Image 20(1):7–11, 1988.
Garibaldi, R.A., Brodine, R.N., and Matsumiya, S. Infections Among Patients in Nursing Homes. New England Journal of Medicine 305:731–735, 1981.
Goldin, G.J. The Influence of Self-Image upon the Performance of Nursing Home Staff. Nursing Homes 34:33–38, 1985.
Goodwin, M., and Trocchio, J. Cultivating Positive Attitudes in Nursing Home Staff. Geriatric Nursing 8(1):32–34, 1987.
Gould, M. Nursing Home Elderly: Social-Environmental Factors. Journal of Gerontological Nursing 18(8):13–20, 1992.
Greene, J.A., Asp, J., and Crane, N. Specialized Management of the Alzheimer's Disease Patient: Does It Make a Difference? Journal of The Tennessee Medical Association (September):559–563, 1985.
Greene, V.L., and Monahan, D.J. Comparative utilization of community-based long-term care services by Hispanic and Anglo elderly in a case management system. Journal of Gerontology 39, 730–735, 1984.
Griffin, K.M., Leftwich, R.A., and Smith, M.S. Current Forces Shaping Long-term Care in the 1990s. The Journal of Long-Term Care Administration 17(3):8–11, 1989.
Hall, G.R. OBRA, MDS, and RAPS In NFs: Learning The Language of Long-Term Care. Paper presented at Psychiatric Nursing Retreat, University of Iowa Hospitals and Clinics, Iowa City, March 1995.
Hall, G.R., and Buckwalter, K.C. From Almshouse to Dedicated Unit: Care of the Institutionalized Elderly with Behavioral Problems. Archives of Psychiatric Nursing VI(1):3–11, 1990.
Hall, G., Kirschling, M.V., and Todd, S. Sheltered Freedom: An Alzheimer's Unit in an ICF. Geriatric Nursing 7(3), 132–137, 1986.
Hare, J., and Pratt, C.C. Burnout: Differences Between Professional and Paraprofessional Nursing Staff in Acute and Long-Term Care Health Facilities. The Journal of Applied Gerontology 7:60–71, 1988.
Harper, M.S., and Alexander, C.D. Profile of the Black Elderly. In: M.S. Harper, ed., Minority Aging: Essential Curricula Content for Selected Health and Allied Health Professionals. Washington, D.C.: U.S. Government Printing Office, 1990.
Harrington, V.L. Nursing Home Abuse: The Tragedy Continues. Nursing Forum 21(3):102–108, 1984.
Hawkins, A.L., Burgio, A.L., and Engel, B. The Effects of Verbal and Written Supervisory Feedback on Staff Compliance with Assigned Prompted Voiding in a Nursing Home. Journal of Organizational Behavior Management 13:137–150, 1992.
Heine, C.A. Burnout Among Nursing Home Personnel. Journal of Gerontological Nursing 12(3):14–18, 1986.
Hickey, T., and Douglass, R.L. Mistreatment of the Elderly in the Domestic Setting. American Journal of Public Health 71:502, 1981.
Holmes, D., Teresi, J., and Holmes, M. Evaluation of the Costs of Caring for the Senile Demented Elderly: A Pilot Study. The Gerontologist 26:158–163, 1983.
Hospital and Healthcare Compensation Service. The 1994–1995 Home Care Salary and Benefits Report. Oakland, N.J.: Hospital and Healthcare Compensation Service, 1994.
Hu, T., Huang, L., and Cartwright, W.S. Differences Among Black, Hispanic, and White People in Knowledge about Long-Term Care Services. Health Care Financing Review 2:51–67, 1986.
IOM (Institute of Medicine). Improving the Quality of Care In Nursing Homes. Washington, D.C.: National Academy Press, 1986.
John, R. The Health of Research on American Indian Elders' Health, Income Security, and Social Support Networks. Pp. 38–50 in: Gerontological Society of America. Minority Elders: Longevity, Economics and Health—Building a Public Policy Base. Washington, D.C.: Gerontological Society of America, 1991.
Jones, D.C. Spatial Proximity, Interpersonal Conflict, and Friendship Formation in the Intermediate Care Facility. The Gerontologist 15:150–154, 1975.
Jones, D.C., and Van Amelsvoort Jones, G.M.M. Communication Patterns Between Nursing Staff and the Ethnic Elderly in a Long-Term Care Facility. Journal of Advanced Nursing 11:265–272, 1986.
Jones, D.C., Bonito, A., Gower, J., and Williams, R. Analysis of the Environment for Recruitment and Retention of Registered Nurses in Nursing Homes. Washington, D.C.: Bureau of Health Professions, Health Resources and Services Administration, U.S. Department of Health and Human Services, 1987.
Kaffenberger, R. Do Profit Oriented Ownership Decisions Lead to More Use of LPNs versus RNs in Nursing Homes? Paper presented at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Kalisch, P., and Kalisch, B. The Advance of American Nursing. Boston: Little, Brown, 1978.
Kane, C. The Outpatient Comes Home: The Family's Response to Deinstitutionalization. Journal of Psychosocial Nursing and Mental Health Services 22:19–25, 1984.
Kane, R.A. Ethics and the Frontline Care Worker: Mapping the Subject. Generations XVIII(3):71–75, 1994.
Kane, R.L., and Kane, R.A. A Nursing Home in Your Future? New England Journal of Medicine 324(9):627–628, 1991.
Kane, R.L., Jorgenson, L.A., Teteberg, B., and Kuwahara, J. Is Good Nursing Home Care Feasible? Journal of the American Medical Association 235:516–519, 1976.
Kane, R.A., Kane, R.L., Arnold, S. et al. Geriatric Nurse Practitioners as Nursing Home Employees: Implementing the Role. The Gerontologist 28:469–477, 1988.
Kayser-Jones, J. A Comparison of Care in a Scottish and United States Facility. Geriatric Nursing 2:44–50, 1981a.
Kayser-Jones, J. Old, Alone, and Neglected. Berkeley and Los Angeles, Calif.: University of California Press, 1981b.
Kayser-Jones, J. The Environment and Quality of Life in Long-Term Care Institutions. Nursing and Health Care 10(3):124–130, 1989.
Kayser-Jones, J. The Use of Nasogastric Feeding Tubes in Nursing Homes: Patient, Family and Health Care Provider Perspectives. The Gerontologist 30:469–479, 1990.
Kayser-Jones, J. Presentation at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Kayser-Jones, J.S., Wiener, C.L., and Barbaccia, J.C. Factors Contributing to the Hospitalization of Nursing Home Residents. The Gerontologist 29:502–510, 1989.
Kemper, P., and Murtaugh, C.M. Lifetime Use of Nursing Home Care. New England Journal of Medicine 324(9):595–601, 1991.
Kermis, M.D. Equity and Policy Issues in Mental Health Care of the Elderly: Dilemmas, Deinstitutionalization, and DRGs. The Journal of Applied Gerontology 6(3):268–283, 1987.
Knapp, M. Nurse Practitioners: Expanded Role in Long-Term Care. The Brown University Long-term Care Quality Letter 6(5):1–2, 1994.
Kolanowski, A., Hurwitz, S., Taylor, et al. Contextual Factors Associated with Disturbing Behaviors in Institutionalized Elders. Nursing Research 43(2):73–79, 1994.
Kosberg, J., and Tobin, S. Variability Among Nursing Homes. The Gerontologist 12:214–219, 1972.
Krout, J.A. The Aged in Rural America. New York: Greenwood Press, 1986.
Kruzich, J.M., Clinton, J.F., and Kelber, S.T. Personal and Environmental Influences on Nursing Home Satisfaction. The Gerontologist 32:342–350, 1992.
Kurowski, B.D., and Shaughnessy, P.W. The Measurement and Assurance of Quality. Pp. 103–132 in: R.J. Vogel and H.C. Palmer, eds. Long-term Care: Perspectives from Research and Demonstrations. Rockville, Md.: Aspen Systems, 1985.
LaRocco, J.M., House, J.S., and French, J.R.P., Jr. Social Support, Occupational Stress, and Health. Journal of Health and Social Behavior 21:202–218, 1980.
Linn, M, Gurel, L., and Linn, B.A. Patient Outcome as a Measure of Quality of Nursing Home Care. American Journal of Public Health 67:337–344, 1977.
Lopez-Aqueres, W., Kemp, B., Plopper, M., Staples, F.R., and Brummel-Smith, K. Health Needs of the Hispanic Elderly. Journal of The American Geriatric Society 32:191–198, 1984.
Lusk, S.L. Violence Experience by Nurses' Aides in Nursing Homes. AAOHN (American Association of Occupational Health Nursing) Journal 40(5):237–241, 1992.
Lyles, Y. Impact of Medicare DRGs on Nursing Homes in the Portland Oregon Metropolitan Area. Journal of The American Geriatrics Society 34(8):573–578, 1986.
Lyman, K.A. Work-Related Stress For Staff In An Alzheimer's Day Care Center: The Effects of Physical Environments. Paper presented at the 40th annual meeting of The Gerontological Society of America, Washington, D.C., 1987.
Maas, M. Professional Practice for the Extended Care Environment: Learning from One Model and its Implementation. Journal of Professional Nursing 5(2):66–76, 1989.
Maas, M., and Buckwalter, K. Nursing Evaluation Research: A Special Alzheimer's Unit. A Final Report. Funded under NR0689. The University of Iowa, Iowa City: National Center for Nursing Research, National Institutes of Health, 1990.
Maas, M., and Jacox, A. Guidelines For Nurse Autonomy/Patient Welfare. New York: Appleton-Century Crofts, 1977.
Maas, M., Buckwalter, K., Kelley, L., and Stolley, J. Family Members' Perceptions: How They View Care of Alzheimer's Patients in a Nursing Home. Journal of Long-Term Care Administration 19(1):21–25, 1991.
Maas, M., Buckwalter, K., Swanson, E., et al. The Caring Partnership: Staff and Families of Persons Institutionalized with Alzheimer's Disease. Journal of Alzheimer's Disease and Related Disorders 9(6):21–30, 1994.
Manson, S.M. Long-term Care in American Indian Communities: Issues for Planning and Research. The Gerontologist 29:38–44, 1989.
Maraldo, P.J. Quality in Long-term Care. Pp. 1–11 in: Mechanisms of Quality in Long-term Care: Service and Clinical Outcomes. Pub. no. 41-2382. New York: National League for Nursing Press, 1991.
Matthew, L., Sloan, P., Kilby, M., and Flood, R. What's Different About a Special Care Unit for Dementia Patients? A Comparative Study. American Journal of Alzheimer's Care and Related Disorders and Research 21(2):16–23, 1988.
McDonald, C.A. Recruitment, Retention, and Recognition of Frontline Workers in Long-Term Care. Generations XVIII(3):41–49, 1994.
McKibbin, R.C. The Nursing Shortage and The 1990s: Realities and Remedies. Kansas City, Mo.: American Nurses Association, 1990.
McKnight's Long-Term Care News. Late Breaking News. 14(7):1, July 1993.
McKnight's Long-Term Care News. Annual DON Salaries Increase 6% to $41,200. 16(3):1, 18, 1995.
Mech, A.B. Evaluating the Process of Nursing Care in Long-Term Care Facilities. Quality Review Bulletin 6:24–30, 1980.
Mechanic, D. The Development of Mental Health Policy in the United States. Pp. 73–90 in: Mental Health and Social Policy. Englewood Cliffs, N.J.: Prentice-Hall, 1980.
Meddaugh, D.I. Staff Abuse by the Nursing Home Patient. The Clinical Gerontologist 6:45–47, 1987.
Mezey, M. Institutional Care: Caregivers and Quality. Pp. 155–166 in: Indices of Quality In Long-Term Care: Research and Practice. Pub. no. 20-2292. New York: National League for Nursing Press, 1989.
Mezey, M. Care in nursing homes: Patients' needs; nursing's response. In Aiken, L., and Fagin, C. (eds.), Nursing in the 90s. Philadelphia: J.B. Lippincott Publishing Co., 1992.
Mezey, M.D. Presentation at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Mezey, M.D., and Lynaugh, J.E. The Teaching Nursing Home Program: Outcomes of Care. Nursing Clinics of North America 24(3):769–780, 1989.
Mezey, M.D., and Scanlon, W. Registered Nurses in Nursing Homes: Secretary's Commission of Nursing. Washington, D.C.: DHHS, 1988.
Mobily, P.R., Maas, M.L., Buckwalter, K.C., and Kelley, L.S. Taking Care of the Caregivers: Staff Stress and Burnout on a Special Alzheimer's Unit. Journal of Psychosocial Nursing 30(9):25–31, 1992.
Mor, V. Presentation at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Mor, V. Invest in Your Frontline Worker: Commentary. The Brown University Long-term Care Quality Letter 7(1):4–5, 1995.
Morioka-Douglas, N., and Yeo, G. Aging and Health: Asian/Pacific Islander Elders. Stanford, Calif.: Stanford Geriatric Education Center, 1990.
Morris, J. Presentation at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Morris, J.N., Hawes, C., Fries, B.E., et al. Designing the National Resident Assessment Instrument for Nursing Facilities. The Gerontologist 30:293–315, 1990.
Movassaghi, H., Kindig, D.A., Juhl, N., and Geller, J.M. Nursing Supply and Characteristics in the Nonmetropolitan Areas of the United States: Findings from the 1988 National Sample Survey of Registered Nurses (Grant No. HAR000004-03). Rockville, Md.: Health Resources and Services Administration, U.S. Department of Health and Human Services, 1992.
Munroe, D.J. The Influence of Registered Nurse Staffing on the Quality of Nursing Home Care. Research in Nursing and Health 13:263–270, 1990.
Murtaugh, C.M., Kemper, P., and Spillman, B.C. The Risk of Nursing Home Use in Later Life. Medical Care 28(10):952–962, 1990.
National Indian Council on Aging. American Indian Elderly: A National Profile. Albuquerque, N.M.: National Indian Council on Aging, 1981.
NCHS (National Center for Health Statistics). Nursing Home Characteristics: Preliminary Data from the 1985 National Nursing Home Survey. G. Strahan. Advance Data from Vital and Health Statistics. No. 131. Pub. No. (PHS) 87-1250. Hyattsville, Md.: NCHS, U.S. Public Health Service, 1987.
NCHS. Characteristics of Registered Nurses in Nursing Homes: Preliminary Data from the 1985 National Nursing Home Survey. G. Strahan. Advance Data from Vital and Health Statistics. No. 152. Pub. no. (PHS) 88-1250. Hyattsville, Md.: NCHS, U.S. Public Health Service, 1988.
NCCNHR (National Citizens' Coalition for Nursing Home Reform). A Consumer Perspective on Quality Care: The Residents' Point of View. Washington, D.C.: NCCNHR, 1985.
NIA (National Institute on Aging). Personnel Needs for Health Needs of the Elderly Through the Year 2020. Administrative Document. Committee on Personnel for Health Needs of the Elderly. Bethesda, Md.: NIA, 1987.
NIA. Progress Report on Alzheimer's Disease: Research Is the Key to Unlocking the Mysteries of Alzheimer's Disease. Pub. no. (NIH) 94-3885. Silver Spring, Md.: NIA, 1994.
Norwich, H.S. A Study of Nursing Care in Geriatric Hospitals. Nursing Times 76:292–295, 1980.
O'Connor, J. LTC Facilities Embrace Assisted Living. McKnight's Long-Term Care News 16(3):1, 42, 1995.
O'Shaunessy, M.A., and Price, M.A. Financing and Delivery of Long-term Care Services for the Elderly. Pp. 191–224 in: C.J. Evashwick and L.J. Weiss, eds. Managing the Continuum of Care. Rockville, Md.: Aspen, 1987.
Parsons, W.A., Myrick, R.D., and Gunnoe, J. The Case of Mr. W. Mental Health Consultation. Journal of Gerontological Nursing 14(8):14–18, 1988.
Penner, L.A., Luderria, K., and Mead, G. Staff Attitudes: Image or Reality. Journal of Gerontological Nursing 10:110–117, 1984.
Peppard, N. Alzheimer's Special Care Nursing Home Units. Nursing Homes 34(5):25–28, 1984.
Pillemer, K. Maltreatment of Patients in Nursing Homes: Overview and Research Agenda. Journal of Health and Social Behavior 29:227–238, 1988.
Pillemer, K., and Hudson, B. A Model Abuse Prevention Program for Nursing Assistants. The Gerontologist 33:128–131, 1993.
Pollick, M.F. Abuse of the Elderly: A Review. Holistic Nurse Practitioner 1(2):43–53, 1987.
Preston, D.B., and Mansfield, P.K. An Exploration of Stressful Life Events, Illnesses, and Coping Among the Rural Elderly. The Gerontologist 24:490–494, 1984.
Rantz, M., and Miller, T. Pp. 26–28 in: Quality Assurance for Long-Term Care: Supplement #3. Gaithersburg, Md.: Aspen Publications, 1994.
Reagan, J. Management of Nurse's Aides in Long-Term Care Settings. Journal of Long-Term Care Administration 14:9–14, Summer 1986.
Revans, R.W. Standards for Morale: Cause and Effect in Hospitals. London: Oxford University Press for the Nuffield Provincial Hospital Trust, 1964.
Rhys-Hearn, C. Staffing Geriatric Wards: Trials of a Package. Nursing Times 75:45–48, 52, 1979.
Richardson, J. Aging and Health: Black American Elders. Stanford, Calif.: Stanford Geriatric Education Center, 1990.
Robertson, J.F., Herth, K.A., and Cummings, C.C. Long-term Care: Retention of Nurses. Journal of Gerontological Nursing 20(11):4–10, 1994.
Rohrer, J.E., Buckwalter, K.C., and Russell, D.W. The Effects of Mental Dysfunction on Nursing Home Care. Social Science and Medicine 28(4):399–403, 1989.
Rovner, B.W., and Rabins, P.V. Mental Illness Among Nursing Home Patients. Hospital and Community Psychiatry 36(2):119–128, 1985.
Roybal, E.R. Federal Involvement in Mental Health Care for the Aged. American Psychologist 39(2):163–166, 1984.
Rudman, D., Alverno, L., and Mattson, D.E. A Comparison of Physically Aggressive Behavior in Two VA Nursing Homes. Hospital and Community Psychiatry 44(6):571–575, 1993.
Ryden, M. Presentation at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Ryden, M.B., Bossenmaier, M., and McLachlan, C. Aggressive Behavior in Cognitively Impaired Nursing Home Residents. Research In Nursing and Health 14(2):87–95, 1991.
Samter, J., Braun, J.V., Culpepper, W.J., and Cohen-Mansfield, J. Description of a Program for Psychiatric Consultations in the Nursing Home. American Journal of Geriatric Psychiatry 2:144–156, 1994.
Savage, B., Widdowson, T., and Wright, T. Improving the Care of the Elderly. In: D. Towell and C. Harries, eds. Innovation in Patient Care: an Action Research Study of Change in a Psychiatric Hospital. London: Croom Helm, 1979.
Scanlon, W.J. A Perspective for Long-term Care for the Elderly. Health Care Financing Review (Annual Supplement):1–15, 1988.
Schnelle, J. Treatment of Urinary Incontinence in Nursing Home Patients by Prompted Voiding . Journal of The American Geriatric Society 38:356–360, 1990.
Schnelle, J. Presentation at Special Session on Staffing and Quality of Care in Nursing Homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Schnelle, J.F., Newman, D.R., and Fogarty, T. Management of Patient Continence in Long- Term Care Nursing Facilities. The Gerontologist 30:373–376, 1990.
Select Committee on Aging, House of Representatives, One hundred and second Congress session. Shortage of Health Care Professions Caring for the Elderly: Recommendations for Change. A Report by the Chairman. Pub. no. 102-915. Washington, D.C.: U.S. Government Printing Office, 1992.
Senior, O.E. Nurse/Patient Dependency. London: Management Services, 1978.
Sheridan, J.E., Vredenburgh, D.J., and Abelson, M.A. Contextual Model of Leadership Influence in Hospital Units. Academy of Management Journal 27:48–57, 1984.
Sheridan, J., Hogstel, M., and Fairchild, T.J. Organization Climate in Nursing Homes: Its Impact on Nursing Leadership and Patient Care. Pp. 90–94 in: L.R. Jouch and J.L. Wall, eds. Best Papers Proceedings 1990. San Francisco: Academy of Management, 1990.
Sheridan, J., White, J., and Fairchild, T.J. Ineffective Staff, Ineffective Supervision, or Ineffective Administration? Why Some Nursing Homes Fail to Provide Adequate Care. The Gerontologist 32:334–341, 1992.
Shields, E.M., and Kick, E. Nursing Care in Nursing Homes. Pp. 195–209 in: L. Aiken, ed. Nursing In The 1980s: Crises, Opportunities, Challenges. Philadelphia: J.B. Lippicott, 1982.
Smith, M., Mitchell, S., Buckwalter, K.C., and Garand, L. Geropsychiatric Nursing Consultation: A Valuable Resource in Rural Long-Term Care. Archives of Psychiatric Nursing VIII(4):272–279, 1994.
Smyer, M., Brannon, D., and Cohn, M. Improving Nursing Home Care through Training and Job Redesign. The Gerontologist 32:327–333, 1991.
Snyder, P. Creating Culturally Supportive Environments in Long-Term Care Institutions. The Journal of Long-Term Care Administration, (Spring):19–28, 1982.
Spector, W.D. Presentation at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Spector, W.D., and Takada, H.A. Characteristics of Nursing Homes that Affect Resident Outcomes. Journal of Aging and Health 3(4):427–454, 1991.
Stahl, D.A. 1995 Leadership Challenges for SNFs. Nursing Management 3:17–19, 1995.
Stein, L, Linn, M.W., and Stein, E.M. Patients' Perceptions of Nursing Home Stress Related to Quality of Care. The Gerontologist 26:424–430, 1986.
Stevens, G.L., and Baldwin, B.A. Optimizing Mental Health in the Nursing Home Setting. Journal of Psychosocial Nursing 26(10):27–31, 1988.
Stolley, J.M., Buckwalter, K.C., and Shannon, M. Caring for Patients with Alzheimer's Disease: Recommendations for Nursing Education. Journal of Gerontological Nursing 17(6):34–38, 1991.
Storlie, F.J. The Reshaping of the Old. Journal of Gerontological Nursing 8:555–559, 1982.
Straus, M.A. Domestic Violence and Homicide Antecedents. Bulletin of The New York Academy of Medicine 62:446–465, 1986.
Strumpf, N. Presentation at special session on staffing and quality of care in nursing homes, at the annual meeting of The Gerontological Society of America, Atlanta, Georgia, November 1994.
Strumpf, N.E., and Knibbe, K.K. Long-Term Care: Fulfilling Promises to the Old Among Us. Pp. 217–225 in: J. McCloskey and H. Grace, eds. Current Issues In Nursing (3rd ed.). St. Louis, Mo.: C.V. Mosby, 1990.
Stryker, R. How To Reduce Employee Turnover In Nursing Homes and Other Health Care Organizations. Springfield, Ill.: Charles C Thomas, 1981.
Swan, J., Torre, A., and Steinhart, R. Ripple Effects of PPS on Nursing Homes: Swimming or Drowning in the Funding Stream? The Gerontologist 30:323–331, 1990.
Swanson, E., Maas, M., and Buckwalter, K. Cognitive and Functional Status: Unit Comparison. Clinical Nursing Research 3(1):27–42, 1994.
Tellis-Nayak, V., and Tellis-Nayak, M. Quality of Care and the Burden of Two Cultures: When the World of Nurse's Aide Enters the World of Nursing Home. The Gerontologist 29:307–313, 1989.
Teresi, J., Holmes, D., Benenson, E., et al. A Primary Care Nursing Model in Long-Term Care Facilities: Evaluation of Impact on Affect, Behavior, and Socialization . The Gerontologist 33:667–674, 1993.
Teresi, J.A., Holmes, D., Ramirez, M., et al. Preliminary Findings: A Study of Ethnic/Racial Conflict Between Nursing Home Staff and Residents. Unpublished manuscript, 1994.
Timko, C., and Moos, R.H. A Typology of Social Climates in Group Residential Facilities for Older People. Journal of Gerontology 46(3):160–169, 1991.
U.S. Department of Justice. Crime in the United States. Washington, D.C.: U.S. Government Printing Office, 1985.
Vladeck, B. Unloving Care: The Nursing Home Tragedy. New York: Basic Books, 1984.
Vladeck, B., and Alfano, G. Medicine and Extended Care: Issues, Problems, and Prospects. Owings Mill, Md.: Rynd Communications, 1987.
Wagnild, G. A Descriptive Study of Nurse's Aide Turnover in Long-Term Care Facilities. The Journal of Long-term Care Administration 16(Spring):19–23, 1988.
Wagnild, G., and Manning, R. The High Turnover Profile: Screening and Selecting Applicants for Nurse's Aides. Journal of Long-term Care Administration 14(Summer):1–4, 1986.
Weiler, K., Buckwalter, K.C., and Curry, J.P. Nurses, Work-Related Stress, and Ethical Dilemmas. Pp. 320–339 in: D.M. Corr and C.A. Corr, eds. Nursing Care in an Aging Society. New York: Springer Publishing Company, 1990.
White, C.M. The Nurse-Patient Encounter: Attitudes and Behavior in Action. Journal of Gerontological Nursing 3:16–20, 1977.
Wilging, P.R. OBRA as a Measure of Quality. Pp. 21–25 in: E.L. Mitty, ed. Quality Imperatives In Long-term Care: The Elusive Agenda. New York: National League for Nursing Press, 1992.
Willcocks, D., Peace, S., and Kellaher, L. Private Lives in Public Places. London: Tavistock Publications, 1987.
Wilson, K.B. Assisted Living: Model Program May Signify the Future. The Brown University Long-Term Care Quality Letter 6(15):1–4, 1994.
Winger, J., Schirm, V., and Stewart, P. Aggressive Behavior in Long-term Care. Journal of Psychosocial Nursing and Mental Health Services 25:28–33, 1987.
Wright, L.K. A Reconceptualization of the "Negative Staff and Poor Care in Nursing Homes" Assumption. The Gerontologist 28:813–820, 1988.
Zimmer, J.G., Watson, N., and Treat, A. Behavioral Problems Among Patients in SNFs. American Journal of Public Health 74(10):1118–1121, 1984.
Zimmerman, D.R. Impact of New Regulations and Data Sources on Nursing Home Quality of Care. Pp. 29–42 in: Mechanisms of Quality in Long-term Care: Service and Clinical Outcomes. Pub. no. 41-2382. New York: National League for Nursing Press, 1991.
Zinn, J.S. The Influence of Nurse Wage Differentials on Nursing Home Staffing and Resident Care Decisions. The Gerontologist 33:721–729, 1993.

































































