D Mental Health Care in the Primary Care Setting
Frank deGruy III, M.D., MSFM1
Introduction
In this paper I will make the case that a major portion of mental health care is rendered in the primary care setting, and always will be, sometimes despite strong disincentives; that a sensible vision of primary health care must have mental health care woven into its fabric; that the primary care setting is well suited to the provision of most mental health services; that despite suboptimal recognition and management of mental disorders and attention to mental health, the structure and operation of primary care can be modified so as to greatly augment the provision of these services; and that the efforts under way in the United States to reform the health care system offer an opportunity to find the most effective of these modifications and to discover fruitful collaborative structures both within the primary care setting and between primary care clinicians and mental health professionals.
Most likely this country will retain a parallel primary mental health system. Among the most interesting and complex issues we face are those having to do with the complementarity and integration of services between these two systems, the proportion and makeup of the population that will avail themselves of these respective systems, the factors that affect the interface between primary care and
specialty mental health care, and the relative cost and effectiveness of mental health care rendered by clinicians within these different systems.
The Range And Complexity Of Primary Care
A Paradigm Problem: The Indivisibility of Mental and Physical Health
I will be speaking of mental health, mental disorders, and mental diagnoses throughout this paper. This convention of language is convenient and powerful and is thoroughly ingrained into contemporary conceptual formulations. It is also fundamentally wrong to speak of mental health as though it were distinct from physical health or health in general; this convention can mislead the unwitting into dangerous and expensive errors. A definitive treatment of this problem would begin with a critique of Meditations on First Philosophy, published in 1641 by Rene Descartes, in which he divided reality into two domains, the physical and the mental. Even if such a critique were within my competence, my purpose here is more concrete and practical, and such an excursion would not be justified. Therefore, I will deal with more practical implications. Whether or not it is inherently impossible to portray accurately the clinical reality of primary care within a Cartesian dualism, one of the consistent consequences of this dualism is inattention to the relationships between these two domains. In primary care these relationships pervade all aspects of the clinical enterprise. Two implications of this disintegration of the psyche from the soma are salient.
First, let us consider the clinical relationship between physical and mental problems. Mental distress, symptoms, and disorders are usually embedded in a matrix of explained or unexplained physical symptoms, as well as acute and chronic medical illnesses.1–3 Generally, primary care clinicians deal with mental symptoms as part of something—part of a larger, more general problem. The nature of primary care, as we will see in a moment, is integrative. The more pronounced the physical symptomatology, whether or not the symptoms have a physical explanation, the greater the likelihood that a primary care patient has a mental diagnosis.2 In other words, mental symptoms and disorders are concentrated in precisely those patients who are visiting their primary care clinician for other reasons—physical disease or at least biomedical problems. Conversely, psychologically distressed patients experience increased physical symptomatology.4 This means that mental illness itself produces symptoms likely to lead one to a primary care clinician. The relationship between physical and mental symptoms is complex and interesting, but I need to note here only that it is inextricable—inevitable. Systems of care that force the separation of "mental" from "physical" problems consign the clinicians in each arm of this dichotomy to a misconceived and incomplete clinical reality that produces duplication of effort, undermines comprehensiveness of care, hamstrings clinicians with incomplete data, and ensures that the patient cannot be completely understood.
The second implication involves patient health beliefs and care preferences. Primary care patients do not view their "mental diagnoses," such as we apply them, as a thing apart from their general health, and they will not tolerate our doing so. One-third to one-half of primary care patients will refuse referral to a mental health professional; 5,6 those who refuse tend to be high medical utilizers with unexplained physical symptoms, but refusers cut across all demographic and diagnostic groups.7 Securing the consent of primary care patients for clinical trials of treatment by mental health professionals for mental disorders is even more problematic, unless the primary care clinician participates in the protocol.8 In other words, a certain large proportion of primary care patients prefer to receive mental health care in medical settings, and this is in part because it is not construed as "mental health care."
Thus, one can describe the range of mental disorders that occur in primary care, and this description is accurate inasmuch as it counts symptoms and diagnoses that are actually present. But when seen from the inside, these symptoms and diagnoses are embedded in a matrix of physical symptoms, disorders, and diseases; other mental symptoms and disorders; and social predicaments and stressors. This context completely changes the meaning and consequences of the identified mental disorders and profoundly affects the manner in which the clinician approaches patients who harbor these disorders. It also changes the strategies of the researcher who wishes to gain an insider's understanding of how primary care patients with "mental" disorders appear to those caring for them. Breaking a patient's predicament into a string or list of problems is acceptable only if one continuously takes account of the relationship between the problems, sees the problems as only a part of what the person is, and understands that the patient's clinical predicament cannot be represented by even a complete list of her or his problems. There is an interaction term between every pair of problems. We need never to forget that the whole is greater than the sum of the parts.
I have belabored this at such length because it has important implications for who manages mental disorders, how they are classified, how primary care clinicians are trained to see and manage them, and how we restructure primary care to make incentives and resources available to deal with these problems. It actually has something to do with a core attribute of primary care, despite its bewildering forms: the primary care clinician has a moral responsibility to the person who is the patient. To the whole person. That person must be taken as a whole; whether we wish it otherwise or not, that means taking responsibility for mental as well as physical well-being. One aspect of this can be called comprehensive care, and another aspect can be called continuity—continuity in the sense that a physician sees a patient regularly until an understanding of the patient's individuality has taken place. Recognition of this inherent inseparability of mind and body also helps account for the vehement reaction primary care clinicians sometimes have to the news that mental disorders are prevalent and largely undiagnosed in their setting; this implies that they are not taking care of their patients, without acknowledgment
of the relatively enormous domains into which they are extending excellent care. This is not to argue that specific mental symptoms or diagnoses do not demand a correspondingly specific set of responses—they do—but these responses are always modified and reordered according to the personal context in which they occur. Mental health care cannot be divorced from primary medical care, and all attempts to do so are doomed to failure. Primary care cannot be practiced without addressing mental health concerns, and all attempts to do so result in inferior care.
The Range of Problems Seen in Primary Care
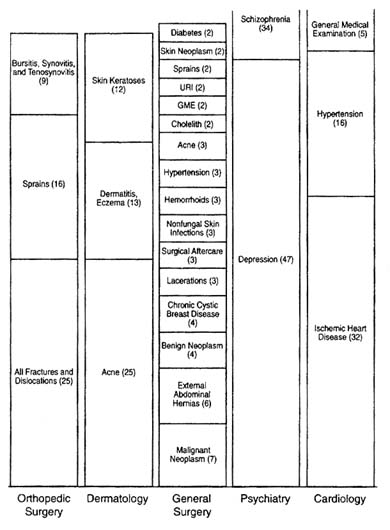
That being said, there is value in breaking a clinical predicament into its constituents and understanding the constituent problems that are causing such high mischief when they interact: let us step outside the complex web of primary care and break the work of the primary care clinician into component problems. We see from Figure D-1 that no single problem or task accounts for a large proportion of time or resources. This is in sharp contrast to most of the specialties and subspecialties. In other words, one defining feature of primary care medicine is the range, diversity, and sheer number of different problems. I am presenting this figure to draw out three implications:
- This range has a marked effect on diagnostic behavior. It creates the need for diagnostic categories as inclusive as possible while retaining management specificity—generalists are "lumpers."
- This range of problems also can degrade the value of diagnostic tests, compared with their value in the hands of specialists, by lowering the pretest or prior probability, and therefore lowering predictive values. This is a warning about applying diagnostic assumptions generated in one setting to another setting.
- Mental health care is but a small proportion of the range of problems faced by the primary care clinician. By the NAMCS data presented here, less than 3 percent of the average caseload is mental health care. We will see in a moment that this is a gross underestimate, but the point still stands: mental health care is only a part of primary care practice. Most of the patients with diagnosable mental disorders appear under a different diagnostic label and are receiving care for problems other than mental illness. In other words, the primary care clinician is laboring under the burden of competing demands during every encounter; this concept of competing demands will be developed more fully as we explore the adequacy of care rendered to patients with mental diagnoses.
Another piece comes into focus when we "transpose the matrix," as it were, and look at the problem list for each patient. The primary care patient has an active problem list containing an average of six problems.9 This means not only
that primary care clinicians are dealing with many problems other than mental health ones but also that each individual patient is dealing with many problems, some of which are mental in nature.
The concept of comorbidity has come into currency to deal with this phenomenon, and in some measure it does. But comorbidity is merely a list of concurrent diagnoses, which does not adequately account for the interactions between these diagnoses. These interactions increase geometrically with the number of comorbid conditions. Sometimes a more comprehensive, fundamental formulation is necessary to understand adequately the constituent problems and the relationship between them. This has implications for how diagnostic and management formulations are transferred into primary care from mental health specialty settings.
The Range of Mental Problems Seen in Primary Care
A great deal of research has gone into describing the psychological problems of primary care patients; I will summarize the most salient features of this research.
Some 10–20 percent of the general population will consult a primary care clinician for a mental health problem in the course of a year. 10,11
About 40–50 percent of primary care patients who are high utilizers exhibit significant psychological distress.4,12 The proportions of pediatric primary care patients with significant psychosocial or psychosomatic problems are about 15 and 8 percent respectively13,14
Some 10–40 percent of primary care patients have a diagnosable mental disorder. The PRIME-MD validation study diagnosed 26 percent of primary care patients with at least one of 18 possible diagnoses in the III–R edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM–III–R) (site range, 18–38 percent) and an additional 13 percent with a subthreshold diagnosis associated with significant functional impairment (site range 10–14 percent).15 The World Health Organization (WHO) Collaborative Study found a prevalence of 21 percent for at least one of their eight possible International Classification of Diseases disorders (site range, 8–53 percent).16 Mood, anxiety, substance abuse, and somatoform diagnoses account for more than 90 percent of the diagnoses in adults15,16 Both the PRIME-MD and the WHO studies cited above documented extensive mental comorbidity: nearly one-third of subjects in the PRIME-MD study had three or more mental diagnoses, whereas in the WHO study all but one of the specific mental diagnoses had comorbidity rates above 50 percent.
The Phenomenology of Mental Problems in Primary Care
When a patient having a mental disorder presents to a primary care clinician, she or he usually does so with a physical complaint1,3 Such presentation results in
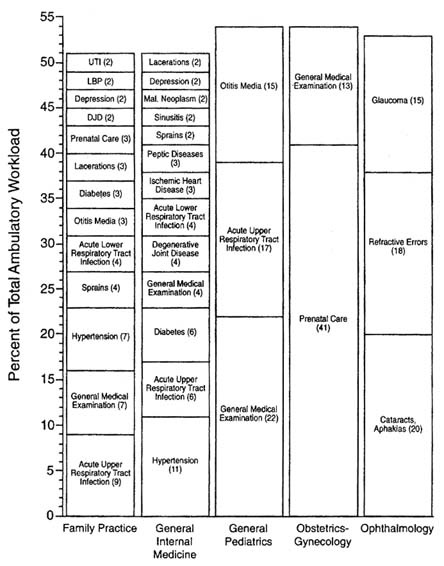
FIGURE D-1 Diagnostic profiles of the 10 largest physician specialities based on all nonreferred ambulatory visits, NAMCS, 1989–1990. All relative standard errors are <30 percent. Values in parentheses are percentages of all visits to the indicated specialty for that diagnostic cluster. Diagnosis cluster key: Acne = acne and diseases of sweat and sebaceous glands; cholelith = cholelithiasis and cholecystitis; depression = depression, anxiety, and neuroses; diabetes = diabetes mellitus; DJD = degenerative joint disease; GME = general medical examination; lacerations = lacerations, contusions, and abrasions; LBP = low back pain; schizophrenia = schizophrenia and affective psychosis; skin neoplasm = malignant neoplasms of skin; sprains = acute sprains and strains; URI = upper respiratory tract infection; and UTI = urinary tract infection. SOURCE: Rosenblatt RA. Identifying primary care disciplines by analyzing the diagnostic content of ambulatory care. J Am Board Fam Pract. 1995;8(1):41. Reprinted with permission.
recognition of the underlying mental diagnosis about half the time, whereas for the small proportion of patients in whom the presenting complaint is emotional distress or a psychological symptom, the mental diagnosis is correctly ascribed in more than 90 percent of cases.1
The mental disorders seen in primary care are probably less severe than those seen in specialty mental health settings; this has been documented most extensively for depression.17–20
Primary care patients with mental diagnoses—even subthreshold mental diagnoses—show profound functional impairment. Wells first demonstrated this with the Medical Outcomes Study (MOS) study, in which depressed patients were seen to have functional impairment comparable to patients with chronic medical conditions such as chronic obstructive pulmonary disease, diabetes, coronary artery disease, hypertension, and arthritis.21 The PRIME-MD data set offers a look at patterns of impairment by specific mental diagnosis and affords a comparison between the relative contributions to impairment of physical and mental disorders. Figures D-2 and D-3 illustrate these findings. One can see that
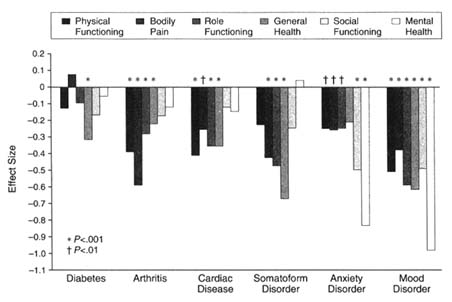
FIGURE D-2 Unique association of common mental and general medical disorders with Short-Form General Health Survey health-related quality-of-life scales. SOURCE: Spitzer et al. Health-related quality of life in primary care patients with mental disorders. JAMA. 1995;274(19):1513. Copyright 1995 by the American Medical Association. Reprinted with permission.
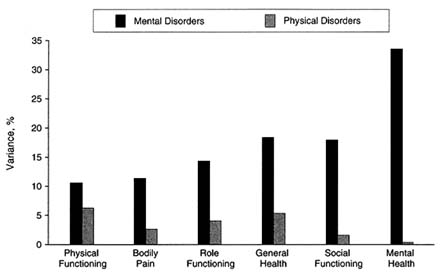
FIGURE D-3 Proportion of variance in Short-Form General Health Survey (SF-20) health-related quality-of-life scales uniquely accounted for by mental disorders and physical disorders (i.e., general medical disorders). SOURCE: Spitzer et al. Health-related quality of life in primary care patients with mental disorders. JAMA. 1995;274(19):1513. Copyright 1995 by the American Medical Association. Reprinted with permission.
different disorders produce different patterns of impairment, but they are generally much more severe than those arising from physical disorders.
Patients with mental diagnoses show consistently higher utilization of medical resources than their unaffected counterparts, generally on the order of twice the baseline utilization rates.22–24 In some cases, such as with somatization disorder, the increased utilization is quite extraordinary—nine times the national norm.25
Confounding these differences between the phenomenology of mental disorders in the primary care and the mental health specialty settings are probable demographic differences between patients who seek care in these respective systems: the old, the less educated, the poor, and the non-white—in other words, the vulnerable—are more likely to appear for care in the primary care setting.21
Classification: The Web of Comorbidity, Threshold, and the Breakdown of Diagnostic Categories
Up to now, primary care clinicians have lacked an adequate classification system for mental disorders, but quite a bit of work is under way in this area. At
this point it is useful to make a distinction between a classification system and a diagnostic system. A classification system establishes categories into which conditions are placed, but the means by which conditions are assigned to one or another of the categories is not necessarily specified. The ICD-9-CM is an example of a classification system; since ICD-9-CM codes are required by all payers for reimbursement of services, it is safe to say that all primary care clinicians use this system. But this system is of little value in advancing our understanding of the nature of mental disorders in primary care, because it contains neither diagnostic criteria nor a systematic framework for clinical decision rules to guide clinicians and researchers in making diagnostic judgments.
On the other hand, the Diagnostic and Statistical Manual for Mental Disorders (DSM) is a diagnostic system. It was developed and published by the American Psychiatric Association. The DSM system, currently in its fourth edition (DSM-IV), is the de facto standard in mental health settings; it is also used by many mental health professionals working in medical settings. This diagnostic system has revolutionized the field of psychiatry and has caused an explosion in our knowledge about mental illness, largely by virtue of its explicit, measurable diagnostic criteria. DSM-IV is linked to the ICD system for billing purposes. However, DSM-IV (and its predecessors) has significant limitations when it is used in the primary care setting, and it is rarely used there. The principal limitation is that the DSM-IV is large, complex, and difficult to navigate. It contains much material that is utterly irrelevant to primary care. It does not address with acceptable simplicity mixed syndromes, subthreshold conditions, and the extensive comorbidity found in the primary care setting. Moreover, the natural history and effectiveness of treatment of many mental syndromes in the primary care setting are incompletely studied; it is not at all clear that it is always worthwhile to identify and treat DSM-IV-defined conditions.
A number of diagnostic systems that are specifically for use in primary care are under development. Two of these are worth mentioning: ICD-10-PHC, based on ICD-10, and DSM-IV-PC, based on DSM-IV. It is too early in the development of these systems to assess their utility, but both are enjoying widespread dissemination, and will most likely evolve into forms more congenial to the demands, constraints, and phenomenology of mental distress in primary care. Specifically, these systems are far less detailed and impenetrable than their parent systems; additionally, DSM-IV-PC is organized into algorithms that begin with presenting complaints.
As described in the introductory paragraphs, some of the problems with mental diagnoses in primary care settings are more fundamental than simply deciding which categories to lump together or which criterion symptoms work best in this setting. In some instances it appears that no combination of DSM criteria adequately captures the nature and extent of mental disturbance that occurs in people appearing for care in the primary medical setting. For example, in a study of somatizing patients in three family practices, deGruy and colleagues
identified a group of patients who met the diagnostic threshold for no DSM-III-R conditions but who had symptoms across several categories (e.g., mood, anxiety, and somatoform) and suffered significant functional impairment.26 These patients had been abused and had generally grown up in dangerous, violent families. These patients have important relationship problems, including with their primary care clinician, and frequently appear for medical care. These are patients who require entirely new diagnostic formulations in order to benefit from appropriate research inquiry and clinical ministrations.
A particularly important diagnostic problem in primary care has to do with the comorbidity between mental and medical illnesses. Two-thirds of primary care patients with a psychiatric diagnosis have a significant physical illness.1,15 It is well established that chronic medical illnesses, taken as a whole, increase the likelihood of depression by two- to threefold.27 Certain disorders, such as parietal cerebrovascular accidents, are associated with an even higher risk of depression.28 Depression in a patient who has suffered a stroke is probably different from that which appears in the absence of concomitant physical disease. It is not at all clear that the condition should be labeled depression in both instances. Moreover, as demonstrated in the PRIME-MD validation study, the mere presence of physical symptoms—explained or unexplained—increases the likelihood of a mental diagnosis.2 Thus, we need diagnostic formulations that take into account this interplay between the biomedical and the psychological and that allow us to address the question of whether conditions should be regarded and managed differently when they occur in the presence of physical illness.
Distress is what usually causes a patient to seek out a primary care clinician, and relief of this distress can be viewed as the hallmark of a successful clinical encounter. Distress has been shown to correlate imperfectly with mental diagnoses. For example, Katon and colleagues showed that only 52 of 119 distressed high utilizers in a large primary care setting met the criteria for a DSM-III-R diagnosis, although 73 percent met the criteria for abridged somatization disorder.29 This interesting finding underscores the need for careful attention to the patients in the ''off-diagonals"—those patients who are distressed without a mental diagnosis (whom clinicians are compelled to care for) and those who are not distressed but who meet the diagnostic criteria for a mental diagnosis (whom clinicians can easily overlook and who may well not benefit from disorder-level therapeutic ministrations).
No matter how refined diagnostic categories and criteria ultimately become, proper management of patients with mental disorders always requires more than diagnostic information. Appropriate management takes into consideration such factors as patterns of functional impairment and patient treatment preferences.30
In summary, the current diagnostic systems for mental disorders, developed for use in mental health care systems, are difficult for primary care clinicians to use and are inadequate to characterize the phenomenology of mental illness as it occurs in primary care settings. Although such efforts as DSM-IV-PC and the
ICD-10-PHC appear to address some of these shortcomings, mental health care in the primary medical setting will continue to be problematic until a thoroughly congenial diagnostic system has been developed and management formulations routinely include patient-specific information beyond diagnosis.
The Varieties of Primary Care Practices
Although it is possible to describe the core responsibilities of a primary care clinician and to describe the range of activities and distribution of diagnoses made and managed in this setting, we should note here that such pooled data can conceal the diversity of practice structures and the actual content of practice across these practices. Some primary care practices deal with children only, some deal with adults only, whereas others deal with both; some practices are in urban areas with a wealth of ancillary resources available nearby, whereas others are rural and self-contained; some practices are made up of large groups with in-house resources such as consultant and laboratory support, social workers, and patient educators, whereas others consist of solo practitioners and an assistant or two; some primary care clinicians have practices that emphasize obstetrics, adolescent medicine, geriatrics, or sports medicine; some practices are family-oriented and some are community-oriented; some practices emphasize procedures whereas others refer all patients needing procedures; some are organized around unique cultural needs; some are organized around occupational concerns; some are organized around teaching programs. This bewildering variety does not even take into account the practice variation caused by variations in reimbursement systems, which are discussed below; nor does it take into consideration the differences that follow from physician preferences and a perceived ability to manage mental health problems.
This extraordinary range of practice content and styles reflects creative local solutions to local problems and interests. This diversity of practice content also applies to the provision of mental health care: some practices offer extensive mental health services, whereas others offer few, and the content of the actual offerings is sometimes very different across practices. Any consideration of the future of primary care will need to be inclusive and accommodating of the plurality of individual practices; a narrow, rigid definition of primary care will most likely injure the ability to fit the practice to the problems at hand.
The Adequacy Of Mental Health Services Rendered In The Primary Care Setting
Diagnosis
More than a dozen studies have examined the rate of recognition of mental disorders in primary care.31 Even though these studies have used different settings
(e.g., community practices versus residency training programs), different patient groups (e.g., adults versus children), different diagnostic criteria, and very different criteria for what constitutes recognition, they converge somewhat on the fact that one-half to two-thirds of patients meeting the criteria for a mental disorder are unrecognized. This rate of nonrecognition is considerably higher when patients present with a somatic rather than a psychologic complaint and when the diagnostic criteria are stringent.1,3
Why is the rate of recognition so low? A number of factors have been identified. Badger and deGruy studied the factors related to the recognition of depression among 47 community-based primary care practitioners using a panel of standardized patients and discovered that almost no physicians knew or used the DSM diagnostic criteria for depression.32 This finding is especially noteworthy in light of the fact that depression is the best known and most widely studied mental disorder in primary care. Thus, insufficient knowledge of diagnostic criteria is one factor related to the low rate of recognition. A correct diagnosis was associated with longer interviews, and with certain patient-centered interviewing behaviors, but not with general interest in psychosocial issues.
There are other factors as well, such as the physician's perception that treatment is effective and that he or she has the time and resources to manage depression effectively.33
Rost and colleagues recently published a fascinating paper on the deliberate misdiagnosis of depression in primary care,34 in which they reported that half of 444 primary care physicians surveyed had deliberately miscoded at least one depressed patient in the previous 2 weeks. The most common reasons for this astounding behavior are worth noting carefully: diagnostic uncertainty, problems with reimbursement, jeopardizing future insurability, and stigma associated with a mental diagnosis. These physicians usually coded a presenting physical complaint rather than the underlying depression. Thus, even when suspected, mental diagnoses are sometimes not recorded because of pressure from insurers and patients not to do so.
Management
Purely on the basis of the rate of underdiagnosis, one could infer that the mental health needs of primary care patients are not being adequately addressed. But the problem is deeper than diagnosis alone; at least a half dozen studies have documented that even when they are recognized and treated, mental disorders (at least depressive disorders) are treated inadequately, both in terms of dosage and duration of antidepressant medication.35,36 Moreover, several naturalistic primary care studies have shown no difference in clinical outcomes between depressed patients who are recognized and treated and depressed patients who are not recognized; this may be because of the inadequacy of treatment or of the low severity and responsiveness of patients spontaneously recognized.37–40 In any
event, it is clear that simple recognition, although perhaps necessary, is insufficient to ensure adequate care.
There is very little evidence assessing the adequacy of treatment of mental disorders other than depression in primary care. Clinical guidelines for treatment in primary care exist only for depression.41 We can, therefore, conclude that for depression, treatments that have been shown to be effective for some patients in primary care are underutilized; for other mental diagnoses, treatments shown to be effective in other settings are underutilized, but their effectiveness in the primary care setting has not been demonstrated and may in fact not exist.
Competing Demands and the Tasks of the Primary Care Clinician
One of the major impediments to the successful integration of mental health care into the primary care setting has been the assumption that diagnostic skills (or aids) and management protocols are sufficient to correct this problem. This assumption leads to particularly unpleasant consequences. Primary care clinicians are busy; their days are full; and they are under continuous demand to provide new or additional clinical services. Often, a clinician's inattention to a problem represents not negligence or unwillingness but a rational setting of priorities among a list of competing demands. After all, the average primary care visit lasts 13 minutes,42 patients have an average of six different problems on their problem list, and they come in with a presenting complaint that demands attention. This is a zero-sum game: there is no room for the provision of new services without either eliminating another service or adding resources to do the additional work. Some glimpse into this predicament can be gained by considering the provision of preventive services. Although family physicians endorse an average of 87 percent of the U.S. Preventive Services Task Force Guidelines, they perform only 20 to 60 percent of them.43–46 The pressure to render more and more services without compensatory augmentation of resources or elimination of competing demands is particularly demoralizing: 25 percent of rural physicians say they are likely or very likely to leave their practices within the next 2 years, principally because the demands of practice are too overwhelming. Thus, this problem of underdiagnosis and undertreatment cannot be remedied by simple provision of guidelines and protocols, no matter how elegant; it will require a reordering of the actual structure and process of primary care.
Incidentally, this equation might be modified by the demonstration that attention to and management of mental disorders resulted in the expenditure of less time or resources for a given benefit to the patient's health.
The Organization of Services and Incentives
At the present time, there is a rather extraordinary set of forces that collude to inhibit provision of mental health care in the primary care setting. Some of these
have been discussed above and will simply be listed here so their collective effect can be weighed.
- Patient resistance to accepting the stigma of a mental diagnosis.
- Somatic presentation of mental distress—patient somatization.
- Inadequate knowledge and skills on the part of the primary care clinician.
- The pace of primary care practice. It has been customary for primary care clinicians to see four or five patients per hour. The enormous weight of prevailing custom, reimbursement, patient expectation, and generalist-specialist relations conspire to maintain this pattern. This leaves insufficient time for detailed psychological assessment or management of mental symptoms. Clinicians may deal with this problem by scheduling frequent return visits for the patient with such symptoms or scheduling occasional longer visits, both solutions that themselves create problems.
- The somatic, biological orientation of medical education. Both undergraduate and residency educational programs tend to emphasize the biomedical, technical aspects of tertiary care. Psychosocial material is devalued as unscientific and irrelevant, or at least of secondary importance.
- Specialist somatization—the insistence upon extensive diagnostic work-ups for somatic complaints and the pursuit of incidental findings in those patients referred for consultation.
- Psychiatry itself, in its recent preoccupation with brain biology and psychopharmacology, has evolved in a way that is rather unhelpful to generalists. This is not to minimize the enormous value of this orientation, but to point out the vacuum that it has created. Primary care clinicians have lost a theoretical framework for understanding the human predicament and giving meaning to symptoms. Today, there is no coherent medical psychology that is taught in every medical school. With certain important exceptions, psychiatrists are most often called into service to prescribe or monitor psychotropic drugs or to make difficult diagnostic decisions about seriously disturbed patients. This leaves the primary care clinician without support when she or he is trying to understand and deal with the "ordinary" mental distress, disorders, and illnesses encountered in the daily practice of primary care.
- Diagnostic systems that do not fit the clinical phenomenology.
- Insurer somatization—in some instances, reimbursement is forthcoming for biomedical diagnoses but not mental diagnoses.
- Finally, the general manner in which patient services are structured and reimbursed can seriously undermine the capacity to render integrated primary mental health care. These service system-level factors will be discussed in detail in the next section.
Capitation, Managed Care, and Gatekeeping
As our health care system undergoes a fundamental transformation, we find innumerable variations in the structure, resources, and incentives that provide natural experiments for judging the effects on patient outcomes and the health system as a whole. Although we can expect these natural experiments to eventually produce voluminous data, at this time there is much more conjecture and hypothesis than knowledge about the effects of variations in the organization of services. The first task is to outline some of the more salient variations in the organization of services and incentives and to describe their effects on the provision of mental health services in primary care.47
The most basic distinction is between fee-for-service, capitated, and salaried clinicians. Within each of these general categories lies an enormous set of variations.
Salaried clinicians represent the simplest category: these people have no incentive to diagnose and manage mental disorders, but neither do they have an incentive to avoid doing so. A complicated or extended patient visit can be accommodated by displacement of subsequent patient visits without financial penalty—unless, of course, the employer controls the scheduling or sets the visit rates. Here we might see high variation in practice style across clinicians, according to their interest in mental health issues and especially according to the productivity incentives that are attached to their basic salaries.
Two features characterize clinicians working under a fee-for-service system: the first is that the system itself is disappearing, particularly for primary care providers. The second is that the effects on the provision of mental health services depend entirely upon what fees are paid for which services. If mental diagnoses are not reimbursable codes, then primary care physicians have no financial incentive to identify, refer, or treat these conditions. If the fee-for-service structure favors procedures over time-intensive talking work, as it has in almost all cases in the past, then again clinicians will be motivated to ignore or avoid mental diagnoses and, when this is not possible, to refer patients having them elsewhere. If the amount of time spent and the complexity of problems addressed are the bases for reimbursement, as they have recently become in the Medicare Resource-based Relative-Value Scale system, then the incentive tips somewhat toward the identification and management of mental disorders. At this point I have located no evidence that addresses the actual effect of this change.
Finally, we come to capitated systems of care and their manifold variations. Capitation has become the de facto standard reimbursement system under managed care and will most likely remain so for the forseeable future. In its most basic form, without any supplemental incentives, clinicians would be motivated not to identify mental health problems in their patients and if identified, would refer them elsewhere for care; if treatment is rendered by the primary care clinician, this system favors low-intensity, short-duration treatments. This presumes,
of course, that the cost of identifying and treating mental disorders is greater than any savings in patient care costs to the primary care clinician that might result from these disorders remaining undiagnosed and untreated. There is an active literature on this so-called cost-offset effect, which at this time is inconsistent and controversial; some evidence suggests that identification and treatment save the system money,48 whereas other findings suggest that it costs money to identify and treat mental disorders in primary care.49,50 There is little controversy about the cost to the primary care provider, however—such savings as accrue tend to result from lower hospitalization and emergency services, and perhaps specialist visits, but not from a lowering of primary care visits. (There are exceptions to this general rule, such as the finding of Smith and colleagues that a specific management of primary care patients with somatization disorders lowers the use of the primary care clinician's services.51) Thus, with some exceptions, identification of mental disorders in primary care is locally expensive, and under a system of straight capitation, the primary care physician will be motivated to avoid this effort.
Of course, the situation is much more complicated than this. Two levels of complexity deserve more detailed discussion. The first is the superimposition of incentives upon the basic capitation structure. The two most common incentives are productivity and quality of care. It is clearly in the best interest of a managed care system to retain clinicians who can see many patients. The "carrot" approach to promoting this end is to offer a financial reward to clinicians who exceed a given volume of patient visits; the "stick" approach is to penalize those who fall below a minimum productivity standard. In both cases this number sometimes undergoes a case-mix adjustment for the complexity of the cases being seen. This incentive structure works against the discovery and management of mental disorders, unless the case-mix adjustment explicitly makes allowance for this added level of complexity. Incentives for quality of care have recently made their appearance; although providing the highest quality of care admittedly costs more money than providing substandard care, it allows managed care organizations to market truthfully their services as being of the highest quality. The organization will generally publish standards of care and measure clinician conformance to these standards. Any condition or set of conditions can be targeted for quality improvement; moreover, there have been innumerable strategies by which the standards are developed and implemented, with important implications for the quality of care rendered. Discussion of these issues is beyond the scope of this paper.
Although there is controversy concerning the cost of identifying and treating mental disorders, there is no such controversy about the value to the affected patients of identifying and treating at least certain mental disorders (such as major depression). Plans that offer the primary physicians an incentive to do this are offering their panel the probability of improved health.
The second level of complexity in capitated systems mentioned above has to
do with the manner in which mental health services are organized in relation to primary care services. One option is to carve out the resources for mental health care and organize them under a separate system. A mental health carve-out has the advantage of preserving resources for mental health care that might be displaced into other services in an integrated system. Such a system may consist of contracts with private mental health professionals or of a unified, plan-wide mental health center consisting of a team of psychiatrists, psychologists, family and other therapists, counselors, group leaders, social workers, and so forth. All patients identified with mental health problems are referred. The mental health professionals working under such a system may themselves be capitated or may work on a fee-for-service basis; their fees may come from the primary clinician's capitation or directly from the plan. The source and structure of such payment obviously affect the nature and extent of services rendered. For example, a primary care clinician would be loath to refer a patient to an unknown mental health provider for an unknown number of visits if he or she were paying for the referral; conversely, if the mental health carve-out is itself capitated, the mental health professionals have an incentive to function more as consultants and educators for the primary care clinician than as a simple referral resource. Such self-evident hypothesized relationships have as yet little empirical corroboration and will not be discussed further, with one exception. The concept of gatekeeper assumes salience under such circumstances. If primary care clinicians must pay other providers for mental health services to their patients, they have a strong incentive to not recognize mental symptoms, and their role has become that of gatekeeper in the worst sense of the word.
Mental health carve-out systems have major drawbacks and in fact can subvert certain core principles and values of primary care—comprehensiveness and continuity. Carve-out providers have no incentive to reduce general medical costs and may in fact try to shift costs into the general medical sector. Moreover, as mentioned in the opening paragraphs, one-third to one-half of patients referred for mental health services fail to accept the referral, and the refusals generally come from patients who are high utilizers. This creates a cohort of untreated patients purely as an artifact of the system's unwillingness to accommodate them in the primary care setting. Disruption of continuity has been shown to result in less adequate treatment for depression52 and to result in more expensive and less satisfactory primary care in general.53 This should serve as a reminder that the artifact of annual enrollment periods, with their characteristic disruption of continuity, injures the quality of care and should be discouraged.
A further useful perspective on this issue can be gained by examining the content of mental health referrals by primary care clinicians. One-half are for V-code diagnoses (usually family relationship problems), and another one-fourth are for uncomplicated mood and anxiety diagnoses. This leads to a fundamental question: Can these problems be managed adequately in the primary care setting? At this time, there is simply no evidence comparing similar patients under carve-out
and integrated systems; some data should emerge soon from the enormous numbers of natural experiments now under way with Medicaid populations. However, the MOS sheds some light on this issue, containing as it does 550 patients with severe depression, 44 percent of whom were managed by primary care physicians, 31 percent by psychiatrists, and 25 percent by other mental health professionals.35 Analysis of these cohorts revealed that the quality of care was significantly higher for the patients treated by psychiatrists than for those treated by generalists, that the cost of care was significantly less in the general medical sector, and that the most cost-effective care could be achieved by shifting some patients from the specialty to the general medical sector and instituting quality improvement measures. This analysis assumed that it was possible to effect a significant improvement in detection and increase the appropriate use of antidepressants. The authors assumed that this would require incentives and resources. But even given these, is it possible to improve significantly the mental health care rendered in the primary care setting? The answer, as discussed in the next section, is an unambiguous "yes."
The alternative to mental health carve-outs is integrated care. As Mechanic argues54 with the possible exception of patients who are seriously mentally ill, basic mental health services can be successfully managed in the primary care setting. Certainly, integrated primary care has been shown to be cost-effective in general principle. Take, for example, the Pike Street Clinic Project.55 This was an integrated, multidisciplinary clinic offering services to indigent elderly in Seattle. All services were coordinated through the primary care physician, who functioned as the case manager. The same services were available to neighbors, but the primary care coordination was not there. With comparable outcomes, Pike Street cost $1,000 per patient per year less. In this instance, the primary care was more expensive, specialty care and social services cost the same, whereas emergency care and inpatient care were much less expensive. With respect to mental health outcomes, the most compelling evidence is again related to the management of depression: both Schulberg and colleagues56 and Katon and colleagues36 have demonstrated that integrating mental health professionals into the primary care setting to accomplish selected aspects of mental health care results in impressive improvements in patient outcomes, sometimes at minimal net cost. The critical factors related to successful outcomes seem to be application of protocol-level standards of care, the maintenance of the relationship between the patient and the primary care physician, and operation of the mental health professionals within the constraints of the primary care setting itself. These studies are the first of many to come; projects addressing a variety of mental diagnoses and symptoms with an even larger variety of collaborative models of care are under way. At this moment the field is ripe for discovering who to integrate into the primary care team, how to integrate them, and to which problems the team should address itself. These research efforts are necessary to convince payers that such integration is more effective and less expensive than the alternatives.
In summary, most mental health care will be rendered in the primary care medical setting or it will not be rendered at all. Primary care clinicians are recognizing and treating only a fraction of the mental health needs of their patients. The reasons for this are good; the competing demands of primary care are such that additional resources (which already exist and which function outside the primary care system) must be brought to bear on this problem. There is evidence that such resources, if organized properly, could result in dramatic improvement in the functional health of primary care patients, at little additional cost to the system.
The Mental Health Services System And The Place Within It Of Primary Care
In some ways we in primary care regard specialty mental health clinicians just as we regard other medical specialists: we each deal with a subset of the other's domain, and each deals with that subset somewhat differently; we view them as resources for consultation and referral for patients with complicated problems, as educators in our training programs, and as colleagues in the general effort to improve the health of the people. These similarities allow us to apply the lessons we learn in our relationships with mental health professionals to our relationships with other specialists. For example, we might expect to see differences in the presentation, natural history, recognition rate, and optimum management for a given diagnostic entity across specialties; we might expect the problem of subthreshold conditions and extensive comorbidity to be an issue; we might expect management recommendations developed in specialty settings to be difficult to implement or downright inappropriate in the primary care setting; we might expect multidisciplinary primary care teams to be useful in augmenting and extending the capacities of the primary care system; and so on.
The mental health system is in some ways unique. To a much larger extent than with any other specialty, there is a primary mental health care system parallel to the primary medical care system. The point of entry into this system is usually either community mental health centers or private mental health professionals, which provide primary mental health care for patients who identify their problem as principally mental. Some of these patients have little or no medical symptomatology, and there is no reason to think that these patients would benefit from having their care integrated into a primary medical setting. Others may have serious or persistent mental illness. These patients are best served by facilities offering multidisciplinary, specialized services such as case workers, psychiatric social workers, and psychopharmacologists. It does not make sense to integrate these resources into ordinary primary care settings, as they would be used too infrequently. However, these patients have a very high burden of medical illness, and their medical care is often haphazard and fragmentary. This is a place where integrating a primary care clinician into the mental health setting makes sense.
The overall care may best be coordinated by the mental health professional, with the primary care clinician serving as a consultant/team member. The concept of a mental health maintenance organization makes sense in this context.57
The relationship between primary care and consultation/liaison (C/L) psychiatry is particularly interesting. C/L psychiatrists work in medical settings and thus provide a vital link between psychiatry and the rest of medicine. But very few psychiatrists work in ambulatory medical settings, and even as primary care clinicians are beginning to understand the nature of mental symptoms and disorders in their patients, there is a need for a corresponding psychiatric understanding of these patients that should converge on a single perspective. Given the sheer burden of mental illness in primary care, such inattention can be regarded as surprising. (It must be said that of the few mental health professionals conducting research inside primary care settings, a number of them are producing knowledge of truly outstanding quality.) Formulations conceived from within the context of psychiatric practice are altogether inadequate—the view from within primary care practice is an absolute prerequisite.
Several years ago Strain, Pincus, and colleagues undertook an ambitious survey of the psychiatric training of general medical practitioners.58 This survey described a rich variety of relationships between the two disciplines, but what was missing was a sense that they were converging on agreement about what was being observed, what needed to be learned, who should teach it, and how the relationship between them should be configured.
Finally, it makes sense to administer some treatments in the primary care setting, but not by primary care clinicians. For example, primary care patients with a preference or an indication for high-intensity services such as cognitive-behavioral therapy or family therapy, patients with chronic diseases requiring extensive patient education and support and perhaps case management, and somatizing patients may benefit from the coordinated, collaborative care of a primary care clinician and a psychologist, family therapist, counselor, social worker, case manager, or other mental health professional. These collaborative arrangements have enormous appeal and offer compelling theoretical advantages, but they must withstand the rigors of systematic evaluation before they can be endorsed without reservation.
Summary Of Implications
Research
We have learned a lot recently about the mental health of our citizens and about the services that we can bring to bear on their mental health problems. However, very little of the research leading to this knowledge has been conducted in the primary care setting. A conspicuous exception to this general statement is the Primary Care Research Program in the Services Research Branch of the
National Institute of Mental Health, which has produced impressive advances in the state of our knowledge for a relatively modest outlay. Since most mental health care occurs in the primary care setting, we have had a profoundly unbalanced mental health research agenda. At this time, the single most effective strategy for improving the mental health of the people of this country and one of the most effective strategies for improving the overall health of these same people would be to make a significant investment in primary care mental health research. The systems are already in place, awaiting our informed modifications and augmentations, to deal with much of the unmet mental health needs in the United States. What follows is a sampling of the kind of knowledge we need to realize this improvement.
- Descriptive work and the need for a new taxonomy, including the following:
- — So-called subthreshold syndromes.
- — High comorbidity syndromes, such as post-traumatic stress disorder, somatizing syndromes, and mixed anxiety-depression.
- — Medical–mental interactions. The relationship between medical illnesses and mental symptoms is bidirectional, or circular, and extremely complex. Since most mental disorders in primary care occur in patients having medical illness, this problem deserves particularly high priority. Unfortunately, untangling these relationships will require expensive, longitudinal cohort studies.
- — Expansion of our preoccupation with mental disorders to include other psychosocial factors and syndromes, such as the relational diagnoses.
- — Attention to patients with high levels of distress or functional impairment, but without a mental diagnosis.
- The natural history of detected and undetected disorders. There is some evidence that detection of certain mental disorders in primary care does not necessarily result in improved patient outcomes.37–40 This surprising finding needs to be explored in terms of detection bias, treatment bias, and treatment fidelity to ensure that our attentions are appropriate and effective.
- Development and refinement of outcome indicators, including:
- — Health-related quality of life and patterns of impairment.
- — Disease-specific outcome measures for mental syndromes common to primary care.
- — Patient satisfaction and its relation to cost and function.
- — The measurement of continuity, in all its varieties, and the assessment of its effects.
- — Utilization, especially beyond primary care services.
- — Indirect costs.
- — Modifier effects of comorbid conditions.
- Models of service delivery. This should involve observational studies during the innumerable natural experiments now under way, as well as effectiveness trials. We need tests of the effectiveness and cost-effectiveness of different collaborative and consultative modes between mental health professionals and primary care clinicians. These need to be condition specific and also need to take into account local variations, such as rurality, ethnic considerations, and prevailing customs. Wide-angle studies that look at the larger trade-offs involved in augmented mental health services are needed.
Finally, testing the transferability of clinical guidelines and therapies shown to be effective in mental health settings into the primary care setting needs to be done. This has been done for depression, and now needs to be done for the other common primary care mental disorders.
Educational
One of the most pressing needs is for the development of a coherent, consistent medical psychology that can be taught to all future clinicians. This should be in the undergraduate curriculum, as should material on the doctor-patient relationship and communication skills. A demonstrated capacity to communicate effectively with patients should be a prerequisite to the practice of primary care, since the essence of our work involves offering a safe, dependable clinical relationship in which any complaint can be received and evaluated. At the level of postgraduate residency training, there is still no agreement on what constitutes a behavioral science curriculum, how much time should be devoted to it, who should teach it, or how and where it should be taught. This is not to suggest that all programs should have identical, indistinguishable curricula, but that we are suffering for lack of a set of core knowledge and skills we can assume are present in all primary care clinicians. Educational leaders across all primary care disciplines should sit down together and draw up a master document dealing with this issue.
Until now we have depended extensively on specialists to educate us. It is clear that this education will be inappropriate unless we educate mental health educators themselves about how mental health and mental health care is different in the primary care setting as compared to the specialty setting. This is, therefore, a call for the placement of mental health educators and trainees in primary medical settings as a principal site of service. This applies to undergraduate medical education as well as resident training.
As managed care plans develop more stringent expectations about the provision of mental health services in primary care, clinicians will have to change their
practice habits. This will require a coherent, sustained educational effort. We have no idea about the most effective way to accomplish this.
Clinical
We must come to terms with what we have learned about mental health in primary care—we cannot unlearn what we have discovered. We must either mobilize our clinical resources to address mental problems or explicitly acknowledge that their prevalence and salience are insufficient to justify the expense and effort that it takes to address them. In some cases, for some disorders, this is probably the best course of action, but the evidence suggests that reordering primary care to accommodate the mental distress of patients would be a good investment.
Therefore, we must proceed to provide the incentives and resources necessary to force a restructuring of primary care along these lines. Nobody knows how to do this yet. For some years this will most likely involve experiments with modified caseloads, interjection of new personnel into the primary health care team, acquisition of skills and tasks by current members of the primary health care team, and new collaborative and consultative relationships with mental health professionals. It will involve the development of clear, explicit clinical expectations coupled with the knowledge, skills, and attitudes necessary to accomplish the expected clinical care. Management guidelines and diagnostic instruments are being developed for the most common mental diagnoses in primary care; now we must learn how to implement these tools into our routine clinical activities. This process will need to transpire under the eye of services researchers, economists, mental health professionals, and primary care clinicians—but mostly patients themselves should decide who will do what to whom.
References
1. Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–569.
2. Kroenke K, Spitzer RL, Williams JB, et al. Physical symptoms in primary care. Predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3:774–779.
3. Kirmayer LJ, Robbins JM, Dworkind M, Yaffe MJ. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry .1993;150:734–741.
4. Katon W, Von Korff M, Lin E, et al. Distressed high utilizers of medical care. DSM-III-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12:355–362.
5. Orleans C, George L, Houpt J, Brodie H. How primary care physicians treat psychiatric disorders: A national survey of family practitioners. Am J Psychiatry. 1985;142:52–57.
6. Von Korff M, Myers L. The primary care physician and psychiatric services. Gen Hosp Psychiatry. 1987;9:235–240.
7. Olfson M. Primary care patients who refuse specialized mental health services. Arch Intern Med. 1991;151:129–132.
8. Schulberg HC, Block MR, Madonia JJ, Rodriguez E, Scott CP, Lave J. Applicability of
clinical pharmacotherapy guidelines for major depression in primary care settings. Arch Fam Med. 1995;4:106–112.
9. Lamberts H. Unpublished data from The Transition Project; 1995.
10. Hankin J, Oktay JS. Mental disorder and primary medical care: An analytical review of the literature . D. No. 5. Washington, D.C.: National Institute of Mental Health; 1979.
11. Schulberg HC, Burns BJ. Mental disorders in primary care: Epidemiologic, diagnostic, and treatment research directions. Gen Hosp Psychiatry .1988;10:79–87.
12. Ormel J, Giel R. Medical effects of nonrecognition of affective disorders in primary care. In: Sartorius N, Goldberg D, deGirolamo G, Costa e Silva J, Lecrubier Y, Wittchen U, eds. Psychological Disorders in General Medical Settings. Toronto: Hogrefe & Huber; 1990:146–158.
13. Office of Technology Assessment, U.S. Congress. Children's mental health: Problems and services. A background paper. Washington, D.C.: Government Printing Office; 1986.
14. Costello E. Diagnosis and management of children in an organized primary health care setting. Bethesda, Md.: National Institute of Mental Health; 1987.
15. Spitzer RL, Williams BW, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 4;272:1749–1756.
16. Ormel J, VonKorff M, Ustun B, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. Results from the WHO collaborative study on psychological problems in general health care. JAMA. 1994;272:1741–1748.
17. Coyne JC, Fechner-Bates S, Schwenk TL. Prevalence, nature, and comorbidity of depressive disorders in primary care. Gen Hosp Psychiatry . 1994;16:267–276.
18. Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry. 1992;14:237–247.
19. Johnson D, Mellor V. The severity of depression in patients treated in general practice. J R College Gen Pract. 1977;237.
20. Sireling L, Paykel ES, Freeling P, Rao BM, S.P. P. Depression in general practice: Case thresholds and diagnosis . Br J Psychiatry .1985;147:113–119.
21. Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients. JAMA. 1989;626:914–919.
22. Shapiro S, Skinner EA, Kessler LG, et al. Utilization of health and mental health services: Three epidemiologic catchment area sites. Arch Gen Psychiatry. 1984;41:971–978.
23. Williams P, Tarnopolsky A, Hand D, Shepherd M. Minor psychiatric morbidity and general practice consultation: the West London Survey. Psychol Med. 1986:1–37.
24. McFarland BH, Freeborn DK, Mullooly JP, Pope CR. Utilization patterns among long-term enrollees in a prepaid group practice health maintenance organization. Med Care. 1985;23:1221–1233.
25. Smith GR. The course of somatization and its effects on utilization of health care resources. Psychosomatics. 1994;35:263–267.
26. deGruy FV, Dickinson L, Dickinson P, Hobson F. NOS: Subthreshold conditions in primary care. The Eighth Annual NIMH International Research Conference on Mental Health Problems in the General Health Care Sector. McLean, Va.: National Institute of Mental Health; 1994.
27. Weyerer S. Relationships between physical and psychological disorders. In: Sartorius N, Goldberg D, de Girolamo G, Costa e Silva J, Lecrubier Y, Wittchen U, eds. Psychological Disorders in General Medical Settings . Toronto: Hogrefe & Huber; 1990:34–46.
28. Wells KB, Golding JM, Burnam MA. Psychiatric disorder in a sample of the general population with and without chronic medical condition. Am J Psychiatry. 1988;145:976–981.
29. Katon W, Von Korff M, Lin E, et al. A randomized trial of psychiatric consultation with distressed high utilizers. Gen Hosp Psychiatry. 1992;14:86–98.
30. Brody DS, Lerman CE, Wolfson HG, Caputo GC. Improvement in physicians' counseling of patients with mental health problems. Arch Intern Med . 1990;150:993–998.
31. Higgins ES. A review of unrecognized mental illness in primary care: Prevalence, natural history, and efforts to change the course. Arch Fam Med. 1994;3:908–917.
32. Badger LW, deGruy FV, Hartman J, et al. Psychosocial interest, medical interviews, and the recognition of depression. Arch Fam Med . 1994;3:899–907.
33. Main D, Lutz L, Barrett J, Matthew J, Miller R. The role of primary care clinician attitudes, beliefs, and training in the diagnosis and treatment of depression. Arch Fam Med 1993;2:1061–1066.
34. Rost K, Smith GR, Matthews DB, Guise B. The deliberate misdiagnosis of major depression in primary care. Arch Fam Med. 1994;3:333–337.
35. Sturm R, Wells KB. How can care for depression become more cost-effective? JAMA. 1995;273:51–58.
36. Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines: Impact on depression in primary care. JAMA. 1995;273:1026–1031.
37. Schulberg H, McClelland M, Gooding W. Six month outcome for medical patients with depressive disorders. J Gen Intern Med 1987;2:312–317.
38. Schulberg H, Block M, Madonia M, Scott C, Lave J, Rodriguez E, Coulehan J. The ''usual care" of major depression in primary care practice. Arch Intern Med. In press.
39. Ormel J, Koeter M, van den Brink W, van de Willige G. Recognition, management and course of anxiety and depression in general practice. Arch Gen Psychiatry. 1991;48:700–706.
40. Simon G, Von Korff M. Recognition, management, and outcomes of depression in primary care. Arch Fam Med. 1995;4:99–105.
41. Panel DG. Depression in primary care. Rockville, Md.: Agency for Health Care Policy and Research; 1993.
42. Bryant E, Shimizu I. Sample design, sampling variance, and estimation procedures for the National Ambulatory Medical Care Survey. Vital and Health Statistics. Public Health Service; 1988.
43. Lewis CE. Disease prevention and health promotion practices of primary care physicians in the United States. Am J Prev Med. 1988;4(Suppl.):9–16.
44. Bass MJ, Elford RW. Preventive practice patterns of Canadian primary care physicians. Am J Prev Med. 1988;4(Suppl.):17–23.
45. Woo B, Woo B, Cook EF. Screening procedures in the asymptomatic adult: a comparison of physicians' recommendations, patients' desire, published guidelines, and actual practice. JAMA. 1985;254:1480–1484.
46. Romm FJ, Fletcher SW, Hulka BS. The periodic health examination: comparison of recommendations and internists' performance. South Med J. 1981;74:265–271.
47. Pincus HA. Assessing the effects of physician payment on treatment of mental disorders in primary care. Gen Hosp Psychiatry. 1990;12:23–29.
48. Richman A. Does psychiatric care by family practitioners reduce the cost of general medical care? Gen Hosp Psychiatry. 1990;12:19–22.
49. Hankin JR, Kessler LG, Goldberg ID, Steinwachs DM, Starfield BH. A longitudinal study of offset in the use of nonpsychiatric services following specialized mental health care. Medical Care. 1983;21:1099–1110.
50. Von Korff M, Katon W, Lin E, et al. Evaluation of cost and cost offset of collaborative management of depressed patients in primary care. The Eighth Annual NIMH International Research Conference on Mental Health Problems in the General Health Care Sector. McLean, Va.: National Institute of Mental Health; 1994.
51. Smith GR, Rost K, Kashner TM. A trial of the effect of a standardized psychiatric consultation on health outcomes and costs in somatizing patients. Arch Gen Psychiatry. 1995;52:238–243.
52. Rogers WH, Wells KB, Meredith LS, Sturm R, Burnam MA. Outcomes for adult outpatients with depression under prepaid or fee-for-service financing. Arch Gen Psychiatry. 1993;50:1002–1003.
53. Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men: A randomized trial. JAMA. 1984;252:2413–2417.
54. Mechanic D. Integrating mental health into a general health care system. Hosp Community Psychiatry. 1994;45:893–897.
55. Baldwin L, Inui TS, Steinkamp S. The effect of coordinated, multidisciplinary ambulatory care on service use, charges, quality of care, and patient satisfaction in the elderly. J Community Health. 1993;18:95–108.
56. Schulberg HC, Madonia MJ, Block MR, et al. Major depression in primary care practice: Clinical characteristics and treatment implications. Psychosomatics. 1995;36:129–137.
57. Scheffler R, Grogan C, Cuffel B, Penner S. A specialized mental health plan for persons with severe mental illness under managed competition. Hosp Community Psychiatry. 1993;44:937–942.
58. Strain JJ, Pincus HA, Gise LH, Houpt JL. The role of psychiatry in the training of primary care physicians. Gen Hosp Psychiatry. 1986;8:372–385.