E Life in the Kaleidoscope: The Impact of Managed Care on the U.S. Health Care Workforce and a New Model for the Delivery of Primary Care
Richard M. Scheffler, Ph.D.
Supported in part by the Bureau of Health Professions, Resources and Health Services Administration, Department of Health and Human Services.
Richard S. Scheffler is professor of health economics and public policy at the School of Public Health and the Graduate School of Public Policy, University of California, Berkeley. Dr. Scheffler earned a Ph.D. in economics at New York University. His published research includes studies of health care workforce policy, managed care, the economics of preventive health measures, and mental health care delivery systems. Dr. Scheffler is currently a member of the Institute of Medicine Committee on the Future of Primary Care and co-author (with Norman S. Waitzman) of a forthcoming book on the physician workforce in the era of managed care.
Abstract
Market forces are producing dramatic changes in health care financing and delivery mechanisms. Payment systems are rapidly moving away from fee for service to capitation and risk sharing between payers and providers. These changes are likely to result in a major reconfiguration of the health care workforce over the next few decades. In the world before managed care, individual physicians and hospitals were the system's principal billing units and workforce research focused primarily on physicians. In the world after managed care, group practices and organized delivery systems are the principal billing units and physicians are one of a number of clinicians on a team of health care professionals. Application of managed care organization staffing ratios to the entire delivery system implies significant physician surpluses (particularly specialists) and shortages
of nurse practitioners and physician assistants. Successful development of the team delivery concept will require development of economic incentive systems that reward team effort. To stimulate thought about the challenges that a team concept produces, this paper presents an innovative model of team health production. Finally, the workforce modification suggests the need for an ambitious research agenda: one that deals with micro- and macro-issues of team and workforce composition, organizational forms and incentives, practice context, and overall health care policy.
Introduction
In response to the projected excess supply of physician specialists,1 the rapid growth of managed care,2 and continued pressure to limit increases in health care costs, the organization of the U.S. health care workforce is likely to undergo dramatic change over the next few decades. Virtually all of the major workforce components are subject to reconfiguration. In broad terms, what will this reconfiguration look like? What are the implications of this reconfiguration for the previously established ideas about how to assess health workforce needs? What should a research agenda for the next few decades look like at this stage of the reconfiguration?
This paper addresses these questions with a special emphasis on primary care as defined by the Institute of Medicine (Institute of Medicine, 1994). The IOM definition emphasizes the integration of services and supports the team delivery of primary care.3
Primary care is the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community (Institute of Medicine, 1994, p. 1).
|
1 |
Although most recent forecasts of physician supply have predicted a surplus of physician specialists (Gamliel et al., 1995; Kohler, 1994), some researchers believe that advancements in medical technology and other factors will create shortages of physicians (Schwartz, Sloan, and Mendelson, 1988; Schwartz and Mendelson, 1990). As explained elsewhere in this paper, projections of the size and composition of the future health care workforce are sensitive to assumptions about patient utilization patterns, use of nonphysician clinicians, and other factors. |
|
2 |
For the purposes of this paper, managed care is defined as health plans and products that involve the integration of health care financing and delivery systems. |
|
3 |
Although this definition does not explicitly mention teams, Chapter 2 of the 1994 IOM report discusses the importance of team structures in primary care (Institute of Medicine, 1994). "Team" is a broad term that connotes a collaborative grouping of individuals whose clinical, managerial, and interpersonal skills can be brought to bear on individual or family health. The composition of the team will vary according to the type of individual or population served. Although teams are often organized in a hierarchical manner, IOM conceives of teams as more democratic, interdisciplinary structures in which clinicians rotate leadership and accountability depending on the patient situation. |
Integration is the key term because it reflects ongoing structural changes in the health care system (Physician Payment Review Commission, 1995). However, this term has multiple meanings. It can connote the integration of primary care and specialty care, the merger of inpatient and outpatient treatment, or a combination of organizational structures and financial incentives such as group practice with capitation (Shortell and Hull, 1995; Shortell, Gillies, and Anderson, 1994). Economists typically view integration in efficiency terms: how do we organize the health workforce in an efficient way without sacrificing quality of care? This is an ambitious goal, but one for which governments, employers, and the public are striving.
It is useful to classify relationships among workforce components in terms that turn on the notion of skills: (1) What is the set of skills unique to each type of clinician? (2) What set of skills can more than one clinician use? (3) What sets of skills are interdependent (i.e., skills that require more than one health care worker)? The first set contains specific skills, the second contains substitutional skills, and the third contains complementary skills. Skill, as defined here, involves clinical, interpersonal, and organization or management competencies.
The relative economic returns to each type of skill since the 1980s after managed care (AMC) are likely to be much different than those prior to the 1980s before managed care (BMC). BMC, the health care workforce functioned in a fee for service (FFS), patient self-referral, and physician-specialty-dominated system. AMC, the health care workforce copes with capitated payment and managed-patient referrals, and strives to integrate primary care and specialty care.
The Health Care Workforce BMC And AMC
BMC, the health system was characterized by few payer restrictions on patient choice of providers, independent provider billing units, and open-ended FFS payment. Patients freely chose the providers whom they believed would provide the best care; freestanding physicians, hospitals, and other providers did the billing; and insurance plans paid virtually all provider bills (Enthoven, 1987; Pauly, 1970). Because insurance payment schedules favored highly specialized, procedure-based skills, this system rewarded specialty over primary care (Delbanco, Meyers, and Segal, 1979; Roe, 1981).
The health system BMC supported nonphysician clinicians to a limited degree. In the 1970s it began to train and license significant numbers of nurse practitioners (NPs) and physician assistants (PAs).4 However, because of physician resistance, legal restrictions, and other barriers, NPs and PAs were delegated
a very limited set of clinical tasks and payment systems ignored complementary skills. NP and PA substitution also did not generate significant economic rewards for physicians, because substitution could result in smaller payments. However, substitution did make economic sense where there were shortages of physicians or, in some rare circumstances, where increased throughput could offset reduced payments (Safriet, 1992; U.S. Congress, Office of Technology Assessment, 1986).
Workforce policy debates of the 1960s, 1970s, and 1980s focused primarily on physician supply issues (Fein, 1967; Ginzberg, 1978; Ginzberg and Ostow, 1984; Scheffler et al., 1978; Schwartz, Sloan, and Mendelson, 1988). The debate dealt with numbers: How many more doctors did we need? Was there a surplus or shortage of primary care doctors or specialists? BMC, the emphasis on physicians made sense, particularly from an economic perspective. However, as discussed later, the focus on physicians is attenuated in the AMC world.
In the AMC world, the predominant payment mode is capitation, patient choice of providers is more restricted, and payers or primary care case managers control access to specialists and hospitals. Under managed care, the financing and delivery of care are integrated, and the billing unit is more likely to be a group practice or network of providers, rather than a solo-practice physician or individual hospital (Physician Payment Review Commission, 1995; Shortell and Hull, 1995).
A long-run-oriented managed care organization under capitation has a strong incentive to find the most efficient combination of health care professionals to deliver quality care to an enrolled population.5 As explained below, in the AMC world collaborative practice among diverse teams of clinicians, rather than a physician specialist orientation, begins to make economic sense. Consequently, PAs and NPs could have a much more important role to play in the AMC health care system.6
The Supply Of PAs And NPs
PAs have generally been physician substitutes supervised by physicians. As of 1993, roughly 27,000 persons had graduated from PA training programs; 23,000 were actually engaged in practice (Bureau of Health Professions, U.S. Department of Health and Human Services, 1994). About 1,600 individuals graduated from U.S. PA training programs in 1992 (Cawley, 1993). Health maintenance organizations (HMOs) currently employ 8 percent of PAs, and if clinic settings are included, almost two-thirds of all PAs work in some type of ambulatory care setting (Bureau of Health Professions, U.S. Department of Health and Human Services, 1994). As of 1992, approximately 43 percent of PAs worked in primary care (family practice, general internal medicine, and general pediatrics). Since the late 1970s the proportion of PAs working in specialty areas has steadily increased. The fastest growth has been in surgical subspecialties, where 22 percent of all PAs now work (Cawley, 1993).
As of 1992, approximately 28,000 NPs were certified by a national organization (such as the American Nurses Association) or a state, and 27,000 of these NPs were employed in nursing positions (Moses, 1994). NPs are increasingly receiving master's-level preparation, and in 1992 approximately 1,500 NPs graduated from U.S. nursing schools with master's degrees (Aiken, Gwyther, and Whelan, 1994). Although an additional 20,000 noncertified NPs also appear to have some level of formal training, the total number of certified and noncertified nurse practitioners is difficult to determine, because licensing and educational requirements vary significantly across the states (Morgan, 1993; Washington Consulting Group, 1994). NPs work in some arenas as physician substitutes and in other arenas as complements providing services such as health prevention, patient education, and counseling. In nine states NPs can establish independent practices7 (Birkholz and Walker, 1994; Henderson and Chovan, 1994; Pearson, 1994). Almost 11 percent of NPs now have hospital admitting privileges and one-third have hospital discharge privileges. About 29 percent work in private practices or HMOs, 23 percent work in hospital outpatient departments, 11 percent work in hospital inpatient departments, and 23 percent in public or community health centers (Washington Consulting Group, 1994). Approximately 42 percent of NPs render primary care (family/general practice, general internal medicine, or general pediatrics) (Physician Payment Review Commission, 1994).
Productivity And Quality Of PAs And NPs
Given the economic incentives associated with capitation, health care delivery
organizations should employ PAs and NPs to the extent that they improve the competitive position of the organizations: by improving productivity, enhancing quality of care, and increasing patient satisfaction.8 This section summarizes the key findings from the literature on productivity and quality of care.
Productivity
Simply put, productivity is output per unit of input. In the context of workforce policy, researchers are interested in comparing the productivity levels of physicians, nonphysician clinicians, and entire teams of clinicians, as well the gains in productivity that might be realized through reconfiguration of the delivery system. It is important to know how many patients can be treated or how many services can be delivered per unit of time (per hour, per day, per month, per year), how this might vary by clinician or team, and how reconfiguration of the delivery system changes the numbers. For example, are PAs or NPs more productive in staff model HMOs than in other settings? How does their productivity compare with those of physicians in different settings? What is the impact on team productivity from adding a second or a third PA or NP to a practice that already employs at least one?
Most productivity studies of PAs and NPs have focused on opportunities for physician substitution (Reinhardt, 1975, 1991). A typical study will ask, "How many tasks currently performed by a physician could be performed by a PA or NP?" The tasks that PAs and NPs can perform in their roles as a physician substitute can vary greatly (Ross, Bower and Sibbald, 1994).9 Table E-1 summarizes key findings from selected productivity studies of PAs and/or NPs over a recent 15-year period and also illustrates the variety of approaches used by researchers to measure PA and NP inputs and outputs.10 Some clear, long-standing patterns have emerged from empirical investigations of PA and NP productivity. Studies generally indicate that the substitution rate of PAs and NPs for physicians is somewhere between one-half and three-fourths; that is, PAs and NPs can substitute for some (but not all) physician roles at that rate. For example, Schneider and Foley (1977) found that the addition of roughly 13 NPs allowed an HMO to reduce its staffing of physicians by 6.72 physicians, a substitution ratio
|
8 |
Whether the organization is a for-profit or nonprofit organization influences how it responds to economic incentives (Pauly, Hillman, and Kerstein, 1990). However, both types of organizations will focus on productivity, quality, and patient satisfaction. |
|
9 |
During its visits to selected primary health care delivery organizations around the United States, the IOM Committee on the Future of Primary Care observed that in response to managed care cost pressures, some of the organizations had transferred certain triage-related tasks from clinicians to nonclinicians. For instance, one of the organizations visited by the committee trained its telephone assistants in the use of a structured patient interview protocol for initial screening of urinary tract infections. |
|
10 |
The Gravely and Littlefield study (1992) listed in Table E-1 also examined the productivity of teams that included clinical nurse specialists other than NPs. |
TABLE E-1 Key Findings from Selected Non-Physician Provider (NPP) Productivity Studies, 1979–1993
of 50 percent. They found a similar substitution rate of NPs for pediatricians. In another study, Scheffler calculated the marginal rate of substitution of PAs for physicians to be 63 percent (Scheffler, 1979). Record et al. (1980) reviewed a large number of productivity studies and concluded that the rate of task delegation (i.e., the percentage of physician tasks that a PA or NP can perform) is typically 0.75 for large practices (four or more providers) and 0.40 for small practices in adult care. In pediatric care, the delegation figures were 0.90 and 0.45, respectively. Because of scale economies, large practices are more likely to use PAs and NPs and tend to delegate a larger proportion of medical services. In a small practice, the volume of services that can be handled by a PA or NP may not be large enough to fill up his or her time (Record et al., 1980).
Comparing productivity levels in different types of settings is complicated by a variety of factors. Some early studies assumed that the patient mix in physician practices did not change with the introduction of PAs or NPs and that the substitutions were representative of all types of medical practices (U.S. Congress, Office of Technology Assessment, 1986). However, if NPs and PAs treat less serious or less risky cases than physicians, simple comparisons of substitution ratios and productivity levels may be misleading. Furthermore, PAs or NPs may add costs to a physician practice that go beyond their salaries and fringe benefits. For example, NPs and PAs might order more tests than physicians or prescribe more drugs, and they may require additional space, supervision, equipment, malpractice insurance, and training. Thus, productivity studies must examine changes in total practice resources, not just salaries.11
Quality of Care and Patient Satisfaction
PAs and NPs have demonstrated that they are able to deliver care in a manner acceptable to patients, and research shows that they deliver more preventive and educational services than physicians. Studies show that PAs and NPs deliver health care services that are comparable, in terms of clinical outcomes, to the care provided by physicians, and the care provided by the nonphysician practitioners is often superior in terms of patient satisfaction and process measures (Brown and Grimes, 1993; U.S. Congress, Office of Technology Assessment, 1986). Furthermore, recent studies that have looked at geriatric care, neonatal intensive care unit care, and colposcopy show that not only primary care but specialty care is in the purview of advanced practice nurses (APNs) such as NPs (Burl and Bonner, 1991; Burl, Bonner, and Rao, 1994; Carzoli et al., 1994; Hartz, 1995). Additionally, the U.S. Department of Health and Human Services has examined National Practitioner Data Bank malpractice reports for APNs, showing them to be much
less frequently reported than physicians (Birkholz, 1995). However, a major limitation of the medical literature on PAs and NPs is the absence of recent (1986 or later), methodologically rigorous studies comparing NPs or PAs with physicians or each other (Scheffler, 1995).
The following appear to be reasonable conclusions regarding quality of care at this time:
- Nonphysician clinicians who have received training equivalent to that of physicians in a technical procedure can perform the procedure as well as physicians.
- Nonphysician clinicians can supply high-quality care for simple acute problems and chronic stable ones. Studies are not adequate to determine whether these providers may occasionally miss a rare diagnosis (and fail to seek consultation12), nor are they adequate to determine whether nonphysician clinicians can treat complicated cases as well as physicians can.
- There is no evidence to support the assertion that independent practice by nonphysician clinicians results in quality of care comparable to that of collaborative practice or that of physician-only care. Neither is there evidence against this assertion. Studies have not been conducted, in part, because of the paucity of such independent practices (Scheffler, 1995).
Health Care Workforce Configuration Studies
This section and the two sections that follow describe several investigations of PA and NP staffing and productivity, the potential impacts of PAs and NPs on the overall health workforce, and two case studies of mature staff-model HMOs. This discussion emphasizes (1) the variations in managed care organizations' workforces that have emerged in recent years and (2) the adjustments necessary to compare workforces across organizations.
Recently, several noteworthy studies of PAs and NPs have appeared. Hooker (1993) studied PA and NP staffing in Kaiser Permanente's Northwest Region (KPNW), which provides prepaid medical care to 380,000 members in the Portland, Oregon, metropolitan area. During 1992, KPNW had 2.5 million patient encounters and employed 520 full-time-equivalent physicians. Hooker analyzed clinical staffing patterns and productivity by specialty. In internal medicine, KPNW used 100 physicians, 13 PAs, and 15.5 NPs, the highest number of nonphysician providers (NPPs) in any specialty other than mental health. KPNW also used significant numbers of NPPs in family practice and obstetrics-gynecology
(OB-GYN), although the ratios of NPPs to physicians were higher in several other specialties. The physician/NPP staffing ratios in family practice and OB-GYN differed from each other, with OB/GYN using more NPs and certified nurse-midwives. Hooker also reported that although physicians and PAs saw similar types of patients NPs delivered almost twice the amount of preventive service and three times the amount of prenatal services. NPs performed most routine physical exams, which suggests that more complex patients were seen by physicians and PAs. That study indicates that KPNW patients' quality ratings (based on patient satisfaction) of NPs and PAs were comparable to the ratings of physicians.
Hooker's study must be viewed in context, as the KPNW model might not be generalizable. KPNW has a long tradition of using NPs and PAs (Hooker, 1993), and Oregon has a relatively liberal medical practice act that allows NPs (but not PAs) to prescribe medication (Henderson and Chovan, 1994). Furthermore, within the Kaiser system the use of NPs and PAs varies dramatically. For example, Kaiser's Northern California Region employs 360 NPs but only a handful of PAs, whereas the Southern California Region has more than 500 PAs and NPs on staff. Many factors apparently influence the differences in NP and PA use, including the supply of physicians, the locations of NP and PA training programs, legal liability considerations, management opinion, physician beliefs about NP and PA effectiveness, and acceptance of nonphysician clinicians by enrollees (Hooker, 1993).
Although not translatable to a non-hospital-based practice environment, Knickman et al. (1992) conducted an important investigation of the potential for substituting nonphysicians for resident physicians at two New York City hospitals. Using a time-motion study, Knickman and his colleagues analyzed physicians' clinical tasks under two different models: a traditional model in which the physician resident is the primary medical manager and an alternative model in which a nonphysician clinician such as an NP performs baseline patient care monitoring. In the traditional model, residents spent almost half of their time on tasks that they could not delegate. However, using the alternative practice model the study found that only 20 percent of the residents' time was nondelegatable.13
Other studies have shown that NPs can work effectively in trauma units (Spisso et al., 1990), geriatric care settings (Burl, Bonner, and Rao, 1994), and neonatal intensive care units (Carzoli et al., 1994). Although it is not possible to quantify productivity gains from these studies, they suggest that the potential for efficiency gains exists in a variety of clinical settings.
Potential Impact Of PAs And NPs On The Overall Health Care Workforce
The studies described above suggest that NPs and PAs can make major contributions to the health care system. However, estimates of the overall impacts of NPs and PAs on the size and composition of the future health workforce vary widely because of the different assumptions that forecasters make about patient utilization rates, physician delegation rates, the extent to which managed care organizations are willing to use NPPs, and other variables. The varying assumptions about managed care organizations reflect the fact that so far, researchers have been able to obtain detailed data on physician and nonphysician staffing patterns for only a handful of HMOs and staffing patterns vary widely among those HMOs that have made data accessible to researchers (Weiner, 1993, 1994).
In 1980, the Graduate Medical Education National Advisory Committee (GMENAC) published its report to the secretary of the U.S. Department of Health and Human Services on the future national supply and requirements for physicians, concluding that there would be a surplus of 70,000 physicians by 1990 (15 percent more than needed) and 145,000 by the year 2000 (30 percent more than needed) (Health Resources Administration, 1981a). These projections were developed by a panel of experts by combining current utilization patterns, projected numbers of medical school graduates and international medical graduates, population trends, and other data. The GMENAC approach to forecasting physician requirements was based on need (''needs-based"): the basic premise was that the requirements should be based on an assessment of the total burden of disease and disability for all people (McNutt, 1981).
Although GMENAC did consider the possibilities for delegating certain physician tasks to NPs and PAs (Health Resources Administration, 1981b), it did not anticipate the subsequent rapid enrollment growth in managed care organizations. Steinwachs and his colleagues (1986) compared actual staffing patterns in three large HMOs in the early 1980s with the national requirements for physicians in 1990 projected by GMENAC. They concluded that compared with the projections of GMENAC, after making adjustments for demographic and other differences between HMO patients and the overall U.S. population, 20 percent fewer primary care physicians for children and 50 percent fewer primary care physicians for adults would be needed to meet national primary care needs. Interestingly, that study found that GMENAC's assumed percentages of primary care encounters that could be handled by nonphysicians (12 percent of adult health care encounters and 15 percent of child health care encounters) were substantially higher than the actual HMO percentages. Nevertheless, the authors' estimates of overall national physician requirements were still lower than the GMENAC projections, primarily because the patient utilization rates reported
by the HMOs were lower than GMENAC's needs-based estimates (Weiner, Steinwachs and Williamson, 1986).
An unpublished 1991 study by Marder, Gaumer, and Minkovitz, using a GMENAC-type model which incorporates clinical experts' judgments about appropriate patient utilization patterns rather than actual FFS or HMO utilization rates, estimated that NPs and PAs could assume responsibility for 630 million visits or slightly more than one-third of the 2.1 billion annual U.S. primary care visits. Marder and his colleagues employed a delegation rate for adult medicine of 30 percent and one for pediatrics of 33 percent. Conservatively, that study indicated that there is a potential shortfall of about 75,000 PAs and NPs in primary care alone. The increased use of PAs and NPs in specialty care suggested by recent trends would exacerbate the shortfall (Cawley, 1993). That study also concluded that there would be surpluses of most types of primary care physicians in the United States by the year 2010 (Marder, Gaumer, and Minkowitz, 1991).
In a more recent study, Weiner extrapolated HMO staffing levels to the entire U.S. physician workforce, adjusting for demographic and other differences between HMOs' enrolled populations and the overall U.S. population. He estimated that national physician requirements in the year 2000 under two reform scenarios that provided for staffing based on HMO patterns would range from 137.5 to 143.8 physicians per 100,000:58.7 to 59.2 primary care physicians per 100,000 and 78.8 to 84.6 specialists per 100,000. Weiner concluded that (1) there will be an overall surplus of about 165,000 physicians by the year 2000, (2) supply and demand of primary care physicians will be in relative balance, and (3) the supply of specialists will exceed the requirements by more than 60 percent. Although Weiner did not project the demand for NPs and PAs, he observed that, in general, HMOs appear to use more NPs and PAs than the overall U.S. health system (23.0 per 100,000 lives in HMOs versus 19.6 per 100,000 lives overall). Thus, his study also implies that demand for NPs and PAs will increase in the AMC world (Weiner, 1994).
Staffing Patterns: Case Studies Of Two Mature HMOs
As part of the IOM study on the future of primary care, clinical staffing data were collected on two mature, West Coast-based HMOs (see Table E-214). These simple case studies illustrate the large staffing variations that apparently exist in the HMO industry and the implications of these variations for the future size and composition of the U.S. health workforce.
|
14 |
Table E-2 presents 1994 staffing data for each HMO plan. I also analyzed staffing for 1992 and 1993 and found that staffing patterns in each plan had been fairly stable over a 3-year period. |
TABLE E-2 1994 Staffing Patterns in Two West Coast Staff Model HMOs
HMO #1
HMO #1 is a West Coast-based staff model plan. In 1994, this HMO had 177 physicians per 100,000 enrollees.15 In addition, HMO #1 used 31 PAs and 42 NPs per 100,000 enrollees. Thus, HMO #1 used 2.4 physicians for each PA or NP.
TABLE E-3 Projected U.S. Health Workforce Based on Selected HMO Staffing Patterns*
In 1994, physician specialists in HMO #1 accounted for 57 percent of the total physician staff and 40 percent of the total clinical staff. Adding specialist PAs and NPs to physician specialists, we observe that 58 percent of HMO #1's clinicians were involved in specialty care.
If HMO #1's clinical staffing ratios are directly applied to the entire U.S. population (see Table E-3), there would be a need for approximately 457,000 total active patient care physicians in the United States, approximately 75,00016 fewer nonfederal physicians than were actually involved in patient care in 1993.17 Moreover, if the entire United States (like HMO #1) used 31 PAs and 42 NPs per 100,000 population, there would be a current need for approximately 80,000 Pas
and 108,000 NPs, resulting in a nationwide shortfall of 57,000 PAs and 81,000 NPs. As noted previously, there are currently 23,000 and 27,000 active certified PAs and NPs, respectively, in the United States.
HMO #2
The second HMO case study also involves a West Coast-based staff model plan. In 1994, HMO #2 had a younger population than HMO #1:9 percent of HMO #2's enrollees were 65 and older, compared with 12 percent of HMO #1's enrollees (see Table E-2). Despite its younger patient population, HMO #2's overall physician staffing ratio was somewhat higher than HMO #1's ratio (185 versus 177 physicians per 100,000 enrollees, respectively), and it also did not use NPs and PAs to the same extent as HMO #1. In 1994, HMO #2 used 15 PAs and 35 NPs per 100,000 enrollees,18 compared with 31 PAs and 42 NPs in HMO #1. Overall, HMO #2 used 3.7 physicians for each PA or NP, about 50 percent higher than HMO #1's physician to PA or NP ratio.
Staffing in HMO #2 was more oriented toward physician specialists. In 1994, 68 percent of HMO #2's physicians (exclusive of OB-GYNs) were specialists, versus 57 percent in HMO #1. Furthermore, 54 percent of HMO #2's overall clinical staff consisted of specialty physicians, compared with 40 percent for HMO #1. Adding specialist PAs and NPs to physician specialists, we observe that 69 percent of HMO #2's clinicians were involved in specialty care, compared with 58 percent in HMO #1.
Projecting HMO #2's staffing ratios over the entire U.S. population (see Table E-3) suggests the need for 477,000 total physicians, resulting in a surplus of 55,000 physicians. The overall need for PAs and NPs in the United States amounts to 39,000 and 91,000, respectively. Thus, even based on HMO #2's staffing patterns (which rely much more on physician specialists than HMO #1), there would be a nationwide shortfall of 16,000 certified PAs and 64,000 certified NPs in relation to the current supply of active professionals.
Results Of Comparison Of HMOs
This simple comparison of staffing patterns in two mature HMOs illustrates some important lessons and indicates the need for more research into the underlying causes of staffing variations in managed care organizations. First, merely counting physicians and specialist physicians does not provide a useful staffing analysis in a managed care world. Researchers must also examine the use of PAs, NPs, and other nonphysician clinicians. Second, researchers cannot merely compare
the number of health professionals used by a plan to the total plan enrollment in order to make inferences about productivity. They need to investigate differences in enrollee and other plan characteristics (enrollee age and sex distribution, severity of patient illness, patient outcomes, staff productivity, and the organizational structure of the clinical practice). Third, there are certain health care workforce parameters that staffing numbers alone cannot reveal, such as complementarity and substitution possibilities within health care teams.
Elements Of A New Model Of Team Health Production
The 1978 IOM definition of primary care and the new (1994) definition both support the delivery of primary care in the context of a collaborative format (Institute of Medicine, 1994). Although there is a substantial body of literature on primary care team models, most of this literature is based on research conducted in FFS settings prior to the 1980s (Baldwin, 1994). What is missing is a conceptual framework for team delivery of primary care in contemporary managed care environments that explicitly considers the role of economic incentives in the health production process.19 This section presents a model that is consistent with the new IOM definition of primary care.
Implicit in the discussion that follows is the notion that current managed care payment incentives may not always produce optimal outcomes in terms of quality of care, patient satisfaction, or efficient use of resources. Whether payment20 incentives can produce optimal outcomes depends on a variety of factors. For example, health care purchasers (e.g., employers and purchasing cooperatives) must be willing and able to balance incentives for high quality and low cost. Even though purchasers are increasingly demanding both high quality and low cost and are developing tools for comparing risk-adjusted costs and outcomes across provider organizations (Giacomini, Luft, and Robinson, 1995; Report Card Project, 1995; U.S. General Accounting Office, 1994b; Winslow, 1995), these tools currently have significant limitations (Epstein, 1995; Giacomini, Luft, and Robinson, 1995; U.S. General Accounting Office, 1994a). This is an important consideration because some physicians may respond to capitation by withholding beneficial treatment (Pauly, 1992; Rodwin, 1993). Furthermore, the effects of current managed care payment incentives on access to care for vulnerable subpopulations such as the poor, the severely mentally ill, and the chronically ill are
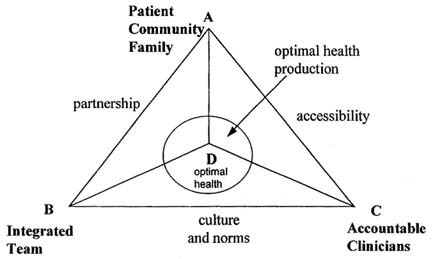
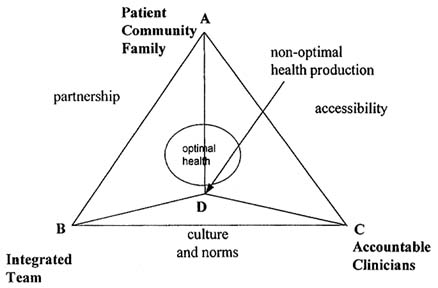
FIGURE E-1 Optimal health production.
not well understood (Davis and Rowland, 1991; Lurie et al., 1992; Safran, Tarlov, and Rogers, 1994).
Optimal Production of Health
This model begins with three basic premises: (1) the ultimate goal of primary care is the optimal health of the patient, produced with the least-cost combination of inputs; (2) the optimal health outcome is achievable; and (3) patients, individual clinicians, and health care teams each contribute certain unique, critical inputs to the health production process.21 For example, patients must comply with medical advice and engage in preventive health behaviors; team members must share information to maintain continuity of care.
In Figure E-1 the circle represents the optimal production of health. The circle varies in size depending on how exact or inexact the measure of a health outcome may be. The more exact the measure of the health outcome, the smaller the circle. Attainment of an optimal health outcome (point D) requires a mix of inputs: from the patient, community, and family (vertex A of the triangle), the integrated team (vertex B of the triangle), and/or individual clinicians who are accountable for the patient's health outcomes (vertex C of the triangle). The
location of the optimal production circle can change depending on whether a particular treatment or disease requires more inputs from the patient, community, and family (the circle would move toward vertex A), individual accountable clinicians (toward vertex C), or the team (toward vertex B). For example, treatment of a simple fracture might find the circle located far away from vertex B because an individual clinician and the patient can accomplish this task with few inputs from the team. In contrast, a treatment regimen for heart disease would require a variety of complex inputs from individual clinicians, the team, and the patient. Therefore, in this situation the circle would be located in the center of the triangle.
The sides of the triangle show the relationships among the three points of the triangle. The role of each accountable clinician is to facilitate access to care: side AC. Optimal access occurs when an individual clinician (e.g., physician, PA or NP) assumes responsibility for the patient's health outcome. Side AB represents the partnership between the patient, the family, and the community, in accordance with the 1994 IOM definition of primary care. Patient outcomes need to be evaluated in the context of this partnership. Finally, the team and the individual clinicians must commit to a patient-centered culture and set of norms that encourage optimal health outcomes and efficient delivery of care. Accordingly, side BC represents culture and norms. Each of these sides may vary in length, depending on the amount of inputs contributed by each element.
Patient goals must be aligned with economic incentives to achieve optimal health outcomes (Dranove and White, 1987). Thus, economic incentives should elicit the least-cost combination of inputs from the patient, community, family, accountable clinicians, and the team that achieves the optimal health outcome. In Figure E-1, the lines from each of the vertices to point D represent the amount of each input: line AD represents the contribution by the patient, community, and family to the production of his or her own health, line CD is the contribution of individual clinicians, and line BD is the contribution provided by the team (above and beyond individual contributions). This joint effort should clearly define mutually determined accountability as well as rewards for the members of the team. In this example the contributions intersect at point D, the optimal health outcome.
Nonoptimal Production of Health
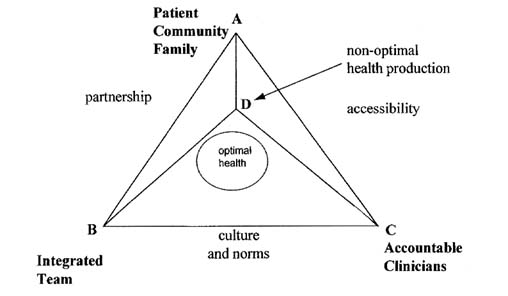
If economic incentives do not work properly, the payment system may elicit a mix of inputs that are too costly for the task at hand and/or that fail to achieve an optimal health outcome. For example, if the incentives stimulate the right amount of inputs from the patient and individual clinicians but fail to adequately reward team collaboration when it is needed, the optimal patient outcome may not be achieved (i.e., point D is outside the circle), as shown in Figure E-2. Alternatively, if the incentives stimulate the right amount of inputs from the
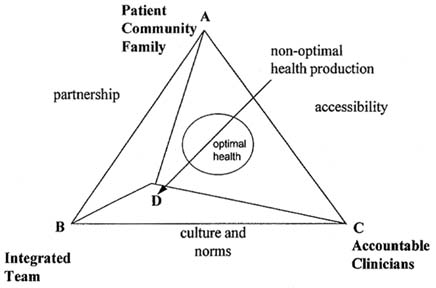
FIGURE E-2 Nonoptimal health production.
patient, family, and community but do not generate the right amount of inputs from both the individual clinicians and team, a suboptimal patient outcome (i.e., point D is outside the circle) may also be achieved, as shown in Figure E-3.
Improperly designed financial incentives could elicit an excessive rather than an insufficient amount of inputs from individual clinicians and teams. Figure E-4 illustrates a situation in which excessive payments have stimulated too many of these types of inputs: the health system relies too much on inputs from clinicians and not enough on the patient, family, and community. For example, a patient's expensive treatment plan for bronchitis fails because he does not receive adequate family and community support for smoking cessation.
To summarize, the challenge for the health care system is to generate an appropriate mix of patient involvement, contributions from individual clinicians, and teamwork. The system requires a balance, in the sense that the patient, the individual providers, and the team must provide just the right level and combination of inputs, so that optimal health outcomes are achieved. The economic reward structure must encourage this balance, but this is not easily accomplished. Heretofore, rewards generally emphasized individual clinicians; rewards for team performance have been rare and rewards (other than intrinsic) for patient participation in the process have been almost nonexistent. In essence, the system seems to have produced the outcome shown in Figure E-4. The challenge for health policymakers who are trying to develop the AMC workforce will be to design economic incentives that produce the optimal health outcome for the patient,
shown in Figure E-1. An additional challenge will be to design work-forces that are economically feasible but that also meet the diverse needs of different populations.
A New Health Care Workforce Research Agenda
This paper has shown that the AMC world will probably be a much different place than the BMC world. If the nation is to develop a health care workforce policy that meets the needs of this new world, policymakers must develop a workforce research agenda attuned to these needs. This section identifies the major gaps in the current health workforce research literature.
Productivity
Productivity studies in the BMC world focused primarily on opportunities for physician substitution: primary care physicians for specialists and PAs and NPs for physicians. The traditional emphasis on substitution has intuitive appeal, but it also has substantial limitations. A key research priority in the AMC world will be to improve and extend our knowledge about complements as well as substitutions. Researchers will also need to identify institutional barriers to productivity, because some practices may be organized in a manner that does not permit realization of the potential productivity gains from PAs and NPs. For example, some practices may simply be too small to efficiently utilize indivisible inputs such as PAs and NPs (Record et al., 1980; Steinwachs, 1992), whereas others may lack adequate information systems to measure costs and patient outcomes (Shortell and Hull, 1995). Also, effective substitution may require redeployment of physicians so that when substitution occurs the physician can perform other, more productive tasks. If there are already too many physicians, substitution of NPs and PAs for physicians may produce less in the way of benefits than we might otherwise expect.22
Legal Restrictions on NPs and PAs
Legal restrictions may adversely affect the ability of NPs, PAs, and other nonphysician clinicians to practice at levels commensurate with their training and skills (Sekscenski et al., 1994). Lack of uniformity among the states and arbitrary
(i.e., not based on well-established differences in clinical skills or patient outcomes) limitations prevent full utilization of PAs and NPs in many settings (Bureau of Health Professions, U.S. Department of Health and Human Services, 1994; Henderson and Chovan, 1994; Jones and Cawley, 1994; Safriet, 1994). An additional tension exists between sets of providers when legal accountability for all actions falls on the physician. Thus, an expanded scope of practice for nonphysician clinicians may require changes in legal liability principles (Chiarella, 1993).
Workforce research in the AMC world could play an important role in shaping the public policy debate about the appropriate role of nonphysician clinicians in the health care delivery system. Although the health policy literature provides many examples of how scope-of-practice laws and payment barriers constrain the effectiveness of non-physician professionals in traditional FFS settings, no recent analyses of controlled or natural experiments clearly establish a cause and effect relationship between specific practice barriers and clinical or economic outcomes. Furthermore, virtually no studies compare the impact of practice barriers on PAs or NPs who work in organized delivery systems with the impact of such barriers on nonphysician professionals who work in FFS settings (Scheffler, 1995). Federal and state practice barriers may have fewer adverse effects on nonphysician practitioners in organized delivery systems, because these systems are less dependent on FFS revenues and may have more flexible work rules or collegial relationships that enhance the effectiveness of all practitioners. For example, recent case study data suggest that health professionals in some organized care settings are able to work around state legal barriers affecting prescriptive authority (Physician Payment Review Commission, 1994).
Quality of Care
As noted above, a significant body of research shows that the quality of care provided by NPs and PAs appears to be comparable to that provided by physicians in terms of clinical outcomes and is often superior in terms of patient satisfaction and process methods. However, there remains a paucity of recent, methodologically rigorous studies comparing the quality of care provided by nonphysician clinicians and physicians. Furthermore, most of the current literature on quality of care is based on research conducted in traditional FFS environments or hospitals rather than managed care environments (Scheffler, 1995; U.S. Congress, Office of Technology Assessment, 1986).
In addition to problems with nonrandom assignment and the possible confounding effects of gender, the following methodological issues should be addressed by future research comparing the quality of care provided by physician and nonphysician clinicians:
- Adequate sample size of patients and clinicians, with use of power analysis to determine sample size and use of statistical significance testing.
- Use of a representative sample of settings and clinicians, not just academic medical center-related sites and providers.
- Allowance for the time factor: if nonphysician clinicians spend twice as much time with patients, for example, it is likely that the patients will report greater satisfaction or improved outcomes.
- Calculation of the percentage of a population of patients for whom nonphysician clinicians seek physician consultation over time, not simply the percentage of visits for which such consultation is requested.
Conclusions
As this paper has shown, the AMC world will demand much more cooperation between physicians and other health professionals, beginning with the teaching of team skills, as well as research into the new methods of professional collaboration. The health care workforce in the BMC world emphasized the physician and promoted specialists over primary care physicians; the AMC world emphasizes efficiency and economy, and it is much more likely to reward delivery organizations that substitute primary care physicians for specialists and NPs, PAs, and other health professionals for physicians. This paper has outlined a variety of studies that indicate the potential for the large-scale substitution of NPs and PAs for physicians.
The AMC world could turn into a zero sum game that pits physicians and other health professionals against one another (Rodgers, 1994; Scherer, 1994), particularly given the absence of a tradition and an educational system that emphasizes collaborative team provision of medical care and the development of professional complements. PAs and NPs were initially accepted by physicians and health policymakers in the 1960s and 1970s, when there was a perceived shortage of physicians. However, we may now have a surplus of physicians, particularly in a number of specialties (Schroeder, 1994a,b). If expanded use of NPs and PAs results in lower incomes for physicians, physician resistance to NPs and PAs may intensify.23 Under these circumstances, some physicians may campaign for additional restrictions on PAs' and NPs' practices, just as they have campaigned for ''any-willing-provider" laws in response to selective contracting by managed care organizations (Caldwell, 1995). On the other hand, with appropriate economic incentives and reorganized methods of delivering health care, the world that evolves after managed care could produce a more cooperative
health care team delivery model. This paper has outlined one way of thinking about the development of such a team concept, a team production of health model, as a stimulus that can be used to consider the potential benefits available from a synergistic approach. Studies of economic incentive systems and organizational frameworks that promote teamwork, balanced health production inputs, and optimal participation could produce great returns.
The AMC world is still evolving and promises to change quite rapidly over the next two decades. This means that workforce research itself may require a new model: The change may be so rapid that researchers will have to become part of the health production and management teams that they have elected to study. Although this requires researchers to take on a new role, they must maintain their neutrality.
Some of the more important topics for a new health workforce research agenda are identified below:
- What federal and state policies will promote an effective market response to the team provision of primary care?
- How will the team delivery of primary care affect funding for and training of health professionals?
- How do micro workforce policies (team composition) and macro workforce policies (training and funding) interrelate?
- What is the potential for development of new models for health care teams in primary care?
- How will the composition of a team vary by patient demographics, culture, and case mix severity?
- What types of payment and incentive programs can be designed and tested to promote the team delivery of primary care?
- What are appropriate measures of productivity and performance for the health care team?
- To what extent do federal and state laws and regulations impede the evolution of innovative health care teams?
- How does the health care team relate to organizational form (staff and group HMOs, IPA, FFS, preferred provider organizations) and the market for health care services?
- What data and information should we collect and disseminate in order to monitor performance and to promote effective decisionmaking?
Acknowledgments
This paper was supported in part by the Bureau of Health Professions. Valuable guidance was provided by Neal A. Vanselow, Karl D. Yordy, and Molla S. Donaldson of the IOM, as well as Fitzhugh Mullan, Robert M. Politzer, and Edward Sekscenski of the Bureau of Health Professions. In addition, Linda
Aiken, Joel Alpert, Jean Johnson, Eugene Jones, David A. Kindig, Kathleen N. Lohr, Thomas G. Rundall, and Eugene S. Schneller provided helpful comments on an earlier draft of the paper.
Special thanks to John M. Hillman (Agency for Health Care Policy and Research predoctoral fellow) and Susan Ivey (National Institute for Mental Health postdoctoral fellow) for their assistance in revising the paper and significantly improving its value. Finally, I appreciate the conceptual contributions of Stephen E. Foreman and Norman S. Waitzman.
References
Abbott, A. 1988. The System of Professions: An Essay on the Division of Expert Labor. Chicago: University of Chicago Press.
Aiken, L.H., Gwyther, M.E., and Whelan, E. 1994. Advanced Practice Nursing Education: Strategies for the Allocation of the Proposed Graduate Nursing Education Account. Philadelphia: Center for Health Services and Policy Research.
American Medical Association. 1994. Physician Characteristics and Distribution in the U.S. G. Roback et al., eds. Chicago: American Medical Association.
Baldwin, D. 1994. The Role of Interdisciplinary Education and Teamwork in Primary Care and Health Care Reform. Rockville, MD: Bureau of Health Professions, U.S. Department of Health and Human Services.
Begun, J., and Lippincott, R.C. 1993. Strategic Adaptation in the Health Professions. San Francisco: Jossey-Bass.
Birkholz, G. 1995. Malpractice Data from the National Practitioner Data Bank. Nurse Practitioner 20(3):32–35.
Birkholz, G., and Walker, D. 1994. Strategies for State Statutory Language Changes Granting Fully Independent Nurse Practitioner Practice. Nurse Practitioner 19(1):54–58.
Blum, H.L. 1983. Expanding Health Care Horizons (Second Edition). Oakland, Calif.: Third Party Publishing.
Brown, S.A., and Grimes, D. 1993. Nurse Practitioners and Certified Nurse-Midwives: A Meta-Analysis of Studies on Nurses in Primary Care Roles. Washington, DC: American Nurses Publishing.
Buchanan, J.L., Bell, R.M., Arnold, S.B., et al. 1990. Assessing the Cost Effects of Nursing Home-Based Geriatric Nurse Practitioners. Health Care Financing Review 11(3):67–78.
Bureau of Health Professions, U.S. Department of Health and Human Services. 1994. Physician Assistants in the Health Workforce: Final Report of the Advisory Group on Physician Assistants and the Workforce. Washington, DC: U.S. Department of Health and Human Services.
Burl, J.B., and Bonner, A. 1991. A Geriatric NP/Physician Team in a Long-Term Care Setting. HMO Practice 5(4):139–142.
Burl, J.B., Bonner, A., and Rao, M. 1994. Demonstration of the Cost-Effectiveness of a Nurse Practitioner/Physician Team in Long-Term Care Facilities. HMO Practice 8(4):157–161.
Caldwell, B. 1995. Managed Care Stumbles Under Weight of State Laws. Employee Benefit Plan Review 49(8):28–30.
Carzoli, R.P., Martinez-Cruz, M., Cuevas, L.L., Murphy, S., and Chiu, T. 1994. Comparison of Neonatal Nurse Practitioners, Physician Assistants, and Residents in the Neonatal Intensive Care Unit. Archives Pediatric and Adolescent Medicine 148(12):1271–1276.
Cawley, J.F. 1993. Physician Assistants in the Health Care Workforce. In The Roles of Physician Assistants and Nurse Practitioners in Primary Care. D.K. Clawson and M. Osterweis, eds. Washington, DC, Association of Academic Health Centers.
Chiarella, E.M. 1993. Nurses' Liability in Doctor-Nurse Relationships. Contemporary Nurse 2(1):6–10.
Cintron, G., Bigas, C., Linares, E., Aranda, J.M., and Hernandez, E. 1983. Nurse Practitioner Role in a Chronic Congestive Heart Failure Clinic: In-Hospital Time, Costs, and Patient Satisfaction. Heart and Lung 12(3):237–240.
Davis, K., and Rowland, D. 1991. Financing Health Care for the Poor. In Health Services Research: Key to Health Policy. E. Ginzberg, ed. Cambridge, Mass.: Harvard University Press.
Delbanco, T.L., Meyers, K.C., and Segal, E.A. 1979. Paying the Physician's Fee: Blue Shield and the Reasonable Charge. The New England Journal of Medicine 301(24):1314–1320.
Dranove, D., and White, W.D. 1987. Agency Theory: New Insights Into the Health Care Industry. Inquiry 24(4):405–415.
Enthoven, A. 1987. The Health Care Economy in the U.S.A. In Health Economics: Prospects for the Future. G.T. Smith, ed. Kent, England: Croom Helm Ltd.
Epstein, A. 1995. Performance Reports on Quality: Prototypes, Problems, and Prospects. The New England Journal of Medicine 333(1):57–61.
Fein, R. 1967. The Doctor Shortage: An Economic Diagnosis. Washington, DC: Brookings Institution.
Gamliel, S., Politzer, R.M., Rivo, M.L., and Mullan, F. 1995. Managed Care on the March: Will Physicians Meet the Challenge? Health Affairs 14(2):131–142.
Giacomini, M., Luft, H.S., and Robinson, J.C. 1995. Risk Adjusting Community Rated Health Plan Premiums: A Survey of Risk Assessment Literature and Policy Applications. Annual Review of Public Health 16:401–430.
Ginzberg, E. 1978. Health Manpower and Health Policy. Montclair, NJ: Allanheld Osmun.
Ginzberg, E., and Ostow, M., eds. 1984. The Coming Physician Surplus: In Search of a Policy. Totowa, NJ: Rowman and Allanheld.
Gold, M., Nelson, L., Lake, T., Hurley, R., and Berenson, R. 1995. Behind the Curve: A Critical Assessment of How Little Is Known About Arrangements Between Managed Care Plans and Physicians. Medical Care Research and Review 52(3):307–341.
Gravely, E.A., and Littlefield, J.H. 1992. A Cost-Effectiveness Analysis of Three Staffing Models for the Delivery of Low-Risk Prenatal Care. American Journal of Public Health 82(2):180–184.
Hartz, L.E. 1995. Quality of Care by Nurse Practitioners Delivering Colposcopy Services. Journal of the American Academy of Nurse Practitioners 7(1):23–27.
Health Resources Administration. 1981a. Report of the Graduate Medical Education National Advisory Committee to the Secretary, Department of Health and Human Services, September 1980. Volume 1, GMENAC Summary Report. Hyattsville, Md.: Health Resources Administration, U.S. Department of Health and Human Services.
Health Resources Administration. 1981b. Nonphysician Health Care Providers Technical Panel Report. Volume 6, GMENAC Summary Report. Hyattsville, Md.: Health Resources Administration, U.S. Department of Health and Human Services.
Henderson, T., and Chovan, T. 1994. Removing Practice Barriers of Nonphysician Providers: Efforts by States to Improve Access to Primary Care. Washington, DC: Intergovernmental Health Policy Project, The George Washington University.
Hooker, R.S. 1993. The Role of the Physician Assistants and Nurse Practitioners in a Managed Care Organization. In The Role of Physician Assistants and Nurse Practitioners in Primary Care. D.K. Clawson and M. Osterweis, eds. Washington, DC: Association of Academic Health Centers.
InterStudy, Inc. 1995. The InterStudy Competitive Edge 5.1. Saint Paul, Minn.: InterStudy Publications.
Institute of Medicine. 1994. Definition of Primary Care: An Interim Report. M. Donaldson, K. Yordy, and N. Vanselow, eds. Washington, DC: National Academy Press.
Jones, P.E., and Cawley, J.F. 1994. Physician Assistants and Health System Reform: Clinical Capabilities, Practice Activities and Potential Roles. Journal of the American Medical Association 271(16):1266–1272.
Kindig, D.A. 1993. What Does the Literature Tell Us About the Potential and Feasible Substitution of Non-Physician Providers for Physicians? A Policy Perspective. Princeton, NJ: The Robert Wood Johnson Foundation.
Knickman, J.R., Lipkin, M., Finkler, S.A., Thompson, W.G., and Kiel, J. 1992. The Potential for Using Non-Physicians to Compensate for the Reduced Availability of Residents. Academic Medicine 67(7):429–438.
Kohler, P.O. 1994. Specialists/Primary Care Professionals: Striking a Balance. Inquiry 31(3):289–295.
Lurie, N., Moscovice, I.S., Finch, M., Christianson, J.B., and Popkin, M.K. 1992. Does Capitation Affect the Health of the Chronically Mentally Ill? Journal of the American Medical Association 267(24):3300–3304.
Marder, W.D., Gaumer, G.L., and Minkovitz, C.S. 1991. GMENAC Revisited: Updated Projections for Selected Specialties. Cambridge, Mass.: Abt Associates, Inc. Unpublished paper.
McNutt, D. 1981. GMENAC: Its Manpower Forecasting Framework. American Journal of Public Health 71(10):1116–1124.
Mendenhall, R.C., Repicky, P.A., and Neville, R.E. 1980. Assessing the Utilization and Productivity of Nurse Practitioners and Physician Assistants: Methodology and Findings on Productivity. Medical Care 18(6):609–623.
Morgan, W.A. 1993. Using State Board of Nursing Data to Estimate the Number of Nurse Practitioners in the United States. Nurse Practitioner 18(2):65–66, 69–70, and 73–74.
Moses, E. 1994. The Registered Nurse Population: Findings from the National Sample Survey of Registered Nurses, 1992. Washington, DC: U.S. Government Printing Office.
Pauly, M.V. 1970. Efficiency, Incentives and Reimbursement for Health Care. Inquiry 7(1):114–131.
Pauly, M.V. 1992. Effectiveness Research and the Impact of Financial Incentives on Outcomes. In Improving Health Policy and Management: Nine Critical Research Issues for the 1990s. S.M. Shortell and U. Reinhardt, eds. Ann Arbor, Mich.: Health Administration Press.
Pauly, M.V., Hillman, A.L., and Kerstein, J. 1990. Managing Physician Incentives in Managed Care: The Role of For-Profit Ownership. Medical Care 28(11):1013–1024.
Pearson, L. 1994. Annual Update of How Each State Stands on Legislative Issues Affecting Advanced Nursing Practice. The Nurse Practitioner 19(1):11–53.
Physician Payment Review Commission. 1993. Reforming Graduate Medical Education (Chapter 4). In Annual Report to Congress, 1993. Washington, DC: Physician Payment Review Commission.
Physician Payment Review Commission. 1994. Nonphysician Practitioners (Chapter 14). In Annual Report to Congress, 1994. Washington, DC: Physician Payment Review Commission.
Physician Payment Review Commission. 1995. Provider-Driven Integration (Chapter 11). In Annual Report to Congress, 1995. Washington, DC: Physician Payment Review Commission.
Record, J., McCally, M., Schweitzer, S., Blomquist, R., and Berger, B. 1980. New Health Professionals After a Decade and a Half: Delegation, Productivity, and Costs in Primary Care. Journal of Health, Politics, Policy and Law 5(3):470–497.
Reinhardt, U.1975. Physician Productivity and the Demand for Health Manpower. Cambridge, Mass.: Ballinger Publishing Company.
Reinhardt, U. 1991. Health Manpower Forecasting: The Case of Physician Supply. In Health Services Research: Key to Health Policy. Cambridge, Mass.: Harvard University Press.
Report Card Project. 1995. Key Findings and Lessons Learned: 21 Plans' Performance Profiles. Washington, DC: National Committee for Quality Assurance.
Robinson, J.C. 1993. Payment Mechanisms, Nonprice Incentives, and Organizational Innovation in Health Care. Inquiry 30:328–333.
Rodgers, C. 1994. Nonphysician Providers and Limited License Practitioners: Scope of Practice Issues. Bulletin of the American College of Surgeons 79(2):12–17.
Rodwin, M.A.1993. Medicine, Money, and Morals: Physicians' Conflicts of Interest. New York: Oxford University Press.
Roe, B.1981. Sounding Board. The UCR Boondoggle: A Death Knell for Private Practice? The New England Journal of Medicine 305(1):41–45.
Ross, F.M., Bower, P.J., and Sibbald, B.S. 1994. Practice Nurses: Characteristics, Workload and Training Needs. British Journal of General Practice 44(378):15–18.
Safran, D.G., Tarlov, A.R., and Rogers, W.H. 1994. Primary Care Performance in Fee-for-Service and Prepaid Health Care Systems: Results from the Medical Outcomes Study. Journal of the American Medical Association 271(20):1579–1586.
Safriet, B. 1992. Health Care Dollars and Regulatory Sense: The Role of Advanced Practice Nursing. The Yale Journal of Regulation 9(2):149–220.
Safriet, B. 1994. Impediments to Progress in Health Care Workforce Policy: License and Practice Laws. Inquiry 31(3):310–317.
Salkever, D.S., Skinner, E., Steinwachs, D.M., and Katz, H. 1982. Episode-Based Efficiency Comparisons for Physicians and Nurse Practitioners. Medical Care 20(2):143–153.
Scheffler, R.M.1979. The Productivity of New Health Practitioners: Physician Assistants and MEDEX. Research in Health Economics 1:37–56.
Scheffler, R.M. 1995. Report on Selected Nonphysician Practitioners in Primary Care: Physician Assistants, Nurse Practitioners, and Certified Nurse Midwives. Unpublished background paper prepared for the Institute of Medicine.
Scheffler, R.M., Weisfeld, N., Ruby, G., and Estes, E.H. 1978. A Manpower Policy for Primary Health Care. The New England Journal of Medicine 298(19):1058–1062.
Scherer, J.L. 1994. Union Uprising: California Nurses React Aggressively to Work Redesign. Hospital and Health Service Networks 68(24):36–37.
Schneider, D.P., and Foley, W.J. 1977. A Systems Analysis of the Impact of Physician Extenders on Medical Cost and Manpower Requirements Medical Care 15(4):277–297.
Schneller, E.S., and Ott, J.B. 1996. Contemporary Views of Change in the Health Professions. Hospital and Health Services Administration . In press.
Schroeder, S.A. 1994a. The Latest Forecast. Managed Care Collides with Physician Supply. Journal of the American Medical Association 272(3):239–240.
Schroeder, S.A. 1994b. Managing the U.S. Health Care Workforce: Creating Policy Amidst Uncertainty. Inquiry 28:266–275.
Schwartz, W.B., Sloan, F.A., and Mendelson, D.N. 1988. Why There Will Be Little or No Physician Surplus Between Now and the Year 2000. The New England Journal of Medicine 318(14):892–897.
Schwartz, W.B., and Mendelson, D.N. 1990. No Evidence of an Emerging Physician Surplus: An Analysis of Change in Physicians' Work Load and Income. Journal of the American Medical Association 263(4):557–560.
Sekscenski, E., Sansom, S., Bazell, C., Salmon, M., and Mullan, F. 1994. State Practice Environments and the Supply of Physician Assistants, Nurse Practitioners, and Certified Nurse-Midwives. The New England Journal of Medicine 331(19):1266–1271.
Shortell, S.M., Gillies, R.R., and Anderson, D.A. 1994. New World of Managed Care: Creating Organized Delivery Systems. Health Affairs 13(5):46–64.
Shortell, S.M., and Hull, K.E. 1996. The New Organization of the Health Care Delivery System: In Strategic Choices for a Changing Health Care System. S.H. ALtman and U.E. Reinhardt, eds. Chicago: Health Administration Press.
Spisso, J., O'Callaghan, C., McKennan, M., and Holcroft, J.W. 1990. Improved Quality of Care and Reduction of Housestaff Workload Using Trauma Nurse Practitioners. Journal of Trauma 30(6):660–665.
Steinwachs, D.M. 1992. Redesign of Delivery Systems to Enhance Productivity. In Improving Health Policy and Management: Nine Critical Research Issues for the 1990s. S.M. Shortell and U. Reinhardt, eds. Ann Arbor, Mich.: Health Administration Press.
Steinwachs, D.M., Weiner, J.P., Shapiro, S., Batalden, P., Coltin, K., and Wasserman, F. 1986. A Comparison of the Requirements for Primary Care Physicians in HMOs with Projections Made by the GMENAC. The New England Journal of Medicine 314(4):217–222.
Tirado, N.C., Guzman, M., and Burgos, F. 1990. Workload Contribution of a Physician Assistant in an Ambulatory Care Setting. Puerto Rico Health Sciences Journal 9(2):165–167.
U.S. Bureau of the Census. 1994. Statistical Abstract of the United States: 1994 (114th edition.) Washington, DC: U.S. Government Printing Office.
U.S. Congress, Office of Technology Assessment. 1986. Nurse Practitioners, Physician Assistants and Certified Nurse Midwives: A Policy Analysis, Health Technology Case Study. Washington, DC: U.S. Government Printing Office.
U.S. General Accounting Office. 1994a. Health Care Reform: "Report Cards" Are Useful But Significant Issues Need to Be Addressed. Gaithersburg, Md.: U.S. General Accounting Office.
U.S. General Accounting Office. 1994b. Health Care: Employers Urge Hospitals to Battle Costs Using Performance Data Systems. Gaithersburg, Md.: U.S. General Accounting Office.
Washington Consulting Group. 1994. Survey of Certified Nurse Practitioners and Clinical Nurse Specialists: December 1992 Final Report to the Bureau of Health Professions, Washington, DC: U.S. Government Printing Office.
Weiner, J.P. 1993. The Demand for Physician Services in a Changing Health Care System: A Synthesis. Medical Care Review 50(4):411–449.
Weiner, J.P. 1994. Forecasting the Effects of Health Reform on U.S. Physician Workforce Requirement: Evidence from HMO Staffing Patterns. Journal of the American Medical Association 272(3):222–230.
Weiner, J.P., Steinwachs, D.M., and Williamson, J.W. 1986. Nurse Practitioner and Physician Assistant Practices in Three HMOs: Implications for Future U.S. Health Manpower Needs. American Journal of Public Health 76(5):507–511.
Winslow, R. 1995. Major Purchasers of Health Services Form Alliance to Evaluate HMO Care. Wall Street Journal, July 3.