5
Primary HIV-Prevention Strategies
Over the past 10 years, African governments—through national AIDS control programs—international development agencies, private voluntary organizations, and other nongovernmental groups across Africa have devoted resources, time, and energy to developing low-cost interventions to arrest the spread of HIV and AIDS. Many different programs have distributed AIDS leaflets, badges, stickers, and other paraphernalia. Messages informing people about the danger of AIDS are regularly broadcast on radio and television, published in newspapers, displayed on billboards, and performed by local entertainers. Hundreds of peer educators across the continent visit local bars, beer gardens, hotels, STD clinics, and work sites to provide AIDS-prevention education and distribute free condoms. Millions of other condoms are being made available at very low cost through social marketing programs. 1 At the start of the epidemic, when many of these interventions were first conceived, the hope was that they would induce a sufficiently large behavior response to contain the epidemic.
How successful have these efforts been at preventing new cases of HIV infection? Despite the many limitations inherent in attempting to evaluate the effectiveness of interventions aimed at HIV prevention, clear evidence is emerging that such efforts can be successful, particularly among higher-risk groups
(World Health Organization, 1992c; Coates, 1993; Lamptey et al., 1993; Choi and Coates, 1994; Stryker et al., 1995). At the same time, however, data from various surveillance systems indicate that current interventions are probably not yet having a significant impact on the epidemic at the continent or even the country level (Lamptey et al., 1993; see also Chapter 3). Despite the fact that levels of AIDS awareness are extremely high across the continent (see Chapter 4), getting people to change their behavior is difficult. Denial, fear, external pressures, other priorities, or simple economics can sometimes keep people from adopting healthier life-styles.
There are many reasons why prevention efforts in Africa have not had as large an impact on the spread of the epidemic as desired. AIDS has struck the continent at a time when it is undergoing its worst financial crisis since independence. In some countries, other catastrophes—such as wars, droughts, or famines—have been more immediate and taken precedence over AIDS-prevention efforts. Throughout the continent, the overall magnitude of the response has been inadequate, and expectations about what could be achieved quickly have been unrealistic. A lack of indigenous management capacity and chronic weaknesses in the public health system have hindered the development and implementation of AIDS control programs. Individuals and organizations working against the spread of AIDS have had to face discrimination, complacency, and even persistent denial in the community. Many AIDS workers have become exhausted after struggling for so long against impossible odds; many others have died (Mann et al., 1992). Myths surrounding modes of transmission hinder the dissemination of correct knowledge and sustained behavior change (see, for example, Krynen, 1994; Nature, 1993; Ndyetabura and Paalman, 1994; Ankomah, 1994).
But getting people to change their behavior is not impossible. Indeed, health educators in Africa have had a fair amount of success in the recent past. For example, broad-based education campaigns have persuaded large numbers of people to have their children immunized against various childhood diseases and educated mothers to give their children oral rehydration formula during episodes of diarrhea. Of course, attempting to modify more personal behavior, such as sexual practices, is more challenging. Yet, family planning programs have been successful even in some of the most disadvantaged countries of the world (see, for example, Cleland et al., 1994). Even the most cautious reviews of behavioral interventions aimed at slowing the spread of HIV conclude that although most have not been rigorously evaluated, some approaches do seem to work (e.g., Oakley et al., 1995). It is important to have realistic expectations about what can and cannot be achieved. Behavior change will never be 100 percent effective: some individuals will never choose to protect themselves, while others will relapse into old patterns of behavior after just a short period of time (Cates and Hinman, 1992; Lamptey et al., 1993).
To increase the likelihood of success, interventions need to be culturally
appropriate and locally relevant, reflecting cognizance of the social context within which they are embedded (see Chapter 2). They should be designed with a clear idea of the target population and the types of behaviors to be changed. In turn, impediments in the social environment to behavior change probably need to be removed or weakened (Turner et al., 1989). Therefore, behavior-change interventions should include promotion of lower-risk behavior, assistance in risk-reduction skills development, and promotion of changes in societal norms (Lamptey, 1994). In Africa, as elsewhere, HIV-prevention messages have included promotion of partner reduction, postponing of sexual debut, alternatives to risky sex, mutually faithful monogamy, consistent and proper use of condoms, better recognition of STD symptoms, and more effective health-seeking behavior.
The purpose of the discussion in this chapter is to delineate opportunities for effecting beneficial behavior changes and to discuss how these opportunities might be realized. The discussion is based on an examination of interventions to achieve behavior change, an effort that has led to the development of a set of basic principles for successful strategies and programs. The remainder of this chapter is organized as follows. First we examine principles and issues in the design and evaluation of behavior-change intervention programs. We then examine the issues that challenge the design of effective interventions targeted to African men, women, and youth, respectively, and highlight strategies that have been implemented to address these issues. Each discussion is followed by an illustrative case study. Lessons learned from these programs are then highlighted. Next follows a discussion of strategies to prevent perinatal HIV transmission. The chapter ends with a set of recommendations for prevention research, which are made in light of the experiences of strategies and programs implemented in Africa to date.
BEHAVIOR-CHANGE INTERVENTION PROGRAM DESIGN AND EVALUATION
The rapid spread of HIV in sub-Saharan Africa since the early 1980s is a result of a multiplicity of factors, many of which have been discussed in previous chapters. Table 5-1 summarizes much of this information. As the table shows, it is analytically convenient to distinguish among four types of factors: (1) individual-level factors (i.e., ones the individual has some control over changing), (2) societal factors that may serve to encourage or discourage high-risk behavior, (3) health infrastructural factors that directly or indirectly facilitate the spread of HIV, and (4) structural factors related to development issues over which the individual has very little control. As the last column in Table 5-1 shows, each of these sets of factors requires a different length of time to bring about positive change.
A basic comprehensive HIV-prevention program should aim to address the
TABLE 5-1 Factors Contributing to Sexual Transmission of HIV in sub-Saharan Africa
|
Level |
Definition |
Examples |
Changes Required |
Comments |
|
Individual |
Factors that directly affect the individual and that the individual has some control in changing |
Biological: • History and/or presence of STDs; • Lack of male circumcision; • Anal intercourse; • Sex during menses; • Traumatic sex; • Cervical ectopy |
• Prevention/treatment of STDs; • Avoidance of sex during menses; • Prevention of traumatic sex |
Achievable in the short term |
|
|
|
Behavioral: • Frequent change of sex partners; • Multiple sex partners; • Unprotected sexual intercourse; • Sex with a commercial sex worker; • Sex with an infected partner; • Lack of knowledge of STDs/HIV; • Low risk perception |
• Abstinence; • Mutual fidelity; • Consistent condom use; • Knowledge and skills of STD/HIV prevention |
Achievable in the short term |
|
Societal |
Factors related to societal norms that encourage high-risk sexual behavior |
• High rates of prostitution; • Multiple partners by men; • Gender discrimination; • Poor attitudes toward condom use; • Social status of women; • Extended postpartum abstinence |
• Improvement in status of women; • Job opportunities for women; • Promotion of mutual fidelity; • Changes in societal attitudes toward condom use |
Achievable in the short to medium term |
|
Infrastructural |
Factors that directly or indirectly facilitate the spread of HIV, over which the individual has very little control |
• Poor availability of condoms; • Poor STD services; • High prevalence of STDs; • Poor communication services |
• Changes in health infrastructure; • Improvement in STD care, behavior-change communication, and condom provision |
Achievable in the short to medium term |
|
Structural |
Factors related to developmental issues, over which both the individual and the health system have very little control |
• Underdevelopment; • Poverty; • Rural/urban migration; • Civil unrest; • Low literacy rates for women; • Laws/policies, including lack of human rights; • Unemployment |
• General economic development programs; • Enactment of appropriate laws/policies; • Income-generating opportunities; • Improvement in education of women |
Feasible in the long term |
four types of factors cited above as contributing to the spread of HIV, particularly those related to health. Steps in a comprehensive strategy include epidemiological and behavioral formative research to help design programs; implementation of behavioral interventions to facilitate individual, group, and societal behavior change; condom provision; structural/environmental strategies that support individual, group, and societal change; and program evaluation to assess success in program implementation, intermediate outcomes, and ultimate impact. In addition, evidence that STDs may facilitate HIV transmission and the interconnectedness of STD and HIV transmission modalities and prevention (see Chapter 3) strongly suggest an important role for STD treatment, control, and prevention in AIDS prevention (Laga et al., 1991; Grosskurth et al., 1995).
Guiding Principles for Behavior-Change Interventions
Interventions designed to modify people's behavior need to be based on sound principles of behavior change. Many behavioral theories are described in the literature and have been applied to understanding HIV risk behavior.2 However, no single theory sufficiently explains individual behavior changes or provides all the essential tools to change behavior (Coates, 1993). As a result, current thinking calls for a complementary combination of theoretical approaches that incorporates the key principles of behavior change into program design.
Seven guiding principles for effective behavior change interventions targeted at HIV/AIDS prevention have evolved. These principles, which are consistent with the behavior science literature and with experience in program development in Africa (Family Health International/AIDSCAP Project, 1995), are as follows:
-
Targeting—Interventions should focus on well-characterized, specific target audiences.
-
Skills development—Interventions should include components that encourage individual acquisition of skills and tools that will help to prevent the transmission of HIV.
-
Support—A supportive social environment needs to be created to foster HIV-prevention interventions and reinforce individual behavior-change efforts.
-
Maintenance—HIV-prevention interventions need to include strategies that will foster the maintenance of behavior change over time.
-
Collaboration—Every effort should be made in the development and delivery
-
of prevention interventions to work collaboratively with other sectors, ministries, and communities so that the potential for synergistic program effects is enhanced.
-
Monitoring and evaluation—Programs must be monitored and evaluated in order to determine intervention implementation integrity, effectiveness, and cost-effectiveness.
-
Sustainability—Because resources are limited and donor support is intermittent, HIV-prevention programs should be designed for sustainability by building capacity to pursue alternative resources.
Evaluation is discussed in detail in the next section. Here we comment further only on the principles of sustainability and of targeting.
For HIV/AIDS-prevention programs to be effective and sustainable, it is critical to build local capacity in both the public and the private sectors. The chronic shortages of human and fiscal resources in most of sub-Saharan Africa often make program design, implementation, and management difficult. Major deficiencies include poor infrastructure and paucity of management and technical skills in both research and intervention programs (see also Chapter 7). Special efforts should be made to improve the technical, organizational, management, and financial skills of individuals, as well as to strengthen institutional infrastructure.
With regard to targeting and audience segmentation in HIV intervention programs, the primary objective is to obtain effective and rapid results by intervening with groups that are at the greatest risk of acquiring and spreading HIV infection (Lamptey and Potts, 1990). Although it would be highly desirable to design prevention programs that are based on a good understanding of the target population and the sociocultural, environmental, and structural context, few prevention programs are based on preliminary, or formative, research findings.
As noted earlier, the groups most commonly targeted are those traditionally seen as at particularly high risk, such as truckers, uniformed service workers, commercial sex workers, or STD patients. Targeting can also extend to other at-risk populations, including out-of-school youth, school children, university students, male and female factory workers, women in the general population, and men away from home. The target audience may be defined by (1) epidemiological risk factors (e.g., HIV prevalence among commercial sex workers); (2) behavioral risk factors (e.g., clients of commercial sex workers); (3) occupation (e.g., factory workers); (4) geographic location (e.g., urban adults); (5) access points (e.g., truck stops); (6) demographics (e.g., gender, age); or (7) relevant sociocultural factors (e.g., widows, street children). In later sections of this chapter, interventions targeted principally to men, to women, and to youth are discussed; although restricting our consideration to these particular groups, we recognize that all interventions should include some attention to the sexual partners of the target group.
INTERVENTION EVALUATION
Just as the stages of an intervention program can be described as design, implementation, and outcome, so can evaluation accompany or follow each of these stages to determine how successfully the program has met its stated objectives. The corresponding stages or types of evaluation are formative, process, and outcome (Coyle et al., 1991).
Formative evaluation of the design of an intervention addresses the question of whether the proposed intervention has the potential to achieve its goals. It considers structural factors that may affect the program. For example, are policies in place to facilitate implementation of the intervention strategies (e.g., a policy requiring sex education in the schools that includes HIV/AIDS prevention)? Formative evaluation also assesses the content, nature, and design of the proposed intervention strategies in terms of success potential. For example, are they skills-based? Are they derived from preliminary, formative research? Do they match the target audience's needs? Are they built on the characteristics of other successful programs?
Process evaluation techniques are used to monitor the program as it is being implemented. The goal is to determine how well short-term program objectives are being met. For example, are condoms being distributed? Are people tested for HIV returning to obtain their results? Is the number of patients attending STD clinics declining?
Outcome evaluation is the last and ultimately the most important stage. It addresses questions about the success of the intervention. For example, has the program succeeded in changing behavior? Has that behavior change been sustained? And finally, has that behavior change succeeded in reducing the incidence of HIV? This assessment of behavioral outcomes should be performed only when there is reason to expect that such outcomes could have occurred and can be measured (i.e., earlier formative evaluation has confirmed that the intervention was well designed, process evaluation has corroborated that the intervention is being carried out well, the observation period has been substantial, behaviors have been measured, and the sample size has been sufficiently large to detect behavioral differences). Good outcome evaluation is rarely feasible unless it is planned as an integral part of the intervention and usually is possible only in the context of studies with adequate research funding and undertaken by research institutions such as universities. Interventions evaluated in this way can serve as models for others that will not undergo as rigorous an outcome evaluation.
While the logical program evaluation sequence outlined above is time-consuming, expensive, and rigorous, following these steps can help avoid wasting scarce funds on evaluations that are limited in their ability to yield useful results and repeating or continuing intervention programs that are limited in their ability to achieve the desired goals (Oakley et al., 1995).
For Africa, as elsewhere, we have limited information on what works well
because of the difficulties in carrying out rigorous evaluations, particularly outcome evaluations (Oakley et al., 1995). While the goal of rigorous evaluation must be maintained over the longer term, there is also demand for a faster, more pragmatic approach. Insistence on pure scientific rigor may be counterproductive for HIV/AIDS-prevention interventions, where innovative methods and program designs are urgently needed, and prevention efforts must rely almost exclusively on behavior change (Coyle et al., 1991).
Examples of programs that have been implemented in sub-Saharan Africa and reported in studies are described briefly in Annex 5-1 and referred to in subsequent sections of this chapter. This is not a comprehensive listing; rather it illustrates recent interventions that have used a variety of strategies and programs in trying to effect positive changes in the behavior of targeted audiences. Many have attempted to conduct modest evaluations with the limited funds available to them. Some of these evaluations suffer from methodological weaknesses so that the results must be interpreted with caution; yet all contribute to the growing effort to evaluate programs, with the twin goals of improving continuing intervention programs and designing new programs that are more effective in achieving results and at lower cost.
Even where the ''gold standard" of an intervention that consists of a randomized trial with high-caliber formative, process, and outcome evaluation cannot be met, there are practical guidelines for program developers. First, at the formative stage, it should be recognized that programs are most likely to achieve desired outcomes when their design is based on the characteristics and principles of existing effective programs, past program experience, formative research, and sound theoretical underpinnings. Even when existing programs have not undergone a gold standard evaluation, if there is consistency and convergence in results from multiple programs in different places and/or over time and/or from multiple measures of results, synthesis and interpretation of findings can guide the design of new programs. Planners must be cautious in applying such findings, maintaining awareness of the potential for biases that can influence the results. Second, while rigorous outcome evaluations are desperately needed, not all programs should attempt to implement them. However, all programs should be required to conduct process evaluation to assess program integrity. Finally, evaluation results should be translated and synthesized into new programmatic guidelines and materials and new training activities so that programs can be improved.
A TYPOLOGY OF INTERVENTION PROGRAMS
HIV-prevention strategies can be classified according to the foundation on which they are based: (1) formal institution-based programs (e.g., at the workplace, school, or clinic); (2) community-based programs (e.g., among informal youth groups or informal women's groups); and (3) population-based programs (e.g., national media campaigns or policy development). These categories are not
mutually exclusive. For example, the same individuals may be reached at work, in special community-based initiatives, or at home through the mass media.
The following sections describe each of these program types in greater detail and illustrate them with studies included in Annex 5-1. Although, as already mentioned, most of these studies lacked the resources to carry out definitive evaluations, we summarize the investigators' reports of quantifiable impacts.
Institution-based Programs
Both institution-based and community-based programs are designed to reach individuals and small groups, with the aim of teaching and reinforcing protective behaviors. They are intended to give individuals the opportunity to acquire information, assess their own risk of HIV, interact with a provider, and obtain relevant behavioral and communication skills that can help in reducing high-risk behavior; they also generate notions of peer norms that are conducive to risk reduction (Lamptey and Coates, 1994).
Institution-based programs include interventions in the workplace (factories, prisons, commercial farms, mining communities, military bases); in schools; and in health facilities, such as STD and family planning clinics, hospitals, and HIV counseling and testing clinics (see studies [4], [5], [7], [8], [10-12], [14-16], [18], and [20-24] in Annex 5-1). Targeted groups within these institutions may not be homogeneous in terms of individual behavior or social norms, and may or may not exhibit more high-risk sexual behavior than the general population. The relative ease of access to these institutional populations renders such programs attractive and potentially cost-effective.
Several institution-based programs in Africa have demonstrated changes in risk behavior (Ngugi et al., 1988 [4]3; Loodts and Van de Perre, 1989; Kamenga et al., 1991; Allen et al., 1992b [7]; Mwizarubi et al., 1992 [12]; Williams and Ray, 1993 [20-24]; Wynendaele et al., 1995). In Rwanda, for example, the initiation of an education, STD treatment, and condom distribution program for all military recruits led to a reduction in the incidence of urethritis (Loodts and Van de Perre, 1989; World Health Organization, 1992c [11]). In Rwanda, 1,458 women attending antenatal and pediatric clinics at the Centre Hospitalier de Kigali received pre-and post-test counseling, were shown an educational video, and were given free condoms. One year later, HIV seroconversion rates had decreased significantly (from 4.1 to 1.8 per 100 person-years among women whose partners were tested and counseled) (World Health Organization, 1992c [10]). Preliminary results from other ongoing programs in Tanzania and Zimbabwe also are encouraging (Mwizarubi et al., 1992 [12]; Williams and Ray, 1993 [20-24]; World Health Organization, 1992c [14]). In Tanzania, a workplace
intervention targets truck drivers, their assistants, and their sexual partners (Mwizarubi et al., 1992 [12]). In Zimbabwe, a workplace-based intervention program targets 4,500 factory employees and their families (Williams and Ray, 1993 [20-24]). This program provides STD treatment, behavior-change intervention, and condoms. The intervention employs a combination of drama, printed materials, group talks, and interpersonal counseling by 64 peer educators.
Although evidence about the impact of counseling and testing on risk behavior is mixed (Higgins et al., 1991), a few evaluations conducted to date in developing countries suggest that such efforts may be effective, at least in the short term, in changing sexual practices under certain circumstances or among certain groups (such as couples) (Higgins et al., 1991; Kamenga et al., 1991; Allen et al., 1992a [7], 1992b [8]; Wynendaele et al., 1995 [5]). In Rwanda, for example, results of an HIV counseling and testing program demonstrated an increase in condom use (Allen et al., 1992b [8]). HIV seroconversion rates were also reported to have decreased among seronegative women whose partners were tested, but not among women whose partners were not tested. In Uganda, an evaluation of a counseling and testing intervention found significant reported decreases in risk behaviors among both seronegative and seropositive individuals (Moore et al., 1993).4
Community-based Programs
Community-based programs use group interventions to reach communities. These interventions include the use of peer educators to reach sex workers or school-aged youth, use of traditional health providers to reach rural communities, or programs targeted to other community groups (see studies [1], [6], [9], [13], [25], and [26] in Annex 5-1).
Community participation can sometimes be a critical factor for program success and sustainability (Lamptey and Coates, 1994; Population Council, 1995). According to the guiding principles described earlier, HIV/AIDS-prevention programs should be designed at the outset with attention to their acceptability within the community and target groups, the external or institutional support required to develop and sustain the skills and talent needed to make them work, and the infrastructure support and the individual and collective commitments needed to maintain them over time (Lamptey and Coates, 1994). Community involvement is often only an empty slogan in programs without any real involvement of the community in decision making.
Few intervention programs implemented to date in Africa have involved such community participation. Notable exceptions are in Uganda (Seeley et al., 1991; Katende and Bunnell, 1993), where, for example, participatory planning and evaluation workshops are being held at the district level so that district health officers, community members, and AIDS educators can participate in the joint planning and evaluation of programs (Barton, 1993).
Evidence of the success of community-based interventions, as reported by various authors, is summarized in column 5 of Annex 5-1. In Accra, Ghana, a pilot educational community-based intervention used local health workers to train and support selected prostitutes as health educators and condom distributors to their peers. Six months after the intervention had begun, reported condom use had increased dramatically (Asamoah-Adu et al., 1994). In Cross River State, Nigeria, a community-based prevention program among full-time prostitutes and their clients resulted in greater use of condoms (Williams et al., 1992 [6]). In a follow-up questionnaire administered 12 months after the baseline survey, 24 percent of prostitutes reported always using condoms with their clients/partners, as compared with 12 percent in the baseline survey. And in Zimbabwe, similar interventions resulted in a dramatic increase in the proportion of sex workers who reported consistent condom use with clients (World Health Organization, 1992c [26]).
Population-based Programs
Population-based programs, using mass media, aim to change societal norms, and provide information as well as individual behavior-change messages to large segments of the population. They may also encourage the enactment of policies to support HIV/AIDS-prevention efforts. Examples include media education programs, condom social marketing programs, and policy changes such as a regulation requiring condom use in brothels. Population-based programs may be targeted to such large segments of the population as adolescents, sexually active males, men and women with multiple partners, or all sexually active men and women (see studies [2], [3], [17], and [19] in Annex 5-1).
Undoubtedly the best known and most widely cited example of a population-based intervention is condom social marketing. For example, a program in Zaire subsidized the price of condoms, increased their distribution, and used innovative commercial marketing techniques to increase condom sales from around 10,000 in 1987 to around 18 million in 1991 (Population Services International, 1992 [17]). Not surprisingly, this model of social marketing has been quickly replicated through the continent.
INTERVENTIONS TARGETING SEXUALLY ACTIVE MEN
Sexually active men have played a critical role in the rapid spread of HIV in
sub-Saharan Africa. Despite the fact that more women than men are now infected (World Health Organization, 1994a), the risk behavior of sexually active men remains the key vector driving the continuing spread of HIV in Africa. The epidemiological parameters of HIV and HIV-related risk behaviors among men are described in Chapters 3 and 4, respectively.
Issues
Perhaps the most significant issue in HIV-prevention in Africa relates to gender inequality. Because men play the dominant role culturally, socially, and economically, they also dominate sexual relationships. Sex is often initiated and controlled by men in both marital and nonmarital relationships. Women have less power in sexual relationships and are often unable to influence sexual relations.
A second and related issue is that in many African cultures, multiple partners and extramarital sexual relationships by men are either accepted or tolerated, and the data show high frequencies of multiple partners. There is higher risk in these situations. A person in a polygynous union in which all partners are supposed to have sexual relations only within that union is at somewhat higher risk of HIV infection than a person in a couple union, simply because there are more people who could potentially fail to stay faithful to that union. However, a person in such a polygynous union is at much lower risk than a person with multiple partners who themselves have multiple partners.
A third issue is that most family planning programs have traditionally targeted women who are married and ignored the role of men. Women have therefore been responsible for initiating behavioral changes related to reproductive health; as a result, female-controlled methods account for the vast majority of contraceptives used (Robey et al., 1992). In 1990, only 0.3 percent of married women of reproductive age were using condoms in sub-Saharan Africa, as compared with 4 percent in all developing countries (Liskin et al., 1990).
A final general issue that influences male sexual risk taking is that, up until recently, condoms had have a poor reputation in Africa. They have been widely regarded as making sex less enjoyable, as well as being a poor disease-prevention method and an ineffective and unreliable contraceptive (see Chapter 4). Condoms are frequently seen as linked to promiscuity and prostitutes and often connote a violation of trust (Ngugi et al., 1988 [4]; May et al., 1990; Allen et al., 1992a [7]). It is not surprising, therefore, that up until very recently condoms have been poorly promoted by family planning providers. Furthermore, access to condoms is a significant problem, especially in rural areas of Africa. Nevertheless, African men have in the past 10 years shown marked changes in attitudes toward condom use for disease prevention. In particular, demand for condoms has grown steeply since 1988, with more than 110 million condoms being distributed in 1994 through social marketing programs alone (Figure 5-1).
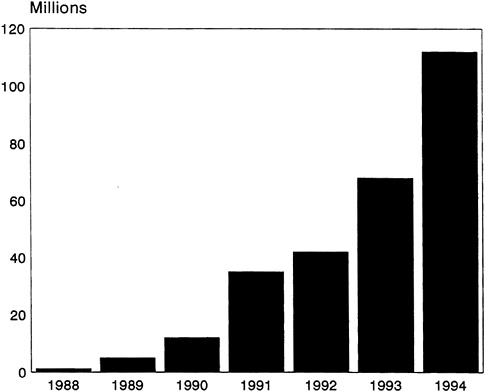
FIGURE 5-1 Population Services International (PSI) Condom Sales in Africa, 1988-1994.
SOURCE: Adapted from PSI (1994c, 1995).
Target Population
Sexually active men who are not in mutually monogamous relationships or men in polygynous relationships where each member of the relationship has no outside partners are potentially at risk of HIV infection. This risk is especially acute in countries such as Tanzania, Uganda, and Zambia, where in certain areas well over one-half of urban commercial sex workers are HIV-positive (U.S. Bureau of the Census, 1994a, 1994b; see also Figures 3-3). HIV-prevention programs in such high-prevalence countries need to reach all sexually active men and women, but special attention still needs to be focused on particular groups of men who are high-risk transmitters. These population subsets include clients of sex workers, male STD patients, men in the uniformed services, truckers or other transport workers, men away from home, prisoners, and fishermen. In some parts of Zambia, for example, the prevalence of HIV among males attending STD clinics ranges from 33 to 60 percent (U.S. Bureau of the Census, 1994b).
TABLE 5-2 Objectives of HIV-Prevention Programs Targeted to Men
|
Individual Behavior Change: • Reduce the number of sexual partners. • Reduce the frequent change of sexual partners. • Learn to recognize STD symptoms, and seek early appropriate treatment. • Accept and use condoms properly and consistently. |
|
Structural/Environmental Changes: • Render condoms available, accessible, and affordable. • Improve treatment of bacterial STDs. • Change the social acceptability of multiple partners by men. • Make STD treatment facilities accessible and affordable. • Reduce the consumption of substances (alcohol) that enhance high-risk behavior. • Promote public policies that enhance low-risk sexual behavior (e.g., condom-only brothels). |
Types of Strategies and Programs
HIV-prevention strategies for men should aim to change individual sexual behavior, improve STD treatment services, provide condoms, change societal norms, and ease structural and environmental impediments to reducing risky behavior (Table 5-2). However, most programs targeted to African men to date have focused only on behavior-change interventions and the provision of condoms. The quality of the interventions varies widely. In some programs, only information services are offered; changes in behavior are not emphasized, and condom supply and availability are intermittent. In others, genuine attempts are made to change behavior; improve STD treatment; and make condoms readily available, accessible, and affordable by the target population (Mouli, 1992 [18]; Williams and Ray, 1993 [20-24]; Laga et al., 1994 [16]).
The following case study from Zaire illustrates a population-based intervention targeted to African men in which behavior change was promoted, and condoms were made available, easily accessible, and affordable.5
Case Study
The Zaire AIDS Media and Condom Social Marketing Project was initiated in 1988 (Population Services International, 1992 [17]). The program developed specific messages targeted to youth aged 12 to 19 and young adults aged 20 to 30.
However, the major beneficiaries were an estimated 13 million sexually active adult males in urban areas, as well as youth of both sexes in rural areas. The objectives of the program were to change attitudes about HIV, to promote behavior change (i.e., increased use of condoms), and to alter social norms regarding safer sexual practices. Innovative media materials were developed based on formative research. AIDS messages were presented in television and radio spot announcements, dramas, music videos, talk shows, interviews, and contests through the country's extensive media network. Condoms were advertised and sold at traditional outlets, such as markets, pharmacies, drug stores, and health clinics, as well as nontraditional outlets, such as hotels, bars, brothels, and village kiosks. In one year, the program produced 28 feature programs about AIDS that were broadcast by radio in 13 local languages, 22 TV spots with AIDS messages, 8 radio dramas that promoted AIDS awareness and safer sexual behavior, 2 songs about AIDS, and 5 AIDS knowledge radio contests. Knowledge, attitude, and practice (KAP) survey results from one target region (Sud-Kivu) were compared with KAP survey results from a nontargeted or "control" region (Equateur). Populations in the target region showed more correct knowledge about AIDS and significantly improved attitudes about risk-taking and risk-taking practices as compared with those in the nontarget or control region. For example, there was an 18 percent difference in the level of knowledge regarding AIDS transmission between those in the target group and control regions as compared with a 2 percent difference in level of knowledge between two groups in the targeted region. The study also demonstrated that only 16 percent in the control region were able to name methods of AIDS prevention, whereas 39 percent in the targeted region knew that postponing of sexual debut, mutual monogamy, and condom use are the most effective methods of AIDS prevention.
In 1991, 18.3 million condoms were distributed through the program, as compared with only 900,000 in 1988. Three-quarters of the condom buyers reported purchasing condoms for AIDS prevention as well as for family planning. Although their estimate can be debated, the project investigators concluded that the program's 1991 condom sales prevented about 7,200 primary cases of HIV/AIDS (Population Services International, 1992 [17]). This estimate does not include a much larger number of secondary infections (infections acquired from the primary cases) prevented.
Several strengths of the Zairian program contributed to its success. First, marketing principles of price, promotion, place, and product were successfully adapted to HIV-prevention strategies and sales of condoms. Second, Zaire's extensive satellite network of TV and radio contributed to impressive national coverage of both urban and rural areas; a major drawback to most HIV-prevention programs is their limited coverage—and subsequent limited impact—as a result of regional, not national, approaches. Third, marketing of condoms through numerous nontraditional outlets greatly expanded the reach of the program and enhanced condom accessibility. A fourth strength was the use of multiple innovative
and culturally relevant marketing approaches to sell condoms and increase purchase behavior. Some of the most popular communication approaches were the use of renowned and persuasive local musicians to present key HIV-prevention messages; the use of theater through radio, television, and play presentations to confront attitudes about HIV; and the use of student notebooks to correct "AIDS myths" and present accurate HIV information to school children. Another strength of the program was partial program cost recovery due to condom sales. The income generated from condom sales was used to meet packaging and marketing costs. It also provided a profit motive for the sale of condoms through shops and bars, a key to establishing a comprehensive distribution network. Although not financially self-sustaining, the intervention was unique in that it generated resources.
Finally, this program is an example of the successful use of the private sector in AIDS prevention. African governments have been slow to admit that they alone do not have adequate human, fiscal, and institutional resources to arrest the epidemic without assistance. Participation by external donors, the commercial sector, private voluntary organizations, nongovernmental organizations, and other community-based organizations is vital to any country's AIDS control program.
Comparable levels of condom sales using mass media and social marketing have been achieved in several African countries, including Ethiopia, Cameroon, Côte d'Ivoire, Burkina Faso, and Zambia (Population Services International, 1994a). Cumulative sales of condoms—the main indicator of success in condom social marketing programs—are shown through 1994 for all of Africa in Figure 5-1 (Population Services International, 1994c, 1995).
Some weaknesses were inherent in the Zairian program. First, an STD treatment component was absent. As discussed in Chapters 2 and 3, STDs play an important role in the sexual spread of HIV in sub-Saharan Africa (Grosskurth et al., 1995). AIDS-prevention programs that exclude STD treatment will have limited impact on the epidemic. Mathematical modeling of the epidemic shows that the combination of partner reduction, STD treatment, and condom use has the greatest impact in slowing the spread of the epidemic (Sokal et al., 1991). A second weakness was inadequate evaluation of the program. Some process and outcome data, such as condom sales and pre-and post-KAP results, are available as indicators of the success of the program. However, a program of this magnitude should have included better behavioral outcome evaluation. Additional data—such as a profile of who was buying the condoms and for what reasons, the proportion of condoms actually used with the aim of preventing HIV infection, and the effect of the program on STD prevalence or incidence—would allow better measurement of the impact of the program. A third weakness of the program approach is the targeting of the general population as opposed to particular groups. Small-group interventions encourage the involvement of the community in program design and evaluation, and give individuals opportunities to interact more closely with the provider. Finally, the primary focus on safer sex
through condom use is a realistic approach for most sexually active men, but other messages—such as postponing of sexual debut, mutual monogamy, and nonpenetrative sex—should be targeted to youth and young adults.
Despite the above weaknesses, condom social marketing interventions such as this program in Zaire are effective channels for condom distribution and behavior-change communication.
Lessons Learned
The strengths and weaknesses of the Zairian condom social marketing program point to several lessons that can be applied in developing future HIV intervention programs.
First, comprehensive and integrated interventions should be developed. Programs targeted to men typically include behavior-change interventions and condom provision. STD treatment, however, is often nonexistent, as in the case of the Zairian program. Given the role of STDs as a cofactor in facilitating HIV transmission, their continuing high prevalence in several African countries underscores the need for integrating STD treatment into future intervention programs.
Second, men are not as difficult to reach with intervention programs as is often assumed. Condom social marketing programs in Africa have been very successful in reaching men at home, at work, in bars and hotels, and at truck stops (Mwizarubi et al., 1992 [12]; Population Services International, 1994a). Other programs have reached men through the workplace, health clinics, prisons, brothels, HIV testing and counseling centers, and community-based initiatives (Mouli, 1992 [18]; Mwizarubi et al., 1992 [12]; World Health Organization, 1992c [10, 11, 14, 26]; Wilson et al., 1992 [25]; Williams and Ray, 1993 [20-24]; Population Services International, 1994a, 1994b, 1994d [19]).
Third, successful programs focus on changing not only individual behavior, but also social norms and other structural and environmental factors that enhance the spread of HIV (see Chapter 2). Interpersonal channels are more important in changing attitudes and social norms concerning the adoption of new behaviors among a large audience, while mass media channels are often more effective at creating awareness and enhancing knowledge of a new idea (Lamptey and Coates, 1994). Consequently, individual and small-group interventions should be combined with general population-based programs.
A fourth lesson to emerge from this case study is that multiple and repeated messages via various media are important in changing behavior. A combination of media programs—such as mass education programs, small media (brochures, posters), interpersonal approaches (STD/HIV counseling and testing, peer education) and educational entertainment (theater, music, and folklore)—has been effective in Zimbabwe, Tanzania, and Ghana (Mwizarubi et al., 1992 [12]; Wilson
et al., 1992 [25]; Williams and Ray, 1993 [20-24]; Asamoah-Adu et al., 1994 [1]).
Finally, HIV-prevention programs in Africa desperately need good evaluation data for assessing program effectiveness and cost-effectiveness. 6 Studies showing the behavioral impact of various intervention programs are in particularly short supply.
INTERVENTIONS TARGETING SEXUALLY ACTIVE WOMEN
More than half of the estimated 11 million adults infected with HIV in sub-Saharan Africa are women (World Health Organization, 1994a, 1995). This section addresses HIV-prevention programs targeting sexually active adult women; the following section addresses programs targeting adolescents, including adolescent girls.
In a recent review article, Heise and Elias (1995) argue convincingly that current HIV/AIDS-prevention efforts are not well suited to meeting the needs of many of the world's women. Indeed, none of the three central elements of HIV/AIDS-prevention efforts in developing countries—encouraging people to reduce their number of sexual partners, promoting the widespread use of condoms, and treating concurrent STDs in populations at risk of HIV—are appropriate for women, whose vulnerability stems from their inability to protect themselves because of their lower cultural and socioeconomic status or their lack of influence in sexual relations (see also du Guerny and Sjöberg, 1993, and Ulin, 1992). For example, results from studies indicate that many infected African women have only one sexual partner (Heise and Elias, 1995). Hence, the greatest source of HIV risk for most sexually active women is their husbands or stable partners, who have multiple other sexual contacts. Heise and Elias (1995) conclude, ''Women need both a new commitment to addressing the underlying inequities that heighten their risk, and new technologies that provide them with a means of HIV protection within their personal control" (Heise and Elias, 1995:931).
Early accounts of the epidemic suggested that the disease in Africa was an urban phenomenon, confined to commercial sex workers and their clients (Van de Perre et al., 1985; Kreiss et al., 1986; Ngugi et al., 1988 [4]). This finding led to the development of intervention programs that focused only on these two groups. Such programs continue to be appropriate because of the high-risk nature of commercial sex. But at the same time, these groups cannot be the sole focus of prevention programs because recent data from antenatal clinics indicate that the prevalence of HIV/AIDS among the general population is rising. Recent data from several countries in Central and Southern Africa reveal that there has been
a dramatic rise in prevalence of HIV among both urban and rural women attending antenatal clinics (Stanecki and Way, 1994).
Research on HIV infection among women has been insufficient and poorly targeted (Faden et al., 1991; Herdt and Boxer, 1991; Hankins and Handley, 1992). When such research is undertaken, it often focuses on women's reproductive function and their role as mothers. Hankins and Handley (1992:967) emphasize the need for more epidemiological and clinical research in HIV progression among women:
Concerted effort on the part of clinicians, researchers, funding agencies, and decision-makers is required for redressing the inequities in both the gender-specific knowledge of the natural history, progression, and outcome of HIV disease and the adequacy of medical and psychosocial care for women with HIV infection. The unique features of HIV infection in women have been subject to both scientific neglect and policy void, situations that can and should be rectified with dispatch.
Some of the controversy regarding research on women stems from concerns about having women of childbearing age participate in drug trials or in intervention trials involving physical or biological agents, such as the female condom or vaginal viricides. There is no evidence that participation in such research harms women (Levine, 1991). Even if there were grounds for excluding women from research with biologically active agents, there is little justification for omitting women from social and behavioral research centered on questions that can help determine the level and nature of HIV risk and inform the development and evaluation of life-saving prevention strategies.
Among researchers, particularly in the developed world, there is growing consensus on the importance of research on disease prevention and progression among women. Reducing the spread of HIV among women is critical to slowing the epidemic. However, complex issues remain.
Issues
One issue is the way in which women have been narrowly categorized in studies. For example, although individual women typically have multiple social roles and functions, research has tended to classify them into discrete social categories, such as prostitute or mother (Caravano, 1991; Herdt and Boxer, 1991).
Rigid male-dominated sexual relations remove much of female sexual behavior, directly and indirectly, from women's own control, so that it is not subject to rational decision making. Holland et al. (1994:223) note the deleterious effects of dominant paradigms on research about women:
The official conceptions of sexuality and models of behavior … were largely based on a view of behavior as a matter of choice by free individuals. … Women's ability to choose safer sexual practices or to refuse unsafe (or any
other) sexual activity was not a question of free choice among equals, but one of negotiation within structurally unequal social relationships.
The perception of unequal roles in sexual decision making has affected the design of behavioral interventions. Across Africa, one sees reliance on a male-focused HIV-prevention strategy that includes condom programs for prostitutes and men, partner-reduction programs for men, and STD treatment programs for men (Heise and Elias, 1995). Even programs targeted to women are limited in focus, addressing solely certain roles women assume, rather than the full range of women's issues and needs (Herdt and Boxer, 1991).
As discussed earlier, few programs have focused on sexually active women in the general population, but rather target high-risk women and men. There are several reasons why such programs have had very little effect on HIV risk for most sexually active women. First, in some circumstances, a woman's exposure to HIV and STDs depends less on her own risk behavior than on the behavior of her sexual partner, over whom she has little control. Second, most women do not possess the necessary negotiating skills and power to ensure condom use. Third, women's access to STD treatment services is very limited, syndromic diagnosis of STDs by women is difficult, and clinical testing of STDs is expensive and not widely accessible.
Gender-specific research that investigates women, their experiences, and their many roles has been deemed ill-defined and impractical by many health researchers. Many researchers and policy makers are skeptical of indirect effects, indirect interventions, and the social research methods required to measure these effects. Clearly, comprehensive research strategies that combine useful information from both qualitative and quantitative research are needed to identify what works in HIV prevention for women as well as men. However, many of the approaches to preventing HIV among the general population of women upset tradition. Public discussions of women's sexual behavior appear to be more sensitive and less open than acknowledgment of men's needs and desires. Women are seen as guardians of culture, as preservers of tradition, and as agents of socialization; in these capacities, they are regarded as the inviolable moral center of many cultures.
While acknowledging that fundamental social change takes time, Heise and Elias (1995:931) argue that the HIV/AIDS epidemic has created two imperatives:
… to begin in earnest to work on changing the underlying causes of women's vulnerability and to pursue vigorously every means possible to strengthen women's immediate ability to protect themselves in the face of the economic and cultural forces currently allied against them. This, in turn, means placing greater emphasis within existing AIDS programs on empowering women and committing major resources to developing new prevention technologies—like vaginal suppositories or foams lethal to the virus—that women can use without their partner's knowledge or consent.
Target Population
Although not mutually exclusive, the following three groups should be considered when designing HIV-prevention strategies and messages targeted to women: (1) sexually active women with multiple partners, such as commercial sex workers; (2) single sexually active women; and (3) sexually active women in formal or informal unions. The vast majority of interventions targeted to women tend to focus on sex workers (who are at highest risk) while ignoring the rest of the population. Even these programs are neither as extensive nor as intensive as those in Thailand, for example, that target commercial sex workers (see, e.g., Hanenberg et al., 1994, and, Visrutaratna et al., 1995). The largest and most difficult group to work with are women in marital unions, whose desire for pregnancy and lack of control over their spouse's sexual behavior pose a challenge to the design of effective interventions.
As with men, HIV-prevention programs that target women should not be designed solely on the basis of risk behavior and epidemiological data. Programs need to address the multiple roles played by women and be cognizant of women's competing statuses and obligations. In thinking systematically about these roles, program managers as well as researchers need to consider individual, social, and environmental factors, such as location of residence, marital status, current and future desires for children, generational status, socioeconomic status, cultural expectations, and religious beliefs.
Types of Strategies and Programs
Programs targeted to women should include the basic program components provided to men—behavior-change interventions, STD treatment, and condom provision—as well as relevant structural changes. Table 5-3 shows the desired objectives of programs that target sexually active women. Some structural interventions that are unique to women include empowerment interventions, policy/legal interventions, and interventions that enhance access to nonhealth sectors.
Empowerment interventions are programs directed toward promoting women's increased skill in self-direction, often through self-organized, peer-led groups. It remains unclear whether these groups produce the anticipated benefit. We know little about how to create conditions that permit women to be empowered in Africa and what it means to be "empowered" in different settings.
Although policy changes and legislation are clearly needed to address status inequalities, women's rights may clash with clan, familial, or other roles. A fundamental issue is that even if laws and policies are changed, the impact of these changes at the local or personal level may be minimal.
Female access to education, other skills, and jobs is essential to redress status inequities. However, reduced expectations regarding schooling for females on the part of men, families, society, and women still persist. Some income-generation
TABLE 5-3 Objectives of HIV-Prevention Programs Targeted to Women
|
Individual Behavior Change: • Reduce the number of sexual partners. • Reduce the frequent change of sexual partners. • Learn to recognize STD symptoms, and seek early appropriate treatment. • Improve sexual communication and negotiating skills for safer sex. • Encourage partners to use condoms properly and consistently. |
|
Structural/Environmental Changes: • Render condoms available, accessible, and affordable. • Improve diagnosis and treatment of bacterial STDs in women. • Change the social acceptability of multiple partners by men. • Make STD treatment facilities accessible and affordable. • Reduce the consumption of substances (alcohol) that enhance high-risk behavior. • Promote public policies that enhance low-risk sexual behavior (e.g., condom-only brothels). |
|
Gender-related Objectives: • Research the multiple roles of women as related to their risk of HIV infection. • Improve the role and status of women to reduce their susceptibility to HIV. • Change cultural practices detrimental to the health and status of women. • Improve access to education. • Improve skills and economic opportunities. • Improve the involvement of women's groups in the design and implementation of interventions. |
programs for women have been successfully attempted (Delehanty, 1993; Leonard, 1994).
Finally, because HIV transmission to women occurs in the context of a dyadic relationship between a man and a woman, strategies that influence this relationship are needed. Interventions targeting women have attempted to include men, but these attempts have been complicated and problematic. Further research will be needed to understand how to facilitate productive and effective intervention strategies that involve both men and women. This research will need to explore the role of the relationship between men and women and its impact on HIV-prevention strategies at the individual, group (e.g., family or kinship), and societal levels. Much of the prevention research issues for women remain largely unexamined. As mentioned earlier, current efforts to reduce HIV transmission among women in Africa have focused on interventions targeted to commercial sex workers. The first case study below describes such an intervention; it is followed by discussion of an innovative empowerment program targeting women in Botswana.
Case Study: An Intervention Targeted to Commercial Sex Workers
In 1988, Projet SIDA7 initiated a research study at the Matonge Women's Health Center in Kinshasa, Zaire (Laga et al., 1994 [16]). The objectives of the project, known as the Women's Health Project, were (1) to determine the prevalence and incidence of STDs, including HIV, among female sex workers in Kinshasa; (2) to study the interactions between STDs and HIV; and (3) to determine the impact of condom promotion and STD detection and treatment on the incidence of HIV and STDs.
A cohort of 531 initially HIV-negative female sex workers was followed for 3 years. The participants were surveyed to determine sexual behavior and practices, health-seeking and preventive-health behavior, and history of STDs over a 2-year period. Participants were screened every month for the presence of syphilis, gonorrhea, chlamydia infection, trichomoniasis, chancroid, and candidiasis and every 3 months for HIV-1; all STDs were treated free of charge. Individual and group counseling was provided to promote condom use, and free condoms were distributed during counseling sessions.
Reported regular condom use with clients increased from 11 to 52 percent and then 68 percent after 6 and 36 months of intervention, respectively. The decline in the monthly incidence of trichomoniasis and gonorrhoea is shown in Figure 5-2. The most significant finding, however, was a decline in the incidence of HIV-1 over time, from 11.7 per 100 woman-years during the first 6 months to 4.4 per 100 woman-years over the last 6 months, 3 years later (Figure 5-3). The risk factors for HIV-1 seroconversion included irregular condom use, gonorrhea, trichomoniasis, and genital ulcer disease. Among women who attended more than 90 percent of their clinic appointments, the HIV-1 incidence was 2.7 per 100 woman-years, compared with 7.1, 20.3, and 44.1 per 100 woman-years among women who attended 76 to 90 percent, 50 to 75 percent, and less than 50 percent of their monthly appointments, respectively. That this gradient remains after controlling for the effects of reported condom use and number of clients implies that STD treatment was a key factor in the decline in STD incidence.
This program demonstrates that a comprehensive prevention program of behavior-change intervention, STD treatment, and condom provision can lead to a reduction in the incidence of both STDs and HIV. Despite the impressive impact of the intervention, however, this type of project is not sustainable or replicable because of the high cost of the intensive research effort involved. A
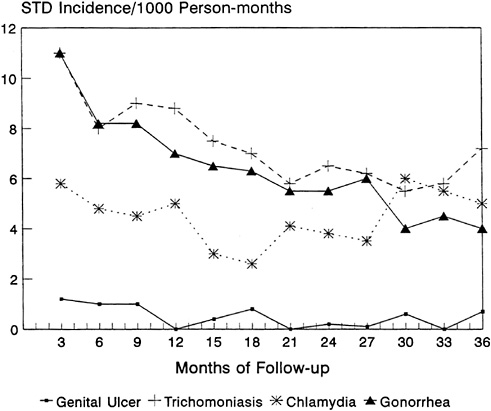
FIGURE 5-2 STD Incidence Among Prostitutes, Kinshasa, Zaire.
SOURCE: Adapted from Laga et al. (1994).
further drawback of this intervention was its focus solely on women; male clients and steady partners were neither targeted nor involved. This omission may be one of the reasons why average condom use with clients did not exceed 60 percent.
Case Study: A Community-based Intervention
A two-stage study of the effectiveness of nurse-managed peer education and support groups for AIDS prevention among women was initiated in Botswana in 1990 (Norr et al., 1992; Tlou, 1995). The objective of the intervention was to heighten women's awareness and knowledge about AIDS and to enhance their communication skills and assertiveness in negotiating for safer sex with their partners.
In the first year of the program, in-depth interviews were conducted with 56 women to explore content and service delivery mechanisms for a peer education
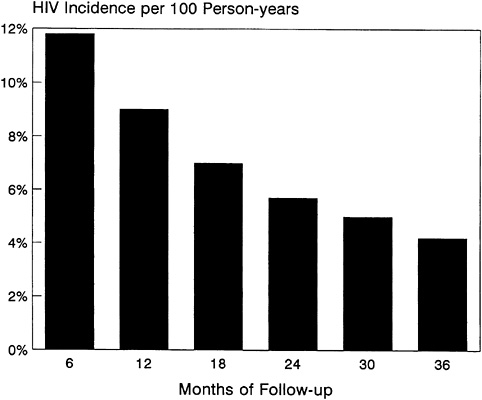
FIGURE 5-3 Trends in HIV Among Prostitutes, Kinshasa, Zaire.
SOURCE: Adapted from Laga et al. (1994).
model appropriate to the culture, values, and resources of Botswana. Training sessions for women included condom skills sessions and practice in how to say "no" to unsafe sexual practices through role playing. In the second and third years, the intervention was extended to 600 women in 12 workplaces in Gabarone. The project is now expanding to 5 rural districts in the county using a training-of-trainers model and is being extended to include primary school teachers and university students.
Positive attitudes toward condoms and expressed confidence in correct condom use increased among the program participants from 35 to 76 percent. Those who reported always using condoms at each sexual encounter increased from 28 to 50 percent. Moreover, participants reported having increased their promotion of safer sex to others, including relatives, children, coworkers, and neighbors. Further evaluation of the program is under way.
There are several commendable elements of this intervention. First, it is a community-based intervention targeted to women in both urban and rural areas, rather than solely to groups traditionally seen as high risk (such as commercial sex workers). Second, it can be replicated at relatively little cost among other
target populations, such as primary school teachers and university students. Third, it attempts to empower women with communication and negotiation skills for safer sex with their partners.
Nevertheless, two weaknesses of this program are evident. After participating in the program, married women still found it difficult to introduce condoms, probably because men were not targeted in the intervention. Moreover, available evaluation indicators were not adequately used to assess the effectiveness and cost-effectiveness of the program.
Lessons Learned
Among the lessons learned from the implementation and evaluation of prevention programs targeting African women to date, we can highlight the following:
-
Programs need to reflect an understanding of, if not directly address, the multiple roles of women, which include wife, mother, housekeeper, and child rearer.
-
Comprehensive models of programs for women are not available. A wider range of tested interventions is needed, including network, group, and community-based interventions; policy interventions; and interventions that focus on power and status. Women's STD programs must develop better ways of identifying symptoms and encourage care-seeking behavior, as well as enhance the provision of sensitive and appropriate medical care. Interventions also need to promote the use of condoms to protect against pregnancy. These interventions will be more effective if the status of women is enhanced through such means as legislation and social policies that protect and expand women's rights.
-
Women are especially vulnerable to HIV. In many cultures, there is pressure to produce children to sustain a marital union. The fact that many men have partners outside of stable unions (see also Chapter 4) also makes women particularly vulnerable to HIV. Monogamous African women frequently report being exposed to HIV through their husbands' other sexual partnerships.
-
Interventions based on individual decision-making models do not take into account women's low power. Low power and low self-esteem are not the same thing; low power in dyadic relationships with men is supported by tradition.
-
Women are often entrusted with preserving traditions, a role that conflicts with social change and may restrict programmatic access to them. Successful design and implementation of interventions for women requires the tacit if not active support of political, religious, and community leaders. Women's roles cannot change in isolation. Male attitudes and behaviors, especially those of sexual partners, must also change.
-
There is a need to develop new technologies and approaches to reach women since women's needs are not directly addressed by those that currently
-
exist. New barrier methods, especially nonspermicidal viricides, are needed. Moreover, new technologies need to be developed for STD diagnosis and new programs implemented to reach infected women.
-
Women need to participate in the research and development of HIV intervention programs targeted to them. Their participation may lead to the identification of new prevention technologies that are responsive to women's needs.
INTERVENTIONS TARGETING YOUTH
Before discussing HIV/AIDS intervention programs that target youth, it is useful to define this group as it is referred to in this chapter. We adopt the WHO definition of adolescents, which includes persons from 10 to 24 years of age (World Health Organization, 1986) and use the terms "youth" and "adolescents" interchangeably.8 People under 10 years old are referred to as children, and those aged 25 and older as adults. We adopt these definitions while acknowledging that in some African cultures, persons over 25, especially if not married, are still considered youth, and some younger than 25, especially if married, are considered adults.
It is imperative that HIV-prevention strategies reach youth before they become sexually active. Lives can be saved by educating youth before they acquire their attitudes about delaying sexual intercourse and about safe sexual practices such as condom use and nonpenetrative sex and by promoting a sociocultural environment that encourages these practices. These messages must be compatible with local mores and cultural beliefs. To the extent that prevention messages are realistic, clear, and expressed in language youth can readily understand, interventions are more likely to have a positive effect. Where social practices conflict with prevention needs, considerable dialogue among public health officials and parents, teachers, politicians, and religious and tribal leaders is needed. Multi-component intervention strategies are important in targeting youth. Innovation, variety, and persuasive messages from respected sources such as peers and influential adults, as well as a supportive environment, play key roles in such programs.
Issues
Perhaps the most important task of adolescents is growing up. Integral to this process is the acquisition of adult skills and habits, including learning about
adult sexual practices. To be accepted as an adult and a member of society in many African cultures, one must prove one's fertility—often in the context of marriage. Many cultures have strong expectations for early marriage and child-bearing soon after puberty, especially for girls. HIV-prevention messages must be developed with a recognition that postponement of sexual debut may be in potential conflict with local mores. Further, even where delay in sexual debut is considered possible or desirable, there is a paucity of information available to adolescents about responsible, safe expressions of sexuality once sexual relations have been initiated.
African adolescents, like adolescents elsewhere in the world, are often unable to discuss openly with their parents their questions, fears, and concerns about sex, marriage, and other adult topics. They also have poor negotiation skills when approached for sex by adults. With the exception of cultures that have adult female initiators, 9 youth have little opportunity for frank discussions with adults about sex. Youth therefore rely heavily on their peers for information. Unfortunately, peer information is often inaccurate. In addition, some youth may feel pressure from their peers to experiment with sex. Elders, who have traditionally been respected and whose guidance has been valued by youth, are now seeing their role and influence being eroded slowly by modern influences. the impact of these significant social changes remains unknown.
The escalating number of children and adolescents orphaned by parents who have died of AIDS is also a critical issue (see Chapter 6). The World Health Organization predicts that by the year 2000, more than 10 million HIV-negative children under age 10—90 percent of them in sub-Saharan Africa—will have lost their mothers to AIDS (World Health Organization, 1992b). Traditionally, orphaned children are absorbed by the extended family. But in many areas, such as the Rakai district in Uganda and the Kagera region of Tanzania, many heads of households have died of AIDS, leaving elderly grandparents to care for multiple sets of children. Inevitably, some children also slip through the cracks in the extended family network and find themselves living on the streets, where modifying high-risk behavior becomes secondary to satisfying basic needs, including food, shelter, and clothing.
Other issues relate to the subgroup of youth that attends school. On the one hand, schools are ideal vehicles for HIV education because they exist everywhere, even in rural areas, and provide easy access to youth. Moreover, schools can reach students daily, making critical reinforcement of prevention messages more practical. But schools as vehicles for HIV-prevention programs have their limitations. Many schools are overcrowded, and in some countries, such as Zambia, schools run double and sometimes even triple shifts per day. Consequently,
most youth do not spend more than a few hours a day at school, hours that are packed with learning the basics. Furthermore, schools as institutions are not homogeneous; there are public schools, private schools, and church schools, all of which have significantly different social climates, structures, and educational resources. In addition, student bodies in schools are heterogenous, ranging from the homeless to the elite. Thus, HIV education approaches need to be appropriate to the particular school environment. Finally, approximately half of all youth in many sub-Saharan African countries do not attend school (World Bank, 1993). These youth are not easily reached, organized, motivated, or tracked and are therefore difficult to target with intervention programs.
In some parts of sub-Saharan Africa, an increase in age at marriage has resulted in the creation of a new subset of youth: unmarried, postpubertal, adolescent girls or young women. This group may be especially vulnerable because the social norms relating to women their age in the past assumed they were married; there are few expectations to guide either the behavior of these girls or the behavior of others toward them. African adolescent girls often become targets of older men, but have few skills to control sexual relations. These girls may be at high risk of STDs, pregnancy, and abuse in addition to HIV infection. An added risk factor for HIV in this group may be biological, because of cervical ectopy (Bulterys et al., 1994). Worldwide, 70 percent of HIV infection among women is estimated to occur in girls between the ages of 15 and 25 (Ankrah, 1994). Adolescent girls in Zimbabwe are five times as likely to be infected with the HIV virus as adolescent boys (Ankrah, 1994).
Government ministries, nongovernmental organizations, and donors have called for long-term strategies to improve the subordinate status of and dearth of educational and employment opportunities for adolescent girls (Gupta and Weiss, 1993; Ankrah, 1994). Increased education, improved equity between girls and boys, and meaningful income-generating activities can help adolescent girls achieve economic security and higher social status, which may, in turn, enable them to avoid high-risk behavior. Intervention programs to date have focused almost exclusively on matters related directly to health (modification of sexual behavior, STD care, family planning-related activities, and condom use). A few notable exceptions have established links to organizations concerned with improving the social and economic situation of young women and shown promising results (Leonard, 1994; Delehanty, 1993).
Policy-based intervention strategies are also needed to influence social norms and change sexual practices that facilitate the spread of HIV in this group, such as the sugar daddy syndrome, child marriage, incest, and rape. Principally because of limited resources, however, virtually no prevention programs in Africa have linked advocacy for protective laws and policies for adolescent girls with program design and implementation.
Interventions to date (UNICEF, 1995; Annex 5-1 in this volume) point to several strategic approaches that should guide HIV-prevention programs targeted
to adolescent girls. First, practical and culturally relevant information needs to be developed and disseminated through existing communication channels, including schools, radio, youth organizations, and traditional channels such as female initiators. Second, such communication should concurrently target adolescent boys and older men, a strategy that is seldom used. Finally, sustained efforts from multiple channels are critical to influencing social norms.
Target Population
Adolescents, like other age groups, are a heterogeneous group for which numerous multifaceted intervention strategies are required to achieve behavior change. Youth intervention strategies can target by access point (e.g., schools, clinics, media, street corners); by age of target audience (with different methods and messages for those aged 10-15, 16-20, and 21 and over); by marital status; and, as discussed earlier, by gender. Adolescents living in urban centers should be targeted differently from their counterparts in rural villages. Youth living in sparsely populated rural areas, such as the eastern province in Cameroon or the desert in Botswana, respond to different intervention approaches than youth living on the streets in large urban centers such as Lagos, Nigeria, or Dar es Salaam, Tanzania. Youth living on the streets have different needs and respond to different messages than youth living in families.
Types of Strategies and Programs
Prevention interventions targeted to youth should include not only individual behavioral but also structural/environmental components (Table 5-4). Yet most interventions targeted to African youth to date have typically focused on behavior-change intervention and the promotion and provision of condoms (UNICEF, 1995; Grunseit and Kippax, 1993). Strategies used have included setting up drop-in centers in the community that encourage youth to stop in on an ad hoc basis; sending outreach workers into markets, bus terminals, and truck stops; organizing community sports activities and clubs; initiating anti-AIDS clubs; and training adults—such as traditional initiators for coming-of-age ceremonies—who have regular access to youth.
HIV intervention programs need to expand beyond health-related components by linking with organizations that have the resources and expertise to incorporate economic, educational, and policy-based components into HIV-prevention programs. Examples are organizations that could improve access to education by providing school fee waivers or stipends or offer income-generating possibilities. Although such linked programs are admittedly difficult to implement, the few that exist have shown exciting results, albeit on a limited scale (Delehanty, 1993; Leonard, 1994).
AIDS care and management, especially coping with death and dying, should
TABLE 5-4 Objectives of HIV-Prevention Programs Targeted to Youth
|
Individual Behavior Change: • Delay sexual debut. • Decrease number of partners or frequency of sex. • Increase consistent and correct condom use. • Develop sexual communication and negotiation skills with regard to condom use. • Develop risk-avoidance skills. • Learn to recognize STD symptoms, and seek early appropriate treatment. • Increase primary HIV-prevention knowledge (e.g., where to buy condoms). • Increase risk perception. • Increase risk-reduction motivation. |
|
Structural/Environmental Changes: • Render condoms available, accessible, and affordable. • Improve diagnosis and treatment of bacterial STDs. • Increase parent-child communication skills. • Improve sexual communication, negotiation, and condom-use skills. • Increase involvement of gatekeepers and youth in intervention program design. • Advocate policies that support the advancement of youth. • Increase access to education for out-of-school youth (e.g, waive school fees). • Link income-generating components with HIV-prevention programs targeted to youth. |
be an additional component of prevention programs targeted to youth, particularly in view of the large numbers of AIDS orphans projected in many African countries. Innovative responses to the burgeoning burden on families of AIDS patients and AIDS orphans are being developed (Delehanty, 1993). In Uganda, for example, orphaned children and adolescents are targeted in an intervention that links an economic development component to a basic comprehensive intervention package of behavior-change communications and STD counseling.
Comprehensive programs for youth should also include gatekeepers who shape and influence a group's culture. Such gatekeepers include community elders, parents, traditional healers, teachers, school administrators, the media, government officials, religious leaders, and adolescent heroes. The Family AIDS Education and Prevention Through Imams (FAEPTI) Project in Uganda, for example, successfully trained indigenous authoritative leaders in AIDS-prevention messages (Kagimu et al., 1995). The program's success was augmented by creating a community-chosen cadre of male and female family AIDS workers who supported and reinforced the imams' public messages on HIV/AIDS prevention.
Although the above examples highlight some of the more innovative approaches, strategies targeting youth to date have had several limitations. In general, comprehensive and integrated HIV-prevention models for African youth
are virtually nonexistent. Instead, single-dimensional approaches have been advocated to address multidimensional problems (e.g., the disproportionate reliance on the "peer educator" approach for all adolescent HIV-prevention needs). In addition, little formative research has been done to tailor messages to specific youth subgroups. Moreover, inappropriate selection criteria have been used to qualify youth as peers, and peer programs have typically been neither well supervised nor well evaluated. Finally, youth have not been regular participants in the planning, design, and evaluation of programs.
The following case study highlights some of the issues and limitations discussed above and is representative of typical interventions targeted to African youth to date.
Case Study
In 1989, results from serosurveys in Addis Ababa, Ethiopia showed that 24 percent of female commercial sex workers between the ages of 12 and 16 were HIV-seropositive (Gebru et al., 1990). These results, while known to the Ministries of Health and Education, were not widely available to the public; a school-based HIV/AIDS education and prevention program was proposed. Before a new program of this type can begin, parents and other community members need to be educated about HIV prevention and the need for HIV education in junior and senior secondary schools. Focus group discussions with students and school teachers also help sensitize adolescents to the risk of HIV and build support and acceptance for the initiation of a strong school-based HIV/STD-prevention effort (Gebru et al., 1990).
A pilot HIV intervention project was implemented during 1990 and 1991, sponsored jointly by the Ministries of Health and Education. WHO/GPA assisted in the development and evaluation of educational materials and teaching methods that were incorporated into the curricular and extracurricular activities of Ethiopia's secondary schools.
The project had four specific objectives: (1) to teach students how to prevent HIV/STD transmission and enhance risk-reduction attitudes; (2) to reduce discriminatory attitudes toward HIV-positive fellow classmates and other community members; (3) to teach skills that would allow the students to disseminate HIV/STD-prevention messages to their families and the wider community; and (4) to train teachers to provide effective AIDS education and to stimulate student interest in becoming community health educators.
The project had multiple components. Innovative classroom curricula and teaching methods were developed that relied on role play, rehearsal of risk-avoidance skills, group discussions, drama, and peer educators. Sessions were held to train teachers and students to use these materials in class and in after-school clubs (such as drama, music, health education, and Red Cross clubs).
Students were also trained to become outreach educators for their family and local communities.
Five experimental schools were randomly selected from schools in Addis Ababa (two senior schools and one junior secondary school) and Debra Birhan (one senior and one junior secondary school). Two comparable junior and two comparable senior secondary schools were designated as controls. Most students in these schools conformed to the normal grade/age range, with 38 percent aged 12-14 and 33 percent aged 15-16, although reported ages ranged from 9 to 22. Examination of baseline data showed no significant differences between the experimental and control schools in terms of demographics, knowledge, and attitudinal variables. Other evaluation design features included a pre and post in-class questionnaire; in-depth student KAP interviews; and random surveys of parents and community members about their HIV/AIDS-related knowledge and opinions and their exposure to student educators and AIDS education materials. Monitoring of the project's implementation was performed by teachers and research assistants through checklists and observations. In addition to frequent supervisory visits by project staff, an evaluation workshop allowed teachers to provide feedback about the success or failure of the program.
Results from the project were positive. While rigorous statistical analysis was not performed, experimental students consistently showed the most knowledge gains. At the post-test, learning differentials between experimental and control groups ranged from 13 to 27 percent for items related to HIV-prevention facts (e.g., condoms reduce HIV risk) and correction of transmission myths (e.g., mosquitoes transmit HIV).
The experimental group also showed a greater change at post-test in their attitude toward classmates and others with HIV/AIDS. For example, at post-test, experimental students showed a 35 percent increase in willingness to care for someone with AIDS as compared with a 15 percent increase among the control students. Experimental students also showed a 26 percent increase in willingness to accept a teacher with AIDS, as compared with a 12 percent increase for control students. Statistical significance, however, was not reported. A "considerable effect" on attitudes toward risky sexual behavior was noted among the experimental students. At post-test, experimental students were more likely than control students to support abstinence (24 percent increase among the experimental groups as compared with a 10 percent decrease among the control groups), to report resisting pressure to have sex (20 percent increase among the experimental groups as compared with a 2 percent increase among the control groups), to think that sex with prostitutes increases the chances of getting AIDS (19 percent increase among the experimental groups as compared with 8 percent among the control groups), and to agree that proper use of a latex condom reduces the chances of getting AIDS (19 percent increase among the experimental groups as compared with an 8 percent increase among the control groups). Adolescent
sexual behavior and condom use were not measured because of political and practical constraints.
The evaluation examined the effects of the peer outreach component in terms of the degree of student participation, coverage in the community, and the degree of change in knowledge and attitudes by those who were exposed to the student educators. Data were collected from 1,056 surveys conducted 3 months after the intervention took place in the community (357 experimental school parents, 349 control school parents, 350 members of the community). The results suggest that student educators were successful in the community. Evidence from the community surveys shows that a majority of the parents and community members surveyed had seen the AIDS textbook from the school and that a majority of the parents had discussed AIDS with their children.10 Parent participation in school-based AIDS drama and music events and poster exhibitions also increased. In Addis Ababa, student presentations were videotaped by the Ministry of Information and then broadcast through its Youth Programme to the community.
This intervention is a good example of a multicomponent, skills-based, school-based HIV-education program that involves youth in the implementation of the program and targets youth early (at ages 11 or 12). The evaluation design lacked behavioral impact data, and the data analysis was simple, but trends in the results were consistent, suggesting that the program was able to achieve its objectives.
Lessons Learned
Several lessons can be learned from this case study and similar evaluations of school-based HIV-education programs in Tanzania (Klepp et al., 1994) and elsewhere in Africa (e.g., World Health Organization, 1994b). First, adolescents need to be reached before they become sexually active. Although some parents fear that an early discussion of sexual behavior may make adolescents prone to earlier sexual debut, a review of the HIV/AIDS-education literature shows that sex/AIDS-education programs do not increase sexual experimentation or promiscuity (Ford et al., 1992; Grunseit and Kippax, 1993; Kirby et al., 1994). In fact, some program planners in sub-Saharan Africa have been surprised to find that the majority of parents in their areas support AIDS education in schools (World Health Organization, 1994b). Furthermore, sex/AIDS-education programs, if well designed, can increase condom use among sexually active adolescents (Kirby et al., 1994). In particular, some African studies have shown that information about condoms can be delivered in schools with parental approval as long as
condoms are presented as the next best alternative to postponing sexual debut until marriage, followed by fidelity after marriage (World Health Organization, 1994b).
Needs assessments and KAP baseline surveys should be conducted with parents and educators, as well as students, before programs are initiated. Such instruments provide important information that helps enlist advocates for program implementation. In addition, they are necessary for designing programs to match local community values, an essential factor in garnering support for school-based HIV programs. In Uganda, for example, results from a KAP survey showed that parents supported AIDS education in the schools, but were not as comfortable with sex education (World Health Organization, 1994b). As a result, program planners presented AIDS education in the context of a comprehensive health-education program, a strategy that helped enlist support for and sustain the program.
Intensive training of educators in the design and delivery of feasible and effective curricula is essential. Training should include—but go beyond—biomedical factors and should address individual teachers' comfort levels in educating about HIV prevention in the classroom. For example, some African intervention programs have included speakers from local family planning organizations to help teachers explore their own values and comfort levels in teaching AIDS-prevention messages (World Health Organization, 1994b). Training should also focus on teaching skills in negotiation and condom use. In addition, interactive and participatory teaching methods should be used in tandem with didactic methods. Participatory methods might include drama, song competitions, poster drawings, games, group discussions, and role playing.
In conclusion, HIV-prevention interventions targeting youth should (1) be introduced throughout the school system and include explicit skills-based education; (2) reduce opposition to AIDS education by providing local information about the magnitude of HIV/STDs in the community to teachers, parents, religious leaders, and other community leaders; (3) include the family and enhance its role in AIDS education targeting youth; (4) provide education for both adolescent males and females regarding their responsibilities in human reproduction and HIV transmission; (5) include child-to-child (peer education) teaching methods, whereby older children share knowledge with younger children and those not attending school; (6) focus on preventing sexual transmission of HIV, with methods, information, and materials that are sensitive to the social context; (7) use interactive teaching methods; and (8) develop innovative strategies, such as teen drop-in centers, for reaching out-of-school youth.
PERINATAL TRANSMISSION
Perinatal transmission of HIV may occur during pregnancy via the placenta, during delivery, or after delivery through breastfeeding (see Chapter 3). Preventing
infection in women has the addition benefit of preventing perinatal transmission. However, many women are already infected, and significant numbers will continue to be infected despite current intervention programs. For these women, other strategies are needed to reduce transmission of HIV to their newborns; several such strategies are described in the remainder of this section, although there are problems with each that limit their applicability in sub-Saharan Africa.
One approach may be the avoidance of breastfeeding by HIV-infected mothers. There are two problems with this strategy: large numbers of pregnant women would have to be tested and counseled for HIV infection and counseled as well in bottle feeding, and safe and affordable alternatives to breast milk would have to be easily available. This approach is not feasible in most countries in sub-Saharan Africa except for an elite urban minority, for economic and sociocultural reasons. The current recommendation by WHO/UNICEF is that all countries, irrespective of HIV infection rates, should continue to promote and support breastfeeding because of its impressive nutritional, immunological, and child-spacing benefits (World Health Organization, 1992a). In particular, WHO (1992a) recommends that in areas such as sub-Saharan Africa, where the primary causes of infant mortality are infectious disease and malnutrition, breastfeeding should be encouraged for all women, regardless of HIV status. The rationale for this recommendation is provided by studies showing that an infant's risk of becoming HIV infected through breast milk is lower than its risk of dying of other causes if deprived of breast milk.
Another approach to prevention of perinatal transmission is the provision of voluntary and confidential counseling and testing services to women who may then choose to avoid or terminate pregnancy. This alternative is unlikely to be feasible in African countries where access to HIV testing is poor, abortion is often illegal and frequently unsafe, and fertility is highly valued.
A third approach is the delivery by caesarean section of infants of HIV-infected mothers in order to minimize the risk of neonatal infection during vaginal delivery. While caesarean section delivery has proven effective in prevention of other viral infections (Minkoff and Duerr, 1994), no definite conclusions can be drawn on the basis of available data concerning its potential protective effect with regard to perinatal HIV transmission. Furthermore, even if the efficacy data were to point to caesarean section as an effective prevention strategy, the increased risk and high cost associated with the procedure render it an infeasible alternative in all but a handful of teaching hospitals in the region.
Another possible approach to reducing the risk of infection during vaginal delivery is vaginal lavage, or washing with a microbicidal agent during delivery. Vaginal lavage has been shown to lower rates of neonatal group B streptococcal infection in newborns and may prove to be helpful in the prevention of HIV transmission during delivery (Minkoff and Duerr, 1994). Potential problems, however, include fetal toxicity and genital mucosal irritation. More research is
needed to quantify the risk of HIV transmission during vaginal delivery and to evaluate the efficacy of vaginal lavage in prevention of HIV transmission.
The most effective means of preventing perinatal transmission from HIV-infected mothers may be the administration of antiviral therapy such as Zidovudine (AZT) to the mother during pregnancy, labor, and delivery and then to the newborn during the first weeks of life. Data from a clinical trial involving 364 births to HIV-positive women showed a 67.5 percent reduction in the risk of HIV transmission attributable to AZT therapy (Centers for Disease Control, 1994). Efforts are now currently in progress to define the minimum dosage schedule for AZT in pregnancy. The trial results led the U.S. Public Health Service to issue new interim recommendations for care of pregnant women who meet the protocol eligibility criteria (Centers for Disease Control, 1994). However, there are several reasons why the therapeutic regimen in the trial (Protocol 076) will not be applicable to women in sub-Saharan countries. The main obstacle is the cost of the drug and sophisticated clinical equipment. Another obstacle is the requirement that babies be bottle fed with costly infant formula. Several studies are now under way to discover whether the trial results can be translated into a preventive strategy that can be used in developing countries, using either a shorter course of AZT treatment around the time of delivery or a lower dose of AZT (Cohen, 1995).
Vitamin A, dubbed ''the anti-infective vitamin" as early as the 1920s, is currently under investigation as an alternative method to reduce vertical transmission. Several recent studies that have evaluated the impact of vitamin A on vertical transmission of HIV give reason for optimism that vitamin A can inexpensively and easily reduce the risk of vertical transmission. In a 2-year study of 338 HIV-positive mothers in Malawi, Semba et al. (1994) found that women with higher serum vitamin A transmitted HIV to their children significantly less often than their vitamin A-deficient counterparts. The results were dramatic: 32.4 percent of women in the most deficient group transmitted HIV, while only 7.2 percent of women in the group with the highest serum vitamin A did so. Unfortunately, the research was nonexperimental, and it is possible that other nutritional or behavioral factors associated with serum vitamin A (such as general nutrition) played a significant role.
Other studies have proposed that the usefulness of vitamin A is as a preventative measure for morbidity associated with HIV/AIDS in children, rather than an inhibitor of HIV transmission per se. This hypothesis posits that vitamin A serves to enhance the immune system, thus reducing the severity of opportunistic infections or the duration of specific illnesses, rather than the likelihood of infection per se. A randomized, placebo-controlled study of 118 children of HIV-infected women in Durban, Natal, found that all children showed improvements in morbidity (measured in child-months of ill health) with vitamin A supplementation and that children who were themselves HIV infected showed particular improvement for diarrhea-related illness (Coutsoudis et al., 1995). A recent review of the effectiveness of vitamin A supplementation in the control of morbidity
and mortality among young children in developing countries concluded that "vitamin A supplementation can effectively reduce mortality rates in young children, and probably also reduce the risk of severe morbidity" (Beaton et al., 1993:66). Although the exact role of vitamin A remains unclear, further research into its effectiveness in inhibiting perinatal transmission and reducing the mortality and morbidity of HIV-infected children is clearly warranted.
RECOMMENDATIONS
Numerous interventions are being implemented throughout Africa, but most are still information-based health education campaigns. Many of the messages communicated are generic or vague and do not address specific risk behaviors. Innovative approaches are typically small scale and lack rigorous evaluation. Furthermore, it is not easy to demonstrate the success of a particular intervention because it is difficult to define and measure such outcome variables as "better health status" and to determine whether the intervention in question was the reason for a desired change. Consequently, the need for solid evaluation research is still urgent.
KEY RECOMMENDATION 2. An increase in research funding for the development of social and behavioral interventions aimed at protecting women and adolescents, especially girls, from infection deserves highest priority.
An important step in arresting the spread of AIDS in sub-Saharan Africa is to recognize that, although African women have relatively high autonomy by the standards of developing countries, their low and separate status remains a major obstacle to HIV prevention. In many societies, the presence of unmarried, postpubertal girls is a new phenomenon. Guidelines for their sexual behavior and that of others toward them are not well established; their low social status makes them particularly vulnerable. Moreover, in many areas of sub-Saharan Africa, high HIV incidence has been detected among adolescents and young adults, especially girls. Research on which to design culturally relevant programs targeted to adolescents and to adults who might be their sexual partners is an important priority.
KEY RECOMMENDATION 3. More evaluation research is needed to correlate process and outcome indicators—such as reported condom sales and behavior change—with reductions in HIV incidence or prevalence.
Rigorous designs, such as controlled intervention studies to assess the effectiveness of different prevention approaches, are needed. To date, few rigorous evaluations of intervention programs in sub-Saharan Africa have been conducted (see reviews in Choi and Coates, 1994, and Crump, 1995). Evaluations that have been reported often lack precision in their measurement of risk behaviors and are therefore not very informative. As a result, few strategies can demonstrate whether they are effective. Barriers to rigorous evaluation research include lack of human resources, expertise, financial resources, and equipment. Overcoming these barriers requires major changes in research infrastructure. Nevertheless, it is a priority to begin now a few large-scale behavioral interventions, including adequate baseline surveys, multiround surveys, and longitudinal studies with comparison cohorts, even if these interventions are relatively expensive. It is only with these types of studies that more definitive information on the effectiveness of various interventions, which is so desperately lacking for most studies in sub-Saharan Africa, can be obtained. The longer such studies are delayed, the longer will exist the uncertainty about which HIV-prevention strategies work best, for whom, and under what circumstances. In the interim, basic program evaluation and some formative and operational research can be completed, and such work should be required by donors as part of program implementation awards.
Recommendation 5-1. Interventions that promote gender equality deserve high priority as AIDS-prevention strategies in every country.
Women's primary source of risk is their society-wide subordination, not their lack of knowledge (Heise and Elias, 1995). Governments can effect change in many ways to empower women: reducing the financial necessity for multiple partnerships by changing laws to give women equal access to training and jobs, equal rights of inheritance and property ownership, equal access to education, and equal wage scales; enacting and enforcing laws against rape; building the capacity of women for collective action; and educating everyone about women's rights. Enhancing the status of women is a long-term strategy that would have many beneficial effects for development, in addition to the likely effect of reducing the transmission of HIV and other STDs.
Recommendation 5-2. In the short term, a female-controlled vaginal microbicide that would allow women to protect themselves without their partner's participation is an urgent research and development priority for international donors.
A microbicide is not a quick-fix substitute for the fundamental structural reforms necessary to achieve gender equality, but rather a temporary and partial response to this problem as it influences HIV transmission (Elias and Heise,
1994; Heise and Elias, 1995). Yet in the same way that the use of spermicides by women can reduce fertility, the use of a microbicide could, in and of itself, help arrest the spread of HIV.
Recommendation 5-3. Research is needed to address the HIV-prevention needs of several other populations with marked vulnerability, particularly the mobile and the disenfranchised.
There is a need to reach mobile individuals and groups with comprehensible and acceptable programs, particularly where linguistic and cultural barriers exist between migrants and the local population. Ways of effectively providing preventive services to the disenfranchised populations in the ever-growing urban slums and in refugee camps need to be developed; a major challenge to such programs is the lack of resources and social support for individuals in such settings.
Recommendation 5-4. Additional research should be conducted to determine the impact of specific STD interventions on the incidence of HIV infection within defined populations.
Research is needed to determine the extent to which STDs help cause HIV infection, to examine the importance of the behavioral synergy of STD and HIV transmission, and to design more effective intervention programs. There is a need for assessment of the relative efficacy and feasibility of various interventions for STD treatment and sexual behavior change in reducing HIV transmission. This research includes assessing the effects of programs that target individuals at high risk of acquiring and transmitting STDs, as well as the effects of community-based STD programs. The interventions themselves could comprise STD education, condom distribution, increased STD screening, and mass antibiotic therapy. Data on the effectiveness of these interventions, particularly those focused on decreasing STD prevalence, are essential for evaluating the impact of STD reduction on the spread of HIV. Behavioral research on ways of ensuring acceptance of various STD control strategies should be directly integrated into the epidemiological research.
Recommendation 5-5. Research is needed to assess the effectiveness and cost-effectiveness of the syndromic approach to STD diagnosis and treatment.
Clinical testing for STDs is expensive and not widely accessible. Therefore, research is needed on better ways to identify STDs more accurately through symptoms. In addition, new screening methods, including urine-based assays for chlamydia and gonorrhea and self-administered vaginal swabs for trichomonas
culture and bacterial vaginosis gram stain, should be incorporated into research. Efforts are needed to make these techniques available and affordable in developing-country settings for surveillance, diagnosis, and validation.
Recommendation 5-6. For long-term program planning and resource allocation, cost-effectiveness studies should be incorporated in donor research work and the cost-effectiveness of HIV prevention compared with that of other health interventions.
Few intervention evaluations have adequately assessed effectiveness in terms of behavior change or seroincidence declines, much less cost-effectiveness. Results of evaluation studies currently in progress in several countries in sub-Saharan Africa (Family Health International/AIDSCAP, 1994) are expected to provide data on the cost-effectiveness of various HIV-prevention strategies. However, determining the effectiveness of HIV-prevention strategies is methodologically complex and will take several more years to complete. In the meantime, since resources are insufficient and may well decline further, efficient resource utilization is paramount. Thus, basic analysis of overall program costs and specific intervention costs is critical. Simple cost analyses and cost-effectiveness estimates could provide data that would be helpful for public health decision making and program design.
Recommendation 5-7. Operations research should be a high priority.
The growth of the HIV/AIDS pandemic in the past 20 years in sub-Saharan Africa has led to the development of institutional and community-based responses and a corresponding need for operations research to improve the effectiveness, cost-effectiveness, and quality of these responses. Primary research needs include scaling up successful experimental interventions, improving the effectiveness and reducing the cost of existing programs, examining the cost-effectiveness of linking HIV prevention with HIV/AIDS care, and improving the sensitivity and specificity of criteria for targeting interventions.
Recommendation 5-8. Research should be undertaken to measure the impact of female-controlled barrier contraceptive use on HIV transmission.
Studies should be undertaken to determine the effectiveness against STDs and HIV of female-controlled barrier contraceptives such as female condoms and spermicides. This research should encompass field-based studies of the acceptability of these methods. Moreover, greater efforts need to be made to integrate appropriate HIV/AIDS-prevention messages and programs for STD diagnosis, referral, and treatment into family planning programs.
Recommendation 5-9. Behavioral research is needed to develop effective pregnancy-related HIV counseling programs.
Given the rapid spread of HIV among women in sub-Saharan Africa, perinatal transmission continues to have a major impact on infant and child morbidity and mortality among populations with a high HIV seroprevalence. Studies using modified treatment regimens with Zidovudine (AZT), hyperimmune gamma globulin, vitamin A, vaginal washes, and other means of intervention should be undertaken to determine their overall effectiveness and cost-effectiveness in decreasing HIV perinatal transmission.
ANNEX 5-1 SELECTED AIDS INTERVENTION PROGRAMS IN AFRICA
|
Country (area) |
Intervention Type |
Target Population and Size |
Program Components |
Key Results |
Reference |
|
1. Ghana |
Community-based |
Commercial sex workers |
• Behavior-change interventions; • Condom provision |
• Consistent condom use among sex workers rose from 6 to 71% in 6 months.; • After the intervention, 64% of those followed up reported always using condoms with clients. |
Asamoah-Adu et al., 1994 |
|
2. Ghana |
Population-based |
Ghanaian youth |
• Behavior-change interventions |
• The proportion of sexually active 15-year-olds fell from 44 to 27%.; • Men reported an 18% decrease in sexual partners over 3 months. |
Family Health International/AIDSCAP, 1992 |
|
3. Guinea |
Population-based |
500,000 couples in Guinea |
• Behavior-change interventions; • Condom provision; • Family planning |
• In the first 6 months, 2.3 million condoms were distributed. |
Hess, 1993 |
|
4. Kenya |
Institution-based |
Female prostitutes and women attending clinics |
• Behavior-change interventions; • HIV testing and counseling; • Free condom provision |
• The proportion of counseled women who use condoms increased from 10% at pre-test to 81% at post-test. |
Ngugi et al., 1988 |
|
5. Malawi |
Institution-based (hospital) |
General population (mostly married males) |
• HIV/STD counseling |
• STD treatment and control significantly improved (88% of those counseled were cured; 77% of those in the control still presented with STDs). |
Wynendaele et al., 1995 |
|
6. Nigeria |
Community-based |
Commercial sex workers |
• Behavior-change interventions; • Condom provision; • STD services; • Vocational and literacy programs |
• Post-counseling, the reported ever use of condoms increased from 41 to 71%. |
Williams et al., 1992 |
|
7. Rwanda (Kigali) |
Institution-based (clinics) |
53 HIV-discordant couples |
• HIV testing and counseling; • Free condom provision |
• Within the first year, the percentage of women never using condoms fell from 25 to 3%.; • Post-test, >60% reported condom use in their most recent sexual intercourse act.; • Post-test, "always" condom use doubled, from 12 to 24%.; • Condom use was associated with a lower rate of new HIV infections.; • Discordant couples using condoms increased from 4 to 57% after one year. |
Allen et al., 1992b |
|
8. Rwanda (Kigali) |
Institution-based (clinics) |
1,458 childbearing women in Kigali |
• HIV testing and counseling; • Free condom provision; • Free spermicide provision; • Behavior-change communications (videotape) |
• Condom use increased from 7 to 22% of women.; • HIV seroconversion rates decreased significantly among women whose partners were tested and counseled. |
Allen et al., 1992a |
|
9. Rwanda |
Community-based |
5 rural communes, 100 km from Kigali |
• Behavior-change interventions; • Condom provision |
• Condom use increased from 4 to 44%.; • Reported ever use of condoms increased from 7 to 50%. |
Mercer et al., 1993 |
|
Country (area) |
Intervention Type |
Target Population and Size |
Program Components |
Key Results |
Reference |
|
10. Rwanda |
Institution-based (clinics) |
1,500 attending clinics in Kigali and their partners |
• Behavior-change interventions; • Condom provision; • Free HIV testing and counseling |
• Consistent condom use rose from 7 to 22% in 1 year.; • Prevalence of gonorrhea decreased from 13 to 6% among HIV-positive women.; • HIV seroconversion rates decreased from 4.1 to 1.8 per 100 person-years among women whose partners were tested and counseled. |
World Health Organization, 1992c |
|
11. Rwanda |
Institution-based (workplace) |
Military recruits |
• Behavior-change interventions; • Condom provision |
• Incidence of urethritis fell from 12 to 5% in 16 months. |
World Health Organization, 1992c |
|
12. Tanzania |
Institution-based (workplace) |
Truck drivers and their partners |
• Behavior-change interventions; • Condom provision |
• Condoms distributed increased from 60,000 to 700,000 in 6 months.; • Condom use among women rose from 50 to 91%.; • Condom use among men rose from 54 to 74%. |
Mwizarubi et al., 1992 |
|
13. Uganda (Rakai) |
Community-based |
Young adults aged 13-39 in rural communities |
• Condom promotion and provision by trained peers and community health workers |
• Reported ever use of condoms increased from 7.6% in 1990 to 12.5% in 1992. |
Konde-Lule et al., 1994 |
|
14. Uganda |
Institution-based (workplace) |
The general population; 400,000 workers |
• Behavior-change interventions; • Condom provision |
• Condom use rose from 3.5% in 1990 to 14.5% in 1991. |
World Health Organization, 1992c; McCombie and Hornik, 1992 |
|
15. Zaire (Kinshasa) |
Institution-based (textile factory and commercial bank) |
149 HIV-discordant couples |
• HIV testing and counseling; • Free condom provision |
• Condom use increased from <5 % to 71%, 60%, and 77% at 1, 6, and 18 months, respectively. |
Kamenga et al., 1991 |
|
16. Zaire |
Institution-based (workplace) |
Commercial sex workers in Kinshasa |
• Behavior-change interventions; • STD treatment; • Condom provisions; • Counseling and testing |
• Condom use among women rose from 8 to 60%.; • Annual HIV incidence fell from 18 to 3% in 2 years. |
Laga et al., 1994 |
|
17. Zaire |
Population-based |
13 million urban youth and their parents |
• Behavior-change interventions; • Condom provision |
• Condom sales rose from 100,000 in 1987 to 18 million in 4 years.; • Fidelity rose from 29 to 46% in 6 months. |
Population Services International, 1994d |
|
18. Zambia (Copperbelt) |
Institution-based (workplace, school) |
2 million people |
• Behavior-change interventions; • STD treatment; • Policy component; • Survival skills workshop |
• Three STDs treated at four clinics declined by 54, 53, and 42%, respectively. |
Mouli, 1992 |
|
19. Zambia |
Population-based |
General population |
• Behavior-change interventions; • Condom provision |
• In the first year of the program, 4.6 million condoms were sold.; • Among condom users, 50% indicated they first used a condom within the months following PSI's condom launch. |
Population Services International, 1994d |
|
Country (area) |
Intervention Type |
Target Population and Size |
Program Components |
Key Results |
Reference |
|
20. Zimbabwe |
Institution-based (workplace) |
4,500 factory, workers, families, and local community |
• Behavior-change interventions; • STD treatment; • Condom provision |
• There was a decrease in the number of STD patients in 3 years.; • There were 37,000 condoms a year distributed. |
Williams and Ray, 1993 |
|
21. Zimbabwe (Marondera) |
Institution-based (workplace) |
Men, women, and youth |
• Behavior-change interventions; • Condom provision; • Income generation for commercial sex workers |
• Condoms distributed rose from 385,000 in 1991 to 962,400 in 1993.; • There was an 80% decrease in STD treatment. |
Williams and Ray, 1993 |
|
22. Zimbabwe (Eastern Highlands) |
Institution-based (workplace) |
15,000 male and female plantation workers and their dependents |
• Behavior-change interventions; • Condom provision; • STD treatment; • Home care & management |
• There were 3,600 condoms/month distributed.; • There was a 59% decline in the number of patients treated for STDs. |
Williams and Ray, 1993 |
|
23. Zimbabwe (Rio Tinto) |
Institution-based (workplace) |
3,500 miners and their families |
• Behavior-change interventions; • Condom provision; • STD treatment |
• Condoms distributed rose from 500/year to 56,000/year after 2 years.; • STD patients at four clinics declined between 47 and 78%. |
Williams and Ray, 1993 |
|
24. Zimbabwe (Mutare) |
Institution-based (workplace) |
150,000 men, women and youth |
• Behavior-change interventions; • Condom provision |
• The incidence of STDs decreased by 48% in 2 years.; • There were 2.5 million condoms distributed in 1992.; • The program was expanded to 10 additional workplaces. |
Williams and Ray, 1993 |
|
25. Zimbabwe (Bulawayo) |
Community-based |
General population and high-risk groups |
• Behavior-change interventions; • Condom provision; • Income generation |
• There were 2.5 million condoms distributed in 2 years; • Consistent condom use in commercial sex workers rose from 5% in 1989 to nearly 50% in 1992.; • Positive attitudes toward condoms and expressed confidence in correct condom use increased from 35 to 76%.; • Those reporting "always" use of condoms increased from 28 to 50%. |
Wilson et al., 1992 |
|
26. Zimbabwe (Gabarone) |
Community-based |
Women in the community |
• Behavior-change interventions; • Communication and negotiation skills workshop |
|
World Health Organization, 1992c |

















































