1
A Review of the Physiology and Nutrition in Cold and in High-Altitude Environments by the Committee on Military Nutrition Research
|
The Effect of Altitude on Cognitive Performance and Mood States |
||||
|
Food Components that May Enhance Mental Performance at High Altitude and in the Cold |
||||
PROJECT OVERVIEW
Military operations are frequently conducted in locations where soldiers are exposed to desert, arctic, and high-altitude environmental extremes. Gradual adaptation to these environments aids physiological acclimatization. However, military missions rarely can be planned to allow lengthy acclimatization periods. The recent Desert Storm operation is an example of an operation conducted under adverse conditions with little time initially for preparation or acclimatization.
Recreational mountain climbers, individuals whose professions involve working outdoors in seasonally cold weather, and people who live in cold or high-altitude environments have the opportunity to plan for their activities in these extreme environments. Individuals who are accustomed to the cold or high altitude learn how to adjust their apparel and activities to maintain an acceptable lifestyle in spite of the external environment.
Regardless of climatic conditions, troops must be supplied with food, weapons, housing, and other support facilities that will enable the immediate performance of their mission.
THE COMMITTEE'S TASK
For many years the Military Nutrition Division (MND) at the U.S. Army Research Institute of Environmental Medicine (USARIEM) has been reviewing the nutritional needs of soldiers in environmental extremes and conducting extensive experimentation both in experimental chambers and in the field to ascertain the changing demands placed on soldiers. The Committee on Military
Nutrition Research (CMNR) of the Food and Nutrition Board (FNB), Institute of Medicine (IOM) previously has been requested to provide reviews and recommendations through workshops and reports (IOM, 1991, 1993, 1994) on nutritional needs of soldiers in environmental extremes. These included fluid replacement and nutrient requirements in hot environments.
In 1993, the CMNR was asked by the MND to review research pertaining to nutrient requirements for working in cold and in high-altitude terrestrial environments. In addition, the committee was asked to make recommendations regarding the application of this information to military operational rations. The committee was thus asked to provide a thorough review of the literature in this area and to interpret these diverse data in terms of military applications. The CMNR was asked to address the increased energy demands of such environments and to consider whether these environments elicit an increased requirement for other specific nutrients. The MND also asked the CMNR to include in their response the answers to the questions listed in Table 1-1. This
TABLE 1-1 Questions Pertaining to Nutritional Needs in Cold and in High-Altitude Environments Posed by the MND to the CMNR
|
Performance |
|
|
• |
What is the effect of cold/altitude exposure on muscle strength and endurance? |
|
• |
Can diet influence these changes? |
|
• |
How does cold/altitude exposure influence appetite? |
|
Health and Medical Aspects |
|
|
• |
Is there concern for increased cardiovascular risk when a high fat diet is consumed for intermittent (7- to 14-d) time periods in the cold? |
|
• |
What nutrients prevent or lessen the signs and symptoms of acute altitude exposure? |
|
• |
Is free radical formation a concern for prolonged (10- to 30-d) military operations at 10,000-15,000 ft (3,048-4,572 m) elevation? |
|
Thermoregulation and Acclimatization |
|
|
• |
Is cold/altitude acclimatization facilitated by prior satisfactory nutritional status or supplemental nutrients? |
|
• |
What nutrients influence thermoregulation? |
|
• |
Does the timing of food ingestion influence cold tolerance? |
|
• |
What is the relationship between fluid intake and thermoregulation in the cold and at altitude? |
|
Nutritional Requirements |
|
|
• |
What are typical energy requirements for work in cold and high-altitude environments? |
|
• |
What is the effect of cold and altitude exposure (at rest) on basal energy requirements? |
|
• |
Does cold or altitude exposure alter the requirement for nutrients other than energy? |
|
• |
What is the sodium requirement for hard physical work in a cold environment? |
|
• |
What is the relationship between fluid intake and food intake in the cold/altitude? |
report thus provides a parallel review to the previous CMNR report on the nutritional needs of individuals actively working in hot climates (IOM, 1993).
These specific issues were summarized by COL Eldon W. Askew (program officer designee) into two overriding questions:
- Aside from increased energy demands, do cold or high-altitude environments elicit an increased demand or requirement for specific nutrients?
- Can performance be enhanced in cold or high-altitude environments by the provision of increased amounts of specific nutrients?
To assist the CMNR in responding to these questions, a workshop was convened on January 31–February 1, 1994 that included presentations from individuals familiar with or having expertise in cold and in high-altitude physiology, energetics, macronutrient and micronutrient requirements, ingestive behavior, psychology, and military rations. In addition, military commanders familiar with working and training personnel in the cold and at high altitudes gave presentations and actively participated in the discussions. The invited speakers discussed their presentations with committee members at the workshop and submitted the content of their verbal presentations as written reports. The committee met after the workshop to discuss the issues raised and the information provided. The CMNR later reviewed the workshop presentations and drew on its collective expertise and the scientific literature to develop the following summary, conclusions, and recommendations that are found in the two chapters in Part I. In writing the first two chapters of this report, the CMNR has used the operational terminology included in Table 1-2.
MILITARY RESEARCH, COMMAND ISSUES, AND RATIONS FOR COLD AND FOR HIGH-ALTITUDE ENVIRONMENTS
The initial presentations at the workshop and the resulting chapters (3 though 6) in Part II of this report present a background for understanding military nutrition issues in the cold and at high altitudes.
The influence of cold and high altitudes on nutritional needs of the soldier has been a topic of interest to the military for many years. In his introduction COL Askew reviews the previous cold- and high-altitude intramural research activities of the Army, research sponsored by Army grants to academic institutions, and military-sponsored workshops or conferences (see Chapter 3 in this volume). COL Askew indicates that early work on cold and on high-altitude physiology and nutrition was typically a collaborative effort between military and civilian scientists. Since the 1970s, the overall extramural research activity supported by the military has significantly decreased, and specific research on nutritional needs in environmental extremes has been conducted largely within military research facilities.
TABLE 1-2 Terms Used in This Report
|
Acclimation |
Adaptive changes to an environment under controlled conditions, such as an environmental chamber (indoors/in the laboratory). |
|
Acclimatization |
Adaptive changes that occur due to exposure to a natural environment (outdoors/in the field). |
|
Altitude Designations |
|
|
At high altitudes |
General term to represent altitudes of 5,280 ft (1,609 m) or more above sea level. |
|
Moderately high altitudes |
8,000 to 11,000 ft (2,438 to 3,353 m). |
|
High altitudes |
12,000 to 18,000 ft (3,658 to 5,486 m). |
|
Extremely high altitudes |
Over 18,000 ft (5,486 m) (above which acclimatization is difficult). |
|
Cold |
Temperature range within which human body has difficulty functioning. 30°F to -30°F (-1°C to -34°C). |
|
Diuresis |
Excretion of urine; commonly denotes transient production of unusually large volumes of urine. |
|
Hypothermia* |
Core body temperature significantly below 95° F (35°C). |
|
|
Mild: Body temperature of 89.6°F to 95°F (32°C to 35°C) |
|
|
Moderate: Body temperature of 82.4°F to 89.6°F (28°C to 32°C). |
|
|
Severe: Body temperature of less than 82.4°F (28°C). |
|
Hypoxia |
Below normal levels of oxygen in arterial blood or tissue, short of anoxia. |
|
Hypohydration |
Decrease in body fluids equivalent to a loss of 1% body mass or more. |
|
SOURCE: Granberg (1991). |
|
Clothing, equipment, state of mind, leadership, physical conditioning, mental attitude, preparation, and nutrition are considered by COL Russell W. Schumacher, Jr. in relation to success in cold and in high-altitude training and operations (see Chapter 4 in this volume). COL Schumacher suggests that the single most significant contributor to successful operations in the cold is a positive attitude. In Chapter 4 he further reviews the necessary components of developing and maintaining positive attitudes in troops in these environmental extremes. He stresses the need for unit commanders to have realistic performance expectations of their troops in the cold and at high altitudes and concludes that daily effort must be put forth to attain and maintain positive troop morale in environmental extremes.
Military operational rations are the principal source of nutrients provided for the soldier in military operations in all environments. Therefore as
background for the report, a review of current rations specified for use in cold environments and the systems for preparation and use of field rations are summarized by LTC Nancy King and CW4 Thomas J. Lange (see Chapters 5 and 6 in this volume; see also IOM, 1995a). A modified table from Chapter 5 listing the nutrient contents of rations for cold-weather use has been reproduced here for clarity (Table 1-3).
The principal ration for group feeding in military field operations currently is the Tray Pack (T Ration). The T Ration is ready-to-heat and -serve, and is provided in low-profile, rectangular metal cans that can be heated quickly in hot water baths. This ration is described in more detail in Chapter 5. The standard T Ration is augmented with a cold-weather supplement module to provide 1,000 kcal per meal extra energy for cold environments. This Arctic T (T Ration supplemented with the cold-weather module) provides approximately 2,400 kcal per meal.
Frequently military missions do not permit group feeding, and individually packaged rations must be provided. The basic individually packaged ration is the Meal, Ready-to-Eat (MRE). The general composition of this ration is discussed in Chapter 5. In cold environments the basic three-ration per day provision is augmented with an additional fourth MRE or an energy supplement providing extra kcal. While the MRE can be consumed cold, individual ration heaters are provided since hot rations are more acceptable to soldiers in a cold environment.
The Ration, Cold Weather (RCW) is dehydrated and can be reconstituted with hot or cold water, or consumed dry. This ration was developed to meet some of the special needs for operating in arctic conditions. The specifics of the ration are discussed in Chapter 5, along with those of another more specialized food packet, the Long-Range Patrol, Improved (LRP I).
CW4 Lange (see Chapter 6 in this volume) summarizes some of the problems of feeding soldiers in the cold. He also discusses the issues of specialized equipment design that have been used to address the arctic and high-altitude conditions that present a very harsh environment for feeding the individual soldier. Problems of sheltering people and equipment as well as food preparation in severely cold and windy conditions are unique. These problems have required the development or improvement of mobile equipment that can function properly in such environments. Examples of these include the Mobile Kitchen Trailer and Kitchen Company Level Field Feeding equipment. These developments are important in providing food to sustain the military effectiveness of the soldier and the unit. Chapters 3 through 6 indicate the need for close coordination between the ration developer and troop support activities to ensure continued improvement in the quality and delivery of nutritionally adequate foods to soldiers operating in these environmental extremes.
THE COLD ENVIRONMENT
PHYSIOLOGICAL CHANGES IN THE COLD
Basic Physiology of Cold Exposure
When exposed to cold environments, the body loses heat through both convective and conductive heat transfer mechanisms. Heat losses are greater if the body is exposed to cold water than to cold air due to the greater heat transfer capacity of water (Gonzalez, 1988). As detailed by Andrew J. Young and colleagues (see Chapter 7 in this volume), the body possesses mechanisms to help maintain core temperature during cold exposure and to reduce heat loss, as well as to restore heat that has been lost. The mechanisms collectively are called thermoregulation.
Peripheral Vasoconstriction and Vasodilation
The principal mechanism to reduce heat loss is the neurologically induced constriction of vessels in the skin and extremities. This response diminishes heat transfer from the body core to the surfaces. As a result, body surface temperatures fall rapidly upon exposure to cold (Veicsteinas et al., 1982). These low skin and extremity temperatures can result in cold injuries, especially to the hands and fingers. A second mechanism, cold-induced vasodilation (CIVD), somewhat offsets the harmful effects of falling skin temperatures. With exposure to cold, vasoconstriction reduces skin temperatures, but then CIVD allows the temperatures to rise within about 10 minutes (Lewis, 1930). Over time the alternation of these two vascular responses results in a rhythmic (or cyclic) rise and fall of skin temperatures (Lewis, 1930).
Metabolic Heat Production
Heat production occurs as the result of voluntary muscular work, by involuntary (central nervous system [CNS]-induced) shivering, or by a combination of both mechanisms. Humans have no unique nonshivering, thermogenic mechanisms for responding to cold (Toner and McArdle, 1988). Nevertheless, as pointed out by Ira Jacobs (see Chapter 10 in this volume), every cellular metabolic process within the body has, as its byproduct, the production of heat. Even the vasoconstrictive activity of vessel walls produces some heat.
TABLE 1-3 Approximate Nutritional Content of Rations Used in Cold-Weather Operations
|
MRDA |
T Ration* (3 meals) |
MRE† (4 meals) |
RCW (1 ration) |
LRP I (3 meals) |
||
|
Nutrient |
Men |
Women |
||||
|
Energy, kcal |
4,500 |
3,500 |
4,323‡ |
5,392 |
4,567 |
4,668 |
|
Protein, g |
100 |
80 |
181 |
197 |
94 |
179 |
|
Carbohydrate, g |
_§ |
_§ |
582 |
669 |
682 |
586 |
|
Fat, g |
_|| |
_|| |
141 |
215 |
163 |
179 |
|
Vitamin A, IU |
5,000 |
4,000 |
15,153 |
16,880 |
8,022 |
8,133# |
|
Vitamin E, mg TE |
10 |
8 |
15# |
22# |
21 |
13# |
|
Vitamin C, mg |
60 |
60 |
208 |
408 |
329 |
183 |
|
Thiamin, mg |
1.6 |
1.2 |
3.5 |
10.8 |
5.7 |
3.7 |
|
Riboflavin, mg |
1.9 |
1.4 |
3.5 |
4.3 |
2.6 |
2.8 |
|
Niacin, mg NE |
21 |
16 |
42 |
52 |
31 |
541 |
|
Vitamin B6, mg |
2.2 |
2.0 |
2.2 |
7.6 |
3.9# |
2.7 |
|
Folacin, µg |
400 |
400 |
339 |
292# |
141# |
132# |
|
Vitamin B12, µg |
3 |
3.0 |
5.3# |
3.5# |
0.8# |
1.8# |
|
Calcium, mg |
800–1,200 |
800–1,200 |
1,687 |
2,052 |
1,379 |
1,149 |
|
Phosphorus, mg |
800–1,200 |
800–1,200 |
2,761 |
3,184 |
2,168 |
2,352 |
|
MRDA |
T Ration* (3 meals) |
MRE† (4 meals) |
RCW (1 ration) |
LRP I (3 meals) |
||
|
Nutrient |
Men |
Women |
||||
|
Iron, mg |
10–18 |
18 |
29 |
24 |
19 |
24 |
|
Sodium, mg |
–** |
–** |
7,374 |
7,292 |
4,720 |
7,740 |
|
Potassium, mg |
_†† |
_†† |
5,626 |
5,424 |
4,084 |
4,419 |
|
Magnesium, mg |
350–400 |
300 |
523 |
556 |
592 |
489 |
|
Zinc, mg |
15 |
15 |
20 |
13# |
11# |
9# |
|
Cholesterol, mg |
_§ |
_§ |
484# |
476# |
183# |
174# |
|
NOTE: MRDA, Military Recommended Dietary Allowances for moderately active military personnel ages 17 to 50 years old operating in cold weather; T Ration, Tray Pack Ration without cold-weather supplement (FY1992); MRE, Meal, Ready-to-Eat (version XII); RCW, Ration, Cold Weather; LRP I, Long-Range Patrol, Improved. * The T Ration cold-weather supplement provides 148 g carbohydrate (53 percent), 29 g protein (11 percent), and 45 g fat (36 percent of total kcal) for a total of 1,110 kcal (Personal communication, M. S. Harrington, U.S. Army Research Institute of Environmental Medicine, Natick, Mass., February 1996). † The MRE is reformulated annually. Values provided are for version XII. The version in current use is XVI. The relative proportions of energy provided by protein, carbohydrate, and fat vary by no more than 1 percent from year to year (Personal communication, L. D. Sherman, U.S. Army Research Institute of Environmental Medicine, Natick, Mass., February 1996). ‡ Cold-weather supplement adds approximately 1,000 kcal. § No MRDA established. || Should not exceed 35 percent of total energy intake. # Data missing (more than 50 percent) or inaccurate. ** No MRDA established. The safe and adequate levels published in the RDA are considered to be unattainable within military foodservice systems. An average of 5,500 mg for men and 4,100 mg for women is the target. †† NO MRDA established. The safe range is 1,875–5,625 mg, based on AR 40–25 (1985). SOURCE: Adapted from AR 40–25 (1985). Record of nutritive values for each ration. |
||||||
Skeletal muscle contractions, either during voluntary exercise or involuntary shivering, are the major source of the metabolic heat produced to protect against cold stress (Horvath, 1981). Heat production parallels an increase in oxygen uptake, the magnitude of which depends on the proportion of the muscle mass engaged in shivering or work and the duration and severity of work being done (Young et al., 1986a). Shivering alone can cause only a fourfold increase over basal rates of heat production, and even the greatest increases in heat production because of shivering alone are less than one quarter of a muscle's maximum contractile activity (Horvath, 1981).
The thermogenic response to voluntary exercise differs with the form of exercise (Toner and McArdle, 1988). Arm-only exercise causes a greater loss of body heat than does leg-only exercise (when both yield the same magnitude of heat production per unit). As a result, leg-only exercise is more efficient in maintaining body core temperatures (Toner et al., 1984). If voluntary exercise does not maintain body core temperatures during cold exposure, involuntary shivering responses are initiated, and heat production then may result from both forms of muscular work. Maximal energy expenditure by skeletal muscles may be reduced by cold exposure, if temperatures decline in muscle, body core, and/or blood. A fall in the temperature of blood reduces its delivery of oxygen to body tissues, because of temperature effects on the oxyhemoglobin dissociation curve (Young, 1990).
Cardiac Responses
The increase in oxygen uptake during shivering thermogenesis is also accompanied by an increase in cardiac output (Muza et al., 1988). This increase is due almost entirely to an increase in stroke volume, which appears to be the result of the increased central blood volume that is associated with cold-induced peripheral vasoconstriction. Resting heart rate remains unchanged (Muza et al., 1988).
Effect of Gender
Almost all studies of physiological responses to cold stress have been conducted in men. However, there is no evidence to suggest that basic mechanisms for peripheral vasoconstriction, cardiovascular responsiveness, and metabolic heat production in the cold are different in men and women. Metabolic changes during the menstrual cycle have not been studied during cold exposure, but basal body temperature is known to vary in response to hormone secretions (Stephenson and Kolka, 1993). Differences in body composition also may play a role, with the higher content of body fat in women and their smaller body surface areas providing some degree of
protection from heat loss. Current knowledge of physiological responses to cold is largely based on studies of healthy young adult males. With the growing numbers of women in the military, they should not be neglected in future studies (IOM, 1995b).
Effect of Age
As reviewed by Young et al. (see Chapter 7 in this volume), general medical knowledge, backed by older physiological studies, suggests that older individuals may respond poorly to severe cold stress. The typical loss of muscle mass that accompanies the aging process undoubtedly plays a role by reducing the capacity for production of heat from metabolic processes. On the other hand, the accumulation of body fat with aging may provide additional protection against heat loss in mid- to late mid-life, but this protection is most likely lost or may change as aging continues. Extremely old individuals are often characterized by a gradual loss of body fat, especially subcutaneous fat. The increase in body surface area in comparison to body mass combines to reduce the mechanisms used to protect against heat loss (Young, 1991). Similar problems would arise in malnourished subjects who have lost both body fat and muscle mass.
Other Factors
Cold acclimatization can occur in humans but it is minimal. Probably the most important modifying factor on the thermoregulatory response to cold is the individual's endowment of subcutaneous fat since fat reduces thermal conductance from the core to body surfaces (Toner and McArdle, 1988). Physical fitness has mixed effects: the fittest individuals show the greatest heat production, but they are also the leanest, and that combined with their higher skin temperatures (from increased heat production) causes them to lose heat more quickly. Older individuals tend to maintain lower body temperatures (Mathew et al., 1986) and have less efficient vasoconstrictive mechanisms, so they are at greater risk for heat loss in cold environments. Generalized malnutrition may also impair thermoregulation. Severe losses of body weight associated with the complex stresses of prolonged military operations could also complicate the normal physiological responses to cold. Emphasis on maintaining an adequate intake of operational rations to prevent excessive weight loss in severe operational environments is important to sustain normal physiological responses to cold (IOM, 1995a). A discussion of nutrient requirements in the cold begins on page 15.
The most important modifying factors for thermoregulation, however, are the behavioral strategies employed in cold environments. Humans don warm,
protective clothing, seek shelter whenever possible, and create or move to warmer environments.
Central Nervous System Function and Sleep
The Role of the Central Nervous System and Sleep during Cold Stress
Central nervous system (CNS) responses are of fundamental importance in body responses to cold stress. Hot and cold sensors in skin, body tissues, and the brain itself continually send signals via afferent nerves to the CNS for monitoring and response, if needed.
As a result, the CNS produces and responds to numerous neurotransmitters, such as catecholamines and serotonin. Both the temperature regulating and sleep regulating functions of the CNS respond to similar neurochemical stimuli. Further, sleep regulating functions of the CNS appear to be linked to those employed in temperature regulation (for discussion, see R. S. Pozos et al., Chapter 8 in this volume).
Stages of Sleep
Sleep consists of a series of repeating cycles of physical and brain wave activity. The sleep cycle may be divided into two main phases. The first phase, referred to as nonrapid eye movement sleep (NREM sleep), can be subdivided further into 4 stages. These are Stage 1, or the transition from the waking to the sleeping state; Stage 2, which is marked by a change in the electroencephalographic (EEG) pattern and the true beginning of NREM sleep; Stage 3, characterized by the onset of Slow Wave (or delta) Sleep (SWS), so-called because of the pattern of EEG activity; and Stage 4 in which SWS continues and begins to display hypersynchronization (Gregory, 1987). The second, deeper, phase of sleep is called REM or Paradoxical Sleep, and is characterized by rapid eye movement, a paradoxical increase in brain wave activity to the level of the waking state, and an increase in physical activity. All stages of sleep are considered necessary for maintenance of normal bodily and mental functions. While NREM sleep ordinarily precedes REM sleep, a sleep-deprived individual can progress almost immediately into REM sleep (Kandel et al., 1991). For this discussion of cold stress, it is important to note that the CNS fails to maintain its temperature regulating functions during REM sleep (Jennings et al., 1993).
Interrelation of Sleep and Temperature Regulation
During REM sleep, neither the cold-sensing nor the warm-sensing neurons fire: the CNS basically shuts down with respect to temperature regulation. In slow wave, NREM sleep, some information on temperature sensation is still received. Sleeping animals exposed to cold will still shiver during NREM sleep, but cease shivering as sleep deepens. Extreme degrees of cold or heat will cause sleeping animals to rouse.
Because temperature regulation ceases during deep REM sleep, a decrease in body temperature usually occurs. This phenomenon appears similar to changes seen in animals in deep hibernation. The sleep-induced decrease in body temperatures spare metabolic activity, and thereby reduce nutritional needs (Jennings et al., 1993).
Sleep and Temperature Regulation in Humans
In humans, the sleep-induced fall in body temperature is reversed on, or shortly before, waking. However, if a sleeping person (in either REM or NREM sleep) is aroused momentarily, core temperatures will fall further each time sleep is interrupted. Prior exercise, prior food intake, and the menstrual cycle all influence core body temperatures during sleep. Giving meals on a precise time schedule appears to help synchronize the temperature regulating clock. On the other hand, if the temperature regulating and sleep inducing clocks become desynchronized, as during military operations for example, appetite and food intake may be adversely affected (Jennings et al., 1993).
In summary, the neural mechanisms involved in sleep regulation appear to interact with those that regulate body temperature. The ability of the CNS to sense and respond to incoming information of a thermal nature is affected by both time of day and stage of sleep. Hence, during REM sleep, the CNS thermoregulatory response is dampened, resulting in a decrease in body temperature similar to that observed in hibernating animals. Extremes in temperature cause arousal in animals. In humans, repeated arousal results in a progressive decrease in core body temperature during subsequent sleep. Temperature in the sleeping human is also influenced by nutritional status, physical activity, hormones, and sleep schedule.
Thermoregulation and Physical Performance
If humans can regulate their core body temperatures properly during periods of physical work, their performance should not be significantly impaired. On the other hand, when physiological temperature-regulating responses cannot cope with environmental (or other) stressors, performance
will decline. Depressed core temperatures can reduce maximal oxygen uptake and maximal cardiac output, and interfere with muscle energy metabolism by accelerating muscle glycolysis and lactate production. Differences in body size, configuration, and composition also influence the ability to maintain body temperatures during stress (see Young et al., Chapter 7 in this volume). Humans can use such external factors as shelter and clothing to help maintain core temperatures.
Drug-Induced Delay of Hypothermia
While most of this report deals with nutritional and physiological aspects of cold exposure, André L. Vallerand (see Chapter 15 in this volume) presents a useful discussion of drug-mediated delay in hypothermia during cold exposure. Earlier work in animals had demonstrated that a variety of drugs can delay the onset of hypothermia, but the relevance to humans was not clear (LeBlanc, 1975). For example, it was well known that dinitrophenol uncouples oxidative phosphorylation and increases substrate oxidation and heat production (Sellers, 1972). However, observations of side effects in obese subjects precluded use of dinitrophenol in humans (Hall et al., 1948).
Recent research by Vallerand and his colleagues (Vallerand et al., 1993) has centered on the evaluation of a commercially available, theobromine-containing ''sports bar" purported to delay hypothermia during cold exposure in humans (see discussion in Chapter 15 in this volume). Comparison of the product with either an isocaloric mixture of carbohydrates or with an unspecified placebo revealed no significant differences in either rectal temperature or body heat debt of cold-exposed volunteers.
The inability to confirm claims made for the commercial sports bar prompted Vallerand and colleagues to study combinations of β-adrenergic agonists with methylxanthines. When compared to a placebo, a mixture of ephedrine (1 mg/kg) and caffeine (2.5 mg/kg) significantly increased metabolic heat production by 19 percent in cold exposed humans (Vallerand et al., 1989). The increase in heat production was derived from a large increase in whole body carbohydrate oxidation. The treatment also reduced the fall in rectal and skin temperature. Additional studies confirmed the value of mixtures of ephedrine with caffeine or theophylline in increasing heat production, decreasing heat debt, and reducing the lowering of body temperature in cold exposed individuals (Astrup et al., 1985, 1992; Dulloo and Miller, 1986; Dulloo et al., 1990).
These interesting results warrant additional studies to define further the benefits and disadvantages of the proposed treatment in improving the cold tolerance of human subjects, including further refinement of the most effective treatment modality. These initial results have significant promise for providing
protection to individuals during cold exposure and therefore have potential military application in specific settings.
CHANGES IN NUTRIENT REQUIREMENTS FOR COLD ENVIRONMENTS
Fluid Balance
Body fluid balance is normally held within a fairly narrow range by a wide range of control measures. Exposure to cold stress, however, typically leads to dehydration, with a cold-induced diuresis (CID) as a major, long recognized contributing factor that is accompanied by reduced blood and plasma volumes (see review by Freund and Sawka, Chapter 9 in this volume). Other contributing causes to dehydration in the cold include losses of body water through respiration and through sweating, as well as through a diminished intake of fluids.
Mechanisms of Cold-Induced Diuresis
The mechanisms of origin of cold-induced diuresis (CID) are not yet entirely clear. It is known that CID can be blocked by administration of antidiuretic hormone (ADH or vasopressin) (Bader et al., 1952; Eliot et al., 1949). Despite early evidence for lowered concentrations of this hormone in plasma of individuals exposed to cold, subsequent research failed to confirm its suspected etiologic role in CID (Lennquist et al., 1974). Later, cold-induced increases in blood pressure, leading to a diminished renal tubular reabsorption of sodium and water became a popular mechanistic explanation for CID (Wallenberg and Granberg, 1976). More recently, studies in humans have shown that repeated immersions in cold water produced an equal diuretic response each time; however, the hypertensive component was lost with the acclimation to cold water immersion (Muza et al., 1988; Young et al., 1987). Currently, the movement of water to the body core caused by cold-induced peripheral vasoconstriction is the most attractive explanation for CID. Hydration status and body posture (Wallenberg and Granberg, 1976) also appear to be confounding factors.
Other Causes of Cold-Induced Losses of Body Water
Losses of respiratory water may also contribute to cold-induced dehydration. Water vapor pressure of cold air is considerably less than under thermoneutral conditions, so additional water can be lost when exhaling fully
saturated warm alveolar air (Brebbia et al., 1957; Mitchell et al., 1972). Exercise-induced hyperventilation also will add to the amounts of water being lost via expired air. In fact, exercise-induced respiratory water losses are probably greater than cold-induced losses.
Exercise-induced sweating is another source of water loss, and is obviously related to the severity and duration of exercise performed as well as the types of clothing worn (Gonzalez et al., 1988; see Freund and Sawka, Chapter 9 in this volume). Some military clothing systems allow for little evaporation, causing large amounts of water from sweating to accumulate near the skin. Such water accumulation can pose additional problems in cold environments.
Performance Decrements Caused by Cold-Induced Dehydration
Although many studies have focused on dehydration in hot environments, few studies have investigated effects of hypohydration on performance in extremely cold conditions. The contributions of hypohydration to observed, cold-induced decrements in maximal aerobic power (![]() o2max), muscular strength and endurance, and/or manual dexterity are also not well understood.
o2max), muscular strength and endurance, and/or manual dexterity are also not well understood. ![]() o2max and physical work capacity are reduced by hypohydration (Sawka and Pandolf, 1990). Small amounts of dehydration can produce alterations in thermal regulation, and higher ratings of perceived exertion during exercise tests (Greenleaf and Harrison, 1986; Montain and Coyle, 1992; Sawka, 1992). Cold-induced dehydration also is accompanied by changes in disposition, leading to sullenness, loss of appetite, breakdown in military discipline, failing physical exertion, and finally exhaustion (Orth, 1949). Such dehydration, therefore, may also contribute to cold injury.
o2max and physical work capacity are reduced by hypohydration (Sawka and Pandolf, 1990). Small amounts of dehydration can produce alterations in thermal regulation, and higher ratings of perceived exertion during exercise tests (Greenleaf and Harrison, 1986; Montain and Coyle, 1992; Sawka, 1992). Cold-induced dehydration also is accompanied by changes in disposition, leading to sullenness, loss of appetite, breakdown in military discipline, failing physical exertion, and finally exhaustion (Orth, 1949). Such dehydration, therefore, may also contribute to cold injury.
In summary, in cold environments, dehydration compounded by CID is a significant factor that is often not given necessary consideration. The mechanisms of CID are not well understood, but overall hydration status appears to play a role. Exercise-induced respiratory water losses and sweating are additional contributors to dehydration in the cold. The changes in performance, appetite, and emotions that are well documented with heat-related dehydration also occur in cold-induced dehydration and can lead to cold injury.
The obvious countermeasure to dehydration is to drink fluids, but this practice is not always possible. Major problems can arise from the logistical constraints in delivery of drinking fluids during military operations in cold environments. In cold weather, fluids for drinking will freeze unless they are held in warm environments or have their solute concentration raised to lower the freezing point. The logistical problem would not be altered appreciably by attempting to meet fluid requirements by melting snow or ice due to the additional weight of heat-producing units. Hyperhydration before cold exposure is a useful strategy if cold stress will be of short duration.
Macronutrients
Energy Sources
The energy requirements of an individual in the cold are discussed in Chapters 11 and 12 in this volume by Peter J. H. Jones and Ian K. K. Lee and by Jacques A. LeBlanc, respectively. Total energy requirement is the sum of (1) the energy expended to maintain body functions (basal energy needs1), (2) the energy expended in processing meals (the thermic effect of food), and (3) the energy expended by physical activities (see Jones and Lee, Chapter 11 in this volume). Exposure to cold environments has been shown to increase the basal energy needs relative to the basal energy requirements measured under thermoneutral conditions (BMR1), which has been attributed to the increased energy demands of thermoregulation in the cold. In addition, activity-related energy expenditure is increased by the cold, due to the increased difficulty of locomotion over snow-covered terrain and the hobbling effect of multi-layered clothing, heavy boots, and packs filled with cold-weather gear.
Until recently, attempts to determine the magnitude of the increase in energy requirements in the cold focused on estimation of food intake, under the assumption that in healthy, weight-stable individuals, intake represents need (Kark et al., 1948).
Studies of energy needs of troops living in cold environments, based on food intake, have suggested that energy needs range from 3,100 to 3,900 kcal/d, (41 to 52 kcal/kg/d for a 75 kg man) depending on the activity performed and the extent of cold exposure (both ambient temperature and duration of exposure) (King et al., 1993; LeBlanc, 1957; Rodahl, 1954). More recent studies in which measures of energy expenditure (based on the doubly labeled water [DLW] method) rather than intake were used as a means of estimating energy need indicate that energy requirements in the cold may vary from 3,400 kcal/d to 4,300 kcal/d (45 to 57 kcal/kg/d for a 75 kg man), depending again on the degree of exposure to the external environment and activity levels (DeLany et al., 1989; Hoyt et al., 1991; King et al., 1993). The difference in estimates of energy requirement as determined by the DLW method compared to food intake estimates may reflect the frequently encountered bias of underreporting in self-reports of food intake found in other research studies (Schoeller, 1990; see Jones and Lee, Chapter 11 in this volume).
Some disagreement exists among data based on self-reported food intake concerning the adequacy of energy intake by military personnel engaged in cold-weather field exercises. While data reviewed by Baker-Fulco (1995) suggests evidence of chronic underconsumption of energy and loss of weight in the cold, evidence presented by LeBlanc (see Chapter 12 in this volume) show that soldiers deployed to cold environments as well as members of arctic expeditions tended to gain weight, at least initially. Enhanced appetite may account for the 1 kg/month gain in weight observed during some studies of subjects experiencing prolonged stays in Antarctica (Milan and Rodahl, 1961). The estimates of energy intake reported by Baker-Fulco as well as by LeBlanc were based on dietary records, which, as mentioned above, tend to underreport caloric intake. In the case of the studies reviewed by Baker-Fulco, the reported caloric deficits were at times too large to account for the reported weight losses. In neither case was it possible to ascertain the activity levels of the subjects. The answer to the question of whether undernutrition is a problem in the cold may hinge upon the activity levels of the personnel in question as well as the amount of rations consumed.
In summary, energy requirements of 41 to 57 kcal/kg/d have been estimated for troops operating under conditions of arctic cold. The Military Recommended Dietary Allowance (MRDA) for energy used in rations designed for consumption in the cold is 4,500 kcal/d (60 kcal/kg/d for a 75 kg man) (AR 40-25, 1985). These present policies on nutrient density for energy needs of troops in the cold thus appear to be sufficient, even when not all the rations provided are consumed.
Determination of the optimal macronutrient ratio. Determination of the optimal macronutrient ratio for provision of energy in the cold must take into consideration a number of factors. These include the caloric density of fat as compared to carbohydrate (or protein); the enhancement of thermogenesis associated with the digestion, absorption, and storage of a particular nutrient (thermic effect of food or TEF); the preferential metabolism in the cold of one nutrient over another; and the preference of a particular nutrient in the diet.
- Relative caloric density and TEF of energy sources. In terms of caloric density, fat provides more than twice the amount of energy per unit mass compared to carbohydrate or protein, so that a ration providing a specific level of calories but higher in fat would be lighter, and easier to transport. Early concepts, largely based on the dietary practices of primitive Eskimos, suggested that an Eskimo-like diet, composed of half fat and half protein, was necessary to survive in chronic conditions of extreme cold (Hoygarrd, 1941). These concepts were compatible with scientific knowledge that high fat intake provides dietary energy with the greatest caloric density. While a high fat ration would have the advantage of light weight and easy portability, a fat-based
- diet has a number of disadvantages in the field and particularly in the cold. A sudden change to a high fat diet has the potential to cause adverse gastric (heartburn) and metabolic effects, the symptoms of which can be difficult to distinguish from a heart attack (IOM, 1992). An additional factor that must be considered in cold environments includes the TEF, which is lower for fat than for either carbohydrates or protein.
- Preferential metabolism of one nutrient over another. The question of whether one macronutrient is preferentially metabolized over another to satisfy energy needs in the cold has been addressed by several groups of investigators. As discussed above, the increase in energy requirements in the cold is attributable to thermoregulation and to increased physical activity. In Chapter 7 of this volume, Young and colleagues review the energy requirements for thermogenesis, which occurs as a result of increased voluntary muscular activity, or in the absence of voluntary activity, involuntary muscle activity (shivering). For over 60 years, evidence has pointed to voluntary physical activity in the cold as well as in thermoneutral conditions being fueled preferentially by carbohydrate, which provides 8 percent more energy per unit of oxygen consumed than does fat (Lusk, 1928). Adequate stores of muscle glycogen are required for provision of energy during periods of intense, prolonged exercise. At a workshop held by the CMNR in 1987 to consider the possible benefits of a calorie-dense ration, Gollnick (Unpublished paper, "Energy production during exercise; influence of diet and training," P. D. Gollnick, Washington State University, Pullman, Wash., 1987) reported the average muscle glycogen content of an 80 kg man to be 480 g (Gollnick 1985) and cited evidence from a study by Edwards and coworkers (1932) reporting that during 6 hours of moderately intense exercise, approximately 415 g carbohydrate was utilized. The ability of muscles to replenish depleted glycogen stores is a function of dietary carbohydrate intake. Also cited by Gollnick was a study by McDougall and colleagues (1977) which showed that, following exercise-induced muscle-glycogen depletion, 80 percent repletion was achieved in 24 hours by feeding either 625 g carbohydrate or a diet containing 50 percent (378 g) carbohydrate. Thus, it has been estimated (IOM, 1992) that a minimum of 400 g of carbohydrate is required per day for glycogen resynthesis. Underconsumption of carbohydrate leads to a depletion of reserves which necessitates reliance upon body fat stores for fuel (Costill, 1988). Although it has been estimated that a typical person's reserve of fat energy is sufficient to meet a 2000 kcal/d energy deficit for over a month, the switch to fat as a primary metabolic fuel (without an adequate period for adaptation) results in decreased physical (and mental) performance (Phinney et al., 1983) and loss of lean body mass (Askew et al., 1987). Thus, while the amount of carbohydrate that should be provided has not been precisely determined, it is the consensus of the CMNR that a minimum of 400 g should be provided. Further research is necessary to define more precisely the
- carbohydrate intake required to replace glycogen at various exercise intensities in cold (and in high-altitude) environments.
The amount of energy required for shivering is proportional to the degree of cold exposure due to changes in intensity with need for heat generation. According to Toner and McArdle (1988), this can contribute to an increase in basal energy requirement of two- to fivefold over the resting metabolic rate in thermoneutral conditions (RMR). A study of men briefly exposed to the cold while at rest, showed an increase in metabolic rate of 2.5-fold over that of RMR. Carbohydrate oxidation rose sixfold while fat oxidation rose by less than twofold (Vallerand and Jacobs, 1989). These authors also reported that in the cold, 51 percent of calories were derived from carbohydrate and 39 percent from fat. (Energy from protein catabolism plays a relatively small role.) This suggests that insofar as shivering contributes to the cold-related energy requirements, these requirements are met by both carbohydrate and fat, with a strong preferential utilization of carbohydrate.
The source of carbohydrate utilized by shivering muscle is discussed by both Young et al. and Jacobs in Chapters 7 and 10 in this volume. The question of whether shivering thermogenesis, like voluntary muscle activity, is dependent upon glucose derived from glycogen and can be enhanced by increasing dietary carbohydrate has attracted a great deal of interest since the discovery of the crucial role of muscle glycogen in voluntary muscle activity and the effect of dietary carbohydrate loading in improving physical performance. Contradictory findings have emerged concerning the contribution of blood glucose versus muscle glycogen stores as energy sources for involuntary shivering (Jacobs, 1993; Martineau and Jacobs, 1989; Young et al., 1989).
Young and colleagues contend that muscle glycogen stores do not seem to be a particularly important substrate for shivering work (see Chapter 7 in this volume for further review). They reported on their study in which muscle biopsies were obtained from volunteers whose muscle glycogen stores had been purposefully expanded or depleted prior to cold exposure. No differences were found in muscle glycogen utilization or thermogenesis during cold-induced shivering in nonexercising volunteers, despite the pre-exposure differences in their stores of muscle glycogen (Young et al., 1989).
In contrast, Jacobs (see Chapter 10 in this volume) reports on studies with a virtually identical experimental design, which showed that the muscular work of shivering in cold water-exposed, nonexercising volunteers was fueled, in part, by muscle glycogen (Martineau and Jacobs, 1988, 1989). These data were in agreement with findings in experimental animals. In addition, the subjects in Jacobs' study who had depleted pre-exposure stores of muscle glycogen showed a small but significant increase in the rate of body cooling compared to subjects with normal or high glycogen stores. Both Young and Jacobs have hypothesized that the difference in results may have stemmed from Jacobs' selection of extremely lean subjects, while Young et al. had used subjects with
more body fat; however, no mechanism has been postulated to explain how this might have brought about the difference in results.
Studies that have been completed since the workshop show that carbohydrate supplementation during brief periods of cold exposure has no influence on cold-induced (shivering) thermogenesis, suggesting that at least in the short-term, energy-substrate mobilization is not a limiting factor in thermogenesis (Glickman-Weiss et al., 1994; Vallerand et al., 1993). An additional study has shown that during brief periods of cold exposure, blood glucose is the primary source of fuel for shivering, with smaller contributions from glycogen and lactate (Vallerand et al., 1995).
In summary, energy is needed in the cold to fuel both voluntary physical activity and involuntary shivering. As in thermoneutral conditions, voluntary muscular activity is fueled primarily by carbohydrate, and at high levels of activity, a minimum of 400 g carbohydrate is recommended per day to replace depleted glycogen stores. The energy requirements of shivering are supplied primarily by carbohydrate, with fat contributing to a lesser degree. It would appear that the carbohydrate utilized as fuel for shivering muscle derives from both blood glucose and the glycogen stored in the muscle itself; however, further investigations with longer cold-exposures may be warranted. The current recommendation of providing 4,600 kcal/d for troops operating in the cold appears to be sufficient to meet the needs for carbohydrate for shivering and voluntary muscle activity.
- Preferential macronutrient distribution. Preference for macronutrient distribution of energy does not appear to change in the cold; the usually chosen distribution is 13 to 16 percent protein, 37 to 38 percent fat, and 48 to 49 percent carbohydrate (Hoyt et al., 1991; King et al., 1993; Swain et al., 1949), which is essentially the same as the choices made under conditions of moderate ambient temperature (Swain et al., 1949) and does not substantiate information about dietary practices of the early Eskimos (which were probably based upon the foods available rather than being an adaptation to energy needs in the cold). The amount of fat being consumed by troops studied under arctic conditions is within the range currently consumed by a large portion of the American population, with the most recent review placing the average intake by young Americans at 34 percent dietary fat (CDC, 1994). While this level of dietary fat is higher than the current dietary recommendations for the general population, which call for a fat intake of no more than 30 percent of total calories (USDA, 1995), these recommendations do not take into consideration the significant increases in caloric requirements under circumstances that may be encountered in the cold.
In summary, there appears to be no change in the preference for one macronutrient over another in the cold. The fat content of the diet, which is higher than current dietary recommendations, may be justified by the higher activity level and circumstances encountered in the cold.
Protein
The protein requirements of individuals working in the cold are mentioned briefly in Chapters 11 and 12, by Jones and Lee and by LeBlanc, respectively. Jones and Lee cite an early study by Issekutz et al. (1962) that reported significant increases in urea production during full-day cold exposures. They interpreted this finding as an indication of an increased use of protein for energy in the cold. Other studies by Rodahl et al. (1962), Jones et al. (1993), and Vallerand and Jacobs (1989) failed to demonstrate any effects of brief cold exposure on fasting protein oxidation. Similarly there was no effect of prolonged cold exposure on fat free mass. In all studies however, dietary records were not maintained so protein intake was not measured.
The MRDAs do not include a higher protein allowance for cold weather (AR 40-25, 1985); the protein allowance of 100 g/d recommended for moderately active males in temperate climates is the same as that recommended for cold. In fact, since the recommended energy allowance is significantly higher for cold (4,500 kcal vs. 3,200 kcal), the percentage of calories to be contributed by protein is significantly lower (9 percent vs. 12.5 percent).
The nutrient contents of military rations employed in the cold are reviewed and compared by LTC King in Chapter 5. The protein content of the Ration, Cold Weather (RCW) (94 g protein per 4,500 kcal or 8 percent of energy intake) is significantly lower than that of the Meal, Ready to Eat (MRE) (197 g per 5,200 kcal or 15 percent of intake in 4 MREs). Thus, the protein content of the RCW is significantly closer to MRDA levels for the cold than is the recommended allotment of MREs. Comparison of the two rations in cold-weather field trials by Edwards et al. (1992) revealed inconsistent effects of the diets on measures of serum protein and albumin as well as blood urea nitrogen (BUN). In addition both groups underconsumed calories and protein and lost body weight, so it is difficult to draw conclusions about the adequacy of protein intake. The authors commented, however, that the protein content of an MRE plan is too high for cold weather consumption. This is because the increase in urea excretion that would result from metabolism of the extra protein would increase the requirement for water, and the availability of drinking water is often restricted in cold environments. The authors therefore recommended limiting protein intake to the level of the RCW. Based on early experiments by Keeton et al. (1946), Askew (1989) recommends a daily intake of 100 g of protein per 4,650 kcal as an optimal level for work in the cold.
The question of whether protein consumption increases during prolonged cold exposure has no definitive answer. While anecdotal evidence has suggested that Eskimos consume diets that derive approximately half of their calories from fat and the rest from protein (see Jones and Lee, Chapter 11 in this volume) (and soldiers participating in an 8-d cold-weather trial voluntarily increased consumption of foods high in protein when offered a mixed diet [Edwards et al., 1992]), several other studies reported no change in relative
protein consumption in the cold. Nevertheless, an increase in protein intake in the cold appears to have a beneficial thermic effect. The thermic effect of feeding (TEF) for protein is higher than that for both carbohydrates and fat, resulting in an increase in body warmth for the 5 to 6 hours following ingestion of a high protein meal (Jéquier, 1993). LeBlanc (see Chapter 12 in this volume) suggests that ingestion of protein late in the day may serve to increase warmth throughout the night and prevent cold-induced waking.
In summary, while there is no evidence for an increased requirement for protein in the cold, if an additional MRE were consumed, protein intake would increase. When water supplies are scarce, there is good reason to maintain protein intake at the MRDA level. The use of the lower protein RCW or supplementation of the MRE with primarily fat-and carbohydrate-containing supplements would be beneficial in minimizing the increase in protein in the face of scarce water supplies.
A protein snack prior to retiring to sleep could provide some benefit from the thermic effect of protein in cold environments.
Vitamins
The influence of cold exposure on the need for vitamins is reviewed by Robert D. Reynolds in Chapter 13 in this volume. Given the extended period of time required for a nutritionally-replete individual to develop vitamin A deficiency and the relatively short duration of most expeditions and field maneuvers, there appears to be little justification for increasing the recommended intake of vitamin A. Likewise, there appears to be little rationale for increasing the recommendations for vitamins D or K. Although Reynolds proposes that increased consumption of vitamin E could possibly increase the oxygen supply for such purposes as energy production, the scientific support for this hypothesis is limited to a few studies (see Chapter 13 in this volume).
Thiamin, niacin, riboflavin, and pantothenic acid play a central role in the production of sufficient energy for thermogenesis. However, there are no experimental data indicating that increased consumption of any of these water-soluble vitamins above MRDA levels (AR 40-25, 1985) (which are always based on energy intake) provides any benefit to the cold-exposed individual (see Reynolds, Chapter 13 in this volume). Therefore, the CMNR does not recommend an increase in the dietary intake of these nutrients beyond MRDA levels. Similarly, there appears to be little justification for increasing the recommendation for vitamin B6, vitamin B12, biotin, or folic acid. Although it has been proposed that vitamin C might play some role in maintaining core and body surface temperatures, the 45-yr old study on which this concept is based has never been confirmed (Thérien et al., 1949).
In summary, there are very few studies that have investigated the influence of vitamin supplementation on resistance to hypothermia. Therefore, there is
little evidence upon which to base recommendations to increase vitamin intake above MRDA levels to help cope with cold stress.
Minerals
Reynolds (see Chapter 13 in this volume) did not identify any scientific basis to justify increased dietary intakes of calcium, phosphorus, or magnesium beyond MRDA levels as a consequence of cold exposure.
The possible effect of micromineral deficiencies on thermoregulation in the cold is discussed by John L. Beard in Chapter 14 in this volume. Chronic deficiency of a number of different trace elements, including iron, zinc, or copper, may lead to defective thermoregulation (Lukaski and Smith, in press). Iron deficiency could be a concern because of its importance in maintaining core body temperature. However, there is no evidence at this time to indicate an increased requirement for iron in cold conditions. Thus, MRDA levels should be sufficient to prevent deficiency of this element.
Trauma and various types of stress are known to increase the urinary excretion of zinc, and increased urinary losses of this trace element have been observed during certain mountaineering expeditions (Rupp et al., 1978). The effect of cold per se on zinc requirements has apparently not been studied. Therefore, it is not possible to draw any conclusions regarding additional requirements for zinc due to cold exposure.
There is no information regarding the effect of cold on dietary copper needs.
Animal studies suggest that selenium deficiency may impair the cold-stimulated thermogenic response. However, as with the other trace elements, deprivation over the several week time span typical of field exercises is not likely to result in deficiencies of microminerals unless tissue reserves were already in a depleted state. Consumption of diets providing MRDA levels of microminerals should provide sufficient nutrients to allow for normal thermoregulatory processes in the cold.
In summary, there appears to be no scientific basis at this time for altering the dietary recommendations for any of the mineral nutrients discussed in this report due to exposure to cold climates; however, additional research is warranted.
APPETITE AND BEHAVIOR CHANGES IN THE COLD
In several long-term studies in cold environments, significant body weight gains were observed (see LeBlanc Chapter 12 in this volume). It is unclear if these weight gains can be attributed to an increase in appetite induced by the cold exposure or if the gains in weight are due to other changes in the
environment and activity patterns of the subjects. Among the other changes common to all the studies described by LeBlanc in Chapter 12 were diet, season of the year, emotional factors caused by isolation, and changes in physical activity (Kark et al., 1948; Lewis et al., 1960; Milan and Rodahl, 1961). Changes in diet alone seem unlikely to be the cause of the weight gain since the foods used in some of the studies were reported to be less palatable than foods consumed before the study. It is well known that a reduction in food intake does not simultaneously occur with a reduction in physical activity. However, it is not clear from these studies that changes in physical activity could account for all of the weight gain. Likewise there is no clear evidence that the weight gain observed in cold environment studies is due to season of the year or emotional factors caused by isolation. LeBlanc suggests in Chapter 12 that cold exposure per se is not a likely cause of the energy imbalance which leads to the weight gains, because weight gains were not observed for individuals during the coldest months of the year. In addition, the weight gains recorded in these studies (see LeBlanc's review in Chapter 12 in this volume) could have resulted from the sudden change in exposure to a cold environment, i.e., lack of acclimatization. Perhaps the subjects would have reached a new stable weight if the study had continued for a longer time. Clearly the study results tend to indicate that exposure to a cold environment does not depress appetite.
THE HIGH-ALTITUDE ENVIRONMENT
PHYSIOLOGICAL CHANGES AT HIGH ALTITUDES
Basic Physiology of High-Altitude Exposure
A variety of physiological and mental responses are initiated by the unique physical and environmental factors which characterize the Earth's high altitudes. As reviewed by Allen Cymerman, Robert B. Schoene, and Inder S. Anand and Y. Chandrashekhar (see Chapters 16, 17, and 18 in this volume, respectively), many of these responses have adverse, mission-threatening impacts on military performance, both in the short-term, as exemplified by acute mountain sickness (AMS)2, and in the long term through diminished physical capacity because of decreased muscle mass and the other effects of the environmental stress on the body. Some of these adverse responses may
progress to pathophysiological, life-threatening conditions such as high-altitude cerebral edema (HACE) and high-altitude pulmonary edema (HAPE)3.
An impressive number of studies has been conducted on mountain climbers, military personnel, and acclimatized individuals residing at or transiently exposed to moderately high altitudes, i.e., 10,000 to 15,000 ft (3,048 to 4,572 m). Far fewer studies have been conducted at extremely high altitudes, i.e., 16,500 ft (5,029 m) and over. Integration of these various studies can be difficult due to:
- numerous confounding variables (e.g., duration and severity of any coexisting physical activity, harsh environmental conditions and temperatures, and/or variations in fluid and food intake);
- interpersonal differences;
- speed of ascent;
- final altitude reached;
- duration of stay at altitude;
- relatively small number of subjects studied at extreme altitudes; and
- methodological difficulties and differences, especially in studies involving salt and water balances and body fluid compartment volumes.
Available data thus are at times conflicting, and are generally difficult to interpret.
Although some of the biophysical stresses of high altitude also can be duplicated and studied in laboratory altitude chambers, difficulties in interpreting field data typically have not been resolved by subsequent testing in altitude chambers. Further, although excellent studies have been done with laboratory animals or livestock exposed to high-altitude environments, their applicability to the human situation remains uncertain.
Biophysical Realities of High Altitudes
High altitude presents an adverse environment that challenges the physiological processes in the body. An individual can adapt (acclimatize) somewhat to these environmental conditions, provided the altitude encountered is not too high (for example, greater than 18,000 ft [5,486 m], which is considered an extremely high altitude). Failure to acclimatize may result in
minor medical illnesses, known collectively as acute mountain sickness (AMS) or major life threatening illnesses (i.e., HAPE or HACE) (see Cymerman, Chapter 16 in this volume).
The challenging environmental conditions at high altitudes include hypobaric hypoxia, dry air, and extreme variations in external temperature. Each of these conditions elicits physiological responses that appear to allow the individual to remain conscious and functional during the first hours and days at high altitude (Cymerman and Rock, 1994).
The governing biophysical factor at high altitudes is the decreasing barometric pressure that characterizes increasing altitude (Cymerman and Rock, 1994). Although the atmospheric concentration of oxygen remains at a constant 20.93 percent at all terrestrial altitudes, the partial pressure of oxygen (pO2 = 0.2093 × barometric pressure) falls along with the decline in barometric pressure. As altitude increases, the lowered oxygen pressure (pO2) in pulmonary alveolae causes a declining saturation of hemoglobin in arterial blood, and a lower oxygen pressure gradient throughout the body, especially at the level of the capillaries, where the pO2 may be close to zero. With low pO2 the blood flow is too rapid to allow appropriate gaseous exchange, resulting in unfavorable conditions for oxyhemoglobin dissociation. Exercise of any kind becomes difficult. Respiratory rate and heart rate increase in response to chemoreceptor activity with resultant modest improvement in oxygen delivery.
The dry air found in high environments adds to the problem of oxygen delivery at altitude. Because air must be moistened to protect the respiratory epithelium, water is added to the air inspired at each breath. As a result, alveolar pO2 is further reduced. This process adds about 47 mm Hg of water vapor pressure to the alveolar gasses. Further exacerbating the alveolar ''crowding" is expired CO2, which contributes 40 mm Hg with normal breathing and increases transiently at altitude. With the higher respiratory rates characteristic of high altitudes, the concentration (and thus partial pressure) of alveolar CO2 declines somewhat with time, allowing alveolar pO2 to increase somewhat with length of exposure (Milledge, 1992; Buskirk and Mendez, 1967). The increased rate of respiration increases fluid loss through the lungs, creating the potential for dehydration if fluid intake is not maintained.
The oxygen dissociation curve for hemoglobin is another important physiological factor at high altitudes. The curve "breaks" at about 14,110 ft (4,300 m), at which point hemoglobin saturation is already decreased to 85 percent of that seen at sea level. At even higher altitudes, small declines in the pO2 of alveolar air result in large declines in arterial blood and hemoglobin saturation, making even the act of breathing hard work.
As altitude increases, ambient temperature decreases at a rate of approximately 3.6°F/984 ft (2°C/300 m) rise in elevation. However, work at high altitudes has the potential for creating extremes of temperature for the individual, with sweating one minute as a result of strenuous work in heavy
clothing, and shivering the next because of cessation of effort. These vacillations as well as the decreased ambient temperature provide further stress to the cardiovascular system. Plasma volume falls, and heart rate increases. Basal energy requirements are elevated in individuals living at altitude, and total energy requirements are elevated in those performing work at altitude.
Physiological Responses at High Altitudes
Many factors contribute to the impaired ability of soldiers to perform at high altitudes. Acclimatization of the various physiological processes occurs at varying rates as cardiovascular, respiratory, and biochemical responses all adapt to maintain a normal hemoglobin saturation.
Within the first 7 days of high-altitude exposure, respiratory rate increases (when pO2 drops below 122 mm Hg) in response to central and peripheral chemoreceptor input to the respiratory centers in the brain. This response is countered by an exaggerated loss of CO 2, leading to central respiratory depression (Bender et al., 1989). The system comes to an equilibrium after about 20 days at high altitudes (Bender et al., 1989).
A rise in cardiac output at rest also occurs at high altitudes, because of an increase in heart rate in the face of a constant stroke volume (Hannon and Vogel, 1977). Plasma volume declines, concentrating the available hemoglobin, and venous return decreases, thus finally depressing stroke volume after the first 3 to 5 days at high altitudes (Hannon and Vogel, 1977). Cardiovascular responses also reduce peripheral blood flow, with a shunting of blood to the heart, lungs and brain. These responses are influenced by an increased secretion of norepinephrine, as evidenced by increases in both plasma and urinary norepinephrine values (Brooks et al., 1991; Cruz et al., 1976; Cunningham et al., 1965; Hoon et al., 1976; Kotchen et al., 1973; Mazzeo et al., 1991; Moncloa et al., 1965; Reeves et al., 1992; Young et al., 1989).
Cardiovascular responses are also influenced by alterations in body salt and water balances. Diuresis upon acute exposure to high altitudes is reported frequently, and is thought to contribute to the concentration of available hemoglobin. Red cell mass increases over time in response to secretion of erythropoietin, providing a more permanent mechanism for maintaining oxygen saturation. Exercise at high altitudes worsens hypoxia, but there is no change in the energy cost of performing a given task. At very high altitudes (18,000 ft [5,486 m]), there is a linear decrease in O2 consumption and exercise performance, and the work of breathing becomes a major factor in itself. The combination of stress, physical activity, and hazardous terrains often leads to physical injuries.
Water Balance at High Altitudes
As reviewed by Anand and Chandrashekhar (see Chapter 18 in this volume), data from more than 50 studies on fluid shifts at high altitudes are conflicting and controversial. Many studies show that diuresis occurs upon acute exposure to high altitudes (for example, Phillips et al., 1969), but an equal number show anti-diuresis (for example, Singh et al., 1990). Few studies have had adequate experimental controls for the insufficient dietary intake observed. This dietary insufficiency could result in diuresis from the excretion of breakdown products of lean and fat tissues. Conversely, water retention is most common at extremely high altitudes, and contributes to AMS as well as to both HAPE and HACE (Anand and Chandrashekhar, 1992; Anand et al., 1990). Exercise also stimulates an accumulation of body electrolytes and water, and may cause the plasma volume to increase (Withey et al., 1983).
Changes in water excretion are influenced by a number of regulatory hormones. Hypoxic subjects, at rest, generally show decreased plasma concentration of aldosterone, which results in a decrease in sodium retention and thus in water retention (Bouissou et al., 1989; Colice and Ramirez, 1985, 1986; Heyes et al., 1982; Hogan et al., 1973; Maher et al., 1975; Maresh et al., 1985; Milledge et al., 1983; Olsen et al., 1992; Raff et al., 1986; Ramirez et al., 1992; Shigeoka et al., 1985; Slater et al., 1969a, b; Sutton et al., 1977). Hypoxia also blunts the normal increase in aldosterone associated with exercise even when the same amount of exercise is done (Maher et al., 1975; Milledge et al., 1983; Olsen et al., 1993; Shigeoka et al., 1985). A decrease in renin activity seems to follow similar patterns. The function of renin is to convert the prohormone angiotensinogen to the active hormone angiotensin. Angiotensin is a potent peripheral vasoconstrictor that promotes renal sodium retention and stimulates secretion of aldosterone by the adrenals. Thus, with hypoxia the renin-angiotensin-aldosterone relationship becomes uncoupled. Responses of antidiuretic hormone (ADH) also differ with the degrees of hypoxia and exercise. ADH secretion decreases when hypoxia is moderate and exercise is light, thus resulting in decreased fluid retention, and increases with extremely high altitudes and/or severe exercise stress, which would increase fluid retention (Bärtsch et al., 1991).
Increases in the stress-related hormones, cortisol and norepinephrine, are associated with both high altitude and exercise and may affect fluid balance. Subjects who are prone to develop AMS have an atypical ADH and aldosterone response, which increases fluid retention (i.e., both hormones tend to increase in concentration in the blood at high altitudes, rather than decrease, with the increases being exaggerated by exercise).
Relatively few data exist on renal function at high altitudes; the small amount of information available suggests that high altitudes lead to a decrease in effective renal plasma flow (ERPF), although glomerular filtration rates are
maintained (Olsen et al., 1993). Undoubtedly, the magnitude of these changes varies, depending on the conditions under which they are measured.
Cymerman (see Chapter 16 in this volume) emphasizes that dehydration is a militarily important factor, especially when exposure to moderately high altitudes is abrupt and accompanied by strenuous exercise. With moderate-altitude exposure, diuresis is an important component of the initial physiological response, anti-diuresis being associated with AMS (Anand et al., 1990). However, fluid losses because of high altitude and exercise may be exacerbated by fluid loss associated with inadequate energy intake. Dehydration is exaggerated by a reduced sensation of thirst with an accompanying reduction in fluid intake (Adolph et al., 1947). The dehydrated state may be further exacerbated by both sensible and insensible water losses. Exercise in bulky clothing induces significant sweating, at a rate as high as 2 liter/h. Insensible losses through skin (minor) and respiratory epithelium may reach 1 to 2 liter/d even without exercise (Milledge, 1992). This respiratory fluid loss also carries with it significant heat losses, which increase the maintenance energy requirement by as much as 1.6 times that at sea level (Gonzalez et al., 1985). At moderately high altitudes, losses of body fluids are proportional to losses in body weight, and there are significant decreases in plasma volume (Jain et al., 1980, 1981; Singh et al., 1986, 1988, 1990). In addition, there are uncontrolled shifts of fluid out of the vascular compartment, which, along with the initial fall in total body water, help lower the stroke volume. Some studies show intracellular dehydration as well. Fluid losses thus contribute to the observed losses of body weight. Dehydration may engender symptoms comparable to those of AMS. Body water must be maintained at high altitudes, but should not be by the ingestion of bacterially-contaminated fluids or snow.
In marked contrast, an accumulation of body salt and water occurs in individuals who remain at extremely high altitudes (over 18,000 ft [5,486 m)] for many weeks. Anand's studies, in 10 asymptomatic soldiers who lived at 22,000 ft (6,706 m) for at least 10 weeks, showed a 20 percent increase in total body water. There was also an 80 percent increase in circulating blood volume because of sizable increases in both plasma volume and red cell volume. Fluid accumulations were accompanied by an 18 percent increase in body sodium, a reduced renal blood flow, and increased circulating concentrations of norepinephrine, cortisol, and aldosterone (Anand and Chandrashekhar, 1992).
Acclimatization to High Altitudes
Acclimatization to moderately high and high altitudes depends upon the swiftness of ascent, as well as the duration of the stay. Individual physiological systems acclimatize at different rates, some taking as little as a few days, others as long as a month to years to fully adjust (see Figure 1-1 below). With
acclimatization there is a continuing hyperventilation over the first 14 days at high altitude, with a slow rise in O2 saturation of hemoglobin. The kidney corrects the respiratory alkalosis, and after a month or so there is an increase in the number of circulating red blood cells in response to increased erythropoietin secretion (see above under "Physiological Responses to High Altitudes"). As a rule acclimatization will occur at elevations up to 17,000 ft (5,182 m), but full acclimatization rarely occurs at extremely high altitudes.
Altitude-Induced Illness
Failure to acclimatize results in a continuum of symptoms. AMS may vary from a minor problem to a militarily incapacitating illness. AMS is characterized by mild to severe headaches, mild to severe nausea and vomiting, and a general lethargy with possible personality changes (Bahrke and Shukitt-Hale, 1993; Hackett et al., 1989). Further, more severe illnesses include an accumulation of fluid in the lungs (HAPE), because of leaking of the endothelial membranes, and in the brain (HACE), possibly because of a similar mechanism. HAPE is characterized by inability to perform, or even to walk, and often includes the production of foamy sputum (Hackett et al., 1989). The
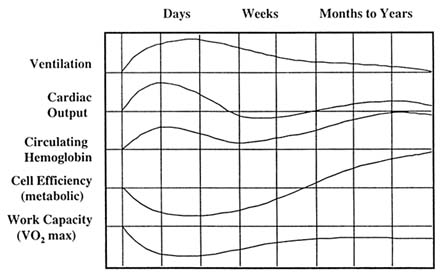
FIGURE 1-1 Approximate size, direction, and temporal changes that occur during acclimatization to 14,000 to 15,000 ft (4,267 to 4,572 m). SOURCE: Adapted from Houston (1982).
accumulation of fluid in the interstitial space increases the distance across which oxygen must diffuse to reach the cells and thus further compromises performance ability.
Acute Mountain Sickness (AMS)
Acute mountain sickness (AMS) has been recognized for centuries, and occurs in most individuals to some degree at altitudes of 11,500 ft (3,505 m) or more. About 25 percent of tourists develop signs of AMS at elevations of only 8,900 to 10,000 ft (2,712 to 3,048 m), the severity and incidence depending upon the rate of ascent (Hackett et al., 1989). A severe bilateral headache is the primary symptom, but AMS also produces extreme fatigue, shortness of breath, and sleep disturbances. The headaches are accompanied by sharp increases in cerebral blood flow velocities, as measured by Doppler techniques. Cerebral symptoms of AMS may be secondary to an initiation of brain edema (Hackett et al., 1989).
Intestinal disturbances, with vomiting, are aggravated by expanding intestinal gas, and gas trapped in nasal sinuses can be particularly painful. AMS severely reduces appetite. The ability to carry out various functions is markedly impaired. AMS is usually self-limiting within 3 to 7 days of exposure.
Strangely, some individuals show no symptoms of AMS, whereas those who suffer AMS once are likely to experience it every time they go to high altitudes. Freedom from AMS seems to be linked to the ability to diurese quickly, and diuretics have been used as therapy. The drugs most widely used to treat AMS are acetazolamide (Diamox), a carbonic anhydrase inhibitor, and adrenocorticoids (especially Decadron) (Hackett et al., 1989). Acetazolamide stimulates breathing and prevents nocturnal periodic respiration; it also stimulates renal bicarbonate excretion to balance the respiratory alkalosis caused by hyperventilation. Acetazolamide is effective at 125 mg given up to twice daily, beginning with the onset of symptoms (Hackett et al., 1989). Adrenocorticoid therapy should be reserved for those seriously ill with AMS due to its failure to promote acclimatization.
Subacute Mountain Sickness
A new syndrome, termed subacute mountain sickness, was observed in healthy young soldiers who had spent several months at extremely high altitudes of approximately 22,000 ft (6,706 m) (Anand et al., 1990). As described by Anand and Chandrashekhar (see Chapter 18 in this volume), the syndrome appeared to be one of severe systemic and congestive heart failure without pulmonary hypertension. About 20 percent of the group developed
shortness of breath, puffiness of the face and eyelids, anasarca (generalized pitting edema), and pericardial fluid accumulation, with a normal heart size and normal pericardium. Left ventricular function was also normal on cardiac catheterization. These accumulations of fluid all disappeared in a few weeks at sea level with no additional therapy.
High-Altitude Cerebral Edema (HACE)
Severe AMS can precede or predispose to cerebral edema, which is termed high-altitude cerebral edema (HACE) (see Cymerman, Chapter 16 in this volume). This edema of the brain tissue is accompanied by engorged cerebral and retinal arteries, extremely high cerebrospinal fluid pressures, and sometimes small cranial and retinal hemorrhages. The edema can be progressive, and even lethal, unless treated rapidly by oxygen administration, by moving the patient quickly to a lower altitude, and/or by using a hyperbaric bag (Hackett et al., 1989).
High-Altitude Pulmonary Edema (HAPE)
An acute build up of fluid transudate in the alveolae and the bronchial tree, associated with pulmonary artery hypertension, is another potential problem of high altitudes (see Cymerman, Chapter 16 in this volume). This high-altitude pulmonary edema (HAPE) is complicated by bronchial secretions that are extremely thick and viscid due to leakage of protein into the alveolar and bronchial fluids. These fluids block gas exchange within the lung. This potentially lethal condition may develop quite quickly, and it requires immediate therapeutic measures, such as oxygen administration and removal of the patient to lower altitudes, which usually correct the problem.
Weight Loss at High Altitudes
Sojourns at high altitudes result in weight loss in most individuals allowed to eat ad libitum (see discussion by Gail E. Butterfield, Chapter 19 in this volume). As pointed out above, some of this weight loss may be a result of diuresis, other contributing factors include a decline in appetite, which accounts for a deficit of almost 200 kcal/d in most studies, and an increase in basal energy needs, which accounts for almost 300 kcal/d. Thus, even a sedentary visitor to high altitudes may experience an energy deficit of at least 500 kcal/d. There is little data to suggest that this deficit is further exacerbated by malabsorption of fat, carbohydrate, or protein.
However, the loss of body weight is often accompanied by negative nitrogen balance, with associated losses of muscle mass, which may significantly impact on performance. The inevitability of this weight loss has been debated, but recent studies by Butterfield and colleagues suggest that strict attention to adequacy of energy intake can essentially eliminate this problem, as well as diminish some of the diuresis of acute exposure (see Chapter 19 in this volume).
The provision of sufficient energy intake to meet energy expenditure needs in experiments where individuals visit high altitudes also ensures the study of true metabolic responses to hypoxia, not malnutrition. Under circumstances of energy balance, Butterfield reports in Chapter 19 in this volume that the primary metabolic fuel at rest and during exercise after acclimatization to high altitudes is carbohydrate (Roberts et al., in press a), with the utilization of fat falling to very low levels (Roberts et al., in press b). Thus, enforced consumption of carbohydrate foods to ensure adequate energy intake is important. In field situations, sufficient time must be allowed for preparation and consumption of adequate energy and carbohydrate to maximize troop productivity and decrease morbidity.
Effects of Age and Gender on Response to Altitude
Little information is available concerning the effects of age and gender on physiologic response to high altitudes. Some investigators claim that women acclimatize better than men (Hannon et al., 1976) in that basal metabolic rates and appetite appeared to return toward sea level values more rapidly in women studied at high altitudes than in men. However, very few studies of women have been conducted, and the impact of menstrual cycle phase on the process of acclimatization is completely unknown, although sex hormones have been shown to influence the key physiologic processes involved in acclimatization (Tatsumi et al., 1995).
In addition, several aspects of energy metabolism known to be affected by altitude in men are also affected by phase of the menstrual cycle at sea level in women. These include food intake (Lyons et al., 1989), basal metabolic rate (Meijer et al., 1992; Webb, 1986), nitrogen balance (Calloway and Kurzer, 1982), and fat utilization (Hackney et al., 1991). Thus, the investigation of the interaction of these factors with altitude and menstrual cycle would be important for understanding the needs of female troops.
The issue of age and high-altitude acclimatization is also not adequately investigated at the present time.
CHANGES IN NUTRIENT REQUIREMENTS AT HIGH ALTITUDES
Macronutrients
Energy Sources
Total dietary energy requirements at altitude are discussed by Reed W. Hoyt and Arnold Honig (see Chapter 20 in this volume). These needs are determined by the type and duration of physical activity, preexisting body energy stores, and environmental conditions. The macronutrient composition used to provide dietary energy depends upon the intensity and duration of the exercise performed, the macronutrients available from body stores and the diet, and environmental conditions.
Troops in the field at high altitudes frequently experience energy deficits as a natural consequence of high energy outputs and limited intakes. Under training circumstances, strenuous exercise (greater than 75 percent of maximum oxygen consumption, ![]() o2max) may be performed for as many as 17 to 18 hours each day. Work expenditures as measured by the DLW technique may reach 4 to 7 times basal metabolic rate (BMR) (Forbes-Ewan et al., 1989; Hoyt et al., 1991). Hoyt and Honig report on a study of 781 soldiers engaged in field maneuvers at altitudes of 7,000 to 11,000 ft (2,134 to 3,353 m), for 3 to 34 days who demonstrated a mean energy expenditure of 3,500 kcal/d, or about 2.2 × BMR (Jones et al., 1990).
o2max) may be performed for as many as 17 to 18 hours each day. Work expenditures as measured by the DLW technique may reach 4 to 7 times basal metabolic rate (BMR) (Forbes-Ewan et al., 1989; Hoyt et al., 1991). Hoyt and Honig report on a study of 781 soldiers engaged in field maneuvers at altitudes of 7,000 to 11,000 ft (2,134 to 3,353 m), for 3 to 34 days who demonstrated a mean energy expenditure of 3,500 kcal/d, or about 2.2 × BMR (Jones et al., 1990).
Military operations at high altitudes may require even greater increases in energy expenditure. Basal metabolic rates at altitude may initially be elevated 20 to 30 percent above those at sea level. After 2 to 3 days, BMR falls and may be maintained at 15 to 16 percent above sea level values. The time course of this elevation varies among studies. Some studies show these acute (20 to 30 percent) increases to be sustained for 1 to 2 weeks while other studies show the elevation to be maintained throughout a 3-wk stay (Butterfield et al., 1992; Meda, 1955; Nair et al., 1971; Stock et al., 1978; Terzioglu and Aykut, 1954). The decline in BMR with acclimatization seems to be the result of inadequate energy intake. Individuals native to high altitudes demonstrate elevated BMRs as compared to individuals at sea level of similar body size, and individuals required to consume the energy at a level equivalent to their need will maintain an elevated BMR throughout altitude exposure.
Although altitude acclimatization increases endurance capacity, there is little change in energy expended at submaximal work loads between altitude and sea level, either acutely or with chronic exposure. Thus, energy expenditure for specific tasks is no different at high altitudes than at sea level (Fulco and Cymerman, 1988; Grover et al., 1986; Young and Young, 1988).
The high energy requirements of training are usually not countered by increased intakes. Rather, dietary intake in field situations is frequently inadequate to meet needs due to decreased palatability of foods provided,
boredom in menus, reluctance to work on a full stomach, lack of fluid availability, odd meal times, anxiety, or self-imposed dieting. In Chapter 20 of this volume, Hoyt and Honig present a review of 11 recent field studies. In these studies the reported energy intakes using dietary records were about 2,400 kcal/d, although approximately 3,600 kcal/d were provided. This intake represented a consumption of only about two-thirds of the rations provided, which created a theoretical energy deficit of almost 1,000 kcal/d.
The anorexia commonly experienced at high altitudes may contribute to this difficult situation. There is some speculation that the anorexia of altitude may serve to limit sodium and water intake with the teleologic consequence of adjusting body stores for better acclimatization (Hoyt and Honig, 1996). However, no research in human subjects has been able to attribute the anorexia of acute mountain sickness to a possible physiological mechanism.
The metabolic fuels used to supply energy requirements during military operations at high altitudes are derived from both dietary sources and preexisting body stores. Most troops have fat stores sufficient to cover an energy deficit of 1,000 kcal/d for 1 to 2 months (fat stores equivalent to about 30,000 to 60,000 kcal, or about 9 kg of fat mass) (Sahlin, 1986). However, glycogen stores, which determine to some extent the endurance capacity of the individual, are more limited. Carbohydrate needs, based on a mean Respiratory Exchange Ratio (R) of 0.85, which represents a carbohydrate contribution to energy supply of about 70 percent (Kleiber, 1961), would need to be at least 400 g/d. Normal rations available to troops supply 580 to 680 g carbohydrate per day (AR 40-25, 1985; see Table 1-3); however, data presented by Hoyt and Honig (see Chapter 20 in this volume) suggest actual carbohydrate intakes of less than 300 g/d. Thus, inadequate carbohydrate intake may exist in troops working at high altitudes, a state which might contribute to diminished performance.
The failure to match dietary fuel supply with physiological need results in a shift in metabolic fuel use toward fat. Increased energy needs at high altitudes may increase the use of body fat under these circumstances of energy deficit. Acclimatization results in a decrease in muscle glycogen utilization (Young et al., 1982) and a decrease in muscle lactate (Green et al., 1989) in individuals functioning under an energy deficit, suggesting to Hoyt and Honig that acclimatization leads to an increase in fat utilization. However, in individuals maintaining adequate energy intake, the situation may be reversed (Roberts et al., in press a).
Estimation of energy requirement in the field is difficult. Hoyt and Honig (see Chapter 20 in this volume) describe a new ambulatory monitor and method that involves estimation of energy expenditure based on body weight, the time during each stride that a single foot contacts the ground (foot contact time), and the nature of the terrain being covered. The resulting estimate is based on the energy cost of supporting body weight and the rate at which this force is generated. The rate of force generation can be estimated as total body
weight divided by the time during each stride that a single foot was in contact with the ground. One relevant finding was that soldiers performing similar tasks in mountainous terrain had energy expenditures proportional to their total weights (Hoyt et al., 1994). This method is currently being tested and still requires validation against other methods, such as the use of doubly labeled water.
In summary, soldiers in field training exercises, particularly those in mountainous, high-altitude terrain, are characteristically in negative energy balance. This deficit is largely attributable to the amount of time spent in physical activity, the weight of work loads, the elevation in basal energy requirements at high altitudes, and the limited consumption of field rations. Food and salt intakes appear to be reduced during the periods of adaptation to altitude. Carbohydrate intakes should be encouraged during such periods of adaptation to altitude.
Protein
A major observation of many of the studies reviewed by Butterfield and by Hoyt and Honig (see Chapters 19 and 20 in this volume, respectively) was the significant loss of lean body mass (LBM) among most of the subjects. The question raised was whether the protein requirement was increased in high-altitude environments or whether this loss in LBM was due only to a negative energy balance. Butterfield points out that the LBM losses were accompanied by losses of both total body weight and fat mass, which indicated that a negative energy balance was a more likely explanation for the LBM loss rather than an increased protein requirement. She further reasons that negative energy balance was likely caused by anorexia coupled with an increased metabolic rate induced by altitude exposure. In studies designed to increase energy intake during high-altitude exposure, Butterfield et al. (1992) demonstrated that if subjects were encouraged to consume sufficient energy to achieve energy balance, body weight losses were corrected and nitrogen balance could be achieved. The implication of these data is that the loss of lean body mass and resulting negative nitrogen balance are due entirely to the negative energy balance caused by anorexia and increased metabolic rate and not to an increase in protein requirements per se. Butterfield et al. (1992) further report that in a study where energy needs were adequately met throughout a 21-d stay at 14,000 ft (4,267 m), both body weight and nitrogen balance were maintained. It should be noted that these studies involved only moderately active, untrained individuals. Further studies involving strenuous exercise such as those performed by military troops on maneuvers, should be conducted using continuous nitrogen balance to define protein requirements in military type activities at high altitudes.
In summary, based on the available data, there is no apparent scientific rationale for increasing the recommended protein allowance for work at high altitudes above the existing MRDA value as provided to soldiers in cold weather rations. Strategies described in previous reports (IOM, 1995a) should be employed to encourage soldiers to eat their rations and thereby meet their energy needs and avoid negative nitrogen balance.
Vitamins
As in the case of cold exposure, no scientific basis was found to recommend increasing dietary recommendations for vitamins A, D, or K for individuals working at high altitudes (see Reynolds, Chapter 13 in this volume). However, the provocative data of I. Simon-Schnass (see Chapter 21 in this volume) showing that high doses (400 mg/d) of vitamin E decreased the exhalation of pentane and the production of thiobarbituric acid-reacting substances (TBARS) by erythrocytes of subjects at high altitudes, suggest that tocopherol may have a role in inhibiting increased lipid peroxidation under such conditions. Furthermore, a high dose of vitamin E appeared to improve the rheological characteristics of blood of subjects at high altitudes (see Reynolds, Chapter 13 in this volume). However, no attempt was made to titrate the dose of vitamin E between the dietary levels typically ingested on such expeditions (17-19 mg/d) and the large intervention dose (400 mg/d), nor was dietary vitamin E controlled. Since no dose-response was observed, it is not possible to arrive at a precise dietary recommendation based on this research. Nonetheless, the committee believes that the data were sufficiently intriguing that additional research along these lines should be encouraged.
As with cold exposure, concern was expressed regarding the adequacy of current dietary recommendations for the water-soluble vitamins essential for energy production (thiamin, niacin, riboflavin, and pantothenic acid) for individuals at high altitudes (see Reynolds, Chapter 13 in this volume). However, the influence of high altitudes on the requirement for these vitamins appears not to have been studied, so there is no basis for modifying these recommendations, which are already related to the levels of energy expended. Also, no data were found regarding the effect of altitude on requirements for vitamin B6, vitamin B12, biotin, or folic acid. Although some altitude simulation studies conducted during the early 1950s indicated that such treatment decreased tissue concentrations of vitamin C in guinea pigs and urinary excretion of ascorbic acid by humans (Boutwell et al., 1950; Mitchell and Edman, 1951), this suggestive research does not permit any quantitative expression of increased vitamin C requirements at high altitudes.
In summary, with the possible exceptions of vitamins E and C, there is little indication that increased vitamin intake is of any benefit to persons exposed to high altitudes. Further research is needed before the recommended
allowances for vitamins E and C could be increased to levels above the current MRDA.
Minerals
No scientific justification could be identified for increasing the dietary intake of calcium, phosphorus, or magnesium beyond MRDA levels because of exposure to high altitudes (see Reynolds, Chapter 13 in this volume). However, adequate iron nutriture is important for individuals working at higher elevations, because of the well-known phenomenon of altitude-induced polycythemia. For example, iron-deficient individuals living at altitudes of 11,800 to 13,500 ft (3,597 to 4,115 m) had a lower maximal workload and voluntary Vo2max than controls with adequate iron status (Beard et al., 1988). Transiently increased iron absorption has been observed following exposure to 15,000 ft (4,572 m) altitude, so that any temporarily increased need for iron was presumably compensated for by this mechanism (Reynafarje and Ramos, 1961). Therefore, there appears to be no reason to advocate dietary intakes of iron greater than MRDA levels because of high-altitude exposure. Urinary excretion of zinc was not increased during an expedition carried out at moderate altitudes (8,000-14,000 ft [2,438-4,267 m]) but urinary zinc losses were significantly elevated during exposure to the very high altitude of 27,726 ft (8,450 m) altitudes (Deuster et al., 1992; Rupp et al., 1978). Urinary losses of zinc averaged between 0.5 and 0.9 mg/d during an expedition to Mt. Everest, with a peak excretion of 3.2 mg/d (Rose et al., 1987). Since the maximum excretion appeared to coincide with periods of greatest physical exertion, these abnormally high urinary losses were thought to be due to muscle breakdown. Losses of body zinc generally accompany negative balances of energy and/or nitrogen. An increased gastrointestinal absorption of the element could compensate for these increased excretory losses of zinc, but further research into the possibility of increased dietary zinc needs at high altitudes is warranted. With regard to copper, there is insufficient information to determine whether dietary copper needs are increased as a result of high-altitude exposure.
In summary, although physiological needs for iron appear to be increased at high altitudes, enhanced compensatory absorption may obviate the need for increased dietary intake. Additional research is warranted to clarify this point. Similarly, the increased zinc losses seen at very high altitudes may be partially compensated by increased absorption.
APPETITE AND BEHAVIOR CHANGES AT HIGH ALTITUDES
Mental Response to High Altitudes
A hypoxic person often experiences personality changes, beginning with euphoria and then depression, with compromised ability to make decisions, especially when severe cold is a confounding factor (Nelson, 1982; Shukitt and Banderet, 1988; Tune, 1964). As noted by Schoene (see Chapter 17 in this volume), high altitudes ''dull the spirit and engender a loss of spontaneity." He also noted, "the higher you go, the slower you go." As hypoxia worsens, there is increasing sensory and mental impairment, with the potential for paranoia and hostility. Patterns of mental response differ with individuals and the time course of acclimatization. Affect and emotions are altered at 14,000 ft (4,267 m) and above to the extent that cohesive groups, such as small military units, may experience a social breakup or dysfunction (Nelson, 1982; Shukitt and Banderet, 1988; Tune, 1964). There may also be decreased ability to perform small motor tasks which may persist after acclimatization.
Sleep is disturbed at altitudes of 14,000 ft (4,267 m) and above. Sleep becomes periodic, often with Cheyne-Stokes breathing4 and periodic awakening accompanied by gasping for breath. There may be as much as a 50 percent reduction in total sleeping time, and a decrease in REM sleep (Anholm et al., 1992; Goldenberg et al., 1992; Normand et al., 1990; Sutton et al., 1979; Weil, 1985; White et al., 1987). This disturbed sleep pattern usually corrects within 3 to 5 days, but in some individuals may last for weeks. The general and REM sleep deprivation may contribute to personality changes.
The Effect of Altitude on Cognitive Performance and Mood States
Physiological changes associated with exposure to altitudes above 10,000 ft (3,048 m) are often accompanied by changes in mood, performance, and appetite (see Chapters 17 and 22 in this volume). The limited available data are based on self-evaluation and suggest that there is mood impairment at high altitudes, including unfriendliness, impaired thinking, and dizziness (Bahrke and Shukitt-Hale, 1993; Van Liere and Stickney, 1963). Other data indicated fatigue, which may have been exacerbated by physical exertion and increased oxygen demand (Shukitt and Banderet, 1988; Shukitt-Hale et al., 1990). In an
altitude chamber, subjects exhibited significant mood deterioration with increases in hypoxic conditions and duration of exposure (Lieberman et al., 1991). Available data thus are suggestive of mood deficits, but more studies are needed.
Data on cognitive performance under hypoxic conditions are also limited. Some results indicate impairment at high altitudes (10,000 ft [3,048 m]), including deficits in reaction time, vigilance, memory, and reasoning ability (Lieberman et al., 1991). Complex task performance also deteriorates, with increased error rate and slowing of performance (Lieberman et al., 1991). Simulation studies in altitude chambers (hypoxic conditions) suggest that such adverse changes increase in severity with greater hypoxia and duration of exposure (Lieberman et al., 1991). There appears to be individual variability in susceptibility to these effects of altitude/hypoxia. Moreover, rate of ascent (onset of hypoxia) influences onset and severity of symptoms (Hansen et al., 1967; Shukitt-Hale et al., 1991a).
In general, mood symptoms of altitude "sickness" develop over about 2 days, with maximal severity at 30 to 40 hours (Carson et al., 1969). Performance decrements occur more quickly and individuals accommodate well before mood changes are maximal. Thus, the temporal development and resolution of behavioral manifestations of hypoxia/high altitude are not simple or uniform (see Barbara Shukitt-Hale and Harris R. Lieberman, Chapter 22 in this volume), or directly tied to decreases in performance.
The underlying mechanisms in the brain responsible for mood and performance deficits at high altitudes are unknown. Some data allow speculation that alterations in certain neurotransmitters might be involved, namely those whose synthesis requires oxygen (catecholamines, serotonin) (Gibson and Duffy, 1981). Recently, more focused behavioral studies in animals point toward changes in acetylcholine formation and release (Shukitt-Hale et al., 1991b, 1993a, b). In addition, the reduced food intake and body weight loss associated with hypoxia at high altitudes may exacerbate direct chemical effects of high altitudes on brain chemistry and function.
Food Components that May Enhance Mental Performance at High Altitudes and in the Cold
Exposure to hypobaric hypoxia and to extreme cold at high altitudes can cause deficits in mental performance. Acclimatization eventually occurs, but only partly corrects cognitive deficits. Performance decrements caused by these and other environmental stressors and the attendant sleep loss can compromise combat operations. Effective countermeasures would be highly desirable, but their development requires an understanding of the specific underlying brain mechanisms causing the decline in mental function in adverse environmental
settings (see discussion by Harris R. Lieberman and Barbara Shukitt-Hale, Chapter 23 in this volume).
For example, one important causal relationship may be the changes in brain catecholamine neurons that accompany stress. During stressful situations, catecholamine neurons increase their firing rate. Over time, the rise in firing rate may deplete the neuron's stores of transmitter, thereby compromising its ability to perform its required functions. Replenishment of transmitter might help to restore normal neuronal function, and overall cognitive function as well. One method for replenishing catecholamine involves administering tyrosine, the catecholamine precursor, to stimulate transmitter production (see Lieberman and Shukitt-Hale, Chapter 23 in this volume; for a more detailed discussion, see Ahlers et al., 1994; Lieberman, 1994; Wurtman and Lieberman, 1989). Indeed, in laboratory studies, increases in catecholamine production and release by neurons occur when tyrosine is administered to animals in a stressful setting (Luo et al., 1993; see Lieberman and Shukitt-Hale, Chapter 23 in this volume). Such tyrosine treatment improved performance in rats in these experimental situations (Ahlers et al., 1994; Luo et al., 1992; Rauch and Lieberman, 1990; Shurtleff et al., 1993). In limited field tests to date, consistent with the results of animal studies, tyrosine treatment maintained some aspects of cognitive performance in soldiers exposed to stressful situations (Ahlers et al., 1994; Banderet and Lieberman, 1989; Lieberman et al., 1990; Shurtleff et al., 1994).
A second causal relationship may be the changes in brain acetylcholine neurons that accompany stress. Acetylcholine neurons, particularly in the hippocampus, are important for normal learning and memory. Stress diminishes the functioning of these cholinergic neurons, with attendant decrements in performance. Preventing acetylcholine depletion during stress might therefore help prevent the loss of cognitive function under stressful conditions.
A variety of plant and animal extracts have been used by Asian practitioners since ancient times to manage stress and increase endurance, as presented by K. K. Srivastava at the workshop (see summary of his unpublished manuscript in Appendix A in this volume). These extracts have been termed adaptogens, and their chemical composition is relatively poorly defined. Careful studies in human subjects to evaluate the true efficacy of adaptogens are lacking. Because of the lack of information on composition and limited data on human or animal trials using these compounds, the CMNR concluded that they could not evaluate these materials or this concept.
Military Considerations
As described in this report, the many adverse physiological reactions, physical, or cognitive performance difficulties, and mood changes at high altitudes, when combined with increased risks for mountain illnesses, trauma,
and malnutrition, create obvious difficulties for military operations. Some of these difficulties can be minimized by appropriate military planning, policies, and training. Troops conducting military operations at high altitudes, as they currently do in several mountainous regions of the world, have unique needs for special training and support. To prevent severe dehydration, water discipline is as essential at high altitudes as it is in the desert, and potable water must be supplied, whatever the logistical problems. Despite the tendencies for high-altitude and AMS-induced anorexia, discipline in food intake must also be enforced and military field feeding doctrines (IOM, 1995a) should include specific mention of environmental extremes. Energy and carbohydrate-rich foods must be provided, as outlined earlier in this chapter. Time to prepare and consume adequate energy must also be allowed. Increased energy needs at high altitudes result from an increase in basal energy needs as well as from strenuous activity. In order to prevent loss of body weight and muscle mass, the foods required to supply these needs must be provided, and they must also be compatible with logistical constraints. Palatability also must be considered; for example, provision of an easily consumed, preferred high energy "finger" food or beverage could be important in maintaining body weight and muscle mass.
Because gradual ascent to altitude and gradual acclimatization are not often compatible with military missions, a high incidence of AMS and breakdown in military unit cohesiveness must be anticipated. Military missions must be planned with the expectation that more than half of the troops will suffer from some degree of AMS, and that up to 25 percent may be transiently incapacitated (Hackett et al., 1989). Additional medical problems must be anticipated in troops who remain at altitudes above 18,000 ft (5,486 m) for many weeks (see Butterfield, Chapter 19 in this volume). Acclimatization to moderately high altitudes (8,000-12,000 ft [2,438-3,658 m]) may be accomplished within a week (many physiological systems adapt in this time, but some take far longer). However, full acclimatization to extremely high altitudes may not occur, and accumulations of body salt and water may become a consistent problem (see Cymerman, Chapter 16 in this volume).
All personnel must be trained to recognize the early symptoms of acute pulmonary edema or cerebral edema. These life-threatening problems are most likely to be observed in those individuals who have experienced difficulty in keeping up the pace and lag behind. Troops assigned to high altitudes should also be trained to master the difficulties in treating and evacuating patients with these altitude-induced conditions, as well as the task of dealing with soldiers who fall victim to the inevitable mountain climbing injuries.
INTERACTIONS OF COLD AND HIGH ALTITUDES
When considering nutritional and physiological aspects of cold and high-altitude environments, it is important to keep in mind that while there are similarities between the two in that high altitudes are frequently cold, there are also important differences. For example, as outlined by COL Askew (see Chapter 3 in this volume), these environments are similar in such characteristics as low ambient temperature, limited available water (mostly from snow and ice), and problems in food preparation. In both, diuresis occurs at least initially, energy requirements for work are increased, carbohydrate is well tolerated, and there appears to be no advantage of extra protein over the usual requirement.
Cold exposure tends to increase appetite and, over time, body weight may increase, whereas at high altitudes, appetite tends to be depressed, and body weight may decrease. Studies done in the cold at elevations above 11,500 ft (3,505 m) have shown further increases in energy need over those in the cold to more than 5,000 kcal/d (Jones et al., 1993; Swain et al., 1949). The dissimilarities also include lower oxygen tension and greater anorexia at high altitudes. Fat as a source of energy is well tolerated in the cold, but carbohydrate is the fuel of choice in low oxygen environments. These factors need to be considered when evaluating potential physiological responses of troops operating in these environments.
SUMMARY
Predictable medical problems can arise when military operations must be conducted in arctic cold, at high altitudes, or during combinations of both stressful conditions. Cold-induced injuries, altitude-induced illnesses, and psychological changes are described in this report. In addition, a great deal is known about the physiological responses used by the body during exposure to extreme cold, and the types of clothing and shelters that are militarily effective. Physiological adjustments, however, cannot mitigate the biophysical reality of declining availability of atmospheric oxygen as altitude increases. Much less is known about nutrient requirements for working in the cold and in extremely high environments.
A number of additional nutritional questions arose and were discussed during the workshop. These focused on possibly altered nutrient requirements for optimal or enhanced performance during operations in cold and/or high altitudes, and for assisting in thermoregulation, acclimatization, and prevention of medical problems. During the workshop, current military rations also were exhibited.
Physiological responses to cold and altitude were reviewed in depth, as were central nervous system functions and the interrelations between sleep and
body temperature regulation. Dangers of acute mountain sickness and high-altitude cerebral and pulmonary edema were considered, as were the effects of cold and of high altitudes on appetite, mood, and both physical and mental performance. A review of available knowledge about altered nutrient requirements at cold and altitude extremes included presentations on fluid balance, energy costs, body weight changes, specific needs for various macro-and micronutrients, and the effects of appetite, gender, and age on these requirements. Discussion of these topics set the stage for the recommendations and conclusions concerning the questions under consideration, some immediately available military approaches, and future research needs, all of which are found in the next chapter.
REFERENCES
Adolph, E.F., and associates 1947 Physiology of Man in the Desert. New York: Interscience Publishers, Inc.
Ahlers, S.T., J.R. Thomas, J. Schrot, and D. Shurtleff 1994 Tyrosine and glucose modulation of cognitive deficits resulting from cold stress. Pp. 301–320 in Food Components to Enhance Performance, An Evaluation of Potential Performance-Enhancing Food Components for Operational Rations, B.M. Marriott, ed. A report of the Committee on Military Nutrition Research, Food and Nutrition Board. Washington, D.C.: National Academy Press.
Anand, I., and Y. Chandrashekhar 1992 Syndromes of subacute mountain sickness: Pathophysiology and manifestations. Pp. 257–275 in The Diagnosis and Treatment of Pulmonary Hypertension, E.K. Weir, S.L. Archer, and J.T. Reeves, eds. Mt. Kisco, N.Y.: Futura Publishing Inc.
Anand, I., R. Malhotra, Y. Chandrashekhar, H. Bali, S. Chauhan, R. Bhandari, and P. Wahi 1990 Adult subacute mountain sickness—a syndrome of congestive heart failure in man at very high altitude. Lancet 335:561–565.
Anholm, J.D., A.C. Powles, R. Downey, C.S. Houston, J.R. Sutton, M.H. Bonnet, and A. Cymerman 1992 Operation Everest II: Arterial oxygen saturation and sleep at extreme simulated altitude. Am. Rev. Respir. Dis. 145:817–826.
AR (Army Regulation) 40-25 1985 See U.S. Departments of the Army, the Navy, and the Air Force.
Askew, E.W. 1989 Nutrition for a cold environment. Phys. Sportsmed. 17:77–89.
Astrup, A., J. Bulow, J. Madsen, and N.J. Christensen 1985 Contribution of BAT and skeletal muscle to thermogenesis induced by ephedrine in man. Am. J. Physiol. 248 (Endocrinol. Metab. 11):E507–E515.
Astrup, A., B. Buemann, N.J. Christensen, S. Toubro, G. Thorbek, O.J. Victor, and F. Quaade 1992 The effect of ephedrine/caffeine mixture on energy expenditure and body composition in obese women. Metabolism 41(7):686–688.
Bader, R.A., J.W. Eliot, and D.E. Bass 1952 Hormonal and renal mechanisms of cold diuresis. J. Appl. Physiol. 4:649–658.
Bahrke, M.S., and B. Shukitt-Hale 1993 Effects of altitude on mood, behavior, and cognitive functioning: A review. Sports Med. 16:97–125.
Baker-Fulco, C.J. 1995 An overview of dietary intakes during military exercises. Pp. 121–149 in Not Eating Enough, Overcoming Underconsumption of Military Operational Rations, B.M. Marriott, ed. A report of the Committee on Military Nutrition Research, Food and Nutrition Board, Institute of Medicine. Washington, D.C.: National Academy Press.
Banderet, L.E., and H.K. Lieberman 1989 Treatment with tyrosine, a neurotransmitter precursor, reduces environmental stress in humans. Brain Res. Bull. 22:759–762.
Bärtsch, P., M. Maggiorini, W. Schobersberger, S. Shaw, W. Rascher, J. Girard, P. Weidmann, and O. Oelz 1991 Enhanced exercise-induced rise of aldosterone and vasopressin preceding mountain sickness. J. Appl. Physiol. 71:136–143.
Beard, J.L., J.D. Haas, D. Tufts, H. Spielvogel, E. Vargas, and C. Rodriguez 1988 Iron deficiency anemia and steady-state work performance at high altitude. J. Appl. Physiol. 64:1878–1884.
Bender, P.R., R.E. McCullough, R.G. McCullough, S.Y. Huang, P.D. Wagner, A. Cymerman, A.J. Hamilton, and J.T. Reeves 1989 Increased exercise SaO2 independent of ventilatory acclimatization at 4,300 m. J. Appl. Physiol. 66:2733–2738.
Bouissou, P., J-P. Richalet, F. Galen, M. Lartigue, P. Larmignat, F. Devaux, C. Dubray, and A. Keromes 1989 Effect of β-adrenoceptor blockade on renin-aldosterone and a-ANF during exercise at altitude. J. Appl. Physiol. 67:141–146.
Boutwell, J.H., J.H. Cilley, L.R. Kransno, A.C. Ivy, and C.J. Farmer 1950 Effect of repeated exposure of human subjects to hypoxia on glucose tolerance, excretion of ascorbic acid, and phenylalanine tolerance. J. Appl. Physiol. 2:388–392.
Brebbia, D.R., R.F. Goldman, and E.R. Buskirk 1957 Water vapor loss from the respiratory tract during outdoor exercise in the cold. J. Appl. Physiol. 11:219–222.
Brooks, G.A., G.E. Butterfield, R.R. Wolfe, B.M. Groves, R.S. Mazzeo, J.R. Sutton, E.E. Wolfel, and J.T. Reeves 1991 Decreased reliance on lactate during exercise after acclimatization to 4,300 m. J. Appl. Physiol. 71:333–341.
Buskirk, E.R., and J. Mendez 1967 Nutrition, environment and work performance with special reference to altitude. Fed. Proc. 26:1760–1767.
Butterfield, G.E., J. Gates, S. Fleming, G.A. Brooks, J.R. Sutton, and J.T. Reeves 1992 Increased energy intake minimizes weight loss in men at high altitude. J. Appl. Physiol. 72:1741–1748.
Calloway, D.H., and M.S. Kurzer 1982 Menstrual cycle and protein requirements of women. J. Nutr. 112:98–108.
Carson, R.P., W.O. Evans, J.L. Shields, and J.P. Hannon 1969 Symptomatology, pathophysiology, and treatment of acute mountain sickness. Fed. Proc. 28:1085–1091.
CDC (Centers for Disease Control and Prevention) 1994 Daily dietary fat and total food energy intakes—Third National Health and Nutrition Examination Survey. Phase 1, 1989–91. Morbid. Mortal. Weekly Rep. 43(7):116–125.
Colice, G., and G. Ramirez 1985 Effect of hypoxemia on the renin-angiotensin-aldosterone system in humans. J. Appl. Physiol. 58:724–730. 1986 Aldosterone response to angiotensin II during hypoxemia. J. Appl. Physiol. 61:150–154.
Cruz, J.C., R.F. Grover, J.T. Reeves, J.T. Maher, A. Cymerman, and J.C. Denniston 1976 Sustained venoconstriction in man supplemented with CO2 at high altitude. J. Appl. Physiol. 40:96–100.
Cunningham, W.L., E.J. Becker, and F. Kreuzer 1965 Catecholamines in plasma and urine at high altitude. J. Appl. Physiol. 20:607–610.
Cymerman, A., and P.B. Rock 1994 Medical problems in high mountain environments: A handbook for medical officers. Technical Report TN 94-2. Natick, Mass.: U.S. Army Research Institute of Environmental Medicine.
DeLany, J.P., D.A. Schoeller, R.W. Hoyt, E.W. Askew, and M.A. Sharp 1989 Field use of D218O to measure energy expenditure of soldiers at different energy intakes . J. Appl. Physiol. 67:1922–1929.
Deuster, P.A., K.L. Gallagher, A. Singh, and R.D. Reynolds 1992 Consumption of a dehydrated ration for 31 days at moderate altitudes: Status of zinc, copper, and vitamin B-6. J. Am. Diet. Assoc. 92:1372–1375.
Dulloo, A.G., and D.S. Miller 1986 The thermogenic properties of ephedrine methylxanthine mixtures: Human studies. Int. J. Obes. 10:467–481.
Dulloo, A.G., J. Seydoux, and L. Girardier 1990 Dietary and pharmacological effectiveness of thermogenic stimulation in obesity treatment. Prog. Obes. Res. 135–144.
Edwards, H.T., R. Margaria, and D.B. Dill 1932 Metabolic rate, blood sugar, and the utilization of carbohydrate. Am. J. Physiol. 108:203–209.
Edwards, J.S.A., D.E. Roberts, and S.H. Mutter 1992 Rations for use in a cold environment. J. Wilderness Med. 3:27–47.
Eliot, J.W., R.A. Bader, and D.E. Bass 1949 Blood changes associated with cold diuresis. Fed. Proc. 8:41.
Forbes-Ewan, C.H., B.L.L. Morrissey, G.C. Gregg, and D.R. Waters 1989 Use of doubly labeled water technique in soldiers training for jungle warfare. J. Appl. Physiol. 67:14–18.
Fulco, C.S., and A. Cymerman 1988 Human performance and acute hypoxia. Pp. 467–95 in Human Performance Physiology and Environmental Medicine at Terrestrial Extremes, K.B. Pandolf, M.N. Sawka, and R.R. Gonzalez, eds. Indianapolis, Ind.: Benchmark Press.
Gibson, G.E., and T.E. Duffy 1981 Impaired synthesis of acetylcholine by mild hypoxic hypoxia or nitrous oxide. J. Neurochem. 36:28–33.
Goldenberg, F., J.P. Richalet, I. Onnen, and A.M. Antezana 1992 Sleep apneas and high altitude newcomers. Int. J. Sports Med. 13 (suppl. 1):S34–S36.
Gollnick, P.D. 1985 Metabolism of substrates: Energy substrate metabolism during exercise and as modified by training. Fed. Proc. 44:353–357.
Gonzalez, R.R. 1988 Biophysics of heat transfer and clothing considerations. Pp. 45–95 in Human Performance Physiology and Environmental Medicine at Terrestrial Extremes, K.B. Pandolf, M.N. Sawka, and R.R. Gonzalez, eds. Indianapolis, Ind.: Benchmark Press.
Gonzalez, R.R., L.A. Stephenson, W.L. Holden, and M.A. Kolka 1985 Respiratory heat loss at altitude: Effect of ![]() o2 peak. Physiologist 27:230.
o2 peak. Physiologist 27:230.
Gray, E. LeB., F.C. Consolazio, and R.M. Kark 1951 Nutritional requirements for men at work in cold, temperate and hot environments. J. Appl. Physiol. 4:270–275.
Green, H.J., J.R. Sutton, P.M. Young, A. Cymerman, and C.S. Houston 1989 Operation Everest II: Muscle energetics during maximal exhaustive exercise. J. Appl. Physiol. 66:142–150.
Greenleaf, J.E., and M.H. Harrison 1986 Water and electrolytes. Pp. 107–124 in Nutrition and Aerobic Exercise, D.K. Layman, ed. Washington, D.C.: American Chemical Society.
Gregory, R.L., ed. 1987 The Oxford Companion to the Mind. New York: Oxford University Press.
Grover, R.F, J.V. Weil, and J.T. Reeves 1986 Cardiovascular adaptation to exercise at high altitude. Exerc. Sports Sci. Rev. 14:269–302.
Hackett, P.H., R.C. Roach, and J.R. Sutton 1989 High altitude medicine. Pp. 1–34 in Management of Wilderness and Environmental Emergencies, P.S. Auerbach and E.C. Geehr, eds. St. Louis, Mo.: CV Mosby Company.
Hackney, A.C., C.S. Curley, and B.J. Niclas 1991 Physiological response to submaximal exercise in mid-follicular, ovulatory and mid-luteal phases of the menstrual cycle. Scand. J. Med. Sci. Sports 1:94–98.
Hall, V.E., F.P. Attardo, and J.H. Perryman 1948 Influence of dinitrophenol on body temperature threshold for thermal polypnea. Proc. Soc. Exp. Biol. Med. 69:413–415.
Hannon, J.P., and J.A. Vogel 1977 Oxygen transport during early altitude acclimatization: A perspective study. Eur. J. Physiol. 36:285–297.
Hannon, J.P., G.J. Klain, D.M. Sudman, and F.J. Sullivan 1976 Nutritional aspects of high altitude exposure in women. Am. J. Clin. Nutr. 29:604–613.
Hansen, J.E., C.W. Harris, and W.O. Evans 1967 Influence of elevation of origin, rate of ascent and a physical conditioning program on symptoms of acute mountain sickness. Milit. Med. 132:585–592.
Heyes, M., F. Manfredi, D. Robertshaw, M. Weinberger, N. Fineberg, and G. Robertson 1982 Acute effects of hypoxia on renal and endocrine function in normal humans. Am. J. Physiol. 243:R265–R270.
Hogan, R., T. Kotchen, A. Boyd, and L. Hartley 1973 Effect of altitude on renin-aldosterone system and metabolism of water and electrolytes. J. Appl. Physiol. 35:385–390.
Hoon, R.S., S.C. Sharma, V. Balasubramanian, K.S. Chadha, and O.P. Mathew 1976 Urinary catecholamine excretion on acute induction to high altitude (3,658 m). J. Appl. Physiol. 41:631–633.
Horvath, S.M. 1981 Exercise in a cold environment. Exerc. Sports Sci. Rev. 9:221–263.
Houston, C.S. 1982 Acclimatization. Pp. 158–160 in Hypoxia: Man at Altitude, J.R. Sutton, N.L. Jones, and C.S. Houston, eds. New York: Thieme-Stratton, Inc.
Hoygaard, A. 1941 Studies on the nutrition and physio-pathology of Eskimos. Det norske videnskapsakademis skrifter. Mat.-Naturv. Klasse no. 9, Oslo.
Hoyt, R.W., and A. Honig 1996 Body fluid and energy metabolism at high altitude. Pp. 1277–1289 in Handbook of Physiology, Section 4: Environmental Physiology, C.M. Blatteis and M.J. Fregley, eds. New York: Oxford University Press for the American Physiological Society.
Hoyt, R.W., T.E. Jones, T.P. Stein, G.W. McAninch, H.R. Lieberman, E.W. Askew, and A. Cymerman 1991 Doubly labeled water measurement of human energy expenditure during strenuous exercise. J. Appl. Physiol. 71:16–22.
Hoyt, R.W., T.E. Jones, C.J. Baker-Fulco, D.A. Schoeller, R.B. Schoene, R.S. Schwartz, E.W. Askew, and A. Cymerman 1994 Doubly labeled water measurement of human energy expenditure during exercise at high altitude. Am. J. Physiol. 35:R966–R971.
IOM (Institute of Medicine) 1991 Fluid Replacement and Heat Stress. A report of the Committee on Military Nutrition Research, Food and Nutrition Board. Washington, D.C.: National Academy Press.
1992 Letter report: Calorie-dense rations. In Committee on Military Nutrition Research Activity Report 1986–1992. A report of the Committee on Military Nutrition Research, Food and Nutrition Board. Washington, D.C.: National Academy Press.
1993 Nutritional Needs in Hot Environments, Applications for Military Personnel in Field Operations. A report of the Committee on Military Nutrition Research, Food and Nutrition Board. Washington, D.C.: National Academy Press.
1994 Food Components to Enhance Performance, An Evaluation of Potential Performance-Enhancing Food Components for Operational Rations. A report of the Committee on Military Nutrition Research, Food and Nutrition Board. Washington, D.C.: National Academy Press.
1995a Not Eating Enough, Overcoming Underconsumption of Military Operational Rations. A report of the Committee on Military Nutrition Research, Food and Nutrition Board. Washington, D.C.: National Academy Press.
1995b Recommendations for Research on the Health of Military Women. A report of the Committee on Defense Women's Health Research, Food and Nutrition Board. Washington, D.C.: National Academy Press.
Issekutz, B., Jr., K. Rodahl, and N.C. Birkhead 1962 Effect of severe cold stress on the nitrogen balance of men under different dietary conditions. J. Nutr. 78:189–197.
Jacobs, I. 1993 Fueling shivering in humans during cold weather immersion. Pp. 6.1–6.3 in The Support of Air Operations under Extreme Hot and Cold Weather Conditions. Advisory Group for Aerospace Research and Development (AGARD) Conference Proceedings 450. Neuilly-sur-Seine, France: North Atlantic Treaty Organization.
Jain, S.C., J. Bardhan, Y. Swamy, B. Krishna, and H. Nayar 1980 Body fluid compartments in humans during acute high-altitude exposure. Aviat. Space Environ. Med. 51:234–236.
Jain, S.C., Y. Swamy, A. Grover, and H. Nayar 1981 Body water metabolism in high altitude natives during and after a stay at sea level. Int. J. Biometeorol. 25:47–52.
Jennings, J.R., C.F. Reynolds III, D.S. Bryant, S.R. Berman, D.J. Buysse, R.E. Dahl, C.C. Hoch, and T.H. Monk 1993 Peripheral thermal responsivity to facial cooling during sleep. Psychophysiol. 30(4):374–382.
Jéquier, E. 1993 Body weight regulation in humans. The importance of nutrient balance . News in Physiological Sciences 8:273–277.
Johnson, R.E., and R.M. Kark 1947 Environment and food intake in man. Science 105:378–379.
Jones, P.J.H., I. Jacobs, A. Morris, and M.B. Ducharme 1993 Adequacy of food rations in soldiers during an arctic exercise measured using doubly labeled water. J. Appl. Physiol. 75:1790–1797.
Jones, T.E., R.W. Hoyt, C.J. Baker, C.B. Hintlian, P.S. Walczak, R.A. Kluter, C.P. Shaw, D. Shilling, and E.W. Askew 1990 Voluntary consumption of a liquid carbohydrate supplement by Special Operations Forces during a high altitude, cold weather field training exercise. Technical Report T20-90. Natick, Mass.: U.S. Army Research Institute of Environmental Medicine.
Kandel, E.R., J.H. Schwartz, and T.M. Jessell 1991 Principles of Neural Science, 3rd ed. New York: Elsevier Science Publishing Company, Inc.
Kark, R.M., R.R.M. Croome, J. Cawthorpe, D.M. Bell, A. Bryans, and R.J. MacBeth. 1948 Observations on a mobile arctic force. J. Appl. Physiol. 1:73–93.
Keeton, R.W., E.H. Lambert, N. Glickman et al. 1946 The tolerance of man to cold as affected by dietary modifications: Proteins vs. carbohydrates, and the effect of vanable protective clothing. Am. J. Physiol. 146:66–83.
King, N., S.H. Mutter, D.E. Roberts, M.R. Sutherland, and E.W. Askew 1993 Cold weather field evaluation of the 18-man Arctic Tray Pack Ration Module, the Meal, Ready-to-Eat, and the Long Life Ration Packet. Milit. Med. 158:458–465.
Kleiber, M. 1961 The Fire of Life. New York: John Wiley and Sons.
Kotchen, T.A., R.P. Hogan, A.E. Boyd, T.K. Li, H.C. Sing, and J.W. Mason 1973 Renin, noradrenaline and adrenaline responses to simulated altitude. Clin. Sci. 44:243–251.
LeBlanc, J. 1957 Effect of environmental temperature on energy expenditure and caloric requirements. J. Appl. Physiol. 10:281–283.
1975 Man in the Cold. Springfield, Ill.: Charles C Thomas.
Lennquist, S., P.O. Granberg, and B. Wedin 1974 Fluid balance and physical work capacity in humans exposed to cold. Arch. Environ. Health 29:241–249.
Lewis, H.E., J.P. Masterton, and S. Rosenbaum 1960 Body weight and skinfold thickness of men on a polar expedition. Clin. Sci. 19:551–562.
Lewis, T. 1930 Observations upon the reactions of the human skin to cold. Heart 15:177–181.
Lieberman, H.R. 1994 Tyrosine and stress: Human and animal studies. Pp. 277–299 in Food Components to Enhance Performance, An Evaluation of Potential Performance-Enhancing Food Components for Operational Rations, B.M. Marriott, ed. A report of the Committee on Military Nutrition Research, Food and Nutrition Board, Institute of Medicine. Washington, D.C.: National Academy Press.
Lieberman, H.R., L.E. Banderet, and B. Shukitt-Hale 1990 Tyrosine protects humans from the adverse effects of acute exposure to hypoxia and cold. Abstr. Soc. Neuro. 16:272.
Lieberman, H.R., B. Shukitt-Hale, L.E. Banderet, and J.F. Glenn 1991 Exposure to hypobaric hypoxia: A method for the comparison of neuropsychologic tests in humans. Abstr. Soc. Neuro. 17:1233.
Lukaski, H., and S. Smith In Effects of altered vitamin and mineral nutritional status on temperature regulation and Press thermogenesis in the cold. In Handbook of Physiology. Washington, D.C.: American Physiological Society.
Luo, S., L. Villamil, C.J. Watkins, and H.R. Lieberman 1992 Further evidence tyrosine reverses behavioral deficits caused by cold exposure. Abstr. Soc. Neuro. 18(1):716.
Luo, S., E.T.S. Li, and H.R. Lieberman 1993 Tyrosine increases hypothermia-induced norepinephrine (NE) release in rat hippocampus assessed by in vivo microdialysis. Abstr. Soc. Neuro. 19:1452.
Lyons, P.M., A.S. Truswell, M. Mira et al. 1989 Reduction of food intake in the ovulatory phase of the menstrual cycle. Am. J. Clin. Nutr. 49:1164–1168.
Maher, J.T., L.G. Jones, L.H. Hartley, G. Williams, and L. Rose 1975 Aldosterone dynamics during graded exercise at sea level and high altitude. J. Appl. Physiol. 39:18–22.
Maresh, C., B. Noble, K. Robertson, and J. Harvey, Jr. 1985 Aldosterone, cortisol, and electrolyte responses to hypobaric hypoxia in moderate-altitude natives. Aviat. Space Environ. Med. 56:1078–1084.
Martineau, L., and I. Jacobs 1988 Muscle glycogen utilization during shivering thermogenesis in humans. J. Appl. Physiol. 65:2046–2050.
1989 Muscle glycogen availability and temperature regulation in humans. J. Appl. Physiol. 66:72–78.
Mathew, L., S.S. Purkayastha, R. Singh, and J.S. Gupta 1986 Influence of aging on the thermoregulatory efficiency of man. Int. J. Biometeorol. 30:137–145.
Mazzeo, R.S., P.R. Bender, G.A. Brooks, G.E. Butterfield, B.M. Groves, J.R. Sutton, E.E. Wolfel, and J.T. Reeves 1991 Arterial catecholamine responses during exercise with acute and chronic high-altitude exposure. Am. J. Physiol. 261:E419–E424.
McDougall, J.D., G.R. Ward, D.G. Sale, and J.R. Sutton 1977 Muscle glycogen repletion after high-intensity intermittent exercise. J. Appl. Physiol. 42:129–132.
Meda, di E 1955 Dispendio di base dell'uomo in montagna. Arch. di Fisiol. 55:144–151.
Meijer G.A.,K.R. Westerterp, W.H. Saris, and F. ten Hoor 1992 Sleeping metabolic rate in relation to body composition and the menstrual cycle. Am. J. Clin. Nutr. 55:637–640.
Milan, F.A., and K. Rodahl 1961 Calorie requirements of man in the Antarctic. J. Nutr. 75:152–157.
Milledge, J.S. 1992 Respiratory water loss at altitude. Newslett. Int. Soc. Mountain Med. 2:5–7.
Milledge, J.S., D. Catley, E. Williams, W. Withey, and B. Minty 1983 Effect of prolonged exercise at altitude on the renin-aldosterone system. J. Appl. Physiol. 55:413–418.
Mitchell, H.H., and M. Edman 1951 Nutrition and Climatic Stress. Springfield, Ill.: Charles C Thomas.
Mitchell, J.W., E.R. Nadel, and J.A.J. Stolwijk 1972 Respiratory weight losses during exercise. J. Appl. Physiol. 22:474–476.
Moncloa, F., M. Gomez, and H. Anda 1965 Plasma catecholamines at high altitudes. J. Appl. Physiol. 20:1329-1331.
Montain, S.J., and E.F. Coyle 1992 Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 73:1340–1350.
Muza, S.R., A.J. Young, M.N. Sawka, J.E. Bogart, and K.B. Pandolf 1988 Respiratory and cardiovascular responses to cold stress following repeated cold water immersion. Undersea Biomed. Res. 15:165–178.
Nair, C.S., M.S. Malhotra, and P.M. Gopinath 1971 Effect of altitude and cold acclimatization on the basal metabolism in man. Aerosp. Med. 42:1056–1059.
Nelson, M. 1982 Psychological testing at high altitudes. Aviat. Space Environ. Med. 53:122–126.
Normand, H., M. Barragan, O. Benoit, O. Bailliart, and J. Raynaud 1990 Periodic breathing and O2 saturation in relation to sleep stages at high altitude. Aviat. Space Environ. Med. 61:229–235.
NRDEC (U.S. Army Natick Research, Development and Engineering Center) 1992 Operational Rations of the Department of Defense. Natick Pamphlet 30-2. Natick, Mass.: U.S. Army Natick Research, Development, and Engineering Center.
Olsen, N., I-L. Kanstrup, J-P. Richalet, J. Hansen, G. Plazen, and F-X. Galen 1992 Effects of acute hypoxia on renal and endocrine function at rest and during graded exercise in hydrated subjects. J. Appl. Physiol. 73:2036–2043.
Olsen, N., J. Hansen, I-L. Kanstrup, J-P. Richalet, and P. Leyssac 1993 Renal hemodynamics, tubular function, and response to low-dose dopamine during acute hypoxia in humans. J. Appl. Physiol. 74:2166–2173.
Orth, G.L. 1949 Food requirements in the arctic regions. Milit. Surg. March:204–206.
Phillips, R., K. Knox, W. House, and H. Jordan 1969 Metabolic responses in sheep chronically exposed to 6,200 m simulated altitude. Fed. Proc. 28:974–977.
Raff, H., R. Sandri, and T. Segerson 1986 Renin, ACTH, and adrenocortical function during hypoxia and hemorrhage in conscious rats. Am. J. Physiol. 250:R240–R244.
Ramirez, G., M. Hammond, S. Agosti, P. Bittle, J. Dietz, and G. Colice 1992 Effects of hypoxemia at sea level and high altitude on sodium excretion and hormonal levels. Aviat. Space Environ. Med. 63:891–898.
Rauch, T.M., and H.R. Lieberman 1990 Pretreatment with tyrosine reverses hypothermia induced behavioral depression. Brain Res. Bull. 24:147–150.
Reeves, J.T., R.S. Mazzeo, E.E. Wolfel, and A.J. Young 1992 Increased arterial pressure after acclimatization to 4,300 m: Possible role of norepinephrine. Int. J. Sports Med. 13 (Suppl. 1):S18–S21.
Reynafarje, C., and J. Ramos 1961 Influence of altitude changes on intestinal iron absorption. J. Lab. Clin. Med. 57:848–855.
Roberts, A.C., G.E. Butterfield, J.T. Reeves, E.E. Wolfel, and G.A. Brooks In Acclimatization to 4,300 m altitude decreases reliance on fat as a substrate. J. Appl. Press a Physiol.
Roberts, A.C., J.T. Reeves, G.E. Butterfield, R.S. Mazzeo, J.R. Sutton, E.E. Wolfel, and In G.A. Brooks Press b-Altitude and B-Blockade augment glucose utilization during exercise. J. Appl. Physiol.
Rodahl, K. 1954 Nutritional requirements in cold climates. J. Nutr. 53:575–588.
Rodahl, K., S.M. Horvath, N.C. Birkhead, and B. Issekutz, Jr. 1962 Effects of dietary protein on physical work capacity during severe cold stress. J. Appl. Physiol. 17:763–767.
Rose, M.S., C.S. Houston, C.S. Fulco, G. Coates, D. Carlson, J.R. Sutton, and A. Cymerman 1987 Operation Everest II: Effects of a simulated ascent to 29,000 feet on nutrition and body composition. Technical Report T15-87. Natick, Mass.: U.S. Army Research Institute of Environmental Medicine.
Rupp, J.W., R.A. Stone, and B.E. Gunning 1978 Sodium versus sodium-fluid restriction in hemodialysis: Control of weight gains and blood pressures. Am. J. Clin. Nutr. 31(10):1952–1955.
Sahlin, K. 1986 Metabolic changes limiting muscle performance. Pp. 323–344 in Biochemistry of Exercise VI, B. Saltin, ed. International Series on Sports Sciences, vol. 16. Champaign, Ill.: Human Kinetics.
Sawka, M.N. 1992 Physiological consequences of hypohydration: Exercise performance and thermoregulation. Med. Sci. Sports Exerc. 24:657–670.
Sawka, M.N., and K.B. Pandolf 1990 Effects of body water loss on exercise performance and physiological functions. Pp. 1–38 in Perspectives in Science. Vol. 3: Fluid Homeostasis During Exercise, C.V. Gisolfi and D.R. Lamb, eds. Carmel, Ind.: Benchmark Press, Inc.
Schoeller, D.A. 1990 How accurate is self-reported dietary energy intake? Nutr. Rev. 48:373–379.
Sellers, E.A. 1972 Hormones in the regulation of body temperatures. Pp. 57–71 in The Pharmacology of Thermoregulation, E. Schonbaum and P. Lomax, eds. Basel, Switzerland: Karger.
Shigeoka, J., G. Colice, and G. Ramirez 1985 Effect of normoxemic and hypoxemic exercise on renin and aldosterone. J. Appl. Physiol. 59:142–148.
Shukitt, B.L., and L.E. Banderet 1988 Mood states at 1600 and 4300 meters terrestrial altitude. Aviat. Space Environ. Med. 59:530–532.
Shukitt-Hale, B., T.M. Rauch, and R. Foutch 1990 Altitude symptomatology and mood states during a climb to 3630 m. Aviat. Space Environ. Med. 61:225–228.
Shukitt-Hale, B., L.E. Banderet, and H.R. Lieberman 1991a Relationships between symptoms, moods, and performance, and acute mountain sickness at 4700 meters. Aviat. Space Environ. Med. 62:865–869.
Shukitt-Hale, B., T. Kadar, A. Levy, M.J. Stillman, J.A. Devine, and H.R. Lieberman 1991b Morphology and muscarinic receptor density in the rat brain following exposure to hypobaric hypoxia. Abstr. Sco. Neuro. 17:1532.
Shukitt-Hale, B., M.J. Stillman, A. Levy, J.A. Devine, and H.R. Lieberman 1993a Nimodipine prevents the in vivo decrease in hippocampal extracellular acetylcholine produced by hypobaric hypoxia. Brain Res. 621:291–295.
Shukitt-Hale, B., M.J. Stillman, B.E. Marlowe, D.I. Welch, R.L. Galli, J.A. Devine, A. Levy, and H.R. Lieberman 1993b Hypobaric hypoxia adversely affects spatial memory in an exposure-dependent fashion. Abstr. Soc. Neuro. 19:363.
Shurtleff, D., J.R. Thomas, S.T. Ahlers, and J. Schrot 1993 Tyrosine ameliorates a cold-induced delayed matching-to-sample performance decrement in rats. Psychopharmacol. (Berl.) 112:228–232.
Shurtleff, D., J.R. Thomas, J. Schrot, K. Kowalski, and R. Harford 1994 Tyrosine reverses a cold-induced memory deficiency in humans. Pharmacol. Biochem. Behav. 47:935–941.
Singh, M., S. Jain, S. Rawal, H. Divekar, R. Parshad, A. Tyagi, and K. Sinha 1986 Comparative study of acetazolamide and spironolactone on body fluid compartments on induction to high altitude. Int. J. Biometeorol. 30:33–41.
Singh, M., S. Rawal, A. Tyagi, M. J. Bhagat, R. Parshad, and H. Divekar 1988 Changes in body fluid compartments on re-induction to high altitude and effect of diuretics . Int. J. Biometeorol. 32:36–40.
Singh, M., S. Rawal, and A. Tyagi 1990 Body fluid status on induction, reinduction and prolonged stay at high altitude of human volunteers. Int. J. Biometeorol. 34:93–97.
Slater, J., R. Tuffley, E. Williams, C. Beresford, P. Sonksen, R. Edwards, R. Ekins, and M. McLaughlin 1969a Control of aldosterone secretion during acclimatization to hypoxia in man. Clin. Sci. 37:327–341.
Slater, J., E. Williams, R. Edwards, R. Ekins, P. Sonksen, C. Beresford, and M. McLaughlin 1969b Potassium retention during the respiratory alkalosis of mild hypoxia in man: Its relationship to aldosterone secretion and other metabolic changes. Clin. Sci. 37:311–326.
Stephenson, L.A., and M.A. Kolka 1993 Thermoregulation in women. Exerc. Sports Sci. Rev. 21:231–262.
Stock, M.J., N.G. Norgan, A. Ferro-Luzzi, and E. Evans 1978 Effect of altitude on dietary-induced thermogenesis at rest and during light exercise in man. J. Appl. Physiol. 45:345–349.
Sutton, J.R., G.W. Viol, G.W. Gray, M. McFadden, and P.M. Keane 1977 Renin, aldosterone, electrolyte, and cortisol responses to hypoxic decompression. J. Appl. Physiol. 43:421–424.
Sutton, J.R., C.S. Houston, A.L. Mansell, M.D. McFadden, P.M. Hackett, J.R.A. Rigg, and A.C.P. Powles 1979 Effect of acetazolamide on hypoxemia during sleep at high altitude. N. Engl. J. Med. 301:1329–1331.
Swain, H.L., F.M. Toth, F.C. Consolazio, W.H. Fitzpatrick, D.I. Allen, and C.J. Koehn 1949 Food consumption of soldiers in a subarctic climate. J. Nutr. 38:63–72.
Tatsumi, K., B. Hannhart, and L.G. Moore 1995 Influences of sex steroids on ventilation and ventilatory control. Pp. 829–864 in Regulation of Breathing, 2nd ed., J. Dempsey and A. Pack, eds. New York: Marcel Dekker.
Terzioglu, M., and R. Aykut 1954 Variations in basal metabolic rate at 1.85 km altitude. J. Appl. Physiol. 7:329–332.
Thérien, M., J. LeBlanc, O. Héroux, and L.P. Dugal 1949 Effets de l'acide ascorbique sur plusiers variables biologiques normalement affectées par le froid. Can. J. Res. (sect. E) 27:349–363.
Toner, M.M., and W.D. McArdle 1988 Physiological adjustments of man to the cold. Pp. 361–399 in Human Performance Physiology and Environmental Medicine at Terrestrial Extremes, K.B. Pandolf, M.N. Sawka, and R.R. Gonzalez, eds. Indianapolis, Ind.: Benchmark Press.
Toner, M.M., M.N. Sawka, and K.B. Pandolf 1984 Thermal responses during arm and leg and combined arm-leg exercise in water. J. Appl. Physiol. 56:1355–1360.
Tune, G.S. 1964 Psychological effects of hypoxia: Review of certain literature from the period 1950 to 1963. Percept. Mot. Skills 19:551–562.
USDA (U.S. Department of Agriculture) 1995 Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans , 1995. Washington, D.C.: Government Printing Office.
U.S. Departments of the Army, the Navy, and the Air Force 1985 Army Regulation 40-25/Naval Command Medical Instruction 10110.1/Air Force Regulation 160-95. ''Nutrition Allowances, Standards, and Education." May 15. Washington, D.C.
Vallerand, A.L., and I. Jacobs 1989 Rates of energy substrate utilization during human cold exposure. Eur. J. Appl. Physiol. 58:873–878.
Vallerand A.L.,I. Jacobs, and M.F. Kavanagh 1989 Mechanism of enhanced cold tolerance by an ephedrine-caffeine mixture in humans. J. Appl. Physiol. 67(1):438–444.
Van Liere, E.J., and J.C. Stickney 1963 Hypoxia. Chicago: University of Chicago Press.
Veicsteinas, A., G. Ferretti, and D.W. Rennie 1982 Superficial shell insulation in resting and exercising men in cold water. J. Appl. Physiol. 52:1557–1564.
Wallenberg, L.R., and P.O. Granberg 1976 Is cold-diuresis a pressure diuresis? Pp. 49–55 in Circumpolar Health, Proceedings of Third International Symposium, R.J. Shephard and S. Itah, eds. Toronto: University of Toronto Press.
Webb, P. 1986 24-hour energy expenditure and the menstrual cycle. Am. J. Clin. Nutr. 44:614–619.
Weil, J.V. 1985 Sleep at high altitude. Clin. Chest Med. 6:615–621.
White, D.P., K. Gleeson, C.K. Pickett, A.M. Rannels, A. Cymerman, and J.V. Weil 1987 Altitude acclimatization: Influence on periodic breathing and chemoresponsiveness during sleep. J. Appl. Physiol. 63:401–412.
Withey, W., J. Milledge, E. Williams, B. Minty, E. Bryson, N. Luff, M. Older, and J. Beeley 1983 Fluid and electrolyte homeostasis during prolonged exercise at altitude. J. Appl. Physiol. 55:409–412.
Wurtman, R.J., and H.R. Lieberman 1989 Use of tyrosine and other nutrients to protect against stress and to enhance and sustain performance. Pp. 67–77 in Stress: Neurochemical and Humoral Mechanisms, Vol. 1, G.R. Van Loon, R. Kvetnansky, R. McCarty, and J. Axelrod, eds. New York: Gordon and Breach.
Young, A.J. 1990 Energy substrate utilization during exercise in extreme environments. Exerc. Sports Sci. Rev. 18:65–117.
1991 Effects of aging on human cold tolerance. Exp. Aging Res. 17:205–213.
Young, A.J., and P.M. Young 1988 Human acclimatization to high terrestrial altitude. Pp. 467–495 in Human Performance Physiology and Environmental Medicine at Terrestrial Extremes, K.B. Pandolf, M.N. Sawka, and R.R. Gonzalez, eds. Indianapolis, Ind.: Benchmark Press.
Young, A.J., W. J. Evans, A. Cymerman, K. B. Pandolf, J. J. Knapik, and J. T. Maher 1982 Sparing effect of chronic high-altitude exposure on muscle glycogen utilization, J. Appl. Physiol. 52:857–862.
Young, A.J., S.R. Muza, M.N. Sawka, R.R. Gonzalez, and K.B. Pandolf 1986a Human thermoregulatory responses to cold air are altered by repeated cold water immersion. J. Appl. Physiol. 60:1542–1548.
Young, A.J., M.S. Rose, J.R. Sutton, H.J. Green, A. Cymerman, and C.S. Houston 1986b Operation Everest II: Plasma lipid and hormonal responses during a simulated ascent of Mt. Everest. J. Appl. Physiol. 66:1430–1435.
Young, A.J., S.R. Muza, M.N. Sawka, and K.B. Pandolf 1987 Human vascular fluid responses to cold stress are not altered by cold acclimatization. Undersea Biomed. Res. 14:215–228.
Young, A.J., M.N. Sawka, P.D. Neufer, S.R. Muza, E.W. Askew, and K.B. Pandolf 1989 Thermoregulation during cold water immersion is unimpaired by low muscle glycogen levels. J. Appl. Physiol. 66:1809–1816.
| This page in the original is blank. |
























































