The Workforce For Health
Edward H. O'Neil, Ph.D., M.P.A.
Associate Professor of Family and Community Medicine, and Codirector, Center for the Health Professions, University of California, San Francisco; Executive Director, Pew Health Professions Commission
I will limit my remarks to two things. The first is to give you some sense of the challenges to the health profession, which have already been addressed by others. Then I would like to focus by looking at specific health professions and offer some comments on the academic health center and its future.
Figure 1 is a picture of the health care system in the United States, circa 1981. Essentially, I would like you to focus on the reality that all of the rules we developed about health care over 50 years—who could practice, what they could practice, where they could practice, how much they were reimbursed, who provided oversight, and who did the policing—were all controlled by the professions. There was token, if any, public input into the design of that system. It emerged in the 50 years after the Second World War principally because in 1950 this country had 7 percent of the world's population and sold 49 percent of the world's goods and services. We could afford a system that was structured in that way.
Now, what is emerging clearly—whatever it may be called—is a system of integrated delivery, whether it is managed, profit driven, or not-for-profit. That system will have essentially three values: One is maintaining or lowering the cost of care, which is essentially the only value that is operative right now and will be for the next four or five years. The second is increasing patient satisfaction as a consumer. We can tell ourselves all we want about the sanctity of the patient–physician relationship, but the reality is that patients have not perceived this as something that has been responsive to their needs and have felt unempowered in that environment. Although the relationship between the provider and the patient is considered the most sacred relationship in health, I suspect that the most important relationship is between one-
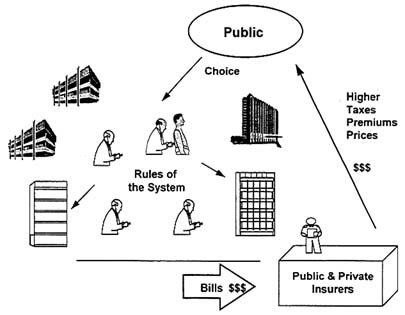
Figure 1 Health care in the United States, circa 1981.
self and one's health. The final value involves improving the quality of patient care outcomes.
The system is moving faster now than even the most aggressive prognosticators thought possible as recently as two or three years ago. By the end of this decade, I believe that in most major markets of this country, 90–95 percent of the population will be enrolled in some sort of integrated system, not owned necessarily all in a single place, but integrated in the sense of long-term contracts or exclusive contracts. Already, in northern California; Portland, Oregon; Seattle, Washington; and the Twin Cities, such patterns of organization are emerging.
The nature of the integration is almost unimportant; horizontal or vertical integration is almost unimportant. However, the size of the system is critical. How the systems come together is something for consultants and attorneys to work on, not something that will have anything ultimately to do with the health of the nation.
This integration is occurring in three phases. Let me focus on one dimension of each, because in each of the three phases there is a cost-control and system value-added dimension that presses severely on health professionals and their work.
The first stage is assembly—the cobbling together of systems. That is going on right now. To try to make sense out of this and then project into the future is foolish because, next year, someone will buy the system on which that analysis is based and the analysis will be useless. In this first phase, limiting access and reducing fees are essentially the means of controlling
costs. This is what is pressing most on professionals as they take on the responsibility for that risk.
The second phase sounds terrific—the integration of this far-flung set of health care resources in management information and decision support systems. This is the promise, the upside.
The downside in integration is having to remove excess capacity from the system. In independent hospitals it made sense to have an operating census of 20 percent. In putting together a system of four or five hospitals, it makes no sense to have each operating with that kind of enrollment. So that is where we remove perhaps 30–50 percent of the hospitals; maybe 40–60 percent of the hospital beds; from 100,000 to 150,000 of the physicians, all of them specialists; and perhaps 200,000–300,000 hospital-based nurses—not because we change the intensity of care delivered in the hospital, but because the hospital is not operating any longer—the work force simply is not there.
Finally, we arrive at a management phase. If there is a silver lining in this rather brutal process, it is in management. If there is an American genius in what we are about, it is bringing a brand new approach to the organization of health care. This not only will redesign the health production function to yield the higher value that has been discussed, but will also change the process by which we produce care. Determine what the inputs are, professional and other, that will actually produce a particular outcome, and then radically redesign in that context the practice of health professionals.
Why the professions are key to this change is obvious, but let me mention a few reasons. There are 10.5 million health care workers in the country, and we spend about $20 billion–$25 billion on education across the continuum of health professions. Health care itself is a labor-intensive process: 70–80 percent of the expenditures in any operating unit will be for labor costs. The professions control cost, waste, and innovation by how they work.
The existing professional structures are not amenable to change. We have essentially a set of 19th-century work rules operating in a 21st-century institution. We have this system that has been dominated by supply. What is it that we want to provide? What is best for us? How do we want to array the community needs to increase demand?
If you do not think we have had a bias toward the supply side in responding to the public's problems, why is it that we build neonatology units in response to low birth weight and prematurity?
All of the professions are tied to this aging model. Medicine is overly focused on individual practitioners providing clinical service to individual patients who present with acute care treatment needs.
Nursing is oriented to an undifferentiated practice across most ranges of nursing today, particularly within a hospital setting. By continuing to operate in this way, the emerging system is demanding different roles for nurses.
Pharmacy is still focused almost exclusively on the physical delivery of a drug, even though we know that the guarantees of quality and other di-
mensions of value added by the pharmacist can be provided in many other settings.
In allied health, the more than 200 different allied health professions still define themselves by the technology or the therapy that created them and build walls around those technologies and therapies to protect themselves.
The transition that is likely to occur over the next decade is one from protectionism, to use a very stark and harsh word, to pragmatism for the professions: from professions defined by a scope of practice—I might even say captured by and suffering from a scope of practice—to a health system that is redesigning itself to meet new values. These values involve particularly, a capacity to lower costs, to deliver health quality at a higher outcome, and to enhance patient satisfaction. This may or may not have anything to do with the scope of practice. The health system itself increasingly has the power to make those decisions and looks to the professions to assist it.
Professions have been unwilling or unable to capture or control quality. There is nothing in 40 years of the literature to indicate that the professions have been up to that task, unless the violation of quality was so egregious as to involve the criminal justice system. Then and only then do the professions have a record of actually policing their own in any effective way.
So now we have quality standards not only developed from the system but demanded by the purchasers of the system. That power shift, more than anything else, will drive and create the new reality.
Controlling information and access to that information has been central since the Middle Ages to the definition of what a profession is about, but we now know that information is abundant, cheap.
The first step is the redesign of the health workplace. This is going on right now with little, if any, public discussion. The market-driven changes are pushing faster and deeper into reform than anything proposed by the Clinton administration.
The next step is reregulation of professional practice, not its deregulation. We do not need to leave the professions or the public out in the cold against these terrible mechanisms of the market—the profit-driven managed care systems. What we need is a set of regulations that serve the public interest at the end of this century, not the end of the last century. Then must come right-sizing—the politically correct word. There is some upsizing necessary in certain professions, but for a couple of important professions, there must be some downsizing. Finally, there is the restructuring of education.
Redesign of the workplace focuses on outcomes, quality, cost, and the information base. It is performance driven. We have touched on all of these.
Flexible, innovative, and adaptable are not words that have been hall-marks of the health professions. We must recognize those professions that once were viable but are no longer useful, and we need to get on with the process of team-oriented education and training. Then costs can be determined.
Reregulate professional practice. Practice acts must be based on demonstrated initial competence, and professional boards must focus on changing
public and care system needs. The role of the consumer in all of this must be enlarged. Continuing competency requirements must be required as a part of that. The entire process must be focused on quality performance, or it simply will not be worth the time invested in it.
Right-size the professions or reduce the number of physicians produced. Too many physicians are being produced by both the graduate and the undergraduate medical education systems. This number cannot be sustained in the system as it is now, much less as it will become.
Reduce and redirect nursing practice toward four-year and advanced practice programs. The size of nursing programs at the diploma and associate degree level must be reduced.
Reduce the number of pharmacists produced. In a system that will rapidly take advantage of information, communication, and transportation technology to distribute drugs, we simply do not need pharmacists handling drugs unless you like the opportunity to visit your local drugstore.
Expand public health programs and increase the number of public health professionals. Several others have said that this is a great day for public health. In the evolution of the management phase, we eventually move to management of the health of populations. We do not have them integrated enough into clinical disciplines. The number of multiskilled allied health workers must increase—not the number of technically driven allied health workers, but the number of allied health workers who are multiskilled.
Make education accountable for cost, time, and performance. If you liked managed health care, you are going to love managed education, because it will be in terms of performance and accountability standards. New skills must be created and offered for professional education.
Remove time and place boundaries. It makes no sense to have a resource tied up in an institution. Move it to an ambulatory community setting. Clearly, we have made major strides in that direction.
Merge with integrated care systems. It makes no sense to affirm a department of community and family medicine today but build it like a department of medicine in 1970. That was the wrong image: research dollars were abundant, and patients were coming into the hospital. To build a primary care department today, build it at Kaiser Permanente; then figure out how to appoint the faculty back to your academic health center. Then create a funding-based educational mention not to research, not to service, not to indirect recovery.
To speak specifically about a few professions, physicians are oversupplied. Figure 2 is a picture of one estimate of specialist positions from the Pew Health Professions Commission. If we continue in this way until 2020, there will be perhaps 190,000 too many specialists for that environment. The horizontal bars represent high and low projections from John Weiner for managed care enrollment.
The challenge for medicine is to build professional identity around managing risk and adding value, not around a set of practices, not around a scope

Figure 2 Forces reshaping physician practice.
of practice, and not around dominance within the system. What can physicians do whose quality cannot be matched by other professions?
Enhance relationship-based care. I believe that the individual ultimately will be looked upon as the place where we add value to health care ourselves. The physician–patient relationship is important, but it needs to be recaptured because frankly it is somewhat tarnished.
Reorient on a primary care paradigm. One obvious feature of this emerging managed care system is that it will be integrated through the primary care disciplines, not through specialty disciplines. This is not to denigrate specialty disciplines; they are still critically important for what they do. They just seem to have proven to be a very expensive way to integrate the entire health care system.
Create new relationships between primary care and specialty care. The relationship must be basically different. One of the most important challenges to medicine is to create a single pathway to a generalist's career so that, rather than having general internal medicine, family medicine, and pediatrics, we have a general medicine pathway with pediatric, geriatric, adult male, and adult female opportunities for specialization.
Ensure continued clinical innovation in the subspecialties. We must recognize this as an important dimension of the health care system and of the biomedical research system, and figure out a way to maintain it without orienting the entire care delivery system toward that model.
Downsize the profession, which I have already mentioned. Use information and communications technology to inform and shape an advanced practice. If there is one profession that will make the most of this opportunity it is medicine. This image of having all information inside the head or in the hands of an individual practitioner is an image from a bygone day. Medicine must embrace this new technology to bring the values that it possesses to health care.
Most nursing still takes place in hospital settings. Figure 3 shows the ratio of registered nurses (RNs) to beds. The average length of stay in days and cities that decrease in the intensity of managed care are also shown. This is a
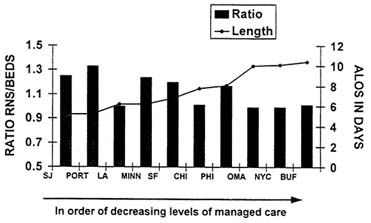
Figure 3 Average length of stay (ALOS) and ratio of registered nurses (RNs) to operating beds, 1992. SOURCES: Statistical Abstract of the United States, 1987, Bureau of the Census, page 90; The Registered Nurse Population, Findings of the National Sample Survey of Registered Nurses, March 1992, Bureau of Health Personnel, Department of Health and Human Services; and The AHA Profile of U.S. Hospitals, 1993/94, American Hospital Association.
Group Health Association of America measure of the intensity of managed care. You can see the correlation between the intensity of managed care and the ratio of RNs to beds. So if a shorter length of stay is a by-product of more intensive managed care, nurses are being utilized in a much higher ratio to beds than in a more conventional setting.
The other point illustrated by this graph is that the complexity of care—the case mix that the nurse sees in the hospital setting—has changed, and the skill base demanded of a nurse is much more sophisticated than in the past.
So the challenges for nursing are to reduce the training capacity radically. The Pew Health Professions Commission recently recommended a 20 percent reduction in training programs for nursing. This is an inadequate beginning for a decrease in the size of training programs. For those who remember the cyclical boom and bust in nursing, remember that boom and bust represents a labor market phenomenon driven on a health care system that was growing from 1960—6 percent of the gross domestic product (GDP)—to this year—15 percent of GDP—with cyclical adjustments. We are talking now about what happens when you reduce insurance premiums by 12 percent over two years as we have in California. You begin to close hospitals, which is a structural adjustment, not a long-term cyclical labor market adjustment.
Expand advance practice training facilities and programs for nursing. Simplify the training degree and practice structure.
One thing we have heard over the past few years is that nursing is its own worst enemy, with a proliferation of degrees, titles, and pathways.
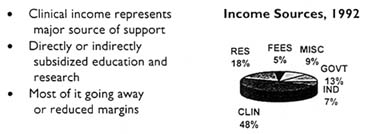
Figure 4 Vulnerable health centers.
Delineate degree practice dimensions for all levels of nursing and focus on care management.
We have heard a lot about the vulnerability of the academic health center. The important message of Figure 4 is that historically, about half of our income has come from clinical services in the last 10 years. We have built an enormous infrastructure.
Figure 5 shows what is happening in research—a familiar story to all of you. The bottom line represents RO1s awarded by NIH; the top represents those reviewed. Not only will we produce more specialists, we will also have a similar growth curve for the production of biomedical investigators. They cannot all have five graduate students and three postdocs in their labs and expect to be funded on a fairly stable base.
In the academic health center this is the challenge. Reduce the demand for specialty education. With declining federal and state support, it simply is not coming back in the way we expected. There needs to be more focus on primary care. Many of our academic health centers have an inadequate patient base for teaching. The patients simply are not there any longer.
More focused demands are being made of health for the health care system. The demand for specialty services, especially middle-tier services—not organ transplants, but undifferentiated cardiology, gastroenterology, and radiology services—is declining radically. Capacity is inadequate to support hospital settings and services. The opportunity exists to develop primary care networks, and the loss of income stream is perilous to the continued existence of hospitals.
On the organizational level, academic health centers will lose considerable parts of their revenue streams, not just from patient care but from research dollars and other sources. We must develop new partnerships. That has been addressed earlier and is absolutely critical for the future. We must incorporate information technology. Hospitals simply will not look like the citadels of the past.
There must be a greater range of diversity of institutions. We have to separate the teaching, research, and clinical service missions and be willing to pull them apart. I don't think we have good figures for what it costs to hold them together, but must find ways to pull them apart and then use technology to relate them as they need to be related.
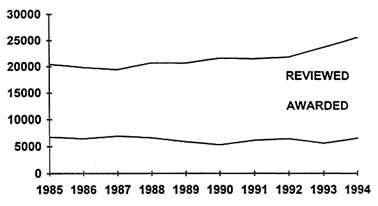
Figure 5 Research changes: competing research projects, 1985-1994.
SOURCE: NIH Extramural Trends FY 84-93, U.S. Department of Health and Human Services, October 1994, page 37.
Conduct clinical service only as it is needed by education and research. Right now we are a proven high-cost provider. We need to develop partnerships with the care delivery system that permit us financially and in terms of patient flow to carry out the education and research mission.
Integrate education and research with other parts of the care system. These are important commodities. We need to make more of our research capacity—our ability to develop and disseminate new knowledge—because knowledge is going to be the coin of the realm in the new system.
Create a virtual academic health center, not one located on a single campus, but one in which research might be spun off; patient care services might be carried out in efficient, patient-oriented care delivery systems; and the educational mission might be carried to the research lab, the patient care delivery site, or the lecture hall. Then create a stable and sustainable financial base.
Finally, Kierkegaard said that ''life can only be understood backwards; but it must be lived forwards.'' Oftentimes with these kinds of projections, we try to give the perfect argument for the future. That is absolutely impossible. However, it is important to be actively engaged in the next 10 years so that we can accurately reflect and understand where we have been.
The Workforce for Health— Response
Paul F. Griner, M.D.
Vice President and Director, Center for the Assessment and Management of Change in Academic Medicine, Association of American Medical Colleges
Dr. O'Neil and other members of the Pew Health Professions Commission should be acknowledged for their important contributions. They have focused our attention on a number of key factors that should influence planning of the health professions work force for the 21st century. Among these are the health status of the population, the growth of knowledge of disease and of the technology to apply that knowledge, and the paradigm shifts that medical centers will have to embrace to help them achieve their missions.
HEALTH STATUS
On some of these points, the Pew Commission report does not go far enough. On others, the challenge is not what but how to address the issue. Perhaps we should start by focusing on the ultimate goal, that is, improving the health status of the population. One of the key recommendations made by the Pew Commission is for a work force that is more oriented to improving the health of the entire population and more inclusive in how it defines health. I agree but suggest that the implications for the number and mix of providers in the health care field are even more profound than has been suggested. The health status of the public will continue to be determined as much or more by social, economic, and cultural determinants than by the amount and quality of health services as we now know them. I emphasize as we now know them. Morbidity and mortality from physical and mental abuse, various addictions, and other preventable conditions, compounded by poverty, lack of education, and the pace of change, will continue to exceed illness and death due to impaired health from nonpreventable causes. This assumption has implications
both for the boundaries of medicine and nursing and for the desirable mix of professionals best suited to address these challenges. It is no longer appropriate to take the position that these are factors outside our realm. While the health professions cannot be held accountable for impaired health status attributable to poverty, crime, and the like, the professions must expand their definition of the boundaries of health care and find ways to interact better with their communities—more involvement with schools, with neighborhood groups, with individual families. The desirable mix of professionals best suited to address these challenges is a point for discussion. Social workers, psychologists, teachers, and parent role models may play more important parts than physicians and nurses. In any case, the implications for both the nature of the work of health care and the mix of team members best suited to that work are significant.
KNOWLEDGE AND TECHNOLOGY
The growth of knowledge of disease and of the technology with which to apply that knowledge is another important variable that has implications for the work force. Change in medical practice is being driven as much by these factors as by the way health care is being delivered and paid for. I suggest that there are more uncertainties around these determinants than around the work force needed to function in a reorganized delivery system. Let's examine the implications of the knowledge being accumulated concerning genetically determined or mediated disease. Will this knowledge influence the number and mix of providers? If so, in what direction? In theory, a reduced burden of illness would be expected from the application of this knowledge. On the other hand, those at greatest risk for disability and death from the more prevalent diseases may have even less access to diagnostic or therapeutic technology than they have today if entitlement programs are scaled back too sharply. Will the lowered resource use anticipated from better knowledge of those not at risk for coronary heart disease be neutralized by the aging of a high-risk minority population whose access to health services is reduced? It is your call.
WORK FORCE
Notwithstanding these considerations that may influence the number and mix of health care professionals needed, it is important to acknowledge an oversupply of physicians and to discuss strategies that might be used to address the problem. The Pew Commission report calls for a limitation on the number of residency training positions, limits on the number of international medical graduates receiving training in this country, and a reduction in the number of U.S. medical schools by as much as 20 percent. There are at least two important points to be made with respect to this recommendation. First, it is premature and potentially damaging to the interests of Americans who seek training for careers in the health professions to call for a reduction in the
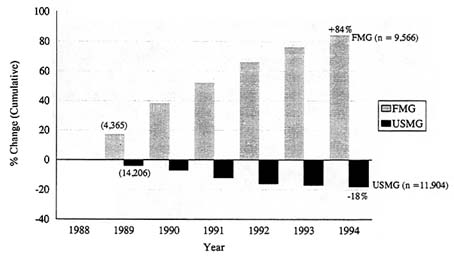
Figure 1 Cumulative percentage change in internal medicine residents, 1988–1994. FMG: foreign medical graduate; USMG: U.S. medical graduate.
number of medical schools or students in the absence of a clear plan to address the excessive number of residency positions in this country and to limit the number of international medical graduates who remain and practice here. The emphasis needs to be on the sequencing of these objectives. It is easier to talk about reducing the number of U.S. medical schools or students than it is to agree on strategies to address the number of residencies and the maldistribution of American and international graduates occupying these residencies.
To reinforce that point, Figure 1 shows the cumulative percentage change in the number of foreign medical graduates (FMGs) in training in internal medicine residencies in the United States since 1989, compared to the change in number of American medical school graduates (USMGs). An 84 percent increase in the number of FMGs contrasts with an 18 percent decrease in USMGs, the result of a continuing increase in the number of residency positions offered and a decline in the number of Americans applying. The result is that by July 1996, there will be more foreign than American medical graduates in residencies in internal medicine in the United States. This trend will be seen across the spectrum of residencies in the United States unless or until a strategy is developed that leads to a reduction in the total number of positions and to limits on the number of FMGs occupying them. This strategy must recognize the demand for foreign-educated physicians as a means of satisfying service needs in our teaching hospitals. Sufficient funds must be made available to those hospitals that provide disproportionate medical services to indigent patients and depend on residents who graduated from foreign schools to provide those services. Additionally, leaders of academic medicine must begin to lead by weaning their institutions away from dependence on graduates of foreign schools. This dependence relates not only to the provision of service. It exists in the biomedical research arena as well.
A second point needs to be made in response to the recommendation to close some U.S. medical schools. Medical schools do not exist in isolation. The missions of research and community service are intimately tied to that of education. For most medical schools, to close the school is to eliminate the social good that emanates from its investment in research and its contribution to the health of the community. If a reduction in the number of students or schools is ultimately found to be a desirable strategy, it makes more sense to some of us to talk about consolidation of medical schools and their teaching hospitals of the kind that is now being played out in New York City, Boston, and the San Francisco Bay Area.
CONCLUSION
Finally, it is worth commenting on whether regulation, the marketplace, or both, will represent the best approach to the necessary downsizing of residency training positions. Regardless of one's intuitive position, it seems clear that better and more timely trend data are required to suggest the best strategy or mix of strategies. Figure 2 shows changes in numbers of trainees in cardiovascular medicine in the United States over the past 5 years. This is the subspecialty, as you all know, that has the greatest oversupply. The inexorable growth in numbers appears to have abated in those areas of the country where oversupply is most quickly recognized, areas where the growth in managed care has been most rapid. So we see a 5 percent reduction in number of positions among academic medical centers in the West; a smaller decline, but a decline, in the Midwest; and a flattening in the South. Only the Northeast has not yet recognized the imperative. Some of us are of the opinion that the number and mix of subspecialty training positions will begin to be influenced
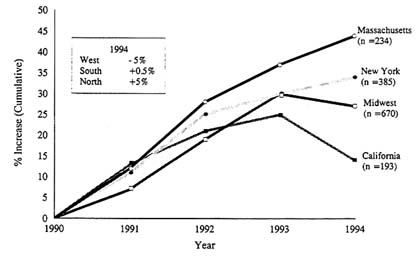
Figure 2 Cumulative percentage increase in cardiovascular medicine fellowships by state and region, 1990–1994.
sufficiently rapidly by the marketplace that regulation will not be required. This will most likely not be the case for the number of core residency positions for reasons that have already been mentioned.
Let me conclude by suggesting the obvious; that is, many past work force projections have missed the mark by a large margin. Although what is proposed today may seem reasonable, there remains much to be learned about the many variables, and their direction, that will continue to influence the actual demand for the health work force. We should continue to monitor and measure the impact of these variables as we continue the debate.
DISCUSSION
DR. LITTLETON: My name is Preston Littleton. I am with the American Association of Dental Schools. This is just a reminder that an academic health center by definition consists of more than a medical school and a teaching hospital. It was really only late in the conversations that we owned up that there are schools of pharmacy, nursing, and dentistry. As we look at these changes, it is imperative that we look at them in a collaborative way as to how all of our professions and our colleges are going to be responding to these changes in market forces. I just wanted to remind everyone that there are more of us out there than just the schools of medicine and the teaching hospitals.
PARTICIPANT: As long as we are on that topic, I would concur that we need to give more recognition to the role that other health professionals play. I believe that as we do a lot of our work force planning, it seems that there is sort of a nod and a wink to the role of nursing and to dentistry, pharmacy, physicians assistants, and other health professionals; but there is not enough focus on what it means for us in the production of primary care physicians.
In the spirit of this event, we also have not looked out very far on this agenda. I have heard a lot about telematics, virtual reality, and virtual surgery; but I do not believe we recognize or have stretched our imaginations far enough to understand how many primary care physicians there will be in the year 2020. If our epidemiologists could tell me the population of this country at that time, whether it will be 260 million or 270 million, I expect that we will probably have, if one would assume that we would have such a gracious society, that everybody would be computer literate, and be involved in having direct access to all of these telematics and everyone would be delivering a significant amount of your own primary care.
We need to reflect on that because it has profound implications for what we are doing in all of the health professions, not only in how we are going to teach. In fact, the total numbers that we are producing could be an enormous excess for all of us. I would just like people to start putting that into their computers and begin to think a little further than 5 or 10 years and to use that imagination of the power that could come from what Dr. Blumberg has
suggested in terms of our knowledge base, what Dr. Detmer has suggested in terms of what truly could be expert systems and, quite frankly, discoveries that have not even been thought of today.
DR. RUBIN: Bob Rubin. I would like to ask Dr. O'Neil, in light of his Kierkegaard quote, whether we have gone past the paradigm of the primary care physician or the primary case manager? Indeed, if 10 percent of the people account for 70 percent of the health care costs, isn't what we really need—particularly given recent articles in the New England Journal of Medicine and JAMA that show that perhaps primary care physicians are not the best managers of chronic disease like heart disease, cancer, and so on—a specialty-dominated system that uses some of the multiskilled allied health professionals that you talked about? Isn't that what we are looking for in 2020 rather than sort of this transitional mode of primary care physicians?
DR. O'NEIL: We certainly had specialty domination in the past that has not seemed to produce the kinds of health outcomes or the kind of health system that you spoke of. Yet I do believe that there is terrific promise for not divorcing specialization and specialized knowledge from the system but creating different ways to get it incorporated, as opposed to the individual practice of specialty physicians. Having primary care physicians and also having those primary care physicians relate to a specialty information base very differently than they relate to them today is as much a viable option for the future to produce the same type of outcome.
PARTICIPANT: What I would like the audience to contemplate also is, as we talk about downsizing the health care industry, academic health centers, and training programs, think about the economic impact that that will have on local communities. We should try to not look like the steel industry. There should be enough intellectual power here to think about what it means when in the Chicago or New York City begin to downsize that whole industry—downsize it appropriately and efficiently. Yet then what should people be training for as an alternative? How can we prepare for that?
DR. LARSON: Dr. Larson, from Georgetown University School of Nursing. I agree, Dr. O'Neil, with your comment on the need to downsize nursing as well as medicine, particularly the diploma and associate degree programs. However, like several other things we have talked about today, public policy does not match the direction in which we need to go. About 95 percent of Medicare funding for nursing education goes to hospitals with diploma programs, and those programs are totally antiquated.















