2
The Neglected Health and Economic Impact of STDs
|
Highlights
|
Sexually transmitted diseases (STDs) are a tremendous health and economic burden on the people of the United States. More than 12 million Americans are infected with STDs each year (CDC, DSTD/HIVP, 1993). In 1995, STDs accounted for 87 percent of all cases reported among the top ten most frequently reported diseases in the United States (CDC, 1996). Of the top ten diseases, five are STDs (i.e., chlamydial infection, gonorrhea, AIDS, primary and secondary syphilis, and hepatitis B virus infection).
Rates of "classical" STDs such as gonorrhea and syphilis are slowly declining in the United States, but rates of a number of STDs in the United States are higher than in some developing regions (Piot and Islam, 1994) and still far exceed those of every other developed country1 (Aral and Holmes, 1991) (Figure 2-1). For example, the reported incidence of gonorrhea in 1995 was 149.5 cases per
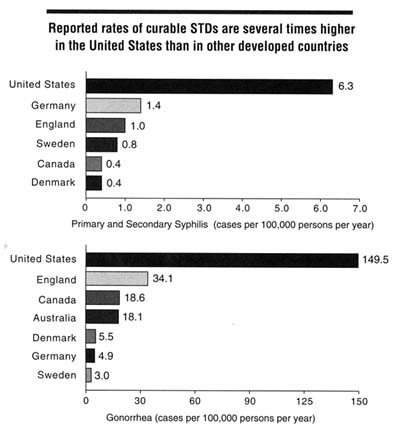
Figure 2-1
Rates of reported syphilis (primary and secondary cases) and gonorrhea in the United States and other developed countries, 1995. SOURCES: 1) Australia: Herceg A, Oliver G, Myint H, Andrews G, Curran M, Crerar S, et al. Annual report of the national notifiable diseases surveillance system, 1995. Communicable Diseases Intelligence, Commonwealth Department of Health and Family Services. October 14, 1996;20:440-464. Rates of primary and secondary syphilis not available; 2) Canada: JoAnne Doherty, Laboratory Center for Disease Control, Division of STD Prevention & Control, Ottawa, Ontario, Canada, personal communication, November 1996; 3) Denmark: Dr. Inga Lind, WHO Collaborating Centre for Reference and Research in Gonococci, Copenhagen, Denmark, personal communication, November 1996; 4) England: Hannah Bowers, Public Health Laboratory Services, Communicable Disease Surveillance Centre, London, England, United Kingdom, personal communication, November 1996; 5) Germany: Dr. Lyle Petersen, Robert Koch Institute, Berlin, Germany, personal communication, November 1996; 6) Sweden: Dr. Kristina Ramstedt, Swedish Institute for Infectious Disease Control, Epidemiological Department, personal communication, November 1996; 7) United States: Division of STD Prevention, Sexually transmitted disease surveillance, 1995. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, September 1996.
100,000 persons in the United States versus 3.0 cases per 100,000 in Sweden (CDC, DSTDP, 1996; Swedish Institute for Infectious Disease Control, unpublished data, 1996). Because actual U.S. rates are estimated to be approximately twice the reported rate, the U.S. rate is 100 times the reported rate in Sweden. Similarly, the reported incidence of gonorrhea in Canada in 1995 was 18.6 cases per 100,000, or approximately 12 percent of the U.S. rate (Laboratory Centre for Disease Control, Canada, unpublished data, 1996). In addition, the rate of primary and secondary syphilis in the United States was 6.3 cases per 100,000 persons versus 0.4 cases per 100,000 persons in Canada. Therefore, rates of curable STDs, including gonorrhea, syphilis, and chancroid are many times higher in the United States than in other developed countries. The differences in rates of viral STDs between the United States and other developed countries, however, appear to be much smaller. Data for viral STDs are much more limited than for bacterial STDs, but do not suggest major differences. For example, a cohort of young Swedish women studied over a 16-year-period showed a cumulative incidence of genital herpes that was comparable to the age-specific increases in herpes simplex virus type 2 antibodies seen during the approximately the same period in U.S. women (Christenson et al., 1992; Johnson et al., 1993). Potential explanations for the observed differences between the United States and other developed countries in rates of curable STDs are presented in Chapter 3.
Further, many new STDs have been discovered or have newly arisen during the antibiotic era. Of these "modern" STDs, some, including HIV infection, human papillomavirus infection, and hepatitis B virus infection, are viral infections that are incurable and are now recognized as major preventable causes of death and disability. The bacterial STDs, such as gonorrhea and syphilis, can be easily diagnosed and successfully treated; others, such as chlamydial infection, are curable but will require a much stronger, coordinated national effort to be brought under control.
Broad Scope and Impact of STDs
STDs affect persons of all racial, cultural, socioeconomic, and religious groups in the United States. Persons in all states, communities, and social networks are at risk for STDs. The estimated incidence and prevalence of major STDs are summarized in Table 2-1.
The term "STD" is not specific for any one disease but denotes the more than 25 infectious organisms that are transmitted through sexual activity and the dozens of clinical syndromes that they cause (Appendix A). With STDs, one infectious organism does not cause one syndrome; rather, there is a matrix of infectious organisms and associated syndromes. For example, some syndromes, such as pelvic inflammatory disease, can be caused by a number of organisms, including Neisseria gonorrhoeae, Chlamydia trachomatis, and other bacteria. Urethritis (inflammation of the canal leading from the urinary bladder) in men is frequently
Table 2-1 Estimated Annual Incidence and Prevalence of Selected Sexually Transmitted Diseases (STDs) in the United States, 1994
|
STD |
Incidence |
Prevalence |
|
Chlamydial infection |
4,000,000a |
Not available |
|
Gonorrhea |
800,000a |
Not available |
|
Syphilis |
101,000 |
Not available |
|
Congenital syphilis |
3,400 |
Not available |
|
Human papillomavirus infection |
500,000-1,000,000 |
24,000,000 |
|
Genital herpes infection |
200,000-500,000 |
31,000,000b |
|
Hepatitis B virus infection (sexually transmitted) |
53,000a |
Not available |
|
AIDS |
79,897c |
185,000d |
|
HIV infection |
Not available |
630,000-897,000e |
|
Chancroid |
3,500 |
Not available |
|
Trichomoniasis |
3,000,000 |
Not available |
|
Pelvic inflammatory disease |
>1,000,000f |
Not available |
|
NOTE: The Division of STD Prevention, CDC, is currently developing a process for systematically generating and updating incidence and prevalence estimates for specific STDs. a Number reflects reported cases to the CDC plus estimated unreported cases. b Based on Johnson RE, Nahmias AJ, Magder LS, Lee FK, Brooks CA, Snowden CB. A seroepidemiologic survey of the prevalence of herpes simplex virus type 2 infection in the United States. N Engl J Med 1989;321:7-12. However, recent data indicate a substantial recent increase in prevalence in the United States (Johnson R, Lee F, Hadgu A, McQuillan G, Aral S, Keesling S, et al. U.S. genital herpes trends during the first decade of AIDS—prevalences increased in young whites and elevated in blacks. Proceedings of the Tenth Meeting of the International Society for STD Research, August 29-September 1, 1993, Helsinki [abstract no. 22]). c Reported cases to the CDC. Source: CDC. HIV/AIDS Surveillance Report. Atlanta: Centers for Disease Control and Prevention, 1995;7(2). d Estimated prevalence of persons diagnosed with AIDS at the end of 1993. All AIDS cases including unreported cases. e Prevalence as of January 1993. Source: Rosenberg PS. Scope of the AIDS epidemic in the United States. Science 1995;270:1372-5. f Based on estimate for 1993 by Siegel (Appendix D of present report), Washington and Katz also estimated more than one million cases per year using older data (Washington AE, Katz P. Cost of and payment source for pelvic inflammatory disease. Trends and projections, 1983 through 2000 [see comments]. JAMA 1991;266:2565-9.). PRIMARY SOURCE: CDC, DSTD/HIVP. Annual Report 1994. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1995. |
||
caused by gonorrhea or chlamydia but can also result from infection with ureaplasma, mycoplasma, and other organisms. Genital ulcers can result from herpes, chancroid, syphilis, or other infections. Vaginal discharge can be caused by trichomonas, bacterial vaginosis, or other infections. Syphilis and HIV infection have myriad clinical manifestations and can mimic many health conditions. In addition, common infections once considered trivial are now known to cause
serious complications. For example, bacterial vaginosis, a frequent cause of vaginitis in sexually active women, was once considered to be a benign condition but has recently been shown to be associated with premature delivery, low birth weight, and pelvic inflammatory disease (Hauth et al., 1995; Hillier et al., 1995). Human papillomaviruses, originally recognized to cause warts, are now known to be important causes of several types of cancer.
Routes of Transmission
Epidemiological and other characteristics of eight common STDs are summarized in Appendix B. STDs are almost always transmitted from person to person by sexual intercourse.2 STDs are transmitted most efficiently by anal or vaginal intercourse, and generally less efficiently by oral intercourse. A few STDs, such as scabies, can also be transmitted without sexual intercourse via direct contact with an infected site of a sex partner. Other more important blood-borne pathogens, such as hepatitis B virus, human T-cell lymphotrophic virus type I, and HIV, are transmitted among adults not only by sexual intercourse, but also by parenteral routes—particularly among intravenous drug users through contaminated injecting drug equipment. The relative contribution of parenteral versus sexual transmission varies according to the risk behaviors of the population and other factors. In addition, pregnant women with an STD may pass their infection to infants in the uterus, during birth, or through breast-feeding.
Summary of Common STDs
Human Papillomavirus Infection
Human papillomavirus is associated with the development of cervical and other genital and anal cancers (Koutsky et al., 1988; Reeves et al., 1989) and is prevalent across all socioeconomic groups in the United States. An estimated 24 million Americans already are infected with human papillomavirus, and as many as one million new human papillomavirus infections occur each year (CDC, DSTD/HIVP, 1995). In one study of female college students presenting for care at a university health center, genital human papillomavirus infections were five times more common than all other STDs combined (Laura Koutsky and King Holmes, University of Washington, unpublished data, 1995).
Herpes Simplex Virus Infection
Sexually transmitted herpes simplex virus infection is widespread in the United States and results in painful recurrent genital ulcers. The ulcers can be treated, but infection persists and ulcers may recur (Quinn and Cates, 1992). Herpes simplex virus can be transmitted to sex partners even when no genital ulcer is present (Mertz et al., 1992) and can also be transmitted from mother to infant during delivery. Approximately 200,000-500,000 new cases of genital herpes occur each year in the United States, and 31 million individuals already are infected (CDC, DSTD/HIVP, 1995). In 1990, the prevalence of antibodies to herpes simplex virus type 2 among persons 15-74 years of age was estimated at 21.7 percent (Johnson et al., 1993). This prevalence estimate suggests that at least one of every four women and one of every five men in the United States will become infected with herpes during their lifetime.
Viral Hepatitis
Hepatitis B virus infection is an STD with severe complications including chronic hepatitis, cirrhosis, and liver carcinoma. Of approximately 200,000 new hepatitis B virus infections in the United States each year, approximately half are transmitted through sexual intercourse (Alter and Mast, 1994; CDC, 1994b; Goldstein et al., 1996). Preliminary data from a large U.S. multisite study indicate that approximately one-third of persons with acute hepatitis B virus infections in 1995 had a history of another STD (CDC, Hepatitis Branch, unpublished data, 1996). In addition to hepatitis B, several other types of viral hepatitis can be transmitted sexually. Hepatitis A is a cause of acute hepatitis, and less than 5 percent of infections are transmitted through fecal-oral contact during sexual intercourse, mostly among men who have sex with men (CDC, 1994b; CDC, Hepatitis Branch, 1995). Hepatitis D (delta) virus is a virus that can be sexually transmitted but requires the presence of hepatitis B virus to replicate. Sexual transmission of hepatitis D virus occurs, but it is less efficiently transmitted through sexual intercourse than hepatitis B virus (Alter and Mast, 1994). Hepatitis C virus, the most common cause of non-A non-B hepatitis, causes chronic liver disease in most infected adults. The efficiency of sexual and perinatal transmission of this virus, however, seems to be low (Alter and Mast, 1994).
Syphilis
After sustaining a steady incidence rate during the 1970s and early 1980s, the rate of syphilis increased sharply from 1987 through 1990 (CDC, DSTDP, 1995), after which rates began to fall. This epidemic illustrates the ability of syphilis and other STDs to reemerge with alarming intensity in populations such as illicit drug users—particularly crack cocaine users—and their sex partners
(Farley et al., 1990; Rolfs et al., 1990). The reemergence of syphilis in this new context rendered traditional prevention efforts less effective (Andrus et al., 1990).
Gonorrhea
Gonorrhea infections in the United States are becoming increasingly resistant to routine antibiotic treatment; this has resulted in increasingly expensive treatments as effective therapeutic options become more limited. As of 1976, all gonorrhea infections were curable by penicillin (Aral and Holmes, 1991). Since then, antibiotic-resistant strains have increased steadily to 2 percent of gonorrhea infections in 1987 and to 30 percent of gonorrhea infections in 1994 (CDC, DSTDP, 1995). The Gonococcal Isolate Surveillance Project of the Centers for Disease Control and Prevention (CDC) measures national trends in gonorrhea antibiotic resistance. The proportion of isolates resistant to penicillin has increased steadily since monitoring began in 1988 (CDC, DSTDP, 1995) (Figure 2-2). In 1994, approximately 30 percent of gonococcal isolates were resistant to tetracycline, penicillin, or both; these antibiotics represent traditional, effective, low-cost treatment for gonorrhea. In addition, resistance to the newer quinolone antibiotics has been documented in the Western Pacific and Southeast Asia and in several U.S. states, indicating that some currently recommended treatment regimens may soon become inadequate (CDC, 1994a; GDHR, Epidemiology and Prevention Branch, 1995).
Chlamydial Infection
Chlamydial genital infection is the most common bacterial STD in the United States; of the more than 4 million cases estimated to occur annually, 2.6 million cases occur among women (CDC, DSTDP, 1995). As many as 85 percent of infections in women and 40 percent of infections in men may be asymptomatic and will not be identified without screening (Fish et al., 1989; Judson, 1990; Stamm and Holmes, 1990). Uncomplicated chlamydial infections can be easily treated with antibiotics (CDC, 1993); however, primarily as a result of unrecognized and untreated cervical infections, more than one million women each year develop pelvic inflammatory disease (Rolfs et al., 1992).
Impact of STDs on Women's Health
Complications of STDs are greater and more frequent among women than men for a number of reasons (Wasserheit and Holmes, 1992). Women are biologically more likely to become infected than men if exposed to a sexually transmitted pathogen. STDs are also more likely to remain undetected in women, resulting in delayed diagnosis and treatment, and these untreated infections are more likely to lead to complications.
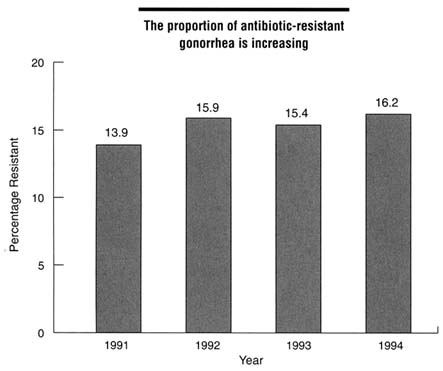
Figure 2-2
Percentage of isolates resistant to antibiotics, Gonococcal Isolate Surveillance Project, 1991-1994. SOURCE: CDC, DSTDP. Sexually Transmitted Disease Surveillance 1994. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1995.
Many STDs are transmitted more easily from man to woman than from woman to man (Harlap et al., 1991). For example, the risk to a woman of acquiring gonorrhea from a single act of intercourse may be as high as 60 to 90 percent, while transmission from a woman to man is about 20 to 30 percent (Holmes et al., 1970; Hooper et al., 1978; Platt et al., 1983; Judson, 1990; Donegan et al., 1994). Among couples where only one partner was initially infected, the annual risk of transmission of herpes simplex virus was 19 percent from man to woman, but only 5 percent from woman to man (Mertz et al., 1992). The comparative efficiency of male-to-female versus female-to-male transmission of HIV seems to differ according to the study population (Haverkos et al., 1992). Studies in the United States (Peterman et al., 1988; Padian et al., 1991) generally have shown greater efficiency of transmission from man to woman than from woman to man, while studies in Haiti (Deschamps et al., 1996) and Europe (de Vincenzi, 1994) have shown no significant gender difference in efficiency of transmission.
STDs are often silent in women, and even when symptoms of STD occur, they may not arouse suspicion of an STD. For example, 30 to 80 percent of women with gonorrhea are asymptomatic, while fewer than 5 percent of men have no symptoms (Hook and Handsfield, 1990; Judson, 1990). Similarly, as many as 85 percent of women with chlamydial infection are asymptomatic compared to 40 percent of infected men (Fish et al., 1989; Judson, 1990; Stamm and Holmes, 1990). When an STD is suspected, it is often more difficult to diagnose in a woman because the anatomy of the female genital tract makes clinical examination more difficult (Aral and Guinan, 1984). For example, a urethral swab and a Gram stain are sufficient to evaluate the possibility of gonorrhea in men, but a speculum examination of the cervix and a specific culture for gonorrhea have been required for women (Hook and Handsfield, 1990). Thus, women with gonorrhea or chlamydial infection are often not diagnosed with an STD until complications, such as pelvic inflammatory disease, occur. Even then, symptoms of pelvic inflammatory disease due to chlamydial infection may be absent or non-specific, resulting in as many as 85 percent of women delaying seeking medical care, thus increasing their risk for long-term complications (Hillis et al., 1993). Fortunately, the advent of newer tests for detecting gonococci and chlamydia in urine may permit testing women for these organisms without pelvic examination in the future, as described in Chapter 4.
Once infected, women are more susceptible than men to complications of certain STDs. For example, women infected with certain types of human papillomavirus are at risk for cancers of the cervix (a relatively common malignancy), as well as cancers of the vagina, vulva, and anus; whereas heterosexual men infected with these human papillomavirus types are at risk only for cancers of the penis (a relatively uncommon malignancy). Another example is the risk of infertility caused by gonorrhea or chlamydial infection, which is much higher in women than in men. Finally, pregnant women and their infants are particularly vulnerable to complications of STD during pregnancy or parturition.
Greater Risk of STDs Among Adolescents
Every year, approximately 3 million American teenagers acquire an STD (CDC, DSTD/HIVP, 1993). During the past two decades, sexual intercourse among adolescents has steadily increased, resulting in an enlarging pool of young men and women at risk for STDs (CDC, 1995c). As a result, STDs, unintended pregnancies, and other health problems that result from sexual intercourse have increased among adolescents in the United States (AGI, 1994). Adolescents (10-19 years of age) and young adults (20-24 years of age) are the age groups at greatest risk for acquiring an STD, for a number of reasons: they are more likely to have multiple sex partners; they may be more likely to engage in unprotected intercourse; and their partners may be at higher risk for being infected compared to most adults (Cates, 1990; Quinn and Cates, 1992; AGI, 1994; CDC, DSTDP,
1995). Compared to older women, female adolescents and young women are also more susceptible to cervical infections, such as gonorrhea and chlamydial infection, because the cervix of female adolescents and young women is especially sensitive to infection by certain sexually transmitted organisms (Cates, 1990). In addition, adolescents and young people are at greater risk for substance use and other contributing factors that may increase risk for STDs than older persons; these issues are discussed in Chapter 3.
Although overall rates of gonorrhea have been declining in the general population for over a decade, this decline has been less pronounced among adolescents than in other age groups. During 1993 and 1994, the gonorrhea rate for 15-19-year-old adolescents actually increased nearly 3 percent (CDC, DSTDP, 1995). The increase in gonorrhea among adolescents can be entirely attributed to increases in gonorrhea among female adolescents of all races, while rates of gonorrhea among male adolescents during this period leveled off. If one takes into account that not all teenagers are sexually active, the actual risk for acquiring an STD among sexually active teens is even higher than the rates themselves may suggest (Aral et al., 1988). Chlamydial infection has been consistently high among adolescents; in some studies, up to 30-40 percent of sexually active adolescent females studied have been infected (Toomey et al., 1987; Cates, 1990). In general, rates of chlamydial are at least two to four times higher than rates of gonorrhea in this age group (Washington et al., 1986; Shafer et al., 1987). Viral STDs also are becoming increasingly prevalent at younger ages as adolescents initiate sexual intercourse earlier (Moscicki et al., 1990). Cervical cancer rates and cohort mortality from cervical cancer (Krone et al., 1995; Kathleen Toomey, Georgia Department of Human Resources, unpublished data, 1996) are increasing among young women, undoubtedly a reflection of increased exposure to STDs such as human papillomavirus.
Other Groups at Risk
Reported STD rates in the United States vary among ethnic and racial groups (CDC, DSTDP, 1995). African Americans and Hispanic Americans have higher reported rates of chlamydial infection, gonorrhea, and syphilis than European Americans. Data on STDs among other ethnic or racial groups are more limited because of their smaller populations in the United States. Rates of certain STDs, however, among some American Indian/Alaska Native populations are high (Toomey et al., 1993). National surveillance data suggest that rates of reportable STDs, except for hepatitis B virus infection (Alter, 1991), are low among Asian Americans/Pacific Islanders compared to the general U.S. population (CDC, DSTDP, 1995).
Although national surveillance data may overrepresent cases diagnosed among some racial and ethnic groups (CDC, DSTD/HIVP, 1995), the higher prevalence of some STDs among African Americans and Hispanic Americans
compared to the European American population has been confirmed by serological population surveys of markers for sexually transmitted infections (Hahn et al., 1989; Johnson et al., 1993). However, serosurvey data indicate that the differences in STD rates among racial and ethnic groups are actually smaller than those suggested by national surveillance data. The reasons for the racial and ethnic differences in STD rates are unclear and complex. Possible explanations include socioeconomic status, variability in access to and utilization of health care, differences in sexual behavior, and varying risk of STDs among sexual networks (Toomey et al., 1993). Some investigators have concluded that factors other than poverty and occupational status account for the observed differences in rates of gonorrhea and chlamydial infection and that nonbehavioral factors, such as geographic segregation, may promote a higher prevalence of these STDs in certain social networks (Ellen et al., 1995). Differences in sexual behavior also cannot entirely explain the racial gap in STD rates. African Americans, for example, are generally more likely to use condoms compared to other groups (Laumann et al., 1994; Anderson et al., 1996).
STDs are transmitted among all sexually active people, including heterosexual persons, men who have sex with men, and women who have sex with women (AMA, Council on Scientific Affairs, 1996). Men who have sex with men are at greater risk for many life-threatening STDs, including HIV infection, hepatitis B virus infection, and anal cancer compared to heterosexual men (AMA, Council on Scientific Affairs, 1996). Other STDs of concern among men who have sex with men include anal syphilis, urethritis, and a range of oral and gastrointestinal infections. While it is well established that men who have sex with men are at increased risk for STDs, including HIV infection, less is known about the risk of STD transmission among women who have sex with women (Kennedy et al., 1995). When compared to men who have sex with men and heterosexual persons, women who have sex only with women (and whose partners do likewise) are at substantially lower risk for acquisition of STDs. Studies show that some women who have sex with women and some bisexual women have high rates of risky behaviors, such as drug use and exchanging sex for drugs or money, as do some heterosexual women (Chu et al., 1990; Bevier et al., 1995). Although women who only have sex with women seem to be at less risk for some bacterial STDs compared to women who have sex with men (Robertson and Schachter, 1981), bacterial vaginosis and genital human papillomavirus infections are not uncommon in such women (Berger et al., 1995; Marrazzo et al., 1996). Most cases of HIV infection among women who have sex with women have been attributed to injection drug use or heterosexual intercourse (Chu et al., 1990, 1994; Cohen et al., 1993; Bevier et al., 1995). Female-to-female transmission of HIV infection seems to be relatively rare (AMA, Council on Scientific Affairs, 1996).
STDs as Emerging Infections
STDs are not a stationary group of infections and syndromes. Eight new sexually transmitted pathogens have been identified since 1980, bringing with them new challenges to prevention and treatment (Table 2-2). The most well-known of the recently described STDs is HIV infection. Since HIV-1 was found to be the cause of virtually all cases of AIDS in the United States in the mid-1980s, a closely related retrovirus, HIV-2, and a more distantly related pair of retroviruses, human T-lymphotrophic virus types I and II (HTLV-I, -II), have been shown to be sexually transmitted as well. In addition, in 1995, scientists confirmed and identified human herpes virus type 8 as a likely sexually transmitted virus and a possible cause of Kaposi's sarcoma and body cavity lymphomas (Chang et al., 1994). In contrast to newly recognized viral STDs, some bacterial STDs, such as syphilis and gonorrhea, have been documented for centuries and have recently reemerged in the United States along with a spectrum of barriers to prevention (Wasserheit, 1994). As demonstrated by the recent finding that bacterial vaginosis in pregnant women increases the risk for premature delivery of a low-birth-weight infant (Hauth et al., 1995; Hillier et al., 1995), the full clinical spectrum of many STDs is still being described. In addition, for many previously described pathogens, such as hepatitis B virus and cytomegalovirus, it has become evident that a major route of adult transmission—often the major route—is sexual. Further, new research shows that many common diseases of previously unknown cause, such as cervical dysplasia, are in fact caused by newly described sexually transmitted pathogens.
These examples of emerging infections (IOM, 1992) make it clear that more STDs will emerge and become established in the United States. This is because of increasing global travel and worsening ecological pressures, such as population
Table 2-2 Sexually Transmitted Pathogens Newly Identified or Newly Recognized as Sexually Transmitted, and Associated Syndromes, 1980-1995
|
Sexually Transmitted Agent (year identified or recognized) |
Associated Syndromes |
|
Human papillomaviruses (1976-present) |
Genital and anal warts, dysplasias, and cancers |
|
HTLV-I (1980) |
T-cell leukemia/lymphoma; tropical spastic paraparesis |
|
HTLV-II (1982) |
Unknown |
|
Mycoplasma genitalium (1981) |
Nongonococcal urethritis |
|
Mobiluncus sp. (1980, 1983) |
Bacterial vaginosis-associated |
|
HIV-1 (1983) |
AIDS |
|
HIV-2 (1986) |
AIDS |
|
Human herpes virus type 8 (1995) |
Kaposi's sarcoma; body cavity lymphoma |
growth and rural-to-urban migration, that contribute to the spread of STDs in both developed and developing countries. The advent of new techniques in biotechnology have allowed the presence of infectious organisms or genetic material from these organisms to be detected, contributing to the recognition of new sexually transmitted infections. These techniques have allowed clinicians and epidemiologists to link specific infectious organisms to the syndromes that they cause.
International Comparisons and the Global Scope of STDs
STDs are severe social, health, and economic burdens worldwide. STDs most commonly affect people who are between the ages of 15 and 44, the group that is most economically productive (Over and Piot, 1993). The World Bank estimates that STDs, excluding AIDS, are the second leading cause of healthy life lost among women between the ages of 15 and 44 in the developing world (Figure 2-3) (World Bank, 1993). STDs are severe public health problems because of their potentially serious complications as well as their potential to increase the efficiency of HIV transmission. One study estimated that the impact of successfully treating or preventing one hundred cases of syphilis among a group at high risk for STDs would prevent 1,200 HIV infections that would otherwise be linked to those one hundred syphilis infections during a 10-year period (Over and Piot, 1993). Over and Piot (1996) also found that, in developing countries, targeting groups with the highest rates of sex partner change markedly improves the cost-effectiveness of HIV and other STD prevention efforts.
The World Health Organization (WHO) Global Programme on AIDS recently estimated regional and global incidence rates for four curable STDs-gonorrhea, chlamydial infection, syphilis, and trichomoniasis (WHO, 1996). Using a database of country-specific prevalence rates and estimated regional prevalence rates for each curable STD, WHO estimated that there were 333 million new cases of the four curable STDs worldwide in 1995 among adults 15-49 years of age. Prevalence rates for other STDs for which estimates are not available, such as human papillomavirus and herpes simplex virus type 2 infections, are much higher, and the number of adults infected is likely to exceed one billion. In addition, in the last few years, STDs have rapidly become epidemic in some areas of the world, such as certain countries of the former Soviet Union. These epidemics have relevance for the United States because Americans are increasingly traveling abroad, and some will have high-risk sexual intercourse during their stay (Moore et al., 1995). With increasing access to international travel and easing of travel restrictions, it is now possible for persons with infectious diseases to spread their infection to others around the world in a matter of hours or days.
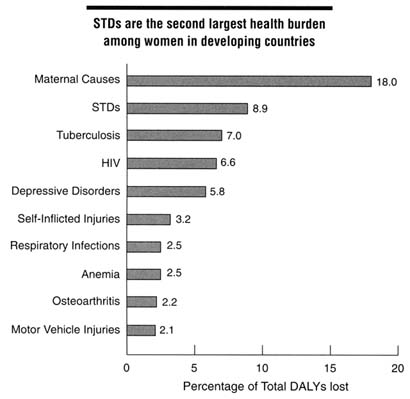
Figure 2-3
Top 10 health burdens among women in developing countries by total DALYs lost, 1990. NOTE: STDs included syphilis, chlamydial infection, gonorrhea, and pelvic inflammatory disease; DALY = disability-adjusted life year. SOURCE: World Bank. World development report, 1993: investing in health. New York: Oxford University Press, 1993.
Health Consequences of STDs
The general population is largely unaware of the health consequences of STDs for three reasons. First, many STDs are often asymptomatic and thus go undetected (Fish et al., 1989; Judson, 1990; Stamm and Holmes, 1990). Second, major health consequences, such as infertility, various cancers, and other chronic diseases, occur years after the initial infection, so that there is a lack of awareness of any link to the original STD (the exception is the public awareness of the connection of AIDS to HIV infection). Third, the stigma associated with having an STD has inhibited public discussion and health education concerning the consequences of STDs and frequently even prevents clinicians from educating
their patients regarding STDs as discussed in Chapter 3. Many sexually transmitted infections can persist for years without evidence of infection until life-threatening complications are recognized. In particular, viral STDs often result in lifelong infection for which there is currently no curative treatment. The serious long-term complications of STDs affecting millions of women, infants, and men in the United States each year are summarized in Table 2-3.
Cancers Caused by STDs
Several sexually transmitted pathogens cause cancer. The direct role of STDs in causing genital cancers has been largely unrecognized. Certain types of sexually acquired human papillomavirus are now considered to be a cause of most cancers of the cervix, vagina, vulva, anus, and penis. Hepatitis B virus, which is usually transmitted either by sexual contact or by intravenous drug use among adults in the United States, is a cause of hepatocellular carcinoma, one of the world's most common forms of cancer. Human T-cell lymphotrophic virus type I (HTLV-I), sexually transmitted among adults and transmitted to infants especially by breast-feeding, causes certain malignancies, including T-cell leukemia and lymphoma. Human herpes virus type 8 (HHV8) is a newly discovered virus, probably sexually transmitted, that may cause Kaposi's sarcoma and certain forms of lymphoma. Epstein-Barr virus (EBV), transmitted among adults by intimate contact, including kissing and sexual intercourse, is associated with other types of lymphoma and with nasopharyngeal (nasal cavity and pharynx) carcinoma.
Cervical Cancer
Carcinoma of the uterine cervix, particularly among women of reproductive age, is now known to be strongly associated with certain oncogenic types of human papillomavirus (NIH, 1996). Of more than 70 types of human papillomavirus that have been identified, several oncogenic forms, such as types 16, 18, 31, and 45, have the strongest association with cervical cancer. Both biological and epidemiological data suggest that human papillomavirus is a dominant etiologic factor for cervical cancer. Studies show that cervical infection with oncogenic types of human papillomavirus is associated with at least 80 percent of invasive cervical cancer cases (NIH, 1996) and that women with human papillomavirus infection of the cervix are 10 times more likely to develop invasive cervical cancer compared to women without human papillomavirus infection (Schiffman, 1992).
Much of the cervical cancer burden related to human papillomavirus infection may be averted by preventing high-risk sexual behaviors (Brinton, 1992), especially avoiding unprotected sex with multiple male partners, some of whom may have chronic genital infection with oncogenic human papillomavirus types. Screening with the Pap smear is currently the best available method for reducing
incidence of, and mortality associated with, invasive cervical cancer, but this is not being widely applied among certain population groups (NIH, 1996).
Approximately 4,900 American women will die from cervical cancer in 1996 (ACS, 1996). Cervical cancer is the second most common cancer among women worldwide, with more than 450,000 new cases estimated to occur each year (Paavonen et al., 1990). It is the most frequently detected cancer among women in many countries in Africa, Asia, Central America, and South America, where case fatality rates are much higher than those in the United States. In this country, approximately 16,000 new cases of cervical cancer are diagnosed each year, placing it third among reproductive tract cancers in women and seventh among all cancers in women (ACS, 1996).
Although these morbidity and mortality statistics are clearly significant by themselves, they do not capture the physical, mental, or psychosocial trauma experienced by the hundreds of thousands of women who develop precancerous cervical lesions. For example, approximately 5 percent of the 50 million Pap smears performed each year are associated with findings consistent with cervical dysplasia (Kurman et al., 1994). These abnormalities result in enormous anxiety among women and their partners and require diagnostic and treatment procedures, including surgery, that are painful, invasive, and expensive.
An especially disturbing recent finding is the increasing incidence of invasive cervical cancer among European American women under age 50 in the last few years (Krone et al., 1995). This new, ominous trend may be related to the high prevalence of human papillomavirus infection recently reported among young women. In one study, nearly half of female college students tested had evidence of genital human papillomavirus infection (Bauer et al., 1991).
Other STD-Related Cancers
Although carcinomas of the vulva, vagina, anus, and penis each occur considerably less frequently than cervical carcinoma, aggregate numbers of vulvar, vaginal, anal, and penile carcinomas equal nearly half the total numbers of cases of cervical cancer in the United States. These cancers are also strongly associated with human papillomavirus infection. Approximately 60 to 90 percent of cancers at these sites are associated with human papillomavirus, particularly types 16 and 18 (Paavonen et al., 1990). Infection with HIV also may increase the risk that human papillomavirus infection will progress to cancer of the cervix or to the other sites mentioned above.
Reproductive Health Problems
STDs represent a serious threat to the reproductive capability of couples, largely because of the impact of STDs on women. A variety of women's health problems all result from unrecognized or untreated STDs. Reproductive health
complications include both short-term (e.g., pelvic inflammatory disease, pregnancy complications, epididymitis) and long-term consequences (e.g., infertility and ectopic pregnancy).
Pelvic Inflammatory Disease
One of the most serious threats to the reproductive capability of women is infection of the upper genital tract, referred to as pelvic inflammatory disease (McCormack, 1994). Most cases of this disease are associated with chlamydial infection and gonorrhea (Jossens et al., 1994), which initially involve the cervix, but in some women disease can spread up into the uterus and through the fallopian tubes into the pelvis and abdominal cavity. Pelvic inflammatory disease is a preventable complication of these sexually transmitted infections (Washington et al., 1991).
Each year, more than one million U.S. women experience an episode of pelvic inflammatory disease (Washington and Katz, 1991; Rolfs et al., 1992). Some cases of acute pelvic inflammatory disease result in abscesses involving the ovaries and fallopian tubes, which require surgical intervention. At least one-quarter of women with acute pelvic inflammatory disease will experience serious long-term sequelae, the most common and important of which are ectopic pregnancy (the development of a fetus outside the uterus) and tubal-factor infertility. Other complications include chronic pelvic pain and pain during intercourse caused by scarring in the pelvis.
The above health problems are all recognized consequences of symptomatic pelvic inflammatory disease. Perhaps even more devastating to women's reproductive health is the more recently described ''a typical pelvic inflammatory disease" (Cates et al., 1993). Women with this syndrome experience only mild symptoms, unrecognized symptoms, or possibly, in many cases, no symptoms ("silent pelvic inflammatory disease") (Wolner-Hanssen, 1995). This more indolent but insidious form of pelvic inflammatory disease is less likely to be detected compared to symptomatic pelvic inflammatory disease, thus placing unsuspecting women at increased risk of disease sequelae (Morell, 1995). Because these cases of a typical pelvic inflammatory disease are also associated with chlamydial and gonococcal infection in women, prevention of these STDs will result in reductions in morbidity of pelvic inflammatory disease heretofore unrecognized, with accompanying decreases in cost and human suffering.
Ectopic Pregnancy
Ectopic pregnancy usually results from partial tubal blockage due to pelvic inflammatory disease. After an episode of pelvic inflammatory disease, a woman is six to ten times more likely to have an ectopic pregnancy compared to women who do not have pelvic inflammatory disease (Marchbanks et al., 1988). Approximately
9 percent of women with laparoscope-confirmed pelvic inflammatory disease experience an ectopic pregnancy for their first pregnancy subsequent to their episode of pelvic inflammatory disease (Weström et al., 1992). In 1992, the estimated number of ectopic pregnancies was 108,800, or 1 in 50 pregnancies (CDC, 1995a). In addition, in the same year, approximately 9 percent of all pregnancy-related deaths were a result of ectopic pregnancy (NCHS, 1994), making ectopic pregnancy one of the leading and most preventable causes of maternal death during pregnancy (Marchbanks et al., 1988). In fact, ectopic pregnancy is the leading cause of first-trimester deaths among African American women (CDC, DSTD/HIVP, 1995).
Infertility
Infertility can occur when the fallopian tubes become blocked or damaged by STDs. Of all infertile American women, at least 15 percent are infertile because of tubal damage caused by pelvic inflammatory disease. This type of infertility is treated by tubal microsurgery (which attempts to repair the damaged tubes) or by in vitro fertilization (in which an egg is surgically removed from the ovary, mixed with sperm and fertilized outside the body, and then placed directly into the uterus, thus bypassing the blocked fallopian tubes). Of all women infertile because of tubal damage, no more than one-half have previously been diagnosed and treated for acute pelvic inflammatory disease. The remaining half have also had pelvic inflammatory disease but had symptoms that were presumably so mild or a typical that they were never treated for the disease. A large prospective study of women who had laparoscopy because of clinical evaluation for pelvic inflammatory disease showed that approximately 16 percent of women with abnormal laparoscopic findings consistent with this disease tried but failed to conceive during the follow-up period, compared to 3 percent of women with normal laparoscopic findings (Weström et al., 1992). Eleven percent of women with abnormal laparoscopic findings became infertile as a result of tubal factor infertility (5 percent were infertile because of other reasons). After one episode of laparoscope-confirmed pelvic inflammatory disease, approximately 8 percent of women developed tubal-factor infertility, with the risk increasing with the severity of the episode. Each subsequent episode roughly doubled the rate of tubal-factor infertility (20 percent after two episodes and 40 percent after three or more episodes). Ectopic pregnancy also substantially increases the risk of tubal-factor infertility. STDs rarely produce infertility in men.
Health Consequences for Pregnant Women and Infants
STDs are associated with multiple acute complications for pregnant women and their infants (Brunham et al., 1990) (Table 2-3). Pregnant women with STDs may transmit the infection to the fetus, newborn, or infant through the placenta
Table 2-3 Major Sequelae of STDs
|
Health Consequence |
Women |
Men |
Infants |
|
Cancers |
Cervical cancer Vulva cancer Vaginal cancer Anal cancer Liver cancer T-cell leukemia Kaposi's sarcoma Body cavity lymphoma |
Penile cancer Anal cancer Liver cancer T-cell leukemia Kaposi's sarcoma Body cavity lymphoma |
|
|
Reproductive health problems |
Pelvic inflammatory disease Infertility Ectopic pregnancy Spontaneous abortion |
Epididymitis Prostatitis Infertility |
|
|
Pregnancy-related problems |
Preterm delivery Premature rupture of membranes Puerperal sepsis Postpartum infection |
|
Stillbirth Low birth weight Conjunctivitis Pneumonia Neonatal sepsis Acute hepatitis Neurologic damage Congenital abnormalities |
|
Neurologic problems |
HTLV-associated myelopathy (paralysis) Neurosyphilis |
HTLV-associated myelopathy (paralysis) Neurosyphilis |
Cytomegalovirus-, herpessimplex- virus-, and syphilis-associated neurologic problems; Group B strep meningitis |
|
Other common health consequences |
Chronic liver disease Cirrhosis |
Chronic liver disease Cirrhosis |
Chronic liver disease Cirrhosis |
(congenital infection), during passage through the birth canal (perinatal infection), or after birth as a result of breast-feeding or close direct contact. Common sexually transmitted infections that have been shown to cause adverse health effects among pregnant women and their infants include chlamydial infection, gonorrhea, syphilis, cytomegalovirus infection, genital herpes, and HIV infection. Other sexually transmitted pathogens transmitted from the mother to the fetus, newborn, or infant may produce mainly delayed manifestations that may appear only after years (e.g., human papillomavirus) or even decades (e.g., hepatitis B virus, human T-cell lymphotrophic virus type I).
Active sexually transmitted infection during pregnancy may result in spontaneous abortion, stillbirths, premature rupture of membranes, and preterm delivery. For example, up to 80 percent of pregnancies associated with untreated early syphilis result in stillbirth or clinical evidence of congenital syphilis in the newborn (Schulz et al., 1990). Preterm delivery accounts for approximately 75 percent of neonatal deaths not caused by congenital malformations (Main and Main, 1991). A recent study confirmed that bacterial vaginosis in pregnant women is associated with premature delivery of a low-birth-weight infant; women with bacterial vaginosis are 40 percent more likely to deliver a premature infant compared to women without this condition (Hillier et al., 1995).
Health Consequences for Infected Infants
Sexually transmitted pathogens that have serious consequences among adults tend to cause even more severe, potentially life-threatening health conditions in the fetus or newborn, whose immune system is immature. Damage to the brain, spinal cord, and the organs of special senses (especially the eyes and the auditory nerves) are of particular concern with many sexually transmitted infections in the fetus or infant. Infections with cytomegalovirus, herpes simplex virus, HIV, and human T-cell lymphotropic virus type I, as well as syphilis and gonococcal and chlamydial infection, all can produce one or more of the above complications. Severe, permanent central nervous system manifestations or fetal or neonatal death can result from congenital syphilis. Infection of the fetus with cytomegalovirus may result in growth retardation, destruction of portions of the central nervous system, auditory nerve deafness, low IQ, and damage to other organs. Similarly, severe neurological damage resulting in mental retardation, other manifestations of severe brain damage, or death can result from herpes simplex virus infections.
Currently, essentially all transmission of HIV to young children in the United States is attributable to mother-to-infant transmission. HIV infection progresses more rapidly in infants than in adults; more than 80 percent of untreated infants will develop symptoms of infection by 18-24 months of age (Pizzo et al., 1995). Survival models suggest that there are two distinct groups of HIV-infected infants with regard to survival: the median age at death for the first group, who have
a high probability of dying within four years, is 5-11 months, and the median age at death for the second group is more than five years (Byers et al., 1993).
Human T-cell lymphotropic virus type 1, a retrovirus that is transmitted sexually among adults, is also transmitted perinatally or postnatally from mother to infant and may result in T-cell malignancies and a progressive form of paralysis known as HTLV-1-associated myelopathy later in life. Ophthalmia neonatorum, an eye infection in newborns, results when infants of women with vaginal gonorrhea or chlamydial infection are infected during delivery. Gonococcal ophthalmia neonatorum often produces severe initial inflammation of the tissues around the eye, which may result in corneal ulcers and eventual blindness. Chlamydial pneumonia is also a common illness among infants born to mothers with chlamydial cervical infection. Hepatitis B virus infection, when acquired during birth, becomes a chronic infection in as many as 90 percent of infected newborn infants and may lead to cirrhosis of the liver or liver cancer during midlife in a large proportion of those infected perinatally.
Health Consequences for Infected Pregnant Women
Pregnant women are at increased risk for complications of STDs. Vaginal and cervical infections with STD pathogens can lead to inflammation of the placenta or fetal membranes, resulting in maternal fever during or after delivery, to wound and pelvic infections after Cesarean section, and to postpartum infection of the uterus that may result in infertility (Brunham et al., 1990). As mentioned previously, ectopic pregnancy caused by previous pelvic inflammatory disease is one of the leading causes of maternal death during pregnancy.
Health Consequences for Men
In the United States, HIV infection is currently much more common among men than among women. Acute health consequences of some STDs (e.g., syphilis) are similar in both men and women. Human papillomavirus is associated with cancer of the penis and anus in men; these cancers, however, are less common than cervical cancer in women. Certain STDs, such as gonorrhea and chlamydial infection, produce complications that are unique or more severe in women than in men. However, both gonorrhea and chlamydial infection produce epididymitis in men and chlamydial infection is associated with Reiter's Syndrome, which seems to be more common among men than among women (Berger, 1990). Urethral stricture is a late manifestation of gonorrhea or chlamydial urethritis and is common in developing countries. Infertility seems to be a rare complication of STDs in men. The role of STDs in prostatitis (inflammation of the prostate gland) is uncertain (Colleen and Mårdh, 1990). Over and Piot (1993) compared the health impact of STDs in men and women and have reported that the health burden
attributed to five STDs (i.e., chancroid, chlamydial infection, gonorrhea, HIV infection, and syphilis) in men was also high.
Deaths Associated with STDs
AIDS-associated deaths, which account for the largest number of STD-related deaths, have received considerable attention. Of 513,486 persons with AIDS reported in the United States through December 1995, more than 62 percent (319,849) have died (CDC, 1995b). As indicated above, many other STDs cause potentially fatal complications in adults as well as in the fetus or infant. The largest number of deaths related to STDs other than AIDS are caused by cervical and other human papillomavirus-related cancers; liver disease (e.g., chronic liver disease and liver cancer) caused by hepatitis B virus; pelvic inflammatory disease and ectopic pregnancy; and various pregnancy, fetal, and neonatal complications.
In a recent study completed by investigators at the CDC, more than 150,000 deaths were directly attributed to STDs, including AIDS, from 1973 through 1992 among American women 15 years of age and older (Ebrahim et al., 1995). According to this report, the three leading causes of STD-related deaths in 1992 among these women were cervical cancer (57 percent of deaths), AIDS (29 percent), and hepatitis B and C virus infection (10 percent), all of which are related to viral STDs (Figure 2-4). From 1972 through 1984, the annual number of these STD-related deaths declined by 24 percent; but from 1984 through 1992, STD-related deaths increased by 31 percent, largely as a result of AIDS-related deaths.
In developing countries, the impact of STDs on health also is very substantial. Even when deaths caused by human papillomavirus and hepatitis B virus were not considered, five other STDs (HIV infection, chlamydial infection, gonorrhea, syphilis, and chancroid) ranked among the top 20 causes of loss of productive life in a sub-Saharan African country (Over and Piot, 1993).
Impact of STDs on HIV Transmission
The evidence that "ulcerative" STDs, such as chancroid, syphilis, and genital herpes, and "inflammatory" STDs, such as gonorrhea, chlamydial, and trichomoniasis, increase the risk of HIV infection has developed incrementally over the past decade. Although the proportion of HIV infections that could be prevented in the United States by preventing other STDs has not yet been well defined, current estimates suggest that much—perhaps most—of the heterosexually transmitted HIV infection could be prevented by reducing other underlying STDs.
Epidemiological Evidence
The earliest cross-sectional studies found an association between genital
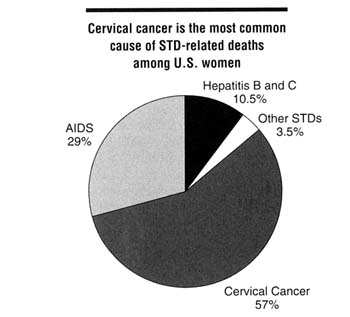
Figure 2-4
Causes of STD-related deaths among U.S. women, 1992. SOURCE: Ebrahim SH, Peterman TA, Zaidi AA, Kamb ML. Mortality related to sexually transmitted diseases in women, U.S., 1973-1992. Proceedings of the Eleventh Meeting of the International Society for STD Research, August 27-30, 1995, New Orleans, LA [abstract no. 343].
ulcers and HIV infection (Kreiss et al., 1986; Greenblatt et al., 1988), but cohort studies were required to assess the temporal relationship between STDs and acquisition of HIV infection and to prospectively obtain other data that might explain away the apparent association. An extensive 1991 review article (Wasserheit, 1992) found that, of 15 studies that had prospectively analyzed the association between STDs and HIV infection, 3 (Cameron et al., 1989; Plummer et al., 1991; Laga et al., 1993) were designed to allow both accurate ascertainment of the occurrence of an STD prior to HIV infection and adjustment for potential confounding by sexual behaviors and condom use.
As summarized in Table 2-4, three prospective cohort studies in Africa have demonstrated increased risk of HIV infection following genital ulcer disease among heterosexual men (Cameron et al., 1989) and among female sex workers3
(Plummer et al., 1991; Nyange et al., 1994). Although the magnitude of the increased risk of transmission attributable to genital ulcers in these studies was expressed as risk ratios ranging from 3.3 to 4.7, Hayes and others (1995) have estimated that genital ulcer disease may increase the per exposure risk of transmission by a factor of 10 to 50 for male-to-female transmission and by a factor of 50 to 300 for female-to-male transmission. Boily and Anderson (1996) also have recently demonstrated that published cohort studies are very likely to underestimate the true magnitude of the increased risk of sexual transmission of HIV conferred by other STDs. Some of these studies have also found that gonorrhea of the cervix (Plummer et al., 1991; Laga et al., 1993; Nyange et al., 1994), chlamydial infection of the cervix (Laga et al., 1993) and vaginal trichomoniasis (Laga et al., 1993), all increase the risk of subsequent HIV infection. Although Laga and others initially reported no increase in HIV infection following genital ulcer disease among female sex workers (Laga et al., 1993), a later study involving the same study population did find such an association (Laga et al., 1994).
In the United States, the multi-center AIDS cohort study found no association between herpes simplex virus type 2 antibody and subsequent HIV infection among men who have sex with men (Kingsley et al., 1990). However, an earlier retrospective cohort study in gay men found that herpes simplex virus type 2 infection was a risk factor for HIV infection (Holmberg et al., 1988). In addition, a study of heterosexual men attending an STD clinic in New York showed that men presenting with chancroid were more likely to become infected with HIV than were men presenting with other STDs (Telzak et al., 1993).
Explaining the Association Between STDs and HIV Infection
The above prospective studies establish the temporal relationship of exposure to STD prior to HIV infection. The observed associations between STDs and HIV infection are compatible with three possible explanations, other than the confounding factors addressed by the study designs:
- STDs increase infectivity of HIV. Persons who have both an STD and HIV infection may be more likely to transmit HIV to others due to the effects of the STD on HIV infectivity, such as increased shedding of HIV.
- STDs increase susceptibility to HIV. Persons with an STD may be more susceptible to a subsequent exposure to HIV, since the STD may compromise the mucosal or cutaneous surfaces of the genital tract that normally act as a barrier against HIV.
- The association between STDs and HIV remains confounded by sexual behavior and/or by immune suppression in persons with sexually acquired HIV. HIV-infected persons may be more likely than uninfected persons to have another STD due to high-risk sexual behavior or because HIV-related immune suppression predisposes to active STD (e.g., by reactivating genital ulcers or by
Table 2-4 Results of Major Epidemiological Studies Regarding the Risk of Subsequent HIV Infection Among Persons with Specific Existing STDs
|
|
|
Relative Risk or Odds Ratios (95% confidence intervals) |
|||||
|
Reference |
Study Site: Population |
Genital Ulcerative Disease |
Syphilis |
Herpes Simplex Virus type 2 |
Gonorrhea |
Chlamydial Infection |
Trichomoniasis |
|
Cameron et al., 1989 |
Nairobi: Male STD patients |
4.7 (1.3, 17) |
|
|
|
|
|
|
Plummer et al., 1991 |
Nairobi: Female sex workers |
3.3 (1.2, 10.1) |
|
|
|
2.7 (0.9, 7.8) |
|
|
Laga et al., 1993 |
Kinshasa: Female sex workers |
|
|
4.8 (2.4, 9.8) |
3.6 (1.3, 11.0) |
1.9 (0.9, 4.1) |
|
|
Telzak et al., 1993 |
New York: Male STD patients |
3.3b (1.1, 10.1) |
|
|
|
|
|
|
Kingsley et al., 1990 |
U.S.: Men who have sex with men |
|
|
1.0 (0.3, 2.9) |
|
|
|
|
Nyange et al., 1994 |
Mombasa: Female sex workers |
4.0 (1.6, 9.9) |
6.5 (1.5, 27.9) |
|
1.8 (1.0, 9.9) |
|
|
- making ulcerative disease harder to cure). Therefore, at any given level of sexual activity, persons exposed to an HIV-infected person may also be exposed to another STD.
Although the third explanation may account for at least some of the association of STDs with subsequent HIV infection, there are strong data to support the concept that STDs increase HIV infectivity and HIV susceptibility. An effect on HIV infectivity is strongly supported by the presence of HIV in genital ulcers (Plummer et al., 1991; Kreiss et al., 1994); by the increased rate of detection of HIV DNA (cell-associated HIV) in cervical swab specimens among women with cervical inflammation (Clemetson et al., 1993; Kreiss et al., 1994; John et al., 1996; Gys et al., 1996; Mostad et al., 1996); by the increased prevalence of HIV DNA in swab specimens from men with gonococcal urethritis (Moss et al., 1995); and by increased concentrations of cell-free HIV RNA in semen from men with gonococcal urethritis (Hoffman et al., 1996). The impact of genital shedding of HIV on sexual or perinatal transmission has yet to be precisely measured but is likely a critical factor in transmission. An effect of other STDs on susceptibility to HIV is supported by studies of couples where one partner was HIV-positive and the other was not. HIV-negative partners who developed genital infections were more likely to become subsequently infected with HIV than were those HIV-negative partners who did not have genital infections (de Vincenzi, 1994; Deschamps et al., 1996).
Evidence of Effect of STD Prevention on HIV Prevention
Several studies provide evidence that early detection and treatment of STDs can have a major impact on sexual transmission of HIV. Moss and colleagues (1995) found that the rate of detection of HIV DNA in urethral specimens among men with gonococcal urethritis fell by half within one to two weeks after curative treatment. It remains unclear if urethral shedding of cell-associated HIV is a good surrogate for HIV infectivity. Moreover, Hoffman and colleagues (1996) recently reported that the concentration of cell-free HIV RNA in semen fell significantly in men after treatment of gonococcal urethritis.
Laga and others (1994) demonstrated that monthly laboratory testing and treatment for STDs reduced the incidence of HIV infection among female sex workers in Zaire. An increasing proportion of visits for STD-related care significantly reduced the incidence of HIV infection over time, among both regular and inconsistent condom users. Nonetheless, such time-series analyses remain subject to participation bias, despite adjusting for frequency of unprotected sex. For example, those with less frequent visits may have had higher-risk partners or riskier behaviors that were not measured. A randomized controlled trial remains essential to prove that STD screening and treatment decrease susceptibility of women to acquisition of HIV.
The strongest data demonstrating that improved STD management reduces sexual transmission of HIV are from the findings of a large, prospective, randomized controlled trial recently completed in Tanzania (Grosskurth et al., 1995a, 1995b). Six pairs of communities were each randomized to receive either improved syndromic management of STDs at the primary care level or the standard management for STDs. Improved syndromic management was developed through extensive training and supervision of primary health center workers, provision of antimicrobials, and educational activities to improve health-care seeking behavior for symptoms of STDs. Sentinel cohorts of one thousand persons per community were followed for two years to measure the incidence of new HIV infections. Overall, the incidence of HIV infection was 42 percent lower in communities with improved management of STDs compared to control communities, and each community with improved STD management experienced a lower incidence of HIV infection compared to the paired control community. The prevalence and incidence of symptomatic urethritis in men and serologic evidence of active syphilis in the sentinel cohorts also were significantly lower in the intervention communities (Hayes et al., 1996). The investigators hypothesized that the reduction of HIV incidence among communities with improved syndromic management of STDs resulted from shortening the duration of STD syndromes among infected persons. These findings suggest that large reductions in STD incidence or prevalence are not necessary to influence HIV transmission. It is possible that greater reductions in STD rates might have produced even greater reductions in HIV incidence.
Estimating the Impact of STDs on HIV Transmission
Estimating the impact of preventive interventions on the transmission of STDs in a population is extremely complex. Static epidemiological models that depend upon relative risks and attributable risks to estimate the contribution of causal factors to noncommunicable disease incidence are not sufficient to estimate the impact of causal factors on communicable diseases, including STDs or HIV (Aral et al., 1996). One also needs to consider partner selection patterns that lead to exposure of uninfected to infected individuals in the population; the prevalence of the causal factor at the point where infected and uninfected individuals mix; and the existence of threshold levels of transmission required to sustain the infection in population subgroups (Anderson and May, 1991).
Retrospective cohort studies in the United States have suggested that other STDs do increase sexual transmission of HIV among men who have sex with men (Darrow et al., 1987; Holmberg et al., 1988). The rapid decline of HIV incidence among these men during the early 1990s was accompanied by rapid declines in STDs such as gonorrhea and syphilis. Declining rates of STDs, along with changing sexual practices, may have contributed to the rapid decline in incidence of HIV infection. However, the strongest evidence for the link between
STD and HIV transmission in the United States is related to heterosexual transmission of HIV. In the United States, heterosexual transmission represents the fastest growing proportion of AIDS cases (CDC, 1994c). Studies indicate that heterosexual transmission of HIV is currently most common among age, ethnic, and socioeconomic groups that have the highest incidence of traditional STDs, such as gonorrhea and syphilis (Ellerbrock et al., 1992; Johnson et al., 1993; Edlin et al., 1994; Levine et al., 1995; Shakarishvili et al., 1995). In addition, increases in syphilis incidence in specific areas throughout the United States have preceded increases in HIV prevalence among prenatal women by about two years (St. Louis et al., 1995). For example, the geographic distribution of reported gonorrhea and syphilis in the United States corresponds closely with the distribution of areas with the highest prevalence of HIV among pregnant women (Figure 2-5).
In the absence of prospective studies or formal trials of strengthened STD interventions to reduce sexual transmission of HIV in the United States (which may not be feasible), mathematical modeling may be essential to assess the potential impact of reducing STDs on HIV transmission. Such models are very complex and dependent on many assumptions related to sexual behaviors, the natural history and epidemiology of STDs, and the interactions between STDs and HIV. Robinson and colleagues (1995) predicted that a 50 percent reduction in the duration of STDs in Uganda could decrease HIV transmission by 43 percent—a prediction remarkably close to that observed in the intervention trial in nearby Tanzania. A number of approaches have been used to model the impact of various determinants on the spread of HIV and other STDs and the influence of other STDs on the HIV epidemic (Appendix C).
Boily has developed a model using published data on the distribution of sexual activity in the United States; estimates of the prevalence and duration of chlamydial infection; the effect of chlamydial on the efficiency of HIV transmission (including effects on infectivity and susceptibility to HIV); assumptions on the patterns of sexual mixing of the U.S. population; and demographic parameters (Appendix C). Given parameter assumptions, the model showed that HIV infection could not be established in the general U.S. heterosexual population in the absence of chlamydial infection (or other STDs with comparable effects on HIV transmission).
The work of Over and Piot (1993) also supports the concept that reducing STDs could have a significant impact on sexually transmitted HIV infections. As mentioned previously, they estimated that successfully treating or preventing one hundred cases of syphilis among high-risk groups for STDs would prevent 1,200 HIV infections that would be linked to those one hundred syphilis infections during a 10-year period.
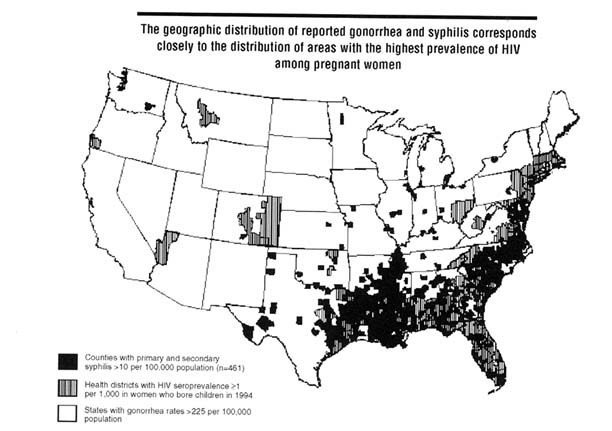
Figure 2-5
Geographic distribution of health districts with highest HIV seroprevalence among women who bore children in 1994, counties with highest reported rates of primary and secondary syphilis in 1993, and states with highest reported rates of gonorrhea in 1993, United States. SOURCE: CDC, Division of STD Prevention, unpublished data, 1996.
Economic Consequences of STDs
While the substantial morbidity caused by STDs is now being more widely recognized, little attention has been paid to what they cost. Limited resources and current competing health care needs, however, are forcing consideration of the economic consequences of STDs as a pivotal criterion for determining the relative urgency of this problem. By this measure also, STDs rank as a formidable health problem.
Estimating STD-Associated Costs
The economic burden of STDs is associated with both direct and indirect cost. Direct costs refer to expenditures for health care and represent the value of goods and services that actually were used to treat STDs or associated sequelae. These direct health care expenditures may be for either medical or nonmedical services and materials. Examples of STD-related direct costs include costs for health professionals' services (i.e., physicians, nurses, and technicians), costs of laboratory services, and cost of hospitalizations for STD (i.e., hospital accommodations and operating room). Resources used for transportation, residential care, special education, and other similar purposes are also considered direct costs. In contrast, indirect costs refer to lost productivity and represent the value of output forgone by individuals with STDs and associated disability. Indirect costs include these lost wages due to not working and/or value of household management that is not performed because of STD-related illnesses. Lost wages due to premature deaths are also considered indirect costs.
The costs of a few STDs have been estimated (IOM, 1985; Washington et al., 1987; Washington and Katz, 1991), but no comprehensive, current analysis of the direct and indirect costs of STDs is available. Such information is vital to accurately depict the full magnitude of the STD problem. Moreover, only with complete STD cost data can the true benefits of investments in STD prevention be assessed. Therefore, the committee commissioned a paper to provide the basis for estimating the economic burden of STDs. Results from this analysis (conducted by Joanna Siegel at the Harvard School of Public Health) are summarized below (Table 2-5) and described in more detail in Appendix D.
Total costs for a selected group of common STDs and related syndromes are estimated to be approximately $10 billion in 1994 dollars (Table 2-5). Important to note is that this rough, conservative estimate does not capture the economic consequences of several other STDs and associated syndromes such as vaginal bacteriosis, trichomoniasis, nongonococcal urethritis, mucopurulent cervicitis, lymphogranuloma venereum, molluscum contagiosum, scabies, and pediculosis pubis. Nor does this estimate include the annual cost of sexually transmitted HIV/AIDS-related illness, which is estimated to be $6.7 billion (Table 2-5). Inclusion of these costs raises the overall cost of sexually transmitted illnesses in the United
Table 2-5 Estimated Costs of Selected STDs and Associated Sequelae in the United States, 1994
|
STD |
Direct Cost (1994$ millions) |
Total Costa (1994$ millions) |
|
Bacterialb |
|
|
|
Chlamydial infection |
1,513.9 |
2,013 |
|
Gonorrhea |
790.6 |
1,051 |
|
Pelvic inflammatory disease |
3,118.8 |
4,148 |
|
Syphilis |
79.4 |
106 |
|
Chancroid |
0.7 |
1 |
|
Viral |
|
|
|
Herpes simplex virus infectionb |
178.3 |
237 |
|
Human papillomavirus infectionc |
2,877.5 |
3,827 |
|
Hepatitis B virus infectiond |
117.0 |
156 |
|
Cervical cancera |
554.0 |
737 |
|
Subtotal STDs (excluding HIV/AIDS) |
7,484.4e |
9,954e |
|
Sexually transmitted HIV/AIDSf |
5,025.0 |
6,683 |
|
Total (including HIV/AIDS)a |
12,509.4 |
16,638 |
|
a Total cost assumes a direct to indirect cost ratio of 3:1 (total cost = direct cost × 1.33); this is based on computed ratios for chlamydia of 1:1 (Washington AE, et al., 1987; see above); pelvic inflammatory disease of 2:1 (Washington AE, Katz P. Cost of and payment source for pelvic inflammatory disease. Trends and projections, 1983 through 2000 [see comments]. JAMA 1991;266:2565-9), and hepatitis B of 1:1 (Hepatitis Branch, CDC, unpublished data, 1996). b Bacterial STD, herpes simplex virus infection, and cervical cancer direct costs estimates from Joanna E. Siegel, Sc.D., Harvard School of Public Health (Appendix D of the present report). Estimate assumes 70 percent of cervical cancer is STD-related. c Human papillomavirus direct cost estimate provided by Laura Koutsky, Ph.D., Center for AIDS and STD, University of Washington, Seattle, based on data from Medicaid and other sources. Cost estimate excludes cost of HPV-related cervical cancer. d Hepatitis B virus infection direct costs based on unpublished data from the Hepatitis Branch, Centers for Disease Control and Prevention, Atlanta. Assumes half of estimated cases are sexually transmitted. e Estimate assumes that the non-pelvic-inflammatory-disease-related costs for chlamydia are approximately $462 million, or approximately 30.5 percent of total chlamydial costs (Washington AE, Johnson RE, Sanders LL. Chlamydia trachomatis infections in the United States: what are they costing us? JAMA 1987;257:2070-2), and the non-pelvic-inflammatory-disease-related costs for gonorrhea are $96.4 million or the cost of just primary treatment for gonorrhea (Appendix D of present report). f HIV/AIDS estimates provided by James G. Kahn, M.D., M.P.H., Institute for Health Policy Studies, University of California, San Francisco, based on data in Hellinger FJ. The lifetime cost of treating a person with HIV. JAMA 1993;270:474-8; CDC. HIV/AIDS surveillance report. Atlanta: Centers for Disease Control and Prevention, 1995;7(2); and Rosenberg PS. Scope of the AIDS epidemic in the United States. Science 1995;270:1372-5. Does not reflect costs of more recently recommended therapeutic regimes for this infection. |
||
States to nearly $17 billion in 1994. These cost estimates underscore the enormous burden of STDs on the U.S. economy. They also represent compelling evidence of the need for effective STD prevention programs, especially in light of the fact that a sizable proportion of the direct costs of STDs results from failure to detect and effectively manage STDs in the initial, acute stage. For example, nearly three-fourths of the $1.5 billion cost of chlamydial infections is due to preventable consequences of untreated, initially uncomplicated infections (Washington et al., 1987; Appendix D).
Sources of Payment for STD-Related Costs
There are limited data regarding who pays for the costs associated with STDs. A study of payment sources for pelvic inflammatory disease from 1983 through 1987 found that private insurance and public payment sources covered 41 and 30 percent, respectively, of the direct costs associated with this STD (Washington and Katz, 1991). During the study period, the proportion of payments from private insurance decreased from 54 to 41 percent. Another study in a Midwest county hospital in 1984 and 1985 showed that 54 percent of total charges associated with pelvic inflammatory disease were not reimbursed by a third-party payer or by county funding to the hospital (Nettleman and Jones, 1989).
Conclusions
STDs affect persons of all racial, cultural, socioeconomic, and religious groups in the United States. Persons of all sexual orientations and sexually active persons in all states, communities, and social networks are at risk for STDs. These diseases are a tremendous health and economic burden on the people of the United States. STDs predominantly affect otherwise healthy youth and young adults, but the consequences can be lifelong. This impact is largely unrecognized by the public and even some health care professionals. Severe complications of STDs include cancer, reproductive health problems, neurologic diseases, and sometimes death. Women and their infants bear a disproportionate burden of these STD-associated complications. The committee estimates that the total annual cost associated with major STDs is approximately $10 billion, which rises to $17 billion when sexually transmitted HIV infections are included. The large number of STD-related deaths and morbidity, and the high costs of managing STDs and their complications, in the United States underscores the importance of effective prevention programs for STDs. Many cases of cancer, infertility, spontaneous abortions, low birth weight, STD-related deaths, and other STD-related conditions are clearly preventable. These data justify investing in effective STD prevention programs to both reduce human suffering and contain health care costs.
The impact of STDs on women's health is substantial. STDs disproportionately impact women because women are more susceptible to infection, they are more likely to have undetected infections, and they are more likely to have STD-related complications compared to men. Adolescents and young adults are at greatest risk for acquiring STDs. Female adolescents appear to be particularly susceptible to several STDs. As described in Chapter 3, adolescents and young adults are also likely to lack information regarding STDs, lack health insurance, and use intoxicating drugs; these factors significantly increase risk for STDs.
Many STDs increase an individual's risk for acquiring and transmitting HIV infection. Therefore, reducing STDs would decrease the incidence of HIV infection in the population. Given the strong association between certain STDs and cervical, liver, and other cancers, cancer prevention programs need to incorporate STD prevention strategies as means for preventing such cancers. As emerging and reemerging infections, new sexually transmitted infections appear on a regular basis and are likely to continue to do so as long as rates of risky sexual behaviors remain high and global economic and demographic factors continue to promote emergence of new STDs. STDs are major international health problems, and all nations will have to contribute to prevention efforts on a global scale.
References
ACS (American Cancer Society). Cancer facts and figures—1996. Atlanta: American Cancer Society, 1996.
AGI (Alan Guttmacher Institute). Sex and America's teenagers. New York: AGI, 1994.
Alter MJ. Heterosexual transmission of hepatitis B and implications for vaccine prevention strategies. Can J Infect Dis 1991;2(suppl A):13A-17A.
Alter MJ, Mast EE. The epidemiology of viral hepatitis in the United States. Gastroenterol Clin of North Am 1994;23:437-55.
AMA (American Medical Association), Council on Scientific Affairs. Health care needs of gay men and lesbians in the United States. JAMA 1996;275:1354-9.
Anderson JE, Brackhill R, Mosher WD. Condom use for disease prevention among unmarried U.S. women. Fam Plann Perspect 1996;28:25-28, 39.
Anderson RM, May RM. Infectious diseases of humans: dynamics and control. Oxford, England: Oxford University Press, Inc., 1991.
Andrus JK, Fleming DW, Harger DR, Chin MY, Bennet DV, Horan JM, et al. Partner notification: can it control epidemic syphilis [see comments]? Ann Intern Med 1990;112:539-43.
Aral SO, Guinan ME. Women and sexually transmitted diseases. In: Holmes KK, Mårdh P-A, Sparling PF, Wiesner PJ, eds. Sexually transmitted diseases. 1st ed. New York: McGraw-Hill, Inc., 1984:85-9.
Aral SO, Holmes KK. Sexually transmitted diseases in the AIDS era. Sci Am 1991;264:62-9.
Aral SO, Holmes KK, Padian NS, Cates W Jr. Overview: individual and population approaches to the epidemiology and prevention of sexually transmitted diseases and human immunodeficiency virus infection. J Inf Dis 1996;174(Suppl 2):S127-33.
Aral SO, Schaffer JE, Mosher WD, Cates W Jr. Gonorrhea rates: what denominator is most appropriate [see comments]? Am J Public Health 1988;78:702-3.
Bauer HM, Ting Y, Greer CE, Chambers JC, Tashiro CJ, Chimera J, et al. Genital human papillomavirus infection in female university students as determined by a PCR-based method. JAMA 1991;265:472-7.
Berger RE. Acute epididymitis. In: Holmes KK, Mårdh P-A, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:641-51.
Berger BJ, Kolton S, Zenilman JM, Cummings MD, Feldman J, McCormack SM. Bacterial vaginosis in lesbians: a sexually transmitted disease. Clin Inf Dis 1995;21:1402-5.
Bevier PJ, Chiasson MA, Hefferman RT, Castro KG. Women at a sexually transmitted disease clinic who reported same-sex contact: their HIV seroprevalence and risk behaviors. Am J Public Health 1995;85:1366-71.
Boily M-C, Anderson RM. Human immunodeficiency virus transmission and the role of other sexually transmitted diseases: measures of association and study design. Sex Transm Dis 1996;23:312-30.
Brinton LA. Epidemiology of cervical cancer—overview. In: Munoz N, Bosch FX, Shah KV, Meheus A, eds. The epidemiology of cervical cancer and human papillomavirus. Lyon, France: IARC, 1992:3-23.
Brunham RC, Holmes KK, Embree JE. Sexually transmitted diseases in pregnancy. In: Holmes KK, Mårdh P-A, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:771-801.
Byers B, Caldwell B, Oxtoby M, Pediatric Spectrum of Disease Project. Survival of children with perinatal HIV infection: Evidence for two distinct populations. Proceedings of the Ninth International Conference on AIDS, June 5-11, 1993, Berlin [abstract no. WS-C10-6].
Cameron DW, Simonsen JN, D'Costa LJ, Ronald AR, Maitha GM, Gakinya MN, et al. Female to male transmission of human immunodeficiency virus type 1: risk factors for seroconversion in men. Lancet 1989; 2:403-7.
Cates W Jr. Epidemiology and control of sexually transmitted diseases in adolescents. In: Schydlower M, Shafer MA, eds. AIDS and other sexually transmitted diseases. Philadelphia: Hanly & Belfus, Inc., 1990:409-27.
Cates W Jr., Joesoef MR, Goldman MB. A typical pelvic inflammatory disease: can we identify clinical predictors? Am J Obstet Gynecol 1993;169:341-6.
CDC (Centers for Disease Control and Prevention). 1993 Sexually transmitted diseases treatment guidelines. MMWR 1993;42(No. RR-14):56-66.
CDC. Decreased susceptibility of Neisseria gonorrhoeae to fluoroquinolones—Ohio and Hawaii, 1992-1994. MMWR 1994a;43:325-7.
CDC. Hepatitis surveillance report no. 55. Atlanta: Centers for Disease Control and Prevention, 1994b:36.
CDC. Heterosexually acquired AIDS—United States, 1993. MMWR 1994c;43:9:156-60.
CDC. Ectopic pregnancy—United States, 1990-1992. MMWR 1995a;44:46-8.
CDC. HIV/AIDS surveillance report. Atlanta: Centers for Disease Control and Prevention, 1995b;7(2).
CDC. Trends in sexual risk behavior among high school students—United States, 1990, 1991, and 1993. MMWR 1995c;44:124-5, 131-2.
CDC. Ten leading nationally notifiable infectious diseases—United States, 1995. MMWR 1996;45:883-4.
CDC, DSTD/HIVP (Division of STD/HIV Prevention). Annual report 1992. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1993.
CDC, DSTD/HIVP. Annual report 1994. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1995.
CDC, DSTDP (Division of STD Prevention). Sexually transmitted disease surveillance 1994. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1995.
CDC, DSTDP. Sexually transmitted disease surveillance 1995. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, September 1996.
CDC, Hepatitis Branch. Epidemiology and prevention of viral hepatitis A to E: an overview . U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1995. [slide set]
Chang Y, Cesarman E, Pessin MS, Lee F, Culpepper J, Knowles DM, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science 1994;266:1865-9.
Christenson B, Bottiger M, Svensson A, Jeansson S. A 15-year surveillance study of antibodies to herpes simplex virus types 1 and 2 in a cohort of young girls. J Infect 1992;25:147-54.
Chu SY, Buehler JW, Fleming PL, Berkelman RL. Epidemiology of reported cases of AIDS in lesbians: United States 1980-1989. Am J Public Health 1990;80:1380-1.
Chu SY, Conti L, Schable BA, Diaz T. Female-to-female sexual contact and HIV transmission. JAMA 1994;272:433.
Clemetson DB, Moss GB, Willerford DM, Hensel M, Emonyi W, Holmes KK, et al. Detection of HIV DNA in cervical and vaginal secretions. Prevalence and correlates among women in Nairobi, Kenya. JAMA 1993;269:2860-4.
Cohen H, Marmor M, Wolfe H, Ribble D. Risk assessment of HIV transmission among lesbians. J Acquir Immune Defic Syndr 1993;6:1173-4.
Colleen S, Mårdh PA. Prostatitis. In: Holmes KK, Mårdh P-A, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:653-61.
Darrow WW, Echenberg DF, Jaffe HW, O'Malley PM, Byers RH, Getchell JP, et al. Risk factors for human immunodeficiency virus (HIV) infections in homosexual men. Am J Public Health 1987;77:479-83.
Deschamps MM, Pape JW, Hafner A, Johnson WD. Heterosexual transmission of HIV in Haiti. Ann Intern Med 1996;125:324-30.
de Vincenzi I. A longitudinal study of human immunodeficiency virus transmission by heterosexual partners. European Study Group on Heterosexual Transmission of HIV [see comments]. N Engl J Med 1994; 331:341-6.
Donegan SP, Jani DB, Flaherty EE, Heeren TC, Rice PA. The male to female transmission of Neisseria gonorrhoeae is influenced by level of antibody to gonococcal reduction modifiable protein (Rmp) or protein III. In: Conde-Glez CJ, Morse S, Rice P, Sparling PF, Calderon E, eds. Pathobiology and immunology of Neisseriaceae. National Institute of Public Health, Cuernavaca, Mexico, 1994 p. 645.
Ebrahim SH, Peterman TA, Zaidi AA, Kamb ML. Mortality related to sexually transmitted diseases in women, U.S., 1973-1992. Eleventh Meeting of the International Society for STD Research, August 27-30, 1995, New Orleans, LA [abstract no. 343].
Edlin BR, Irwin KL, Faruque S, McCoy CB, World C, Seranno Y, et al. Intersecting epidemics—crack cocaine use and HIV infection among inner-city young adults. Multi-center Crack Cocaine and HIV Infection Study Team . N Engl J Med 1994;331:1422-7.
Ellen JM, Kohn RP, Bolan GA, Shiboski S, Krieger N. Socioeconomic differences in sexually transmitted disease rates among black and white adolescents, San Francisco, 1990 to 1992. Am J Public Health 1995;85:1546-8.
Ellerbrock TV, Lieb S, Harrington PE, Bush TJ, Schoenfisch SA, Oxtoby MJ, et al. Heterosexually transmitted human immunodeficiency virus infection among pregnant women in a rural Florida community. N Engl J Med 1992;327:1704-9.
Farley TA, Hadler JL, Gunn RA. The syphilis epidemic in Connecticut: relationship to drug use and prostitution. Sex Transm Dis 1990;17:163-8.
Fish AN, Fairweather DV, Oriel JD, Ridgeway GL. Chlamydial trachomatis infection in a gynecology clinic population: identification of high-risk groups and the value of contact tracing. Eur J Obstet Gynecol Reprod Biol 1989;31:67-74.
GDHR (Georgia Department of Human Resources), Epidemiology and Prevention Branch. Fluoroquinolone resistant Neisseria gonorrhoeae in Georgia. Georgia Epideml Rep 1995;11:2-3.
Goldstein S, Alter M, Moyer L, Kaluba J, Mahoney F, et al. The incidence and epidemiology of acute hepatitis B in the United States; 1989-1994. Ninth Triannual International Symposium on Viral Hepatitis and Liver Disease, April 21-25, 1996, Rome [abstract no. A234].
Greenblatt RM, Lukehart SA, Plummer FA, Quinn TC, Critchlow CW, Ashley RL, D'Costa LJ, Ndinya-Achola JO, Corey L, Ronald AR, Holmes KK. Genital ulceration as a risk factor for human immunodeficiency virus infection. AIDS 1988;2:47-50.
Grosskurth H, Mosha F, Todd J, Mwijarubi E, Klokke A, Senkoro K, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomized controlled trial [see comments]. Lancet 1995a;346:530-6.
Grosskurth H, Mosha F, Todd J, Senkoro K, Newell J, Klokke A, et al. A community trial of the impact of improved STD treatment on the HIV epidemic in rural Tanzania: 2. Baseline survey results. AIDS 1995b;9:927-34.
Gys PD, Fransen K, Diallo MO, Ettiegne-Traore V, Maurice C, Hoyi-Adansou YM, et al. The association between cervico-vaginal HIV-1 shedding and STD, immunosuppression, and serum HIV-1 load in female sex workers in Abidjan, Côte D'Ivoire. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. WeC 332].
Hahn RA, Magder LS, Aral SO, Johnson RE, Larsen SA. Race and the prevalence of syphilis seroreactivity in the United States population: a national sero-epidemiologic study. Am J Public Health 1989;79:467-70.
Harlap S, Kost K, Forrest JD. Preventing pregnancy, protecting health: a new look at birth control choices in the United States. New York: Alan Guttmacher Institute, 1991.
Hauth JC, Goldenberg RL, Andrews WW, Dubard MD, Copper RL. Reduced incidence of preterm delivery with metronidazole and erythromycin in women with bacterial vaginosis. N Engl J Med 1995;333:1732-6.
Haverkos HW. Female-to-male transmission of HIV [letter]. JAMA 1992;268:1855.
Hayes R, Mwijarubi E, Grosskurth H, Heiner J, Fosha F, Mayaud P, et al. Improved STD treatment significantly reduces prevalence of syphilis and symptomatic urethritis in rural Tanzania. Eleventh International AIDS Conference, July 7-12, 1996, Vancouver [abstract no. LB.C.6062].
Hayes RJ, Schulz KF, Plummer FA. The cofactor effect of genital ulcers on the per exposure risk of HIV transmission in sub-Saharan Africa. J Trop Med Hyg 1995;98:1-8.
Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, Martin DH, et al. Association between bacterial vaginosis and preterm delivery of a low birth-weight infant. N Engl J Med 1995;333:1737-42.
Hillis SD, Joesoef R, Marchbanks PA, Wasserheit JN, Cates W Jr., Westrom L. Delayed care of pelvic inflammatory disease as a risk factor for impaired fertility. Am J Obstet Gynecol 1993;168:1503-9.
Hoffman I, Maida M, Royce R, Costello-Daly C, Kazembe P, Vernazza P, et al. Effects of urethritis therapy on the concentration of HIV-1 in seminal plasma. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. mo.C.903].
Holmberg SD, Stewart JA, Gerber AR, Byers RH, Lee FK, O'Malley PM, et al. Prior herpes simplex virus type 2 infection as a risk factor for HIV infection. JAMA 1988;259:1048-50.
Holmes KK, Johnson DW, Trostle HJ. An estimate of the risk of men acquiring gonorrhea by sexual contact with infected females. Am J Epidemiol 1970;91:170-4.
Hook EW III, Handsfield HH. Gonococcal infections in the adult. In: Holmes KK, Mårdh PA, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:149-65.
Hooper RR, Reynolds GH, Hones OG, Zaid A, Weisner PJ, Latimer KP, et al. Cohort study of venereal disease. I: The risk of gonorrhea transmission from infected women to men. Am J Epidemiol 1978;108:136-44.
IOM (Institute of Medicine). New vaccine development: establishing priorities; vol. I, Diseases of importance in the United States. Washington, D.C.: National Academy Press, 1985.
IOM. Emerging infections: microbial threats to health in the United States. Washington, D.C.: National Academy Press, 1992.
John G, Nduati R, Mbori-Ngacha D, Overbaugh J, Welch M, Richardson B, et al. Cervico-vaginal HIV-1 DNA in pregnancy. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. WeC. 331].
Johnson R, Lee F, Hadgu A, McQuillan G, Aral S, Keesling S, et al. U.S. genital herpes trends during the first decade of AIDS—prevalences increased in young whites and elevated in blacks. Proceedings of the Tenth Meeting of the International Society for STD Research, August 29-September 1, 1993, Helsinki [abstract no. 22].
Jossens MO, Schachter J, Sweet RL. Risk factors associated with pelvic inflammatory disease of differing microbial etiologies. Obstet Gynecol 1994;83:989-97.
Judson FN. Gonorrhea. Med Clin North Am 1990;74:1353-67.
Kennedy MB, Scarlett MI, Duerr AC, Chu SY. Assessing HIV risk among women who have sex with women: scientific and communication issues. J Am Med Wom Assoc 1995;50:103-7.
Kingsley LA, Armstrong J, Rahman A, Ho M, Rinaldo CR Jr. No association between herpes simplex virus type-2 seropositivity or anogenital lesions and HIV seroconversion among homosexual men [see comments]. J Acquire Immune Defic Syndr 1990; 3:773-9.
Koutsky LA, Galloway DA, Holmes KK. Epidemiology of genital human papillomavirus infection. Epidemiol Rev 1988;10:122-63.
Kreiss JK, Koech D, Plummer FA, Holmes KK, Lightfoote M, Piot P, et al. AIDS virus infection in Nairobi prostitutes. Spread of the epidemic to East Africa. N Engl J Med 1986;314:414-8.
Kreiss JK, Willerford DM, Hensel M, Emonyi W, Plummer F, Nkinya-Achola J, et al. Association between cervical inflammation and cervical shedding of human immunodeficiency virus DNA. J Infect Dis 1994;170:1597-601.
Krone MR, Kiviat NB, Koutsky LA. The epidemiology of cervical neoplasms. In: Luesley D, Jordan J, Richart RM, eds. Intraepithelial neoplasia of the lower genital tract. New York: Churchill Livingston, Inc., 1995: 49.
Kurman RJ, Henson DE, Herbst AL, Nolter KL, Schiffman MH, for the 1992 National Cancer Institute Workshop. Interim guidelines for the management of abnormal cervical cytology. JAMA 1994;271:1866-9.
Laga M, Alary M, Nzila N, Manoka AT, Tuliza M, Behets F, et al. Condom promotion, sexually transmitted diseases treatment, and declining incidence of HIV-1 infection in female Zairian sex workers. Lancet 1994;344:246-8.
Laga M, Manoka A, Kivuvu M, Malele B, Tuliza M, Nzila N, et al. Non ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS 1993;7:95-102.
Laumann EO, Gagnon JH, Michael RT, Michaels S. The social organization of sexuality: Sexual practices in the United States. Chicago: University of Chicago Press, 1994.
Levine WC, Hughes E, Turner N, et al. Dual epidemics of syphilis and HIV infection among adolescent African-American women in Houston, 1988-1993. Eleventh Meeting of the International Society for STD Research, August 27-30, 1995, New Orleans, LA [abstract no. 51].
Main DM, Main EK. Preterm birth. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: normal and problem pregnancies. 2nd ed. New York: Churchill Livingstone, Inc., 1991:829-80.
Marchbanks PA, Annegers, JF, Coulam CB, Strathy JH, Kurland LT. Risk factors for ectopic pregnancy. A population-based study. JAMA 1988;259:1823-7.
Marrazzo JM, Stine K, Handsfield HH, Kiviat NB, Koutsky LA. Epidemiology of sexually transmitted diseases and cervical neoplasia in lesbian and bisexual women. 18th Conference of the National Lesbian and Gay Health Association, July 13-16, 1996, Seattle, WA [abstract no. C2483]
McCormack WM. Pelvic inflammatory disease [see comments]. N Engl J Med 1994;330:115-9.
Mertz GJ, Benedetti J, Ashley R, Selke SA, Corey L. Risk factors for the sexual transmission of genital herpes. Ann Intern Med 1992;116:197-202.
Moore J, Beeker C, Harrison JS, Eng TR, Doll LS. HIV risk behavior among Peace Corps volunteers. AIDS 1995;9:95-9.
Morell V. Attacking the causes of ''silent" infertility. Science 1995;269:775-7.
Moscicki AB, Palefsky J, Gonzales J, Schoolnik GK. Human papillomavirus infection in sexually active adolescent females: prevalence and risk factors. Pediatr Res 1990;28:507-13.
Moss GB, Overbaugh J, Welch M, Reilly M, Bwayo J, Plummer FA, et al. Human immunodeficiency virus DNA in urethral secretions in men: association with gonococcal urethritis and CD4 depletion. J Infect Dis 1995; 172:1469-74.
Mostad S, Welch M, Chohan B, Reilly M, Overbaugh J, Mandaliya K, et al. Cervical and vaginal HIV-1 DNA shedding in female STD clinic attenders. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. WeC 333].
NCHS (National Center for Health Statistics). Advanced report of final mortality statistics, 1992. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, Hyattsville, MD, 1994. Monthly vital statistics report 43(6 Suppl).
Nettleman MD, Jones RB. Proportional payment for pelvic inflammatory disease: who should pay for chlamydial screening? Sex Transm Dis 1989;16:36-40.
NIH (National Institutes of Health). Consensus Development Conference statement on cervical cancer. National Institutes of Health, Bethesda, MD, April 1-3, 1996.
Nyange P, Martin H, Mandaliya K, Jackson D, Ndinya-Achola JO, Ngugi E, et al. Cofactors for heterosexual transmission of HIV to prostitutes in Mombasa Kenya. Ninth International Conference on AIDS and STD in Africa, December 10-14, 1994, Kampala, Uganda.
Over M, Piot P. HIV infection and sexually transmitted disease. In: Jamison DT, Mosley WH, Measham AR, Bobadilla JL, eds. Disease control priorities in developing countries. New York: Oxford University Press, 1993:455-527.
Over M, Piot P. Human immunodeficiency virus infection and other sexually transmitted diseases in developing countries: public health importance and priorities for resouce allocation. J Infect Dis 1996; 174 (Suppl 2):S162-75.
Paavonen J, Koutsky LA, Kiviat N. Cervical neoplasia and other STD-related genital and anal neoplasias. In: Holmes KK, Mårdh P-A, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:561-92.
Padian N, Shiboski SC, Jewell NP. Female-to-male transmission of human immunodeficiency virus. JAMA 1991;266:1664-7.
Peterman TA, Stoneburner RL, Allen JR, Jaffee HW, Curran JW. Risk of human immunodeficiency virus transmission from heterosexual adults with transfusion-associated infections [published erratum appears in JAMA 1989;262:502]. JAMA 1988;259:55-8.
Piot P, Islam MQ. Sexually transmitted diseases in the 1990s. Global epidemiology and challenges for control. Sex Transm Dis 1994;21(2 Suppl):S7-S13.
Pizzo PA, Wilfert CM, Pediatric AIDS Siena Workshop II. Markers and determinants of disease progression in children with HIV infection. Report of a consensus workshop June 4-6, 1993, Siena, Italy. J Acquire Immune Defic Syndr Hum Retrovirol 1995;8:30-44.
Platt R, Rice PA, McCormack WM. Risk of acquiring gonorrhea and prevalence of abnormal adnexal findings among women recently exposed to gonorrhea. JAMA 1983;250:3205-9.
Plummer FA, Simonsen JN, Cameron DW, Ndinya-Achola JO, Kreiss JK, Gakinya MN, et al. Cofactors in male-female transmission of human immunodeficiency virus type 1. J Infect Dis 1991;163:233-9.
Quinn TC, Cates W Jr. Epidemiology of sexually transmitted diseases in the 1990s. Adv Host Defen Mech 1992; 8:1-37.
Reeves WC, Rawls WE, Brinton LA. Epidemiology of genital papillomaviruses and cervical cancer. Rev Infect Dis 1989;11:426-39.
Robertson P, Schachter J. Failure to identify venereal disease in a lesbian population. Sex Transm Dis 1981;8:75-6.
Robinson NJ, Mulder DW, Auvert B, Hayes RJ. Modeling the impact of alternative HIV intervention strategies in rural Uganda. AIDS 1995; 9:1263-70.
Rolfs RT, Galaid EI, Zaidi AA. Pelvic inflammatory disease: trends in hospitalizations and office visits, 1979 through 1988. Am J Obstet Gynecol 1992;166:983-90.
Rolfs RT, Goldberg M, Sharrar RG. Risk factors for syphilis: cocaine use and prostitution. Am J Public Health 1990;80:853-7.
Rosenberg PS. Scope of the AIDS epidemic in the United States. Science 1995;270:1372-5.
Schiffman MH. Recent progress in defining the epidemiology of human papillomavirus infection and cervical neoplasia. J Natl Cancer Inst 1992;84:394-8.
Schulz KF, Murphy FK, Patamasucon P, Meheus AZ. Congenital syphilis. In: Holmes KK, Mårdh P-A, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:821-42.
Shafer MA, Prager V, Shalwitz J, Vaughan E, Moscicki B, Brown R, et al. Prevalence of urethral Chlamydia trachomatis and Neisseria gonorrhoea among asymptomatic, sexually active adolescent boys. J Infect Dis 1987;156:223-4.
Shakarishvili A, Groseclose SL, Hadgu A, Johnson RE, Hayman CR, Miller CA, et al. Chlamydial trachomatis genital infection in disadvantaged young women across the United States: findings from the U.S. Job Corps. Eleventh Meeting of the International Society for STD Research, August 27-30, 1995, New Orleans, LA [abstract no. 23].
Stamm WE, Holmes KK. Chlamydial trachomatis infections in the adult. In: Holmes KK, Mårdh P-A, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:181-93.
St. Louis ME, Gwinn M, Nakashima A, Davis S, Steinberg S, Wasserheit JN, et al. Covariation of HIV infection among childbearing women with other sexually transmitted diseases in the United States. Eleventh Meeting of the International Society for STD Research, August 27-30, 1995, New Orleans, LA [abstract no. 50].
Telzak EE, Chiasson MA, Bevier PJ, Stoneburner RL, Castro KG, Jaffe HW. HIV-1 seroconversion in patients with and without genital ulcer disease . A prospective study. Ann Int Med 1993;119:1181-6.
Toomey KE, Moran JS, Raffety MP, Beckett GA. Epidemiological considerations of sexually transmitted diseases in underserved populations. Infect Dis Clinics N Am 1993;7:739-52.
Toomey KE, Rafferty MP, Stamm WE. Unrecognized high prevalence of Chlamydia trachomatis genital infection in an isolated Alaskan Eskimo population. JAMA 1987;258:53-6.
Washington AE, Cates W Jr., Wasserheit JN. Preventing pelvic inflammatory disease [see comments]. JAMA 1991;266:2574-80.
Washington AE, Johnson RE, Sanders LL. Chlamydia trachomatis infections in the United States: what are they costing us? JAMA 1987;257:2070-2.
Washington AE, Johnson RE, Sanders LL, Barnes RC, Alexander ER. Incidence of Chlamydial trachomatis infections in the United States: using reported Neisseria gonorrhoea as a surrogate. In: Oriel D, Ridgeway HG, Schachter J, et al., eds. Chlamydial infections. Cambridge, England: Cambridge University Press, 1986:487-90.
Washington AE, Katz P. Cost of and payment source for pelvic inflammatory disease. Trends and projections, 1983 through 2000 [see comments]. JAMA 1991;266:2565-9.
Wasserheit JN. Epidemiologic synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis 1992; 9:61-77.
Wasserheit JN. Effect of changes in human ecology and behavior on patterns of sexually transmitted diseases, including human immunodeficiency virus infection. Proc Natl Acad Sci 1994;91:2430-5.
Wasserheit JN, Holmes KK. Reproductive tract infections: challenges for international health policy, programs, and research. In: Germain A, Holmes KK, Piot P, Wasserheit JN, eds. Reproductive
tract infections: global impact and priorities for women's health. New York: Plenum Press, 1992.
Weström L, Joesoef R, Reynolds G, Hagdu A, Thompson SE. Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results . Sex Transm Dis 1992;19:185-92.
WHO (World Health Organization), Global Programme on AIDS. Global prevalence and incidence of selected curable sexually transmitted diseases: overview and estimates. Geneva: WHO, 1996.
Wolner-Hanssen P. Silent pelvic inflammatory disease: is it overstated? Obstet Gynecol 1995;86:321-5.
World Bank. World development report, 1993: Investing in health. New York: Oxford University Press, 1993.









































