9
Managed Care
Managed care has become an important trend in drug abuse treatment. In response to the escalating costs of treatment, managed care proposes to contain costs, increase access, and ensure quality. It entails many changes from traditional fee-for-service coverage, including changes in the organization, financing, and delivery of services—most recognizably through case management, which seeks to match patients to the most appropriate, yet least restrictive, treatment setting.
Despite its enormous growth, there is a dearth of peer-reviewed research about whether managed drug abuse care is achieving these goals. Due to the proprietary nature of data collected by private managed care organizations and the competitive managed care market, most of the studies conducted to date are from Medicaid or other publicly subsidized programs. Further, research has not addressed concerns about patients being denied treatment or being undertreated; the quality of care being reduced; or the cost of care being shifted to families, public health and welfare agencies, and the criminal justice system (Mechanic et al., 1995). Evaluations of the performance of managed care are largely in the form of anecdotal reports, proprietary evaluations, and studies published in journals that are not peer reviewed. The paucity of independent, peer-reviewed research on a topic of such pervasive importance presents health services researchers with an opportunity to provide crucial information to policymakers, payers, providers, and consumers.
This chapter describes the modest body of research on the topic, relying exclusively on government-sponsored or peer-reviewed, published
research. It identifies significant research opportunities in areas such as access, costs, utilization, and treatment outcomes, including quality of care. It also examines the formidable barriers to research and the need to ensure the rapid translation of research results into clinical practice. This chapter uses the term ''managed drug abuse care" to refer to the drug abuse component of managed behavioral health care, the branch of managed care that administratively combines the traditionally separate areas of drug abuse and mental health.
OVERVIEW
Managed behavioral health care is characterized by a variety of approaches designed to control the cost of services by altering the treatment decisions of both patients and providers (IOM, 1989; Mechanic et al., 1995). There is no single model of managed behavioral health care, and the various approaches are evolving rapidly in a dynamic and highly competitive market, thereby hampering research efforts to characterize them and to evaluate their impact. The overall goal is to alter the orientation and restrain the costs of behavioral health care through changes in the organization, financing, and delivery of services. By incorporating the elements of managed care, which are described later in this section, projected costs can be reduced by up to 30 or 40 percent, according to some industry estimates (Geraty et al., 1994).
Virtually unheard of a decade ago, the burgeoning industry of managed behavioral health care is estimated to cover more than 102 million people across the United States, most of whom are insured under employer-sponsored private health insurance (Oss, 1994). This estimate represents the majority of those covered under employer health care plans, given that 143 million people in the U.S. population have such coverage (CRS, 1994). The figure of 120 million enrollees refers to those eligible individuals whose private or public insurance covers managed behavioral health care, not to those who receive treatment. According to a recent, nationally representative survey, about 50 percent of specialty drug abuse providers, both publicly and privately owned, report that an average of 23 percent of their clients have their treatment paid for by managed care (T. D'Aunno, University of Chicago, personal communication, 1995).
Managed behavioral health care is offered most commonly through one of two general types of managed care organizations: health maintenance organizations (HMOs) or carve-out vendors (also known as managed behavioral health care organizations or MBHCOs) (Table 9.1). These organizations are under contract mostly to employers and public agencies, which pay for some or all of the cost of care. Carve-out vendors are fiscal and management intermediaries that typically contract with pro-
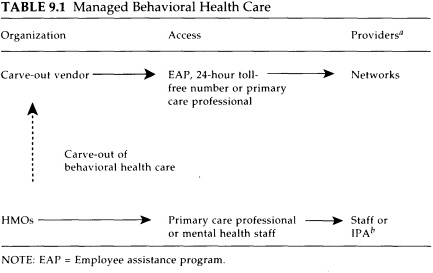
a Institutions, programs, and practitioners.
b Independent practice association, a group of office-based practitioners who operate on a fixed budget under contract to an HMO.
SOURCES: Freeman and Trabin (1994); Suzanne Gelber, Brandeis University, personal communication (1996).
viders for the actual delivery of mental health and drug abuse services through groups of preferred providers organized as networks. Access to the network is controlled by a "gatekeeper" (typically a primary care physician, an evaluation counselor, or a professional with an employee assistance program) who assesses the need for treatment and is responsible for referrals; it is critical that the gatekeeper function be performed by someone credentialed in drug abuse treatment. Carve-out vendors may be specialized units within larger managed care organizations, or they may function independently. It would appear that at each stage in the contracting and subcontracting of treatment there would be additional administrative costs that are not being put into treatment.
Staff model HMOs (those HMOs with salaried staff on-site) have traditionally provided managed behavioral health care through their own staff. Increasingly, however, both staff model HMOs and independent practice association (IPA) HMOs1 are entering into contracts or joint ventures with carve-out vendors to administer and deliver behavioral health
care. Likewise, a traditional fee-for-service (or indemnity) medical insurer may "carve out" behavioral health care through a contract with a carve-out vendor. In such a plan, which accounts for almost 30 percent of managed behavioral plans, the behavioral health care benefit is managed via a network even though other health care benefits in the same plan are not (Foster Higgins, Inc., 1994).
Despite the diversity of managed behavioral health care models, they share four common elements that derive from broader managed care principles (Shueman and Troy, 1994): (1) selective contracting, (2) mechanisms for monitoring or managing services, (3) financing structure, and (4) benefit structure (described below).
Selective Contracting
Managed care organizations refer drug abuse patients to selected individual and institutional providers with whom the companies have negotiated set fees for service, either at a discount from standard rates or on a capitated basis (see below). Patients are penalized financially for using providers outside the network, and the in-network benefits package and provider network tend to be more inclusive and comprehensive. In addition to establishing fees, the contracts between organizations and providers stipulate the providers' roles in adhering to the organization's protocols and procedures for managing patient care, reporting results, and allowing the organization to audit care on a confidential basis.
Mechanisms for Monitoring or Managing Services
These procedures ensure the necessity, appropriateness, and quality of care. They typically involve readmission review; utilization management to refer patients to the most appropriate providers and medically necessary services; utilization management prior to, during, and after discharge from inpatient or 24-hour care; and intensive case management of complex or high-risk cases.
Financing Structure
Managed care organizations commonly operate on a fixed administrative fee basis, on a budget referred to as "capitation" (a flat dollar fee per covered beneficiary), or on a flat fee per case. Rates are negotiated in advance with the employer or entity that hires the managed behavioral health care organization. When the expected rate is exceeded, the managed care organization assumes some or all of the financial risk. This financial risk is sometimes shared "downward" with network practitio-
ners. Risk sharing is intended to provide incentives to deliver cost-effective and innovative services.
Benefit Structure
A benefit plan outlines the services and providers that are covered and the terms of coverage (e.g., beneficiary deductibles or copayments; service duration or limits). Under managed care, the benefit plan usually is designed to give incentives to both patients and providers for early intervention (although this often has not been the case for illicit drug and alcohol dependence), the use of network providers, and the use of services consistent with medical efficacy.
An important element is whether drug abuse benefits are offered as part of an integrated medical plan—a "carve-in" policy—or whether they are separated (like dental care) from other medical services in a "carveout" policy. Carve-in policies, most common in staff model HMOs, offer the potential advantages of increased provider communication and coordination, destigmatization, and accounting for cost offsets (reduced medical costs stemming from treatment of the drug abuse).2 Carve-in policies are potentially advantageous for drug-abusing patients with medical or psychiatric problems (e.g., compliance with antituberculosis therapy has been shown to be most effective when patients' daily medication is directly observed by a health care provider in the context of a treatment program) (Chaulk et al., 1995). It is less burdensome on the patient and more fruitful for public health, because of better compliance, when patients can obtain their primary care and drug abuse treatment at the same site.
On the other hand, carve-out vendors offer the advantages of linkage with employee assistance programs, more specialized medical staff (e.g., medical directors and clinical case managers), more elaborate protocols, more specialized quality management, more extensive customer services and comprehensive network, and the ability to offer a consistent benefit plan anywhere in the United States (S. Gelber, Brandeis University, personal communication, 1996). They also offer a cost-saving alternative for employers who want to retain traditional indemnity medical insurance for employees but feel they cannot afford the expense of unmanaged behavioral health care. One disadvantage is that carve-out vendors may have incentives for cost-shifting,3 because they usually have no responsi-
bility for the provision and/or funding of patients' medical services (Mechanic et al., 1995). This is also true to a lesser extent for carve-in vendors, because they are generally responsible for all health care services. Another disadvantage is fragmentation of the sites of service delivery, which may prove problematic, especially in emergency situations with suicidal patients, since drug abusers often have co-occurring psychiatric disorders (see Chapter 8) (Regier et al., 1990). Data from the National Comorbidity Study revealed that 41-66 percent of those with a lifetime addictive disorder also have a lifetime history of at least one psychiatric disorder (Kessler et al., 1996). Patients with co-occurring addictive and psychiatric disorders are thought to be treated most effectively in integrated systems of care (Osher, 1996).
Drug abuse practitioners and treatment facilities have not fully embraced managed behavioral health care. Their reasons are varied but likely emanate from concerns about decreased professional autonomy, lower fees, the potential for decreased confidentiality of patient records, and enhanced supervision by individuals who may not be credentialed in drug abuse treatment.
Growth of Drug Abuse Treatment Benefits
By the early 1990s, almost 100 percent of employer health plans in medium and large corporations covered some type of drug abuse benefits, either managed or unmanaged. That was in stark contrast to 1983, when only about 43 percent of employers made such provisions (BLS, 1992, 1994). The growth in drug abuse coverage stemmed from rising employee demand, state mandates, and awareness by employers and clinicians that untreated drug abuse reduces productivity and contributes to absenteeism, health problems, theft, and accidents (IOM, 1995). Drug abuse benefits in conventional, unmanaged indemnity policies were usually subject to special limitations that were more restrictive than general health benefits. The limitations usually pertained to the total number of days of care available per year or to the total dollar amount that could be spent per year, per confinement, or per lifetime. For example, a typical policy restricted inpatient drug abuse care to 30 days per year, restricted outpatient care to 20 to 30 visits per year, and/or contained maximum dollar amounts such as $50,000 per lifetime for all treatment modalities (BLS, 1992, 1994).
By the mid-1980s, managed behavioral health care began to take hold, particularly due to employer pressures for cost containment and the availability of venture capital financing for new carve-out providers (Freeman and Trabin, 1994). Another impetus came from studies showing that many, but not all, drug abuse patients could be treated just as cost-effec-
tively in outpatient settings as they could in more costly inpatient settings (Center of Alcohol Studies, 1993; Alterman et al., 1994). Managed care promised the attractive alternative of lower costs, increased access, and more clinically appropriate treatment. It became so alluring that by the mid-1990s, industry surveys showed private managed behavioral health care enrollment to have increased from 48 million to 60 million over a two-year period (Geraty et al., 1994). Instead of relying on previous benefit plan limitations in treatment dollars or days of coverage, managed care organizations stressed benefit flexibility and patient matching to the most appropriate level of care through individual case management, utilization review, and provider networks. Patient placements were dictated by placement criteria that typically were developed internally but were not made available publicly.
One important means of referral into managed drug abuse care has been through employee assistance programs (EAPs). These are workplace programs, usually paid for by employers, designed to help employees address problems that affect their performance, including drug abuse problems. EAPs began in the 1950s as internal occupational alcohol programs run by recovering alcoholics. They often referred alcohol-dependent employees to self-help groups such as Alcoholics Anonymous (Mucnick-Baku and Traw, 1992). Since then, EAPs have proliferated nationwide and have expanded to address other employee problems. With respect to employee drug use, EAPs typically perform a brief assessment or crisis intervention and make referrals to treatment programs. They may also monitor treatment and provide follow-up counseling as part of continuing care. EAPs generally do not provide treatment services (although some offer short-term counseling); rather, they help to ensure that employees receive the treatment they need and return to productive employment. Some EAPs are internal or external stand-alone programs, whereas others are integrated into a treatment network organized through a carve-out vendor and serve as a gateway to treatment (Freeman and Trabin, 1994). A review of EAPs has been performed by the National Research Council (NRC, 1994).
Public Versus Private Systems
The initial growth in managed behavioral health care originally took place in the private sector, through employer-sponsored health insurance, but this trend is changing rapidly. State and local agencies, which pay for the majority of drug abuse clients in treatment, have been forced by budget pressures to turn to carve-out vendors or HMOs to oversee their programs for low-income drug abusers. In other words, state and local authorities are beginning to purchase services from some of the
same organizations under contract to private employers. While it is not known how many Medicaid recipients or other publicly subsidized clients are covered by managed behavioral health care, about 7.8 million (25 percent) Medicaid recipients are enrolled in managed care in general (Rowland et al., 1995). A number of states—including Massachusetts, Ohio, and Minnesota—have developed managed drug abuse care for their Medicaid patients through special waivers from the agency that oversees the Medicaid program, the Health Care Financing Administration (HCFA).4 About 30 states have waivers approved or pending (Kushner, 1995).
Greater reliance on carve-out vendors and HMOs to manage public and private drug abuse patients may have the potential to reverse the historic separation between privately and publicly funded drug abuse treatment providers. An earlier Institute of Medicine (IOM) report described the drug abuse treatment system as a "two-tiered system" (IOM, 1990). A private tier of providers serves clients who have private health insurance or sufficient resources to pay for expensive treatment out of pocket. The public—tier-which accounts for the majority of clients and treatment expenditures (Batten et al., 1992)—serves mostly indigent clients and is made up of publicly owned programs or private not-for-profit programs whose revenues are largely from public agencies. Publicly funded clients are heavier users of drug abuse services than privately funded clients, in part because they enter treatment with a greater degree of impairment and more associated psychiatric and medical problems. They also often lack the financial, social, and emotional resources available to private populations. Among public sector patients, disabled clients who receive Supplemental Security Income use services with far greater intensity than other publicly subsidized clients (Callahan et al., 1994), thus underscoring the importance of associated problems in contributing to the complexity and expense of treatment. It will be important to monitor the outcome of treatment provided to both public and private clients if these sectors are integrated under managed care.
The major stakeholders in managed drug abuse treatment are regulators, payers, managed care organizations, providers, advocates, and clients (Figure 9.1). In a typical example, an employer or public purchaser hires a managed care organization, which in turn contracts with mental health and drug abuse practitioners to offer services to enrollees. In 1992,
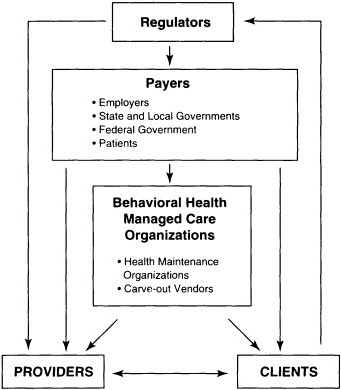
FIGURE 9.1 Stakeholders in behavioral health managed care.
Massachusetts was the first state to transfer all of its non-HMO Medicaid patients to a private carve-out vendor, which established a network of mental health and drug abuse providers. In contrast, the Department of Veterans Affairs (VA) medical centers still function as both the payer for and the provider of a range of drug abuse, psychiatric, and medical treatments in a capitated arrangement. These medical centers operate somewhat like HMOs, but without many of the managed care elements described earlier.
Until there is a solid body of independent research evaluating managed drug abuse care, both the putative benefits and the risks remain unsubstantiated. Thus far, managed drug abuse care has largely eluded scrutiny by the health services research community for reasons described at the end of this chapter. The models of managed drug abuse care are best developed for employed, middle- to upper-class patients. These patients are much less disabled than lower-income, publicly subsidized pa-
tients who are likely to have greater treatment needs. However, there is little published information about the most elementary characteristics of managed drug abuse treatment, such as staff-client ratios, staff training, and frequency and duration of services. Even less is known about the impact on patient care of financial incentives to curtail costs. Finally, although managed behavioral health care organizations appear to be increasingly willing to publish their patient placement criteria, little is known about whether these criteria are actually adhered to by those responsible for making placements. Thus, there is a need to undertake studies of the organization, financing, and characteristics of managed drug abuse care.
The committee recommends that the appropriate federal agencies (e.g., the Substance Abuse and Mental Health Services Administration [SAMHSA], the Health Care Financing Administration [HCFA], the National Institute on Drug Abuse [NIDA], and the National Institute on Alcohol Abuse and Alcoholism [NIAAA]) and private organizations undertake studies of the organization, financing, and characteristics of drug abuse treatment in the managed care setting, including variations in the content, intensity, continuum of care, and duration of treatment as they relate to patient needs.
Particular attention needs to be given to well-controlled studies of patient outcomes for private and public sector patients, credentials of gatekeepers, accountability systems, and patient placement criteria.
ACCOMPLISHMENTS AND RESEARCH OPPORTUNITIES
Access, Costs, and Utilization
Four major studies have examined the impact of managed care on access to drug abuse treatment, cost of treatment, and utilization of services. All four were conducted in naturalistic, nonexperimental settings, and three of the four examined Medicaid populations (Table 9.2). These studies were methodologically diverse and examined various models of managed care, but all four compared managed care with unmanaged care and/or alternative models of managed care—the kinds of comparisons that are most compelling for those responsible for choosing among different managed and unmanaged plans for their beneficiaries.
In 1992, Massachusetts instituted a privately contracted managed care program for Medicaid patients. Research on this program documented a 48 percent reduction in drug abuse treatment expenditures per enrollee in the first year of the program, compared with the prior year's fee-for-
TABLE 9.2 Access, Cost, and Utilization Comparisons Between Managed Substance Abuse Treatment and Fee-for Service Treatment
|
Study |
Comparison Groups |
Client Types |
Number of Clients |
Access |
Cost per Enrollee |
Utilization |
|||
|
Callahan et al., 1994a |
Before v.s. after |
Public |
375,000 |
5% |
|
-48% |
|
IP |
-69% -4% 20% |
|
Ellis, 1992a |
Before v.s. after |
Private |
140,000 |
-43% |
|
-72% |
|
IP OP OC |
-41% 19% 54% |
|
Asher et al., 1995b |
County v.s. PPO v.s. HMO v.s. FFS |
Public |
10,000 |
County PPO HMO FFS |
4.9% 3.9% 2.0% N/A |
County PPO HMO FFS |
$4,553c $5,397 $7,720 $4,840 |
County PPO HMO FFS |
35.7 units 11.7 units 11.8 units 18.6 units |
|
Minnesota Department of Human Services, 1995b |
Fund (FFS) v.s. prepaid |
Public |
740d |
N/A |
|
N/A |
|
Fund IP Fund OP Prepared IP |
48% 52% 27% |
|
|
Prepaid OP |
73% |
|||||||
|
IP = inpatient; N/A= not applicable; OC = office claims; OP = outpatient; PPO = preferred provider organization. a These studies were before- and after-comparisons; data are presented in relative values. b These studies compared several plans during one time period; data are presented in absolute values. c Cost per client instead of cost per enrollee. d 1994 clients only. |
|||||||||
service (FFS) system (Callahan et al., 1994). This average decrease reflected a 67 percent reduction in expenditures for 24-hour care and an 8 percent increase in outpatient expenditures per enrollee. Access, as measured by the number of service users for every 1,000 enrollees, increased by 4.6 percent.5 Inpatient length of stay declined by 25.4 percent. Inpatient admissions for drug abuse treatment declined by 69 percent from the prior year, much of which was attributed to the program's provision for detoxification in nonhospital settings (where utilization surged). Denial of request for 24-hour care was about 7 percent at the beginning of the program but declined to about 3 percent by the end of the first year. Because of the absence of data from the prior year, there was no basis for comparison with denials in the earlier FFS program, which was also the case with quality of care. Nevertheless, providers perceived quality improvements relative to the FFS system, according to a provider survey included in the analysis.
Some of those same trends were found in the second year of the managed care program. Enrollment increased by 3 percent, and there was a gain in access of 5 percent (in terms of the number of users per 1,000 enrollees) compared with the first year (Beinecke et al., 1995). Inpatient utilization continued to decline, but acute residential days increased by 72 percent. Expenditures for inpatient and outpatient drug abuse care declined by 32 and 9 percent, respectively. Surveys of providers and patients reinforced the earlier year's perception of improved access and quality.
A study of privately insured patients found some similar results (Ellis, 1992). This study took advantage of a natural experiment by a private employer whose health coverage extended to 140,000 employees, retirees, and dependents. The employer mandated managed drug abuse and mental health benefits through a preferred provider organization (PPO) at the beginning of the third year of this four-year study (1986-1990). Access, cost, and utilization were compared between year two and year four. For drug abuse treatment, the study found that access—as measured by the number of patients per 1,000 enrollees—declined by 43 percent. This dramatic decline was most likely the result of an increase in the average charge per inpatient episode of treatment, leading fewer to seek treatment, rather than to patients' being denied treatment. The average charges per enrollee declined by 72 percent over the two-year period, from $778 to $216. The decrease was attributed to reductions in the number of patients seeking treatment, the number of episodes per patient, and the average
charges per episode. Correspondingly, inpatient episodes per patient declined by 41 percent, outpatient episodes increased by 19 percent, and office visit claims increased by 54 percent. Clearly, the paramount finding of the study was the significant decline in drug abuse treatment costs per enrollee.
A third study examined the Minnesota Consolidated Chemical Dependency Treatment Fund, which pooled different funding streams for publicly subsidized drug abuse clients who had previously been treated in a patchwork of programs with varying requirements for eligibility and service delivery. The Minnesota fund operated on a FFS basis but incorporated standardized assessment and treatment placement criteria, features of managed care. The fund increased access by about 30 percent and was associated with lower costs per treated client relative to prior years (Minnesota Department of Human Services, 1993).
Because of perceived opportunities for further cost savings, the Minnesota fund is being phased out in favor of legally mandated prepaid plans. This transition was examined in a study comparing a sample of prepaid plan admissions with a matched, randomly selected sample of fund admissions; both plans have the same patient placement criteria (Minnesota Department of Human Services, 1995). The study examined treatment placement, completion, and length of stay each year over a three-year period. In 1994, prepaid clients were far less likely to be placed in inpatient settings (27 percent for prepaid plan clients versus 48 percent for fund clients). Correspondingly, 73 percent of prepaid admissions were to the outpatient setting, compared with 52 percent of fund admissions. There were no differences in severity of inpatient admissions, treatment completion rate, or outpatient length of stay. Neither access, cost, nor outcome comparisons were made between the two programs in this study.
The fourth study is the only one thus far to compare several different models of managed care with a FFS model (Figure 9.2; Asher et al., 1995). The study was the outgrowth of a Pennsylvania law, passed in 1988, that was designed to provide Medicaid patients with a broader continuum of drug abuse care. Before passage of the legislation, Medicaid clients were restricted to costly hospital-based services, methadone maintenance, and outpatient drug-free services; they were denied access to short- and longterm residential services. When the new statewide system was implemented, Medicaid enrollees were assigned to one of four types of providers: a county agency, an HMO, a PPO, or a FFS.6 The first three groups
had varying features of managed care, whereas the FFS group was considered the "control" group. The county providers used a mix of managed and unmanaged elements; they operated on a fixed budget and used a case manager to assign patients to the most appropriate care, but each service was reimbursed on an FFS basis.
Drug abuse treatment services were provided to 10,000 clients over the course of an 18-month study period from 1990 to 1991. The demographic characteristics of each study group were similar, but the pretreatment level of drug abuse severity was unknown (except for county clients). Measures of access, cost, and utilization were examined retrospectively (see next section for discussion of outcome findings), and on all of these measures, county clients fared the best and HMO clients fared the worst.
County clients experienced the highest degree of access (4.9 percent of eligible recipients), followed by PPO clients (3.9 percent) and then by HMO clients (2 percent); the degree of access was not documented for FFS clients. County patients also received the greatest average number of units of service for the lowest average cost per client, followed by FFS patients and then by PPO patients; the HMO provided the least amount of services for the greatest cost per patient (Figure 9.2). A unit of service was calculated by a special formula that created comparability across different service modalities. The FFS group received the most inpatient care, whereas the HMO group received the least. HMO patients with the greatest need for services were given intensive outpatient treatment almost exclusively, an option not available to the four other groups of patients.
The four studies described in this section allow some tentative conclusions. All of the studies reported lower costs in managed drug abuse care relative to traditional FFS plans. In almost all of the studies, there appeared to be a shift in the delivery of treatment from inpatient to outpatient settings. These findings are consistent with those of a comprehensive literature analysis of managed care plan performance since 1980 for all medical services (Miller and Luft, 1994).
Nevertheless, the studies described in this section were not rigorous from an experimental point of view. All were performed in naturalistic settings in which random assignment was not possible, and there were no controls for patient severity. Furthermore, the types of managed care plan under study varied widely. In light of those limitations, it is difficult to draw firm conclusions—or to extrapolate findings—about access, cost, and utilization. There also are virtually no data on the extent of denial of treatment and its impact, a topic discussed later in this chapter.
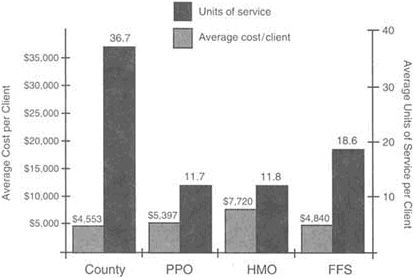
FIGURE 9.2 Cost and utilization comparisons of three managed care models and a fee-for-service model for Pennsylvania Medicaid patients. The county model had the lowest average cost per client for the highest average number of units of service. The second best performer was the fee-for-service model, which had the second lowest cost and the second highest units of service. SOURCE: Asher et al. (1995).
The committee recommends that the appropriate federal agencies (e.g., SAMHSA, NIDA, NIAAA) and private organizations support research on the impact of drug abuse treatment in the managed care setting, including studies on: client access, costs, and utilization; effectiveness and cost-effectiveness of drug abuse treatment under managed care; quality of drug abuse treatment in the managed care setting and its impact on treatment outcomes; development of uniformly accepted patient placement criteria that have predictive validity; and denial of treatment, undertreatment, and cost-shifting practices by providers of managed care (including comparisons between carve-in and carve-out vendors).
Outcomes
Policymakers and employers are placing increasing emphasis on monitoring treatment outcomes under all health care delivery systems, both managed and unmanaged. The purposes of studying outcomes are
TABLE 9.3 Measures of Treatment Effectiveness
|
Reduction in drug use |
|
Abstinence from drug use |
|
Completion of drug treatment |
|
Readmission to drug treatment |
|
Time until readmission to treatment |
|
Client satisfaction with treatment |
|
Improvement in health status and well-being |
|
Improvement in employment and productivity |
|
Reduction in criminal activity |
to determine treatment effectiveness and cost-effectiveness, to improve program performance on the basis of quality, and to improve resource allocation. With those purposes in mind, this section discusses research on the most important outcomes of managed drug abuse care, namely, effectiveness, cost-effectiveness, quality of care, cost offsets, and cost-shifting.
Effectiveness
A universal question asked of managed care is, Does it work? However, the more appropriate questions facing employers and policymakers are slightly different. They need to decide, from among many competing plans, which plan offers the most effective services for their beneficiaries. The key questions are, Does managed care work compared to fee-for service care? and What models of managed care are more effective than others? Measures of the effectiveness of drug abuse treatment, which are used in one or more of the studies cited in this chapter, are listed in Table 9.3.
The first evidence of the effectiveness of managed behavioral health care came from the mental health field. The Medical Outcome Study, a large two-year observational study, compared prepaid care with FFS care for a variety of chronic medical illnesses, including depression. 7 The depression component of the study, which evaluated treatment outcomes for 617 depressed patients, found no differences in treatment effectiveness between the two payment systems when patients were treated by
psychologists and general medical clinicians (Rogers et al., 1993). However, patients with more severe psychiatric disorders, who tended to be treated by psychiatrists, fared worse under prepaid care; those patients used less antidepressant medication over time and had greater limitations in role and physical functioning. Because there was no difference in the baseline degree of impairment between FFS and prepaid patients seen by psychiatrists, the investigators concluded that the differences in outcomes were based on the care received. This conclusion prompted investigators to recommend that policymakers focus attention on patients with the highest levels of impairment.
Two published studies have addressed the effectiveness of managed drug abuse care. The first, described earlier, examined treatment effectiveness in relation to treatment modality in Pennsylvania Medicaid clients (Asher et al., 1995). Treatment modality was a proxy for different types of managed care providers because each provider relied more heavily on one type of modality. The outcome measures covered criminal activity, economic status, medical care, and readmission to drug and alcohol treatment. Comparing the post- with the pretreatment period, the study found that intensive outpatient treatment (which was provided only by HMOs) was the least effective modality, whereas 24-hour longterm residential treatment—a combination of case management techniques and FFS reimbursement—was the most effective modality.
Another study examined the relative effectiveness of managed care and unmanaged care models provided at a single facility for drug abuse treatment, the Castle Medical Center in Hawaii (Renz et al., 1995). Researchers undertook a retrospective review of 1,594 patient records in order to examine treatment outcome and length of stay. Treatment outcome was defined in this study in terms of recidivism (i.e., the return to treatment at the same or higher level of care at any time within the two year study period [January 1, 1990, through December 31, 1991]). Castle Medical Center afforded the opportunity to study the impact of managed care because it provided treatment to four separate groups of patients that were distinguished on the basis of reimbursement mechanisms: intensive managed care, traditional managed care, private pay, and state funded.
The study found that, with respect to recidivism, there were no differences among the four groups in spite of significant baseline differences in age, gender, marital status, and ethnicity. The analysis revealed no significant interactions between these demographic variables and the study findings. In fact, the highest degree of recidivism was dictated not by method of payment but by patient severity (i.e., a high number of ICD-9 [International Classification of Diseases] diagnoses at baseline). With respect to length of stay (defined as the total number of days spent in
treatment converted into weighted hours by a special formula), significant differences among the four groups emerged. The state-funded group had the shortest length of stay, followed by the intensive managed care group and then the traditional managed care group. This suggested to the authors that the state-funded and intensive managed care patients could be treated at lower cost than the traditional managed care patients without compromising treatment effectiveness, although they noted that other outcome measures should be studied besides recidivism.
One of the greatest problems in using client records is the lack of measures of treatment effectiveness. Relapse is a common measure used in research because it is one of the few objective outcome measures for which data are readily available. The Addiction Severity Index, which is one of the most comprehensive and commonly used research instruments for measuring effectiveness, takes about 45-60 minutes to administer at baseline and about 20 minutes at follow-up. It requires administration by a trained technician. Due to the length of time and cost, this type of research instrument would not be feasible in routine clinical use for a variety of reasons. One new outcome instrument, which is being developed to assess the effectiveness of alcoholism treatment, requires only 5 minutes for the average clinician to complete and 20 minutes for the average patient (Rost et al., 1996). There is a critical need for similar, easy to-administer instruments that measure the effectiveness of drug abuse treatment in clinical settings.
One outcome study that did use the Addiction Severity Index, but has not yet been published, compared the effectiveness of FFS drug abuse treatment with that of HMOs. In 1991, when the study began, 75 percent of the study population—Philadelphia Medicaid patients treated by 11 separate programs-were FFS patients; by 1995, 70 percent were treated by HMOs. Each year randomly selected samples of patients were followed through treatment and for six months postdischarge. Since the dramatic shift to managed care was not foreseen at the start of this study, comparisons between FFS and HMO treatment were considered to be inadvertent findings. Patients treated in 1995 received fewer services and experienced worse outcomes relative to those treated in the first year of the study, which suggests superior treatment under FFS (T. McLellan, University of Pennsylvania, personal communication, 1996).
Cost-Effectiveness
The cost-effectiveness outcome measure provides an economic evaluation by comparing alternative treatments to determine which produces a desired outcome for the lowest cost (Center of Alcohol Studies, 1993). There have been only two studies of cost-effectiveness of managed drug
abuse care, both performed at the VA medical center in Philadelphia (Alterman et al., 1994, 1996). VA medical centers operate somewhat like HMOs insofar as they have a fixed annual budget, but they do not incorporate many of the other features of managed care presented earlier. Therefore, the studies described below might be characterized as comparisons between different treatment modalities or intensities, rather than between different models of managed care. They are included here primarily because of their methodological value for future research and the absence of other published cost-effectiveness studies.
The first study compared the costs and effectiveness of day-hospital and inpatient treatment for cocaine dependence. Day-hospital treatment, which consisted of 27 hours per week of treatment, was far less costly than inpatient treatment, which consisted of 48 hours per week. The subjects, 111 male veterans, were assigned randomly to one of the two treatments, after excluding subjects who refused to be randomized and those with the most severe dependence and associated problems (because it would have been unethical and inappropriate to randomize them). This study is unusual because it is the only one described in this chapter to have used random assignment.
The study found no significant differences between day-hospital and inpatient treatment in terms of effectiveness; both were effective at reducing drug use and improving psychological functioning and health status for mildly and moderately impaired patients (Alterman et al., 1994). For example, six months after the one month of treatment, 53 percent of dayhospital and 47 percent of inpatient clients were abstinent from cocaine usage, as determined by the follow-up Addiction Severity Index and urinalysis. There were no significant differences between the two groups on entry into the study, including measures of drug use and social functioning. The most profound difference was the cost. The one-month episode of day-hospital treatment cost providers $2,260, whereas the episode of inpatient treatment cost $6,146. Researchers concluded that day-hospital treatment was more cost-effective, although they still viewed inpatient treatment as best for patients with serious physical, psychiatric, and/or motivational problems, since day-hospital clients were found to be less likely to complete the recommended course of treatment.
A follow-up study compared a scaled-down version of day-hospital treatment (12 hours per week) with an even less intensive outpatient regimen of 6 hours per week (Alterman et al., 1996). The treatments lasted four weeks and the follow-up took place three months after treatment entry. The 50 cocaine-dependent subjects were not assigned randomly, but a random assignment study is now in progress. Contrary to expectations, both groups had similar outcomes on measures of drug use, psychological functioning, and health status. In addition, there were no dif-
ferences between the two groups in program attendance, treatment completion, or baseline demographic and drug use measures. Given its lower cost and similar effectiveness, outpatient treatment offered at this lower level of intensity was clearly more cost-effective, but without random assignment and a longer follow-up period, the investigators did not view the results as generalizable.
Quality of Care
Another fundamental question about managed care models is whether they increase or decrease the quality of care relative to FFS care. The answer is likely to depend on what indicator of quality is used, how it is measured, and the model of managed care that is studied. Some of the major indicators of quality relate to patient satisfaction, time to relapse, and severity of relapse. Other quality indicators relate to the process of care delivery, such as the credentials of providers, the appropriateness of placement, and adherence to practice guidelines (Shueman and Troy, 1994).
Very few studies have examined the quality of managed drug abuse care; some have been cited earlier in this chapter. In the study of managed care versus FFS coverage for the Massachusetts Medicaid population, researchers used readmission rates to 24-hour care as a proxy measure for quality, under the assumption that inadequate treatment would necessitate readmission in a short period (Callahan et al., 1994). No significant differences in quality were found, because readmission rates within 30, 60, and 90 days of discharge were similar under both systems (the data were combined for mental health and drug abuse patients). However, this period of time may not have been sufficient to capture the extent of readmission, because a significant number of relapses occur between three and six months after treatment completion (Woody and Cacciola, 1994). Renz and coworkers (1995) also defined quality in terms of recidivism rates, finding no differences between managed and unmanaged patients.
A study by independent researchers in 1990 found the content of managed care practices to vary considerably (Garnick et al., 1994b). This telephone survey of 31 managed behavioral health care firms found a broad range of professionals to be responsible for case management. Researchers were not able to identify the percentage of cases to which a case manager with specialized qualifications in drug abuse or mental health treatment was assigned. The study found large variations in utilization review programs. In terms of clinical criteria for authorizing admissions, all firms had requirements for timeliness in responding to patient and practitioner requests, but many held their actual criteria confidential. In the time since this survey was done, however, managed behavioral health
care firms have become more forthcoming about the release of their placement criteria (SAMHSA, 1995).
In one of the few studies of patient placements in a mental health setting, Thompson and coworkers (1992) studied the level of care to which 9,055 patients were assigned by one carve-out vendor. This 30-month study found that over time, more and more patients were being referred away from inpatient care without regard to severity, reflecting a policy decision to limit the use of inpatient services. This finding prompted the authors to question the quality of the care provided by the vendor.
Appropriate placement criteria are viewed as an important measure of quality and an important predictor of treatment outcome (SAMHSA, 1995). That is why there is a major emphasis on identifying placement criteria that could be adopted uniformly by all drug abuse treatment providers, including managed care organizations. One set of criteria, prepared by the American Society of Addiction Medicine and used by many managed care organizations, addresses a broad continuum of care. These criteria were developed by a consensus group, and although they are not universally accepted, they are viewed by the drug abuse field as a stepping stone to the creation of a new generation of uniform placement criteria (SAMHSA, 1995). Currently there is a large randomized trial to determine their predictive validity (D. Gastfriend, Massachusetts General Hospital, personal communication, 1995). However, placement criteria alone do not ensure quality placements. The experience, judgment, and credentials of those who make placement decisions, as well as the fiscal incentives under which they operate, are likely to play important roles. These factors have not been investigated thus far.
Accrediting organizations and the managed behavioral health care industry itself are becoming more active in quality assurance. Initiatives are under way by the National Committee on Quality Assurance and by the Joint Commission on Accreditation of Health Care Organizations. Through its member association, the American Managed Behavioral Healthcare Association, the industry has announced plans to release its first standardized "report card" on access, consumer satisfaction, and preliminary indicators of quality. Member companies have agreed to collect data on up to 30 distinct measures, thus enabling comparisons to be made about their performance.
Medical Cost Offsets
Medical cost offsets are defined as reductions in other areas of medical care utilization as a result of treatment in a given area. The opportunities for cost offsets with drug abuse treatment are potentially vast because of the array of medical conditions associated with untreated dependence,
including AIDS, tuberculosis, and fetal effects (see Chapter 7). At least 60 medical conditions can be caused, in whole or in part, by alcohol, tobacco, and illicit drugs (Fox et al., 1995).
Research reveals that treatment for psychiatric disorders and alcoholism significantly lowers medical care utilization for patients covered by both HMOs and traditional FFS arrangements (Jones and Vischi, 1979; Holder and Blose, 1992; Hoffman et al., 1993). Families of treated alcoholics also experience lower medical care utilization (Holder and Hallan, 1986; Spear and Mason, 1991). Drug abuse treatment is associated with lower subsequent medical costs, but there are fewer studies and they often do not separate the impact of alcohol versus illicit drug dependence and treatment. Yu and coworkers (1991) found reductions in medical costs for one group of privately insured patients treated for illicit drug and/or alcohol problems. A large study of publicly funded drug abuse treatment programs in California found reductions in health care costs of 23.5 percent following treatment (Gerstein et al., 1994). This study also found large offsets in criminal justice system costs due to reductions in illegal behavior.
With the advent of managed care, there is greater potential for realizing cost offsets. The reason for this possibility is managed care's emphasis on accountability and the appropriateness of treatment (i.e., tailoring treatments to each individual client's needs [Mechanic et al., 1995]). Capturing cost offsets is more likely for carve-in policies, in which the provider covers drug abuse, mental health, and medical treatment. The provider stands to realize significant reductions in overall medical care utilization by treated patients and their families. Carve-out vendors do not realize these savings themselves and, thus, may have financial incentives to shift health care costs to other health care providers, a topic discussed in more detail in the next section.
Cost-Shifting
Cost-shifting occurs when the costs of care are transferred from the treatment provider to other health care providers, families, schools, public health and welfare agencies, or the criminal justice system. If, for example, a patient is denied coverage for treatment or is covered insufficiently, the patient or family may have to pay for treatment costs. If the patient and the family are unable to pay for treatment and no financial assistance is offered, the dependence can go untreated. Untreated drug abuse places a great burden on society in terms of lost productivity and additional criminal activity, as well as health care costs (IOM, 1995). Involuntary discharge of opioid-dependent clients from methadone programs, which were publicly financed and unmanaged, resulted in higher
rates of readdiction and higher arrests and incarceration rates, according to several studies (Prendergast et al., in press).
It is simply not known whether some types of managed care contribute to, reduce, or have no effect on cost-shifting. Carve-out firms may have incentives for cost-shifting because they do not bear the consequences (Mechanic et al., 1995). The extent of cost-shifting is difficult to identify and track because the costs can appear in many different areas. One of the many problems is that untreated drug dependence can lead to loss of jobs and loss of private health benefits, at which point the paper trail ceases.
BARRIERS TO RESEARCH
Problems abound in conducting research on the impact of managed care on drug abuse treatment. The problems fall under two general areas: (1) access to and utility of data and (2) variations in coverage. These problems are so intractable, and research funding is so competitive, that academic researchers face hurdles in securing research grants from NIDA, NIAAA, and SAMHSA, all of which are under fiscal constraints. Consequently, little research has been undertaken, as demonstrated throughout this chapter.
In terms of data access, one problem is the proprietary nature of data collected by managed care organizations treating privately insured patients. It is for this reason that most of the studies cited in this chapter are from Medicaid or other publicly subsidized programs. Managed care organizations offering private coverage are reluctant to grant researchers access to their data, given the highly competitive market in which they operate and their concerns about protecting patient confidentiality. The records of public providers can also be difficult to access at times because of the fragmentation in sources of payment. For example, records for a facility's Medicaid patients are kept separate from those for patients funded by local, state, and federal block grants. Loss of coverage from one source of payment means that patients must be switched to different payment systems that often carry different eligibility and benefit structures. It becomes very difficult to follow public patients during a treatment episode or through repeated episodes. The fragmentation of payment systems and the desultory impact on treatment propelled the State of Minnesota to create a special consolidated fund that was described earlier in this chapter.
Even if researchers gain access to patient data, problems do not cease. Administrative data sets containing claims and utilization information are often separate from medical records. The records may be incomplete, sometimes lacking important information-such as whether a drug abuse
diagnosis refers to alcohol, other drugs, or both. Records often lack information about whether the patient has a co-occurring psychiatric disorder. Since people with co-occurring psychiatric disorders and drug abuse account for a sizable proportion of the mental health and drug abuse populations in treatment—and for much higher than average utilization and charges—their inclusion in a sample of drug abusers might skew findings (Garnick et al., in press). Some of the additional problems faced by researchers are the failure to capture and detail utilization; missing information about deductibles and prescription drug claim data (usually handled by a separate data system); sparse demographic data; and lack of information about benefits (Garnick et al., 1994a).
Variations in benefit plans pose other problems. Coverage may change over time under the same plan, leading to different patterns of utilization. There are variations in benefits and in placement criteria across different plans, thus making it difficult to aggregate patients from different plans, even in the same treatment facility. This compromises the ability to carry out large-scale studies.
There is some cause for optimism, however, as managed behavioral health care organizations become more receptive to uniform patient placement criteria (SAMHSA, 1995). Uniformity will enable greater ease in comparing disparate patient populations. Employers and policymakers are requiring more attention to tracking of patient outcomes in contracts with managed care organizations. Additionally, managed behavioral health care organizations are expanding their use of information technology, a trend that is expected to improve large-scale data collection and electronic interchange (Freeman and Trabin, 1994). The industry's member association has embarked on the design of a common data set. Finally, as the public sector moves toward greater reliance on private managed behavioral health care organizations to administer treatment for publicly subsidized patients, there are likely to be heightened requirements for data collection, analysis, and dissemination. These changes may provide a more favorable environment in which to conduct research.
One innovative strategy for research is greater reliance on modeling, by using strategies analogous to those used to predict prevalence or health costs of other diseases such as AIDS. Modeling would obviate the need for access to all medical records. Modeling might be particularly useful in comparing the costs of patient care in different types of managed care. For example, patient assessment could be used to yield diagnoses and needs for care. The costs for treatment of drug abuse and associated psychiatric and medical problems could then be estimated under different scenarios, such as carve-in versus carve-out care.
Managed care organizations may also become interested in forming partnerships with the public sector in data collection and analysis. Both
public and private agencies appear to be eager to use the fruits of research in more rational program design and to promote managed care as a means of improving access, preserving quality, and lowering costs. Once these improved data sets are in place, researchers will for the first time be in a position to confirm or refute the allegations of cost-shifting, denial of treatment, and undertreatment under managed drug abuse care.
In light of the formidable barriers to the conduct of research, the committee recommends that the appropriate federal agencies (e.g., SAMHSA, NIDA, NIAAA) and private organizations work together to develop innovative research strategies and funding mechanisms to ensure that research proceeds on the impact of drug abuse treatment in the managed care setting. Innovative funding mechanisms may include contracts, memoranda of understanding, and publicprivate partnerships.
CONCLUSION
The only definitive conclusion to be reached on the pivotal claims of managed health care—that it enhances access, lowers cost, and ensures quality—is that there are insufficient data. The modest body of research does point to lower costs and less reliance on inpatient care. However, treatment outcomes are still unknown due to the current lack of research on the effectiveness and cost-effectiveness of managed care treatment. Additionally, there is no research on what could potentially be inadequacies in managed drug abuse care: denial of treatment; undertreatment; and cost shifting to other providers, public health and welfare agencies, and the criminal justice system. The committee urges appropriate federal and private agencies to undertake the studies recommended throughout this chapter.
REFERENCES
Alterman Al, O'Brien CP, McLellan AT, August DS, Snider EC, Droba M, Cornish JW, Hall CP, Raphaelson AH, Schrade FX. 1994. Effectiveness and costs of inpatient versus day hospital cocaine rehabilitation. Journal of Nervous and Mental Disease 182(3):157-163.
Alterman Al, Snider EC, Cacciola JS, May DJ, Parikh G, Maany I, Rosenbaum PR. 1996. A quasi experimental comparison of the effectivenes of 6- versus 12-hour per week outpatient treatments for cocaine dependence. Journal of Nervous and Mental Disease 184(1 ):54-56.
Asher M, Friedman N, Lysionek C, Peters C. 1995. Evaluation of the Implementation of Pennsylvania's Act 152. 1988. The Quantitative Findings. Villanova, PA: Human Organization Science Institute, Villanova University.
Batten H, Prottas J, Horgan CM, Simon LJ, Larson MJ, Elliott EA, Marsden ME. 1992. Drug Services Research Survey Final Report: Phase II. Contract number 271-90-8319/1. Submitted to the National Institute of Drug Abuse, February 12, 1992. Waltham, MA: Bigel Institute for Health Policy, Brandeis University.
Beinecke RH, Goodman M, Rivera M. 1995. An Assessment of the Massachusetts Managed Mental Health/Substance Abuse Program: Year Three. Boston: Suffolk University, Department of Public Management.
BLS (Bureau of Labor Statistics). 1992. Substance Abuse Provisions in Employee Benefit Plans. Bulletin 2412. Washington, DC: Department of Labor, Bureau of Labor Statistics.
BLS (Bureau of Labor Statistics). 1994. Employee Benefits in Small Private Establishments, 1992. Bulletin 2441, Tables 50-52. Washington, DC: Department of Labor, Bureau of Labor Statistics.
Callahan JJ, Shepard DS, Beinecke RH, Larson M, Cavanaugh D. 1994. Evaluation of the Massachusetts Medicaid Mental Health/Substance Abuse Program . Submitted to the Massachusetts Division of Medical Assistance, Mental Health Substance Abuse Program. Waltham, MA: Institute for Health Policy, Brandeis University.
Center of Alcohol Studies, Rutgers University. 1993. Socioeconomic Evaluations of Addictions Treatment. Prepared for the President's Commission on Model State Drug Laws. Piscataway, NJ: Rutgers University.
Chaulk CP, Moore-Rice K, Rizzo R, Chaisson RE. 1995. Eleven years of community-based directly observed therapy for tuberculosis. Journal of the American Medical Association 275:945-951.
CRS (Congressional Research Service). 1993. Medicaid: An Overview. 93-144 EPW. Washington, DC: Library of Congress, CRS.
CRS (Congressional Research Service). 1994. Health Insurance. Report No. IB91093. Washington, DC: Library of Congress, CRS.
Ellis RP. 1992. Drug Abuse Treatment Patterns Before and After Managed Care. Prepared under contract #271-89-8516 for the Third Annual Advisory Committee Meeting. Washington, DC, April 27-29, 1992. Boston, MA: Boston University.
Foster Higgins, Inc. 1994. Managed Behavioral Healthcare Quality and Access Survey Report. Prepared for the American Managed Behavioral Healthcare Association. Washington, DC: AMBHA.
Fox K, Merril JC, Chang HH, Califano JA Jr. 1995. Estimating the costs of substance abuse to the Medicaid hospital care program. American Journal of Public Health 85(1):48-54.
Freeman MA, Trabin T. 1994. Managed Behavioral Healthcare: History, Models, Key Issues, and Future Course. Prepared for the Center for Mental Health Services, SAMHSA.
Garnick DW, Hendricks AM, Comstock CB. 1994a. Measuring quality of care: Fundamental information from administrative datasets. International Journal for Quality in Health Care 6(2):163-177.
Garnick DW, Hendricks AM, Dulski JD, Thorpe KE, Horgan C. 1994b. Characteristics of private-sector managed care for mental health and substance abuse treatment. Hospital and Community Psychiatry 45(12):1201-1205.
Garnick DW, Hendricks AM, Drainoni ML, Horgan CM, Comstock C. In press. Private sector coverage of people with dual diagnoses. Journal of Mental Health Administration.
Geraty R, Bartlett J, Hill E, Lee F, Shusterman A, Waxman A. 1994. The impact of managed behavioral healthcare on the costs of psychiatric and chemical dependency treatment . Behavioral Healthcare Tomorrow March/April:18-30.
Gerstein DR, Johnson RA, Harwood HJ, Fountain D, Suter N, Malloy K. 1994. Evaluating Recovery Services: The California Drug and Alcohol Treatment Assessment (CALDATA). Sacramento, CA: California Department of Alcohol and Drug Programs.
Hoffmann NG, DeHart SS, Fulkerson JA. 1993. Medical care utilization as a function of recovery status following chemical addictions treatment. Journal of Addictive Diseases 12:97-108.
Holder HD, Blose JO. 1992. The reduction of health care costs associated with alcoholism treatment: A 14-year longitudinal study. Journal of Studies on Alcohol 53(4):293-302.
Holder HD, Hallan JD. 1986. Impact of alcoholism treatment on total health care costs: A six-year study. Advances in Alcohol and Substance Abuse 6(1):1-15.
IOM (Institute of Medicine). 1989. Controlling Costs and Changing Patient Care? The Role of Utilization Management. Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1990. Treating Drug Problems. Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1995. Development of Medications for the Treatment of Opiate and Cocaine Addictions: Issues for the Government and Private Sector. Washington, DC: National Academy Press.
Jones KR, Vischi T. 1979. Impact of alcohol, drug abuse and mental health treatment on medical care utilization: A review of the research literature. Medical Care 17(12):1-82.
Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. 1996. The epidemiology of co-occurring addictive and mental disorders in the National Comorbidity Survey: Implications for prevention and service utilization. American Journal of Orthopsychiatry 66(1):17-31.
Kushner JN. 1995. Managing State Managed Care Contracts. Treatment Improvement Exchange Communique. Rockville, MD: Center for Substance Abuse Treatment, SAMHSA.
Mechanic D, Schlesinger M, McAlpine DD. 1995. Management of mental health and substance abuse services: State of the art and early results. Milbank Quarterly 73(1):19-55.
Miller RH, Luft HS. 1994. Managed care plan performance since 1980. Journal of the American Medical Association 271(19):1512-1519.
Minnesota Department of Human Services. 1993. 1993 Status Report on the Minnesota Consolidated Chemical Dependency Treatment Fund, Report to the Minnesota Legislature from the Chemical Dependency Program Division. St. Paul, MN: Minnesota Department of Human Services.
Minnesota Department of Human Services. 1995. Research News. St. Paul, MN: Minnesota Department of Human Services, Chemical Dependency Division.
Mucnick-Baku S, Traw KL. 1992. Employee Assistance Programs: An Evolving Human Resource Management Strategy. Washington, DC: Washington Business Group on Health.
NRC (National Research Council). 1994. Under the lnfluence? Drugs and the American Work Force. Washington, DC: National Academy Press.
Osher FG. 1996. A vision for the future: Toward a service system responsive to those with co-occurring addictive and mental disorders. American Journal of Orthopsychiatry 66(1):71-76.
Oss ME. 1994. Managed behavioral health programs widespread among insured Americans. Open Minds Newsletter 8(3). Gettysburg, PA: Behavioral Health Industry News, Inc.
Prendergast ML, Anglin MD, Maugh TH, Hser Y. In press. The Effectiveness of Treatment for Drug Abuse. Draft manuscript prepared April 7, 1994 for NIDA Treatment Services Research Branch. Los Angeles: UCLA Drug Abuse Research Center.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. 1990. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association 264(19):2511-2518.
Renz EA, Chung R, Fillman TO, Mee-Lee D, Sayama M. 1995. The effect of managed care on the treatment outcome of substance use disorders. General Hospital Psychiatry 17:287-292.
Rogers WH, Wells KB, Meredith LS, Sturm R, Burnam A. 1993. Outcomes for adult outpatients with depression under prepaid or fee-for-service financing. Archives of General Psychiatry 50:517-525.
Rost KM, Ross RL, Humphrey J, Frank S, Smith J, Smith GR. 1996. Does this treatment work? Validation of an outcomes module for alcohol dependence. Medical Care 34(4):283-294.
Rowland D, Rosenbaum S, Simon L, Chait E. 1995. Medicaid and Managed Care: Lessons from the Literature. Report of the Kaiser Commission on the Future of Medicaid. Menlo Park, CA: Kaiser Foundation.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1995. The Role and Current Status of Patient Placement Criteria in the Treatment of Substance Use Disorders. Treatment Improvement Protocol Series. Rockville, MD: Center for Substance Abuse Treatment.
Shueman SA, Troy WG. 1994. Managed Behavioral Health Care: An Industry Perspective. Springfield, IL: Charles C Thomas.
Spear SF, Mason M. 1991. Impact of chemical dependency on family health status. International Journal of the Addictions 26(2):79-87.
Thompson JW, Burns BJ, Goldman HH, Smith J. 1992. Initial level of care and clinical status in a managed mental health program. Hospital and Community Psychiatry 43(6):599-603.
Woody G, Cacciola J. 1994. Review of remission criteria. In: Widiger T, Frances A, Pincus H, First M, Ross R, Davis W, eds. DSM-IV Sourcebook, Vol. 1. Washington, DC: American Psychiatric Association Press. Pp. 81-92.
Yu J, Chen PJ, Harshman EJ. 1991. An analysis of substance abuse patterns, medical expenses and effectiveness of treatment in the workplace. Employer Benefits Journal September:26-30.




























