1
Introduction
In communities, health is a product of many factors, and many segments of the community have the potential to contribute to and share responsibility for its protection and improvement. Changes in public policy, in public- and private-sector roles in health and health care, and in public expectations are presenting opportunities and challenges for communities addressing both the overall health status of the population and more specific health issues. Performance monitoring can be used as a tool to assess activities in many sectors and to promote collaboration and accountability in working toward better health for the whole community, especially within the framework of a community-based health improvement process.
This report from the Institute of Medicine (IOM) Committee on Using Performance Monitoring to Improve Community Health outlines the elements of an ongoing and evolving health improvement process, discusses the role that performance monitoring can play, and offers tools to help communities develop and use performance indicators. In its proposals and recommendations, the committee is responding to the need it sees to introduce a conceptual framework for using performance monitoring concepts to improve community health as a whole–as opposed to monitoring performance within specific community entities. This report also addresses the need to look beyond community health assessment to ways to establish accountability for health improvement.
Drawing on lessons from a variety of current activities, the committee brings to community health improvement an approach that focuses on integrating the roles of clinical personal health services, public health, and a broad array of other elements in the community, and on developing monitoring systems that can function in this integrated context. The committee is not attempting to prescribe what communities should do to address their health concerns or who should be responsible for what, but it is encouraging communities to adopt a systematic approach to health improvement that makes use of performance monitoring tools to help them achieve their goals.
A BROADER UNDERSTANDING OF HEALTH
Contributing to the interest in health improvement and performance monitoring is a wider recognition that health embraces well-being as well as the absence of illness. For both individuals and populations, health depends not only on health care but also on other factors including individual behavior, genetic makeup, exposure to health threats, and social and economic conditions. The health field model , as described by Evans and Stoddart (1994) and discussed further in Chapter 2, presents these multiple determinants of health in a dynamic relationship. The model's feedback loops link social environment, physical environment, genetic endowment, an individual's behavioral and biologic responses, disease, health care, health and function, well-being, and prosperity. The committee found this model to be an effective basis for its work.
Health in the community can be seen as the product of the changing mix and interactions of these factors over time. The multidimensional perspective reinforces the value of public health's traditional emphasis on a population-based approach to community health issues. It also provides a basis for looking to many segments of the community to address factors affecting health and well-being, making it appropriate to bring a wide array of parties to the table as interested stakeholders and accountable partners.
A COMMUNITY PERSPECTIVE
The committee adopted as a starting point for its discussions of ''community" a definition offered by Labonte (1988): individuals with shared affinity, and perhaps a shared geography, who orga-
nize around an issue, with collective discussion, decision making, and action. Geography emerged as a critical point of reference in the committee's discussions. Although geographic (or civic) boundaries cannot adequately capture all of the potentially meaningful communities to which individuals might belong, they are a practical basis for analysis within the limitations of current data systems. Depending on the health issue, the relevant geographic unit (e.g., county, city, census tract) may vary.
A wide range of individuals, organizations, and agencies, many of whose roles are not within the traditional domain of health care or public health, have an effect on and a stake in a community's health (Patrick and Wickizer, 1995). These entities can include individual health care providers, public health agencies, health care organizations, purchasers of health services, and community organizations explicitly concerned with health. They can also include other government agencies (e.g., housing, human services, public safety), schools, business and industry, faith communities, and other community groups that may not usually be seen as having any explicit health-related role. Entities such as state health departments, federal agencies, managed care organizations, and national corporations have a broader scope than a single community but often have an important role at the local level.
As communities respond to the multiple factors involved in various health issues, all parties will have to sort out their roles and responsibilities. The specific pattern will vary over time and from community to community, depending on the mix and interaction of factors contributing to health. To optimize the unique contributions of these interdependent sectors, it will be important to address issues of accountability and shared responsibility for various aspects of community health. In most communities, there will be only limited experience with widespread collaborative or coordinated efforts among these diverse groups. A common language and an understanding of the multidimensional nature of the determinants of health will help community stakeholders work together effectively. Finding a way to accommodate diversity in values and goals will be another important task. Participation in the process of community-wide social change will also be needed for performance monitoring to succeed in improving health (Green and Kreuter, 1990).
The committee recognizes that there are limitations in a community-based approach to health improvement. Some of the factors affecting health in a community will originate elsewhere and may not be modifiable by efforts within the community. "Outside"
influences are also a factor because of the geographic mobility of the population of most communities. Current health status in any given community reflects the combined and cumulative effects of factors operating over time in many other communities. These confounding influences must be taken into account in developing and implementing health improvement efforts based on accountable performance.
GROWING INTEREST IN PERFORMANCE MONITORING
Performance monitoring has gained increasing attention as a tool for managing processes and improving their outcomes. It is an important component of the activities characterized as "reinventing government" (Osborne and Gaebler, 1992; Gore, 1993; Hatry et al., 1994), and increasingly, it is being used to evaluate the delivery of personal health care services and to examine population-based activities addressing the health of the public.
As used by the committee, the term "performance monitoring" applies to a continuing and evolving process—anchored in a context of shared responsibility and accountability for health improvement—for (1) selecting and using a limited number of indicators that can track critical processes and outcomes over time and among accountable stakeholders; (2) collecting and analyzing data on those indicators; and (3) making the results available to inform assessments of the effectiveness of an intervention and the contributions of accountable entities.
Although many performance monitoring activities are focused on specific organizations such as health plans or hospitals, there is a growing appreciation of the importance of a dynamic, population-based perspective. Only at the population level is it possible to look at the impact of a broad range of health determinants, among which a specific element such as health care services may play only a limited role. Furthermore, a population-based perspective is necessary to see whether health improvement efforts are meeting the needs of all segments of the community.
Performance Monitoring in Health Care
Developments in private-sector health care, particularly in the area of managed care, are contributing to the interest in and tools available for performance monitoring. Managed care and integrated health systems are expanding rapidly in most parts of the
country, and in some markets there is strong competition. They are serving not only the privately insured but also Medicaid programs and a growing share of the Medicare population. Throughout the country, employers and other major purchasers of health services are demanding, and receiving, information on costs and performance that will help them select among plans. Less widely, consumers are seeking information that can help them make informed choices about their health care and health care providers. Individual health plans, consumer groups, and national organizations have developed a variety of reporting systems, often with summary "report cards."
Various initiatives are under way to develop and promote standardized performance indicators. One of these is the Health Plan Employer Data and Information Set, HEDIS, produced by the National Committee for Quality Assurance (NCQA, 1993, 1996). HEDIS is a defined set of performance measures used by employers and managed care organizations to compare health plans on the basis of quality, access and patient satisfaction, delivery of preventive services, membership and utilization, financing, and descriptive management information. In the newer versions, special consideration has been given to identifying measures appropriate for monitoring services for Medicaid beneficiaries. In another national-level activity, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO, 1996) has promulgated standards, the focus of which in recent years has been in keeping with a broader philosophy of performance monitoring and outcomes. More recently, the Foundation for Accountability (FAcct, 1995) is reviewing and recommending other sets of indicators that employers and consumers can use to assess health plan performance. A more specialized set of performance measures has been developed by the American Managed Behavioral Healthcare Association (AMBHA, 1995), specifically for the mental health and chemical dependency services offered by its members.
In many ways these activities build on work being done in the health care sector on quality assessment and quality improvement and on outcomes research. For example, the definition of quality of care formulated by the IOM (1990) directs attention to the importance of good performance in achieving good health outcomes.1 Quality improvement techniques, which have been
adapted from their industrial origins for use in individual health care settings, rely on repeated measurements of performance and outcomes to identify problems and assess the effectiveness of corrective actions (e.g., see Berwick et al., 1990). Community-wide performance monitoring would extend these principles and techniques beyond individual health care settings. Several cities have been part of a demonstration project to test just such an approach (Nolan and Knapp, 1996).
Performance Monitoring in the Public Sector
In the public sector, two primary themes have emerged: assessing the performance of local health departments and assessing the population's health status. The "core functions" of public health identified in The Future of Public Health (IOM, 1988)—assessment of health needs and resources, policy development, and assurance that needed activities are performed—have become the basis for judging the performance of local health departments. Tools such as PATCH (Planned Approach to Community Health) (Kreuter, 1992; CDC, 1995), APEXPH: Assessment Protocol for Excellence in Public Health (NACHO, 1991), Healthy Communities 2000: Model Standards (APHA et al., 1991), and the Healthy Cities/Healthy Communities model (National Civic League, 1993; Flynn, 1996) are available to help health departments assess their ability to perform those functions. These materials also provide guidance on efforts to assess and respond to community health needs.
Formal measures of effective performance by health departments are being developed and tested (Miller et al., 1994a,b; Studnicki et al., 1994; Turnock et al., 1994a,b, 1995). The initial focus on health departments is now widening to include other elements of the community (Richards et al., 1995). Still needed are research and evaluation to determine the impact that performance of activities related to the core functions of public health, by health departments or other entities, has on health in the community.
Other activities have focused on health status measurement. Healthy People 2000: The National Health Promotion and Disease Prevention Objectives (USDHHS, 1991) outlines 22 categories of measurable health objectives in health status, risk reduction, and services and protection, including both process and outcome measures. Many state and local health departments have adapted the national objectives to their own circumstances. Healthy Commu-
nities 2000: Model Standards (APHA et al., 1991) is designed specifically to assist this process. In addition, agencies and organizations with an interest in a specific health issue or a specific population group have made use of particular subsets of the Healthy People 2000 objectives (e.g., American College Health Association, 1990; MCHB, 1991).
Some federal block grant programs (e.g., in prevention and public health services, maternal and child health, and substance abuse) have reporting requirements for states that include health status and outcomes measures, often drawn from or similar to those in Healthy People 2000. Proposals by the U.S. Department of Health and Human Services for Public Health Performance Partnership Grants would require new reporting measures that are intended to focus on the link between grant-supported activities and health outcomes (USDHHS, no date). In general, however, health status assessments have provided baseline information about community health needs but have not explicitly addressed the performance of specific entities in the community, which raises different measurement and community action issues.
Accountability for Efficient and Effective Action
Performance monitoring is also a response to concerns about ensuring the efficient and effective use of resources, particularly financial resources. Overall, higher levels of health care spending in the United States than in most other countries have not produced higher levels of health, measured in terms such as life expectancy or infant mortality. Both public- and private-sector decision makers see a need to use limited funds in ways that optimize health outcomes. This concern is consistent with a heightened interest in accountability for the use of those funds and the outcomes produced.
There is a need to account for performance and outcomes within individual organizations (e.g., a health department or a health plan), but from the committee's perspective, there must also be a way to monitor performance and outcomes for communities as a whole. Looking at the results of many separate efforts will not provide a comprehensive community picture, and those separate efforts cannot, by themselves, ensure that health improvement achieves its goals.
A FRAMEWORK FOR COMMUNITY HEALTH IMPROVEMENT
The committee has based its work on a vision for community health improvement that relies on shared responsibility across a broad range of community stakeholders, combined with individual accountability to ensure that responsibilities are not ignored or abandoned. This has led to a proposal for a community health improvement process (CHIP), described in more detail in Chapter 4, through which a community can assess health needs in the population and also develop interventions and monitor performance and outcomes.
A Process to Support Health Improvement
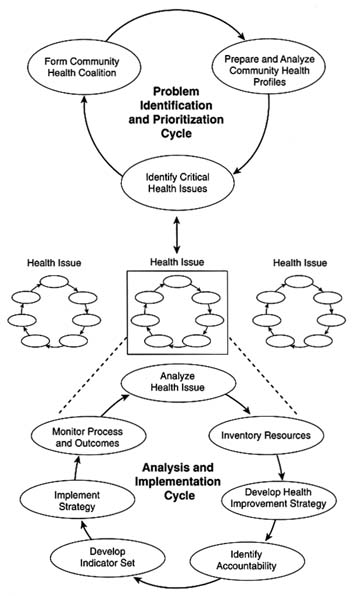
A CHIP would operate through two primary interacting cycles, both of which rely on analysis, action, and measurement (see Figure 1-1). A broad problem identification and prioritization cycle focuses on building a community stakeholder coalition, monitoring community-level health indicators, and identifying specific health issues as community priorities. The second cycle—an analysis and implementation cycle—is a series of processes to devise, implement, and evaluate the impact of health improvement strategies for priority health issues. More than one analysis and implementation cycle may be operating at the same time if a community is responding to multiple health issues. The overall process differs from other health assessment and health-related performance monitoring models primarily because of its emphasis on measurement to link performance and accountability.
As envisioned by the committee, a CHIP can be implemented in a variety of community circumstances, and communities can begin working at various points in either cycle and with varying resources in place. The process must be seen as iterative and evolving rather than linear or short term. One-time activities, briefly assembled coalitions, and isolated solutions will not be adequate. The process must also be able to accommodate the dynamic nature of communities and the interdependence of community activities. Both community-level monitoring data and more detailed information related to specific health issues must feed back into the system on a continuing basis to guide subsequent analysis and planning. This information loop is also the means by which a CHIP links performance to accountable entities among the community stakeholders.
Selecting and Using Indicators
The CHIP cycles make use of two kinds of indicators. The problem identification and prioritization cycle calls for development of a community health profile that can provide basic information about a community's demographic and socioeconomic characteristics and its health status and health risks. This profile would provide background information that can help a community interpret other health data. Comparing these data over time or with data from other communities may help identify health issues that should receive more focused attention. The committee's proposal for a community profile appears in Chapter 5.
The analysis and implementation cycle operationalizes accountability for health improvement through sets of concrete, specific, and quantitative performance indicators linked to "accountable entities" in the community that can contribute to health improvement. A key element is linking "performance" to health outcomes. This requires both an understanding of the factors that function as determinants of a particular outcome and of scientific evidence to support the expectation that specific actions will have the desired health impact. Scientifically sound (i.e., reliable and valid) measures of performance and outcomes must also be possible. In the context of the committee's broad definition of health, appropriate indicators can be diverse.
Selecting indicators requires careful consideration of how to gain insight into progress achieved in the health improvement process. A set of indicators should balance population-based measures of risk factors and health outcomes and health systems-based measures of services performed and should also include measures for the various accountable entities in the community, including those whose primary mission is not health specific. A balance is needed among indicators that reflect short-term gains and those that measure more fundamental changes in community health. In selecting health issues and performance indicators, communities must make strategic choices that are consistent with their specific aims and circumstances. In Chapter 5, the committee reviews criteria to guide the selection of indicators, and Appendix A illustrates the application of the committee's proposals with prototype sets of community-level performance indicators for several specific health issues.
Data and Measurement Concerns
The committee found that existing indicators and data collection tools (e.g., HEDIS or state and national health surveys) are often not available for use at the community level and that available information systems are not adequate for identifying or analyzing problems, making choices for action among alternative problems and interventions, or tracking the effectiveness of interventions. Even when tools for health indicator development and implementation exist, communities may not have the necessary resources and circumstances for creating an operational health improvement process.
As envisioned by the committee, a community-based performance monitoring program will require an enhanced information infrastructure that can support monitoring diverse phenomena in the many sectors that contribute to the health of populations, including clinical care, environmental services, individual and public education, community social services, and public policy that promotes behavioral change. In some settings, it may be possible to build on information systems developed to support functions such as the delivery of health or human services or to establish links among existing data systems.
Also needed will be the capability to provide information on the health status of a community, including threats to its future health; to inform decisions about how to improve the health of the public; and to document change in community health and in performance of health-related functions. The value of the information technologies will depend on the ability of some segment of the community to analyze and understand the data produced and make them accessible to diverse community audiences.
ISSUES FOR CONSIDERATION
It is in this context that the IOM Committee on Using Performance Monitoring to Improve Community Health was charged with examining the use of performance monitoring to protect and improve the health of communities and with developing prototypical sets of performance indicators for specific health concerns. As discussions progressed during the course of the study, performance monitoring emerged as a critical tool in a broader health improvement process. Thus, the committee aims to explicate its vision for a community health improvement process that applies the techniques of performance monitoring and to demonstrate the
value of the process to a diverse set of community stakeholders with an interest in and influence on health. Emphasized in this is the importance of improving our understanding of the factors that contribute to health in communities, particularly within the field model framework (Evans and Stoddart, 1994). Current limitations in that understanding often make it difficult to establish whether changes in performance will lead to improvements in health in the community, as measured through assessments of individuals.
The implications of the current social, scientific, and policy climate for community health improvement efforts and the further development of health-related performance monitoring are also a consideration. For example, some question whether meaningful responsibility and accountability for community health can be established across a range of largely autonomous entities, none of which controls all of the elements that may be critical to success (Nerenz, 1996). A different concern is that the diversity of performance monitoring developments will not achieve sufficient coordination to provide the kind of comprehensive approach that the committee believes is needed. Because performance monitoring will generally require some degree of change in the way institutions or communities make decisions and take actions, the committee also explored the processes that lead to such changes.
The committee addressed some of the challenges that must be met if performance monitoring is to progress. Despite the recognition of its value, the implementation of performance monitoring may be hindered by lack of community capacity to mount such an effort or to overcome the measurement demands it can create (see Chapter 4). There may also be concerns that rigorous monitoring could reveal poor or ineffective performance or that newer, more diverse approaches to health improvement will alter traditional patterns of responsibility and control for some sectors of the community.
The committee faced the challenged of identifying and presenting essential elements of a health improvement process and performance monitoring activities while avoiding a prescription for specific actions. It has, however, developed tools that communities can apply or adapt to their needs. In particular, the committee focused on the process of indicator selection and the development of prototypical indicator sets to use in an ongoing effort to evaluate performance and health outcomes related to specific health issues. It also presents a proposal for a set of indicators that could form the core of a community profile.
Every community will have to look at health questions from its own perspective and scrutinize its priorities and opportunities to respond. Those priorities and opportunities will vary depending on a community's particular health and social environment. Practical matters of budget and timing will also influence the way in which communities choose health priorities and performance indicators. The committee presents specific recommendations intended to address essential elements of what needs to be done to support effective performance monitoring and its integration into a community health improvement process. It has, however, avoided recommendations on how communities should go about these tasks.
The committee seeks to reach a wide audience with this report: public health agencies at the local, state, and federal levels; health care providers and organizations in the public and private sectors; employers; important public-sector purchasers of health care services for their employees and for programs such as Medicare and Medicaid; agencies and organizations with responsibilities in areas such as child health, elder health, mental health, and substance abuse; agencies with diverse community responsibilities including social services, education, and criminal justice; and a wide variety of community organizations. Others for whom the committee expects the report to have value are accrediting organizations, educators, and those who set research agendas, including foundations and other funding organizations.
UNDERLYING ASSUMPTIONS
The committee's examination of the issues related to community health improvement and performance monitoring reflects underlying assumptions on several issues.
-
Effective use of limited resources: Limited resources, long a factor in much of the public sector and increasingly a concern in the private sector, make it necessary to improve the efficiency and effectiveness with which those resources are used. That is, resources must be used for appropriate purposes and in ways that efficiently promote desired results. The health improvement process outlined by the committee will provide a broad perspective from which to guide and assess resource use in a community. This process and its performance monitoring elements can contribute to efficiency and effectiveness by providing information on what is being done in the community, what sectors of the commu-
-
nity are taking action, and what the impact is on community health status.
-
A conceptual model of the determinants of health: The committee believes that the health improvement process and its performance monitoring component will be more effective if they are based on a conceptual model that can frame the interacting factors contributing to a community's health and can direct attention to the broad array of actions that could be expected to improve health.
-
Shared responsibility among diverse stakeholders: Fundamental to the committee's work is the recognition that a wide range of individuals and organizations will have to recognize and accept that they have a shared and interdependent role in community health. Action in many sectors of society, not merely improvements within public health or health care delivery systems, will be necessary, and no one group will be able to successfully address community-wide health issues alone. Broad inclusiveness across stakeholders should be a starting point in a community's approach to the health improvement process, but it may have to be balanced by expectations for more selective involvement with specific health issues.
Although acceptance of shared responsibility is an essential element of the committee's framework, many communities may find it challenging to establish a sufficiently collaborative environment. There must also be a willingness to act. Motivation for action may come from sources such as good will, self-interest, regulation, or a combination of these.
-
Trust and equity: By documenting actions and outcomes, performance monitoring can support increased public trust that ''the system" is working. It can also, as part of a broader health improvement process, guide community actions toward minimizing major discrepancies in health status among subpopulations to promote greater equity in health throughout the community.
THE COMMITTEE'S REPORT
This report presents the committee's assessment of conceptual and operational considerations in community-based health improvement efforts and the contribution that performance monitoring can make. Chapter 2 examines the determinants of health from the broad perspective offered by the field model. This broad perspective is an essential element of the committee's approach to health improvement and performance monitoring. Chapter 3 ex-
amines issues in managing social change, the role of coalitions, and challenges in achieving consensus on accountability and responsibility.
In Chapter 4, the committee outlines its framework for a community health improvement process to help communities monitor overall health status, establish priorities, and assess progress in issue-specific efforts; the chapter also examines capacities needed to support this process. Chapter 5 presents the committee's proposal for a community health profile and discusses issues in selecting performance indicators to be used in addressing specific health issues. Presented in Appendix A are prototype sets of issue-specific indicators developed by the committee to illustrate how communities might apply the concepts outlined in this report.
Chapter 6 concludes the report with the committee's recommendations for steps to be taken by various parties to move toward the health improvement and performance monitoring processes envisioned by the committee.
REFERENCES
AMBHA (American Managed Behavioral Healthcare Association). 1995. Performance Measures for Managed Behavioral Healthcare Programs. Washington, D.C.: AMBHA Quality Improvement and Clinical Services Committee.
American College Health Association. 1990. Healthy Campus 2000: Making It Happen. Baltimore: American College Health Association.
ALPHA (American Public Health Association), Association of Schools of Public Health, Association of State and Territorial Health Officials, National Association of County Health Officials, United States Conference of Local Health Officers, Department of Health and Human Services, Public Health Service, Centers for Disease Control. 1991. Healthy Communities 2000: Model Standards. 3rd ed. Washington, D.C.: APHA.
Berwick, D.M., Godfrey, A.B., and Roessner, J. 1990. Curing Health Care: New Strategies for Quality Improvement. San Francisco: Jossey-Bass.
CDC. 1995. Planned Approach to Community Health: Guide for the Local Coordinator. Atlanta, Ga.: CDC, National Center for Chronic Disease Prevention and Health Promotion.
Evans, R.G., and Stoddart, G.L. 1994. Producing Health, Consuming Health Care. In Why Are Some People Healthy and Others Not? The Determinants of Health of Populations. R.G. Evans, M.L. Barer, and T.R. Marmor, eds. New York: Aldine De Gruyter.
Flynn, B.C. 1996. Healthy Cities: Toward Worldwide Health Promotion. Annual Review of Public Health 17:299–309.
FAcct (Foundation for Accountability). 1995. Guidebook for Performance Measurement: Prototype. Portland, Ore.: FAcct. September 22.
Gore, A. 1993. From Red Tape to Results: Creating a Government That Works Better and Costs Less. Report of the National Performance Review. Washington, D.C.: U.S. Government Printing Office.
Green, L.W., and Kreuter, M.W. 1990. Health Promotion as a Public Health Strategy for the 1990s. Annual Review of Public Health 11:319–334.
Hatry, H., Wholey, J.S., Anderson, W.F., et al. 1994. Toward Useful Performance Measurement: Lessons Learned from Initial Pilot Performance Plans Prepared Under the Government Performance and Results Act. Washington, D.C.: National Academy of Public Administration.
IOM (Institute of Medicine). 1988. The Future of Public Health. Washington, D.C.: National Academy Press.
IOM. 1990. Medicare: A Strategy for Quality Assurance. Vol. I. K.N. Lohr, ed. Washington, D.C.: National Academy Press.
JCAHO (Joint Commission on Accreditation of Healthcare Organizations). 1996. Joint Commission Standards [WWW document]. URL http://www.jcaho.org/stds.html
Kreuter, M.W. 1992. PATCH: Its Origin, Basic Concepts, and Links to Contemporary Public Health Policy. Journal of Health Education 23:135–139.
Labonte, R. 1988. Health Promotion: From Concepts to Strategies. Health Care Management Forum 1(3):24–30.
MCHB (Maternal and Child Health Bureau). 1991. Healthy Children 2000: National Health Promotion and Disease Prevention Objectives Related to Mothers, Infants, Children, Adolescents, and Youth. Pub. No. HRSA-M-CH 91-2. Rockville, Md.: U.S. Department of Health and Human Services, Health Resources and Services Administration.
Miller, C.A., Moore, K.S., Richards, T.B., and McKaig, C. 1994a. A Screening Survey to Assess Local Public Health Performance. Public Health Reports 109:659–664.
Miller, C.A., Moore, K.S., Richards, T.B., and Monk, J.D. 1994b. A Proposed Method for Assessing the Performance of Local Public Health Functions and Practices. American Journal of Public Health 84:1743–1749.
NACHO (National Association of County Health Officials). 1991. APEXPH: Assessment Protocol for Excellence in Public Health. Washington, D.C.: NACHO.
National Civic League. 1993. The Healthy Communities Handbook. Denver: National Civic League.
NCQA (National Committee for Quality Assurance). 1993. Health Plan Employer Data and Information Set and User's Manual, Version 2.0 (HEDIS 2.0). Washington, D.C.: NCQA.
NCQA. 1996. HEDIS 3.0 Draft for Public Comment. Washington, D.C.: NCQA. July 15.
Nerenz, D.R. 1996. Who Has Responsibility for a Population's Health? Milbank Quarterly 74:43–49.
Nolan, T.W., and Knapp, M. 1996. Community-wide Health Improvement: Lessons from the IHI-GOAL/QPC Learning Cooperative. The Quality Letter for Healthcare Leaders 8(1):13–20.
Osborne, D., and Gaebler, T. 1992. Reinventing Government: How the Entrepreneurial Spirit Is Transforming the Public Sector. Reading, Mass.: Addison-Wesley.
Patrick, D.L., and Wickizer, T.M. 1995. Community and Health. In Society and Health. B.C. Amick, S. Levine, A.R. Tarlov, and D.C. Walsh, eds. New York: Oxford University Press.
Richards, T.B., Rogers, J.J., Christenson, G.M., Miller, C.A., Taylor, M.S., and Cooper, A.D. 1995. Evaluating Local Public Health Performance at a Community Level on a Statewide Basis. Journal of Public Health Management and Practice 1(4):70–83.
Studnicki, J., Steverson, B., Blais, H.N., Goley, E., Richards, T.B., and Thornton, J.N. 1994. Analyzing Organizational Practices in Local Health Departments. Public Health Reports 109:485–490.
Turnock, B.J., Handler, A., Dyal, W.W., et al. 1994a. Implementing and Assessing Organizational Practices in Local Health Departments. Public Health Reports 109:478–484.
Turnock, B.J., Handler, A., Hall, W., Potsic, S., Nalluri, R., and Vaughn, E.H. 1994b. Local Health Department Effectiveness in Addressing the Core Functions of Public Health. Public Health Reports 109:653–658.
Turnock, B.J., Handler, A., Hall, W., Lenihan, D.P., and Vaughn, E. 1995. Capacity Building Influences on Illinois Local Health Departments. Journal of Public Health Management and Practice 1(3):50–58.
USDHHS (U.S. Department of Health and Human Services). 1991. Healthy People 2000: National Health Promotion and Disease Prevention Objectives . DHHS Pub. No. (PHS) 91-50212. Washington, D.C.: Office of the Assistant Secretary for Health.
USDHHS. No date. Performance Measurement in Selected Public Health Programs: 1995–1996 Regional Meetings. Washington, D.C.: Office of the Assistant Secretary for Health.