1
Overview
The Medicare Program
Medicare is the single largest payer in the U.S. health care system, purchasing about 19 percent of all personal health care services. The program pays for 30 percent of U.S. expenditures for hospital services, 21 percent of expenditures for physician services, and 40 percent of expenditures for home health care services (Congressional Budget Office, 1995c). In 1995 the Medicare program paid $178 billion, 11 percent of the total federal budget, to cover 37 million individuals. Medicare is the nation's largest single business-type operation and is larger than General Motors, the largest private company in the United States (Fortune, 1995).
Medicare provides coverage to 33 million elderly individuals (those over age 65), 4 million disabled individuals, and about 210,000 people with end-stage renal disease (Prospective Payment Assessment Commission, 1995). The Medicare population has nearly doubled since the program began, growing from 19.5 million in 1967 to 37 million in 1995. This increase reflects the aging of the population and the rising number of disabled beneficiaries. The oldest old (ages 85 and older), disabled individuals under age 65, and those with end-stage renal disease are
Medicare's fastest-growing groups. During the 1990s, the number of Medicare beneficiaries has been growing at 1 to 2 percent annually (Physician Payment Review Commission, 1996).
Medicare Part A provides coverage for inpatient hospital, home health, hospice, and limited skilled nursing facility services. Medicare Part A is financed from the Hospital Insurance Trust Fund, paid for primarily through a payroll tax on employers and employees. Beneficiaries are responsible for deductibles and copayments. The Congressional Budget Office forecasts that Part A spending will increase by 10.2 percent in 1995, with annual growth rates of between 7.5 and 10 percent projected for the rest of the decade (Congressional Budget Office, 1995b). A recent report by the trustees of the Social Security and Medicare trust funds forecast that unless changes are made, the Hospital Insurance Trust Fund will run out of money by 2001 (Board of Trustees, 1996).
Medicare Part B coverage is optional and helps pay for covered beneficiaries' physician services, medical supplies, and other outpatient treatments and is financed by a combination of general tax revenue (about 75 percent of program costs) and enrollee premiums (about 25 percent of program costs). In addition to their premiums, beneficiaries are responsible for copayments and deductibles. According to the Congressional Budget Office, Medicare Part B spending is expected to increase by 10.9 percent in fiscal year 1995, and to average 12 to 13 percent annual rates of increase through the remainder of this decade (Congressional Budget Office, 1995b).
The distribution of Medicare expenditures for different services has shifted over time, partially because of greater reliance on ambulatory rather than inpatient medical care. Between 1980 and 1995 Medicare spending for inpatient hospital services declined from 66 to 44 percent, whereas spending for home health services increased from 1 to 8 percent. In the same time period spending for post-acute-care services—skilled nursing facility, home health, and hospice services—increased from 3 to 13 percent.
As it is presently structured the Medicare program provides incomplete protection; for example, it provides poor catastrophic coverage, no coverage for outpatient prescription drugs, and high deductibles and copayments for hospitalization costs. The Medi-
care benefit package is less generous than about 85 percent of the employer-based plans primarily because of comparatively high deductibles and copayments (Iglehart, 1992). The program covers less than half of all health care costs incurred by elderly individuals and even less of all health care costs incurred by the oldest old, who require more nursing home care. Although the Medicare benefit package has remained reasonably constant over the years, enrollees' out-of-pocket medical care costs represent an increasing share of their incomes. In 1994 out-of-pocket spending on acute-care services and premiums averaged 21 percent of the incomes of all elderly individuals, moving to 30 percent on average for the poor elderly and people over age 80 (Moon and Mulvey, 1996).
Most elderly beneficiaries (89 percent) have supplemental coverage to fill in the gaps that Medicare does not cover. More than one third of these individuals receive such insurance from a former employer, whereas another one third buy supplemental insurance (Medigap) for themselves. Eleven percent lack supplemental insurance altogether, and 12 percent of Medicare beneficiaries are protected from some or most out-of-pocket health care costs by the Medicaid program. Since 1988 state Medicaid programs have been required to pay Medicare Part B premiums and cost-sharing for all qualified Medicare beneficiaries (QMBs) whose incomes are less than 100 percent of the federal poverty threshold and whose assets are below a certain level. For low-income beneficiaries whose incomes are between 100 and 120 percent of the federal poverty level, Medicaid pays for Medicare Part B premiums only. Individuals must apply for Medicaid in their state to be eligible. Less than half of the eligible QMB population has applied for Medicaid payments (Neumann et al., 1995).
Medicare Managed Care
Since the early 1970s the federal government has supported the voluntary enrollment of Medicare beneficiaries in managed care programs through a number of demonstration projects. The 1982 Tax Equity and Financial Responsibility Act, which became operational in 1985, gave Medicare beneficiaries the option to enroll in federally-qualified health maintenance organi-
zations (HMOs) and competitive medical plans, all of which offer Medicare-covered benefits and the majority of which also offer coverage of cost sharing and supplemental services that replace Medigap policies. 1 Beneficiaries may choose to enroll in an HMO when they become eligible for Medicare or at other times that Medicare HMOs offer open enrollment. Plans must have at least one 30-day open season each year and may offer additional open enrollment periods. Furthermore, they must allow enrollment at other times to beneficiaries who have been disenrolled because of contract termination or nonrenewal by another managed care plan. Medicare beneficiaries can disenroll from their plans at the end of any month.
The Health Care Financing Administration's (HCFA's) managed care program has different types of contracts. Until recently, the only private health plans (risk contracts or risk plans) available to Medicare beneficiaries were HMOs, under which plans receive capitated payments for the beneficiaries whom they enroll. In general enrollees who select a risk plan are required to use the plan's network of providers and to agree to obtain all covered services through the plan, except in emergencies.
Capitation payments to the plans are based on an estimate of local fee-for-service costs and are established for each county at 95 percent of the adjusted average per capita cost (AAPCC) for Medicare fee-for-service beneficiaries. HCFA adjusts the AAPCC for enrollees' demographic characteristics such as age, sex, Medicaid eligibility, and residence in an institution such as a nursing home. The "risk adjustment" attempts to prevent HMOs from benefiting from favorable selection of health risk, which occurs when HMOs enroll beneficiaries who are healthier (and therefore less costly to care for) than those in the fee-for-service sector. In 1995 AAPCC monthly rates ranged from a low
of $177.32 to a high of $678.90 (U.S. General Accounting Office, 1996).
Under current law risk contract HMOs can retain profits up to the level earned on non-Medicare business. Profits that exceed this amount must be returned to enrollees either in out-of-payment reductions or enhanced benefits. On the basis of guidelines issued in October 1995, selected risk contracts will now be able to include a point-of-service option, upon HCFA's approval, which will allow beneficiaries to use providers outside a plan's network. HCFA expects that the point-of-service benefit may encourage more beneficiaries to join managed care plans.
Plans also can enter into cost contracts under which they are paid on a fee-for-service basis for the reasonable costs of services provided to their enrolled Medicare beneficiaries.2 Medicare beneficiaries in cost contract HMOs may seek care outside of the HMO at Medicare's expense—a benefit that is not available under risk contracts.
Medicare SELECT, another plan option, offers a network-based supplemental insurance (Medigap) policy that provides coverage for Medicare cost sharing. Medicare SELECT was created as a demonstration project in 1990 to offer beneficiaries in up to 15 states a new Medigap insurance option. In 1995 it was authorized to expand to all states. It could be made permanent in 1998.
Under its demonstration authority, HCFA also has operated a number of social HMO (SHMO) pilot projects with the purpose of providing a broad spectrum of acute- and long-term-care services to the frail elderly under a managed care system. In these types of projects HMOs receive higher reimbursements in exchange for providing home-based custodial care. The SHMO demonstrations also receive Medicaid funding.
In 1995, HCFA announced a new demonstration project called Medicare Choices, designed to offer flexibility in contracting requirements and payment methods for health plans and other organized delivery systems that wish to participate in
Medicare. Its broader purpose is to test beneficiaries' response to a range of health care delivery system options and to evaluate their suitability for Medicare.
The Medicare Managed Care Population
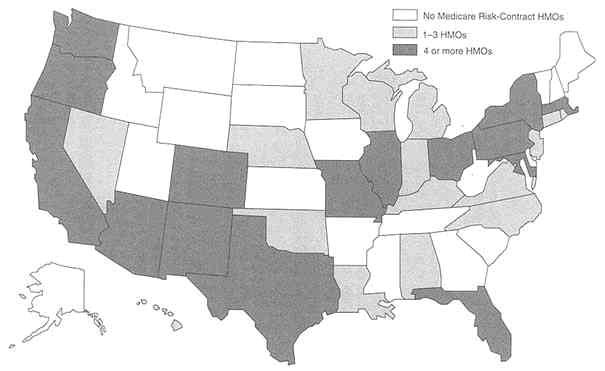
Although risk contracts make up the bulk of the Medicare managed care market and have accounted for most of the program's growth (with 197 risk contracts serving 3.4 million beneficiaries as of March 1, 1996), Figure 1-1 and Table 1-1 show that enrollment is concentrated in a few states and a few large HMOs. About 55 percent of Medicare HMO enrollees live in California and Florida and represent approximately 36 and 19 percent of the beneficiaries in those two states, respectively (Office of Managed Care, Health Care Financing Administration, 1996). Similarly, 10 large HMOs enroll 44 percent of all Medicare beneficiaries. As of August 1995, 31 states had no or insignificant enrollment in Medicare risk contract HMOs (U.S. General Accounting Office, 1996).
States with the highest concentrations of Medicare enrollees have one or both of two characteristics: they contain mature health care markets in which managed care has become a dominant mode of health care delivery for the population under age 65, and they are in areas of the country with high AAPCCs (U.S. General Accounting Office, 1996). As shown in Figure 1-2, to attract Medicare beneficiaries, participating HMOs are increasingly turning to the use of additional incentives: charging elderly enrollees zero premiums as well as offering popular benefits such as routine physicals, eye and ear examinations, and immunizations. About half of the HMOs offer outpatient prescription drug coverage. Over the past 3 years the number of HMOs charging Medicare beneficiaries no premiums for the services provided increased from about 26 to about 49 percent (U.S. General Accounting Office, 1996).
A number of recent studies indicate that changes in employment-based health care coverage for retirees is another factor contributing to the recent rapid rate of growth of Medicare beneficiary enrollment in HMOs (Interstudy, 1995; U.S. General Accounting Office, 1996). The rising cost of health care coverage for retirees is forcing a growing number of firms to drop or
TABLE 1-1 State and Territorial Enrollment in Medicare and the Percent of Beneficiaries Enrolled in Managed Care Plansa (Data as of January, 1996)
|
STATE |
Medicare Enrollees (% of national total) |
National Rank |
Medicare Managed Care Enrollees |
Percent of State’s Medicare Population Enrolled in a Managed Care Plan |
|
Alabama |
645,000 (1.7) |
19 |
12,952 |
2 |
|
Alaska |
34,000 (0.09) |
52 |
0 |
0 |
|
Arizona |
604,000 (1.6) |
21 (tie) |
184,742 |
31 |
|
Arkansas |
424,000 (1.1) |
31 (tie) |
0 |
0 |
|
California |
3,653,000 (9.8) |
1 |
1,302,713 |
36 |
|
Colorado |
424,000 (1.1) |
31 (tie) |
92,757 |
22 |
|
Connecticut |
504,000 (1.3) |
26 |
15,259 |
3 |
|
Delaware |
101,000 (0.27) |
48 |
0 |
0 |
|
District of Columbia |
78,000 (0.21) |
50 |
11,568 |
15 |
|
Florida |
2,630,000 (7.03) |
3 |
487,906 |
19 |
|
Georgia |
837,000 (2.2) |
12 |
2,954 |
0.35 |
|
Hawaii |
151,000 (0.4) |
43 |
50,092 |
33 |
|
Idaho |
150,000 (0.4) |
44 |
0 |
0 |
|
Illinois |
1,622,000 (4.3) |
7 |
117,585 |
7 |
|
Indiana |
825,000 (2.2) |
14 |
12,446 |
2 |
|
Iowa |
475,000 (1.3) |
29 |
9,300 |
2 |
|
Kansas |
384,000 (1.03) |
34 |
9,484 |
2 |
|
Kentucky |
589,000 (1.6) |
23 |
5,420 |
1 |
|
Louisiana |
583,000 (1.6) |
24 |
34,311 |
6 |
|
Maine |
203,000 (0.54) |
38 |
0 |
0 |
|
Maryland |
604,000 (1.6) |
21 (tie) |
19,631 |
3 |
|
Massachusetts |
936,000 (2.5) |
11 |
105,667 |
11 |
|
Michigan |
1,353,000 (3.6) |
8 |
8,260 |
1 |
|
Minnesota |
632,000 (1.7) |
20 |
118,500 |
19 |
|
Mississippi |
399,000 (1.07) |
33 |
0 |
0 |
|
Missouri |
835,000 (2.2) |
13 |
50,958 |
6 |
|
Montana |
131,000 (0.35) |
45 |
0 |
0 |
|
Nebraska |
250,000 (0.67) |
36 |
3,684 |
1 |
|
Nevada |
195,000 (0.5) |
39 |
50,690 |
26 |
|
New Hampshire |
157,000 (0.4) |
42 |
0 |
0 |
|
New Jersey |
1,173,000 (3.1) |
9 |
43,846 |
4 |
|
New Mexico |
212,000 (0.57) |
37 |
31,915 |
15 |
|
New York |
2,647,000 (7.08) |
2 |
252,511 |
10 |
|
STATE |
Medicare Enrollees (% of national total) |
National Rank |
Medicare Managed Care Enrolleesb |
Percent of State's Medicare Population Enrolled in a Managed Care Plan |
|
North Carolina |
1,033,000 (2.8) |
10 |
4.043 |
0.39 |
|
North Dakota |
103,000 (0.28) |
47 |
731 |
0.71 |
|
Ohio |
1,671,000 (4.5) |
6 |
46,803 |
3 |
|
Oklahoma |
489,000 (1.3) |
27 |
18,006 |
4 |
|
Oregon |
470,000 (1.3) |
30 |
157,645 |
34 |
|
Pennsylvania |
2,075,000 (5.6) |
5 |
182,885 |
9 |
|
Puerto Rico |
481,000 (1.3) |
28 |
0 |
0 |
|
Rhode Island |
169,000 (0.45) |
41 |
18,425 |
11 |
|
South Carolina |
512,000 (1.4) |
25 |
0 |
0 |
|
South Dakota |
117,000 (0.3) |
46 |
0 |
0 |
|
Tennessee |
774,000 (2.1) |
16 |
0 |
0 |
|
Texas |
2,091,000 (5.6) |
4 |
167,080 |
8 |
|
Utah |
188,000 (0.5) |
40 |
30,558 |
16 |
|
Vermont |
83,000 (0.22) |
49 |
708 |
1 |
|
V.I./Guam/ American Samoa |
18,000 (0.05) |
53 |
0 |
0 |
|
Virginia |
822,000 (2.2) |
15 |
5,121 |
1 |
|
Washington |
690,000 (1.8) |
18 |
104,804 |
15 |
|
West Virginia |
330,000 (0.88) |
35 |
7,726 |
2 |
|
Wisconsin |
763,000 (2.0) |
17 |
11,387 |
1 |
|
Wyoming |
61,000 (0.16) |
51 |
0 |
0 |
|
United Mine Workersc |
n/a |
n/a |
81,545 |
n/a |
|
TOTAL |
37,382,000(100) |
|
3,872,618 |
10 |
|
a Enrollee data (19,186) for Social Health Maintenance Organizations (SHMOs) are included in the total Medicare Managed Care enrollees. Totals do not necessarily equal the sum of rounded components. b Medicare Managed Care Enrollees include: TEFRA Risk, Cost, SHMOs, and Health Care Prepaid Plans. c United Mine Workers is a separate entity within Health Care Prepaid Plans (HCPP). SOURCES: HCFA/Office of Managed Care/Bureau of Data Management and Strategy and U.S. Department of Commerce/Bureau of the Census. |
||||
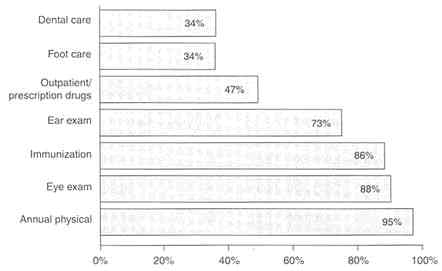
FIGURE 1-2 Percent of Medicare managed care risk contract plans that offer additional benefits.
SOURCE: Medicare Chart Book prepared by The Henry J. Kaiser Family Foundation and The Institute for Health Care Research and Policy, Georgetown University, 1995, p. 18. Reprinted with permission of the Henry J. Kaiser Family Foundation.
redefine this benefit by adding greater cost-sharing provisions for beneficiaries. This trend is making HMO enrollment more attractive to elderly beneficiaries, given that a growing number of plans offer more extensive coverage without deductibles or coinsurance.
Medicare beneficiaries often face a difficult trade-off between lower cost HMO risk plans or staying with their own physician. This is more obvious in low penetration areas of the country where fewer physicians join HMO networks. Although some research studies indicate that out-of-pocket costs remain the major determinant in deciding what plan an elderly beneficiary will join, other focus groups and survey findings indicate that a portion of the elderly population places even a higher value on the ability to remain with their doctor and their network of specialists and are willing to pay additional dollars in order to do so. Health care is a major priority and preoccupation for many elderly individuals and the value of continuing their relationship with trusted and known providers is often a higher
consideration than gaining access to the most affordable plan (personal communication July 22, 1996, Randall Brown, Senior Fellow, Mathematica Policy Research, Inc.).
Restructuring Medicare and the Context for the IOM Study
Early conversations about having the Institute of Medicine (IOM) conduct a study on accountability and informed purchasing for Medicare beneficiaries in an environment of broader choice and managed care began against a background of rising concern about the pressing need to dramatically reduce the rate of growth in entitlement spending and focused congressional interest in transforming the Medicare program to give beneficiaries the same health plan choices that have shown promise for holding down costs in the private sector. In the fall of 1995 the U.S. House Committee on Ways and Means of the 104th Congress first introduced the Medicare Preservation Act of 1995 (H.R. 2425). The Act contained provisions to expand the types of health plans to be offered to the elderly beyond traditional fee-for-service and HMOs to include point-of-service plans, provider service networks, and medical savings accounts. The bill contained financial incentives for the elderly to leave traditional Medicare and enroll in managed care plans, provisions that were largely eliminated in the Medicare provisions of the Balanced Budget Act of 1995 (H.R. 2491), which was vetoed by the President on December 6, 1995.
Congressional proposals to expand Medicare health plan options (Medicare Plus) stipulated that health plans contracting with Medicare be required to meet minimum standards in a number of areas, including solvency, quality assurance, service capacity, and consumer protections. In most cases plans would need to be licensed to bear insurance risk under state laws. Medicare Plus plans would provide benefits to beneficiaries in about the same manner as Medicare HMOs do today. The plans would receive capitated payments from the Medicare program for each beneficiary whom they enrolled. Plans would be responsible for providing at least the level of benefits that the current Medicare program provides, plus any additional benefits that the plan offered. Plans could modify the manner of
cost sharing, as long as the total cost sharing did not exceed the cost-sharing guidelines for the fee-for-service program.
To further encourage and facilitate the move to managed care, the legislation provided for a structured enrollment process and the requirement that beneficiaries be provided with more information about their options. A coordinated annual enrollment period would occur each year, during which beneficiaries would be able to change plans if they so desired. To assist beneficiaries in executing their choices, the congressional proposals required the Secretary of the U.S. Department of Health and Human Services to ensure that beneficiaries receive adequate information about their coverage options.
Activities at HCFA
In 1995 HCFA announced the Medicare Choices demonstration project, which would allow non-HMO managed care plans such as provider networks and POS plans to enroll Medicare patients for the first time, using a variety of payment mechanisms. The project was intended to test beneficiaries' responses to a range of health care delivery system options and to evaluate the suitability of those options for Medicare. The request for proposals explicitly encouraged a range of organizations, in addition to traditional HMOs, to submit applications, and it solicited applications from organizations in markets where Medicare managed care participation was relatively low (Health Care Financing Administration, U.S. Department of Health and Human Services, 1995). The HCFA solicitation produced inquiries from 400 managed care plans in 47 states. HCFA asked 52 plans to submit applications and in April 1996 announced 25 final candidates.
Although there is general agreement for the need to reduce Medicare spending and even on the potential merit and value of providing Medicare beneficiaries with the same array of health plan options available to the population under age 65, questions continue to be raised about the scope and pace of change being proposed and whether the necessary infrastructure for providing information, protections, and accountability are in place to enable Medicare beneficiaries to move safely and responsibly into what is for the vast majority of them a new frontier of
health care delivery for this population: managed care. Although managed care has become the norm for the employed population, for most elderly individuals it represents uncharted waters, even with today's dramatic growth in the level of Medicare HMO enrollment.
How is the Medicare Market Different?
Demographics
Although Medicare has uniform eligibility and financing requirements and all elderly beneficiaries have access to the same basic benefit package, individuals served under the program are extremely diverse in terms of sociodemographic characteristics and health needs. As a group Medicare beneficiaries are older and sicker than patients who have traditionally used managed care plans (Vladeck, 1995).
Among the Medicare-eligible population, 46 percent are ages 65 to 74, 31 percent are ages 75 to 84, and 12 percent are ages 85 and older (Henry J. Kaiser Family Foundation, 1995). Four and a half million of the Medicare-eligible population are persons under age 65 with disabilities or individuals with end-stage renal disease. Figure 1-3 illustrates that 57 percent of Medicare beneficiaries are women, 43 percent are men, and 84 percent of beneficiaries are white. Medicare beneficiaries, like the general population, tend to reside in urban areas (74 percent for Medicare beneficiaries versus 79.7 percent for the total U.S. population) (Henry J. Kaiser Family Foundation and Institute for Health Care Research and Policy, Georgetown University, 1995; Bureau of the Census, 1995).
The oldest old (ages 85 and over), persons under age 65 with disabilities, and individuals with end-stage renal disease have been Medicare's fastest-growing populations. The 31.2 million people in the United States over the age of 65 in 1990 is expected to grow to 52 million by the year 2020. In the same period, the very old, those age 85 and older, will more than double in size, from 3.1 million to 6.5 million people.
Although there is a perception that Medicare beneficiaries are relatively better off than their younger counterparts, three-quarters of older people have annual incomes of less than
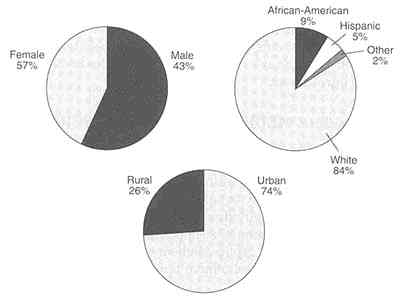
FIGURE 1-3 Distribution of Medicare population by gender, race, and residence, 1992.
SOURCE: Medicare Chart Book prepared by The Henry J. Kaiser Family Foundation and The Institute for Health Care Research and Policy, Georgetown University, 1995, p. 4. Reprinted with permission of the Henry J. Kaiser Family Foundation.
$25,000, as shown in Figure 1-4. In 1992 about 83 percent of Medicare program spending was on individuals in this income group. Eighteen percent of the Medicare population have annual incomes of between $25,000 and $50,000, and 5 percent have annual incomes greater than $50,000.
Recent reports indicate that many elderly may buy into managed care because of its lower price and affordability (U.S. General Accounting Office, 1996). Financially, they may not have any viable alternative even when they have credible grievances or are dissatisfied with managed care. This places a special burden on developing public accountability parameters to ensure adequate performance and access standards.
Both the aged and disabled groups have relatively high levels of education, with over 50 percent of each group having graduated from high school or attended college. The median number of school years completed among the population age 65
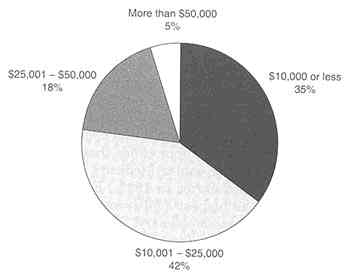
FIGURE 1-4 Distribution of elderly beneficiaries, by income, 1992.
SOURCE: Medicare Chart Book prepared by The Henry J. Kaiser Family Foundation and The Institute for Health Care Research and Policy, Georgetown University, 1995, p. 2. Reprinted with permission of the Henry J. Kaiser Family Foundation.
or older has risen steadily in the past 20 years (Adler, 1995). Obscured in these statistics, however, are the sizable number of elderly individuals with inadequate functional literacy skills. A recent study to assess the ability of patients to perform the wide range of literacy tasks required to function in the health care environment found a higher prevalence of inadequate functional health literacy skills among elderly individuals than among individuals in younger age groups (Williams et al., 1995).
Health Status and Risk Selection
Data from the Medicare Current Beneficiary Survey indicate that almost half of the aged Medicare beneficiaries (45.8 percent) rate their health as excellent or very good, a proportion that is ''remarkably stable" across age groups. On the other hand, only 17 percent of the disabled rate their health as excellent or very good, whereas 57.8 percent rate their health as fair or poor (Adler, 1995, p. 175). A Henry J. Kaiser Family Founda-
tion survey reports that 30 percent of Medicare beneficiaries rate their health as fair to poor (Henry J. Kaiser Family Foundation, 1995). Self-assessed health has been shown to be a reliable predictor of future health care utilization.
Similar to the rest of the population, a small proportion of all Medicare beneficiaries consumes a significant share of total Medicare spending: 10 percent of the beneficiaries account for 70 percent of program expenditures. Per capita spending for the elderly, however, is roughly four times that for the rest of the population. Annual per capita Medicare spending averaged about $4,000 for beneficiaries in 1993. For the 10 percent of beneficiaries with the highest health costs, Medicare spent an average over $28,000 per beneficiary. Medicare paid no benefits on behalf of the healthiest 20 percent of beneficiaries (Henry J. Kaiser Family Foundation and Institute for Health Care Research and Policy, Georgetown University, 1995). As the Medicare market becomes more competitive, protections must be put into place to ensure that plans do not engage in practices that discriminate against high-risk patients.
Much of the literature suggests that Medicare beneficiaries enrolled in HMOs have tended to be healthier than those enrolled in the traditional Medicare program, although a more recent study indicates that the Medicare HMO population is becoming more broadly based and that its overall health status mirrors that of the non-HMO population (Price Waterhouse LLP, 1996). Nevertheless, the concern that HMOs may limit access to necessary care remains. Although conventional fee-for-service care is thought to promote the excessive utilization of medical services, there is concern that providers may overreact to the financial incentives to limit utilization, leading to reduced access to needed services by the elderly (Clement et al., 1994).
The potential for risk selection in Medicare health plans is a particularly serious concern. Some plans may draw beneficiaries whose health care costs are expected to be low (favorable selection); others may attract beneficiaries with complex medical problems and whose health care costs are expected to be high (adverse selection) (Physician Payment Review Commission, 1996). The problem of risk selection is greater under Medicare both because beneficiaries enroll as individuals and be-
cause variability in health care expenditures among elderly and disabled enrollees is far greater than those among the general population (Aaron and Reischauer, 1995). In addition, opportunities for biased selection are shaped by the rules and practices of the present market. For example, the current ability of Medicare beneficiaries to change health plans every month, unlike the typical annual open enrollment seasons for employees, enhances the opportunities for biased selection, as does the ability of an HMO to decide whether or not to enter the Medicare market and the type of contract options it will make available to beneficiaries (Miller and Luft, 1994).
A number of studies have shown that the elderly generally suffer from a lack of understanding about basic health care coverage and therefore are not equipped to operate effectively in an environment of broader choice. Consumers are unable to make effective choices because the variation and array of coverage are confusing (McCall et al., 1986; Jost, 1994). The availability of state-of-the-art information is critical for consumer choice (and voice), but such information for the Medicare population is still in a stage of infancy.
Information Dissemination
Unlike the population under age 65, Medicare beneficiaries have had relatively little exposure to diverse managed care models and have been shown to be more apprehensive and concerned about managed care than their younger counterparts (The Robert Wood Johnson Foundation, 1995). Much of this concern and apprehension is linked to the possibility that beneficiaries, in joining a managed care plan, will no longer be able to stay with their current physician (Frederick/Schneiders, 1995).
The lack of familiarity with managed care underscores the importance of providing beneficiaries with information that will enable them to make informed choices. Numerous studies, however, have shown that Medicare beneficiaries are poorly informed about what the traditional Medicare program covers and have very limited understanding of what managed care is or what the specific benefits of a particular managed care plan are (Sofaer, 1993; McCall et al., 1986; Rice, 1987; Davidson, 1988).
Medicare beneficiaries are not particularly distinguished from other consumers in their lack of understanding of their insurance coverage; such information has been shown to be not important to most people until they become sick (Mechanic, 1989; Pemberton, 1990). Older individuals, however, process information differently than young adults, finding more difficulty understanding information when it is new or complicated (Davidson, 1988). Surveys indicate that it takes more time and that it is more resource intensive to educate the elderly than younger individuals about their health care choices. Elderly beneficiaries like to have information presented to them in a variety of formats and have a particular preference for face-to-face interactions. Materials and approaches used to inform the employed population about their health care options may not be well suited to the elderly population. 3
The Committee's Charge
The current debate over offering Medicare beneficiaries more choice in health plans as a vehicle for reform and deficit reduction stimulated the Institute of Medicine to appoint a committee that would provide guidance to policy makers and decision makers on ensuring public accountability by and on behalf of Medicare beneficiaries in a system of expanded choice and with a growing role for managed care.
Three tasks framed the committee's charge:
- to commission background papers from experts and practitioners in the field that review the literature and synthesize aspects of the leading issues and current policy proposals as they pertain to ensuring public accountability and informed purchasing in a system of broadened choice;
- to guide, develop, and convene an invitational symposium to (1) examine what is known (or not known) about ensuring
- public accountability and informed purchasing in the current Medicare program and other health plans, (2) recommend how public accountability and informed purchasing can be ensured for Medicare beneficiaries in managed care and other health plan choices, and (3) discuss options and strategies that can be used to help government and the private sector achieve the desired goals in this arena; and
- to produce a report that will include the commissioned background papers, a summary of the symposium discussion, and recommendations on the major issues that need to be addressed to ensure public accountability and the availability of information for informed purchasing by and on behalf of Medicare beneficiaries in managed care and other health care delivery options.
Definitions and Study Approach
Definitions
At its first meeting the committee spent considerable time discussing the context of its charge and establishing some working definitions of choice and managed care, public accountability, and informed purchasing by and on behalf of Medicare beneficiaries. Each of these deserves a note of clarification for the purpose of this report.
Choice and Managed Care
The committee's original name was, "Medicare Managed Care: Assuring Public Accountability and Informed Purchasing for Beneficiaries." At its first meeting the committee felt strongly that responsibility for public accountability and informed purchasing should not be limited to the new plans that would be offered to beneficiaries but should pertain equally to the traditional Medicare program. Although the committee acknowledged that the traditional Medicare program remains very popular among the elderly, it should not be excluded from the measures of accountability and performance that will be required of managed care plans. Choice for the purpose of this report refers to all of the health plan options (e.g., traditional
Medicare and other indemnity plans, medical savings accounts, and Taft-Hartley-sponsored plans) not only managed care arrangements.
The committee recognized that there is not a universally accepted definition of managed care. As the managed care industry continues to evolve, the boundaries between different types of plans will become increasingly blurred. Therefore, for the purpose of this report the committee selected to define managed care broadly to include the following:4
Any product or arrangement that seeks to coordinate or control the use of health services by its enrolled members. Arrangements can involve a defined delivery system or providers with some form of contractual arrangement with the plan. Types of plans can range from simple PPOs to more tightly structured HMOs.
Public Accountability
A 1994 IOM study, Defining Primary Care: An Interim Report, defined the term accountability as the quality or state of being responsible or answerable. Accountability also has been defined to mean "subject to the obligation to report, explain or justify" (Random House, 1983).
For the purpose of this report, the committee discussed the difference between "accountability" and "consumer protections" and suggested that accountability for services could be viewed as the equivalent of ensuring the safety of products through consumer protections. Consumer protections are usually mediated on a case-by-case basis, whereas accountability usually implies a broader concept to include responsibility to a group and to a larger public.
During the committee's deliberation the article, "What is
Accountability in Health Care?" was published (Emanuel and Emanuel, 1996). The article reflects the notion that occasionally a single word comes to dominate discussions about a topic and becomes a "keyword." Such a keyword can serve as a "shorthand expression for an entire view; and persons with diverse perspectives affirm its perspective" (Emanuel and Emanuel, 1996, p. 229). In the current health policy dialogue, accountability has become a keyword.
In health care the matrixes of accountability (the who, what, and how) have traditionally been shared by three different domains: the professional, political, and economic domains. Part of the rationale for the present IOM activity was the concern on the part of some stakeholders that under a more market-oriented Medicare program, the locus of accountability may shift markedly from the public to the largely untested private sector. Such a shift in accountability would have special relevance for elderly individuals, who in the past have relied on providers and government to provide the necessary assurances and protections.
For the purpose of this report the committee selected to define public accountability as accountability to the public, defining public as beneficiaries in the first instance, but also the larger public as interested parties and taxpayers, and to define government as the elected representatives of the citizenry.
Although public accountability may mean different things to different people, most would accept the basic premise that managed care (choice) plans should be held accountable to both Medicare beneficiaries and the public at large: to Medicare beneficiaries because of the contractual arrangements between managed care plans and their Medicare enrollees and to the general public because it pays (through Medicare taxes, Part B premiums, and general revenues) for the care that is provided.
Considering the mandate of this report, the committee discussed some additional elements of public accountability and determined that these should include the following:
- requirements for disclosure and the dissemination of relevant and useful information,
- the capacity to assess and report whether contracted services are performed responsibly and effectively,
- requirements as a public program financed by taxpayer dollars to see that the needs of individuals are balanced against the wise use of collective resources, and
- a special level of responsibility as the purchaser of health care for elderly beneficiaries, many of whom are vulnerable.
Informed Purchasing by and on Behalf of Beneficiaries
If there is little dissension over the need for public accountability and informed purchasing, the question of how to ensure it is far more contentious. Some will argue that market competition and informed purchasing are the best guarantees of access to high-quality services. Others argue for a strong federal regulatory and oversight role and advocate for extensive regulations in a number of areas including marketing, access, quality, appeals and grievances, data collection, and solvency. Others propose a middle ground that would permit a greater role for the market, with its potential to be more efficient and innovative and as a better expression of consumer wants and desires, yet leave to government the role of limiting the number of market entrants to those that meet certain minimum standards of performance and that offer certain minimum protections. Each of these three models (market, directed, and assisted) results in a different matrix of accountabilities.
Without adequate, reliable, comparable, and timely information, it is not possible to exercise informed choice. At its first meeting, the committee discussed the problem that even under the best of circumstances, some elderly people, particularly extremely frail and cognitively impaired individuals, would not be able to exercise choice on their own. The committee was struck by a report from the Alina Health Plan, a major HMO in Minnesota serving a large Medicare population, which reported that for almost half of the plan's elderly enrollees, major decisions about medical care are made not by the enrollees but by a spouse, a family member, or a caretaker (Mastry, 1995). The committee wanted the title of its activity to reflect the reality that for a significant part of the Medicare population, the responsibility of informed purchasing will need to be delegated in
some manner. This has implications for how the information infrastructure is developed and disseminated for this group.
Several members of the committee noted that the term beneficiary may be inappropriate in a more market-oriented health care system. In today's competitive choice environment, beneficiaries will be regarded increasingly as consumers and customers who can vote with their feet and who will need to be satisfied. The thrust of this report focuses on identifying accountability systems, resources, and the knowledge base that will help beneficiaries to become informed and effective consumers, even as it applies to traditional Medicare.
Study Approach
In considering the best way to accomplish its task, the committee arrived at a number of approaches and conclusions that shaped its agenda.
- The committee's focus was on beneficiaries/consumers (rather than plan managers, clinicians, or payers of care). The committee used the analogy of wholesale and retail information that had been well-described in a recent paper by Lynn Etheredge (Etheredge, 1995). The success of the choice paradigm will require Medicare beneficiaries to act as consumers and individual purchasers and to move from having a passive role to having an active voice, a new role and responsibility that succeeds only if information and standards of accountability that are directly relevant, meaningful, and accessible to them are developed. Until now most of the information on quality and performance has been developed for private group purchasers, managers, clinicians, and some public payers.
- The present study was initiated with the expectation that Medicare legislation providing broader beneficiary choice would pass the U.S. Congress before the study was completed. The committee used the Medicare provisions of H.R. 2491, the Balanced Budget Act of 1995, as a template for its work agenda and for the focus and structure for its deliberations. Although, President Clinton vetoed the final bill, the committee believes that the bill's Medicare reform provisions still provide a useful and relevant framework for reform.
- The science-based and peer-reviewed literature on public accountability and informed purchasing for Medicare beneficiaries under a market-oriented choice paradigm is sparse since the field is young and continues to evolve at an unprecedented pace. The state-of-the-art information in this arena resides primarily among a number of large private and public purchasers that currently define the field and various other organizations and agencies such as the National Committee on Quality Assurance (NCQA), HCFA, the U.S. General Accounting Office, the Physician Payment Review Commission (PPRC), the Foundation for Accountability, and the Agency for Health Care Policy and Research, which have a major interest in and programs directed to this area. With that in mind, the committee developed a symposium primarily around real-world experts who could comment on and respond to the commissioned papers, to other relevant and available research findings, and to the Medicare reform proposals from their well-recognized experiences.
- The committee was primarily interested in learning about current best practices in the public and private sectors as they relate to public accountability, informed purchasing, and competition based on excellence. There was a caution that the term best practices should be reserved for interventions that had been tested and evaluated on the basis of quality and cost-effectiveness and that the term promising interventions or models might be more accurate.
- The committee was fortunate to be able to commission eight papers—including five literature reviews and two case studies that review the state-of-the-art and consider a continuum of organizational and policy options for assuring public accountability and informed purchasing-written by national experts. These papers cover the most critical aspects of ensuring public accountability and informed purchasing for Medicare beneficiaries in an environment of choice.
-
- To frame the symposium dialogue and the committee's later deliberations, the committee asked Lynn Etheredge to write a paper proposing a conceptual framework for ensuring public accountability and informed choice from the perspective of beneficiaries by looking at how and where the various loci of responsibilities would be placed in the continuum of three alternative potential models: letting the market prevail (market
- model), letting government decide what is best (directed model), or providing a larger role for the market but leaving to government the responsibility of weeding out the bad apples (assisted model). Each model requires a different matrix of accountability and informed purchasing.
- A paper by Elizabeth Hoy, Elliott Wicks, and Rolfe Faland reviews current best practices for structuring and facilitating consumer choice of health plans, looking at model programs developed by leading private and public purchasers.
- A third paper, by Joyce Dubow, focuses particularly on the special considerations required to move Medicare beneficiaries as a more vulnerable cohort into managed care arrangements.
- A paper by Susan Edgman-Levitan and Paul Cleary reviews the literature on what information consumers want and need and their ability to assess issues of quality and accountability.
- Carol Cronin's paper summarizes what is known about how to most successfully reach and educate beneficiaries about choice.
- A paper by Patricia Butler focuses on the effectiveness of current federal and state regulatory activities designed to satisfy and protect consumers in managed care plans.
- Two case studies were also commissioned. The committee was aware of several U.S. General Accounting Office studies indicating that HCFA needed to improve its HMO monitoring processes and, furthermore, that as currently staffed and organized, HCFA may not be well structured to respond to the complex, rapidly changing health care system and would need to develop a new set of tools and authorities to operate as an effective purchaser of risk contracts (Cunningham, 1996; U.S. General Accounting Office, 1995a-f; Special Committee on Aging, U.S. Senate, 1995). The committee commissioned a paper to summarize HCFA's recent efforts directed at improving and streamlining its data collection and performance monitoring as well as to review HCFA's recent investments in beneficiary and customer communications. A case study of the California Public Employees' Retirement System (CalPERS) was also commissioned. CalPERS is frequently referred to as a model of group
- purchasing in a competitive environment on the basis of performance and consumer satisfaction measures.
- The symposium agenda, a list of the participants, and a list of the commissioned papers are provided in Appendixes B, C, and D, respectively. The symposium was organized as an expert hearing with an emphasis on fact finding from the perspective of published research, current practices, and well-regarded firsthand expertise from the field.
In considering its work and statement of task, the committee had to be mindful of the relatively short time frame within which this report had to be completed and the limited resources available to support the commissioned papers/research syntheses and the symposium activity. Given the committee's broad charge and the many issues that potentially fall under the rubric of ensuring public accountability and informed purchasing in an environment of choice and managed care, the committee believed that it was important and essential to set some priorities, parameters, and caveats regarding its work agenda. They are as follows:
- The task of the committee was not to judge the value of managed care as a vehicle for providing more appropriate, cost-effective care to Medicare beneficiaries or to reducing the rate of escalation in the costs of the Medicare program over time. The committee operated under the assumption that managed care plans will continue to grow and develop and to be made available to the Medicare population. Several members of the committee, however, expressed concern that any balanced appraisal by the elderly population of the potential of managed care to provide better care may be made more difficult for two important reasons. One, current proposals to restructure Medicare are being viewed by many elderly as a means of financing deficit reduction and achieving other political objectives. Two, in the case of all areas of health in which fundamental changes are being proposed, the media tends to focus on areas of discord and contention, contributing perhaps to additional anxieties among the already risk-averse elderly population.
- In looking at the issue of public accountability and the
- availability of information for informed purchasing, the committee's major focus was the consumer (Medicare beneficiary) rather than plans, clinicians, or group purchasers. Much of the current information relating to performance and quality has been developed for these groups and may not be useful or relevant to the Medicare population.
- The committee was asked to focus its attention on the issue of choice and the number and range of health plans, not the inherent merit or value of individual types or forms of plans to be offered (i.e., preferred provider organizations [PPOs] versus medical savings accounts versus unrestricted fee-for-service indemnity coverage).
- Although the committee recognizes the great diversity of the Medicare population, this report focuses primarily on the ''mainstream" Medicare beneficiary. The committee realizes that severely disabled individuals and dually eligible beneficiaries (individuals who enrolled in both Medicare and Medicaid) may need different and additional protections with regard to public accountability and informed purchasing. It was not possible within the scope of this particular study to reflect adequately on the special and additional information and accountability requirements that may be needed by the disabled and the dually eligible as they enter a more market-oriented delivery environment.
- Many of today's elderly are particularly apprehensive about managed care and are concerned about their ability to make informed choices among health plan options. The committee heard evidence that the move to a choice paradigm with an emphasis on managed care represents greater challenges and problems for the current generation of Medicare beneficiaries, particularly the older cohort. With the increasing role of managed care, there is every expectation that future Medicare beneficiaries will have had considerable experience with this new delivery structure and therefore will be better informed and more comfortable consumers of managed care.
- The committee did not focus on the issue of risk selection, although it acknowledges that it is a major problem that must be addressed.
- Although the issues of fraud and abuse, estimated by the
- U.S. General Accounting Office to be in the range of 10 percent of Medicare health care costs, are a significant problem in the Medicare program, they were outside the mandate of the present study.
- The committee focused much of its work on learning from model programs and major purchasers in the private sector, with the full realization that Medicare as a government social insurance program requires, in many important respects, a different response. The committee also heard considerable testimony from public purchasers including state-based organizations and HCFA.
- In defining parameters and vehicles to promote public accountability and informed purchasing, the committee recognizes the importance of maintaining the necessary flexibility in order to respond in a timely, appropriate fashion to a dynamic and evolving marketplace.
The committee's major charge and responsibility was to provide direction and guidance on how to promote public accountability and informed purchasing by and on behalf of Medicare beneficiaries in a new market-oriented environment characterized by choice and managed care. The committee was cognizant that in the new health care marketplace, Medicare beneficiaries as consumers or customers will be given both greater freedom and more responsibility for choosing their health plans and for making many of the important decisions associated with purchasing their health care and judging its value, adequacy, and responsiveness. Given the breadth and scope of its charge, the committee recognizes that many of the issues and topics that it addressed will benefit from additional review and analysis as better data and research findings become available.
It should also be noted that the committee was carefully formulated to reflect a balance of expertise particularly relevant to its charge. It included two experts from health plans, two individuals from the world of large purchasers-one public and one private, two consumer advocates with special expertise in elderly consumers in the health care marketplace, an expert on state insurance laws and regulations, a geriatrician, and an economist who has written extensively on the issue of opening choice and the structure of choice under market conditions.