G
Medicare Managed Care: Issues for Vulnerable Populations
Joyce Dubow*
Introduction
Recent interest in managed care, a system of care that accepts responsibility for the delivery of health services and the financing of coverage, stems largely from its purported ability to save money.1 In the private sector, employers have turned to managed care to contain steadily rising outlays for employee health insurance premiums. Now, the U.S. Congress also seeks to curb Medicare's rate of growth by restructuring the Medicare program through the introduction of a broader range of health care options that feature managed care arrangements (Balanced Budget Act of 1995). However, the plan to shift the Medicare
program so rapidly to managed care raises key questions about this approach, in part because the intended shift is so rapid and also because many are not persuaded that managed care plans are ready for a large influx of vulnerable new members (Braveman and Bennett, 1995). Others caution that the expectations of managed care are unrealistic (Ginzberg, 1995; Mashaw and Marmor, 1995; Meyer et al., forthcoming).
Unlike their younger counterparts, Medicare beneficiaries have had relatively little exposure to diverse managed care models. As of January 1996, only slightly more than 10 percent, or approximately 4 million individuals, have been enrolled in any form of managed care, mainly risk-based health maintenance organizations (HMOs). Enrollment is concentrated in just a few areas. In January 1996, about 50 percent of the Medicare beneficiaries enrolled in risk-based HMOs lived in just four states, California, Florida, Arizona, and New York (Health Care Financing Administration, Office of Managed Care, 1995a). Furthermore, those beneficiaries who have been enrolled in Medicare HMOs have tended to be healthier and younger than those enrolled in the traditional Medicare program (Brown et al., 1993). In January 1994, only 4.8 percent of Medicare risk enrollees were disabled (compared with approximately 11 percent in the traditional Medicare program) (Health Care Financing Administration, Office of Managed Care Operations and Oversight Team, 1995b). Finally, a recently released survey of Medicare beneficiaries (U.S. Department of Health and Human Services, 1995a) indicates that many beneficiaries (64 percent) do not even know if they live in areas where they could currently enroll in a managed care plan—this, in spite of the fact that three fourths of beneficiaries do have such an option. Thus, managed care is unknown or unfamiliar to many beneficiaries.
The purpose of this paper is to consider the prospect of managed care enrollment for Medicare beneficiaries, particularly those who are vulnerable. How can such individuals be expected to fare in a health delivery environment that is vastly different from the one that most of them have known and understood? The paper first defines "vulnerable" and presents selected demographic characteristics of such individuals. The experiences of vulnerable individuals in managed care programs is
then considered by examining some of the research literature with regard to medical outcomes, patient satisfaction, and disenrollment. Ways that managed care plans currently organize to treat their vulnerable enrollees are presented, and promising innovations and practices that appear to have potential for the successful treatment of vulnerable or high-risk persons are highlighted. Finally, the unique responsibility of public (versus private) purchasers to safeguard the interests of Medicare and Medicaid beneficiaries is identified and the protections that are needed by vulnerable populations enrolled in managed care plans are described.
Definition of Vulnerable
The changing demographic characteristics of the Medicare population will have a profound effect on the future of the program, particularly with respect to expenditures and the provision of services to beneficiaries. As policy makers develop strategies for restructuring Medicare, it is imperative that they take into account the individuals who use and rely on program benefits. Medicare beneficiaries are vulnerable because of age-related physiologic changes, multiple chronic physical and mental conditions, limited social resources, and a limited ability to manage change (Bates and Brown, 1988). Those segments of the Medicare population that are growing will have the greatest needs: the "old old," people of color, those with disabilities such as end-stage renal disease (ESRD), and cognitive impairments. Therefore, delivery systems must adjust to address the unique needs of an older, frailer population.
To one degree or another, virtually the entire Medicare population can be considered vulnerable because of its greater need for health care services and the higher health care costs that beneficiaries incur on account of their age, health status, economic status, or disability. To be sure, many of the "young old" are vibrant and healthy. Nevertheless, as a group, Medicare beneficiaries need more health care services, develop more chronic conditions as they age, and on average, have relatively low-incomes and who, but for Social Security and Medicare, would be poor. Therefore, in this paper, "vulnerable populations" are considered Medicare beneficiaries, both aged and dis-
abled, including those dually eligible for Medicaid and Medicare.
As of 1994, there were 36.7 million Medicare beneficiaries of whom 32.6 million were aged (age 65 and over) and 4.1 million were disabled (Health Care Financing Administration, Bureau of Data Management and Strategy, 1995). This estimate includes 229,000 persons with ESRD.
In 1994, 14 percent of all Medicare beneficiaries were minorities: 8 percent were African Americans, 2 percent were Asian or Pacific Islanders, less than 1 percent were American Indian or Native Alaskan, and 4 percent were of Hispanic origin (who may be of any race) (American Association of Retired Persons/U.S. Department of Health and Human Services, Administration on Aging, 1995). Seventy-four percent of beneficiaries lived in urban areas, whereas 26 percent were from rural areas. The racial compositions of those living in urban and rural areas were similar, with whites making up about 84 percent of the beneficiary population in urban areas and 87 percent in rural areas (Health Care Financing Administration, 1995). Elderly populations of color, as a percentage of the total U.S. population, are projected to increase; by 2020, 21 percent of elderly persons are projected to be persons of color; by 2050, 30 percent (American Society on Aging, 1992).
Disabled beneficiaries account for a growing proportion of total Medicare enrollees. In 1994, disabled enrollees accounted for 11 percent of all beneficiaries, a proportion that is projected to increase to 17 percent by the year 2010; the ESRD population is projected to double by this date, largely because of improved technology and a greater availability of dialysis machines (Health Care Financing Administration, Office of Research and Demonstration, 1995; U.S. General Accounting Office, 1995a). With respect to their racial composition, 18 percent of disabled Medicare beneficiaries are African Americans. Ten percent of beneficiaries are of Hispanic origin (Adler and Phil, 1995).
Age
In 1992, 12.7 percent of the U.S. population or 33.2 million people, were 65 years of age or over (American Association of Retired Persons, U.S. Department of Health and Human Ser-
TABLE G-1 Actual and Projected Growth of those 65 and over, 1990, 2030 (percent of total population)
|
Year |
=65 |
65-74 |
75-84 |
=85 |
|
1990 |
12.6 |
7.3 |
4.0 |
1.3 |
|
2030 |
21.8 |
12.0 |
7.1 |
2.7 |
|
SOURCE: U.S. Congress, Senate, et al., 1991. |
||||
vices, Administration on Aging, 1995). The older population, as a proportion of the total population, has tripled in this century. By 2030, the number of persons over age 65 is expected to grow to 65.6 million, representing 22 percent of the total population (Table G-1). There is an upward trend in life expectancy. The increase in life expectancy since 1970 has resulted from declines in mortality among middle-aged and elderly persons U.S. Congress, Senate, et al., 1991) (Figure G-1).
Like the general population, the elderly population is growing older. By 2000, of the 35 million persons who will be 65 years of age or older, half will be between the ages of 65 and 74 and almost half will be age 75 or over (U.S. Congress, Senate, et al., 1991). The population over age 85 is the fastest-growing portion of the population.
In 1994, among Medicare beneficiaries, 46 percent were between 65 and 74 years of age; as a percentage of total Medicare enrollees, the number of people in this age group has been steadily declining (Health Care Financing Administration, Bureau of Data Management and Strategy, 1995; Health Care Financing Administration, Office of Research and Demonstration, 1995). Thirty-one percent were between the ages of 75 and 84, and almost 12 percent were age 85 and over, a group whose numbers have steadily been increasing as a percentage of the total Medicare population (Health Care Financing Administration, Bureau of Data Management and Strategy, 1995; Health Care Financing Administration, Office of Research and Demonstration, 1995). In 1994, Medicare expenditures were greatest for the cohort over age 85; Medicare expenditures for this group are projected to increase sixfold from 1987 to 2040 (Schneider
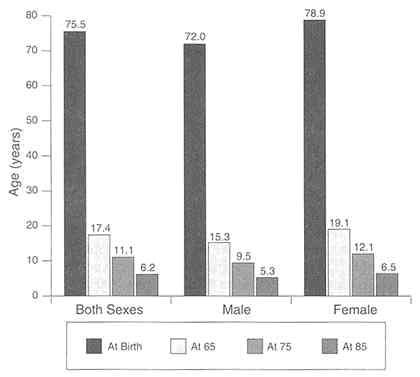
FIGURE G-1 Life expectancy at birth and at age 65, 75, and 85, 1991.
SOURCE: U.S. Department of Health and Human Services, 1995d, Table 1, pp. 136-137.
and Guralnik, 1990). Of the disabled population on Medicare, almost 35 percent were under 45 years of age, 27 percent were between the ages of 45 and 54, and 38 percent were between the ages of 55 and 64.
Health Status
Data from the Medicare Current Beneficiary Survey indicate that when asked how each would rate his or her own health compared with the health of others the same age, almost 46 percent of aged Medicare beneficiaries rated their health as excellent or very good, a proportion that is considered "remarkably stable" across all age groups (Adler and Phil, 1995). However, other survey results (Figure G-2) suggest that individual
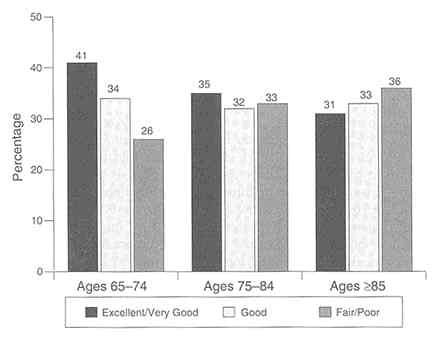
FIGURE G-2 Self-reported health status, percent distribution of persons by age according to respondent-assessed health status, 1992.
SOURCE: U.S. Department of Health and Human Services, 1995d, Table 1, p. 36.
perceptions of health may decline with age. Self-assessed health status also differs markedly by disability status and race. Only 17 percent of disabled beneficiaries and approximately 25 percent of African Americans reported their health as excellent or very good (Adler and Phil, 1995; Health Care Financing Administration, 1995).
Data from a 1994 National Research Corporation survey indicate that those Medicare beneficiaries enrolled in HMOs report health status similar to those receiving care in the traditional Medicare program. Forty-seven percent of HMO members considered their health status to be excellent or very good, whereas 46 percent in the fee-for-service program considered their health status to be excellent or very good (Group Health Association of America, 1995d).
Disability and Chronic Health Care Problems
Medicare beneficiaries have diverse needs and service preferences that range from medical care for those with acute chronic conditions to services that help individuals compensate for chronic health problems or disability.
With advancing age, the incidence of acute conditions diminishes as chronic conditions become more frequent (U.S. Congress, Senate, et al., 1991). In 1991, the Institute of Medicine reported that among those age 60 and over, 8 of 10 had one or more chronic diseases or impairments (Pope and Tarlov, 1991). The top 10 chronic conditions for people over 65 years of age in 1989 were arthritis, hypertension, hearing impairment, heart disease, cataracts, deformity or orthopedic impairment, chronic sinusitis, diabetes, visual impairment, and varicose veins (U.S. Congress, Senate, et al., 1991). Chronic conditions are the main cause of disability among elderly persons (Bates and Brown, 1988).
Researchers use different measures to assess varying degrees of impairment, in part, on the basis of how well individuals function in the community. The following data illustrate variations in the prevalence of disability in the population over age 65 reflecting three different ways of evaluating impairment from less to more severe. (1) In 1991-1992, almost half of those over 65 years of age had difficulty with or were unable to perform everyday activities such as seeing words and letters, hearing normal conversations, having their speech understood, and climbing stairs without resting. (2) A more limited number, about 22 percent, had difficulty with or needed personal assistance with specific tasks (i.e., instrumental activities of daily living that help them remain in the community), such as keeping track of money, preparing meals, or getting around outside the home. (3) Finally, about 15 percent had difficulty with an activity of daily living (ADL) such as getting in and out of bed, bathing, eating, or dressing (McNeil, 1993).
In addition to functional impairments, many older persons also have mental or cognitive impairments. The various forms of dementia that affect behavioral, emotional, and social functioning are the primary mental disorders of elders. Other causes of cognitive impairment in elderly persons include delirium, the
toxic effects of medications, trauma, and psychiatric illness. The prevalence of dementia among those over 65 years of age living in the community is approximately 3 to 6 percent, with the prevalence increasing with advancing age (Callahan et al., 1995). Nationally, in 1991, the total cost for those with senile dementia was estimated at $67 billion (Callahan et al., 1995). Nearly 5 million individuals over 65 years of age experience serious symptoms of depression. However, this estimate may undercount the prevalence of this condition because depression is probably underdiagnosed (Rolnick et al., 1994). There is research indicating that rates of depression are high among chronically ill, older adults (Williams et al., 1995). Approximately 5 percent of older adults have an anxiety disorder, with perhaps 10 to 20 percent displaying anxiety symptoms (Smyer, 1993).
Utilization of Services
Those over 65 years of age use more health services than younger persons. On average, in 1993, those over age 65 had almost 10 physician contacts compared with approximately 6 visits for those under age 65 (U.S. Department of Health and Human Services, Public Health Service, 1995). Likewise, in 1992, those over age 65 averaged 2,711 hospital days per 1,000 persons compared with about 456 days per 1,000, for persons 0 to 64 years of age (Gabel et al., 1994; Health Care Financing Administration, Bureau of Data Management and Strategy, 1995). Differences in the utilization of health services between younger and older populations appear to hold true in managed care as well. In 1992, HMO members who were group enrollees averaged 3.9 ambulatory physician encounters per year, compared with 7 ambulatory physician encounters per Medicare risk enrollee (Gabel et al., 1994). In 1992, HMO enrollees over 65 years of age averaged 1,295 hospital days per 1,000 persons, compared with 270 days per 1,000 members for HMO enrollees 64 and under (Gabel et al., 1994).
Income and Poverty Status
In 1994, 83 percent of Medicare spending was on behalf of
those with annual incomes under $25,000, suggesting that Medicare (as well as Medicaid) primarily serves the needs of lower-income individuals (Armstead et al., 1995). In fact, as a group, Medicare beneficiaries are people who have relatively low-incomes. In 1993, 30 percent of all Medicare beneficiaries had annual incomes under $20,000; more than 20 percent had annual incomes under $10,000 (The Public Policy Institute/American Association of Retired Persons, 1995, using Current Population Survey data) (Table G-2).
In 1994, the poverty rate for persons over age 65 was 11.7 percent. The threshold used by the Census Bureau to establish poverty status for the elderly is lower than that for other age groups (The Public Policy Institute/American Association of Retired Persons, 1995) (Table G-3). As a result, older persons must have lower incomes than younger persons to be considered ''poor" by the federal government.
In 1994, 2.5 percent of elderly persons had incomes under 50 percent of the federal poverty level, 11.7 percent had incomes below 100 percent of the federal poverty level, and almost 18.7 percent had incomes below 125 percent of the federal poverty
TABLE G-2 Income of Persons Covered by Medicare in 1993
|
Family Income in Thousands ($) |
Age 0-64, % |
Age =65, % |
Total, % |
|
0-10 |
30.4 |
20.2 |
21.3 |
|
10-20 |
25.2 |
30.1 |
29.5 |
|
20-30 |
17.4 |
19.2 |
19.0 |
|
30-50 |
15.9 |
17.9 |
17.7 |
|
50-75 |
7.5 |
7.6 |
7.6 |
|
75-100 |
2.3 |
2.5 |
2.5 |
|
>100 |
1.3 |
2.5 |
2.4 |
|
Total |
100.0 |
100.0 |
100.0 |
|
SOURCE: The Public Policy Institute/AARP. Compiled from Current Population Surveys, March Supplement, 1994, Bureau of the Census. |
|||
TABLE G-3 Threshold Income for Federal Poverty Level, 1994
|
|
Elderly |
Nonelderly |
|
Single |
$7,108 |
$7,718 |
|
Couple |
$9,976 |
$8,967 |
|
SOURCE: The Public Policy Institute/American Association of Retired Persons, 1995, Current Population Survey Data. |
||
level (The Public Policy Institute/American Association of Retired Persons, 1995).
Social Security accounts for half or more of annual income for approximately 60 percent of elderly persons. Thirty-two percent of older persons rely on Social Security for 80 percent of their incomes (Health Care Financing Administration, 1995).
Medicaid
The Medicaid program assists low-income Medicare beneficiaries with premiums, deductibles, and Medicare cost-sharing requirements under the Qualified Medicare Beneficiary program. For those who are eligible, it also covers benefits not covered by Medicare, such as prescription drugs and long-term care. Less than one third of poor elderly persons are Medicaid beneficiaries, and less than 10 percent of elderly people with incomes between 100 and 200 percent of the federal poverty level are covered under Medicaid. In 1995, nearly 5 million Medicare beneficiaries received some assistance from Medicaid (Health Care Financing Administration, 1995). Although only 12 percent of Medicaid beneficiaries are elderly, 28 percent of Medicaid program expenditures are made on behalf of this population; three quarters of this spending goes for long-term care services (The Kaiser Commission on the Future of Medicaid, 1995).
Out-of-Pocket Expenditures
Out-of-pocket health costs represent a substantial burden for older Americans. This is especially true for those with lower incomes. Low-income beneficiaries pay a larger share of their incomes for out-of-pocket costs than those with higher incomes. Furthermore, the oldest old pay even larger out-of-pocket costs than their younger elderly counterparts. Compared with younger persons, the elderly spend nearly four times more out-of-pocket for health costs than those under 65 years of age ($2,519 versus $668) (American Association of Retired Persons, The Urban Institute, 1995).
Experiences of Vulnerable Individuals in Managed Care
In its report, Access to Health Care in America, the Institute of Medicine asserted that regular care is necessary for those with chronic conditions to improve functioning and minimize discomfort. Although regular care does not always prevent adverse consequences of chronic conditions, the absence of such care is associated with more negative outcomes for individuals (Millman, 1993). For those who are sick, poor, or disabled, special attention must be paid to ensure that such vulnerable persons actually have access to and receive regular care.
The different incentives that exist in managed care and fee-for-service care have important implications for beneficiaries in terms of access, use of services, and health outcomes. Clement and colleagues (1994, p. 1492) have written that "whether . . . reductions in services (that managed care plans achieve) are due to a more judicious use of services, rather than limiting beneficial care, remains uncertain." Schlesinger and Mechanic (1993, p. 129) note that "because norms of appropriate treatment are ill-defined for many chronic conditions, it is difficult to determine if reduced spending or shifts in the nature of service have led to poorer outcomes."
Most managed care plans have had little experience treating older, sicker, or disabled patients (Armstead et al., 1995; Tanenbaum and Hurley, 1995). Although some analysts believe
that managed care can well serve the majority of the population, such plans may not be suitable for those who make heavier use of the health care system. There is also evidence that elderly persons and those who are disabled are apprehensive about changes that will "force" them into managed care plans. In focus groups conducted in 1995, the greatest concerns expressed by seniors who were not enrollees in managed care plans were the restrictions on physician choice and the perceived lower quality of care in HMOs (Frederick/Schneiders, Inc., 1995).
Advocates for those with chronic illnesses are concerned as well about managed care. "The fear among . . . patients, their families, and advocates is that managed care organizations—prepaid health plans that share the risk of losing money on services-are too inexperienced, too inflexible, and too profit-oriented to meet their special needs" (Families USA Foundation, 1995, p. 1). Others express concerns about the financial incentives in managed care. "Many mental health advocates, who believe that the financial incentives inherent in HMOs, as well as HMOs' lack of experience in providing services to seriously mentally ill individuals, could lead to ineffective or inappropriate care, and a deterioration in the mental health status of these persons" (Christianson and Osher, 1994, p. 899). Still others recognize that although "managed care itself is not the enemy," . . . there are plans that "cut costs by recruiting the healthiest patients, rationing care by making it inconvenient to obtain, and denying care by a variety of mechanisms" (Kassirer, 1995, p. 50). Patients with chronic illness have ''ongoing, often complex and expensive health care needs [that] make them unattractive in a capitated environment" (Safran et al., 1994, p. 1579). These kinds of concerns are raised often and must be taken seriously. The research evidence is limited because managed care has not been the major health delivery system for vulnerable populations. Furthermore, the industry is changing rapidly. Thus, what is known about one particular model may not necessarily apply to the newer managed care entrants. Nevertheless, some of the research evidence may be helpful in predicting how vulnerable populations will experience managed care.
Health Outcomes
In general, HMOs save money by reducing the use and intensity of services. A comprehensive examination of the Medicare HMO risk program conducted by Mathematica Policy Research, Inc., found that Medicare risk plans may spend about 10.5 percent less than the Health Care Financing Administration (HCFA) would have spent for the provision of all medical services in the fee-for-service sector.2 These savings result from the reduction of the number of hospital days and the average length of stay, but not hospital admissions. Furthermore, enrollment in HMOs increased the likelihood that beneficiaries will receive some services (e.g., physical examinations and skilled nursing facility care), but reduced their intensity or frequency (e.g., skilled nursing facility stays rather than rehabilitation hospital stays and fewer home health visits). Finally, HMOs increased the use of some services for members who were in the poorest health but reduced the intensity of services more for this group than for other enrollees. The Mathematica study found that, compared with fee-for-service plans, HMOs produced similar outcomes for inpatient and ambulatory care (Brown et al., 1993).
Other researchers have studied whether the conclusions from the Medicare Competition Demonstrations apply to the ongoing Medicare Managed Risk Program. Clement and colleagues (1994) compared Medicare beneficiaries in risk HMOs with two symptoms, chest pain and joint pain, with their fee-for-service plan counterparts to determine differences in access to care and medical outcomes. The authors reported three consistent findings: (1) For both conditions, HMO enrollees were less likely to report that they had seen a specialist than those in fee-for-service plans. (2) HMO enrollees were less likely to have reported that follow-up care had been recommended. (3) Despite these differences, outcomes were similar for HMO and fee-for-
service enrollees in three of four outcomes measures. Only among HMO patients was there less symptomatic improvement of joint pain. The authors observe that "less intensive HMO care may have led to less satisfactory outcomes for some patients" (Clement et al., 1994, p. 1491). The fact that HMO enrollees experienced less relief from joint pain is a concern, because arthritis is a chronic condition commonly found among elderly persons and, in the view of Clement et al., "should have been better ameliorated." Clement has suggested that failure of HMO patients to have experienced improvement similar to those in fee-for-service plans could reflect an overall lack of knowledge about the management of chronic illnesses in the elderly (Winslow, 1994).
Additionally, Clement and colleagues (1994) observe that the reduced likelihood of referral to specialists "warrants consideration." This is an important issue for individuals with chronic conditions, many of whom rely on the care of specialists for treatment. However, Clement and colleagues acknowledge that "for most symptoms and illnesses the appropriate rate of specialty referrals, as with other resource-intensive practice styles, is unknown" (Clement et al., 1994, p. 1491).
A recent study provides another perspective on the use of specialty physicians and practice site. No "meaningful differences" were found among nonelderly patients with either hypertension or non-insulin-dependent diabetes who received care from either generalist or specialist physicians in an HMO, individual practice association (IPA), or fee-for-service setting (Greenfield et al., 1995). The authors concluded that (with respect to physiologic, functional, and mortality outcomes measures) there was "no evidence that any one system of care or physician specialty achieved consistently better 2-year or 4-year outcomes than others" (p. 1436) for the conditions studied.
Carlisle and colleagues (1992) compared elderly HMO and fee-for-service patients who had been hospitalized with acute myocardial infarction to evaluate the quality of care for this condition provided to Medicare beneficiaries. The study showed no significant mortality differences between HMO members and fee-for-service beneficiaries, although HMO compliance with process criteria was greater in three of five outcomes measures (Carlisle et al., 1992).
A randomized trial of elderly Medicaid beneficiaries found that enrollment in prepaid plans had no adverse effect on poor, elderly Medicaid beneficiaries during the year that the patients were evaluated. Although the enrollees in prepaid plans used significantly less care, there was no indication that they experienced poorer health as a result (Lurie et al., 1994).
Although the studies noted above are examples of evidence that HMOs have satisfactorily treated older or chronically ill patients, there is also evidence in the research literature that finds this model wanting with respect to vulnerable populations. The following describes several studies that point up concerns.
Safran and colleagues (1994) compared staff/group model HMOs, IPAs, and traditional fee-for-service plans to determine the extent to which each of five core dimensions of high-quality primary care (accessibility, continuity, comprehensiveness, coordination, and accountability) were received by chronically ill patients3 The results showed that neither prepaid systems nor fee-for-service plans provide primary care optimally. The prepaid plans (HMOs and IPAs) provided increased financial access and coordination and "reduced patient-physician continuity and comprehensiveness of care and, in many cases,… diminished organizational access and interpersonal treatment" (p. 1583).
The authors examined access from two perspectives, financial and organizational. Financial access was a greater barrier in fee-for-service plans because of requirements for higher out-of-pocket costs. However, organizational barriers were greater in some, although not all, HMOs studied. In the cases in which organizational access was a barrier, patients reported difficulties in receiving medical care on short notice and longer waits for emergency treatment. The authors observed that organizational barriers to access are disruptive to the continuity of care (which might be of particular significance to those with chronic
conditions). With respect to continuity, the results showed some overlap on scores on the high end among the three types of plans studied, but showed that the prepaid plans produced a range of scores that extended much lower than those for the fee-for-service plans. The lower comprehensiveness of care4 score for HMOs may reflect "organizational access barriers and/or HMO referral practices" (p. 1584). The authors suggest that HMO patients may opt to see other providers rather than wait to see their own providers. Also, HMOs rely on primary care providers more than IPAs or fee-for-service plans do. Thus, in that study HMO patients were less likely than their IPA and fee-for-service counterparts to see a specialist for primary care. (Less than 5 percent of HMO patients received primary care from a specialist.5
Shaughnessy and colleagues (1994) found most home health care outcomes in fee-for-service plans to be better than those in HMOs. (There were no differences in outcomes for wound patients and patients receiving intravenous therapy.) Schlenker (forthcoming) found that HMO home health care costs are "significantly lower" than those in fee-for-service plans, even after controlling for case mix, demographic characteristics, region, and agency factors. Despite reduced expenditures for home health care, HMOs did not substitute other services for home health care services. Shaughnessy and colleagues (1994) observed that "relative to the fee-for-service sector, it appears that HMOs tend to approach some aspects of home health care with more of a 'maintenance' philosophy than a rehabilitative or restorative philosophy" (p. 219). If true, this would have enormous implications for the vulnerable populations under discussion here, whose very quality of life could depend on achieving or maintaining maximum function. Shaughnessy and colleagues noted that the findings were most pronounced among HMO patients whose care was contracted out to home health agencies. Thus, the ways in which managed care plans organize the provi-
sion of services has implications for patient care as well. Shaughnessy and colleagues further observed that the HMOs may not be aware of the "potential value of home health care in terms of service integration, patient preference, quality of life, and patient benefits in terms of functioning" (p. 219). These conclusions should be of particular concern to Medicare beneficiaries because "home health care has provided a 'safety net' for major reductions in institutional care. . . . In fact, reductions in home care are likely to lead to increased uses of and expenditures for other services" (Schlenker, forthcoming, p. ii).
Outcome studies of HMO patients with serious mental illness show conflicting findings (Christianson and Osher, 1994). In a literature review of studies of patients with severe mental illness, Christianson and Osher cited the RAND medical outcomes study that reported no significant difference in the recognition and treatment of depression by psychiatrists in HMOs, group practice, and solo practice settings. However, HMO patients "receive a less intensive style of care than comparable persons under fee-for-service coverage." Still citing the RAND study, Christianson and Osher noted that HMO patients were less than half as likely as fee-for-service patients to be seen by a psychiatrist. The RAND study indicated that there is some evidence that among patients of psychiatrists, some HMO members with depression experience worse outcomes than those in fee-for-service plans (Rogers et al., 1993). However, depressed patients of general clinicians or nonphysician mental health specialists showed no differences in clinical or functioning outcomes by type of payment. Lurie and colleagues (1992) conducted a randomized controlled trial to determine the effect of type of payment on the health outcomes of Medicaid enrollees with chronic mental illness and found that there were no significant differences between prepaid and fee-for-service patients, at least in the short run.
The RAND Health Insurance Experiment examining the health outcomes of individuals randomly assigned to HMOs and fee-for-service plans concluded that there were different effects for high- and low-income HMO enrollees who entered the experiment with health problems (Ware et al., 1986). Compared with their fee-for-service counterparts, HMO enrollees with high incomes showed "significant improvement," while low-income
sick HMO enrollees reported "significantly more bed-days per year due to poor health and more serious symptoms" than those in fee-for-service plans. The authors observed that the "results suggest that high and low-income groups may realize different benefits from prepaid group practice and fee-for-service" (p. 1021).6
Patient Satisfaction
In general, surveys of the satisfaction of HMO members indicate that they are more satisfied with the out-of-pocket cost of care and the reduced paperwork burden in managed care than those in fee-for-service but that they are less satisfied with access to care, including availability of specialist referrals and restrictions on the choice of physicians. These findings are consistent across several surveys (e.g., Clement et al., 1992; The Commonwealth Fund, 1995; U.S. Department of Health and Human Services, 1995c). A 1994 study of Medicare HMO enrollees found that 84 percent remained in the same plan, 6 percent switched to another HMO in their area, 6 percent disenrolled for reasons unrelated to the plan, and 4 percent returned to fee-for-service plans (Group Health Association of America, 1995c).
A recent survey of enrollees in managed care plans found that nonelderly sick enrollees reported more problems getting the health services that they or their providers believed that they needed and more difficulty getting to see specialists than those in fee-for-service plans (The Robert Wood Johnson Foundation, 1995). Compared with sick or disabled patients in fee-for-service plans, enrollees in managed care plans also reported that they waited longer for appointments, that managed care physicians failed to explain what they were doing during visits,
and that the medical care that they provided was not correct or appropriate. Sicker HMO members also complained about specialist care. Compared with fee-for-service patients, more managed care enrollees thought that specialist care was incorrect or inappropriate, the examination that they received was not thorough, and that the time that the physician spent with them was inadequate. The sick or disabled managed care enrollees also reported lower out-of-pocket costs than their fee-for-service counterparts.
Disenrollment
The findings from disenrollment studies are also instructive. In 1993, although the majority of Medicare beneficiaries surveyed by the Office of the Inspector General (OIG) of the U.S. Department of Health and Human Services reported they received the services they needed, 20 to 25 percent of those who disenrolled claimed that they failed to receive primary care, referrals to specialists, and HMO coverage of emergency care (U.S. Department of Health and Human Services, 1995c). Another OIG report indicated that among HMOs with higher disenrollment rates, more enrollees reported service access problems (U.S. Department of Health and Human Services, 1995b). Disenrollees rated their health status lower than enrollees rated their health status and reported a greater decline in health status during their HMO enrollment. Disenrollees who were disabled or who had ESRD reported difficulty getting access to care more often than beneficiaries over the age of 65 did. HMOs with more experience in the Medicare risk HMO program showed the largest decreases in their disenrollment rates over time.
Other studies of disenrollment from Medicare HMOs have found that disenrollees "have characteristics usually associated with high use of services" (Porell et al., 1992). They were poorer, more likely to be disabled, and more likely to report a problem requiring hospitalization. However, an earlier look at disenrollment in the Medicare Competition Demonstrations found that, "among the variables that indicate an association between health status and disenrollment, only the amount of Part B Medicare expenditures prior to joining the HMO ap-
proached a level of significance that indicated a relationship may exist" (Langwell and Hadley, 1989, p. 71). Also looking at the Medicare Competition Demonstrations, Retchin and associates concluded that "although disenrollees were more likely to experience functional declines (in one or more ADLs), at follow-up, these declines were of marginal statistical significance and most likely due to baseline differences" (Retchin et al., 1992, p. 665).
Service Delivery
Several years ago, Fox and colleagues (1991) recognized that there was a dearth of research about the delivery of services to older persons in managed care. They and others have proposed research agendas to fill this gap (e.g., Davis et al., 1994; Lewin/ICF, 1990). Although interest in managed care research has grown considerably, results and conclusions remain sparse. Managed care is still evolving. Without firm and consistent evidence, it would be premature to make judgments about the effectiveness of current practices. The term "best practices" should be reserved for those that have been tested and evaluated on the basis of the quality and cost-effectiveness of the care provided.
Nevertheless, many managed care plans are actively involved in demonstrating different approaches to the provision of care of their vulnerable populations (see, e.g., Group Health Association of America, 1995a; Health Care Financing Administration, Division of Policy and Evaluation, Office of Managed Care, 1994). These might be called "promising interventions" or "models of care" (Teresa Fama, Deputy Director, Chronic Care Program, Washington, D.C., personal communication, November 1995). As Medicare enrollment continues to increase, plans that have heretofore had few older, disabled, or chronically ill members will be confronted with the greater diversity of needs of such individuals. Undoubtedly, they will look to current practices, as well as experiment with other interventions to care for their Medicare enrollees.
Pawlson (1994) has suggested that the "acute disease paradigm" (an isolated event with a single, proximate cause) that has been the hallmark of the U.S. health care system is no
longer appropriate for large numbers of the population. Instead, a "chronic complex illness model" that involves a broader range of variables appears more suitable in treating and assessing the quality of care for chronic illnesses. "The aim of therapy must be multi-faceted, . . . modifying the rate of change of declining physiologic functions and concomitant functional impairments as well as addressing psychologic and social adjustment to illness" (Pawlson, 1994, p. 37). Quality measurement should include the patient's assessment of his or her illness and how well different aspects of treatment (e.g., pain amelioration) have been addressed.
It would seem that managed care plans are logical settings for the implementation of "population-based medicine," "a strategy for designing and implementing an organized approach to providing for the care of clinical problems, particularly chronic problems, through the application of epidemiologic principles and data" (Voelker, 1994; Wagner et al., 1995a, p. 12). For example, using computer algorithms, Group Health Cooperative of Puget Sound identifies enrollees by such characteristics as age, sex, health status, health complaints, and disease diagnoses. Once subgroups have been identified, specific services and programs can be developed for them. By differentiating the clinical needs of subsets of the health plan's population, more effective planning can ensure that the unique needs of these groups are met and that optimum outcomes are achieved.
The HMO Group Geriatric Interest Group (consisting of representatives from The HMO Group and Kaiser Permanente) has identified the essential features of caring for elderly patients. These include "unanimous agreement from provider and administrative staff that the elderly present unique issues and challenges; emphasis on independence, quality of life issues, and prevention of acute illness; support systems and resources for providers who care for elderly patients; a targeting mechanism for early identification of health and related problems; a good information system; ongoing collaborative efforts with organizations and universities specializing in geriatric efforts; and ability to maximally utilize community resources" (Wagner, 1993, p. 133).
Use of Geriatricians
Friedman and Kane (1993) studied the use of geriatricians by Medicare risk contractors. As of June 1991, 53 percent of the HMOs studied had one or more geriatricians. In 76 percent of the plans with such physicians, geriatricians provided primary care; they served as consultants in 61 percent of the plans. Friedman and Kane concluded that ''geriatricians and many of the elements of organized geriatric practice are used [in HMOs] to a much lesser extent than experts recommend" (Friedman and Kane, 1993, p. 1144).
However, on the basis of randomized trial in an HMO, Epstein and colleagues (1990) recommended that "if geriatric assessment is to be used effectively in the ambulatory setting, tight targeting of the most severely ill or medically unstable patients may be necessary" (p. 543). Their study found that consultative geriatric assessment that involves only limited follow-up was not of benefit to most older, ambulatory enrollees in HMOs.
Practices of Some Medicare Managed Risk Program HMOs
Kramer and associates (1992) have described the geriatric care provided by group/staff model Medicare HMOs. On the basis of their visits to seven HMOs, they identified six strategies employed by these programs: (1) identifying high-risk patients, (2) assessing multiproblem patients, (3) treating multiproblem patients, (4) rehabilitating patients after acute medical events, (5) reducing medication problems, and (6) providing long-term and home health care. The authors noted that these strategies were often linked. For example, the presence of a system to identify high-risk patients usually indicated the use of an assessment tool as well.
Several of the HMOs screened or were planning to screen new enrollees to (1) determine patient status in areas such as functional disability, medication use, cognitive status, incontinence, and home safety or (2) to identify high-risk patients. In some plans, geriatricians provided referral guidelines to primary care physicians to help identify patients who would ben-
efit from geriatric assessment. Once identified, patients were referred to multidisciplinary assessment teams or were provided with appointments or the screening information was forwarded to the primary care physician. Kramer and colleagues (1992) noted that geriatricians or those who had specialized training in geriatrics participated in most of the assessment programs.
Typically, the geriatric assessments included functional evaluation, mental status testing, medications review, a depression test, and a review of the member's social and home environment. Follow-up to the assessment varied by plan. In some cases, the assessment team was authorized to make the necessary changes in the patient's regimen; in others, the assessment team referred the patient back to his or her primary care physician.
There are those practicing in HMOs who suggest that a "geriatric focus" should include an interdisciplinary approach to coordinate multiple support and medical services (Calkins et al., 1995). However, Calkins and colleagues also note that plans need more information to implement this approach. Several of the plans studied by Kramer and associates (1992) coordinated the treatment of patients presenting several problems by integrating the activities of health providers with different specialties, sometimes at one site. Thus, for example, FHP integrated the care for such patients at particular sites, where physicians had smaller panels and were able to have longer visits with their geriatric patients.
Other methods observed on the site visits by Kramer and associates (1992) were the use of skilled nursing facilities for intensive rehabilitation and post-acute-care, programs to profile medication use, and expanded coordination with social service providers. Widespread use of geriatric nurse specialists was also observed among the plans visited.
Primary Care Model for Chronic Care Illness
In considering a basic care model for chronically ill patients, Wagner and colleagues (1995b) have identified current deficiencies in the care of chronic illness: irregular or incomplete assessments, inadequate or inconsistent patient education, unintended deviations from accepted guidelines, and patient dissatisfaction
because of inadequate information and psychosocial support. Wagner and associates have reported "real uncertainty as to whether to build integrated systems based in and supportive of primary care, . . . or to develop highly focused, specialized 'carve out' systems for various patient groups" (Wagner et al., 1995a, p. 27).
Group Health Cooperative of Puget Sound's Center for Health Studies has received funding from the Chronic Care Initiatives in HMOs to evaluate the primary care approach. The project will incorporate the elements that appear to be associated with good outcomes in chronic care illness: "systematic assessments, preventive interventions, effective education, psychosocial support, and consistent follow-up" (Chronic Care Initiatives in HMOs, undated; Wagner et al., 1995a). Frail elderly patients or patients with diabetes will be identified through disease registries to attend a chronic care clinic periodically. These patients will be followed by midlevel providers who will monitor patient compliance with a prescribed care plan and schedule follow-up visits. Care will be provided through existing primary care practices that will receive organizational support from the health plan. This support will include the development and dissemination of guidelines and information about treatments and services that have been shown to improve outcomes in the target populations, provider training, and so forth. Blocks of practice time will be devoted to the target population, periodically but regularly. At each miniclinic session: "planned assessments, visits, and a group meeting; standardized assessment of clinical and health status; development and execution of care plans constructed mutually with patients incorporating practice guidelines and reminders; continuous individual patient education; opportunities for group support; and systematic follow-up" are envisioned (Wagner et al., 1995a, p. 17).
Cooperative Health Care Clinic
The Kaiser Foundation Health Plan of Colorado has developed the Cooperative Health Care Clinic. This project is intended to integrate solutions to the physical, physiologic, and environmental problems of elderly patients with cardiovascular disease, lung disease, diabetes, or degenerative joint disease
(Chronic Care Initiatives in HMOs, undated; Scott and Robertson, 1995). The objective is to reduce the cost of care for these patients and to improve health status "through better preventive medicine, maintenance of independent living and improvement in access to care" (Scott and Robertson, p. 1) and improved patient and provider satisfaction. The model uses a multidisciplinary team that meets with groups of 12 to 30 patients every 4 to 6 weeks. The session provides "medical and functional assessment, group education, coordination of services between primary care and other health professionals, and an opportunity for the group to socialize with each other" (Group Health Association of America, 1995a; Scott and Robertson, 1995, p. 1).
Integration of Acute and Long-Term-Care Services
Patients needing chronic care services require a full range of treatment modalities that often span areas covered by acute and long-term-care insurance coverage. There have been several demonstrations to integrate acute and long-term-care services, most notably the Program of All-Inclusive Care for the Elderly (PACE)/On Lok projects and the Social Health Maintenance Organizations. These programs have tried to improve coordination by bridging through common financing, acute-care benefits, and home and community-based long-term-care services.
The On Lok Senior Health Services was initially developed in 1971 as an adult day health center. It later received Section 1115 waivers that enabled it to receive capitation payments to provide comprehensive medical and social service benefits (e.g., primary medical and nursing care, day health, hospitalization, transportation, meals, and in-home services) through multidisciplinary teams to a nursing home-certified population. On Lok has since been replicated throughout the country through PACE. In general, although members of the On Lok/PACE projects have severe impairments, they are not as dependent in activities in daily living as nursing home residents (Weiner and Skaggs, 1995).
The Fallon Healthcare System is the first HMO to establish a PACE site, the Elder Service Plan (ESP) (Group Health Asso-
ciation of America, 1995a). Designed to enable frail elderly persons to remain in their homes, ESP focuses on preventive and rehabilitative services that permit enrollees to maintain maximum independence. It provides a full range of services, including physician and nursing services, home care, meals, recreational therapy, and transportation to and from the ESP center.
Even in the absence of full financial integration of coverage for acute and long-term care, some plans permit case managers to authorize services outside the covered range of benefits, thereby increasing the plan's ability to be responsive to the unique needs of individuals and, at the same time, saving through more efficient use of plan resources (Fama and Fox, 1995). Those authors noted that case management is being used to shorten hospital utilization by reducing the length of stay for acute episodes of chronic conditions and assisting patients in returning home instead of entering skilled nursing or long-term-care facilities. They point to Family HealthCare Services (a subsidiary of Sierra Health Services, which provides all post-acute and long-term-care services to Sierra Health Services enrollees), whose case management approach is to "maintain enrollees in the least restrictive and most safe and cost-effective setting. . . . Case managers consider the whole range of alternative care settings and services-from skilled nursing facilities to group homes and from skilled nursing services to home maker services" (Fama and Fox, 1995).
SeniorCare Options Program
The SeniorCare Options Program is sponsored by Allina Health Plans Group. Operating under the flexible benefits option of HCFA's Medicare Managed Risk Program, SeniorCare Options is a Medicare risk plan that offers Medicare beneficiaries "open access" to approximately 6,500 providers, including primary care and specialists. For a slightly higher premium, enrollees may self-refer directly to specialists. Upon enrollment, each new beneficiary is assigned a care advisor (either a geriatric nurse or a social worker) who assists the enrollee in navigating through the health plan. The care advisor performs a case management function and identifies low-, moderate-, and
high-risk beneficiaries when they enter the plan by means of a health assessment tool that was developed with assistance from geriatricians at the University of Minnesota. Depending on the level of need, enrollees receive more or less intensive follow-up. A care plan is developed for individuals with multiple problems, that is reevaluated regularly (Olivia Mastry, Director, Center for Healthy Aging, Medica Health Plans, Minneapolis, Minnesota, December 1995).
Case Management
The Chronic Care Initiatives in HMOs studied the use of case management in 18 HMO Medicare risk contractors having more than 20,000 members and five other plans that did not meet this enrollment criterion. They concluded that "case management is currently being performed based on managerial judgment rather than on research findings" (Pacala et al., 1994, p. 2). According to that report, case management (including screening, assessment, care planning, the execution of a case management plan, and monitoring) is widely used in HMOs to treat older patients, but the plans do not carry out this function consistently. Nevertheless, the plans surveyed apparently are committed to using case management, and most reported that they are planning to expand its use. Most case management occurs in the hospital setting, and most patients are referred by providers for case management even if other screening mechanisms are in place.
All HMOs in the study were found to screen enrollees for case management, although they used different screening criteria. The criteria used most often were based on diagnoses (most commonly, congestive heart failure, chronic obstructive pulmonary disease, diabetes, stroke, and cancer), high use or cost, site of care (most often, hospitals), functional limitation, age, and living circumstance. One third of the plans used surveys to identify enrollees who met the targeting criteria. However, as noted above, most of those receiving case management were referred by providers.
Once identified, 80 percent of the plans conducted some form of assessment, and virtually all of those assessed were accepted for case management. Thirteen percent of the plans used a
comprehensive geriatric assessment that was performed by a geriatrician and a multidisciplinary team. Most of the HMOs developed care plans, and most did so through multidisciplinary teams. However, in some cases, a case manager arranged care without a care plan and without consulting the enrollee or the provider. The plans reviewed cases at various intervals, depending on the site of the case management program.
Pacala and colleagues (1994) developed a typology to describe the case management activities of the HMOs studied. They found that the programs fell along a continuum based on the intensity of contact with the patient. At the highest levels of intensity, case management resembled the activity in social health maintenance organizations, whereas at the lowest intensity, it resembled "an elaborate utilization review model" (Pacala, undated, p. 21).
Protecting the Public Interest
Even without the impetus of federal legislation, managed care in the Medicare program will continue to grow. To protect beneficiaries, HCFA has a fiduciary responsibility to hold its managed care contractors publicly accountable for the cost and quality of care that they provide. As the nation's largest purchaser of managed health care, HCFA has acknowledged that "it is not just like any private sector purchaser"—it must hold its contractors to "a higher standard" (Vladeck, 1995, p. 2). Accordingly, careful and comprehensive oversight coupled with consumer protections are critical to ensuring that the services provided are accessible and meet quality standards. To be effective, HCFA must take several steps.
National, Uniform Standards
National, uniform standards must apply to the plans that Medicare offers to beneficiaries. At a minimum, these standards should address fiscal solvency, access and availability of services, quality of care, marketing and enrollment practices, physician credentialing, utilization review, data collection, and grievance and appeals processes. HCFA needs such standards
to monitor contractor performance and to serve as a basis for its enforcement and sanction activities.
Useful, Reliable Information
As Medicare expands the choice of plans available to beneficiaries, the importance of useful, reliable information about the availability, quality, and outcomes of services will grow. If consumers are given choices, they must be given the tools to exercise informed choice. Because there is evidence that consumers are most interested in receiving information from people like themselves, patient-reported information will play an important role for vulnerable populations, especially as better methods are developed to survey and report specific information about subpopulation groups.
The methods used to collect the data that are then reported to consumers are also important. Information should be collected in a manner that will ensure comparability across health plans. Consumer satisfaction data should be standardized and collected and audited by an external entity. Consumers may be legitimately wary of data that have been collected by the plans themselves. Research is needed to learn more about the kinds of information that different consumers will find useful and the best ways to disseminate such information. It is necessary, however, to begin at once with the best information that is currently available. Different dissemination strategies should be used to ensure that all segments of the beneficiary population will find the information understandable.
Quality Assurance and Improvement and External Quality Review
Some aspects of health care delivery cannot be ensured adequately through information alone. Managed care plans must demonstrate and document the ongoing effectiveness of their internal quality review processes through performance measurements and external reviews. New performance measurement systems should include measures of access to and timeliness of care, the appropriateness of the setting and treatment, and premature hospital discharges. For the chronically ill, it is particu-
larly important to track the continuity of care across multiple settings, including home health and other long-term-care settings, and to assess the interpersonal aspects of care, such as patient-physician communication.
Managed care plans must also be subject to the ongoing review of professional external quality review and improvement organizations. There are those who would substitute accreditation for external review (Balanced Budget Act of 1995). Indeed, many private purchasers rely solely on accreditation as a means of distinguishing among managed care plans. However, the fact that a plan is accredited merely is an indication that it has the systems in place to produce high-quality care. This represents just a point-in-time description of the plan's capabilities. Beneficiaries need assurances not only that systems are in place but also that there are processes to determine whether the structures and systems are actually working in practice. Therefore, there is a need for ongoing external quality review to detect problems that may not be revealed through an accrediting process.
Grievance and Appeals
Inevitably, in a system that restricts choice and limits care to "medically necessary services," there will be disagreements between the health plan and its enrollees. A critical beneficiary protection is a grievance and appeals process that enables enrollees to receive timely and clear information about the specific reasons for denials of a service or payment and the right to appeal a denial. For vulnerable populations, it is especially important that the methods of communicating information about the grievance and appeals process be tailored to meet their specific needs.
Beneficiaries must retain the right to a review by an independent decision maker outside of the managed care plan, using medical expertise when appropriate, and then access to the federal courts. Of critical importance to vulnerable populations is an expedited review process that includes specific deadlines for situations in which failure to receive care or referral for specialized treatment promptly could jeopardize the patient's health or preclude optimal outcomes. These protections are so essential
to beneficiaries that a plan's failure to comply with requirements, including rules that pertain to timeliness, should result in automatic approval of the disputed service or claim.
Conclusion
For the employed population under age 65, the U.S. health care system has shifted to managed care. As this trend continues, it is possible to contemplate the disappearance of "pure" fee-for-service plans in the private sector. However, in the Medicare program, 90 percent of beneficiaries still receive their care through traditional fee-for-service arrangements. Although this may change over time, it is not yet certain whether enrollment in managed care plans among older Americans will reach the same level as that among individuals in the private sector. There is no indication that HMOs will cease to attract younger and healthier Medicare beneficiaries. The question is whether the more vulnerable beneficiaries will also voluntarily enroll.
There are those who believe that current efforts to expand managed care in the Medicare program may in the end result in reduced rather than enhanced choices for beneficiaries, especially for those who are poorer or sicker. "One should not underestimate the importance of changes in Medicare's fee-for-service reimbursement policy for the prospects of managed care. The major revolution in commercial managed care has been driven largely by pricing and restrictions on choice of indemnity coverage, not simply the availability of managed care alternatives" (Lawlor, 1995, p. 16). If only the very sick remain in the traditional program, causing the Medicare fee-for-service risk pool to deteriorate and eventually become economically unsustainable, the cost of fee-for-service care could become so expensive that only those with high incomes will be able to choose this option. Then, the genuine choice between fee-for-service and managed care plans would disappear. If this becomes the case, many Medicare beneficiaries could find themselves in managed care plans whether they want to be in them or not.
Those who do enroll in managed care plans are entitled to do so with the confidence that their health and related needs will be met by these plans—that is, that services will be available,
accessible, and affordable. Today, would such confidence be justified?
Medicare beneficiaries are substantially different from those who have typically enrolled in managed care organizations. Several of the researchers whose works were cited in this paper observed indications that the plans studied lacked experience dealing with particular types of chronically ill patients or did not understand the importance of certain treatment modalities that are of importance to those with chronic care needs (e.g., Clement et al., 1994; Shaughnessy at al., 1994). Furthermore, the research evidence is inconclusive. Some studies indicate that older individuals and/or those with chronic conditions have fared well, whereas others indicate that the experiences of older, sicker populations have been less than satisfactory. Moreover, the studies that have been conducted have been hampered by the absence of well-defined norms to adequately evaluate plan performance, particularly in the treatment of chronic conditions. It would be imprudent to generalize from the findings because the reported results may have been peculiar to the model type of the plans investigated, the payment arrangements, or the particular market in which the plans were situated. Clearly, a great deal of research is needed before it will be possible to make unequivocal statements, in either direction, about the experiences of vulnerable populations in managed care plans.
Regrettably, waiting for research results will not be an option for today's beneficiaries. The U.S. Congress is poised to expand managed care and other options in Medicare in the short term. At the same time, Congress is also intent on achieving ''savings" from the Medicare program. These savings will be realized in both the traditional and managed care programs. Unfortunately, the present payment methodology used to reimburse HMOs is widely recognized as flawed (U.S. General Accounting Office, 1995b). The adjusted average per capita cost methodology does not contain an adequate risk adjuster, thereby giving plans an incentive to "cherry pick" the healthiest risks. The U.S. General Accounting Office (GAO) has identified several promising efforts in the area of risk adjustment but predicts that an effective risk adjuster is not likely to be available in the near future (U.S. General Accounting Office, 1994). This
means that plans will not be properly compensated for their vulnerable members, encouraging them either to avoid enrolling high-cost, high-risk individuals or to refrain from serving such members adequately, if they do enroll. The absence of an adequate risk adjuster underscores the importance of oversight on the part of HCFA to ensure that financial incentives that do not interfere with the provision of appropriate care and to help minimize any perverse incentives the reimbursement methodology might permit. A standardized benefit package would also help to mitigate risk selection.
Although many factors may influence physician decision making (e.g., the plan's quality assurance system, the physician's personal ethics, malpractice concerns, and the desire to retain patients [Gold and Reeves, 1987]), recently, the role of financial incentives on physician behavior has been receiving widespread coverage in the media. Several years ago, GAO recognized that, in the absence of proper controls, incentive payments to physicians had the potential to have a negative impact on the quality of care provided to Medicare beneficiaries. At that time, GAO suggested that "the closer financial incentives are linked to decisions about individual patients, the greater the potential threat to quality of care" (U.S. General Accounting Office, 1988). GAO identified four features that were most likely to affect quality adversely: shifting HMO risk to physicians by holding physicians responsible for the cost of all services, distributing incentives on the basis of individual physician cost performance, paying a percentage of HMO savings on patients as incentives, and measuring physician cost performance over a short period of time. It is disturbing that these practices are still commonly found in physician incentive programs of managed care plans.
Many are advocating for the disclosure of the financial incentives used by managed care plans. Although this is a start, it is doubtful that most consumers will comprehend the complex arrangements in use. To avoid the possibility of financial incentives interfering with the quality of services provided, HCFA must identify and ban practices that can be detrimental to patients.
In spite of these reservations, it must be said that managed
care does have great potential to serve vulnerable beneficiaries. Managed care plans can provide more effective management, coordinate multiple medical and social problems, and exercise greater flexibility to provide the care that beneficiaries might require (Fama and Fox, 1995; Retchin et al., 1992; Tanenbaum and Hurley, 1995). However, as Schlesinger and Mechanic (1993) have noted, "the capacity of a prepaid plan to provide appropriate treatment to enrollees with persistent and severe illness depends to a considerable extent on the way the plan is organized" (p. 129). Those who are vulnerable must be assured that a comprehensive package of safeguards that includes rigorous standards for public accountability, accessible grievance and appeals mechanisms, and skilled professional oversight will be put in place and maintained by HCFA. Better-integrated and better-organized systems of care promise potentially-high-quality and effective care, but only if a commitment is made at the outset to strong quality assurance, a service ethic that cares for the whole person, and outreach to those in the community who are most in need.
References
Adler, G. S., and M. Phil. 1995. Medicare beneficiaries rate their medical care: New data from the MCBC. Health Care Financing Rev. 16(4):175-187.
American Association of Retired Persons, Administration on Aging, U.S. Department of Health and Human Services. 1995. A Profile of Older Americans. Washington, D.C.: The Association.
American Association of Retired Persons, The Urban Institute. 1995. Coming Up Short: Increasing Out-of-Pocket Health Spending of Older Americans. April. Washington, D.C.: The Public Policy Institute.
American Society on Aging. 1992. Serving Elders of Color: Challenges to Providers and the Aging Network. San Francisco, Calif.: The Society.
Armstead, R., P. Elstein, J. Gorman. 1995. Toward a 21st century quality measurement system for managed care organizations. Health Care Financing Rev. 16(4):25-37.
Bates, E. W., and B. S. Brown. 1988. Geriatric care needs and HMO technology. Med. Care 26:488-498.
Braveman, P., and T. Bennett. 1995. Let's take on the real dragon: Profiteering in health care. J. Public Health Policy 6:261-268.
Brown, R. S., J. W. Bergeron, D. G. Clement, J. W. Hill, and S. M. Retchin. 1993. The Medicare Risk Program for HMOs. Final Summary Report on Findings from the Evaluation. Final Report. February 18. Princeton, N.J.: Mathematica Policy Research, Inc.
Calkins, E., D. Dempster, and T. Kroll. 1995. Progress in geriatric care. HMO Pract. 9:27-31.
Callahan, C. M., H. C. Hendrie, and W. Tierney. 1995. Documentation and evaluation of cognitive impairment in elderly primary care patients. Ann. Intern. Med. 122:422-429.
Carlisle, D. M., A. L. Siu, E. B. Keeler, E. A. McGlynn, K. L. Kalin, L. V. Rubenstein, and R. H. Brook. 1992. HMO vs. fee-for-service care of older persons with acute myocardial infarction. Am. J. Public Health 82:1626-1630.
Christianson, J. B., and F. C. Osher. 1994. Health maintenance organizations, health reform, and persons with serious mental illness. Hosp. Community Psychiatry 45:898-905.
Chronic Care Initiatives in HMOs. (undated). Project summaries. Washington, D.C.: Chronic Care Initiatives in HMOs.
Clement, D. G., S. M. Retchin, M. H. Stegall, and R. S. Brown. 1992. Evaluation of Access and Satisfaction with Care in the TEFRA Program. Final Report. October 28. Princeton, N.J.: Mathematica Policy Research.
Clement, D. G., S. M. Retchin, R. S. Brown, and M. H. Stegall. 1994. Access and outcomes of elderly patients enrolled in managed care. JAMA 271:1487-1492.
The Commonwealth Fund. 1995. Executive Summary. In Patient Experiences in Managed Care. New York: The Commonwealth Fund.
Congressional Budget Office. 1995. Memorandum. The effects of managed care and managed competition. Congressional Budget Office, Washington, D.C.
Davis, K., K. S. Collins, and C. Morris. 1994. Managed care: Promises and concerns. Health Affairs 13:178-185.
Epstein, A. M., J. A. Hall, M. Fretwell, M. Feldstein, M. L. DeCiantis, J. Tognetti, C. Cutler, M. Constantine, R. Besdine, R. Rowe, and B. J. McNeil. 1990. Consultative geriatric assessment for ambulatory patients-A randomized trial in a health maintenance organization. JAMA 263:538-544.
Fama, T., and P. D. Fox. 1995. Beyond the benefit package. HMO Pract. 9:179-181.
Families USA Foundation. 1995. Managed care: Serving the chronically ill and disabled. States of Health 5(6):1-5.
Fox, P. D., L. Heinen, A. M. Kramer, and S. Palsbo. 1991. Initiatives in Service Delivery for the Elderly in HMOs. February. Princeton, N.J.: The Robert Wood Johnson Foundation.
Franks, P., C. M. Clancy, and P. A. Nutting. 1992. Gatekeepers revisited—protecting patients from over treatment. N. Engl. J. Med. 327:424-429.
Frederick/Schneiders, Inc. 1995. Analysis of Focus Groups Concerning Managed Care and Medicare. Prepared for The Henry J. Kaiser Family Foundation. Washington, D.C.: Frederick/Schneiders, Inc.
Friedman, B. R., and L. Kane. 1993. HMO medical directors' perceptions of geriatric practice in Medicare HMOs. J. Am. Geriatr. Soc. 41:1144-1149.
Friedman, E. 1995. The power of physicians: Autonomy and balance in a changing system. Paper presented at National Health Policy Forum, George Washington University. May. Washington, D.C.
Gabel, J. R., T. H. Dial, J. Hobart, L. Pan, C. Bergsten, A. Bernstein, M. Opanga, H. Whitmore, C. Barnes, and S. Palsbo. 1994. Industry Profile. Washington, D.C.: Group Health Association of America.
Ginzberg, E. 1995. A cautionary note on market reforms in health care. JAMA 274:1633-1634.
Gold, M., and F. Reeves. 1987. Preliminary Results of the GHAA—BC/BS Survey on Physician Incentives in Health Maintenance Organizations. November. Washington, D.C.: Group Health Association of America, Research Department.
Greenfield, S., W. Rogers, M. Mangotich, M. F. Carney, and A. R. Tarlov. 1995. Outcomes of patients with hypertension and non-insulin dependent diabetes mellitus treated by different systems and specialities—results from the medical outcomes study. JAMA 274:1436-1444.
Group Health Association of America. 1995a. Innovative Answers for America's Health Care: Best Practices in HMOs. Washington, D.C.: Group Health Association of America, Research Department.
Group Health Association of America. 1995b. 1995 Sourcebook on HMO Utilization Data. Washington, D.C.: Group Health Association of America.
Group Health Association of America. 1995c. Medicare Beneficiaries Who Choose HMOs Stick with Them; Only 4 Percent Return to Fee-For-Service. June 8. Press release. Group Health Association of America, Washington, D.C.
Group Health Association of America. 1995d. Medicare at 30: An opportunity for all Americans. Discussion paper, July Meeting, 1995. Group Health Association of America, Washington, D.C.
Health Care Financing Administration. 1995. Medicare: A Profile. February. Washington, D.C.: U.S. Department of Health and Human Services.
Health Care Financing Administration, Bureau of Data Management and Strategy. 1995. 1995 Data Compendium. March. Baltimore, Md.: U.S. Department of Health and Human Services.
Health Care Financing Administration, Division of Policy and Evaluation, Office of Managed Care. 1994. A Collection of Best Practices of Managed Care Organizations. Washington, D.C.: Government Printing Office.
Health Care Financing Administration, Office of Managed Care (Operations & Oversight Team). 1995a. Medicare Managed Care Contract Report (data as of January 1, 1996). Baltimore, Md.: U.S. Department of Health and Human Services.
Health Care Financing Administration, Office of Managed Care (Policy & Program Improvement Team). 1995b. Analysis of age distribution of Medicare beneficiaries in fee-for-service vs. managed care risk plans. Health Care Financing Administration, Baltimore, Md. March 22. Internal memorandum.
Health Care Financing Administration, Office of Research and Demonstration. 1995. Health Care Financing Review, Medicare and Medicaid Statistical Supplement, 1995. Baltimore, Md.: U.S. Department of Health and Human Services.
The Henry J. Kaiser Family Foundation. 1995. Medicare and Managed Care. Menlo Park, Calif.: The Henry J. Kaiser Foundation.
The Kaiser Commission on the Future of Medicaid. 1995. Policy Brief—Medicaid and the Elderly. Washington, D.C.: The Kaiser Commission on the Future of Medicaid.
Kassirer, J. P. 1995. Managed care and the morality of the marketplace. N. Engl. J. Med. 333:50-52. Kramer, A. M., P. D. Fox, and N. Morgenstern. 1992. Geriatric care approaches in health maintenance organizations. J. Am. Geriatr. Soc. 40:1055-1067.
Kronick, R., Z. Zhou, and T. Dreyfus. 1995. Making risk adjustment work for everyone. Inquiry 32(Spring):41-55.
Langwell, K. M., and J. P. Hadley. 1989. Evaluation of the Medicare competition demonstrations. Health Care Financing Rev., Special Rep. 11(2):65-80.
Lawlor, E. F. 1995. Is Managed Care the Answer? The Public Policy and Aging Report 6(5/6): 1995. Chicago: Center on Aging, Health and Society, University of Chicago.
Lewin/ICF. 1990. A Research and Demonstration Agenda on Health Services Delivery to Older Persons in HMOs. A report on a workshop convened by the Robert Wood Johnson Foundation and the National Institute on Aging, November 15, 1990. Fairfax, Va.: Lewin/ICF.
Lurie, N., I. S. Moscovice, M. Finch, J. B. Christianson, and M. K. Popkin. 1992. Does capitation affect the health of the chronically mentally ill? Results from a randomized trial. JAMA 267:3300-3304.
Lurie, N., J. Christianson, M. Finch, and I. Moscovice. 1994. The effects of capitation on health and functional status of the Medicaid elderly. Ann. Intern. Med. 120:506-511.
Mashaw, J. L., and T. R. Marmor. 1995. Real talk about Medicare. Washington Post. December 5, p. A19.
McNeil, J. M. 1993. Americans with Disabilities: 1991-92, Data from the Survey of Income and Program Participation. Current Population Reports, Household Economic Studies, P70-33. December. Washington, D.C. : Bureau of the Census.
Meyer, J., S. Silow-Carroll, and M. Regenstein. Forthcoming. Managed Care and Medicare. Washington, D.C.: American Association of Retired Persons/The Public Policy Institute.
Miles, S. H., E. P. Weber, and R. Koepp. 1995. End-of-life treatment in managed care: The potential and the peril. West. J. Med. 163:302-305.
Millman, M., ed. 1993. Access to Health Care in America. Committee on Monitoring Access to Personal Health Care Services, Institute of Medicine. Washington, D.C.: National Academy Press.
Pacala, J. T., C. Boult, and K. W. Hepburn, L. Morishita, R. Reed, R. A. Kane, F. G. Kane, and J. K. Malone. 1994. Case Management in HMOs. Final Report. Washington, D.C.: Chronic Care Initiatives in HMOs.
Pawlson, L. G. 1994. Chronic illness: Implications of a new paradigm for health care. J. Quality Improvement 20:33-39.
Pope, A. M., and A. R. Tarlov, eds. 1991. Disability in America: Toward a National Agenda for Prevention. Washington, D.C.: National Academy Press.
Porell, F. W., C. Cocotas, P. J. Perales, C. P. Tompkins, and M. Glavin. 1992. Factors Associated with Disenrollment from Medicare HMOs. Findings from a Survey of Disenrollees. Waltham, Mass.: Health Policy Research Consortium, Brandeis University.
The Public Policy Institute/American Association of Retired Persons. 1995. Memorandum from K. B. Wu to Legislation and Public Policy Division. November 13, 1995. The Public Policy Institute, Washington, D.C.
Retchin, S. M., D. G. Clement, L. F. Rossiter, B. Brown, R. Brown, and L. Nelson. 1992. How the elderly fare in HMOs: Outcomes from the Medicare competition demonstrations. Health Services Res. 27:651-669.
The Robert Wood Johnson Foundation. 1995. Sick people in managed care have difficulty in getting services and treatment, new survey reports. June 18. Press release. The Robert Wood Johnson Foundation, Princeton, N.J.
Rogers, W. H., K. B. Wells, L. S. Meredith, R. Strum, and A. Burnam. 1993. Outcomes for adult outpatients with depression under prepaid or fee-for-service financing. Arch. Gen. Psychiatry 50:517-525.
Rolnick, S. J., J. Garrard, L. Luepke, K. Hogan, and R. Heinrich. 1994. Selfreported depressive symptoms in a HMO seniors population: The process of case identification. Pp. 811-819 in Conference proceedings from Navigating Reform: HMOs, Managed Care in a Time of Transition. Washington, D.C.: Group Health Institute.
Safran, D. G., A. R. Tavlov, and W. H. Rogers. 1994. Primary care performance in fee-for-service and prepaid health care systems. JAMA 27:1579-1586.
Schlenker, R. E. Forthcoming. Home health payment legislation: Review and recommendations. Washington, D.C.: American Association of Retired Persons/Public Policy Institute.
Schlesinger, M., and D. Mechanic. 1993. Challenges for managed competition from chronic illness. Health Affairs Suppl. Managed Competition 12:123-137.
Schneider, E. L., and J. M. Guralnik. 1990. The aging of America: Impact on health care costs. JAMA 263:2335-2340.
Scott, J. C., and B. J. Robertson. 1995. Kaiser Permanente Medical Care Program, Denver, Colorado-Cooperative Health Care Clinic. Project summary presented at the Robert Wood Johnson Invitational Conference on Chronic Care Initiatives in HMOs, Washington, D.C., April 27-28, 1995.
Shaughnessy, P. W., R. E. Schlenker, and D. F. Hittle. 1994. Home health care outcomes under capitated and fee-for-service payment. Health Care Financing Rev. 16:187-222.
Smyer, M. A. 1993. Testimony at the Forum on Mental Health and the Aging before the Special Committee on Aging, U.S. Senate. 103d Cong., July 15, 1993, Serial No. 103-10.
Sulmasy, D. P. 1995. Managed care and managed death. Ann. Intern. Med. 153:133-136.
Tanenbaum, S. J., and R. E. Hurley. 1995. Disability and the managed care frenzy: A cautionary note. Health Affairs 14(4):213-219.
U.S. Congress, Senate, Special Committee on Aging, the American Association of Retired Persons, the Federal Council on the Aging, the U.S. Administration on Aging. 1991. Aging in America-Trends and Projections. Washington, D.C.: U.S. Department of Health and Human Services
U.S. Department of Health and Human Services. 1995a. Medicare Beneficiary Interest in HMOs. October. OEI-004-93-00142. Washington, D.C.: Office of the Inspector General, U.S. Department of Health and Human Services.
U.S. Department of Health and Human Services. 1995b. Medicare Risk HMO Performance Indicators. October. OEI-06-91-00734. Washington, D.C.: Office of the Inspector General, U.S. Department of Health and Human Services .
U.S. Department of Health and Human Services. 1995c. Beneficiary Perspectives of Medicare Risk HMOs. March. OEI-06-91-00730. Washington, D.C.: Office of Inspector General, U.S. Department of Health and Human Services.
U.S. Department of Health and Human Services. 1995d. Vital and Health Statistics, Trends in the Health of Older Americans: U.S., 1994. DHHS Pub. No. (PHS)95-1414. Public Health Service, Centers for Disease Control and Prevention. Hyattsville, Md.: National Center for Health Statistics.
U.S. Department of Health and Human Services, Public Health Service. 1995. Health United States 1994. Centers for Disease Control and Prevention. DHHS Pub. No. (PHS)95-1232. May. Hyattsville, Md.: National Center for Health Statistics.
U.S. General Accounting Office. 1988. Medicare: Physician Incentive Payments by Prepaid Health Plans Could Lower Quality of Care. Pub. No. GAO/HRD-89-29. December. Washington, D.C.: U.S. General Accounting Office.
U.S. General Accounting Office. 1993. Medicaid: States Turn to Managed Care to Improve Access and Control Costs. Pub. No. GAO/HRD-83-46. March. Washington, D.C.: U.S. General Accounting Office.
U.S. General Accounting Office. 1994. Medicare: Changes to HMO Rate Setting Method Are Needed to Reduce Program Costs. Pub. No. GAO/ HEHS 94-119. September. Washington, D.C.: U.S. General Accounting Office.
U.S. General Accounting Office. 1995a. Medicare: Enrollment Growth and Payment Practices for Kidney Dialysis Services. Pub. No. GAO/HEHS96-33. November. Washington, D.C.: U.S. General Accounting Office.
U.S. General Accounting Office. 1995b. Medicare Managed Care: Growing Enrollment Adds Urgency to Fixing HMO Payment Problem. Pub. No. GAO/HEHS 96-21. November. Washington, D.C.: U.S. General Accounting Office.
Van de Water, P. N. 1995. CBO Testimony on Federal Entitlement Spending before the Committee on the Budget, U.S. Senate. February 1. Washington, D.C.: Congressional Budget Office.
Vladeck, B. C. (Administrator, Health Care Financing Administration, U.S. Department of Health and Human Services). 1995. Statement before the U.S. Senate Special Committee on Aging, August 3, 1995.
Voelker, R. 1994. Population-based medicine merges clinical care, epidemiologic techniques. JAMA 271:1301-1302.
Wagner, A. 1993. Geriatric care in HMOs. HMO Pract. 7(3):133-135.
Wagner, E. H., and T. V. Bledsoe. 1990. The RAND Health Insurance Experiment & HMOs. Med. Care 20:191-200.
Wagner, E. H., B. T. Austin, and M. Vonkorff (Center for Health Studies, Group Health Cooperative of Puget Sound). 1995a. Improving outcomes in chronic illness. Paper presented at the Robert Wood Johnson Invitational Conference on Chronic Care Initiatives in HMOs, Washington, D.C., April 27-28, 1995.
Wagner, E., J. Scott, N. Euchner, and D. Reuben. 1995b. New models for the delivery of primary care for people with chronic conditions. Paper presented at the Robert Wood Johnson Invitational Conference on Chronic Care Initiatives in HMOs, Washington, D.C., April 27-28, 1995.
Ware, J. E., W. H. Rogers, A. Ross Davies, G. A. Goldberg, R. H. Brook, E. B. Keeler, C. D. Sherbourne, and J. P. Newhouse. 1986. Comparison of health outcomes at a health maintenance organization with those of fee-for-service care. Lancet 1(8488):1017-1022.
Weiner, J., and J. Skaggs. 1995. Current Approaches to Integrating Acute and Long-Term Care Financing and Services. Washington, D.C.: The Public Policy Institute/American Association of Retired Persons.
Williams, S. J., R. L. Seidman, J. A. Drew, B. L. Wright, J. P. Elder, and M. E. McGann. 1995. Identifying depressive symptoms among elderly Medicare HMO enrolless. HMO Pract. 9(4):168-173.
Winslow, R. 1994. HMO quality is rated similar to other care. Wall Street Journal. May 18, 1994.









































