2
The Computer-Based Patient Record: Meeting Health Care Needs
In recent years, computerization of patient records has increased at a moderate rate and this trend is likely to continue, particularly as technology improves and becomes more affordable and as the demand for health care information increases. If future patient records are merely automated versions of most current records, however, an opportunity to improve a fundamental resource for health care will have been lost. For example, in the patient record of the future, the committee seeks the ability to access quickly a list of current problems, a trail of clinical logic, the patient's health status, and the most recent information about various treatment options for the patient's condition. Easy access to and sound organization of data elements can be provided by automation of patient records, but the availability of the data elements depends on whether practitioners collect and record such data in the first place. Further, access to bibliographic and knowledge databases will require new functions not provided by traditional patient records.
Thus, the automation of patient record retrieval, maintenance, and use is necessary, but not sufficient, for record improvement. Given existing and emerging computer technologies and the evolving nature of health care, the committee believes that the patient record can, must, and will develop to meet the expanding needs of the health care field. This chapter identifies the attributes of future patient records that are required to meet these needs, discussing several of them in detail to highlight the scope and complexity of the issues to be addressed.
Defining Health Care Needs
The quality of a patient record or a patient record system depends on its ability to meet the needs and requirements of those who use it. As discussed
below, those users include, but are not limited to, physicians and nurses delivering care to patients. The committee followed three steps suggested by the continuous quality improvement model to develop its vision of an improved patient record and record system: (1) identify the customers; (2) understand their requirements; and (3) translate those requirements into functional characteristics of the system (Donabedian, 1966, 1988; Batalden and Buchanan, 1989; Berwick, 1989). 1
Patient Record Users
The committee broadly defined the users of patient records as those individuals who enter, verify, correct, analyze, or obtain information from the record, either directly or through an intermediary. All users of the patient record ultimately support patient care. They differ, however, in how and why they use the record.
Some users have daily contact with the record, others access the record sporadically, and still others never actually handle the record but rely on data derived from it. An exhaustive list of patient record users would essentially parallel a list of the individuals and organizations associated directly or indirectly with the provision of health care. Patient record users provide, manage, review, or reimburse patient care services; conduct clinical or health services research; educate health care professionals or patients; develop or regulate health care technologies; accredit health care professionals or provider institutions; and make health care policy decisions. All of these kinds of users are ''customers" of the patient record, and their needs should be met by patient record systems of the future.
Users are individuals, but they most commonly perform their functions on behalf of institutions. Boxes 2-1A and 2-1B identify types of individuals and organizations that rely on patient records or the data they contain. These lists are illustrative rather than comprehensive and indicate the wide range of users and settings in which patient records are employed.
The full array of patient record users and the respective needs of each were too extensive for the committee to address fully. Therefore, it identified five major categories of users that it considered the most significant and representative. Specifically, the committee focused on practitioners (physicians,
|
1 |
As stated by Juran (1989), the remaining steps of the quality improvement process are as follows: (4) design a system capable of supplying these functional characteristics; (5) implement the design; (6) prove the value of the system; and (7) stabilize or further improve the system, depending on the results of ongoing evaluation. Given the scope of its charge, the committee stopped short of designing such a system; it did, however, accomplish an intermediate step by determining the technological implications of the functional requirements of future patient record systems (see Chapter 3). |
|
BOX 2-1A Patient Care Delivery (Providers) Chaplains Dental hygienists Dentists Dietitians Laboratory technologists Nurses Occupational therapists Optometrists Pharmacists Physical therapists Physicians Physician assistants Podiatrists Psychologists Radiology technologists Respiratory therapists Social workers Patient Care Delivery (Consumers) Patients Families Patient Care Management and Support Administrators Financial managers and accountants Quality assurance managers Records professionals Risk managers Unit clerks Utilization review managers Patient Care Reimbursement Benefit managers Insurers (federal, state, and private) Other Accreditors Government policymakers and legislators Lawyers Health care researchers and clinical investigators Health sciences journalists and editors |
nurses, and other health professionals), patients, administrators, third-party payers, and researchers.2
Patient Record Uses
Just as the range of patient record users includes more than physicians, nurses, and other health care professionals, patient record uses extend beyond direct patient care. Similar to a comprehensive list of users, a complete list of uses would be quite long. Boxes 2-2A and 2-2B list examples of primary and secondary uses of patient records.
Primary uses of patient records are associated with the provision of patient care, that is, with providing, consuming, managing, reviewing, supporting, and charging and reimbursing patient care services. Secondary uses of patient records are not considered necessary for a particular encounter between a patient and a health care professional, but such uses influence
|
BOX 2-1B Health Care Delivery (inpatient and outpatient) Alliances, associations, networks, and systems of providers Ambulatory surgery centers Donor banks (blood, tissue, organs) Health maintenance organizations Home care agencies Hospices Hospitals (general and specialty)* Nursing homes Preferred provider organizations Physician offices (large and small group practices, individual practitioners) Psychiatric facilities Public health departments Substance abuse programs Management and Review of Care Medicare peer review organizations Quality assurance companies Risk management companies Utilization review and utilization management companies Reimbursement of Care Business health care coalitions Employers Insurers (federal, state, and private) Research Disease registries Health data organizations Health care technology developers and manufacturers (equipment and device firms, pharmaceutical firms, and computer hardware and software vendors for patient record systems) Research centers Education Allied health professional schools and programs Schools of medicine Schools of nursing Schools of public health Accreditation Accreditation organizations Institutional licensure agencies Professional licensure agencies Policymaking Federal government agencies Local government agencies State government agencies |
|
BOX 2-2A Patient Care Delivery (Patient) Document services received Constitute proof of identity Self-manage care Verify billing Patient Care Delivery (Provider) Foster continuity of care (i.e., serve as a communication tool) Describe diseases and causes (i.e., support diagnostic work) Support decision making about diagnosis and treatment of patients Assess and manage risk for individual patients Facilitate care in accordance with clinical practice guidelines Document patient risk factors Assess and document patient expectations and patient satisfaction Generate care plans Determine preventive advice or health maintenance information Remind clinicians (e.g., screens, age-related reminders) Support nursing care Document services provided (e.g., drugs, therapies) Patient Care Management Document case mix in institutions and practices Analyze severity of illness Formulate practice guidelines Manage risk Characterize the use of services Provide the basis for utilization review Perform quality assurance Patient Care Support Allocate resources Analyze trends and develop forecasts Assess workload Communicate between departments Billing and Reimbursement Document services for payments Bill for services Submit insurance claims Adjudicate insurance claims Determine disabilities (e.g., workmen's compensation) Manage costs Report costs Perform actuarial analysis |
the environment in which patient care is provided. Education, research and development, regulation, and policymaking are all considered secondary uses of the patient record.
Practical considerations forced the committee to focus on certain high-priority record uses rather than on all possible functions of the record. The four major categories of patient record uses considered by the committee were direct patient care, administration and management, reimbursement, and research.
Translating Customer Needs Into System Requirements
Proper system design means achieving a patient record system that properly fits, interacts with, and communicates in the accepted manner of every user community the system supports. This kind of design is necessary if automated patient record systems are to be adopted by users. The committee defined the needs of patient record users in terms of system function and issues of implementation and operation. System function is what the system enables users to do and what it does for them. Implementation and operation issues relate to the factors users consider in acquiring and installing a system. These factors are important regardless of the form of the record (e.g., paper or computer-based).
The specific features users seek in patient records and record systems are described below in terms of the computer-based patient record (CPR). Most of these desired features are common to two or more major kinds of record users. Unique concerns or needs of a user group are also identified. Box 2-3 presents an overview of user requirements.
|
BOX 2-2B Education Document health care professional experience Prepare conferences and presentations Teach health care professions students Regulation Serve as evidence in litigation Foster postmarketing surveillance Assess compliance with standards of care Accredit professionals and hospitals Compare health care organizations Research Develop new products Conduct clinical research Assess technology Study patient outcomes Study effectiveness and cost-effectiveness of patient care Identify populations at risk Develop registries and databases Assess the cost-effectiveness of record systems Policy Allocate resources Conduct strategic planning Monitor public health Industry Conduct research and development Plan marketing strategy |
|
BOX 2-3 Record Content Uniform core data elements Standardized coding systems and formats Common data dictionary Information on outcomes of care and functional status Record Format "Front-page" problem list Ability to "flip through the record" Integrated among disciplines and sites of care System Performance Rapid retrieval 24-hour access Available at convenient places Easy data input Linkages Linkages with other information systems (e.g., radiology, laboratory) Transferability of information among specialties and sites Linkages with relevant scientific literature Linkages with other institutional databases and registries Linkages with records of family members Electronic transfer of billing information Intelligence Decision support Clinician reminders "Alarm" systems capable of being customized Reporting Capabilities "Derived documents" (e.g., insurance forms) Easily customized output and other user interfaces Standard clinical reports (e.g., discharge summary) Customized and ad hoc reports (e.g., specific evaluation queries) Trend reports and graphics Control and Access Easy access for patients and their advocates Safeguards against violation of confidentiality Training and Implementation Minimal training required for system use Graduated implementation possible |
In compiling the list of user requirements, the committee noted two special considerations. First, user needs can conflict with each other—not just among groups (e.g., patients and practitioners need confidentiality, but claims payers seek access to detailed clinical information), but also within a single user group (e.g., doctors want access to information to be very fast, but they may also want to be able to sort information according to complicated logical rules, which slows response times). To the extent possible, the committee resolved such conflicts by using sensible rules of priority. In
several cases, however, the conflicts remained nettlesome and are discussed in Chapter 4 as particular challenges to future patient record development.
Second, at a technological frontier, customers may have difficulty expressing or even imagining a need. This situation may well occur with the computer-based patient record, which contains opportunities for functional characteristics that most users would not think to request. The pioneering designer must not only ask, "What do people want?" but also, "What would people want if they knew what could be done for them?"
Patient Record Functions
The traditional function of patient records has been to store information relevant to the care of a patient for subsequent retrieval. Patient record systems should offer users at least two additional functions. First, records should be able to guide the process of clinical problem solving. Second, records should support clinicians with decision analysis, reminders, risk assessment, and other "intelligent" features not available with paper records.
Storage
The attributes associated with the storage function are record access (i.e., availability, convenience, speed, and ease of use), quality, security, flexibility, connectivity, and efficiency.
ACCESS First and foremost, users want to retrieve information easily when and where they need it. Other features of a patient record system are essentially irrelevant to users if they cannot gain access to the system, to the records in the system, or to the data in the records.
Access can be described in terms of availability, convenience, reliability, 3 and ease of use. A patient record system should allow authorized clinical users convenient access to any record 24 hours a day. This requirement implies an adequate number of conveniently located terminals or work-stations, no system downtime, no lost records or data, and access to the record by more than one user at the same time. Nonclinical users typically require access to patient record data at least during standard working hours.
Different users need different levels and kinds of information (see Box 2-4). The ease with which users locate or retrieve needed data elements depends largely on the record format. Current paper record formats tend to segregate rather than integrate information; to facilitate communication of
needed information, an integrated format is necessary. Thus, records should contain a front-page problem list to allow users to locate desired information. In addition, record systems should allow users to "flip through" or easily scan records; a table of contents or index would be helpful for this purpose.
|
BOX 2-4 A patient record database contains many data elements, and each user community has a unique, definable "view" of the database that brings together the elements needed by that community. (Some communities also have specialized or occasional views for special circumstances.) Some views overlap, and some data elements appear in many views. Other data elements appear only in one view. For each view that supports a given user community, processes are needed to organize its contents, manipulate and display it in various ways, and allow users to commingle views. System-level processes that automatically support all views (e.g., calendar-date management, screening for access authorization to maintain confidentiality) are also required. For example, in a teaching hospital:
|
Several other capabilities are needed for optimal access. Users should be able to display information at different levels of detail. Moreover, the system should permit virtually every data item to be used as a key for retrieval and should also enable users to access subsets of data. All users, regardless of their level of computer expertise, should be able to enter most queries without the intervention of a programmer; thus, an English-like retrieval language should be part of the system.
Accessing information when needed includes more than finding an available terminal; from the user's point of view, it means an adequate (i.e., fast) system response time. Users want to perform their tasks at least as fast as they currently perform them with paper records. Extremely rapid retrieval of information, measured in fractions of a second, is an essential function for primary users of the CPR. In addition, clinicians, who are accustomed to writing or dictating their entries to patient records, want a comparable method in the CPR system to add data to the record.
From the users' perspective, the difficulty involved in learning to use a system also affects access. Thus, operation of patient record systems should require only minimal training.4 Training for physicians in particular should be short and easy, preferably occurring "on line" and at their convenience. Many physicians are unwilling to devote large blocks of time to learning a new record system, even if ultimately it might make their work easier. In addition, built-in, displayable "help" documentation on system operation and the data elements should be available to both clinical and nonclinical users.
The question of patient access to records is debated among practitioners. It is likely, however, that the trend toward increasing patient access will continue. Some providers consider it appropriate for patients to enter data (e.g., historical medical information) into their records routinely. Recently, functional status and preferences among various treatments have been identified as data that could be recorded by patients to assist practitioners in developing care plans.
Some practitioners encourage patients to audit their records for accuracy and completeness; they may also use the record for patient education. Indeed, as patients become increasingly computer-literate, knowledge-seeking consumers of health care services, the CPR may function as an important patient education tool by offering patients access to resources such as MEDLINE.
DATA QUALITY The notion of data quality has several attributes: legibility, accuracy, completeness, and meaning. CPR systems eliminate the need for handwriting and thus improve legibility. Accuracy of CPRs can be enhanced by data entry screens and logical rules that flag or block inappropriate entries for particular data fields. To the extent that CPRs reduce the need for an intermediary to enter data (i.e., for transcription), a potential source of errors (and cost) is removed. When errors do occur, for legal purposes the original entry and the correction should both be preserved (Waller, in this volume). Data accuracy also has implications for the security and reliability of CPR systems insofar as the systems must ensure that data are not lost or unknowingly corrupted.5
The completeness of patient records for subsequent users depends in part on agreement among users about uniform core data elements. Without such uniformity, what one patient record user views as complete data may be considered incomplete by another. Data completeness implies that systems will accommodate the currently expected range and complexity of clinical data and that they will permit new data fields to be added and obsolete data fields to be identified.6
For patient records to meet user needs, patient problems and the current status of patient problems should be clearly noted in the record. In addition, it is essential that the health care provider's rationale for clinical decisions be clearly documented. Lack of a recorded rationale hinders the ability of subsequent users of the record to make appropriate judgments regarding patient care, quality assurance, utilization review, reimbursement, and research.
For purposes of health services research, patient health status is the single most important data element that is usually missing from the patient records of today. Formal, interpretable information on health status is a precondition both to case mix or risk factor adjustment and to assessment of the outcomes of care. The research community clearly wants health status information, collected in a standard format, to be a routine part of the record of the future. Such records should also document health risk factors (e.g., smoking).
Technology assessment, clinical investigation, and health services research have been slowed by the lack of reliable, valid, standardized, consistently
collected information on the health status and functional level of patients (Ellwood, 1988; Roper et al., 1988). Moreover, practitioners may benefit from routine availability of health status measures. Some evidence suggests that without such measurements in routine clinical practice, physicians and other health care professionals often overlook significant impairments and changes in function among their patients (Nelson, 1990). In the past two decades, many health services researchers have worked to develop, test, and refine health status measures with sound psychometric characteristics (Katz, 1987; Lohr and Ware, 1987; McDowell and Newell, 1987; Lohr, 1989). These kinds of methodological advances could greatly increase the practical application of standardized health status data.
The committee acknowledged that the question of whether and how soon health status assessment will influence the quality of care remains to be addressed. To gain a better understanding of the value of health status measures, the committee supported their widespread adoption as a component of the patient record—but under conditions that would permit evaluation of whom they help and of how best they can be employed. The committee did not identify an optimal set of health status measurement instruments, as this determination was not part of its charge. Rather, to broaden the base of potential comparisons of case mix, care, morbidity, and outcomes, the committee noted the potential value of standardizing or otherwise increasing the compatibility of those instruments now in common use.
It remains unclear how outcome data can be gathered and used unobtrusively, inexpensively, and conveniently enough that such activities will become widespread. Merely adopting a computerized record format may not overcome the barriers that so far have impeded the diffusion of health status measurement into routine clinical practice. Computerization may make the analysis of such information easier but may not affect its collection.
The completeness of patient records depends in part on the time it takes to add new information to the record, once that information is available. Data completeness can be enhanced by linkages between CPR systems and ancillary systems (e.g., laboratory, radiology), which permit the transfer of results from ancillary systems to the CPR in the hospital, physician's office, or other provider setting as soon as such results are available.
Maintaining the quality of patient data also requires that the data have meaning for users. Effective retrieval and use of information from patient records depend on consistency in naming or describing the same findings, clinical problems, procedures, drugs, and other data within a single patient record, across many patient records in a single record system, or in other systems that contain data relevant to the understanding and treatment of patient problems. Communication among practitioners can be aided by a common clinical data dictionary and a clinical coding system that are interchangeable any clinical data common to different specialists or professions
but specific enough to describe the detailed data unique to a profession or specialty.
Health care researchers have a special need for record systems that provide more uniform results than are provided by current systems. Consistent description of clinical content becomes more important with the aggregation of data from many patient records—as in outcomes research, for example. Standardized data dictionaries, coding schemes, and uniform data sets permit more complete, reliable analyses of care and disease patterns involving multiple sites.7
SECURITY CPR systems have two security requirements. First, as discussed in Chapter 1, patient and provider privacy must be protected. Second, data and software must be safeguarded against tampering and unintentional destruction. These requirements demand both system and data security measures. System security refers to the measures taken to keep computer-based information systems safe from unauthorized access and other harm. Data security involves protection of data from accidental or intentional disclosure to unauthorized persons and from unauthorized alteration.
Data security includes both data confidentiality and data integrity. Data confidentiality is a ''requirement whose purpose is to keep sensitive information from being disclosed to unauthorized recipients" (National Research Council [NRC], 1991:52). Confidentiality requires appropriate action by physicians, nurses, midwives, secretaries, medical technicians, paramedical staff, social workers, hospital managers, computer staff, and research investigators in health care facilities to safeguard the privacy of patient information. Confidentiality also requires that computer systems refuse access to unauthorized individuals.
In its narrowest sense, data integrity refers to the consistency and accuracy of data stored in computer-based systems. It is a "requirement meant to ensure that information and programs are changed only in a specified and authorized manner" (NRC, 1991:54). Data integrity is of paramount importance to the CPR, and care must be taken, especially in distributed CPR systems (see Chapter 3), to ensure that records can be completely restored in the event of system failures.
A broader definition of data integrity could also be appropriately applied to patient data. Data are said to have integrity if they comply with an a priori stated expectation that they have a defined set of attributes. This a
priori set of attributes is unique to the data, to the process operating on the data, and to the data holder. Such attributes might include timeliness (e.g., every data element is posted within five minutes of availability), completeness (e.g., a certain set of data elements must be part of the record), and accuracy (e.g., there are no spelling errors, every address has a zip code).
Data integrity in future patient records might be enhanced by including a data validity field that would flag data that might not be correct. Data validity would be an additional parameter against which integrity could be judged and thereby controlled. Informing subsequent users that an entry might be incorrect would allow them to discount or ignore the information.
FLEXIBILITY Users assign high priority to flexibility in records; they do not want to be forced to use the record in a universally uniform or prescribed manner. Thus, future CPR systems should permit customization of data entry formats, reporting formats, and display formats—both for and, in some cases, by specific users. Patient record user needs are simply too many and too varied for any one combination of input, reporting, or display options. Furthermore, research has shown that the ability to customize computer interfaces according to one's preferences and work habits increases user acceptance of computer systems (Bikson et al., 1987).
Conventional formats should be designed and available as default modes, but the users of the patient record of the future should find the record easy to mold to their individual, local needs. Different formats for displaying information on the screen or on paper should be available. The record should also permit integration across disciplines and professional specialties and provide different "views"8 of patient data for different users (see Box 2-4).
Flexibility is also required to meet the varied reporting needs of users, particularly physician specialties. Doctors need record information available both in easily accessible, standard reporting formats (such as letters, insurance forms, school and camp certificates, etc.) and in formats they can easily customize according to specialty and individual taste. Therefore, the CPR system should contain a user-friendly report generator for physicians and others who wish to design specialized reports for their own use.
CONNECTIVITY Connectivity denotes the potential of the record or record system to establish links or to interact effectively with any sort of provider
or database that may improve the care of the patient. Three different interfaces are important in such interactions: the interface among records or record systems of different provider institutions, the interface between the record and other repositories or potential repositories of information that may be useful in caring for the patient, and the interface between the record and a practitioner.
Linkages among the various clinical records pertaining to a single patient are also important to users, who often want a longitudinal patient record—records from different times, providers, and sites of care that are linked to form a lifelong view of a patient's health care experiences. Linkages are also needed to transfer patient data from one care setting to another (e.g., from physician office to hospital) to facilitate service coordination.
Linking the records of family members, or the records of individuals who received a certain procedure in a particular facility, may prove useful for some types of epidemiological analysis. The aggregation of patient data for large-scale analysis, however, requires more complicated kinds of linkages. Integration of relevant subsets of data across institutional boundaries is especially important as researchers attempt to understand diseases and episodes of illness independent of the particular institution or health care professional with whom patients find themselves at a particular phase of their illness.
Patient record systems should also offer linkages to other databases and other sources of information.9 Desirable linkages include databases that contain scientific literature and bibliographic information, administrative information (e.g., coverage for a particular elective procedure for a given insurance plan), medical practice guidelines, insurance claims, and disease registries.
Connectivity makes several other demands on the system as well. To make it simple for the practitioner to interact with the record, data entry must be almost as easy as writing, and databases must be organized in such a way that any terminal or microcomputer on the system can retrieve requested data. As noted earlier, communication among practitioners depends on common data dictionaries and clinical coding systems. To interface easily with a database or registry requires a different sort of connectivity. Workstations must be designed with telecommunications interfaces that allow the user to switch almost instantly between the information in the record and its relevant counterpart in the external knowledge base.
EFFICIENCY Users want to minimize expense, effort, complexity, and waste. To achieve such efficiencies, computer-based patient record systems must include certain capabilities—in particular, one-time data entry and performance of routine tasks. Further, CPR systems should be designed so that data content is streamlined and unnecessary data are not collected.
Any data entered into the system should be available for a variety of uses, eliminating the need for redundant data entry. (The need for manual extraction of data and re-entry procedures greatly diminishes the value of a system.) The system should be designed to ensure that data are available to support patient care, organizational operations, and decision making. Thus, data must be viewed as an organizational resource, not property "owned" or controlled by the departments that happen to collect them or that are the primary users of the data.
The CPR system should be a part of an integrated patient care information system. If the system is hospital based, it should communicate with systems in the clinical laboratory, pharmacy, respiratory therapy, other ancillary services, referring physician offices, and other care settings (e.g., home, nursing home) so that data will not require manual transcription from one system to another. If the system is based in a physician's office, it should communicate with the computer systems of local clinical laboratories, pharmacies, hospitals, and other physicians' offices.10
CPR systems should facilitate the movement of data into, within, and outside of the automated patient record. In particular, they should permit raw and aggregated data to be moved to another electronic database for further analysis and storage. For example, a hospital or individual physician should be able to extract selected information electronically from a patient care database to send to other internal or external (perhaps national) databases.11 In addition, the system should have no trouble accepting data directly from electronic monitoring devices and other patient care equipment.
Health care professionals perform many routine administrative tasks in the course of providing services, and they seek ways to reduce this administrative burden so that they can devote more time to direct patient care, research, and education. Patient record systems should provide the capacity to generate routine documents based on record data automatically, to submit insurance claims electronically, and to report adverse reactions or occurrences of tracked diseases automatically.
Computer-based records must be designed to avoid the mere replication
of paper record features and behaviors that, upon reflection, have little or no value to users. Examples of waste include information that is routinely collected but never used; inflexible, redundant formats for recording data that result in duplicative information (e.g., obsolescent manual medication files); and retrospective quality assurance that could be replaced with online quality assurance. Such features and behaviors add cost rather than quality to the record system.
The committee did not specifically investigate the nature or scope of such wasted effort in present-day records, but members shared the general impression that it abounds. In developing the CPR, time would be well spent in practical research to identify and remove these "non-value-added" steps, features, and data elements, with the intent of producing a record that is leaner, less complex, and more streamlined than that of today. This process is likely to require changes in regulations or laws, and the committee urges that such changes be analyzed, recommended, and adopted (see Chapter 5).
Guidance of Clinical Problem Solving
It has been suggested that a physician's thought process is formed in part by his or her interaction with the patient record (Young, 1987). According to Weed (1968), a properly formatted patient record can guide clinicians through the process of clinical problem solving. It was this intention that led Weed to design the problem-oriented medical record (POMR) (Weed, 1968; Margolis, 1979).12
Studies investigating the use of the problem-oriented format to record the patient care process report three advantages over non-problem-oriented
(i.e., source-oriented or other) formats. First, the chance of follow-up for a problem listed in the problem list is significantly greater (Simborg et al., 1976; Starfield et al., 1979). In other words, the POMR's front-page problem list is a particularly useful feature. Second, it is easier to relate information in the record to a relevant problem (Aranda, 1974). Third, the format reflects an orderly process of problem solving, a heuristic that aids in identifying, managing, and resolving patients' problems (Weed, 1968).
The committee unanimously believes that patient records should guide and reflect clinical problem solving and that the mere translation of current record formats, data, and habits from paper to computer-based systems will not alone produce the range of improvements in care potentially achievable in a truly reformed patient record system. Current systems include behaviors and record forms that produce substantial waste, imprecision, and complexity in a care system less and less able to tolerate that burden. The committee also believes that the shift from a paper to a computer-based system offers an opportunity to study and improve clinical approaches and methods that are reflected in the record. Some formats are likely to be more effective than others in guiding and encouraging the use of an efficient, scientific problem solving method in the clinical process.
The committee did not reach unanimity regarding the choice of a single preferred record format to support improved clinical care. A majority maintained that no clearly superior alternative existed to warrant specific recommendation; this group therefore concluded that, at present, the primary pertinent requirement of a CPR is that it be sufficiently flexible to accommodate a wide range of present and future record formats.
Although it did not specifically recommend use of the POMR, the committee did consider certain components of the POMR to be highly desirable in any computer-based record system. Those components include (1) a structured, systematically collected database; (2) an easily reviewed and updated problem list; and (3) routine recording of clinical formulations and plans for care and follow-up. The committee urges continuing research to develop, design, and assess improved record formats that, over time, are likely to be used more consistently throughout the health care system.
A minority of committee members maintained that one patient record format—the problem-oriented medical record first described by Weed—offers a superior alternative in guiding and supporting scientific reasoning and clear communication in medical practice. Those who favored the POMR format argued that it is a general model that rests on a firm theoretical foundation and that its slow diffusion over the past two decades reflects in part practical barriers that may be overcome in a computer-based record environment. They recommend that clinicians use the POMR unless a specific alternative format is preferred in a particular practice setting.
Practitioner Support
Given the volume and complexity of the information required to provide patient care, users want the patient record to be more than a repository of data. Computer-based record systems can support practitioners by providing at least five kinds of tools that are not available with paper records. These tools include mechanisms for focusing attention, for patient-specific consultation, for information management, for data analysis, and for implementing quality assurance and cost management policies.
Human cognition has measurable limitations, and as a result humans "predictably overlook rare and uncommon events" (McDonald and Tierney, 1988:3435). Automated record systems can help practitioners recognize out-of-range values or dangerous trends, remember needed actions, recall available options, and make better clinical decisions. Human memory is imperfect, especially when the task involves remembering a large set of items or recalling the same items repeatedly. The computer can be relied on to remember large numbers of items accurately and to check routinely whether the practitioner has forgotten any standard items relevant to the diagnosis or treatment of a particular problem. Some of these reminders may be critical, and they can be linked to alarms (such as beep tones or messages) that warn the practitioner before trouble occurs.13 (For example, an alarm might be triggered when two incompatible drugs are prescribed together.)
CPR systems can also provide easy access to clinical decision support systems that provide "custom-tailored assessments or advice based on sets of patient-specific data" (Shortliffe et al., 1990:469). Currently available patient-specific consultation systems suggest differential diagnoses, indicate additional information that would help to narrow the range of etiologic possibilities, suggest a single best explanation for a patient's symptoms, or provide advice on therapy (Shortliffe et al., 1990).
CPR systems can support practitioners in the patient care setting by providing easy access to knowledge and bibliographic databases. Such access will free practitioners from relying on memory for infrequently used information. Moreover, computer-based record systems can help educate practitioners and keep them up-to-date on new developments by providing access
|
13 |
As discussed in Chapter 4, a significant factor to be addressed in CPR system development and implementation is the need for system users to change certain behaviors. The availability of reminders in either preventive or emergency situations will require practitioners to change their behavior; as a result, such reminders may not at first be embraced warmly by practitioners. Indeed, the value of this technology must be sufficiently demonstrated before practitioners will change their behavior. |
to bibliographic information when they need it (Association of American Medical Colleges, 1986; Haynes et al., 1989).
CPR systems can provide descriptive, graphical, and statistical analyses of clinical data using standard statistical software packages. In addition, CPR data can be rearranged and analyzed for ongoing quality assessment and to provide physicians and patients with quantitative assessments of the risks of conditions and treatments. (These assessments would promote formal decision analysis of many problems that at present cannot benefit from such analysis because of the lack of required data.) CPR system capabilities can facilitate these tasks in several ways: (1) rapid searching through single or multiple records; (2) sorting information in one record or information aggregated across multiple records; (3) aggregating data across patients by hospital, patient care unit, and department; and (4) allowing easy abstraction of information throughout patients' hospital stays or episodes of care.
Finally, CPR systems should offer practitioners and health care managers a means for implementing quality assurance and cost-management policies at the time and site of care (Barnett et al., 1978; Barton and Schoenbaum, 1990; Tierney et al., 1990). CPR systems can also be a resource for guiding policies and practice by providing analysis of past clinical experience within a provider setting (McDonald and Tierney, 1988).
Implementation and Operation Issues
Managers of health care organizations are faced with ever-increasing demands for data. From outside their organizations, requests come from regulators, payers, and community interest groups, among others; from inside their institutions, inquiries come from researchers and those responsible for utilization management and quality assurance. These managers are well aware that few existing record systems can meet these demands. They also recognize, and are wary of, both the cost and the conflict that may be incurred if they attempt to introduce major changes in record systems. Many institutions lack the capital for a sudden conversion to new computer architectures. Even if the funds were available, however, some managers are concerned that physician-management relationships, already strained in many medical organizations, could be further disrupted by an institution's insistence that physicians accept a new method or pattern of record keeping.
Nevertheless, administrators generally seem to prefer that the patient record not be frozen in its present form. They seek to implement change to a new system in a phased sequence, so that it can be more easily managed. Most user groups, but especially institutional managers, will have trouble implementing a vastly modified record system all at once. Proper design of advanced systems must involve well-considered plans for phasing in the changes that are going to be made. Otherwise, provider institutions in
particular will feel extended beyond their financial and organizational capabilities.
The Future Patient Record
The promise of significantly improved health care through the technological capabilities of computers constitutes the basis for the committee's vision of future patient records and patient record systems. The committee offers this vision to help readers picture what such records and systems can do and to serve as a standard against which current and future CPR systems can be compared.
Future patient records will have many more users and uses than present records. Direct providers of care (physicians, nurses, dentists, and other health care professionals) will remain the users of highest priority in design considerations. The needs of all users, however, can be accommodated to an extent not possible in current record systems.
The committee identified five objectives for future patient record systems. First, future patient records must support patient care and improve its quality. Second, they must enhance the productivity of health care professionals and reduce the administrative and labor costs associated with health care delivery and financing. Third, they must support clinical and health services research. Fourth, they must be able to accommodate future developments in health care technology, policy, management, and finance. Fifth—and the committee placed great emphasis on this—patient confidentiality must be maintained while these objectives are being met.
In the patient record of the future, the entire notion of such a record will be broadened from that of a location or device for keeping track of patient care events to that of a resource with much enhanced utility in patient care, management of the health care system, and extension of knowledge. Properly designed and used, the record will provide an accurate longitudinal account of care. The record system will also be broadened to include functions beyond those available in current record systems; it will help to improve care by reminding, linking, and guiding health care professionals and organizations. In short, the record of the future will be an asset in managing and improving the care of patients.
In the past, the basic function of a patient record was to store patient data for use by those involved in patient care. Even this classic function will be broader in the future, however, especially with respect to the key feature of flexibility. Different health care professionals require record information to be retrieved and displayed in different formats. Today, both paper and computer records are often cumbersome tools for information retrieval and display. The record of the future will be far more flexible and will permit users to design and utilize reporting formats tailored to their special needs.
Future patient records will provide new dimensions of record functionality through links to other databases, decision support tools, and reliable transmission of detailed information across substantial distances. To meet the needs of practitioners, future patient record systems will be linked to knowledge bases, clinical decision support systems, statistical software packages, and video or picture graphics. In hospitals, various departmental systems (e.g., finance, laboratory, nursing, radiology) will be able to communicate with the patient record system. Physician offices will be able to communicate with local hospitals and with national bibliographic resources such as MEDLINE. In the larger health care environment, computer-based information management systems will be able to communicate with information systems of provider institutions, third-party payers, and other health care entities.
As noted in the committee's definition of a patient record system, people are also a system component. Optimal functioning of future systems poses four conditions for users. First, they must have confidence in the data (which implies that data must be entered directly by the practitioner who collected it, reliably integrated among all sources, and accurately retrieved whenever needed). Second, they must use the record actively in the clinical process. Third, they must understand that the record is a resource for studying the effectiveness and efficiency of clinical processes, procedures, and technologies. Fourth, they must be capable of using future computer-based record systems efficiently.
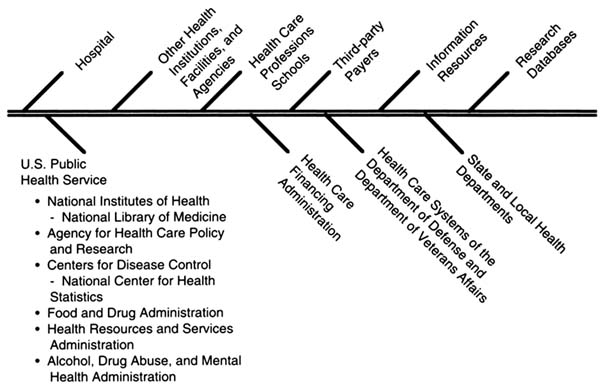
The committee visualizes the CPR as the core of health care information systems. Figure 2-1 illustrates the various types of interactions in which CPR systems will be required to engage. Such systems must be able to transmit data to other types of clinical and administrative information systems within provider institutions; they must also be able to transmit data to other provider institutions or to secondary databases. (For example, CPR systems in physicians' offices should be able to communicate with local hospitals.) In addition, CPR systems must also be able to accept data from other internal and external computer-based systems.
Figure 2-2 illustrates the committee's vision of a national health care information system. Such a system would support the transmission of data for clinical purposes and, with appropriate confidentiality measures, for reimbursement and research purposes. It would also bring information resources (e.g., MEDLINE) to virtually all practitioners. A national health care information system would require that local, regional, and national networks be established. These networks would provide the means to transmit a laboratory report from a hospital to a physician's office or to send a patient record across the country. A national health care information system with these and other capabilities could support the coordination and integration of health care services across settings and among providers of care.
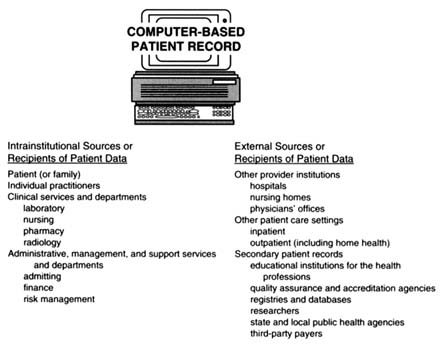
FIGURE 2.1 Computer-based patient records as the core of health care information systems.
In delineating its vision of a national health care information system, the committee is not proposing that a single CPR system be imposed on health care providers; indeed, no single CPR system is likely to meet the wide range of CPR user needs. Imposing a single system on health care providers is likely to result in the loss of desirable flexibility. Moreover, there is no mechanism for accomplishing such a task in the pluralistic health care system of the United States. Nevertheless, the committee believes all CPR systems must meet minimum connectivity requirements and offer a set of standard functions. To accommodate various user communities and institutions, however, the committee anticipates that a range of CPR systems will be available. For example, CPR systems will offer a range of additional functions and come in a variety of sizes; they will also have varying price tags, depending on individual provider requirements. In other words, the committee seeks a national transportation system for patient data. The transportation system will require an infrastructure (e.g., networks) and standards for connectivity and security but will retain a substantial amount of flexibility.
The notion of a health care information system should not suggest that all patient data will be collected in a monolithic database. Rather, CPR data
should be collected so that they can produce quality secondary records; subject to appropriate controls, these records can be added to institutional, local, regional, national, or international databases as needed for clinical, administrative, or research purposes.
In summary, the committee believes that the computer-based patient record can play an increasingly important role in the health care environment. This role begins in the care process by providing patient information when needed and by supporting clinical decision making. It extends to the management of care by establishing a mechanism by which quality assurance procedures and clinical practice guidelines (including the most recent warnings on contraindications and adverse reactions to therapies) can be brought to health care professionals at the time and site of patient care. It also includes providing opportunities for reducing administrative costs associated with health care financing and collecting administrative data for internal and external review. It encompasses enhancing health care professional education by supporting independent, lifelong learning. Finally, it extends to capturing relevant, accurate data necessary for technology assessment, health services research, and related studies concerning the appropriateness, effectiveness, and outcomes of care.
References
Aranda, J. M. 1974. The problem-oriented medical records: Experiences in a community hospital. Journal of the American Medical Association 229:549–551.
Association of American Medical Colleges. 1986. Medical Education in the Information Age: Proceedings of the Symposium on Medical Informatics . Washington, D.C.
Barnett, O. G., R. Winickoff, J. L. Dorsey, M. M. Morgan, and R. S. Lurie. 1978. Quality assurance through automated monitoring and concurrent feedback using a computer-based medical information system. Medical Care 16:962–970.
Barton, M. B., and S. C. Schoenbaum. 1990. Improving influenza vaccination performance in an HMO setting: The use of computer-generated reminders and peer comparison feedback. American Journal of Public Health 80:534–536.
Batalden, P. B., and E. D. Buchanan. 1989. Industrial models of quality improvement. Pp. 133–159 in Providing Quality Care: The Challenge to Clinicians, ed. N. Goldfield and D. B. Nash, D.B. Philadelphia, Pa.: American College of Physicians.
Berwick, D. M. 1989. Sounding board: Continuous improvement as an ideal in health care . New England Journal of Medicine 320:53–56.
Bikson, T. K., B. A. Gutek, and D. A. Mankin. 1987. Implementing Computerized Procedures in Office Settings: Influence and Outcomes . Santa Monica, Calif.: The RAND Corporation.
Donabedian, A. 1966. Evaluating the quality of medical care. Milbank Memorial Fund Quarterly 44(pt. 2):166–203.
Donabedian, A. 1988. The quality of care. How can it be assessed? Journal of the American Medical Association 260:1743–1748.
Ellwood, P. M. 1988. Shattuck lecture—Outcomes management: A technology of patient experience. New England Journal of Medicine 23:1549–1556.
Haynes, R. B., M. Ramsden, K. A. McKibbon, C. J. Walker, and N. C. Ryan. 1989. A review of medical education and medical informatics. Academic Medicine 64: 207–212.
Juran, J. M. 1989. Juran on Quality Planning. New York: McGraw-Hill.
Katz, S., ed. 1987. The Portugal conference: Measuring quality of life and functional status in clinical and epidemiological research. Journal of Chronic Diseases 40:459–650.
Lohr, K. N., ed. 1989. Advances in health status assessment: Conference proceedings. Medical Care 27(suppl.):S1–S294.
Lohr, K. N., and J. E. Ware, Jr., eds. 1987. Proceedings of the Advances in Health Assessment Conference. Journal of Chronic Diseases 40(suppl. 1):1S–193S.
Margolis, C. Z. 1979. Problem-oriented record: A critical review. Paediatrician 8:152–162.
McDonald, C. J., and W. M. Tierney. 1988. Computer-stored medical records: Their future role in medical practice. Journal of the American Medical Association 259:3433–3440.
McDowell, I., and C. Newell. 1987. Measuring Health: A Guide to Rating Scales and Questionnaires. New York: Oxford University Press.
Nelson, E. C. 1990. Using outcomes measures to improve care delivered by physicians and hospitals. Pp. 201–211 in Effectiveness and Outcomes in Health Care, ed. K. A. Heithoff and K. N. Lohr. Washington, D.C.: National Academy Press.
NRC (National Research Council). 1991. Computers at Risk: Safe Computing in the Information Age. Washington, D.C.: National Academy Press.
Roper, W. L., W. Winkenwerder, G. M. Hackbarth, and H. Krakauer. 1988. Effectiveness in health care: An initiative to evaluate and improve medical practice. New England Journal of Medicine 18:1197–1202.
Shortliffe, E. H., L. E. Perreault, L. M. Fagan, and G. Wiederhold, eds. 1990. Medical Informatics Computer Applications in Health Care . Reading, Mass.: Addison-Wesley Publishing Company.
Simborg, P. W., B. H. Starfield, and S. D. Horn. 1976. Information factors affecting problem follow-up in ambulatory care. Medical Care 14:848–856.
Starfield, B., D. Steinwachs, I. Morris, G. Bause, S. Siebert, and C. Westin. 1979. Concordance between medical records and observations regarding information on coordination of care. Medical Care 17:758–766.
Tierney, W. M., M. E. Miller, and C. J. McDonald. 1990. The effect on test ordering of informing physicians of the charges for outpatient diagnostic tests. New England Journal of Medicine 322:1499–1504.
Weed, L. L. 1968. Medical records that guide and teach. New England Journal of Medicine 12:593–600, 652–657.
Young, D. W. 1987. What makes doctors use computers? Discussion paper. Pp. 8–14 in Use and Impact of Computers in Clinical Medicine, ed. J. G. Anderson and S. J. Jay. New York: Springer-Verlag.