6
Program Design and Implementation
This chapter addresses issues of design and delivery of health and related services to improve reproductive health. We start by reviewing data showing the great variation in existing capacity and utilization of reproductive health services. Next we discuss organizational issues for reproductive health programs. Finally, we discuss an illustrative, generalized strategic plan for measures to improve reproductive health and describe steps that are being taken in two countries.
No one program design or service configuration can be formulated to promote reproductive health in all settings. Instead, given the limited empirical research available, we review and discuss the features of effective interventions. The chapter emphasizes the organizational setting for effective reproductive health initiatives, including the selection of prevention and treatment approaches, the advantages and disadvantages of service integration, and management by governmental and nongovernmental institutions. The experiences of past and ongoing large-scale health initiatives, in such areas as family planning, primary health care, child immunization, infectious disease control, and environmental sanitation, offer lessons in how to define and develop reproductive health programs. There is no technological or programmatical "magic bullet" for reproductive health care.
EXISTING SERVICE CAPACITY AND UTILIZATION
Almost all countries have some infrastructure in place to deliver related
maternal and child health (MCH) and family planning services at different levels of facility. Some have services for the prevention, diagnosis, and treatment of sexually transmitted diseases (STDs), though these are typically weak and poorly coordinated with other health services. Most countries also have health education or communication programs, though again the quality and funding is often low, and these efforts are poorly coordinated with other prevention and treatment services. Hence, organizing delivery for reproductive health services does not typically start from a zero base; rather, it requires strengthening coordination, linkage, or integration and diversifying existing services, as well as adding new ones.
Table 6-1 presents information on existing MCH and family planning service capacity obtained through the Demographic and Health Surveys (DHS) service availability module (SAM) administered either through direct facility visits or to key informants in sample clusters (communities). 1 In the eight countries, services are reasonably accessible to most clusters, at a facility within 30 kilometers. Coverage of basic services ranges varies widely across countries: for example, residents in 93 percent of the sampled clusters in Thailand have access to immunization services at a hospital, compared with only 35.2 percent of the Nigerian DHS clusters. In approximately one-half of the 624 clusters in Bolivia, residents have access to a constellation of six types of MCH services, as well as contraception, from a nearby hospital.2 These aggregate data only show availability of services at the community level, of course; they do not show the great variation in quality of services (Fisher et al., 1994) or in barriers to access that may exist.
The availability of contraceptive services is highly associated with the availability of MCH services. This pattern reflects the common practice of integration of contraceptive with MCH services in health facilities. These
TABLE 6-1 Maternal and Child Health and Family Planning Service Availability to Sample Clusters of Eight Selected Countries with DHS Data: in percent
|
|
|
|
Maternal and Child |
|
|
Country and Year |
Numbera (and type) |
Facilityb type |
Prenatal |
Delivery |
|
Bolivia |
624 |
Hospital |
54.3 |
54.6 |
|
1989 |
|
Health center |
72.4 |
50.3 |
|
|
|
Clinic |
30.1 |
38.0 |
|
|
|
|
|
|
|
Colombia |
181 |
Hospital |
|
|
|
1986 |
|
Health center |
|
|
|
|
|
Clinic |
|
|
|
|
|
|
|
|
|
Philippines |
744 |
Hospitald |
93.3 |
92.6 |
|
1993 |
|
Other facility |
96.9 |
65.6 |
|
|
|
|
|
|
|
Thailand |
192 |
Hospital |
|
|
|
1988 |
(rural) |
Health center |
|
|
|
|
|
Clinic |
|
|
|
|
|
Pharmacy |
|
|
|
|
|
|
|
|
|
Egypt |
120 |
Hospital |
29.2e |
33.3e |
|
1989 |
(rural) |
Government center |
88.3 |
85.8 |
|
|
|
Government family planning clinic |
43.3 |
40.0 |
|
|
|
Private family planning clinic |
10.0 |
1.7 |
|
|
|
|
|
|
|
Kenya |
508 |
Hospital |
71.6 |
71.5 |
|
1993 |
|
Health center |
78.5 |
60.0 |
|
|
|
Dispensary |
40.2 |
5.5 |
|
|
|
|
|
|
|
Tanzania |
319 |
Hospital |
50.2 |
50.8 |
|
1991 |
(mainland) |
Health center |
54.9 |
46.7 |
|
|
|
Dispensary |
81.2 |
73.0 |
|
|
|
|
|
|
|
Nigeria |
165 |
Hospital |
39.4 |
39.4 |
|
1990 |
(rural) |
Health center |
33.3 |
27.9 |
|
|
|
Clinicg |
37.6 |
36.9 |
|
a See text and footnote 1 for explanation of community (cluster) samples. b Nearest facility of each type within 30 kms. of cluster; in Bolivia, family planning services at nearest facility where available. c Any service. d Nearest hospital or nearest other health facility if nearest was not a hospital. |
||||
|
Health Services Offered |
|
|
|
|
|
|
Postnatal |
Immunization |
Rehydration |
Growth |
Other |
Family Planning |
|
54.6 |
46.2 |
52.1 |
49.4 |
|
54.8 |
|
67.8 |
68.3 |
58.0 |
70.2 |
|
58.8 |
|
37.5 |
10.1 |
24.2 |
23.6 |
|
28.5 |
|
|
|
|
|
|
|
|
|
|
74.6 |
|
76.8c |
76.8 |
|
|
|
59.1 |
|
59.1 |
86.2 |
|
|
|
37.0 |
|
44.8 |
30.4 |
|
|
|
|
|
|
|
|
93.0 |
90.6 |
|
|
|
90.0 |
|
93.5 |
97.3 |
|
|
|
94.2 |
|
|
|
|
|
|
|
|
|
93.2 |
|
|
95.3c |
95.3 |
|
|
69.3 |
|
|
69.3 |
69.3 |
|
|
58.3 |
|
|
|
72.4 |
|
|
79.2 |
|
|
|
90.6 |
|
|
|
|
|
|
|
|
|
13.3e |
34.2e |
|
39.2 |
77.5 |
|
|
82.5 |
88.3 |
|
92.5 |
66.7 |
|
|
37.5 |
41.7 |
|
45.8 |
90.8 |
|
|
2.5 |
7.5 |
|
17.5 |
49.2 |
|
|
|
|
|
|
|
|
|
72.0 |
|
|
|
67.3 |
|
|
79.3 |
|
|
|
76.6 |
|
|
43.1 |
|
|
|
40.7 |
|
|
|
|
|
|
|
|
48.3 |
53.0 |
45.8 |
52.0 |
|
50.8 |
|
45.8 |
53.6 |
0.0 |
54.2 |
|
55.2 |
|
54.9 |
82.1 |
0.3 |
80.9 |
|
79.3 |
|
|
|
|
|
|
|
|
39.4 |
35.2 |
32.1 |
20.6 |
26.1f |
37.6 |
|
30.3 |
41.2 |
36.9 |
23.6 |
30.3 |
21.8 |
|
31.5 |
29.1 |
27.3 |
16.9 |
18.8 |
20.0 |
|
e For all Egyptian facilities, availability of services based on reported number of clients for service type in past month. f Nutrition demonstration. g Health clinic, maternity center, or maternity home. |
|||||
data do not necessarily reflect the full availability of contraceptive supplies, which are often distributed through private stores and pharmacies and providers. Still, the concurrent availability of family planning and MCH care suggests that efforts to ensure availability of treatment for reproductive tract infections (RTIs), along with targeted information, education, and communication services, can be built on an existing service capacity.
Table 6-2 shows recent estimates of total fertility rates, infant mortality rates and perinatal mortality ratios, maternal mortality ratios, and service utilization for countries and subnational regions where there have been DHS surveys. Along with wide variation of mortality rates, there is wide variation in estimates of service utilization. Prenatal care coverage
TABLE 6-2 Selected Reproductive Health Outcomes and Service Utilization for 51 Demographic and Health Surveys
|
Country |
TFR |
MMR |
IMR |
ANC |
DEL |
CPRM |
PMR |
|
Botswana |
4.9 |
250 |
37 |
92 |
77 |
32 |
25 |
|
Burkina |
6.9 |
930 |
94 |
59 |
42 |
4 |
80 |
|
Burundi |
6.9 |
1300 |
75 |
79 |
19 |
1 |
60 |
|
Cameroon |
5.8 |
550 |
65 |
79 |
64 |
4 |
75 |
|
Central African Republic |
5.1 |
700 |
97 |
67 |
46 |
3 |
80 |
|
Eritrea |
6.1 |
— |
— |
49 |
21 |
4 |
— |
|
Ghana |
5.5 |
740 |
66 |
86 |
44 |
10 |
90 |
|
Ivory Coast |
5.7 |
810 |
89 |
83 |
45 |
4 |
55 |
|
Kenya |
5.4 |
650 |
62 |
95 |
45 |
27 |
45 |
|
Liberia |
6.7 |
560 |
144 |
83 |
58 |
6 |
130 |
|
Madagascar |
6.1 |
490 |
93 |
78 |
57 |
5 |
65 |
|
Malawi |
6.7 |
560 |
134 |
90 |
55 |
7 |
70 |
|
Mali |
7.1 |
1200 |
108 |
31 |
18 |
1 |
100 |
|
Ondo Nigeria |
5.9 |
— |
56 |
80 |
59 |
4 |
— |
|
Namibia |
5.4 |
— |
57 |
87 |
68 |
26 |
60 |
|
Niger |
7.4 |
1200 |
123 |
30 |
15 |
2 |
100 |
|
Nigeria |
6.0 |
1000 |
87 |
57 |
31 |
4 |
90 |
|
Rwanda |
6.2 |
1300 |
85 |
94 |
26 |
13 |
65 |
|
Senegal |
6.0 |
1200 |
68 |
74 |
47 |
5 |
80 |
|
Sudan |
4.7 |
660 |
70 |
70 |
69 |
6 |
55 |
|
Tanzania |
6.3 |
600 |
92 |
92 |
53 |
13 |
65 |
|
Togo |
6.4 |
420 |
81 |
82 |
46 |
3 |
90 |
|
Uganda |
6.8 |
1200 |
— |
91 |
38 |
8 |
70 |
|
Zambia |
6.5 |
940 |
107 |
92 |
51 |
9 |
70 |
|
Zimbabwe |
4.3 |
570 |
53 |
93 |
69 |
42 |
40 |
|
Bangladesh |
3.4 |
850 |
87 |
26 |
10 |
36 |
85 |
|
Egypt |
3.6 |
170 |
— |
39 |
46 |
46 |
45 |
|
Indonesia |
2.9 |
650 |
57 |
82 |
37 |
52 |
45 |
|
Jordan |
5.6 |
150 |
34 |
80 |
87 |
27 |
30 |
|
Kazakstan |
2.5 |
60 |
— |
92 |
99 |
46 |
30 |
|
Country |
TFR |
MMR |
IMR |
ANC |
DEL |
CPRM |
PMR |
|
Morocco |
3.3 |
320 |
62 |
45 |
40 |
42 |
45 |
|
Pakistan |
5.4 |
340 |
91 |
26 |
19 |
9 |
70 |
|
Philippines |
4.1 |
280 |
34 |
83 |
53 |
25 |
25 |
|
Sri Lanka |
2.7 |
140 |
25 |
97 |
87 |
41 |
25 |
|
Thailand |
2.2 |
200 |
35 |
77 |
66 |
64 |
20 |
|
Tunisia |
4.2 |
170 |
50 |
58 |
69 |
40 |
40 |
|
Turkey |
2.7 |
180 |
53 |
62 |
76 |
35 |
50 |
|
Yemen |
7.7 |
1400 |
83 |
26 |
16 |
6 |
70 |
|
Bolivia |
4.8 |
650 |
75 |
53 |
47 |
18 |
55 |
|
Brazil |
3.4 |
220 |
76 |
74 |
— |
57 |
45 |
|
Northeast Brazil |
3.7 |
— |
75 |
64 |
70 |
54 |
— |
|
Colombia |
3.0 |
100 |
28 |
83 |
85 |
59 |
25 |
|
Dominican Republic |
3.3 |
110 |
43 |
97 |
92 |
52 |
35 |
|
Ecuador |
4.2 |
150 |
58 |
70 |
61 |
36 |
45 |
|
El Salvador |
4.2 |
300 |
71 |
— |
86 |
45 |
35 |
|
Guatemala |
5.1 |
200 |
51 |
53 |
35 |
27 |
45 |
|
Mexico |
4.0 |
110 |
47 |
71 |
70 |
45 |
40 |
|
Haiti |
4.8 |
1000 |
74 |
68 |
46 |
13 |
95 |
|
Paraguay |
4.7 |
160 |
34 |
84 |
66 |
35 |
40 |
|
Peru |
3.5 |
280 |
55 |
64 |
53 |
33 |
35 |
|
Trinidad and Tobago |
3.1 |
90 |
26 |
98 |
98 |
44 |
— |
|
NOTES: TFR = total fertility rate; MMR = maternal mortality ratio; IMR = infant mortality rate; ANC = antenatal care; DEL = proportion of births delivered by medically trained attendant; CPRM = modern contraceptive prevalence; PMR = perinatal mortality rate. SOURCE: Data from Demographic and Health Surveys and World Health Organization and UNICEF (1996). |
|||||||
is notably high, but these estimates do not gauge the quality or adequacy of that care (see Chapter 5). Some countries, such as Trinidad and Tobago, the Dominican Republic, and Kazakstan, have already achieved very high rates of attended deliveries, while rates are far lower in countries such as Mali, Niger and Pakistan.3 Utilization of reproductive health
|
3 |
Unfortunately, reliable direct estimates of maternal mortality ratios are available for only a small, unrepresentative sample of the countries shown in Table 6-2. The estimates reported here were imputed, or were adjusted, using models with fertility rates and proportions of births attended by trained personnel as independent variables (World Health Organization and UNICEF, 1996). Likewise, perinatal mortality ratios are imputed for many of these countries as proportions of total infant mortality, using variables highly correlated with those shown in Table 6-2. Because of this lack of independence of measurement or estimation, we cannot use these aggregate data to show how the service utilization models affect the demographic outcomes; nevertheless, the data suffice to illustrate the range among countries. |
services, particularly for RTI/STD treatment and prevention, is only superficially known, largely due to difficulties of measurement and incomplete reporting of service statistics.
As the limitations of these DHS SAM and household data indicate, national assessments are needed of the distribution, accessibility, quality, and acceptability of existing services for reproductive health concerns. Countries vary by mortality and morbidity conditions as well as levels of economic well-being.
LESSONS LEARNED FROM LARGE-SCALE HEALTH PROGRAMS
Reviews of effective organizational models for health programs often cast their conclusions in terms of lessons learned from what are considered ''best practices." Reviews of health program development in developing countries over several decades (e.g., Simmons and Lapham, 1987; Mosley, 1988; Bulatao, 1993; Liese, 1995) suggest that at least two factors can influence successful performance: a focused commitment to achieving program objectives and access to adequate resources. (Public-private partnership in service provision, a third important condition, is discussed in the next chapter.)
Focused Objectives
Commitment to promote and support a new health initiative can be demonstrated in different ways, such as vesting the health initiative under the authority of strong, capable and senior leadership; formulating or reformulating national policy; undertaking highly visible strategic planning, including the adoption of clear, explicit goals and objectives; or implementing an active and comprehensive agenda to achieve those program goals and objectives. The governments of Malaysia, Indonesia, Kenya, and Egypt, for example, elevated the visibility of their support for family planning services by placing them under the supervision of national coordinating boards or councils. In Egypt, India, and Indonesia, these programs eventually acquired ministry status. In Thailand, China, Brazil, and Uganda, HIV / AIDS, schistosomiasis, tuberculosis, malaria, and other communicable diseases have received specialized status in central ministries of health. Such commitment to program visibility, strategic management and institution building will be required for reproductive health programs to achieve their goals.
As much as political or managerial commitment can influence health program performance, the ability to monitor results appears to be equally important. As Liese (1995:352) comments, "Successful disease control
organizations would tend to be production organizations" which adopt a "clear result orientation and a sharp focus on measurable disease control activities." Measurable results provide program management with an unambiguous means of gauging performance. Access to trend information on performance indicators provides decision makers with a standard basis by which to determine the adequacy and efficiency of their efforts. Other large-scale health programs focused on disease control—STDs/HIV, malaria, and tuberculosis, for example—have benefitted from registry data on new and recurring infection cases to calculate incidence and fatality rates. Child immunization programs have diligently monitored levels of immunization through rapid assessment and national health surveys (UNICEF, 1995). Family planning programs similarly monitor the contraceptive prevalence rate and method mix to assess the extent of contraceptive practice, while MCH programs have emphasized infant and child mortality rates, antenatal and delivery care coverage, and children's nutritional status as the key indicators of their performance.
Reproductive health programs will likewise benefit if their achievement can be defined and measured. Given the diversity of programs, a single comprehensive indicator is unlikely to prove useful. Reproductive health programs may target outcomes, such as reduction in STD/HIV prevalence, increased contraceptive practice, universal prenatal care and child immunization, increased levels of obstetrical complications managed by medical staff, and elimination of maternal mortality.
An emphasis on measurable program achievements does have some risks. The pressure on workers to achieve simple targets could lead to coercion of clients and distortion of fundamental objectives. For example, family planning workers given method-specific targets, or targets for numbers of acceptors of all methods, may not have direct incentives to ascertain client needs and inform them about all options. They may even have perverse incentives for fraud or aggressive promotion of contraceptives. Effective reproductive health programming will require a reorientation of existing MCH, family planning, and STD services toward the health needs of women, newborns, and men in terms of service quality standards. An example is India's experience with replacing contraceptive acceptors targets for its family welfare program (see Townsend and Khan, 1996).
The program evaluation literature suggests that managerial focus on achieving measurable results will tend to strengthen the chances of effective program implementation. An initial challenge to reproductive health programs is for them to determine which synergistic, measurable results can be feasibly pursued.
Adequate Resources
Health initiatives have foundered because insufficient resources were allocated. Some, like the primary health care movement and safe motherhood, seem to have stalled for lack of organizational and financial resources. Obstetric care has been an underemphasized component of MCH programs. International assistance has traditionally given priority to contraceptive services, MCH (primarily for antenatal care and traditional birth attendant training), and nutrition, with less than 1 percent going toward obstetric care (Nowak, 1995).
In order to build the institutional and administrative capacity to implement an effective reproductive health program, new or re-invigorated health initiatives must be sufficiently supported in terms of personnel, financing, materials and equipment, medical supplies, and information. Costa Rica, for example, increased its public expenditure on health care coverage from 4.5 percent in 1972 to 7.5 percent in 1981 and 8.0 percent in 1991 (World Bank, 1985, 1993). Between 1970 and 1980 Costa Rica enjoyed a 71 percent decline in infant mortality from 68 to 20 deaths per 1,000 births (Rosero-Bixby, 1986). As Chapter 7 shows, a package of reproductive health services can be provided at a per capita cost that is within the reach of many governments. 4
ORGANIZATIONAL ISSUES FOR REPRODUCTIVE HEALTH PROGRAMS
Three organizational issues cut across the types of reproductive health services we have discussed in preceding chapters: the scope or breadth of services, service intergration, and the need to inform potential clients and create demand for unfamiliar services.
Breadth of Services
Several international organizations have recently proposed combinations of services for reproductive health programs, either generic programs or for particular countries (e.g., World Health Organization, 1994; Measham and Heaver, 1996). A prominent example is the Mother-Baby Package, a package of reproductive health services (described in Chapter 7 and Appendix C). The breadth and scope of the services to be delivered presents a formidable challenge in design, execution, administration, and evaluation.
Table 6-3 shows a possible allocation among community-based activities and levels of facility in the health system of the major health-sector interventions discussed in the preceding chapters. For this table (and for the cost models described in Appendix C), we assume that there are three levels of health care facility, although in several countries, particularly for urban populations, a two-tier system is used. Each of the major categories of reproductive health intervention involves tasks for each of the levels of the system; the higher level facilities need to be able to perform the functions of lower-level facilities as well, since in practice very few hospitals exclusively treat serious cases referred from health centers.
Several interventions and treatments listed are known to be effective in addressing a number of key sexual and reproductive morbidities. Some of these services are needed continuously over an adult's reproductive lifetime, while others are necessary only during various stages of reproduction, such as after conception, during and after pregnancy, or for the newborn. For example, postconception services may include pregnancy testing and counseling and induced abortion, as well as postabortion services for family planning and STD prevention. Postabortion care is important for the treatment of complications and prevention of additional unwanted pregnancies. Coordination could also require training staff, especially at the field level, in multiple technical areas to provide high-quality, competent and comprehensive reproductive health care to clients. In some cases, this may best be accomplished by using MCH/family planning workers to emphasize specific tasks known to be effective, while deleting other less effective ones.
The interventions shown in Table 6-3 will require coordination and linkage across levels and within the relevant service clusters. Those addressing fertility through postconception services should be coordinated with those addressing pregnancy health. For example, the latter might involve three clusters of services: (1) prenatal care, such as nutrition counseling and supplements, screening for syphilis and other STDs, treatment of these infections, maternal tetanus immunization, fetal monitoring for intrauterine growth, and delivery planning; (2) delivery care, particularly, referral for complications, attended delivery by trained personnel especially for complications, appropriate instrument delivery, and immediate newborn care, including prophylaxis for neonatal ophthalmia; and (3) postpartum care, such as lactation and nutrition counseling, infection control, and family planning.
The simultaneous delivery of different clusters of services at different levels of the health care system imposes major demands on clinical and nonclinical training, acquisition and distribution of essential drugs, contraceptives, nutrition supplements and equipment, worker supervision, and client record-keeping. Program planners must achieve an operational
TABLE 6-3 Illustrative Division of Reproductive Health Interventions Among Levels of the Health Care System
|
Health Intervention |
Community Level |
Health Post |
Health Center |
District Hospital |
|
Prevention of Violence, Promotion of Healthy Sexualitya |
IECb about violence, sources of support; IEC about health effects of female circumcision (where needed) |
Treatment of victims, referral to sources of legal and community support |
Treatment of victims, referral to sources of community support |
Treatment for severe cases |
|
Prevention and Management of RTIs/STDs |
IEC messages on symptoms; Promotion of safe sex, partner reduction; Condom distribution |
Syphilis testing and treatment for pregnant women; Partner notification and referral; Syndromic management (vaginal discharge, lower abdominal pain, genital ulcers, etc.); Infection control |
Syndromic management (vaginal discharge, lower abdominal pain, genital ulcers, etc.); Infection control |
Laboratory diagnosis and treatment of RTIs; Infection control |
|
Prevention and Management of Unintended Pregnancies |
IEC for contraceptive methods; Community-based distribution; social marketing of condoms, oral pills |
Counseling/screening for contraception; Counseling and referral for menstrual regulation or abortion; Provision of injectable contraceptives, IUD insertions; Counseling and treatment of contraceptive side effects |
Menstrual regulation/MVA abortion; Performing surgical contraception on set days; Post-abortion counseling and contraception; Counseling and treatment of contraceptive side effects |
Surgical contraception; Abortions through 20 weeks, where indicated; Post-abortion counseling and contraception |
compatibility among service clusters, availing themselves of possible arrangements for linkage, coordination, or integration. Their decisions can be guided by establishing targeted levels of effectiveness in terms of outreach and coverage and by defining measurable outcomes and developing protocols to guide activities of staff by type of facility.
Hardee and Yount (1995) identify potential linkages among traditional health programs that can strengthen access to reproductive health services. For example, an aim to reduce the level of unsafe abortion could explicitly involve linking family planning and maternity care services with information, education, and communication programs to generate demand for family planning prior to conception. Clients obtaining induced abortions or postabortion care would be provided or referred to family planning services. This linkage would mean coordinating the service provision of the two programs, including defining referral guidelines for abortion clients. Similarly, because STDs increase the probability of a potentially fatal ectopic pregnancy, STD management services could be coordinated with family planning by having former STD clinics automatically provide contraceptive counseling and supplies to male and female clients at risk of unwanted conceptions and having family planning clinics screen for gonococcal and chlamydial cervicitis.
Integration of Services
To what extent services should be integrated is a central issue in reproductive health care (e.g., Hardee and Yount, 1995; Pachauri, 1995). By virtue of its broad definition, reproductive health includes services traditionally offered through a number of categorical programs, particularly those responsible for managing STDs and pregnancy and maternal health problems.
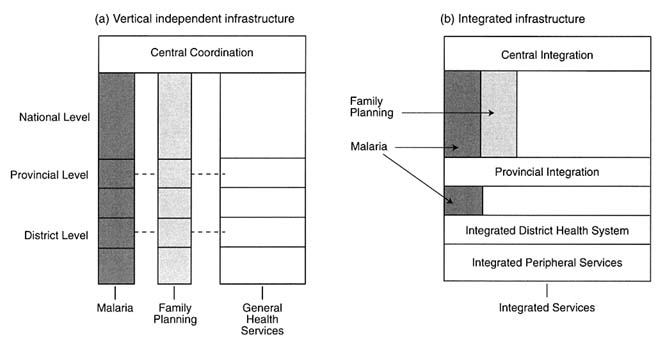
Smith and Bryant (1988) illustrate two types of integration, using malaria and family planning programs as examples (see Figure 6-1). Both kinds of programs have enjoyed a certain degree of autonomy within public health programming, largely due to their access to financial and material resources, some of which has been externally available from international donors. In panel (a), malaria and family planning programs are two of three (with general health services) program blocks; each is administered and implemented somewhat autonomously and has different field staff. In panel (b), the two programs are independently administered at the central level, but their services are delivered in an integrated manner by multipurpose field staff. Reproductive health programs, if organized along highly vertical lines, might resemble one of the columns in panel (a). In the configuration shown in panel (b), in contrast, reproductive health would maintain some separate identity near the central
level of administration but have its services delivered by the same field personnel who are responsible for other general health services. These two forms of service organization have been variously called the "hour glass" shape (b) or "broken zipper" model (a) (Cleland et al., 1994). The question of which structural configuration provides the most synergistic and efficient use of resources is often cast in terms of verticality versus integration.
Integrating formerly categorical programs in an overall reproductive health program may require little more than a reorganization of administrative authority and reallocation of resources for the delivery of relevant services. Such rearrangements could demand a greater degree of political and administrative support than is required to deliver a completely new medical treatment or technology. Bureaucratic inertia or territorial priorities may resist or thwart reorganization efforts (Simmons and Phillips, 1987). To the extent medical protocols are involved, physician versus nonphysician control of relevant technologies and therapies within programs can inhibit efforts to combine them. In Bangladesh, for example, attempts to link child immunization and other health functions to family planning outreach—to make outreach sites better known and used by rural women—have been only moderately successful because at the operational level they require a great deal of coordination of plans between physicians in the health wing of the Ministry of Health and Family Welfare and nonmedical family planning officers in the family planning wing (Haaga and Maru, 1996).
Some services need to be organized as vertical programs because they are meant to reach geographically concentrated or otherwise distinct populations. Programs for persons at high risk of STDs, such as sex workers, for example, would benefit little from integration into general health services. Programs for adolescents and for men may include some that benefit and others that do not benefit from linkage to programs reaching married women. The perceived needs of clients, their convenience, and concerns for privacy, have to be considered, not just operational efficiency and administrative convenience. In contrast, programs designed to provide complementary services for neglected health problems to populations already in contact with the health or family planning services would be particularly good candidates for integration into existing programs, rather than the setting up of new vertical programs. Detection and treatment of syphilis in pregnant women and syndromic management of RTI symptoms are clear examples.
Some of the functions discussed in the preceding chapters might usefully be considered as partially integrated. For example, the provision of essential care of obstetric complications requires facilities, equipment, and trained personnel that will not be available at sites providing the first
level of care in family planning or prenatal care. But implementation of that essential care is likely to require efforts to stimulate community awareness of complications and of where to seek treatment; all first-line health care providers, for both women and men, could usefully have this educational role added to their duties.
Inevitably, additional integration issues will be confronted at the field level, where health personnel and facility resources do not usually expand in proportion to the service demands entailed by new or combined categorical programs. Smith and Bryant (1988:917) note:
It is also here [at the district health system] that the multitude of special programs found at the national level often falls on the shoulders of a small team charged with numerous responsibilities for promotive, preventive, curative, and rehabilitative services for a local community. It is thus here that integration usually occurs by necessity, if not choice. It is also often at the health center or clinic that the conflicting demands of many specialized programs are resolved, for better or worse, by arbitrary decisions.
Mercenier and Prevot (1983) similarly view integration as the assumption of operational responsibility by the health workers who are best suited for particular tasks. They suggest that the process of integration too often has been considered an administrative problem of structures, while complex human resources issues—such as the orientations and practices of health workers—have been overlooked. Thus, integration of services, while appealing as an organizing rationale for reproductive health care, is not a panacea. The quasi-experimental literature on integration of services shows mixed results (Simmons and Phillips, 1987).
A number of service delivery issues can arise with integration (Hardee and Yount, 1995): (1) adequacy of the existing health infrastructure and referral procedures to overcome weaknesses; (2) need for continuous medical support, supplies, and logistics; (3) provision of accurate and up-to-date service delivery guidelines; (4) integration of records systems, primarily at the district level and below; (5) delegation of tasks downward to overcome staff shortages and decrease the physical distances to reaching women; and (6) ensuring the adequacy, competency, and supervision of service personnel. The capacity-building aspects of reproductive health programs will need to address escalating demands for crosstraining of field health personnel with the lateral inclusion of more technical and specialized services.
Although the need for reallocation of resources for such program or service combinations seems self-evident, relatively little empirical research is available on how to effect compatible structures. Cates and Stone (1992) note fundamental differences in the characteristics of clients
receiving RTI and family planning services, from those receiving other services and variation in service ''cultures": the risks of RTIs and of unintended pregnancies both involve sexual contact and both are higher for younger than for older individuals. Important gender differences exist in that women bear the physiologic responsibility of pregnancy, are more susceptible to sexually-transmitted infection by men than the reverse, and are less symptomatic than men. Yet men make up three-quarters of the clients at STD clinics, since they are more likely to recognize symptoms and more likely to seek health care. Sensitizing clinic and outreach staff to the varying profiles of populations at risk of RTIs and STDs and unwanted pregnancies will be necessary.
Health services to prevent RTIs and STDs have different orientations. Family planning counseling tends to be less directive than STD counseling. Because STDs are communicable diseases that can spread rapidly in subpopulations, STD clinics are more likely to operate as urgent care facilities, providing immediate, short-term treatment to infected clients and their sex partners. Family planning clinics, in contrast, adopt a stance more appropriate to preventive care: they exist to support clients' proactive efforts to avoid unintended conception. Different therapies (antibiotic versus hormonal or surgical treatment) for the two types of services also require different technical skills on the part of providers. There can be conflicting goals, as well. Barrier contraceptive methods, which are not considered particularly efficacious for prevention of unwanted pregnancy, offer the greatest protection against STDs. Until female-controlled contraceptive methods are developed that can protect against both STDs and unwanted pregnancy, encouraging clients to use barrier methods exclusively may challenge the operating philosophies, service attitudes, and policies of many family planning providers (Daley, 1994). The likelihood of achieving full-scale, service-level compatibility in family planning and STD clinics, or similar linkages, ultimately may depend on the degree to which interest in and commitment to comprehensive reproductive health care permeate all levels of the program infrastructure.
A key question concerning integration is whether separate services are needed for women and men, young people, (particularly unmarried young people), and married couples. Again, no simple generalization is possible; both integration and separation have their advantages, and they have different weight in different cultures. There are advantages to specialization by clinic staff and counsellors, comparable to the advantages of "audience segmentation" in mass communications. Clients' (and sometimes providers') embarrassment and stigmatization are often barriers to the use of reproductive health services, but only local experience can show whether these are minimized by having separate waiting areas, clinic times, or buildings, or whether separating services in this way actually
increases embarrassment for those seen to be using the services. Young people may have fewer opportunities or socially acceptable reasons for trips to specialized health facilities or pharmacies, and so would have to be reached in fixed or mobile clinics located in or near schools or workplaces. Where there is significant opposition to particular services, like abortions, contraception, and STD treatment for unmarried people, their health rationale may be emphasized by integration with other health services.
Concern with minimizing the social burden on clients is not only important for overall questions of strategy and program design; it should also influence management and quality assurance. Family planning clinics have been criticized for a lack of concern about privacy and waiting times and places (Bruce, 1990), and the same criticism could be directed against other health facilities in many countries. Program managers need not take embarrassment and stigmatization as givens in the social environment in which they are working; rather, need to understand it can be reduced by the arrangements of waiting spaces and consultation and examination areas, and by improving patient and record flow. For example, Marie Stopes clinics providing women's health care in several developing countries, including some where other health services pay little heed to client privacy and confidentiality of records, have shown that this is possible (Toubia, 1995).
The reproductive health movement has emerged out of a microlevel orientation, namely, providing care for all reproductive concerns of women. Hence, issues of service integration for reproductive health may revolve more around organizing services to be client-oriented and accessible in one place at one time or through referral links. To what extent these are the service utilization preferences of women and men needing and seeking such care is an important research issue.
Decentralization
Like service integration, decentralization, popularized during the primary health care movement, has both advantages and disadvantages (Smith and Bryant, 1988). Among the former is that it puts authority in the hands of managers, often at the district level, who are better acquainted with local conditions than managers in central organizations. A lower tier administrative unit may be more responsive to the needs of local users and accountable for the consequences of the unit's decisions. Decentralization may offer resource flexibility and facilitate capacity building by adapting training investments to local needs. Decentralization shifts accountability to district managers and planners, providing them with increased authority and responsibility to address local needs.
Among their disadvantages, decentralized services do not exploit economies of scale, and they require greater management capabilities. Evidence of the overall effectiveness of decentralization schemes is mixed (Heaver, 1995). Smith and Bryant (1988) argue that the district health system is a useful compromise between centralization and complete decentralization. They recommend that authorities at the district level set priorities and design and implement centrally defined health interventions. Yet as population needs in STD management and treatment and pregnancy and nutrition care are likely to vary geographically, some degree of decentralization may be useful for reproductive health program design.
Neither integration nor decentralization guarantees an effective program. A strong achievement orientation can produce success in a variety of service configurations:
What the study could not [author's italics] find was that organizational structure in itself influences effectiveness. … Based on the empirical research, the main conclusion was that there is no best structure to organize disease control programs (Liese, 1995:357).
The differences between these approaches [vertical or integrated] frequently seem exaggerated and misconstrued. … As such it is a bureaucratic argument and the divisionary effects of a selective approach on the development of sustainable and efficient health services have been overlooked (Gish, 1992:183-184).
Generating Demand for Reproductive Health Services
Partly due to past neglect of many needs in reproductive health, services are often unfamiliar and poor in quality. Reproductive health care providers need to stimulate the demand for services at the same time that they are meeting the demand. This is especially true for essential care for obstetric complications, but it also applies to better quality family planning services and programs for prevention and treatment of RTIs. Processes surrounding sex and reproduction are especially likely to be considered natural and unalterable, not as symptoms of treatable illness. Because women tend to suffer many reproductive morbidities—sexually transmitted disease, pregnancy and delivery complications, and unwanted sex—in a "culture of silence" (Khattab, 1992), effective demand for treatment may be very low in the initial stages of the reproductive health programming. Individual awareness of symptoms, available services, and motivation to treat any infections or undesirable outcomes may be fairly minimal.
An important lesson from the history of family planning programming is the social legitimation of new types of health care that can be
conferred by high levels of political commitment and by specific demand-generation activities. As Cleland and Wilson (1987) point out, ideational change was crucial for the fertility transition in developing countries, as couples became aware of their ability to regulate childbearing. Whether through commercial mass media or public information, education, and communication campaigns, exposure to family planning and health messages can influence reproductive attitudes and preferences and promote healthy behaviors. Interpersonal contact with outreach workers from social and health programs may help form and crystallize latent demand for reproductive health improvements. Significant results from this type of program intervention have been observed for family planning in some countries (Simmons and Phillips, 1992).
Reproductive health programs would benefit from population-based evidence of clients' needs for reproductive health care. Informational, educational, communication, and promotional activities are needed to strengthen and motivate health-seeking and help-seeking behavior on the part of client populations. A significant disparity between the projected prevalence of reproductive health morbidities and individual recognition of and motivation to seek treatment can be a costly problem. Early investments in coordinating, linking, or establishing various service infrastructures, such as STD and family planning clinics, may take place but quickly be seen as an inefficient use of resources if adults at risk do not seek care through these facilities. Clients must be able and want to connect their ailments to available care and obtain effective treatment. Awareness-raising and demand creation activities could target health practitioners and service providers as well, since too often the latter's own technical limitations, attitudes, and predispositions toward particular therapies prevent women and men from receiving appropriate care and referral. For example, maternity care providers may blame women for seeking late treatment for health problems, such as obstetrical complications.
An advantage of having a full complement of reproductive health services can be the increase in the number of opportunities for contact. A health care worker's visit with a new mother for postpartum counseling is an opportunity to speak with her about her own nutritional needs, family planning in the context of STD prevention needs, breastfeeding, child immunization, and so on. This outreach, through childhood and the sexual and reproductive lifetime of adults, exposes household members to reproductive health information and counseling. As a result, demand and motivation for such care may increase.
Quality assurance for more complicated services should become easier once both the public and the providers learn to expect decent services and accountability. Creation of demand for services should be seen
as a concomitant to the "supply-side" interventions, not as a precondition for them.
IMPLEMENTING REFORM OF HEALTH SERVICES
How then should program designers and managers proceed to select among possible interventions to improve reproductive health? Given the lack of detailed empirical studies in a wide variety of settings, judgment must be informed by professional experience, practical considerations, and broad generalizations. McGinn et al. (1996) suggest a framework for setting priorities in international reproductive health programs that includes six key factors: (1) the severity, magnitude and consequences of the reproductive health problem; (2) the relative efficacy of potential interventions; (3) the program requirements, in terms of appropriate sites or facility levels; (4) the marginal costs of introducing and sustaining the interventions relative to population covered; (5) the capacity of four components of the health system—human resource management, support and supervision, logistics, and financial management; and (6) the context of cultural, policy and legal constraints.
One approach that has proved useful in public health both in calling attention to goals and in translating broad goals into a sequence of actions for which managers can be held accountable is to set out measurable objectives, with a timetable for reaching them. The "Healthy People" objectives for the year 2000 for the United States are an example. Some of the objectives have been achieved or will be achieved before that year; others almost certainly will not be achieved. In a federal system where subnational levels of government have significant roles in public health, the private sector provides most health care, and education and other sectors must be involved, there is an advantage to having such objectives clearly stated so all the participants can refer to them over the course of a long effort. Such objectives have been set at a global level as well, for example, at the world summit for children in 1990, when representatives of governments and international agencies committed to trying to achieve reductions of specified percentages in infant and child mortality rates, maternal mortality rates, and prevalence of protein-energy malnutrition and micronutrient deficiencies.
The International Conference on Population and Development in 1994 did not specify new global objectives for reproductive health. Likewise, we do not believe that such a global effort would be useful at this stage. As we argue in the preceding chapters, there are common goals for reproductive health, but the nature and severity of specific problems, and the resources to overcome them, vary greatly across settings. Without meaning to detract from commitment to global objectives already adopted, we
recommend that governments of developing countries adopt a national-level process to specify objectives and timetables, specifying the strategies to achieve them and the agencies and communities that are expected to help achieve them.
Table 6-4 gives an example of what the outcome of the process could be. The first column lists the positive goals of reproductive health that were used as the vision for this report. The second column lists specific objectives, which can be either instrumental, intermediate steps toward these goals, or measurable changes in indicators of reproductive health in the population at large. These objectives should have some target date attached. The third column lists examples of strategies designed to achieve the objectives, and the fourth lists "critical partnerships," agencies and segments of the population needed to put the strategies into action. This last column highlights the importance of intersectoral involvement for the success of an expanded concept of reproductive health. The partnerships need to be specified, since most of the strategies would be unworkable as "top-down" or single-agency missions. Each of the strategies listed here would also have implications for applied research and training needs.
The advantage in linking goals, objectives, and strategies this way is partly that it helps synthesize what could otherwise be a long, incoherent list of isolated actions. It also helps avoid the problem, called suboptimization by economists, whereby agencies focus on objectives too narrowly defined, or stated only in terms of their own outputs, to the detriment of the larger social goals they were meant to serve.
The process of tailoring and completing such a table to make it relevant to local conditions itself could be valuable by stimulating new collaboration and data-based decision making. Leadership and political commitment would be required, but a purely top-down process would be unlikely to achieve much, since most countries already have a sufficient stock of policy pronouncements, plan documents, similar materials. Any such table would need to be revised periodically. There is hope that technical advances—diagnostic tests for STDs, microbicides, new contraceptives—will radically change the "menu" of cost-effective interventions in ways we cannot now foresee. If the reproductive health movement gains strength in a country, the list of relevant actors would also change, to include new nongovernmental organizations, community groups, and professional associations, new agencies or interagency task forces, and the like. A table like this would be put to good use if the first column changed not at all, the second column changed only very slowly as old objectives are achieved or new ones set, and the other columns are updated continually.
Table 6-4 is illustrative; the panel anticipates that the entries in this
TABLE 6-4 Illustrative National-Level Objectives for Reproductive Health
|
Goal-Specific Objectives |
Strategies to Achieve Objectives |
Critical Partnerships |
|
(1) Reproductive Health Goal: Every sex act free of coercion, and based on informed and responsible choice |
||
|
Eliminate commercial sex involving children, by [year] |
Enforcement of existing laws and penalties for sexual exploitation of children |
Police and judicial system, Newspaper editors and reporters, parent groups, religious leaders, nongovernmental organizations working for children |
|
Reduce incidence of female genital mutilation by [proportion], by [year] |
Information campaign about health consequences of female genital mutilation |
Public- and private-sector health care providers, religious leaders, social-science and communication researchers |
|
Reduce percentage of women beaten by husband or partner by [proportion], by [year] |
Enforcement of laws; promotion of awareness of violence; better detection and treatment referrals in health and family planning clinics |
Police and judicial system, religious and other community leaders, health care providers, teachers |
|
Provide sexuality education appropriate to grade level in all schools, by [year] |
Develop and adopt appropriate curricula and other materials; train teachers and principals |
Parent associations, private-school associations, curriculum researchers and evaluators, religious leaders |
|
(2) Reproductive Health Goal: Every sex act free of infection |
||
|
Subgoal: Reduction of the number of sex partners |
||
|
Increase average age of coital debut to 17 years, by [year] |
Health promotion via mass media; health education in schools (with component to to build sexual negotiation skills); community-based peer intervention programs; legal sanctions against marriage at younger ages; legal sanctions against adults engaging in sex with minors |
Religious and lay community leaders; mass media (TV, radio, print media); community-based organizations ministry of education, teachers; behavioral interventions experts; judicial system; medical and family planning communities |
|
Decrease percentage sexually active persons who have had >1 sex partner in last 12 months by [proportion], by [year] |
Health promotion via mass media; health education in schools (with component to build sexual negotiation skills); targeted community-based intervention programs |
Religious and lay community leaders; ministry of education, teachers; mass media (TV, radio, print media); community-based organizations; behavioral interventions experts; medical and family planning communities |
|
Subgoal: Increased condom use |
||
|
Increase percentage consistent and correct condom use among sexually active persons <30 years old who have had >1 sex partner in last 12 months by [proportion], by [year] |
Condom social marketing; targeted, community-based intervention programs; health education in schools (with component on condom use); assure adequate condom supplies at all clinical and community distribution points |
Religious and lay community leaders; mass media (TV, radio, print media); community-based organizations; ministry of education, teachers; behavioral interventions experts; agency that sets import tariffs; pharmaceutical companies; medical and family planning communities |
|
Subgoal: Improved health education |
||
|
Increase percentage of population >12 years old who can correctly describe 2 ways to prevent STDs/RTIs by [proportion], by [year] |
Health promotion via mass media; health education in schools (with skills building component); targeted, community-based intervention programs |
Religious and lay community leaders; mass media (TV, radio, print media); community-based organizations; ministry of education, teachers; behavioral interventions experts; medical and family planning communities |
|
Goal-Specific Objectives |
Strategies to Achieve Objectives |
Critical Partnerships |
|
Subgoal: Improved counseling |
||
|
Increase the percentage of clients seeking family planning, STD, postpartum or primary health care services who also receive STD risk assessment and contraceptive method counseling for prevention of both infection and pregnancy by [proportion], by [year] |
Development and dissemination of guidelines on risk assessment and counseling for both pregnancy and infection tailored to local sociocultural context |
Behavior intervention experts and medical and family planning communities |
|
Subgoal: Improved STD/RTI management |
||
|
Increase the percentage of family planning, prenatal, and primary health care clients who are appropriately tested and treated for STDs and other RTIs by [proportion], by [year] |
Development and dissemination of STD/RTI detection and treatment guidelines at a minimum: abdominal, pelvic, and genital exams; syndromic management of STDs in symptomatic men and women using WHO algorithms; prenatal syphilis screening. Whiff (KOH) test; pH and microscopy of vaginal secretions strongly recommended for women with signs or symptoms of abnormal discharge. Tests for chlamydia and gonorrhea should be included if feasible.; Development and dissemination of guidelines for notification of sex partners of patients diagnosed with STDs.; Assure adequate laboratory and anti-microbial supplies in all clinics |
Medical and family planning communities, agency that sets tariffs, pharmaceutical companies, pharmacists, public and private laboratories, and behavioral interventions experts |
|
Subgoal: Infection Control |
||
|
Increase percentage of providers of delivery, IUD insertions, and abortion services who can document adherence to infection control guidelines by [proportion], by [year] |
Development and dissemination of infection control guidelines; assure adequate supplies and equipment |
Medical and family planning communities |
|
(3) Reproductive Health Goal: Every pregnancy and birth intended |
||
|
All couples have access to more than one method of effective contraception, by [year] |
Train providers in clinical methods; strengthen logistical system for resupply methods |
Public and private health care providers, family planning nongovernmental, pharmacists |
|
Young adults know about contraceptive options, where to obtain supplies/services and information about effective use, health effects, by [year] |
School health curricula; mass media (information, education, and communication efforts; public service announcements); health care/family planning provider training (initial refresher); packages for emergency contraception, train providers |
Family planning nongovernmental organizations, health care providers, social marketing agencies/mass media, teachers/principals/school administration, pharmacists |
|
All sexually active women have access to safe legal abortion in first trimester, by [year] |
Legalization of abortions; health care provider training and quality assurance |
Legislators; health administrators, quality assurance managers; health care providers |
|
Contraceptive supplies and services, and safe abortion and post-abortion care, affordable to the poor, by [year] |
Implement and monitor sliding-fee scales, outreach services in poor communities |
Legislators/taxpayers, health sector planners, hospital/clinic administrators, family planning program administrators |
|
Goal-Specific Objectives |
Strategies to Achieve Objectives |
Critical Partnerships |
|
(4) Reproductive Health Goal: Every pregnancy/birth safe |
||
|
Increase percentage of women with complications attended by trained medical staff by [proportion], by [year] |
Increase knowledge of warning signals, where to go in emergencies; increase availability of reliable transport to essential care for obstetric complications facilities; increase number of hospitals/clinics trained/ equipped to provide essential care for obstetric complications; institute targeted subsidies, reduce unauthorized fees |
Community leaders, teachers; first level health care providers; family planning workers |
|
Increase percentage of women with complications correctly managed by [proportion], by [year] |
Quality assurance/provider training (competency-based); eliminate financial incentives for inappropriate obstetric interventions |
Hospital/clinic administration |
|
Decrease clinic/hospital care fatality rate for women and newborns by [proportion], by [year] |
Quality assurance/provider training (competency-based); develop protocols |
Hospital/clinic administrators, medical education and licensing authority, health care providers |
|
Reduce prevalence of anemia among women aged 15-49 by [proportion], by [year] |
Distribution of iron/folate supplements in adequate amounts to all pregnant women; information, education, and communication campaign about iron-rich foods |
Health educators, mass communications, first-level prenatal care providers |
sample table will not prove to be the agreed reproductive health strategy for every country. In this spirit, we have avoided giving real target dates; these must be determined during the national-level process. The rationales for our choice of objectives and strategies is given in the chapters above; the table provides an overview to help in translating concepts to implementation steps. This is certainly not meant to be a comprehensive design for the health sector, nor an exhaustive list of current programs that promote one or another goal of reproductive health. However, it may be useful as a checklist or point of departure to ensure that a comprehensive reproductive health strategy is being built.
We have argued that the process of externalizing and reforming existing services and creating new ones to meet reproductive health needs will vary among countries. This process has already begun in many countries, of course. In the rest of this section we discuss examples of government efforts to implement a reproductive health agenda in Mexico and Uganda. The Mexican case highlights how organizational issues have been addressed to raise the visibility of reproductive health; the Ugandan case highlights steps taken to strengthen existing services in a very poor country.
Implementing a Reproductive Health Program in Mexico
Since 1974 the Mexican government has been strongly committed to achieving fertility reduction through a national family planning program (Riquer Fernandez, 1995). Currently, the public sector provides the majority (71%) of contraceptive users with their family planning methods (Pathfinder International, 1995). At the ICPD, Mexico endorsed the Programme of Action without reservations (unlike several other Latin American countries, which expressed reservations about some controversial sections dealing with reproductive rights and health) (United Nations, 1994).
After the ICPD, two formerly separate divisions of the Ministry of Health—maternal and child health and family planning—were merged into a new General Directorate of Reproductive Health. In addition, an intersectoral body that sets family planning priorities and monitors programs changed its title from the Interinstitutional Group on Family Planning to the Interinstitutional Group on Reproductive Health (GISR). The GISR includes all national institutions that provide health services, as well as the National Population Council, the Education Ministry, the family welfare program, and six nongovernmental organizations that are active in the women's health and rights movement—the Information Group on Reproductive Choice and the Safe Motherhood Committee. The GISR is the most recent incarnation of a coordinating body on family planning that dates back to 1976 (Martínez Manatou, 1994).
In 1995 the GISR issued a 5-year plan that incorporated several key aspects of the ICPD agenda—the Reproductive Health and Family Planning Program (Grupo Interinstitucional de Salud Reproductiva, 1995). The program defines reproductive health as ''the capacity of individuals and couples to enjoy a satisfactory, healthy and safe sexual and reproductive life, with the absolute freedom to decide in a responsible and informed manner on the number and spacing of their children." This definition comprehends a broad range of services: family planning; perinatal health; adolescent reproductive health; women's health; early detection and treatment of infertility and reproductive cancers; and prevention, detection and treatment of STDs, including HIV/AIDS. The document emphasizes improving quality of services, instituting a gender perspective in service delivery, ensuring reproductive rights, providing a wide range of method choices, and attending to previously ignored populations (adolescents, men, and indigenous peoples).
Several steps have been taken toward implementing an ambitious agenda. At least one of the major public health care providers, the Mexican Institute of Social Security (IMSS), has a structure that favors service integration. Most of its services for the insured population are provided by family physicians in primary care clinics called family health units. Therefore, family planning is integrated with other health services and has been for many years through the predominant role of the family physician. With the new policy framework, attempts are being made to integrate less traditional services, such as cervical cancer prevention and treatment and STD screening, into the family physicians' services. The other major provider of public health services in Mexico is the Ministry of Health, which serves the population not insured through social security. Various new programs have recently been introduced or gained renewed attention in the ministry, including maternal mortality committees in hospitals, postabortion care, and modules for adolescents.
There are several barriers to full implementation of this reproductive health and rights program. The government has expanded the range of family planning method choice somewhat; however, there is still a strong emphasis on physician-controlled, long-term methods. Clients who are using condoms, for example, are not counted as contraceptive users by most health institutions. This attitude toward barrier methods can be problematic in a country where HIV is a growing problem for women in stable unions—the traditional target groups served by family planning programs. The prevalence of STDs among the general population is unknown and, in general, STD programs have been neglected in Mexico. Nonetheless, the Mexican government has taken important steps to promote integration and expansion of reproductive health services in a context of serious economic constraints.
Strengthening Services for Reproductive and Maternal Health in Uganda5
With external assistance, the government of Uganda has begun an effort to strengthen health programs associated with childbirth and sexual behavior in selected districts. Through this new initiative, it expects to increase use of health services and adoption of behaviors to reduce unwanted pregnancies, HIV infection, and maternal and child mortality.
Under Uganda's newly decentralized government structure, the principal responsibility for the provision of primary health care rests with district administrations, although the central Ministry of Health retains policy making, quality control, technical support, and monitoring and evaluation functions and responsibility for all public hospitals. Most districts are ill-equipped to cope with prevailing reproductive health problems. The public health sector is characterized by low salaries, skills, and motivation of staff and insufficiencies in facilities, equipment, supplies, supervision, training and other support systems.
Projected government, donor, and household expenditures on health for 1996-1997 are about $202 million, about $10 per capita. Of this, about $36 million represent recurrent government expenses, another $36 million recurrent donor expenses, with the remaining $130 million being household expenditures. Nongovernmental organizations provide about 60 percent of the health care in Uganda and are often highly dependent on donor funding. There is very limited private-sector provision of modern health care outside urban areas, and few alternatives to public-sector services.
Despite the large proportion of public expenditure currently spent on hospitals, increased emphasis on primary care is an official priority. User fees are charged in most public-sector facilities. Although revenues collected are currently low and financial management procedures and controls are weak, the Ministry of Health now places a priority on local revenue generation, alternative financing mechanisms such as insurance, and increased private-sector provision of care.
The new reproductive/maternal health initiative has four specific objectives. The first is to increase the availability of services by expanding the number of public and private-sector clinical staff capable of providing an integrated package of reproductive/maternal health services. Integrated services will include:
-
family planning;
-
prenatal care, including screening for pregnancy complications;
-
maternal nutrition counseling, and tetanus vaccination;
-
intrapartum care, including safe deliveries, responses to common obstetric emergencies (along with complications of illegal abortions), and appropriate referral systems;
-
care of the neonate;
-
postnatal care, including the promotion of exclusive breastfeeding, optimal weaning practices, and full childhood immunization;
-
syndromic STD diagnosis and treatment, based on laboratory validation of management algorithms;
-
HIV testing and counseling, with integration of family planning and STD services; and
-
family planning, STD treatment, and counseling for HIV-positive individuals.
This first objective will support the provision of in-service training in the above areas as well as the improvement of preservice training capability at nursing, medical and paramedical schools. Community volunteers, including traditional birth attendants, will be trained to provide education and counseling related to family planning; maternal and infant health and nutrition, including the promotion of breastfeeding and proper weaning practices; and HIV and other STDs and to refer clients to clinics with trained providers. Volunteers will also sell condoms and oral contraceptives that are provided through a social marketing program. Traditional birth attendants are also to be trained to recognize signs of pregnancy complications and supervised by trained midwives. Continued emphasis will be placed on social marketing to increase the number of outlets selling contraceptives and antibiotics for STD treatment, as well as on upgrading the MCH logistics system that distributes such supplies to public facilities.
The second objective is improved quality of services, including improved, routine supervision of clinic and community-based service providers. Trained providers are to be observed during service delivery to assess compliance with formal standards and education and counseling techniques learned during training. The government plans to coordinate with and train district authorities and facility personnel to maintain and accurately report service statistics related to maternal and child health. This will enable monitoring the quantity of various services provided, their provision in an integrated manner, and compliance with service-delivery protocols (including those for STD treatment).
The third objective, enhanced sustainability of services, is to be achieved through several strategies, including standardized financial management systems at health facilities.
The last objective is to increase individuals' desire to use services and
adopt behaviors to improve reproductive/maternal health. Service utilization is to be promoted directly by providing accurate information about services and outlet location. Information, education, and communication efforts will concentrate on reducing perceived barriers to service use (such as rumors and misconceptions) and broadening public awareness of the availability and utility of HIV counseling and testing and the link between STDs and HIV. Other desired behavior changes (e.g., correct infant feeding, improved maternal nutrition, condom use, reduction in sexual partners, delayed sexual debut, spousal communication on reproductive health) are to be promoted by encouraging people to assess their risk for unwanted pregnancy, poor pregnancy outcomes, and HIV infection and to obtain care accordingly. Behavior change will also be promoted through mass media campaigns, including talk radio, serial dramas, and music and through similar local activities such as dramas, video shows, and music competitions.