APPENDIX A WHO Recommendations for Treatment of STD-Associated Syndromes
In 1991, the World Health Organization (WHO) (1991) published recommendations for the comprehensive management of patients with sexually transmitted diseases (STDs) within the broader context of control, prevention and care programmes for STD and human immunodeficiency virus (HIV) infection. A WHO Advisory Group Meeting on Sexually Transmitted Diseases Treatment subsequently reviewed and updated treatment recommendations in the light of recent developments (World Health Organization/UNAIDS, 1997). This appendix presents the revised recommendations for a syndromic approach to the management of patients with STD symptoms. It discusses the management of the most common clinical syndromes caused by sexually transmitted agents and provides flow charts (algorithms) for the management of each syndrome.
The use of appropriate standardized protocols is strongly recommended in order to ensure adequate treatment at all levels of health service. Such standardized treatment also facilitates the training and supervision of health providers, delays the development of antimicrobial resistance in sexually transmitted agents, such as Neisseria gonorrhoeae and Haemophilus ducreyi, and is an important factor in rational drug procurement.
For all these conditions (except vaginitis) the sexual partner(s) of patients should also be examined for STDs and promptly treated for the same condition(s) as the index case. Partner notification and management are considered in the full report of the WHO Advisory Group (World Health Organization/UNAIDS, 1997).
Note. The therapies for uncomplicated gonorrhea, syphilis, chancroid, and granuloma inguinale are all described in Section 3 (World Health Organization/UNAIDS, 1997).
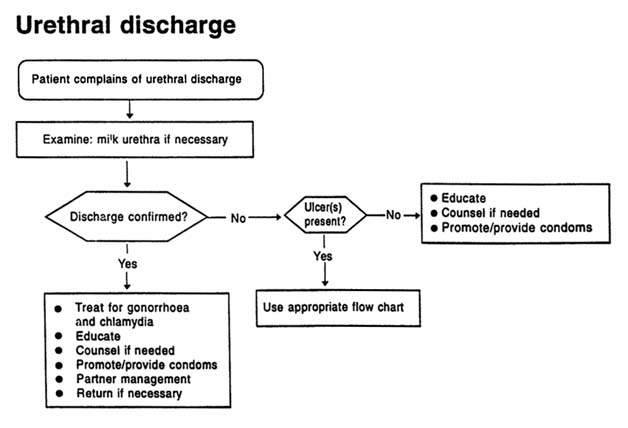
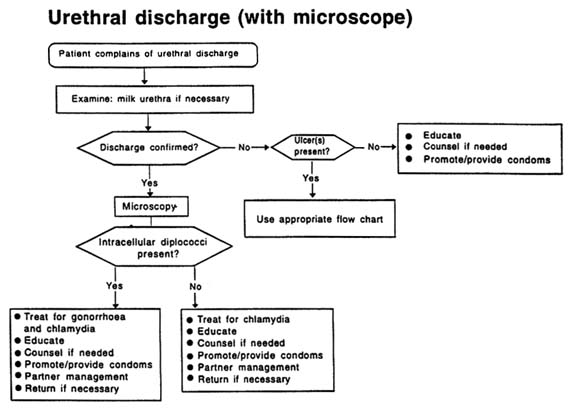
URETHRAL DISCHARGE
Male patients complaining of urethral discharge and/or dysuria should be examined for evidence of discharge. If none is seen, the urethra should be gently massaged from the ventral part of the penis towards the meatus. If microscopy is available, a urethral specimen should be collected; a Gram-stained urethral smear showing more than 5 polymorphonuclear leukocytes per field (×1000) in areas of maximal cellular concentration is indicative of urethritis.
The major pathogens causing urethral discharge are N. gonorrhoeae and C. trachomatis. Unless a diagnosis of gonorrhoea can be definitively excluded by laboratory tests, the treatment of the patient with urethral discharge should provide adequate coverage of these two organisms.
Recommended Regimens (see Figures A-1 and A-2)
therapy for uncomplicated gonorrhoea
plus either
doxycycline, 100mg orally, twice daily for 7 days
or
tetracycline, 500mg orally, 4 times daily for 7 days.
Alternative regimen when tetracyclines are contraindicated or not tolerated
therapy for uncomplicated gonorrhoea
plus
erythromycin, 500mg orally, 4 times daily for 7 days.
Alterative regimen where single-dose therapy for gonorrhoea is not available
trimethoprim (80mg) / sulfamethoxazole (400mg), 10 tablets orally, daily for 3 days
plus either
doxycycline, 100mg orally, twice daily for 7 days
or
tetracycline, 500mg orally, 4 times daily for 7 days.
Note. This regimen should only be used in areas where trimethoprim/sulfamethoxazole has been shown to be effective against uncomplicated gonorrhoea.
Follow-up
Patients should be advised to return if symptoms persist 7 days after start of therapy.
Persistent or recurrent symptoms may be due to poor compliance, reinfection, infection with a resistant strain of N. gonorrhoeae or infection with T. vaginalis. Where symptoms persist or recur after adequate treatment of the index patient and partner(s), both (or all) should be referred for laboratory investigation. The investigation should include a Gram stain to confirm the presence of urethritis and to look for N. gonorrhoeae. T. vaginalis may be identified by microscopic examination of a first-voided urine sample, although this test has a fairly low sensitivity in comparison with a culture. If the presence of T. vaginalis is confirmed, metronidazole, 2g, should be given as a single oral dose.
Note. Patients taking metronidazole should be cautioned to avoid alcohol.
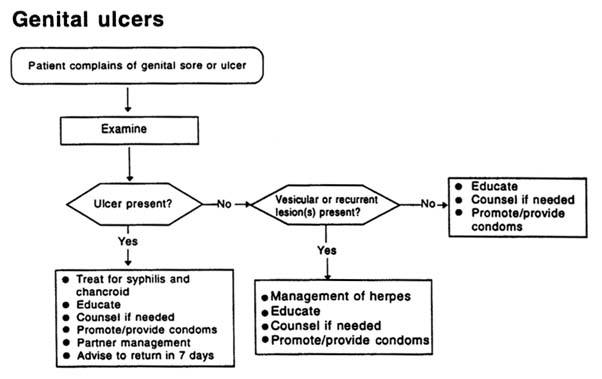
GENITAL ULCERS
The frequency with which genital ulcers are caused by specific organisms varies dramatically in different parts of the world. Clinical differential diagnosis of genital ulcers is inaccurate, particularly in settings where several etiologies are common. Clinical manifestations may be further altered in the presence of HIV infection.
After examination to confirm the presence of genital ulceration, treatment appropriate to local etiologies and antibiotic sensitivity patterns should be given. For example, in areas where both syphilis and chancroid are prevalent, patients with genital ulcers should be treated for both conditions at the time of their initial presentation to ensure adequate therapy in case of loss to follow-up. In areas where granuloma inguinale is also prevalent, treatment for this condition should be included.
Laboratory-assisted differential diagnosis is rarely helpful at the initial visit, and mixed infections are common. For instance, in areas of high syphilis incidence, a reactive serological test may reflect a previous infection and give a misleading picture of the patient's present condition.
Recommended regimens (see Figure A-3)
therapy for syphilis
plus either
therapy for chancroid
or
therapy for granuloma inguinale
Genital ulcer and HIV infection
In HIV-infected patients, prolonged courses of treatment may be necessary for chancroid. Moreover, where HIV infection is prevalent, an increasing proportion of cases of genital ulcers are likely to harbor herpes simplex virus. Herpetic ulcers may be atypical and persist for long periods in HIV-infected patients.
Follow-up
Patients with genital ulcers should be followed up weekly until the ulceration shows signs of healing.
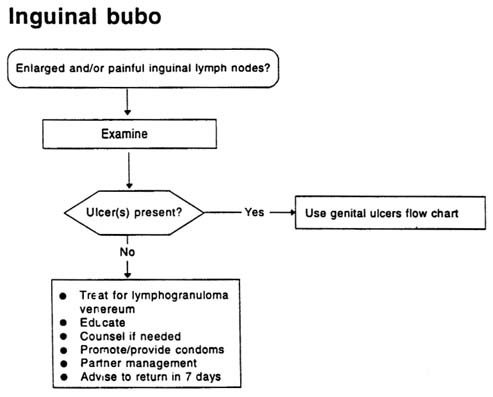
INGUINAL BUBO
Inguinal bubo, an enlargement of the lymph nodes in the groin area, is rarely the sole manifestation of an STD and is usually found together with other genital ulcer diseases. Nonsexually transmitted local and systemic infections (e.g., infections of the lower limb) can also cause swelling of inguinal lymph nodes.
Recommended regimens (see Figure A-4)
doxycycline, 100mg orally, twice daily for 14 days
or
tetracycline, 500mg orally, 4 times daily for 14 days.
Alternative regimen:
erythromycin, 500mg orally, 4 times daily for 14 days
or
sulfadiazine, 1g orally, 4 times daily for 14 days.
Some cases may require longer treatment than the 14 days recommended above. Fluctuant lymph nodes should be aspirated through
healthy skin. Incision and drainage or excision of nodes will delay healing and is contraindicated.
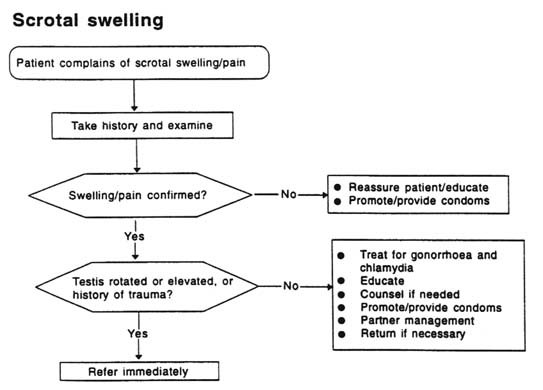
SCROTAL SWELLING
Scrotal swelling can be caused by trauma, a tumor, torsion of the testis or epididymitis. Inflammation of the epididymis is usually accompanied by pain, oedema and erythema and sometimes by urethral discharge, dysuria and/or frequency. The adjacent testis is often also inflamed (orchitis), producing epididymo-orchitis. Sudden onset of unilateral swollen scrotum may be due to trauma or testicular torsion and requires immediate referral. When not effectively treated, STD-related epididymitis may lead to infertility. The most important causative organisms are N. gonorrhoeae and C. trachomatis.
Recommended regimen (see Figure A-5)
therapy for uncomplicated gonorrhoea
plus either
doxycycline, 100mg orally, twice daily for 7 days
or
tetracycline, 500mg orally, 4 times daily for 7 days.
Alternative regimen when tetracyclines are contraindicated or not tolerated
therapy for uncomplicated gonorrhoea
plus
erythromycin, 500mg orally, 4 times daily for 7 days.
Alternative regimen where single-dose therapy for gonorrhoea is not available
trimethoprim (80mg) / sulfamethoxazole (400mg), 10 tablets orally, once daily for 3 days
plus
doxycycline, 100mg orally, twice daily for 7 days
or
tetracycline, 500mg orally, 4 times daily for 7 days.
Note. This regimen should only be used in areas where trimethoprim/sulfamethoxazole has been shown to be effective against uncomplicated gonorrhoea.
Adjuncts to therapy
Bed rest and scrotal elevation until local inflammation and fever subside.
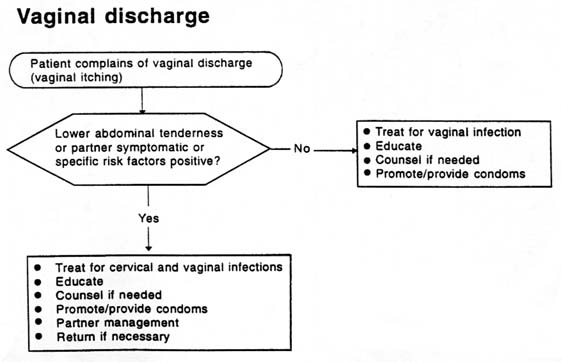
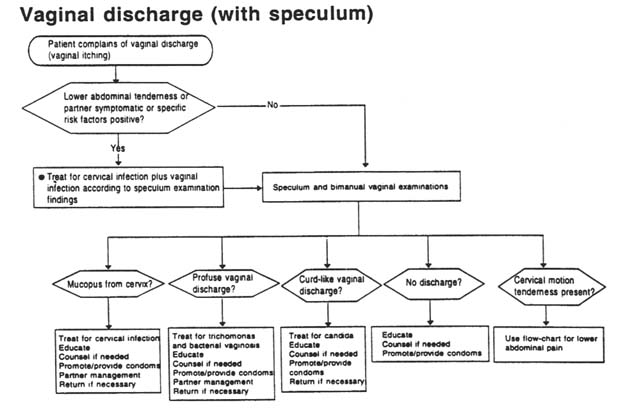
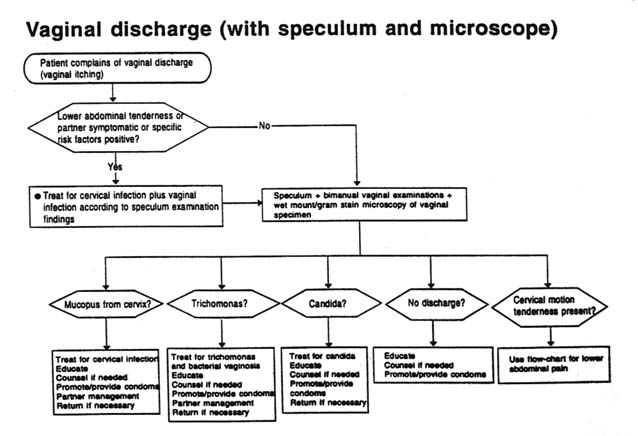
VAGINAL DISCHARGE
Vaginal discharge is most commonly caused by vaginitis, but it may also be the result of cervicitis. N. gonorrhoeae and C. trachomatis infection cause cervicitis, and Trichomonas vaginalis, Candida albicans and a synergistic combination of Gardnerella sp. and anaerobic bacterial infection (bacterial vaginosis) cause vaginitis. Effective management of cervicitis is more important from a public health point of view, as cervicitis may have serious sequelae. However, clinical differentiation between the two conditions is difficult. The symptom of vaginal discharge is neither sensitive nor specific for either condition. Recent studies suggest that an assessment of the woman's risk status helps greatly in making a diagnosis of cervicitis, but further evaluation using the flow charts below is needed, particularly with regard to risk factors, which vary from country to country. Where it is not possible to differentiate between cervicitis and vaginitis, and risk assessment is positive, patients should be treated for both conditions.
Cervicitis
Recommended regimen (see Figures A-6, A-7, and A-8)
therapy for uncomplicated gonorrhoea
plus either
doxycycline, 100mg orally, twice daily for 7 days
or
tetracycline, 500mg orally, 4 times daily for 7 days.
Note. Tetracyclines are contraindicated in pregnancy.
Alterative regimen when tetracyclines are contraindicated or not tolerated
therapy for uncomplicated gonorrhoea
plus
erythromycin, 500mg orally, 4 times daily for 7 days.
Alterative regimen where single dose therapy for gonorrhoea is not available
trimethoprim (80mg) / sulfamethoxazole (400mg), 10 tablets orally, once daily for 3 days
plus either
doxycycline, 100mg orally, twice daily for 7 days
or
tetracycline, 500mg orally, 4 times daily for 7 days.
Note. This regimen should only be used in areas where trimethoprim/sulfamethoxazole has been shown to be effective against uncomplicated gonorrhoea. Tetracyclines are contraindicated in pregnancy.
Vaginitis
Recommended regimen (see Figures A-6, A-7, and A-8)
metronidazole, 2g orally as a single dose,
or
metronidazole, 400-500mg orally, twice daily for 7 days
plus either
nystatin, 100 000 IU intravaginally, once daily for 14 days
or
miconazole or clotrimazole, 200mg intravaginally, once daily for 3 days
or
clotrimazole, 500mg intravaginally, as a single dose.
Note. Patients taking metronidazole should be cautioned to avoid alcohol.
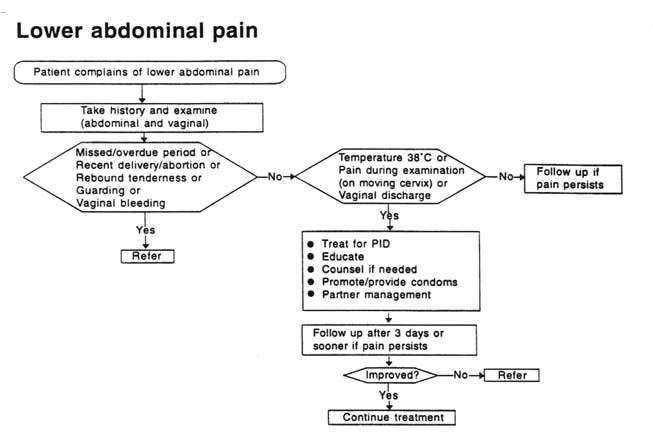
LOWER ABDOMINAL PAIN
All sexually active women presenting with lower abdominal pain should be carefully evaluated for the presence of salpingitis and/or endometritis—pelvic inflammatory disease (PID). In addition, routine bimanual and abdominal examinations should be carried out on all women with a presumptive STD since some women with PID or endometritis will not complain of lower abdominal pain. Women with endometritis may present with complaints of vaginal discharge and/or bleeding and/or uterine tenderness on pelvic examination. Symptoms suggestive of PID include abdominal pain, dyspareunia, vaginal discharge, menometrorrhagia,
dysuria, pain associated with menses, fever, and sometimes nausea and vomiting.
PID is difficult to diagnose because clinical manifestations are varied. PID becomes highly probable when one or more of the above symptoms are seen in a woman with adnexal tenderness, evidence of lower genital tract infection, and cervical motion tenderness. Enlargement or induration of one or both fallopian tubes, tender pelvic mass, and direct or rebound tenderness may also be present. The patient's temperature may be elevated but is normal in many cases. In general, clinicians should err on the side of overdiagnosing and treating milder cases.
Hospitalization of patients with acute pelvic inflammatory disease should be seriously considered when: (a) the diagnosis is uncertain; (b) surgical emergencies such as appendicitis and ectopic pregnancy need to be excluded; (c) a pelvic abscess is suspected; (d) severe illness precludes management on an outpatient basis; (e) the patient is pregnant; (f) the patient is unable to follow or tolerate an outpatient regimen; (g) the patient has failed to respond to outpatient therapy; or (h) clinical follow-up 72 hours after the start of antibiotic treatment cannot be guaranteed. Many experts recommend that all patients with PID should be admitted to hospital for treatment.
Etiological agents include N. gonorrhoeae, C. trachomatis, anaerobic bacteria (Bacteroides spp. and Gram-positive cocci). Facultative Gramnegative rods and Mycoplasma hominis have also been implicated. As it is impossible to differentiate between these clinically, and a precise microbiological diagnosis is difficult, the treatment regimens must be effective against this broad range of pathogens. The regimens recommended below are based on this principle.
Inpatient Therapy
Recommended regimens (see Figure A-9)
1. ceftriaxone, 500mg by intramuscular injection, once daily
plus
doxycycline, 100 mg orally or by intravenous injection, twice daily, or tetracycline, 500mg orally 4 times daily
plus
metronidazole, 400-500mg orally or by intravenous injection, twice daily, or chloramphenicol, 500mg orally or by intravenous injection, 4 times daily.
2. clindamycin, 900mg by intravenous injection, every 8 hours
plus
gentamicin, 1.5 mg/kg by intravenous injection every 8 hours.
3. ciprofloxacin, 500mg orally, twice daily, or spectinomycin 1g by intramuscular injection, 4 times daily
plus
doxycycline, 100mg orally or by intravenous injection, twice daily, or tetracycline, 500mg orally, 4 times daily
plus
metronidazole 400-500mg orally or by intravenous injection, twice daily, or chloramphenicol, 500mg orally or by intravenous injection, 4 times daily.
Note. For all three regimens, therapy should be continued until at least 2 days after the patient has improved and should then be followed by either doxycycline, 100mg orally, twice daily for 14 days, or tetracycline, 500mg orally, 4 times daily, for 14 days. Patients taking metronidazole should be cautioned to avoid alcohol. Tetracyclines are contraindicated in pregnancy.
Outpatient Therapy
Recommended regimen
single-dose therapy for uncomplicated gonorrhoea (single-dose ceftriaxone has been shown to be effective; other single dose regimens have not been formally evaluated as treatments for PID)
plus
doxycycline, 100mg orally twice daily, or tetracycline, 500mg orally, 4 times daily for 14 days
plus
metronidazole, 400-500mg orally, twice daily for 14 days.
Note. Patients taking metronidazole should be cautioned to avoid alcohol. Tetracyclines are contraindicated in pregnancy.
Alternative regimen where single dose therapy for gonorrhoea is not available
trimethoprim (80mg) / sulfamethoxazole (400mg), 10 tablets orally once daily for 3 days, and then 2 tablets orally, twice daily for 10 days
plus
doxycycline, 100mg orally, twice daily, or tetracycline, 500mg orally, 4 times daily for 14 days
plus
metronidazole, 400-500mg orally, twice daily for 14 days.
Note. This regimen should only be used in areas where trimethoprim/sulfamethoxazole has been shown to be effective in the treatment of uncomplicated gonorrhoea. Patients taking metronidazole should be cautioned to avoid alcohol.
Adjuncts to therapy: removal of an intrauterine device (IUD)
The IUD is a risk factor for the development of PID. Although the exact effect of removing an IUD on the response of acute salpingitis to antimicrobial therapy and on the risk of recurrent salpingitis is unknown, removal of the IUD is recommended soon after antimicrobial therapy has been initiated. When an IUD is removed, contraceptive counseling is necessary.
Follow-up
Outpatients with PID should be followed up at 72 hours and admitted if their condition has not improved.
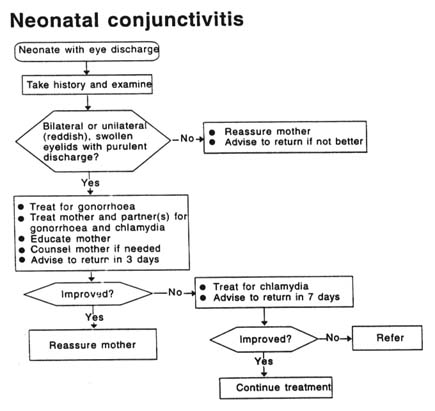
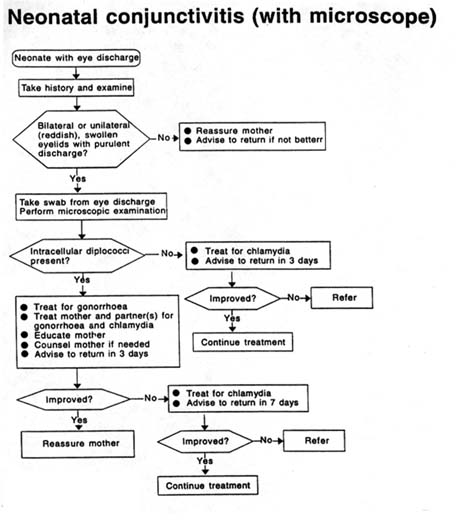
NEONATAL CONJUNCTIVITIS
Neonatal conjunctivitis (ophthalmia neonatorum) can lead to blindness when caused by N. gonorrhoeae. The most important sexually transmitted causes of ophthalmia neonatorum are N. gonorrhoeae and C. trachomatis . In developing countries, N. gonorrhoeae accounts for 20–75 percent and C. trachomatis for 15–35 percent of cases brought to medical attention. Other common causes are Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus spp. and Pseudomonas spp. Newborn babies are generally presented because of redness and swelling of the eyelids or ''stricky eyes," or because of discharge from the eye(s).
REFERENCES
World Health Organization 1991 Management of Patients with sexually transmitted diseases: Report of a WHO Study Group WHO Technical Report Series, No. 810. Geneva, Switzerland: World Health Organization.
1997 Management of Sexually Transmitted Diseases. World Health Organization, Joint United Nations Programme on HIV/AIDS Publication, Document GPA/TEM/94.1 Rev. 1., Sections 2.1-2.7:3-17. Geneva, Switzerland: World Health Organization.