5
Accountability and Quality in End-of-Life Care
The days when medical care was a small private matter between patient and general practitioner are long gone and will never return.
Rashi Fein, Medical Care, Medical Costs, 1986
The relationship between patient and practitioner—this once small, private matter—is now enmeshed in a very large and complex system that delivers the benefits of medical progress to the people of the United States. That system depends on an often bewildering array of organizational, financial, and monitoring arrangements that link medicine, government, business, and other institutions. By fragmenting the patient-physician relationship and often putting personal physicians at a distance from their dying patients, these arrangements may diminish the knowledge and intimacy that contributes to a professional's feeling of individual responsibility. The unintentional result may be to leave no one participant clearly responsible for a patient's overall experience.
Thus, at the individual, organizational, and community level, cultivating responsibility and establishing accountability for the quality of care for patients approaching death are especially important tasks. This chapter begins by examining basic concepts of accountability and quality. It then presents evidence of quality problems in end-of-life care and reviews basic concepts of quality assessment and improvement. The discussion particularly emphasizes the importance of broadening the understanding of outcomes relevant to dying patients and those close to them. The last two sections consider instruments for measuring quality and guidelines for improving clinical practice. This discussion should be read in the context of other chapters of this report that discuss additional avenues for protecting and improving the quality of care.
This chapter—consistent with the rest of this report—emphasizes that a comprehensive strategy for improving care at the end of life must focus not only on the structures, processes, and outcomes of care but also on the
environmental factors—such as laws, financing mechanisms, and educational programs—that shape the delivery of care. Unless environmental causes of poor quality care are understood and addressed, efforts to improve organizational and individual behavior may prove disappointing. In this context, quality measurement and improvement strategies should
- allow clinicians and others directly responsible for end-of-life care to evaluate and improve what they are doing on a continuing basis;
- help policymakers, patients, families, and the public to hold organizations and individuals accountable for how reliably and effectively they care for dying patients; and
- support systematic research on the effects of different clinical, organizational, and financing options for end-of-life care and on the effectiveness of alternative strategies for improving care and outcomes for patients and those close to them.
Overall, the committee concluded that more effort is warranted to assess patient experiences at the end of life; to evaluate the benefits and burdens of common end-of-life interventions (e.g., mechanical ventilation), including how they are experienced and valued by patients and families; to understand how perceptions, values, and preferences may change during the course of dying; and to improve physician understanding of patient and family preferences. As emphasized throughout this report, the knowledge base about the dying process and the effectiveness of different care strategies is limited. This, in turn, limits efforts to establish and refine standards or benchmarks against which care processes and outcomes can be assessed and improved.
Concepts of Accountability and Quality
Accountability
Under the banner of accountability, a variety of public and private policymakers, purchasers, health care organizations, researchers, and others have joined together to develop new methods to monitor and influence patient care in hospitals, managed care plans, and other settings. Dictionary definitions of accountability emphasize the state of being answerable or being obliged to report, explain, or justify (see, e.g., The American Heritage Dictionary, 1993). The concept immediately raises the question—"accountability for what?" This report argues that health care personnel and organizations have, in general, not been held responsible for the quality of care for dying patients. In the absence of systems that can measure outcomes and identify problems across care settings, even those who identify themselves
as responsible for supportive end-of-life care—palliative specialists, hospice personnel, ethics consultants, chaplains, and others—may not always know whether they are fulfilling their responsibilities.
The concept of accountability also raises the question—"accountability to whom?" The health professions have traditionally defined their accountability with reference to those they serve (e.g., patients, students) and to their fellow professionals and the standards of performance they have collectively created. For more than a century, however, state and federal governments in the United States have been developing regulatory mechanisms to supplement or, in some instances, replace professional accountability. A recent IOM report defined public accountability for those serving Medicare beneficiaries as involving not only beneficiaries but also "the larger public as interested parties and taxpayers" (IOM, 1996b, p. 31). In addition, private organizations, including hospitals, health plans, and other organizations, have established mechanisms of accountability. As a result, any one clinician or health care organization may be accountable to multiple parties whose expectations may not be fully compatible.
A third question—"how are professionals and organizations to be held accountable?"—requires a complex answer that involves a mix of social norms, regulations, economic incentives, measurement tools, and information reporting mechanisms. The notion of accountability to one's own conscience and a recognized set of ethical standards (e.g., the Hippocratic Oath or one of its successors) is appealing because it implies an internalized, ever-vigilant control mechanism. It is also part of what defines and dignifies a profession. It likewise provides a basis for trust that patients' vulnerability will not be exploited by physicians and other health professionals for "power, profit, prestige, or pleasure" (Pellegrino, 1991, p. 80). External regulations, reporting requirements, and accreditation standards have a role to play, but the imposition of external rules and monitoring does not make up for a lack of trust or trustworthiness.
The "invisible hand of the market" is yet another mechanism of accountability that relies on decisions by millions of informed consumers (and their agents) that, in theory, reward good performers and penalize poor performers. In health care, making quality a meaningful factor in such decisions is, today, an embryonic undertaking in which the quality of end-of-life care is largely invisible. Price is a more easily understood and comparable variable and the extent to which purchasers actually consider quality in their decisions is controversial.
Quality of Care
The quality of health care should contribute to the quality of living and the quality of dying but, as noted in Chapter 1, it is not synonymous with
them. Another IOM committee has defined quality of care as "the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge" (IOM, 1990, p. 21). This definition covers both individuals and populations, which is consistent with increasing concerns about how resources can be employed to the greatest social advantage. The definition acknowledges the relevance of professional knowledge, which includes experience and judgment as well as the important but still limited results of biomedical and clinical research. Notably, the definition deliberately omits resource constraints on the grounds that judgments of what constitutes excellent, acceptable, or unacceptable quality should be independent of constraints on resources. Decisionmakers cannot and should not, however, ignore resources in making decisions about what level of quality is desirable and affordable for a particular institution, population, or community. This means paying attention to quality and value both for those covered by public and private insurance arrangements and for those excluded from such arrangements.
Similarly, although the definition of quality of care applies generally, the specifics will differ depending on patient circumstances and goals of care. That is, the desired outcomes for a dying patient will differ in some respects from the outcomes desired when prevention of a disease is still relevant or cure is still possible. Even for patients diagnosed with incurable illnesses that are likely to prove fatal within a matter of months, the outcomes that are meaningful early in the dying trajectory (e.g., physical functioning and independence) may become less so as the progress of the disease and the imminence of death makes such outcomes less realistic and heightens the relevance of physical and emotional comfort, resolution in personal relationships, and issues of spiritual meaning or peace.
Quality Assessment and Improvement
Quality of care may be assessed in several ways (see, e.g., Donabedian, 1966; IOM, 1990; Blumenthal, 1996). Assessments may be implicit (e.g., rated by clinicians without reference to defined standards) or explicit (e.g., based on written criteria). They may be used to judge performance (e.g., rate it acceptable or unacceptable, or better or worse than for a comparable organization) or to improve performance (e.g., identify reasons for poor outcomes) or both. Assessments may be internal (e.g., clinical audits undertaken by those providing care) or external (e.g., undertaken by purchasers, government officials, or others not involved in providing care). External processes have involved such mechanisms as licensure, accreditation, information reporting, performance ratings or comparisons, inspections, and
penalties for noncompliance, some of which have been evolving for over a century.
In recent years, reliance on external strategies has been criticized as costly and relatively ineffective, and strategies emphasizing internal responsibility for continuing improvement in quality have been encouraged (see, e.g., Batalden and Buchanan, 1989; Berwick, 1989; Berwick et al., 1990; IOM, 1990; Horn and Hopkins, 1994). Continuous quality improvement (CQI) models (sometimes termed Total Quality Management or TQM) are generally described in terms of a set of reinforcing principles for implementing change. These principles include targeting systemic defects (e.g., burdensome protocols for patient referral) rather than individual mistakes; encouraging close relationships among the participants in health care transactions (e.g., physicians, patients, purchasers); using planning, control, assessment, and improvement activities that are grounded in statistical and scientific precepts and techniques; feeding statistical information back to practitioners on how their practices may differ from their peers' or depart from evidence-based standards for practice; standardizing processes to reduce the opportunity for error and link specific care processes to outcomes; and striving for continuous improvement in contrast to merely meeting established goals or criteria (IOM, 1992).
Typical of quality improvement strategies reflecting these principles are the guidelines recommended by the American Pain Society for the treatment of acute pain and cancer pain (APS, 1995). The guidelines, which focus on inpatient care and address institutions rather than single individuals, are summarized in Box 5.1. They do not explicitly consider the special circumstances of dying patients but are consistent with the discussion in Chapter 3.
Evidence of Quality Problems in End-of-Life Care
Conventionally, several broad types of health care quality problems have been differentiated (see, e.g., IOM, 1990). They are overuse of care (e.g., unwanted treatments or hospitalizations; diagnostic tests that will not inform patient care but may cause physical and emotional distress); underuse of care (e.g., failure to assess and treat pain; late referral for hospice care, premature hospital discharge); poor technical performance (e.g., errors in surgical technique); and poor interpersonal performance (e.g., inept communication of difficult news). In general, underuse of care is more difficult to detect than overuse. For example, in population-based analyses, it may be difficult to distinguish problems of inadequate access to care from problems of undertreatment for identified patients (IOM, 1990).
Care at the end of life is characterized by problems in each of these areas. Said differently, systems have much room to improve the extent to
|
BOX 5.1 Guidelines for Improving the Quality of Treatment for Acute Pain and Cancer Pain
|
||||||||||||||||||
which they are providing the right care at the right time in the right way. Overuse and underuse of care may occur simultaneously, for example, when futile efforts to cure are continued at the expense of efforts to relieve physical and psychological symptoms and help patients and families prepare emotionally, spiritually, and practically for death. The discussion below emphasizes overuse of certain interventions (including hospitalization) and undertreatment of symptoms. Untimely referral to hospice, which has already been cited as a problem, is a form of underuse as is inattention to patient and family needs for nonmedical support. Poor technical performance, for example, miscalculation of medication dosages for pain or other symptoms, has been little studied; for purposes of this discussion it is considered an aspect of undertreatment. Problems in patient-physician communication were considered in Chapter 3, and Chapters 4, 6, 7, and 8 discuss different aspects of quality of care related to settings of care, financing mechanisms, and public policies.
The Problem of Unrelieved Symptoms
Numerous studies indicate that dying patients and patients with advanced illnesses experience considerable amounts of pain and other physical and psychological symptoms (Donovan et al., 1987; Foley, 1993; AHCPR, 1994a; Cherny et al., 1994; Miaskowski et al., 1994; Seale and Cartwright, 1994; Ward and Gordon, 1994; Donnelly and Walsh, 1995a,b; Breitbart, Rosenfeld et al., 1996; Lynn, Teno et al., 1997). Pain prevalence has been the focus of many of these studies. For example, Bonica (1990) found that 75 percent of patients with advanced cancer experienced pain; over a quarter of the patients described the pain as very severe, and 40 percent to 50 percent described it as moderate to severe. Portenoy and colleagues (1994) reported that more than 60 percent of cancer patients they studied reported pain. Several studies of nursing home patients have reported that from 40 percent to over 80 percent of nursing patients have pain (Roy and Michael, 1986; Ferrell et al., 1990; Sengstaken and King, 1993; Morley et al., 1995; Wagner et al., 1996).
The prevalence of pain is better mapped for cancer than for other diagnoses. One of the few large studies to look at a range of diagnoses (nine altogether, including three cancer diagnoses) in seriously ill hospitalized patients found severe pain reported by about 40 percent of family members of conscious patients (Lynn, Teno, et al., 1997). Pain has been reported in 30 percent to 80 percent of HIV-infected individuals with the higher levels and more persistent levels of pain reported in AIDS patients (Lebovits et al., 1989; Schofferman and Brody, 1990; Breitbart, McDonald, et al., 1996; Breitbart, 1997). Studies suggest that pain is experienced in 55 to 85 percent of patients with multiple sclerosis (Moulin, 1989). Pain is a defining characteristic of coronary artery diseases, although relief of the pain may be a less immediate priority than the diagnosis and treatment of the complications of the disease (AHCPR, 1994b).
Reports on end-of-life symptoms other than pain are more limited and, like those for pain, typically involve cancer patients. In an analysis of nine studies of cancer symptoms in the last week of life, Ingham and Portenoy (1994) found reported shortness of breath in 9 percent to 52 percent of patients, nausea in 3 percent to 71 percent of patients, vomiting in 12 to 50 percent of patients, and pain in 12 percent to 99 percent of patients (over 30 percent for 7 of the 9 studies). Donnelly and Walsh (1995b) reported that pain, fatigue, and loss of appetite were the most common and severe symptoms across a range of advanced cancers. Portenoy et al. (1994) found that 40 percent to 80 percent of the patients they studied "experienced lack of energy, pain, feeling drowsy, dry mouth, insomnia, or symptoms indicative of psychological distress" (p.183). They also found that the mean number of symptoms per patient was 11 and that the number of symptoms
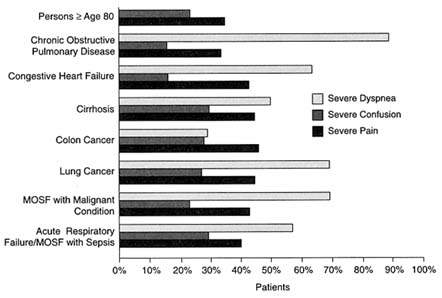
FIGURE 5.1 Rates of severe symptoms in patients three days before death, as reported by family members.
NOTE: Family members of elderly patients were not asked about dyspnea. MOSF = multiple organ system failure.
Source: Lynn, Teno et al., 1997, p. 102. Reprinted with permission from the Annals of Internal Medicine. The American College of Physicians is not responsible for the accuracy of this reprint.
was highly related to measures indicating poorer quality of life. Bruerà likewise has found patients reporting multiple symptoms, with weakness, loss of appetite, and pain most common (Bruera, 1993).
The earlier cited study of hospitalized patients who were seriously ill with one of nine diagnoses reported moderate to high rates of symptoms for many patients. The results for severe pain, severe dyspnea, and severe confusion by diagnosis are presented in Figure 5.1.
A British study, which was able to compare 1987 results with an earlier 1969 study, examined symptoms for cancer and noncancer patients. The reports, presented in Table 5.1, were obtained in after-death interviews with persons identified through a sample of death certificates and determined to be knowledgeable about the decedents' care (Seale and Cartwright, 1994).
In general, prevalence and severity studies have certain limitations or characteristics that need to be recognized. For example, they are limited to
TABLE 5.1 Symptoms Reported in 1969 and 1987 for Cancer and Other Deaths in Two English Studies
|
|
Cancer deaths (%) |
Other deaths (%) |
All deaths (%) |
|||
|
|
1969 |
1987 |
1969 |
1987 |
1969 |
1987 |
|
Pain |
87 |
84 |
58 |
67a |
66 |
72a |
|
Trouble with breathing |
47 |
47 |
44 |
49 |
45 |
49 |
|
Vomiting, feeling sick |
54 |
51 |
21 |
27a |
30 |
33 |
|
Sleeplessness |
69 |
51a |
41 |
36 |
49 |
40a |
|
Mental confusion |
36 |
33 |
36 |
38 |
36 |
37 |
|
Depression |
45 |
38 |
31 |
36 |
36 |
36 |
|
Loss of appetite |
76 |
71 |
37 |
38 |
48 |
47 |
|
Constipation |
42 |
47 |
23 |
32a |
28 |
36 |
|
Bedsores |
24 |
28 |
13 |
14 |
16 |
18 |
|
Loss of bladder control |
37 |
25a |
24 |
55 |
28 |
23a |
|
Unpleasant smell |
26 |
19 |
11 |
13 |
15 |
14 |
|
Number of deaths (=100%)b |
215 |
168 |
570 |
471 |
785 |
639 |
|
a Difference between 1969 and 1987 significant at the 5% level. b Small numbers of deaths for whom inadequate information was available are included in the total but have been excluded from this and other tables in this book when calculating percentages. SOURCE: Seale and Cartwright, 1994. Used with permission. |
||||||
the extent that patients are unable to report symptoms because they have mental or physical problems that preclude or compromise communication.
Another limitation is that prevalence and even severity measures by themselves do not indicate the importance of a symptom to patients and families (Lynn, Teno et al., 1997). In one study of various symptoms in
cancer patients, the "proportion of patients who described a symptom as relatively intense or frequent always exceeded the proportion who reported. it as highly distressing" (Portenoy et al., 1994, p. 183). Thus, two patients could report the same duration, frequency, or intensity of a symptom but differ in the extent to which they found the symptom distressing or difficult to tolerate. Similarly, the same symptom may become a source of greater or lesser distress to a person as death approaches and different things become important to them.
Further, although studies reporting pain and other symptoms, particularly those involving cancer pain, are often interpreted as indicating undertreatment, some of the studies have not explicitly investigated the use, lack of use, or misuse of palliative therapies. Studies that have attempted to assess treatment directly have, however, generally found problems.
In one study that explicitly assessed pain treatment practice for cancer outpatients, Cleeland and colleagues (1994) found that 42 percent of patients were not appropriately treated. A study of ambulatory AIDS patients identified pain treatment as inadequate in 85 percent of patients; for example, strong opioids, which are recommended for patients with severe pain, were prescribed in only 8 percent of such patients (Breitbart, Rosenfeld, et al., 1996). Another study, which found pain reported by 78 percent of randomly selected patients hospitalized in an academic medical center, discovered that only 49 percent of those patients had a progress note mentioning pain in their chart (Donovan et al., 1987). Patient reports and their recording are important because caregiver recognition or estimates of pain do not necessarily match patient reports (see, e.g., Cleeland, 1989; Grossman et al., 1991; Au et al., 1994; APS, 1995).
In a study of nursing home patients, 60 percent of the patients with needs for pain management received effective pain care, whereas the rest had problems ranging from no medication to ineffective type or frequency of medication (Wagner et al., 1996). Cherny and Catane (1995) concluded that from 64 percent to 80 percent of patients admitted for palliative medicine and hospice services had inadequately relieved pain. These and other studies reporting variable pain management practices and results (Jadad and Browman, 1995; Kimball and McCormick, 1996) suggest the need for more research to understand practice patterns and their effectiveness (Wennberg, 1984, 1991).
Explicit findings of undertreatment are consistent with professional perceptions of treatment inadequacies. For example, a survey of physicians in five hospitals found that 8 of 10 physicians agreed that the most common form of narcotic abuse was undertreatment of pain (Solomon et al., 1993). In 1990, concern about unrelieved symptoms led to a statement from a National Cancer Institute workshop that "undertreatment of pain and other
symptoms of cancer is a serious and neglected public health problem" (cited in AHCPR, 1994a, p. 8).
Reviews of pain research have suggested that pain can be fairly readily relieved in approximately 70 percent to 90 percent of cancer patients and that a significant proportion of the remainder can find relief short of complete sedation (see, e.g., Takeda, 1986; Walker et al., 1988; Goisis et al., 1989; Schug et al., 1990; Zech et al., 1995; Portenoy and Kanner, 1996). These and other studies also suggest that the high doses of opioids needed to relieve pain in certain patients rarely hasten death (Citron et al., 1984; Brescia et al., 1992; Wilson et al., 1992). At least one analysis of several studies of the effectiveness of the World Health Organization's pain management guidelines, however, suggested the need for more rigorous evaluation and concluded that, until then, "it would be inappropriate to judge the performance of clinicians, programs, and institutions …" based on whether or not they applied these specific guidelines (Jadad and Browman, 1995, p. 1872; see also WHO, 1990; Grond et al., 1991, 1993; Ventafridda et al., 1987, 1990).
Although the research base is often weaker than for pain, effective strategies also exist in many cases to relieve certain other symptoms including shortness of breath, vomiting, and depression (Cohen et al., 1991; Bruera, Miller, et al., 1992; Bruera, Schoeller, et al., 1992; Breitbart and Holland, 1993; Doyle et al., 1993; Gavrin and Chapman, 1995). Certain other problems—for example, wasting, loss of appetite, and fatigue—have proved less amenable to intervention, although Chapter 9 discusses promising directions in research for the problem of wasting and loss of appetite. Strategies to relieve these symptoms could also prolong life.
A number of comprehensive and specialized clinical guides are available to help physicians, nurses, and other health professionals provide effective palliative care for many patients.1 These guides also suggest a number of barriers to effective palliative care beginning with inadequate clinician knowledge. Box 5.2, which is reprinted from the cancer pain guidelines of the Agency for Health Care Policy and Research (AHCPR), lists barriers to pain and the studies identifying them. It is the committee's experience that many of these barriers apply to other symptoms.
One of the major problems identified in the AHCPR pain guidelines was inadequate assessment of pain. Clinicians and researchers have developed and tested formal instruments for systematically assessing pain and thereby identifying whether change in treatment is needed. These instru-
|
BOX 5.2 Barriers to Cancer Pain Management
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
ments include both written or oral questions and visual or figurative elements. Some of these instruments are cited in Appendix F. In addition to their use in assessing and guiding patient care, these instruments also may be useful in monitoring provider performance and evaluating the outcomes of different types of care. As discussed in a later section of this chapter, the development of reliable and valid instruments for measuring other symptoms and determining how they affect patient well-being is a continuing need.
The Problem of Overtreatment
In the context of end-of-life care, overtreatment involves both care that is clinically inappropriate and care that is not wanted by the patient, even if some clinical benefit might be expected. Fear of unwanted treatment at the end of life is an important factor in initiatives promoting advance care planning (Emanuel, 1991; Hill and Shirley, 1992; Solomon et al., 1993). Such fear—and the loss of control it implies—may also contribute to interest in assisted suicide.
Unfortunately, documented preferences do not rule out unwanted care. For example, a study of AIDS patients reported that nearly one in two who wanted care focused on comfort were receiving aggressive curative or life-prolonging treatments (Teno et al., 1991). In a large study of seriously ill hospitalized patients, about 1 patient in 10 was reported to have had care provided that was inconsistent with preferences (Lynn, Teno, et al., 1997), and doctors were often unaware of what patient preferences actually were (SUPPORT Principal Investigators, 1995). Departures from patient preferences sometimes involved more use of life-sustaining interventions than wanted and sometimes less. For the same study, investigators considered rates of medical ventilation, coma, and intensive care unit (ICU) interventions as indicators of possible inappropriate treatment in the last few days of life. In the initial phase of their study, they found that more than a third of the patients spent at least 10 days in the ICU and nearly half received mechanical ventilation during their last 3 days of life.
Another study that surveyed physicians at five hospitals on a number of issues in end-of-life care found that 55 percent of those surveyed felt that they sometimes provided "overly burdensome" treatments to patients, whereas only 12 percent said they sometimes gave up too soon on patients (Solomon et al., 1993, p. 16). Overall, when asked about the inappropriate use (but not inappropriate underuse) of several treatments, a majority expressed concern about mechanical ventilation, cardiopulmonary resuscitation, artificial nutrition and hydration, and dialysis. Each of these interventions has been the subject of considerable debate about the circumstances under which their use promises no or virtually no benefit.
Much of the recognition of overtreatment stems from countless personal experiences, some documented in print, others conveyed in conversation. In general, the committee concluded that concern about overuse of certain kinds of advanced technologies at the end of life is warranted. Given current cost containment pressures, it will, however, be important to monitor for signs of increasing underuse of such interventions. In addition, it would be useful to understand whether one factor in overtreatment is clinician uncertainty about or unfamiliarity with effective palliative care strategies, including methods of withdrawing mechanical ventilation and other life-sustaining technologies so as to cause minimum distress to patients and families (Brody et al., 1997).
Dimensions of Quality in Care at The End of Life
The literature on quality of care has traditionally distinguished three dimensions for analysis: structure, process, and outcome (Donabedian, 1966, 1980; IOM, 1990). The emphasis in recent years has been increasingly on the outcomes of care, but quality improvement requires an understanding of how structures and processes interact with environmental and patient characteristics to produce outcomes (see, e.g., Chassin et al., 1986; IOM, 1990; Lohr, 1992; Fowler, 1995; Berwick, 1996; Blumenthal, 1996; Brook et al., 1996). Several analyses have recently focused attention on how these concepts can be useful in strategies to measure, monitor, and improve the quality of care for those approaching death (Byock, 1996; Merriman, 1996; Stewart, 1996; Teno, 1996b; AGS, 1997; Donaldson, 1997; Stewart et al., forthcoming).
Table 5.2 depicts the committee's general conceptualization of structure, process, and patient/family outcomes and the larger environmental context as they relate to care at the end of life (see Stewart et al., forthcoming, and Patrick, forthcoming, for alternative conceptualizations). (Economic outcomes, including expenditures for end-of-life care, are discussed in Chapter 5.)
Structures and processes of care are not neatly separable categories, but they can be generally distinguished for purposes of discussion. For analyses intended to identify contributors to good and bad outcomes, the focus is on specific variables (e.g., staffing level or pain management) and their potential for manipulation rather than on their label.
In contrast to structure and process measures, the environmental elements are essentially "givens" rather than variables that can be manipulated by those directly responsible for care at the end of life. Such elements may be particularly important for those with advanced illness. For example, a person who lives alone in a rural area where outpatient or home care resources are scarce may very well face a higher likelihood of institu-
TABLE 5.2 Dimensions of Quality in Care of Dying Patients and Related Quality Strategies
|
Context |
Structures |
Processes |
Outcomes |
|
Culture, norms, social institutions |
Care settings (home, institution) |
Establishing diagnosis and prognosis |
Physical (symptoms, function) |
|
Demographic |
Personnel (staff, volunteers, numbers, training) |
Establishing goals and plans |
Psychological (emotional, cognitive) |
|
Geography |
Clinical policies (protocols, guidelines) |
Providing palliative and other patient care |
Spiritual |
|
Economic system, resources |
Information and decision support systems |
Caring for families, bereavement care |
Perceptions of care, burden of care |
|
Political system, policies, regulations |
Financial policies (free care, target profit levels) |
Coordinating care including transfers among settings |
Dignity, control over decisionmaking |
|
Individual and family characteristics |
|
Monitoring, improving care |
Survival |
tionalization than a city resident living with a family member. An affluent community is likely to support more health care institutions and services and attract better trained personnel, although high-technology medical centers are not necessarily better than (or as good as) community hospitals at providing supportive and appropriate care.
Structural Aspects of Quality of Care
The link between specific health care structures and outcomes is a matter of continuing dispute based on modest and sometimes conflicting research (see, for example, IOM, 1986; Mor, 1987; Relman, 1988; IOM, 1990; Lansky, 1993; SUPPORT Principal Investigators, 1995; IOM, 1996c).
Nonetheless, because structural elements are such visible and intrinsic elements of organized caregiving, the effort to identify and establish how structures affect outcomes is understandable. This effort is undergirded by a network of organizations and procedures for establishing consensus on structural standards and for accrediting or otherwise certifying that health care facilities, organizations, and personnel meet these standards.
Several organizations, including the Health Care Financing Administration, the Joint Commission on Accreditation of Healthcare Organizations, and the National Hospice Organization, have identified a variety of structural characteristics thought to increase the likelihood that dying patients will be served well. These characteristics, which generally have been emphasized hospices, have been set forth in the Medicare program's conditions of participation, materials for voluntary accreditation or certification, and documents of technical assistance. They typically involve written institutional policies related to such matters as staff credentials and composition, advance care planning, emergency response procedures, information systems, safe physical environments, and governing mechanisms that protect and respect patients.
Notwithstanding a general interest in structural elements of quality care, the mere existence of regulations and policies does not guarantee their conversion into desired processes or outcomes of care. This is another reason for the interest in continuous quality improvement strategies that focus on internal rather than external mechanisms of quality assessment and assurance.
Care Processes and Quality
Processes of care have been a major focus of public and private efforts intended to improve health outcomes (Donabedian, 1966, 1982; IOM, 1990; Wilson and Cleary, 1995; Wilson and Kaplan, 1995). The same holds true for care at the end of life (see, e.g., Doyle et al., 1993; Higginson, 1993; SUPPORT Principal Investigators, 1995; Tolle, 1996a). The broad process dimensions set forth in Table 5.2 reflect the discussion in Chapter 3 and do not identify specific variables—such as elements of pain management—that might be considered in assessing the quality of care in a particular setting. Assessments also may consider utilization statistics for various services (e.g., home nursing visits, emergency transfers, diagnostic tests, length of hospital stay) as indicators of care processes.
Sometimes, process-of-care measures (e.g., rates of influenza immunization for elderly people) are relied on as proxies for outcomes (e.g., rates of influenza and its complications) when outcomes data are unavailable or too demanding to collect with available resources. Process measures are, however, important in their own right as they help evaluators to under-
stand how care is provided, how an intervention changes other aspects of the care process, and how processes might be improved to achieve better patient outcomes or greater efficiency. For example, the SUPPORT study, which is discussed at several points in this report, was a process intervention intended to improve decisionmaking for very seriously ill patients (SUPPORT Principal Investigators, 1995; see also the Hastings Center Report, Special Supplement, Vol. 25, No. 6, 1995).
Furthermore, it has been suggested that "some processes are valued more than [some] outcomes" (Teno, 1996b, p. 8). Communication with patients and families and responsiveness to their desires to be involved in decisionmaking are examples of highly valued processes. More generally, when cure or prolonged life are no longer dominant goals, the processes of caring for the body, mind, and spirit affirm the dignity and value of those approaching death and can be appreciated in and of themselves.
Broadening the Understanding of Outcomes
The limitations of mortality rates and physiological indicators (e.g., blood pressure) as measures of health outcomes or quality of care have been pointed out in other contexts (see, e.g., IOM, 1990; Patrick and Bergner, 1990; Patrick and Erickson, 1993). It is particularly obvious that other measures are necessary for examining the quality of patient and family care at the end of life. As one committee member phrased it in discussing her critical care practice, "if the quality of care in my palliative care practice were judged by mortality rates, I would look pretty bad because 85 percent of my patients die." Similarly, nursing home administrators trying to reduce inappropriate hospitalizations of dying patients have particular reason to be concerned that mortality data be used carefully in judging their performance.
Caution is particularly important when outcomes are linked to reimbursement for care. If severity of illness and other patient characteristics are inadequately considered, outcome measurements may lead to mistaken judgments about quality of care and may inappropriately reward those who achieve good scores because they avoid less healthy people (Thomas and Ashcraft, 1989, 1991; Iezzoni, 1992; IOM, 1993a; Hopkins and Carroll, 1994).
Although a focus on measures other than mortality might seem to deflect attention from death, it instead underscores that a lot more happens to most dying people than the specific event of their death. Nonetheless, the understanding of what it means to live well while dying and how to measure the quality of dying remains at an early stage.
Outcomes as experienced by patients are increasingly being recognized by clinicians and researchers. Many commonly used physiological indica-
tors (e.g., blood pressure, cholesterol level) may not be strongly linked to outcomes as experienced by patients. Thus, outcomes related to physical and mental functioning and well-being must be identified to evaluate the impact of social, economic, medical, and other actions intended to improve individual or population health. For those approaching death, common measures of function and well-being may have only limited relevance. Conversely, measures that are particularly sensitive to the experiences of older people may not be as well suited to younger people with advanced illnesses.
In reviewing the hospice literature, Mor (1987) identified several categories of outcomes for attention. They include pain and other symptoms, performance status, satisfaction with care, psychosocial state, secondary morbidity, and site of death. A more expansive listing has been proposed by the American Geriatrics Society (AGS) as part of its efforts to focus attention on the quality of end-of-life care (AGS, 1997) (see Box 5.3). The AGS list, which has been endorsed by more than 30 organizations, includes both outcomes (e.g., satisfaction) and aspects of care processes (e.g., advance planning, aggressive care near death). To focus more narrowly on patient and family outcomes, the committee identified major categories of outcomes relevant to assessments of the quality of life for dying patients. The six categories summarized in Table 5.3 mostly parallel the dimensions of care discussed in Chapter 3 but extend them somewhat. For example, a patient's overall quality of life can be expected to reflect the patient's physical, emotional, spiritual, and practical circumstances, including those that are not specifically a function of their health status or health care. In addition, patient and family perceptions of care are increasingly recognized as important in their own right.
Measurement Instruments and Issues
It is axiomatic in the continuous quality improvement literature that "if you don't measure it, you can't improve it." To that end, a number of instruments for measuring quality of care and patient status and well-being have been developed, and work to adapt these instruments or develop others helpful in improving care for seriously ill and dying patients is proceeding on many fronts. An August 1996 workshop, convened in conjunction with the committee's August meeting, examined many instruments for measuring and assessing outcomes and quality of care in the context of quality improvement for care at the end of life. One objective was to propose a preliminary "toolkit" of instruments to measure end-of-life care (Teno, 1996b). The committee was able to read the papers drafted for the workshop, participate in the workshop, and review the workshop summary and initial recommendations. (For more information see Appendix F and www.gwu.edu/˜cicd/TOOLKIT.HTM). The committee concluded that the
|
BOX 5.3 Quality Domains Suggested by the American Geriatric Society Physical and emotional symptoms. Pain, shortness of breath, fatigue depression, fear, anxiety, nausea, skin breakdown, and other physical and emotional problems often destroy the quality of life at its end Symptom management is regularly deficient. Care systems should focus upon these needs and ensure that people can count on a comfortable and meaningful end of their lives. Support of function and autonomy. Even with the inevitable and progressive decline with fatal illness, much can be done to maintain personal dignity and self-respect. Achieving better functional outcomes and greater autonomy should be valued. Advance care planning. Often, the experience of patient and family can be improved just by planning ahead for likely problems, so that decisions can reflect the patient's preferences and circumstances rather than responding to crises. Aggressive care near death—site of death, CPR, and hospitalization. Although aggressive care is often justified, most patients would prefer to have avoided it when the short-term outcome is death. High rates of medical interventions near death should prompt further examination of provider judgment and care system design. Patient and family satisfaction. The dying patients peace of mind and the family's perception of the patient's care and comfort are extremely important. In the long run, we can hope that the time at the end of life will be especially precious, not merely tolerable. We must measure both patient and family satisfaction with these elements: the decisionmaking process, the care given the outcomes achieved, and the extent to which opportunities were provided to complete life in a meaningful way. |
preliminary toolkit was indeed just that, preliminary and awaiting refinement. It recommended an extensive process of testing, adapting, and developing instruments that are (1) relevant to the experiences of dying patients and those close to them, (2) sensitive to the effects of changes in care, and (3) efficient and practical to use. Additional collaborative work to develop this toolkit is planned.
Instruments
Dozens, even hundreds, of instruments exist to measure health status or quality of life (McDowell and Newell, 1996). For example, one recent review reported 159 different instruments used in the 75 articles analyzed (Gill and Feinstein, 1994). Some were fairly narrow (e.g., hand grip strength,
|
Global quality of life. Often a patient's assessment of overall well-being illuminates successes and shortcomings in care that are not apparent in more specific measures. Quality of life can be quite good despite declining physical health, and care systems that achieve this should be valued. Family burden. How health care is provided affects whether families have serious financial and emotional effects from the costs of care and the challenges of direct caregiving. Current and future pressures on funding health care are likely to displace more responsibility for services and payment onto families. Survival time. With pressures upon health care resources likely to increase, there is new reason to reason to worry that death will be too readily accepted. Purchasers and patients need to know how survival times vary across plans and provider systems. In conjunction with information about symptoms, satisfaction, and the other domain listed here, such measures will allow insights into the priorities and tradeoffs within each care system. Provider continuity and skill. Only with enduring relationships with professional caregivers can patient and family develop trust, communicate effectively, and develop reliable plans. The providers also must have the relevant skills, including rehabilitation, symptom control, and psychological support. Care systems must demonstrate competent performance on continuity and provider skill. Bereavement. Often health care stops with the patient's death, but the suffering of the family goes on. Survivors may benefit with relatively modest interventions. SOURCE: AGS, 1997. |
word recall) whereas others (e.g., Sickness Impact Profile) were more comprehensive. Some instruments have been tested and validated in end-of-life care; most have not. A few are designed for use with family members. Box 5.4 presents some illustrative items that were selected to indicate the kinds of questions being asked of seriously ill or dying patients and their families.
Various groups (IOM, 1990; Medical Outcomes Trust, 1995; Stewart, 1996; Lynn, 1997) have defined attributes of useful measures. Box 5.5 offers one widely cited list, which combines technical and practical methodological considerations. The main focus of the committee was more on clinical and research uses of measures than on external performance monitoring and rating.
TABLE 5.3 Categories of Patient/Family Outcome Measures for End-of-Life Care
|
Overall quality of life |
Spiritual well-being |
|
|
|
|
Physical well-being and functioning |
Patient perceptions of care |
|
|
|
|
Psychosocial well-being and functioning |
Family well-being and perceptions (before and after patient's death) |
|
|
|
Measurement Issues and Problems
Developing measures of patient status or quality of care that meet these requirements is a significant challenge for any arena of health care (see, e.g., Ware et al., 1988; Fowler et al., 1994), but measures appropriate to the special circumstances of dying patients and their caregivers present particular problems (Mor, 1987; Cella and Tulsky, 1990; Cohen and Mount, 1992; Byock, 1996; Ingham, 1996; Merriman, 1996; Puchalski, 1996; Roach, 1996; Stewart, 1996; Teno, 1996b; Wilkinson, 1996; Donaldson, 1997). Some problems are most relevant to ongoing quality assessment by organizations delivering care, whereas others apply mainly to researchers
(see Chapter 9). Several of the problems have contributed to the reluctance of external performance monitoring or certifying organizations to include indicators important for dying patients.
Consistent with the discussion of undertreatment, pain measures have been more extensively developed and evaluated than measures for other symptoms common among people approaching death. The strategies employed in developing, testing, and refining pain assessment instruments have provided useful models and lessons for those working in other areas. Among the issues that have been identified for a variety of symptoms and circumstances are the following.
The Timing of Assessments
Timing involves two questions: when and how often to schedule assessments of patient and family experiences and perceptions. At a minimum, the committee believes that it is important to try to make assessments when death is expected within a few weeks, although this will not always be possible. Such assessments may include questions that extend back in time (e.g., to diagnosis); accuracy with respect to events may thereby suffer but the perceptions are still important. Nonetheless, because predictions of death are so imprecise, some patients may be evaluated three days before death, others three weeks before death, and others not at all. In addition, many patients will be unable to be interviewed because of cognitive impairment or some other reason. Thus, interviews with families may be important as a source of more representative information on patients' experiences—as well as on their own experience before and after their loved one's death (Addington-Hall and McCarthy, 1993).
Frequent assessments of symptoms may be integral to ongoing effective management of pain and other symptoms. Indeed, proponents of better pain management have urged that pain be regarded as a fourth vital sign (in addition to breathing, heartbeat, and blood pressure). The Edmonton Symptom Assessment System (ESAS), which was designed to chart nine symptoms for cancer inpatients, is intended for use twice a day and is designed to be quick and easy to use and interpret (Bruera and McDonald, 1993). Such charting may both guide day-to-day care and allow patterns of care (e.g., good versus poor symptom control) to be assessed from patient records.
Frequent assessment may not always be either possible or the best use of limited resources. For example, an extensive home and inpatient palliative auditing process developed in England calls for audits at the time of referral and then weekly (Higginson, 1993). Even with this system, early experience in its use found that audits were often missed for items related to financial matters, spiritual status, family anxiety, and communication between family and patient. In addition, a comprehensive assessment may be
|
BOX 5.4 Illustrative Examples of Items Proposed to Measure Individual Perceptions or Experiences
|
||||||||||||||||||
difficult given that many patients are referred for palliative care very late in their illness, when the effort to help may take precedence over the effort to assess quality or outcomes. Assessment may also be difficult for patients whose probability of death is sufficiently unpredictable that they are not categorized as dying, referred to hospice or similar programs, or otherwise "captured" by those attempting to assess the quality of care. One result is that assessments are often made retrospectively—after a patient's death and using recorded data or surrogates—rather than during the dying process.
The Role of the Patient or a Surrogate as a Source of Patient Information
Seriously ill and dying patients may not be able to report for themselves because of the physical or mental impairments produced by their illness. Even a patient who can articulate that "it hurts" may not be able to rate current or recent pain in the ways required by an assessment instrument. In addition, as noted earlier, the timing of death is not easily predicted. The
|
||||||||||||||||||
question thus arises whether a surrogate—someone such as a family member or a caregiver—can provide reliable and valid information on the patient's experience. Some studies suggest that surrogates tend to report more distress than do patients (Higginson et al., 1994). Note that the issue here is whether surrogates can "speak" for patients, not what they say about their own status or experience, which is important to assess in its own right.
The committee urges continued research to assess the degree to which patient and surrogates perceptions match (when both can be measured), the extent to which different surrogates provide different reports, the reasons for differences, and the bases for choosing a proxy. Such research is neither simple nor inexpensive but is a high priority for quality assessment and improvement for patients approaching death.
|
BOX 5.5 Desirable Attributes of Outcomes Assessment Instruments Based on Criteria Developed by the Medical Outcomes Trust Conceptual and measurement model: (a) "underlying rationale for and description of the concepts that the measure is intended to assess and the relationships between or among those concepts" and (b) "the instrument's scale and subscale structure and the procedures that are used to create the scale scores" Reliability: "the degree to which an instrument is free of random error" or, less formally, the stability of results when the instrument is used by different raters or at different times Validity: "the degree to which an instrument measures what it purports to measure" Responsiveness: "an instrument's ability to detect change in outcomes that matter" to patients, clinicians, or relevant others Interpretability: "the degree to which one can assign qualitative meaning—that is, clinical or commonly understood connotations—to qualitative scores" Respondent and administrative burden: these involve "the time, energy, financial resources, personnel, or other resources required" of respondents or those administering the instruments Alternative forms: "all the ways in which the instrument might be administered other than in the original ways" (e.g., to proxies rather than patients) Cultural and language adaptations: the degree of "conceptual and linguistic equivalence between the original instrument and its adaptations" SOURCE: Medical Outcomes Trust, 1995 (material in quotes); Lohr et al., 1996. |
The Relative Emphasis on Ratings of Satisfaction versus Reports About Care
Measures of satisfaction with care are widely used and sometimes relied on entirely or primarily as indicators of quality of care. Such measures have a variety of limitations, particularly those instruments that are developed informally without systematic validation (Ware, 1978; Ware and Hays, 1988; Ware et al., 1988; Ahorony and Strasser, 1993; Gerteis et al., 1993). One problem is that the gap between categories in typical rating scales (e.g., between excellent and very good or between points 4 and 5 on a five-point scale) may be different than suggested by the words or numbers
used to describe categories (Ware and Hays, 1983; Teno, 1996a; Allen Russell, Center for Health Research, personal communication, May 1996; see more generally, discussions of interval and ordinal measurement in Blalock, 1979; Kerlinger, 1986). For example, the difference between a service rated excellent (or 5) versus very good (4) may be more important than the difference between a very good (4) versus a good (3) rating—both to caregivers and to competitors in a vigorous market. Indeed, those who rate a service as "only" very good or good may actually have serious concerns that the simple ratings do not reveal.
One response to the apparent limitations of ratings is to emphasize patients' reports about care (e.g., whether different options for care were explained) (Cleary et al., 1991; Gerteis et al., 1993; Teno, 1996a,b). Although this approach may be somewhat more demanding, it has the advantage of providing more specific perceptions that may be useful in correcting problems. At this time, it seems reasonable to suggest that both ratings and reports be tested (Teno, 1996a).
The Scope and Depth of the Instrument
This chapter has outlined many dimensions of end-of-life care and quality of life that warrant assessment. Unfortunately, the circumstances of many dying patients—including physical and mental status, location in a home rather than institutional setting, and family problems—may make it difficult to ask any questions, much less a large number of them. That is one reason for interest in identifying one or two indicators (e.g., patient's or surrogate's report of overall satisfaction or inadequately relieved pain) that are both attention getting and likely to point to broader quality problems. Depending on the purpose of an assessment (e.g., everyday patient care, research project), the selection of questions may vary.
The Relevance of Measures of Function
Measures of physical and psychological functioning are widely used to assess well-being and outcomes of care for people suffering from chronic illnesses or impairments, being treated for serious medical problems, undergoing function-impairing treatments, or even experiencing relatively good health. For people with advancing, eventually fatal medical problems, the relevance of particular functional indicators or capacities may change as their illness progresses. At an early stage of illness, for example, the ability to drive may seem paramount; later the ability to get out of bed may be a primary concern. How assessment instruments and their interpretation should reflect these kinds of changes needs further investigation.
The Meaning of Symptoms
Although some symptoms are more evident to observers than others (e.g., vomiting or incontinence versus pain or fatigue), the meaning of symptoms to patients and their impact on overall quality of life are intrinsically subjective (Ward and Gordon, 1996). Some may find pain or incontinence terribly distressing; others may be less affected. Some may find pain less distressing than any mental haziness induced by medications. As discussed in Chapter 1, suffering has dimensions beyond specific physical or psychological indicators. Some outcomes measures ask patients or others to assess symptoms by rating them on a descriptive scale (e.g., from no pain to severe pain). Others ask for an assessment of the effect of the symptom on the patient (e.g., from no pain to pain that is severe, continuous, and overwhelming in its impact on physical or cognitive functioning) (Higginson, 1993).
Sensitivity to Change or Differences in Patient Status
To be useful in guiding quality improvement, instruments should provide interpretable and meaningful information about changes in patient status that may occur as a function of disease or treatment. They should also be sensitive to the range of differences in patients whose care is being assessed. Some instruments are designed primarily for use in relatively healthy populations and may not capture some outcomes relevant to people with progressive debilitating or life-threatening conditions. This has been a problem with "report cards" that attempt to provide overall ratings for managed care plans but do not consider services and outcomes for people with serious acute and chronic medical problems.
The Need for Disease- or Condition-Specific Measures.
Not only the stage of illness but the nature of the illness itself may be relevant to the choice of quality or outcomes measures. In addition, providers of care may be more proficient in caring for some kinds of illnesses (e.g., cancer) than others (e.g., Alzheimer's disease). The importance of condition-specific measures is an empirical question that can, in principle, be answered by testing instruments for reliability and validity across different patient conditions. Only a few instruments have been subjected to such investigation. Some instruments were originally developed for particular categories of patients (e.g., the Health Assessment Questionnaire for arthritis patients) whereas others were not. In either case, the instruments may or may not have been used, tested, or adapted for different kinds of patients. Patient differences by diagnosis may diminish as death is thought to be
imminent, in which case disease-specific measures may be less relevant at this stage.
Although measures of symptoms and satisfaction with care raise a variety of problems, spiritual constructs may be particularly troublesome both to define and translate into operational measures (Mor, 1987). A literature review by Puchalski (1996) identified 30 potential instruments for assessing spirituality or spiritual well-being. Several generally used quality of life measurement instruments include questions on spirituality. In the context of end-of-life issues, spiritual well-being has been defined in essentially nonreligious terms as "meaningful existence, ability to find meaning in daily experience, ability to transcend physical discomfort, readiness for death" (Stewart, 1996). Some measures of these qualities have been incorporated and tested in instruments for assessing end-of-life care (Byock, 1996; Merriman, 1996).
In addition to working with hospitals and hospices providing palliative care, researchers developing quality of life, quality of dying, and quality of care measures for dying patients should seek other ways to extend experience with different measures and populations. One strategy would be to continue to press the National Institutes of Health to require quality of life measures in a greater range of clinical trials and to analyze the experience of patients who die under both experimental and control protocols. The committee makes such a recommendation in Chapter 9.
Guidelines for Clinical Practice
Recent years have seen considerable interest in the use of clinical practice guidelines to improve the appropriateness, effectiveness, and cost-effectiveness of care (see, e.g., Brook et al., 1986; Chassin et al., 1986; Lohr et al., 1986; PPRC, 1988, 1989; Roper et al., 1988; Audet et al., 1990; and IOM, 1990, 1992).2 Practice guidelines have the potential to contribute to quality of care for dying patients in several ways as part of multifaceted quality improvement strategies.
First, by describing specific processes of care identified as effective, guidelines may improve the technical provision of care. Although experience, physical skill, attention to detail, and similar factors contribute to technical proficiency, good performance also depends on a solid under-
standing of what constitutes effective care (e.g., selection of analgesic or route of administration) or correct performance of a technical task (e.g., giving an injection). To the extent that the evidence base is weak, as it is for much end-of-life care, the potential of guidelines to improve care is reduced. In any case, to inform potential users, guidelines should be accompanied by documentation of (a) the strength of the evidence and consensus associated with specific recommendations and (b) the processes and participants involved in developing the guidelines (IOM, 1992).
Second, guidelines that explicitly and clearly describe appropriate care for particular clinical problems such as management of specific symptoms provide a basis for problem identification and correction. Thus, they can help those responsible for detecting patterns of undertreatment (e.g., failure to prescribe pain medications at all or in sufficient amounts and frequencies) or overtreatment (e.g., use of artificial hydration when ice chips and glycerin swabs would be more comfortable for a patient nearing death).
Third, guidelines that include good explanations of possible outcomes (e.g., potential benefits and burdens of a third course of chemotherapy) can contribute to better communication and shared decisionmaking on the part of patients and practitioners. Guidelines that specify expected outcomes also provide a tool for comparing care in different settings and assessing the effectiveness of different or new interventions.
Unfortunately, the lack of interest in dying patients that is noted throughout this report is reflected in the scarcity of guidelines for end-of-life care and in the lack of a strong evidence base for developing such guidelines. Some guidelines for symptom management, for example, those for treating cancer pain, may be useful with patients approaching death, although they may not be sensitive to the shifting and balancing of goals of care that occurs as patients near death. Other guidelines focus on ethical and legal rather than clinical aspects of end-of-life care. For example, when the Milbank Memorial Fund sponsored a meeting of specialty societies in September 1996 to review clinical guidelines relevant to end-of-life care and to discuss areas for future work, almost all the examples it received from meeting participants dealt with ethical issues such as informed consent and surrogate decisionmaking.
The committee did not attempt a systematic review of guidelines, but it did review examples of guidelines for managing life-threatening illnesses that might be expected to discuss evaluation and management of the end stage of the illness. Many were silent. For example, guidelines for diagnosis and management of unstable angina developed by a private, government-funded panel do not cite advance care planning or end-of-life concerns in the discussion of patient counseling, the algorithms for medical management or cardiac procedures, or the index (AHCPR, 1994b). For heart failure guidelines (AHCPR, 1994c), the discussion of patient/family counseling
refers to advance directives and advice for family members in the event of sudden death. The guidelines do not, however, cover care for patients for whom invasive therapy is rejected and medical management is failing.
Somewhat more cognizant of care issues involving patients near the end of life are several guidelines for nursing home care issued by the American Medical Directors Association (AMDA). These guidelines used several AHCPR guidelines as the basis for statements on depression, heart failure, pressure ulcers, and urinary incontinence (AMDA, 1996). The preface explicitly states that the guidelines usually assume that recovery or rehabilitation is the goal of care but that this is not always the case. For example, for patients for whom palliation of symptoms is the primary goal of care, the AMDA guidelines note that standard care (e.g., to undertake a comprehensive diagnostic work up for incontinence) may be foregone to minimize distress (e.g., avoid pain) based on a specific assessment of the benefits and burdens for an individual patient.
Considerable experience with practice guidelines has reinforced the observation that the availability of guidelines does not ensure their implementation (Eisenberg, 1986; Lomas, 1991; Lomas et al., 1991; Foley, 1995; Bookbinder et al., in press). Although new educational strategies such as academic detailing3 are being tested as part of guidelines implementation strategies, additional approaches appear necessary to implement guidelines in ways that improve outcomes including relief of pain and other symptoms (IOM, 1992; AHCPR, 1994a; APS, 1995). These approaches include
- providing for clinician participation in the development of guidelines (to encourage "buy-in");
- incorporating guidelines in continuous quality improvement initiatives that include feedback of statistical information on organizational and clinician performance;
- integrating guidelines and outcomes measures into computer-based patient information and decision support systems; and
- linking acceptance of guidelines and compliance to health plan contracting requirements or financial incentives.
Such approaches would, in general, appear relevant both for organizations that care for a broad range of patients and those that focus more
specifically on care at the end of life. Just like guidelines themselves, the effectiveness of implementation strategies cannot be assumed but must, instead, be evaluated. This process has begun in some areas of end-of-life care (see, e.g., Dietrick-Gallagher et al., 1994; Ward and Gordon, 1994, 1996).
Conclusion
This chapter has stressed the importance of cultivating responsibility and establishing accountability for the quality of care for patients approaching death. Central to both tasks is information that can be used to measure outcomes and quality of care, identify and correct problems, and improve system and individual performance. Methods of quality measurement and improvement are works in progress throughout the health care system. For care at the end of life, these methods are, by and large, at a fairly early stage of development. Taken together, however, various available methods and instruments do begin to capture some aspects of what Chapter 1 set forth as elements of a decent or good death—a death free from avoidable distress and suffering; in general accord with patient and family wishes; and reasonably consistent with clinical and ethical standards.
The committee here has emphasized that there is a role for both internal and external quality assurance and improvement mechanisms including guidelines for clinical practice. In general, it accepts the argument that efforts should focus on the identification and correction of systemic problems rather than searching narrowly for individual bad actors. It has stressed the importance of outcomes measures but also acknowledged that it is important to assess structures and processes of care and to understand the impact of legal, financial, cultural, and other variables. Such knowledge will help distinguish those factors that health care organizations and professionals may directly act to improve from other factors that are either not subject to influence by providers or require cooperation by others, such as those who determine how different health care services are financed. A high priority is research and methodology development involving the creation and refinement of measurement instruments relevant to goals for patients approaching death and the links between outcomes of care and the environmental, structural, and process-of-care factors that determine outcomes.
Other chapters of this report identify many sources of quality of care and accountability problems. For example, Chapters 3 and 4 have pointed to problems of coordination and continuity in a system that moves patients among many different health care settings and personnel. Chapter 6 points to financing incentives that encourage overtreatment of some patients and undertreatment of others and that generally discourage careful and time-consuming symptom assessments, counseling, and consultations. Chapter 7
will highlight the problem of anti-addiction drug policies that inappropriately target the medical use of opioids to control pain and other symptoms. In considering education and research, Chapters 8 and 9 reinforce the theme of inattention to the needs of dying patients, with the latter chapter also revisiting some methodological issues in assessing those needs.
































