2
A Profile of Death and Dying in America
To die of old age is a death rare, extraordinary, and singular … a privilege rarely seen.
Montaigne, Of Age, 1575
Death is not what it used to be.1 For most of human history, medicine could do little to prevent or cure illness or extend life, and living to an old age required considerable good fortune. Dying—like being born—was generally a family, communal, and religious event, not a medical one. Because many deaths occurred at home, people were likely to care for dying relatives and, thus, to have a fairly personal and direct experience with dying and death.
In the United States, death at home in the care of family has been widely superseded by an institutional, professional, and technological process of dying. That process—its positive aspects not with standing—has distanced the final stage of life from the rest of living. Additionally, the mobility of Americans quite literally puts distance between many younger and older family members. Adults, even into middle age, may never have lived near or cared for someone who was dying. "A long-distance phone call announcing the passing of grandpa or grandma takes the place of the intimate, firsthand experience of a loved one's death" (DeSpelder and Strickland, 1996, p. 19). For many, the most common images of death are those presented in the news and entertainment media, which tend to focus
on the sensational, violent, or sentimental and which often depict death as an event without much social or personal context.
This chapter provides a brief epidemiological profile of dying and death in the United States, an overview of research on attitudes toward dying and death, and a short concluding reflection on cultural characteristics that influence attitudes and practices related to the end of life. Although the shifts in the rates and causes of death over time are, in considerable measure, the result of nonmedical factors such as better public health measures and economic development, they also reflect—and, in turn, shape—the technological capacities and organizational characteristics of health care including its continued emphasis on acute rather than chronic illnesses. Understanding when, why, where, and how people die and what they think about death and dying can help policymakers ask better questions about whether health care and supportive services are appropriately organized and distributed to fit the needs of dying patients and their families.
The discussion below shows that Americans, on average, live much longer now than they did at the end of the nineteenth century and that death in infancy has moved from routine to rare. Those who die in old age tend to die of different causes than those who die young, and for both younger and older people, the major causes of death and the typical experience of dying differ from 100 years ago.
The dying process today tends to be more extended, in part, because medical treatments can control pneumonia, kidney failure, and other immediate causes of death that accompany cancer, heart disease, and other "slow killers." Because death from these conditions can often be postponed, questions about life-prolonging treatment become central issues for patients, families, and clinicians. In the process, the tasks of preparing for death and caring well for those who are dying can be neglected, and opportunities for spiritual growth or completion of important relationships can be missed.
By arguing for changes in attitudes and practices related to dying and death, the committee does not endorse a romantic view of the past. In earlier ages, familiarity with death did not necessarily translate into kind treatment of the dying, particularly for those marked by disfiguring conditions. Likewise, familiarity did not banish fear, shame, or other difficult emotions in the face of death.
When People Die: The Aging of America
Although less than 1 percent of Americans will die this year, the total number of deaths will be well over 2 million. In 1995, estimated deaths in the United States were 2,312,180 (Rosenberg et al., 1996), up from 1,989,841 in 1980 (NCHS, 1985) and 2,148,463 in 1990 (NCHS, 1994). To put this number in some perspective, 1995 estimated births in the United
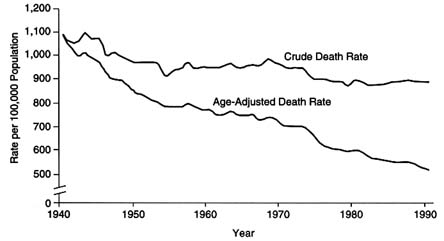
FIGURE 2.1 Crude and age-adjusted death rates: United States, 1940–1990.
Source: Singh et al., 1996.
States numbered 3,900,089—the lowest level in almost two decades (Rosenberg et al., 1996).
Further perspective is provided by an examination of trends in death rates over time. In 1900, the crude death rate was about 1,720 per 100,000 population (U.S. Department of Commerce, 1975) compared with a rate of 880.0 per 100,000 in 1995 (Rosenberg et al., 1996). Between 1940 and 1995, the age-adjusted mortality rate, which takes the aging population into consideration, fell relatively steadily, from 1,076.1 deaths per 100,000 resident population in 1940, to 585.5 deaths per 100,000 resident population in 1980 (Singh et al., 1996), and to 503.7 in 1995 (Rosenberg et al., 1996) (see Figure 2.1).
The typical American can now expect to live a lengthy life and die at an old age. In 1900, average life expectancy at birth was less than 50 years (Figure 2.2).2 In 1995, the estimated life expectancy reached 75.8 years, matching the all-time high attained in 1992. Women may now expect to live nearly 79 years and men, almost 73 years (Rosenberg et al., 1996). Among those who reach age 75, women may expect to live, on average, 11.9 additional years, while men can expect to live 9.7 years longer.
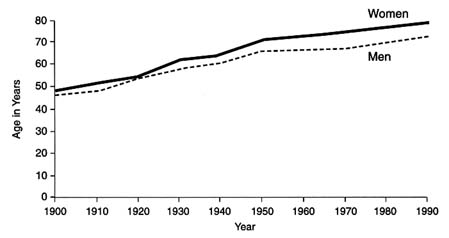
FIGURE 2.2 Life expectancy at birth by gender, 1900–1990. Source: Robert Wood Johnson Foundation, Chronic Care in America: A 21st Century Challenge.
Princeton, N.J.; August 1996.
The decline in death rates and the increase in life expectancy coexist, however, with significant racial differences. In 1995, black males had an age-adjusted death rate (1,006.9 per 100,000 resident population) almost twice that of white males (611.2). Black females had an age-adjusted death rate (566.2 per 100,000 resident population) more than one and one-half times that of white females (365.6) (Rosenberg et al., 1996). Similarly, estimates based on 1995 data show that an average black woman could expect to live 74.0 years compared to 79.6 for white women. For black men, estimated life expectancy at birth was 65.4 years compared to 73.4 for whites.
The increase in life expectancy has come primarily from reduction in child—especially infant—mortality. In 1900, the death rate for newborns and infants under the age of 1 was 162.4 per 1,000. This rate fell steeply once a child reached the age of 1 and was only matched by those people who survived beyond the age of 85. By 1970, the infant mortality rate had fallen to 21.4 per 1,000, and all adults age 65 and over died at a greater rate than that (U.S. Department of Commerce, 1975). Estimates for 1995 indicate that less than 2 percent of deaths involved people under 15 years of age, whereas 73 percent involved those age 65 and over (49 percent in the 65 to 84 age group and the other 24 percent in the 85 and older group (Rosenberg et al., 1996).
As a result of changing mortality patterns, those age 65 and over constitute an increasingly large number and proportion of the U.S. population. In 1994, this age group accounted for approximately 1 in 8 persons (13
percent) of the population; in 2030, when the large baby boom cohort has entered old age, 1 in 5 persons (20 percent) is expected to be in this age group (Hobbs and Damon, 1996). These demographics explain this report's emphasis on older people.
Why People Die: Causes of Death
A century ago, communicable diseases—in particular, influenza, tuberculosis, and diphtheria—were leading causes of death in the United States. Heart disease, stroke, and cancer ranked fourth, fifth, and ninth (Brim et al., 1970). Today and for many years previous in the United States (and economically advanced nations generally), the three leading causes of death for the population as a whole have been heart disease, cancer, and stroke. Preliminary data for 1995 estimate that these causes—which disproportionately affect older people—accounted for 62 percent of all deaths and 67 percent of deaths for those age 65 and older (Rosenberg et al., 1996, p. 31). For children, however, causes of death are quite different (Rosenberg et al., 1996). For children ages 1 to 14, the leading causes of death are unintentional injuries, cancer, congenital abnormalities, and homicide.
Consistent with data on death rates and life expectancy, data on causes of death by race and age offer a grim picture of the racial and social disparities that characterize life in America for certain groups. For all black males in 1993, homicide, HIV infection, and unintentional injuries preceded stroke as the third, fourth, and fifth leading causes of death (PHS, 1996). After heart disease and cancer, Hispanic males were most likely to die from unintentional injuries and HIV infection. Suicide was among the ten leading causes of death for American Indian or Alaskan Native and Asian or Pacific Islander women but not for white, black, or Hispanic women.
As Table 2.1 shows, in 1995, among white infants, the leading cause of infant mortality was congenital anomalies (165.2 deaths per 100,000 live births); among black infants, it was the second leading cause but the actual death rate (199.1) was considerably higher than for whites. Disorders relating to short gestation and unspecified low birth weight were the leading cause of death for black infants and the third most important for white infants, but these rankings do not reveal the disparity in actual death rates of 292.0 and 64.6 respectively (Rosenberg et al., 1996).
Those who die from chronic illness—and their survivors—will look to care systems for somewhat different kinds of physical, emotional, spiritual, and practical support than those who experience violent or premature death. The committee focused on the former group but recognized the need for systems able to care reliably and well for people with different problems and needs.
TABLE 2.1 Infant Mortality Rates for the Ten Leading Causes of Infant Death, by Race: United States, January 1995
Where People Die: Death in Institutions and Residences
Over the last century, death has moved out of homes and into institutions. In 1949, national statistics revealed that 49.5 percent of deaths occurred in institutions (39.5 percent in general hospitals and the rest in psychiatric and other kinds of hospitals and nursing homes); by 1958, the comparable figure had risen to 60.9 percent (47.6 percent for general hospitals) (Brim et al., 1970). Final mortality statistics for 1980 indicated that 74 percent of deaths occurred in institutions (60.5 percent in hospitals and 13.5 percent in other institutions) (Brock and Foley, 1996, p. 5).
In the early and mid-1980s, two developments provided some incentives for change in this pattern. First, Medicare began to cover hospice care in 1983 (Hoyer, 1996), and private insurance coverage for hospice also began to spread. Second, and more broadly, starting in 1983, Medicare phased in a new prospective, per-case method of paying hospitals to encourage reduced use of inpatient hospital care. Inpatient hospital deaths for Medicare beneficiaries showed a modest decline (McMillan et al., 1990). Nursing home death rates increased, particularly for the oldest old (Sager et al., 1989; Brock and Foley, 1996). Although deaths in residences were not identified as a separate category in national reporting of vital statistics until 1989, McMillan et al. (1990) interpreted less specific data as indicating a particular increase in the percentage of cancer deaths occurring at home.
For 1992, U.S. mortality statistics showed about 57 percent of deaths occurring in hospitals (excluding those declared dead on arrival), 17 percent in nursing homes, 20 percent in residences, and 6 percent elsewhere (including those declared dead on arrival at the hospital). Of the deaths in hospitals, approximately 84 percent occurred in inpatient units with most of the rest taking place in emergency departments or outpatient clinics.
Site of death varies by age. For example, in 1980, 8 percent of those age 65 to 74 died in institutions other than hospitals or medical centers (mainly nursing homes) compared to 34 percent of those in the 85 and over age group (Riley et al., 1987). Unfortunately, data on the site of death, although improving, are still incomplete, and more detailed data (e.g., by age) are not routinely published.
Patterns for site of death also vary considerably across the nation. Medicare data for 1990 suggest that most of the Pacific Coast and Mountain states had less than 40 percent of beneficiary deaths occurring in hospitals. Data from Oregon indicate that deaths in that state are almost evenly distributed across hospitals, nursing homes, and homes (with a small additional percentage accounted for, e.g., by people declared dead at the site of an accident) (Tolle, 1996a). In contrast, Medicare data show that from Texas and Oklahoma through the South, Middle Atlantic states, and
New England states, the figure for hospital deaths was above 40 percent or even 50 percent in many areas (Pritchard et al., 1994). Nonetheless, it seems reasonable to expect that, in the future, deaths will occur more often outside the hospital than in the immediate past. Delivery systems and financing practices designed for inpatient care will need to be reevaluated to see how well they fit the circumstances and needs of patients dying at home or in nursing homes.
Data on site of death tell only a part of the story about the end of life. Relatively little is known about where dying patients spend their last few months. For example, the statistics reported above do not capture the experience of many older patients who live in nursing homes and are then transferred to hospitals on the day they die. In 1985, according to the Survey of the Last Days of Life (SLDOL) (which was limited to one part of Connecticut), 33 percent of women aged 65 to 74 but only 17 percent of those aged 85 and over died in the hospital after being transferred there from a private residence in the community within the last three months of their lives (Brock and Foley, 1996) (see Table 2.2). Among those in the 85 and over group, 21 percent of men and 35 percent of women spent their entire final three months in a nursing home and died there; about 8 percent of men and 9 percent of women died after being transferred from a nursing home to a hospital. The issue of patient transfers and the quality of end-of-life care are considered further in Chapter 4.
To say simply that someone spent their last days at home or in the hospital says little about the environment in which they died. A hospice unit within a hospital, for instance, may provide more support and comfort for the dying patient and the family than an intensive care unit. For those dying at home, hospice personnel are more intensively trained than other home care personnel to provide physical, psychological, spiritual, and practical care. In addition, for those who qualify for the hospice benefit, additional services are available (e.g., respite care for families) that are not normally covered by Medicare.
In 1993, the reported number of patients served by hospice was 256,900, indicating that only about 11 percent of the nearly 2.27 million people who died received hospice services (Christakis, 1996). More recent data from the National Hospice Organization estimated the number of those served by hospices in 1995 at 390,000, about 17 percent of the 2.31 million deaths that year (NHO, 1996a).
Although beneficiaries must have a life expectancy of six months or less to qualify for the Medicare hospice benefit, most patients spend much less time under hospice care. An analysis of a sample of Medicare beneficiaries admitted to hospice found a median length of survival after admission of 36 days (Christakis and Escarce, 1996). Notably longer median stays were found for patients with dementia (74 days) and chronic obstructive pulmo-
TABLE 2.2 Percentage Distribution for Locations Lived During the Last 90 Days of Life, According to Age and Sex (Survey of the Last Days of Life)
nary disease (76.5 days), but these patients comprised less than 5 percent of the sample. Similar proportions of patients died within 7 days of admission (15.6 percent) or more than 180 days after admission (14.9 percent), and about 8 percent lived more than a year.3
|
3 |
Many important questions have yet to be answered about hospice care including: which patients are appropriate for hospice referral and at what point in their illness; what the cost implications are of earlier referral; and what financial, cultural, or other factors affect the use of hospice services. Chapter 6 urges caution in government actions to penalize hospices caring for patients who outlive their six month prognoses. A recent story in the Boston Globe about a woman who lived more than a year longer than expected under hospice care illuminated the uncertainty of predicting the time of death (Foreman, 1996). |
How People Die: Symptoms of Impending Death
Detailed studies of the experience of dying are fairly limited, but the available data indicate both a considerable degree of commonality in the dying process and enough variability that no uniform model of caregiving or preparing for death will suffice. Common physiological signs of imminent death (i.e., death likely to occur within a few hours or days) include: "hypersomnolence, disorientation, irregular breathing, excessive secretions, visual and auditory hallucinations, decreased clarity of sight, decreased urine production, mottled skin, cool extremities, and truncal warmth" (Gavrin and Chapman, 1995, p. 269; also, many hospice publications). Some of these signs (e.g., disorientation, irregular breathing, hallucinations) may be distressing to families and perhaps to patients, whereas others (e.g., truncal warmth) may not.
The SLDOL study mentioned earlier reported that on the last day of life, three out of four elderly patients were nonambulatory, and 40 percent had difficulty recognizing family (Brock and Foley, 1996). Fifty-five percent were unable to eat, 44 percent were short of breath, and 33 percent reported some pain. The study also reported that 53 percent of patients were perceived to be in good or excellent health one year before their death with this number falling to 24 percent one month before death and to 11 percent the day before death. Unlimited mobility fell from 59 percent one year before death, to 30 percent one month before, and then to 13 percent on the day before death. Cognitive function declined at a slower rate than did physical function. One year prior to death, 87 percent of decedents had no difficulty with cognitive ability, as did 78 percent at the one-month mark, and 51 percent the day before death.
A patient's cognitive abilities may have a significant effect on caregivers, including their inclination to deny impending death or to become more emotionally distant. Figure 2.3 depicts rates of consciousness and ability to communicate in the three days before death as reported by family members in a large study of severely ill hospitalized patients (Lynn et al., 1996). A study of advanced cancer patients found that in the week before death, approximately half volunteered that they felt fatigued or mentally hazy/confused (Coyle et al., 1990). Generalized weakness, pain, shortness of breath, and anxiety were reported by more than a quarter of these patients.4
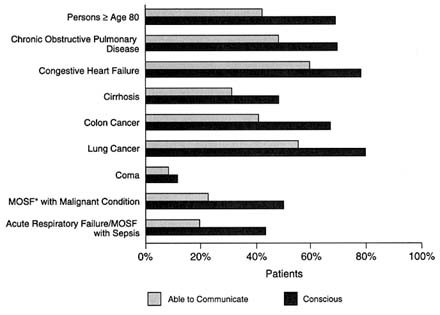
FIGURE 2.3 Rates of consciousness and ability to communicate (in patients 3 days before death, by medical condition, as reported by family members). *MOSF, multiple organ system failure. Source: Adapted from Lynn, J., Teno, J.M., Phillips, R.S., et al. Perceptions by family members of the dying experience of older and seriously ill patients. Annals of Internal Medicine 126(2): 97–106, 1997.
In addition to the nature of their disease, age affects people's experience of dying. Prior to death, according to data from the established Populations for Epidemiologic Studies of the Elderly, those dying at older ages experience more disability than those dying at younger ages (Guralnick et al., 1991).5 With the aging of the large baby boom generation, it is evident that these high disability rates "can have grave implications for the total population burden of morbidity and disability in future years" (Guralnick et al., 1991, p. 447).
The impact of age and disability will differ somewhat depending on trends in chronic disability among older people. The compression of mor-
bidity hypothesis posits that an increase in healthier life styles means that people will have relatively less disability before they die and, thus, that increasing life spans will mean less disability than would otherwise be expected. Evidence on this hypothesis has been mixed (see, e.g., Leibson et al., 1992; Leigh and Fries, 1994; Moons and Mackenbach, 1994; Tu and Chen, 1994). A recent analysis, however, reported declines in the prevalence of chronic disability among the elderly in the United States with recent declines (1989–1994) greater than in earlier years (1982–1989) (Manton et al., 1997).
Attitudes Toward Dying and Death
Reliable and valid research on American attitudes toward dying and death is surprisingly limited. In part, this reflects conceptual and methodological difficulties, for example, imagining hypothetical and—given current life expectancy—often far-distant situations (e.g., being incurably ill or comatose). The most intensive studies often rely on small, opportunistic samples, especially college students, but more methodologically rigorous surveys rarely focus on dying and death. One consequence is that it may difficult to assess how current initiatives to change perspectives and practices in end-of-life care actually affect attitudes.
Much of the social science literature on attitudes, particularly that generated in the 1970s and 1980s, has focused on the psychological construct of "death anxiety" (variously and confusingly viewed as a realistic fear of a real threat or as a neurotic over-reaction to the general prospect of death). In addition to reliance on small unrepresentative samples, critics have identified numerous conceptual methodological problems in such research (see generally the review by Neimeyer and van Brunt, 1995). For example, simple scales assume a single dimension of anxiety whereas fears or concerns about death appear to involve multiple dimensions including fears of pain and suffering, fears of the unknown, and concerns about the death of significant others. The growing interest in measures of quality of life has brought new perspectives to the field and an interest in identifying and improving the more rigorous instruments, such as the Death Attitude Profile-Revised (Wong et al., 1994; see also Thorson and Powell, 1994 and Chapter 5 of this report).
Broader public opinion polls have rarely dealt with anxieties about death. A 1995 poll sponsored by the American Association of Retired Persons (AARP) found that a substantial majority of those surveyed reported that thinking about death did not bother them (with 68 percent of those 18 to 64 and 76 percent of those 65 and over agreeing)(AARP, 1995). An earlier Gallup Poll indicated that most Americans rarely think about death (Gallup and Newport, 1991), which some might interpret as reflect-
ing death anxiety or denial. However, despite characterizations of the United States as a "death-denying society," direct evidence for this thesis is "remarkably sparse" (Neimeyer and van Brunt, 1995, p. 52). Moreover, some evidence suggests that education aimed at altering attitudes may sometimes arouse death anxiety rather than dampen it (McClam, 1980; Testa, 1981; Rigdon and Epting, 1985; Durlak and Riesenberg, 1991; Durlak, 1994).
Public opinion research has tended to focus on specific issues such as attitudes about assisted suicide, hospice, or advance directives. Since 1977, 13 surveys conducted by the National Opinion Research Center (NORC) have asked whether doctors should be legally allowed to painlessly end a patient's life if the patient and family request it. During this period, the percentage of respondents agreeing has risen from approximately 60 percent to about 70 percent. The 1996 poll showed that support was highest among younger people (over 75 percent in the 18 to 34 age group) and lowest among older people (about 60 percent in those age 65 and over). On the issue of whether a person has the right to end his or her own life (in an unspecified fashion) because of incurable illness, NORC surveys report a shift from majority disagreement in the 1970s and early 1980s to majority agreement in recent years (64 percent in 1996).
The NORC findings are generally consistent with other research (Harvard School of Public Health/Boston Globe Poll, 1991; Blendon et al., 1992; Foreman, 1996). A Gallup Poll taken in late summer 1996, however, reported that only 50 percent of those surveyed believed physician-assisted suicide should be legal (NHO, 1996b). This compared to 75 percent of those in an April 1996 Gallup Poll who responded positively to a question that was similar to the NORC question in not using the term suicide (Foreman, 1996). The late summer survey showed that women were less likely to believe that physician-assisted suicide should be legal and less likely to predict that they would avail themselves of that option should they become terminally ill.
Patient preferences regarding end-of-life care have been a particular interest of researchers, clinicians, and policymakers as reflected in the considerable literature on advance directives and similar measures, which is discussed in Chapter 3. When questioned about who people would want to make final choices about their care if they were seriously ill, a 1994 Louis Harris Poll reported that 67 percent of the national sample said that they wanted to make the decisions, but 28 percent wanted their doctor to decide (Medica Foundation, 1994).
Two Gallup Polls, one in 1992 and another in 1996, found 9 out of 10 respondents reporting that they would prefer to be cared for at home if they were terminally ill with six months or less to live (Seidlitz et al., 1995; Foreman, 1996; NHO, 1996b). These results are consistent with smaller studies (Townsend et al., 1990; McCormick et al., 1991). Although a ma-
jority of patients in both Gallup surveys expressed interest in a comprehensive program of end-of-life care at home, not all of those who were interested identified the term "hospice" with such a program. In the 1996 survey, 70 percent of respondents reported that they would seek hospice care, and 62 percent said they would still seek curative care. The latter figure indicates that people do not necessarily wish to forego curative efforts when they accept comprehensive palliative care.
Other research suggests that younger people express more willingness to forego resuscitation or ventilator support than do older people when they are asked hypothetical questions about preferences in the event of terminal illness (Gallup and Newport, 1991). A small study of patients seen at a Veterans Affairs medical center found that almost half said they would accept intubation and ventilator support even if the outcome would be persistent mental deficits (Mazur and Merz, 1996). In one exploratory study investigating patient views of states worse than death, coma, severe dementia, and loss of such functions as the ability to feed oneself were cited as possibly worse than death, but the stability of such views is unknown (Pearlman et al., 1993).
Surveys tend to highlight "mainstream" attitudes, or at least those attitudes easily tapped by pollsters, but there really is no "one" American attitude toward death and dying (Koenig and Gates-Williams, 1995; see also Appendix D). For example, studies of attitudes about advance directives and preferences for end-of-life care tend to show that whites are more favorably inclined to advance directives than African Americans and more likely to indicate that they would forego life-sustaining therapy (Caralis et al., 1993; Garrett et al., 1993; Steinberg et al., 1996). In a study of cancer patients (not necessarily terminally ill), researchers found cultural differences in views on family roles, information disclosure, expression of pain, and attitudes toward illness (Die Trill and Holland, 1993). In a study of 800 elderly patients, the University of Southern California found that the family dynamics in immigrant Korean or Mexican families allowed for less patient autonomy than in black or white families that had not recently immigrated (Blackhall et al., 1995; see also Mydans, 1995). The immigrant families were far more likely to believe that the truth about terminal diagnoses should be withheld from patients. Families, and not patients, were considered the proper decisionmakers in end-of-life care.
Conclusion
Dying is a both a biological process and a psychological and social experience that occurs in a cultural context. Trying to characterize briefly the distinctive aspects of the dominant American culture that influence attitudes toward death and dying is a task fraught with the risk of oversim-
plification, overstatement, or even caricature. The dominant culture—as expressed in the news and entertainment media, the professions, and other prominent social institutions—tends to be loosely described as Western (or European-American) and Judeo-Christian. The United States is, however, far from a cultural monolith. As described above, important cultural differences in attitudes and practices regarding end-of-life care exist within the United States, and these are often divided along racial, ethnic, and religious boundaries (Koenig and Gates-Williams, 1995; see also Appendix E). Nonetheless, the committee's experience with various health care systems and its review of comparative analyses points to the influence on end-of-life care of an actively interventionist medical profession, a deeply ingrained public philosophy of individualism, and a general American unwillingness to accept limits—including aging and death.
The interventionist bent of U.S. medicine, apparent in clinical practice and medical literature, has been widely noted (see, for example, Fuchs, 1974; Sontag, 1978; Aaron and Schwartz, 1984; Schroeder, 1984; Payer, 1988; McPherson, 1989; Aaron, 1991; Jecker, 1991; Jecker and Emanuel, 1995).6 Even a century ago, physician Oliver Wendell Holmes, Sr., was asking, "how could a people which has a revolution once in four years, which has contrived the Bowie knife and revolver … be content with any but 'heroic' practice?" (cited in Davies et al., 1983, p. 912).
The United States generally has high rates of surgery, diagnostic tests, and other procedures compared to other countries, even with neighboring Canada (see, e.g., Bunker, 1970; Notzon et al., 1987; McPherson, 1989; Aaron and Schwartz, 1990; Tu et al., 1997). Overall, a "technological imperative" (Fuchs, 1974) seems to characterize medical practice, including care of the dying. The result of this medical activism, some argue, can be tragic. Callahan has, for example, described "an unwillingness to let nature take its course" that often leads to an impersonal and unwittingly cruel "death in a technologic cocoon" (Callahan, 1995, p. 228). One study of physicians and nurses reported that nearly half of those interviewed admitted to having acted contrary to their consciences, mostly by providing overly burdensome treatment (Solomon et al., 1993).
The individualist strain in U.S. society seems to have become more evident in health care in recent decades and may, in some measure, be a response to excessive medical intervention. Traditionally, physicians have
been guided primarily by the principle of beneficence (doing good on someone else's behalf) rather than by the principle of autonomy (generally acting in accord with the wishes of informed patients) (see, e.g., President's Commission, 1983; Katz, 1984; Englehardt, 1986; Jonsen and Toulmin, 1988; Pellegrino and Thomasma, 1988; Kapp, 1989; Childress, 1990; Emanuel and Emanuel, 1992; Pellegrino, 1993; Beauchamp and Childress, 1994). Critics of this emphasis on beneficence characterize it as paternalistic, with too little regard for patients' concerns and values. The more recent ascendence of the principle of autonomy shows itself in the attention paid to issues such as patient preferences, informed consent, and physician-assisted suicide.
The stress on autonomy has, in turn, been criticized for sometimes being contrary to individual patient welfare and for being inimical to collective well-being (see, e.g., McCullough, 1988; Etzioni, 1991; Agich, 1995). For example, in contrasting the highly individualistic United States with the more community-minded Canada and Western Europe, observers repeatedly cite the lack of a "social contract" in the United States that would provide a basic level of health care (or, at least, insurance coverage) for all residents. In the United States, these critics argue, people may have the theoretical right to make their own medical choices, but many do not have the financial access to minimal care necessary for implementation of those choices. Moreover, a preoccupation with autonomy may encourage inattention to patients' concerns about their families (Doukas and Gorenflo, 1993). For example, in one public opinion poll, the most frequently expressed fear about death was the fear of being a burden to one's family (Foreman, 1996).
As noted earlier, some critiques characterize American culture as one that, in addition to being strongly individualistic, also is "death denying" and regards "death as a kind of accident, a contingent event that greater prevention, proven technology, and further research could do away with" (Callahan, 1995, p. 227). Although research support is limited, a cursory glance at bookstore shelves, magazine articles, advertisements for plastic surgery and miraculous herbal remedies, and similar sources would suggest that Americans are, at the very least, not very sanguine about aging (illustrated by, e.g., the cover article, "How Science Is Searching for Ways to Keep Us Forever Young," in the November 25, 1996 issue of Time magazine and also by books such as Stop Aging Now! [Carper, 1995] and Stay Young the Melatonin Way [Bock and Boyette, 1995]). Other critiques have suggested that Americans do not deal very well with dying and death and suffer much avoidable angst and expense as a result (see, e.g., Kübler-Ross, 1969; Veatch, 1979). A more sanguine view is that people in the United States are not so much death-denying as focused on the notion "of bringing
to bear every possible resource to prolong active and healthy life" and of accepting death only when "it is felt to be inevitable" and, then, trying "to mitigate its connections with suffering" (Parsons, 1963, p. 61).
The next chapter considers dimensions of caring at the end of life and ways of mitigating suffering. Each dimension involves patients, families, and clinicians in decisions that are often painful to make and difficult to implement. The nature and range of these decisions reflect the consequences of a century's worth of changes that have altered when, why, where, and how people die and intensified the need for better support for dying patients and those close to them.

















