3
Caring at the End of Life
When you come into my room … Sit at my "mourning bench" if you are my physician listen to me, talk truthfully to me
Steven Schmidt, When You Come into My Room, 1996
The twentieth century has seen birth and death—and much that happens in between—become events for institutional management. For most Americans, physicians direct and hospitals regulate many details of life's beginning and ending, sometimes excessively so. Technical and technological responses to illness can leave little time or thought for talking with patients, listening to their concerns, caring for them as people not diseases, and sitting at their "mourning bench," in the poetic words of Steven Schmidt, a sufferer from Crohn's disease (Schmidt, 1996).
The aggressively technical treatment of many kinds of health problems has been questioned, moderated, and sometimes spurned as its limits—not just its benefits—have been increasingly recognized. (See, for example, Wennberg and Gittelsohn, 1973, 1982; Illich, 1976; Reiser, 1978, 1993; Starr, 1982; Brook et al., 1986; Chassin et al., 1986; Blendon, 1988; Roper et al., 1988; Ware et al., 1988; Wennberg et al., 1988; Stevens, 1989; Cassell, 1991; Rothman, 1991; Gerteis et al., 1993; and Nelson and Nelson, 1995.) Attempts to mitigate the negative consequences of advanced technologies and narrow medical approaches to human problems have sometimes been based on the results of research or systematically defined professional consensus; other times, their basis has been primarily ethical or philosophical. Such attempts involve an acknowledgment that death brings losses but also a declaration that people can grow emotionally and spiritually as death approaches (see, e.g., Bernard and Schneider, 1996; Byock, 1997a; de Hennezel, 1997).
At life's beginning, birthing centers, selective use of medications and
surgical procedures, home birthing, renewed use of midwives, and child-birth education classes represent some responses to medical overreaching. At life's end, hospice and the recognition of a patient's right to refuse treatment likewise are indicative of medicine's need to recognize its limits. More general initiatives to change the nature of caregiving, which have been diverse and occasionally controversial, also may influence care at the end of life. Such initiatives include efforts to
- employ less invasive or disabling care options such as lumpectomy for certain breast cancers and "watchful waiting" for benign prostatic hypertrophy (see, e.g., Brook et al., 1986; Barry et al., 1988; Wennberg et al., 1988; Jackson, 1990);
- recognize the value of the caring function of medicine in addition to the curing and life-prolonging functions (see, e.g., Wheeler, 1990; Cassell, 1991; Gerteis et al., 1993);
- design friendlier environments of care as exemplified in warmer and more welcoming physical spaces, reduced noise levels, and displays of photographs and other personal items in patient or resident rooms (see, e.g., Gerteis et al., 1993);
- strengthen the quantity and quality of communication with patients and families, respond to requests for patient education, and recognize cultural differences (see, e.g., Greenfield et al., 1985; Koenig and Gates-Williams, 1995; Nelson and Nelson, 1995);
- develop instruments for assessing patient outcomes and perceptions of their care as a basis for establishing more accountability for clinician and system performance (see, e.g., Ware et al., 1988; Berwick et al., 1990; Gold and Wooldridge, 1995; and Chapter 5 of this report); and
- incorporate and welcome the contributions of many different health care personnel and of supportive services such as music and art therapy and other psychological approaches (see, e.g., Hurney, 1990; Sourkes, 1991; Connell, 1992; Larsson and Starrin, 1992; Breslow, 1993; Skaife, 1993).
The number and variety of these initiatives reinforce the basic messages that people—not diseases or technologies—are the central concern of health care and that people are much more than their illnesses. These initiatives likewise reinforce—and indeed have shaped and been shaped by—efforts to improve care for those approaching death and to establish palliative care as a legitimate clinical field. One practical challenge to those responsible for activating major changes in health care delivery is to distinguish intellectual or ideological fads from more enduring strategies and shifts in values.
This chapter focuses primarily on the patient, those close to the patient, and those directing and providing end-of-life care. It emphasizes that the experience and fear of unrelieved symptoms are fundamentally important
in their own right, as are concerns about loss of control and abandonment. The discussion attempts to provide a broad perspective on strategies for helping people live well while dying, but it does not attempt to serve either as a palliative care text or as more than an overview of the sources of support and comfort that lie outside the health care system. It also acknowledges that, particularly for those dying at home, professional caregivers may not have a substantial presence and that some may find medical care intrusive, especially if caregivers are not alert to patient and family wishes. Still, many patients and those close to them welcome an attentive medical presence, and for some, the absence of supportive and effective medical care may lead to despair and thoughts of suicide.
Differences in Dying Pathways: Illustrative Cases
Over 300 years ago, the playwright John Webster wrote in The Duchess of Malfi, "I know death hath ten thousand several doors for men to take their exits." The doors to death remain many and varied, although, as Chapter 2 described, today's most common patterns of death differ in key ways from the past. This section supplements the definitional and statistical discussions presented in Chapters 1 and 2 with a more qualitative consideration of how people may die and how care for dying patients may need to be adjusted to their circumstances.
Figure 1.1 depicted three prototypical trajectories of dying: sudden and unexpected; steady decline; and slow decline marked by periodic crises, one of which brings death. In addition to those people who are recognized as incurably ill with a clearly defined disease such as cancer or amyotrophic lateral sclerosis, two other groups are of interest. One consists of very old people who are functioning reasonably well but who are frail and have limited reserves to face an acute illness such as influenza or an injury such as a broken hip. Although these people initially may be expected to recover from the acute problem and their dying would not have been seen as likely in advance, a relatively minor event can precipitate a catastrophic cascade of complications that lead to death. The other group likewise consists of very old people whose organ systems are slowly deteriorating and who seem to just "wear out." That is, they have gradually diminishing cardiac function combined with osteoarthritis or some other condition that limits stair climbing, then housekeeping, and then other self-care tasks. Alzheimer's disease may develop, or stroke or renal failure, and pneumonia or other infections may become more frequent with flagging immune response. Whatever organ system is most relentlessly failing may be labeled the primary cause of death, but this is in the context of other less obviously failing organ systems.
Patients' experiences while dying are differently shaped by the nature of their illness; by patient, family, and others' reactions to it; and by the care provided for their physical, psychological, spiritual, and practical needs. To convey this variety of patient circumstances and needs, the committee composed a series of vignettes or synthetic case histories. The cases were selected to illustrate that the dying process for any given patient is determined by an interplay of many variables including the patient's illness, which will determine a particular "trajectory" of the illness, and the patient's personal circumstances and values, including economic and social status, ethnic and religious background, and presence of family and friends.
The cases draw on the experiences of committee members, published sources, including popular biographies, presentations at meetings, and conversations with many individuals and groups. None exactly depicts a real patient, and each is simplified to highlight differences in patients' needs and the ways in which care may be well or poorly fitted to those needs. Some describe situations that are reasonably common but not necessarily typical. Others describe unusual situations that particularly strain care systems or underscore the inevitable limits of human arrangements in coping with every possible problem. As explored further in Chapter 4, the dying process is also affected by the health care system, including the care options available in different communities and the expertise, values, and circumstances of health care professionals.
"Joleen Wright"
This case, which draws on committee members' experiences in caring for older people with varying problems, illustrates the difficulties that clinicians face in making decisions for patients who are not fully competent mentally and who have no family surrogate to act on their behalf.
Joleen Wright, an 87-year-old woman living in a nursing home, had been pleasantly convivial and moderately demented for some time. No family or friends were known. It was very hard to discern her preferences, as she "lived in the present" and did not trouble herself about future possibilities. She had chronic hypertension and hearing and motion deficits.
Gradually over a few weeks, she started doing "poorly," walking less, eating less, and seeming more distant. Over the next two weeks, a comprehensive evaluation in her nursing home setting turned up very little. Blood tests, physical exams, and chest x-rays were all normal, but she then became short of breath and was hospitalized. By the time she arrived at the emergency room, her blood pressure had declined to dangerous levels. She had mild problems with oxygenation, probably due to pulmonary edema, and was started on monitoring and careful fluid balance. Within 24 hours,
she had multiple attachments (e.g., IV, cardiac monitor, urine catheter) for monitoring and treatment and was restrained in bed to keep the connections in place. Her skin was breaking down on her shoulder blades. She was able to indicate "yes" or "no" to questions about her comfort but showed little insight or attention.
No definite reversible diagnoses surfaced despite appropriate work-up. Her condition worsened, and she faced the need for mechanical ventilation. The care team anguished over whether to continue intrusive care in the intensive care unit in order to establish a clear diagnosis or to shift toward a primarily palliative approach. Her condition continued to deteriorate, and she became minimally responsive. After a team meeting, the care team decided to institute hospice-type care and not to seek a court's involvement in getting a guardian. Joleen Wright died comfortably 36 hours later. Because no consent to autopsy could be obtained, the diagnosis remained a mystery.
"Horace Bowman"
The following case illustrates problems that patients and families can encounter with high-technology intensive care that is aimed solely at life-prolonging measures and not organized to consider the whole patient, the benefit/burden ratio of treatment, and the needs of family members for communication attentive to their concerns.
Horace Bowman was a 74-year-old man whose wife had died the year before. He had problems with angina and peripheral vascular disease but continued to smoke about a pack of cigarettes a day. He had not completed any advance directives and had been uncomfortable discussing possible future ill health.
He collapsed in the street after suffering a massive heart attack and was rushed to a major hospital center. His daughter lived across the country and flew in to be with her father. She found him unable to communicate because he was intubated, and his consciousness fluctuated. When he was alert, he clearly experienced pain and agitation.
Mr. Bowman's daughter wanted to discuss her father's chances of recovery and whether intensive care was helping. She found several physicians involved in her father's care, none of whom were willing to talk with her for more than a couple of minutes. On the fifth hospital day, the cardiac surgeon presented her with consent forms for an emergency revascularization procedure. She asked what the chances were that her father would survive and recover in any meaningful way. Rather than answer these questions, the surgeon merely noted that surgery was the "only hope." The daughter felt pressured to sign the forms.
As Mr. Bowman was being prepared for emergency surgery, he went into cardiac arrest and, despite prolonged resuscitation, died. The daughter felt that the intensive care environment deprived her of the opportunity to spend time with her father, made informed decisionmaking difficult if not impossible, and subjected her father to intrusive tests and interventions that would make her memory of his dying a continuing source of guilt and regret. She was, however, too drained of energy to complain and felt no one would respond anyway.
"Mike Pelli"
This case synthesizes the multiple phases of a child's serious chronic illness, which may at any time become life-threatening. After surgery that helped Mike gain several years, the recurrence of symptoms marked the beginning of an unpredictable trajectory toward death, a pattern also noted after palliative surgery for complex congenital heart disease and central nervous system anomalies (the two most common lethal congenital problems of infants). The case illustrates the need for ongoing evaluation and flexible care planning. It also points to a role in the process for the hospital ethics committee.
At the age of 10, Mike Pelli lapsed into a hepatic coma. He was previously diagnosed with biliary atresia (a defect of the bile ducts leading from the liver) at the age of 2 months. He was born to a single mother who was employed as a secretary and who had traditional health insurance with significant cost sharing for medications and various outpatient services (e.g., physician visits, rehabilitation).
At the age of two and a half, Mike had surgical treatment. For nearly six years, the surgery provided improved liver function; reduction in jaundice and malabsorption; and adequate growth, school performance, and development. Mike required five medications each day and multiple outpatient visits for adjustment of medications, nutritional counseling, and treatment of exacerbations of jaundice. All of this treatment placed a growing financial burden on the mother from medical expenses and loss of income when she had to take off from work to attend to Mike's medical problems. At 8 years of age, Mike began to experience repeated episodes of abdominal pain and vomiting blood. With deteriorating liver function, he required more outpatient treatment but was also admitted to the hospital several times. As a result of spending more and more time away from work, the mother lost her job and her health insurance. Mike and his mother were forced to move into a crowded apartment with relatives.
As Mike's condition deteriorated, the medical team proposed that he receive a liver transplant. This was discussed in detail with the mother and
with Mike, an intelligent 10 year old. Both wanted the procedure, and Mike was placed on the transplant list. Hospital social workers noted that he qualified for government-sponsored health insurance.
Then, Mike developed severe hepatic coma and was admitted to the pediatric intensive care unit. Without a liver transplant, his prognosis was very poor. The hospital ethics committee evaluated his medical condition, the prognosis with and without transplantation, the patient's and the mother's wishes, the obligations to the patient, and the issues related to defining when treatment no longer benefits Mike. The mother insisted that everything be done to keep Mike alive.
After two weeks, a donor was identified, and Mike underwent a liver transplant. He initially responded well and regained consciousness within 48 hours of the operation. However, on the third postoperative day, he complained of a severe headache, had a seizure, and became comatose. During initial discussion, Mike's mother refused discontinuation of the ventilator. A day later after strong evidence of brain death and a visit with members of the ethics committee, Mike's mother agreed to the removal of life support. As monitors and other supports were removed by a physician and nurse known to the family, relatives comforted Mike's mother.
"Martha Nielson"
This illustrative case suggests the complexities of caring for very elderly people, in this instance, a married couple. Some complexities are related to specific disease processes, in this case, congestive heart failure; others relate to the more general frailty and pattern of physical failure associated with advanced age.
Martha Nielson, an 86-year-old woman, lived with her 92-year-old husband, George, in their son-in-law's and daughter's "in-law" apartment. She was diagnosed with congestive heart failure several years earlier and used supplementary oxygen almost constantly. For the most part, she managed reasonably well and, during a period of five years, successfully underwent a hip replacement and cataract surgery, both of which improved her quality of life and functioning. She also had three hospitalizations for congestive heart failure, each of which left her somewhat weaker.
In addition, George Nielson began failing physically and mentally in multiple ways and needed more help with personal care than the family could provide. The family arranged with a local home health agency for visits by a home health aide. The first aide proved unreliable, and the next two were not much better. Finally, arrangements with another agency worked well, although after a few weeks it was clear that home care was no longer feasible. After a number of visits to area nursing homes, the daughter
arranged for Mr. Nielson to enter a nearby facility that would accept Medicaid if that became necessary.
Shortly before Easter, Martha Nielson became severely short of breath, and her daughter took her to a nearby hospital, where she had been treated before. After 36 hours, her physician of seven years reluctantly concluded—following consultations—that his patient would not survive this time. He hoped that using oxygen, diuretics, and morphine as comfort measures would provide enough time for family members out of state to arrive to say their good-byes. Most were with her when she died. Mr. Nielson was too frail to leave the nursing home and did not seem to understand fully what was happening. Five months after Martha Nielson's death, George Nielson died in his sleep.
"Eduardo Santos"
This case points to the frequent problem of inadequate pain management and the experience and role of family members. It portrays, in particular, the struggles of a daughter with her own feelings and the growth she finds in solving problems about her father's care.
Camille Santos was the 27-year-old daughter of Eduardo Santos, a 67-year-old Hispanic man sent home from the hospital to die of lung cancer. Their relationship had always been one of distant love and respect, but as the father's disease progressed, his daughter became increasingly alienated and depressed and withdrawn from her family. The father tried to protect his family from the reality of his progressing disease by maintaining a positive attitude and focusing on hope.
Upon returning home, Eduardo Santos quietly complained of severe unrelenting pain, but his physician declared there was nothing else that he could do. The family felt it was disrespectful to bother the doctor, although the father finally was moaning and begging for relief. The family was immobilized and clearly unable to act. There was no durable power of attorney document, although such a document would probably not, by itself, have helped this family.
Camille Santos turned to a local hospice where a social worker provided information about feasible and effective pain management, helped her through role playing to prepare for discussions with her family and her father's physician, and generally gave her encouragement and emotional support. When the physician again responded negatively to requests for stronger pain medication, the daughter was ready to ask for referral to the hospice, which quickly provided effective pain relief and guidance about how the family should prepare for Mr. Santos' death. After her father died peacefully at home with his family at his side, Camille Santos reported that
her ability to make a difference in his dying and death had changed her view of herself and given her confidence that she could do things on her own.
"Paul Bates"
Some people die unable to communicate and without a family member or other person who knows them to make decisions on their behalf. This case is adapted from a hypothetical teaching case used in an ethics seminar (S. Tolle, Oregon Health Sciences University, personal communication).
Paul Bates was a 57-year-old homeless man brought to the emergency room by a "friend" who dropped him off and left. In the emergency room, he provided a history of weight loss, cough, fever, and chills. He said that he had not previously received care in the community. After examination and testing, he was diagnosed with "necrotizing pneumonia." Shortly after admission, he got out of bed unobserved and was found unconscious in cardiac arrest. He was resuscitated after intubation, fluids, and 20 minutes of external cardiac massage. During the next 24 hours in the medical intensive care unit, Mr. Bates' condition deteriorated with evidence of septic shock, and he then became comatose. Calls to shelters, the police department, social service agencies, and other hospitals failed to uncover any family members or friends who could act as a surrogate. After five days, physicians decided to stop life support, and Paul Bates died shortly thereafter.
"Andrew Lindts"
This case illustrates a situation that is difficult not because physical, emotional, and spiritual caring were neglected but because the patient's personal characteristics and values were not responsive to this caring. The point is not to blame patients or caregivers but to caution against regarding what appear to be unfortunate outcomes as necessarily the result of failures in care.
Andrew Lindts was a 45-year-old business executive who suddenly noticed some weakness in his left leg and intermittent fatigue. A hard-driving personality, he ignored these symptoms. During a meeting, he abruptly developed generalized tremors and collapsed. He was diagnosed with a high-grade, malignant brain tumor with a likely prognosis of less than one year. He and his wife Laura were told about the diagnosis and prognosis and counseled about the options, which were highly unlikely to eliminate the tumor but might prolong his life—at the cost of significant unpleasant side effects.
Mr. Lindts appeared to accept his diagnosis not as a fatal illness but as a problem that he could overcome, just as he had overcome a variety of business setbacks. He had more than sufficient financial resources and personal connections to consult nationally regarded specialists. Despite cautions by these specialists, he demanded the most aggressive curative therapies. Even the term life-prolonging sounded too feeble for him to accept.
Initially, Mr. Lindts brushed off the physicians and friends who compassionately and sensitively tried to help him understand his medical situation and prognosis. For a while, he eagerly accepted positive thinking as a curative tool and consulted with its most optimistic adherents. As his symptoms worsened, he became increasingly depressed and wondered whether religion might help. Drawing yet again on his status and connections, he talked with several prominent religious leaders and was baptized.
Eventually confined to bed, Mr. Lindts continued to place heavy emotional pressure on family, friends, and caregivers, who coped as best they could. At the same time, he also showed signs of being ready to "let go" and told his wife and his doctor that he did not want life-sustaining interventions if he lapsed into a coma. He finally became relatively uncommunicative due both to his disease and his medications. He lost consciousness and died, with his family present, 11 months after the diagnosis. Family and friends were relieved but felt guilty about this reaction.
These cases illustrate how people approach death along many different paths. Some deaths are harder than others because of the nature of the disease, the characteristics of patients and their families, or the lack of care appropriate to these circumstances. As they seek to provide reliably excellent care for the usual kinds of patients, systems must also prepare to care well for atypical patients and problems. The remainder of the chapter considers several broad aspects of caring at the end of life:
- determining and communicating diagnosis and prognosis;
- establishing clinical and personal goals with patients and those close to them; and
- fitting care strategies—physical, psychological, spiritual, and practical—to patient goals and circumstances.
-
Determining and Communicating Diagnosis and Prognosis
Diagnosis
For life-threatening medical problems, the process of establishing a diagnosis and prognosis is more than a technical and analytical exercise for
clinicians to use in developing a plan to manage patient problems. It has an important interpersonal component that includes sensitive regard for what a period of testing and investigation may involve for patients in the form of uncertainty, anxiety, dread, physical discomfort, confusion, and isolation. Sensitive regard does not necessarily imply hiding the implications or intermediate findings of the diagnostic process. That may not be possible, nor may it be wise. A testing period can provide patients a time for reflection and initial coping that may buffer somewhat the shock of a terminal diagnosis. For those spared bad news (this time, at least), the process may encourage patients and clinicians to discuss the future prospect of a life-threatening illness or injury.
Prognosis
Once a diagnosis is established, the question of prognosis often follows.1 For patients and those close to them, estimates of survival time may guide practical decisions (e.g., financial arrangements, travel plans of distant family members) and prompt attention to the spiritual and other ramifications of dying, including the prospect of reconciliation with family or friends. As noted elsewhere in this report, predicting length of survival is not a precise science. Prognostic uncertainty complicates referral to hospice under the Medicare benefit, which requires that patients be certified as having six months or less to live. Government auditors have investigated hospice care for patients who have lived longer than six months and have issued financial penalties (see Chapter 6). These investigations may further discourage timely referral to hospice, which is a long standing problem that may be less a funtion of prognostic uncertainty than of reluctance to acknowledge the approach of death (Christakis, 1994, 1995; Christakis and Escarce, 1996).
Life expectancy is the most prominent feature of prognosis, but prognoses may also include qualitative assessments of the likely physical and mental course of the person's illness to death. Just as planning will be affected by estimates of how long a patient has, it will also be affected by the prospects for physical disability, mental dysfunction, and dependency. Prognosis is usually not a one-time assessment but rather involves periodic reassessment of a patient's prospects.
Several clinical predictive models have been developed and have demonstrated their value in helping clinical investigators, intensive care directors, clinicians, and researchers understand patient risk factors as an ele-
ment in making decisions and evaluating outcomes (see, e.g., Knaus et al., 1986, 1991, 1995; Pollack et al., 1987; Tores et al., 1987; Chang, 1989; Chang et al., 1989; Diamond, 1989; Selker, 1993; Zimmerman et al., 1994; Hamel et al., 1995; Lynn et al., 1995, 1996). Notwithstanding the value of these models, establishing prognosis is not and probably can never be an exact science. The limits of prognosis involve a mix of methodological and statistical issues as well as problems related to the applicability of the models in actual clinical practice. For example, it takes a very large database to provide the information necessary for precise estimates of survival for different kinds of patients. Given the relatively small numbers of deaths among children, this poses a particular problem for those working with pediatric prognostic models (Pollack et al., 1994). In addition, the complexity of these models may limit their acceptance by physicians and families. A background paper (Appendix D) prepared by a member of this committee lays out these issues.
Communication
Physician and patient narratives reveal that the communication of grave diagnoses and prognoses is a source of profound apprehension and uncertainty (see, e.g., Nuland, 1994; ABIM, 1996b; see also more generally, Katz, 1984; Seravalli, 1988; Buckman, 1993; Gerteis et al., 1993; Strickland and DeSpelder, 1995). Poor communication can traumatize patients and families, interfere with the ability to participate in decisionmaking, and generally undermine their capacity to cope with life-threatening illness. It may likewise haunt physicians and prompt them to avoid patients in a time of particular vulnerability and need. Not surprisingly, a prominent component of initiatives to improve medical education in end-of-life care includes role playing and other exercises involving the communication of bad news to patients and families (see Chapter 8).
Clinicians, counselors, ethicists, researchers, and lawyers have contributed to guidance on how to initiate communications with patients and families about life-threatening medical problems (see, e.g., Katz, 1984; Buckman, 1993; Gerteis et al., 1993; Campbell, 1994; Minnesota Hospice Organization, 1995; Quill, 1995; ABIM, 1996b; Moldow and Carlsen, 1996; Ptacek and Eberhardt, 1996). Effective communication is a skill that, ideally, is informed by such humanistic qualities as compassion, empathy, and sensitivity. Some general principles of patient-clinician communication as well as more specific suggestions for communicating difficult news are summarized in Box 3.1 and illustrated with examples in Box 3.2. A recent review of the literature on this topic suggested that patients and physicians tended to agree on these principles but that little empirical research has been done to test differences in approaches (Ptacek and Eberhardt, 1996).
More generally, patients and family should be able to get as much information as they want; for some, that will be a great deal, for others, much less. The basic view of those caring and advocating for people who are dying is that patients and those close to them should always be able to have their questions answered fully, and they should be able to get information when they need it, day or night. These needs may not be well under-
|
BOX 3.1 Communicating a Bad Prognosis to Patients and Families
|
||||||||||||||||||||||||||||||||||||||||
|
BOX 3.2 Examples of Communicating a Bad Prognosis
|
stood by many clinicians. Some studies have suggested that many people do not understand terms used by their physicians, and physicians tend to underestimate patients' desires for information (McCormick and Conley, 1995). Moreover, clinicians who see patients on very tight schedules that are arranged to meet productivity or profit objectives may not provide patients and families with the opportunity to raise their most troubling questions.
Although recent decades have, seen a generally beneficial emphasis on patient autonomy and more open communication about death, the committee cautions that it may be neither humane nor absolutely necessary to impose explicit communication on those people who regard talking about death as unwise, unlucky, or a violation of their spiritual beliefs. Moreover, those who have experienced discrimination and deprivation may distrust a judgment that their prognosis is terminal and the suggestion that aggressive attempts to prolong life will be ineffectual and even hurtful. Thus, sensitivity to the social and cultural values and experiences of patients and those close to them is important in guiding communications about care at the end of life.
Some patients, including infants and mentally incapacitated people, are not directly involved in discussions of diagnosis or prognosis or in decisions about care. Parents, adult children, and others play the central role. Com-
municating with older children and adults with greater but still limited mental capacity presents special challenges both in communicating information and considering treatment preferences. (See Chapter 7 for a discussion of legal issues.)
Parental grief, variations in children's emotional and intellectual development or maturity, and uncertainty about what a particular child can cope with make deciding when and what to tell children a particular challenge (see, e.g., Bluebond-Langer, 1978; Wass and Corr, 1984; Smith et al., 1993; Stevens, 1993; Kliegman, 1994; Buckingham, 1996). Children may draw conclusions about their condition from adult behavior without being explicitly informed; to assume that they are unaware can lead to neglect of their fears and anxieties. If secrecy or pretense was the primary stance 30 years ago, today the dominant view endorses open communication matched to the child's conceptual and emotional maturity and desire to talk.
Table 3.1 presents a framework for caregivers' communication with dying children. In addition to diagnosis and prognosis, communication about fears, wishes, pain or other symptoms, and preferences or feelings about treatment also presents especially sensitive issues for children at different levels of development and for their parents.
Establishing Goals and Plans
Sensitivity to patients and family values is also important in communication to establish goals and plans for end-of-life care. One fundamental principle of patient-centered care is "to ask, not assume: to ask patients what they want to know, to suggest questions that patients might have" and to develop culturally sensitive interview protocols to elicit patient perceptions, expectations, and preferences and goals (Gerteis et al., 1993, pp. 39–40). A related principle is to understand that preferences and goals may change as an illness progresses so that some concerns recede in importance as others become more dominant.
Sometimes, a patient's preference may be to defer as much as possible to the physician, the hospice team, or family and to avoid direct discussion of options, risks, and benefits (Medica Foundation, 1994; Koenig and Gates-Williams, 1995). Thus, physicians, nurses, social workers, and others caring for dying patients cannot assume that patients will wish to discuss death explicitly or will want to be actively involved in planning their care. Physicians, likewise, cannot assume that patients will initiate a discussion of preferences and expectations, although some patients and families certainly will. Whether patients, families, or physicians initiate a discussion, many of the communication strategies presented in Box 3.1 will apply.
Some goals, such as those related to symptoms, life-sustaining interventions, and other clinical matters, may be explored with physicians, nurses,
TABLE 3.1 General Suggestions for Age-Appropriate Communication for Dying Children
|
Ages |
Main concept of death |
Communication approach |
|
0–2 |
None |
Provide maximum physical relief and comfort |
|
2–7 |
Death is reversible, a temporary restriction, departure, or sleep |
Minimize child's separation from parents. If parents unavailable, provide reliable and consistent substitute. |
|
|
|
Correct misperceptions of illness as punishment for bad thoughts or actions. Evaluate for feelings of guilt, resentment. |
|
7–11/12 |
Death is irreversible but capricious |
Evaluate for fears of abandonment, destruction, or body mutilation. Be truthful and open. Provide details about treatment. Reassure that treatments are not punishments. Maintain access to peers. Foster child's sense of control, mastery. |
|
12+ |
Death is irreversible, universal, personal, but distant |
Reinforce comfortable body image, self-esteem. Allow ventilation of anger. Provide privacy. Support reasonable measures for independence. Be clear, honest, and direct. Maintain access to peers. Consider mutual support groups. |
|
SOURCE: Adapted from Wass, 1984. Used with permission. |
||
and other clinicians as well as family. Discussion of goals related to existential or spiritual issues may involve trained chaplains and social workers. Social workers may also be very much involved in discussions of finances, the availability of services, and coping mechanisms. One challenge for those involved with dying patients and those close to them is to establish effective communication among members of the health care team and relevant administrative personnel. The goals of care need to be clear and accepted by all.
For some people, it may be feasible and valuable for communication about end-of-life care to begin well before a diagnosis of incurable illness. For example, a physician with an established relationship with a patient may, during a routine medical visit, initiate a brief discussion about preferences in the event of a catastrophic illness or injury or about the identification of a surrogate decisionmaker. The advantages of early discussion may include encouraging at least basic preparations for the unexpected (e.g., signing a durable power of attorney); reinforcing the relationship between clinician and patient; and laying the foundation for later, more specific discussions (Teno and Lynn, 1996). This kind of communication may be less likely to occur when patients lack a continuing relationship with a personal physician.
Elements of Advance Care Planning
The details of advance care planning may be highly specific to patients and families, but certain general elements can be identified. These elements are not so much a matter of specific documents—although such documents can be very useful—as they are parts of an ongoing process that includes discussions with patients and those close to them about what the future may hold; what the patient and family want to achieve as life ends; what options are available—and what their potential benefits and burdens are; what preferences should guide decisions; what practical issues should be anticipated; and, depending on the circumstances, what immediate steps should be taken. In this broad sense, advance care planning provides an important basis for a cooperative effort, first, to understand people's physical, emotional, practical, and spiritual concerns; second, to prevent distressing and unwanted interventions; and, finally, to secure what the patient, family, and care team will regard as a good death.
In addition to raising a variety of practical issues and actions, those offering support may suggest that patients and families go through a values exercise to clarify what they hope for and fear. One approach to such an exercise is included in Box 3.3.
Advance care planning often includes written directives. The directives and their legal context are discussed in Chapter 7. Table 3.2 suggests the kinds of issues to be raised with patients depending on their health status, cultural backgrounds, and preferences. In general, the guidelines for communication identified earlier in Box 3.1 will apply to advance care planning discussions.
The stability of patient preferences about treatment at the end of life is an important concern but one not investigated in-depth. What might seem desirable when death is a distant, abstract possibility may be frightening when one is actually diagnosed with an eventually fatal disease. Once people
|
BOX 3.3 Values Questionnaire Adapted from the Vermont Ethics Network
|
||||||||||||||||||||||||||||||||||||||
have become quite ill, they—and those close to them—may still change their perceptions of the benefits and burdens of continuing or foregoing treatment. A large study of seriously ill hospitalized patients found that most patients desired cardiopulmonary resuscitation during their initial interview and 70 percent expressed that preference two months later. Of those preferring resuscitation initially, 85 percent maintained that view whereas of those preferring no resuscitation, 69 percent sustained that view (Rosenfeld, Wenger, et al., 1996). Dialysis patients in another study varied greatly in their desires that previously prepared advance directives be followed as compared with allowing surrogates to exercise discretion (Sehgal, 1992). Given these considerations, communication about goals, options, and preferences should not be envisioned as a single event but as a process that occurs as a patient moves toward death.
Issues in Advance Care Planning
Overall, experience with advance care planning indicates that continued investigation is needed to determine the value and limits of such planning and the factors that make it more or less likely to occur and to be helpful to patients and clinicians. The general literature on decisionmaking and decision implementation and the research on advance care planning specifically suggest that effective advance care planning depends on several factors (see, e.g., Lo et al., 1986; Brunetti et al., 1991; Emanuel, 1991; Sachs et al., 1992; Emanuel, 1994; Emanuel and Emanuel, 1994; Morrison et al., 1994; Virmani et al., 1994; Emanuel et al., 1995; Lo, 1995; SUPPORT Principal Investigators, 1995). These factors include:
- patient and family knowledge. As indicated earlier, some patients and families may want to defer to physician judgments and choices. Patient knowledge is also a consideration in advance care planning. Research suggests that a significant proportion of patients are not familiar with such instruments as living wills or durable powers of attorney, that patients may not understand the language used in these instruments, and that patients may be more optimistic about their prospects and options than is warranted (Murphy et al., 1989; Joos et al., 1993; Teno, Lynn, Wenger, et al., 1997). Interventions to inform patients and provide them the opportunity to complete advance directives have generally shown increases—often substantial—in the proportion of patients with advance directives (Reilly et al., 1994; Baines, Barnhart, et al., 1996; Hammes and Rooney, 1996; Teno, Lynn, Wenger, et al., 1997). In contrast, one study of interest in advance directives found that the 5 percent of patients who were not at all interested in advance directives were more likely than the other 95 percent to have spent time in an intensive care unit (Gilligan and Jensen, 1995).
TABLE 3.2 Adapting Advance Care Planning to Patient Circumstances: Possible Issues and Actions
|
Health status |
Issues for discussion |
Actions |
Persons to lead action |
|
Healthy |
Surrogate decisionmaker |
Suggest completion of durable power of attorney |
C |
|
|
Health concerns |
Discuss possibilities in a medical emergency |
C, P |
|
|
Preferences or beliefs |
Discuss values and preferences with surrogate |
P |
|
|
|
Document strong preferences in patient record |
C |
|
Diagnosis of serious illness |
Surrogate decisionmaker |
Complete durable power of attorney |
P |
|
|
Prognosis and options |
Discuss possible and likely outcome states in relation to care options |
C, P, F |
|
|
Preferences or beliefs |
Discuss values and preferences in the event of an emergency |
P |
|
|
|
Document preferences in patient record |
C |
|
Diagnosis of life-threatening illness |
Surrogate decisionmaker |
Determine status and location of durable power of attorney documents |
C, P, F |
|
|
Preferences |
Discuss and document preferences for end-of-life care and make arrangements as appropriate |
C, P, F |
|
|
Goals |
Discuss hopes and expectations for the last stage of life |
C, P |
|
|
Contingency plans |
Make specific plans for likely complications and urgent situations |
C, P, F |
-
- patient and family socioeconomic characteristics. Some research suggests that those most likely to have an advance directive are white, elderly, educated, and tend to plan for the future. For example, one study found that 34 percent of people with estate wills also had advance directives, while only 7 percent of those without estate wills had such directives (Sachs, 1994). Another report indicated that African Americans and Hispanic Americans were less willing than others studied to complete advance directives (Caralis et al., 1993).2
- clinician characteristics and clinician-patient relationship. Little specific appears to be documented about clinician characteristics associated with greater or lesser discussion and acceptance of patient goals and preferences for end-of-life care. For example, the SUPPORT study found that only about 60 percent of the physicians who had received information on patient prognosis actually reported that they had the information and only about a third recalled receiving information on patient preferences, but the investigators did not report data on physician characteristics linked to these
- results (SUPPORT Principal Investigators, 1995). Elsewhere, the study investigators have reported that some physician behaviors were associated with specially status (e.g., cardiologists being less likely to write DNRs than pulmonologists or intensive care specialists) (Hakim et al., 1996). More generally, many believe that the dominant medical culture makes it difficult for physicians to accept patient wishes to forego treatment, at least when clinicians see some chance for successful treatment (see, e.g., Katz, 1984; Schneiderman et al., 1993; Nuland, 1994; Annas, 1995; and Chapter 8 of this report).
- characteristics of educational and decisionmaking processes. Inadequate processes for patient and family advance care planning and lack of clinical information about patient prognosis and preferences have been identified as problems. Efforts to improve information, decisionmaking, and outcomes have sometimes proved disappointing. Most notably, one stimulus to the consideration of new strategies is the disappointing results of a major intervention to improve discussions and knowledge of hospital patients' preferences through information and counseling (SUPPORT Principal Investigators, 1995). The patients assigned to the intervention (or their surrogates) were not more likely to report a discussion with a physician about resuscitation or prognosis, to have their preferences known to their physician, to have DNR orders documented, to have them documented earlier, to spend fewer days in the intensive care unit, or to have different levels of resource use. Almost half the DNR orders were documented during the last two days before death, and barely half of patients who preferred not to be resuscitated had DNRs written (Hakim et al., 1996). The percentage of patients with some kind of advance directive was essentially unchanged at about one in five, but those in the intervention group who had such directives were more likely to have them documented in the medical record (Teno, Lynn, Wenger, et al., 1997).
- organizational structures and processes. Increasingly, organizational systems are viewed as major determinants of practice patterns including practices related to care at the end of life (Pritchard et al., 1994; Reilly et al., 1994; Berwick, 1995; Blumenthal and Scheck, 1995; Solomon, 1995). The focus then becomes identifying and remedying faulty processes rather trying to identify, change, or punish faulty individuals. The SUPPORT investigators discovered considerable differences among the five medical centers they studied, and factors associated with these differences are still being studied. In general, it might be expected that values and practices might differ from general community hospitals to highly specialized academic medical centers. Likewise, an organization with strong computer-based patient records and information systems should be better able to document patient directives, make information readily available to clinicians, and provide data allowing outcomes to be assessed and problems
- identified. Individual studies suggest that it is possible to have high rates of advance directive documentation (Hammes and Rooney, 1996).3
- cultural and legal factors. The influence of cultural values and beliefs on patient and family preferences and behaviors has been suggested above and in Chapter 2. The role of medical culture is evident throughout this report. The most obvious attempt by public officials to support patient preferences is the Patient Self-Determination Act (PSDA). The PSDA is still relatively recent. Its implementation has been complicated and its effects remain uncertain. Chapter 7 considers the PSDA and other legal considerations in end-of-life care, and Chapter 6 considers economic issues. The specific effects of financial incentives on advance care planning have yet to be adequately studied. Cultural differences also appear to play a role both in the individual use of advance directives and physician regard for such directives (Sehgal et al., 1996).
Given this multiplicity of influences on advance care planning and the limited evidence of the effectiveness of written directives, it is not surprising that a number of observers have questioned the emphasis on such documents (see, e.g., Lynn, 1991; Lo, 1995; Solomon, 1995; Emanuel, 1996). One commentator has argued for the testing of more rigorous models of structured decisionmaking that draw on studies of shared decisionmaking that focus on factors that are most amenable to change (Emanuel, 1995b). Others stress the need to change organizational processes, structures, and values. Chapter 5 focuses on such changes in the broader context of efforts to assess and improve the quality of care.
Fitting Care to Goals and Circumstances
Fitting care to patient goals and circumstances involves periodic appraisal by patients, families, clinicians, and others of a number of factors. Box 3.4 highlights questions that will be relevant for most patients, except those whose dying process is so rapid that palliative and other interventions are precluded.
Dimensions of End-of-Life Care
Care at the end of life is particularly intense in its attention to different dimensions of the illness experience. These dimensions, each of which may vary in importance at different stages in the process of dying, include the physical, emotional, spiritual, and practical.
The Physical Dimension of Care
Physical comfort is a basic priority in care for those who are dying. Physical care emphasizes the prevention and relief of symptoms and includes attention to hygiene, nutrition, skin care, and other physical factors that affect patient well-being.
Beyond the initial evaluation of a patient and the development and acceptance of a care plan, physicians may be most active in evaluating and managing especially difficult symptoms such as intractable pain. On a day-to-day basis, high-quality physical care is, in large measure, a function of high-quality nursing care that considers individual patient circumstances (e.g., proximity of death) in responding to symptoms (e.g., suctioning secretions). Nursing care includes both professional services and care by family and others close to the patient. Physical therapists, pharmacists, nutritionists, and others play variable roles depending on specific patient needs, and the availability of family care can be a major consideration in determining whether home hospice care is feasible for a patient. (The concept of the palliative care team is discussed further in Chapter 4.)
Good end-of-life care requires solid familiarity with the incidence of specific symptoms associated with various illnesses and understanding of symptom pathophysiology and complexity, especially coexistence of multiple symptoms. Box 3.5 lists major physical and psychological symptoms that dying patients may experience, depending on the nature of their disease and other variables. Sometimes these symptoms are a result of efforts to cure illness or prolong life. As is true in caring for all patients, the first step in excellent end-of-life care is conducting a careful patient history and examination to identify medical and personal factors that may be responsible for the patient's symptoms.
In addition, family and other nonprofessionals involved with caring for someone with advanced illness may need to be prepared to recognize and cope with physical and emotional symptoms and to recognize when to seek professional help. Hospices typically assist with such preparation. The American College of Physicians (1995) has prepared a home care guide for family, friends, and hospice workers caring at home for people with advanced cancer. The guide, which offers much information and advice that would be useful for other advanced illnesses, covers a wide range of physi-
|
BOX 3.4 Assessments Needed in Devising Palliative Care Plan
|
||||||||||||||||||||||||||||||||||||
cal problems (e.g., tiredness, nausea, pain), emotional issues (e.g., companionship, depression, anxiety), and practical concerns (e.g., getting information from medical staff and help from community agencies).
The Psychological Dimension
The psychological dimension of end-of-life care, which encompasses both cognitive function and emotional health, calls for openness and sensitivity to the feelings and emotional needs of both the patient and the family. It includes—but is not limited to—the identification and treatment of depression, anxiety, and other common psychological problems identified in Box 3.5. Care typically combines clinical and nonclinical elements. For example, depression can often be clinically diagnosed and managed with medications and psychological interventions, but spiritual and other forms
|
||||||||||||||||||||||||||||||
of caring may complement or—for some—supplant typical medical treatments for depression.
The controversy over assisted suicide has focused particular attention on the role of depression in desire for assisted suicide (see, e.g., Lee and Ganzini, 1990; Cochinov et al., 1992; 1994; Block and Billings, 1995; Ganzini and Lee, 1997; Groenewoud et al., 1997). The diagnosis and management of depression in people with advanced illness is, however, important in its own right, although conventional treatments such as slow-acting medications or psychotherapy may be of limited value for those with a limited prognosis or restricted communication capacities.
Psychological caring involves recognizing and managing emotional barriers to accepting incurable illness and preparing for death. For example, when a family insists—against completely uniform medical advice—that "heroic" life-prolonging measures be attempted for an irreversibly uncon-
|
BOX 3.5 Major Physical and Psychological Symptoms Pain |
|
Bowel Problems Constipation may be cause by certain medications, emotional stress, reduced intake of food and liquid, or decreased activity. Diarrhea is less common than constipation in cancer patients but is considerably more common in HIV-infected patients. Bowel incontinence is a major disability for dementia and stroke patients, causing serious burdens to patients and their families. Mouth Problems Dying patients may be troubled by various mouth problems, including dry mouth, sores, dental problems, and infections. These symptoms, which are uncomfortable or painful in themselves, tend to make eating, drinking, and taking of medication unpleasant, and they thus may lead to dehydration and malnutrition. Meticulous moistening and cleanliness can be among the most important services to prevent suffering in a patient nearing death. Skin Problems Skin problems that cause distress may arise from the underlying disease, treatments for the disease, or both. Problems include itching, dryness, chapping, acne, sweating, extreme sensitivity to touch, dark spots, and pressure sores. In addition to causing physical discomfort, skin problems may be perceived by patients as indignities to be hidden from others. Lymphedema Tissue swelling due to the failure of lymph drainage may be caused by infection or by therapies such as surgery and radiation. It is often uncomfortable, unsightly, and movement limiting. Ascites The accumulation of liquid in the abdomen occurs in 15 percent to 50 percent of terminal cancer patients and in virtually all patients who die of liver failure. Ascites cause a feeling of bloating, as well as discomfort from the stretching. Confusion Confusion is a mental state in which patients react inappropriately to their environment because they are disoriented or bewildered. Confusion may be caused by decreasing mental capacity or by medications and may render patients unable to care for themselves. They may mistake their own abilities and overexert themselves or lose their balance. Confusion also complicates communication between patient and family or caregivers. Dementia A common cognitive complication in the older elderly and in younger patients with such diseases as AIDS and stroke, dementia may begin with subtle symptoms, such as apathy, social withdrawal, and difficulty in concentrating. If progressive, dementia moves through deterioration in verbal and motor responses to a complete inability of patients to move about or care for themselves. |
|
Anxiety Anxiety is a biological and emotional reaction to stressful situations, including diagnosis of an incurable illness and the approach of death. If the sense of dread, danger, or tension is severe, it may interfere with the ability to eat or sleep and may be associated with shortness of breath, nausea, diarrhea, or increased heart rate. Depression Although emotions such as sadness are common with the approach of death, clinical depression is a more serious condition. At its most severe, depression is syndrome of sad mood and over whelming despair that saps the psychic and physical energy that is necessary for coping with illness. It may interfere with appetite, sleeping, personal hygiene, and social interactions, including communication with family and caregivers. In some depressive symptoms may be caused by a chemical imbalance created by medications or disease. Source: Doyle et al., 1993; Stedman's Medical Dictionary, 1994; ACP, 1995. |
scious patient, the specific response may depend on the extent to which the family is understood to be expressing grief, guilt, religious teachings (or, possibly, misunderstanding of these teachings), or inadequate knowledge of the patient's condition. The appropriate response might be to arrange conversations with a social worker, psychologist, chaplain, or clinician skilled in explaining medical problems to lay people. A hospital ethics committee may also be involved.
One issue that many cancer, AIDS, and other patients are confronting is prolonged survival following the diagnosis of life-threatening illness that involves a high likelihood of death and intensive medical interventions (NCI, 1990; Nessim and Ellis, 1991; Zampini and Ostroff, 1993; Loscalzo and Zabora, 1996; Sullivan, 1996). Another problem for cancer and AIDS patients is that these illnesses still tend to be stigmatizing even for those whose physical problems are still minimal.
Emotional care extends beyond a patient's death to concern for grieving families and friends (IOM, 1984; Zimmerman, 1986; Buckingham, 1996). In cases of sudden death, bereavement care may be all that can be offered. Such care may range from providing a time and a place for survivors to be alone with the body to extensive grief counseling.
The Spiritual Dimension
For many, the approach of death inspires a search for meaning, peace, or transcendence that can replace fear and despair with hope and serenity
(see, generally, Hoy, 1983; Reed, 1986, 1987; Sodestrom and Martinson, 1987; Hay, 1989; Kaczorowski, 1989; Speck, 1993; Byock, 1996, 1997a). Hope for a cure may persist in those with incurable illnesses, but other kinds of hope can also be a bulwark in the face of death. One can have hope of comfort, personal growth, love, reconciliation, courage, renewed happiness for one's family, or illumination about the mystery that is death.
The search for meaning or spiritual comfort in the face of death is often guided by religious and philosophical beliefs. Even for patients and families without a religious or philosophical belief system, counseling or discussions with chaplains, carefully selected hospice volunteers, or others with special empathy and insight may prove comforting. The needs of "nonreligious" people sometimes, however, create "a measure of confusion" for those who are not accustomed to this perspective (Speck, 1993, p. 517).
The role of spiritual caring is, in principle, widely recognized in hospital provisions for chaplains and religious services and inclusion of chaplains or other religious advisers in hospice and hospital palliative care teams. How well trained and prepared these individuals are to provide spiritual support dying patients and their families needs more systematic study as does the nature and variability of support provided to patients and families by the religious congregations with which they are personally affiliated.
Because nurses spend considerable time with patients, they are often well placed to identify those who could benefit from discussion of spiritual issues. Some clinicians and patients will find prayer or other shared spiritual experience comfortable and comforting. Marked religious differences between patient and caregiver can, however, sometimes create problems.
The clinician's role is, at a minimum, to avoid obstructing spiritual explorations. Such obstruction is unlikely to be willful but instead to reflect the clinician's own discomfort with death as an existential phenomenon rather than a technical problem to be analyzed and solved. In any case, "to ask people to assess where someone has reached in the personal search for existential meaning is quite daunting" (Speck, 1993, p. 517).
Spiritual—like emotional—caring embraces those close to the patient and extends beyond the patient's death. Sensitive end-of-life care has traditionally made provision for religious rituals, such as the "last rites" of the Catholic Church, the Islamic rituals around the time of death, or the after death and burial practices of the Jewish faith.
The Practical Dimension
Individuals and organizations helping those with advanced illness, especially illness expected to end in death, can do much to alleviate the practical burdens that typically accompany such illness. They can advise and assist patients and families in arranging home health services, in mak-
ing changes in physical features of the home, in shopping for groceries and doing other routine errands, in coping with visitors, and in juggling work schedules.
The willingness of those in the community to be of help can make an important difference in the experience of patients and families. Beyond providing pastoral care and friendly visitors, churches can deliver very concrete help in the form of meals, home repairs, transportation, and shopping. Neighbors who rally round those in distress not only provide practical help but symbolize community values. Employers can be flexible about working hours, vacation time, and reemployment opportunities for caregivers. Groceries and pharmacies can deliver to homes. In dozens of ways, communities can be supportive—or can leave very sick people and their families to fend for themselves. Clearly, the latter course makes caring well for those approaching death a much more emotionally, practically, and financially burdensome task.
Box 3.6 suggests just some of the practical issues that dying patients and those close to them may have to face. Some are not applicable to those who die suddenly or very quickly, and some are more relevant to those whose dying is managed in the home rather than in an institution.
The practical often overlaps with the physical, emotional, and spiritual dimensions of caring, and these three latter dimensions also mix with each other. For example, helping someone maintain a positive self-image—so important in emotional well-being—may require assistance with the most mundane matters, such as bathing, shaving, or shampooing hair. On a more profound level, in achieving a sense of meaning or peace or transcendence, a person may find that physical discomfort or disfigurement shifts from being an overwhelming problem to a peripheral concern. Conversely, delusions and other mental side effects of disease or medications can impede a person's spiritual journey. The basic point is that caring that attends to one need may serve other needs as well.
Variations in Emphases and Models of Care
Care for a dying patient may include preventive, life-prolonging, rehabilitative, and palliative care in varying proportions depending on the patient's medical problems and preferences. For example, for a patient for whom death is thought to be weeks, months, or even years distant, preventive services such as influenza immunizations may help extend meaningful life. For a patient who will be confined to bed for an extended period, meticulous skin care can prevent distressing pressure ulcers.
Rehabilitative care may be appropriate for patients who can be restored to a higher level of functioning that provides them with more control
|
BOX 3.6 Practical Dimensions of Care for Patients and Families
|
||||||||||||||||||||||||||||||||||||
and reduces burdens on caregivers. Although there may be no prospect of cure or long-term survival, some therapeutic interventions may allow a patient to live meaningfully for a somewhat longer time. This time may be just a few weeks or months, but such extra time can be precious, for example, to those anticipating a family wedding or birth.
As curative trials fail or symptoms intensify, the emphasis on comfort care becomes more important. At this stage, use of antibiotics and other care intended to prolong meaningful life may continue, or they may be foregone in favor of care that comforts but does not seek to prolong dying. Concern about a patient's quality of life while dying is central and not to be lost in preoccupation with technical assessments and tasks.
Good patient management is generally aided by clarity about the goals of care. If the goal is life extension, then symptom treatment may be subordinated to survival, and substantially burdensome interventions may be appropriate, because they are consistent with the patient's wishes. If the goal is a good death, then symptom management is pursued vigorously even if that pursuit has the unintended, though foreseeable, consequence of compromising survival; burdensome diagnostic and therapeutic interventions aimed at the illness are rarely appropriate in this context.
Table 3.3 shows one way of envisioning shifting emphases of care as they might relate to patient and family goals, disease stage, attitudes, preferences, interventions, effects, and other elements. Time in the different categories may vary enormously. In particular, many medical problems are not curable, and those who experience them may spend much of their life supported by life-prolonging or symptomatic care or both. Some of these people will, in fact, die of other problems; and, if death is not sudden, the care for those problems may be superimposed on the longer-standing condition.
For situations in which the categorizations in Table 3.3 fit well, many clinicians find them helpful because concepts and terms help organize and regularize care plans. The labels serve as a shorthand for communicating a coherent plan of care.
Nevertheless, Table 3.3's clear-cut categorization of strategies may not work well for a broad range of complicated situations. In particular, it is reasonable to think that people, even when very ill, may want to pursue multiple goals: maintaining a positive self-image, continuing a social role (e.g., as a virtuous family member), limiting impoverishment, avoiding physical suffering, prolonging life, and retaining control. Also, for many patients, various overall courses of care are possible. The potential effects of each possible plan of care on achieving each goal are different and uncertain. In such situations, which might be quite common, shorthand labels for plans and goals (e.g., a goal of life extension versus a good death) would poorly reflect reality. Instead, trade-offs among goals are central and
TABLE 3.3 Primary Emphases of Care for Those with Different Goals Related to Life-Threatening Illness or Injury
|
|
Primary Care Goal |
||
|
Aspects of Care |
Curative |
Life-prolonging, palliative |
Symptomatic, palliative |
|
Impact on disease |
Eradicate |
Arrest progression |
Avoid complications |
|
Acceptable side effects |
Major |
Major-moderate |
Minor-none |
|
Psychological attitude |
"Win" |
"Fight" |
"Accept" |
|
Preference for CPR |
Yes |
Probably |
Probably not |
|
Hospice candidate |
No |
No |
Probably |
|
Symptom prevention/ relief |
Secondary |
Balanced |
Primary |
|
Support for family |
Yes |
Yes |
Yes |
|
Advance care planning |
Yes |
Yes |
Yes |
|
Bereavement support |
Not usually |
Sometimes |
Usually |
|
SOURCE: Adapted from Baines, Gendron, et al., 1996. |
|||
reflect a gradual evolution of understanding about what can actually be achieved in light of responses to time and treatments.
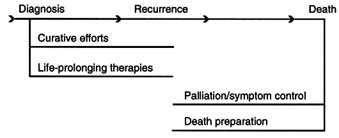
New Models of Care at the End of Life: Mixed Management
Although health care and public language have been comfortable with a "transition from cure to care" concept, the committee concluded that this traditional conceptualization does not capture or support the reality of simultaneously pursuing a broad array of desired ends. Figure 3.1 (A) represents this traditional view of patient management in a typical trajectory of cancer death. It shows that early in the course, curative efforts and life-prolonging therapies are offered, and then at some point, the futility of these therapies is recognized. The objectives of care switch to palliation of symptoms during the remaining months of life.
Although Figure 3.1 (A) seems a rational model, it may limit the acceptance of new ideas about the benefits of various therapies for those who are dying. Further, it is not enough to emphasize control of symptoms once
they are well established. If identified and impeccably managed earlier in the trajectory of illness, many of the symptom problems that afflict dying patients could be either eliminated or more readily managed.
For example, the body does not usually accommodate physiologically to chronic pain (Meyer et al., 1994; Woolf and Doubell, 1994). Indeed, unrelieved painful stimuli may alter the neurotransmission of pain in the central nervous system, with consequent hypersensitization and the development of an enhanced pain state, now more difficult to manage (Coderre et al., 1993). Recent studies show that early intervention may actually prevent pain from occurring in certain forms of advanced cancer (Hortobagyi et al., 1996; Paterson et al., 1996). The use of prophylactic bisphosphonate to prevent adverse skeletal events in patients with multiple myeloma and breast cancer provides a tangible example of the concept of prevention as part of palliative care. Psychosocial problems, confusional states, and, possibly, the cachexia-anorexia-asthenia syndrome are other problems that can be more successfully managed if a preventive model of care is adopted.
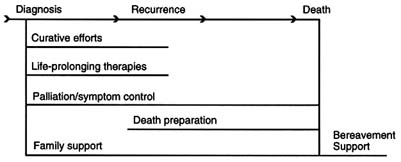
One way of graphically reflecting the adoption of this principle is shown in Figure 3.1 (B). Although an improvement upon Figure 3.1 (A), this model continues to clearly separate palliative from curative or life-prolonging therapies. It suggests that the two are mutually exclusive and that there are no therapies that can sometimes prolong life, sometimes palliate, and sometimes do both. Adoption of this model would continue to result in the neglect of therapies that are normally viewed as curative or life-prolonging but that also may be used to prevent or relieve symptoms.
Consider, for example, the current realistic aims of therapy for metastatic non-small-cell carcinoma of the lung and carcinoma of the pancreas with chemotherapy. Recent clinical trials show only modest or very modest evidence that such therapy prolongs life (Non-small Lung Cancer Collaborative Group, 1995; Chlebowski et al., 1996; Moore et al., 1996). These trials, however, do document major benefits to patients in terms of relief of pain, easing of shortness of breath, improvements in nutrition, and the maintenance of better functional status. In this case, the use of chemotherapy should be regarded as effective palliative therapy.
As in other areas of medical care, early recognition and treatment of a problem and use of preventive measures when problems may reasonably be predicted can limit the ultimate severity of pain and other symptoms. This implies the need to clearly identify and reassess the goals of treatment throughout a course of illness.
For many patients at the end of life, mixed management is the appropriate conceptual model of care. It allows ongoing efforts to extend life while still preparing for death and comforting the patient and family. For example, a patient with severe chronic obstructive pulmonary disease might
A. Traditional Model for Cancer Care
B. Revised Model for Cancer Care
C. Mixed Management of Various Eventually Fatal Illnesses
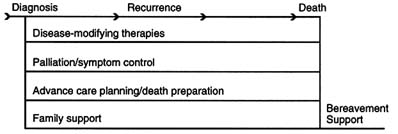
FIGURE 3.1 Alternative models of end-of-life care.
reasonably want a trial on a ventilator and also the opportunity to say farewell in case the trial failed and the ventilator was to be withdrawn.
Figure 3.1 (C) reflects the reality and ideal of end-of-life care in which therapies are not rigidly divided into preventive, curative, rehabilitative, palliative, and other categories but are creatively considered for their potential benefit (or burden) regardless of a patient's prognosis. This is consistent with Table 3.3, which distinguished curative, palliative, and other primary goals of care rather than categorizing therapeutic approaches that may, in
fact, serve different goals for different patients. It is also consistent with Chapter 1's definition of palliative care as involving the prevention and relief of suffering through early identification and impeccable assessment and treatment of symptoms, both physical and psychological.
Mixed management near death may be commonplace in the care of the frail elderly but does not seem to be as frequently articulated or practiced with those facing the end of life with chronic organ system failure or cancer. It seems likely that attending to "ongoing negotiation" rather than one dominant goal of care might well merit development for these patients.
This need is underscored by the fact that prognosis for many courses to death are ambiguous, even very near to death. In one study of severe congestive heart failure, half of patients who died were—on the day before they died—assigned prognoses of a greater than 50-50 change to live two months (Lynn et al., 1996). Rather than counsel patients about a likely imminent downward trajectory, the team should ensure that the patient understands the limits of what medicine can do to prolong life and that all attempts will be made to palliate and prevent suffering. Clinicians need to engage patients and families in realistic discussions about the risks of death and provide them full opportunity to ask questions and make plans. Because people will vary in what they want to know and decide, clinicians need to be especially sensitive to patient cues about their desires.
Conclusion
Care at the end of life has both a specific focus on those approaching death and a very expansive interest in the patient's family and friends; the health care team; and, ideally, the larger, caring community that tends to its members in both health and sickness. This caring community most immediately includes neighbors, co-workers, employers, and members of religious and voluntary service organizations, but it also extends to those in government and communications whose policies or images may nourish the caring spirit or subvert it.
Major objectives of end-of-life care are to prevent and relieve pain and other distressing symptoms while respecting patient preferences and dignity and offering concern and reassurance to patients and those close to them. Care at the end of life attends to physical, emotional, spiritual, and practical dimensions of the experience of life-threatening illness. It involves a continuing process of assessing and reassessing needs and the therapies and other assistance intended to help patients live well while dying.
The experience of dying is significantly determined by systems of care. They can powerfully support care along all its dimensions or they can put formidable obstacles in the way of good care at the end of life. The next chapter explores the structures of health care that shape how people die.





































