12
Health Reform in Russia and Central Asia
Jeni Klugman and George Schieber with Timothy Heleniak and Vivian Hon
INTRODUCTION
The impressive achievements in health status that set the former Soviet Union apart from its neighbors of comparable income are under pressure. Stresses at the individual and household levels associated with the collapse of the inherited economic system have been compounded by sharply reduced funding for health services.
Improvements in health status in Russia and Central Asia will depend on a number of factors. Income growth and its distribution are probably the most important determinants in the long run. Maintaining educational achievements, especially of women, is also important. Health programs will play a critical role, in particular through the development of cost-effective interventions, health promotion, and improvements in water and sanitation.
The findings, interpretations, and conclusions expressed herein are entirely those of the authors and should not be attributed in any manner to the World Bank, its affiliated organizations, or members of its Board of Executive Directors or the countries they represent. An earlier version restricted to Central Asia was presented at a World Bank/EDI Senior Policy Seminar held in Ashgabad, Turkmenistan, in June 1996, and was revised in light of comments from national participants. The analysis of Central Asia draws on contributions of Peter Cowley (ABT Associates) on epidemiological analysis and Jack Langenbrunner, Michael Borowitz, and Sheila O'Dougherty (ABT Associates) on the experience of financing reform. It also benefited from the advice and cooperation of colleagues, in particular Robert Anderson, Richard Feachem, Lev Freinkman, Victor Gabor, Billy Jack, Rita Klees, Robert Liebenthal, Costas Michalopoulos, Helga Muller, Bernard Funck, Barbara Ossowicka, Maria Vannari, Gero Verheyen, and an anonymous reviewer. Annie Minofu provided excellent production assistance.
This paper surveys health-care reform in Russia and Central Asia in the context of the socioeconomic, epidemiological, and institutional realities facing these countries. Following this introduction, the next section examines demographic and epidemiological trends in the region. The third section evaluates current health systems, highlighting their primary strengths and weaknesses. The reform agenda facing health policymakers is investigated in the fourth section. The final section contains concluding observations.
The goals of health-sector reform can be stated in fairly noncontroversial terms: to improve the health status of the population, ensure equity and access, improve efficiency, improve clinical effectiveness, and ensure quality and consumer satisfaction. Reaching those goals, however, is a far less tractable task. This paper attempts to provide an empirical as well as conceptual overview of these issues. While there are important distinctions among the countries, some generalizations are possible. Indeed, the problems of financing and delivering health services in an efficient and equitable way present a difficult challenge for all countries, rich and poor.
It should be noted that macroeconomic performance is a critical element in the analysis of health outcomes and policy reform. The average level of national income per capita is clearly important. Increased income allows individuals and households to buy better living and housing conditions and more health care. Similarly, economic growth expands government revenue possibilities, and thus the opportunities to provide preventive and curative health services, safe water and sanitation systems, better-quality and safer food, and education, for example. Because rising average incomes tend to reduce poverty, there is generally a strong link between incomes and health status. World Bank analysis suggests that more than 75 percent of the difference in child mortality across countries is associated with income differences, and that the relation is causal rather than merely associative: in a sample of 58 developing countries, a 10 percent increase in income per capita, all else being equal, reduced infant and child mortality rates by between 2.0 and 3.5 percent (World Bank, 1993c).
HEALTH STATUS: DEMOGRAPHIC AND EPIDEMIOLOGICAL TRENDS
People living in Russia and Central Asia enjoy relatively good human development outcomes, especially relative to income levels. High rates of literacy, coupled with relatively high life expectancy, mean that the United Nations' human development ranking of each country at independence was higher than if it had been based on income alone, especially for the poorer countries (Klugman and Schieber, 1996:Table 1). This section explores the demographic and epidemiological trends underlying health status in Russia and Central Asia, focusing on the period since 1991.
Demographic Trends
Recent demographic trends provide a useful basis from which to evaluate the performance of the health systems and needed reforms in Central Asia and Russia. In summary, the population of Central Asia is young, and likely to become younger in some countries. Even though fertility rates have recently declined, population growth remains high. In contrast, the Russian population is aging and has experienced an extraordinary drop in both crude birth rate and fertility, while significant return migration has had an even larger absolute impact on the population. Since 1989, mortality rates have tended to increase, and life expectancy has declined dramatically throughout the region (Klugman and Schieber, 1996). Most of Central Asia experienced significant population increases between 1989 and 1995, while all the Central Asian countries except Turkmenistan had a combination of high natural increase with outmigration.
It is clear, however, that these developments in Central Asia and Russia represent a rapid acceleration of trends that have been evident for several decades. Birth rates have been declining slowly since the 1960s. The flow of Russians and other nationalities into Central Asia began to reverse direction in the mid-1970s. Stagnation and then declines in life expectancy in Russia began in 1965.
Fertility, as measured by either the crude birth rate or the total fertility rate, has generally declined since 1989 (see Table 12-1). Total fertility rates in Central Asia are nonetheless still high relative to Russia (1.4) and Organization for Economic Cooperation and Development (OECD) countries (averaging 1.9). In 2015, Tajikistan, Turkmenistan, and Uzbekistan are still expected to have roughly the same skewed age structures they have today, with more than 40 percent of their populations below age 16 and less than one in ten people above working age.
The outmigration of Russians and other Slavic and European nationalities from Central Asia has had, and will continue to have, an enormous impact on the demographics of the region. The Russian population is older and more urbanized, with birth rates between one-third and one-half those of the titular nationalities and higher death rates, resulting in much lower rates of natural increase. This trend of differential natural growth rates is long-standing, but has become even more marked in recent years. In terms of nationality composition, the Central Asian countries can be classified into two groups: Kazakstan and Kyrgyz Republic with their much larger Russian populations (38 and 22 percent, respectively, in 1989) on the one hand, and the remaining three countries, each less than 10 percent Russian, on the other. Outmigration has played a much more important role in the former group. In Russia, with an overall positive inflow of people from other parts of the former Soviet Union, internal migration and the direction of flows of return migrants have affected the regional distribution of the population; in particular, there have been signifi-
TABLE 12-1 Selected Demographic and Health Characteristics of Russia and the Central Asian States, 1989-1994
|
Country |
Crude Birth Rate (per 1,000) |
Crude Death Rate (per 1,000) |
Rate of Natural Increase (per 1,000) |
Total Fertility Ratea |
Infant Mortality Rate (per 1,000 births) |
Maternal Mortality Rate (per 100,000 live births)b |
Life Expectancy (years)c |
|
1989 |
|||||||
|
Russia |
14.7 |
10.7 |
3.9 |
2.0 |
17.8 |
47.4 |
69.6 |
|
Kazakstan |
23.0 |
7.6 |
15.4 |
2.9 |
26.0 |
53.1 |
68.7 |
|
Kyrgyz Republic |
30.4 |
7.2 |
23.2 |
3.9 |
32.4 |
42.6 |
68.5 |
|
Tajikistan |
38.7 |
6.5 |
32.2 |
5.2 |
43.3 |
38.9 |
69.4 |
|
Turkmenistan |
35.0 |
7.7 |
27.3 |
4.4 |
54.8 |
55.2 |
65.2 |
|
Uzbekistan |
33.3 |
6.3 |
27.0 |
4.2 |
38.1 |
42.8 |
69.2 |
|
1994b |
|||||||
|
Russia |
9.4 |
15.6 |
−6.2 |
1.4 |
18.6 |
51.6 |
64 |
|
Kazakstan |
18.2 |
9.6 |
8.6 |
2.3 |
27.4 |
49.6 |
65.8 |
|
Kyrgyz Republic |
24.6 |
8.3 |
16.3 |
3.3 |
29.6 |
44.5 |
65.4 |
|
Tajikistan |
28.2 |
7.0 |
21.2 |
4.3 |
45.9 |
74.0 |
67.7 |
|
Turkmenistan |
32.0 |
7.9 |
24.1 |
4.0 |
42.9 |
44.4 |
63.9 |
|
Uzbekistan |
29.4 |
6.6 |
22.8 |
3.8 |
32.7 |
24.1 |
67.9 |
|
Percent change, 1989-1994 |
|||||||
|
Russia |
−35.4 |
44.4 |
−259 |
−30.0 |
2.8 |
6.7 |
|
|
Kazakstan |
−20.9 |
26.3 |
−44.2 |
−20.1 |
5.4 |
−6.6 |
−4.2 |
|
Kyrgyz Republic |
−19.1 |
15.3 |
−29.7 |
−15.6 |
−8.6 |
4.5 |
−4.5 |
|
Tajikistan |
−27.1 |
7.7 |
−34.2 |
−17.7 |
6.0 |
90.2 |
−2.4 |
|
Turkmenistan |
−8.6 |
2.6 |
−11.7 |
−9.1 |
−21.7 |
−19.6 |
−1.8 |
|
Uzbekistan |
−11.7 |
4.8 |
−15.6 |
−9.1 |
−14.2 |
−43.5 |
−2.0 |
|
a The total fertility rate (TFR) is a synthetic measure of the number of children a woman would have if she passed through her childbearing years at the current age-specific fertility rates. Figures are for 1993. b Figures for total fertility rate and maternal mortality rate are for 1993; figures for life expectancy are for 1994 except Tajikstan (1992) and Uzbekistan (1993). c Figures are for 1994, except Tajikistan (1992) and Uzbekistan (1993). SOURCES: Commonwealth of Independent States Statistical Committee, national statistical offices; World Health Organization Health-for-All Global Indicators Data Base. |
|||||||
cant net reductions in the numbers of people living in outlying regions of the North, East Siberia, and the Far East (Klugman and Schieber, 1996).
Crude death rates have increased in each country, most dramatically in Russia, Kazakstan, and the Kyrgyz Republic. The crude death rate in Russia now significantly exceeds that in Central Asia. Life expectancies have declined in all the countries since 1989, most seriously in Russia.1 The male-
female life expectancy gap has widened in all the countries except Turkmenistan, but again most dramatically in Russia. The infant mortality rate has worsened in Russia, Kazakstan, and Tajikistan, but improved elsewhere.
Age-specific mortality trends reveal distinct patterns. In Central Asia, those with the largest increases in death rates have tended to be younger, aged 10-30. In Russia, the largest increases in mortality during the transition period have been among those aged 35-44, especially males. External causes explain the largest portion of rising death rates for both men and women, and may be linked to the stress and uncertainty associated with the transition (Nell and Stewart, 1994). Moreover, while age-adjusted mortality rates from cardiovascular disease have tended to decline in Western Europe (by 35 to 50 percent between 1960 and 1985), they have risen dramatically in the Soviet Union over the past three decades (Chernichovsky et al., 1996; Klugman and Schieber, 1996:Table 4; Murray and Bobadilla, 1994; Shkolnikov et al., 1994).
Epidemiological Situation
The epidemiological situation of a population is a clear indicator of its health needs and demands. International historical experience suggests that changes in the pattern of disease among a population proceed in two steps: the first is the demographic transition, when mortality from infectious diseases declines, and, partly as a result, fertility decreases as well; the second is the epidemiological transition, when the population becomes older, and noninfectious diseases become the main causes of mortality (World Bank, 1993).
Russia appears largely to have passed through the demographic transition, although reports of infectious disease outbreaks have been fairly frequent in recent years. In Central Asia, however, pre-epidemiological transition conditions, such as a high prevalence of infectious diseases and high infant mortality, coexist alongside health problems such as ischemic heart disease, emphysema, and motor traffic accidents, which are typical in richer industrial countries (Phillips et al., 1992). Moreover, some previously eradicated disorders have seen a resurgence. In some Central Asian countries, such as Turkmenistan and Tajikistan, classic pre-demographic transitional disorders such as acute respiratory infections and diarrheal diseases cause high infant mortality, indicating that they have never been completely controlled in these areas. High mortality (and morbidity) from other disorders surrounding childbirth continue. Russia's infant mortality rate is significantly lower than the rates in Central Asia.
Maternal mortality rates were high in all the countries prior to independence; since then, experiences have diverged (Table 12-1). Maternal mortality rates in Uzbekistan are now reported to be only about half the regional average as a result of declines in fertility and infant mortality rates of 9 and 14 percent, respectively. A comprehensive program aimed at women of child-
bearing age was launched in 1991, including special preventive and treatment centers and the promotion of birth spacing, although these initiatives may be too recent to have had such striking results.
Infectious diseases have generally not been important in determining the health of the general population, with the possible exceptions of tuberculosis and diphtheria. While the incidence of tuberculosis may be underreported, the official incidence of diphtheria has risen sharply across the region. In the Kyrgyz Republic and Tajikistan, the rates rose in both countries from about 0.2 per 100,000 in 1990 to 6.8 and 33.4, respectively, in 1994. Rates in Russia rose from 0.8 to 27 over the same period. Available evidence suggests that the rates of sexually transmitted diseases (STDs) have also risen rapidly—in Russia, from 32.2 cases per 100,000 in 1990 to 127.3 in 1994—even though rates are still likely to be underreported. Very few AIDS cases, fewer than 100, have been reported in the entire region.
THE INHERITED HEALTH SYSTEMS
This section describes and evaluates the basic health systems of Russia and Central Asia in terms of expenditures and the availability and use of services. The systems are discussed in the context of the goals of health system reform: improving health status, ensuring access and equity, achieving microeconomic and macroeconomic efficiency, improving clinical effectiveness, and ensuring quality and consumer satisfaction.
The systems in Russia and Central Asia are based on the centrally planned national health service model of the former Soviet Union. The characteristics of this system were, and largely remain, as follows:
-
Eligibility—The entire population is eligible for services.
-
Benefits—The state provides all necessary health services at no charge.
-
Financing—The public system is financed from the general state budget (e.g., national general revenues), enterprise budgets, and extrabudgetary funds. Private payments in the past were limited to a few nonessential services and some unofficial payments to public providers for preferential treatment.
-
Payment of Medical Care Providers—Virtually all facilities were owned by the state, and all health-care personnel were state employees. Polyclinics and hospitals were reimbursed on the basis of 18 category line item budgets. Physicians and other health personnel were salaried employees. Provision and financing were combined (the public financing authority owned, budgeted, and managed facilities).
-
Service Delivery System—The system was conceptually a well-integrated hierarchical structure of feldsher stations; health posts; polyclinics; and local-, regional-, and national-level hospitals. The human and physical capital
-
infrastructure of the system was based on planning norms used to allocate facilities and personnel across geographic areas. Quality of care was enforced through a hierarchical review process based on reprimanding inappropriate behavior. Public health programs were targeted to maternal and child health and communicable diseases.
While there were significant differences across the countries of the former Soviet Union, these centrally planned systems generally performed well prior to the breakup in terms of equity, access, and the achievement of relatively good overall health outcomes for the amounts spent.2 On the other hand, the systems tended to be underfunded by Western standards (as social sectors were given low priority in the planning process), were inefficient, provided low-quality care, allowed little consumer choice, and were prone to informal payments for preferential treatment. Moreover, the systems were unable to cope with the epidemiological transition (Chernichovsky et al., 1996; Field, 1995; Knaus, 1981).
The disruptions associated with the breakup of the Soviet Union exacerbated these problems (Table 12-2). As a result, there is a broad range of problems in the health-care financing and delivery systems in all these countries:
-
Declining health status of the population due to environmental risk factors and socioeconomic trends that have drastically increased mortality from heart disease, violence, injuries, and suicides
-
Poorly structured or nonexistent public health programs for health promotion, disease prevention, family planning, adult health, occupational health, and environmental health
-
Chronic underfunding (as an ''unproductive" service sector) relative to the systems in Western countries, with low wages for physicians, nurses, and other health-care workers
-
A rigid 18-category budgeting system for paying polyclinics, physicians, and hospitals, which provides few incentives for economic efficiency and tends to encourage inpatient over outpatient treatment, as well as care at the highest, most expensive levels of the system
-
Too many physicians, too many specialists, and a lack of professionalism among physicians resulting from the state-enforced breakup of professional associations
-
Poorly trained primary-care physicians, limited inpatient and outpatient diagnostic capacity, too many hospital beds, excessive utilization of services (particularly inpatient care), and the obsolete and poor condition of the capital stock
TABLE 12-2 Key Macroeconomic Indicators During the Transition
|
Country |
1995 GDP as a Percent of GDP 1990a |
Average Inflation (percent) |
Registered Unemploymentb |
Real Wage 1995 as a percent of Real Wage 1990 (1990 = 100) |
||
|
|
|
1993 |
1995 |
1994 |
1995 |
|
|
Kazakstan |
46 |
1,660 |
180 |
1.0 |
2.1 |
27 |
|
Kyrgyz Rep. |
50 |
1,210 |
50 |
0.6 |
3.0 |
20 |
|
Russia |
62 |
895 |
189.2 |
6.1 |
7.8 |
35 |
|
Tajikistan |
47 |
2,140 |
400 |
— |
1.8 |
4 |
|
Turkmenistan |
58 |
1,630 |
1,005 |
— |
— |
29c |
|
Uzbekistan |
82 |
1,230 |
320 |
0.7 |
0.3 |
52 |
|
a GDP = gross domestic product; figures for Tajikistan and Turkmenistan refer to net material product. b Registered unemployment, except for Russia, the figures for which are based on the (broader) International Labor Organization definition. c 1994 real wage. SOURCE: Goskomstat SSSR. |
||||||
-
Outdated treatment norms that promote ineffective medical practice, inefficient facility configurations, and staffing norms that restrict facility managers from making rational staffing decisions
-
A lack of modern quality assurance systems
-
Inefficient and outmoded production, procurement, distribution, and management systems for pharmaceuticals; outmoded lists of essential drugs; and coverage/reimbursement policies that encourage individuals to be hospitalized to receive free drugs
-
Little or no consumer choice
-
No accountability on the part of consumers or medical care providers for the consequences of their decisions
-
Confusion about roles and responsibilities at the national level as responsibility for financing and delivering health care has been decentralized
-
Hospitalization used as a safety net to compensate for inadequate referral systems, poor transportation and housing, the high costs of food and pharmaceuticals, and the health sector's generally being relied on by governments as an employment maintenance mechanism
These problems are fundamental and affect almost every aspect of health care at all levels. Nonetheless, the system retains substantial elements of success. These include an extensive and well-integrated hierarchical system of feldshers, health stations, polyclinics, and local, regional, and national hospitals; access to care for all as a right—and the associated equitable distribu-
tion of health resources in terms of household income and location; and, at least until recently, relatively good health outcomes for the limited moneys spent.
Expenditures and Availability and Use of Services
Available evidence on financial indicators and the availability and use of services in Russia and Central Asia reveal certain differences among the countries. However, both the levels and trends over time for most measures are markedly similar.
Expenditures
Table 12-3 and Figures 12-1 and 12-2 provide information on health expenditures measured in a variety of ways for 1990-1994: as a share of gross domestic product (GDP), on a real per capita basis, and per capita in U.S. dollars. Unfortunately, because of a lack of information on private spending, only public spending on health is presented. Even these figures may not be strictly comparable, since countries may spend different amounts through enterprises and extrabudgetary funds that may not be captured. Furthermore, one must be cautious in interpreting health expenditure-to-GDP ratios, as there are serious GDP valuation issues concerning whether certain commodities (e.g., oil and gas) are valued at local or world market prices. Similar problems occur in developing real health expenditure trends, which are extremely sensitive to the price deflators chosen. In Russia, and probably Central Asia as well, the GDP deflator probably significantly understates health-sector inflation resulting from price liberalization and elimination of import subsidies for pharmaceuticals. Thus, the reported levels of expenditure are overstated, perhaps significantly (King and Proskuryakova, 1996).
In all the countries except Russia and Tajikistan, the (public) health expenditure-to-GDP ratio (the percentage of national income going into the health sector) has declined since 1990, prior to the breakup of the Soviet Union (Figure 12-1). Although the health expenditure-to-GDP ratio is the most commonly used measure of expenditure performance, one must also analyze real per capita health spending to get a complete picture. For comparisons of the absolute levels of spending across countries, spending must be converted into one numeraire currency, as in Table 12-3.
The health sector appears to have been somewhat protected, at least in terms of its share of a declining economy, in Russia, Tajikistan, and Uzbekistan. The elasticities of health spending relative to GDP (that is, the annual percentage change in health spending relative to the annual percentage change in GDP) for all six countries are clustered between 0.87 and 1.07. An elasticity of 0.87 means that a 10 percent change in GDP was accompanied by
TABLE 12-3 Public Health Expenditures, 1990-1994
|
Country and Indicator |
1990 |
1991 |
1992 |
1993 |
1994 |
|
Russia |
|||||
|
Health Expenditure-to-GDP Ratio |
2.5 |
2.4 |
2.5 |
3.3 |
4.1 |
|
Real per Capita Health Spending as % of 1990 |
100 |
92 |
81 |
99 |
107 |
|
Per Capita Health Spending ($US [PPPsa]) |
206 |
198 |
134 |
166 |
183 |
|
Kazakstan |
|||||
|
Health Expenditure to GDP Ratio |
3.3 |
4.2 |
2.1 |
2.5 |
2.0 |
|
Real per Capita Health Spending as % of 1990 |
100 |
118 |
54 |
56 |
37 |
|
Per Capita Health Spending ($US [PPPs]) |
183 |
203 |
86 |
86 |
56 |
|
Kyrgyz Republic |
|||||
|
Health Expenditure to GDP Ratio |
4.1 |
3.6 |
3.2 |
2.6 |
3.2 |
|
Real per Capita Health Spending as % of 1990 |
100 |
77 |
57 |
39 |
36 |
|
Per Capita Health Spending ($US [PPPs]) |
136 |
124 |
83 |
56 |
62 |
|
Tajikistan |
|||||
|
Health Expenditure to GDP Ratio |
4.8 |
4.5 |
5.2 |
5.4 |
6.4 |
|
Real per Capita Health Spending as % of 1990 |
100 |
84 |
75 |
51 |
46 |
|
Per Capita Health Spending ($US [PPPs]) |
117 |
101 |
87 |
63 |
60 |
|
Turkmenistan |
|||||
|
Health Expenditure to GDP Ratio |
3.7 |
3.7 |
2.0 |
1.8 |
1.2b |
|
Real per Capita Health Spending as % of 1990 |
100 |
92 |
47 |
34 |
17 |
|
Per Capita Health Spending ($US [PPPs]) |
— |
— |
— |
— |
— |
|
Uzbekistan |
|||||
|
Health Expenditure to GDP Ratio |
4.6 |
4.6 |
4.7 |
4.1 |
4.0 |
|
Real per Capita Health Spending as % of 1990 |
100 |
96 |
87 |
72 |
66 |
|
Per Capita Health Spending ($US [PPPs]) |
131 |
135 |
124 |
103 |
95 |
|
NOTE: Health expenditures are deflated by the GDP deflator. a ppp = Purchasing Power Parity. b If Turkmenistan's reported GDP is not adjusted for world market prices for its exports, the 1994 health expenditure to GDP ratio is 2.7. Such adjustments have little or no effect in the preceding years. SOURCE: Klugman and Schieber (1996) and World Bank data. |
|||||
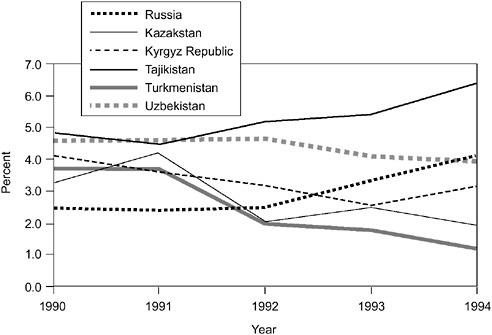
FIGURE 12-1 Public health expenditures as percentage of GDP, 1990-1994.
SOURCE: Adapted from Klugman and Schlieber (1966:18).
an 8.7 percent change in health spending.3 In other words, in countries with elasticities below 1.0, health expenditures increased less rapidly than GDP (which, in inflation-adjusted terms, declined significantly in all countries, as shown in Table 12-2).
Real GDP has fallen substantially throughout the region since 1990 (Table 12-2), in several countries by 50 percent or more. Reductions in real health spending have largely paralleled these trends. Real public health spending in 1994 also fell throughout the region, by half or more in all the countries except Russia and Uzbekistan. Given the large increases in population in Central Asia, real per capita health spending suffered even larger declines over the period 1990-1994. In 1994, it was just 17 percent of the 1990 level in Turkmenistan and 66 percent in Uzbekistan (Figure 12-2). General declines of these magnitudes have led to a serious deterioration of the health infrastructure. With the attendant general declines in income and socioeconomic conditions, these trends are contributing to the increased morbidity and mortality and worsening health status of the population.
There is little information on private-sector spending. Survey data from Russia indicate that, although private health expenditures average less than 2
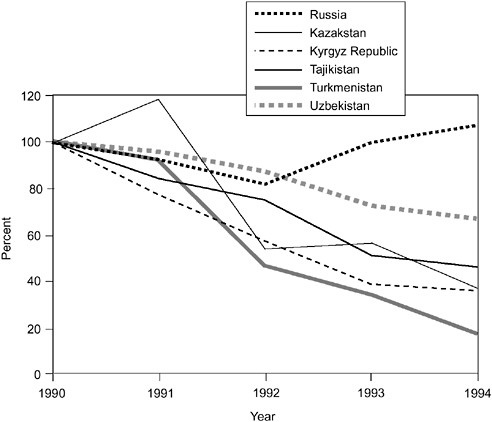
FIGURE 12-2 Real per capita public health expenditures, 1990-1994 (with 1990 set at 100 percent). SOURCE: Adapted from Klugman and Schlieber (1966:20).
percent of all household expenditures, they are higher for the poor than for the nonpoor, and the poor tend to use preventive services less often. About 28 percent of those unable to obtain prescribed medications cited insufficient money as the cause (Klugman, 1996; Zahoori et al., 1996). However, other survey data from the Kyrgyz Republic and Kazakstan indicate that out-of-pocket payments by individuals for pharmaceuticals, as well as for many normally publicly covered inpatient services, are quite high. Household survey evidence from the Kyrgyz Republic shows that between 1993 and 1994, formal charging for medical consultations increased significantly, from 11 to 25 percent of the population. Informal payments to medical staff are also widespread and likely to be increasing-reported by about one in four inpatients. By far the most significant item of private medical expenditure is drugs (Abel-Smith and Falkingham, 1996; Klugman and Schieber, 1996). An October 1994 survey in a South Kazakstan oblast found that over 35 percent of users of pharmaceuticals and hospital services were making large out-of-pocket payments for these services (Langenbrunner et al., 1996).
One legacy of the Soviet period was the widespread ownership, provision, and/or financing of social services by enterprises and collective farms, which extended to health facilities. Russia's Ministry of Economy estimates that enterprises owned and maintained 8 percent of all outpatient clinics and 6 percent of all hospitals in the country overall, though the shares were much higher in certain regions (Mikhailev, 1996). Evidence suggests that the enterprise facilities are of significantly higher quality than those of government authorities (World Bank, 1997). The transition has led many enterprises to close or divest social facilities, although not without problems. Uzbekistan is an outlier in that the Ministry of Health, up to 1996, was explicitly encouraging greater employer provision of health care. As these enterprises are increasingly privatized and state subsidies are withdrawn, any health services they continue to provide should be regarded as private, not public, health expenditures.
In absolute U.S. dollar terms, using purchasing power parities to convert (i.e., a special exchange rate that takes into account cost-of-living differences across countries), per capita health spending ranges from $56 in Kazakstan to $183 in Russia. This compares with health expenditures of $149 in Egypt, $185 in Turkey, and $374 in Jordan, for example (World Bank, 1997). Spending is well below the 8.1 percent health expenditure-to-GDP ratio and $1500 per capita expenditures for OECD countries (of which 75 percent is public) (Schieber et al., 1994). Perhaps more pertinent is whether these countries can maintain the vast health infrastructures that were developed when more budget resources were available.
Availability and Use of Services
As shown in Table 12-4, Russia and Central Asia (like all countries of the former Soviet Union) are characterized by large quantities of inputs and high rates of hospital use. Central planning norms led to large numbers of hospital beds and physicians, while the system for paying hospitals provided strong incentives to keep beds filled. Poorly paid health personnel at the lower levels of the system, often lacking appropriate equipment, supplies, and medications, had incentives simply to refer individuals up the system rather than treat them. Since higher levels had better physicians, equipment, and supplies, individuals also had incentives to bypass lower levels of the system.
All these factors are reflected in the basic statistical profiles of the delivery systems in Russia and Central Asia. In terms of physicians, in 1994 the physician/population ratios varied from 2.1 physicians per 1000 population in Tajikistan to 3.8 in Russia, with a six-country average of 3.3. This compares with an OECD average of 2.5. Since 1990, these ratios have fallen slightly in all six countries except Uzbekistan. Nonetheless, the ratios throughout, except for that in Tajikistan, are still well above the OECD average.
TABLE 12-4 Availability and Use of Services, 1990-1994
|
Indicator |
1990 |
1991 |
1992 |
1993 |
1994 |
|
Russia |
|||||
|
Physicians per 1,000 population |
4.1 |
4.1 |
3.9 |
3.9 |
3.8 |
|
Hospital beds per 1,000 population |
13.1 |
12.7 |
12.2 |
12.1 |
11.9 |
|
Admission rate (% of population) |
22.8 |
21.8 |
21.0 |
21.6 |
21.6 |
|
Hospital days per capita |
3.8 |
3.6 |
3.6 |
3.6 |
3.6 |
|
Average length of stay (days) |
16.6 |
16.7 |
17.0 |
16.8 |
16.8 |
|
Occupancy rate (%) |
79 |
79 |
80 |
82 |
84 |
|
Kazakstan |
|||||
|
Physicians per 1,000 population |
4.0 |
3.8 |
3.9 |
3.8 |
3.6 |
|
Hospital beds per 1,000 population |
13.7 |
13.7 |
13.5 |
13.2 |
12.1 |
|
Admission rate (% of population) |
22.9 |
22.6 |
21.3 |
20.2 |
17.6 |
|
Hospital days per capita |
3.7 |
3.6 |
3.5 |
3.3 |
3.0 |
|
Average length of stay (days) |
16.0 |
16.0 |
16.3 |
16.3 |
16.8 |
|
Occupancy rate (%) |
79 |
79 |
78 |
76 |
74 |
|
Kyrgyz Republic |
|||||
|
Physicians per 1,000 population |
3.4 |
3.4 |
3.3 |
3.1 |
3.1 |
|
Hospital beds per 1,000 population |
12.0 |
12.1 |
11.9 |
10.7 |
9.6 |
|
Admission rate (% of population) |
23.0 |
22.5 |
21.7 |
19.9 |
17.0 |
|
Hospital days per capita |
3.4 |
3.4 |
3.3 |
3.0 |
2.6 |
|
Average length of stay (days) |
14.9 |
14.9 |
15.3 |
15.3 |
15.4 |
|
Occupancy rate (%) |
80 |
78 |
78 |
80 |
78 |
|
Tajikistan |
|||||
|
Physicians per 1,000 population |
2.6 |
2.4 |
2.3 |
2.2 |
2.1 |
|
Hospital beds per 1,000 population |
10.7 |
10.7 |
11.2 |
10.6 |
8.8 |
|
Admission rate (% of population) |
21.0 |
20.5 |
16.3 |
— |
— |
|
Hospital days per capita |
3.0 |
3.0 |
2.4 |
— |
— |
|
Average length of stay (days) |
14.3 |
14.6 |
14.5 |
— |
— |
|
Occupancy rate (%) |
94 |
88 |
— |
— |
— |
|
Turkmenistan |
|||||
|
Physicians per 1,000 population |
3.6 |
3.7 |
3.6 |
3.6 |
3.5 |
|
Hospital beds per 1,000 population |
11.5 |
11.6 |
11.4 |
11.7 |
11.5 |
|
Admission rate (% of population) |
19.8 |
19.4 |
18.4 |
18.4 |
16.6 |
|
Hospital days per capita |
3.1 |
2.9 |
2.7 |
2.7 |
2.5 |
|
Average length of stay (days) |
15.6 |
15.2 |
14.7 |
14.9 |
15.1 |
|
Occupancy rate (%) |
73 |
72 |
69 |
70 |
64 |
|
Uzbekistan |
|||||
|
Physicians per 1,000 population |
3.4 |
3.4 |
3.3 |
3.3 |
3.4 |
|
Hospital beds per 1,000 population |
12.5 |
10.9 |
10.8 |
9.4 |
8.8 |
|
Admission rate (% of population) |
24.6 |
24.5 |
23.6 |
22.0 |
19.3 |
|
Hospital days per capita |
3.6 |
3.6 |
3.5 |
3.2 |
2.8 |
|
Average length of stay (days) |
14.8 |
14.8 |
15.0 |
14.5 |
14.3 |
|
Occupancy rate (%) |
83 |
82 |
85 |
88 |
87 |
|
SOURCE: World Health Organization, Health-for-All Global Indicators Data Base; Church and Koutanev (1995). |
|||||
Available evidence reveals widespread reductions in the number of beds, hospital admission rates, and lengths of stay since 1990 (Table 12-4). Nonetheless, the levels remain high and exceed those in OECD countries, which have substantially larger elderly populations. Since 1990, the ratio of hospital beds to population has declined significantly in most of the countries, but the levels are still well above the OECD average (8.4 compared with the regional average of 10.5). Hospital admission rates (percentage of the population admitted to a hospital each year) average 18.1 percent in the region, and in all six countries remain above the OECD average of 16.2 percent. Since 1990, admission rates have declined in all six countries. Hospital occupancy rates average 79 percent in the six countries of the region, slightly above the OECD average. Since 1990, occupancy rates have declined in all the countries except Uzbekistan and Russia. The average length of a hospital stay varies from 14.3 days in Uzbekistan to 16.8 in Russia and Kazakstan, with a six-country average of 15.5 days. Given the young population structure in most of Central Asia, these lengths of stay are high as compared with the 14.4 day average in OECD countries. Average lengths of stay have increased in four of the six countries. The number of hospital days per person per year ranges from 2.4 in Tajikistan to 3.6 in Russia, with a six-country average of 2.8, which again exceeds the OECD average of 2.5. Since 1990, the number of bed days per capita has declined in all six countries.
The foregoing evaluation reveals striking health-sector trends. Public funding has been substantially reduced, yet the health infrastructure in terms of personnel and facilities remains extensive, inefficient, and not fully adjusted to reduced funding levels. Health outcomes, except in Russia, are still good relative to those of other countries with comparable incomes; overall, however, mortality rates have increased, life expectancy has declined, and certain infectious diseases appear to be on the rise. It is evident that basic public health programs and treatment norms are not well targeted to dealing with the population's underlying health needs, especially given sharply reduced funding. The reforms being initiated now, at different stages in all six countries, address these problems.
HEALTH POLICY REFORM AGENDA
Policymakers in each of the six countries of the region have developed a clear consensus on the need for a reorientation of spending priorities—toward more effective public and environmental health programs, an emphasis on primary care, less hospital-based tertiary care, and the provision of appropriate financial incentives. This section addresses the health reform agendas of the six countries and examines how these countries could implement such reforms, as well as the factors likely to influence their effectiveness.
All six countries have either initiated or are contemplating reforms to address the underlying financing and delivery problems facing their health systems.4 The generic policies being pursued by virtually all these countries are similar:
-
Obtain additional financing through nonbudgetary sources, such as earmarked payroll taxes on employers; voluntary insurance; and other private financing, including patient cost sharing.
-
Reduce pressure on the national budget by decentralizing the financing of health care to the regional and local levels.
-
Get better value for the money spent by separating financing from provision and having money follow patients.
-
Improve system efficiency by introducing incentive-based provider payment mechanisms.
-
Improve the service delivery system by restructuring it to favor primary care, promoting general and family medical practice, and eliminating unneeded hospital capacity.
-
Institute major reforms in pharmaceutical regulation, management, essential drug lists, procurement, management, distribution, and pricing.
Reforms in health-care financing have been implemented in Russia and several Central Asian countries and are being developed in others. The basic principles of the Russian reforms in terms of use of insurance funds and decentralization of financing and delivery are generally being emulated by the Central Asian countries. Russia passed health insurance legislation in 1991, which was modified before being implemented in late 1993. Since Russia has progressed the furthest to date, much of the following discussion pertains to the Russian experience.
The basic goal of Russia's health insurance legislation was to infuse new nonbudgetary revenues into the system and introduce efficiency by separating financing from provision (Chernichovsky et al., 1996; Sheiman, 1994). Ownership of most health-care facilities was turned over to oblast, municipal, and rayon governments. New revenues would be obtained through a 3.6 percent payroll tax on enterprises to pay for the health care of their workers. Local governments would make contributions for the nonworking population. Contributions from firms and local governments would go to Territorial Health Insurance Funds (THIFs) in each of the 89 oblasts (regions). These THIFs would enter into contracts with noncommercial insurance companies, which would contract with health-care providers. Consumers would choose their insurance companies. A small percentage of the payroll tax, 0.2 of the 3.6 percent, would go to the Federal Mandatory Health Insurance Fund (FMHIF),
which would use these funds for fiscal equalization in health spending and general administrative purposes.
The new system started functioning in late 1993, when payroll tax contributions began to flow to THIFs. THIFs first made payments to insurers, and to providers in those areas without insurance companies, in 1994. Implementation has proceeded unevenly throughout Russia's 89 oblasts and has been fraught with major problems—bureaucratic, financial, and operational—as well as fraud. With the decentralization of financing and delivery responsibility to each of the 89 oblasts (some 90 percent of all health financing is now being raised locally), the Russian Ministry of Health (MOH) has had little to do with implementing the new system. Some oblasts have not implemented the system at all; others have implemented it in only some rayons; many have implemented it without insurance companies since insurers did not exist and/ or did not find it profitable to enter the market.5 Major bureaucratic turf battles have occurred between the Oblast Health Authorities, which are reluctant to give up their control over the health system, and the THIFs. There have been allegations and investigations of fraudulent use of funds by some THIFs and their managers, and MOH has been attempting to gain control over the health insurance funds.
Given the vagueness of certain aspects of the enacted legislation, such as the benefit package and the contribution levels of local governments for the nonworking population, as well as the significant economic difficulties described above, the system in many oblasts faces severe financial problems. It would appear that rather than adding funds to the system through the payroll tax, local governments have simply reduced their previous levels of public financing for the health sector. Thus, it does not appear that the goal of infusing significant amounts of new funding through payroll tax contributions has succeeded.
On the other hand, THIFs are operating in most oblasts. Since the lack of funding has deterred insurance companies from entering the market, THIFs have often entered directly into incentive-based arrangements with health-care providers. In many cases, these arrangements may be superior in efficiency and productivity to the previous 18-category line item budgeting system. Thus, the system has to some degree succeeded in separating financing from provision and instilling incentive-based provider payment mechanisms. Yet given the availability and use patterns shown in Table 12-4, there does not appear to have been much change in health-sector performance. Moreover, the limited participation of insurance companies and the highly vertically integrated nature of the state-owned monopolistic service delivery system have resulted in
little additional consumer choice and competition among providers. In fact, placing insurance companies between the consumer and the THIF has often been criticized as adding an unnecessary layer that simply increases administrative costs.
With the Russian elections over and a renewed government interest in social policies, the partially implemented health insurance system is under close scrutiny, and major changes are being actively considered. These developments are being watched closely by the Central Asian countries as they grapple with many of the same problems resulting from their common legacy. Reforms in Central Asia are thus focusing on health insurance funds as a source of new nonbudgetary revenues, decentralization and separation of financing and provision, and measures to encourage efficiency through the use of new incentive-based health-care provider payment mechanisms.
After Russia, Kazakstan and the Kyrgyz Republic have progressed the furthest in introducing legislation to establish health insurance funds based on contributions from employers for the working population and from government for the nonworking population. Both countries have also experimented with health insurance and provider payment reforms based on general practitioner fund-holding mechanisms6 in selected regions. Turkmenistan has established a publicly run voluntary insurance system to pay for outpatient pharmaceuticals and provide for priority use of publicly covered services. There is also a focus on improving both primary care and the effectiveness of public health systems. The intent to focus scarce resources on the most cost-effective interventions is reflected in burden-of-disease and cost-effectiveness studies undertaken in several countries. Other important objectives include developing lists of essential drugs and reforming the procurement, regulation, management, and distribution of pharmaceuticals. Decentralization of financing and use of capitation-based transfers from national to local governments are under way in a number of countries, including Uzbekistan.
Nationwide implementation of health insurance legislation in Kazakstan and the Kyrgyz Republic was delayed and has only recently begun because of depressed economic conditions and the limited ability of employers to make the requisite contributions. Turkmenistan's voluntary insurance program faces major financial difficulties due to premium collection problems, larger-than-foreseen pharmaceutical demand, and the lack of an actuarially sound contribution base. Uzbekistan is also in the process of developing legislation to establish insurance funds based on employer contributions, and is considering provider payment changes, as well as basic benefit packages predicated on cost-effectiveness criteria. Several countries are also considering explicit
privatization of certain services. Tajikistan is in a somewhat earlier stage of designing its reforms.
In general health policy terms, the reforms focus on the five major areas of health-care financing and delivery: financing (i.e., sources of revenue), eligibility, benefits, payment of health-care providers, and the delivery system. Each of these areas is discussed in turn below.
Financing
Most of the focus in current reform debates has been on financing—raising revenues available for health care. Given the large declines in national income and budget revenue described earlier, policymakers are seeking additional financing through extrabudgetary sources and private contributions. There has also been a tendency to decentralize financing responsibilities to local governments, as described in the preceding section. A number of key issues have arisen:
-
Adequacy of financing from both state and employer sources under the various health insurance approaches
-
Ability of regional and local governments to finance their shares
-
Administrative costs of such approaches
-
Roles and responsibilities of national and subnational health authorities and insurance funds
Depressed economic activity in the region has effectively precluded raising additional revenues from both public and private sources. The extensive infrastructures that existed before the economic decline have become unaffordable. Regional and local governments are often unable to afford the increased health-care responsibilities being placed upon them. Enterprises are having serious economic problems, cannot afford to pay additional taxes, and are attempting to divest themselves of their social-service infrastructures and responsibilities. As Russia and the countries of Central Asia struggle with their economic and social priorities, the key task may be learning to develop more efficient systems that are far less extensive than in the past.
The advantages and costs of establishing and running health insurance funds of the types legislated in Russia, Kazakstan, and the Kyrgyz Republic must be considered. Basing insurance coverage on employment means individuals lose their coverage when they are unemployed, and either become uninsured or are insured at the expense of the state. Moreover, there are administrative costs associated with establishing and operating such funds. Multiple funds have higher administrative costs than single funds (Poullier, 1992). Similarly, voluntary insurance approaches, such as the one adopted in Turkmenistan, unless carefully designed, can be fiscally unsound as a result of
favorable selection by sick individuals, as well as lack of a sound actuarial base for premiums.
Changing the source of financing does not enhance the efficiency of the delivery system. Countries such as Canada and the United Kingdom have maintained their general revenue funding bases while successfully implementing payment mechanisms to encourage efficiency. Furthermore, general revenue-based approaches tend to pool risks more equitably than social insurance-based models, as evidenced by the difficulties experienced by both Germany and Japan in pooling risks among multiple sickness funds and government programs. All these issues should be carefully weighed, along with the effects of increased payroll taxes on labor demand and on enterprise viability and competitiveness. Whatever approach is chosen, the financing base must be actuarially sound; that is, the revenues from the designated sources must be sufficient to pay for the individuals and benefits that are covered under the program.
There is a need to clarify the roles of the various levels of government, health-care providers, health insurance funds, and health insurance companies. The relationships and responsibilities of the various agencies involved in health care have been problematic in a number of countries implementing reforms. There is often a preoccupation with financing issues to the detriment of basic public health, policy development, and rational system management—especially in Russia, where confusion and turf battles between financing and health authorities at all levels have been frequent.
Eligibility
One of the great strengths of the previous system was universal entitlement—all citizens were covered. If reform efforts in the region follow the normative tenet applied in most Western market countries that all individuals should have access to care based on need and pay for care on the basis of their ability to do so, insurance reforms and privatization strategies will need to be carefully designed. This will be especially so if private financing is pursued for certain groups and employer and state responsibility for others, to ensure that some individuals do not fall through the cracks and lose eligibility. Moreover, multiple systems are more complicated to administer, have greater difficulty in controlling costs, and, as discussed above, may have more difficulty in distributing risks equitably.
Benefits
People in Russia and Central Asia are accustomed to a system that, at least in theory, provided individuals with all their necessary care free of direct expenditures. Costs did not escalate out of control because of budget caps and
supply constraints—constraints that may be less effective as these systems become more open-ended and private. In any financing system, whether based on general revenue or insurance contributions, it is essential that the contribution levels for employers and the state be set to cover the costs of the benefits package covered under the system.7 This has not been the case in Russia or Central Asia. Part of the problem is political—the perception of taking away the ''unlimited" benefits people used to have.
The other part of the benefit issue is financial: the payroll taxes on enterprises and the required (and not specified) government contributions for those not in the labor force must be sufficient to pay for the individuals and benefits covered under the system. Most former Soviet governments have refused to face this issue directly. Authorities do not want to admit that they cannot afford to cover the services that have been promised. Rational policy would suggest that the state establish realistic expectations on the part of the population and then meet its commitments to finance that level of services. Even in systems still based on public general revenue financing, governments need to consider ways of limiting the package of services available free of charge.
Despite the principle of access to free health care, the situation in practice is very different. Individuals always made informal payments to providers for preferential treatment, and, as discussed earlier, many now pay for certain services out of pocket. For example, survey evidence from the Kyrgyz Republic indicates that the ability to pay is a major problem: the total costs of one episode of ill-health exceeded the monthly income of the entire household in 20 percent of cases, while nearly half of all patients reported severe difficulty finding money to pay for their hospitalization. Moreover, as overall health service utilization rates have fallen in the Kyrgyz Republic, the poorest are least likely to seek medical assistance. In 1994, about two-thirds of households in the top income quintile sought medical help outside the home, compared with only 41 percent of those in the bottom quintile (Abel-Smith and Falkingham, 1996). A similar situation was found in a South Kazakstan oblast (Langenbrunner et al., 1996). The challenge for policymakers in all these countries is to design formal benefit and cost-sharing structures that will capture these largely informal payments in a way that enhances the revenue position of the government while not impeding access to care, especially for the poor.
A related policy concern is determining which services will be provided to the entire population as basic public health services (e.g., immunizations, vector control) and which personal health services should be provided through the insurance benefit package and/or private payments. Such decisions can be assisted by burden-of-disease/cost-effectiveness studies (Godinho, 1996). Such studies enable ranking of health interventions on cost-effectiveness grounds, and provide an empirical basis for deciding which services are to be covered for the entire population as basic public health services, which are to be included in the publicly funded insurance benefit package, and which will not be covered by public programs because they are not affordable and/or of low priority (World Bank, 1993). This is especially important for Russia because of the large declines in male and female life expectancy, and for Central Asia because of the large burden of pretransitional diseases.
Payment of Health-Care Providers
The methods used to pay hospitals, polyclinics, and physicians have important effects on access to care, economic efficiency, clinical effectiveness, quality of care, and consumer satisfaction (Barnum and Saxenian, 1995; Jencks and Schieber, 1991; Langenbrunner et al., 1996). As discussed above, the 18-category normatively based line item budgeting system and salary reimbursement of health-care personnel provide few incentives for efficiency. Health systems in the former Soviet Union have a large quantity of generally low-quality inputs that are not used efficiently. Disproportionate levels of financing and care are rendered at the highest and most costly levels of the system as a result of budget norms, greater availability of supplies and equipment, free pharmaceuticals, and the best physicians being in higher-level hospitals, as well as poor referral and transportation networks and a lack of penalties for consumers or physicians for bypassing lower levels of the system. The deteriorating economic situation also inhibits health authorities from eliminating redundant personnel for fear of exacerbating the unemployment situation.
Virtually all former socialist economies, middle-income Latin American countries, and Western industrial OECD countries are separating provision from financing, having money follow patients in the context of an overall global budget, and adopting incentive-based payment mechanisms for healthcare providers (Schieber, 1995). Experiences in Eastern European countries, Russia, the Kyrgyz Republic, and Kazakstan suggest that the incentive-based systems initially developed and implemented in the OECD countries can work just as effectively in the former socialist economies.
Numerous experiments with new provider systems in Russia date back to the late 1980s, when certain Russian oblasts and republics were allowed to experiment with innovative systems under the New Economic Mechanisms being put in place. Further experiments in provider payment reforms have
taken place over the past several years through the U.S. Agency for International Development's ZDRAV Reform program in Siberia and Central Russia. Both sets of experiments have focused on risk-sharing approaches, case payments, and managed care, and indicate the viability of implementing such approaches in Russia as long as up-front development work is done carefully, and the systems deal effectively with inherent tradeoffs among costs, quality, and access. The general practitioner capitation/fund-holding experiments in Siberia, for example, led to large reductions in inpatient spending, decreases in hospital days, and significant increases in outpatient visits (Langenbrunner et al., 1996).
In Central Asia, the most extensive demonstrations of new provider payment systems are evident in Kazakstan, while the Kyrgyz Republic is undertaking a major demonstration project in general practitioner fund holding (Langenbrunner et al., 1996). In Kazakstan, the most detailed evaluation took place in Dzheskasgan, where a territorial medical organization (TMO) representing local providers and facilities restructured the financing, organization, and payment of health care along several dimensions. The restructured system implemented a new financing mechanism (health insurance fund) for the employed through a payroll tax and capitation payments from the state budget for those not working; established primary-care groups as fundholders who received capitated budgets for their services, including bonus payments to adjust salaries based on economic performance; gave hospitals a case-mix-adjusted flat payment per diem based on historical costs; and instituted contracts between all facilities and the TMO, which then signed a contract with the health insurance fund.
The results of the experiment were generally consistent with expectations: primary-care visits increased, the ratio of general-practice physicians to specialists in polyclinics increased, hospital admissions declined by over 25 percent, and the number of hospital beds decreased from 14.7 to 10.7 per 1000 population. Other, less positive results included a significant number of inappropriate in-patient admissions, continued high referral rates from polyclinics to hospitals, little increase in hospital efficiency, and no increase in the use of preventive services.
Unintended negative effects from health-care reforms in other former socialist economies have included the nonprovision of services, large volume increases, and rising shares of inpatient expenditures. These problems occurred because the new payment systems contained design flaws, including a lack of global budgets in physician fee-for-service and hospital case-based payment systems; open-ended payments for hospitals, coupled with reduced budgets and payments to lower levels of the system, resulting in increased inpatient hospital shares; no monitoring of necessary referrals and quality in capitation-based systems; and inadequate training and/or involvement of relevant stakeholders in the design and implementation phases.
There are a number of issues of particular importance in Russia and Central Asia as a result of the interest of policymakers in general practitioner fund holding, capitation, and case-based payments for hospitals. First, it is essential to define the package of services to be covered under either a general practitioner fund-holding or full-capitation approach. Second, it is important to set the average payment at a level that covers the costs of providing that set of services efficiently. Third, it is important for the capitation rate to be risk-adjusted so that health-care providers will accept sicker patients. The difficulties of doing this should not be underestimated, as there is ample evidence from the United States of insurers and managed-care organizations accepting only healthier patients, leaving the sicker and more costly cases to the public sector (Hadley and Langwell, 1991; Miller and Luft, 1994). Fourth, access, quality, costs, and referrals to other provider levels must be carefully monitored. To work as planned, these systems will require major restructuring and retraining/reorganization of physicians so that cases can be appropriately treated at lower, less costly, ambulatory levels of the system, which currently lack the diagnostic capacity, supplies, and equipment to function in this manner.
The design of provider payment systems is one of the keys to efficiency and long-run financial sustainability. It is also one of the most complex areas of reform in Russia and Central Asia, as these reforms must be accompanied by appropriate management information and quality assurance systems, as well as training of managers at all levels of the system. On the other hand, even simple changes, such as providing facility managers with global instead of line item budgets and eliminating outmoded staffing norms, would result in efficiency improvements. Delaying reforms in this area because of a lack of financing is a shortsighted response. Without reform, both rich and poor countries will continue to get poor value for the money expended.
Delivery System Reforms
There is a recognized need in Russia and Central Asia for restructuring service delivery systems, reducing and retraining health staff, adopting modern medical treatment protocols, better targeting public and environmental health programs, and rationalizing the pharmaceutical sector. Reductions of beds are taking place as a matter of economic necessity. However, it is necessary to develop a strategic approach to hospital rationalization. Such an approach would address, among other things, the need to reduce the excessive specialization and duplication in the hospital system; to promote outpatient care by developing the necessary diagnostic and treatment capacity, including ambulatory surgery centers; and to ensure adequate supplies and pharmaceuticals. There is also a need to retrain physicians in general and family practice, while increasing the ratio of nurses to physicians (Hensher, 1996). Russia is
expending considerable effort to train physicians in the "new" specialties of general and family practice. Making providers autonomous entities is a first step in this direction. Several Russian oblasts and the Kyrgyz Republic are actively moving ahead to restructure their delivery systems, assisted by World Bank projects. Provider payment systems being implemented in Russia, the Kyrgyz Republic, and Kazakstan provide the financial incentives to reinforce delivery system changes. Whether governments will be able to take the difficult step of eliminating surplus employees, given the economic climate, remains to be seen.
In the area of basic health services, all the countries recognize the need to adopt new treatment protocols, which in many cases reflect ambulatory-based treatment regimens and shorter lengths of hospitalization. Burden-of-disease/ cost-effectiveness studies show that the Central Asian countries have a high disease burden both from pre-epidemiological transition diseases affecting women and children and from noncommunicable diseases such as cancer, heart disease, and stroke. A significant part of this disease burden is attributable to social factors such as diet, smoking, alcohol abuse, and violence. Better public and environmental health programs, as well as the availability of appropriate equipment and supplies at the primary-care/feldsher levels targeted at acute respiratory infections and diarrheal diseases, could have a cost-effective impact on improving the health status of mothers and children. Similarly, adult prevention programs focused on lifestyles and substance abuse could help reduce current and future costs associated with treating chronic conditions. This is especially important in Russia and Central Asia given recent declines in life expectancy.
Quality of care could also be significantly improved by adopting modern quality assurance systems rather than the current systems, which rely on sanctions. The former systems are necessary concomitants of provider payment changes and have accompanied the provider payment reforms currently being developed and implemented in Russia, the Kyrgyz Republic, and Kazakstan.
Another area of importance is the development of policymaking and management capacity at the national and local levels and of necessary data for decision making, both economic and epidemiological. Effective and integrated management structures at the central, regional, local, and individual facility levels are essential. As the health systems undergo reform, it is essential to ensure that the data needed for management of the system are collected and transmitted to appropriate decision makers at all levels, including consumers.
It is important as well that national governments not abrogate their public health, staff training, environmental health, and quality assurance functions as the transition to insurance-based and decentralized systems pervades the reforms in these countries. All these countries need to develop national health accounts so they will know the total level of resources committed to the health
sector by source of payment and type of service. Russia is currently in the process of developing such accounts under a World Bank project.
The pharmaceutical sector is also a major area for reform in all six countries. Many of the problems with pharmaceutical production, management, distribution, and pricing stem from inherent structural weaknesses of the old planned production and distribution system, as well as the disruptions associated with the transition to a market economy. As a low-priority sector under Soviet planning norms, the pharmaceutical industry was subject to low overall investment, capacity, technology, and quality. There were little advanced Western production technology and very limited investment in research, and no plants met international Good Manufacturing Practice (GMP) quality standards. Distribution was through a state monopoly, and there was little relationship between production and demand. Moreover, the integrated production structure of the Eastern Bloc led to a focus on heavy industrial investment in Russia, while much of the light industry that produced the final pharmaceutical products was located in other Soviet republics and Eastern Europe. This production and distribution chain was severely disrupted by the breakup, and the prices of raw materials and finished products have escalated. Similarly, there were major problems in the management of pharmaceuticals, including essential drug lists and treatment protocols for the rational use of drugs.
Each of the governments in Russia and Central Asia is seeking ways to reduce budgetary expenditures on pharmaceuticals. Privatization of the pharmaceutical sector and the consequent diversification of sources of financing may allow financial responsibility to shift from state budgets to households by enabling better-off patients to buy pharmaceuticals privately. The resulting savings are likely to be relatively small, however, given the very modest purchasing power of most of the population at present. Reducing costs by increasing efficiency in the sector will depend on several interrelated reforms that face governments around the world, including (1) defining a list of essential drugs; (2) training physicians, pharmacists, and consumers in the rational use of drugs; (3) shifting from brand-name to generic drugs; (4) improving procurement methods (e.g., international competitive bidding) and drug management; and (5) developing sound pharmaceutical pricing policies (e.g., competition policy). Further thought should also be given to redefining the population groups that receive subsidies for drug purchases.
CONCLUSION
The challenge to Russia and the Central Asian countries is to improve the health status of their populations at a time of economic decline while maintaining the strengths of the old system in terms of equity and access. Countries need to maximize the efficiency and effectiveness of their systems, subject to the limited funding available. Since 1990, six countries have faced major economic
declines, and they cannot afford the extensive and inefficient systems of the past. Doing more with less is the name of the game in the short run.
Perhaps most important in terms of direct improvements in health status is the need to restructure current public health activities. This includes maternal and child health programs, family planning, school health, occupational health, environmental health, adult health promotion and disease prevention, substance abuse, and road safety. Given serious overall fiscal pressures in the short term, additional resources to foster these efforts can be obtained only by making efficiency improvements in the current system and formalizing the current official and unofficial systems of user charges. Efficiency improvements can be achieved by restructuring the inefficient health delivery systems, which still have too many staff and too many beds, as well as providing financial incentives for consumers and providers to behave efficiently and introducing modern management and quality assurance systems. The current system of official and unofficial "user charges" should be formalized so the additional revenues will flow to responsible health authorities and can be used for appropriate priority health activities. Such formal user charges should be designed to provide incentives for consumers to use services efficiently while at the same time exempting vulnerable populations, such as the poor, from excessive out-of-pocket payments.
Major reforms are also needed in staff training and medical education. Norms of all kinds—clinical treatment protocols, facility structural characteristics, and staffing—must be eliminated or modernized both to improve health outcomes and to enable facility managers to manage their facilities efficiently. Pharmaceutical sectors need to be reformed in terms of procurement, distribution, management, pricing, rational use of drugs, quality, essential drug lists, and generic substitution. Policymakers will need to address all these difficult issues as the health-care systems in these countries adjust to changing needs and economic realities. Effective reforms now will provide the basis for improved health status, adjustment to the epidemiological transition, improved quality and consumer satisfaction, and long-run financial sustainability.
REFERENCES
Abel-Smith, B., and J. Falkingham 1996 Financing Health Services in Kyrgyzstan: The Extent of Private Payments. Unpublished paper, London School of Economics and Political Science, London.
Anderson, B., and B. Silver 1995 Assessing Trends and Levels in Mortality in the Newly Independent States: Cautionary Notes . Research Report No. 95-326, Population Studies Center, University of Michigan.
Barnum, H., J. Kutzin, and H. Saxenian 1995 Incentives and Provider Payment Methods. Human Resources Development and Operations Policy Working Paper No. 51, World Bank, Washington, DC.
Chernichovsky, D., E. Potapchik, H. Barnum, and T. Tulchinsky 1996 The Russian Health System in Transition: Coping with Old and New Challenges. Paper prepared for The World Bank. Moscow.
Commonwealth Independent States (CIS) various years Demographic Yearbook. Statistical committee. Moscow.
1996 Statistical Bulletin no. 1. Moscow.
Church, M., and E. Koutanev 1995 Report on Health Trends in Central Asia. Almaty, Kazakstan: Abt Associates, Inc.
Field, M. 1995 The Health Crisis in the Former Soviet Union. Social Science and Medicine. 41(11): 1469-1478.
Godinho, J. 1996 Integrated Cost-Effective Care: The Missing Link Between Community, Primary, and Secondary Care. Paper prepared for the Economic Development Institute (EDI) Senior Policy Seminar on Health Reform Implementation in Central Asia. The World Bank, Washington, D.C.
Goskomstat various years Demograficheskiy Yezhegodnik SSSR. Soyuza Sovietskikh Sotsialisticheskikh Respublikakh (SSSR) (State Committee on Statistics of the USSR). Moscow: Finansy i statistika.
Hadley, J., and K. Langwell 1991 Managed care in the United States: Promises, evidence to date and future directions. Health Policy (19):91-118.
Hensher, M. 1996 Rationalization and Management of Hospitals. Paper prepared for the Economic Development Institute (EDI) Senior Policy Seminar on Health Reform Implementation in Central Asia. London Health Economics Consortium, London.
Jencks, S., and G. Schieber 1991 Containing U.S. Health Care Costs: What Bullet to Bite. Health Care Financing Review (Annual Supplement): 1-12.
King, T., and T. Proskuryakova 1996 Changes in Health and Education Expenditures in Russia Since 1991. World Bank, Washington, DC.
Klugman, J., ed. 1996 Poverty in Russia: Public Policy and Private Responses. Washington, DC: World Bank.
Klugman, J., and G. Schieber 1996 A Survey of Health Reform in Central Asia. World Bank Technical Paper No. 344, World Bank, Washington, DC.
Knaus, W. 1981 Inside Russian Medicine: An American Doctor's First-Hand Report. New York: Everest House Publishers.
Langenbrunner, J., S. O'Dougherty, and M. Borowitz 1996 A Review of Selected Financing and Reform Activities in Russia and Central Asian Republics. Paper prepared for the EDI Senior Policy Seminar on Health Reform Implementation in Central Asia. Abt Associates, Bethesda, MD.
Mikhailev, V. 1996 Restructuring Social Assets: The Case of the Health Care and Recreational Facilities in Two Russian Cities, in Restructuring Social Benefits in Russian Enterprises. Organization for Economic Cooperation and Development, Paris.
Miller, R., and H. Luft 1994 Managed care plan performance since 1980. Journal of the American Medical Association 271(19):1512-1519.
Murray, C., and J-L Bobadilla 1994 Epidemiological Transitions in the Formerly Socialist Economies: Divergent Patterns of Mortality and Causes of Death. Health Transition Working Paper Series No. 94.07, Harvard Center for Population and Development Studies, Boston, MA.
Nell, J., and K. Stewart 1994 Death In Transition: The Rise in the Death Rate in Russia Since 1992. Florence: UNICEF International Child Development Centre.
Phillips, M., R. Feachem, and J. Koplan 1992 The emerging agenda for adult health. In The Health of Adults in the Developing World, R. Feachem, T. Kjellstrom, C. Murray, M. Over, and M. Phillips, eds. New York: Oxford University Press.
Schieber, G. 1995 Preconditions for health reform: Experiences from the OECD countries. Health Policy (32):279-293.
Schieber, G., J-P. Poullier, and L. Greenwald 1994 Health system performance in OECD countries: 1980-92. Health Affairs 13(4):100-112.
Sheiman, I. 1994 Forming the system of health insurance in the Russian federation. Social Science and Medicine 39(10): 1425-1433.
Shkolnikov, V., F. Meslé, and J. Vallin 1994 Recent Trends in Life Expectancy and Causes of Death in Russia, 1970-1993. Pp. 3465 in Premature Death in the New Independent States, J.-L. Bobadilla, C.A. Costello, and F. Mitchell, eds. Committee on Population, National Research Council. Washington, DC: National Academy Press.
World Bank 1993 World Development Report 1993: Investing in Health. New York: Oxford University Press.
1996a Kazakstan: The Impact of Transition on Budgetary Expenditures in Health and Education. Washington, DC.
1996b Kazakstan: Transition of the State. Report No. 15353-KZ. Washington, DC.
1996c Kyrgyz Republic: Health Sector Reform Project. Staff Appraisal Report. Report No. 15181-KG. Washington, DC.
1996d Russian Federation: Health Reform Pilot Project. Staff Appraisal Report. Report No. 15585-RU. Washington, DC.
1996e Tajikistan: A Country in Transition: An Economic Update. Report No. 15421-TJ. Washington, DC.
1996f Turkmenistan: Rationalizing the Health Sector. Report No. 14861-TM. Washington, DC.
1997 Hashemite Kingdom of Jordan: Health Sector Study. World Bank Country Study. Washington, DC.
World Health Organization various years WHO Statistical Information System Health-For-All Global Indicators Database, Geneva.
Zahoori, N., L. Kline, S. Broome, B. Popkin, and L. Kohlmeier 1996 Monitoring Health Conditions in the Russian Federation. The Russian Longitudinal Monitoring Survey 1992-95. Report submitted to the U.S. Agency for International Development, Carolina Population Center, University of North Carolina at Chapel Hill, North Carolina.





























