2
Workshop on Pharmacokinetics and Drug Interactions in the Elderly and Special Issues in Elderly African-American Populations
This chapter summarizes the presentations made at the IOM workshop and the discussions that took place among the speakers, committee, and participants (see the Appendix for the workshop agenda and lists of the speakers and participants). Each speaker was asked by the committee to address issues related to the effect of age, gender, race, ethnicity, and the environment on the topic of his or her presentation.
PHYSIOLOGY OF AGING1
Multiple parameters at the cellular and system levels change with age (Table 2.1), and many of these changes have pharmacokinetic and pharmacodynamic implications. Although it is thought that drug absorption is not markedly altered by age, drug distribution, excretion, and metabolism can be affected by a number of the physiological changes associated with aging. For example, age-related changes in body composition with loss of lean body mass and decreased total body water can lead to decreased volume for the distribution of some drugs. These changes can be exaggerated in the presence of disease. The most consistent age-related change affecting drug excretion is the decrease in renal drug clearance resulting from decreased blood flow to the kidneys and decreased renal mass. Data on age-related changes in hepatic drug clearance have been less consistent and may be more complex.
|
1 |
This section is based on workshop presentations by Drs. Jane Cauley, Keith Ferdinand, Jeffrey Halter, and Fran Kaiser. |
TABLE 2.1 Selected Physiological Age-Related Changes in Body Function and Composition
|
Autonomic nervous system |
|
|
Peripheral |
|
|
↓ Baroreflex responses ↓ Beta-adrenergic responsiveness, ↓ receptors ↓ Signal transduction ↓ Muscarinic parasympathetic responses Preserved alpha responses |
|
|
Central |
|
|
↓ Dopamine receptors ↑ Alpha responses ↑ Muscarinic parasympathetic responses |
|
|
Body composition |
↓ Lean body mass ↓ Muscular mass, ↓ creatinine production ↓ Skeletal mass ↓ Total body water ↑ Percent adipose tissue (until age 60, then ↓) |
|
Cellular |
DNA damage and ↓ DNA repair capacity ↓ Oxidative capacity ↑ Fibrosis Lipofuscin accumulation |
|
Ears |
Loss of high frequency hearing |
|
Endocrine |
Menopause, ↓ estrogen and progesterone secretion ↓ Testosterone secretion ↓ Growth hormone secretion ↓ Vitamin D absorption and activation ↑ Incidence of thyroid abnormalities ↑ Incidence of diabetes (decreased insulin sensitivity or increased insulin resistance) ↑ Bone mineral loss |
|
Eyes |
↓ Lens flexibility ↑ Time for pupillary reflexes (constriction, dilation) ↑ Incidence of cataracts |
|
Gastrointestinal |
↓ Hepatic mass ↓ Hepatic blood flow ↓ Splanchnic blood flow ↑ Transit time |
|
Heart |
↓ Intrinsic heart rate and maximal heart rate ↓ Diastolic relaxation ↑ AV conduction time ↑ Atrial and ventricular ectopy |
|
Immune system |
↓ T-cell function |
|
Joints |
Degeneration of cartilaginous tissues Fibrosis, ↓ elasticity |
|
Nose |
↓ Smell |
|
Pulmonary |
↓ Vital capacity ↓ Lung elasticity |
|
Renal |
↓ Renal blood flow ↓ Renal mass ↓ Glomerular filtration ↓ Renal tubular secretion and reabsorption ↓ Ability to excrete a free-water load |
|
Vasculature |
↓ Endothelin-dependent vasodilation ↑ Peripheral resistance ↑ Systolic pressure |
Researchers still do not fully understand the physiological mechanisms of aging or the interaction of age-related changes with drug actions (see, e.g., Box 2.1). Moreover, investigators are only beginning to explore variations among individuals and the role of numerous environmental and genetic factors including gender, race, socioeconomic status, physical activity, and other modifiers that interact with the physiological aging process and affect pharmacology.
Research on the physiology of aging is complicated by difficulties in distinguishing the effects of normal aging from the consequences of coexisting diseases. There is significant variability among individuals (in physical and mental health status and a number of other parameters) that increases with age, and researchers must determine whether the variability is due primarily to disease or to an effect associated with normal aging. At the cellular level, changes due to aging may appear distinct (e.g., increased collagen cross-linkage, decreased elasticity, and alteration in DNA degradation) while in the whole organism, changes due to normal aging are often difficult to separate from disease processes.
|
BOX 2.1: Homeostatic Control Systems Age-related changes in homeostatic control systems present a challenge to the study of the physiological effects of drug therapy. For example, aging has a number of effects on the autonomic nervous system including increased circulating adrenergic catecholamines, decreased resting parasympathetic nervous system tone, and downregulation of peripheral adrenergic receptor function and vasomotor responsiveness, all of which may contribute to the age-related impairment of baroreceptor function. Because the autonomic nervous system plays an adaptive role in modulating the overall body response to a variety of medications, the interaction of age-related changes with drug effects must be considered. An example of this interaction is the use of diuretics or potent alpha-blocking vasodilators for hypertension. Because diuretics can decrease fluid volume, people with baroreceptor dysfunction, such as elderly persons, may be at increased risk for developing postural hypotension during diuretic therapy. Similarly, blockade of alpha-constrictor effects in the presence of blunted heart rate responses (and decreased intravascular volumes) may predispose to postural hypotension. In fact, most symptomatic orthostatic hypotension occurring in older adults can be directly traced to medication use. |
In addition, there are a number of areas in which research is beginning to challenge previous assumptions about aging. For example, osteoporosis, long thought of primarily as a disease risk for Caucasian and Asian women, has become a concern for African-American women as well (with the onset occurring approximately 10 years later than in other elderly female populations). Elderly men are also at risk for osteoporosis, although little is known about the extent of this risk. Research on changes in the endocrine system has in the past primarily focused on women and the relationship between loss of estrogen and bone disease, and more recently, cardiovascular disease. There is still much to be learned about changes in the level of testosterone in men during the aging process (Kaiser and Morley, 1994). Preliminary intervention studies show positive benefits for testosterone replacement (Morley et al., 1993). Studies are ongoing to compare the effects of endogenous versus exogenous hormones (Box 2.2).
The significance of distribution of body weight is of increasing research interest, and the implications of poor nutrition and weight loss are only beginning to be explored in elderly populations (Clarkston et al., 1997). It has been noted that high waist-to-hip ratios are associated with a higher prevalence of diabetes, hypertension, and coronary artery disease. The Baltimore Longitudinal Study on Aging found that, with aging, there is an increase both in upper and central body fat distribution, with most men having a higher waist-to-hip ratio than most women of comparable age (Shimokata et al., 1989).
|
BOX 2.2 Biological Effects of Endogenous and Exogenous Hormones Hormone replacement therapy is widely used in the United States, particularly for its protective effects in reducing the incidence of osteoporosis in postmenopausal women (Cauley et al., 1995). One area of ongoing research is a comparison of the physiological effects associated with endogenous hormones versus exogenous hormone administration. For example, blood concentrations of serum estrogens after estrogen replacement therapy at currently recommended doses are in the range of 153 pg/mL of estrone and 40 pg/mL of estradiol. This contrasts to physiological levels among postmenopausal women, not on hormone replacement therapy, in the range of 30 pg/mL of estrone and 8 pg/mL of estradiol. Estrogen replacement therapy also appears to be associated with significant reductions in the risk of coronary death and death due to stroke. The mechanism of this protective action has not been fully elucidated or separated completely from the selection bias of socioeconomic status found in retrospective studies to date, but potential mechanisms include effects on metabolic processes that produce beneficial changes in lipids and lipoproteins, as well as direct effects on the arteries themselves to improve arterial function. Although there is a strong association of exogenous estrogen administration with reduced cardiovascular disease in women, preliminary research has found no association between endogenous estrogen levels and heart disease in women (Cauley et al., 1994). Studies of the relationship of breast cancer and uterine cancer with endogenous or exogenous estrogens are ongoing. This area of research is one example of the numerous avenues for research on pharmacotherapy in the elderly. Pharmacotherapies such as hormone replacement therapy, raise a number of important questions including the consequences of long-term exposure to medications and the most appropriate methodologies for studying the effects of these drugs on older persons. Observational studies are an appropriate design to use in evaluating long-term exposures, since randomized clinical trials over 10–15 years are inappropriate for this age group. |
Issues in Elderly Minority Populations
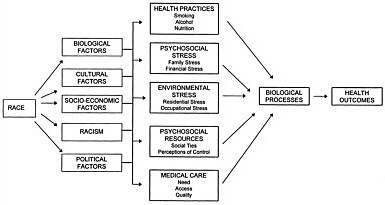
Although the disease burden falls heavily on elderly minority populations, researchers have not fully explored the pathophysiology of disease processes in various minority populations. Health-seeking behavior, socioeconomic status, nutrition, physical and economic access to medications, adherence to prescription regimens, and access to medical care all play a significant role in the prevalence and treatment of diseases in the minority elderly (Figure 2.1). Research is needed to more fully understand the variations between ethnic and racial groups in the time of appearance of disease, the disease processes that dominate, and the effectiveness of treatment interventions.
Hypertension, diabetes, renal disease, and their complications are generally more prevalent in elderly African Americans than in elderly Caucasians. In addition, African Americans frequently have more severe sequelae of hypertension, with higher rates of cardiovascular morbidity and mortality. Isolated systolic hypertension is disproportionately prevalent in African-American women. The cardiovascular risks associated with systolic hypertension have only recently been recognized. The Systolic Hypertension in the Elderly Program (SHEP), a multicenter study of community-based ambulatory elderly patients, has shown that treatment of isolated systolic hypertension can significantly improve cardiovascular survival and decrease risk of stroke in elderly patients (SHEP Cooperative Research Group, 1991). However, as in many studies, there was not significant representation from minority patients.
Studies indicate an earlier onset of hypertension in African Americans and suggest differing responses to antihypertensive medications. Recent studies have shown that African-American hypertensive cohorts had a higher response rate to treatment with calcium channel antagonists and diuretics and a lower response rate to treatment with ACE (angiotensin-converting enzyme) inhibitors and beta-blockers (reviewed in Jamerson, 1993). Possible physiological explanations include variations in the regulation of salt and water balance, variations in the angiotensin–renin system, differing sensitivities to the vasodilator bradykinin, or angiotensin-converting enzyme polymorphism. Thus, further research is needed to optimize the development of effective clinical therapeutic regimens.
INTRACELLULAR RESPONSES2
Pharmacokinetics
The therapeutic effect of a drug will be produced only when the appropriate concentration of the drug is present at its site(s) of action. Many medications act by binding to receptors at the cell surface; other medications require intercellular transport. Transport across cell membranes may occur through passive diffusion or facilitated diffusion (i.e., carrier-mediated transport in which there is no input of energy) or active transport through carrier-mediated membrane transport. At this time there are few data that examine the effects of age, sex, or ethnicity on transport mechanisms.
|
2 |
This section is based on workshop presentations by Drs. Darrell Abernethy, Grant Wilkinson, and Kurt Rasmussen. |
In addition to the transport of the drug to the site of action, drug concentration also depends upon the extent and rate of drug absorption, distribution, protein binding, and elimination. Important age-related changes in body composition and functioning (see Table 2.1) are relevant to drug disposition and, in turn, affect drug concentration. These changes have significant implications for clinical therapeutics in the elderly (Scharf and Christophidis, 1993).
The absorption of drugs (which affects the duration and intensity of drug action) does not generally appear to be significantly impaired in the elderly; however, the distribution of drugs may be affected. Certain physiological and physiochemical properties including cardiac output and regional blood flow will determine how a drug is distributed through the body. The drug is distributed to the heart, liver, kidney, brain, and other highly perfused organs during the first few minutes after absorption. Delivery to muscle, viscera, skin, and fat occurs later and at a lower level (Benet et al., 1996). In addition, distribution may be limited to the vascular compartment by the drug binding to plasma proteins, particularly albumin and alpha1-acid glycoprotein. As the production of albumin by the liver generally declines with age, there may be an age-related rise in the free fraction of any highly albumin-bound drug. Although this change does not by itself cause an increase in the drug concentration, it may be a marker for other alterations that may be associated with increased drug sensitivity. As lean body mass falls and total body water falls, both in absolute terms and as a percentage of body weight, the volume of distribution of highly lipid- or water-soluble drugs will be affected.
Altered drug elimination is also a consideration in the elderly. Drugs are eliminated from the body either by metabolism (primarily by the liver) or by excretion (primarily by the kidney). Drug metabolism in the liver occurs by a variety of reactions such as oxidations, reductions, or hydrolytic processes. In addition, drugs may be metabolized by conjugation reactions, such as acetylation, glucuronidation, or sulfation. There is evidence to suggest that oxidative metabolism decreases with age, whereas conjugative metabolism appears to be less affected by aging (Scharf and Christophidis, 1993). It is known that liver mass decreases with age, as does hepatic blood flow (see Table 2.1). Additionally, oxidative metabolism may also be influenced by smoking, genetics, gender, concurrent diseases, and frailty.3 Renal function also declines with age, as reflected by declines in creatinine clearance. When creatinine clearance falls below 30mL/minute, 4 the excretion of drugs that are eliminated mainly by the kidneys decreases significantly and
|
3 |
In general, frailty is the term used by health professionals to describe elderly persons who require assistance with mobility and activities of daily living, have abnormal laboratory findings, and suffer with co-occurring medical conditions including Alzheimer' s disease, multi-infarct cerebrovascular disease, Parkinsonism, osteoporosis, or healed fractures (Scharf and Christophidis, 1993). |
|
4 |
Normal creatinine clearance in a young adult is 100–120 mL/minute. After age 40, creatinine clearance on average falls by 10 percent for every decade of life (Lee, 1996). |
the risk of accumulation of the drug and its metabolites increases (Lee, 1996). Although measures of creatinine clearance provide dosing guidelines for drugs that are excreted exclusively by the kidneys, changes in hepatic metabolism with age and pathology are more difficult to estimate quantitatively.
Inter- and intraindividual variability in the pharmacokinetics of many drugs is largely determined by variations in hepatic drug clearance as described by the parameters of hepatic blood flow and metabolic capacity. These parameters may be altered as a result of liver disease, genetic differences in enzyme content, and drug interactions. Several metabolizing enzymes have been identified and characterized at the gene, mRNA, and protein level, as have their substrate specificities, including N-acetyltransferase (NAT) and isoforms of cytochrome P450 5 (e.g., CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A). Some of these isoforms (e.g., NAT2, CYP2C19, and CYP2D6) exhibit genetic polymorphism such that there are subpopulations that may include a small group of people (3 percent–10 percent) who are homozygous and have the poor metabolizing phenotype (i.e., they have an impaired ability to metabolize specific chemicals or drugs) or the extensive metabolizing phenotype, which consists of both the homozygous and the heterozygous genotypes. In many different ethnic and racial groups (e.g., African Americans, Caucasians, Asians, Native Alaskans, and North Africans) there are differences in the frequency of the deficient alleles. For example, in African Americans, the frequency of the poor metabolizing allele for debrisoquine sulfate (an antihypertensive drug that is a specific substrate for CYP2D6) and for over 40 cardiovascular and central nervous system drugs is lower than in Caucasians. Thus, in populations of African Americans the proportion of people who cannot metabolize these drugs extensively is smaller. Asians also exhibit a significantly lower frequency of the poor metabolizing characteristic (~1 percent) than Caucasians (~7 percent) for CYP2D6 substrates.
Studies of the effects of physiological aging on the distribution and elimination of drugs in representative populations of the elderly are complex. Multiple confounding variables (e.g., gender, race, ethnicity, body weight, and exposure to caffeine, nicotine, and alcohol) and concomitant diseases, increase the difficulty of understanding the implications of age-related changes on clinical therapeutics in the elderly population.
|
5 |
Cytochrome P450 (CYP) is a primary component of the oxidative enzyme system. Individual differences in enzyme activity and susceptibility to induction are genetically determined. Rates of biotransformation (which fosters elimination of drugs) may vary significantly among individuals. |
Cardiovascular Physiology
Cardiovascular disease is the single largest cause of death in the elderly. Although basal cardiac output is maintained in the elderly by an increase in ventricular size and greater stroke volume than in the young, maximal- and stress-related responses are decreased. With regard to cardiac and arterial function, the following changes are also characteristic of aging:
-
decreased intrinsic heart rate,
-
impaired diastolic function (e.g., slowed cardiac diastolic relaxation),
-
increased atrial and ventricular ectopy,
-
prolonged AV conduction times and increased repolarization times,
-
decreased elasticity of the aorta and large vessels,
-
impaired baroflex function, and
-
impaired vascular endothelium-mediated function (Stolarek et al., 1991; Lakatta, 1993; Lakatta et al., 1987, 1993; Craft and Schwartz, 1995).
The physiology and pharmacology of the autonomic nervous system and the sympathetic regulation of the cardiovascular system are clearly affected by aging. Normally, stretch receptors in the systemic and pulmonary arteries and veins monitor intravascular pressures; the resulting afferent impulses alter sympathetic activity. An increase in blood pressure stimulates arterial baroreceptors, which results in the inhibition of central sympathetic outflow. In the opposite manner, when blood pressure falls, decreased afferent impulses diminish central inhibition, resulting in an increase in sympathetic outflow, withdrawal of parasympathetic tone, and a rise in arterial pressure. Thus, baroreceptors play an important role in blood pressure regulation. However, baroreceptor reflex activity appears to decline with age.
There appear to be significant age-related changes in adrenergic receptors.6 Although circulating norepinephrine levels increase in the elderly, there is no change in the sensitivity to the vasoconstrictor alpha1-adrenoceptor while there is evidence for both a decline in peripheral beta-adrenoreceptor numbers and decreased activity of the G-coupled protein complex and related intracellular second messengers. Age-related changes in central nervous system adrenoreceptor responses are less clear (White et al., 1994).
|
6 |
Alpha-adrenergic receptors (there are distinct alpha1- and alpha2-receptor subtypes) mediate vasoconstriction, intestinal relaxation, and pupillary dilation. Beta-adrenergic receptors (the three distinct subtypes are beta1, beta2, and beta3) stimulate heart rate and increase contractility, vasodilation, bronchodilation, and lipolysis. |
Neurotransmitter Receptors
The brain is one of the most complex organ systems in terms of drug actions and disease. Research on the mechanisms of signal transduction, or intercellular communication, in the brain over the past two decades has shown that simple models of synaptic transmission (involving the release of neurotransmitters, which bind to specific receptors and either stimulate or inhibit neural activity) are not sufficient to explain all of the effects of neurotransmitters on neurons. It has been observed that a medication that acts at one or more neuronal receptors may also change neuronal activity by more than one mechanism depending on prevailing conditions at the receptor site.7 However, the biological significance of having varied mechanisms of intracellular communication among neurons in the brain also depends on the part of the brain involved and its complex connections and pathways to other brain regions, as well as on the composition of neurotransmitters and receptors present in specific brain regions.
These varied mechanisms of neural activity underly both long- and short-term responses of neurons. For example, short-term effects may include inhibition or excitation of neuronal activity affecting the release of neurotransmitters along brain pathways (chains of neurons comprising subsystems with specific functions). However, research has identified a variety of subtypes of many neurotransmitter receptors (e.g., dopamine and serotonin receptors) that function differently and exhibit different pharmacological responses. In addition, some neurotransmitters exert effects by binding to receptors coupled to ion channels (proteins that regulate the flow of specific ions, e.g., chloride and sodium), and many neurotransmitters affect a cascade of intracellular chemical reactions that, eventually, lead to changes in gene expression in the neural cells. Such long-term effects of neural transmission are often mediated by proteins in neuronal membranes coupled to receptors and a variety of so-called “second messenger ” molecules that act inside cells to regulate many cell processes including changes in gene expression. All of these reactions may be affected by aging; however, they also provide targets for therapeutic interventions.
Neurological diseases present important challenges to medication development and use in the elderly. Two neurological disorders often associated with aging are Alzheimer's and Parkinson's disease. Alzheimer's disease is clearly age related (it is uncommon in young or middle-aged persons) with a prevalence as high as 47 percent in people over 85 years, and this disease is the leading cause of cognitive impairment in the elderly population. The pathological features of Alzheimer's disease include neuritic plaques, neurofibrillary tangles, and the death and disappearance of nerve cells in the cerebral cortex. The densities of forebrain
|
7 |
Similarly, it is by means of different receptors that norepinephrine can cause constriction in vessels of the skin and dilation of those in muscles. Acetylcholine too has an excitatory function, but it can also be inhibitory, depending on prevailing conditions at the receptor site. |
cholinergic neurons are markedly decreased in cortical and hippocampal (but not striatal) areas in Alzheimer's disease; however, there does not seem to be a corresponding decrease in postsynaptic receptors. Thus, the preserved postsynaptic receptors provide a target for therapeutic intervention.
Parkinson's disease is a disorder of middle or late life that involves the nigrostriatal dopaminergic system and is characterized by changes in the aggregates of melanin-containing nerve cells in the brain (the substantia nigra and locus coeruleus) (Isselbacher et al., 1994). The dopamine carrier (dopamine uptake complex) is involved in the uptake of the dopamine released into the synaptic cleft at the level of nigrostriatal dopaminergic neurons. With increasing age, the number of dopamine terminals in the striatum decreases. Clinical symptoms in Parkinson's disease do not appear until almost total depletion of dopamine has occurred in the striatum. In fact, it appears that Parkinsonian symptoms become apparent only when there is at least 80 percent degeneration of the dopamine terminals. That suggests the existence of either a compensatory mechanism to offset the loss of nigrostriatal dopaminergic neurons or a significant basal excess of terminals (Anglade et al., 1995). In addition, positron emission tomography (PET) scans suggest that there are fewer postsynaptic dopamine receptors. The depletion of postsynaptic receptors coupled with the degeneration of the dopaminergic pathway provides a significant challenge to the development of a pharmacotherapeutic intervention.
CHRONIC USE OF MEDICATIONS8
Treating the health problems of older patients presents a number of challenges, as these patients frequently have multiple health problems. For example, elderly patients who survive a myocardial infarction may have chronic ischemic heart disease, hypertension, and other related chronic conditions such as diabetes. Each of these conditions may require one or more medications, thereby increasing the risk of drug–drug interactions as well as the side effects of each of the drug therapies. This is complicated by the recent trend toward the use of multiple drug regimens as the most efficacious way to treat a variety of common chronic conditions (e.g., osteoporosis, hypertension, coronary artery disease, diabetes, congestive heart failure, and chronic lung disease). In addition, these conditions may be chronic, requiring long-term use of the medications. The duration of therapy and the effect of chronic use of medications are areas of increasing concern. As life expectancy lengthens, there will be increased numbers of older persons with chronic conditions who might require pharmacotherapeutic treatment for decades. Further, many patients also use over-the-counter medications and a wide range of dietary supplements, vitamins, and other nutraceuticals for which the physiological actions and interactions with medications are largely unknown.
|
8 |
This section is based on workshop presentations by Drs. Louis Lasagna, Bruce Pollock, and Wayne Ray. |
Measuring Drug Use
It is important to be able to measure past and current drug exposure when treating multiple comorbidities in the elderly and when enlisting elderly participants into clinical trials on drug effects and outcomes. However, it is often difficult to measure drug exposures accurately.
There are a number of complexities in measuring medication use. First, the information collected about the medication must be very specific. Within the same class of drug compounds there can be wide differences in adverse effects. Product formulations can vary between manufacturers, and information on the formulation is needed to distinguish various dosage forms and their respective effects. Second, information is needed on the timing of drug use and the subsequent occurrence of adverse effects. Acute effects, such as psychomotor impairment associated with psychotropic drugs, occur while the medication is in use, whereas other adverse effects may occur once drug use has stopped. Third, the dose is an important measure because many adverse and beneficial effects of drugs vary with dose—for example, the risk of serious peptic ulcer disease associated with the use of nonsteroidal anti-inflammatory drugs (NSAIDs).
The three techniques most commonly used to measure drug exposure are biologic measurement, interviews, and the use of pharmacy or other medical records. Each of these methods has its strengths and weaknesses in terms of obtaining valid data, particularly on the chronic use of medications. Current biological measurements (e.g., blood or urine tests) provide precise data; however, it is difficult to get people into the laboratory to take these tests and the cost of the tests may be a prohibitive factor. Additionally, biomarkers are needed to determine long-term past exposures.
Interview techniques generally provide accurate data on current medication use, particularly when combined with inspection of medication containers. However, retrospective drug use is more difficult to recall and document. There also appears to be a confounding issue related to the responses made by well and sick individuals about past medication use.
Pharmacy records provide a reasonable surrogate for drug exposure and are often the best method for assessing the history of drug use because they allow detailed tracking over time. Additionally, these records are relatively free from information bias. Unfortunately, the dispensing of medications does not necessarily correlate with actual drug use, and compliance is difficult to measure with this method. Moreover, pharmacy records have their own inherent weaknesses: patients do not always get their medications at the same pharmacy, outpatient
and inpatient pharmacy record systems are rarely integrated, and most pharmacy records do not contain information on nonprescription medication use.
Chronic Drug Use
As the average lifespan of the population increases, it becomes important to shift focus from the acute effects of medications to their chronic effects in older patients. Some medications that are now prescribed for the elderly may be used for 20–30 or more years (e.g., antihypertensives, hormone replacement therapy, antidepressants, NSAIDs).
Depression, for example, is a relatively common condition in the elderly that is associated with considerable medical and social morbidity (Ruegg et al., 1988; Stewart, 1993). Although the prevalence of depression has not been found to differ by race, there are some indications that depression is an undertreated problem among African Americans (Brown et al., 1995). Pharmacotherapeutic treatments for depression must be carefully monitored in elderly patients because the consequences of treatment failure due to undermedication and the risk of drug toxicity resulting from overmedication may be more severe in older patients than in younger adults (Salzman, 1993; Pollock, 1996). One class of medications, selective serotonin-reuptake inhibitors (SSRIs), are increasingly prescribed to treat depression. However, the SSRI clinical trials were conducted primarily in younger patients, and there is a paucity of data on the effects of SSRIs on elderly patients. There is some preliminary data, however, showing that adverse effects in the elderly (e.g., insufficient antidiuretic hormone secretion, weight loss, extrapyramidal symptoms) differ considerably from those seen in younger persons, although the effects of chronic use of pharmacotherapeutic treatment of depression in the elderly are largely unknown. Maintenance doses of antidepressants have been shown to be effective in delaying the relapse of depression in elderly patients (Katz and Alexopoulos, 1996), but studies are needed on the long-term effects of these medications (Leo, 1996). Recent data on the prospective use of neuroleptics raise concerns about the extreme susceptibility of older patients to both acute and chronic neurological side effects. In particular, African Americans and patients with diabetes seem to be at increased risk for tardive dyskinesia (Pollock and Mulsant, 1995).
There are a number of additional areas in which ongoing research has been inconclusive about the risks and benefits of chronic drug use. For example, it has been found that there is a lower relative risk associated with fractures and heart disease among women who initiated estrogen replacement therapy within 5 years of menopause and who continue long-term use. However, there are unresolved questions about the possibility of an increased risk of uterine and breast cancer due to estrogen replacement therapy. Treating high cholesterol levels late in life has raised questions, inasmuch as there is some evidence that low choles-
terol levels are associated with lowered serotonin function and greater risk of symptoms of depression.
Another issue to be considered in the chronic use of medications is the impact of medications with longer half-lives (e.g., alendronate, a new treatment for osteoporosis with a terminal half-life of approximately 10 years). Postmarketing surveillance will be important for evaluating the long-term effects and adverse outcomes of drugs that are used over long periods of time.
Use of Nutraceuticals
In addition to prescription and over-the-counter medications, there is a diverse group of other substances of interest—nutraceuticals. The term nutraceuticals is relatively new and is typically used to encompass dietary supplements, vitamins, herbal medications, sport drinks and energy bars, and herbal teas (DeFelice, 1991). These products have not been considered drugs, and most have not been examined with regard to their safety and efficacy. There are concerns about nutraceutical use by the elderly that relate to cost, unsubstantiated health claims, toxicity, and nutrient–drug interactions (Geriatrics Newsletter, 1996). However, neither the academic research community nor the food industry has made funding research and development a priority for this growing class of compounds. It has been difficult in the past to obtain persuasive data about traditional herbal remedies. In addition, there is disagreement over terminology (Are these products foods, supplements, drugs, etc.?), the dose that distinguishes a “food supplement” from a “drug,” the data required by the Food and Drug Administration (FDA) to support health claims, the regulatory authority of the FDA over many of these products, and the manner in which nutraceuticals should be regulated. Further, the panoply of nutraceuticals has resulted in a deluge of information regarding their utility, with a paucity of research to support the claims of benefits, cures, or preventive effects. This situation, coupled with the often-held belief that the American diet is nutritionally adequate and a lack of knowledge regarding nutritional factors and malnourishment in the elderly, result in confusion regarding the status of nutraceuticals in the diet of elderly persons. What is known, however, is that the potential risks and benefits to the elderly resulting from the use of various nutraceuticals beyond current recommended doses are controversial. Very high amounts of these substances can interfere with normal metabolism, clinical laboratory tests, and with the action of prescribed medications. These reactions may cause serious problems for the elderly, particularly for those people with deteriorating health and inadequate nutrient intake. It has been suggested that elderly or chronically ill persons should not use high-potency nutraceuticals without medical supervision (Geriatrics Newsletter, 1996).
PHARMACOECONOMICS9
Increasingly, health care decision makers are insisting on having better information about the cost-effectiveness of pharmacotherapies. In addition to clinical and quality-of-life outcomes, clinical trials sponsored both by the pharmaceutical industry and the federal government are integrating analyses of the cost-effectiveness and cost consequences of pharmacotherapy as outcome variables.
The elderly population was estimated to spend an average of $500 per capita for prescription drugs in 1991 (Long, 1994). This spending is disproportionate within the elderly population, with approximately 11 percent of the elderly population accounting for nearly half of the expenditures on prescription drugs (Long, 1994). The cost of medications is of concern to older persons, many of whom live on fixed incomes. Approximately 45 percent of the elderly population do not have insurance coverage for prescription drugs (Long, 1994), and many elderly people with insurance coverage cannot afford the high copayments, coverage limits, or both, for prescription medications. Medicare does not cover payments for outpatient prescription drugs, and as a result there is a piecemeal, inconsistent approach to prescription drug coverage that includes Medigap policies, Medicaid, other state assistance, retirement programs, and health maintenance organizations. Restrictive formularies, limited participation of pharmacies, and caps on reimbursements are other issues that many elderly persons face as a result of piecemeal prescription drug programs.
The economics of pharmacotherapy for the elderly encompass many factors beyond the direct cost of drugs including transportation costs, paid and unpaid assistance in the home for managing health care problems, and the cost of hospitalizations. The potential loss of earned income or productivity may also be an issue among those age 65 or over, and it is important to consider the intangible costs of pharmacotherapy, particularly on quality of life. In addition, there are costs associated with drug-related morbidity and mortality,10 which may result from treatment failures due to noncompliance or undercompliance with prescription regimens or adverse drug reactions, including those due to interactions with other medications, nutraceuticals, or foods. The fact that adverse drug reactions are more prevalent in the elderly population is in large part attributable to the increased number of medical problems they face, particularly chronic conditions in older patients and their increased use of medications. A further cost to society, which has not been well studied, is the undertreatment of medical conditions, which can have economic consequences by leading to inappropriate treatments or to the eventual presentation of more severe symptoms (an example of this is the undertreatment of glaucoma in elderly AfricanAmericans). The prevalence and cost of undertreatment are not well understood relative to pharmacotherapy.
|
9 |
This section is based on the workshop presentation by Dr. Andy Stergachis. |
|
10 |
Drug-related morbidity and mortality for the entire U.S. population has been estimated to cost $76 billion (Johnson and Bootman, 1995). |
Pharmacoeconomic research focuses on the economic savings resulting from use of medications—i.e., the relative trade-off between spending on pharmaceuticals and subsequent savings in medical care costs. There has, however, been little research focused on the cost-effectiveness of therapies that stratifies cost-effectiveness ratios by age. One study that has used this approach examined the cost-effectiveness of thrombolytic therapies and found the lowest (least favorable) cost-effectiveness ratio in younger patients and the most favorable in older patients (Mark et al., 1995). More studies are needed that stratify pharmacoeconomics as an endpoint not only by age, but also by other factors, such as quality of life, in an effort to provide the most cost-effective treatments.
There is a paucity of information regarding drug utilization among minority elderly persons and even less research on the economics of drug utilization among groups according to race and ethnicity. Fillenbaum and coworkers (1993) found a lower utilization of prescription and nonprescription drugs among African-American elderly populations than among Caucasian elderly populations. In both groups, health status and use of medical services were found to be the strongest predictors of prescription drug use. This contrasts somewhat with the 1987 National Medical Care Expenditure Survey, which found no significant differences in the percentage of African-American and Caucasian Medicare beneficiaries who received one or more drugs.
Few differences have been found in the percentage of elderly Americans with insurance coverage for prescription drugs by race or ethnicity; however, the type of coverage generally varies. Medicaid is more predominant among African Americans; employer-provided retirement assistance programs are more common among the younger old (age 60 –74 years), particularly among Caucasians. A recent survey found that African Americans reported having more financial problems than Caucasians in covering their medical care expenses, including prescription drugs (Blendon et al., 1995). Research is needed to better understand the relationship between race and ethnicity and the economics of pharmacotherapy. It is, however, important to remember that there are other confounding variables within the heterogeneous elderly population.
Recent trends in health care delivery may have a significant impact on pharmacoeconomic studies. Increasing numbers of not only Medicaid recipients, but also Medicare enrollees, are moving to managed care plans, with the greatest growth occurring in Medicaid-based managed care plans. Many managed care plans currently provide prescription drug coverage for the elderly, but it is too early to evaluate the extent of coverage, the time frame for coverage, and its relative effect on the health of this group. State Medicaid databases are an important source of data for research on pharmacoeconomics, and there is concern that managed Medicaid plans will result in the loss of access to data on drug
utilization and health outcomes. The unintended result of that would be to limit studies on pharmacotherapy in elderly populations.
CLINICAL TRIAL RECRUITMENT11
Clinical trials are conducted to establish the safety and efficacy of drugs. There are several phases of clinical development of a drug. Phase I studies are usually conducted to establish a drug's safety. These are small trials that typically involve only healthy volunteers to determine pharmacokinetics and overall safety. Phase II studies establish a drug's pharmacological actions and note adverse reactions in individuals affected by the disease or condition for which the drug is targeted. Phase III studies evaluate a drug's benefits and risks in larger numbers of patients and in special populations. The data collected in Phase III studies help to better define safety and efficacy and provide important information to enable physicians to use the drug effectively. Phase IV postmarketing studies generally evaluate the drug under normal use conditions (OTA, 1993).
Until recently, most of the volunteers who have enrolled in clinical trials have been young Caucasian men. It is only in the past few years that citizen groups have pointed out this deficiency and ground rules for participation by women of child-bearing potential have been established, allowing their rather common inclusion in clinical studies. The elderly typically have not been recruited for clinical trials because of their multiple comorbidities, high prevalence of chronic illness, and chronic medication use (Wenger, 1993). As a consequence many studies have age-based exclusions (Gurwitz et al., 1992). However, the systematic exclusion of elderly populations from clinical trials leaves many questions unanswered with regard to age –disease interactions, disease– disease interactions, disease–drug interactions, and age–drug interactions. These questions remain unanswered for elderly minority populations as well. Yet, increases in the size of the elderly population, increases in the range and extent of health problems associated with aging, and subsequent increase in the use of medications by the elderly (Chapter 1) make it imperative to study the safety and efficacy of drugs in this population. It has been estimated, for example, that if an effective medication could be developed to produce a 5-year delay in the age of onset of Alzheimer's disease, it would reduce the prevalence of this disease by 50 percent in one generation. If, for all diseases, the postponement of dependency for 1 month could be achieved for all people over 65 years of age, the cost savings would be approximately $5 billion per month, or $60 billion per year.
|
11 |
This section is based on the workshop presentations by Drs. Richard Corriveau, Gregory Sachs, Nanette Wenger, and Jackson Wright. |
A few additional demographic points that make pharmacotherapeutic research for the elderly imperative include
-
the size of the population of the oldest old is increasing markedly;
-
health status will decline and comorbidity will increase progressively with aging; and
-
almost one half of the current U.S. population can anticipate living to age 80.
Given the statistics and demographics regarding the elderly, the FDA issued a guideline in 1989 for testing drugs in the elderly. The guideline was intended to encourage routine and thorough evaluation of the elderly in an effort to provide physicians with sufficient information regarding the use of drugs in older patients. The guideline states that, “there is no good basis for the exclusion of patients on the basis of advanced age alone, or because of the presence of any concomitant illness or medication, unless there is reason to believe that the concomitant illness or medication will endanger the patient or lead to confusion in interpreting the results of the study. Attempts should therefore be made to include patients over 75 years of age and those with concomitant illness and treatments, if they are stable and willing to participate (FDA, 1989).” Although the FDA guideline is useful in providing a message that exclusion from a trial because of chronologic age is not appropriate, researchers are not legally required to follow the guideline (Gurwitz, 1993).
Nevertheless, there remain significant barriers to the inclusion of the elderly in clinical trials. Paradoxically, however, the barriers to their inclusion in trials are also the reasons to study this population. The barriers include
-
the complexity of the elderly population, which can confound the study interpretation because of multiple diseases and therapies and coexisting psychological and social problems;
-
differing physiology and pathophysiology in the elderly as compared to younger populations;
-
problems with obtaining proper informed consent in those elderly patients who are confused,who are demented or become so during the study, or who have declining or fluctuating cognition; and
-
the costs associated with recruitment and surveillance of the elderly, and the need for a larger sample size.
There are methodological issues, however, that can be utilized to overcome some of the barriers. With regard to the effects of heterogeneity and the associated increase in variability in response, trials can be stratified by clinically meaningful parameters such as the number of co-occurring illnesses, the number of drugs, measures of health status, and general measures of disability. Stratifying by those parameters can limit the effects of heterogeneity. Stratification may
include groups that age successfully, groups that demonstrate typical aging (with illness and disability), and the frail elderly (i.e., those with multiple illnesses and severe disability). Outcomes that either maintain or enhance independence and functional status may be assessed, and outcomes that address prevention or complications of existing disease may be considered. In addition, a variety of endpoints should be examined other than mortality. More appropriate endpoints to consider in this population may include morbidity and functional status, quality of life, impact on coexisting illnesses, and cost-effectiveness.
Other aspects of methodology that need to be explored include the selection of a subpopulation of older persons for a trial based on the purpose of that trial (e.g., a drug intervention trial may more appropriately involve a heterogeneous group of elderly to test efficacy in a broad sample, whereas targeted interventions may involve a more homogeneous subpopulation). Selection of the subpopulation of elderly persons may condition the intervention (e.g., the specific design of an exercise intervention is unlikely to be similar for healthy and ill older persons). Finally, selection of the subpopulation may affect the generalizability of the results (Harris, 1993).
Ethical considerations may need to be broadened with regard to the participation of elderly persons in clinical trials. Whereas previously the emphasis was on symptomatic relief, it may be important to include quality of life and prolongation of life as issues that should be considered in future studies. In addition, there may be a need to identify population subsets with the greatest potential for benefit or for harm from an intervention.
Complicating the ethical issues related to this group is the number of elderly persons with dementia. The capacity to make decisions and give informed consent is a difficult issue. Statistically, the elderly are more likely than the young to be affected by dementia or to be cognitively impaired. Furthermore, this population more frequently suffers from delirium and psychiatric illnesses than do younger cohorts. All of these conditions raise questions about the ability to give consent to participate in studies. There is also a concern about nursing home residents and their ability to give consent free from coercion. Further, elderly persons may be subject to abuse by others and are more likely to be impaired by the toxic metabolic effects of illness. Nonetheless, research with elderly persons who are capable of making decisions is governed by exactly the same principles and processes as clinical research with other age cohorts. The researcher clearly has an obligation to investigate and determine the cognitive capacity of each potential study participant (Dubler, 1993).
The recruitment of elderly minority populations into clinical trials, especially African Americans, has proved to be difficult. A variety of factors have contributed to this situation:
-
occurrences of research exploitation of minority populations (e.g. sickle-cell screening programs, involuntary sterilization, and the Tuskegee syphilis experiments);
-
the limited access of many minority persons to health care (including high-technology and costly interventions);
-
a lack of trust placed in the medical community (e.g., the view of AIDS as being a genocidal plot);
-
frustration over an inability to have access to costly pharmacotherapeutic interventions once medications are chosen as the therapy of choice;
-
a poor understanding of the need for clinical trials;
-
a poor understanding of the safeguards in place in human subject research; and
-
difficulty in getting to the site of a trial.
Yet it is important to include minorities in drug trials, as there may be significant differences in drug metabolism and therapeutic outcomes between ethnic groups. Cross-cultural validation of quality-of-life measures and utility measures (i.e., patient preferences and values) are also important in assessing the efficacy of drug therapies.
Several mechanisms have been suggested to overcome some of these difficulties. It is important to obtain the endorsement of community physicians and leaders within the African-American community. Additionally, clinical trials should be advertised at cultural events and community gathering places (e.g., churches, barber shops). Ensuring that study participants are treated with dignity and respect is another critical factor. Other mechanisms to increase African-American participation in clinical trials include
-
the association and collaboration of universities and historically African-American colleges in administering trials;
-
educating individuals and communities about the benefits of participation in trials and about the safeguards in place for human subject research;
-
recruiting minority researchers and staff to enlist patients into clinical trials;
-
educating and disseminating information to the community about the knowledge that will be gained from the study and its potential impact on disease prevalence within the minority community; and
-
providing transportation (or reimbursement for travel) to the study site.
The ability and commitment of researchers to accommodate the study population will affect success in minority recruitment. This issue is important both to ensure equal generalizability in populations that may demonstrate differences in drug metabolism from those seen in other ethnic groups and to validate cross-cultural quality-of-life measures.
INFORMATION DISSEMINATION12
Disseminating the immense amount of frequently changing and technically detailed information about pharmacotherapeutic interventions in a timely manner presents an ongoing challenge. The targets for this information—physicians, pharmacists, other health professionals, and patients—each have their own set of information needs and ways they access information.
Physicians and Pharmacists
Information on new medications and on drug interactions changes rapidly. As a result, some of the biggest challenges facing physicians and pharmacists concern updating existing information and accessing new information. Health professionals are trained to remember large amounts of information, unfortunately, they find it difficult to forget outdated information. Having an efficient way of delivering information so that it reaches health professionals at the time they are making decisions about drug therapy and writing or filling a prescription is a key need. Information is also critically needed when patients are being monitored for compliance and intended outcomes.
Determining a patient's current and prior drug profile is another challenge. Many elderly persons have several diseases and take numerous medications, and they frequently see several health care professionals and obtain their medications in a variety of locations. All of these factors make it difficult to individualize drug information and to track prescriptions. The disparate nature of the health care system and the inadequacies of medical records place the information burden on patients by requiring them to remember each of their numerous medications. Additionally, it is important for information dissemination to flow in two directions—i.e., health care professionals need to educate patients on appropriate medication use and drug interactions, and they also need to receive information from their patients regarding their medication use, adverse effects, and other negative and positive outcomes.
Patients
The elderly population varies with regard to their knowledge and understanding of drug-related information. At one end of the spectrum are elderly patients who are extremely knowledgeable about their health and their medica-
|
12 |
This section is based on the workshop presentations by Dr. Stephen Pauker and Dr. Jeffrey Halter. |
tions. Pharmaceutical advertisements, direct mail information, and the growth of consumer health information and the Internet all assist patients who want to be well informed and want to discuss this information with their health care professional. Addressing the questions of well-informed patients raises a number of issues including the need for high-quality data and an increased length of time for patient-health professional interaction.
Toward the other end of the spectrum are those older persons who may have decreased cognitive function primarily related to the speed with which they process information (Park and Halter, In press). Older patients may have less working memory capacity, may experience visual and hearing limitations, and may have problems sorting out critical information. Although they generally have more experience with the medical system, they tend to seek out less information when making medical decisions than do younger persons. Drug-related information is often presented using complex terminology, and older patients can get overloaded with the extensive amounts of information that are not provided in an accessible or coherent way. Thus, the challenge is to present drug-related information in a manner that is comprehensible to the entire spectrum of the elderly patient population and that will assist them in making informed decisions about their medical treatment. In addition, attempts to overcome challenges in the elderly population such as impaired vision, poor manual manipulation skills, and memory lapses may be assisted by devising new methods for distributing medications, such as by automating pillboxes or other medication delivery systems.
Cultural differences and disparate ethnic backgrounds between health care providers and elderly patients from minority populations may interfere with the effective transfer of information about drug use and potential side effects. Further, health care providers may not be aware of the community groups and service resources that are available to provide information to patients of different ethnic backgrounds regarding their medication use.
INVESTIGATORS13
There are serious shortfalls in the number of primary care physicians and internists trained in geriatrics, the number of physicians trained in geriatrics, and the number of geriatricians involved in research and education, including geriatric pharmacology research. As with many other fields of medical research, funding is increasingly scarce and more time-consuming to secure, and the economic realities resulting from changes in the health care system are diverting funds away from research training. Moreover, the applied nature of much of
|
13 |
This section is based on the workshop presentations by Drs. Jesse Roth and John Ruffin. |
geriatric pharmacotherapy research puts it outside the mandate of funding agencies such as NIH. In addition, geriatric medicine fellowships have been shortened from 2 or 3 years to 1 year which has resulted in inadequate time for research and an almost exclusive focus on clinical training. Another problem in attracting geriatricians to research endeavors is the need for clinical geriatricians to treat the increasing numbers of elderly patients.
Thus, there is a need to develop mechanisms for attracting and retaining researchers in geriatrics. There are many decision points along a typical career path that may be addressed to reach this goal. First, it is important to attract young people who are in college or recently graduated. New approaches suggested by the workshop speakers included a 1- or 2-year postbaccalaureate program that would provide research assistant positions in geriatric medicine programs linked to pharmacology and clinical therapeutics. Such a postbaccalaureate program offered by schools of medicine or pharmacy could provide exposure to research and clinical activities and to a series of role models including geriatric physicians, clinical pharmacists, and investigators evaluating drugs used with the elderly. The predoctoral Intramural Research Training Award fellowship at NIH was suggested as a model for a postbaccalaureate program in geriatric pharmacology and clinical therapeutics. The latter program would include schools of pharmacy and pharmacy clinicians. The post-baccalaureate program, in addition to providing inspiration and role models for nascent researchers, would also provide much needed assistance to their mentors, young investigators in the field.
The beginning years of the research track are often difficult due to an increasing gap between the availability of initial funding and the assurance of long-term funding. As originally conceived, there was continuing support from fellowship training to first awards to independent grant support. However, the gap has widened between fellowship training and independent support. This issue needs to be addressed in order to assure continuity of support for young investigators. Loan-forgiveness programs could be developed modeled on the NIH loan-forgiveness program for researchers in AIDS. Stipends that are competitive with salaries for people with similar experience are needed. Potential sources for such stipends include the FDA, the Department of Veterans Affairs, the Department of Defense, pharmaceutical companies (models include the programs sponsored by Merck in partnership with the American Federation for Aging Research or the program sponsored by Pfizer in partnership with the American Geriatrics Society), foundations (e.g., the Hartford and Brookdale Foundation programs), or insurance companies. Another potential mechanism is the NIH R03 grant, a one-time research award available to young investigators so they can garner the preliminary data needed to apply for more definitive funding such as an NIH First Independent Research Support and Transition Award (R29) or an NIH Independent Investigator Award (R01). It is equally important to retain midcareer professionals in this field. Mechanisms for support
at this stage of the career include merit awards at the midcareer level and research sabbaticals to retrain midcareer geriatricians in research methodologies.
Recruiting minority students into the field of geriatrics, and specifically geriatric pharmacology and clinical therapeutics, is of importance. Collaborations and true partnerships are needed between minority institutions (e.g., historically black colleges and universities) and academic health sciences centers to provide minority students with extensive research training in this field. The National Institute of General Medical Sciences and the NIH Office of Research on Minority Health have initiated model programs to build these partnerships through an M.S.–Ph.D. program. Students at minority institutions who are accepted into a master's program at the minority institution are simultaneously accepted into the Ph.D. program at the affiliated academic health sciences center. The student can choose his or her research subject from either institution and have research mentors at both. Programs that are truly collaborative will benefit the entire community and will increase the number and diversity of motivated, well-trained investigators.
SUMMARY OF THE WORKSHOP14
The topics presented in this workshop fall into two main categories: approaches to research issues and the resources needed to carry out research. The research issues that need to be addressed in this field are numerous and can overwhelm the resources available for investigator-initiated research. It is crucial to overcome the traditional linear way of thinking about sciences moving exclusively from the laboratory bench to the bedside and instead recognize that research ideas need to be exchanged between the laboratory, clinical, and social sciences. Future research should emphasize interdisciplinary efforts and should not overlook the role of the social sciences in studying pharmacotherapy in elderly populations. The broad scope of important research questions will have to be addressed by encompassing a range of methodologies including observational as well as traditional experimental studies.
Ensuring adequate, sustained research funding is of critical importance —without that, it will be impossible to pursue answers to the research questions identified for this field. As discussed throughout the workshop, there are a number of innovative methods that could be implemented to increase recruitment of minority elderly populations in clinical trials. In addition, the maintenance of professional career paths will require new and expanded approaches and funding mechanisms. Finally, the changes taking place in the health care system will continue to present challenges and will require a reassessment of the optimal way to answer the numerous questions on pharmacokinetics and drug interactions in elderly populations.
|
14 |
This section is based on the summary presentation by Dr. Marcus Reidenberg. |
REFERENCES
Anglade P, Tsuji S, Javoy-Agid F, Agid Y, Hirsch EC. 1995. Plasticity of nerve afferents to nigrostriatal neurons in Parkinson 's disease. Annals of Neurology 37(2):265–272.
Benet LZ, Kroetz DL, Sheiner LB. 1996. In: Hardman JG, Limbird LE, Molinoff PB, Ruddon RW, Gilman AG, eds. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 9th edition. New York: McGraw-Hill.
Blendon RJ, Scheck AC, Donelan K, Hill CA, Smith M, Beatrice D, Altman D. 1995. How white and African Americans view their health and social problems: Different experiences, different expectations. Journal of the American Medical Association273(4):341–346.
Brown DR, Ahmed F, Gary LE, Milburn NG. 1995. Major depression in a community sample of African Americans. American Journal of Psychiatry 152(3):373–378.
Cauley JA, Gutai JP, Glynn NW, Paternostro-Bayles M, Cottington E, Kuller LH. 1994. Serum estrone concentrations and coronary artery disease in postmenopausal women. Arteriosclerosis and Thrombosis 14(1):14–18.
Cauley JA, Seeley DG, Ensrud K, Ettinger B, Black D, Cummings SR. 1995. Estrogen replacement therapy and fractures in older women. Study of Osteoporotic Fractures Research Group. Annals of Internal Medicine122(1):9–16.
Clarkston WK, Pantano MM, Morley JE, Horowitz M, Littlefield JM, Burton FR. 1997. Evidence for the anorexia of aging: Gastrointestinal transit and hunger in healthy elderly vs. young adults. American Journal of Physiology 272(1 Pt 2):R243–R248.
Craft N, Schwartz JB. 1995. Effects of age on intrinsic heart rate, heart rate variability, and AV conduction in healthy humans. American Journal of Physiology 268:H1441– H1452.
DeFelice SL. 1991. Feeding the nutraceutical revolution. Pharmaceutical Executive March:78–84.
Dubler NN. 1993. Inclusion of elderly individuals in clinical trials: Ethical issues . In: Wenger NK, ed. Inclusion of Elderly Individuals in Clinical Trials: Cardiovascular Disease and Cardiovascular Therapy as a Model. Kansas City, MO: Marion Merrell Dow, Inc. Pp. 51–57.
FDA (Food and Drug Administration). 1989. Guideline for the Study of Drugs Likely to Be Used in the Elderly. Rockville, MD: FDA Center for Drug Evaluation and Research.
Fillenbaum GG, Hanlon JT, Corder EH, Ziqubu-Page T, Wall WE, Brock D. 1993. Prescription and nonprescription drug use among black and white community-residing elderly. American Journal of Public Health 83(11):1577–1582.
Geriatrics Newsletter. 1996. Facts: Vitamin and mineral supplement use among the elderly. Geriatrics Newsletter: Nutrition 5(6).
Gurwitz JH. 1993. Food and Drug Administration guideline for the study of drugs in elderly patients: An investigator and clinician perspective. In: Wenger NK, ed. Inclusion of Elderly Individuals in Clinical Trials: Cardiovascular Disease and Cardiovascular Therapy as a Model. Kansas City, MO: Marion Merrell Dow, Inc. Pp. 205–212.
Gurwitz JH, Avorn J. 1991. The ambiguous relation between aging and adverse drug reactions. Annals of Internal Medicine 114(11):956–966.
Gurwitz JH, Col NF, Avorn J. 1992. The exclusion of the elderly and women from clinical trials in acute myocardial infarction. Journal of the American Medical Association 268(11):1417–1422.
Harris T. 1993. How might heterogeneity in the older population increase the risk of J-shaped curves in clinical trials. In: Wenger NK. Inclusion of Elderly Individuals in Clinical Trials: Cardiovascular Disease and Cardiovascular Therapy as a Model. Kansas City, MO: Marion Merrell Dow, Inc. Pp. 25–38.
Isselbacher KJ, Braunwald E, Wilson JD, Martin JB, Fauci AS, Kasper DL, eds. 1994. Harrison's Principles of Internal Medicine. 13th edition. New York: McGraw-Hill.
Jamerson K. 1993. Prevalence of complications and response to different treatments of hypertension in African Americans and white Americans in the U.S. Clinical and Experimental Hypertension 15(6):979–995.
Johnson JA, Bootman JL. 1995. Drug-related morbidity and mortality: A cost-of-illness model. Archives of Internal Medicine 155:1949–1956.
Kaiser FE, Morley JE. 1994.Gonadotropins, testosterone, and the aging male. Neurobiology of Aging 15:559–563.
Katz IR, Alexopoulos GS. 1996. Concensus update conference: Diagnosis and treatment of depression in late life. American Journal of Geriatric Psychiatry4(Suppl 1):S1– S95.
King G, Williams DR. 1995. Race and health: A multidimensional approach to African-American health. In: Amick BC, Levine S, Tarlov AR, Walsh DC, eds. Society and Health. New York: Oxford University Press.
Lakatta EG. 1993. Cardiovascular regulatory mechanisms in advanced age. Physiological Reviews 73(2):413–467.
Lakatta EG, Mitchell JH, Pomerance A, Rowe GG. 1987. Human aging: Changes in structure and function. Journal of the American College of Cardiology 10(2 Suppl A):42–47.
Lakatta EG, Cohen JD, Fleg JL, Frohlich ED, Gradman AH. 1993. Hypertension in the elderly: Age- and disease-related complications and therapeutic implications. Cardiovascular Drugs and Therapy 7(4):643–653.
Lee M. 1996. Drugs and the elderly: Do you know the risks? American Journal of Nursing 96(7):25–31.
Leo RJ. 1996. Movement disorders associated with the serotonin selective reuptake inhibitors. Journal of Clinical Psychiatry 57(10):449–454.
Long SH. 1994. Prescription drugs and the elderly: Issues and options. Health Affairs 13(2):157–174.
Mark DB, Hlatky MA, Califf RM, Naylor CD, Lee KL, Armstrong PW, Barbash G, White H, Simoons ML, Nelson CL, Clapp-Channing N, Knight JH, Harrell FE, Simes J, Topol EJ. 1995. Cost-effectiveness of thrombolytic therapy with tissue plasminogen activator as compared with streptokinase for acute myocardial infarction . New England Journal of Medicine 332(21):1418–1424.
Morley JE, Perry HM, Kaiser FE, Kraenzle D, Jensen J, Houston K, Mattammal M, Perry HM Jr. 1993. Effects of testosterone replacement therapy in old hypogonadal males: A preliminary study. Journal of the American Geriatric Society 41(2):149– 152.
OTA (Office of Technology Assessment). 1993. Pharmaceutical R&D: Costs, Risks, and Rewards. Washington, DC: OTA.
Park DC, Halter JB. In press. Cognitive aging research: Implications for medical patients and medical practices. In: Processing of Medical Information in Aging Patients: Cognitive and Human Factors Perspective. Mahway, NJ: Lawrence Erlbaum, Inc.
Pollock BG. 1996. Clinical relevance of pharmacogenetic variations in drug metabolism in the elderly. Drug Information Journal 30:669–674.
Pollock BG, Mulsant BH. 1995. Antipsychotics in older patients: A safety perspective. Drugs and Aging 6:312–323.
Ruegg RG, Zisook S, Swerdlow NR. 1988. Depression in the aged: An overview. Psychiatric Clinics of North America 11(1):83–99.
Salzman C. 1993. Pharmacologic treatment of depression in the elderly. Journal of Clinical Psychiatry 54(Suppl):S23–S28.
Scharf S, Christophidis N. 1993. Prescribing for the elderly: Relevance of pharmacokinetics and pharmacodynamics . Medical Journal of Australia 158:395–402.
SHEP Cooperative Research Group. 1991. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Journal of the American Medical Association 265(24):3255–3264.
Shimokata H, Andres R, Coon PJ, Elahi D, Muller DC, Tobin JD. 1989. Studies in the distribution of body fat. II. Longitudinal effects of change in weight. International Journal of Obesity 13(4):455–464.
Stewart RB. 1993. Advances in pharmacotherapy: Depression in the elderly: Issues and advances in treatment. Journal of Clinical Pharmacy and Therapeutics 18(4):243– 253.
Stolarek I, Scott PJ, Caird FI. 1991. Physiological changes due to age. Implications for cardiovascular drug therapy. Drugs and Aging 1(6):467–476.
Wenger NK, ed. 1993. Inclusion of Elderly Individuals in Clinical Trials: Cardiovascular Disease and Cardiovascular Therapy as a Model. Kansas City, MO: Marion Merrell Dow, Inc.
White M, Roden R, Minobe W, Khan MF, Larrabee P, Wollmering M, Port JD, Anderson F, Campbell D, Feldman AM, et al. 1994. Age-related changes in beta-adrenergic neuroeffector systems in the human heart. Circulation 90(3):1225–1238.