CHAPTER 4
Public Policies
This chapter summarizes the current policy status of children in immigrant families and places this contemporary portrait in the context of previous immigration and social welfare policies that have determined their access to health and social services over time. It analyzes new data, collected for the committee, on the use of benefits by immigrant families prior to welfare reform. The chapter then provides information about health care for children in immigrant families. It examines patterns of health insurance coverage, access to and use of health services, and barriers to access.
It is beyond the scope of this report to do more than touch on the highlights of U.S. immigration history (see also Barkan, 1996; Bodnar, 1985; Daniels, 1990; Hing, 1993; Kraut, 1982; National Research Council, 1997), let alone social welfare history. Nevertheless, it is important to have some understanding of earlier practices and policies that have, by design, brought foreign-born children to the United States and provided for them once they arrived.
PROVISION OF PUBLIC BENEFITS
Current Eligibility
The most important policies affecting immigrants after arrival in the United States have been the fairly generous rules that have governed access by legal immigrants to mainstream public benefit programs, such as income support (formerly Aid to Families with Dependent Children, AFDC), health and nutrition benefits, social services, and public education. Following several years of intense national debate over the costs of immigration, particularly over the use of public benefits by immigrants, the 104th Congress enacted the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (hereafter referred to as welfare reform). This law, among other changes, fundamentally altered the legal structure for providing these public benefits to immigrants, adults and children alike.1 The Balanced Budget Act of 1997 substantially reversed several major provisions of welfare reform, restoring roughly half of the $23 billion ($11.4 billion) in federal savings that were expected to result from the provisions targeted to immigrants (Congressional Budget Office, 1997). And, as of this writing, efforts to restore benefits to immigrants are ongoing at the federal level.
The law's impact on immigrant children derives in large part from the programmatic reach of new restrictions on immigrants' eligibility for public benefits, which encompass the benefit programs of Medicaid, Supplemental Security Income (SSI), the Food Stamp Program,2 and noncash services (such as child care) delivered under Temporary Assistance to Needy Families (TANF, for-
merly Aid to Families with Dependent Children). Not only have immigrant children been direct beneficiaries of many of these programs, but also many of those who did not receive benefits themselves live in families in which a family member was eligible for and received benefits. For example, children constituted an estimated 17 percent of noncitizens losing food stamps, but almost two-thirds (64 percent) of households headed by a noncitizen that received food stamps also included children (Smolkin et al., 1996). To the extent that overall family resources for meeting basic needs are reduced, children in immigrant families will be likely to feel the impacts. These concerns about the possible negative effects of the policy changes on children in immigrant families have been met by alternative views that emphasize possible deterrent effects of the changes on future immigration and on immigrants' interest in and ability to remain in the United States.
Five shifts in public policy introduced by welfare reform are particularly significant for immigrant children. (Tables 4-1 and 4-2 summarize the major changes in eligibility for benefits that have arisen from this recent legislation.) First, the law draws a new line between legal immigrants and citizens in determining eligibility for public benefits; such a line was formerly drawn between illegal and legal immigrants. Prior to welfare reform, legal immigrants were eligible for public benefits on essentially the same terms as U.S.-born citizens (Fix and Zimmerman, 1995).3 Currently, most immigrants (except for refugees) who are in the United States legally are barred from eligibility for food stamps,
TABLE 4-1 Program Eligibility Prior to Welfare Reform
|
|
Legal Immigrants (Permanent Residents) |
Refugees / Asylees |
Undocumented Immigrants (Illegal Immigrants) |
|
Food Stamps |
Income of sponsor deemed for 3-5 years after entry |
Same eligibility rules as citizens. |
Ineligible. |
|
WIC |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
No bars to eligibility. |
|
School Lunch |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
Eligible. |
|
SSI |
Income of sponsor deemed for 3-5 years after entry |
Same eligibility rules as citizens. |
Ineligible. |
|
MEDICAID |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
Eligible for emergency services only. |
|
Title XX Social Services |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
Eligible. |
|
AFDC |
Income of sponsor deemed for 3-5 years after entry |
Same eligibility rules as citizens. |
Ineligible. |
|
State and Local Benefits |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
Eligibility requirements varied by state. |
|
Head Start |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
No bars to eligibility. |
|
Maternal and Child Health |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
No bars to eligibility. |
|
Child Care Block Grant |
Same eligibility rules as citizens. |
Same eligibility rules as citizens. |
No bars to eligibility. |
and immigrants who arrived after August 22, 1996, are barred from a range of other federal means-tested benefits, including income assistance (TANF) and Medicaid for their first five years in the country.
Noncitizens' eligibility for SSI, which was restricted under welfare reform, was restored in the Balanced Budget Agreement of 1997. The restoration was limited, however, to elderly and disabled immigrants who were receiving SSI benefits at the time welfare reform was enacted or who were in the United States on August 22, 1996, and who later become disabled. Future immigrants will be barred—a change that will affect immigrant children largely indirectly, through a loss of benefits to adult family members who constitute the major share of immigrants receiving SSI.
In addition, many of the benefits for which undocumented children were previously eligible are likely to be withdrawn. This includes the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), most services provided under the Title XX Social Services Block Grant, and Head Start. Undocumented children retain their eligibility for emergency Medicaid, public immunization programs, and the school lunch program.
The place of the recently enacted State Children's Health Insurance Program (SCHIP) in this reformulation of eligibility remains unclear, although it appears that it will be considered a federal means-tested program and so will follow the rules that apply to Medicaid. This program, enacted as part of the Balanced Budget Act of 1997, provides funds to states to enable them to initiate and expand the provision of child health insurance to uninsured, low-income children under age 19. States may spend the new funds in one of three major ways: to extend Medicaid coverage to additional children, to support a separate state child health insurance program, or to do a combination of the two. States may also spend 10 percent of the funds for outreach activities, administrative costs, or direct purchase or provision of health services to children.
Within this overall structure, states have broad discretion in fashioning their programs with respect to specific issues such as eligibility, benefits, and cost sharing (see English, 1998; Institute of Medicine, 1998). States are still required, however, to provide
TABLE 4-2 Post-Welfare Reform Program Eligibility
|
|
Legal Immigrants (Permanent Residents) Arriving before August 23, 1996 |
Legal Immigrants (Permanent Residents) Arriving after August 23, 1996 |
Refugees / Asylees |
Undocumented Immigrants (Illegal Immigrants) |
|
Food Stamps (Federal) |
Ineligible.a |
Ineligible. |
Eligible, time limit is 5 years after admission |
Ineligible. |
|
Food Stamps (State) |
Eligibility varies by state. |
Eligibility varies by state. |
State option to provide benefits after refugees have been in the U.S. more than 5 years |
Ineligible. |
|
WIC |
Eligible. |
Eligible. |
Eligible. |
Eligibility varies by state. |
|
School Lunch |
Eligible. |
Eligible. |
Eligible. |
Eligible. |
|
SSI |
Legal aliens who were receiving SSI benefits and legal aliens in the country before August 22, 1996 who will become disable will continue to be eligible |
Ineligible with certain exceptions |
Eligible for 7 years after entry |
Ineligible. |
|
Medicaid |
State option. |
Barred for first 5 years; state option afterwards |
Eligible for 7 years after entry |
Ineligible. |
legal immigrants with some health and social service programs, such as those delivered under the Community Health Services Program, the Migrant Health Program, services delivered under the Public Health Services Act, and the Maternal and Child Health Block Grant, many of which are extremely important to immigrant families. Furthermore, the 10 percent funds for outreach and direct provision of health services included as part of SCHIP may presumably be used for services, such as migrant health centers, that immigrant families have traditionally used.
Second, refugees arriving after August 22, 1996, will be eligible for SSI and Medicaid for seven years and for TANF and food stamp benefits for five years following their arrival. This change represents a significant departure in refugee resettlement policy by imposing time limits on benefits, which were previously unrestricted. In addition, refugees who were here prior to welfare reform are also subject to the five-year limitation on food stamp benefits. About 10 percent of immigrants in any given year are refugees (Fix and Passel, 1994), but they comprise a substantial proportion of some immigrant groups, such as Cubans, Eastern Europeans, and Southeast Asians.
Third, the locus of many decisions affecting immigrant children's eligibility for benefits has shifted from the federal government to the states. States will be faced with an intricate array of eligibility requirements and sponsorship rules. For example, states are in the process of determining current immigrants' eligibility for such major benefits as income assistance and health insurance (the new federal restrictions apply largely to future immigrants). To date, none of the major immigrant-receiving states (California, Florida, Illinois, New York, and Texas) has limited current legal immigrants' access to TANF, Medicaid, or Title XX block grant programs. States are, however, showing wide variation in their decisions about whether to replace lost federal funds with state-funded programs for immigrants arriving after the enactment of welfare reform.
This devolution of responsibility for immigrant policy is likely to result in substantial state and even within-state variation in the benefits that both legal and undocumented immigrant children receive. For example, although California has decided to eliminate undocumented children from WIC, other states such as New
York have not. Furthermore, some states such as Maryland and New York have decided to use state funds to provide food assistance to immigrant children, but not to adults. In New York, these funds are provided as part of a cooperative state-county program. As a result, noncitizen children, youth, elderly, and disabled food stamp recipients in New York City have retained benefits, but their counterparts in other New York counties (e.g., Erie County) have not.
Fourth, new mandatory federal reporting requirements compel state agencies that administer federal housing, SSI, and TANF programs to furnish the U.S. Immigration and Naturalization Service (INS) four times each year with names, addresses, and other qualifying information on any immigrants known to be unlawfully in the United States. Some are concerned that enactment of this new responsibility by agencies that serve immigrant children will act as a disincentive for undocumented parents of citizen and legal, noncitizen children to seek aid for which these children are eligible and from which they could benefit. However, this remains an open question.
Fifth, the requirement for verification of immigration status has been expanded to apply to all ''federal public benefits," the definition of which remains to be determined but could be quite broad. Likely to be included, for example, is Head Start, maternal and child health programs, the Child Care and Development Block Grant, and other programs that have benefited immigrant children. Children who apply to enroll in these programs will now be required to verify their immigration status, which could create a disincentive to enrollment, particularly for children whose parents are undocumented. In addition, the INS has recently promulgated long and complex new regulations that set out the new verification requirements for federal programs (Federal Register, November 17, 1997:61345-61416) and will be providing requirements for verification in state and local benefit programs. Complexity could give rise to confusion among implementers and, accordingly, inconsistent service delivery.
In sum, children in immigrant families, including those who have entered and are residing in the United States legally, now face major new restrictions and constraints on eligibility for benefits ranging from income supports to nutrition and health cover-
age. Their access to these benefits will now be conditioned by their date of arrival in the United States, entry status, state of residency, and progress through the naturalization process. This represents a marked shift in the nation's policies for immigrant children.
Access Prior to Welfare Reform
Throughout America's history, immigrants have had a profound effect on the composition of the country's population and have presented daunting social and economic challenges to successive American generations. During the last century, federal immigration or admissions policies have played a deliberate role in shaping the number and characteristics of foreign-born people admitted to the United States. These policies have been inclusionary by both historical and international standards (Melville, 1995), as well as comprehensive and explicit in their intent and rationale (for more information on the history of U.S. immigration, see National Research Council, 1997). More recently, they have been accompanied by policies that focus on the control of illegal immigration, including intensive border enforcement, employer sanctions, and verification and reporting requirements in the workplace and in social service agencies.
Characteristics of the current wave of immigrants have been shaped to a large extent by: (1) the 1965 amendments to the Immigration and Nationality Act, which established family reunification as a central basis for immigration4 and removed the numerical cap on the immigration of immediate relatives of U.S. citizens (a priority that was reasserted by the 1990 Immigration Act); (2) growth in humanitarian admissions fostered by the Refugee Act of 1980, which also established a program for settling and
assisting refugees; (3) the Immigration Reform and Control Act (IRCA) of 1986, which established inclusionary strategies, such as the legalization of 2.7 million formerly illegal immigrants, as well as exclusionary strategies to control illegal immigration; (4) the Immigration Act of 1990, with provisions for doubling the visas available for highly skilled immigrants and their families from 58,000 to 140,000 per year, authorizing the creation of a new category of "diversity immigrants" who would be admitted from countries that had sent comparatively few immigrants to the United States historically, and opening a significant new door to safe refuge in the United States by creating a temporary protected status; and (5) the Illegal Immigrant Reform and Immigrant Responsibility Act of 1996, which requires that sponsors of legal immigrants have incomes that exceed 125 percent of the poverty line, after taking into account the sponsor, his or her family, and the arriving immigrant and family members accompanying the arriving immigrant. The overall impact of these policies has been, thus far, to increase the number and share of immigrants from developing countries, notably Mexico, Southeast Asia, and Central America, many of whom have low labor market skills relative to the U.S.-born population (National Research Council, 1997).
In contrast to these relatively unrestricted, comprehensive, and explicit immigration policies, the United States has had no explicit immigrant policy guiding the settlement and orientation of immigrants, or determining the nature and amount of public benefits available to immigrants after arrival (Fix and Passel, 1994; Simon, 1989); the exception is resettlement policies focused on refugees. Instead, immigrants have experienced varied eligibility criteria in the context of specific legislation regarding public benefits. Different immigrant groups have had very different access to resources depending on the array of private, philanthropic, and government programs and benefits available to them at their time and place of arrival. The degree to which private agencies and federal, state, and local governments have shouldered or shared primary responsibility for providing resources needed by children in immigrant families to ensure their healthy development has also changed over time.
Private Sources of Assistance
A century ago, health care and other assistance for immigrants was provided mainly by private charities and self-help benevolent fraternal organizations. In fact, prior to the 1930s, impoverished children in need of medical services, immigrant and citizen alike, received them from health care facilities affiliated with religious institutions, such as church-affiliated hospitals, or from physicians employed by private charities or ethnic lodges and labor unions to which workers paid dues. Almshouses, supported all or in part by public funds, were available only to the destitute, including immigrants (Kraut, 1994).
Children who received medical attention upon arrival on Ellis Island or at any other immigration depot received no further attention from the federal government once they left the facility and were admitted to the United States. No federal programs existed for poor and needy children. Children's health, especially impoverished children in immigrant families, was the responsibility of state and municipal governments and private charity in the decades prior to the New Deal.
Children who attended school had the greatest access to health education and health care early in the 20th century. Initially, the public school teacher bore the main responsibility of vigilance between annual physician examinations, alerting the school doctors to suspicious signs of ill health among students. Increasingly, however, the school nurse became crucial not only in detecting disease but also in health education, including educating parents about health care for their children. School nurses treated minor ailments, thus preventing loss of instruction time, and provided health care outreach to parents.
Aside from particular ailments or disabilities, poor diet, improper personal hygiene, and insufficient health and exercise were among the most common causes of disease and disability in immigrant schoolchildren (Baker, 1939; Kraut, 1994; Riis, 1890; Spargo, 1906). In response to the problem of hunger, some reformers advocated a program of low-cost or free school lunches for poor schoolchildren. In New York, school lunches were provided in 17 schools by 1914, 11 of those in immigrant neighborhoods, with the support of philanthropists such as Andrew
Carnegie and Solomon Guggenheim. In 1919, the New York City Board of Education was funded to assume responsibility for serving school lunches—a precursor to both the federal school breakfast and lunch programs and to the federal Food Stamp Program.
Children and adolescents who were not in school presented a complex health care problem. Those working in sweatshops or doing piece work at home were not under the surveillance of teachers, school doctors, or school nurses. Yet the health of working children and youth was threatened by some of the same occupational hazards that threatened the health and shortened the lives of their elders, including such occupational diseases as lead poisoning, phosphorous necrosis, and silicosis (Gold, 1930; Kraut, 1994; Rosner and Markowitz, 1987, 1991). Children and youth living and working in congested environments were susceptible, as were their parents and older coworkers, to tuberculosis. Deprived of fresh air and healthy exercise, normal physical development was also curbed (Kraut, 1994; Stella, 1904, 1908).
In urban areas, health care for working children and adolescents was available at dispensaries or from visiting nurses financed by private charities or urban governments. However, immigrant children and youth often received care from the fraternal lodges to which they or their parents belonged. For example, Germans created and joined the Arbeiter-Kranken-und-Starbe Kasse der Vereinigten Staaten von Amerika (the Workingman's Sick and Death Benefit Fund of the United States), Eastern European Jews created and joined the Landsmannschafn (regionally based fraternal organizations), and Cuban cigar makers contributed part of their wages to the formation of clinicas, providing access to health insurance or services (Davis, 1921; Kalet, 1916; Kraut, 1995; Mormino and Pozzetta, 1987). In addition, visiting nurses and health educators in settlement houses, such as Lillian Wald's Henry Street Settlement and Jane Addams's Hull House, sought to bring information about health and access to basic health care to America's newest resident children and families.
Over time, however, the cooperative traditions many immigrants brought from their home countries eroded with assimilation; more recent immigrants often did not have such resources. Moreover, as the costs of health care escalated, the resources of even the most successful benevolent associations and ethnic la-
bor unions became increasingly inadequate to the task of paying for the cost of care.
Public Assumption of Responsibility
Although the federal government assumed responsibility for inspecting the health of immigrants at the border after 1890, it was not until the 1930s that it began to provide direct financial assistance to the poor, including immigrant families. Prior to this time, however, the federal government had assumed some responsibility for gathering data on children. In 1912, the Children's Bureau was established as a fact-finding agency and was allocated $25,640 to "investigate and report upon all matters pertaining to the welfare of children and child life among all classes of our people." Staffed largely by social workers and educators of a progressive bent, the Children's Bureau through its investigators reported data on child poverty, child health, and child labor, in particular, which in time-provided the justifications for federal programmatic involvement in these arenas.
The New Deal marked the first major initiative by the federal government to establish programs aimed at fostering the health of Americans, especially the poorest. Driven largely by public health concerns, funds were authorized for medical and nursing care; emergency dental work; the construction of hospitals, health clinics, and sewage plants; maternal and child care; care for physically disabled children; and the promotion of state and local public health agencies. The basic architecture of a system for distributing funds for health care, while recognizing special needs, including those of children, was well established by the late 1930s.
Since that time, punctuated by a major expansion of direct federal responsibility for the care of the country's poor in the 1960s, legal immigrant as well as U.S.-born poor children have benefited increasingly from federal assistance programs, the largest of which have been Medicaid, food stamps, SSI, and Aid to Families with Dependent Children (AFDC). Programs focused on children, such as WIC, childhood immunization programs, emergency medical services, Head Start, the school lunch and breakfast programs, and Title IV foster care and adoption assistance, have also been of great importance to immigrant children,
including undocumented children who have been eligible for these programs from their inception.
As they have emerged over the past three decades, federal policies regarding immigrants' access to public benefits have incorporated three important features.
The first is the federal government's preemption of state power to determine noncitizens' eligibility for state or federally funded public benefits programs. Prior to 1972, federal statutes controlling state or local public benefit programs contained no eligibility restrictions based on immigration status; they were silent on the matter of immigrant eligibility. In the absence of federal mandates, the states established their own citizenship and alien residency requirements. In the 1970s, however, the federal government began to expressly impose restrictions on immigrant access to public benefits in response to concerns about illegal immigration, paired with concerns about major expansions in the costs of public benefits. Since then, through explicit legislative and regulatory provisions, the federal government has retained the power to establish immigrants' eligibility for federal benefits.
The second feature is the restriction of benefits for illegal and temporary immigrants—but not, for the most part, for legal permanent residents. Through the late 1970s, restrictions on immigrants' use of benefits were limited to undocumented and to temporary immigrants (students, tourists, and temporary workers, for example). Illegal immigrants were barred from AFDC, SSI, food stamps, and full Medicaid benefits, retaining their access to emergency services funded under Medicaid. In the late 1970s, concerns began to emerge that some recently arrived legal immigrants were abusing the welfare system. These concerns led to the imposition of new requirements that effectively withheld food stamp, SSI, and AFDC benefits for three years after the arrival of some immigrants who were not refugees.
This withholding of benefits was accomplished by a policy called "deeming." Under deeming the income of an immigrant's sponsor is deemed to be available to the immigrant for purposes of qualifying for means-tested benefit programs. When the incomes of sponsors and immigrants are combined, it is typically the case that they are so high that they disqualify the immigrant from receiving benefits. In addition, poor immigrants typically
will not be granted a visa unless their sponsors sign an affidavit of support, which is a pledge by the sponsor to (1) support the sponsored immigrant and (2) reimburse the government for benefits provided during the period the affidavit is in effect.
Affidavits of support have not been enforced, however, because they have been determined by the courts to be a moral and not a legal obligation. In the past, the affidavit of support has been in effect during the period of deeming—typically three years. Hence, the sponsor's obligation lapsed as the government's began. The argument in favor of sponsor deeming and requiring an affidavit of support is that the government can admit immigrants who are poor at the time of entry without worrying excessively about the public fiscal burdens. The argument opposing the new laws is that they erect multiple overlapping barriers to benefit use, including affidavits of support that are in effect until the immigrant naturalizes, bars to public benefits until naturalization, and deeming in public benefit programs.
A third feature of immigrant policy in the modern era is the preferred treatment of refugees, who have experienced comparatively unrestricted access to benefits since the end of World War II. Refugees, who now represent between 10 and 15 percent of legally admitted immigrants, have been eligible for state and federal public benefit programs on the same terms as citizens from the date of their arrival. Although deeming in AFDC, SSI, and food stamps has been applied to legal permanent residents, it has not been extended to refugees (who are not sponsored).
In sum, the majority of children in immigrant families reside in the United States legally and in accord with immigration policies that have repeatedly identified family reunification as a central and explicit goal of immigration. These children now face a complex and newly redefined array of eligibility criteria for public benefits that, as of 1996, categorically exclude many of them from coverage and leave many others subject to the decisions of state governments. This new landscape of immigrant policies for children, although not unprecedented in the modern era,5 represents a major departure from the policies of the last 25 years.
USE OF PUBLIC BENEFITS
National attention and research have focused on the use of public benefits by immigrant adults and households (Bean et al., 1997; Blau, 1984; Borjas and Hilton, 1996; Borjas and Trejo, 1991; Fix and Passel, 1994; Jensen, 1988; Simon and Akbari, 1996; Tienda and Jensen, 1986). The literature on this issue has yielded mixed results. Studies that have focused on cash benefits (e.g., AFDC, SSI, other welfare) have generally reported that immigrants are more likely to receive various forms of public assistance than the U.S.-born, in large part because immigrants are more likely to be poor and thus eligible for benefits. Among the U.S.-born and immigrants with similar socioeconomic and demographic characteristics, immigrants are less likely to receive welfare from many specific programs. However, the proportion using at least one form of noncash benefit is higher among immigrants than comparable U.S.-born residents. It is important to determine exactly which forms of public assistance immigrants are more likely to receive, and whether this is a function of their immigrant status per se or of their disadvantaged socioeconomic and demographic circumstances independent of their immigration status.
Almost no research has examined these issues from the perspective of children (but see Currie, 1997, for an exception), even though they constitute a large share of the immigrant population and represent a sizeable fraction of the welfare caseload. To fill this gap, the committee had analyses conducted of the Survey of Income and Program Participation (SIPP) (Brandon, 1998) and the Panel Study of Income Dynamics (PSID) (Hofferth, 1998) to provide information about children in families that received public assistance.6 The discussion in this section relies on these analy-
ses and is most appropriately viewed as an initial look at patterns for children in the reliance of their families on public assistance prior to welfare reform, that is, the extent to which children live in families in which at least one person in the household receives benefits from a designated public program.
The analyses conducted for the committee focused on the following public assistance programs for which children in immigrant families or members of their families have been eligible: AFDC, food stamps, Medicaid, SSI, heating assistance, housing assistance, school lunches, and other welfare. The indicator of cash assistance consisted of AFDC, SSI,7 and other welfare (general assistance and miscellaneous state assistance). The indicator of noncash assistance combined Medicaid, food stamps, heating assistance, and housing assistance.
Comparisons focused on differences in receipt by immigrant generation, comparing first-generation (foreign-born) with both second-generation (U.S.-born children of immigrant parents) and third- and later-generations (U.S.-born children of U.S.-born parents), as well as by ethnicity. On one hand, first-generation children experience relatively high poverty rates and therefore might be expected to show higher rates of receipt than later-generation children. On the other hand, all persons born in the United States are eligible to apply for public benefits, and legal immigrants are eligible to apply for more benefit programs than are undocumented immigrants. This would lead us to expect U.S.-born families with U.S.-born children to have the highest likelihood of receipt, followed by U.S.-born children in immigrant families.
Patterns of Receipt by Generation and Ethnicity
Tables 4-3 and 4-4 show the incidence of public assistance participation by immigrant generation and ethnicity for the PSID and SIPP analyses, respectively. It is important to note that these analyses do not statistically exclude the effects of sociodemo-
TABLE 4-3 Percent of Children in Families Receiving Public Assistance by Race, Ethnicity, and Generation in the Panel Study of Income Dynamics: 1992
|
|
AFDC |
SSI |
Other Welfare |
Food Stamps |
Medicaid |
Housing |
Heat |
Cash |
on-Ncash |
Total |
|
First-generation Mexican |
3 |
0 |
7 |
47 |
38 |
17 |
25 |
10 |
59 |
61 |
|
Second-generation Mexican |
5 |
3 |
4 |
26 |
24 |
7 |
10 |
11 |
37 |
38 |
|
Third- and later-generation Mexican |
18 |
5 |
3 |
30 |
26 |
11 |
18 |
23 |
44 |
45 |
|
First-generation Cuban |
4 |
6 |
0 |
22 |
25 |
4 |
2 |
7 |
32 |
32 |
|
Second-generation Cuban |
4 |
8 |
5 |
25 |
37 |
6 |
1 |
16 |
40 |
40 |
|
Third- and later-generation Cuban |
7 |
20 |
0 |
10 |
31 |
5 |
0 |
27 |
35 |
35 |
|
Other Hispanic |
23 |
3 |
5 |
24 |
27 |
11 |
17 |
23 |
29 |
29 |
|
White |
4 |
2 |
1 |
8 |
8 |
2 |
5 |
6 |
14 |
14 |
|
Black |
27 |
6 |
5 |
42 |
37 |
25 |
17 |
34 |
58 |
60 |
|
Other |
5 |
3 |
3 |
14 |
18 |
7 |
0 |
11 |
24 |
27 |
|
Total |
9 |
3 |
2 |
17 |
17 |
8 |
9 |
13 |
26 |
27 |
|
Source: Hofferth (1998). |
||||||||||
graphic, economic, or other differences that characterize these groups.
In general, first-generation immigrant children are more likely than later-generation children to live in families receiving public assistance, and second-generation children are about as likely as third- and later-generation children to live in families receiving public assistance (see the Total rows for the generations, overall, in Tables 4-3 and 4-4). Compared with white children, higher probabilities of receipt of public assistance from specific programs were usually found for Mexican, Cuban, other Hispanic, and Asian children.
In the PSID analyses, which encompassed Mexican-origin, Cuban-origin, and other Hispanic children, the range of those living in families that received at least one form of public assistance among those listed was from 29 to 61 percent. First-generation Mexican-origin children accounted for the 61 percent figure, which dropped to 38 percent in the second generation and 45 percent in the third generation. These children lived in families that were substantally more likely to rely on noncash than on cash benefits. In the SIPP analyses, which encompassed immigrants from a wider range of regions of the world, the range was from 16 to 57 percent. The range for Mexican-origin children was from 44 to 47 percent across the generations, with greater reliance on noncash than on cash benefits for the first and second generations. However, third- and later-generation black children have high rates of receipt as well (59 and 60 percent across all programs in the SIPP and PSID analyses, respectively). Indeed, the gap between third- and later-generation black and white children in receipt of public assistance is greater than that between each of these groups and virtually every immigrant generation group, and it is greater than the differences within the immigrant population.
In general, these analyses correspond to the previous literature on adult immigrant populations, showing higher rates of assistance among immigrants—especially first-generation immigrants—than among U.S.-born families (see Borjas and Hilton, 1996).
Determinants of Receipt of Public Assistance
Having discussed patterns of receipt of public assistance by immigrant generation and ethnicity, it is important to determine whether these patterns are explained by other characteristics of the families, particularly their demographic characteristics and poverty level. In general, the comparatively high rates of public benefit receipt among first-generation families were found to result from greater need—that is, from their disadvantaged socioeconomic and demographic circumstances, not from their immigration status per se. When controls were added for group differences along such dimensions as poverty, marital and health status of the parents, parental education, and number of children in the family, the generational differences either disappeared or were reversed (Brandon, 1998; Hofferth, 1998). In addition, the refugee status of many immigrants from certain countries, such as Cuba and Southeast Asia, is likely to account for higher levels of receipt among these groups.
Among children in families with similar socioeconomic and demographic circumstances, first- and second-generation children as a whole are less likely than third- and later-generation children to receive both cash and noncash benefits. The same is true for Mexican-origin children with similar characteristics: first- and second-generation children are less likely than the third and later generations to receive cash and noncash public assistance. For a wide range of benefits (AFDC, SSI, food stamps, Medicaid, and other welfare), first- and second-generation Mexican-origin children are either no more likely or are less likely than both third- and later-generation white and third- and later-generation Mexican-origin children with similar socioeconomic and demographic characteristics to live in families that receive benefits. Third- and later-generation Mexican children, however, are generally more likely than third-and later-generation white children with the same socioeconomic and demographic characteristics to receive benefits.
The situation is quite different for Asian children in immigrant families. At specific socioeconomic levels, first-generation Asian children are more likely than second-generation children
TABLE 4-4 Percent of Children in Families Receiving Public Assistance by Race, Ethnicity, Country of Origin, and Generation in the Survey of Income and Program Participation: 1986-1992
|
Generation with Ethnicity |
AFDC |
SSI |
Other Welfare |
Food Stamps |
Medicaid |
Housing |
Heat |
Cash |
NonCash |
Total |
|
First generation |
17 |
11 |
1 |
28 |
22 |
10 |
8 |
21 |
35 |
36 |
|
Second generation |
10 |
6 |
1 |
22 |
16 |
7 |
8 |
13 |
28 |
29 |
|
First and second generation |
12 |
7 |
1 |
23 |
17 |
8 |
8 |
15 |
29 |
31 |
|
Third and later generation |
13 |
5 |
1 |
21 |
15 |
8 |
10 |
14 |
27 |
28 |
|
First-generation Mexican |
17 |
4 |
2 |
36 |
24 |
10 |
9 |
20 |
45 |
46 |
|
Second-generation Mexican |
12 |
8 |
1 |
36 |
22 |
10 |
13 |
15 |
43 |
44 |
|
Third- and later-generation Mexican |
24 |
6 |
2 |
40 |
29 |
11 |
19 |
25 |
46 |
47 |
|
Cuban |
3 |
8 |
0 |
22 |
13 |
2 |
4 |
5 |
32 |
32 |
|
First-generation Asian |
27 |
20 |
0 |
31 |
31 |
16 |
7 |
34 |
36 |
39 |
|
Second-generation Asian |
14 |
10 |
0 |
17 |
14 |
7 |
2 |
20 |
20 |
24 |
|
Third- and later-generation Asian |
18 |
6 |
3 |
23 |
7 |
9 |
1 |
25 |
25 |
28 |
|
First-generation Western European |
4 |
0 |
0 |
26 |
10 |
0 |
5 |
4 |
27 |
28 |
|
Second-generation Western European |
7 |
4 |
0 |
13 |
10 |
3 |
4 |
8 |
17 |
18 |
|
Third- and later-generation Western European |
7 |
3 |
1 |
13 |
9 |
6 |
6 |
8 |
18 |
19 |
|
First-generation Eastern European |
4 |
0 |
0 |
15 |
5 |
13 |
9 |
4 |
27 |
27 |
|
Second-generation Eastern European |
3 |
0 |
0 |
5 |
14 |
1 |
3 |
3 |
17 |
17 |
|
Third- and later-generation Eastern European |
4 |
1 |
0 |
9 |
7 |
5 |
7 |
5 |
16 |
16 |
|
Other Hispanic |
26 |
9 |
1 |
38 |
32 |
18 |
12 |
27 |
53 |
57 |
|
White |
7 |
4 |
1 |
14 |
9 |
5 |
6 |
8 |
19 |
19 |
|
Black |
35 |
14 |
2 |
51 |
40 |
23 |
22 |
37 |
58 |
59 |
|
Other |
22 |
7 |
4 |
45 |
37 |
12 |
5 |
27 |
53 |
57 |
|
Total |
13 |
6 |
1 |
21 |
15 |
8 |
8 |
14 |
27 |
28 |
|
Source: Brandon (1998). |
||||||||||
to live in families receiving benefits from these programs, and second-generation children are more likely to receive benefits than third- and later-generation children only for SSI. This pattern in part reflects the refugee status of children from Vietnam, Cambodia, Laos, and Thailand, which allows them automatic and unrestricted eligibility for many public benefits. In 1990, children from these countries accounted for about 27 percent of all first-generation Asian children, but only 7 percent of all second-generation Asian children. Among those with similar socioeconomic and demographic characteristics, Asian children of all generations are more likely to live in families that receive AFDC than third- and later-generation white children.
Many Cuban-origin children in immigrant families are also entitled to refugee benefits and, not surprisingly, their patterns of reliance on public assistance are similar to those of Asian children. Among those with similar demographic and socioeconomic circumstances, first- and second-generation Cuban-origin children are more likely than either third- and later-generation Cuban children or third- and later-generation white children to live in families that receive SSI and food stamps. Comparable proportions of first- and second-generation Cuban-origin children and of third-and later-generation white children with similar demographic and socioeconomic characteristics live in families that receive AFDC, but third- generation Cuban-origin children are more likely than third- and later-generation white children to live in families that receive AFDC.
Among children from Western Europe, first-generation children are no more likely or are less likely than later-generation children in similar demographic and socioeconomic circumstances to live in families receiving public assistance. The pattern for Eastern Europeans is more similar to that of Asians. At specific socioeconomic levels, first-generation children with Eastern European origins are more likely than second-, and third-, and later-generation children with Eastern European origins to live in families receiving other welfare, Medicaid, and housing and heat assistance.
Assessment of Recent Changes
It is premature to assess the effects of the recent changes in policies affecting immigrants' access to public benefits, because many federal and state decisions have yet to be made regarding definitions, eligibility, and implementation of these policies with special relevance to immigrant children, and because the impacts of the reforms are only beginning to be felt. However, given the sizeable numbers of children in immigrant families who will be affected, a full and accurate portrait of the effects of the reforms must include specific attention to the various ways in which these children are affected.
Such an assessment will need to consider: (1) the direct effects on children of their elimination from eligibility for basic benefit programs, ranging from health care and nutrition to social services; (2) the indirect effects on noncitizen and citizen children in immigrant families that are likely to ensue from family members' loss of benefits; and (3) the indirect effects that may arise from such potentially chilling practices as new verification and reporting requirements on immigrant parents' efforts to obtain benefits for their children. It will also be important to monitor the ramifications of the nation's changing policies for local agencies and institutions—formal and informal—that have traditionally provided benefits and services to children in immigrant families. Also of interest are efforts to assess the incentives and disincentives to future immigration of families with children and to return migration on behalf of these families that arise from the reforms.
With regard to direct effects, because so many programs are affected, it will be important to assess outcomes across a wide range of developmental domains. Family- and household-level effects, such as overcrowding, that may arise from diminished resources to dependent family members also warrant attention. Consideration of synergistic effects that arise from interactions among different benefits and programs, as well as cumulative effects over time, will be critical. State variation in outcomes will be especially important to assess, given the high likelihood of growing variation in states' treatment of immigrant children and their families.
Indirect effects may be just as far-reaching as direct effects, given that, as of 1997, more than 7 million citizen children (10 percent of all children) live in families that include noncitizen parents (Fix, 1997). Children of immigrants often have a different immigration status than their parents. In general, they are more likely to be citizens and hence to be entitled to different public benefits than their parents. It is critical to understand how this situation manifests itself in a policy context in which the government is curbing benefits to noncitizens, many of whom, as parents, are responsible for accessing services on behalf of their citizen and noncitizen children.
HEALTH COVERAGE AND ACCESS
All children require access to health services to ensure that preventive services are provided as recommended, acute and chronic conditions are diagnosed and treated in a timely manner, and health and development are adequately monitored so that minor health problems do not escalate into serious and costly medical emergencies. Both health insurance coverage and having a usual source of care facilitate access to health care (Holl et al., 1995; Institute of Medicine, 1998; Lieu et al., 1993; Newacheck et al., 1996; Simpson et al., 1997; U.S. General Accounting Office, 1997).
Little systematic research has examined how immigration and citizenship status are related to health insurance coverage and access to care. This gap in the research literature has been especially acute for children. The committee had analyses conducted of existing national data sets8 to provide descriptive data on health insurance coverage and access to health services by children in immigrant families prior to implementation of both welfare reform and the new State Children's Health Insurance Program (Brown et al., 1998). Much of the discussion in this chapter relies on these analyses and, as such, is most appropriately viewed
as an initial look at an evolving system of health care financing and delivery for children in immigrant families.
Health Care Insurance
Over the past 30 years, the health care of most children in this country has been funded through one of three arrangements: employment-based insurance, public benefits, and charity arrangements. The majority of them receive health coverage through their parents' employer-sponsored health insurance (59 percent of 0- to 17-year-olds in 1995) (Institute of Medicine, 1998, citing Employee Benefit Research Institute, 1997b). 9 They receive care primarily from private physicians and private hospitals or from health maintenance organizations (HMOs). Public-sector financing for children's health care coverage comes primarily from Medicaid, a federally and state-financed program administered by states that pays for health services for children who meet low-income eligibility criteria or categorical requirements, such as being in foster care or being disabled.
In 1995, approximately 1 in 4 children was enrolled in Medicaid (Employee Benefit Research Institute, 1997a). Similarly, Medicaid provides the only source of coverage for about 1 in 4 children in immigrant families (Brown et al., 1998). Medicaid beneficiaries may receive their care from private physicians and private hospitals but, because they often have difficulty finding private providers who accept Medicaid payments, these patients obtain much of their care from public hospitals and clinics and community-based services. In general, children in immigrant families are substantially less likely to use a doctor's office or private clinic as their usual source of care than are other children. Instead, they rely more heavily on public hospitals and community and migrant health centers (Brown et al., 1998).
Since 1987, there has been a decline of 8 percent in the share of children receiving employer-based coverage and an increase of almost 8 percent in Medicaid coverage (Institute of Medicine,
1998, citing Employee Benefit Research Institute, 1997b). This association suggests that some children may have been dropped from or lost private health insurance coverage because they became eligible for Medicaid. Most analysts suspect that some employers and employees have dropped private health insurance to take advantage of expanded eligibility for Medicaid, but the size of the effect is unknown and remains in dispute (Cutler and Gruber, 1996, 1997; Dubay and Kenney, 1997). There is, however, growing evidence that, in response to their increasing costs for health benefits, employers have raised the contributions that employees must make as their share of health insurance premiums, and that these rates have increased faster for family coverage than for individual coverage (Fronstin and Snider, 1996-1997; Kronick and Gilmer, 1997). This factor may have contributed considerably more to the decline in employment-based insurance than did expansions of Medicaid eligibility.
Approximately 14 percent of children do not have any insurance coverage. The great majority of them live in working families, but their parents either work for employers who do not offer insurance, or they perceive the health benefits offered by their employer as unaffordable. Traditionally, uninsured children have received care that is available as charity in emergency rooms, public hospitals, state and local health departments, community and migrant health centers, and other publicly funded health facilities. But many have simply gone without needed care.
Numerous studies have demonstrated that children who have neither private health insurance nor public coverage such as Medicaid have less access to both preventive and acute or chronic health care than insured children (Brown, 1989; Brown et al., 1998; Currie and Gruber, 1996; Currie and Thomas, 1995; Holl et al., 1995; Institute of Medicine, 1998; Lieu et al., 1993; Newacheck, 1992; Newacheck et al., 1996; Stoddard et al., 1994; U.S. General Accounting Office, 1997; Wood et al., 1990). Uninsured children are less likely to have seen a doctor in the past year or to receive required preventive services, such as well-child visits and immunizations, as recommended by the American Academy of Pediatrics (1995). They are also less likely to receive a doctor's care for injuries and common illnesses of childhood, such as acute earaches and asthma, that can have serious consequences if left un-
treated (Overpeck and Kotch, 1995; Stoddard et al., 1994). The differences between being insured and being uninsured in access and use of health care have recently been demonstrated for children in immigrant families, for whom Medicaid eligibility is associated with increases in the probability of having received at least one doctor's visit in the previous year (Currie, 1997).
Patterns of Coverage
First-generation (noncitizen) and second-generation (citizen) children are at a significantly higher risk of being uninsured than are third- and later-generation (citizen) children (see Figure 4-1).10 With increasing time in the United States, measured by immigrant generation within ethnic groups, rates of insurance coverage increase (see also Leclere et al., 1994, comparing recent with older adult immigrants). First-generation (noncitizen) children in every ethnic group are substantially more likely to lack insurance than later-generation (citizen) children, and they are more likely to be uninsured than even third- and later-generation black children, who generally have high rates of uninsurance. Overall, first-generation children are most likely to be uninsured (36 percent), followed by second-generation children (21 percent) and third-generation children (11 percent). Even among children whose parents work full-time, year-round, children in immigrant families are more likely to be uninsured than are third- and later-generation children.
Hispanic children are the most likely to lack health insurance. They have the highest uninsured rates for each generation (rang-
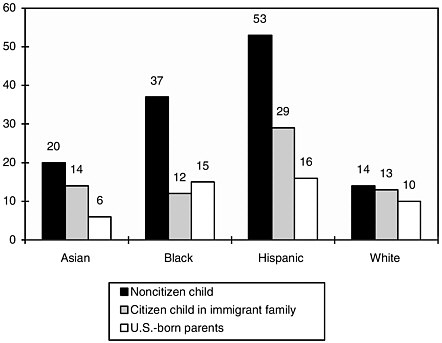
FIGURE 4-1 Percentage of children without health care insurance: 1995. Source: March 1996 Current Population Survey. Brown et al. (1998).
ing from 53 percent for first-generation children to 16 percent for third- and later-generation children) compared with non-Hispanic children. In contrast, by the second generation, Asian children do not differ significantly from third- and later-generation white children in their rates of uninsurance; third- and later-generation Asian children have the lowest uninsured rate of any group, including third- and later-generation white children.
The finding of high uninsurance rates among Hispanic immigrant children compared with immigrant children from other ethnic groups was replicated in analyses that controlled for family structure, parents' education and employment, and family income—that is, among those with similar demographic and socioeconomic circumstances, first-generation Hispanics are more likely to lack health insurance coverage than other first-generation children. Among second-generation children, however, Hispanics, Asians, and whites had quite comparable rates of
uninsurance when they had similar family structure and socioeconomic status. This suggests that these demographic and socioeconomic factors may play a larger role in explaining ethnic differences in insurance coverage among second-generation children than among first-generation children, for whom such factors as legal status, English proficiency, and knowledge of the U.S. health care system and benefits may play important roles as well.
As is true for all children, the cost of health insurance is the main reason for lack of coverage among children in immigrant families, regardless of ethnicity. Beliefs about coverage (e.g., that it is not needed, dissatisfaction with coverage, or lack of belief in health insurance) are not important reasons for lack of coverage for any immigrant group (Brown et al., 1998).
Sources of Coverage
Among insured children in immigrant families, the source of insurance varies by ethnic group and by immigration and citizenship status (see Table 4-5). For every ethnic group (Hispanic, Asian, black, and white), second-generation (citizen) children are more likely to have employment-based coverage than first-generation (noncitizen) children. An even larger share of third- and later-generation (citizen) children have employer-sponsored coverage.
These generational trends, however, camouflage large differences by ethnicity. Hispanic children—whether first- or second-generation—are less likely to receive employment-based coverage than corresponding generations of white, black, and Asian children. It is especially striking that, by the second generation, about two-thirds of Asian, black, and white children and adolescents have employment-based health insurance, compared with only 35 percent of second-generation Hispanic children. Among third-generation children, a substantially lower share of both black and Hispanic children have employment-based insurance than Asian and white children.
Medicaid has compensated for some of these disparities, reducing the risks of uninsurance for some children in immigrant families, despite their participation rates, which are lower than low-income third- and later-generation children. Second-genera-
TABLE 4-5 Children's Health Care Insurance Coverage: 1995
|
|
Uninsured |
Employment-based Insurance |
Medicaid |
Otherc |
Total |
|
All Childrena |
|
|
|
|
|
|
Citizen child with U.S.-born parents |
11% |
66% |
17% |
6% |
100% (N=58,3000,000) |
|
Citizen child in immigrant family |
21% |
52% |
23% |
5% |
100% (N=9,621,939) |
|
Noncitizen child |
36% |
35% |
23% |
6% |
100% (N=2,340,744) |
|
Asianb |
|
|
|
|
|
|
Citizen child with U.S.-born parents |
6% |
69% |
12% |
12% |
100% (N=474,005) |
|
Citizen child in immigrant family |
14% |
66% |
13% |
7% |
100% (N=1,774,134) |
|
Noncitizen child |
20% |
45% |
26% |
9% |
100% (N=607,263) |
|
Blackb |
|
|
|
|
|
|
Citizen child with U.S.-born parents |
15% |
42% |
40% |
4% |
100% (N=10,180,000) |
|
Citizen child in immigrant family |
12% |
69% |
17% |
3% |
100% (N=709,113) |
|
Noncitizen child |
37% |
40% |
17% |
6% |
100% (N=181,155) |
|
Hispanicb |
|
|
|
|
|
|
Citizen child with U.S.-born parents |
16% |
45% |
36% |
3% |
100% (N=3,703,829) |
|
Citizen child in immigrant family |
29% |
35% |
34% |
2% |
100% (N=4,638,045) |
|
Noncitizen child |
53% |
22% |
22% |
3% |
100% (N=1,148796) |
|
Whiteb |
|
|
|
|
|
|
Citizen child with U.S.-born parents |
10% |
74% |
10% |
7% |
100% (N=43,210,000) |
|
Citizen child in immigrant family |
13% |
68% |
12% |
7% |
100% (N=2,465,344) |
|
Noncitizen child |
14% |
53% |
23% |
10% |
100% (N=400,260) |
|
Source: March 1996 Current Population Survey. Brown et al. (1998). a Includes individuals with ''Other race/ethnicity" b "Hispanic" includes all Hispanic persons from the Americas, "Asian," "Black," and "White" do not include any persons of Hispanic heritage. c "Other" includes privately purchased health insurance, Medicare, and other public programs. |
|||||
tion Hispanic children are more likely than any other second-generation group to receive Medicaid. Among first-generation children, however, Hispanic, Asian, and white children enroll in Medicaid at similar levels (ranging from 22 to 26 percent); only first-generation black children enroll at lower rates (17 percent). Among third- and later-generation children, black and Hispanic children enroll in Medicaid at similar and relatively high rates (40 percent and 36 percent, respectively), whereas a much smaller share of Asian (12 percent) and white children (10 percent) rely on Medicaid.
Looking beyond these broad ethnic categories to patterns of insurance coverage among children from specific countries of origin reveals wide variation within ethnic groups. Approximately half of first-generation children from Cuba, Mexico, and Central America are uninsured, probably reflecting the generally low educational attainment that characterizes recent immigrants from these countries, which in turn tends to limit employment to jobs that do not offer health benefits. Those from South America are more likely to have health insurance, although 39 percent are still not covered.
Children in more advantaged families from other sending countries—such as Hong Kong, Japan, Singapore, and Taiwan; Europe; China; and the Philippines, Malaysia, and Indonesia—all rank higher in their rates of insurance coverage than those from Latin American countries. These children have higher rates of employment-based health insurance, which workers with higher levels of educational attainment typically can obtain. In contrast, rates of uninsurance among Korean-origin children are very high (38 percent) and, by the second generation, exceed levels for children in immigrant families from all other sending countries, perhaps as a result of the relatively high rates of self-employment among Korean families.11
First-generation children from Cambodia, Laos, and Vietnam are most likely to be insured, reflecting very high levels of Medic-
aid coverage (64 percent) rather than employment-based health insurance (24 percent). This holds as well for second-generation children in families from these sending countries, despite their parents' relatively low educational levels, high poverty rates, and low participation in the labor force. These children and families from Southeast Asia have been granted refugee status since 1975, which opens the door to relatively generous Medicaid eligibility provisions.
USE OF HEALTH CARE
Given that health insurance facilitates the access of children to care, differences in coverage should be reflected in differential patterns of access to and use of health care. But access to health care services depends on more than health insurance coverage; it also requires that families develop a connection to the health care system for their children—a regular practitioner or place that can provide continuity of care over time and even across family members and serve as a guide to appropriate preventive care and needed specialized services. Having a regular source of care has been found consistently to increase the use of health care services and to enhance referrals to complex care when needed (Andersen and Davidson, 1996; Berk et al., 1995; Newacheck et al., 1996). Children who are publicly or privately insured are more likely to be connected to the health care system through a doctor (Holl et al., 1995; Kogan et al., 1995; Lieu et al., 1993; Newacheck et al., 1996).
There is virtually no research on the access of immigrant children and adolescents to health care, nor on the factors that affect access for this population. The analyses conducted for the committee (Brown et al., 1998) used the number of physician visits "during the past 12 months" as the best available measure of access. This measure combines visits for illness care together with those for preventive care. It is reasonable to assume that children who do not receive at least the minimum number of visits annually that are recommended by the American Academy of Pediatrics (AAP) will not be receiving adequate preventive care. Of course, even if they receive the minimum number of visits, the content of the care may not meet AAP recommendations.
These analyses revealed that first-generation children are less likely than either second- or third- and later-generation children to have had at least one doctor's visit during the previous 12 months (Table 4-6). One-third (32 percent) of first-generation children had not visited a doctor, compared with 18 percent of second- and third- and later-generation children.
These differences were found between first-generation and U.S.-born (second- and third-generation) Hispanic, Asian, and white, but not black, children. For all ethnic groups, first-generation children were also found to be more likely (28 percent) than second-generation children (8 percent) and third- and later-generation children (5 percent) to lack a usual provider or source of health care (Figure 4-2). However, Hispanic children in immigrant families were less likely to have a usual provider or source of care than are non-Hispanic children in immigrant families. The vast majority of second- and third- and later-generation children of all ethnicities, including Hispanics, are connected to a usual source of care. The patterns for first- and second-generation children hold regardless of their health insurance status—whether they are uninsured, have Medicaid coverage, or have private or other coverage.
However, as has been demonstrated repeatedly for children in general, without health care insurance, children in immigrant families are less likely to have a connection to the health care system (51 percent lack a usual source of care) than those having coverage. Other evidence indicates that the expansions in Medicaid eligibility that characterized the mid-1980s to early 1990s led to comparable and substantial decreases in the share of children who went without any doctor's visits in a 12-month period (Currie, 1997). This was the case for children in immigrant families (with at least one immigrant parent) and U.S.-born children in U.S.-born families, despite lower enrollment on the part of immigrant children relative to their eligibility rates (approximately 50 percent of the eligible children in immigrant families were covered, compared with 66 percent of the eligible children of the other group). For U.S.-born children with U.S.-born parents—but not for children in immigrant families—becoming eligible for Medicaid was also associated with increases in hospitalization rates.
Both health insurance coverage and having a usual source of
TABLE 4-6 Children Who Did Not See a Doctor in the Past Year (Percentage), 1994
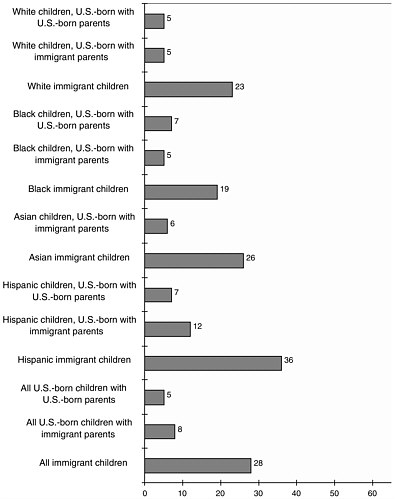
FIGURE 4-2 Children without a usual person or place for medical care: 1994. Note: Sample size of "Asian Children, U.S.-Born with U.S.-Born Parents" was too small to make a reliable estimate. Source: 1994 National Health Interview Survey. Brown et al. (1998).
care independently and strongly affected the probability that a child in an immigrant family made at least one doctor's visit during the year. Children in immigrant families who are uninsured and who have no usual source of care have the lowest probability of having seen a doctor. Those who are uninsured but have a usual source of care, as well as those who have private health insurance or Medicaid coverage but no usual source of care, both have a substantially greater probability of seeing a doctor. Fi-
nally, children who have health care coverage and a usual source of care have the greatest probability of having visited a doctor (Brown et al., 1998).
These relationships applied to children regardless of whether they were first, second, or third and later generation. They characterized Hispanic, black, Asian, and white children alike. Analyses that focused on second-generation children and controlled for family income and maternal education, however, found that some ethnic groups fared worse than others when they lacked insurance or a usual source of care. Specifically, Asian children were substantially less likely than other children to have seen a doctor in the past 12 months when they lacked both health insurance and a usual source of care.
In sum, children in immigrant families show patterns of primary health care use, as measured by having had a doctor's visit in the past year, that correspond closely to their patterns of insurance coverage and reports of having a usual source of care. These patterns and relationships, in turn, replicate those found in the pediatric health services research literature for children in general. Health care for children in immigrant families, as for all children, benefits from insurance coverage and from families' efforts to establish an ongoing connection with the health care system.
BARRIERS TO HEALTH CARE
Children do not always get appropriate health care when it is needed. They are dependent on their parents and guardians to seek care and to accept, understand, and implement the advice of health care providers. Having insurance and a regular source of health care facilitates all children's use of health services, but these factors do not guarantee entry into the health care system.
Systemic and personal factors can pose barriers that deter children from receiving the care they need (Institute of Medicine, 1994a). With the exception of isolated ethnographic studies (Baer, 1996; Baer and Bustillo, 1993; Gold et al., 1996), there is a dearth of research in this area that is specific to children in immigrant families. It is reasonable to expect, however, that some children in immigrant families may experience the kind of barriers that pri-
marily affect children in low-income families who lack insurance or who receive Medicaid coverage, because they are similarly poor. Children in immigrant families may also experience barriers arising from their parents' lack of knowledge about the health care system in the United States, attitudes about accepting public benefits, or from language and cultural differences between parents and providers.
Medicaid and Reduced Access to Care
Limited availability of neighborhood-based primary health care facilities is frequently cited as a barrier to appropriate and timely health care by low-income families. Physicians are not required to participate in Medicaid, and 25 percent of U.S. physicians report that they do not include Medicaid patients in their practices. Approximately a third of physicians limit the number of Medicaid patients they treat (Mitchell, 1991) in part because of low fees paid by Medicaid,12 red tape, and potential exposure to greater liability in treating poor, sick patients (Rowland and Salganicoff, 1994). Even Medicaid patients seen by physicians may be referred to public clinics for immunizations (Ruch-Ross and O'Connor, 1994).
In view of these problems, it is not surprising that many uninsured and Medicaid-covered children receive care in emergency departments and hospital clinics. Among the Medicaid population, clinics, outpatient departments, and emergency departments account for 37 percent of all visits, compared with 17 percent of visits among the privately insured (Rowland et al., 1992). Both uninsured and lower-income children are less likely to go to a physician's office for their routine care than insured and more advantaged children and youth (Holl et al., 1995; Simpson et al., 1997).
Extensive use of emergency departments and clinics undermines continuity of care and leads to lower quality of care (Erzen et al., 1997; Evans et al., 1997; Halfon et al., 1996; Holl et al., 1995; Rodewald et al., 1997), a problem for all children that is exacer-
bated among those with chronic conditions. Moreover, it is not clear how emergency departments and clinics that low-income families rely on and that provide important sources of care for many uninsured children and youth may be affected by the recent wave of hospital closures and mergers, the takeover of not-for-profit hospitals by for-profit companies, and declining government support for public hospitals.
The Shift to Managed Care
In principle, some features of managed care, such as coordination of care by case managers and assignment of care providers to specific patients on a long-term basis, have the potential to improve access to care in the low-income eligible population. Evidence to date is mixed, however, and there are virtually no data on how immigrant children are faring in managed care settings.
A 1995 review of more than 130 studies of Medicaid managed care by the Kaiser Foundation (Rowland et al., 1995) found that managed care reduced use of emergency department and specialist care, but it did not lead to consistent changes in the overall number of doctor's visits. Access to preventive care did not consistently rise or fall, and it remained lower for the Medicaid population than for the nonpoor population. None of the studies in the Kaiser report focused specifically on immigrants. In addition, specialized services such as transportation or language translation, which are needed by many Medicaid beneficiaries and by immigrants as well, may not be offered by conventional managed care plans.
Culture and Language
For many immigrants arriving in the United States today, access to health care is likely to be complicated by cultural perceptions of health and health care that differ from Western concepts and by communication problems caused by language barriers (de Leon Siantz, in review; Munoz et al., 1986). A rich literature has characterized the ways in which culture shapes perceptions, explanations and experiences of illness, help-seeking patterns, and responses to treatment (Angel and Thoits, 1987; Harwood, 1981;
Kleinman, 1978, 1980). The fears of immigrant parents that health care providers will fail to understand or will even disparage their beliefs about their children's health and health care, whether founded or not, may discourage health care use (Institute of Medicine, 1994b; Keefe et al., 1979), although one study of Vietnamese immigrants found that differing beliefs did not act as a barrier to accessing Western medicine (Jenkins et al., 1996). Furthermore, the dearth of bilingual health care practitioners and multilingual health messages may undermine the ability of immigrant children and their families to receive health information, communicate with health providers, and identify health services in their community (Andersen et al., 1981; Giachello, 1994; Moll et al., 1976; Solis et al., 1990; Wood et al., 1995).
There is a strong consensus among health care professionals that the delivery of high-quality health care and mental health services to immigrant children and their families must be done in ways that are culturally competent and culturally sensitive and must take into account language barriers (American Academy of Pediatrics, 1997b). In a study supported by the Health Resources Services Administration, Tirado (1995) defined cultural competence as "a level of knowledge and skills to provide effective clinical care to patients from a particular ethnic or racial group," and cultural sensitivity as "a psychological propensity to adjust one's practice styles to the needs of different ethnic or racial groups." The American Medical Association (1994) defines cultural competence as ''the sensitivity, cultural knowledge, skills, and actions of practitioners that meet the needs of patients from diverse backgrounds."
Several guides have been developed to help providers become more culturally competent (see, for example, American Psychiatric Association, 1994; Cross, 1992; Isaacs and Benjamin, 1991; Lynch and Hanson, 1992). They emphasize the importance of valuing cultural diversity, assessing the culture of the health care delivery system and its interface with the cultures represented by the client population, and incorporating knowledge about the culture-based beliefs and practices of the client population into health care delivery. Efforts that involve recognizing social networks and natural helpers have also been discussed in the literature (see Institute of Medicine, 1994b). Yet few applied graduate
medical training programs provide courses that address these issues or offer opportunities to work with diverse populations (Allison et al., 1994).
To date, moreover, although there is an extensive literature that argues for the need to deliver culturally competent care, it relies heavily on anecdotal evidence (e.g., case studies, providers' personal experiences) and data from small nonrepresentative samples of patients. Research is clearly needed to develop a body of knowledge about how cultural differences, distinct from differences due to other factors such as social class, function to promote or deter the delivery of appropriate and effective health care to immigrant children. The perspectives of parents and children, as well as of a range of health care professionals, are needed. Important questions concern the effects of culturally competent care or its absence on parents' willingness to seek health care for their children; on the accurate communication of symptoms and diagnoses; and on parents' acceptance, understanding, and appropriate implementation of treatment recommendations.
SUMMARY
Prior to welfare reform, second-generation children, who account for three-fourths of all children in immigrant families, were nearly identical to third- and later-generation children in their likelihood of living in families receiving public assistance. First-generation children, however, were more likely than second- and third- and later-generation children to live in families with at least one person receiving public benefits. Among Mexican-origin children, who account for about one-third of all children in immigrant families, the first, second, and third and later generations are all more likely than third- and later-generation white children to live in families receiving public benefits.
It is disadvantaged socioeconomic and demographic circumstances that account for high levels of public assistance receipt among first-generation children as a whole, and among Mexican-origin children in immigrant families. Indeed, their rates of reliance on public assistance are either similar to or lower than those of third- and later-generation black children, who are also highly disadvantaged. For children with similar socioeconomic and de-
mographic circumstances, both first- and second-generation children, generally, as well as first- and second-generation Mexican-origin children, are less likely than third- and later-generation white children to be living in families receiving welfare from most programs.
Beyond generational patterns, it is clear that, with welfare reform, the new restrictions on eligibility for many of the benefits applied to immigrant families are likely to have a disproportionate effect on children whose families are from countries that have either tended to send relatively impoverished people to the United States, such as Mexico, or have been the source of major waves of refugees, such as Southeast Asian nations, Bosnia, and the former Soviet Union.
With regard to health care coverage and access, the committee's analyses, which pertain to the situation prior to welfare reform, indicate that substantial disparities in uninsurance rates—not fully explained by family work status or income—characterize children in immigrant families. First-generation children are about three times more likely, and second-generation children are about twice as likely to lack health insurance than are third- and later-generation children. Hispanic children are particularly disadvantaged, showing both high rates of uninsurance and low rates of employer coverage relative to Asian, black, and white children of all generations.
In large part due to the automatic eligibility of refugees for Medicaid, Southeast Asian children exhibit very low rates of uninsurance despite their very low socioeconomic status. This, combined with the high rates of employment-based coverage for children from most other Asian sending countries, leaves Asian children in immigrant families overall with rates of insurance coverage that do not differ significantly from those of third- and later-generation white children. It is critical to note that the aggregating by broad ethnic groups, which is required by the small sample sizes of existing surveys, obscures the tremendous variations in patterns of insurance coverage that no doubt characterize children from different counties of origin.
When children in immigrant families are insured, they are more likely to have a usual source of care and to have seen a physician. As is true for children in general, both health insurance
coverage and an ongoing connection to the health care system are independently associated with increased reliance on appropriate preventive care. It is their combined effect, however, that most strongly affects children's chances of having seen a physician in the past year. First-generation immigrant children and, to a lesser extent, second-generation children are at higher risk than third- and later-generation children of being uninsured, less likely to have a usual health care provider, and less likely to have seen a doctor in the previous year.
The evidence reviewed by the committee consistently indicates that the health behaviors of these children and their parents are not fundamentally different from those of other children and parents. Medicaid coverage, in particular, appears to increase the number of children in immigrant families who make doctor's visits during the year, without simultaneously increasing hospitalization rates or doctor's visits beyond an annual check-up. Recent reductions in health care coverage—affecting potentially 1 in 4 first-generation children if current rates of Medicaid coverage for these children hold—are likely to result in poorer access to health care, fewer usual providers or sources of care, and fewer regular doctor's visits than is already the case for this population of children, who prior to welfare reform were already disproportionately likely to lack insurance and consistent health care.












































