Health Work Force Policy
by Linda H. Aiken, Ph.D.
Trustee Professor of Nursing and Sociology, and Director, Center for Health Services and policy research, University of Pennsylvania
The health work force is the infrastructure on which our health care system has been built and will depend in the future. As such, the work force can be enabling or restrictive in shaping future health care arrangements. Recognition of the centrality of the health care work force in determining the nation's health care arrangements has motivated the sustained interest of the Institute of Medicine (IOM) over its first 25 years. The purpose of this chapter is to consider work-force-related issues that have been the subject of IOM's attention and that will continue to be important as the IOM moves into its second 25 years.
PUBLIC INTEREST
The supply and distribution of most occupations in the United States is left to market forces and individual and societal preferences. The health care work force, however, has long been a matter of public policy concern because the availability of medical care is perceived to be a public good, unique features of medical care create unusual market conditions, and public subsidies for medical education and health services are large. The public wants access to conveniently located, high-quality, affordable health care services. The appropriateness and quality of health care, however, are more difficult for consumers to
evaluate than are other kinds of services, and the consequences of making a mistake can be fatal. The uncertainty that consumers feel regarding their medical needs and their reduced sensitivity to physicians ' fees due to the widespread availability of health insurance have given rise to the observation that physicians can both induce demand for their services and set their own prices (Feldstein, 1979). Where there are more surgeons, there is more surgery (Bunker, 1970). And contrary to what might be expected under usual market conditions, physicians' fees are often higher in locales with a large supply of physicians, as in many urban areas, than in communities with fewer physicians. Thus, an increase in the supply of physicians becomes a critical factor in national health expenditures, whereas, for example, having more computer programmers would not increase the cost of computing.
Specialty choice, while an individual physician's decision, is of public policy relevance because a specialty influences where providers locate, the constellation of services they provide, the populations they serve, and the cost of their services. Under fee-for-service arrangements that have until recently been the norm in the United States, market forces promoted an ever-increasing supply of specialists, perpetuating a long-standing geographic maldistribution of physicians despite very large increases in the number of practicing physicians.
The belief that government can influence the supply, type, and location of health care providers through its financing of education and practice is the driving force behind most federal and state health work force policy initiatives. Public funds constitute about 40 percent of the $1 trillion the nation spends annually on health services. In addition, public subsidies of medical education are substantial. Medicare financing of graduate medical education alone totals over $6 billion a year including both the direct costs of residency training ($1.6 billion) and payments to teaching hospitals to offset the “indirect” costs of education (COGME, 1994). As public financing of health professions education and health services has increased, the debate about whether and how to use public funds to shape the future health care work force has intensified.
HISTORICAL CONTEXT
When the IOM was established 25 years ago, public policy debate about the medical work force was well under way. Many of the issues of concern then dominate the policy debate today: how many physicians are needed; the imbalance in the production of generalists relative to specialists; the geographic maldistribution of physicians; the influx of international medical graduates; continuing problems of access to care among some populations; the potential for nonphysician providers to help meet health care shortfalls; and escalating costs of medical care (Stevens, 1971; Millman, 1980). what is dif-
ferent now that casts a new light on the work force debate is the extent to which evolving market forces, spurred by the rapid growth of managed care, will create a more competitive market for health services, thus obviating the need for the kinds of regulatory interventions that have been proposed heretofore (PPRC, 1995a).
The beginnings of the IOM coincided with the publication of several influential blue ribbon reports on the health care work force. The report of the Citizens Commission on Graduate Medical Education (the Millis report), published in 1966, called attention to the underproduction of “primary physicians” who would “serve as the primary medical resource and counselor to an individual or family.” The Millis report recommended a central, unified planning authority that would achieve a better balance between the interests of the specialty groups and the health needs of the population, including greater emphasis on what came to be known as primary care. Over the succeeding years, the recommendations from the Millis report have been echoed in various IOM reports. The IOM throughout its history has been a proponent of more and better primary care, and more central work force planning.
Medicare was enacted during this period, bringing a substantial new source of federal funding to graduate medical education. Medicare paid hospitals for reasonable costs associated with the care of beneficiaries. Graduate medical education and the education of nurses and paramedical personnel were designated as justifiable costs eligible for Medicare reimbursement on the grounds that Medicare patients benefit from having well-trained providers.
The Carnegie Commission report published shortly after the implementation of Medicare in 1970 concluded that the nation had a shortage of physicians and recommended a 50 percent increase in medical school admissions. The Carnegie Commission report was the catalyst for public policy work force interventions that resulted in an increase in medical school enrollments and in the number of medical schools. The recommendation that the federal government provide greater direct funding of instructional costs in response to the financial instability of a number of medical schools at the time, including some of the nation's leading institutions, led to one of the first congressionally mandated studies undertaken by the IOM on work force issues—Costs of Education in the Health Professions (1974). This study still stands as the one of the most complete studies of the costs of health professions education, and the only one on nursing, which came to light when President Clinton's Health Security Act proposed a new graduate nurse education fund and cost estimates were needed to design the payment policies governing the new fund.
In 1980, before increased enrollments had time to influence the supply of practicing physicians, yet another physician work force planning group—the Graduate Medical Education National Advisory Committee (GMENAC)—concluded that the nation had a surplus of physicians, a perception that has persisted ever since. The contrast between the recommendations of the
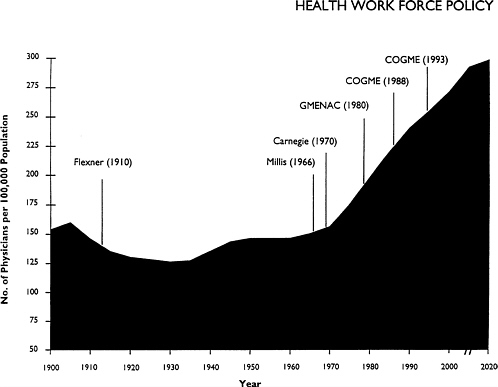
Figure 1. Physician-to-population ratios, 1900–2020. COGME = Council on Graduate Medical Education; GMENAC = Graduate Medical Education Advisory Committee. SOURCE: Department of Health and Human Services, Reports to Congress and the President, selected years.
Carnegie Commission and those of GMENAC, separated in time by only a decade, illustrates the difficulty of using policy to shape the health care work force. The educational pipeline in medicine is so long that it takes decades for policy interventions to have an impact. By the time (1) an imbalance in the work force (1) is recognized, (2) a consensus develops to implement new policies, and (3) enough time elapses for the policies to take effect, circumstances may be radically different from those that motivated the policy change originally.
The decision to close many medical schools as a result of the Flexner report of 1910, for example, resulted in a decline in physician-to-population ratios and a perception of an insufficient supply of physicians lasting for decades (see Figure 1). The correction in supply that occurred during the 1970s is generally believed to have resulted in more physicians than are needed, creating a surplus that could persist for decades. Whether the physician surplus is a positive or a negative factor as regards the evolution of future health care arrangements is a matter of debate. On the one hand, the supply of physicians is part of the explosive growth of national health expenditures. Reducing the rate of growth in expenditures threatens physicians' incomes and motivates opposition to needed reforms in the nation's health care system. On the other hand,
the very fact that there are so many physicians is an important enabling factor in the explosive growth of managed care.
NEW CIRCUMSTANCES
Compared to traditional fee-for-service arrangements, managed care organizations employ fewer physicians overall, many fewer specialists per capita, and more advanced practice nurses (Weiner, 1994). These new estimates have fueled the debate over whether regulation of graduate medical education is needed to reduce the growth in the aggregate supply of physicians and to change the specialty mix, or whether changes in market forces accompanying the rapid growth of managed care will be sufficient to bring about the necessary correction. Primary care physicians' incomes are increasing faster than in years past and at a rate that exceeds that for many specialists (Jaklevic, 1994). In addition, the National Resident Matching Program reported that in 1995, 51 percent of medical students selected first-year residency training positions in primary care, an increase over previous years. Advocates for letting the market work point to these trends as evidence that desired change is occurring without regulatory intervention. Moreover, it has been widely noted that even if the recommendations made by the Council on Graduate Medical Education (COGME) and other groups to reduce the number of residency positions to 110 percent of the class size of U.S. medical schools and to allocate 50 percent of the positions to primary care were achieved, it would take until 2040 for half of practicing physicians to be generalists. Over that period of time, changing market forces could well bring about the desired outcomes without the regulation of graduate medical education. Advocates of regulation counter this by arguing that if recommendations to change graduate medical education had been implemented when they were proposed in the 1970s, national health expenditures would be significantly lower now and many of the most intrusive aspects of government regulation of medical practice could have been avoided.
Another perspective on the work force that has not received as much attention as it merits is the view that the work force is not as out of balance as the advocates of primary care maintain. Contrary to the conventional wisdom, the ratio of primary care physicians to the population has been relatively stable since 1960. The mantra so often repeated of the substantial increase in specialists as a proportion of all physicians does not translate into a decline in the supply of primary care physicians. Moreover, the supply of primary care services is greater than the number of primary care physicians because two other groups provide substantial amounts of primary care: specialist physicians and advanced practice nurses/physician assistants. One of the most comprehensive studies of medical practice conducted since the IOM was established documented empirically the existence of a substantial “hidden system of primary
care” provided by specialists. One in five Americans was estimated to have received continuing general care from a specialist (Aiken et al., 1979). There is no reason to believe that specialists have reduced this component of their practices in the interval since the Mendenhall study, and there are many reasons to believe that it has probably increased as the competition among a growing number of specialists for limited numbers of specialty patients has increased. There are close to 28,000 active advanced practice nurses, at least three-quarters of whom provide primary care. Add to that another 16,000 or more physician assistants, and the aggregate supply of nonphysician primary care providers substantially exceeds the shortfall in primary care projected by COGME for the year 2000.
The presumption that the specialty mix of U.S. physicians is out of balance with population needs and a major contributor to escalating health care costs needs reevaluation in light of changes in health care arrangements (Kassirer, 1994). American physicians have had a long-standing preference for specialty training for at least 60 years. Likewise, the American public has traditionally placed a high value on access to specialty care. The predominance of fee-for-service insurance plans permitting self-referrals to specialists reflected consumers' as well as physicians' preferences. Evidence that consumers retain these preferences is suggested by consumers' concerns about physician choice and access to specialty care that were successfully exploited by opponents of national health reform legislation in 1994. It is not clear that American consumers, if given the choice, would be willing to trade off access to specialty care and the latest technological innovations in medicine for better primary care.
The most compelling reason to ration care by specialists is its cost. The concept of primary care gatekeepers emerged, in large part, to ration specialty care rather than to improve the integration, continuity, and quality of care. In traditional fee-for-service arrangements, specialist care has been more costly because specialists have been able to command higher fees and employ more costly diagnostic and treatment modalities. In a system with an explicit budget, it is not clear that specialists would be more costly than primary care physicians, particularly in the treatment of chronic illness. Recent evidence from the Medical Outcomes Study, for example, demonstrates that specialists provide more cost-effective treatment of depression than do primary care physicians. There is at least anecdotal evidence that primary care physicians do not relish spending so much of their time in the allocation of services as compared to providing care directly. After all, the primary care movement has been predicated on the need to change the content and style of care, not just its organization.
Perhaps the chronically ill, who account for a large share of total medical care utilization, would fare better under the continuing care of specialists; primary care physicians would then be relieved of some of their most time-
consuming case management responsibilities. There are many examples of successful collaboration between advanced practice nurses and specialist physicians in the care of the chronically ill dating back to the first demonstrations using nurse practitioners (see Lewis and Resnick, 1967). At present, specialty services in some HMOs use nurse practitioners to provide 40–60 percent of the visits in specialty clinics such as dermatology and orthopedics (Weiner, 1994). Now that managed care has established a strong momentum in the United States, and cost differences between generalists and specialists can be moderated in ways other than by rationing specialty care, the role of specialists should be reevaluated. The IOM is particularly well suited and positioned to take a leadership role in such an endeavor. It seems counterproductive not to use to full potential in new health care arrangements the large cadre of specialists trained at great public expense.
EFFECTIVENESS OF WORK FORCE POLICIES
The relative lack of success in achieving a health care work force that is perceived to be in balance with national needs tends to be interpreted as a failure of public policy. To the contrary, public policies have been highly effective, especially in increasing the national supply of both physicians and nurses. There is little question that the $1.6 billion a year Medicare spends on graduate medical education has an impact on the supply and specialty mix of physicians. The number of nurses per capita increased 100 percent from 1972 to 1983, owing in large part to funds made available through the Nurse Training Act (IOM, 1983; Eastaugh, 1985). Immigration policies, although controversial, have been successfully employed to augment the domestic supply of nurses in local labor markets during nurse shortages (DOL, 1995).
The problem is not the failure of public policies, but the lack of linkages between the policies guiding large expenditures and work force priorities set by planning entities such as COGME and the Division of Nursing of the Health Resources and Services Administration. For example, most Medicare graduate medical education expenditures are devoted to the training of specialists, not primary care physicians, even in the face of strong evidence that the nation has an excess supply of specialists. Likewise, Medicare subsidizes the training of international medical graduates through its policies of funding more residency positions than can be filled by U.S. graduates, thus contributing to an excessive supply of practicing physicians. Medicare is the largest source of federal funding for nursing and allied health education, but its policies prevent the funds from being used to support the kinds of providers judged by IOM study committees and other blue ribbon policy groups to be most needed, that is, nurse practitioners, physician assistants, physical therapists, and other university-educated allied health professionals (IOM, 1983, 1989).
Aside from inconsistent federal policies that undermine health work force planning at the national level, the use of Medicare hospital payments as the primary federal policy vehicle for health professions education is becoming increasingly problematic as the need for providers trained in ambulatory care grows. Medicare Part A is not an optimal vehicle for funding generalist physician, graduate nurse, or allied health education because of its primary purpose of funding hospital care (Eisenberg, 1989; PPRC, 1993b; Aiken-and Gwyther, 1995). While various IOM reports have commented on the problems associated with the use of Medicare as a primary funding vehicle for health professions education, the IOM has not focused directly on the development of alternative policy options. If Medicare financing of graduate medical education continues, the IOM could and should contribute to the design of alternative mechanisms that eliminate the present institutional bias that distorts training.
Evaluation of the adequacy of the health care work force at present and for the future depends upon the outcome criteria of interest. There are a number of possibilities including the magnitude and growth of national health expenditures, the affordability of care to patients, diversity of service type and mix, and educational opportunities to pursue a career of choice. Although all of these merit consideration, perhaps none is more important than ensuring access to appropriate care for everyone. While the nation's present health work force is not optimally configured in terms of use of resources, and there is little doubt that there is excess capacity, from the perspective of access to conventional medical care, the present work force provides an adequate-to-excellent services infrastructure for most Americans.
ACCESS TO CARE AND THE WORK FORCE
The IOM has been concerned with access to care throughout its history (IOM, 1993) and has directed considerable attention to subgroups experiencing particular barriers to appropriate care, including the homeless, people with HIV/AIDS, the poor, and the elderly. Inadequate health insurance coverage ranks high among the reasons for poor access to appropriate health services. Yet, as has been documented in IOM reports, the maldistribution of the health care work force by specialty and location remains an important factor in the nation's residual access problems. The recent failed attempt of national health care reform to move closer to universal health insurance coverage renewed interest in a long-standing debate regarding the extent to which insurance reform would solve the nation's existing access problems without other policy initiatives including those pertaining to the health work force.
Elderly Americans have had the equivalent of President Clinton's Health Security Card for 30 years. Yet some Medicare beneficiary subgroups have not obtained access to mainstream medical care even with universal health insur-
ance coverage (PPRC, 1995b). These groups include African Americans and residents of urban health professional shortage areas and urban poverty areas. Compared to all Medicare beneficiaries, these groups are less likely to see a physician in a year. They have fewer medical visits but are more than twice as likely as other beneficiaries to rely on hospital emergency rooms for care. Their use of preventive services, pap smears, for example, is far below average—one of multiple indicators suggesting that hospital outpatient departments and emergency rooms do not provide the equivalent care afforded those who use office-based practices. They experience more outlier hospitalizations and have a significantly higher mortality rate (PPRC, 1993b). That these access problems exist in an insured population residing, for the most part, in urban areas that have high physician-to-population ratios raises important questions regarding the effectiveness of health work force policies in resolving the nation's residual access problems. It is therefore instructive to review what is known about the impact of work force policies on access to care.
The ratio of physicians to the population has increased by more than 80 percent since 1960, with the majority of new physicians settling in metropolitan areas. The increase in physician supply in urban areas has been great enough to constitute a serious test of the “trickle down” theory, which posits that if the number of physicians increases enough, eventually more will practice in underserved neighborhoods. That the most serious residual access problems among insured Medicare beneficiaries persist in urban areas is evidence enough that increasing the supply of physicians is not an efficient way to solve the nation 's residual access problems.
Financial incentives have, in recent years, become a popular public policy vehicle for attempting to influence physicians' practice patterns and choice of location. One such major initiative was Medicare's physician payment reform in the late 1980s. The new Medicare fee schedule increases the relative compensation to physicians for primary care services and for office visits for management and evaluation services, decreases relative compensation for diagnostic and surgical procedures, and reduces the disparities in compensation by geographic location (Ginsburg and Lee, 1991).
While it is still too early to evaluate the ultimate impact of the Medicare fee schedule on access, the early signs are not encouraging. The good news is that the fee schedule has not adversely affected access to care for Medicare beneficiaries as a whole (PPRC, 1995b). However, trends in the use of services by underserved populations have remained largely unchanged since 1986. If anything, the number of office-based practices continues to decline in urban poverty areas, and beneficiaries residing in such areas have increased their use of hospital outpatient clinics and emergency rooms (PPRC, 1993b).
It can be argued that the Medicare fee schedule is a blunt instrument for the purpose of directing financial incentives to enhance access for particular population subgroups. Moreover, its overall objective is to reduce the rate of
growth in Part B expenditures, rather than to improve access. Thus, Medicare added to the financial incentives created within the new fee structure bonus payments to physicians practicing in physician shortage areas. The bonus payment system began in 1989 with an incentive payment of 5 percent for services rendered in rural health professional shortage areas. In 1991, bonus payments were increased to 10 percent and extended to urban shortage areas. By 1992, some 28,500 physicians received bonus payments totaling over $63 million. In urban areas, however, three-quarters of the services for which bonuses were paid were specialty services rather than primary care, and only one-third of Medicare beneficiaries receiving services in urban health professional shortage areas actually lived there. There is little evidence to suggest that bonus payments benefited the target population. And, not surprisingly, no gains in access can be documented over the period that bonus payments have been available.
One work force option that holds promise for bringing more primary care to inner city areas—and has never been given a real test—is the development of incentives to encourage advanced practice nurses and physician assistants to locate practices there. Three decades after these providers were introduced into the U.S. health care system as a strategy for improving access to primary care, their effective utilization remains hampered by legal, financial, and professional barriers to practice. Medicare does not reimburse nurse practitioners and physician assistants directly except in rural areas. This is noteworthy because the federal government was instrumental in promoting the concept of nonphysician providers in primary care, supporting their education, and funding research on their efficacy and acceptability to consumers. Medicare payment policies for advanced practice nurses and physician assistants are yet another example of inconsistent federal work force policy.
The IOM has likewise been inconsistent in its recommendations regarding advanced practice nurses and physician assistants. Its 1978 report A Manpower Policy for Primary Care recommended no further increase in numbers of nurse practitioners and physician assistants because of increasing numbers of physicians in the educational pipeline. Five years later, another report, Nursing and Nursing Education: Public Policies and Private Actions (1983), noted the growing demand for advanced practice nurses in all settings and called for increased federal support of graduate nurse education. The current IOM study on nurse staffing in hospitals and nursing homes is again considering the role of advanced practice nurses and physician assistants, particularly in view of possible reductions in residency training and the gaps in medical coverage such reductions would create in many hospitals.
The continuing controversy over the appropriate role and use of advanced practice nurses and physician assistants is motivated by two issues: the perceived oversupply of physicians and the cost implications of extending third-party fee-for-service reimbursement to new groups when the trend is away
from fee-for-service payment in general. The most compelling public policy rationale for promoting the use of advanced practice nurses and physician assistants is inadequate access to health care by some groups despite very large increases in physician supply and the failure of various financial incentives to physicians to substantially change this negative picture. The continuing erosion in the number of office-based physicians in poor, inner city areas suggests that if an alternative is not found, the poor will be permanently relegated to large institutional care settings including emergency rooms, which do not have a good record of providing preventive services, continuity of care, or community outreach. Federally funded community health centers have a better record of providing appropriate care in underserved areas. Yet the ongoing financing of such centers has been and looks as if it will continue to be problematic. A major expansion of such centers would be required to fill the unmet need—something that seems unlikely in the near term.
Trends in physician practice patterns run counter to the establishment of new office-based practices in poor, inner city areas. These types of communities are not likely to be able to sustain the large multispecialty groups that have replaced solo and partnership practices. The scale of businesses that survive in these settings is smaller than most physicians prefer—more on the order of storefront practices. Advanced practice nurses and physician assistants, in contrast to physicians, exhibit preferences for smaller-scale office practices when such options are viable. Most of these practitioners now work in larger, organized medical settings because reimbursement policies and ambiguous or uncertain legal issues restrict their choice of practice locations and settings (Safriet, 1992; Sekscenski et al., 1994). As Cooper (1994) notes in his comprehensive review of research on the physician work force, it is not clear that rural and inner city access problems can be solved by achieving better balance within the physician work force; access, he argues, is a system problem requiring organizational solutions. The establishment of storefront practices of advanced practice nurses and physician assistants with physician consultation, embedded in a referral network that provides the full spectrum of services, may be one of those structural changes.
Managed care arrangements do employ advanced practice nurses and physician assistants in larger numbers than fee-for-service settings, and their continued growth is likely to offer increased practice options for nonphysician providers. But the fastest-growing managed care model is the independent practice association type in which office-based practices constitute the services network. The infrastructure of office practices is weak in poor, inner city neighborhoods, suggesting that managed care organizations will have difficulty providing adequate access to their enrollees in these neighborhoods, and that the growth of managed care is not a necessary solution for the absence of providers in inner city neighborhoods.
Would advanced practice nurses and physician assistants be likely to practice in underserved neighborhoods if they were reimbursed by Medicare and qualified as eligible providers in managed care networks? Even in the absence of direct Medicare reimbursement, nurse practitioners, nurse midwives, and physician assistants do locate in urban and rural health professional shortage areas, and in larger proportions than do physicians (OTA, 1986). More important, given the long-standing access problems in these communities, a rational public policy would encourage every willing provider to practice rather than foster barriers that discourage qualified providers from practicing.
A reason often advanced for limiting Medicare direct reimbursement to advanced practice nurses and physician assistants is the presumed high cost of extending payment to additional providers. Reliable estimates of the cost of direct reimbursement to advanced practice nurses and physician assistants were lacking until the Health Security Act included such a provision. Both the Health Care Financing Administration and the Congressional Budget Office, in response to the president 's proposal, estimated 5-year costs. Both estimates were less than 0.5 percent of Medicare Part B expenditures (Aiken and Salmon, 1994:323). In aggregate dollars, the cost of reimbursing advanced practice nurses and physician assistants to provide covered services was, in order of magnitude, comparable to expenditures on physician bonus payments, which have not yet proven to be effective in increasing access to care for underserved populations.
CONCLUDING COMMENTS
Health work force policy issues are as or more important now than they were at the time of the Institute's founding. It may be that the long-standing debate on whether or not to regulate graduate medical education will be resolved not by work force policies but by political pressures to reduce federal outlays. Federal expenditures of $6 billion a year to subsidize education for an occupation widely believed to be available in adequate numbers, whose members' average incomes are on the order of 5 times greater than the average American's income, seem like a highly visible target for federal budget reductions. Moreover, it is increasingly evident that such large untargeted subsidies have not achieved many of the objectives held by their advocates, including increasing ethnic and cultural diversity in the health care work force, providing an equitable geographic distribution of health care resources, and ensuring reasonable access to appropriate health care for all Americans.
The IOM is well positioned to make an important contribution to national health work force policy. Its interdisciplinary membership representing the broad array of health professions, its commitment to the advancement of science as well as clinical care, and its broad social agenda to improve the na-
tion's health provide the perspective and influence needed to inform and shape the discourse about options for the inevitable restructuring of the medical education enterprise. Medical and health professions education has become intricately enmeshed in the highly successful medical research enterprise, which needs to be preserved. And we have come to rely on medical education and its associated teaching institutions to fill the health services gaps left in a system that does not provide universal health insurance coverage to all of its citizens. There will be no greater challenge for the IOM in its second quarter-century than contributing to the evolution of a rational medical education system that can provide the appropriate work force on which our future health care system will depend while enabling the continued advance of medical science and technology and protecting the health of the nation as it struggles to extend the guarantee of access to health services to all.
REFERENCES
Aiken, Linda H., and Gwyther, Marni E. 1995. Medicare funding of nurse education: A case for policy change. Journal of the American Medical Association 273(19):1528–32.
Aiken, Linda H., and Salmon, Marla. 1994. Health care workforce priorities: What nursing should do now. Inquiry 31:318–29.
Aiken, Linda H., Lewis, Charles E., Craig, John E., Mendenhall, Robert, Blendon, Robert, and Rogers, David E. 1979. The contribution of specialists to the delivery of primary care: A new perspective. New England Journal of Medicine 300:1363–70.
Bunker, John P. 1970. Surgical manpower: A comparison of operations and surgeons in the United States and in England and Wales. New England Journal of Medicine 282:135–44.
Carnegie Commission on Higher Education. 1970. Higher Education and the Nation'sHealth: Politics for Medical and Dental Education. New York.
Citizens Commission on Graduate Medical Education. (1966). The Graduate Education of Physicians Chicago: American Medical Association.
Cooper, Richard A. (1994). Seeking a balanced physician workforce for the 21st century. Journal of the American Medical Association 272:680–7.
Council on Graduate Medical Education (COGME). 1994. Recommendations to Improve Access to Healthcare Through Physician Workforce Reform (4th Report). Health Resources Administration.
Department of Health and Human Services (DHHS). 1992. Health Personnel in the United States: Eighth Report to Congress (Pub. No. HRS-P-OD-91-1). Department of Health and Human Services.
Department of Labor (DOL). 1995. Report to the Secretary of Labor on the Immigration Nursing Relief Act of 1989. Washington, D.C.: Immigration Nursing Relief Advisory Committee, U.S. Department of Labor.
Eastaugh, Stevens R. 1985. The impact of the nurse training act on the supply of nurses, 1974–1983. Inquiry 22:404–17.
Eisenberg, John M. 1989. How can we pay for graduate medical education in ambulatory settings? New England Journal of Medicine 320:1525–30.
Feldstein, Paul J. 1979. Health Care Economics. New York: John Wiley.
Ginsburg, Paul B., and Lee, Philip R. 1991. Physician Payment. In Health ServicesResearch, Eli Ginzberg (ed.) Cambridge, Mass.: Harvard University Press.
Institute of Medicine (IOM). 1993. Access to Health Care in America. Washington, D.C.: National Academy Press.
Institute of Medicine (IOM). 1989. Allied Health Services:Avoiding Crises Washington, D.C.: National Academy Press.
Institute of Medicine (IOM). 1983. Nursing and Nursing Education: Public Policies and Private Actions Washington, D.C.: National Academy Press.
Institute of Medicine (IOM). 1978. A Manpower Policy for Primary Care. Washington, D.C.: National Academy Press.
Jaklevic, Mary C. 1994. Primary-care docs see incomes rise.Modern Healthcare January 26:64.
Kassirer, Jerome P. 1994. Access to specialty care. New England Journal of Medicine 331(17): 1151–3.
Lewis, Charles E., and Resnick, Barbara A. 1967. Nurse clinics and progressive ambulatory care. New England Journal of Medicine 277:1236–41.
Millman, Michael C. 1980. Politics and the Expanding Physician Supply. New York: Universal Books.
Office of Technology Assessment (OTA). 1986. Nurse Practitioners, Physician Assistants, and Certified Nurse Midwives: A Policy Analysis (Health Technology Case Study No. 37). Washington, D.C.: U.S. Government Printing Office.
Physician Payment Review Commission (PPRC). 1993a. Annual Report to Congress. Washington, D.C.: Physician Payment Review Commission.
Physician Payment Review Commission. 1993b. Monitoring Access of Medicare Beneficiaries. Annual Report to Congress (Report No. 93-2). Washington, D.C.: Physician Payment Review Commission.
Physician Payment Review Commission (PPRC). 1995a. The Changing Labor Market for Physicians. Annual Report to Congress Washington, D.C.: Physician Payment Review Commission.
Physician Payment Review Commission. 1995b. Monitoring Access of Medicare Beneficiaries. Annual Report to Congress (Report No. 95-1). Washington, D.C.: Physician Payment Review Commission.
Safreit, Barbara. 1992. Health care dollars and regulatory sense: The role of advanced practice nursing. Yale Journal on Regulation 9:417–87.
Sekscenski, E., Sansom, S., Bazell, C., Salmon, M., and Mullan F. 1994. State practice environments for physician assistants, nurse practitioners, and certified nurse midwives. New England Journal of Medicine 331:1266–71.
Stevens, Rosemary. 1971. American Medicare and the Public Interest. New Haven: Yale University Press.
Weiner, Jonathan. 1994. Forecasting the effects of health reform on U.S. physician workforce requirement. Journal of the American Medical Association 272:222–30.
The Health Work Force: Issues for Policy Analysis
by Uwe E. Reinhardt, Ph.D.
James Madison Professor of Political Economy, Princeton University
All modern nations worry about the training of the increasingly specialized work force that will staff their economies. There is concern over the number of persons trained for specialized, technically demanding work in various fields and subfields. There is concern over the geographic distribution of such specialists and, more recently, over their demographic mix. There is perennial concern also over the methods by which the specialized work force is trained and over the content of that training. Finally, there is concern over the trade-offs that need to be made to finance the training of these specialists equitably and efficiently.
Although leaders of every major economic sector worry thus about the people that will operate their sector in the future, probably none of them rivals the health sector in its worry over the future health work force. Ever since the turn of the twentieth century, there have been a series of commissions and studies projecting either shortages or surpluses of doctors or nurses. As Marilyn Field reports in her chapter, since the early 1970s the Institute of Medicine (IOM) has been a major player in this endeavor, although by no means the only one. Studies on the health work force continue within the walls of the Institute, and elsewhere, as this essay is written.
There are at least three major reasons why the health work force has attracted such abiding attention from policymakers.
First, modern health care involves matters of life and death. There has always been general anxiety among policymakers that the nation may be inadvertently short of this or that specialized health personnel and that ill health or death may be the result. There is a parallel concern that a surplus of physicians will at the least drive up the cost of health care, but may also lead to needless and sometimes dangerous medical interventions.
Second, there has been a general consensus in this country that all academically qualified members of society, regardless of income, gender, and race, ought to have access to the health professions for which they qualify. This has certainly been the feeling since World War II, which helped to foster an egalitarian ethos among Americans. This egalitarian ethic inevitably makes government a major source of financing for the education and training of American health professionals. But whenever government becomes a major source of finance for anything, there must be an accompanying public policy on just what is to be procured with those public funds and for whom. That circumstance alone would make the health work force a matter of public policy, even if there were no concern over impending shortages or surpluses in the health work force.
Finally, it is government's responsibility to assure all Americans of critically needed health care. That mandate, too, makes it incumbent upon government to worry about the number of health professionals and their geographic distribution. It forces government to step in where the private sector leaves major gaps. For example, because graduates from American medical schools have for decades shunned residency slots in the low-income, inner cities, government has filled that void with international medical graduates (IMGs), without whom many inner city hospitals simply could not function. The importation of human capital (i.e., persons who have been at least partially educated and trained abroad) evidently is a matter of public policy requiring continued review. It is a quite controversial issue that lies at the intersection of health policy and international trade policy.
Policy analysis on the health work force has proceeded on two quite distinct strands. The first has been positive analysis, concerned chiefly with work force projections and the analytic ingredients going into those projections. The second has been normative policy analysis designed to explore on behalf of both private and public policymakers alternative options for public policy and, on occasion, to recommend particular courses of action.
THE HEALTH WORK FORCE: METHODOLOGICAL ISSUES
Throughout the early history of health work force analysis, there had been a tendency to examine each type of health professional (physicians, nurses, technicians, etc.) separately and to think in terms of ideal, fixed ratios between the number of such professionals and the underlying populations. In the jargon of economists, the health care production process was thought of as one rigidly constrained by fixed input –output coefficients. Anyone who sincerely believes that such a model fairly describes the health sector naturally will be driven to incessant worries over the right future number of particular types of health professionals.
Economists have argued for decades that this fixed-coefficient model is a distorted caricature of the real world and that its use can do great harm.1 Theory suggests, and empirical research has demonstrated, that there are wide ranges over which one type of health professional can be substituted for another type in the production of health care. Figure 1 seeks to illustrate this point schematically.
In Figure 1, variable Sj denotes a quantity of health services of type j (e.g., office visits with a physician or inpatient days). As is increasingly being recognized, there is not just one set of health services that can respond properly to a given set of morbidities. Almost daily one reads in the literature how easily outpatient services can be substituted for inpatient care in the treatment of particular illnesses. In what has come to be called “disease management,” pharmaceutical companies search jointly with doctors and hospitals for so-called best treatment practices, possibly with the view of substituting products produced by the pharmaceutical industry for human labor or other capital inputs in the treatment of specific diseases.
But there clearly is not just one “best treatment” for a given illness. What is best in that context depends not only on purely clinical trade-offs among inputs, but also on the relative cost of these inputs. Where human labor—especially highly trained human labor—is relatively expensive, the best treatment method is apt to be relatively intensive in its use of equipment (including computers) and pharmaceutical products. Where human labor is relatively cheaper, a more labor-intensive treatment regimen may be better. It is a point that had traditionally left physicians uncomfortable —because its permits money to enter the treatment decision—but one that is being imparted to them now with some force by the managers of the emerging managed-care industry.
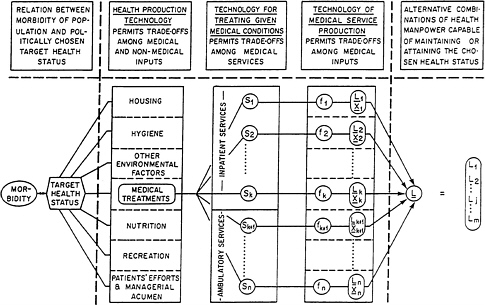
Figure 1. Potential trade-offs in the production of health. SOURCE: Reprinted, with permission, from Reinhardt (1991), Figure 9-1; copyright 1991, Harvard University Press.
The array of variables {L1, L2, . . . ,Lm} in Figure 1 represents the entire array of health professionals that may be used to produce a given volume of health services. Variable L1, for example, may denote a number of cardiologists, L3 a number of internists, L14 a number of registered nurses, and so on. The array {X1, X2, . . . , Xk} represents a set of nonlabor inputs used in the production of health services—for example, floor space, medical equipment, and computers. Finally, the notation fj denotes a so-called production function, that is, an estimated mathematical equation that describes the transformation of labor and nonlabor inputs into health services of type j. Production functions can be used to identify the manner in which these inputs can be substituted for one another in production.
Conceptually, one can imagine one such production function for each distinct type of health service in the entire imaginable array of health services (e.g., visits with a primary care physician, a normal delivery, a coronary bypass graft). Econometric research in the 1970s yielded a number of such empirical production functions.2 They pointed to great flexibility in the link between the requirement of particular kinds of health services and the requirement of particular types of health workers (including physicians). Unfortunately, policymakers lost interest in health work force issues during the 1980s and research of this sort ceased. One would expect it to have a revival as part of the current hunt for best treatment practices.
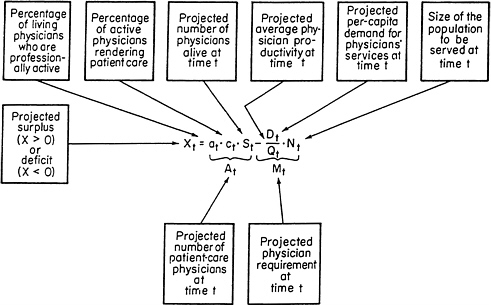
Figure 2. A simple forecasting equation for physician manpower. SOURCE: Reprinted, with permission, from Reinhardt (1991), Figure 9-6; copyright 1991, Harvard University Press.
Figure 2 illustrates the traditional methodology for projecting the future availability and requirement of one particularly important health professional: the physician. The figure is largely self-explanatory.3 It makes graphic just how difficult it is to ascertain whether or not the nation will have a physician shortage or surplus at some time t in the future. Although the schematic may not appear to consider the potential role of any substitute professionals (e.g., nurse practitioners or physician assistants), they actually do enter indirectly through the productivity variable Qt, which denotes the annual number of physician services expected to be produced per full-time-equivalent physician in some future year t. That productivity variable depends very much on the particular manner by which tasks are allocated among members of the broader health care team.
On the supply side, the easiest projection always is the number of physicians likely to be alive at future time t. Most of those physicians are already practicing at the time of the projection or they are in a predictable pipeline. Less certain, however, is the additional annual influx of IMGs. This depends strongly on U.S. immigration policies, which, in turn, are driven by the need of certain American hospitals—for example, inner city hospitals in New York and New Jersey—for the relatively cheap, quasi-indentured labor
provided by residency programs.* But even if the number of physicians alive at time t were reasonably well known, one still has to estimate what proportion of them will be professionally active at time t (variable at) and what fraction of those would be active mainly in clinical care (variable ct). In recent years, for example, the latter variable has been strongly influenced by the growing cost of malpractice insurance, which has driven many physicians into early retirement. In the future, ct is likely to be buffeted again by the strictures of managed care, which many older physicians will find nettlesome. The strictures will likely drive many older physicians into early retirement and many younger ones out of patient care and into administration. Managed care will also depress variable ct.
Projecting future physician requirements on the demand side of the health sector is much more difficult than supply-side projections. The relatively easiest part of estimating the demand is projecting the future population, broken down into sociodemographic groupings that are relevant for estimating the future utilization of health services (in this case, physician services). But even these projections are rather uncertain. Next, one must project future physician productivity (variable Qt in Figure 2), which depends on the number of weeks future physicians will work per year, on the number of hours they will work per week, and on the number of physician services they will produce per hour. There is some evidence that all three components may be affected by the gender composition of the future physician work force. Past research suggests that female physicians tend to work fewer weeks per year and fewer hours per week, and to see fewer patients per hour than do their male counterparts.4 It is not known, however, whether this differential is a transitory or a permanent phenomenon. Therefore it is a matter for further inquiry. As already noted, the productivity variable Qt is also strongly driven by the delegation of tasks from physicians to other health professionals and, indeed, to equipment. That relation also deserves sustained future analysis.
The conceptually most troublesome issue in projecting future physician requirements is variable Dt in Figure 1—the projected future per capita utilization of physician services. Should that projection be a normative magnitude, based on expert opinion about the population's future need for physi-
|
* |
Hospital leaders may object to this characterization with the argument that residency training costs the hospital money over and above what it would have to spend on health care in the absence of that training. That may be true for many or most hospitals. But it is difficult to square that argument with the cry heard among many inner-city hospitals that they could not function without the services provided by IMGs. Clearly, IMGs provide a labor service more cheaply than would the next alternative source of that labor. |
cian services, or should that projection be a positive, objective assessment of the number of physician services per capita that is likely to be demanded at time t in the market for health services? That has been the longest-running, unresolved question in research on the health work force.
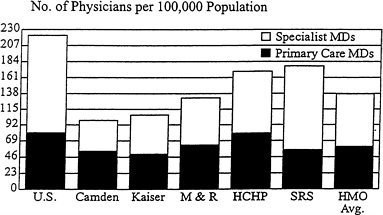
Figure 3. Physician requirements under managed care. SOURCE: David Burnett, M.D., University Hospital Consortium. Reprinted with permission.
People who are not economists—particularly physicians—generally tend to favor the normative, needs-based approach. It conforms to the idea that all members of society should receive all the care they need. For example, in its well-known report, the Graduate Medical National Advisory Commission based its projections of variable Dtstrictly on a needs-based approach. Economists criticize the approach,5 not because they do not share the physicians' social ethic in these matters, but based on the hard-nosed realization that this social ethic is merely wishful thinking, and that the market is always the all-powerful, final arbitrator in health care, as it is in all other economic spheres. Economists argue that it makes little sense to train a health work force for a normative utilization pattern that the market and the political process simply will not underwrite financially. For that reason, economists typically project the per capita utilization variable Dt as their best objective estimate of actual utilization, given their best estimate of future per capita income, insurance coverage, the price of physician services, and other variables thought to determine the actual use of physician care by the population.6
Alas, anyone who seeks to project the actual per capita use of a particular health service a decade hence is quickly led to the realization that the task presupposes a rather extensive empirical model of the entire health care sector that, in turn, is merely an embedded part of a much larger model of the entire economy. Attempts to develop such larger models have been notoriously unsuccessful.7 Even if such a model could be estimated with a reasonable accuracy, its estimated parameters would be merely summaries of
an institutional past. They could not accommodate major future shifts in the institutional framework—for example, a wholesale shift from fee-for-service compensation of physicians to capitation.
Figure 3 illustrates the potential effect such a shift can have on future physician requirements. The estimates shown in that diagram represent simulations based on actual staffing patterns in a selected number of HMOs. The simulations were made by the University Hospital Consortium in its ongoing effort to model the impact of capitated managed care on the future health work force. They corroborate Jonathan Weiner 's recent estimate that if between 45 percent and 60 percent of the American work force were enrolled in HMOs by the year 2000, there might emerge by that time a surplus of some 165,000 patient-care physicians in the United States.8 This is an enormous surplus in a total projected supply of some 600,000 physicians. At this time, it is anybody's guess how the health system would react to such a surplus and whether that surplus actually will come about. It is a prospect the IOM will undoubtedly monitor closely in the decade ahead. In a health system undergoing the rapid, often unpredictable changes now besetting ours, sustained monitoring of the markets for the health work force, rather than long-range forecasting, would seem to be the much more productive use of limited research resources.
THE HEALTH WORK FORCE: POLICY ISSUES
One can compress the major current policy issues related to the health work force into the following four broad questions:
-
How should the training of health professionals be financed—that is, who should be responsible for it, what should be compensated, and how and to whom should those payments be made?
-
What should be the content of medical education and training, especially in a world characterized by rapid technological changes and by rising social tensions among ethnic groups and income classes, tensions that will tangent directly on health care?
-
Should the government or a quasi-governmental body of experts regulate the size, specialty composition, and geographic distribution of the health work force or can that be left to the private market?
-
Given the highly personal interactions on which health care is based, how important is it that the racial and ethnic composition of the health work force mirror the composition of the population to be treated and, if that is important, how can a proper match be achieved?
Financing the Training of the Health Work force
In most industrialized countries, the education and training of health professionals is collectively financed. The professionals themselves pay little if anything out of pocket toward their own training, other than the income that is forgone during training—the so-called opportunity cost of professional training. That approach is based on two premises. First, there is the assumption that this form of human capital yields benefits far beyond those that can be captured by the health professionals themselves in the form of income (although it is not clear just what these external benefits may be). In the jargon of economists, professional training is viewed as a quasi public good. Second, there is the ethical premise that there should be absolutely no financial barrier between an academically qualified applicant and the education and training for which that applicant qualifies. At the policy level, these two premises reinforce each other. Their logical implication is the collective financing of health professional education (and of education in general).
The financing of health professional education and training in the United States is not based on any such clear-cut premises. Instead, it has been pulled hither and thither by two opposing premises that, together, have begotten a system of financing almost beyond anyone 's comprehension and certainly beyond anyone's proper control.
On the one hand, there is the view that the education and training of a professional is nothing other than an investment in a particular form of capital—namely, human capital—whose pecuniary and nonpecuniary returns accrue almost fully to the professionals themselves and not to society at large. From the latter assumption follows the proposition that the professionals themselves should pay for the investment in their own human capital. Critics of that theory argue that its application would preserve the learned professions mainly for the offspring of the upper-income classes. That need not be so, however, if the professionals were granted easy access to a financial, human-capital market that stood ready to finance education and training under term loans that could be amortized with periodic installments over many years, paid out of the trainee's own future income.
This type of human-capital market exists in the United States only in rudimentary form. The fact is that politicians and the public they represent have never been quite comfortable with the premises underlying the human-capital approach. Many policymakers actually favor the socialized approach used elsewhere in the industrialized world, and so probably does the American public. Thus, instead of embracing either the completely socialized financing of professional education adopted by other nations or the pure capitalist approach favored by American libertarians, American health work force policy has occupied a middle ground. The general public and the pro-
fessional trainee share in the cost of professional education in proportions that vary over time and space.
Not surprisingly, this hybrid system is exceedingly complex. It funnels money to health professional schools from a great variety of relatively uncoordinated sources. An allegedly small amount of that money comes from tuition paid directly by the trainees. Other parts come from direct government grants, from special direct and indirect allowances for residency training paid by government as well, from research contracts with private and public clients, and from charges added to fees for the patient care rendered by the faculty practice plans of medical schools and by teaching hospitals.
This multipipe financing system has two untoward consequences. First, it literally precludes proper accountability for these funds on the part of the recipient schools. Their finances remain opaque to the outside world and, quite possibly, even to the management within. Second, multipipe financing has granted these schools undue autonomy, for it allows them to divide and rule. In particular, the system has immunized health professional schools from the rest of the health care market, allowing them to produce health professionals in numbers and in a mix that suit their own idiosyncratic preferences and deviate significantly from the ideal staffing pattern proposed in virtually any study on the health work force.9
The financing of health professional training is bound to come in for special scrutiny in the coming decade, for at least two reasons. First, much of the money for health professional training has come from government, both state and federal. Squeezed by rising expenditures on the one hand and a latent tax revolt on the other, government is apt to review the rationale for subsidizing the production of often highly paid professionals of which the nation is said to have too many all around. Second, the rapid spread of capitated managed care will make it much more difficult to recoup the cost of medical education and residency training from private payers through higher fees for patient care. Once these cross-subsidies have been squeezed out of the system by the competing capitated health care networks, a new way will have to be found to finance the operations of our health professional schools.
It is a safe guess that the IOM will be one of the organizations to which policymakers will look for guidance on this issue. When that analysis begins in earnest, the entire range of issues surrounding the financing of academic health centers and of teaching hospitals will be on the table, along with a review of the proper allocation of these costs to the trainees and to the general public. The analysis will involve unsolved conceptual issues (e.g., methods of proper cost allocation within academic health centers), philosophical issues (e.g., the definition of “fairness” in providing access to health professional training), and issues of policy implementation (e.g., the development of criteria on which public subsidies to either trainees or their schools should be based, or whether these subsidies should be paid as grants
to the health professional schools or as stipends that travel with the student).10 All of these are issues that ought to have been resolved long ago, but that were somewhat neglected in the last two decades because of a lack of interest among policymakers.
The Content of Health Professional Training
Although American academic health centers have long been at the frontier of medical innovation, their curricula for health professional training have been remarkably stable—perhaps too stable.11 As noted, these curricula appear to have been driven more by the preferences of the health professional schools than by the requirements of the market for health services.12 This is another area likely to be revisited again in the coming decade.
For one, the education and training of an American physician is long by international standards. It is also very expensive. While that outlay of time and money have bought academic and clinical excellence overall, it is not clear that it can be justified at the margin, that is, that the cost of the extra year or two at the margin is matched by commensurate incremental benefits. This question becomes particularly germane in light of the widespread consensus that this nation produces too many medical specialists and possibly not enough primary-care physicians.
There is the added question of whether the locus of residency training is at all suitable for the career profile of the typical American physician. Because the public sector pays for the bulk of residency training, and because these funds flow almost exclusively to teaching hospitals, the typical resident probably experiences too much training in high-tech tertiary care and not enough training in the ambulatory sector, where most of a physician's professional time is spent. Here, too, a sector driven by inertia and finely honed skills of turf protection will require searing scrutiny from outside—the kind, one would hope, the IOM might be able to supply.†
Finally, it can be asked whether the academic content of health professional training might not require a review at this time. At issue is the proper balance between “education” and “training.” For example, how well is society served by the heavy traditional emphasis on the natural sciences in premed and medical education, at the cost of education in the social sciences and in philosophy? Should not a demonstrated, solid understanding of ethics, sociology, economics, and management science be part of the core of the health professional's basic education? If so, who should provide that educa-
|
† |
This would require very careful deliberations on the composition of the relevant study panel. |
tion? Should it be part of the candidate's undergraduate education in college, or should that material be imparted in medical school or even during residency training, when it can be tailored more specifically to the daily work of a practicing health professional?
Regulation vs. Market
The third and fourth questions asked earlier in this section raise the issue as to whether the training of health professionals in this country should be regulated by the government or whether it can be left to the decentralized decisions of the marketplace. If current forecasts of a major physician surplus are at all near the mark, for example, should government arbitrarily limit the overall size of the graduating class from American medical schools, and should it prohibit the immigration of IMGs? Should government specify the mix of medical specialties that is to be trained and the allocation of residency slots in each specialty to regions and within regions? Should government use its fiscal and regulatory powers to reallocate medical school places to particular groups now deemed to be underrepresented in the nation's supply of physicians?
As little as a year ago, the consensus among work force experts on all of these questions was that the government should take on this regulatory task. Although that position has had its critics,13 it was supported more or less in toto by the influential Council on Graduate Medical Education, by the equally influential Physician Payment Review Commission, and even by the American Association of Medical Colleges. It was explicitly incorporated in President Clinton 's Health Security Act. In the meantime, support for that position has waned, for at least two reasons.
First, the election of November 1994 is widely interpreted as a sign that the general public has lost faith in government's ability to fine-tune the health care sector in society's best interest. One may argue whether or not that lack of faith is justified, but it is now a political parameter that public policy will respect.
Second, the idea to regulate the size and composition of the nation 's health work force was born in an era when the providers of health care were compensated under a virtually open-ended fee-for-service system that literally rewarded them for artificially stimulating the demand for their services. In that world, our health professional schools could produce whatever mix of professionals pleased them. These schools could be certain that, within very broad limits, the market would absorb whatever mix of professionals they produced.
That world is fast disappearing. It is being replaced by networks of mini-health systems whose revenue comes in the form of a flat capitation payment
and which, therefore, operate strictly as cost centers whose income falls with the resource intensity of medical treatments. In these cost centers, physicians along with other health professionals have the status of employees or of quasi-employees whose contracts can be canceled at will by the network. In that world, the mix of health professionals that will find gainful employment in health care will be dictated by the managers of the capitated health care networks. It is not clear why that role needs to be complemented by the highly intrusive government regulation proposed in the Health Security Act. If government does seek a constructive role in this new health care market, it should collect and disseminate reliable information on the markets for the health work force. Potential entrants into the field—for example, college undergraduates—can then make their career decisions fully informed of the risks they confront in health care. That approach would put health work force policy on a par with public policy toward the other learned professions.14
At this time, American medical schools annually move close to 17,000 medical graduates into residency training. An additional 3,000–4,000 residency slots are filled with IMGs. Even if it were decided not to have government regulate the capacity of American medical schools and the composition of residency slots, there is the question whether the United States is well served by its open-door policy toward IMGs. As noted, in the short run these physicians do fill an acute need for affordable labor at some of the nation's inner city hospitals. In the long run, however, they will continue to add to the projected physician surplus. Does this make sense?
If the number of physicians in the United States is to be limited at all through government intervention, would not a logical first step be to reduce or to eliminate the influx of IMGs, preserving the privilege of medical practice for graduates from American medical schools? That proposal has a strong resonance among American parents and their offspring, but it does not have a compelling economic logic. It has not been demonstrated that IMGs who pass all the examinations imposed on American medical graduates are somehow less well qualified to practice medicine in this country than are their American counterparts. Proposals to limit the influx of IMGs tend to appeal to the nationalistic impulses that so often propel trade restrictions (e.g., the steel, textile, and automobile industries). If one adopts strictly the viewpoint of American consumers, IMGs actually are a relatively cheaper source of human capital than are American graduates, because a good part of the imported human capital has been financed abroad and comes to the United States gratis.
In short, the proper public policy toward IMGs is actually far more complex, even at the conceptual level, than it might appear at first blush. Extensive research and public debate are warranted before any new policy is implemented.
CONCLUDING OBSERVATIONS
Limits of space have confined this essay to a rather broad survey of the major questions that have driven health work force policy in the past and that will occupy it in the future. After lying almost dormant for close to two decades, work force policy has once again moved closer to center stage as the government grapples with the problem of financing health professional education, and as the institutions providing that education grapple with ever more tightly constrained budgets. Although these issues will be explored by a number of institutions, it is to be hoped and it can be expected that the IOM will continue to be a major contributor to that inquiry and debate, as it has been so effectively in the past.
Indeed, at the risk of appearing self-congratulatory, it is appropriate to mention that the Institute constitutes a remarkable bargain for the rest of society. Its members bring to the table an extraordinarily diverse, wide expertise that is quite deep. They donate that expertise freely to the many studies undertaken by the Institute, without any compensation other than the satisfaction of making a social contribution and of sharing some time with highly intelligent colleagues. To appreciate the extraordinary leverage the Institute provides its clients, one need only imagine the total that would obtain if every member of every study panel featured by the Institute billed his or her time at the hourly rate customary among Washington lawyers or at the rates the members could (and sometimes do) charge as expert witnesses in the tort system.
NOTES
1. In this connection, see Eli Ginzberg, “The physician shortage reconsidered,” The New England Journal of Medicine 252(2):85–7, 1966; Rashi Fein, The Doctor Shortage: An Economic Diagnosis, Washington, D.C.: The Brookings Institution, 1967; and Uwe E. Reinhardt, Physician Productivity and the Demand for Health Manpower, Cambridge, Mass.: Ballinger, 1974.
2. See Uwe E. Reinhardt, ibid.; and Kenneth R. Smith, Marianne Miller, and Frederick L. Golloday, “An analysis of the optimal use of inputs in the production of medical services,” Journal of Human Resources 7(2):208–52, 1972.
3. For a more detailed discussion, see Uwe E. Reinhardt, “Health manpower forecasting: The case of physician supply,” pp. 234–83 in Eli Ginzberg, ed., Health Services Research: Key to Health Policy, Cambridge, Mass.: Harvard University Press, 1991.
4. See, for example, Katherine Langwell, “Factors affecting the incomes of men and women physicians: An exploratory analysis,” Journal of Human Resources 17(2):261–75, 1982.
5. See, for example, Uwe E. Reinhardt, “The GMENAC forecast: An alternative view,” American Journal of Public Health, 71(10):1149–57, 1982.
6. For an excellent example of such an analysis, see William B. Schwartz, Frank A. Sloan, and Daniel MN. Mendelson, “Why there will be little or no physician surplus between now and the year 2000,” The New England Journal of Medicine 318(14):892–7, 1988.
7. Donald E. Yett, Leonard Drabek, Michael D. Intriligator, and Larry T. Kimball, “The Use of An Econometric Model to Analyze Selected Features of National Health Insurance” (mimeographed), Los Angeles: The University of Southern California, 1971.
8. Jonathan P. Weiner, “Forecasting the effects of health reform on U.S. physician requirements: Evidence from HMO staffing patterns,” Journal of the American Medical Association 272(3):222–30, 1994.
9. A careful analysis of this problem is provided in Robert H. Ebert and Eli Ginzberg, “The reform of medical education,” Health Affairs 7(Suppl.):5–38, 1988. See also Uwe E. Reinhardt, “An economist's perspective,” pp. 96–103 in the same volume.
10. For a lengthier discussion of these issues, see Uwe E. Reinhardt, “Planning the nation's health work force: Let the market in,” Inquiry 31(Fall):250–63, 1994.
11. For a collection of thoughtful essays on this topic, see Barbara Castel and David E. Rogers, eds., Clinical Education and the Doctor of Tomorrow, New York: New York Academy of Medicine, 1989.
12. Robert H. Ebert and Eli Ginzberg, op. cit., note 9.
13. See Uwe E. Reinhardt, op. cit., note 10.
14. For further detail on this proposal, see Uwe E. Reinhardt, op. cit., note 10.





























