A History of Implants
Attempts to improve the look of the breast by augmenting its size and shape date back to the late 1880s. Among the materials inserted in breasts early on were ivory, glass balls, ground rubber, ox cartilage, and sponges, sacs, and tapes made from various synthetic substances. Later came rubber, Teflon, and silicone.
Some breasts were augmented by injection. In the 1940s, an array of liquid substances were injected into the breast, such as paraffin and petroleum jellies. Later, industrial silicone fluid and medical-grade silicones were injected into the breast by unlicensed practitioners, sometimes in staggering amounts. These methods of breast injection caused pain, skin discoloration, ulceration, infection, disfigurement, breast loss, liver problems, respiratory distress and pulmonary embolism, and even coma and death. The frequency of capsular contracture with presilicone implants may have reached 100%. Between 12,000 and 40,000 women received breast injections in Las Vegas before the procedure was declared a felony under Nevada state law in 1976.
MODERN GENERATIONS OF IMPLANTS
In 1963, Dow Corning Corporation introduced the first silicone-gel-filled implant. The earliest Dow shells had a high-molecular-weight “gum ” filled with amorphous silica, and the gel in the implant was platinum cured. By the early 1970s, the Dow Corning Dacron-patched implant had achieved stunning popularity, accounting by one estimate for 88% of all implants sold.
These early implants had thick shells and gels. The silicone rubber elastomer shell usually had seams and a smooth surface. The inside contained a firm silicone gel and fluids. Rupture rates were low because of the tough shell, but complications from capsular contracture were common and gel-fluid seepage was probably considerable.
Some implants had internal dividers to keep the gel from sagging into the central part of the implant. Seal patches were used to close up any holes or slits left by manufacturers or the valve entrance to an expander, and are still used for manufacturing today's seamless implants.
By the late 1960s, Dow's shells had become less thick and were seamless. And in 1968, Heyer Schulte Corporation became the first domestic manufacturer of saline-filled implants. Early saline implants were fragile and heavy, with audible “sloshing,” and there was a very high deflation rate of up to 76%, probably because of the high-temperature vulcanizing process used to “cure ” or strengthen the contents.
The original thick-shell models were replaced in the 1970s and early 1980s by implants with thin shells. But these had a greater tendency to rupture and deflate. These “second-generation” implants were generally smooth surfaced and had high contracture and gel-fluid seepage rates. More flexible gels were introduced by various companies from 1972 to 1975, and thinner elastomer shells were introduced starting in 1972.
Another development in the 1970s was a polyurethane foam coating on the implant shell. This coating appeared to reduce contracture and was popular; an estimated 110,000 women or more received this type of implant before it was discontinued in 1991. The polyurethane coating appeared to diminish capsular contracture by causing an inflammatory reaction. This reaction discouraged formation of fibrous tissue around the capsule. But the polyurethane coating started disintegrating almost immediately, so that what eventually remained was a mostly smooth implant surrounded by a capsule containing foam fragments. Pain, fluid accumulation, and infection were reported. The foam fragments were one reason a polyurethane-coated implant was difficult to
remove. There is no hard evidence to support the idea that the polyurethane foam could lead to cancer. Beginning in the mid-1980s, most implant models were sold with a textured shell surface. The theory of texturing was similar to that of a polyurethane coating; that is, the growth of tissue into the irregular spaces of the shell would prevent collagen and other fibrous tissue from forming excess growth around the implant capsule.
Textured implants might also encourage the development of synovium, a thin membrane that secretes synovial fluid, a clear, sticky substance. Synovium may be a natural result of friction from the movement common in all breast implants.
Another innovation in the second-generation implants was the “double lumen.” These implants had two cavities and two shells, which were either “patched” together or had one shell floating freely inside the other. The double lumen was an attempt to provide the cosmetic benefits of gel in the inside cavity, while the outside lumen contained saline and could be used for an expander or even for injections of antibiotics or steroids. The saline lumen was also thought to control contracture and gel and fluid seepage or rupture, but studies over the years have largely disproved such theories.
Various types of expanders evolved over the years, some of them with permanent valves. A barrier coating on the inside of the shell was developed in the 1980s to help prevent silicone-gel “bleeding” or seepage. Rupture frequencies for silicone-gel implants were as follows:
-
first generation (from 1963 to 1972)—very low,
-
second generation (from 1972 to mid-1980s)—50 to 95% after 12 or more years, and
-
third generation (from mid-1980s to present)—still uncertain, but possibly about 10% in 5 years.
This modern third generation of implants, which dates from the mid-1980s, also saw improved silicone-gel implants, saline implants with much better deflation rates, and stronger shells with barrier layers and texturing. Although these data are incomplete, this generation of implants may offer lower rates of deflation and rupture, fewer contractures, and less gel diffusion or “bleeding.”
There was no standard breast implant in America. Since 1962, there have been some 240 different types, made by at least 10 manufacturers. Given variations in sizes, shapes, types of valves and patches, gels, and shells, one estimate puts at 8,300 the number of different types of implants available with slight variations over the years.
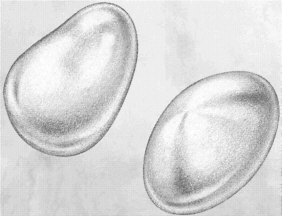
A majority of implants in place today are “single-lumen” (one-cavity) models filled with silicone gel. The shell (“elastomer”) is made of silicone rubber and has an inside barrier coating of fluorosilicone or a modified layer of elastomer to help prevent silicone fluid from escaping. The outside of the shell often has a textured surface; tissue grows into this surface, stimulating an inflammatory reaction. This inflammation can delay the development of the fibrous tissue that causes capsular contracture.
In the 1990s, saline-filled, single-lumen implants almost completely replaced the formerly popular gel-filled models because of the 1992 PDA moratorium on the use of silicone gel. In addition, the popularity of immediate implant reconstruction after mastectomy has grown, from 3% of implants in 1983 to more than 25% in 1992. Reconstruction with implants reached its zenith of 40% of all implants in 1990; since then, more women have chosen to have a breast constructed out of tissue from other parts of the body (the “flap” form of reconstruction). But this is a more difficult operation and not suitable for all women.
It remains to be seen whether implants of this third generation will continue to be used or if forthcoming study results (and FDA decisions) will bring about still another generation of implants. Furthermore, there is less information available about saline implants than silicone-gel implants—silicone gel was the “fill of choice” until the 1990s. Saline implants contain a harmless saltwater solution, cannot have silicone leakage (because they don't contain silicone), and appear to have lower rates of capsular contracture. Still, the jury will be out until more studies are forthcoming.





