HEALTH RISK ASSESSMENT FOR NERVE AGENT GD (SOMAN)
DRAFT REPORT
September 1996
(editorial corrections made April 1997)
Prepared for
Environmental Risk Assessment Program
Strategic Environmental Research Development Program
Prepared by
Life Sciences Division
OAK RIDGE NATIONAL LABORATORY*
Oak Ridge, Tennessee 37831
Submitted to
Material Chemical Working Group
Advisory and Coordinating Committee
Environmental Risk Assessment Program Strategic Environmental Research Development Program
PREFACE
This report assesses the potential non-cancer and cancer effects of chemical agent GD (CAS No. 96-64-0).
This document supports the activities of the Material/Chemical Risk Assessment Working Group of the Environmental Risk Assessment Program, a cooperative endeavor of the Department of Defense, Department of Energy, and Environmental Protection Agency. This working group is developing toxicity values for selected chemicals of concern at federal facilities. Toxicity values will be submitted for consideration by the EPA's IRIS Consensus Process for inclusion on IRIS (EPA's Integrated Risk Information System). The Material/Chemical Risk Assessment Working Group consists of Drs. Jim Cogliano (chair) and Harlal Choudhury (U.S. EPA), Dr. Bruce Briggs (Geo-Centers); Lt. Cmdr. Warren Jederberg and Dr. Robert L. Carpenter (U.S. Naval Medical Research Institute); Dr. Elizabeth Maull and Mr. John Hinz (U.S. Air Force Occupational and Environmental Health Directorate); Drs. Glenn Leach and Winnie Palmer (U.S. Army Center for Health Promotion and Preventive Medicine); Drs. Robert Young and Po-Yung Lu (Oak Ridge National Laboratory).
This document was written by Dr. Robert A. Young, Life Sciences Division, Oak Ridge National Laboratory, Oak Ridge, TN. Internal peer review was provided by Dr. Robert Young, Dr. Annetta Watson, and Mr. Robert Ross.
TABLE OF CONTENTS
LIST OF TABLES
|
Table 1. |
RBC-ChE Activity in Different Species |
|||
|
Table 2. |
Lethality Data for Agent GD |
|||
|
Table 3. |
RBC-ChE Levels in 90-Day Subchronic Study of GD |
|||
|
Table 4. |
Plasma-ChE Levels in 90-Day Subchronic Study of GD |
|||
|
Table 5. |
GD-Induced RBC-AChE Inhibition in Female Rats |
|||
|
Table 6. |
GD-Induced RBC-AChE Inhibition in Male Rats |
|||
|
Table 7. |
GD-Induced Plasma-AChE Inhibition in Female Rats |
|||
|
Table 8. |
GD-Induced Plasma-AChE Inhibition in Male Rats |
1.
INTRODUCTION
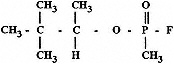
Military nerve agents are organophosphate compounds containing either a fluorine, sulfur, or cyanide substituent group (Dacre, 1984). GD contains a fluoride substituent group (GA contains a cyanide substituent group and VX a sulfur group). The chemical synonyms, Chemical Abstract Service (CAS) and Army identification numbers (DA, 1974; Dacre, 1984), and chemical formula for GD are as follows:
|
Agent GD: |
Methylphosphonofluoridic acid, 1,2,2-trimethylpropyl ester; Pinacoloxymethylphosphoryl fluoride; Pinacolyl methylphosphonofluorididate; Soman CAS No. 96-64-0; |
1.1 PHYSICAL/CHEMICAL PROPERTIES
Agent GD is a colorless liquid with a molecular weight of 182.2 (DA, 1974); it has a vapor density of 6.3 (air = 1) and a liquid density of 1.02 g/mL at 25°C (DA, 1974). The vapor pressure of GD is 0.4 mm Hg at 25°C. In distilled water it has a solubility of 21 g/L at 20°C (DA, 1974).
1.2 ENVIRONMENTAL FATE
1.2.1 Air
Data specifically regarding the fate of GD in the atmosphere were not located. However, because of its volatility, GD is expected to disperse realtively quickly.
1.2.2 Water
Agent GD may hydrolyze to relatively nontoxic hydroflouric and pinacolyl methylphosphonic acids (MacNaughton and Brewer, 1994; Rosenblatt et al., 1995). The hydrolysis rate is a function of temperature and pH; the rate is minimum between pH 4 and 6. The t1/2 for GD is approximately 100 hours with 20 × t1/2 being required to attain a 1 × 106 reduction in GD concentration.
1.2.3 Soil
GD is likely to undergo hydrolysis in most soils. As noted above, the rate of hydrolysis will be dependent upon temperature and pH. According to Morrill et al. (1985), evaporation is the primary mechanism for the loss of the GA and GB nerve agents from soil. Although the G agents are liquids under ordinary environmental conditions, their relatively high volatility and vapor pressure permits them to be disseminated in vapor form. Because of this volatility, GD is not expected to persist in soils.
2. MECHANISM OF ACTION
Nerve agents are inhibitors of acetylcholinesterase (AChE), an enzyme responsible for deactivating the neurotransmitter acetylcholine (AChE) at some neuronal synapses and myoneural junctions. By a mechanism of phosphorylation, nerve agents act as substrates for the enzyme thereby preventing deactivation of acetylcholine. The organophosphate-inhibited enzyme can be reactivated by dephosphorylation, but this occurs at a rate that is slower than the rate of reactivation of acetylcholine (deactivated by acetylcholinesterase). Consequently, there is a depletion of acetylcholinesterase and a buildup of acetylcholine. In addition, the nerve agent-enzyme complex can also undergo an ''aging" process (thought to be due to a loss of an alkyl or alkoxy group), whereby it becomes resistant to dephosphorylation (see review by Munro et al., 1994). Differences in rates of aging and reactivation may be important in evaluating toxicity data especially when extrapolating from animal studies to humans. In vitro tests conducted by Grob and Harvey (1958) indicate that both GA and GB combine with cholinesterase almost irreversibly during the first hour of their reaction. Sidell and Groff (1974) reported that the GB-ChE complex ages very rapidly in vivo, with 45–70% completion by 5 hours after infusion. In contrast, the complex formed between ChE and the nerve agent VX does not age significantly, and the rate of spontaneous reactivation can be as fast as 1%/hr in humans (Sidell and Groff, 1974).
2.1 Effects of Organophosphate Agents on the Nervous System
The anticholinesterase effects of the organophosphate nerve agents can be characterized as being muscarinic, nicotinic, or central nervous system (CNS)-related. Muscarinic effects occur in the parasympathetic system (bronchi, heart, pupils of the eyes; and salivary, lacrimal and sweat glands) and result in signs of pulmonary edema, bradycardia, miosis, tearing, and sweating. Nicotinic effects occur in somatic (skeletal/motor) and sympathetic systems, and result in muscle fasciculation, muscle weakness, tachycardia, and diarrhea. Effects on the CNS by organophosphates are manifested as giddiness, anxiety, emotional lability, ataxia, confusion, and depression (O'Brien, 1960).
Although the inhibition of cholinesterase within neuro-effector junctions or the effector itself is thought to be responsible for the major toxic effects of organophosphate agents, these compounds can apparently affect nerve-impulse transmission by more direct processes as well. Direct effects may occur on excitable tissues, receptors, and ionic channels. According to Somani et al. (1992), the direct action of nerve agents on nicotinic and muscarinic ACh receptors may occur when concentrations in the blood rise above micromolar levels, whereas at lower levels the action is mainly the result of inhibition of AChE. Albuquerque et al. (1985) have shown that agent GA, as well as agents GB and GD are capable of changing receptor sites in a manner similar to that exhibited by acetylcholine, which promotes the conductance of electrophysiological signals associated with stimulation of neuromuscular function. VX "may directly affect a small population of muscarinic ACh receptors that have a high affinity for [3H]-cis-methyldioxalane binding" (Somani et al., 1992). VX may also counteract the effects of ACh by acting as an open channel blocker at the neuromuscular junction, thereby interrupting neuromuscular function (Rickett et al., 1987).
Exposure to some organophosphate cholinesterase inhibitors results in a delayed neuropathy characterized by degeneration of axons and myelin. This effect is not associated with the inhibition of acetylcholinesterase, but rather with the inhibition of an enzyme described as neuropathy target esterase (NTE); however, the exact mechanism of toxicity is not yet fully understood (Munro et al., 1994). For some organophosphate compounds, delayed neuropathy can be induced in experimental animals at relatively low exposure levels, whereas for others the effect is only seen following exposure to supralethal doses when the animal is protected from the acute toxic effects caused by cholinesterase inhibition.
Although there is the potential for nerve agents to have direct toxic effects on the nervous system or to cause delayed neuropathy, there is no evidence that such effects occur in humans at doses lower than those causing cholinesterase inhibition. However, it should be noted that there is very little animal or human data evaluating the potential effects of long-term exposure to low doses. Nevertheless, for the purpose of evaluating potential health effects, inhibition of cholinesterase is generally considered the most useful biological endpoint.
2.2 Effect on Blood Cholinesterases
In addition to being found in the nervous system, acetylcholinesterase also occurs in the blood where it is bound to the surface of red blood cells (termed RBC-ChE or RBC-AChE). RBC-AChE activity, as well as the activity of a second type of cholinesterase found in blood plasma (butyrylcholinesterase, or plasma cholinesterase) have been used to monitor exposure to organophosphate compounds (pesticides and nerve agents). Because ACh is the primary neurotransmitter of the nervous system, changes in RBC-AChE activity are generally considered to be the more appropriate bioindicators of potential effects (Morgan, 1989). There is also evidence that RBC-AChE is as sensitive as brain ChE to the effects of nerve agents. Grob and Harvey (1958) reported that the in vitro concentrations producing 50% depression of brain-ChE and RBC-AChE activity were the same in the case of GA (1.5 × 10-8 mol/L), and only slightly different (3 × 10-9 mol/L and 3.3 × 10-9 mol/L) in the case of GB. However, in vivo animal studies indicate a poor correlation between brain and RBC-AChE in cases of acute exposures (Jimmerson et al., 1989), and this is reflected in the fact that blood cholinesterase activity may not always be correlated with exposure or with signs and symptoms of toxicity (Holmstedt, 1959). Acute exposures to high concentrations may cause immediate toxic effects before significant changes occur in blood ChE activity, and repeated exposures over a period of several days or more may result in a sudden appearance of symptoms due to cumulative effects (Grob and Harvey, 1958). Conversely, blood ChE activity can become very low without overt signs or symptoms during chronic exposures to low concentrations of organophosphates. This may be due to a slower rate of recovery of RBC-AChE compared to tissue ChE, or to noncholinesterase-dependent recovery pathways for neural tissue (Grob and Harvey, 1958). Sumerford et al. (1953) reported that orchard workers exposed to organophosphate insecticides had RBC- and plasma-ChE values as low as 15% of normal values without any other signs or symptoms of exposure. Animal studies have demonstrated that chronic exposures to low concentrations of organophosphate insecticides and nerve agents can result in increased tolerance levels (Barnes, 1954; Rider et al., 1952; Dulaney et al., 1985). Similarly, Sumerford et al. (1953) reported increased levels of tolerance to organophosphate insecticides in people living near orchards treated with organophosphate insecticides. Such adaptation may result from increased rates of formation of blood ChE, or from increased rates of detoxification. Additional information on the development of tolerance to organophosphate cholinesterase inhibitors can be found in a review paper by Hoskins and Ho (1992).
The blood cholinesterases may, to some degree, provide a protective effect by binding with some fraction of the anticholinesterase compound (Wills, 1972). However, not all nerve agents bind equally well with all cholinesterases. In tests conducted on dogs, Holmstedt (1959) found that GA affected RBC and plasma cholinesterase to a nearly equal degree. In contrast, agent VX preferentially inhibits RBC-AChE (70% compared with about 20% inhibition of plasma ChE) (Sidell and Groff, 1974). Rodents (but not humans) have other enzymes in the blood, termed aliesterases, which can bind organophosphates, thereby reducing the amount available for binding with acetylcholinesterase (Fonnum and Sterri, 1981). Agent GB binds with aliesterases; however, according to Fonnum and Sterri (1981), VX has a quartenary ammonium group which prevents it from being a substrate for aliesterases. The strong specificity of agent VX to AChE may account, in part, for the fact that it is much more acutely toxic than agents GA and GB (Munro et al., 1994).
2.2.1 Intra- and Interspecies Variation in Blood Cholinesterase Activity
Although blood cholinesterase activity is used as a measure of exposure to organophosphate compounds, baseline activity levels can vary between individuals and between species. According to Wills (1972), both plasma- and RBC-AChE activity are generally lower in women than in men. Sidell and Kaminskis (1975) reported that, for a test population of 22 human subjects, the highest coefficient of variation of RBC-AChE was 4.1% per single subject; the average range of variation was ± 2.1% for men and ± 3.1% for women. In individuals studied for one year, the RBC-AChE activity varied by 11% in men and 16% in women. Yager et al. (1976) reported a 10.0% intra-individual coefficient of variation for RBC-AChE and 14.4% for plasma-ChE. Callaway et al. (1951) estimated that with only one preexposure measurement, the smallest measurable decrease was 15% of the baseline value for RBC-AChE activity and 20% of the baseline for plasma-ChE.
A small subpopulation of men and women have a genetic defect causing their blood cholinesterase activity to be abnormally low (Evans et al., 1952; Harris and Whitaker, 1962). For homozygous individuals, the activity can be as low as 8–21% of the normal mean (Bonderman and Bonderman, 1971). Morgan (1989) suggests that these individuals may be unusually sensitive to organophosphate anticholinesterase compounds.
Data compiled by Ellin (1981) reveal that the RBC-AChE activity for humans is slightly higher than that for monkeys and much higher than that for rats and other laboratory animals (Table 1). These differences in RBC-AChE activity may affect a species' sensitivity to a particular organophosphate compound. At the same time, the relative amount of plasma cholinesterase and other compounds in the blood that can bind to the organophosphate agents must also be considered. For example, rodents, but not humans, have high levels of aliesterases (AE) in the blood, and these compounds may provide rats and mice with a higher level of resistance to some anticholinesterase compounds (McNamara and Leitnaker, 1971).
2.2.2 Potency of Nerve Agents as Cholinesterase Inhibitors
The potency of the anticholinesterase activity of nerve agents and other organophosphates is expressed by the bimolecular rate constant (ki) for the reaction of the phosphate compound with the enzyme and by the molar concentration causing 50% inhibition of the enzyme when tested in vitro (I50). I50 data for several organophosphate nerve agents have been tabulated by Dacre (1984). The relationship between I50 and ki as a function of time (t) is expressed by the following equation (Eto, 1974):
(1)
Table 1. RBC-ChE Activity in Different Species
|
Species |
RBC-ChE activity (µmol/mL/min) |
Optimum substrateaconcentration (M) |
|
Human |
12.6 |
2 × 10-3 |
|
Monkey |
7.1 |
2 × 10-3 |
|
Pig |
4.7 |
1 × 10-3 |
|
Goat |
4.0 |
2 × 10-3 |
|
Sheep |
2.9 |
2 × 10-3 |
|
Mouse |
2.4 |
2 × 10-3 |
|
Dog |
2.0 |
2 × 10-2 |
|
Guinea pig |
2.7 |
2 × 10-3 |
|
Rabbit |
1.7 |
5 × 10-3 |
|
Rat |
1.7 |
5 × 10-3 |
|
Cat |
1.5 |
5 × 10-3 |
|
Source: Ellin, 1981 a Acetylthiocholine iodide concentration for maximum RBC-ChE activity. |
||
The pI50 (negative log of the molar concentration causing 50% inhibition) for GD is 9.2 as reported by Dacre (1984).
Relative potency of nerve agents can also be expressed in terms of the in vivo dose necessary to produce the same level of cholinesterase inhibition by a specific exposure route. As would be expected, the effectiveness of the agents in inhibiting cholinesterase is closely correlated with their acute toxicity (see Appendix A).
3. TOXICOLOGY
3.1 Introduction
Health and environmental impacts of nerve agents and related compounds (organophosphate insecticides) have been reviewed by O'Brien (1960), Matsumura (1976), Dacre (1984), Carnes and Watson (1989), Watson et al. (1989), and Munro et al. (1994). A brief general discussion of the toxicology of nerve agents and related organophosphate pesticides is given below.
Nerve agents are acutely toxic by all routes of exposure. Initial symptoms of acute poisoning are fatigue, headache, mild vertigo, weakness, and loss of concentration. Moderate exposures result in miosis and excessive sweating, tearing, and salivation. Acidosis and hyperglycemia may also occur in addition to muscular weakness, muscular twitching, lacrimation, urination, and defecation. Acute poisoning can result in prostration, clonic convulsions (rapid repetitive movements) and tonic convulsions (limbs stretched and rigid) (Matsumura, 1976). Exposures sufficiently high to cause convulsions have resulted
in brain lesions and cardiomyopathy in laboratory animals (Singer et al., 1987).
In addition to the immediate toxicity of the nerve agents, there is concern that exposures may lead to chronic neurological effects similar to those reported for some organophosphate insecticides. Included among these possible effects are organophosphorus-induced delayed neuropathy (OPIDN), EEG changes, and long-term psychological disturbances (Munro et al., 1994). OPIDN, which appears 5–30 days after exposure, manifests itself as muscle weakness, tingling, and twitching followed by paralysis (Munro et al., 1994). Histopathological changes, which consist of degeneration of axons and myelin of the nervous system, can be correlated, not with inhibition of acetylcholinesterase, but rather with inhibition of NTE; however, the exact mechanism of toxicity is not yet fully understood (Munro et al., 1994). OPIDN has not been observed in humans exposed to the nerve agent GD, however, it has been demonstrated that GB can induce this effect in chickens (a species which is normally used to test for OPIDN) (Gordon et al. 1983). The GB IC50 for NTE inhibition was 0.1 µM, a concentration considerably higher than known lethal concentrations in chickens (Willems et al., 1984).
Acute exposures to nerve agents are known to cause EEG changes (Grob and Harvey, 1958; Sidell, 1992) which may persist for long periods of time after exposure (Metcalf and Holmes, 1969; Duffy et al., 1979; Duffy and Burchfiel, 1980); however, the reported changes have been considered to be clinically insignificant and not correlated with behavioral or physiological changes (DHHS, 1988). Acute exposures can also induce neuropsychological changes; however, there is no evidence of these effects persisting for months or years as has been reported for some organophosphate insecticides (Savage et al., 1988; Gershon and Shaw, 1961; Mick, 1974; Rodnitzky, 1974; Wagner, 1983; Tabershaw and Cooper, 1966). The available data for the organophosphate insecticides suggest that chronic neuropsychological effects (excluding OPIDN) do not occur in the absence of significant changes in blood cholinesterase. The same conclusion may apply to the organophosphate nerve agents.
3.2 Short-term Toxicity
Bucci et al. (1992a) conducted range finding studies with GD. The test material was administered by gavage to male and female CD rats once per day, 5 days per week for 2 weeks. These studies indicated that the maximum tolerated dose was 70 µg/kg/day and a dose of 300 µg/kg/day was lethal to 100% of the test animals.
In a study by Blick et al. (1994), rhesus monkeys were administered GD (soman) parenterally daily for 5 days. The effects of the treatment on performance of a well-learned, compensatory trackning task was assessed, and an ED50 of 0.97 µg/kg/day for decrement in this performance was obtained. This decrement in performance was concurrent with a 85–90% inhibition of serum ChE. The 0.97 µg/kg/day dose was about 40% of the single acute dose required to produce a similar performance decrement. It was also noted that the single acute dose (2.43 µg/kg) was associated with a 65–70% serum ChE inhibition.
Acute lethality data for GD are summarized in Table 2.
Table 2. Lethality Data for Agent GD
|
Exposure route |
Species |
LD50(µg/kg) |
References |
|
oral |
human |
5–20 (est.) |
Somani et al., 1992 |
|
percutaneous |
human |
50–300 (est.) |
Somani et al., 1992 |
|
intravenous |
mouse |
42 |
Tripathi and Dewey, 1989 |
|
|
dog |
10 |
Abbrecht et al., 1989 |
|
subcutaneous |
rabbit |
20 |
Harris et al., 1984 |
|
|
guinea pig |
26–30 |
Sterri, 1981; Maxwell et al., 1987b; |
|
|
|
|
Anderson et al., 1989; Sparenborg et al., 1989 |
|
|
rat |
70–165 |
Somani et al., 1986; Petrali, 1989; Maxwell et al., 1987a, 1987b; Lennox et al., 1985 |
|
intramuscular |
monkey |
3.8–15.3 |
Petras, 1984; Baze, 1993; Wall et al., 1990; |
|
|
|
|
Switzer et al., 1980 |
|
|
rabbit |
15 |
Olson et al., 1989 |
|
|
mouse |
98 |
Jones et al., 1984 |
3.3 Subchronic Toxicity
In a subchronic study conducted by the National Center for Toxicological Research (Bucci et al., 1992a), male and female CD rats (12/sex/group) were administered GD by gavage at dose levels equivalent to 17.5, 35.0 and 70 µg GD/kg/day. The doses were given once per day, 5 days per week for 13 weeks. All animals were observed daily for clinical signs of toxicity and weighed weekly. Necropsy examination was performed on all animals. Terminal body and organ weights were recorded. Microscopic evaluation was performed on all high-dose and control animals, and on those tissue of lower dose animals that were abnormal at necropsy. Hematological analyses and clinical chemistry (including RBC and plasma cholinesterase) were evaluated in the same 6 male and 6 female rats in each dose group one week before the exposures began and also at weeks 1, 3, 7, and 13. In addition, at necropsy a hemisection of each brain was prepared and tested for NTE.
Relative to untreated controls, the group mean body weight gain was significantly decreased (p<0.001) in the high-dose (70 µg/kg/day) males (b.w. change 160.9 in controls vs. 83.7 g). A decrease in body weight gain also occurred in female rats (75 vs 59 g decrease for high-dose and controls, respectively) but the difference was not statistically significant. A definitive dose-response was not present in either males or females.
Although changes were observed in some clinical chemistry and hematologic parameters, the changes were spurious, not dose-related and were not biologically relevant. Brain NTE was not altered in rats dosed with GD. Histopathological examinations revealed no gross or microscopic findings that could be attributed to treatment with GD. Special attention was given regarding intercostal and cardiac muscle lesions, and neurological lesions which have been previously reported in rats treated with GD (McLeod, 1985; Singer et al., 1987). However, none of these lesions was observed in GD-treated rats.
RBC-AChE and plasma-ChE levels are shown in Tables 3 and 4. Considerable variability was noted among the control and treatment group baseline values. A dose-related decrease in plasma-ChE levels in both male and female rats was observed for weeks 1 and 7. Relative to untreated rats, significant (p<0.05) depression of plasma cholinesterase levels was observed in both males and females of the high-dose group during week 1 (25% and 33% for males and females, respectively) and week 7 (20% and 33% for males and females, respectively), and in males of the 35 µg/kg/day group during week 7 (28%). In females, the plasma-AChE levels exceeded pretreatment (baseline) values by week 13 but remained depressed (54%, 66%, and 50% in the low, mid, and high dose groups, respectively) in males at week 13 although not significantly so. Upon comparing treatment groups with controls, no significant changes in RBC-AChE levels were noted by the study authors. Data for week 3 were highly variable and appear to reflect inaccuracies or problems with the AChE assay procedure.
Table 3. RBC-ChE Levelsa in 90-Day Subchronic Study of GD in CD Ratsa
|
|
|
Week of treatment |
||||||||
|
Dose (µg/kg/d) |
Sex |
-1 |
1 |
%b |
3 |
%b |
7 |
%b |
13 |
%b |
|
0 |
F |
1609(252) |
2461(136) |
153 |
2497(186) |
155 |
1674(127) |
104 |
1341(397) |
83 |
|
17.5 |
F |
1462(153) |
2445(191) |
167 |
1790(144) |
122 |
1236(201) |
85 |
1313(280) |
89 |
|
35.0 |
F |
1466(167) |
2244(179) |
153 |
1817(127) |
124 |
1381(90) |
94 |
1310(280) |
89 |
|
70.0 |
F |
1025(152) |
2544(367) |
250 |
1695(52) |
165 |
1556(96) |
152 |
1296(168) |
126 |
|
0 |
M |
1955(108) |
2340(149) |
119 |
2043(212) |
105 |
2323(116) |
119 |
1904(106) |
97 |
|
17.5 |
M |
1764(158) |
1862(95) |
106 |
1211(125) |
69 |
1784(90) |
101 |
1774(161) |
100 |
|
35.0 |
M |
1977(78) |
1820(153) |
92 |
1435(320) |
73 |
1681(28) |
85 |
1562(68) |
79 |
|
70.0 |
M |
1859(142) |
1964(205) |
105 |
973(48) |
52 |
1753(139) |
94 |
1720(148) |
92 |
|
Source: Bucci et al., 1992a a Values given as mean IU/L and (SEM) b Percent of baseline |
||||||||||
Table 4. Plasma-ChE Levelsa in 90-Day Subchronic Study of GD in CD Ratsa
|
|
|
Week of treatment |
||||||||
|
Dose (µg/kg/d) |
Sex |
-1 |
1 |
%b |
3 |
%b |
7 |
%b |
13 |
%b |
|
0 |
F |
1401(148) |
1542(175) |
110 |
437(52) |
31 |
1976(198) |
141 |
2959(358) |
190 |
|
17.5 |
F |
1571(322) |
893(185) |
57 |
1131(422) |
72 |
968(109) |
61 |
2275(320) |
145 |
|
35.0 |
F |
1560(207) |
593(50) |
38 |
337(80) |
22 |
673(96) |
43 |
2303(179) |
148 |
|
70.0 |
F |
1344(190) |
446(81)* |
33 |
950(180) |
71 |
439(40)c* |
33 |
1951(179) |
145 |
|
0 |
M |
543(51) |
377(44) |
69 |
685(290) |
126 |
340(18) |
63 |
431(39) |
78 |
|
17.5 |
M |
631(131) |
245(29) |
39 |
500(293) |
79 |
204(19) |
32 |
339(34) |
54 |
|
35.0 |
M |
632(47) |
198(16) |
31 |
276(63) |
44 |
174(14)* |
28 |
414(32) |
66 |
|
70.0 |
M |
610(98) |
153(11)* |
25 |
370(59) |
61 |
122(7)* |
20 |
308(16) |
50 |
|
Source: Bucci et al., 1992a a Mean IU/L and (SEM) b Percent of baseline (week -1). * p<0.05, different from control value (0 µg/kg/day) |
||||||||||
The plasma- and RBC-AChE data from the Bucci et al. (1992a) study were re-analyzed by ORNL (using standard deviations) with ANOVA and Dunnett's and Scheffe's Comparisons. In the re-evaluation, RBC and plasma cholinesterase levels were compared to respective controls for the same sampling times as well as to the pre-exposure values within each group (Tables 5–8). This analysis also indicated an absence of definitive changes in RBC-AChE levels that could be attributed to GD treatment. During week 3 in females and week 7 in males, RBC-AChE levels of all GD treatment groups were significantly lower (p<0.05) than controls but the response did not exhibit a dose-relation in either group. In females during week 1, RBC-AChE levels in the control and all treatment groups were inexplicably elevated relative to baseline (week -1) values. For plasma-AChE, a dose-related significant decrease (p<0.05) relative to controls was detected during weeks 1 and 7 for both male and female rats. With the exception of high-dose females at week 3, a comparison of values to pre-exposure levels indicated that plasma-AChE levels of both the mid and high-dose groups were significantly (p<0.05) lower at weeks 1, 3, 7 and 13 for females and males. Under the conditions of this study, GD treatment appeared to affect plasma-AChE levels at a dose as low as 17.5 µg/kg as exemplified by the significant (p<0.05) decrease relative to controls and the reduction in plasma-ChE at week 1 to 39% of baseline in males and to 57% of baseline in females. For plasma-AChE, decreases in activity appeared to be dose-related. It is uncertain why similar findings were not observed for RBC-AChE.
Table 5. GD-Induced RBC-AChE Inhibition in Female CD Rats (Dunnett's Comparison)
|
|
Week |
||||
|
Dose (µg/kg/day) |
-1 |
1 |
3 |
7 |
13 |
|
0 |
1609 |
2461a |
2497aa |
1674 |
1341 |
|
17.5 |
1462 |
2445a |
1790b |
1236b |
1313 |
|
35.0 |
1466 |
2244a |
1817b |
1381 |
1310 |
|
70.0 |
1025b |
2544a |
1556 |
1296 |
|
|
Source: Bucci et al., 1992a a Significantly different (p<0.05) relative to pre-exposure baseline value (week -1) b Significantly different (p<0.05) relative to respective weekly control value. |
|||||
Table 6. GD-Induced RBC-AChE Inhibition in Male CD Rats (Dunnett's Comparison)
|
|
Week |
||||
|
Dose (µg/kg/day) |
-1 |
1 |
3 |
7 |
13 |
|
0 |
1955 |
2340 |
2043 |
2323 |
1904 |
|
17.5 |
1764 |
1862 |
1784b |
1774 |
|
|
35.0 |
1977 |
1820b |
1435a |
1681b |
1562 |
|
70.0 |
1859 |
1964 |
1753b |
1720 |
|
|
Source: Bucci et al., 1992a a Significantly different (p<0.05) relative to pre-exposure baseline value (week -1) b Significantly different (p<0.05) relative to respective weekly control value. |
|||||
Table 7. GD-Induced Plasma-AChE Inhibition in Female CD Rats (Dunnett's Comparison)
|
|
Week |
||||
|
Dose (µg/kg/day) |
-1 |
1 |
3 |
7 |
13 |
|
0 |
1401 |
1542 |
437a |
1976 |
2659a |
|
17.5 |
1571 |
893b |
1131 |
968b |
2275 |
|
35.0 |
1560 |
337a |
2303a |
||
|
70.0 |
1344 |
950 |
1951a |
||
|
Source: Bucci et al., 1992a a Significantly different (p<0.05) relative to pre-exposure baseline value (week -1) within treatment group. b Significantly different (p<0.05) relative to respective weekly control value. |
|||||
Table 8. GD-Induced Plasma-AChE Inhibition in Male CD Rats (Dunnett's Comparison)
|
|
Week |
||||
|
Dose (µg/kg/day) |
-1 |
1 |
3 |
7 |
13 |
|
0 |
543 |
377 |
685 |
340 |
431 |
|
17.5 |
631 |
245b |
500 |
204b |
339 |
|
35.0 |
632 |
276a |
414a |
||
|
70.0 |
610 |
370a |
|||
|
Source: Bucci et al., 1992a a Significantly different (p<0.05) relative to pre-exposure baseline value (week -1) within treatment group. b Significantly different (p<0.05) relative to respective weekly control value. |
|||||
3.4 Chronic Toxicity
There was no information concerning the effects of GD following chronic exposure.
3.5 Nervous System Effects
As noted in section 3.1, the neurotoxic effects following acute exposures to nerve agents such as GD can range from minor symptoms such as fatigue, headache, mild vertigo, weakness, and loss of concentration to convulsions, respiratory arrest and death.
Evidence of delayed neurotoxicity was not observed in the previously described rat study by Bucci et al. (1992a). A delayed neurotoxicity study in SPF white leghorn chickens was also negative (Bucci et al., 1992b).
3.6 Developmental and Reproductive Effects
There are no studies evaluating the developmental or reproductive effects of GD in humans or laboratory animals.
3.7 Carcinogenicity and Genotoxicity
No information is available regarding the potential carcinogenicity of agent GD in humans.
In a 90-day gavage study in rats, Bucci et al. (1992) found no neoplastic changes attributable to GD treatment. The study was, however, of insufficient duration to be suitable for a cancer bioassay. No additional data are available regarding the potential carciogenicity of GD in animals.
Goldman et al. (1987) reported on the results of genotoxicity studies of agent GD. In tests on bacteria and mammalian cell cultures, GD was not genotoxic or mutagenic when tested with and without metabolic activation. There were no biologically significant increases in mutations when tested in the Ames Salmonella assay using five revertant strains (TA135, TA100, TA98, TA1537, and TA1538) both with and without metabolic activation. GD did not induce a significant increase in forward mutations when tested on mouse L5178Y lymphoma cells at concentrations of 50, 100, or 200 µg/mL, and no increase in sister chromatid exchanges (SCE) was observed when Chinese hamster ovary cells were exposed in vitro to 200 µg/mL of GD. Mice treated in vivo with a maximally tolerated intraperitoneal dose of 300 µg GD/kg did not exhibit a significant increase in SCE in splenic lymphocytes. Exposure of rat hepatocytes to GD concentrations as high as 600 µl/3ml culture medium (2.5 × 106 hepatocytes) did not result in DNA damage or unscheduled DNA synthesis.
4. ORAL REFERENCE DOES FOR GD
4.1 Cholinesterase Inhibition as an RfD Endpoint
The endpoint for defining a maximum acceptable exposure level for nerve agents such as GD is considered to be the level at which no significant depression in blood cholinesterase activity occurs. In humans, 15% inhibition of RBC-AChE is generally considered to be the minimum change that can be observed with any statistical reliability (Callaway et al., 1951). Existing human response data (Marquis, 1988) indicate that human RBC-AChE inhibition of as much as 20% is not associated with adverse clinical signs or symptoms and should be considered only as evidence of organophosphate exposure. This contention is supported by the U.S. EPA (1995a) which reports scientific agreement that statistically significant inhibition of cholinesterase in multiple organs and tissues accompanied by clinical effects constitutes a hazard; however, in the absence of clinical effects, such inhibition may not be of biological significance. It is generally agreed that inhibition of RBC and/or plasma cholinesterase contributes to the overall hazard identification of cholinesterase inhibiting agents by serving as biomarkers (U.S. EPA, 1995a). Animal data have shown that exposure to low doses of nerve agents for extended periods of time can result in low blood ChE activity levels without signs of toxicity. Bucci et al. (1992c) found no evidence of toxicity in rats dosed i.p. with GA (up to 112 µg/kg), even though RBC-AChE activity was reduced about 37% in females (relative to controls). In oral toxicity studies conducted on GB, Bucci et al. (1992a) found that gavage doses of 0.3 mg/kg/day to rats caused nearly a 50% reduction in RBC-AChE activity without signs of toxicity. Goldman et al. (1988) reported no signs of toxicity, but 78–80% reduction in RBC-AChE activity, in Sprague-Dawley rats dosed subcutaneously with 1.0 µg VX/kg/day over 30 days. Rice et al. (1971) reported that whole blood cholinesterase of sheep dosed with 15 µg VX/day was reduced to 4–5% of the normalized baseline values (during the last 3 weeks of the dosing period) without any signs of toxicity. Rice et al. (1971) also found that sheep showing signs of toxicity (not described) at higher dose levels recovered fully after the exposures ended. Further complicating the evaluation is the extreme variability in ChE levels of individual animals and different sexes and ages of the same species (Halbrook et al., 1992). Possible changes in blood ChE that may occur with increasing age of the animals requires comparisons with concurrent controls, because the absence of a significant difference from pre-exposure values may be due to age-related increases in ChE in the dosed animals.
Blood ChE activity has been used by EPA as the critical endpoint in the establishment of oral RfDs for organophosphate insecticides (U.S. EPA 1995b; 1995c). In the case of malathion (U.S. EPA, 1995b), the no-observable-effect-level was identified as the highest oral dose level at which no significant change in RBC-AChE or plasma ChE was recorded in 5 human volunteers who received the compound orally for 47 days (Moeller and Rider, 1962). The next highest dose was associated with a depression of about 25% in both RBC-AChE and plasma ChE, but no clinical signs of toxicity. The EPA approach, also used for other organophosphate pesticides, is, therefore, to identify as LOAELs statistically significant decreases in ChE levels (RBC-AChE, plasma-ChE, or brain-ChE), and to base RfDs on NOAELs where the change in ChE is not statistically significant. This approach is also used in this report so that the RfDs developed for the nerve agents will not be disproportionally different from those for the organophosphate insecticides. In evaluating the experimental data for the nerve agents, added weight was given to those cases where significant changes in ChE occurred relative to both control and pre-exposure values and where there was evidence of a dose-response relationship.
In the derivation of an oral RfD, human oral exposure data are preferred (as in the case of malathion); however, such data are not available for GD. The only subchronic or chronic exposure studies for GD that were found in the available literature consist of a 90-day study in which rats were given GD by gavage (Bucci et al., 1992a).
The use of the subchronic rat study for developing an oral RfD for GD is complicated by the fact that rodents have a much lower RBC-AChE activity level compared to humans (Ellin, 1981, see Table 1). By itself, this could cause rats to be relatively more sensitive than humans to anticholinesterase compounds; however, the lower RBC-ChE activity may be offset by the presence of aliesterase in rat blood. Aliesterase, which is not present in humans (Cohen et al., 1971), is known to bind to and thereby reduce the toxicity of cholinesterase inhibitors (Fonnum and Sterri, 1981). Other species differences, such as the rates of aging of the nerve agent-ChE complex, the rates of synthesis of plasma cholinesterase in the liver, and the levels of AChE in various parts of the nervous system (see Ivanov et al., 1993) may also result in differences in species' sensitivities. There are insufficient data to determine the relative susceptibilities of humans and rodents to GD; therefore, for the purpose of this assessment, the EPA method will be followed which assumes that humans may be as much as ten times more sensitive to a chemical than laboratory animals.
4.2 Derivation of the Oral RfD for GD
The subchronic rat study conducted by Bucci et al. (1992a) is used here to derive an oral RfD for GD. This study is described in detail in section 3.2. Briefly summarized, the results of this study showed statistically significant (p <0.05) decreases in plasma-ChE activity levels in male and female CD rats dosed by gavage once per day, 5 days per week for 13 weeks. There were no definitive dose-related changes in RBC-ChE, and NTE levels were not significantly affected by the GD treatment.
The lowest tested dose (17.5 µg/kg/day = 0.0175 mg/kg/day) is considered a LOAEL because of the statistically significant reduction in plasma ChE (relative to controls) and also because the plasma-ChE activity during week 1 was reduced to 39% of baseline in males and 57% of baseline in females. This dose is adjusted to a 7 day/week exposure period by using a factor of 5/7; i.e., 5/7 × 0.0175 mg/kg/day = 0.0125 mg/kg/day. The RfD can then be calculated according to the following formula.
(2)
where
|
UF1 |
= |
10 (sensitive subpopulations) |
|
UF2 |
= |
10 (animal to human extrapolation) |
|
UF3 |
= |
3 (although plasma-AChE is not expected to be inhibited at longer exposures, however, an uncertainty factor was incorporated to account for effects possibly unrelated to plasma-AChE inhibition) |
|
UF4 |
= |
3 (LOAEL to NOAEL extrapolation; altered plasma-AChE is not overtly toxic) |
|
UF5 |
= |
3 (data base incomplete due to lack of chronic oral studies in two species, and studies assessing reproductive/developmental effects) |
|
MF |
= |
1 (no additional modifications needed). |
An uncertainty factor of 10 for sensitive subpopulations is considered necessary because some individuals have a genetic defect causing their blood cholinesterase activity to be abnormally low (Evans et al., 1952; Harris and Whitaker, 1962). These individuals, therefore, may be unusually sensitive to organophosphate anticholinesterase compounds.
An uncertainty factor of 10 is used for animal-to-human extrapolation because there is no evidence suggesting that humans less sensitive to GD than are laboratory animals.
An uncertainty factor of 3 is used to extrapolate from a subchronic to chronic exposure. In the derivation of the oral RfDs for other organophosphate compounds, the EPA has used NOAELs for cholinesterase inhibition following short-term exposures without adjustment for a more prolonged exposure period because of the unlikelihood that the endpoint would change over time (i.e., a subchronic-to-chronic UF of 1 was used). In addition, animal data indicate that maximum ChE inhibition may occur 30–60 days or more after exposure begins, after which it levels off or even shows recovery. In the Bucci et al. (1992a) study, both plasma and RBC-AChE levels exhibited signs of recovery at week 13, especially for the lower doses (Tables 5–8). Therefore, increased ChE inhibition is not expected to occur at longer exposure periods. However, an uncertainty factor of 3 is used because studies are not available to verify that adverse effects would not occur following chronic exposures.
A LOAEL-to-NOAEL uncertainty factor of 3 is used instead of 10 because the endpoint, cholinesterase inhibition, was not associated with signs of toxicity.
The database for GD lacks chronic oral studies in two species, and studies assessing reproductive/developmental effects. Because studies on other organophosphate cholinesterase inhibitors, including a multigeneration study on agent VX, indicate that reproductive/developmental effects are unlikely, a full uncertainty factor of 10 is not warranted.
Therefore,
(3)
(4)
(5)
4.3 Comparison of RfD with Toxicity Data
Only limited data regarding exposure to GD are available for comparison to the proposed RfD. An oral LD50 of 5–20 mg/kg for humans was estimated by Somani et al., (1992). The proposed RfD of 0.005 µg/kg is considerably lower than this value. The proposed RfD is more than 2 orders of magnitude below the ED50 dose (0.97 µg/kg) shown to produce performance decrements in rhesus monkeys after five consecutive days of dosing (Blick et al., 1994). Nieminen et al. (1990) reported behavioral effects concurrent with reduced blood AChE levels in rats given single i.p. injections of GD at doses of 4 or 20 µg/kg.
6. REFERENCES CITED
Abbrecht, P.H., R.R. Kyle and H.J. Bryant. 1989. Nebulized atropine for treatment of organophosphate toxicity. USAMRDC Med. Def. Biosci. Rev. pp. 201–205. (cited in Somani et al., 1992).
Anderson, D.R., L.W. Harris and W.J. Lennox. 1989. Subacute vs. acute physostigmine pretreatment against soman poisoning. USAMRDC Med. Def. Biosci. Rev. pp. 511–514. (cited in Somani et al., 1992).
Albuquerque, E.X., S.S. Deshpande, M. Kawabuchi, Y. Aracava, M. Idriss, D.L. Rickett, and A.F. Boyne. 1985. Multiple actions of anticholinesterase agents on chemosensitive synapses: Molecular basis for prophylaxis and treatment of organophosphate poisoning. Fund. Appl. Toxicol. 5:S182–S203.
Barnes, J.M. 1954. Organo-phosphorus insecticides. The toxic action of organo-phosphorus insecticides in mammals. Chem and Ind. January 2, 1954, pp. 478–480.
Baze, W.B. 1993. Soman-induced morphological changes: An overview in the non-human primate. J. Appl. Toxicol. 13: 173–177.
Blick, D.W., F.R. Weatherby, Jr., G.C. Brown and M.R. Murphy. 1994. Behavioral toxicity of anticholinesterases in primates: Effects of daily repeated exposure. Pharmacol. Biochem. Behav. 48: 643–649.
Bonderman, R.P. and D.P. Bonderman. 1971. A titrimetric method for differentiating between atypical and inhibited human serum pseudocholinesterase. Arch. Environ. Health 22:578–581. (Cited in Hayes, 1982)
Boskovic, B. 1981. The treatment of soman poisoning and its perspectives. Fundam. Appl. Toxicol. 1: 203–213.
Bucci, T.J., R.M. Parker and P.A. Gosnell. 1992a. Toxicity Studies on Agents GB and GD (Phase II), 90 Day Subchronic Study of GD (Soman) in CD-Rats. Final Report. Prepared for U.S. Army Biomedical Research and Development Laboratory, Fort Detrick, MD. FDA 224-85-0007.
Bucci, T.J., R.M. Parker and P.A. Gosnell. 1992b. Toxicity Studies on Agents GB and GD (Phase II): Delayed Neuropathy Study of Soman in SPF White Leghorn Chickens. Final Report. Prepared for U.S. Army Biomedical Research and Development Laboratory, Fort Detrick, MD.
Bucci, T.J., R.M. Parker, J.A. Crowell, J.D. Thurman and P.A. Gosnell. 1992c. Toxicity Studies on Agent GA (Phase II): 90 Day Subchronic Study of GA (Tabun) in CD Rats. Final Report. Prepared for the U.S. Army Biomedical Research and Development Laboratory, Fort Detrick, MD. DTIC AD-A258020.
Burchfiel, J.L., F.H. Duffy and V.M. Sim. 1976. Persistent effects of sarin and dieldrin upon the primate electroencephalogram. Toxicol. Appl. Pharmacol. 35: 365–369.
Callaway, S., D.R. Davies and J.P. Rutland. 1951. Blood cholinesterase levels and range of personal variation in a healthy adult population. Br. Med. J. 2:812–816.
Carnes, S.A. and A.P. Watson. 1989. Disposing of the U.S. chemical weapons stockpile: An approaching reality. JAMA 262:653–659.
Cohen, E.M., P.J. Christen and E. Mobach. 1971. The inactivation by oximes of Sarin and Soman in plasma from various species. I. The influence of diacetylmonoxime on the hydrolysis of Sarin. J.A. memorial issue. North-Holland Publishing Company, Amsterdam.
DA (U.S. Department of the Army). 1974. Chemical Agent Data Sheets, vol. 1. Edgewood Arsenal Special Report, EO-SR 74001. Defense Tech, Inform. Center, Alexandria, VA.
Dacre, J.C. 1984. Toxicology of some anticholinesterases used as chemical warfare agents - a review. In: Cholinesterases: Fundamental and Applied Aspects, M. Brzin, E.A. Barnard and D. Sket, eds., Walter de Gruyter, New York. pp. 415–426.
DHHS (U.S. Department of Health and Human Services, Centers for Disease Control). 1988. Final recommendations for protecting the health and safety against potential adverse effects of long-term exposure to low doses of agents: GA, GB, Mustard (H, HD, T), and Lewisite (L) . Federal Register 53: 8504–8507.
Duffy, F.H., J.L. Burchfiel, P.H. Bartels, et al. 1979. Long-term effects of an organophosphate upon the human electroencephalogram. Toxicol. Appl. Pharmacol. 47:161–176.
Duffy, F.H. and J.L. Burchfiel. 1980. Long-term effects of the organophosphate sarin on EEGs in monkeys and humans. Neurotoxicol. 1:667–689.
Dulaney, M.D., Jr., B. Hoskins and I.K. Ho. 1985. Studies on low dose subacute administration of Soman, Sarin and Tabun in the rat. Acta pharmacol. et toxicol. 57: 234–241.
Ellin, R.I. 1981. Anomalies in Theories and Therapy of Intoxication by Potent Organophosphorus Anticholinesterase Compounds. Special Publication USABML-SP-81-003, AD A101364. U.S. Army Medical Research and Development Command, Biomedical Laboratory, Aberdeen Proving Ground, MD.
Eto, M. 1974. Organophosphorus Pesticides: Organic and Biological Chemistry. pp. 123–231. CRC Press, Cleveland, OH.
Evans, F.T., P.W.S. Gray, H. Lehmann and E. Silk. 1952. Sensitivity to succinylcholine in relation to serum cholinesterase. Lancet 1:1129–1230. (Cited in Hayes, 1982).
Fonnum, F. and S.H. Sterri. 1981. Factors modifying the toxicity of organophosphorus compounds including soman and sarin. Fund. Appl. Toxicol. 1:143–147.
Gershon, J.L. and F.H. Shaw. 1961. Psychiatric sequelae of chronic exposure to organophosphorus insecticides. Lancet (June 24, 1961):1371–1374.
Goldman, M., A.K. Klein, T.G. Kawakami and L.S. Rosenblatt. 1987. Toxicity Studies on Agents GB and GD. Final Report from the Laboratory for Energy-Related Health Research to U.S. Army Medical Research and Development Command, Fort Detrick, MD. AD A187841.
Goldman, M., B.W. Wilson, T.G. Kawakami, L.S. Rosenblatt, M.R. Culbertson, J.P. Schreider, J.F. Remsen, and M. Shifrine. 1988. Toxicity Studies on Agent VX. Final Report from the Laboratory for Energy-Related Health Research to U.S. Army Medical Research and Development Command, Fort Detrick, MD. AD A201397
Gordon, J.J., R.H. Inns, M.K. Johnson, et al. 1983. The delayed neuropathic effects of nerve agents and some other organophosphorus compounds. Arch. Toxicol. 52:71–82. (Cited in Munro et al., 1994)
Grob, D. and J.C. Harvey. 1958. Effects in man of the anticholinesterase compound Sarin (isopropyl methyl phosphonofluoridate). J. Clin. Invest. 37(1):350–368.
Halbrook, R.S., L.R. Shugart, A.P. Watson, N.B. Munro and R.D. Linnabary. 1992. Characterizing biological variability in livestock blood cholinesterase activity for biomonitoring organophosphate nerve agent exposure. J. Amer. Vet. Med. Assoc. 201:714–725.
Harris, L.W., Lennox, W.J. and B.G. Talbot. 1984. Toxicity of anticholinesterase: Interactions of pyrdiostigmine and physostigmine with soman. Drug Chem. Toxicol. 7: 507–526. (cited in Somani et al., 1992)
Harris, H. and M. Whitaker. 1962. The serum cholinesterase variants. Study of twenty-two families selected via the ''intermediate" phenotype. Ann. Hum. Genet. 26:59–72. (Cited in Hayes, 1982)
Holmstedt, B. 1959. Synthesis and pharmacology of dimethylamidoethoxyphosphoryl cyanide (Tabun) together with a description of some allied anticholinesterase compounds containing the NP bond. Acta Physiol. Scand. 25 (Suppl. 90):1–120.
Hoskins, B. and I.K. Ho. 1992. Tolerance to organophosphate cholinesterase inhibitors. In: Organophosphates: Chemistry, Fate and Effects, J.E. Chambers and P.E. Levi, eds. Academic Press, new York, pp. 285–297.
Ivanov, P., B. Georgiev, K. Kirov, L. Venkov. 1993. Correlation between concentration of cholinesterase and the resistance of animals to organophosphorus compounds. Drug Chem. Toxicol. 16:81–99
Jimmerson, V.R. T-M. Shih and R.B. Mailman. 1989. Variability in soman toxicity in the rat: Correlation with biochemical and behavioral measures. Toxicology 57:241–254.
Jones, D.E., I. Koplovitz, D.G. Harrington, D.E. Hilmas and C.J. Canfield. 1984. Models for assessing efficacy of therapy compounds against organophosphates (OP). Proc. Fourth Annu. Chem. Def. Biosci. Rev. US Army Medical Research and Development Command, pp. 1–38. (cited in Somani et al., 1992)
Lennox, W.J., L.W. Harris, B.G. Talbot and D.R. Anderson. 1985. Relationship between reversible acetylcholinesterase inhibition and efficacy against soman lethality. Life Sci. 37: 793–798. (cited in Somani et al., 1992)
MacNaughton, M.G. and J.H. Brewer. 1994. Environmental chemistry and fate of chemical warfare agents. Final Report, Project 01-5864, Southwest Research Institute, San Antonio, TX. Prepared for Dept. of the Army Corps, Corps of Engineers.
Marquis, J.K. (ed.). 1988. Cholinesterase inhibition as an indication of adverse toxicologic effects. Review draft (June, 1988). Prepared for the Risk Assessment Forum, U.S. Environmental Protection Agency, Washington, DC.
Matsumura, F. 1976. Toxicology of Insecticides. pp. 17–46, 64–78, 142–152, 403–444, 462–464. Plenum Press, New York, NY.
Maxwell, D.M., D.E. Lenz, W.A. Groff, A. Kaminskis and H.L. Froehlich. 1987a. The effects of blood flow and detoxification on in vivo cholinesterase inhibition by soman in rats. Toxicol. Appl. Pharmacol. 88: 66–76.
Maxwell, D.M., K.M. Brecht and D.E. Lenz. 1987b. Effect of carboxylesterase inhibition on carbamate protection against soman toxicity. Proc. Sixth Chem. Def. Biosci. Rev., pp. 17–24. (cited in Somani et al., 1992)
McLeod, C.G., Jr. 1985. Pathology of nerve agents: perspectives on medical management. Fund. Appl. Toxicol. 5: S10–S16.
McNamara, B.P. and F. Leitnaker. 1971. Toxicological Basis For Controlling Emission of GB Into the Environment. EASP 100–98, AD 914271L. U.S. Army, Medical Research Laboratory, Edgewood Arsenal, Aberdeen Proving Ground, MD.
Metcalf, D.R. and J.H. Holmes. 1969. EEG, psychological, and neurological alterations in humans with organophosphorus exposure. Ann. N.Y. Acad. Sci. 357–365.
Mick, D.L. 1974. Collaborative study of neurobehavioral and neurophysiological parameters in relation to occupational exposure to organophosphate pesticides. In: Behavioral Toxicology: Early Detection of Occupational Hazards. C. Xintaras, B.L. Johnson and I. de Groot, eds. Center for Disease Control, National Institute for Occupational Safety and Health, Washington, DC. pp. 152–153.
Moeller, H.C. and J.A. Rider. 1962. Plasma and red blood cell cholinesterase activity as indications of the threshold of incipient toxicity of ethyl-p-nitrophenyl thiobenzenephosphorate (EPN) and malathion in human beings. Toxicol. Appl. Pharmacol. 4:123–130.
Morgan, D.P. 1989. Recognition and Management of Pesticide Poisonings, 4th ed., EPA-540/9-88-001, U.S. Environmental Protection Agency, Washington, DC.
Morrill, L.G., L.W. Reed and K.S.K. Chinn. 1985. Toxic Chemicals in the Soil Environment. Volume 2. Interaction of Some Toxic Chemicals/Chemical Warfare Agents and Soils. Oklahoma State University TECOM Project 2-CO-210-049, Stillwater, OK. Available from DTIC, AD-A158 215 .
Munro, N.B., K.R. Ambrose and A.P. Watson. 1994. Toxicity of the organophosphate chemical warfare agents GA, GB, and VX: Implications for public protection. Envir. Health Perspect. 102:18–38.
Nieminen, S.A., A. Lecklin, O. Heikkinen and P. Ylitalo. 1990. Acute behavioral effects of the organophosphates Sarin and Soman in rats. Pharmacol. Toxicol. 67: 36–40.
Olson, C.T., R.G. Menton, R.C. Kiser, D.W. Hobson, G.S. Dill, R.L. Joiner and J.R. Stewart. 1989. Evaluating the efficacy of antidote drug combinations against soman toxicity in the rabbit. USAMRIDC Med. Def. Biosci., Rev., pp. 667–670. (cited in Somani et al., 1992)
O'Brien, R.D. 1960. Toxic Phosphorus Esters: Chemistry. Metabolism, and Biological Effects. pp. 175–239. Academic Press New York, NY.
Petrali, J. P. 1989. Anticholinesterase toxicity of endothelial cells. USAMRDC Med. Def. Biosci. Rev. pp 95–98. (cited in Somani et al., 1992)
Petras, J.M. 1984. Brain pathology induced by organophosphate poisoning with nerve agent soman . Porc. Fourth Annual Chem. Biosci. Rev., AD B089975, p. 407. (cited in Baze, 1993)
Rice, G.B., T.W. Lambert, B. Haas and V. Wallace. 1971. Effect of Chronic Ingestion of VX on Ovine Blood Cholinesterase. Technical Report DTC 71–512, Deseret Test Center, Dugway Proving Ground, Dugway UT.
Rickett, D.J., J.F. Glenn, W.E. Houston. 1987. Medical defense against nerve agents: New directions. Mil. Med. 152:35–41.
Rider, J.A., L.E. Ellinwood and J.M. Coon. 1952. Production of tolerance in the rat to octamethylpyrophosphoramide (OMPA). Proc. Soc. Exptl. Biol. Med. 81:455–459.
Rodnitzky, R.L. 1974. Neurological and behavioral aspects of occupational exposure to organophosphate pesticides. In: Behavioral Toxicology: Early Detection of Occupational Hazards. C. Xintaras, B.L. Johnson and I. de Groot, eds. Center for Disease Control, National Institute for Occupational Safety and Health, Washington, DC. pp. 165–174.
Rosenblatt, D.H., M.J. Small, T.A. Kimmell and A.W. Anderson. 1995. Agent decontamination chemistry technical report. Draft. Environmental Quality Office, U.S. Army Test and Evaluation Command.
Savage, E.P., T.J. Keefe, L.M. Mounce, et al. 1988. Chronic neurological sequelae of acute organophosphate pesticide poisoning. Arch. Environ. Health 43:38–45.
Sidell, F.R. 1992. Clinical considerations in nerve agent intoxication. In: Chemical Warfare Agents, S. Somani, ed., Academic Press, N.Y., pp 155–194.
Sidell, F.R. and W.A. Groff. 1974. The Reactivatibility of Cholinesterase Inhibited by VX and Sarin in Man. Toxicol. Appl. Pharmacol. 27:241–252.
Sidell, F.R. and A. Kaminskis. 1975. Temporal intrapersonal physiological variability of cholinesterase activity in human plasma and erythrocytes. Clin. Chem. 21:1961–1963,
Singer, A.W., N.K. Jaax, J.S. Graham and C.G. McLeod, Jr. 1987. Cardiomyopathy in Soman and Sarin intoxicated rats. Toxicol. Letters 36:243–249.
Somani, S.M., E. Giacobini, A. Boyer, M. Hallak, A. Khalique, L. Unni, M. Hannant and E. Hurley. 1986. Mechanisms of action and pharmacokinetics of physostigmine in relation to acute intoxication by organofluorophosphates. Reports submitted to U.S. Army Medical Research and Development Command, Fort Detrick, Maryland. (cited in Somani et al., 1992)
Somani, S.M., R.P. Solana and S.N. Dube. 1992. Toxicodynamics of nerve agents. In: Chemical Warfare Agents, Somani, S., ed. Academic Press, Inc. New York. pp. 67–123.
Sparenborg, S., N.K. Jaax and D.J. Braitman. 1989. Novel anticonvulsants protect against seizures and brain damage induced by the cholinesterase inhibitor soman. USAMRIDC Med. Def. Biosci., Rev., pp. 119–122. (cited in Somani et al., 1992)
Sterri, S.H. 1981. Factors modifying the toxicity of organophosphorous compounds including dichlorvos. Acta Pharmacol. Toxicol. 49: 67–71. (cited in Somani et al., 1992)
Sumerford, W.T., W.J. Hayes, J.M. Johnston, K. Walker and J. Spillane. 1953. Cholinesterase response and symptomatology from exposure to organic phosphorus insecticides. AMA Arch. Ind Hyg. Occup. Med. 7:383–398. (Cited in Ho and Hoskins, 1984)
Switzer, R.C., M.R. Murphy, S.K. Campbell, S. Z. Kerenyi, S.A. Miller and S.K. Hartgraves. 1989. Soman-induced damage to selected populations of neurons in rat and rhesus monkey brains. USAMRDC Med. Def. Biosci. Rev., pp. 107–110. (cited in Somani et al., 1992)
Tripathi, H.L. and W.L. Dewey. 1989. Comparison of the effect of diisopropylfluorophosphate, sarin, soman, and tabun on toxicity and brain acetylcholinesterase activity in mice. J. Toxicol. Environ. Health, 26: 437–446. (cited in Somani et al., 1991)
Tabershaw, I.R. and W.C. Cooper. 1966. Sequelae of acute organic phosphate poisoning. J. Occup. Med. 8:5–20.
Thienes, C.H. and T.J. Haley. 1972. Clinical Toxicology. Lea and Febiger, Philadelphia, PA. pp. 95–115.
U.S. EPA (U.S. Environmental Protection Agency). 1995a. Proposed Guidelines fo Neurotoxicity Risk Assessment. Fed. Reg. 60 (192): 52032-52056.
U.S. EPA (U.S. Environmental Protection Agency). 1995b. Oral RfD Assessment for Malathion. Integrated Risk Information System (IRIS). Online file. Environmental Criteria and Assessment Office, Office of Health and Environmental Assessment, Cincinnati, OH.
U.S. EPA (U.S. Environmental Protection Agency). 1995c. Oral RfD Assessment for Ethion. Integrated Risk Information System (IRIS). Online file. Environmental Criteria and Assessment Office, Office of Health and Environmental Assessment, Cincinnati, OH.
Wall, H.G., N.K. Jaax and I.J. Hayward. 1990. Motor activity and brain lesions in soman intoxicated rhesus monkeys. Proc. of the Workshop on Convulsions and Related Brain Damage Induced by Organophosphorous Agents, ADA222912, Army Medical Research Institute of Chemical Defense, Aberdeen Proving Ground. pp. 21–29. (cited in Baze, 1993)
Wagner, S.L. 1983. Organophosphates. In: Clinical Toxicology of Agricultural Chemicals. pp. 205–246. Noyes Data Corporation, Park Ridge, NJ.
Watson, A.P., K.R. Ambrose, G.D. Griffin, et al. 1989. Health effects of warfare agent exposure: implications for stockpile disposal. Environ. Prof. 11:335–353.
Watson, A.P. and N.B. Munro. 1990. Reentry Planning: the Technical Basis for Offsite Recovery Following Warfare Agent Contamination. ORNL-6628. Oak Ridge National Laboratory, Oak Ridge, TN.
Willems, J.L. M. Nicaise and H.C. De Bisschop. 1984. Delayed neuropathy by the organophosphorous nerve agents soman and tabun. Arch. Toxicol. 55: 76–77. (cited in Somani et al., 1992)
Wills, J.H. 1972. The measurement and significance of changes in the cholinesterase activities of erythrocytes and plasma in man and animals. CRC Crit. Rev. Toxicol. 1:153–202.
Yager, J., H. McLean, M. Hudes and R.C. Spear. 1976. Components of variability in blood cholinesterase assay results. J. Occup. Med. 18:242–244.
APPENDIX A
Comparison of RfDs, ChE Inhibition and Toxicity Data for GA, GB, GD and VX
|
Endpoint |
GA (µg/kg/day) |
GB (µg/kg/day) |
GD (µg/kg/day) |
VX (µg/kg/day) |
Ref. |
|
RfD |
0.04 |
0.02 |
0.004 |
0.0006 |
This report |
|
Estimated no-effect level for RBC-AChE inhibition |
- |
1.0 |
- |
0.24 |
GBd VXa |
|
27–33% inhibition of RBC-AChE in humans/oral dose |
- |
2.3 (3 days) |
- |
0.2-2.0 |
GB - Grob and Harvey, 1958; VX-this report |
|
RBC-AChE inhibition in humans/i.v. dose |
- |
- |
1.5-2.0 (30%) |
1.0 (50%) |
DA, 1974; Sidell and Groff, 1974 |
|
50–60% RBC-AChE inhibition in humans/oral dose |
- |
10 |
- |
2.4 |
GB - Grob and Harvey, 1958; VX-Sidell and Groff, 1974 |
|
50% brain ChE inhibition in vitro |
1.5 × 10-8 (c) |
0.3 × 10-8 (c) |
- |
- |
Grob and Harvey, 1958 |
|
Acute toxic effects in humans/oral dose |
- |
20–30 |
- |
2–4.5 |
GB - Thienes and Haley 1972; Grob and Harvey, 1958; VX-Sidell and Groff, 1974 |
|
human oral LD50 (estimated) |
25–50b |
5–20b |
5–20 |
3–10b |
Somani et al., 1992 |
|
rat oral LD50 |
3700 |
870–1060 600 |
400 |
77–128 |
DA, 1974 Grob & Harvey, 1958 |
|
monkey i.v. LD50 |
50 |
20 |
- |
6–11 |
DA, 1974 |
|
rat i.v. LD50 |
70 |
45–63 |
50 |
6.9–10.1 |
Dacre, 1984 |
|
rat i.p. LD50 |
490, 800 |
250 218 |
- |
37–55 |
DA, 1974 RTECS, 1995 |
|
a Based on ratio of oral to i.v. doses (2.4 and 1.0 µg/kg, respectively) required for 50% RbC-ChE inhibition and the estimated i.v. no effect dose of 0.1 µg/kg b Values were estimated from animal data. c Molar concentration d Estimated from RBC-ChE50 values for GB and VX. |
|||||






























