APPENDIX C
Medically Necessary Dental Services
B.Alex White, D.D.S., Dr.P.H., Lauren L.Patton, D.D.S., William G.Kohn, D.D.S., and James A.Lipton, D.D.S., Ph.D.
OVERVIEW
The Balanced Budget Act of 1997 directed the Secretary of Health and Human Services to request the National Academy of Sciences to analyze “the short- and long-term benefits, and costs to Medicare” of extending Medicare coverage for certain preventive and other services. Congress directed that the report include specific findings with respect to coverage of a number of services, including medically necessary dental services.
The purpose of this background paper is to present scientific evidence related to medically necessary dental services for selected medical conditions or in conjunction with certain medical procedures. This review is not intended to make specific recommendations about the clinical management of oral conditions or the prevention of oral complications or to address the entire range of diseases, conditions, or procedures for which medically necessary dental services may be indicated. Rather the intent is to review the evidence about certain oral health interventions in preventing or reducing morbidity and/or mortality for selected medical conditions. For a very limited set of medical diagnoses or under very specific clinical conditions, dental services are covered under Medicare. Evidence on the effectiveness of dental services in these circumstances is not covered in this review, although some information may be included for clar-
Senior Investigator, Center for Health Research, Kaiser Permanente Northwest Division; Associate Professor, Department of Dental Ecology, University of North Carolina at Chapel Hill; Associate Director for Science, Division of Oral Health, Centers for Disease Control and Prevention; Assistant Director for Training and Career Development, Division of Extramural Research, National Institute of Dental and Craniofacial Research, National Institutes of Health.
ity. The primary focus is on the effectiveness of dental services not currently covered by Medicare.
What Are Medically Necessary Dental Services?
Several definitions of medically necessary dental services have been proposed. In 1995, the National Alliance for Oral Health held a consensus conference on medically necessary dental services and proposed the following definition: “that care that is a direct result of, or has a direct impact on, an underlying medical condition and/or its resulting therapy” (Consensus Conference, 1995). The consensus conference also noted that such care was integral to comprehensive treatment to ensure optimum health outcomes and could potentially reduce health care expenditures for treatment of complications.
In 1990, the American Dental Association’s House of Delegates adopted the following comprehensive definition of medically necessary dental services:
the reasonable and appropriate diagnosis, treatment, and follow-up care (including supplies, appliances, and devices) as determined and prescribed by qualified, appropriate health care providers in treating any condition, illness, disease, injury, or birth developmental malformations. Care is medically necessary for the purpose of controlling or eliminating infection, pain, and disease; and restoring facial disfiguration, or function necessary for speech, swallowing, or chewing.
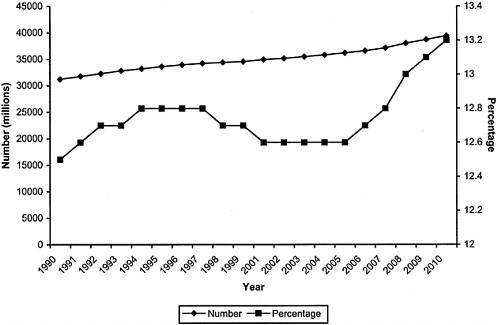
Several important points are implied by these definitions, which are illustrated in Figure C-1. First, medically necessary dental services can be provided across a continuum of underlying diseases or conditions. Medically necessary dental services may be provided to prevent the onset of a disease
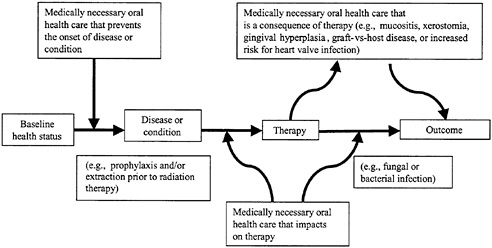
FIGURE C-1 A model of medically necessary dental services.
or condition, to manage oral conditions that can impact medical care (e.g., fungal or bacterial infections from oral sources), or to manage the oral manifestations of treatment (e.g., xerostomia secondary to radiation therapy). Medically necessary dental services are not restricted to or defined by an established set of medical diseases or conditions. Rather, it is the potential impact of oral health on medical outcomes, including the onset of certain diseases and the effect of medical treatment on oral health, that defines medically necessary dental services. Second, medically necessary dental services include preventive, diagnostic, and treatment services and are not limited only to diagnosis or selected procedures. Identification of potential oral sources of infection through an oral examination alone, for example, will not eliminate the infection. Additional treatment will be necessary to improve health outcomes. Finally, medically necessary dental services should have a measurable impact on morbidity and/or mortality and improve physiological, clinical, and/or behavioral outcomes of care for the defined medical disease or condition.
Selected Clinical Conditions Under Consideration
Numerous medical diseases and conditions may require medically necessary dental services to improve health outcomes, including developmental and acquired maxillofacial defects, developmental disabilities, diabetes, hemophilia, orphaned diseases (e.g., ectodermal dysplasia), and anesthesia for uncooperative pediatric and other patients. Time and resource constraints required that only a limited number of diseases and conditions be considered. Consequently, this background paper focuses on these five diseases or conditions: head and neck cancer, leukemia, lymphoma, organ transplantation, and repair or replacement of heart valve defects. The five conditions are a subset of a much larger set of diseases and conditions for which medically necessary dental services may be indicated. These were selected based in part on their prevalence and on the level of evidence for clinical management. The potential oral complications associated with these conditions are shown in Table C-1.
Currently Covered Dental Services Under Medicare
With certain exceptions, Medicare does not cover dental services. Figure C-2 illustrates current Medicare coverage policy for dental services. First, Medicare does not cover any services that are beyond the scope of the dental practice. Each state determines which services fall within and outside the scope of dental practice. Reimbursement for dental services under Medicare cannot go beyond what is allowed in each state.
TABLE C-1 Selected Medical Diseases and Conditions and Potential Oral Complications Associated with Treatment
|
Clinical Condition |
Potential Complication(s) |
|
Head and neck neoplasms |
Secondary to radiotherapy: xerostomia, rampant dental caries, mucositis, osteoradionecrosis, infection Secondary to surgery: hard- and soft-tissue defects |
|
Leukemia and lymphoma |
Stomatotoxicity of chemotherapy and total-body irradiation; early septicemia from oral organisms; possibility of acute and chronic graft-versus-host disease (for bone marrow transplantation); hemorrhage |
|
Organ transplantation |
Infection from oral organisms secondary to immunosuppression; gingival hyperplasia secondary to immunosuppressive drugs |
|
Heart valve repair or replacement |
Valvular infection from oral organisms |
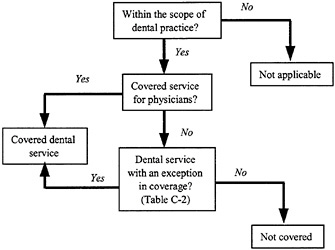
FIGURE C-2 Overview of current Medicare coverage policy for dental services.
Given the scope of dental practice, services that are covered for physicians are also covered for dentists. The term “physician,” when used in connection with the performance of any function or action, includes a doctor of dental surgery or of dental medicine who is legally authorized to practice dentistry by the state in which he or she performs such function and who is acting within the scope of his or her license when performing such functions (section 1861(r)(2)
of the Social Security Act (42 USC 1395x)). Such services include any otherwise covered service that may legally and alternatively be performed by doctors of medicine, osteopathy, and dentistry (e.g., dental examinations to detect infections prior to certain surgical procedures; treatment of oral infections, hemorrhage, and mucositis; and interpretations of diagnostic x-ray examinations in connection with covered services).
Specific dental services that are usually provided only by dentists are not covered. Under current Medicare statute, no payment can be made under Part A (hospital) or Part B (physician) for any expenses incurred for items or services:
where such expenses are for services in connection with the care, treatment, filling, removal, or replacement of teeth or structures directly supporting the teeth, except that payment may be made under Part A in the case of inpatient hospital services in connection with the provision of dental services if the individual, because of his/her underlying medical condition and clinical status or because of the severity of the dental procedure, requires hospitalization in connection with the provision of such services. (Section 1862(a)(12) of the Social Security Act (42 USC 1395y))
The coverage or exclusion of any given dental service is not affected by the professional designation of the physician rendering the services (i.e., an excluded dental service remains excluded and a covered dental service is still covered whether furnished by a dentist or a doctor of medicine or osteopathy).
The limited exceptions to coverage for dental services under Medicare are summarized in Table C-2. Under Part B (physician services), if an otherwise noncovered procedure or service (e.g., removal of teeth) is performed by a dentist as “incident to” and as an integral part of a covered procedure or service performed by the same dentist (e.g., surgery of the jaw), the total service performed by the dentist on such an occasion is covered. For example, the reconstruction of a ridge performed primarily to prepare the mouth for dentures is a noncovered procedure. However, when the reconstruction of a ridge is performed as a result of, and at the same time as, the surgical removal of a tumor (for other than dental purposes), the totality of surgical procedures is a covered service. Likewise, the wiring of teeth is a covered service when it is done in connection with the reduction of a jaw fracture if the reduction and wiring are performed by the same practitioner.
Second, tooth extractions to prepare the jaw for radiation treatment of neoplastic disease are covered services. This is an exception to the requirement that to be covered, a noncovered procedure or service performed by a dentist must be incident to and an integral part of a covered procedure or service performed by him or her. Ordinarily, the dentist extracts the patient’s teeth, but another physician (e.g., a radiation oncologist) administers the radiation treatments.
TABLE C-2 Current Medicare Coverage for Dental Services
|
Clinical Condition |
Covered Service |
Part A (hospital) |
Part B (physician) |
|
Underlying medical condition and clinical status require hospitalization for dental care |
Inpatient hospital services only |
X |
|
|
Severity of dental procedure requires hospitalization for dental care |
Inpatient hospital services only |
X |
|
|
Any oral condition for which nondental services are covered |
All dental services if incident to and an integral part of covered procedure or service |
|
X |
|
Neoplastic jaw disease |
Extractions prior to radiation |
|
X |
|
Renal transplant surgery |
Oral or dental examination on an inpatient basis |
Xa |
Xb |
|
aIf the dentist is on staff at the hospital where the service is provided. bOutpatient payment for physicians only. |
|||
Finally, an oral or dental examination performed on an inpatient basis as part of a comprehensive workup prior to renal transplant surgery is a covered service. The purpose of the examination is not for the care of the teeth or structures directly supporting the teeth. Rather, the examination is for the identification, prior to a complex surgical procedure, of existing medical problems where the increased possibility of infection would not only reduce the chances for successful surgery but also expose the patient to additional risks in undergoing such surgery. Such a dental or oral examination would be covered under Part A of the program if performed by a dentist on the hospital’s staff or under Part B if performed by a physician. (When performing a dental or oral examination, a dentist is not recognized as a physician under section 1861(r) of the law; see Carriers Manual section 2020.3.)
Whether such services as the administration of anesthesia, diagnostic x-rays, and other related procedures are covered depends on whether the primary procedure being performed by the dentist is itself covered. Thus, an x-ray taken in connection with the reduction of a fracture of the jaw or facial bone is covered. However, a single x-ray or x-ray survey taken in connection with the care or treatment of teeth or the periodontium is not covered.
Based on current statute, regulations, and the Coverage Issues and Carriers Manuals, it appears that an oral examination would be a covered service for a person with certain oral conditions if (1) the management of the condition in-
cluded a covered service and (2) the person providing the covered service also performed the oral examination. For example, individuals with a fractured mandible would require an oral examination as an integral part of the management of the fracture. The oral examination would be covered for the dentist if that dentist is also treating the fracture. Another example might include crowns on teeth for individuals requiring an obturator following head and neck surgery if the crowns are a necessary part of obturator placement. Likewise, for persons with neoplastic jaw disease, oral examination would be covered if they required extractions prior to radiation. For persons with neoplastic jaw disease who were edentulous or who did not require an extraction, the examination would not be covered. For the five medical conditions considered here, currently covered and noncovered services are shown in Table C-3.
The information presented here on coverage for dental services is contained within current statute, regulations, and coverage manuals. Certain Medicare fiscal intermediaries have made exceptions for coverage of certain procedures such as examinations for persons with head and neck neoplasms regardless of whether the person had an extraction. Given the lack of clarity and variability among carriers, this information is not included here.
Increasing Number of Persons 65 and Above Who Are Retaining Natural Teeth
During the next 10 years, the number of persons 65 years of age and over who are eligible for Medicare will increase from an estimated 34.5 million in 1999 to about 39.4 million in 2010 (Figure C-3) (U.S. Bureau of the Census Statistics, www.census.gov/population/www/index.html).
By 2010, individuals 65 years of age and older will represent about 13.2% of the U.S. population, up from about 12.7% in 1999. Not only will the number of persons 65 and above increase, the proportion maintaining some or all of their natural dentition will also increase, as suggested by epidemiological data spanning the past 35 years. The first National Health Examination Survey, conducted in 1960–1962, found that about 45.1% of men and 53.0% of women aged 65–74 years were edentulous (without teeth) (NCHS, 1973). For 75- to 79-year-old men, the percentage edentulous was 55.7%; for 75- to 79-year-old women, the percentage edentulous was 65.6%.
The National Health and Nutrition Examination Survey, conducted between 1971 and 1974, found that the edentulism prevalence declined to about 45.5% among persons 65 to 74 years of age, 43.6% among men and 47.0% among women (NCHS, 1981). An epidemiological study conducted by the National Institute of Dental Research in 1985–1986 found that among persons 65 years old and over attending senior centers, 41.1% were edentulous (NIDR, 1987).
TABLE C-3 Summary of Dental Services Currently Covered and not Covered Under Medicare for Selected Diseases or Conditions
|
Disease or Condition |
Dental Services Currently Covered Under Medicare |
Dental Services not Currently Covered Under Medicare |
|
Head and neck neoplasms |
Extraction of teeth prior to radiation Oral examination if extractions are to be performed |
Oral examination if no extractions are to be done prior to radiation Preventive care to reduce risk of radiation caries (e.g., fluoride trays, supplemental topical fluoride) Treatment of radiation caries |
|
Leukemia and lymphoma |
Management of mucositis, hemorrhage, and related side effects of underlying disease |
Oral examination prior to treatment Dental treatment to reduce risk of infection or eliminate infection prior to or following treatment |
|
Organ transplantation |
Management of infection following transplantation Oral examination prior to renal transplant surgery on an inpatient basis |
Oral examination for transplants other than kidney Oral examination for renal transplants on an outpatient basis Dental treatment to reduce risk of infection or eliminate infection for any transplantation prior to or following transplant |
|
Heart valve repair or replacement |
None |
Oral examination prior to repair or replacement Dental treatment to reduce risk of infection or eliminate infection prior to or following repair or replacement of valve |
The 1989 National Health Interview Survey found that self-reported edentulism had declined to about 28.4% among persons 65 to 74 years of age and 43.0% among persons 75 years of age and over (Bloom et al., 1992). The Third National Health and Nutrition Examination Survey, Phase I, conducted between 1988 and 1991, reported an edentulism rate of 26.0% among persons 65 to 69
years of age, 31.1% among persons 70 to 74 years of age, and 43.9% among persons 75 years of age and older (Marcus et al., 1996). Most recently, data from the 46 states that participated in the oral health module of the 1995–1997 Behavioral Risk Factor Surveillance System (BRFSS) indicated that about 22.9% of persons 65–74 years of age and 26.7% of persons 75 years of age or over were edentulous (MMWR, 1999). Given this trend, one would hypothesize that the proportion of Medicare-eligible persons 65 years of age or over who may require medically necessary dental services will increase.
Decision Framework for Medically Necessary Dental Services
Figure C-4 illustrates a generic decision model for medically necessary dental services that applies to each of the five diseases and conditions under consideration here and serves as a framework for the literature review and synthesis. As noted earlier, medically necessary dental services can occur in the context of a disease or condition.
Among persons with selected diseases or conditions, following the diagnosis and prior to initiation of medical therapy, a pretreatment oral assessment may or may not be provided. An explicit decision is required to provide the care, which is represented by the filled square in Figure C-4. This assessment may include a clinical examination and radiographs. Some of those assessed will have potential oral sources of infection or other complications. Dental care prior
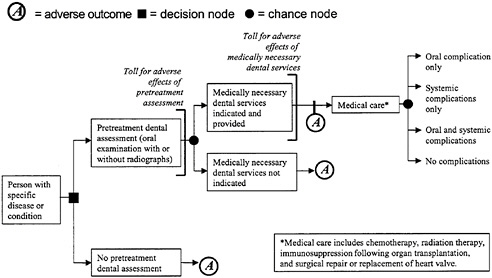
FIGURE C-4 Decision model for medically necessary dental services.
to medical treatment may be indicated and provided. The chance nature of this event is represented by the filled circle in Figure C-4. In conjunction with, or as a consequence of, medical therapy, individuals may develop oral complications associated with the medical treatment (e.g., mucositis or xerostomia), systemic complications from oral sources (e.g., infection or hemorrhage), or some combination thereof. Each of these can adversely affect the outcome of medical therapy by increasing morbidity, mortality, and cost. The purpose of this background paper is to review and assess the literature to determine the extent to which medically necessary dental services can reduce the likelihood of these complications or lessen their effect.
Decision Analytical Framework
Specific analytic questions guided our literature search and synthesis efforts. For each of the conditions under consideration, we initially sought to address the following question: Is there direct evidence that medically necessary dental care—including screening, diagnostic and preventive services, and treatment—provided to persons with a defined medical diagnosis prior to or during acute therapy for that diagnosis improves health outcomes? Direct evidence is evidence that relates a diagnostic strategy or therapeutic intervention to the occurrence of a principal health outcome (Eddy et al., 1992). Outcomes by definition are multidimensional. In this context, principal health outcomes refer to those outcomes that are of most interest to the patient, such as symptoms, functional status, morbidity, and death (Fleming and DeMets, 1996). Our goal, then, was to identify studies that related a specific dental intervention—oral examination and treatment prior to organ transplantation, for example—to an outcome—improved quality-of-life and decreased mortality, for example.
When direct evidence was not identified, we sought to identify indirect evidence that related to medically necessary dental services for each of the conditions being considered. Indirect evidence requires two or more bodies of evidence to relate the diagnostic strategy, exposure, or therapeutic intervention to the principal health outcome (Eddy, et al., 1992). For example, one study may demonstrate that a screening and treatment protocol for patients prior to heart valve replacement eliminates potential sources of oral infection. A second study may demonstrate that oral sources of infection are important contributors to valve failure. Neither study alone provides direct evidence that screening and treatment prior to heart valve replacement reduce morbidity or mortality; together, the two studies provide indirect evidence that screening and treatment to eliminate oral sources of infection prior to heart valve replacement improve principal health outcomes.
A number of questions guided our efforts to survey and synthesize indirect evidence to support medically necessary dental services. These questions reflect the various components of the decision framework illustrated in Figure C-4.
-
The first question related to the effectiveness of pretreatment assessment prior to initiation of therapy to reduce risks of adverse outcomes such as postoperative infection or osteoradionecrosis. Assessment procedures are not without risk, and adverse effects can occur (represented by a toll).
-
During assessment, the clinician may identify oral conditions that require dental care prior to medical treatment, including extractions and selected periodontal procedures. Such procedures may result in adverse effects (represented by a toll).
-
In the third phase, during which medical therapy occurs, oral complications may arise from the therapy (e.g., mucositis), systemic complications may arise from oral sources (e.g., infection), some combination of oral and systemic complications may arise, or no complications may arise.
-
In the final phase, following medical therapy, oral complications may impact on principal health outcomes such as osteoradionecrosis secondary to radiation-induced xerostomia, graft-versus-host disease in bone marrow transplant recipients, or infection in an immunosuppressed individual.
General Analytic Approach
Evidence of the effectiveness of dental services for the five diseases and conditions under consideration was obtained from the published literature. We conducted a comprehensive search of the literature from 1980 through 1999 to obtain relevant references using the following search terms: dentistry, dental care, oral surgical procedures, periodontal diseases, head and neck neoplasms, leukemia, lymphoma, organ transplantation, and heart valve diseases. We further limited the search results to human studies published in English. Results from these searches were provided to each author, who reviewed this information and conducted additional searches as indicated, including additional search terms, additional years, or both.
CONDITION 1: HEAD AND NECK CANCER
Introduction
Head and neck cancers represent about 4% of all cancers diagnosed in males and 2% of cancers diagnosed in females (USDHHS, 1991). The American Cancer Society’s (ACS’s) Department of Epidemiology and Surveillance Research estimates that 29,800 new oral cavity and pharynx cancers and 10,600 new larynx cancers will occur in the United States in 1999 (Landis et al., 1999). Incidence in the 65 years and over age group has been relatively stable over time. The estimated annual change in incidence from 1973 to 1996 was −0.4% for cancers of the oral cavity and pharynx and +0.4% for cancers of the larynx (Ries et al., 1999). The National Cancer Institute’s (NCI’s) Surveillance, Epi-
demiology, and End Results (SEER) Program regional treatment data suggest that 44.7% of oral cavity and pharynx cancer patients and 49.2% of larynx cancer patients are 65 years or older (SEER, 1993). If these estimates are applied to the ACS U.S. case estimates, this age group accounts for about 13,220 new oral cavity and pharynx and 5,215 new larynx cancer cases. Largely due to failure of early detection, the majority of oral cancer cases are diagnosed after regional or distant spread, resulting in an overall five-year survival rate for oral cavity and pharynx cancers of 55% among U.S. whites and 32% among African Americans (Landis et al., 1999).
Radiation and/or surgery are the primary treatment methods for new cases of head and neck cancers, with a lesser role played by chemotherapy (Shaha and Strong, 1995). Recently described organ-preserving protocols using neoadjuvant chemotherapy with cisplatin and fluorouracil followed by radiation therapy are gaining acceptance for larynx cancer and can be expected to result in increasing oral morbidity (Shah et al., 1997; Spaulding et al., 1994). SEER estimates that for patients diagnosed with cancer of the oral cavity and pharynx from 1988 to 1993, 53.8% of all ages and 49.7% of those age 65 and above received radiation therapy alone or in combination with other modalities as treatment for their cancer (SEER, 1993). For cancer of the larynx over this same time period, SEER estimates that 73.9% of all ages and 74.2% of those age 65 and above received radiation therapy alone or in combination with other modalities as treatment for their cancer (SEER, 1993). Radiation delivered in therapeutic doses to the head and neck region results in a number of acute and chronic complications (Beumer et al., 1979a,b).
The purpose of this systematic review is to evaluate the evidence base for expanding Medicare coverage in the arena of medically necessary dental services for the head and neck cancer patient treated with radiation therapy. The emphasis is on dental services that may be necessary in the course of radiation therapy because radiation therapy may have a poor outcome if the appropriate dental services are not included. Current Medicare Part B coverage for dental services for beneficiaries with head and neck neoplasms is limited to “extraction of teeth to prepare the jaw for radiation treatment of neoplastic disease” (Table C-3).
Methods
This review is based on a search of the literature from the MEDLINE database from 1966 to March 1999, including studies identified from reference lists in core articles obtained in the search. In addition to the search terms used for all topics in this appendix, as described in the section on general analytic approaches, separate searches were conducted specifically on the head and neck topic with key words as follows: (1) (head and neck cancer and radiation and oral complications).ti,ab.rw,sh; (2) (oral cancer and radiation and dental).ti,ab.rw,sh; (3) (radiotherapy and head and neck neoplasms).ti,ab.rw,sh;
(4) (head and neck cancer and radiation therapy and dental).ti,ab.rw,sh; and (5) (quality of life and radiotherapy and mouth neoplasms/or tongue neoplasms/or mandibular neoplasms/or oral cancer).ti,ab.rw,sh. The literature search resulted in 60 original papers from the selected search terms and 55 additional articles from the core paper reference lists. Inclusion criteria for papers accepted for closer review were the following: the study was identified as a randomized clinical trial, a case-control study, a cross-sectional observational cohort study, or a controlled follow-up study. Case reports and smaller case series (less than 50 cases) were excluded from further review. Only studies involving subjects over 18 years of age were accepted.
General Observations from the Literature Search
The systematic review of the literature revealed that our knowledge in this area is based primarily on multicase series from academic health centers reporting oral complication rates and the influence of dental factors on complications among radiated patients involved in prospective observational studies or retrospective cohort analyses. Few randomized clinical trials have evaluated the impact of oral health interventions on treatment outcome (Dreizen et al., 1977; Horiot et al., 1983; Marx et al., 1985). One group is currently conducting a multicenter international study to validate its recently proposed model to guide preradiation dental treatment decisionmaking in patients with head and neck cancer (Bruins et al., 1998).
The number of comparative multicase cohort studies of the efficacy of different treatment protocols is limited. The efficacy of various preradiation dental assessment and treatment approaches (e.g., aggressive dental extraction versus dental preservation) is determined largely through time cohort comparisons of outcomes (Bedwinek et al., 1976; Keys and McCasland, 1976; Murray et al., 1980a,b). It became evident that large, well-designed, case-control prospective studies are urgently needed in this important area. Current management recommendations are based on limited clinical studies supplemented by expert opinion and consensus as discussed at the National Institutes of Health Consensus Development Conference on Oral Complications of Cancer Therapies: Diagnosis, Prevention and Treatment, held in Bethesda, Maryland, in April 1989 (NIH, 1989).
Acute and Chronic Complications of Radiation Therapy to the Head and Neck Region
Orofacial complications are unfortunately common with all modalities of treatment for head and neck malignancy (Dreizen, 1990). High-dose radiation therapy delivered by external beam, implant devices (brachytherapy), or both may be required to manage more than half of head and neck neoplasms (SEER,
1993). Of the early or acute orofacial complications requiring consideration and management solely during the course of therapy, oral mucositis is one of the most common and distressing. Mucositis decreases the quality of life by causing pain and interfering with nutritional intake and may require cessation of radiation until some healing occurs. Mucositis surveillance and management commonly occur in conjunction with radiation treatments and are already covered by Medicare; hence, these are not a focus of this review.
Chronic or longer-term orofacial complications of radiation to the head and neck region include xerostomia and consequent dental demineralization or “radiation” caries (when salivary glands are radiated), trismus (when muscles of mastication are radiated), and osteoradionecrosis (ORN) (Beumer et al., 1979a,b; Dreizen, 1990). Salivary gland tissue is highly susceptible to radiation damage at both the acinar cell and the vascular levels, resulting in reduction in resting or basal and stimulated salivary flow (Liu et al., 1990; Valdez et al., 1992). The extent and permanency of xerostomia depend on the total radiation dose delivered and the volume and type of salivary gland tissue in the field of radiation (Liu et al., 1990; Valdez et al., 1992). With conventional bilateral external beam radiotherapy doses of 60–70 Gy to the parotid glands, saliva production decreases rapidly, with eventual 95% reduction and limited recovery (Dreizen et al., 1977). Partially radiated glands (e.g., mantle field or unilateral field) have less diminution in flow, 30–40% and 50–60%, respectively (Liu et al., 1990). Detrimental changes in salivary constituents also occur, such as lowered pH and lowered bicarbonate concentration resulting in decreased buffering capacity (Funegard et al., 1994). As a consequence of xerostomia, tooth demineralization and cavitation can occur at a rapid rate and involve atypical “radiation caries” patterns of decay on the incisal or cuspal tips and the cervical regions of teeth (Makkonen, 1987; Markitziu et al., 1992).
The most serious, although uncommon, orofacial complication is ORN. Radiation to the bone results in endarteritis obliterans, with small-vessel thrombosis and a slow protracted loss of osteocytes and osteoblasts with a consequent slow bone remodeling that leads to the risk of bone necrosis and subsequent infection (Dreizen, 1990). The mandible is at greater risk with its more compact bone of higher density and poorer blood supply than the maxilla. Higher radiation dose, fraction size, and number of fractions increase the risk as do continued tobacco and alcohol abuse, poor nutritional status or oral hygiene, and immune defects (Kluth et al., 1988). Although ORN may occur spontaneously, trauma is a significant precipitating event, with dental extractions being a common traumatic event. Trauma from tooth extraction and periodontal disease contributes to the three times higher ORN incidence in dentate than edentulous patients (Murray et al., 1980a,b). The highest incidence of ORN occurs when extractions immediately proceed or follow radiation therapy (Epstein et al., 1987). Figure C-5 shows a proposed mechanism for the consequences of radia-
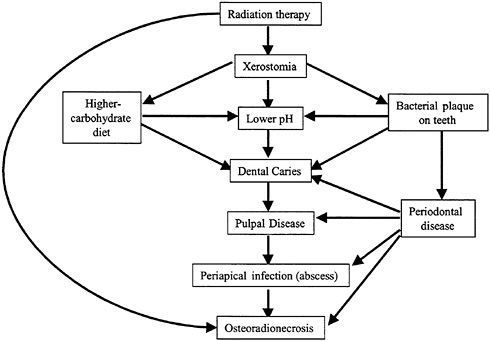
FIGURE C-5 Proposed mechanism for the interaction of radiation and oral cavity dental processes leading to pathology of radiation injury. SOURCE: Modified from Keys and McCasland, 1976.
tion therapy in the oral cavity, including the potential for necrotic breakdown of the mandible or maxilla.
Pretreatment Dental Assessment
Expert opinion and professional consensus suggest that to be effective, pretreatment dental assessment should be conducted by knowledgeable dental professionals in collaboration with the radiation oncologist and head and neck cancer surgeon. Oral health care interventions and long-term maintenance should be implemented with education and motivation programs to enhance patient understanding and compliance (Wright, 1990). The goals of pretreatment assessment include identification of possible sources and sites of ORN, presurgical assessment for prosthetic rehabilitation, and initiation of a preventive protocol for radiation-induced caries (Sonis et al., 1990). Comprehensive oral evaluation includes clinical, radiographic, and adjunctive components (Sonis et al., 1990). Teeth with compromised long-term prognosis due to pulpal or periodontal infection in the poorly compliant patient should be extracted prior to radiation, while intact teeth can be preserved under certain circumstances in the highly motivated patient who is able to maintain ideal oral hygiene, can adhere to rig-
orous preventive oral health regimens, and has access to comprehensive dental care. A recent model has been proposed to assist the clinician conducting the pretherapy oral screening in identification and elimination of the dental risk factors (Bruins et al., 1998). This model transforms clinical criteria for evaluating dental pathological conditions and malignancy- and patient-related conditions into probability estimates used to determine the choice between restoring and extracting a given tooth prior to radiation.
Prevalence of Dental Disease in the At-Risk Population
The oral health status of individuals diagnosed with new head and neck cancers has been evaluated by oral screening prior to radiation therapy in several cancer treatment centers (Brown et al., 1990; Lockhart and Clark, 1994; Roos et al., 1996). Between 33 and 43% of head and neck cancer patients are edentulous at the time of diagnosis (Lockhart and Clark, 1994; Niewald et al., 1996; Roos et al., 1996). While a full complement of adult teeth is 32, 75 upper- to middle-class dentate preradiation patients with a mean age of 60 years had—on aver-age—10 teeth remaining in one U.S. observational study by Lockhart and Clark (1994). On oral screening, 94% of these patients had some plaque and calculus, 66% had significant bone loss, and 71% had decay in one or more teeth. Consistent with this was an observational cohort of oral cancer patients in Germany with a mean age of 55.5 years reporting dental findings obtained on 126 patients prior to radiation that indicated a mean of 11 teeth remaining (Niewald et al., 1996). This German population had an average of 2.4 carious, 1.0 necrotic, 2.4 loose, and 0.7 destroyed teeth. One case-control study indicated that 100 dentate patients with head and neck squamous cell carcinoma examined prior to radiation had greater extent of tartar buildup (53% versus 35%), greater extent of moderate to severe gingival inflammation (63% versus 42%), and more decayed teeth (59% versus 39%) than 214 tumor-free controls (Maier et al., 1993).
Preventive Dental Treatment Needs
Baseline dental treatment needs for the dentate population of preradiation patients have been identified in observational studies. Both dentate and edentulous patients undergoing any comprehensive pretreatment oral assessment would be evaluated by comprehensive oral examination and dental or panoramic radiographs. The percentage of dentate patients requiring specific preventive or therapeutic dental services is as follows: dental prophylaxis or scaling, 20–95%; dental restorations, 55–64% (mean five teeth); extractions, 44–75% (mean six teeth); and endodontic therapy, 0–7% (Brown et al., 1990; Epstein et al., 1999; Lockhart and Clark, 1994; Niewald et al., 1996; Roos et al., 1996; Toljanic et al., 1998).
Efficacy of Pretreatment Care: Aggressive Extraction—No Prevention Versus Dental Preservation Approach
Perhaps the most significant impact dental care can have on improving the clinical outcome of radiation treatment for the head and neck cancer patient is the ability of adequate pretreatment care to reduce the risk for ORN of the jaws. A paradigm shift occurred in the early 1970s to a dental preservation approach from the approach of routine whole-mouth extractions or at least extraction of all teeth in the field of radiation, regardless of dental status, in an attempt to prevent ORN. The earlier aggressive extraction approach was not coupled with dental caries preventive measures, so postradiation extractions frequently became necessary for teeth that had not been removed prior to radiation. Keys and McCasland (1976) compared outcomes of two time cohorts of patients with cancer of the head and neck (excluding larynx) treated at the Walter Reed Army Medical Center using fairly constant radiation techniques, dose levels, and treatment policy. A preservation-oriented comprehensive dental care program (DCP) was instituted in 1969 with the following objectives: to reduce radiation caries incidence, to preserve as many useful teeth as possible for optimal dental function while avoiding edentulous arches for which prosthodontic alternatives are limited, to prevent significant ORN, and to provide a mechanism for continuing maintenance of optimal dental health during and after cancer therapy. The comprehensive program involved three phases: (1) before radiation, (2) during radiation, and (3) after radiation. Phase I consisted of an oral evaluation and a caries control program including prophylaxis, oral hygiene instructions, daily fluoride gel application, restoration of active decayed teeth, and needed extractions. Phase II consisted of oral hygiene reinforcement. Phase III consisted of all subsequent definitive dental and prosthetic care.
Results comparing 115 radiation patients treated under the DCP between 1970 and 1974 with the last 74 patients radiated prior to the program’s institution revealed that all aspects of the dental condition were improved under the DCP (Keys and McCasland, 1976). Full-mouth extraction cases were reduced from 36% of pre-1970 patients to 6% in 1970–1974 under the DCP. Additional results of the DCP protocol revealed increases in teeth saved (from 50 to 78%) and decreases in teeth extracted postradiation (14 to 2%), reduced need for restorations postradiation (37 to 10%), lower caries incidence (46 to 12%), and fewer edentulous arches (49 to 43%). Although no cost analysis was available, some data on dental effort were reported. Of 1,113 teeth involved before 1970, 49% were extracted and 1% restored prior to radiation versus 22 and 10%, respectively, of 1,915 teeth cared for under the DCP. Postradiation dental effort included extractions of 7% of teeth, restoration of 16%, and other care (includes prosthetic and endodontic care) of 6% before the DCP versus 2% extraction, 8% restoration, and 4% other under the DCP. Patients managed prior to the DCP had—on average—six more dental visits (23.1 versus 17.3) than those managed
under the DCP, with reduction in average number of pretreatment visits per patient from 9.4 to 8.0 and posttreatment visits from 13.7 to 9.3. Incidence of ORN was historically low at Walter Reed, with only 13 patients exhibiting this problem from 1950 to 1970. One case of ORN developed during the DCP protocol (1970–1974). Hence, no conclusions can be drawn with regard to the DCP’s influencing ORN rates.
One of the mainstays of the dental preservation approach in the radiation-induced xerostomic patient is the use of daily topical fluoride to prevent tooth decay. The earliest randomized, placebo-controlled prospective clinical study of the efficacy of topical fluoride to prevent caries in 42 xerostomic, irradiated patients was conducted at one of the leading U.S. cancer centers, M.D. Anderson Hospital and Tumor Institute in Texas, by Dreizen and coworkers (1977). Dental prophylaxis, oral hygiene instructions, and dental restorations preceded randomization. Patients (n=13) on the regimen of oral hygiene, 1% sodium fluoride (NaF) gel in plastic carriers, and unrestricted diet had significantly (p<.001) lower caries incidence (3.23 versus 22.21 mean decayed, missing, and filled tooth surfaces—DMFS) than the group (n=14) on the oral hygiene-placebo gel-unrestricted diet regimen. The nine patients who began in the placebo gel group and were crossed over to the fluoride gel group due to a postradiation caries upsurge evident on a three-month interval exam also had significantly (p<.001) lower caries incidence (3.67 versus 22.21 mean DMFS) than the group on the oral hygiene-placebo gel-unrestricted diet regimen. Restriction of sucrose in the diet added to the NaF gel regimen (n=11) further reduced the mean DMFS to 0.55. In this study, patients were reexamined every 3 months, for an average of 9 months for the placebo gel group, 26 months for the NaF gel group, 22 months for the crossover group, and 13 months for the NaF gel and sucrose restriction group.
Subsequently, several clinical trials have been conducted to compare the efficacy of different fluoride regimens where no fluoride-free control groups were used. Horiot and coworkers (1983) enrolled 222 irradiated patients in a prospective randomized protocol to compare daily applications of topical NaF gel with high-content fluoride toothpaste (1,350 parts per million [ppm] F−). At 12–36 months’ follow-up, dental caries were observed in 3% of gel patients versus 11% (p=.1) of toothpaste patients. Al-Joburi and coworkers (1991) enrolled 184 dentate postradiation patients (mean dose 57 Gy) in a clinical trial of the efficacy of two fluoride systems to prevent radiation caries. One-year reexamination of 143 patients for coronal and root surface caries revealed significantly higher decay rates for the noncompliant patients (p<.05) compared to either the group using daily brushed-on 0.4% stannous fluoride (SnF) gel or the group using 1.1% NaF gel applications for the first three months followed by twice daily remineralizing mouthwash for the last nine months. Comparison of the fluoride treatments indicated that continual daily use of SnF brush-on gel was superior to three-month NaF gel or nine-month remineralizing mouth rinse in preventing root caries. Pochanugool and coworkers (1994) reported on a small, single-center
clinical trial involving 73 postradiation patients, where the dental effects of three topical fluoride regimens were compared by simple sampling. The three regimens were: (1) 1% NaF gel applied daily in a plastic tray, (2) 1% NaF oral solution used five minutes a day, and (3) combined gel and oral solution use. A dental care program involving preradiation screening, restoration, and extraction of condemned teeth was in effect at the time of this trial. Groups were comparable in follow-up time and age, with total radiation dose of 45–76 Gy (mode 70 Gy) for all patients. The need for further restorations varied by treatment group from 68.2% using the NaF solution, to 65.5% on NaF gel, to 54.4% using both. Need for further extractions varied from a low of 6.9% for the NaF gel group to a high of 22.7% for the NaF solution group, suggesting some increased ability to preserve teeth for the NaF gel users. Obtaining adequate patient compliance with daily fluoride gel applications in custom carriers remains a challenge, necessitating regular dental follow-up (Epstein et al., 1995, 1996).
Expert opinion suggests that to maximize the impact of pretreatment assessment, it should occur at least two weeks prior to therapy initiation to allow adequate time for recommended treatment and healing (Keys and McCasland, 1976; Sonis et al., 1990). When the urgency of radiation precludes ideal timing of oral screening and treatment, the initial dental evaluation should be conducted as soon as possible to form the basis of a preventive dental treatment plan for reducing complication risks. Comprehensive protocols for the prevention of oral sequelae resulting from head and neck radiation therapy have been presented (Jansma et al., 1992).
Influence of Paradigm Shift to Dental Preservation on Incidence of Osteoradionecrosis
The incidence of ORN declined in the 1970s and after, with changes in the approach to oral preparation for radiation therapy presumably playing a major role in this decline (Table C-4). One of the earliest demonstrations of the potential for dental conservation to reduce the incidence of the most morbid radiation complication, ORN, was conducted at M.D.Anderson (Bedwinek et al., 1976). Bedwinek and coworkers (1976) compared two periods of dental management for patients treated with definitive radiation to the oral structures with respect to incidence and precipitating factors for ORN. During a period of elective dental extraction (1/1/66–6/30/69), 203 patients (19.7%) developed ORN, with precipitating factors assigned as follows: dental extraction (11.8%), denture irritation (2.5%), and spontaneous (5.4%). In contrast, during the subsequent period of dental conservation (7/1/69–6/30/71), 178 patients (7.9%) developed ORN, with precipitating factors assigned as follows: dental extraction (2.3%), denture
TABLE C-4 Osteoradionecrosis Incidence in Studies of 100 or More Cases
|
Year |
Author(s) |
Radiation Years |
Location |
No. of Subjects |
No. ORN |
% ORN |
Dental Preservation Program in Place? |
|
1966 |
Grant and Fletcher |
1954–1962 |
M.D.Anderson (TX) |
176 |
66 |
37.5 |
No |
|
1967 |
Rahn and Drone |
1960–1962 |
M.D.Anderson (TX) |
120 |
53 |
44 |
No |
|
1971 |
Rankow and Weissman |
1965–1968 |
Columbia (NY) |
176 |
12 |
6.3 |
No |
|
1972 |
Beumer et al. |
1961–1969 |
UCSF (CA) |
354 |
10 |
3.6 |
Unknown |
|
1972 |
Wang |
1959–1968 |
Mass General (MA) |
262 |
15 |
6 |
Unknown |
|
1974 |
Marciani and Plezia |
Not reported |
Allen Park VA (MI) |
220 |
23 |
10.5 |
No |
|
1976 |
Bedwinek et al. |
1966–1969 |
M.D.Anderson (TX) |
203 |
40 |
19.7 |
No |
|
|
|
1969–1971 |
|
178 |
14 |
7.9 |
|
|
1981 |
Horiot et al. |
1972–1979 |
Ctr. Leclerc (France) |
208 |
4 |
2 |
Yes |
|
1986 |
Marciani et al. |
1976–1984 |
Lexington VA (KY) |
109 |
3 |
3 |
Yes |
|
1987 |
Epstein et al. |
1977–1984 |
UBC (Canada) |
1,000 |
27 |
2.7 |
Yes |
|
1987 |
Makkonen et al. |
1974–1977 |
U.Turku (Finland) |
224 |
0 |
0 |
Unknown |
|
1987 |
Schweiger |
1979–1983 |
Mem Sloan-Ket (NY) |
324 |
6 |
1.8 |
Unknown |
|
1989 |
Widmark et al. |
1974–1979 |
U.Goteborg (Sweden) |
431 |
19 |
4.4 |
Unknown |
|
1992 |
Kumar et al. |
1980–1988 |
Med Col Bikaner (India) |
1,104 |
14 |
1.2 |
Yes |
|
1996 |
Niewald et al. |
1988–1992 |
U.Saarland (Germany) |
116 |
10 |
8.6 |
Yes |
|
1998 |
Toljanic et al. |
1986–1993 |
U.Chicago (IL) |
193 |
9 |
4.7 |
Yes |
irritation (1.1%), and spontaneous (4.5%). Dental conservation at M.D.Anderson involved restorative dental procedures, regular oral prophylaxis, and daily fluoride applications.
Murray and coworkers (1980a,b) extended the analysis on the M.D.Anderson cohort by comparing 404 subjects in an even later dental conservation period (7/1/71–12/31/75) with 249 subjects managed by elective dental extraction in the original 1/1/66–6/30/69 time period. ORN rates were reduced from 24.5% in the first period to 19.1% in the second period (p=.06) (Murray et al., 1980a). This study included more subjects and a longer observation time than the previous report of Bedwinek and coworkers (1976). Using multivariate logistic regression, Murray and coworkers (1980a;b) identified several ORN risk factors: a 5-fold higher risk for tumors near the mandible; tumor doses above 80 Gy created a 2.9-fold higher risk than doses below 50 Gy; and the dentate had a 2.6-fold higher risk than the edentulous. In reviewing incidence of necrosis by cause, in the elective extraction period, etiology was assigned to extractions prior to radiation for 32.4% ORN cases and to postradiation extractions in 2.9%, compared to 5.2 and 6.5%, respectively, in the dental conservation period. Spontaneous or unknown cause of ORN rose from 38.2% of cases to 74.0% of cases over these time periods. In a further evaluation of dental factors, Murray and coworkers (1980b) showed that ORN is most likely in the first 3–12 months following radiation, although the risk persists indefinitely. Timing of extractions influenced necrosis risk, with significantly higher necrosis rate among postradiation extraction patients than the rest of the dentate (p=.004) and those whose extractions occurred prior to radiation.
Kluth and coworkers (1988) at West Virginia University conducted a small case-control study of factors contributing to the development of ORN among patients receiving radiation for head and neck malignancies between July 1973 and June 1983. This study revealed an ORN rate of 10.3% during this period among patients followed for 18 months or until death. This resulted in 14 ORN cases among 135 radiated patients. Controls were 28 of the remaining 121 non-ORN patients matched for age, sex, general medical condition, tumor location, and stage (to some extent). Tumor stage among the ORN cases was slightly more advanced (85% Stage III, IV, or recurrent cancer among cases versus 64% of controls), although the control group received slightly higher radiation doses (50–70 Gy for 57% cases and 79% controls). ORN occurred in 4 of 14 patients receiving less than 50 Gy. Although the majority of patients in both groups had moderate to severe xerostomia, the dentate ORN cases (6/8) were more likely to have poor oral hygiene than controls (0/19). Inadequacy of preradiation dental care was apparent among 5 of 14 cases and 0 of 28 controls. Two patients in each group received inade-quate postradiation dental follow-up. Among ORN cases,
five of nine with teeth had extractions before radiation, and two had extractions during or after radiation. In the control group, 6 of 19 patients with teeth had preradiation extractions and 3 had postradiation. Continued heavy tobacco and alcohol use were also more common among cases than controls (10 of 14 cases versus 0 of 28 controls).
Additional studies using cohorts of ORN patients have reported on dental factors identified as precipitating events. Beumer and coworkers (1984) analyzed risk factors for 83 episodes of ORN at the University of California at Los Angeles over an 11-year period ending July 1982. The most common precipitating factors were postradiation extractions (22 of 83; 26.5%), periodontal disease (19 of 83; 22.8%), and preradiation extractions (17 of 83; 20.4%). A recent analysis by Curi and Dib (1997) of necrosis risk factors among 104 cases of ORN of the jaws treated from 1972 to 1992 revealed that 89.4% resulted from induced trauma and 10.6% were spontaneous necrosis. More individuals with ORN had no preradiation oral care (57.7%) than had oral care (42.3%). Two peaks of ORN incidence were evident: the first peak less than 12 months from completion of radiation, with 16% resulting from oral or dental infections, and the second peak from 24 to 60 months after radiation, with 60% resulting from oral or dental factors, largely trauma from dental extractions. Breakdown of extraction sites has become a well-accepted causal event for ORN, suggesting that dental treatment planning aimed at limiting extractions to unsalvageable teeth is the most prudent approach to preparing the patient’s mouth for the effects of radiation. Evidence is accumulating to support the paradigm shift toward dental preservation and away from radical preradiation extractions, which is the approach that current Medicare coverage supports.
Is There a Role for Prophylactic Hyperbaric Oxygen Therapy in the Prevention of Osteoradionecrosis from Postradiation Extractions?
Marx et al. (1985) have proposed a role for prophylactic hyperbaric oxygen (HBO) therapy in facilitating head and neck surgical wound healing and thus preventing ORN resulting from postradiation surgical trauma induced by extractions. HBO stimulates angiogenesis, with increased neovascularization and optimization of cellular levels of oxygen for osteoblast and fibroblast proliferation, collagen formation, and support of in-growing blood vessels, thus improving the healing capacity of hypoxic radiated tissue (Myers and Marx, 1990). Marx and coworkers (1985) at the University of Miami reported the use of a prophylactic regimen of HBO delivered prior to traumatic dental surgery in the postradiation patient treated with 60 Gy or higher dose. This randomized prospective multicenter clinical trial indicated a reduction of ORN from 29.9% among 37 patients (31 of 137 socket wounds) covered with penicillin during and after extractions to 5.4% among 37 patients (4 of 156 socket wounds) who un-
derwent 20 sessions of preoperative and 10 sessions of postoperative HBO (Marx et al., 1985). Using a cost analysis, the $8,000 average total cost of their HBO-ORN preventive protocol with its 94.6% prevention rate stood up favorably against the average total cost (normalized to 1984 dollars) of $30,000 to $69,000 for ORN treatment (Marx et al., 1985).
Given the high cost and limited availability of prophylactic HBO, its use has remained controversial (Clayman, 1997; Lambert et al., 1997; Maxymiw et al., 1991). Maxymiw and coworkers (1991) in a single-technique 72-patient case series at Princess Margaret Hospital in Toronto reported no ORN resulted from postradiation extractions where 196 teeth were in the direct field of radiation (median dose of 50 Gy) by using prophylactic penicillin, low-dose or no vasoconstrictor-containing local anesthesia, atraumatic surgical technique, and largely single-tooth extractions. Similarly, Lambert and coworkers (1997) reported no ORN among 47 patients followed on average 2.9 years after receiving prophylactic HBO using the Marx protocol prior to postradiation multiple extractions. HBO may have the greatest prophylactic benefit when multiple adjacent teeth in the direct field of radiation require extraction. This need occurs most commonly when radiation patients have no or inadequate preradiation dental evaluation and treatment or when they fail preventive measures.
What Treatment Is Required to Manage Osteoradionecrosis of the Jaws?
Conservative measures are used initially following the development of bone necrosis in almost all cases. These consist of oral saline or antiseptic (e.g., chlorhexidine) rinses, oral antibiotics (e.g., metronidazole, clindamycin, amoxicillin) during times of acute infection episodes, and/or significant pain and gentle sequestrectomy. In the study of Beumer and coworkers (1984) at the University of California, Los Angeles, conservative measures healed 30 of 83 (36.1%) episodes, with greatest success with ORN induced by denture irritation or preradiation extractions and least success with bone exposures occurring spontaneously or in direct association with remaining dentition. Treatment beyond conservative management was required in the remaining 53 episodes as follows: surgical sequestrectomy, 18 (21.7%); radical jaw resection, 13 (15.7%); HBO alone, 6 (7.2%); HBO and surgical sequestrectomy, 6 (7.2%); and HBO with mandibular resection, 10 (12%). Radical mandibular resection was reserved for patients whose necrosis proceeded to intractable pain and/or pathological fracture usually accompanied by orocutaneous fistula. In a British study examining 22 ORN cases that were severe enough to require jaw resection identified among 2,853 radiated patients, dental extractions pre-, during, and postradiation were found to be causative in 10 cases (Coffin, 1983).
In recent years, HBO has gained an important role in treating radiation complications for head and neck cancer patients (Myers and Marx, 1990), often
in conjunction with surgical management. A study of 29 patients treated with HBO for ORN of the mandible from 1984 to 1992 revealed that nearly all patients also underwent sequestrectomy (16 of 29 subjects; 55%) or mandibular resection (11 of 29 subjects; 38%) (van Merkesteyn et al., 1995). In a long-term follow-up study of 20 cases of ORN treated with HBO between 1975 and 1989, Epstein and coworkers (1997) reported that the majority (60%) remained resolved. Recurrences presented in 2 patients, suggesting that postradiation patients remain at risk of ORN indefinitely. HBO treatment of ORN is now covered by Medicare.
What Is the Quality of Life Impact of Head and Neck Cancer Treatment?
Oral complications following radiation therapy for oropharyngeal carcinoma adversely affect quality of life (Bundgaard et al., 1993; De Graff et al., 1999; Epstein et al., 1999; Teichgraeber et al., 1985). A recent survey of 65 postradiation patients using the general quality-of-life survey (the European Organization for Research and Treatment of Cancer [EORTC] Quality of Life Questionnaire QLQ-C30), with added oral symptom and function scales, revealed the following: 91.8% had dry mouth; 75.4%, changes in taste; 63.1%, dysphagia; 50.8%, altered speech; 48.5%, difficulty with dentures; 43%, difficulty chewing or eating; and 38.5%, increased tooth decay (Epstein et al., 1999). Pain, which was present in 58.4%, interfered with daily activities in 30.8%. The frequency of oral side effects correlated with radiation treatment fields and dose.
Responses of 188 posttherapeutic subjects with upper aerodigestive tract cancers to the same health-related quality-of-life (HRQL) instrument were analyzed to investigate the hypothesis that dental status is a predictor of HRQL (Allison et al., 1999). Two multivariate models containing age, gender, employment status, cancer site, and disease stage, plus a dental status category, were developed. Significantly worse HRQL was identified among those who were partially dentate with no prostheses. This group reported significantly more “problems with their teeth,” more “trouble eating,” and more “trouble enjoying their meals.” The dental status category of edentulous patients with prostheses predicted a significantly better HRQL. Hence, a full complement of either healthy natural teeth or functional prosthetic teeth is valued by the postradiation patient.
Summary
This systematic review of the literature, focused on dental services that may be medically necessary in the context of radiation therapy to the jaws, has indicated that radiation results in poorer patient outcomes in the absence of a dental preservation program to maintain oral health. Adverse outcomes include increased
incidence of radiation-induced dental caries often necessitating postradiation dental extractions and subsequent increased frequency of the most debilitating outcome of radiation to the jaws, ORN of the jaws. Prior to the 1970s a relatively aggressive extraction approach, often full-mouth extractions, coupled with no preventive services, was the treatment of choice. Preradiation extractions were found to be a risk factor for ORN, supporting a paradigm shift toward extraction of only the unsalvageable teeth while preserving the functional teeth with needed restorations, periodontal care, and caries-preventive daily fluoride treatments. It would appear that expanding Medicare coverage to include preradiation preventive dental care and routine postradiation preventive services for the head and neck cancer patient would effectively promote better clinical outcomes and would be consonant with the current standard of care for managing these individuals.
Based on data from several studies described above, Figure C-6 illustrates the clinical effectiveness of a dental preservation approach that may reduce the incidence of ORN by an average of 78%, or 8 percentage points—from 10.2% to 2.25%—largely due to reducing the both preradiation and postradiation oral surgical intervention. Under the aggressive extraction approach, most cases of ORN attributable to dental factors are attributable to preradiation extractions.
CONDITIONS 2 AND 3: LEUKEMIA AND LYMPHOMA
Introduction
Leukemia, an abnormal proliferation of white blood cells, and lymphoma, a disease affecting the lymphoid tissue, are distinct but related conditions. Treatment for these diseases is similar, involving high-dose chemotherapy and/or radiation therapy, resulting in profound immunosuppression. With both leukemia and lymphoma, the rationale for medically necessary dental services is to reduce or eliminate the risk of infection during treatment and to manage any complications that may occur, either during or following treatment. Consequently, background information and evidence for medically necessary dental services are presented together.
Methods
This review identified all publications from 1985 to 1999 that examined (1) the prevention and treatment of oral complications of leukemia and lymphoma caused by chemotherapy and bone marrow transplantation, and (2) oral side effects of various modalities of chemotherapy for leukemia and lymphomas. These publications were identified through MEDLINE.
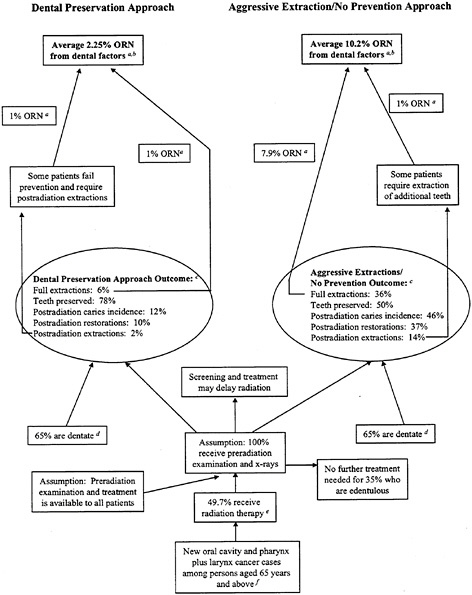
FIGURE C-6 Clinical effectiveness of dental preservation approach in reducing osteoradionecrosis (ORN) as adverse medical outcome. Estimated net reduction of 78% ORN cases with preservation approach. SOURCES: a: Murray et al. (1980a,b); b: Bedwinek et al. (1976); c: Keys and McCasland (1976); d: Lockhart and Clark (1994), Niewal et al. (1996), and Roos et al. (1996); e: SEER (1993); and f: Landis et al. (1999).
Leukemia
The term leukemia signifies a heterogeneous group of neoplasms arising from malignant transformation of hematopoietic cells. Leukemic cells prolifer-
ate primarily in the bone marrow and lymphoid tissues, where they interfere with normal blood formation and immunity, and ultimately migrate into the peripheral blood, thereby infiltrating other tissues. Leukemias are classified according to the predominant cell type and as either acute or chronic, based on their natural history, with the former having a rapid clinical course. Causes of most leukemias are unknown, but various forms show association with certain genetic abnormalities, excessive exposure to ionizing radiation or certain chemicals, or retroviruses.
Patients with leukemia often present with fatigue, paleness, unexplained weight loss, repeated infections, bruising, and nosebleeds or other hemorrhages. In children, these signs can appear suddenly. Chronic leukemia can progress slowly with few symptoms. The various forms strike both sexes and all ages. Because the symptoms and signs are common to a variety of less serious conditions, early detection is often difficult. Diagnosis is made using blood tests and bone marrow biopsy.
Leukemia Incidence and Burden
An estimated 30,200 new cases of leukemia are anticipated in 1999, about evenly divided between acute leukemia and chronic leukemia (ACS, 1999; Ries et al., 1999). Leukemia is expected to strike many more adults (27,900) than children (2,300) this year. Acute lymphocytic leukemia accounts for about 1,500 (65%) of the cases of leukemia among children. In adults, the most common types are acute myeloid (about 10,100 cases) and chronic lymphocytic (about 7,800 cases). The incidence of leukemias in general is greatest among those individuals 65 years of age and older, with 0.051% of the population (or 51.4 per 100,000) newly affected each year. An estimated 22,100 deaths are anticipated from leukemia in 1999 (ACS, 1999; Ries et al., 1999).
The one-year relative survival rate for patients with leukemia is 63%. Survival drops to 43% at five years after diagnosis, due primarily to the poor survival of patients with some types of leukemia such as acute myelocytic. Survival for patients with acute lymphocytic leukemia has improved dramatically—from a five-year relative survival rate of 38% in the mid-1970s to 55% in the late 1980s. Survival rates for children increased from 53 to 78% over the same time period.
Five-year survival rates are lowest among the 65-year and older population for the acute myeloid and acute lymphocytic leukemias. Relatively slight differences are found among males and females for five-year survival rates for all leukemias except the chronic myeloid variety.
Leukemia—Clinical Oral Aspects
About 89% of patients with undiagnosed acute lymphocytic leukemia have oral problems associated with disease onset; 22% of these cite these problems as their reason for seeking medical care. Almost two-thirds of patients with other
forms of acute leukemia demonstrate oral changes during the early, undiagnosed stages of disease. One-third of these seek medical evaluation for oral changes such as gingival oozing or bleeding, petechiae, hematoma or ecchymosis formation, oral ulceration, pharyngitis, gingival infection, or gingival hyperplasia (Sonis et al., 1995).
Intensive cancer chemotherapy and ionizing radiation result in oral mucositis in 36–100% of patients. Erythema and edema progress to ulceration and often mucosal bleeding accompanied by mild burning to severe pain. Mastication and deglutition may be intolerable. These clinical changes have important systemic implications for myelosuppressed patients who have had bone marrow transplantation (BMT), including risk of microbial invasion with serious regional or systemic infections. Despite many different approaches to palliation, there has been little substantive improvement in the ability to prevent or treat therapy-induced oral mucositis in patients with cancer. Most clinicians recommend dental treatment in patients undergoing BMT before it is started.
Lymphoma
The term lymphoma signifies neoplasms primarily of the lymphoid tissues. The two major variants of malignant lymphoma are non-Hodgkin’s lymphoma and Hodgkin’s disease. Although both tumors infiltrate reticuloendothelial organs, they differ from each other in both biological and clinical behavior, and are generally regarded as different diseases.
Patients with lymphoma present with enlarged lymph nodes, itching, fever, night sweats, anemia, and unexplained weight loss; fever may be intermittent for periods of several days or weeks. Risk factors are largely unknown, but partially involve reduced immune function and exposure to certain infectious agents. Persons with organ transplants are at higher risk from altered immune function. HIV and human T-cell leukemia/lymphoma virus-I (HTLV-I) are associated with increased risk of non-Hodgkin’s lymphoma. In Africa, the Epstein-Barr virus is implicated in Burkitt’s lymphoma. Other possible risk factors include occupational exposure to herbicides and perhaps other chemicals.
Lymphoma Incidence and Burden
An estimated 64,000 new cases of lymphoma are projected in 1999, including 7,200 cases of Hodgkin’s disease and 56,800 cases of non-Hodgkin’s lymphoma (ACS, 1999; Ries et al., 1999). Since the early 1970s, incidence rates for non-Hodgkin’s lymphoma have nearly doubled; during the 1990s, the rate of increase appeared to be slowing. Incidence rates for Hodgkin’s disease have declined over the past two decades, especially among the elderly. About 27,000 deaths in 1999 (non-Hodgkin’s lymphoma, 25,700; Hodgkin’s disease, 1,300) are anticipated.
Non-Hodgkin’s disease has an incidence rate among the population 65 years of age or older that is eight times greater than among those under 65 years and is far more common among males than females. About 0.075% of the population, or 75.5 per 100,000 people, age 65 years and older develop non-Hodgkin’s lymphoma each year. Among the population over 65 years old, males are about 1.5 times more likely than females to develop both Hodgkin’s disease and non-Hodgkin’s lymphoma.
Survival rates vary widely by cell type and stage of disease. The one-year relative survival rates for Hodgkin’s and non-Hodgkin’s lymphoma are 93 and 70%, respectively; the five-year rates are 82 and 51%. Ten years after diagnosis, the relative survival rates for Hodgkin’s and non-Hodgkin’s disease decline to 77 and 44%, and the 15-year survival rates to 66 and 36%, respectively.
The five-year survival rate for all types of lymphomas is less than 50% for individuals 65 years of age and older. No difference in survival is apparent among those over 65 years of age for either of the two types of lymphomas.
Lymphoma—Clinical Oral Aspects
Oral manifestations of Hodgkin’s disease are limited. Patients usually present complaining of increasing unilateral painless swelling of the neck (Sonis et al., 1995). If the disease is widespread, patients may complain of difficulty with breathing and shortness of breath due to involvement of the mediastinal nodes.
Non-Hodgkin’s lymphoma may appear in the mouth as a primary tumor or as a secondary manifestation of a tumor elsewhere. Most commonly, this lymphoma is manifest as a nonhealing painless ulceration with a pebbly, uneven surface that appears to glisten, with ill-defined borders, that undermines surrounding mucosa. The gingiva, palate, and tonsillar areas are most frequently affected. For the most part, the oral aspects of the lymphomas and leukemias are related to treatment.
Oral Complications of Treatment for Leukemia and Lymphoma: Chemotherapy and Bone Marrow Transplantation
Chemotherapy is the major clinical approach used for overall treatment of leukemia and is a key component of the management approach for lymphomas (Sonis et al., 1995). About 40% of all patients receiving chemotherapy develop oral side effects. In general, hematologic malignancies, such as leukemia and lymphoma, tend to be associated with the highest frequency of oral complications. Side effects tend to be directly related to the specific antineoplastic agent used, the drug dose administered at a given time, the timing of administration (single dose versus spread over time), and whether radiotherapy is administered at the same time. Oral side effects of chemotherapy are potentiated by radiotherapy.
Oral complications of cancer chemotherapy may be direct or indirect (Sonis et al., 1995). Direct problems result from a drug’s direct effect on oral tissues. The most common direct oral effects are mucositis and ulceration, usually occurring within five to seven days after drug administration. Oral mucosal ulceration complicating bone marrow transplantation interferes with patients’ comfort and nutrition and may lead to systemic infection derived from the mouth. The mucosal injury results from epithelial damage due to the cytotoxic effects of chemotherapy and radiation conditioning as well as from superficial oropharyngeal infection (Weisdorf et al., 1989). Other direct oral effects include xerostomia and neurotoxicity, most frequently affecting the mandibular molars. Indirect effects include infection (e.g., bacterial, fungal, or viral) or oral bleeding secondary to thrombocytopenia.
Bone marrow transplantation is being employed increasingly to treat types of cancer such as leukemia. The most common forms of BMT are allogeneic (in which marrow is transferred from a genetically matched donor to the recipient) and autologous (in which marrow is harvested from the patient, treated, preserved, and then reinfused after the patient receives chemotherapy). Patients receiving allogenic transplants are at risk not only for the direct and indirect effects of chemotherapy but also for graft-versus-host disease. Oral complications are the most frequent side effect of this disease and include lichen planus-like lesions, producing significant discomfort and xerostomia.
New treatment protocols using highly specific monoclonal antibodies directed at lymphoma cells and high-dose chemotherapy with BMT are now under investigation in selected patients who relapse after standard treatment.
Tables C-5 and C-6 present the dental and oral management considerations and manifestations as they relate to systemic aspects of Hodgkin’s disease (Table C-5) and non-Hodgkin’s lymphoma (Table C-6).
Oral Sources of Septicemia in Patients with Hematologic or Lymphatic Malignancies
Many potentially pathogenic microbial species inhabit the oral cavity. Oral microorganisms are normally harmless, leading to relatively minor, low-grade dental infections in the individual with a competent immune system. When leukemia, chemotherapy, or bone marrow transplantation compromise the immune system by producing dramatic declines in neutrophil (white blood cells, which hold the bacteria at bay) counts, however, these normal oral species may be dangerous if they gain access to the blood circulation (Wingard, 1990). Dental plaque, dental caries, and periodontal infections harbor bacteria that may result in hematogenous seeding (blood-borne infection) and septicemia. Seeding may occur through areas of oral mucositis or ulceration, through sites of gingival inflammation, with professional dental treatments, and with activities such as normal chewing and brushing (reviewed in Lockhart and Schmidke, 1994).
TABLE C-5 General Dental and Oral Considerations in Hodgkin’s Disease
|
Systemic Aspect |
Related Dental and Oral Management Consideration |
|
Functionally immunosuppressed, at risk for infection |
Chronic oral infections may become acute. Sources of oral infection should be eliminated |
|
Effects of radiotherapy, especially mantle or supradiaphragmatic radiation, which involves the neck and inferior border of the mandible |
Xerostomia as a consequence of radiation to the submandibular and sublingual salivary glands. Radiation caries can be frequent and troublesome. Oral therapy includes frequent prophylaxis, low-sucrose diet, salivary flow stimulation, and routine use of topical fluorides |
|
Chemotherapy, which may cause myelosuppression |
Oral infection and hemorrhage |
|
SOURCE: Adapted from Sonis et al., 1995, pp. 270–271. |
|
Dreizen and coworkers (1986) at M.D.Anderson Hospital in Texas reported on oral complications of antileukemia chemotherapy in 1,500 patients from 17 to 82 years of age. Daily oral exams and the culturing of suspicious oral lesions at least twice made it unlikely that contamination occurred during their hospitalizations. Oral infections, either single or polymicrobial, were documented in 513 (34.2%) patients. Candida and other fungi were causative in 20.7%, herpes simplex virus in 8.8%, gram-negative aerobic bacilli (Pseudomonas, Klebsiella, Escherichia, Enterobacter, Serratia, Proteus) in 8.1% and gram-positive cocci (Staphylococcus, Streptococcus) in 4.3%. Drug-induced mucositis and oral hemorrhages occurred in 16.3 and 13.6% of the population, respectively.
Bergmann (1989) determined the prevalence of acute oral infections and estimated their role as a possible cause of 78 episodes of fever in 46 immunocompromised patients with hematologic malignancies monitored with daily clinical and microbiological investigations. Overall acute infections were present in 92% of febrile episodes, with oral infections (largely acute candidiasis and infected mucosal ulcers) during 78% and extraoral infections (largely septicemia and pneumonia) during 73%. Acute oral infections were a probable cause of fever in 14% of febrile episodes and a possible or contributing cause of fever in a further 26%. Bergman (1988) further examined 19 septicemic episodes in this study population and, by comparing blood and oral surveillance cultures, found a probable oral focus of septicemia in two cases (10.5%), with an additional probable or possible source in six cases (31.6%). He suggests that prevention and elimination of oral infection may reduce the morbidity and perhaps mortality in these patients.
Overholser and coworkers (1982) followed 22 newly diagnosed hospitalized patients with acute nonlymphocytic leukemia from the initiation of chemo-
therapy until remission. Of interest were acute exacerbations, during myelosuppressive chemotherapy, of asymptomatic periodontal disease present at admission. In these 22 patients, 47 acute exacerbations developed, including 13 of periodontal origin, with all but 3 of these 13 occurring during pronounced neutropenia (<100 neutrophils per microliter).
Heimdahl et al. (1989) reported on the clinical, pathological, and laboratory features of oral infections in 181 consecutive patients treated with BMT at the Karolinska Institute in Sweden between 1975 and 1987. Indication for BMT in this study was leukemia in 131 (77%) subjects who had a mean age of 28 years (range 1–54); 53 patients (29%) had dental infections that needed treatment (41 underwent extractions) before BMT. BMT was postponed because of oral infection in 10 (6%) patients. Four patients were medically unstable for dental treatment and underwent BMT with existing periapical infection; one of these four turned into an acute phase during treatment and required systemically administered antibiotics and surgery. In 59 patients, microbiologically confirmed septicemia was observed during the neutropenic phase, which resulted in death in 12 patients. Septicemia was caused by oral organisms (alpha streptococci) in 24 of 59 (41%) patients, and this was associated with increased frequency of oral ulceration, particularly when methotrexate was used. Antiviral prophylaxis appeared to be protective. No attempt was made in this study to directly associate alpha streptococci with specific oral sites.
In a cohort study of 49 patients with hematologic malignancy on high-dose chemotherapy examined weekly by a dentist who obtained bacterial cultures from saliva samples, Richard and coworkers (1995) found that 7 of 49 (14%) developed a viridans streptococcal bacteremia during the study. Viridans strep-
TABLE C-6 General Dental and Oral Considerations in Non-Hodgkin’s Lymphomas
|
Systemic Aspect |
Related Dental and Oral Management Consideration |
|
May appear in mouth as a primary tumor or as a secondary manifestation of a tumor elsewhere |
Most commonly found as a nonhealing, painless ulceration with a pebbly, uneven surface that appears to glisten. Borders of ulcer are not well defined and may undermine surrounding mucosa. The gingivae, palate, and tonsillar areas are most frequently affected |
|
Treatment relies on multiagent chemotherapy and radiotherapy |
High frequency of oral complications associated with chemotherapy |
|
SOURCE: Adapted from Sonis et al., 1995, pp. 271–272. |
|
tococci with the same ribotype as the strain responsible for the bacteremia were recovered from the mouths of all bacteremic patients before the onset of bacteremia, with no shared ribotypes among patients. They concluded that their results support the idea that the oral mucosa was the portal of entry for Streptococcus viridans that caused bacteremia in their patients, and they advocate the use of first-line antibiotic regimens aimed at gram-positive organisms for high-risk patients repeatedly exposed to aggressive chemotherapy. While recognizing that there are ubiquitous oral reservoirs of viridans streptococci and only selective bacterial seeding occurs, suggesting unknown determinants of organism virulence, these authors also concluded that local oral prophylaxis or cleaning could be cost-effective for the prevention of streptococcal infections.
Greenberg et al. (1982) conducted a two-phase study of the role of oral flora in septicemia among patients with acute leukemia. In the first phase, nine patients aged 24–66 with acute nonlymphocytic leukemia who were admitted to the Oncology Unit at the Hospital of the University of Pennsylvania were followed. Each had a fever of 101°F or higher for eight or more hours. Blood, stool, sputum, urine, throat, oral mucosa, gingival sulcus, and oral ulcer cultures were obtained. Following a febrile episode, the investigators categorized infections as either oral site, likely oral site, likely extraoral site, extraoral site, or unknown. Six oral infections (three pericoronitis, one periapical, one infected oral ulcer, and one endodontic-periodontic lesion) were identified. Four of these met the associated-with-septicemia criteria, which included localized oral signs and symptoms, absence of other signs and symptoms, culture of the same organism from the oral infection and from blood in moderate to heavy amounts, and absence of the organism in cultures from other body sites. Septicemic oral organisms included Klebsiella (two), Enterobacter (one), and Staphylococcus epidermidis (one).
Role of Prechemotherapy Dental Treatment in Reducing Septicemias
In Phase 2 of the Greenberg et al. (1982) study, dental screening and selected preventive intervention were undertaken prior to chemotherapy on 24 medically able patients ages 20–74. This was in contrast to Phase 1, when treatment was delayed until the onset of a febrile episode. Dental treatment was required by nine patients prior to chemotherapy: periodontal therapy only in three cases, extractions only in three cases, and periodontal therapy and extractions in three cases. These 24 patients experienced 55 febrile episodes. Six septicemias occurred, but no definitive source was identified using the previous criteria. The source for three was suspected to be periodontal or gingival, but patients had no localized symptoms in two cases (Enterococcus and Klebsiella) and gingival symptoms only in one case (Klebsiella). These three patients did not receive
prechemotherapy periodontal treatment due to the severe complications of their leukemia on admission.
Peterson et al. (1990) included some original data from a small study at the University of Maryland Cancer Center of 33 newly diagnosed patients with acute nonlymphocytic leukemia who were randomized to receive either limited or thorough mechanical oral hygiene (OH) prior to remission induction: 18 underwent limited OH and 15 underwent thorough mechanical OH (e.g., dental scaling) prior to induction chemotherapy. The limited OH group had five acute systemic infections clinically documented as periodontal in origin versus only one such infection in the thorough OH group. Each group also had four acute oral nonperiodontal infections, and seven (limited OH) and nine (thorough OH) patients had acute esophageal, pulmonary, or pharyngeal infections. This trend suggests that thorough dental scaling prior to chemotherapy would be of benefit in reducing subsequent risk of acute periodontal infection during neutropenia.
Toljanic et al. (1999) reported a prospective study of 48 consecutively entered patients with hematologic (90% leukemia) or solid malignant neoplasms (6% lymphoma) admitted for treatment at the University of Chicago Hospitals between 1993 and 1995. Prechemotherapy dental examination resulted in scoring dental lesions as mild to moderate versus severe, and acute versus chronic. Patients with acute dental pathology associated with nonsalvageable teeth (n= 3) underwent prechemotherapy dental treatment (extractions) to remove the source of infection. Patients diagnosed with chronic dental pathology only (n= 38) received no prechemotherapy dental treatment regardless of the severity of the score for this pathology. Each patient experienced at least one episode of severe neutropenia (absolute neutrophil count below 500 cells per microliter) lasting several days. Severe chronic pathology judged to be at risk of acute exacerbation under immune suppression was diagnosed in 21 patients. Of these 21 higher-dental-risk patients, 2 had intertherapy febrile episodes resulting from odontogenic sources. The authors recommend that a comprehensive exam be completed prior to chemotherapy to identify acute presentations of dental disease that require aggressive pretherapy treatment to prevent local exacerbation or systemic spread of ongoing infection. However, routine prechemotherapy treatment of chronic dental disease, especially disease of mild to moderate risk, may not be warranted.
Although the problem of infections of oral origin during hematologic malignancy, chemotherapy, or BMT-induced immune suppression is well documented and various preventive oral health and pretreatment dental protocols have been advocated (Epstein, 1990; Meurman et al., 1997; Peterson, 1990); they are based largely on clinical experience, expert opinion, and indirect evidence from small clinical or observational cohort studies, rather than large multicenter controlled clinical trials. There is limited direct evidence that eradication of dental infection prior to immunosuppressive chemotherapy improves the prognosis of patients with leukemia.
Oral Mucositis Treatment
Oral mucositis is the major toxic oral side effect of chemotherapy and bone marrow transplantation for leukemia and lymphoma. It thus has the greatest potential to interfere with medical care for these diseases. The randomized clinical trials have indicated that potentially effective treatments for reducing the severity or incidence, or at least providing palliation, of oral mucositis include the following:
-
Acyclovir (Bergmann et al., 1995)
-
Topical oral G-CSF (filgrastin) mouth rinses (Karthaus et al., 1998)
-
Propantheline (Ahmed et al., 1993)
-
Glutamine (Anderson et al., 1998)
-
Helium-neon lasers (Barasch et al., 1995; Cowen et al., 1997)
-
“Intensive oral health care” (Borowski et al., 1994)
-
Patient-controlled analgesia with morphine (Coda et al., 1997; Hill et al., 1990; Pilliteri and Clark, 1998)
-
Tretinoin topical cream (Cohen et al., 1997)
-
Chlorhexidine mouth rinse (Ferretti et al., 1988)
-
Vitamin E (Lopez et al., 1994)
-
Relaxation and imagery training (Syrjala et al., 1995) Lack of effect was found for the following approaches:
-
Chlorhexidine mouth rinse (Epstein et al., 1992; Weisdorf et al., 1989)
-
Prostaglandin E2 (PGE2) (Labar et al., 1993)
For dental and gingival conditions associated with chemotherapy for lymphoma, the following was found effective for prevention and treatment: twice-daily rinsing with an amine fluoride-stannous fluoride mouthwash (Laine et al., 1993; Meurman et al., 1991).
Ineffective procedures for dental and gingival conditions included chlorhexidine mouth rinse (Wahlin, 1989). It should be noted that the efficacy of chlorhexidine mouth rinse for gingival and dental conditions in these patients has been controversial.
CONDITION 4: ORGAN TRANSPLANTATION
Introduction
This review evaluates the evidence for expanding Medicare coverage of medically necessary dental care in solid organ transplant patients. Only a small number (470 of 20,935 total solid organ transplants in 1997) of liver, lung, heart, or pancreas transplants are provided to Medicare-eligible recipients (UNOS,
1999) (Table C-7). In 1972, the Social Security Act was amended to cover the medical costs associated with end-stage renal disease (ESRD) for eligible patients under Medicare. Currently, the vast majority of renal transplants are covered under Medicare or the Veterans Administration. Most oral complications, however, are similar across various organ transplants and are related primarily to a transplant recipient’s net state of immunosuppression and the drug therapies utilized. Current Medicare Part B coverage for dental services for beneficiaries receiving a solid organ transplant is limited to “oral or dental examination performed on an in-patient basis as part of a comprehensive work-up prior to renal transplant surgery” (Table C-2).
Solid organ transplantation has become an accepted part of standard medical therapy for irreversible failure of a variety of organs. More than 20,000 organ transplants were performed in 1998 (Table C-8), and an estimated 75,000 transplant recipients are alive today.
The waiting list (Table C-9) and waiting time to transplant continue to grow, however, and numerous individuals die each year awaiting transplant.
Despite a recent increase in the number of living donors not only for kidneys but also for other organs such as lung, liver, and pancreas, organ donor shortage is at the forefront of problems in this field. Given these factors, the importance of maximizing the potential for success of each transplant is critical. Chronic rejection and infection are the most important factors leading to transplant failure. Transplant teams strive to eliminate potential sources of infection prior to transplantation and to minimize the effects of the drug-induced chronic immunosuppression that is required for long-term graft success.
The mouth is a potential source of local and systemic infection. Medical and dental references typically cite the need for a comprehensive oral examination and elimination of potential oral sources of infection prior to transplant surgery. This section examines the evidence that the provision of oral health care, pre-and/or posttransplant, affects short- or long-term graft survival, affects patient survival, or reduces postoperative complications.
TABLE C-7 Number of Transplant Recipients Aged 65 Years and Above, United States, 1997
|
Kidney: 12,357* |
Heart: 165 |
|
Liver: 264 |
Lung: 40 |
|
Pancreas: 1 |
Heart-lung: 0 |
|
*Includes all renal transplants since most are covered under Medicare through the ESRD program. SOURCE: UNOS, 1999. |
|
TABLE C-8 Number of Transplants Performed in the United States in 1998
TABLE C-9 UNOS National Patient Waiting List for Organ Transplants (as of May 12, 1999)
|
Type of Transplant |
Registrations for Transplants |
Patients Waiting for Transplants |
|
Kidney |
43,734 |
41,833 |
|
Liver |
13,181 |
12,987 |
|
Pancreas |
453 |
442 |
|
Pancreas islet cell |
118 |
118 |
|
Kidney-pancreas |
1,915 |
1,847 |
|
Intestine |
120 |
120 |
|
Heart |
4,267 |
4,248 |
|
Heart-lung |
248 |
244 |
|
Lung |
3,299 |
3,250 |
|
Totals |
67,335 |
63,219* |
|
NOTE: UNOS policies allow patients to be listed with more than one transplant center (multiple listing); thus the number of registrations is greater than the actual number of patients. *Some patients are waiting for more than one organ, therefore the total number of patients is less than the sum of patients waiting for each organ. |
||
Methods
This material is based on evidence gathered from a MEDLINE (Ovid) search of the biomedical scientific literature from 1984 to April 1999, studies identified from reference lists in core articles obtained in the MEDLINE search, and personal communications with transplant center clinicians. Initial search inclusion criteria included randomized clinical trials, case-control studies, cross-sectional observational cohort studies, or controlled follow-up studies. Search terms included organ transplantation and oral; dentistry, dental; mouth; stomatitis; complications. Separate searches were also conducted with each type of organ transplant and the dental-related key words.
This systematic review of the literature revealed that our knowledge in this area is based primarily on case reports from individual transplant centers reporting oral complications posttransplant and indirect evidence of biological plausibility based on the potential for local and systemic infection from oral sources in immunosuppressed individuals. Numerous articles in the literature from experienced clinicians at academic research centers cite the need to provide oral health care to immunosuppressed patients and suggest protocols for their care. This review suggests that much of the relevant information is derived empirically; nevertheless, it is the standard of medical care in a large number of organ transplant centers. A well-documented adverse oral consequence related to receiving transplant therapy, gingival enlargement from the use of cyclosporine and nifedipine (and other calcium-channel blockers), is also reviewed.
Infections
A basic tenet is that all infections should be eliminated before transplantation (Fishman and Rubin, 1998). Infection is a contraindication to transplantation because the immunosuppressive therapy required postoperatively can lead to a fulminant infection. Improvements in immunosuppressive protocols have resulted in reduced graft rejection even in poorly matched donor-receptors. Unfortunately, immunosuppressive drugs also suppress host defenses against bacterial, viral, and fungal infections (Ruskin et al., 1992). Infection is a major cause of death in renal transplant patients and most often occurs in the first six months following transplant, when immunosuppressive therapy is at its peak (Naylor et al., 1988). About two-thirds of solid organ transplant recipients will experience infectious complications in the first year after transplantation. Most transplant recipients will require some level of lifelong immunosuppressive therapy, making infection a lifetime concern.
Early infections range from common cystitis in 40–50% of patients, surgical wound infection, transfusion-related infection before or during organ transplantation (especially hepatitis C transmission), dialysis-related sepsis, urinary tract infection, and aspiration pneumonia. Delayed infections most often occur due to
virus (herpes simplex [HSV], cytomegalovirus [CMV], Epstein-Barr virus [EBV]), fungus (Candida albicans), or other opportunistic organisms (Finberg and Fingeroth, 1998; Kusne and Manez, 1997; Muzyka and Glick, 1995). Since the advent of cyclosporine therapy, opportunistic infections have become less common; yet infections with Pneumocystis organisms, CMV, EBV, HSV, herpes zoster, and Cryptococcus still occur (Fischel et al., 1991; Hanto, 1998; Schweitzer et al., 1991).
Immunosuppressed organ transplant patients are more susceptible to oral infections, especially those of fungal or viral origin. The oral cavity is also a source of gram-negative enterococcal infections (Pseudomonas, Proteus, Klebsiella). Oral fungal infections have been reported to occur in 6 to 42% of liver transplant patients (Colonna et al., 1988; Kusne, 1988). Candidiasis is the most frequently implicated fungal infection, although Mucor and Aspergillus have also been reported. No evidence could be found that these intraoral fungal infections spread systemically. Additionally, medications routinely taken by transplant recipients such as immunosuppressants, antifungals, antibiotics, aminoglycosides, steroids, and narcotics may mask the signs and symptoms of oral infection.
CMV and HSV commonly infect humans, with serological evidence in 40–80% of adults (Berry et al., 1988). In the vast majority of people, these infections are asymptomatic. More than 75% of organ transplant patients are sero-positive for CMV (Rubin and Tolkoff-Rubin, 1988). CMV and HSV infections manifesting as nonspecific oral ulcers are frequently found in the first six months posttransplant. These ulcers may occur anywhere along the gastrointestinal tract, and prophylactic screening and preemptive treatment protocols are followed at most transplant centers. CMV is a major cause of graft rejection infections. The mouth is a frequent site of nonspecific ulcers that often harbor CMV, and CMV has also been isolated from areas of gingival hyperplasia. The diagnosis of CMV may be difficult to make in a transplant patient; therefore the patient should be examined regularly for this disease. In the mouth, a biopsy of a lesion can be immunohistochemically stained to confirm the presence of CMV (Epstein et al., 1993). HSV infections are also common in transplant recipients, and the mouth is a frequent site of ulcers. Oral lesions suggestive of infection should be evaluated by cytological examination, culture, and/or biopsy when indicated (MacPhail et al., 1995; Rees, 1998; Samaranayake et al., 1986).
Increased susceptibility to infections has implications for dental care because transient, usually asymptomatic, bacteremias occur from chewing, brushing, and a wide variety of dental manipulations, particularly those involving the mucous membranes (Haffajee and Socransky, 1994; Okabe et al., 1995; Strom et al., 1998; van der Meer et al., 1992). Certain bacteremias may cause serious complications in these already compromised patients. Life-threatening systemic infections with common oral pathogens such as Streptococcus viridans, Lacto-
bacillus, and Candida albicans have been reported (Antony et al., 1996; Reyna et al., 1982).
Longer-term posttransplant, more than 80% of patients have a good result from transplantation and are maintained on minimal long-term immunosuppressive therapy with good function. Their infectious disease problems are similar to those of the general community and are primarily respiratory (Fishman and Rubin, 1998).
Immunosuppression Therapy
Appropriate immune suppression is critical for long-term graft survival. Immunosuppressive therapy is usually provided by various combinations of glucocorticoids, azathioprine, cyclosporine, tacrolimus, monoclonal antibody OKT 3, or antilymphocyte globulin. Almost all renal transplant immunosuppressive regimens include cyclosporine or tacrolimus, and appropriate serum levels are essential to prevent graft rejection. Higher serum levels are associated with more severe adverse side effects. Serum levels can be increased unintentionally by simultaneous intake of various drugs; thus, the prescription of any drug for patients receiving immunosuppressive drugs should be preceded by medical consultation (McCauley, 1997; Naylor and Fredericks, 1996).
Cyclosporine is an excellent immunosuppressant drug that is often prescribed following organ transplantation because it selectively suppresses cell-mediated immunity. Cyclosporine appears to block the formation and release of interleukin-2 and thus prevents the amplification of the T-cell response to a foreign body. Unlike most other immunosuppressants, it does not interfere with bone marrow function. It is most often used in combination with low doses of glucocorticoids, usually prednisone, and/or azathioprine.
Complications of the drug include nephrotoxicity, renal vasculopathy, hypertension, chronic renal interstitial fibrosis (which is also common in heart transplantation), neurotoxicity, gingival overgrowth, and increased susceptibility to malignancies, including B-cell lymphoma; squamous cell carcinoma of the skin, lip, or oral mucosa; or Kaposi’s sarcoma. Malignancy may be transmitted from the donor or develop de novo after transplantation (Gruber et al., 1994; Jonas et al., 1997; Lipkowitz and Madden, 1994; Sheil et al., 1993); oral malignancies have been reported within sites of cyclosporine-induced gingival overgrowth (Rees, 1998; Varga et al., 1998). Cyclosporine-induced perioral dermatitis has been described, characterized by red papules, pustules, and scaling of the chin, upper lip, and nasolabial fold (Cohen, 1994).
Oral hairy leukoplakia may occur in HIV-negative individuals taking cyclosporine, and gingival overgrowth is a well-recognized occurrence. An incidence of about 30% or more has been observed in several studies (Seymour et al., 1997). Newer immunosuppressant drugs such as tacrolimus, sirolimus, and mycophenalate mofetil are now available as cyclosporine substitutes when appro-
priate. These agents appear to induce fewer side effects, and no gingival overgrowth has been reported to date.
Pre-Transplant Oral Considerations
Although liver, heart, lung, or pancreas transplant patients will present with their own unique and complex medical problems that may have other oral manifestations, their oral concerns relative to the immunosuppressive and transplant therapies will be quite similar to renal transplant recipients. Pre- and posttransplant screening, diagnosis, treatment, counseling, and follow-up considerations are similar. This discussion of the oral manifestations of renal transplant patients and considerations for the pre- and posttransplant care of this group will serve to illustrate the available evidence for the medical necessity of providing such care across all transplantation organ groups.
Most renal transplant candidates will be in some stage of renal failure that will present unique oral problems requiring the dental provider’s careful attention and special considerations. An increase in salivary calculus has been described. Conversely, caries incidence is reduced, possibly from plaque inhibition related to increased levels of salivary urea (DeRossi and Glick, 1996). Uremic stomatitis appears as dry, burning, painful oral tissues covered by a gray exudate or by mucosal ulcerations. Xerostomia may be common and may be accompanied by parotid enlargement or parotid infection. Enamel hypoplasia and discoloration of the teeth may be present in children along with pulpal narrowing. Candidal overgrowth may be common, and bacterial and viral infections may occur. Secondary hypoparaythyroidism may lead to bony changes, including loss of density, loose teeth, jaw enlargement, and pain. Spontaneous gingival hemorrhage, ulcerations, and petechial lesions are common (Cohen, 1994; DeRossi and Glick, 1996; Ferguson and Whyman, 1998; Rose and Kaye, 1990; Ziccardi et al., 1992) as is periodontal inflammation.
One recent study found that 100% of 45 renal dialysis patients had periodontal disease (Naugle et al., 1998). This is not surprising, given that national adult oral health data indicating that about 85% of all adults have some form of periodontal disease, with 7–13% having more severe forms (NHANES III, 1996). In addition, recent analysis of data from the Third National Health and Nutrition Examination Survey (NHANES III) indicates that about 30% of adults in all age groups have at least one untreated carious lesion (CDC, unpublished data). Even though oral health and disease have not been documented in a systematized manner in this particular patient population, there is no reason to suggest that this group would have better-than-average oral health. On the contrary, surveys of other medically compromised patient groups suggest that these individuals suffer poor oral health (Maier et al., 1993). Additionally, diabetes was the primary diagnosis among 44% of new renal transplant recipients in 1998. Diabetic patients have been demonstrated to have a higher prevalence of more
severe periodontal disease (Genco and Löe, 1993; Löe, 1993; Oliver and Tervonen, 1994).
In many transplant centers, an individual is not cleared for transplantation if oral infection exists. This may result in a potential recipient losing an opportunity if an appropriately matched organ becomes available during a period of serious dental infection and an increased wait time, causing increased risk of morbidity and mortality (Naugle et al., 1998). Cadaver kidneys must be transplanted within about 48 hours from the time they are removed from the donor. Liver, heart, and lungs are viable for only a matter of hours. However, although it has been long surmised that any active oral disease such as periodontal disease or active periapical lesions may compromise the success of a transplant, specific evidence of this fact is lacking.
What Type of Dental Services Could Be Considered Medically Necessary?
Numerous authors have asserted that the dentist should participate in treatment planning and provide necessary pretreatment for transplant patients. Also, under ideal circumstances, all potential oral foci of infection should be eliminated prior to transplant placement (Cohen, 1994; Kusne and Manez, 1997; Naylor et al., 1988; Rees 1998; Rose and Kaye, 1990). A basic tenet of transplant therapy is to prevent infection, and dental screening tests should identify likely sources of oral infection. Because many areas of oral pathology are intra-bony and not readily apparent from the visual or tactile basic clinical dental examination, a radiographic survey is an important part of a pretransplant screening. A full mouth series of periapical and bitewing x-rays and a panoramic x-ray will typically provide a complete view of potential dental disease. Supplemental films can be ordered as required.
Early Detection of Dental Problems
Does early detection of potential dental problems improve the long-term outcome of the organ transplant? Does early detection improve the likelihood of a favorable outcome compared to waiting to see if a problem develops?
Direct evidence is not available to answer these questions. Indirect evidence, however, suggests that eliminating potential dental infections will prevent transplant delay for some individuals and posttransplant infections in others. Identification and treatment of severe dental problems prior to transplantation should decrease the chance of an untoward infection during the postoperative period of most intense immunosuppression. Peritransplant prophylactic antibacterial, antifungal, and antiviral strategies developed for nonoral infections are likely to control potential oral infections as well. No descriptive studies of overall dental disease status in transplant patients were found. Given
the relatively high dental disease rates among U.S. adults, however, the probability of oral infections occurring in the population of transplant recipients is high.
Posttransplant Considerations
Patients remain at some level of immunosuppression for the rest of their lives and will be at higher risk of infection. Dentists need to be cognizant of this and be vigilant for signs of dental infection. A renal patient’s dental problems can compromise his or her general health in more ways than just loss of function, esthetics, and comfort. However, no evidence could be found for levels of dental disease higher than in the normal population or for effects of dental disease on the potential for chronic graft rejection, the most common cause of graft failure.
About 30% of dentate renal transplant patients medicated with cyclosporine alone experience significant gingival overgrowth that requires surgical excision (Thomason et al., 1994). This figure increases to 40% when patients are medicated with both cyclosporine and nifedipine. Gingival hyperplasia may preclude one from eating and maintaining proper nutrition (Svirsky and Saravia, 1989). Several studies have shown that the development and severity of gingival overgrowth is related to the levels of oral hygiene and gingival inflammation, although these results are not always consistent (King et al., 1993; Thomason et al., 1993). The development of gingival hyperplasia is also frequent in those with pretransplant periodontitis or hyperplasia (Varga et al., 1998). Nephrotoxicity and neurotoxicity may be more severe in patients immunosuppressed with tacrolimus, although gingival enlargement has not been identified in association with this drug (Adams and Famili, 1991).
The true incidence of cyclosporine-induced gingival enlargement is difficult to determine since the drug is often used for organ transplant patients in combination with antihypertensive drugs such as the calcium channel blocking agent nifedipine, which is also associated with gingival overgrowth (Thomason et al., 1996, Wilson et al., 1998). Studies have indicated that both the incidence and the severity of gingival overgrowth are increased when patients are medicated with both cyclosporine and nifedipine (Thomason et al., 1993). Recent reports indicate that nifedipine-induced gingival overgrowth can be reversed by using alternative calcium channel blocking drugs such as amlodipine or isradipine (Jorgensen, 1997; Westbrook et al., 1997). Other calcium channel blockers, however, may induce increased plasma levels of cyclosporine, while nifedipine does not. This may explain the frequent use of nifedipine in postrenal transplant patients (Sakurai et al., 1995).
Treatment for drug-induced gingival overgrowth includes establishment of effective oral hygiene and discontinuance or reduction in dosage of the causative drug when possible. The pathogenesis of this untoward effect is uncertain, and
the expression of gingival overgrowth and various periodontal and pharmacological variables remains a contentious issue. Clinical measures to prevent the occurrence of either cyclosporine- or nifedipine-induced gingival overgrowth are not reliable.
Cyclosporine-induced gingival overgrowth may affect all parts of the gingiva, but it has been suggested that the gingival changes are more pronounced in the anterior regions (Bartold, 1987; Rateitschak-Pluss et al., 1983; Wondimu et al., 1993). Surgical removal of enlarged gingiva is often necessary to facilitate patient function, oral hygiene measures, and aesthetics. It has been estimated that about 50% of individuals who develop gingival hyperplasia will require surgery.
Other Oral Lesions in Transplant Recipients
Only two studies were found that examined the prevalence of oral lesions in transplant recipients (King et al., 1994; Thomason et al., 1997). One study examined 159 renal transplant recipients and 160 matched controls. In this population, the prevalence of hairy leukoplakia (HL) and leukoplakia was 11.3 and 10.7%, respectively, compared with 0 and 5% in the controls. In HIV-infected individuals, HL is regarded as a marker for progression to AIDS (Katz et al., 1992). Hairy leukoplakia is thought to be caused by the EBV, but the clinical significance of HL in transplant patients has not been determined. In organ transplant patients, it may be regarded as an indication of severe immunosuppression. It remains to be seen whether the occurrence of HL is related to graft survival (Seymour et al., 1997). In this same study, oral candidiasis was observed in 9.4% of renal transplant recipients compared with 2.5% of controls; 3.8% of renal transplant recipients exhibited erythematous candidiasis, but this was not seen in the controls. The candidal infections and HL also have a well-established association with the immune suppression that accompanies HIV infection. In this study, the prevalence of oral lesions was 54.7% in renal transplant recipients and 19.4% in controls (King et al., 1994). Oral malignancies, particularly skin and lip cancers and Kaposi’s sarcoma (Jacobs et al., 1981), have been found with higher prevalence in immunosuppressed organ transplant patients.
Summary
Fewer than 15,000 organ transplants performed in the United States in 1997 were among Medicare beneficiaries. Most of these were kidney transplant patients covered under the ESRD provision of the Social Security Act.
Currently, only a pretransplant dental screening performed on an inpatient basis is allowed under Medicare Part B. Transplant recipients are highly motivated to maintain their recovered health status and are generally compliant with pharmacotherapy and medical follow-up. In addition to routine blood tests and
monitoring of immunosuppressive drug levels, recipients require immunization updates, screening for malignancy, hypertension, hyperlipidemia, and ophthalmological and dental complications. Little information is available about the consistent implementation of any of these health maintenance strategies, but dental care is desired by transplant patients and recommended by most medical authorities. In one small survey of 60 liver transplant patients, 75% sought annual dental examination (Zeldin et al., 1998). This number is slightly higher than the 62% of the U.S. population that typically seeks dental care annually. A study of 160 renal transplant recipients in London also showed slightly more transplant patients visiting a dentist annually than a matched control group (57.9% to 51.3%); 45.6% visited a hospital dental facility versus 7% of controls (King and Thornhill, 1996).
The major question is whether dental care provided pre- and/or posttransplant improves the outcome of medical transplant care. No controlled clinical studies have examined morbidity and mortality in transplant recipients relative to the provision of oral health care pre- or posttransplant. Nor have there been studies that demonstrate improved quality of life or less frequent complications. Anecdotal and some case reports indicate that oral infections can delay transplantation or severely complicate the postoperative course. Although most oral medicine textbooks and reviews advise that restoration to good oral health is a prerequisite for any patient who is immunosuppressed or about to undergo immunosuppressive therapy such as organ transplantation, this advice is primarily a result of tradition and collective medical experience rather than rigorous study. In addition, this broad category of patients represents a tremendous diversity of medical complication. It is difficult even within one organ category to standardize what a “typical” patient would be and to limit necessary care to only a particular segment of that population. There is great variation in the characteristics of patients, coexisting conditions, and other such factors. Given the enormous number of procedures and the individual circumstances of patients, limiting insurance coverage to a host of separately validated and specifically described procedures is impractical.
There are two cardinal therapeutic rules to be followed by clinicians in dealing with infections in transplant patients: (1) prevention is better than treatment; and (2) when treatment is required, the major determinant of the success of therapy is the rapidity with which the diagnosis is made and effective therapy is initiated. Oral disease is present and is a potential source of active infection in these medically compromised individuals. Although limited studies have been conducted on the oral health status of these individuals, some do suggest a high rate of periodontal infection and dental decay.
Dental management is complicated because of the oral disease and medical problems seen in this population. These patients survive under narrowly controlled conditions of intake and activity as well as under great physiological and psychological stress, with medications, diet, intensive treatments, limited life-
style, and dependence on others. Dental treatment, even minor procedures, can present major problems for the clinician. Because of transplant patients’ immunosuppressed condition, additional precautions are often necessary, including hospitalization, which can add significantly to the costs of care. Most medically controlled renal failure and transplant patients, however, can be safely and adequately treated in the private dental office.
The importance of pretransplantation workup and continued follow-up posttransplantation to eliminate any oral source of infection is emphasized. Hyperplasia from cyclosporine and/or nifedipine can be minimized with excellent oral hygiene. Persistent candidiasis and opportunistic infections also occur in patients that are immunosuppressed. Marked advances in immunosuppressive therapies, improved medical and surgical techniques, increased numbers of candidate patients, particularly in the pediatric population, and greater insurance recognition will mean that dentists will have an increasingly greater role in the management of organ transplant patients.
Although direct evidence of benefit from clinical trials is not available, this has been a neglected area of clinical research, and practices have been governed by experience. Dental examination and elimination of sources of oral infection appear to be the de facto standard of care at most transplant centers, and extending Medicare coverage to these individuals would be consistent with the current standard.
CONDITION 5: HEART VALVE REPAIR OR REPLACEMENT
Introduction
Valvular heart disease refers to one of several abnormalities of heart valve thickness and movement responsible for stenosis (pathological narrowing of the orifice of the valve) and regurgitation (backward flow of blood through the valve). Abnormalities may include mitral or aortic valve stenosis or regurgitation, tricuspid and pulmonary valve diseases, and congenital abnormalities. Treatment of valvular heart disease may involve medications or surgical repair or replacement. Surgical repair or replacement of a heart valve increases a person’s likelihood of endocarditis, an inflammation of the endocardium. Endocarditis may be acute (usually caused by pyogenic organisms such as hemolytic streptococci or staphylococci) or subacute (usually caused by Streptococcus viridans or S. faecalis). Surgical repair or replacement with a prosthetic heart valve creates opportunities for bacteria to adhere to the valve and/or endocardium. The bacteria form vegetations that may enter the bloodstream and spread the infection to other parts of the body. Treatment of such infections requires long-term antibiotic therapy (four to six weeks) and may require valve replacement. Oral flora, particularly streptococcus, are implicated in approximately 40 percent of infective endocarditis cases (Roberts, 1999; Strom et al, 1998; van der Meer et al, 1992).
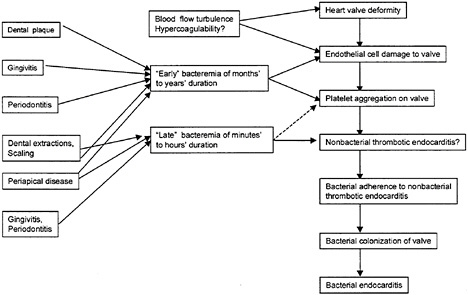
FIGURE C-7 Proposed causal model of dental-associated endocarditis. SOURCE: Drangsholt, 1998.
This review focuses specifically on medically necessary oral health care that is provided prior to surgical repair or replacement. Antibiotic prophylaxis prior to dental care for at-risk persons—with either valvular heart disease or a prosthetic heart valve—is not considered here.
One suggested model for the association between oral diseases and endocarditis is shown in Figure C-7 (Drangsholt, 1998). Dental plaque (accumulation of mainly oral microorganisms and their products that adheres to the teeth), gingivitis (inflammation of the gingiva as a response to bacterial plaque), periodontitis (inflammation of the periodontium or the supporting structures of the teeth), and certain dental procedures, such as scaling and root planing and dental extractions, may result in early bacteremias of months or years duration. In the presence of heart valve deformity or endothelial cell damage to the valve, platelets may adhere to the valve and result in nonbacterial thrombotic endocarditis (NBTE). Bacteria may adhere to the NBTE, colonize, and result in acute or subacute endocarditis, depending on the organism. Gingivitis, periodontitis, certain dental procedures, and periapical diseases (infections around the apex of the root of a tooth) may result in late bacteremias of minutes to hours duration and follow a similar cascade of events.
TABLE C-10 Medicare DRGs Associated with Valvular Heart Procedures and Complications
|
DRG |
Description |
|
104 |
Cardiac valve procedures with cardiac catheterization |
|
105 |
Cardiac valve procedures without cardiac catheterization |
|
126 |
Acute and subacute endocarditis |
|
135 |
Cardiac congenital and valvular disorders age >17 with cardiac catheterization |
|
136 |
Cardiac congenital and valvular disorders age >17 without cardiac catheterization |
|
137 |
Cardiac congenital and valvular disorders age 0–17 |
|
SOURCE: Health Care Financing Administration, Medicare Provider Analysis and Review file: www.hcfa.gov/stats/medpar.htm (last updated December 15, 1998). |
|
Medicare Utilization and Reimbursement of Valvular Heart Disease
Estimates of the number of discharges and Medicare reimbursements for valvular heart diseases were obtained from the Health Care Financing Administration Medicare Provider Analysis and Review (MEDPAR) file (http://www.hcfa.gov/stats/medpar.htm). Six diagnosis-related groups (DRGs) were included and are shown in Table C-10.
The number of discharges for valvular heart diseases among Medicare beneficiaries is increasing. Between 1990 and 1995, the number of discharges increased from about 42,700 to 58,800 (Figure C-8). Of these, acute and subacute endocarditis accounted for about 3,900 in 1990 and 4,950 in 1995.
Total inpatient days for valvular heart procedures between 1990 and 1995 are shown in Figure C-9. For all DRGs, the total number of inpatient days declined over the six-year period. Acute and subacute endocarditis declined from about 14% of inpatient days to about 10% of inpatient days during the period.
Medicare reimbursement for valvular heart disease procedures increased over the six-year period (Figure C-10). In 1990, Medicare reimbursed about $1.05 billion for these six DRGs. By 1995, this amount had increased to about $1.61 billion. Reimbursements for acute and subacute endocarditis represented between 4 and 5% of the total reimbursement.
Methods
This review is based on a literature search of the MEDLINE database from 1980 through March 1999. Search terms included dentistry, dental care, endocarditis, and heart valve diseases. Studies identified as a randomized clinical trial, a case-control study, a cross-sectional observational cohort study, or a controlled follow-up study were included in the review. Case reports and smaller
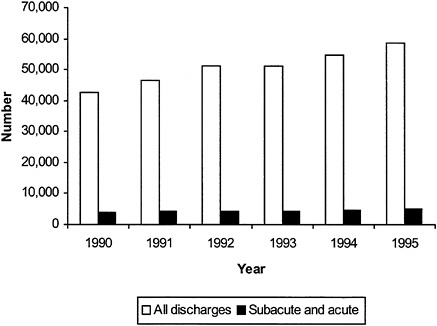
FIGURE C-8 Number of Medicare discharges for valvular heart repair or replacement, 1990–1995. SOURCE: Health Care Financing Administration, Medicare Provider Analysis and Review file: www.hcfa.gov/stats/medpar.htm (last updated December 15, 1998).
case series (less than 50 cases) were excluded from further review. Only studies involving patients over 18 years of age were accepted. Studies reporting on the risk of bacterial endocarditis associated with dental care and the need for antibiotic premedication were excluded.
Only studies that assessed risk reduction associated with elimination of dental disease and potential oral sources of infection were included, since this analysis focuses on dental disease, rather than its treatment, as a risk factor for endocarditis.
Results
No studies were identified that met the inclusion criteria addressing the efficacy or effectiveness of medically necessary oral health care in reducing pre-, peri-, or postoperative valvular repair or replacement complications.
One study (Terezhalmy et al., 1998) reported the findings of a comprehensive clinical and radiographic regional examination on 156 consecutive patients with valvular heart disease requiring mechanical or bioprosthetic valve implan-tation in 1993 at the Cleveland Clinic Foundation. These patients were referred by the Department of Thoracic and Cardiovascular Surgery to the Section on Oral Medicine, Department of Dentistry. About 38% were women, and the mean age was 62.8 years (median 66 years, range 26 to 87 years).
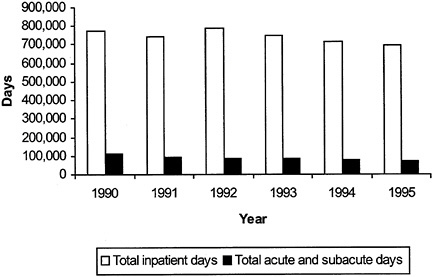
FIGURE C-9 Total inpatient days for all admissions, and acute and subacute days, among Medicare beneficiaries, 1990–1995. SOURCE: Health Care Financing Administration, Medicare Provider Analysis and Review file: www.hcfa.gov/stats/medpar.htm (last updated December 15, 1998).
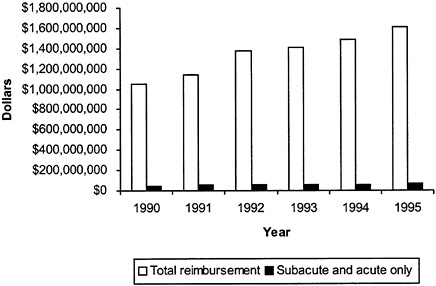
FIGURE C-10 Medicare reimbursement for valvular heart disease. SOURCE: Health Care Financing Administration, Medicare Provider Analysis and Review file: www.hcfa.gov/stats/medpar.htm (last updated December 15, 1998).
TABLE C-11 Selected Clinical and Radiographic Findings Among 156 Patients Undergoing Mechanical or Bioprosthetic Valve Implantation, 1993
|
Clinical Variable |
No. or % |
|
Mean number of teeth |
19.3 |
|
Mean number of decayed teeth |
1.1 |
|
Mean number of decayed tooth surfaces |
2.5 |
|
Percentage of patients with at least one periapical abscess associated with a decayed or restored tooth |
15.4% |
|
Percentage of patients with evidence of past root canal treatment |
30.8% |
|
Percentage distribution of patients by level of periodontal disease |
|
|
Type I: Gingivitis |
4.5% |
|
Inflammation of the gingiva characterized clinically by changes in color, gingival form, position, surface appearance, and presence of bleeding and/or exudate) |
|
|
Type II: Early periodontitis |
50.0% |
|
Progression of the gingival inflammation into the deeper periodontal structures and alveolar bone crest, with slight bone loss. The usual periodontal probing depth is 3–4 mm with slight loss of connective tissue attachment and slight loss of alveolar bone |
|
|
Type III: Moderate periodontitis |
26.9% |
|
A more advanced stage of the above condition, with increased destruction of periodontal structures with noticeable loss of bone support possibly accompanied by an increase in tooth mobility. There may be furcation involvement in multirooted teeth |
|
|
Type IV: Advanced periodontitis |
16.7% |
|
Further progression of periodontitis with major loss of alveolar bone support usually accompanied by increased tooth mobility. Furcation involvement in multirooted teeth is likely |
|
Selected oral health findings from this study are shown in Table C-11. No comparison group was identified, so one cannot determine whether the disease burden in this group is higher than in other groups. The extent of medically necessary oral health care provided to these patients prior to surgery and subsequent outcomes were not reported.
ACKNOWLEDGMENTS
In response to questions raised at the Committee’s public workshop on Medically Necessary Dental Care (May 19–20, 1999, see also Appendix A), Dr. James Lipton and Dr. Jane Atkinson of the National Institute for Dental and Craniofacial Research contacted a group of experts throughout the country to get information about the accepted dental procedures and associated costs for patients with lymphoma, leukemia, and head and neck cancer. The responses were very helpful in developing this background information and the Medicare cost
estimates. In addition to Drs. Lipton and Atkinson, the assistance of the following individuals is gratefully acknowledged: Mark Schubert, D.D.S., M.S.D., Fred Hutchinson Cancer Research Center and University of Washington School of Dentistry; Douglas E.Peterson, D.M.D., Ph.D., School of Dental Medicine, University of Connecticut Health Center; Peter B.Lockhart, D.D.S., Department of Oral Medicine, Carolinas Medical Center; J.B.Epstein, D.M.D., M.S.D, Department of Dentistry, British Columbia Cancer Agency; Stephen Sonis, D.M.D., D.M.S., Brigham and Women’s Hospital and Department of Oral Medicine and Diagnostic Sciences, Harvard School of Dental Medicine; Sook-Bin Woo, D.M.D., D.M.S., Division of Dentistry, Brigham and Women’s Hospital; Spencer Redding, D.D.S., University of Texas Health Sciences, San Antonio; Bruce Barker, D.D.S., Department of Oral Pathology, University of Missouri Kansas City; Gerry Barker, R.D.H., M.Sc., Dental Oncology Support Services, Univiversity of Missouri Kansas City.
REFERENCES
Overview
Bloom B, Gift HC, Jack SS. Dental Services and Oral Health: United States 1989. National Center for Health Statistics. Vital Health Statistics 1992; 10(183).
Consensus Conference on Medically Necessary Oral Health Care. Final Recommendations. National Alliance for Oral Health. Special Care in Dentistry 1995; 15(5):201–202.
Eddy DM, Hasselblad V, Shachter R. Meta-Analysis by the Confidence Profile Method: The Statistical Synthesis of Evidence. San Diego: Academic Press, 1992.
Fleming TR, DeMets DL. Surrogate end points in clinical trials: Are we being misled? Annals of Internal Medicine 1996; 125:605–613.
Marcus SE, Drury TF, Brown LJ, Zion GR. Tooth retention and tooth loss in the permanent dentition of adults: United States, 1988–1991. Journal of Dental Research 1996; 75(Special Issue):684–695.
Morbidity and Mortality Weekly Report (MMWR). Total tooth loss among persons aged greater than or equal to 65 years—selected states, 1995–1997. MMWR 1999; 48(10):206–210.
National Center for Health Statistics (NCHS). Vital and Health Statistics. Series 11, Number 27. Loss of Teeth in Adults, United States—1960–1962. DHEW Publication Number (HRA) 74–1280. August 1973.
National Center for Health Statistics (NCHS). Vital and Health Statistics. Series 11, Number 223. Decayed, Missing, and Filled Teeth Among Persons 1–74 Years, United States. DHHS Publication Number (PHS) 81–1673. August 1981.
National Institute for Dental Research (NIDR). The National Survey of Oral Health in U.S. Employed Adults and Seniors: 1985–86. NIH Publication Number 87–2868. Bethesda, MD. August 1987.
Head and Neck Cancer
Al-Joburi W, Clark DC, Fisher R. A comparison of the effectiveness of two systems for the prevention of radiation caries. Clinical Preventive Dentistry 1991; 13:15–19.
Allison PJ, Locker D, Feine JS. The relationship between dental status and health-related quality of life in upper aerodigestive tract cancer patients. Oral Oncology 1999; 35:138–143.
Bedwinek JM, Shukovsky LJ, Fletcher GH, Daley TE. Osteoradionecrosis in patients treated with definitive radiotherapy for squamous cell carcinomas of the oral cavity and naso- and oropharynx. Radiology 1976; 119:665–667.
Beumer III J, Silverman Jr S, Benak SB. Hard and soft tissue necroses following radiation therapy for oral cancer. Journal of Prosthetic Dentistry 1972; 27:640–644.
Beumer III J, Curtis T, Harrison RE. Radiation therapy of the oral cavity: Sequelae and management, part 1. Head and Neck Surgery 1979a; 1:301–312.
Beumer III J, Curtis T, Harrison RE. Radiation therapy of the oral cavity: Sequelae and management, part 2. Head and Neck Surgery 1979b; 1:392–408.
Beumer J, Harrison R, Sanders B, Kurrasch M. Osteoradionecrosis: Predisposing factors and outcomes of therapy. Head and Neck Surgery 1984; 6:819–827.
Brown RS, Miller JH, Bottonley WK. A retrospective oral/dental evaluation of 92 head and neck oncology patients, before, during and after irradiation therapy. Gerodontology 1990; 9:35–39.
Bruins HH, Koole R, Jolly DE. Pretherapy dental decisions in patients with head and neck cancer. A proposed model for dental decision support. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 1998; 86:256–267.
Bundgaard T, Tandrup O, Elbrond O. A functional evaluation of patients treated for oral cancer. A prospective study. International Journal of Oral and Maxillofacial Surgery 1993; 22:28–34.
Clayman L. Management of dental extractions in irradiated jaws: A protocol without hyperbaric oxygen therapy. Journal of Oral and Maxillofacial Surgery 1997; 55:275–281.
Coffin F. The incidence and management of osteoradionecrosis of the jaws following head and neck radiotherapy. British Journal of Radiology 1983; 56:851–857.
Curi MM, Dib LL. Osteoradionecrosis of the jaws: A retrospective study of the background factors and treatment in 104 cases. Journal of Oral and Maxillofacial Surgery 1997; 55:540–544.
De Graeff A, de Leeuw JRJ, Ros WJG, Hordijk GJ, Blijham GH, Winnubst JAM. A prospective study on quality of life of patients with cancer of the oral cavity or oropharynx treated with surgery with or without radiotherapy. Oral Oncology 1999; 35:27–32.
Dreizen S. Description and incidence of oral complications. U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health. Consensus Development Conference on Oral Complications of Cancer Therapies: Diagnosis, Prevention, and Treatment. National Cancer Institute Monographs 1990; 9:11–15.
Dreizen S, Brown LR, Daly TE, Drane JB. Prevention of xerostomia-induced dental caries in irradiated cancer patients. Journal of Dental Research 1977; 56:99–104.
Epstein JB, Emerton S, Kolbinson DA, Le ND, Phillips N, Stevenson-Moore P, Osoba D. Quality of life and oral function following radiotherapy for head and neck cancer. Head and Neck 1999; 21:1–11.
Epstein JB, van der Meij EH, Emerton SM, Le ND, Stevenson-Moore P. Compliance with fluoride gel use in irradiated patients. Special Care in Dentistry 1995; 15:218–222.
Epstein JB, van der Meij EH, Lunn R, Stevenson-Moore P. Effects of compliance with fluoride gel application on caries and caries risk in patients after radiation therapy for head and neck cancer. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 1996; 82:268–275.
Epstein JB, van der Meij EH, McKenzie M, Wong F, Lepawsky M, Stevenson-Moore P. Postradiation osteonecrosis of the mandible. A long-term follow-up study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 1997; 83:657–662.
Epstein JB, Wong FLW, Stevenson-Moore P. Osteoradionecrosis: Clinical experience and a proposal for classification. Journal of Oral and Maxillofacial Surgery 1987; 45:104–110.
Funegard U, Franzen L, Ericson T, Henriksson R. Parotid saliva composition during and after irradiation of head and neck cancer. Oral Oncology, European Journal of Cancer 1994; 30B:230–233.
Grant BP, Fletcher GH. Analysis of complications following megavoltage therapy for squamous cell carcinomas of the tonsillar area. American Journal of Roentgenology 1966; 96:28–36.
Health Care Financing Administration (HCFA). Medicare Carrier’s Manual, Part B. Coverage and Limitations, Section 2136: Dental Services.
Horiot JC, Bone MC, Ibrahim E, Castro JR. Systemic dental management in head and neck irradiation. International Journal of Radiation Oncology, Biology and Physics 1981; 7:1025–1029.
Horiot JC, Schraub S, Bone MC, Bain Y, Ramadier J, Chaplain G, Nabid N, Thevenot B, Bransfield D. Dental preservation in patients irradiated for head and neck tumors: A 10-year experience with topical fluoride and a randomized trial between two fluoridation methods. Radiotherapy and Oncology 1983; 1:77–82.
Jansma J, Vissink A, Spijkervet FK, Roodenburg JL, Panders AK, Vermey A, Szabo BG, Gravenmade EJ. Protocol for the prevention and treatment of oral sequelae resulting from head and neck radiation therapy. Cancer 1992; 70:2172–2180.
Keys HM, McCasland JP. Techniques and results of a comprehensive dental care program in head and neck cancer patients. International Journal of Radiation Oncology, Biology and Physics 1976; 1:859–865.
Kluth EV, Jain PR, Stuchell RN, Frich JC Jr. A study of factors contributing to the development of Osteoradionecrosis of the jaws. Journal of Prosthetic Dentistry 1988; 59:194–201.
Kumar HS, Bihani V, Kumar V, Chaundhary RK, Kumar L, Punia DP. Osteoradionecrosis of mandible in patients treated with definitive radiotherapy for carcinomas of oral cavity and oropharynx. A retrospective study. Indian Journal of Dental Research 1992; 3:47–50.
Lambert PM, Intriere N, Eichstaedt R. Management of dental extractions in irradiated jaws: A protocol with hyperbaric oxygen therapy. Journal of Oral and Maxillofacial Surgery 1997; 55:268–274.
Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1999. CA—A Cancer Journal for Clinicians 1999; 49:8–31.
Liu RP, Fleming TJ, Toth BB, Keene HJ. Salivary flow rates in patients with head and neck cancer 0.5 to 25 years after radiotherapy. Oral Surgery, Oral Medicine and Oral Pathology 1990; 70:724–729.
Lockhart PB, Clark J. Pretherapy dental status of patients with malignant conditions of the head and neck. Oral Surgery, Oral Medicine and Oral Pathology 1994; 77:236–241.
Maier H, Zoller J, Hermann A, Kreiss M, Heller W-D. Dental status and oral hygiene in patients with head and neck cancer. Otolaryngology, Head and Neck Surgery 1993; 108:655–661.
Makkonen TA, Kiminki A, Makkonen TK, Nordman E. Dental extractions in relation to radiation therapy of 224 patients. International Journal of Oral and Maxillofacial Surgery 1987; 16:56–64.
Manciani RD, Ownby HE. Osteoradionecrosis of the jaws. Journal of Oral and Maxillofacial Surgery. 1986; 44:218–223.
Manciani RD, Plezia RA. Osteoradionecrosis of the mandible. Journal of Oral Surgery 1974; 32:435–440.
Markitziu A, Zafiropoulos G, Tsalikis L, Cohen L. Gingival health and salivary function in head and neck-irradiated patients. A five-year follow-up. Oral Surgery, Oral Medicine and Oral Pathology 1992; 73:427–433.
Marx RE, Johnson RP, Kline SN. Prevention of osteoradionecrosis: A randomized prospective clinical trial of hyperbaric oxygen versus penicillin. Journal of the American Dental Association 1985; 111:49–54.
Maxymiw WG, Wood RE, Liu F-F. Postradiation dental extractions without hyperbaric oxygen. Oral Surgery, Oral Medicine and Oral Pathology 1991; 72:270–274.
Murray CG, Herson J, Daly TE, Zimmerman S. Radiation necrosis of the mandible: A 10-year study. Part I. Factors influencing the onset of necrosis. International Journal of Radiation Oncology, Biology and Physics 1980a; 6:543–548.
Murray CG, Herson J, Daly TE, Zimmerman S. Radiation necrosis of the mandible: A 10-year study. Part II. Dental factors; onset, duration and management of necrosis. International Journal of Radiation Oncology, Biology and Physics 1980b; 6:549–553.
Myers RAM, Marx RE. Use of hyperbaric oxygen in postradiation head and neck surgery. U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health. Consensus Development Conference on Oral Complications of Cancer Therapies: Diagnosis, Prevention, and Treatment. National Cancer Institute Monographs 1990; 9:151–157.
National Institutes of Health (NIH). National Institutes of Health Consensus Development Conference Statement: Oral complications of cancer therapies: Diagnosis, prevention, and treatment. Journal of the American Dental Association 1989; 119:179–183.
Niewald M, Barbie O, Schnabel K, Engel M, Schedler M, Nieder C, Berberich W. Risk factors and dose-effect relationship for osteoradionecrosis after hyperfractionated
and conventionally fractionated radiotherapy for oral cancer. British Journal of Radiology 1996; 69:847–851.
Pochanugool L, Manomaiudom W, Im-Erbsin T, Suwannuraks M, Kraiphibul P. Dental management in irradiated head and neck cancers. Journal of the Medical Association of Thailand 1994; 77:261–265.
Rahn AO, Drone JB. Dental aspects of the problems, care, and treatment of the irradiated oral cancer patient. Journal of the American Dental Association 1967; 74:957–966.
Rankow RM, Weissman B. Osteoradionecrosis of the mandible. Annals of Otology 1971; 80:603–611.
Ries LAG, Kosary CL, Hankey BF, Miller BA, Edwards BK (eds). SEER Cancer Statistics Review, 1973–1996. Bethesda, MD: National Cancer Institute, 1999.
Roos DE, Dische S, Saunders MI. The dental problems of patients with head and neck cancer treated with CHART. Oral Oncology, European Journal of Cancer 1996; 32B:176–181.
Schweiger JW. Oral complications following radiation therapy: A five-year retrospective report. Journal of Prosthetic Dentistry 1987; 58:78–82.
Shah JP, Karnell LH, Hoffman HT, Ariyan S, Brown GS, Fee WE, Glass AG, Goepfert H, Ossoff RH, Fremgen A. Patterns of care for cancer of the larynx in the United States. Archives of Otolaryngology—Head & Neck Surgery 1997; 123:475–483.
Shaha AR, Strong EW. Cancer of the head and neck. Pp. 355–377 in Murphy GP, Lawrence W Jr, Lenhard RE Jr. (eds). American Cancer Society Textbook of Clinical Oncology, 2nd ed. Atlanta: American Cancer Society, 1995.
Sonis ST, Woods PD, White BA. Pretreatment oral assessment. U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health. Consensus Development Conference on Oral Complications of Cancer Therapies: Diagnosis, Prevention, and Treatment. National Cancer Institute Monographs 1990; 9:29–32.
Spaulding MB, Fischer SG, Wolf GT. Tumor response, toxicity, and survival after neoadjuvant organ-preserving chemotherapy for advanced laryngeal carcinoma. The Department of Veterans Affairs Cooperative Laryngeal Cancer Study Group. Journal of Clinical Oncology 1994; 12:1592–1599.
Surveillance, Epidemiology, and End Results (SEER) Program Public Use CD-ROM (1973–93). Washington, D.C.: National Cancer Institute, DCPC, Surveillance Program, Cancer Statistics Branch. 1993.
Teichgraeber J, Bowman J, Goepfert H. New test series for the functional evaluation of oral cavity cancer. Head and Neck Surgery 1985; 8:9–20.
Toljanic JA, Ali M, Haraf DJ, Vokes EE, Moran WJ, Graham L. Osteoradionecrosis of the jaws as a risk factor in radiotherapy: A report of an eight-year retrospective review. Oncology Reports 1998; 5:345–349.
U.S. Department of Health and Human Services, Public Health Service. Healthy People 2000: National Health Promotion and Disease Prevention Objectives. Washington, DC, 1991.
Valdez IH, Atkinson JC, Ship JA, Fox PC. Major salivary gland function in patients with radiation-induced xerostomia: Flow rates and sialochemistry. International Journal of Radiation Oncology, Biology and Physics 1992; 25:41–47.
Van Merkesteyn JPR, Bakker DJ, Porgmeijer-Hoelen AMMJ. Hyperbaric oxygen treatment of osteoradionecrosis of the mandible. Experience in 29 patients. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 1995; 80:12–16.
Wang CC. Management and prognosis of squamous-cell carcinoma of the tonsillar region. Radiology 1972; 104:667–671.
Widmark G, Sagne S, Heikel P. Osteoradionecrosis of the jaws. International Journal of Oral and Maxillofacial Surgery 1989; 18:302–306.
Wright WE. Pretreatment oral health care interventions for radiation patients. U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health. Consensus Development Conference on Oral Complications of Cancer Therapies: Diagnosis, Prevention, and Treatment. National Cancer Institute Monographs 1990; 9:57–59.
Leukemia and Lymphoma
Ahmed T, Engelking C, Szalyga J, Helson L, Coombe N, Cook P, Corbi D, Puccio C, Chun H, Mittelman A. Propantheline prevention of mucositis from etoposide. Bone Marrow Transplant 1993; 12:131–132.
American Cancer Society (ACS). Cancer Facts and Figures—1999: Selected Cancers. Atlanta: ACS, 1999.
Anderson PM, Ramsay NK, Shu XO, Rydholm N, Rogosheske J, Nicklow R, Weisdorf DJ, Skubitz KM. Effect of low-dose oral glutamine on painful stomatitis during bone marrow transplantation. Bone Marrow Transplant 1998; 22:339–344.
Barasch A, Peterson DE, Tanzer JM, D’Ambrosio JA, Nuki K, Schubert MM, Franquin JC, Clive J, Tutschka P. Helium-neon laser effects on conditioning-induced oral mucositis in bone marrow transplantation patients. Cancer 1995; 76:2550–2556.
Bergmann OJ. Oral infections and septicemia in immunocompromised patients with hematologic malignancies. Journal of Clinical Microbiology 1988; 26:2105–2109.
Bergmann OJ. Oral infections and fever in immunocompromised patients with haematologic malignancies. European Journal of Clinical Microbiology and Infectious Diseases 1989; 8:207–213.
Bergmann OJ, Ellermann-Eriksen S, Mogensen SC, Ellegaard J. Acyclovir given as prophylaxis against oral ulcers in acute myeloid leukaemia: Randomised, double blind, placebo controlled trial. British Medical Journal 1995; 310:1169–1172.
Borowski B, Benhamou E, Pico JL, Laplanche A, Margainaud JP, Hayat M. Prevention of oral mucositis in patients treated with high-dose chemotherapy and bone marrow transplantation: A randomised controlled trial comparing two protocols of dental care. European Journal of Cancer: B Oral Oncology 1994; 30B:93–97.
Coda BA, O’Sullivan B, Donaldson G, Bohl S, Chapman CR, Shen DD. Comparative efficacy of patient-controlled administration of morphine, hydromorphone, or sufentanil for the treatment of oral mucositis pain following bone marrow transplantation. Pain 1997; 72:333–346.
Cohen G, Elad S, Or R; Galili D, Garfunkel AA. The use of tretinoin as oral mucositis prophylaxis in bone marrow transplantation patients: A preliminary study. Oral Diseases 1997; 3:243–246.
Cowen D, Tardieu C, Schubert M, Peterson D, Resbeut M, Faucher C, Franquin JC. Low energy helium-neon laser in the prevention of oral mucositis in patients undergoing
bone marrow transplant: Results of a double blind randomized trial. International Journal of Radiation Oncology, Biology, and Physics 1997; 38:697–703.
Dreizen S, McCredie KB, Bodey GP, Keating MJ. Quantitative analysis of the oral complications of antileukemia chemotherapy. Oral Surgery, Oral Medicine, Oral Pathology 1986; 62:650–653.
Epstein JB, Vickars L, Spinelli J, Reece D. Efficacy of chlorhexidine and nystatin rinses in prevention of oral complications in leukemia and bone marrow transplantation. Oral Surgery, Oral Medicine, Oral Pathology 1992; 73:682–689.
Epstein JR. Infection prevention in bone marrow transplantation and radiation patients. NCI Monographs 1990; 9:73–85.
Ferretti GA, Ash RC, Brown AT, Parr MD, Romond EH, Lillich TT. Control of oral mucositis and candidiasis in marrow transplantation: A prospective, double-blind trial of chlorhexidine digluconate oral rinse. Bone Marrow Transplant 1988; 3:483–493.
Greenberg MS, Cohen SG, McKitrick JC, Cassileth PA. The oral flora as a source of septicemia in patients with acute leukemia. Oral Surgery 1982; 53:32–36.
Heimdahl A, Mattsson T, Dahllof G, Lonnquist B, Ringden O. The oral cavity as a port of entry for early infections in patients treated with bone marrow transplantation. Oral Surgery, Oral Medicine, Oral Pathology 1989; 68:711–716.
Hill HF, Chapman CR, Kornell JA, Sullivan KM, Saeger LC, Benedetti C. Self-administration of morphine in bone marrow transplant patients reduces drug requirement. Pain 1990; 40:121–129.
Karthaus M, Rosenthal C, Huebner G, Paul H, Elser C, Hertenstein B, Krauter J, Scharmann T, Geissler RG, Heil G, Ganser A. Effect of topical oral G-CSF on oral mucositis: A randomised placebo-controlled trial. Bone Marrow Transplant 1998; 22:781–785.
Labar B, Mrsic M, Pavletic Z, Bogdanic V, Nemet D, Aurer I, Radman I, Filipovic-Grcic N, Sertic D, Kalenic S, et al. Prostaglandin E2 for prophylaxis of oral mucositis following BMT. Bone Marrow Transplant 1993; 11:379–382.
Laine P, Meurman JH, Murtomaa H, Lindqvist C, Torkko H, Pyrhonen S, Teerenhovi L. One-year trial of the effect of rinsing with an amine fluoride-stannous fluoride-containing mouthwash on gingival index scores and salivary microbial counts in lymphoma patients receiving cytostatic drugs. Journal of Clinical Periodontology 1993; 20:628–634.
Lockhart PB, Schmidke MA. Antibiotic considerations in medically compromised patients. Dental Clinics of North America 1994; 38:381–402.
Lopez I, Goudou C, Ribrag V, Sauvage C, Hazebroucq G, Dreyfus F. Treatment of mucositis with vitamin E during administration of neutropenic antineoplastic agents. Annales de Medecine Interne (Paris) 1994; 145:405–408.
Meurman JH, Laine P, Murtomaa H, Lindqvist C, Torkko H, Teerenhovi L, Pyrhonen S. Effect of antiseptic mouthwashes on some clinical and microbiological findings in the mouths of lymphoma patients receiving cytostatic drugs. Journal of Clinical Periodontology 1991; 18:587–591.
Meurman JH, Pyrhonen S, Teerenhove L, Lindquist C. Oral sources of septicemia in patients with malignancies. Oral Oncology 1997; 33:389–397.
Overholser CD, Peterson DE, Williams LT, Schimpff SC. Periodontal infection in patients with acute nonlymphocytic leukemia. Prevalence of exacerbations. Archives of Internal Medicine 1982; 142:551–554.
Peterson DE. Pretreatment strategies for infection prevention in chemotherapy patients. NCI Monographs 1990; 9:61–71.
Pillitteri LC, Clark RE. Comparison of a patient-controlled analgesia system with continuous infusion for administration of diamorphine for mucositis. Bone Marrow Transplant 1998; 22:495–498.
Richard P, Amador Del Valle G, Moreau P, Milpied N, Felice MP, Daeschler T, Harousseau JL, Richet H. Viridans streptococcal bacteraemia in patients with neutropenia. Lancet 1995; 345:1607–1609.
Ries LAG, Kosary Cl, Hankey BF, Miller BA, Edwards BK (eds). SEER Cancer Statistics Review, 1973–1996. Bethesda, MD: National Cancer Institute, 1999.
Sonis ST, Fazio RC, Fang L (eds). Principles and Practice of Oral Medicine, 2nd ed. Philadelphia: WB Saunders, 1995.
Syrjala KL, Donaldson GW, Davis MW, Kippes ME, Carr JE. Relaxation and imagery and cognitive-behavioral training reduce pain during cancer treatment: A controlled clinical trial. Pain 1995; 63:189–198.
Toljanic JA, Bedard J-F, Larson RA, Fox JP. A prospective pilot study to evaluate a new dental assessment and treatment paradigm for patients scheduled to undergo intensive chemotherapy for cancer. Cancer 1999; 85:1843–1848.
Wahlin YB. Effects of chlorhexidine mouthrinse on oral health in patients with acute leukemia. Oral Surgery, Oral Medicine, Oral Pathology 1989; 68:279–287.
Weisdorf DJ, Bostrom B, Raether D, Mattingly M, Walker P, Pihlstrom B, Ferrieri P, Haake R, Goldman A, Woods W, et al. Oropharyngeal mucositis complicating bone marrow transplantation: Prognostic factors and the effect of chlorhexidine mouth rinse. Bone Marrow Transplant 1989; 4:89–95.
Wingard JR. Oral complications of cancer therapies. Infectious and noninfectious systemic consequences. NCI Monographs 1990; 9:21–26.
Organ Transplantation
Adams CK, Famili P. A study of the effects of the drug FK 506 on gingival tissues. Transplant Proceedings 1991; 23:3193–3194.
Antony SJ, Stratton CW, Dummer JS. Lactobacillus bacteremia: Description of the clinical course in adult patients without endocarditis. Clinical Infectious Diseases 1996; 23:773–778.
Bartold PM. Cyclosporine and gingival overgrowth. Journal of Oral Pathology 1987; 16:463–468.
Berry NJ, Burns DM, Wannamethee G, Grundy JE, Lui SF, Prentice HG, Griffiths PD. Seroepidemiological studies on the acquisition of antibodies to cytomegalovirus, herpes simplex virus and human immunodeficiency virus among general hospital patients and those attending a clinic for sexually transmitted diseases. Journal of Medical Virology 1988; 24:385–393.
Cohen SG. Renal disease. Chapter 15, pp. 487–509 in Lynch MA, Brightman VJ, Greenberg MS (eds). Burket’s Oral Medicine, 9th ed. Philadelphia: JB Lippincott, 1994.
Colonna II JO, Winston DJ, Brill JE, Goldstein LI, Hoff MP, Hiatt JR, Quinones-Baldrich W, Ramming KP, Busuttil RW. Infectious complications in liver transplantation. Archives of Surgery 1988; 123:360–364
DeRossi SS, Glick M. Dental considerations for the patient with renal disease receiving hemodialysis. JADA 1996; 127:211–219.
Epstein JB, Sherlock CH, Wolber RA. Oral manifestations of cytomegalovirus infections. Oral Surgery, Oral Medicine, Oral Pathology 1993; 75:443–451.
Ferguson GA, Whyman RA. Dental management of people with renal disease and renal transplants. New Zealand Dental Journal 1998; 94:125–130.
Finberg R, Fingeroth J. Infections in transplant recipients. Chapter 136, pp. 840–846 in Harrison’s Principles of Internal Medicine, 14th ed. New York: McGraw-Hill, 1998.
Fischel RJ, Payne WD, Gillingham KJ, Dunn DL, Sutherland DE, Matas AJ, Najarian JS. Long-term outlook for renal transplant recipients with one-year function. “Doctor, what are my chances?” Transplantation 1991; 51:118–122.
Fishman JA, Rubin RH. Infection in organ-transplant recipients. New England Journal of Medicine 1998; 338:1741–1750.
Genco RJ, Löe H. The role of systemic conditions and disorders in periodontal disease. Periodontology 2000 1993; 98:98–116.
Gruber SA, Gillingham K, Sothern RB, Stephanian E, Matas AJ, Dunn DL. De novo cancer in cyclosporine-treated and non-cyclosporine-treated adult primary renal allograft recipients. Clinical Transplantation 1994; 8:338–395.
Haffajee AD, Socransky SS. Microbial etiological agents of destructive periodontal diseases. Periodontology 2000 1994; 5:78–111.
Hanto DW. Transplantation. Journal of the American College of Surgery 1998; 186:232–239.
Health Care Financing Administration (HCFA). Medicare Carrier’s Manual, Part B. Coverage and Limitations, Section 2136: Dental Services.
Jacobs C, Brunner FP, Brynger H, Chantler C, Donckerwolcke RA, Hathway RA, Kramer P, Selwood NH, Wing AJ. Malignant diseases in patients treated by dialysis and transplantation in Europe. Transplant Proceedings 1981; 13:729–732.
Jonas S, Rayes N, Neumann U, Neuhaus R, Bechstein WO, Guckelberger O, Tullius SG, Serke S, Neuhaus P. De novo malignancies after liver transplantation using tacrolimus-based protocols or cyclosporine-based quadruple immunosuppression with an interleukin-2 receptor antibody or antithymocyte globulin. Cancer 1997; 80:1141–1150.
Jorgensen MG. Prevalence of amlodipine-related gingival hyperplasia. Journal of Periodontology 1997; 68:676–678.
Katz MH, Greenspan D, Westenhouse J, Hessol NA, Buchbinder SP, Lifson AR, Shiboski S, Osmond D, Moss A, Samuel M, et al. Progression to AIDS in HIV-infected homosexuals and bisexual men with hairy leukoplakia and oral candidiasis. AIDS 1992; 6:95–100.
King GN, Thornhill MH. Dental attendance patterns in renal transplant recipients. Oral Diseases 1996; 2:145–147.
King GN, Fullinfaw R, Higgins TJ, Walker RG, Francis DM, Wiesenfeld D. Gingival hyperplasia in renal allograft recipients receiving cyclosporin-A and calcium antagonists. Journal of Clinical Periodontology 1993; 20:286–293.
King GN, Healy CM, Glover MT, Kwan JT, Williams DM, Leigh IM, Thornhill MH. Prevalence and risk factors associated with leukoplakia, hairy leukoplakia, erythematous candidiasis, and gingival hyperplasia in renal transplant recipients. Oral Surgery, Oral Medicine, Oral Pathology 1994; 78:718–726.
Kusne S, Manez R. Infectious complications. Chapter 11, pp. 315–332 in Shapiro R, Simmons RL, Starzl TE (eds). Complications of Renal Transplantation. Stamford, CT: Appleton & Lange, 1997.
Kusne S, Dummer JS, Singh N, Iwatsuki S, Makowka L, Esquivel C, Tzakis AG, Starzl TE, Ho M. Infections after liver transplantation. An analysis of 101 consecutive cases. Medicine (Baltimore) 1988; 67:132–143.
Lipkowitz GS, Madden RL. Transmission of Kaposi’s sarcoma by solid organ donation. Transplant Science 1994; 4:9–11.
Löe H. Periondontal disease. The sixth complication of diabetes mellitus. Diabetes Care 1993; 16:329–334.
MacPhail LA, Hilton JF, Heinic GS, Greenspan D. Direct immunofluorescence vs. culture for detecting HSV in oral ulcers: A comparison. JADA 1995; 126:74–78.
Maier H, Zoller J, Herrmann A, Kreiss M, Heller W-D. Dental status and oral hygiene in patients with head and neck cancer. Otolaryngology, Head and Neck Surgery 1993; 108:655–661.
McCauley J. Medical complications. Chapter 11, pp. 299–313 in Shapiro R, Simmons RL, Starzl TE (eds). Complications of Renal Transplantation. Stamford, CT: Appleton & Lange, 1997.
Muzyka BC, Glick M. A review of oral fungal infections and appropriate therapy. JADA 1995; 126:63–72.
Naugle K, Darby ML, Bauman DB, Lineberger LT, Powers R. The oral health status of individuals on renal dialysis. Annals of Periodontology 1998; 3:197–205.
Naylor GD, Fredericks MR. Pharmacologic considerations in the dental management of the patient with disorders of the renal system. Dental Clinics of North America 1996; 40:665–683.
Naylor GD, Hall EH, Terezhalmy GT. The patient with chronic renal failure who is undergoing dialysis or renal transplantation: Another consideration for antimicrobial prophylaxis. Oral Surgery, Oral Medicine, Oral Pathology 1988; 65:116–121.
Okabe K, Nakagawa K, Yamamoto E. Factors affecting the occurrence of bacteremia associated with tooth extraction. International Journal of Oral and Maxillofacial Surgery 1995; 24:239–242.
Oliver RC, Tervonen T. Diabetes—A risk factor for periodontitis in adults? Journal of Periodontology 1994; 65:530–538.
Rateitschak-Pluss EM, Hefti A, Rateitschak KH. Gingival hyperplasia from cyclosporin A medication. SSO Schweiz Monatsschr Zahnheilkd 1983; 93:57–65.
Rees TD. Drugs and oral disorders. Periodontology 2000 1998; 18:21–36.
Reyna J, Richardson JM, Mattox DE, Banowsky LH, Nicastro-Lutton JJ. Head and neck infection after renal transplantation. JAMA 1982; 247:3337–3339.
Rose LF and Kaye D. Internal Medicine for Dentistry, 2nd ed. CV Mosby, St. Lewis, pp 567–570, 1990.
Rubin RH, Tolkoff-Rubin NE. Opportunistic infections in renal allograft recipients. Transplant Proceedings 1988; 20:12–18.
Ruskin JD, Wood RP, Bailey MR, Whitmore CK, Shaw BW. Comparative trial of oral clotrimazole and nystatin for oropharyngeal candidiasis prophylaxis in orthotopic liver transplant patients. Oral Surgery, Oral Medicine, Oral Pathology 1992; 74:567–571.
Sakurai K, Drinkwater D, Sutherland DE, Fleischmann J, Hage A, Yonemura C. Dental treatment considerations for the pre- and post-organ transplant patient. Journal of the California Dental Association 1995; 23:61–66.
Samaranayake LP, MacFarlane TW, Lamey PJ, Ferguson MM. A comparison of oral rinse and imprint sampling techniques for the detection of yeast, coliform and Staphylococcus aureus carriage in the oral cavity. Journal of Oral Pathology 1986; 15:386–388.
Schweitzer EJ, Matas AJ, Gillingham KJ, Payne WD, Gores PF, Dunn DL, Sutherland DE, Najarian JS. Causes of renal allograft loss. Progress in the 1980s, challenges for the 1990s. Annals of Surgery 1991; 214:679–688.
Seymour RA, Thomason JM, Nolan A. Oral lesions in organ transplant patients. Journal of Oral Pathology and Medicine 1997; 26:297–304.
Sheil AG, Disney AP, Mathew TH, Amiss N. De novo malignancy emerges as a major cause of morbidity and late failure in renal transplantation. Transplant Proceedings 1993; 25:1383–1384.
Strom BL, Albrutyn E, Berlin JA, Kinman JL, Feldman RS, Stolley PD, Levison ME, Korzeniowski OM, Kaye D. Dental and cardiac risk factors for infective endocarditis: A population-based, case-control study. Annals of Internal Medicine 1998; 129:761–769.
Svirsky JA, Saravia ME. Dental management of patients after liver transplantation. Oral Surgery, Oral Medicine, Oral Pathology 1989; 67:541–546.
Thomason JM, Seymour RA, Rice N. The prevalence and severity of cyclosporin and nifedipine-induced gingival overgrowth. Journal of Clinical Periodontology 1993; 20:37–40.
Thomason JM, Seymour RA, Ellis J. The periodontal problems and management of the renal transplant patient. Renal Failure 1994; 16:731–745.
Thomason JM, Seymour RA, Ellis JS, Kelly PJ, Parry G, Dark J, Wilkinson R, Ilde JR. Determinants of gingival overgrowth severity in organ transplant patients. An examination of the role of HLA phenotype. Journal of Clinical Periodontology 1996; 23:628–634.
Thomason JM, Ellis JS, Kelly PJ, Seymour RA. Nifedipine pharmacological variables as risk factors for gingival overgrowth in organ-transplant patients. Clinical Oral Investigations 1997; 1:35–39.
United Network for Organ Sharing (UNOS). 1998 Annual Report of the U.S. Scientific Registry for Transplant Recipients and the Organ Procurement and Transplantation Network—Transplant data: 1988–96. Richmond, VA, 1999.
Van der Meer, JTM, Thompson J, Valkenburg HA, Michel MF. Epidemiology of bacterial endocarditis in the Netherlands. II. Antecedent procedures and use of prophylaxis. Archives of Internal Medicine 1992; 151:1869–1873.
Varga E, Lennon M, Mair L. Pre-transplant gingival hyperplasia predicts severe cyclosporine-induced gingival overgrowth in renal transplant patient. Journal of Clinical Periodontology 1998; 25:225–230.
Westbrook P, Bednarczyk EM, Carlson M, Sheehan H, Bissada NF. Regression of nifedipine-induced gingival hyperplasia following switch to a same class calcium channel blocker, isradipine. Journal of Periodontology 1997; 68:645–650.
Wilson RF, Morel A, Smith D, Koffman CG, Ogg CS, Rigden PA, Ashley FP. Contribution of individual drugs to gingival overgrowth in adult and juvenile renal transplant patients treated with multiple therapy. Journal of Clinical Periodontology 1998; 25:457–464.
Wilson RL, Martinez-Tirado J, Whelchel J, Lordon RE. Occult dental infection causing fever in renal transplant patients. American Journal of Kidney Diseases 1982; 11:354–356.
Wondimu B, Dahllof G, Berg U, Modeer T. Cyclosporin-A-induced gingival overgrowth in renal transplant children. Scandinavian Journal of Dental Research 1993; 101:282–286.
Zeldin G, Magyars J, Klein PJ, Thuluvath J. Immunization, screening for malignancy, and health maintenance in the liver transplant recipient. American Society of Transplant Surgeons. Abstract 1998.
Ziccardi VB, Saini J, Demas PN, Braun TW. Management of the oral and maxillofacial surgery patient with end-stage renal disease. Journal of Oral and Maxillofacial Surgery 1992; 50:1207–1212.
Heart Valve Replacement and Repair
Drangsholt MT. A new causal model of dental diseases associated with endocarditis. Annals of Periodontology 1998; 3:184–196.
Roberts GJ. Dentists are innocent! “Everyday” bacteremia is the real culprit: A review and assessment of the evidence that dental surgical procedures are a principal cause of bacterial endocarditis in children. Cardiology 1999; 20:317–325.
Strom BL, Albrutyn E, Berlin JA, Kinman JL, Feldman RS, Stolley PD, Levison ME, Korzeniowski OM, Kaye D. Dental and cardiac risk factors for infective endocarditis: A population-based, case-control study. Annals of Internal Medicine 1998; 129:761–769.
Terezhalmy GT, Safadi TJ, Longworth DL, Muehrcke DD. Oral disease burden in patients undergoing prosthetic heart valve implantation. Annals of Thoracic Surgery 1997; 63:402–404.
Van der Meer, JTM, Thompson J, Valkenburg HA, Michel MF. Epidemiology of bacterial endocarditis in the Netherlands. I. Patient characteristics. Archives of Internal Medicine 1992; 151:1863–1868.