4
Medically Necessary Dental Services
From the outset, the Medicare program has excluded coverage “for services in connection with the care, treatment, filling, removal, or replacement of teeth or structures directly supporting the teeth” (Section 1862(a)(12) of the Social Security Act). The 1965 legislation authorizing the program provided a narrow exception that payment could be made “in the case of inpatient hospital services in connection with the provision of dental services if the individual, because of his/her underlying medical condition and clinical status, or because of the severity of the dental procedure, requires hospitalization in connection with the provision of such services.”
As described in regulations and the program manuals used by the intermediaries and carriers who administer Medicare claims, the Health Care Financing Administration (HCFA) has interpreted the statutory exceptions language to permit payments for professional dental services when they are performed as an “integral part” of covered inpatient procedures (Carriers Manual, section 2136 [HCFA, 1999b]). For example, if the extraction of a tooth in the line of a jaw fracture is integral to treatment of the jaw injury, then dental treatment (i.e., the extraction) is covered. If a beneficiary has to be hospitalized for a dental procedure (e.g., an extraction not integral to a covered medical service) to be safely performed given his or her clinical status, Medicare covers the hospital services but not the dental procedure itself. In general, Medicare-covered services that are within the scope of practice (as defined by states) for a physician as well as a dentist are covered when provided by a dentist. Examples include management of mucositis and treatment of oral infections using antibiotics.
TABLE 4–1 Medicare Coverage of Dental Services as Specified in Statute or by the Health Care Financing Administration
|
Clinical Condition |
Medicare-Covered Service |
|
Underlying medical condition and clinical status requires hospitalization for dental care |
Inpatient hospital services only (Medicare Part A) |
|
Severity of dental procedure requires hospitalization for dental care |
Inpatient hospital services only (Medicare Part A) |
|
Any oral condition for which nondental services are covered |
All dental services if incident to and an integral part of a covered procedure or service performed by the same person (Medicare Part B) |
|
Neoplastic jaw disease |
Extractions prior to radiation and prior to oral examination if extractions occur (Medicare Part B) |
|
Renal transplant surgery |
Oral or dental examination on an inpatient basis (Medicare Part A if performed by hospital-based dentist; Part B if performed by a physician) |
Table 4–1 summarizes Medicare’s limited coverage of dental services. The summary is based on HCFA policy statements rather than on sometimes conflicting carrier policies.
HCFA has explicitly approved coverage exceptions for the extraction of teeth to prepare the jaw for radiation treatment of cancer (Carriers Manual, section 2136 [HCFA, 1999b]) and for an oral examination performed as part of a comprehensive inpatient work up prior to kidney—but not other organ—transplantation (Coverage Issues Manual section 50.26 [HCFA, 1999b]). HCFA has proposed additional exceptions based on arguments that the services would reduce the risk of infection and other complications, but its Technology Advisory Committee suggested that such exceptions (which would include some approved earlier) went further than the Medicare statute allowed and that Congress needed to indicate its approval of coverage based on such an argument (TAC, 1996).
Neither the statutory nor the regulatory language related to coverage exceptions for dental services is straightforward to interpret.1 Moreover, carrier inter-
pretation is not always consistent. For example, at least one carrier’s policies appear to approve coverage for an oral examination not only for kidney transplant patients but also for heart, liver, and other covered organ transplants, whether performed on an outpatient or an inpatient basis (e.g., see Conway, 1995; WPSIC, 1996).
DEFINING MEDICALLY NECESSARY DENTAL SERVICES
The 1997 Balanced Budget Act, which provided for this study, included no definition of “medically necessary dental services.” One definition of such services is found in a bill submitted earlier in 1997 (but not passed). It called for coverage of “dental services that are medically necessary as a direct result of, or will have a direct impact on, an underlying medical condition if the coverage of such services is cost-effective” (H.R. 1288, introduced April 10, 1997). It also included explicit provisions for Medicare to cover dental care related to several specific illnesses. The bill’s language—minus the wording about cost-effectiveness—is similar to that used three years earlier in a bill that included “medically necessary oral health care” in a proposed set of “basic benefits” to be covered as part of broad health care reform (H.R. 3600, introduced May 1994). This earlier proposal also included oral care intended to control pain and infection and to restore function. The committee understands these definitions of medically necessary services—particularly the one proposed in 1997—to be narrowly constructed (1) to continue the general exclusion of Medicare coverage for dental care2 but (2) to broaden the scope of the exceptions to include dental care needed to prevent or effectively manage systemic conditions including the oral complications of specific illnesses or their medical treatment.
Certainly, the prevention and management of oral infection have significant health implications when such infection has the potential to increase systemic morbidity in patients who are immunocompromised or otherwise at greater risk of adverse medical outcomes because of their underlying health problems. The importance of immunosuppression as a medical problem reflects scientific and
|
|
formed by a physician. This manual (unlike the Carriers Manual) also says that a dentist is not recognized as a physician when performing such an examination. |
therapeutic developments that have occurred in the three decades since the adoption of Medicare.
From the broader perspective of individual and public health, the coverage-oriented definitions of “medically necessary dental services” are unduly narrow. The concept that such care involves only care related to an “underlying medical condition” could suggest to some for example, that periodontal or other tooth-related infections are somehow different from infections elsewhere. More generally, such narrow definitions could imply that the mouth can be isolated from the rest of the body, a notion neither scientifically based nor constructive for individual or public health.3 Thus, the remainder of this chapter refers to “medically necessary dental services,” using quotation marks as a reminder of the term’s specialized and restricted meaning in this discussion of Medicare coverage policy and, more generally, of the difficulty of precisely defining such care in most contexts.4 (Appendix C includes further examination of the concept of “medically necessary dental services.”)
Given the limited time and resources available, the committee could provide an evidence-based consideration of “medically necessary dental services” only for a subset of services that might qualify for this designation. The next section of this chapter reviews the approach the committee took to selecting and assessing specific medical conditions and associated dental services. The rest of the chapter reviews the evidence for each condition and presents the estimated costs to Medicare of covering the dental services examined. The final section summarizes the committee’s findings and its conclusions about Medicare coverage for the general category of dental care needed to prevent or effectively manage nondental illnesses or injury including oral complications of other therapies. The background paper commissioned by the committee is found in Appendix C.
ASSESSMENT APPROACH: INTERVENTION, POPULATION, AND OUTCOMES
The selection of conditions and services for assessment was guided in part by historical context. A few months before the passage of the 1997 Balanced Budget Act, legislation had been introduced, first, to cover a specific set of “medically necessary dental services” that were described as “cost-effective” and, more generally, to provide for future coverage of other services subsequently determined to “result in reductions in expenditures…that exceed expenditures resulting from such coverage” (H.R. 1288, April 1997). This latter
requirement is quite stringent; generally, services are considered to be cost-effective (i.e., to have net benefits worth the costs) whether or not they produce cost savings that fully offset direct service costs. The more restrictive language reflects the rules that Congress has adopted requiring increases in spending in one area to be offset by cuts elsewhere or by increased taxes.
The five conditions listed in the 1997 bill had been presented in prior analyses of health conditions that sought to identify those for which the cost of covering inpatient dental services would likely be offset by savings related to complications avoided, especially additional hospitalization (Cameron et al., 1995; Rutkauskas, 1995). The five conditions were
-
head and neck cancer,
-
leukemia,
-
lymphoma,
-
organ transplantation, and
-
valvular heart disease.
Although the Balanced Budget Act provisions calling for this study did not mention any particular conditions, the committee decided that those identified in the prior 1997 legislative proposal were a reasonable focus for its analyses. Table 4–2 summarizes current Medicare coverage (as specified by HCFA) of dental services for these conditions.
Following the general approach set forth in Chapter 2, the committee began by defining the specific dental services that would be investigated for the five identified conditions. It assumed that these services follow referral from a physician caring for a patient with one of the designated medical conditions. The dental care normally provided for these conditions includes a mix of preventive services (e.g., oral examinations to detect infections that might compromise transplant outcomes, cleaning of the teeth to eliminate potential sources of infection) and treatment services (e.g., extraction of abscessed teeth or treatment of gingival or gum enlargement associated with use of cyclosporin). The specific services examined for each condition are described in Appendix C and later sections of this chapter.
The population of interest includes Medicare beneficiaries age 65 and over as well as younger people qualified for Medicare on grounds of disability or diagnosis of end-stage renal disease (ESRD). Evidence related to all age groups was reviewed.
The potential beneficial outcomes investigated include reduced mortality and morbidity due to more effective prevention or management of oral problems related to the five medical conditions or to complications of their treatment. More generally, dental care may improve patient knowledge of good oral health habits. In addition, dental care may bring quality-of-life benefits related to appearance and self-esteem and enjoyment or comfort in eating. Preservation of
teeth is clearly valued by many, although data on the value that people place on teeth—having most of their teeth, a few teeth, or no teeth, or having good versus bad teeth—indicate that the value varies in different cultural subgroups (Hollister and Weintraub, 1993; Slade et al., 1996; Strauss and Hunt, 1993). Potential harms of dental care include the possibility that such care may exacerbate infection or infection risks; cause pain, disfigurement, or functional impairment; or delay other treatment. The literature identified by the committee focused on morbidity (including pain and other discomfort) rather than on quality-of-life outcomes.
TABLE 4–2 Summary of Dental Services Currently Covered and not Covered Under Medicare for Selected Diseases or Conditions
|
Disease or Condition |
Dental Services Currently Covered Under Medicare |
Dental Services not Currently Covered Under Medicare |
|
Head and neck cancer |
Extraction of teeth prior to radiation Oral examination if extractions are to be performed |
Oral examination if no extractions are to be done prior to radiation Preventive care to reduce risk of radiation caries (e.g., fluoride trays, supplemental topical fluoride) Treatment of radiation caries |
|
Lymphoma and leukemia |
Management of mucositis, hemorrhage, and related side effects of underlying disease |
Oral examination prior to treatment Dental treatment to reduce risk of infection or eliminate infection prior to or following treatment |
|
Organ transplantation |
Management of infection following transplantation Oral examination prior to renal transplant surgery on an inpatient basis |
Oral examination for transplants other than kidney Outpatient oral examination performed by a dentist prior to kidney transplant Dental treatment to reduce risk of infection or eliminate infection for any transplantation prior to or following transplant |
|
Heart valve repair or replacement |
None |
Oral examination prior to repair or replacement Dental treatment to reduce risk of infection or eliminate infection prior to or following repair or replacement of valve |
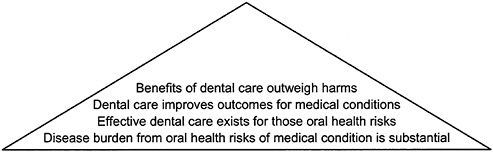
FIGURE 4–1 Evidence pyramid for assessing “medically necessary dental services.”
SOURCE: Adapted from IOM/NRC, 1999, p. 89.
To guide its assessment of the evidence about dental care for these five conditions, the committee adapted the evidence pyramid introduced in Chapter 2 as shown in Figure 4–1. One distinguishing feature of Figure 4–1 compared to the generic pyramid is that it requires a link between a nondental condition or treatment and either dental services or dental complications. The first tier of the pyramid refers accordingly to the relationship between the medical conditions listed earlier and oral health conditions. The relationship could be manifest either as an increased risk to oral health caused by the medical condition (or its treatment) or as an increased risk to systemic health related to poor oral health. The tiers above refer to the effectiveness of dental care in treating oral problems and improving outcomes for the medical condition.
A test that met all of the criteria in Figure 4–1 would clearly have benefits compared to usual care, but the extent of benefit relative to the cost to Medicare, a health plan, or society generally would still have to be considered. The committee did not formally assess the cost-effectiveness of the dental services considered here. As called for by its charge, it did estimate the cost to Medicare of covering these services. Part of this analysis included identifying any offsetting savings to Medicare that might occur as a result, for example, of shorter or avoided hospital stays or reduced use of hyperbaric oxygen therapy for complications associated with treatment for head and neck cancer.
HEAD AND NECK CANCER
Burden of Disease
Cancers of the head and neck are commonly defined to include primary or metastatic cancers involving the oral cavity, pharynx, and larynx5 but to exclude
cancers invoving other parts of the head, notably the eyes, skin, thyroid, and brain. The treatments, as well as head and neck cancer itself, can have serious implications for the health of the patient.
Cancers of the head and neck are more common among persons age 65 and older than among younger persons. Statistics often track invasive cancers of the oral cavity and pharynx and cancers of the larynx separately (SEER, 1999).6 These two categories of head and neck cancers account for approximately 2.6 and 1.6 percent, respectively, of all cancers.
An estimated 29,800 new cases of cancer of the oral cavity and pharynx are expected to be diagnosed in 1999, more than 48 percent (or nearly 14,400) in people age 65 or older (ACS, 1999a). The age-adjusted incidence rate (1992–1996) in those diagnosed at age 65 or older is 45.0 per year per 100,000 population, compared to 6.5 per 100,000 in younger persons. Five-year relative survival rates (1989–1995) do not differ greatly by age—52.3 percent for those age 65 or older and 54.1 percent for younger persons. The lifetime risk of being diagnosed with cancers of the oral cavity or pharynx is 1.47 percent for men and 0.73 percent for women, while the lifetime risk of dying of this cancer is 0.41 percent for men and 0.23 for women.
For cancer of the larynx, an estimated 10,600 new cases are expected in 1999, nearly 55 percent (or about 5,800) in patients age 65 or older. The five-year age-adjusted incidence rate in those age 65 or older is 19.7 per 100,000, compared to 2.3 per 100,000 in younger persons. Five-year relative survival rates again do not differ greatly by age—63.2 percent for those age 65 or older and 65.7 percent for younger persons. The lifetime risk of being diagnosed with cancer of the larynx is 0.72 percent for men and 0.18 percent for women, while the lifetime risk of dying of this cancer is 0.22 percent for men and 0.06 for women.
Most cancers of the oral cavity, pharynx, and larynx are squamous cell carcinomas (affecting the outer layers of the tissue covering the cavity and structures). Epidemiological studies have repeatedly shown head and neck cancers to be positively associated with use of tobacco and alcohol, with both independent and interactive effects. Viral exposures and nutritional deficiencies also are associated with these cancers (reviewed in Carroll et al., 1998).
A dentist or physician may detect cancers of the oral cavity and upper pharynx while the lesions are still asymptomatic. This is more likely for people undergoing regular oral examinations, although evidence has been described as
|
|
of the digestive tube lying between the esophagus and the mouth and nasal cavities. The larynx, which includes the vocal cords, lies below the pharynx and connects to the trachea or windpipe. |
|
6 |
Unless otherwise indicated, data are from the most recent report of the National Cancer Institute’s Surveillance Epidemiology and End-Results Program (SEER), which is available at www-SEER.ims.nci.nih.gov/publications. |
“insufficient” to justify recommendations for or against routine screening for oral cancer (USPSTF, 1996, p. 175). In general, however, patients with cancer of the head and neck tend not to be identified until the disease is fairly advanced.7 The exception is cancer of the vocal cords, where even a very tiny tumor will result in notable hoarseness and thus is likely to be noticed sooner (reviewed in Carroll et al., 1998).
Treatment of Cancers of the Head and Neck
Treatment for most cancers of the head and neck involves radiation, surgery, or a combination, although some chemotherapy is also used (see Appendix C, and Carroll et al., 1998). Treatment is a team effort, involving the head and neck medical oncologist, radiation oncologist, head and neck surgeon, dentist, and other personnel. Surgery to excise cancerous tumors can impair function and appearance. Dental services may be an integral part of treatments to reduce or correct such damage.
Surgery can be especially difficult and risky around the fine structures of the larynx. As a result, clinicians have pressed ahead with the development of chemotherapy (often with radiation) for laryngeal cancers.8 Anticancer drugs in general work by inhibiting cell division in active tissues, which has the side effect of inhibiting healing and growth in the healthy tissue lining the mouth. The resulting irritation and inflammation of the oral mucosa is called mucositis, which can be treated by both physicians and dentists and is discussed further below.
Radiation therapy is used with surgery for most cancers of the oral cavity and pharynx. Radiation, like chemotherapy, can affect both tumor cells and healthy cells. The damage to healthy tissue depends on the size and number of radiation doses and on the location of the tumor and the therapy. Radiation therapy can be from either an external source or an implant; in some cases, both are necessary (Carroll et al., 1998).
The oral side effects of cancer treatment that result from drugs, radiation, and surgery will often be managed by the physicians or surgeons overseeing treatment. For instance, they may modify the dose of anticancer drugs, take a “break” in the course of radiation therapy, or prescribe therapeutic mouthwashes
to allow serious mucositis to heal. In any case, such management would generally fall under the scope of practice for a physician and would therefore be covered even if delivered by a dentist. Radiation therapy has additional, and specifically dental, implications that are examined next.
Oral Health Problems Associated with Radiation Treatment of Cancers of the Head and Neck
Because radiation therapy disrupts cell division in healthy tissue as well as in tumor(s), it also affects the function and structure of the oral mucosa (lining of the mouth) and underlying organs and tissues such as salivary glands and bone. If directed at the lymph nodes in the jaw area, radiation may impinge in varying degrees on the salivary glands, which are very sensitive to radiation effects. Radiation can irreversibly damage these glands, resulting in insufficient production of saliva, known technically as xerostomia (dry mouth). Saliva is important to keep the oral tissues moist and to buffer the acidity of the oral environment, which is critical both to reducing bacterial growth and infection and to laying down new mineral deposits that keep the teeth strong and dense. After radiation, the teeth tend to become demineralized (more porous) and to develop cavities easily, a tendency so marked that it has the special name radiation caries.
Radiation for head and neck cancer is also an important contributing factor in less common but very serious adverse consequences to the underlying bone. Especially in high or multiple doses, radiation affects bone by injuring the small vessels that supply blood to the cells in the bone, so that these cells die. The death of bone cells means that remodeling, which occurs continuously in healthy living bone tissue, proceeds very slowly, as does healing, with the result that the bone becomes susceptible to infection. The bone cell death resulting from radiation is called osteoradionecrosis (ORN). In head and neck radiation, the lower jaw or mandible is the most susceptible because it is a very dense bone, having a relatively low proportion of cells and blood supply to start with. ORN can require surgery to excise the dead tissue, which can in turn leave the jaw and face badly disfigured as well as functionally impaired—with serious consequences for the patient’s quality of life.
The likelihood of ORN is increased by trauma to the bone, including the trauma to the jawbone caused by a tooth extraction (Murray et al., 1980a,b, reviewed in Appendix C). The effect of such trauma on the risk of ORN is especially marked when the extraction or other trauma occurs near (before or after) the time of the radiation (Epstein et al., 1987, reviewed in Appendix C). This occurs presumably because the radiation damage to blood vessels makes healing a recent extraction wound more difficult.
Dental Care for Patients Undergoing Radiation Therapy for Cancer of the Head and Neck
Thirty years ago, the standard of care for patients with head and neck cancer involved extracting teeth before beginning radiation therapy. HCFA has ruled that this treatment meets the criteria for coverage as an exception to Medicare’s general exclusion of dental care, even though extraction is generally carried out as a separate step rather than as an integral part of the radiation therapy. The rationale for covering such extractions was that tooth removal would preclude radiation-related caries and the possible later need for extractions that would increase the risk for ORN.
In the 1970s, however, dentists began to experiment with aggressive tooth-sparing approaches to dental care before, during, and after radiation therapy for head and neck cancer. The new approach to care called for a preradiation program to improve and protect the patient’s oral health through an evaluation, careful oral hygiene, fluoride applications, restoration of the teeth that were salvageable, and removal of unrestorable or periodontally diseased teeth with adequate healing time if possible. During and after radiation, this approach called for the patient to continue very thorough oral hygiene and home fluoride treatments. After radiation therapy, the dentist provides further monitoring and restoration as needed (Keys and McCasland, 1976, as reviewed in Appendix C). None of the care involved in this tooth-preserving approach is covered by Medicare unless an extraction occurs prior to radiation, in which case the oral examination may also be covered.
Absent unexpected negative research findings, the role of tooth-preserving therapy should continue to increase. Surveys of the population ages 65 to 74 taken in 1971–1974 and in 1985–1986 show that the percentage of older persons who have lost all their teeth dropped from 45 to 41.1 percent, a trend that has continued (Bloom et al., 1992; Marcus et al., 1996; MMWR, 1999; NIDR, 1987). In recent years, approximately 33 to 43 percent of patients diagnosed with head or neck cancers have already lost all their teeth (Appendix C; Lockhart and Clark, 1994; Niewald et al., 1996, Roos et al., 1996). Of those retaining some teeth, the average patient still possesses only about a third of the full complement of 32 adult teeth, and most have accumulations of plaque and some tooth decay (Lockhart and Clark, 1994; Niewald et al., 1996). The challenge is how best to manage such patients to minimize further dental and medical problems—including loss of additional teeth, bone destruction, surgical treatment, functional impairment, and disfigurement—associated with radiation therapy for patients with head and neck cancer.
Effectiveness of Dental Care in Improving Health Outcomes for Head and Neck Cancer Patients Treated with Radiation
No randomized controlled trials have compared the effectiveness of tooth-preserving protocols and protocols that emphasize tooth extraction without preventive care for head and neck cancer patients undergoing radiation therapy. One of the earliest retrospective studies comparing tooth-preserving and aggressive tooth extraction protocols was carried out at Walter Reed Army Medical Center (Keys and McCasland, 1976). It showed that patients in the tooth-preserving protocol lost fewer teeth than their predecessors treated under an aggressive tooth extraction protocol. (Other key patient care procedures, including the radiation techniques and doses, remained stable during the time periods compared.) Patients in the tooth-preserving protocol also required fewer dental visits both before and after radiation therapy (Keys and McCasland, 1976). ORN rates were historically low before and after the change in protocol, so the study did not demonstrate an effect on ORN.
Another retrospective analysis during the same period, however, demonstrated the potential for dental conservation to reduce ORN (Bedwinek et al., 1976). Researchers at M.D.Anderson compared two periods of dental management for patients treated with radiation to the jaws. Among those treated when extractions were the favored treatment, 19.7 percent developed ORN, with the precipitating factors assigned to dental extraction (11.8 percent), denture irritation (2.5 percent), and spontaneous or unknown causes (5.4 percent). During the period that tooth-preserving protocols were in place, 7.9 percent developed ORN, with the precipitating factors assigned to dental extraction (2.3 percent), denture irritation (1.1 percent), and spontaneous or unknown causes (4.5 percent). Other research indicates that the highest incidence of ORN occurs when extractions immediately precede or follow radiation therapy (Epstein et al., 1987).
Studies to identify causes of ORN have repeatedly identified extractions and lack of preventive dental care as major contributing factors (Beumer et al., 1984; Curi and Dib, 1997; Kluth et al., 1988; Murray et al., 1980a,b). As tooth-preserving treatments have become more common and the rate of ORN has dropped, unknown causes of ORN are proportionately more likely to be identified as causes than are extractions.
Evidence from a randomized, placebo-controlled trial suggested that fluoride treatments following radiation were responsible for much of the effectiveness of the tooth-preserving protocols in reducing postradiation caries in patients with xerostomia (Driezen et al., 1977). Patient compliance with daily fluoride application on an indefinite basis is a challenge, just as patient compliance is challenging in other areas; compliance may likewise be increased by contact with clinicians (see Epstein et al., 1995, 1996; see also Chapter 5).
Because ORN is associated with injury to blood vessels and failure to heal, several centers have investigated the use of hyperbaric oxygen (HBO) therapy to prevent ORN resulting from extractions after radiation therapy. HBO, which supplies oxygen at a higher concentration than in normal air, may facilitate healing by promoting blood vessel formation and supporting tissues that are poorly supplied with oxygen. HBO therapy has been used prophylactically to help avoid ORN and to treat patients who have developed ORN. Although the treatment has been reported to be effective, the equipment required is not currently available in many places and is expensive even when available (Marx et al., 1985; Myers and Marx, 1990).
HBO prevention of ORN can be less expensive than treatment of serious ORN, but both are considerably more costly per patient than tooth-preserving dental care and self-care. Although tooth-preserving dental interventions for those with head and neck cancer are not covered by Medicare, HCFA has approved coverage of HBO therapy for osteoradionecrosis (Coverage Issues Manual, section 35.10 [HCFA, 1999b]). As noted earlier, the extraction of teeth to prepare the jaw for radiation treatment of neoplastic disease such as head and neck cancer is covered by Medicare. The costs to Medicare of adding coverage for certain tooth-preserving dental services for head and neck cancer patients and the possible offsetting savings are discussed later in this chapter.
LEUKEMIA AND LYMPHOMA
The first parts of this section discuss the general burden of disease and the oral health problems associated with leukemia and lymphoma and the treatment of these cancers. The later parts present a combined discussion of the management of oral health problems associated with these conditions or their treatment.
Leukemia
Burden of Disease
Leukemias are malignancies of the blood cells and blood-forming organs. They account for about 1.7 percent of all cancer cases (ACS, 1999a). Of the four major kinds of leukemia, the incidence of three—chronic lymphocytic leukemia, acute myeloid leukemia, and chronic myeloid leukemia—is higher in those age 65 and over than in those younger than 65 (SEER, 1999).9 The incidence is only slightly lower for the fourth kind, acute lymphocytic leukemia. All leukemias taken together are predicted to cause 30,200 new cases in 1999. Of these cases, 56.4 percent (or about 17,000) are expected to be diagnosed in patients age 65 or older. The incidence rate in those age 65 or older is 51.4 per 100,000, compared
to 5.8 per 100,000 in younger persons. Five-year survival rates also vary by age, 33.9 percent for those age 65 or older and 51.2 percent for younger persons. For specific types of leukemia, five-year survival rates for the older age group are less than 6 percent for the acute leukemias and do not exceed 25 percent for chronic myeloid leukemia. For chronic lymphocytic leukemia, the five-year survival rate is 65.9 percent for those age 65 or older, compared to 78.8 percent for younger persons.
Leukemia is typically diagnosed by blood and bone marrow tests. The lifetime risk of being diagnosed with any leukemia is 1.38 percent for men and 1.06 percent for women, and the lifetime risk of dying from leukemia is 0.94 percent for men and 0.77 percent for women.
Oral Health Problems and Leukemias
Oral symptoms are a common reason for patients to seek care that leads to a diagnosis of leukemia. The majority of those found to have acute or chronic leukemia have such symptoms early in the course of the disease. Symptoms include bleeding or infected gingiva (gums), gingival overgrowth, hemorrhagic points (petechiae) or spots (ecchymoses) resulting from reduced platelet levels (thrombocytopenia), ulcers, and other inflammations. Because those with leukemia often have suppressed immune systems due to the disease (and may become more immunosuppressed as a result of chemotherapy), they are at higher than usual risk of oral and other infections. Septicemia is a major cause of death in leukemia patients (Bodey et al., 1978; Rintala, 1994; as discussed in Appendix C).
Treatment for Leukemias
Medical treatment for acute leukemias typically involves single- or multiple-agent chemotherapy with supportive red blood cell or platelet transfusions to manage the anemia and thrombocytopenia often associated with the disease. Because chronic lymphocytic leukemia often progresses slowly and is not curable with current treatments (which generally have unpleasant side effects), it is often managed conservatively by observation and treatment of associated infections, anemia, hemorrhage due to platelet deficiency, and other complications of the disease. For chronic myeloid leukemia, the only cure is bone marrow transplant, which is generally not recommended for older patients. Chemotherapy, radiation, or biologic therapy may lengthen survival for some patients with this type of leukemia.
Lymphoma
Burden of Disease
Lymphomas are malignancies of the lymph system. One type, Hodgkin’s disease, is most common in two age groups—young adults and those over 55 (NCI, 1999a). The incidence of Hodgkin’s disease is declining, however, especially among those 65 and over. In 1999, 7,200 new cases of Hodgkin’s disease are predicted to cause 7,200 new cases, less than 0.6 percent of all new cancer cases. The disease still accounts for about 1.9 percent of all cancer cases (ACS, 1999a). Of the new cases, only 15 percent (about 1,100) are expected to be diagnosed in patients age 65 or older. The incidence rate in those age 65 or older is 3.6 per 100,000, compared to 2.6 per 100,000 in younger persons (SEER, 1999).10 Five-year survival rates are 45.3 percent for those age 65 or older and 86.6 percent for younger persons. The lifetime risk of being diagnosed with Hodgkin’s disease is 0.24 percent for men and 0.20 percent for women, whereas the lifetime risk of dying from it is 0.06 percent for men and 0.04 percent for women.
Non-Hodgkin’s lymphoma, which actually includes nearly 30 types of cancers, presents a very different epidemiological picture. The same data and estimate sources predict 56,800 new cases in 1999, 4.6 percent of all new cancer cases and 3.6 percent of all cancer cases taken together. Of the new cases, 51.6 percent (or 29,300) are expected to be diagnosed in patients age 65 or older. The incidence rate in those age 65 or older is 75.5 per 100,000, compared to 9.2 per 100,000 in younger persons. Five-year survival rates differ less by age, 46.7 percent for those age 65 or older and 54.4 percent for younger persons. The lifetime risk of being diagnosed with non-Hodgkin’s lymphoma is 2.08 percent for men and 1.71 percent for women, while the lifetime risk of dying from it is 0.96 percent for men and 0.92 percent for women.
Oral Health Problems and Lymphomas
Lymphoma patients, particularly Hodgkin’s disease patients, are at increased risk for infections of all sorts. Non-Hodgkin’s lymphoma patients can develop mouth ulcers. As discussed below, other oral problems may follow the treatment of either disease.
Treatment for Lymphomas
Depending on the type of lymphoma, treatment may include radiation, chemotherapy, or both. Early stages of non-Hodgkin’s lymphoma may be treatable by radiation alone, but later-stage disease often requires both treatment modalities. Chemotherapy and radiation may be used alone or in combination for
patients with Hodgkin’s disease, depending on the stage and other characteristics of the disease (NCI, 1999a).
Oral Health Problems Related to Treatment for Leukemia and Lymphoma
In addition to oral symptoms arising from the disease (leukemia or lymphoma) itself, chemotherapeutic treatment (including high-dose chemotherapy with bone marrow transplant) frequently induces oral health problems, in particular, mucositis and stomatitis (an inflammatory condition of the mouth). These problems arise both from immunosuppression, which results from damage to the blood-forming cells in the bone marrow, and from direct drug toxicity to the oral mucosal cells lining the mouth.
Severe mucositis and stomatitis can involve extensive ulceration, intense pain, and disfiguring destruction of tissue. These problems may interfere sufficiently with chewing or swallowing to cause malnutrition or dehydration. In addition, while patients are severely immunosuppressed from chemotherapy, they may experience acute exacerbations of asymptomatic periodontal disease (Overholser et al., 1982). In general, the more extensive the chemotherapy, the more serious and widespread these adverse oral conditions are likely to be. For some patients, adjustment of the chemotherapy regimen (types and amounts of drugs) may reduce the severity of mucositis or stomatitis.
When patients with lymphoma are treated with radiation that includes the jaw area (where many lymph nodes are located), these patients—like those with head and neck cancer—may suffer injury to the salivary glands and resulting xerostomia. Xerostomia, as described earlier, promotes infection, demineralization of the teeth, and dental caries. Systemic infection is also a threat when patients have preexisting oral infections and when oral tissue damaged by chemotherapy becomes secondarily infected. Researchers have documented oral lesions colonized by one or more types of organisms in 34 percent of patients undergoing chemotherapy for leukemia (Dreizen et al., 1986). One cohort study that tracked bacteremia (presence of viable bacteria in the circulating blood) and bacterial cultures from saliva in high-dose chemotherapy patients suggests that the oral mucosa likely was the point of entry for the infecting organism but could not demonstrate that oral sources were exclusively responsible (Richard et al., 1995). Research also suggests that acute oral infections may contribute to fevers and septicemia in these immunocompromised patients, but the specific contribution of oral organisms remains unclear (Bergmann, 1988, 1989; Greenberg, 1990; Greenberg et al., 1982). Older age, type of cancer, and oral health status prior to chemotherapy have been identified as risk factors for the subsequent development of chemotherapy complications (Sonis and Clark, 1991).
Dental Care for Patients with Leukemia or Lymphoma
As described in Appendix C, the standard evaluation for patients diagnosed with leukemia or lymphoma includes a careful oral examination and full-mouth radiographs to identify both existing infection and potential sources of infection. In addition to cleaning of the teeth, indicated periodontal or extraction procedures, and instruction in oral hygiene, mouth rinses may be prescribed to prevent or control microorganisms associated with oral infection and reduce the probability and severity of mucositis and stomatitis and systemic infection. Other patient management goals for leukemia and lymphoma patients are to relieve symptoms and encourage adequate nutrition and hydration. Topical anesthetics, saline rinses, and other strategies, which may be prescribed by both physicians and dentists, may provide some relief of symptoms.
Because bacteria in the mouth may enter the bloodstream through oral ulcers and areas of mouth tissue breakdown, the goals of dental care for patients who have developed treatment-related stomatitis or mucositis include reducing the level of organisms in the mouth and preventing any breach of its epithelial lining that provides an avenue for infection. Histopathological or microbiological analysis to identify the infectious organisms involved may be useful in guiding antimicrobial therapy (Dreizen et al., 1983; Ostchega, 1980; Schimpff 1990).
Effectiveness of Dental Care in Improving Health Outcomes for Leukemia and Lymphoma Patients
No large, multicenter, randomized clinical trials have assessed the effectiveness of dental interventions to prevent or manage oral or systemic complications of chemotherapy for leukemia or lymphoma patients. A few controlled studies suggest that dental care (examination, periodontal treatment, and extractions for unrestorable teeth) for leukemia patients prior to chemotherapy may prevent or reduce subsequent episodes of septicemia and prevent or reduce the severity of common oral complications of chemotherapy that are associated with the prior burden of oral disease (Borowski, 1994; Levy-Polack et al., 1996; Peterson, 1982, 1990). Unfortunately, these studies involve few elderly patients.
A recent study with no control group that tested the effect of not treating chronic dental disease prior to chemotherapy concluded that treatment for chronic problems could be safely postponed with little effect on the subsequent risk of acute dental disease (Toljanic et al., 1999). It also concluded that a prechemotherapy oral examination was still needed to identify acute dental disease for treatment to prevent local exacerbations or systemic spread of infection
These few studies of prechemotherapy dental treatment have involved mostly or entirely leukemia patients, who tend to receive aggressive, combination chemotherapy that is associated with more severe immunosuppression. Ad-
ditional studies would be needed to determine the effects of prechemotherapy dental treatment on lymphoma (and other cancer) patients.
For prevention and treatment of oral infections, research has produced inconsistent findings about the effectiveness of different mouth rinses, notably chlorhexidine (a standard broad-spectrum antimicrobial that can bind to oral surface tissue but is not readily absorbed in the gastrointestinal tract) (e.g., see Epstein et al., 1992; Ferretti et al., 1988; Wahlin, 1989; Weisdorf et al., 1989; as discussed in Appendix C). Some other prescription drugs have also been studied for their effectiveness in the management of specific oral infections, but the committee did not further review prescription rinses and other outpatient drugs that are not now covered by Medicare.
SOLID ORGAN TRANSPLANTS
Burden of Disease
As briefly reviewed in Chapter 4 and Appendix D, many medical conditions can lead to the failure of major organs including the kidney, heart, liver and lung, and thus to consideration for transplantation. Immunosuppressive drugs are essential to reduce the chance of graft rejection in transplant recipients. Renal failure accounts for the great majority of transplants among Medicare beneficiaries.11 Many younger patients receiving other kinds of transplants qualify for Medicare at some point before or after the transplant due to disability. As described further in Chapter 5, more than 20,000 solid organ transplantations were performed in the United States in 1998 (UNOS, 1999a). According to regional data from 1997, more than 12,000 kidney transplants and several hundred heart and liver transplants were performed in Medicare-eligible patients age 65 and over (UNOS, 1999a; see Table 5 of Appendix C).
Oral Health Problems and Organ Transplantation
The primary oral health issues for recipients of solid organ transplants are related to the drug therapy they must take to control graft rejection. This immunosuppressive therapy limits their ability to fight infections. Posttransplant infections can lead to very serious consequences including hospitalization, loss of the grafted organ, return to dialysis, retransplantation, or death. Thus, as people are evaluated before, during, and after transplantation, a central goal is to identify and eliminate existing infections and obvious potential sources of infection. These include infections associated with the mouth, although there is no direct evidence of serious infections linked specifically to oral sources (see Appendix
C). Some transplant centers will not operate on a patient with an active oral infection.
People with suppressed immunological function are vulnerable to several kinds of bacterial, viral, and fungal infectious agents that may be harbored in the mouth and elsewhere in the body. Many organisms that do not normally create problems in healthy people are a threat to those with suppressed immune systems. For example, a transient, typically asymptomatic bacteremia often occurs following various dental treatments, especially those involving the gums. This condition is of no concern in the patient with a fully functioning immune system but may be dangerous in the severely immunosuppressed transplant recipient.
Cytomegalovirus (CMV) and herpes simplex virus (HSV) are common in humans (found in 40–80 percent of adults who are asymptomatic), and most transplant patients test positive for CMV (Berry et al., 1988; Rubin and Tolkoff-Rubin, 1988; reviewed in Appendix C). In transplant patients the viruses are frequently found in oral ulcers during the six months immediately following surgery, but they may occur elsewhere along the gastrointestinal tract.
Some of the immunosuppressive drugs so necessary to the transplant recipient have the unfortunate side effect of gingival overgrowth. Gingival overgrowth, a condition of gum enlargement, makes removal of bacteria through brushing and flossing of teeth more difficult. It can also be disfiguring and can interfere with eating and maintenance of adequate nutrition. CMV has been found in areas of gingival overgrowth.
In addition to the risks associated with posttransplant immunosuppressive therapy, certain common causes of organ failure (or their treatment) may put people at higher risk of oral problems. Diabetes is a common cause of renal failure and is associated with periodontal disease in its own right, and untreated oral disease may complicate effective diabetic management (Grossi and Genco, 1998). Hypertension is another common cause of organ failure, and its treatment with certain calcium channel blockers is associated with gingival overgrowth (in addition to any overgrowth caused by certain immunosuppressants).
The overall rate of periodontal disease, caries, and abscesses is not documented specifically for transplant candidates, but it is reasonable to expect that these conditions are at least as common in these populations as in adults generally. In the most recent National Health and Nutrition Examination Survey, approximately 20–30 percent of older adults were found to have moderate periodontal disease (which would not necessarily indicate active disease that poses a risk of self-infection), and serious disease was found in approximately 5 percent (with higher percentages for men and lower for women) (Albandar and Kingman, 1999). Although some studies have linked posttransplant infections to organisms ubiquitous in the oral cavity (e.g., lactobacillus, as well as several fungi) (Suresh et al., 1996; reviewed in Appendix C), the rate of posttransplant infection associated with oral sources specifically is not documented. Similarly, the extent to which oral problems associated with diabetes or the use of certain
calcium channel blockers contributes to poor outcomes for transplant patients is not known.
Dental Care for Patients Before or After Organ Transplantation
As noted above, the standard of care for transplant candidates includes the prevention and elimination of oral infection. Such care involves an oral examination that includes visual and tactile inspection of the mouth and is usually accompanied by x-rays. An oral examination also typically includes instruction in personal oral hygiene (brushing, flossing, use of antiseptic mouth rinses) intended to help patients avoid posttransplant gingivitis and other oral problems. At least one controlled study has found less gingivitis, plaque, or gingival overgrowth in transplant patients who received hygiene instruction compared to those who did not (Somacarrera et al., 1996; reviewed in Appendix C).
Dental prophylaxis (not currently covered by Medicare for any patient group) removes plaque, a tenacious film of germs that adheres to the teeth, and calculus (tartar) that can build up to cause periodontal disease. When periodontal disease is diagnosed, treatment—which can be limited or quite extensive—removes hardened plaque, calculus, and infected tissue under the gum and smoothes the root surfaces of teeth so that damaged tissue can heal and reattach to the teeth. If damage to teeth or gums is serious enough, teeth may have to be extracted. If the base of the tooth root is infected, a root canal may be performed.
As noted earlier, HCFA has ruled that an inpatient oral examination prior to renal transplant is covered but the ruling does not mention beneficiaries receiving other kinds of transplants. Some carriers, however, provide for such coverage in their local medical policies. Dental care prescribed following an oral examination is not covered. In addition to services normally provided by dentists, both dentists and physicians may manage oral infections with drugs. These drugs are not covered by Medicare if provided on an outpatient basis.
Effectiveness of Dental Care in Improving Health Outcomes for Organ Transplant Recipients
As described in Appendix C, no direct evidence is available regarding the effect on survival of prevention, early detection, or treatment of oral health problems in transplant patients. As noted above, people with oral infections may be ruled out for transplants at some transplant centers, but the committee found no research comparing patient outcomes in centers with and without this policy. It also found no studies comparing transplant patients who had received periodic oral prophylactic services with those who had not. For those with identified oral infections, no trials have compared different treatment strategies. One controlled
study, as mentioned above, did suggest that oral hygiene instruction reduced subsequent oral problems, but the study did not examine more important outcomes such as acute or chronic graft rejection.
More generally, controlled studies have not evaluated the overall strategy of identifying and eliminating infection prior to transplantation. The approach is based on biological principles, experience, and concern about the significant mortality and morbidity risks that infection poses to transplant recipients taking immunosuppressive drugs.
HEART VALVE REPAIR OR REPLACEMENT
Burden of Disease
Heart valve disease may arise congenitally or develop later in life. The diseased valve is functionally impaired so that it cannot open properly, close sharply, or both. This causes irregularities in blood flow through the heart, which are often first heard with a stethoscope. Some valve disease can be treated with medication, but other cases require surgical repair or even replacement with synthetic or transplanted tissue.
Those with valve disease are at risk of endocarditis, a serious and often fatal inflammation of the tissue lining the chambers of the heart. Any sort of uneven or rough surface, which may be present with a diseased, abnormal, repaired, or replaced valve, creates a niche where bacteria can lodge and multiply to cause endocarditis. Such infections can be difficult and costly to treat. Those at high or moderate risk of endocarditis include people with a prosthetic heart valve or past episodes of endocarditis and those with certain other cardiac problems including a number of congenital cardiac conditions (AHA, 1999). Although mitral valve prolapse has frequently been cited as a risk factor, only those meeting certain criteria (e.g., mitral regurgitation demonstrated by Doppler examination) appear to be at higher-than-normal risk for endocarditis.
Data on the incidence and prevalence of heart conditions are less extensive than data for common cancers. Population-based studies in limited geographic areas in the United States have reported an overall incidence of 1.7 to 4.0 cases per 100,000 (Berlin et al., 1995). According to Medicare records, the number of Medicare-paid hospital stays involving heart valve disease has been increasing (from 42,700 in 1990 to 58,800 in 1995), and the number of stays for which endocarditis was specifically reported has also increased (from 3,900 in 1990 to 4,950 in 1995) (HCFA data discussed in Appendix C). The American Heart Association (AHA, 1999) reported more than 16,000 hospital discharges for bacterial endocarditis in all age groups in 1995. In 1996, valvular heart disease was listed as the cause of death in more than 17,000 cases in the population overall and was mentioned as a factor in almost 36,000. In 1995, the latest year for which information was available, bacterial endocarditis was specified in 2,100
reports of death in the population overall (AHA, 1999). Among other heart conditions, diseases of the arteries and congestive heart failure each accounted for more than 43,000 deaths in 1995.
Many studies of risk factors and other aspects of endocarditis are based on data from major medical centers that treat many patients referred from other communities. A study undertaken by investigators at the Mayo Clinic that compared incidence cases for Olmstead County, Minnesota, with referral cases seen at the clinic reported that age was a much more significant factor in the community cohort than in the hospital cohort. For the former, the incidence rate was nearly 9 times higher for those age 65 and over than for younger age groups (Steckelberg et al., 1990). The population-based incidence rate for those age 70–79 was 18 per 100,000; it was 40 per 100,000 for those age 80 or older.
Oral Health Problems and Heart Valve Disease
The oral cavity in general, and common oral infections in particular, can provide sources of organisms that may lead to heart valve infection, which in turn can lead to endocarditis. Clinicians have observed an association between oral disease and endocarditis, and Appendix C describes a causal model offering a possible explanation (after Drangsholt, 1998).
The oral cavity harbors a lot of bacteria, most commonly in the form of plaque, but also associated with gingivitis, periodontitis, and periapical disease (infection around the base of the tooth root). Oral flora, particularly streptococcus, are implicated in approximately 40 percent of cases of infective endocarditis (Roberts, 1999; Strom et al., 1998; van der Meer et al., 1992a). Bacteremia can arise from dental procedures but also from such routine activities as tooth brushing and chewing, especially if extensive oral infection and inflammation are present. Patients with dentures may develop bacteremias associated with poorly fitting dentures.
Although dental procedures for hygiene, restoration, or extraction of diseased teeth can cause breaks in the epithelium lining the mouth that allow bacteria to spill into the bloodstream causing bacteremia, most cases of orally related endocarditis are not attributed to dental procedures (Bonow et al., 1998; Pallasch and Slots, 1996). The burden of oral disease of itself is a concern for the patient at high risk of endocarditis (Strom, 1998; van der Meer, 1992b).
Dental Care for Patients Undergoing Surgery for Heart Valve Disease
Standard clinical practice is to eliminate as many potential sources of oral infection as possible before a patient undergoes a surgical procedure to repair or replace a defective heart valve. This typically involves an oral examination and x-rays, thorough cleaning, and treatment for any gingival, periodontal, or peri-
apical disease identified. None of these services are covered by Medicare. Standard practice also includes prophylactic use of antibiotics prior to bacteremia-producing dental procedures (Bonow et al., 1998).
Effectiveness of Dental Care in Promoting Better Health Outcomes for Patients with Heart Valve Disease
The committee and the authors of the background paper were unable to locate any published controlled studies on the effectiveness of dental care prior to heart valve repair or replacement. Further, they found no such studies documenting the effectiveness of antibiotic prophylaxis during dental or other bacteremia-inducing procedures involving people at risk of endocarditis. A randomized controlled trial, especially one assessing treatment and outcomes in elderly patients, would be difficult to organize in part because the main outcome of concern—infective endocarditis—is relatively uncommon. Less rigorous comparative studies might be possible for some topics, for example, the value of a preoperative dental examination before cardiac surgery.
The committee and the background paper authors managed to find one 1997 paper describing the dental health of 156 patients with valve disease requiring a prosthetic valve implant (Terezhalmy et al., 1997). Nearly all of the patients had some level of significant periodontal disease, suggesting that they would be at increased risk if untreated prior to surgery. This study did not include a comparison group and provided no information on the patients regarding either their dental care prior to surgery or the prevalence of endocarditis subsequent to surgery.
Bacteremia can cause local pockets of infection wherever the bacteria get caught and accumulate—for example, on the irregular surface of a diseased or surgically repaired heart valve. One case control study found that patients who have undergone valve surgery or have other valve abnormalities remain indefinitely at increased risk of endocarditis (Drangsholt, 1998).
In summary, the committee was unable to find any published clinical trial data bearing on whether dental care prior to heart valve repair or replacement affects the outcome of valve surgery. The explanatory model addressing the observed association between oral disease and endocarditis is intellectually attractive but not supported by direct evidence at this time.
ESTIMATED COSTS TO MEDICARE OF EXTENDING COVERAGE
The committee considered the likely costs of extending limited Medicare coverage for dental services provided in conjunction with surgery, chemotherapy, radiation, or pharmacological treatment for beneficiaries with the serious medical conditions reviewed above. Box 4-1 summarizes the assumptions and data on
which the estimates are based. As explained in Chapter 2, the cost estimation approach follows the generic practices (e.g., not discounting estimates to present value) used by the Congressional Budget Office (CBO) in making estimates for Congress. A more detailed presentation of the committee’s cost estimates and the associated assumptions and data sources appears in Appendix E, which was prepared in consultation with the committee and background paper authors.
|
BOX 4–1 Summary of Estimated Costs to Medicare for “Medically Necessary Dental Care” Associated with Certain Medical Conditions Coverage Model Assumptions
Cost Estimate Assumptions for Years 2000–2004 (see also Appendix E)
|
|||||||||||||||||||||||||||||||||||
|
Cost Estimate Assumptions for Years 2000–2004
Data Sources
Estimated Costs (in millions) to MEDICARE, 2000–2004
|
The committee’s estimates of Medicare costs are based on a series of assumptions, some of which have supporting evidence or data but others of which are best guesses based on committee judgment in the absence of such information. The estimates are intended to suggest the order of magnitude of the costs to Medicare of extending coverage, but they could considerably higher or lower than what Medicare might actually spend were coverage policies changed. The tables in Appendix E allow readers to vary some of the committee’s assumptions and calculate alternative estimates
The total net cost to Medicare of covering services for the five conditions examined for the five-year period from 2000 to 2004 is estimated to be $155.8
million. This estimate takes into account $5.6 in offsetting savings from reduced medical care costs and $51.9 million in offsets related to increases in the Medicare premium that would result from increased Medicare spending for the elderly.
The main procedures likely to be needed by patients with the five medical conditions are similar: examination and diagnostic radiographs; restorations where possible; extractions where restoration is not an option; and treatment of periodontal, gingival, and periapical disease. The overall cost per patient is driven primarily by the number of visits that each patient would be likely to need. The average number of dental visits per patient is based on the judgment of committee members and background paper authors. Except for head and neck cancer patients undergoing radiation therapy, visits were assumed only for patients with teeth. Head and neck cancer patients are typically examined to identify any retained tooth roots, impacted teeth not detected by visual inspection, and any residual bone pathology warranting treatment prior to radiation therapy. The proportion of older people with no teeth appears to have been declining (Bloom et al., 1992; Marcus et al., 1996; MMWR, 1999) and could reach lower levels for the period 2000–2004. This would mean more dental examinations and higher costs.
The number of Medicare beneficiaries likely to experience one of the conditions mentioned was estimated using Medicare or Surveillance Epidemiology and End-Results (SEER) incidence data for the conditions applied separately to the aged and disabled Medicare Part B beneficiaries. The cost estimates assume coverage only for the year of the transplant procedure or other surgery, radiation therapy, or chemotherapy, although some patients (e.g., transplant recipients taking immunosuppressive drugs) will be at risk indefinitely. Longer periods of coverage would raise the estimates.
Payments were calculated on a per-visit basis, based on 1987 data from the National Medical Expenditure Survey. Figures were adjusted to reflect the increased intensity of service likely for the treatment population compared to the general population. The figures were also adjusted for inflation since 1987 and for expected Medicare discounts, copayments, and Medicare premium offsets (see Appendix E). The cost per visit was then multiplied by the expected average number of visits per patient.
Based on the research described earlier in this chapter and in Appendix C, offsetting savings due to the dental services (as opposed to increases in Medicare premiums) were applied only for head and neck cancer. As discussed in Appendix E, previous HCFA and CBO estimates of the cost to Medicare of extending coverage of medically necessary dental treatments have included a broader range of conditions and services than the committee’s estimates.
STATEMENTS OF OTHERS ON “MEDICALLY NECESSARY DENTAL SERVICES”
The U.S. Preventive Services Task Force did not examine the narrowly focused kinds of services examined in this chapter. It has examined counseling to prevent dental and periodontal disease and stated that “counseling patients to visit a dental care provider on a regular basis, floss daily, brush their teeth daily with a fluoride containing toothpaste, and appropriately use fluoride for caries prevention and chemotherapeutic mouth rinses for plaque prevention is recommended based on evidence for risk reduction from these interventions” (USPSTF, 1996, p. 711).12 It also stated that “while examining the oral cavity, clinicians should be alert for obvious signs of oral disease” (p. 711), but it concluded that there was “insufficient evidence to recommend for or against routine screening of asymptomatic persons for oral cancer by primary care clinicians.” (p. 175).
The House of Delegates of the American Dental Association (ADA) has defined “medically necessary dental care” to include care to control or eliminate infection, pain, and disease and has resolved that the ADA “make every effort on behalf of patients to see that the language specifying treatment coverage in health plans be clarified so that medical necessary adjunctive care, essential to the successful treatment of a medical condition being treated by a multidisciplinary health care team, is available to the patient” (Conway, 1995, p. 188). The ADA endorsed the AHA recommendations related to endocarditis (see below). It also recommended more research on specific heart conditions and dental procedures, following the publication of a recent study in Annals of Internal Medicine (Strom et al., 1998) that concluded that dental treatment did not appear linked to infective endocarditis and that antibiotic prophylaxis should be reconsidered. An accompanying editorial encouraged the AHA, the Infectious Diseases Society of America, and others to rise to the challenge of crafting appropriate new recommendations (Durack, 1998).
To prevent bacterial endocarditis, the American Heart Association has recommended prophylactic regimens for high- and moderate-risk patients undergoing dental, oral, respiratory tract, or esophageal procedures (Bonow et al., 1998). The recommendations related to dental practice were, as noted above, endorsed by the ADA’s Council on Scientific Affairs. The recommendations were based on retrospective studies, animal studies, and in vitro susceptibility data. The AHA noted, however, that no randomized and carefully controlled human trials had established the effectiveness of antibiotic prophylaxis in protecting against endo-
carditis in patients with underlying structural heart disease. It also noted that most cases of endocarditis are not attributed to invasive procedures.
In addition to recommendations relating to antibiotic prophylaxis, the AHA has recommended that those at risk for bacterial endocarditis should establish and maintain the best possible oral health to reduce the potential for bacteremia. They should seek regular professional care and undertake thorough self-care, including brushing of teeth, use of dental floss, and other plaque-removal techniques. For patients undergoing cardiac surgery (e.g., heart valve repair), the AHA recommended a careful preoperative evaluation and the completion of required dental treatment before cardiac surgery whenever possible to reduce the potential for late postoperative endocarditis.
The American Society of Transplantation (formerly the American Society of Transplant Physicians) developed guidelines for evaluating renal transplant candidates. These include recommendations to identify and treat overt infections and assess patients for possible occult infections including dental caries (Kasiske et al., 1995).
The National Institutes of Health held a Consensus Development Conference on Oral Complications of Cancer Therapies: Diagnosis, Prevention, and Treatment in 1989 (NIH, 1989). Conclusions included that (1) all cancer patients should have an oral examination before initiation of cancer therapy; (2) treatment of preexisting oral disease is essential to minimize oral complications in all cancer patients; (3) prophylactic acyclovir is beneficial in selected patients to prevent HIV reactivation. (4) precise diagnosis of mucosal lesions and specific treatment of fungal, viral, and bacterial infections are essential; (5) mucosal ulcerations should alert the cancer team to the risk of systemic infection; (6) the best current treatments for chronic xerostomia include fluorides, attention to oral hygiene, and sialagogues (agents that promote the production of saliva); (7) osteoradionecrosis can be prevented and, when present, is best managed with hyperbaric oxygen alone or with surgery; and (8) in the pediatric population, it is important to recognize the long-term consequences of radiation therapy, which include dental and developmental abnormalities and secondary malignancies. Given the limited research base, the conference also recommended that studies of oral complications be incorporated into ongoing and future cooperative clinical oncology group protocols.
In 1999, the National Institute of Dental and Craniofacial Research (NIDCR), one of the National Institutes of Health, launched a health awareness campaign: Oral Health, Cancer Care, and You: Fitting the Pieces Together. Partners in this campaign include the National Institute of Nursing Research (NINR), the Centers for Disease Control and Prevention (CDC), the National Cancer Institute (NCI), and the Friends of the NIDCR. Materials are available through the National Oral Health Information Clearinghouse, an information dissemination service of NIDCR. The campaign promotes medically necessary oral care prior to, during, and after cancer treatment to prevent or reduce the
incidence and severity of oral complications, enhancing both patient survival and quality of life (NIDCR, 1999).
COMMITTEE FINDINGS AND CONCLUSIONS
The committee utilized the extensive review of literature provided by the panel of background paper authors, four experts in dental research. The committee also benefited from a two-day public workshop featuring many guest speakers and attended by members of the public with expertise in dental research and hospital-based dental practice (see Appendix A). Unfortunately, little systematic research is available to assess the prevention and management of the oral-medical problems examined in this chapter.13 Standards of practice for these problems have been developed, often on the basis of plausible biological reasoning but without much evidence from well-controlled clinical trials. The committee’s findings, as discussed in this chapter, are summarized briefly below. Its conclusions about Medicare coverage follow.
Findings
Cancers of the Head and Neck
Disease Burden. The committee found that cancers of the head and neck are relatively common, accounting for approximately 3.3 percent of the total estimated new cancers for 1999 and about 4 percent of overall cancer prevalence. Of the estimated 40,000 new cases reported each year, almost half are diagnosed in patients age 65 or older. Treatment is associated with serious oral health risks including damage to the salivary glands, radiation-related caries, and osteoradionecrosis.
Dental Care Effectiveness. The committee found that standard clinical practice for head and neck cancer patients anticipating radiation to the jaw includes reliable identification of active and potential oral health problems for which effective management exists. Evidence is limited but supports the effectiveness of tooth-preserving regimens—especially the role of topical fluoride applications—for head and neck cancer patients prior to and after radiation therapy. Evidence suggests the tooth-preserving approach (not covered by Medicare) is associated with lower rates of ORN and, thus, overall better patient outcomes than the older strategy that emphasized tooth extractions (covered by Medicare).
Benefits Versus Harms. The committee found evidence suggesting that tooth-preserving therapies are preferable to full mouth extraction not only in limiting ORN but also in avoiding some of the functional and quality of life problems associated with tooth loss. Not all patients, however, are able to adhere to the rigorous hygiene and fluoride treatment programs required by this strategy. To the extent that such patients can be identified prior to therapy, these individuals may benefit more from full mouth extraction to avoid the greater risk of extractions after radiation. Both classes of patients, however, benefit from oral examination and assessment. The committee found no types of patients that would be more likely to suffer harm from oral examination and appropriate treatment compared to no oral care.
Leukemia
Disease Burden. The committee found that leukemia is a relatively common form of cancer, with approximately 30,000 new cases reported annually. The incidence rate in the population age 65 or older is much greater than that in the under age 65 group, and survival rates are lower than for younger people. Leukemia patients, who are often immunosuppressed from their disease, are especially susceptible to septicemia, which is a leading cause of death. Oral health problems are common from both the disease and its treatment. Chemotherapy can cause mucositis, which can lead to serious secondary and systemic infections. Another treatment, bone marrow transplantation, also can result in oral health problems such as xerostomia, oral lesions, and oral infections, which may contribute to systemic infection.
Dental Care Effectiveness. The committee found that standard clinical practice includes reliable identification of active and potential oral health problems for which effective dental and medical management exists. The committee found clinical experience to be suggestive that dental cleaning and restoration or extraction services are effective in reducing oral infection in leukemia patients as in other patients. Limited direct evidence from small studies suggests that dental treatments for leukemia patients prior to chemotherapy that is focused on the elimination of acute oral infection and prevention of bacteremia may (a) prevent or reduce subsequent episodes of septicemia and (b) prevent or reduce the severity of the common oral complications of chemotherapy associated with a prior burden of oral disease.
Benefits Versus Harms. In addition to the scarcity of direct evidence about the systemic benefits of dental treatment, patient perspectives on possible benefits and harms of dental treatments related to the overall management of leukemia have not been explicitly assessed. To the extent that dental care helps to eliminate oral sources of infection and reduce patient discomfort and dys-
function, the committee finds it biologically plausible that dental care promotes a better overall health outcome. An experienced oncologist is in the best position to judge whether a particular leukemia patient should be referred to a dentist for further examination and treatment, taking into account the risk of any delay in the initiation of chemotherapy.
Lymphoma
Disease Burden. Lymphoma is more common than cancers of the head and neck or leukemia, with approximately 64,000 new cases of lymphoma reported in a year, approximately 57,000 of which are non-Hodgkin’s lymphoma. The incidence rate in the population age 65 or older is almost eight times higher for non-Hodgkin’s lymphoma and is somewhat higher for Hodgkin’s disease, compared to the population under age 65. Survival rates are lower in older people. Both non-Hodgkin’s lymphoma and Hodgkin’s disease are treated with radiation and often chemotherapy as well (especially Hodgkin’s disease), so the treatment can result in increased oral health problems such as mucositis and dental caries due to xerostomia.
Dental Care Effectiveness. The committee found that standard clinical practice includes reliable identification of active and potential oral health problems for which effective dental and medical management exists. The committee located no published clinical trials providing direct evidence that dental care improves health outcomes of treatment for non-Hodgkin’s lymphoma or Hodgkin’s disease or prevents or reduces the severity of treatment-related oral problems. The committee found clinical experience to be suggestive that reduction of oral sources of infection by extraction of abscessed teeth and periodontal cleaning prior to chemotherapy may prevent some septicemias in patients with non-Hodgkin’s lymphoma or Hodgkin’s disease.
Benefits Versus Harms. In addition to the lack of direct evidence about health benefits, patient perspectives on possible benefits and harms of dental treatments related to the overall management of lymphoma patients have not been explicitly assessed. To the extent that dental care helps to reduce oral infection and patient discomfort, the committee finds it biologically plausible that dental care promotes a better overall health outcome.
Organ Transplantation
Disease Burden. The committee found that organ transplants occur less frequently than the cancers mentioned earlier, but they have become much more common in the last 15 years, with about 20,000 organ transplants performed in the United States annually. All organ transplant recipients require some level of
immunosuppressive therapy, especially at the time of and just after the transplant operation, and they are therefore more susceptible to infection. The committee found no data, however, documenting infections from specifically oral sources in immunosuppressed transplant patients. Regarding the treatment following a transplant, the committee noted that gingival overgrowth is a well-known adverse effect of some immunosuppressive drugs, although it is less severe with newer products and must be managed by a physician or dentist along with other adverse drug effects.
Dental Care Effectiveness. The committee found that the standard clinical practice of preparing a patient to receive a transplant includes reliable identification of active and potential oral health problems for which effective dental and medical treatments exist. The committee located no published clinical trials providing direct evidence that dental care improves health outcomes for transplant recipients. Clinical experience suggests that dental cleaning and restoration or extraction services are effective in reducing oral infection in transplant candidates, as in other patients. In general, however, controlled studies have not evaluated the overall strategy of identifying and eliminating infection prior to transplantation. The approach is based on biological principles and experience.
Benefits Versus Harms. In addition to lack of direct evidence of systemic benefits, patient perspectives on possible benefits and harms of dental treatments related to the overall management of transplant surgery and maintenance have not been explicitly assessed. To the extent that it helps to reduce oral infection, the committee finds it biologically plausible that dental care promotes a better overall health outcome.
Heart Valve Repair and Replacement
Disease Burden. The committee found that the number of hospital stays involving heart disease paid for by Medicare has been increasing and had reached 58,800 by 1995. Endocarditis was specifically reported in 4,950 of these cases. The committee found that valvular disease causes a substantial disease burden in the Medicare population and that endocarditis, although relatively uncommon, is associated with significant mortality and morbidity. Clinicians have observed an association between oral disease (gingivitis, periodontitis, periapical disease) and endocarditis.
Dental Care Effectiveness. The committee found that the standard clinical practice for preparing a patient for valve surgery includes reliable identification of active and potential oral health problems for which dental and medical treatments exist. Clinical experience is suggestive that cleaning and restoration or extraction services are effective in reducing infection in patients preparing to
undergo valve surgery, as in other patients. The committee located no published clinical trials providing evidence that dental care improves the overall health outcome of patients undergoing valve surgery.
In addition, the committee found no controlled studies demonstrating that dental procedures increase the incidence of endocarditis by introducing oral bacteria into the bloodstream, although the committee did find the model to be biologically plausible. Poor oral health may, however, produce bacteremia in the course of routine activities such as tooth brushing or chewing.
Benefits Versus Harms. In addition to the lack of direct evidence of systemic benefit or harm, patient perspectives on possible benefits and harms of dental treatments related to the overall management of patients undergoing valve surgery have not been explicitly assessed. To the extent that dental care helps to reduce oral infection, the committee finds it biologically plausible that dental care promotes a better overall health outcome.
Possible Directions for Future Research
The committee identified several areas in which further research would be helpful, although it did not attempt to set priorities. In general, it was disappointed to find so little evidence documenting the effectiveness of accepted clinical practices in the oral health care of patients with leukemias, lymphomas, cardiac valvular disease planned for valve replacement or repair, and organ transplants. Lack of evidence is not itself evidence that the current standards of care are inappropriate, but it does point to the desirability of studies that could help assess the benefits and harms of that care.14
Widespread acceptance of such standards, coupled with the biological plausibility of the clinical protocols for identifying and eliminating infections, may however make controlled studies difficult to design and carry out. Nonetheless, the recent retrospective case-control study of antibiotic prophylaxis to prevent endocarditis in patients with various heart conditions suggests that some trials could in fact be devised to clarify practice within standards of appropriate scientific and ethical rigor (Strom et al., 1998). Given the risk of infection and grave outcomes for such patients, the committee encourages efforts to devise and implement such studies. For example, a prospective study designed to control for differences in patient populations and other factors could compare hospitals that
include a dental examination and indicated treatment as part of standard preoperative care for cardiac surgery patients with those that rely on physicians to identify patients with dental problems needing further evaluation and treatment. Controlled research is also feasible to test the effectiveness of different dental care protocols for leukemia and lymphoma patients prior to or during chemotherapy.
Research on education and other strategies to encourage patient adherence to self-care regimens is important in dental care as in other areas. For example, even at the risk of tooth loss and bone damage, some patients who have undergone radiation therapy for cancers of the head and neck do not follow the recommended but very rigorous self-care routines, which may result not only in worse health outcomes but also in higher Medicare costs.
The committee was interested in emerging reports linking improved oral health to improved health outcomes for people with systemic conditions not evaluated in this study. A primary example is diabetic patients for whom treatment of periodontal infection is associated with better blood glucose control (Grossi et al., 1997; Grossi and Genco, 1998; Westfelt et al., 1996). Given the prevalence of diabetes and its significance as a problem among older adults, further study of the implications of oral health status and the effect of dental care should be encouraged.
In addition, the link between oral health and coronary artery disease and stroke remains an important area for further research (Beck et al., 1996). With new research suggesting a relationship between oral health status and pneumonia (an important cause of mortality and morbidity in older people), further investigation of this link and of the effectiveness of dental care and oral hygiene in preventing pneumonia also is warranted (Limeback, 1998; Scannapieco, 1999; Yonayama et al., 1999).
Finally, although AIDS patients constitute a relatively small proportion of Medicare beneficiaries, the burden of suffering associated with oral problems is significant. The contribution of dental care to better health status and quality of life has so far been little studied (Capilouto et al., 1991; Migliorati et al., 1994). The results of new research on the relationships between oral and systemic diseases for these and other medical conditions not studied in this report could inform both clinical practice and future coverage policies.
Conclusions
The committee concluded that the direct evidence to support coverage for “medically necessary dental services” varies depending on the medical condition to which dental services are related. Such evidence is, in general, lacking rather than negative or ambiguous. More and better research is needed on the systemic implications of dental problems and dental interventions to guide clinicians in
caring for people with serious health problems and policymakers in supporting financial access to effective care.
Although no large randomized clinical trials have investigated outcomes of dental care for head and neck cancer patients receiving radiation therapy to the jaws, the committee concluded that small retrospective studies of patients treated before and after implementation of tooth-preserving protocols provide limited direct evidence that the replacement of tooth extraction protocols with tooth-preserving protocols prior to radiation can reduce xerostomia-induced radiation caries and associated postradiation tooth extractions that place patients at high risk for osteoradionecrosis. Other retrospective analyses show higher rates of ORN for patients with inadequate dental care and preradiation extractions. HCFA has approved coverage of extractions but not of tooth-preserving strategies. Given this limited evidence, the severe consequences of radiation-induced osteoradionecrosis, and Medicare’s investment in treating patients with head and neck cancer, it is reasonable for Medicare to cover both tooth-preserving care and extractions, which may be medically appropriate for certain patients. Patients should be referred for dental examinations by their oncologist.
The committee also concluded that weak direct evidence suggests that the provision of dental care targeted to prevent or eliminate acute oral infection for leukemia patients prior to chemotherapy can prevent or reduce subsequent episodes of septicemia and prevent or reduce the oral complications of treatment. Given this limited evidence, the severe consequences of septicemia and other complications of chemotherapy, and Medicare’s investment in treating leukemia patients, it is reasonable for Medicare to cover a dental examination, cleaning of teeth, and treatment of acute infections of the teeth or gums for a leukemia patient prior to chemotherapy. Again, patients would be referred to a dentist by their physician.
The committee concluded that the evidence is insufficient to support positive or negative conclusions about dental services for patients with lymphoma, organ transplants, and heart valve repair or replacement. Direct evidence through controlled clinical trials is lacking rather than negative or ambiguous. Indirect evidence and biological plausibility are suggestive that health outcomes may be improved by the elimination of oral sources of infection that may cause septicemia in the immunosuppressed lymphoma or organ transplant patient or endocarditis in the patient with a diseased, abnormal, or surgically repaired or replaced heart valve. Dental services for persons with these life-threatening illnesses do not differ from currently covered medical services that are considered prudent care but for which no controlled clinical studies exist. Widely accepted clinical protocols for identifying and eliminating all infections and potential sources of infection before transplantation are based largely on biological principles, animal studies, and clinical experience, not controlled tri-
als. The committee’s conclusion does not negate the value of clinical judgment in selecting appropriate individual patients for such interventions.
Although the evidence base for “medically necessary dental services” is mixed and frequently based on weak research designs, the committee is concerned about interpretations of the current law that could preclude HCFA from approving further coverage exceptions for dental services to identify and eliminate oral infections or potential sources of infection for immunocompromised high-risk patients. As noted earlier, widely accepted clinical protocols for identifying and eliminating all infections and potential sources of infection before transplantation are based on biological principles and clinical experience, not controlled trials. The committee is also concerned about legislative proposals requiring that “medically necessary dental services” produce savings that exceed the direct costs of care. As described in Chapter 5, even elimination of the three-year limit on coverage of immunosuppressive drugs—drugs that clearly improve outcomes for transplant recipients—is unlikely to meet this standard.
Given the scientific and therapeutic advances since the creation of Medicare in 1965 and the concerns about current coverage interpretations, the committee concludes that it is reasonable for Congress to update the statutory language relating to coverage of dental services so that it would clearly cover dental care that is effective in preventing or reducing oral and systemic complications associated with serious medical conditions and their treatment. Specifically, the committee suggests that Congress should direct the Health Care Financing Administration (with assistance as appropriate from the Agency for Health Care Policy and Research and the National Institutes of Health) to develop recommendations—on a condition-by-condition basis—for coverage of dental services needed in conjunction with surgery, chemotherapy, radiation, or pharmacological treatment for a life-threatening medical condition. The phrase “in conjunction with” would allow HCFA to limit the window of coverage to a specified period before or after surgery or other treatment but would not require that the services be provided at the same time as or as an immediate part of a surgical or other procedure. This minimal revision in the 1965 exclusion of coverage for dental services would not alter Medicare’s basic focus on treatment of acute illness or injury.
If Medicare were to cover “medically necessary dental services” for some or all of the medical conditions reported here, it is uncertain how many beneficiaries in each category would avail themselves of this benefit. The referral for “medically necessary dental care” would likely come from the treating physician at the time of diagnosis or planning of the medical therapy. The patient’s physician would in this way serve as a gatekeeper for this benefit, especially among patients who are not under regular dental care. In addition, physicians would continue to manage many oral problems themselves, for example, by prescribing antibiotics and therapeutic rinses.




































