5
Immunosuppressive Drugs for Transplant Patients
Successful transplantation of human organs is one of the most dramatic achievements of modern medicine. The first successful kidney transplant was performed in 1954 between identical twins, and the first transplants of other organs such as pancreas, liver, and heart followed in the 1960s. Organ transplantation was, however, restricted by the limited effectiveness of the treatment then available to control the body’s rejection of grafted organs. With the development of more effective immunosuppressive drugs in the 1980s, transplants have become an accepted treatment for an increasing number of deadly diseases (described in detail in Appendix D, Part 1). More than 20,000 transplants were performed in 1998. With the increasing survival of recipients with functioning grafts, estimates of the number of people now living with a graft range up to 125,000, but a precise figure is not available.
Today, a major limit on transplantation is the shortage of organs available. Nearly 65,000 people were registered on waiting lists for organ transplantation in 1998, and more than 4,500 were removed from waiting lists due to death (UNOS, 1999b). Maintaining the health of transplanted organs not only protects the recipients of transplants from death, retransplantation, or other trauma; it also protects a scarce resource. Immunosuppressive drugs are essential for these dual protections, but their high cost means that most transplant recipients need financial assistance to pay for them.
Immunosuppressive drugs prescribed to recipients of solid organ transplants represent one of the few exceptions to the statutory exclusion of Medicare coverage for outpatient drugs. Even so, coverage is limited to three years
following a transplant, which is an increase from the initial single year of coverage authorized in 1986.1 Consistent with the provisions in the 1997 Balanced Budget Act calling for the present report, this chapter investigates the benefits of eliminating the three-year coverage limit on immunosuppressive drugs and the costs to Medicare of that step. The analysis here differs from that in Chapters 3 and 4 because the emphasis is less on the effectiveness of the drugs themselves than on the effects of the coverage limitation on patient outcomes. As this chapter and Appendix D describe, the former is well documented but the latter is not.
The special status of immunosuppressive drugs for transplant recipients has evolved through a complex series of incremental exceptions to the basic framework of Medicare coverage established in 1965. The next section reviews this evolution as context for the analysis of coverage issues that follows. Appendix D, Part 2 provides more detailed background.
EVOLUTION OF IMMUNOSUPPRESSIVE DRUG COVERAGE BY MEDICARE
When the Medicare program was created, outpatient drugs (and drugs in general) played a markedly smaller role in the treatment of people with serious medical problems. Many people died from conditions that now can be either cured or managed effectively for years by drugs that were not available in 1965. With the growing supply of effective drugs have come higher costs in this as in many other areas of medicine. What was once seen as a minor part of the financial burden of illness is now a major worry for many Medicare beneficiaries and an increasing concern for policymakers.
Nonetheless, coverage for immunosuppressive drugs arose less from concerns about high-cost outpatient drugs in general than from a historical anomaly, the creation by Congress of a special entitlement to Medicare for those diagnosed with permanent kidney failure (end-stage renal disease, or ESRD). For a condition that meant near-certain death, the emerging technologies of dialysis and renal transplantation could be lifesaving. Medicare coverage made these treatments financially accessible and promoted the development of dialysis services around the country (IOM, 1991).
Because transplantation was both rare and risky in 1972, the Medicare amendments mainly affected dialysis, a more developed but still relatively early-stage technology that had been introduced to clinical practice on a limited basis in the early 1960s. As long as ESRD patients were treated with dialysis, they were assured of Medicare benefits—and this remains true today. If, however,
patients received a transplant, their eligibility lapsed after one year and did not, in any case, include outpatient medications. The assumption at the time was that a renal graft cured ESRD. As it became evident the transplantation created its own set of continuing medical needs for those who survived past one year, in 1978, the one-year limit on Medicare benefits for renal transplant recipients was extended to three years. This three-year limit remains in place for people who cannot qualify for Medicare by virtue of age or disability.
Although the need for immunosuppressive drugs was recognized when the ESRD benefit was created and then extended for transplant patients, the drugs available were neither effective nor expensive enough to prompt an exception to Medicare’s general exclusion of coverage for outpatient drugs. After the introduction of much more effective immunosuppressive drugs, starting with cyclosporine in 1983, transplantation became much more successful. Likewise, immunosuppressive therapy became much more expensive, in part because the new drug regimens were very costly to patients and in part because the drugs would be used for many years as survival times lengthened.
As the combination of the longer survival of transplant recipients and the heavy financial burden for immunosuppressive drugs became increasingly understood, Congress in 1986 authorized Medicare coverage of immunosuppressive drugs for one year following a Medicare-covered transplant.2 This coverage was extended to three years (on a phased-in basis) beginning in 1995.
People with ESRD have a special entitlement to Medicare that other transplant recipients lack. Regardless of age or eligibility for disability benefits, they become Medicare eligible by virtue of being diagnosed with ESRD, and they remain eligible for benefits for three years following the transplant. If, however, someone with ESRD has employer-sponsored or other group health insurance, the group plan has primary payment responsibility for 30 months following the diagnosis, with Medicare serving as secondary payer to cover certain costs not covered by the group plan.
Recipients of other solid organ grafts establish and retain eligibility for Medicare coverage in the same way as other non-ESRD patients, namely, by reason of age or disability. Many establish eligibility through disability demonstrated prior to or while recovering from transplant surgery. Nonetheless, if they remain eligible for Medicare for a three-year period following their transplant, these other transplant recipients also have the special benefit of immunosuppressive drug coverage for three years.
Table 5–1 summarizes current Medicare policy (prior to the changes noted in footnote 1) for covered transplant recipients. Some proposals to eliminate the three-year limit on Medicare coverage of immunosuppressive drugs would extend coverage indefinitely only for transplant recipients who remained eligible for Medicare by virtue of age or disability (H.R. 1115). Another bill would also include those who are no longer eligible for general Medicare benefits, primarily renal transplant recipients (S. 631). The latter bill would also extend indefinitely legislation that makes Medicare the secondary payer for beneficiaries covered under a group health plan. This would limit Medicare costs but continue to discourage employment and provide an incentive for transplant recipients to establish and maintain eligibility for coverage by reason of disability.
ASSESSMENT APPROACH
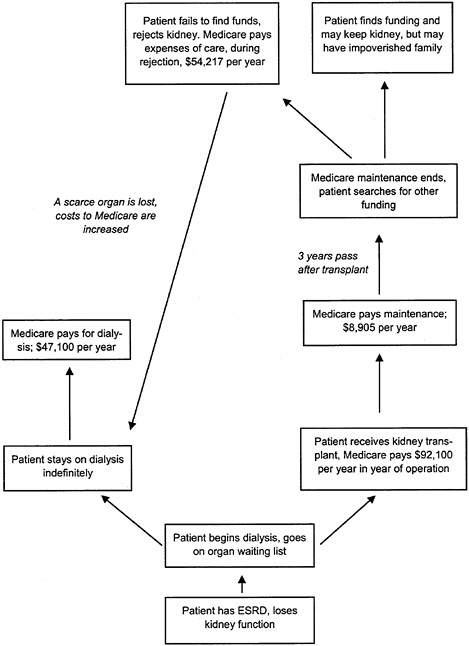
Following the approach described in Chapter 2, the committee explored the evidence base related to the effectiveness of immunosuppressive drugs and the effect of current time limits on Medicare’s coverage of these drugs. It adapted the evidence pyramid discussed in Chapter 2. Figure 5–1 shows two pyramids, the lower one relating to immunosuppressive drug therapy and the upper one to the coverage extension. For both “interventions,” the desired outcomes are patient survival, graft survival, minimal complications or side effects, and good health-related quality of life. Health-related quality of life has additional dimensions for the “coverage intervention” related to the stress that people may experience in trying to arrange alternative financial access to care when Medicare coverage ends.
In contrast to the interventions discussed in Chapters 3 and 4, the evidence base for the lower pyramid is strong and is only briefly reviewed below. The real question for the committee involved coverage, that is, whether there is an additional burden of disease stemming from the loss of Medicare coverage related to people not following their prescribed immunosuppressive regimen and whether this behavior is related to lack of financial access. Here the committee sought evidence that coverage could result in enhanced adherence by patients to drug regimens and improved outcomes, taking possible harms into account.
Even if all the criteria in Figure 5–1 were met, the extent of benefit relative to the cost to Medicare or society generally would still have to be considered. As explained earlier, this report provides estimates of costs to Medicare only and does not include formal assessments of cost-effectiveness. It does explore briefly (in Chapter 6) the various ethical questions arising from special Medicare entitlements or exceptions to the outpatient drug exclusion for a few categories of expensive drugs that leave other needed drug therapies still uncovered.
TABLE 5–1 Summary of Current Medicare Coverage Policy on Transplants
|
|
Pretransplant |
Up to 3 Years Posttransplanta |
More than 3 Years Posttransplant |
|||
|
Patient Characteristics |
Immuno Drugs |
Standard Servicesb |
Immuno Drugs |
Standard Services |
Immuno Drugs |
Standard Services |
|
Renal Transplant |
|
|||||
|
Patient disabled or ≥65 |
NA |
Y |
Y |
Y |
N |
Y |
|
Patient not disabled or ≥65 |
NA |
Y |
Y |
Y |
N |
N |
|
Other Covered Organ Transplant |
|
|||||
|
Patient disabled or ≥65 |
NA |
Y |
Y |
Y |
N |
Y |
|
Patient not disabled or ≥65 |
NA |
N |
N |
N |
N |
N |
|
NOTE: NA=not applicable; N=not covered; Y=yes, covered. aReference for coverage of immunosuppressive drugs: Social Security Act (SSA), Title XVIII, section 1861(s)(2)(J); reference for other eligibility for renal transplant recipients: SSA, Title II, section 226A. bStandard services are those normally covered under Medicare (e.g., dialysis services, physician care prior to or following transplantation). |
||||||
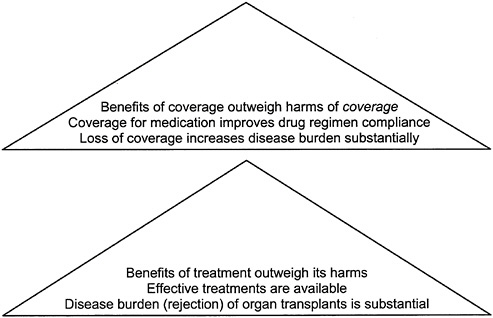
FIGURE 5–1 Evidence pyramids for extending coverage of immunosuppressive drugs.
BURDEN OF DISEASE
Organ transplantation has become the treatment of choice for a number of advanced life-threatening conditions. In 1997, the latest year for which data on primary diagnoses were available (UNOS, 1999a), nearly two-thirds of those receiving kidney transplants had glomerular diseases (diseases of the basic filtering unit of the kidney), diabetes, or hypertensive nephrosclerosis. The majority of liver transplants resulted from noncholestatic cirrhosis (59 percent), with another 14 percent due to cholestatic liver disease or cirrhosis. The great majority of heart transplants were due to either coronary artery disease (45 percent) or cardiomyopathy (42 percent). The much less common lung transplants are most often the result of emphysema or chronic obstructive pulmonary disease (37 percent), cystic fibrosis (19 percent), or idiopathic pulmonary fibrosis (14 percent).
In 1998 alone, the United Network for Organ Sharing (UNOS) reported that well over 20,000 solid organ transplants were performed in the United States. Table 5–2 shows their distribution.
For some conditions such as congenital malformation of an organ, transplantation cures the condition that made the operation necessary. In other cases such as viral hepatitis or diabetes, the condition persists and may ultimately destroy the transplanted organ, which can result in death, retransplantation, or—for patients with renal transplants—a return to dialysis.
TABLE 5–2 Number and Types of Transplants Performed in 1998
|
Type |
Number |
|
Kidney-pancreas |
965 |
|
Kidney alone |
11,990 |
|
Pancreas alone |
253 |
|
Liver |
4,450 |
|
Heart |
2,340 |
|
Heart-lung |
45 |
|
Lung |
849 |
|
Intestine |
69 |
|
Total |
20,961 |
|
SOURCE: UNOS Scientific Registry data as of April 14, 1999. Double kidney, double lung, and heart-lung transplants are each counted as one transplant. |
|
In 1995 there were more than 70,000 persons in the United States living with a functioning transplanted kidney. With roughly 12,000 kidney transplants performed per year and more than 80 percent of patients surviving five years with a functioning graft, this number is now estimated at over 80,000, but the exact figure is not known. Numbers of liver, heart, and other transplants are smaller, but the long-term survival of both grafts and recipients is growing rapidly—the total number of all living transplant recipients has been estimated, as previously mentioned, at up to 125,000.
The increasing success of transplantation has brought great benefits to many people. It has also created a new—but almost always more tolerable—type of burden, the continued need for immunosuppression to manage the continued risk of graft rejection.
Need for Immunosuppression
As described in more detail in Appendix D, Part 1, it quickly became apparent based on observations from animal research and early organ transplants in humans that the survival and functioning of grafted organs required suppression of the recipient’s natural immune response to the graft. The immune system reacts to the presence in the body of proteins that do not belong to the individual, whether these proteins are from ragweed pollen, infecting bacteria, blood of another blood type, or an organ from the body of another individual. For a transplanted organ, this reaction leads to organ rejection and eventual destruction. Absent successful intervention, the death of the “host” follows.
In the early days of transplantation, physicians and researchers hoped that the patient would accommodate the graft completely and thus render pharmacological immunosuppression unnecessary. Although a degree of accommodation does occur in most patients, allowing the dosages of immunosuppressive drugs to be reduced, accommodation is not so complete as to allow drug-free graft survival in any but rare cases involving particularly tolerant organs. The liver, for instance, needs less immunosuppressive support than other types of grafts, and a few liver transplant recipients (less than 1 percent) have been able eventually to cease immunosuppressive therapy. Most patients, however, cannot cease immunosuppressive therapy without serious risk of graft rejection.3
Although research has demonstrated the effectiveness of immunosuppressive drugs, they are not 100 percent effective. Some patients still experience acute rejection of their graft despite immunosuppressive therapy, and others suffer chronic rejection that may eventually lead to graft failure.4 Acute rejection is most common in the first few months after the transplant. In 1995, graft loss during the first year after a kidney transplant was reported as about 12 percent (USRDS, 1998; discussed in Appendix D, Part 1), but more recently, various centers have reported lower rates of early graft loss due to acute rejection: 7 to 8 percent (Gaston, 1998). Chronic rejection, the gradual failure of an organ due to immunologic rejection, is a more complex phenomenon, or at least more difficult to measure, and it varies by organ. In the more immunologically tolerant liver, for instance, chronic rejection has been reported to account for only 9 to 10 percent of late graft loss (Abbasoglu et al., 1997). In the kidney, on the other hand, chronic rejection has been considered a major cause of late graft loss, but this is now being reexamined. One center had reported chronic rejection as the primary cause of graft loss in 44 percent of cases of loss between six months and approximately four to five years after transplantation. When the cases attributed to chronic rejection were critically reevaluated, however, more than half appeared to have involved lack of patient adherence to demanding medication regimens rather than ineffectiveness of the drugs themselves (Gaston, 1998). It is therefore difficult to tell how many cases of graft loss that have
been labeled chronic rejection actually represent a failure of therapy rather than patient noncompliance.
In summary, the rate of graft loss due to acute rejection has decreased as more effective drugs have been introduced; the rate of late graft loss due to chronic rejection may be lower than believed; and it could perhaps be reduced by greater attention to factors affecting patients’ ability to take their medications as prescribed. Neither form of rejection, however, has been eliminated. The goal of achieving adequate immunosuppression, even with today’s more effective drugs, remains a challenge that cannot be met for every patient.
Waiting Lists for Transplantation
The increased transplant success rate has meant that renal transplantation became a better treatment for ESRD than dialysis. For kidneys and other organs as well, increased success has made the supply of donated organs a critical concern.
The relative scarcity of organs is evident in the growing number of patients on the waiting lists for transplantation (Table 5–3). This growth is due in part to the increasing number of people with organ failure and in part to the improved safety and effectiveness of the procedure that allows it to be offered to a wider population of patients including some who have survived the failure of a first grafted organ. Long waits for a transplant—waits that may end in death before an organ becomes available—are a significant part of the burden of the diseases treated by transplantation. The main “treatment” for these waits would be an increase in organ donation or the development of effective, acceptable alternatives to human organs. For the present, however, every transplanted organ that is successfully maintained also helps prevent further increases in the waiting list and waiting times.
Further, patients whose grafts have failed and who have successfully applied for a second graft may have a worse prognosis than the patient who is receiving a graft for the first time, due in part to the likelihood of increased immunologic sensitivity among patients who have already had a graft. This phenomenon has been reported in adult recipients of, for example, regrafts of hearts (Chan and Hunt, 1998), livers (Markmann et al., 1997), and kidneys (Cecka, 1997). It should also be noted, however, that the largest body of data, which involves renal regrafts, indicates that the gap between the outcomes of first and second transplants has been cut in half in recent years (Cecka, 1997). Any retransplantion uses a donated organ from a very small pool and leaves some other patients on the waiting list longer.
TABLE 5–3 Number of Patients on Waiting Lists at Year’s End, Selected Years
AVAILABILITY OF EFFECTIVE TREATMENT
Questions that the committee had to grapple with in the previous chapters—whether evidence showed that the clinical intervention proposed for coverage improves outcomes—have largely been settled in the case of immunosuppression after organ transplantation.5 As shown in Table 5–4, more than 75 percent of kidneys, livers, hearts, and even lungs are now functioning one year after transplantation, and in all categories except lung grafts, more than 60 percent of the grafts are still functioning five years after transplantation. Patients are surviving at somewhat higher rates than grafts. More than two-thirds of transplant recipients now survive at least five years.
Of the four classes of drugs that have contributed to the major improvements in graft and patient survival in recent years, products in one class (antilymphocyte agents) are used on a short-term basis and, thus, are not a Medicare coverage issue. Products in the other three classes (antiproliferative agents, corticosteroids, and calcineurin phosphatase inhibitors) are used on a long-term basis. Physicians generally prescribe a combination regimen for long-term use because the different classes of drugs work in different ways and have different side effects. The combination approach helps achieve high levels of immunosuppression without letting any particular type of side effect become as bad as it might otherwise be.
TABLE 5–4 Graft and Patient Survival Rates at One and Five Years
The level of immunosuppression needed varies from person to person, depending on the immunologic compatibility of the recipient and the graft. As the time after transplant increases, physicians generally decrease the dose of immunosuppressive agents on an empirical basis, testing small changes to see whether side effects can be reduced without threatening graft rejection.
The major benefits of immunosuppressive drugs for transplant recipients are clear: longer survival and improved quality of life (Wolfe et al., 1999). A functioning renal graft has the great advantage of working all the time, rather than periodically like dialysis, so the transplant patient generally feels healthier and has fewer dietary restrictions. Further, a transplanted kidney works while the patient does other things, but dialysis requires the patient to spend several long periods a week undergoing treatment, which can be very disruptive to work and other activities. Nonetheless, kidney transplant patients do at least have an alternative in the case of graft failure. Patients suffering failure of another vital organ have no options except transplantation.
The major harm that comes from immunosuppressive drugs is the result of a suppressed immune system. That is, the suppressed immune system protects against graft rejection but simultaneously leaves patients at risk from many organisms that normally are present but kept under control by a properly functioning immune system. Many patients take some prophylactic medication, and all require close monitoring for emerging infections.
Each immunosuppressive agent also has its own specific complement of other adverse effects, as does any effective drug. These side effects can include hypertension, decreased kidney function, diabetes, various gastrointestinal complaints, leukopenia or thrombocytopenia, unusual growth of gums or hair, and an increased tendency to develop malignancies. Management of these side effects often requires additional medications.
Although this committee did not systematically address quality of life or cost-effectiveness, one analysis of renal transplantation in Canada compared kidney transplantation to dialysis (starting from the initiation of either procedure) on the basis of several health-related quality measures (Laupacis et al., 1996). Except for the first month following transplantations, all showed higher quality-of-life scores for transplant recipients during both the year of the transplant and the following year (compared to the first two years of dialysis). The quality-adjusted life years (QALYs) for the transplant and subsequent year were 0.65 and 0.62, respectively. The comparable figures for dialysis were 0.53 and 0.51.
Overall, the benefits of immunosuppression for transplant patients are widely accepted as outweighing the harms. Nonetheless, this partial listing of harms makes clear that these patients require continued medical monitoring and often additional therapies to sustain the benefits achieved by transplantation.
BARRIERS TO ADEQUATE THERAPY
For many medical problems including those examined in this report, the existence of effective treatment does not ensure that it will be available to and used by all who could benefit from it. Medicare coverage has helped make transplantation and posttransplantation therapy available to thousands of people, but the cost of continued care, especially immunosuppressive drug therapy, is a problem for many after the three-year coverage period for drugs has passed. Nonetheless, it is not clear to what extent financial problems contribute to people’s failure to follow their treatment regimens or to what extent this accounts for graft rejection and failure.
Following Complex Drug Regimens: General Issues
Despite the critical importance of immunosuppressive drugs, a significant proportion of patients—several studies estimate about 22 percent—do not take their drugs as prescribed (Greenstein and Siegal, 1999). This lack of compliance6 with the treatment regimen puts patients at risk of graft loss. Because patients may be reluctant to admit that they are not taking their drugs as prescribed, the amount and type of noncompliance are difficult to assess, which makes a direct link to graft loss difficult to establish. A study cited earlier from one transplant center suggests that noncompliance is a significantly more important cause of graft loss in patients who have had a successful transplant than has previously been appreciated (Gaston, 1998).
The compliance responsibilities of transplant patients are formidable. A representative kidney transplant medication regimen could very well include an immunosuppressive agent from each of the three classes described earlier, plus a routine prophylactic antibiotic, an antifungal medication, and medications for concomitant conditions including hypertension, angina, hypocalcemia (depletion of calcium and consequently bone disease, which is common among patients who are or have recently been on dialysis), and short- and long-acting antacids for gastrointestinal side effects. A patient on this regimen would have to take at least eight medications in the morning, another four in the evening, plus antacids and antifungal mouth treatments after every meal and before going to bed.
The reasons for lack of full compliance are varied (e.g., see Raiz et al., 1999; Siegal and Greenstein, 1997). With such complex medication regimens, problems may include ordinary forgetfulness, difficult or stressful living ar-
rangements, or inadequate understanding of the importance of spacing doses throughout the day or in relation to meals. Lack of formal education may contribute to a lack of understanding for some patients. In addition, the side effects of many immunosuppressive drugs are unpleasant and can make compliance difficult. Because noncompliance with immunosuppression can have such serious consequences, transplant professionals have developed various strategies to help patients, for example, assisting them in designing a clear schedule and suggesting various reminder aids. Some transplant centers not only emphasize compliance as part of their pretransplant preparation of patients but also ask patients to sign a written contract agreeing to comply with the prescribed regimen to maintain the donated organ.
One review of studies of patient compliance pointed to greater compliance of patients just prior to physician contact (Cramer, 1995). This suggests that compliance might be increased by more frequent contact with health care workers.7 Maintaining such contact may be a greater problem for those renal transplant recipients who reach not only the three-year coverage limit for immunosuppressive drugs but also the three-year limit on Medicare coverage overall, including coverage for physician visits.8
Patient compliance is a concern in many areas of medicine, not just transplantation. Urquhart (1996) reviewed studies of compliance, concluding that roughly 30 percent or more of patients do not comply with their prescribed therapy regimens, regardless of the severity of the consequences. In one revealing study, researchers introduced medical students to the difficulties that patients face by electronically monitoring the students’ compliance with a two- or three-times-a-day drug regimen over a two-week interval (Kastrissios et al., 1996). Although 71 percent of the doses were taken, only 46 percent were taken at the prescribed frequency (doses per day) and 28 percent at the prescribed intervals (hours between doses). The most common explanation given by the students, a hectic schedule, would apply to many patients as well.
In older people, compliance difficulties are associated with a variety of factors, including multiple medications and concern about the cost of the medi-
cations (Cool et al., 1990; Coons et al., 1994), both of which are often aspects of the regimen that transplant patients must manage. Nonetheless, studies indicate that elderly patients in general tend to be more compliant with their regimens than younger patients (Bame, 1995; Greenstein and Siegal, 1999).
Cost of Immunosuppressive Drugs
The cost of the combination immunosuppressive drug regimens can vary widely (see Appendix D, Part 1, Table D-1). For example, the least expensive three-part combination regimen might cost roughly $5,900 per year and could be sufficient for many patients. Those who did not do well on this combination might require one or more of the higher-priced drugs, which could bring the cost to more than $16,000 per year.9
As noted above, many transplant patients require additional outpatient medications such as antihypertensive agents and antibiotics for infections. Medicare does not cover these outpatient drugs for any beneficiary.
Because immunosuppressive therapy is complex, patients must be monitored for both drug effectiveness and side effects by an experienced physician. As described above, clinical and laboratory services are covered only for long-term transplant survivors who remain eligible for Medicare by virtue of age or disability (“ESRD-only” patients lose coverage after three years).10 Informal estimates suggest that the visits and laboratory work solely to monitor immunosuppressive drugs could cost such a patient roughly $500 to $700 per year. Any additional problems, infections, or side effects would result in additional costs.
An important question for this study is whether longer coverage of immunosuppressive drugs will result in better outcomes for transplant recipients. The answer depends on the degree to which the lack of coverage for the costs of the medication stands as a significant barrier between the patient and adequate immunosuppression. (Cost is not the only factor in noncompliance, as mentioned above; see also Dew et al., 1999.)
Expiration of Medicare Coverage and Alternative Funding
As the committee heard during its workshop on coverage for immunosuppressive drugs (see Appendix A), a number of programs have been created to provide drugs to those without coverage. Still, it may be difficult or impossible
for some patients to assemble sufficient assistance from one or more programs to solve the problem of long-term, stable access to the drugs needed. Some are eligible for Medicaid programs that cover the drugs; others will have coverage under a spouse’s insurance; still others may qualify for assistance from companies that manufacture the drugs; and charitable programs may assist more. Some patients may be able to work and find employment that offers health benefits. However, the structure of existing public programs provides incentives for patients to retain their status as disabled to avoid losing Medicare coverage.
Identifying or qualifying for the public or private programs that assist people in paying for or otherwise obtaining needed drugs is a complex undertaking. Programs vary from location to location and also change over time. Patients often need the help of a specialist to locate, apply for, and maintain assistance for their medical expenses (Jacobs, 1998; Sisson et al., 1994). One group documented a substantial increase in compliance with medications when its transplant center provided a specialist to assist patients in assembling coverage (Paris et al., 1998). Several workshop participants reported that patients assist one another and are sometimes forced to resort to seeking compassionate but illegal help to obtain medications. For example, patients may share or lend drugs to help someone through a coverage gap. “Underground” networks have been organized to buy drugs from less expensive foreign sources11 or to secure donations of unused drugs from the families of deceased patients.12
Evidence About the Effects of Providing or Withdrawing Coverage13
As noted earlier, if the elimination of time limits on the coverage for immunosuppressive drugs is viewed as an “intervention,” the desired results are both improved outcomes in graft survival, and also increased ability of patients to engage in normal activities of living. Although both the effects of immunosuppressive drugs themselves and the effort currently required for maintenance of coverage (e.g., submitting bills or otherwise following Medicare requirements) may have some negative implications, the loss of coverage has many more negative aspects, including devoting exorbitant time and energy to the pursuit of
alternative ways of getting the needed drugs, and of course, the risk of graft rejection if those alternative strategies should fail. This effort can disrupt marriage and family life, threaten the continuation or resumption of a satisfying work life, and otherwise take a heavy toll on people’s quality of life. These kinds of outcomes have been little studied or measured in a systematic way, but they must be acknowledged. Fortunately, not all transplant recipients have to continue indefinitely in that mode because some are able to develop longer-term strategies to secure access to their medication. Figure 5–2 sketches some, but by no means all, of the consequences to the patient and to Medicare that may result after Medicare coverage for immunosuppressive drugs ceases.
Data about the effects of the Medicare coverage limit are sparse. Not surprisingly, no randomized studies compare the results for patients provided coverage and those not provided coverage for immunosuppressive drugs. One analysis based on a sample of 1990 Medicare records for 7,949 renal transplant patients showed that the rate of graft loss decreased steeply during the first six months after the operation (risk of rejection is highest just after the operation is performed), but then remained stable through the end of the year and beyond (Eggers, 1999; Eggers and Milan, 1998). Given that the time limit for Medicare coverage of immunosuppressants was one year in 1990, this analysis does not indicate any dramatic impact of coverage expiration. The data were not, however, stratified by beneficiary income or any income surrogate, and for technical reasons, the analysis may have been limited in its ability to detect all graft failures.
Another report, this time for a single kidney transplant center, describes a natural experiment on loss of Medicare coverage, again when the coverage limit was one year. For one group of patients who could manage some but not full payment, doses of cyclosporine were reduced. For a second group that had found no way to pay at all, cyclosporine was eliminated completely. The outcomes for these two groups were later compared to a third group of similar patients at the center who were able to finance their full dose of cyclosporine. Patients were followed, and otherwise cared for, through at least three years. Patients in the no-dose group exhibited more late-stage acute rejection than the reduced-dose or full-dose group. The reduced-dose and full-dose groups did not differ significantly. Although this was not a randomized, controlled trial, patients were matched, so the data suggest that it may be better to reduce the dose than discontinue it, if at all possible (Sanders et al., 1993). The results may also suggest that the optimum dose of immunosuppressive drugs has yet to be determined—and may be lower than now believed.
The same transplant center completed a further study on the relation of resources for purchasing cyclosporine to patient outcomes. This analysis was made possible by another natural experiment—initiatied by the National Organization for Rare Diseases (NORD)—of an indigent drug access program for cyclosporine. The study followed a group of NORD participants at the center who were socioeconomically matched with the no-dose group previously ob-
served; both groups were then followed for an additional 2.5 to 5 years. The no-dose group and the NORD program participants had exhibited similar rates of acute rejection prior to the NORD intervention. After the intervention, members of the no-dose group experienced significantly more episodes of rejection, resulting in increased risk of graft loss; NORD program participants did not experience any increase in their episodes of rejection (Sanders et al., 1996). Further data suggesting that financially induced noncompliance is reversible were described at the committee workshop.14 Researchers reported the results of an analysis of national data comparing renal graft survival at one and three years posttransplant for high- and low-income groups. When Medicare coverage was available for only one year, the high- and low-income transplant recipients had similar rates of graft survival at one year, but the high-income group had significantly better rates of graft survival at three years. When Medicare coverage was extended to three years, the high- and low-income groups had similar rates of survival at both one and three years posttransplant (Woodward et al., 1999). Like the study of the NORD intervention, this study showed a statistically significant association between better outcomes and better access to funding, whether through private means or public programs.
Another study relevant to some of these issues is underway, sponsored by the National Kidney Foundation in cooperation with George Mason University. Unfortunately, the results were not available before this report was completed.
To summarize, some level of noncompliance with prescribed medications may be an expected—if unfortunate—aspect of outpatient management of any illness. The evidence described above, although not based on strong controlled studies, suggests that for some groups of transplant patients the lack of Medicare coverage for medications is a factor contributing to noncompliance and worse patient outcomes, especially for low-income people without alternative insurance through a family member (or their own work). Some patients may badly need help in paying for their immunosuppressants, whereas others may be in less financial need (though perhaps still in need of help to locate and manage other coverage programs).15
The data reviewed did not address the less easily quantified burdens of coverage loss. These include its emotional toll and its diversion of the time and talent of so many individuals from other purposes to arranging access to medications. (The latter is described in Appendix D, Part 2 as the “survival paradox.”)
Another factor to consider in estimating the effect of extending Medicare coverage is the effect such a decision might have on drug pricing. Although Medicare is today a major payer for immunosuppressive drug therapy for transplants, the time limit on coverage means that other parties including Medicaid, private insurers, patients and families, charitable organizations, and drug companies themselves participate in the overall financing of access. Depending on the specifics of the policy, eliminating the time limit on coverage would reduce the involvement of these parties to varying degrees.16 This could affect manufacturers’ pricing of the drugs and possibly the choice of drugs by physicians and patients. It might seem that if Medicare were the major if not the only buyer for this use, then it might be able to negotiate or otherwise secure better prices, at least when multiple sellers exist (which is not the case for drugs still under patent). This would, however, require potentially controversial legislative changes in the way Medicare pays for covered prescription drugs. The Balanced Budget Act of 1997 provided that the Health Care Financing Administration limit payments to the lower of the billed charge or 95 percent of the average wholesale price.
Congress could also establish a cap on Medicare payments per patient per year, with patients responsible for any amounts over the cap. Such a cap could, for example, be set initially at the level of the lowest-cost accepted or commonly prescribed multidrug immunosuppressive regimen. It could also be set arbitrarily based on budgetary considerations. Given some clinical flexibility in moving patients from higher-cost to lower-cost regimens, this could put pressure on manufacturers to reduce prices for the most expensive drugs. Undoubtedly, some patients who could not be managed with less expensive regimens would face substantial costs, although they would still benefit from the extension of coverage past the current 3-year limit. Whether existing private programs to help cover drug costs for those without coverage would be continued for those with partial coverage is unknown.
ESTIMATED COSTS TO MEDICARE OF EXTENDING COVERAGE
As discussed in Chapter 2, the cost estimation approach of the committee generally follows the generic practices (e.g., not discounting estimates to present value) employed by the Congressional Budget Office (CBO) in making estimates for Congress. A more detailed presentation of the committee’s cost estimates and their associated assumptions and data sources appears in Appendix E, which was prepared by the Lewin Group in consultation with the committee and background paper author.
The committee’s estimates of Medicare costs are based on a series of assumptions, some of which have supporting evidence or data but others of which are best guesses based on committee judgment in the absence of such information. The estimates are intended to suggest the order of magnitude of the costs to Medicare of extending coverage, but they could be considerably higher or lower than what Medicare might actually spend were coverage policies changed. The tables in Appendix E allow readers to vary some of the assumptions and calculate alternative estimates.
Box 5-1 summarizes the assumptions and data used to develop the estimates. It includes one estimate that assumes coverage for immunosuppressive drugs is extended only for transplant recipients eligible for Medicare by reason of age or disability. A second estimate assumes that the drug coverage is also extended for currently covered “ESRD only” renal transplant recipients who lose other Medicare coverage after three years because they are not either disabled or at least age 65. For the five-year period 2000 to 2004, the total net estimated cost to Medicare of eliminating the three-year limit on coverage of immunosuppressive drugs for the first, smaller group would be $778.4 million, taking into account $553.9 million in savings from avoiding a return to dialysis for those with failed renal grafts. Adding the “ESRD only” group would raise the total net estimated cost to $1,060.1 million, taking into account $830.4 million in offsetting savings.
|
BOX 5–1 Summary of Estimated Costs to Medicare for Extending Coverage of Immunosuppressive Drugs After Transplant Operations Coverage Model Assumptions
Cost Estimate Assumptions for Years 2000–2004 (see also Appendix E)
|
|
Cost Estimate Assumptions for Years 2000–2004
Data Sources
Estimated Costs (in millions) to Medicare, Summed over 2000–2004
|
In order to estimate the cost to Medicare of eliminating the three-year limit on coverage of immunosuppressants for transplant recipients, the different clinical circumstances of renal and nonrenal transplant recipients must be taken into account. Most ESRD patients who receive renal transplants have an alternative treatment available, dialysis. Other transplant patients do not have an alternative long-term treatment; they either survive with a graft or die while waiting for a graft or later if the graft fails and retransplantation is not an option. Renal transplant is certainly preferred by most patients and physicians, but dialysis still exists as a life-extending option for someone whose graft fails.
The cost estimates assume that only a subset of renal transplant recipients who suffer graft failure after three years do so for reasons related to cost. As described earlier and in Appendix D, various factors contribute to graft rejection including lack of patient adherence to demanding drug regimens. After considering the very limited and inadequate information on the role of financial pressure, the committee estimated that one-third of renal graft failure might be attributed to lack of financial resources (2.5 percent of the 7 percent failure rate after three years).
Renal transplant recipients also differ from other patients because their ESRD diagnosis qualifies them for three years of posttransplant Medicare coverage without the need to meet the age or disability requirements that apply to others. This raises the question of how the three-year limit on immunosuppressive drugs would be eliminated for ESRD versus other Medicare-covered transplant recipients. For purposes of one estimate, the committee assumed that the time limit on coverage of immunosuppressive drugs would be eliminated only for those transplant recipients who stay eligible for Medicare coverage after three years by reason of age or disability. For purposes of the other estimate, the committee assumed that Congress would extend coverage to all Medicare-covered transplant recipients including those now qualified by virtue of ESRD diagnosis alone.
The committee assumed that costs would be offset by savings from extended primary-payer requirements for beneficiaries covered by employer health plans. As explained in Appendix E, the committee assumed for both the first and the second cost estimates that each of the relevant beneficiary populations would drop by 25 percent.
For the purpose of estimating costs for renal transplant recipients, the committee considered the likely cost of the immunosuppressive drugs required to maintain a renal graft compared to the cost of returning a patient with a failed graft to dialysis. The initial cost of a transplant is high relative to dialysis. Data presented at the committee workshop (Table 5–5) showed that Medicare’s 1994 expenditures per ESRD patient (controlling for differences in patient survival) were highest for patients transplanted that year and lowest for patients who were maintaining grafts transplanted in previous years (Eggers, 1999). The yearly cost of dialysis was almost as high as the cost of treating someone for graft failure.
TABLE 5–5 Medicare Expenditure per ESRD Patient, 1994
|
Situation |
Medicare Expenditure |
|
Kidney transplant |
$92,100 |
|
Transplant maintenance |
8,905 |
|
Maintained on dialysis |
47,100 |
|
Graft failure |
54,217 |
The “break-even” point for transplantation occurs when the total cost of a transplant and subsequent maintenance equals the cost of maintaining someone on dialysis for the same period of time. After the break-even point, maintaining someone with a kidney transplant costs the Medicare program less than maintaining someone on dialysis. According to Eggers (1999), the break-even point for Medicare occurred at 3.1 years in 1994, down from 4.6 years in 1989. That is, if the graft could be maintained for 3.1 years, then transplantation would become less expensive than dialysis would have been had the patient survived on dialysis for that period. The change between 1989 and 1994 probably reflects both changes in transplant care and the substantial increase in the cost of dialysis following the introduction of coverage for erythropoietin, a drug for dialysis-induced anemia. In sum, not only is maintaining a functioning transplant preferred by physicians and patients, it is clearly less costly over the long-term than maintaining a patient on dialysis.
In estimating the cost of extending coverage for immunosuppressive drugs, the gross cost of coverage for transplant recipient patients is not reduced by a premium offset as were the gross cost estimates in the preceding chapters. This is because the beneficiary premium (set by statute at 25 percent of total Part B expenditures) is based only on payments for the aged beneficiary population and most Medicare costs for transplant recipients are for people under age 65.
The committee was not asked to estimate savings to the federal-state Medicaid program that might result from elimination of Medicare’s time limit on immunosuppressive drugs. In 1996, the CBO estimated that the federal share of Medicaid expenditures for Medicare-Medicaid-eligible beneficiaries would be reduced $6 million per year in 2000 and 2001 if the time limit on coverage of immunosuppressive drugs was eliminated for Medicare-eligible transplant patients (CBO, 1996). As explained in Appendix E, if the CBO estimates were adjusted to reflect inflation and this committee’s coverage extension assumptions for the larger beneficiary population (including “ESRD only”), the estimated five-year savings (2000 to 2004) to the federal Medicaid program would total $49 million. Clearly, some patients and families would also benefit finan-
cially from the extension of Medicare coverage for immunosuppressive drugs, but the committee found no solid estimate of these benefits.
STATEMENTS OF OTHERS ON COVERAGE FOR IMMUNOSUPPRESSANTS
More policy attention has been devoted to renal transplantation than to the transplantation of other organs, reflecting the greater number of these operations and the longer experience with transplantation as a successful treatment modality in the case of ESRD. The disparity in the number of transplants of different types of organs may decrease as continuing developments in the technology of transplantation are reflected in the increased success rate of other types of transplants. At this time, policy statements by other groups tend to focus on renal transplantation.
The committee noted that a previous (IOM, 1991) report included coverage policy recommendations at the request of the Congress. In Kidney Failure and the Federal Government, the IOM committee then in place recommended that all ESRD patients who are citizens or resident aliens of the United States be eligible for Medicare coverage, that the time limit on coverage for immunosuppressive drugs be eliminated, and that other Medicare benefits also be extended to these patients without time limits. The earlier report did not address transplants of organs other than the kidney.
The Office of Technology Assessment (OTA) released a report, Outpatient Immunosuppressive Drugs Under Medicare, in 1991. OTA did not make recommendations to Congress, but, rather, analyzed a series of policy options. Regarding the time limit on coverage, OTA observed that if Congress decided to make a change in this aspect of Medicare law, it could either extend coverage for a limited time (which is what Congress eventually did) or eliminate the time limit altogether. OTA noted that extending coverage would reduce any inequity in access to transplants due to ability to pay and that eliminating the time limit completely would accomplish this best. OTA also noted that such a step would be likely to shift financing from other sources to Medicare.
In a 1997 position statement entitled The Decade of Transplantation, the American Society of Transplant Physicians (ASTP; since renamed American Society of Transplantation, AST) called for extending payment for immunosuppressive drugs for transplants from the current three years to the life of the graft. The AST argued that the ESRD program would experience dramatic savings by extending graft life through appropriate drug regimens. They did not give details on how these savings would be realized. Presumably, they would result from lower rates of graft rejection followed by return to dialysis or retransplantation.
The National Kidney Foundation (NKF) also advocates the elimination of the time limits on Medicare coverage. It too argues that this would save Medicare money.
COMMITTEE FINDINGS AND CONCLUSIONS
In developing its findings and conclusions, the committee benefited from the review of the literature presented in Appendix D and the discussion during a public workshop that included clinicians, researchers, and members of the public (see Appendix A). Unfortunately, little systematic research is available to assess the health and cost consequences of the current coverage limit on immunosuppressive drugs. The committee’s findings, as discussed in this chapter, are summarized briefly below. Its conclusions about Medicare coverage follow:
Findings
Burden of Disease. The committee found strong evidence that organ transplants, the majority of which are kidney transplants, are increasingly common, with more than 20,000 performed per year and approximately 80,000 patients now living with functioning grafts. The committee found further strong evidence that virtually all transplant recipients require immunosuppressive drugs to avoid immunologic rejection of their grafts.
Effective Treatments Available. The committee found strong evidence that the immunosuppressive agents now available are effective in reducing organ rejection. Rates of long-term recipient survival with functioning grafts have increased, but patients who do not get adequate doses of immunosuppressive drugs have a higher rate of rejection than transplant recipients who can maintain the appropriate drug regimen.
Benefits of Drugs Outweigh Harms. The committee found strong evidence that although immunosuppressive agents can have serious side effects, their benefits to transplant patients outweigh the side effects. The committee noted that the chronic condition of immunosuppression is generally manageable under the supervision of experienced physicians. The alternative treatment for patients with ESRD, dialysis, does not provide the same quality of life as a functioning renal graft. The alternative for those with other kinds of organ failure is generally death.
Burden of Disease from Noncompliance. The committee found a body of literature that, although small and not including randomized controlled trials, was still persuasive that some otherwise functioning grafts are lost because of the patient’s lack of compliance with the immunosuppressive drug regimen.
Coverage Effective in Reducing Noncompliance. The committee found a body of literature which, although small and not including randomized controlled trials, still suggested that lack of financial access to necessary drugs is
one factor in lack of compliance with immunosuppressive drug regimens and such noncompliance contributes to graft failure and loss.
Benefits of Coverage Outweigh Harms. For the individual, the health and other benefits of drug coverage surely outweigh possible harms. The potential harm of extending Medicare coverage would involve not the transplant recipient but other Medicare beneficiaries who might benefit if the same resources were directed elsewhere within Medicare. A cost-effectiveness analysis could very well identify alternative uses of these resources that would result in more benefit (e.g., QALYs) for these resources, The committee recognized this trade-off as a critical issue, but also an issue beyond the scope of this report.
Possible Directions for Further Research
The committee was hampered by lack of evidence in several areas, including not only medical questions pertaining to transplantation but also factors affecting patient compliance with medical advice and the comparison of the costs of alternative treatments that receive substantial public funding. Given the cost and risks associated with long-term use of immunosuppressive drugs, the prospect of alternatives that are safer, less expensive, or both is obviously attractive.
For the present, a better understanding of the factors that support or obstruct compliance with therapeutic regimens would be helpful. Compliance is clearly a complex phenomenon that is difficult to study. However, because noncompliance puts pressure on an already scarce lifesaving resource, it is important to try to identify barriers to compliance that are amenable to mitigation through dose alteration, financial, educational, or other strategies. Research indicating that patients are more compliant just before contact with health care professionals suggests that research on practical, affordable ways of increasing such contacts might be productive.
For example, a considerable body of research involving telephone contact has accumulated in recent years, and attention is now being paid to the role of e-mail in changing communication between physicians and their patients. A 1996 IOM report discussed several applications of regular or even automated telephone patient monitoring programs while noting that the literature evaluating the effectiveness of telemedicine was sparse (IOM, 1996). Several other recent publications report encouraging results with telephone and/or other electronic contacts both to monitor clinical signs and to encourage compliance with drug regimens (Alemi et al., 1996, Finkelstein et al., 1996; Friedman et al., 1996, 1998; Hetzer et al., 1998); although other reports indicate that some applications have been less successful with some patient groups (Alemi et al., 1997).
The committee also encourages the National Kidney Foundation and George Mason University in their survey of kidney transplant patients. The sur-
vey may improve understanding of the impact of coverage on both patient compliance and other social and economic activities such as employment.
Conclusions
Good evidence supports patients’ continued need for immunosuppressive therapy and the increased risk of graft loss if they cannot follow the prescribed drug regimen. Given this evidence and the existing Medicare policy of supporting organ transplants, the rationale for eliminating the current time limits for coverage of immunosuppressive drugs for all solid organ transplant recipients is strong. Although people who lose coverage often find ways to obtain sufficient drugs to maintain immunosuppression, experience and limited evidence suggest that some grafts—and some lives—are eventually lost for lack of coverage. The estimated five-year net cost to Medicare of eliminating the three-year limit on coverage would be approximately $778 million if extended coverage were limited to those eligible by virtue of age or disability, and $1.06 billion if the time limit was also removed for those who have been Medicare-eligible only by reason of an ESRD diagnosis.
In addition to the economic and possible clinical consequences of time-limited drug coverage for transplant recipients, the committee notes that current policy has societal implications. Organs are a scarce resource for which demand far outstrips supply. Every graft failure that results in retransplantation is a special burden on this limited supply. Beyond those immediately affected, the larger society of citizens has a strong interest in the successful maintenance of grafts to protect their potential access or that of their loved ones.
From a societal perspective, elimination of the time limit on coverage of immunosuppressive drugs for transplant patients presents some delicate ethical and policy considerations. On the one hand, recipients of organ transplants who are eligible for Medicare by reason of age, disability, or ESRD already have a drug benefit that few other classes of beneficiaries have, and ESRD-qualified Medicare beneficiaries are generally treated as a special group. On the other hand, termination of the drug benefit at the end of three years may result in more graft loss, more expenses for treatment of graft rejection and possible return to dialysis, and added demands for scarce organs for retransplantation. The committee returns to this issue in Chapter 6.