State Programs Can Reduce Tobacco Use
National Cancer Policy Board
INSTITUTE OF MEDICINE NATIONAL RESEARCH COUNCIL
Growing attention is focused on how states can prevent deaths due to tobacco use. Thus state governors, state legislators, and their staffs currently must decide whether to fund tobacco control programs, and, if they do, how much to spend on them.
The National Cancer Policy Board (a joint program of the Institute of Medicine and the National Research Council) is charged with carrying out policy analyses to help the nation deal with cancer; in 1997, it quickly identified tobacco’s role as the foremost cause of cancer deaths as its first topic of concern.1 The board followed debates taking place in state capitals throughout 1998 and 1999, and decided in July 1999, in consultation with the Board on Health Promotion and Disease Prevention of the Institute of Medicine, that it would be useful to summarize evidence about the effectiveness of state tobacco control programs and to briefly describe those programs for state government officials.
Tobacco control will likely remain on the agenda of many states for several years. Public health advocates, tobacco firms, tobacco growers, retailers, and the general public have all been drawn into the debate. This report does not address the merit of tobacco control compared to alternative uses of state funds or attempt to balance the interests of contending stakeholders; instead, it focuses on the narrower question of whether state tobacco control programs can reduce smoking and save lives. As states contemplate increasing their tobacco control efforts, many have asked if such programs can make a difference. The evidence is clear: They can.
The stakes are high. Tobacco use kills more Americans each year than any other cause. The estimated 430,000 deaths attributed to tobacco use annually are far more than those caused by illegal drugs, homicides, suicides, AIDS, motor vehicle accidents, and alcohol combined.2 Lung cancer kills more Americans than breast and prostate cancer combined,3 and tobacco accounts for over 30% of all cancer deaths and a comparable fraction of deaths due to heart and lung diseases. Yet despite these risks, many, many people start smoking each year. In 1996, over 1.8 million people became daily smokers, two-thirds of them (1.2 million) under age 18.4
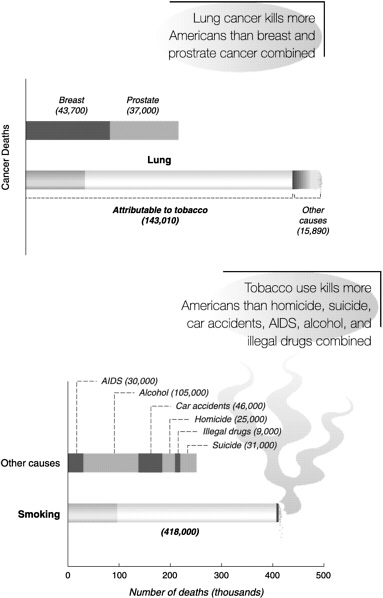
SOURCES: American Cancer Society, “1999 Facts and Figures: Selected Cancers,” available at www.cancer.org/statistics/cff99/selected_toc.html (top), and Centers for Disease Control and Prevention, “Comparative Causes of Annual Deaths in the United States,” available at www.cdc.gov/tobacco/andths.htm (bottom).
Over the past decade, states have moved to the forefront of tobacco control. Starting with California in 1988, and followed by Massachusetts, Arizona, Oregon, and other states, referenda have increased tobacco excise taxes and dedicated a fraction of the revenues to reducing tobacco use. Legislatures in other states—such as Alaska, Hawaii, Maryland, Michigan, New Jersey, New York, and Washington—have increased tobacco taxes substantially, raising questions about how much of the revenue should go to tobacco control. In addition, settlements of law-suits against tobacco firms to recoup state monies spent through Medicaid have now resulted in individual state revenue streams (in Florida, Minnesota, Mississippi, and Texas) or in revenues anticipated through the Master Settlement Agreement with the other states and territories signed in 1998. In aggregate, these agreements could transfer as much as $246 billion from tobacco firms to states over the next 25 years.
What Is the Evidence that State Programs Make a Difference?
The best evidence for the effectiveness of state tobacco control programs comes
|
Resources on State Tobacco Control Programs
|
from comparing states with different intensities of tobacco control, as measured by funding levels and “aggressiveness.” For example, when California and Massachusetts mounted programs that were more “intense” than those of other states, they showed greater decreases in tobacco use compared to states that were part of the American Stop Smoking Intervention Study (ASSIST) funded by the National Cancer Institute.10 From 1989 to 1993, when the Massachusetts program began, California had the largest and most aggressive tobacco control program in the nation, and it showed a singular decline in cigarette consumption that was over 50% faster than the national average.11 A recent evaluation of the Massachusetts tobacco control program showed a 15% decline in adult smoking—compared to very little change nationally—thus reducing the number of smokers there by 153,000 between 1993 and 1999.12 States that were part of the ASSIST program, in turn, devoted more resources to tobacco control than did other states except Massachusetts and California, and they showed in aggregate a 7% reduction in tobacco consumption per capita from 1993 to 1996 compared to non-ASSIST states.13 Such a “dose-response” effect is strong evidence that state programs have an impact; that more tobacco control correlates with less tobacco use, and that the reduction coincides with the intensification of tobacco control efforts.
A second line of evidence comes from observing effects on tobacco consumption beyond those associated with price. When tobacco prices rise, sales should drop, and when prices drop, sales should rise. Yet price alone does not explain the observed consumption patterns. In the first 2 years after Oregon’s ballot initiative was implemented, for example, cigarette consumption dropped by over 11%, which is 5% more than would be expected from the price increase alone.14 The recently reported decreases in tobacco use in Alaska, California, and Florida similarly exceed what would be expected from price increases alone. Moreover, when cigarette prices dropped nationwide during 1992–1994, consumption rose in states with small tobacco control efforts but did not rise in 11 of 14 ASSIST states;15 consumption also plateaued in California and Massachusetts. This suggests that tobacco control measures limited the increase in tobacco sales expected as a result of a price drop.
In the review of tobacco control program elements that follows, results are reported in ranges, and sometimes those ranges are large. It is generally quite diffi-cult to attribute a reduction in tobacco use to any single factor; often, many factors work in parallel. The underlying message is quite clear, however: Multifaceted state tobacco control programs are effective in reducing tobacco use.
Counteradvertising and Education
Counteradvertising and public education campaigns have become standard elements of tobacco control, although their funding levels and aggressiveness vary considerably among the states. Counteradvertising campaigns can convey a variety of messages and can be aimed at different audiences. An evaluation of the California tobacco control program concluded that it
was most effective in its early years, when the highest-impact advertisements emphasized deceptive practices undertaken by tobacco firms.16 Evaluators concluded that the program became less effective when spending for counteradvertising dropped (from $16 million in 1991 to $6.6 million by 1995), and when the advertisements began to focus on health risks rather than tobacco industry practices.17 As a result, the program’s advisory committee made its foremost 1997 goal to “vigorously expose tobacco industry tactics.”18 A “natural experiment” under way in Florida may provide further insight. The Florida Pilot Program, funded by that state’s tobacco settlement, created the edgy “Truth Campaign” and SWAT (Students Working Against Tobacco) program. During its first year, tobacco use among youths decreased dramatically. The second-year budgets for both programs were seriously threatened in the Florida legislature—at one point facing extinction—but funding was partially restored. The program director was removed and the counteradvertising campaign was said to be heading “in a new direction.”19 The budget for public media is slated to drop from $24 million to $18 million in the second year. If the rate of decline in tobacco consumption among youths stalls in Florida, as it did in California after 1994, this would provide further evidence that the “dose” of tobacco control predicts its impact.
School-based tobacco prevention programs are also part of state tobacco control programs. The effectiveness of school-based programs varies. They are most effective when the message is delivered repeatedly and is taken as seriously and promoted as powerfully as are other forms of drug abuse education. Properly implemented school programs can, however, lower smoking prevalence from 25% to 60%.20 These programs have been evaluated repeatedly,21 and in 1994 CDC produced a set of guidelines for school-based programs.22 States will want to take care in implementing school-based programs, however, because they can consume considerable resources to little effect; a 1996 meta-analysis showed only a modest impact for most programs. The 1994 Institute of Medicine report Growing Up Tobacco Free noted the variable results of school-based programs but concluded that they should be part of a comprehensive tobacco control strategy because educating school-age children and adolescents about the consequences of tobacco use is clearly important to sustain a smoke-free norm.23
Experimentation with the content and style of counteradvertising and education programs will and should continue, subject to evaluation to enable improvements and increase their impact. With that in mind, the American Legacy Foundation is being established with funding from the Master Settlement Agreement. Its duties will include funding and oversight of a national counteradvertising campaign. Many states are also planning major increases in their counteradvertising and education initiatives.
Establishing Smoke-Free Workplaces and Public Spaces
The main impetus for smoke-free environments grew from concern about exposing nonsmokers to the toxic effects of tobacco smoke. Making worksites, schools, and homes smoke-free zones is a
powerful strategy for reducing tobacco use overall because it boosts quit rates and reduces consumption.24 A 1996 review, for example, estimated that smoke-free workplaces reduced the number of smokers by 5% on average (meaning that almost one in five smokers quit, as smoking prevalence is about 25%) and reduced use among continuing smokers by 10%.25 Another review attributed over 22% of the tobacco consumption drop in Australia between 1988 and 1995, and almost 13% of the drop in the United States between 1988 and 1994, to smoke-free workplace policies.26 The death toll and ill-health attributable to involuntary smoking are thoroughly documented in a Surgeon General’s report, a report from the federal Environmental Protection Agency (EPA), and a study by the California EPA.27 Federal regulations prohibit smoking in federal buildings and in airplanes. In some states and localities, laws and ordinances proscribe smoking in workplaces, schools, public spaces, restaurants, and other sites. Creating smoke-free workplaces and public spaces reduces tobacco use among smokers while reducing involuntary smoking by nonsmokers.28 Smoking restrictions have been a major focus of some states’ tobacco control efforts and are a central thrust of much activity at the county and city levels.
Increasing Prices Through Taxation
Raising the price of tobacco products through taxation is one of the fastest and most effective ways to discourage children and youths from starting to smoke and to encourage smokers to quit.29 In 1994 and 1998, the Institute of Medicine recommended price increases of $2 per pack (or equivalent for other tobacco products), based on levels needed to approach the health goals in Healthy People 2000 and to approach parity with other countries that have effective tobacco control programs. Wholesale prices have increased an average of $0.65 per pack nationwide since the Master Settlement Agreement was signed in 1998, the federal excise tax was raised to $0.24 per pack in the Balanced Budget Act of 1997, and six states now have excise taxes over $0.75 per pack. Even high-tax states remain short of the Institute’s recommended level, however, and 20 states have excise taxes below $0.20 per pack. The wholesale price and excise tax increases do not necessarily imply equal increases in retail prices that consumers see, as discounts to retailers are commonplace for tobacco products, and local business factors are important. It is nonetheless clear that the floor for prices has risen, even if the ceiling is variable.
Economists have reached a consensus that a cigarette price increase of 10% will decrease total consumption by about 4%. Most economists now believe the response is larger (i.e., about 8%) among youths, based on recent studies. Conclusions about whether price disproportionately affects children and youths are based on fewer data than larger studies of total tobacco consumption. A classic 1990 study showed that responsiveness to price (elasticity of demand) increased over time from 1970 to 1985 but found little difference between adults and youths.30 A more recent review of more elaborate studies showed elasticities in the range noted above; it also found that youths were more
sensitive to price, as demonstrated by fewer youths starting to smoke and reduced consumption among continuing youth smokers.31 An April 1998 report from the Congressional Budget Office reviewed many studies of price and consumption. It found unequivocal evidence that increased prices reduce use, although details about the mechanisms and effects are not completely understood.32
Proposals to increase cigarette taxes face strong opposition. (Interestingly, tobacco taxes are one of the few taxes for which a majority of Americans favor increases, especially if the revenues derived are dedicated to tobacco control.33) The principal policy concern is that tobacco taxes are regressive, because tobacco use is more common among people with low incomes, and thus the poor spend proportionately more of their incomes on cigarettes. Tax increases are actually less regressive than simple projections suggest, however, because the poor are more sensitive to price and their consumption falls more sharply when prices rise. The World Bank supports increasing tobacco excise taxes for its public health impact and notes that judgments about regressiveness “should be over the distributional impact of the entire tax and expenditure system, and less on particular taxes in isolation.”34
Governors and legislators have raised concerns about increasing prices on tobacco because revenues from excise taxes might drop, along with payments expected under the Master Settlement Agreement (because payments to states are tied to sales). States concerned about revenue loss have an effective option—raising the state excise tax rate. The World Bank notes that “empirical evidence shows that raised tobacco taxes bring greater [overall] tobacco tax revenues.”35 Reduced consumption will also ultimately lead to lower health costs to states through Medicaid and other health programs. In one study, the health benefits due to lower rates of heart attack and stroke began quickly, and the health benefits more than offset the program’s costs after 1 year.36 The immediate economic and health benefits are later compounded by reductions in cancer and other chronic diseases.
Supporting Treatment Programs for Tobacco Dependence
Nicotine addiction, like other addictions, is a treatable condition. Treatment programs for tobacco dependence can work. States have two major roles in treating tobacco dependence: (1) educating tobacco-dependent people about their treatment options through public health programs, and (2) ensuring that medical programs cover and reimburse the costs of the treatments. As of 1997, only 22 states and the District of Columbia covered such treatment under Medicaid, leading to a recommendation that state Medicaid agencies “incorporate explicit language into their managed-care contracts, policy briefs, lawsuit provisions, and Medicaid formularies.”37 States can take guidance on policies to improve tobacco treatments from a report by the Center for the Advancement of Health.38
Community-based resources such as centralized “quitlines” and workplace wellness programs can increase access to cessation programs. State governments are among the largest employers in most
states, and a major employer in all. States can ensure that their employees have access to treatment through their health plans, and smoking bans in state buildings can increase cessation and reduce tobacco use among continuing smokers. States can also pass laws to create smoke-free businesses, public buildings, and worksites. State and local media campaigns that reinforce nonsmoking norms also enhance motivation to quit, reduce tobacco use among those who continue to smoke, and prevent relapse.39
Much can be done to improve access to and the effectiveness of treatment programs within medical systems. More than 70% of smokers visit a primary health care provider at least once a year. Systematic reviews conclude that routine, repeated advice and support can increase smoking cessation rates by 2- to 3-fold.40 Physicians, nurses, psychologists, dentists, and other health professionals are more likely to give such advice and support if they practice in a system that encourages such behavior through practice-based systems for tracking smoking status, office-based written materials for smokers to take home, training of health professionals in screening and advising patients, coverage of cessation programs by health plans, and reimbursement for treatments by payers (including Medicaid).
Most people who use tobacco—at all ages—express a desire to quit, but only a small fraction succeed on their own. Although many who do quit do so without formal treatment, treatment clearly improves cessation rates. Controlled studies generally report 30%–35% cessation rates at 1 year for intensive treatments and 10%–20% cessation rates for less-intensive treatments.41 Treatment for addiction to tobacco products ranks high in cost-effectiveness among health program spending options.42 Programs that combine behavioral therapies with pharmacotherapies (i.e., medications) have the best results, and evidence-based guidelines recommend that all smokers should be offered both. Behavioral programs can be delivered in group settings (in person) or individually (in person or by telephone). FDA-approved medications include nicotine replacement agents (in gum, patch, nasal spray, or inhaler delivery systems) and the antidepressant drug bupropion.
Treatment works, but there is ample room for improvement. Despite evidence of its effectiveness, relatively few smokers seek out formal treatment, and relapse rates are high. Improving smoking cessation success rates would be especially important in certain target populations. For example, Massachusetts placed an emphasis on reducing smoking among pregnant women because it would produce long-lasting benefits for the prospective mothers and reduce risks to their children. As a result, the number of mothers who smoked during pregnancy dropped by almost 48% during 1990–1996, a rate far ahead that of any other state.43
Enforcing Youth Access Restrictions44
It has long been illegal—in every state—to sell tobacco products to minors, but until recently, enforcement was lax. The federal Synar Amendment ties federal block grant monies to improved compliance with state laws proscribing such sales. States risk reduced payments from
the Substance Abuse and Mental Health Administration if they fail to meet compliance targets. The federal government has never withheld state funds based on the Synar Amendment, but such withholding is under discussion for several states that have not met Synar targets. Enforcement of youth sales, with mandatory ID-card inspection of those 26 and younger, was the central thrust of a 1996 FDA tobacco regulation. This part of the regulation remains in force pending a U.S. Supreme Court ruling about FDA’s jurisdiction over tobacco products. States now have FDA contracts to enforce and monitor youth sales. Several reports have noted that enforcing laws against sales to minors can reduce tobacco consumption.45 Although one 1997 study of enforcement showed no decline in youth smoking,46 the authors attributed the lack of impact to insufficient merchant compliance47 and developed a model approach that is being used in Massachusetts.48 Excessive focus or exclusive reliance on youth access restrictions can siphon resources and political will from more powerful tobacco control measures.49 Yet all U.S. jurisdictions have youth access laws, and if those laws are to become meaningful, they must be enforced.50
Monitoring Performance and Evaluating Programs
Today’s tobacco control programs build on decades of research and demonstrations. The scale and scope of tobacco control in the United States—particularly in the most aggressive states—has grown considerably over the past decade, and the proper balance and content of program elements are the subjects of continuing debate. Tobacco control can improve over time only if (a) its elements are assessed, (b) state programs that choose different strategies are compared, and (c) research to improve the programs is carried out. Governors and state legislators, moreover, need to be able to be accountable for the use of public dollars. This does not imply that results will be quick; significant reductions in tobacco use take years even in states where tobacco control has clearly been effective.
Performance monitoring of public health programs is receiving increased attention.51 Measures to monitor the performance of tobacco control programs are in place, and efforts are under way to improve them.52 Without specified goals and ways of measuring progress, the effectiveness of public monies spent on such programs is hard to judge, so state tobacco control programs should include resources for evaluation and research as part of a comprehensive tobacco control program.
Conclusions
-
Tobacco control programs can reduce tobacco use, thus saving lives.
-
Tobacco control programs can incorporate many different elements modeled on existing state programs that have proved effective.
-
The effects of counteradvertising and education depend on their “intensity” and “dose.”
-
Smoke-free worksite policies reduce illness and death from involuntary smoking, increase smoking cessation, and
-
reduce consumption among continuing smokers.
-
Raising excise taxes on tobacco products can reduce tobacco use while increasing state revenues.
-
Tobacco addiction is treatable, and treatment programs are cost effective.
-
The enforcement of youth access laws will not achieve its full potential impact until merchant compliance rates are high.
-
To ensure accountability and enable future improvements in tobacco control programs, state tobacco control programs must be evaluated and have explicit goals coupled to performance measures.
![]()
Notes
|
1. |
The Institute of Medicine (IOM) examined state tobacco control efforts in Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youths, B.S.Lynch and R.J.Bonnie, eds., Washington, D.C.: National Academy Press, 1994 (www.nap.edu/catalog/4757.html), as did the National Cancer Policy Board in Taking Action to Reduce Tobacco Use, Washington, D.C.: National Academy Press, 1998 (www.nap.edu/catalog/6060.html). |
|
2. |
Health and cost statistics are from the Office of Smoking and Health, Centers for Disease Control and Prevention (CDC) web site, www.cdc.gov/tobacco. The Master Settlement Agreement is available through the National Association of Attorneys General at www.naag.org/tob2.htm. |
|
3. |
Wingo P.A., Ries L.A.G., Giovino G.A., et al. Annual report to the nation on the status of cancer, 1973–1996, with a special section on lung cancer and tobacco smoking. Journal of the National Cancer Institute 91:675–690, 1999. |
|
4. |
Centers for Disease Control and Prevention. Incidence of initiation of cigarette smoking—United States, 1965–1995. Morbidity and Mortality Weekly Report 47(39):837–840, 1998. |
|
5. |
Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs. Atlanta: CDC, 1999 (www.cdc.gov/tobacco/bestprac.htm). |
|
6. |
Centers for Disease Control and Prevention, general materials (www.cdc.gov/nccdphp/osh/pubs1.htm) and technical reports (www.cdc.gov/nccdphp/osh/pubs2.htm). |
|
7. |
The model legislation is available from the Advocacy Institute web site at www.advocacy.org/stf/glantz.htm. |
|
8. |
Campaign for Tobacco-Free Kids, “Statewide Programs,” (www.tobaccofreekids.org/html/statewide_programs.html), 1999; Coalition for a Tobacco-Free Pennsylvania and Governor Tom Ridge, press release, 1999; The Gallup Organization, Final Technical Report: Independent Evaluation of the California Tobacco Control Prevention and Education Program, Methods and Procedures, Wave I Data, 1996–1997, and Final Technical Report: Independent Evaluation of the California Tobacco Control Prevention and Education Program, Wave I Data, 1996–1997, Rockville, Md.: Author, 1998; Centers for Disease Control and Prevention, Best Practices…, op. cit.; Centers for Disease Control and Prevention, Office of Smoking and Health, “State and National Tobacco Control Highlights” (www.cdc.gov/tobacco/statehi/statehi.htm), 1999; State of Arizona, Office of the Auditor General, Performance Audit: Department of Health Services’ Tobacco Education and Prevention Program, Phoenix, 1999; Minnesota Health Improvement Partnership Tobacco Work Group, Tobacco Use |
|
|
Prevention and Reduction in Minnesota: Elements, Roles, and Costs of a Comprehensive Approach, St. Paul: Minnesota Department of Health, 1999; Oregon Department of Human Resources, Oregon Health Division, “Tobacco Prevention and Education Program Report,” Portland, 1999; Attorney General’s Task Force, “A Comprehensive Tobacco Prevention and Control Plan for Washington State,” (www.wa.gov:80/ago/pubs/tobacco.pdf), 1998; Institute of Medicine, Growing Up Tobacco Free, op. cit.; Meeting materials, Task force to end smoking in Maryland 1999; California Department of Health Services, Toward a Tobacco-Free California: Renewing the Commitment, 1997– 2000, Sacramento: Author, 1999; Pierce J.P., Gilpin E.A., Emery S.L., White M.M., Rosbrook B., and Berry C.C., Has the California tobacco control program reduced smoking? Journal of the American Medical Association 280(10):893–899, 1998; Tobacco Control Program, A Model for Change: The California Experience in Tobacco Control, Sacramento: California Department of Health Services, 1998; Abt Associates, Independent Evaluation of the Massachusetts Tobacco Control Program: Third Annual Report Summary (1996), and Fourth Annual Report (1998), Cambridge, Mass.: Author, 1998; National Cancer Policy Board, Taking Action, op. cit.; National Association of Attorneys General, “Tobacco Settlement Summary” (www.naag.org/glance.htm), 1999; Pierce J.P., Gilpin E.A., Emery S.L., et al., Tobacco Control in California: Who’s Winning the War? An Evaluation of the Tobacco Control Program, 1989–1996, La Jolla: University of California at San Diego, 1998; Florida Department of Health, Office of Tobacco Control, Florida Youth Tobacco Survey Reports 1 through 8 (April-December 1998) and Vol. 2, Report 1 and supplement (April and March 1999). |
|
9. |
Epstein J., Garcia J., and Lynch B. Advocating for State Tobacco Control: An American Cancer Society Planning Guide. Atlanta: American Cancer Society, 1998. |
|
10. |
Data presented at a National Cancer Policy Board workshop by Marc Manley, National Cancer Institute; Dileep Bal, California Department of Health Services; and Carolyn Celebucki, Massachusetts Department of Public Health; July 15, 1997 (www.national-academies.org/cancerbd). |
|
11. |
Pierce et al., Tobacco Control, and “Has the California…,” op. cit. |
|
12. |
Biener L.W. Progress Toward Reducing Smoking in the Commonwealth of Massachusetts from 1993 Through FY 1999. Boston: Center for Survey Research, University of Massachusetts at Boston, 1999. |
|
13. |
Manley M.W, Pierce J.P, Gilpin E.A, Rosbrook B., Berry C., and Wun L.M. Impact of the American Stop Smoking Intervention Study on cigarette consumption. Tobacco Control 6(Suppl. 2):S12–S16, 1997. |
|
14. |
Centers for Disease Control and Prevention. Decline in cigarette consumption following implementation of a comprehensive tobacco prevention and education program—Oregon, 1996–1998. Morbidity and Mortality Weekly Report 48(7):140–143, 1999. |
|
15. |
Manley, “Impact of the American…,” op. cit. |
|
16. |
Pierce et al., Tobacco Control…and “Has the California…,” op. cit. |
|
17. |
Pierce et al., ibid. |
|
18. |
Tobacco Education and Research Oversight Committee (California). Recommendation, 1997–2000. Sacramento: California Department of Health Services, 1997. |
|
19. |
Givel M.S. and Glantz S.A. Tobacco Industry Political Power and Influence in |
|
|
Florida, 1979–1999. San Francisco: University of California at San Francisco, 1999. |
|
20. |
Centers for Disease Control and Prevention, Best Practices…, op cit., p. 16. |
|
21. |
Glynn T., Essential elements of school-based smoking prevention programs, Journal of School Health 59:181–188, 1989; Institute of Medicine, Growing Up Tobacco Free, op. cit.; Centers for Disease Control and Prevention, Preventing Tobacco Use Among Young People: A Report of the Surgeon General, Washington, D.C.: U.S. Department of Health and Human Services, pp. 209–292, 1994 (www.cdc.gov/tobacco/sgryth2.htm); Rooney B.L. and Murray D.M., A meta-analysis of smoking prevention programs after adjustment for errors in the unit of analysis, Health Education Quarterly 23:8–64, 1996. |
|
22. |
Centers for Disease Control and Prevention. Guidelines for School Health Programs to Prevent Tobacco Use and Addiction. Atlanta: CDC, 1994 (www.cdc.gov/nccdphp/dash/nutptua.htm). |
|
23. |
Institute of Medicine, Growing Up Tobacco Free, op. cit.; Rooney and Murray, “A meta-analysis…” op. cit. |
|
24. |
Glantz S.A. Back to basics: Getting smoke-free workplaces back on track. Tobacco Control 6:164–166, 1997. |
|
25. |
Evans W.N., Farrelly M.C., and Montgomery E. Do Workplace Bans Reduce Smoking? (NBER Working Paper No. W5567) Cambridge, Mass.: National Bureau of Economic Research, 1996 (papers.nber.org/papers/W5567). |
|
26. |
Chapman S., Borland R., Scollo M., Brownson R.C., Dominello A., and Woodward S. The impact of smoke-free workplaces in declining cigarette consumption in Australia and the United States. American Journal of Public Health 89:1018–1023, 1999. |
|
27. |
Centers for Disease Control, The Health Consequences of Involuntary Smoking: A Report of the Surgeon General, Washington, D.C.: U.S. Department of Health and Human Services, 1986; U.S. Environmental Protection Agency, Respiratory Health Effects of Passive Smoking: Lung Cancers and Other Disorders, Washington, D.C.: EPA, 1992; California Environmental Protection Agency, Health Effects of Exposure to Environmental Tobacco Smoke: A Report of the California Environmental Protection Agency, Smoking and Tobacco Control Monographs No. 10 (NIH Pub. No. 99–4645), Bethesda, Md.: National Cancer Institute, 1999. |
|
28. |
Stillman F.A., Becker D.M., Swank R.T., et al., Ending smoking at the Johns Hopkins Medical Institutions, Journal of the American Medical Association 264(12):1565–1569, 1990; Grigham J., Gross J., Stitzer M.L., and Felch L.J., Effects of a restricted work-site smoking policy on employees who smoke, American Journal of Public Health 84:773–778, 1994; Kinne S., Kristal A.R., White E., and Hunt J., Work-site smoking policies: Their population impact in Washington State, American Journal of Public Health 93:1031–1033, 1993; Woodruff T.J, Rosbrook B., Pierce J., and Glantz S.A., Lower levels of cigarette consumption found in smoke-free workplaces in California, Archives of Internal Medicine 153(12):1485–1493, 1993; Brenner H. and Fleischle B., Smoking regulations at the workplace and smoking behavior: A study from southern Germany, Preventive Medicine 23:230–234, 1994; Jeffery R.W., Kelder S.H., Forster J.L., French S.A., Lando H.A., and Baxter J.E., Restrictive smoking policies in the workplace: Effects on smoking prevalence and cigarette consumption, Preventive Medicine 23:78–82, 1994; Farrelly M.C., Evans W.N., and Sfekas E.S., The impact of workplace smoking bans: Results from a national survey, Tobacco |
|
|
Control 8:272–277, 1999; Farkas A.J., Gilpin E.A., Distefan J.M., and Pierce J.P., The effects of household and workplace smoking restrictions on quitting behaviors, Tobacco Control 8:261–265, 1999; Evans et al., “Do workplace bans…,” op cit. |
|
29. |
Chaloupka F. and Warner K., The Economics of Smoking, in A.J.Culyer and J.P. Newhouse, eds., The Handbook of Health Economics, New York: Elsevier Science, in press, or contact Kenneth Warner, University of Michigan School of Public Health; Institute of Medicine, Growing Up Tobacco Free, op. cit., chapter 6. |
|
30. |
Wasserman J., Manning W.G., Newhouse J.P., and Winkler J.D. The effects of excise taxes and regulations on cigarette smoking. Journal of Health Economics 10:43–64, 1991. |
|
31. |
Chaloupka F.J. and Grossman M.Price, Tobacco Control Policies, and Youth Smoking (NBER Working Paper W5740). Cambridge, Mass.: National Bureau of Economic Research, 1996 (papers.nber.org/papers/W5740). |
|
32. |
Congressional Budget Office. The Proposed Tobacco Settlement: Issues from a Federal Perspective. Washington, D.C.: U.S. Government Printing Office, 1998 (www.cbo.gov/showdoc.cfm?index=407&sequence=0&from=1). |
|
33. |
Chaloupka and Warner, “The Economics of Smoking…,” op cit. |
|
34. |
World Bank. Curbing the epidemic: Governments and the economics of tobacco control. Tobacco Control 8:196–201, 1999. |
|
35. |
World Bank, ibid. |
|
36. |
Lightwood J.M. and Glantz S.A., Short-term economic and health benefits of smoking cessation: Myocardial infarction and stroke. Circulation 96:1089–1096, 1997. |
|
37. |
Barker D.C., Orleans C.T., and Schauffler H.H. Tobacco treatment services should be covered under Medicaid. Tobacco Control 7:92, 1998. |
|
38. |
Center for the Advancement of Health. Treating Tobacco Dependence in the U.S. Washington, D.C.: Author, 1998 (www.cfah.org/tobacco.htm). |
|
39. |
Glantz, “Back to basics…,” op. cit.; Stillman et al., “Ending smoking…,” op. cit.; Grigham et al., “Effects of a restricted …,” op. cit.; Kinne et al., “Work-site smoking policies…,” op. cit.; Woodruff et al., “Lower levels of cigarette consumption…,” op. cit.; Brenner and Fleischle, “Smoking regulations…,” op. cit.; Jeffery et al., “Restrictive smoking policies…,” op. cit.; Farrelly et al., “The impact of workplace smoking bans…,” op. cit.; Farkas et al., “The effects of household…,” op. cit.; Evans et al., “Do Workplace Bans…,” op. cit. |
|
40. |
Curry S.J. Cessation from tobacco use. Cancer Causes and Control 8(Suppl. 1):S9–S11, 1997. |
|
41. |
An evidence-based guideline was published by the Agency for Health Care Policy and Research: Fiore M.C., Bailey W.C., Cohen S.J., et al. Smoking Cessation: Clinical Practice Guideline No. 18 (AHCPR Pub. No. 96–0692). Rockville, Md.: U.S. Department of Health and Human Services, 1996. The guideline is currently being revised under a contract from the National Cancer Institute to the Medical College of Wisconsin. For a review of cessation programs and statistics, see Curry, ibid., and Institute of Medicine, Growing Up Tobacco Free, op. cit., chapter 5. |
|
42. |
Cromwell J., Bartosch W.J., Fiore M.C., Hasselblad V., and Baker T., Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Journal of the American Medical Association 278(21):1759–1766, 1997; Warner K.E., Cost-effectiveness of smoking-cessation therapies: Interpretation of the evidence and |
|
|
implications for coverage, Pharmaco-economics 11(June):538–549, 1997. |
|
43. |
G.Connolly and D.Turner-Bowker, Massachusetts Department of Public Health Tobacco Control Program, personal communication, November 18 and 22, 1999, citing National Vital Statistics Report 47(10), November 19, 1998 (Centers for Disease Control and Prevention). |
|
44. |
The history of youth access proscriptions and the Synar Amendment is reviewed in Institute of Medicine, Growing Up Tobacco Free, op. cit., chapter 7; the FDA regulation is available on line at www.fda.gov/opacom/campaigns/tobacco.html. |
|
45. |
Jason L.A., Ji P.Y., Anes M.D., and Birkhead S.H., Active enforcement of cigarette control laws in the prevention of cigarette sales to minors, Journal of the American Medical Association 266(22):3159–3161, 1991; DiFranza J.R., Carlson R.R., and Caisse R.E., Reducing youth access to tobacco, Tobacco Control 1:92, 1992; Forster J.L., Murray D.M., Wolfson M., Blaine T.M., Wagenaar A.C., and Hennrikus D.J., The effects of community policies to reduce youth access to tobacco, American Journal of Public Health 88:1193–1198, 1998; for a review, see Institute of Medicine, Growing Up Tobacco Free, op. cit., chapter 7. |
|
46. |
Rigotti N.A., DiFranza J.R., Chang Y., Tisdale T., Kemp B., and Singer D.E. The effect of enforcing tobacco-sales laws on adolescents’ access to tobacco and smoking behavior. New England Journal of Medicine 334:1044–1051, 1997. |
|
47. |
DiFranza J.R. and Rigotti N.A. Impediments to the enforcement of youth access laws. Tobacco Control 8:152–155, 1999. |
|
48. |
DiFranza J.R., Celebucki C.C., and Seo H.G. A model for the efficient and effective enforcement of tobacco sales laws. American Journal of Public Health 88:1100–1101, 1998. |
|
49. |
Glantz S.A. Editorial: Preventing tobacco use—the youth access trap. American Journal of Public Health 86:156–158, 1996. |
|
50. |
Institute of Medicine, Growing Up Tobacco Free, op. cit. |
|
51. |
The theory and some examples are described in Institute of Medicine, Improving Health in the Community: A Role for Performance Monitoring, J.S.Durch, L.A.Bailey, and M.A.Stoto, eds., Washington, D.C.: National Academy Press, 1997, and applied to tobacco control on pp. 11–17 of Taking Action to Reduce Tobacco Use (see Note 2). The Centers for Disease Control and Prevention’s Best Practices report (see Note 5) is a much more detailed application, with state-by-state benchmarks. |
|
52. |
Davis R.M., An overview of tobacco measures, Tobacco Control 7(Suppl.):S36–S40, 1998; Wakefield M.A. and Chaloupka F.J., Improving the measurement and use of tobacco control “inputs,” Tobacco Control 7:333–335, 1998; Alciati M.H., Frosh M., Green S.B., et al., State laws on youth access to tobacco in the United States: Measuring their extensiveness with a new rating system, Tobacco Control 7:345–352, 1998; Centers for Disease Control and Prevention, Best Practices…, op. cit.; National Cancer Policy Board, Taking Action…, op. cit., pp. 11–18; Center for the Advancement of Health, Development of Tobacco Performance Indicators for Managed Care, Washington, D.C.: Author (www.cfah.org). |














