5
Immunization Finance Policies and Practices
This chapter examines the finance policies and practices that enable the performance of the five roles of the national immunization system discussed in Chapters 2 through 4. Recognizing that immunization is the shared responsibility of the private and public sectors, including federal, state, and local governments, we consider how roles and responsibilities for immunization are distributed across different levels of government. We give particular attention to how current policies and practices establish the set of arrangements used to manage the community health system, target needy groups, ensure accountability within the public and private health care sectors, and allocate costs for these efforts. Our emphasis in this chapter is on children, since childhood immunization initiatives have been a major area of emphasis within the Section 317 program and the exclusive focus of the Vaccines for Children (VFC) effort. Although the federal government has established national goals to improve the rate of coverage for adult immunization among different age groups and special populations, financial resources to support this effort have been extremely limited and remain largely undocumented at the federal and state levels.
When public health clinics served as the primary point of service for delivering immunizations directly to disadvantaged populations, they had self-contained programs that performed multiple functions, including the purchase and administration of vaccines, the measurement of infectious disease patterns, the analysis of vaccine coverage rates and safety concerns, the development of programs to improve immunization
coverage, and the performance of immunization policy and leadership roles within their communities. The public clinics were able to draw on patient revenues for specific services to help finance multiple types of public health activities.
The emphasis on providing vaccines as a fundamental part of primary health care in the private sector and the creation of the VFC program separated these roles. Vaccine purchase and service-delivery responsibilities were shifted largely to the private sector (although many public clinics continue to immunize children under Medicaid contracts and other service arrangements to meet the needs of children in local communities who do not qualify for federal assistance). Public health agencies were expected to sustain their traditional prevention and measurement efforts, while also assuming new responsibilities for administering the VFC program by enrolling private providers and monitoring a much larger set of immunization records. The policy role of public health agencies was thus expanded to include encouragement and oversight of private-sector performance in meeting national immunization goals; however, the VFC program did not provide the additional administrative resources that would enable the exercise of these functions at the local level.
This redefinition of roles and responsibilities occurred during a time when federal resources for state immunization infrastructure efforts were diminishing, and greater reliance was being placed on the states and the private sector to meet national health needs. States took on new responsibilities for the health care of infants and children through programs such as the State Children’s Health Insurance Program (SCHIP), for example, which provided greater opportunity to work with managed care organizations in providing primary health care services (including immunizations) for Medicaid families.
These transitions and shifts in roles and responsibilities have resulted in ambiguity with regard to leadership, measurement, and finance responsibilities for the national immunization system. Resolving this ambiguity will require careful consideration of the level of oversight and resources necessary to ensure that the private and public health sectors can each contribute effectively in addressing national immunization needs. The new system of private-sector responsibility for clients who were once served by public health clinics is still evolving, and an array of issues is emerging that requires careful consideration before judgments are made about the successes or limitations of this new approach. In this context, the following sections review in turn the immunization roles and responsibilities and associated finance policies and practices of the private sector, local health departments, the states, and the federal government.
PRIVATE-SECTOR ROLES AND RESPONSIBILITIES
As noted earlier, most children receive their immunization services today from a private health care provider. Although the federal and state governments purchase more than half of the childhood vaccines distributed in the United States, private-sector health plans play an equally important role in determining how immunizations are delivered and influence how the costs of vaccine purchase, vaccine administration, and record keeping are distributed across the different levels of the immunization system. Three important concerns deserve attention in considering the roles and responsibilities of the private sector within this system: (1) whether immunization is a covered benefit within primary care health plans offered in the private sector, (2) whether private health plans monitor the immunization coverage levels of their members to determine whether their rates are up to date, and (3) whether private health plans are prepared to take action to improve coverage rates if disparities are found within their membership or their members’ communities.
Immunization as a Covered Benefit
Most but not all private health plans include immunizations, but health plans and insurers do not cover all immunizations fully as a covered benefit. Private plans are more likely to cover immunizations for infants and children than for adults.1 A preliminary draft of the Healthy People 2010 report included a goal of increasing to 90 percent the number of 2-year-old children who receive vaccinations as part of comprehensive primary care (baseline: 66 percent in 1996), which would constitute a 50 percent improvement over the year 2000 objectives (Department of Health and Human Services [DHHS], 1998). To achieve this goal, immunizations must be covered within primary care health plans. But even though earlier health objectives (DHHS, 1999) included a proposal to have all private plans cover immunizations fully as a basic benefit (Objective 20.15), many plans do not do so.2
Coverage of adult vaccines as a benefit within private health plans is highly variable and remains largely undocumented. The Healthy People 2010 objectives include increasing the level of coverage to 90 percent for annual influenza vaccinations (baseline: 63 percent in 1997) and for one-time pneumococcal vaccinations (baseline: 43 percent in 1997) for noninstitutionalized adults aged 65 and older (DHHS, 2000). The 2010 objectives also propose increasing the level of coverage to 60 percent for annual influenza vaccinations (baseline: 25 percent in 1997) and for one-time pneumococcal vaccinations (baseline: 11 percent in 1997) for noninstitutionalized high-risk adults aged 18 to 64. However, no initiative has been
announced within the federal or state governments that would advocate mandatory coverage of these vaccines within private health plans.
The National Vaccine Advisory Committee (NVAC) has recommended that the private health sector assume greater responsibility for improving and sustaining high levels of immunization coverage. For example, NVAC concluded in 1999 that the nation’s immunization system is incomplete and cannot ensure the timely vaccination of the 11,000 U.S. infants born each day with a schedule that incorporates newly recommended vaccines (NVAC, 1999a). NVAC offered 15 recommendations for improving the immunization delivery system in both the public and private health sectors, including efforts to expand the scope of immunization coverage in private health plans (NVAC, 1999a). Among these recommendations were the following:
-
All health insurance plans, including Employee Retirement Income Security Act (ERISA) self-insured plans, should offer first-dollar coverage for childhood vaccines recommended in the harmonized immunization schedule (NVAC, 1999a).3
-
Managed care organizations and managed Medicaid plans should ensure complete immunization of their members based on the harmonized schedule. These efforts should include the use of effective strategies to improve and maintain immunization coverage rates, such as reminder and/or recall systems, practice-based coverage assessments, and provider incentives and education (see Chapter 4).
-
All immunization providers, public and private, should assess the immunization coverage levels within their practices annually with assistance from state and local health departments, professional associations, and managed care organizations and other insurers.
One source of continuing uncertainty within both private and public health plans is the changing nature of the recommended immunization schedule (see Chapter 2). The federal government does not set universal immunization standards for the entire population. National recommendations are developed through collaboration among governmental bodies (e.g., the Advisory Committee on Immunization Practices [ACIP]) and professional advisory organizations (e.g., the Committee on Infectious Diseases of the American Academy of Pediatrics [AAP]), whose recommendations influence the scope of coverage benefits within federal programs such as Medicaid/Early and Periodic Screening, Diagnosis, and Treatment (EPSDT), SCHIP, and VFC. These same recommendations are considered by private health plans and state health agencies, which issue guidelines and enact requirements for their own populations, including immunization standards for school entry, day care licensing, and insur-
ance coverage. As a result, immunization coverage requirements are not mandatory, and benefits vary by state and by health plan (see Appendix G).
Difficulties in Achieving Immunization Coverage Goals
In negotiating Medicaid or SCHIP contracts with private health care plans, many states have included immunization rates as key performance measures. Recent legislation, such as the Balanced Budget Act of 1997, has required health maintenance organizations (HMOs) that provide services for public beneficiaries to develop internal quality assurance processes that can be reviewed externally to assess contractor performance in meeting certain goals. To assist this effort, the Health Care Financing Administration (HCFA) has undertaken several quality-of-care activities, including a quality improvement system for managed care (known as QISMC). These initiatives are designed to help the states comply with their legal requirements to develop and implement quality assessment and improvement strategies. Public health officials have technical skills and expertise that can support these initiatives, but financial resources to support collaborative efforts involving HCFA, CDC, and state officials are not readily available within each state.
State health finance agencies can hold providers accountable for outcomes and performance in areas such as quality of care and basic benefits coverage through health contract negotiations as well as the use of incentives or penalties. State officials have indicated, however, that they often avoid adding such requirements to Medicaid health plans because doing so would make the plans unduly burdensome, and could discourage private providers or managed care organizations from participating in Medicaid at all or enrolling hard-to-reach participants. Similarly, private health plans with Medicaid or SCHIP contracts may incur additional costs in the use of evidence-based prevention strategies, such as recall and/or reminder systems, immunization registries, practice-based coverage assessments, and provider education.
In theory, physicians within a managed care system will offer preventive services (including immunization) that reduce the probability of costly illnesses. In the ideal world, managed care’s emphasis on population-based health outcomes, analysis of small-area variations, data tools, provider profiling and accountability, coverage of prevention services, and benchmarking should promote the achievement of high immunization coverage rates for enrolled populations (Mullen, 1999). In practice, however, frequent changes occur in the mix of clients, providers, and health plans. Half of those enrolled in managed care plans do not remain for longer than 3 years. The transience of hard-to-reach patients contributes to a diffusion of responsibility, since providers are not obligated to check
on or improve the immunization status of clients who visit their offices only once.
At present, little compelling evidence has emerged that managed care plans do any better or worse than fee-for-service systems in improving the immunization status of their members (Fairbrother et al., 1996). More important, variations in measurement and the movement of covered populations make it difficult to compare plan performance in improving immunization rates. The exclusion of providers that serve predominantly low-income clients or hard-to-reach groups from enrollment or assessment measures can contribute to positive measures of immunization coverage that suggest good performance. Such exclusionary practices are difficult to detect, especially in the absence of small-area population-based assessments that have sufficient sensitivity to reveal disparities in coverage rates and service utilization patterns among vulnerable groups. The lack of national or state-level trend data for Medicaid and other disadvantaged populations within private health plans (whether capitated managed care organizations or fee-for-service) also makes it difficult to follow immunization coverage rates within high-risk groups. States and local communities thus rely on special population-based studies to monitor coverage rates and to determine whether private plans within their areas are providing immunizations as expected (see Box 5–1). These special studies are generally financed by state public health agencies or CDC; both types of studies are commonly supported by the Section 317 program.
Inconsistencies in the measurement of immunization status within high-risk populations inhibit efforts to monitor community health, as well as the impact of private health plans on client and community outcomes. The absence of reliable data confounds attempts to hold plans accountable for the quality of their performance in improving the health status of their most vulnerable participants.
Several factors make it difficult to monitor service-delivery patterns within the private sector:
-
Large numbers of uninsured and Medicaid families shift between public health clinics and private health plans (often as a result of monthly eligibility determinations), and the scattering of immunization records becomes a significant problem in establishing accountability requirements within multiple health plans. In California, for example, 40 percent of children lose Medicaid each year (Kuttner, 1999; Fairbrother, 2000; Fairbrother, 1999).
-
Most health plans do not provide separate reimbursements to service providers for immunizations that are included in capitation payments for primary care or well-baby services for infants and children.
|
BOX 5–1 Small-Area Analysis for Detroit and Newark Detroit, Michigan, and Newark, New Jersey, are cities with high poverty rates and large minority populations. Detroit residents in particular have problems with access to primary care. The immunization coverage rates of both cities are among the lowest for municipalities in the country and are well below the rates in the rest of their respective states. Detroit’s rate for the 4:3:1 series for 2-year-olds in 1998 was 71.6 percent, while the rate for the rest of Michigan was 80.0 percent; Newark’s rate in the same year was 66.3 percent, while that for the rest of New Jersey was 85.9 percent. In Detroit, a multiyear CDC grant funds the university-based Child Health Network Immunization Project (CHNIP), providing $1.5 million for each of 5 years for innovations in practices designed to improve immunization coverage and for evaluation of these practices. The Detroit Medical Center at Wayne State University initially undertook neighborhood-specific door-to-door surveys to determine local health care resources and access to primary care providers. These surveys represented an effort to identify neighborhoods in which children were most at risk for underimmunization, and thus the most appropriate targets for CHNIP’s outreach and facilitation services. This neighborhood-based assessment was conducted independently of the city’s health department, which has neither the technical nor financial resources needed to conduct this type of study. The Newark health department likewise has not conducted any small-area surveys of immunization coverage or access to primary care in recent years. It has, however, applied to the State of New Jersey for Public Health Priority Funds— state-appropriated monies that must be used for state-identified priorities—to conduct a study of immunization coverage rates within selected neighborhoods. City health officials and leaders appreciate the value of small-area analysis of immunization coverage rates in identifying pockets of need and targeting resources and special interventions accordingly. They frequently lack the resources needed to conduct such special studies and interventions as a routine function, however, and thus depend for this purpose on state and federal initiatives and resources. |
-
Immunizations for adolescents and adults may generate bills, but such data often are not available in a form that would allow comparisons of service patterns across health plans or regions.
-
Although some plans may incur costs for developing and maintaining medical records data, the costs of compiling (or searching) immunization information are not recorded separately. As noted earlier, such compilation can be labor-intensive if records are scattered across multiple health settings.
Improving Performance and Implementing Prevention Methods
Managed care organizations based in large group practices (such as Kaiser Permanente and the Henry Ford Health System) have developed comprehensive medical record databases (often in electronic form) that provide information on a patient’s health history, including immunizations. Such databases create provider performance profiles and, on occasion, may generate reminder-recall notices for immunization updates. Managed care organizations that serve Medicaid and other low-income populations (e.g., those served by SCHIP) expanded rapidly in the 1990s. These plans have less fully developed central patient information systems and contend with disenrollments of around 4 percent per month, often the result of monthly eligibility determinations (Kuttner, 1999; Fairbrother 2000; Fairbrother 1999). Thus, the potential for enrollment-based data systems to improve immunization coverage levels for Medicaid and SCHIP enrollees has not yet been realized.
Furthermore, given competition among various care networks and cost-containment practices of Medicaid managed care providers, data sharing efforts or performance assessment measures will be difficult to implement in the absence of a broader strategic approach that can provide either stability for clients (e.g., 1- or 2-year eligibility periods for services such as Medicaid or SCHIP); stability in the vaccine schedule; or financial incentives for providers so they can commit administrative resources to promoting high immunization coverage rates, the addition of new vaccines, and efforts to cover hard-to-reach populations. Restructuring financial incentives and payment methods for small inner-city practices in particular so they can implement quality improvement and preventive approaches (such as reminder-recall systems) would help mitigate personal and systemic barriers to care for families that already have access to a medical home and a primary care provider.
In ensuring that significant disparities in access to vaccines and coverage do not emerge within vulnerable groups, state public health agencies will need to assume leadership and coordination roles in the assessment, documentation, and improvement of immunization rates in the private sector. Other IOM reports (1988 and 1997) have described in detail the information gathering and analytical functions associated with these roles. Since the delivery of immunization services has shifted from the public to the private sector over the past decade, careful attention will need to be focused on ways to gather and compare data on immunization status, vaccine coverage benefits, and service-delivery costs from both public and private health insurance plans. Key concerns include the following:
-
What is the appropriate measure of coverage of a given population? (the whole population? all of those enrolled with a selected group of providers? those enrolled for a certain length of time with certain providers?)
-
How do we know we have accurate data on selected groups within a given population? What sample size and population characteristics are the appropriate selection criteria?
-
What level of vaccine coverage is an acceptable measure of immunization coverage within a given population?
-
What constitutes a reasonable effort to determine and improve coverage levels within specific population groups?
In addition to the assessment of immunization coverage levels, public health agencies are consistently encouraged to exercise leadership in working with private providers to adopt model strategies (such as routine audits and reminder-recall systems) to maintain high rates of coverage. A recent NVAC report, for example, urges indemnity health and self-insured plans to cover immunization benefits for their members, and recommends that all Medicaid-enrolled providers who immunize children participate in the VFC program (NVAC, 1999a). Despite this encouragement, a national consensus about the implications of not meeting certain performance standards does not yet exist. Who is to be held responsible if a large percentage of Medicaid clients do not acquire immunizations in a timely manner? Who is obligated to ensure that high-risk adults are encouraged to receive influenza and pneumococcal vaccines?
How to finance such assessment, assurance, and leadership roles lies at the crux of the present study. It is clearly in the national interest to have a strong public health system in place nationwide that can provide reliable data and indicators, and support public and private health care providers and local communities in improving their immunization performance. At the same time, private health plans and providers need to share the burden of incorporating prevention efforts into their practices and programs (see Box 5–2). A shared partnership, responsive to local needs and resources, can integrate public health activities within the complex maze of state health finance and health insurance initiatives to improve the health status of vulnerable groups.
Finding 5–1. Child and adult immunization coverage requirements are not mandatory, and benefits vary by state and by health plan. Disparities in covered benefits between public and private health plans and within the private sector make it difficult both to assess immunization levels and to fix responsibility for addressing coverage gaps on a populationwide basis.
|
BOX 5–2 Rochester Private-Public Partnership Approach One example of a coordinated, strategic private-public partnership approach has been demonstrated in Rochester, New York, with favorable results. Szylagyi (1999) prepared a randomized sample of 30,000 charts from Rochester’s 80 pediatric provider practices, and reported 1993 coverage rates as follows: 55 percent in the inner city, 65 percent in the remaining urban areas, and 75 percent in the suburbs. The study tested the impact of an intervention consisting of a tiered reminder-recall-outreach intervention, with outreach (the most expensive approach) targeted to the most hard-to-reach portion (5–10 percent) of the study population. The results of the tiered intervention included a 20 percent increase in immunization coverage and an 11 percent increase in preventive service visits, which had the spillover effect of increasing anemia screening (by 12 percent) and lead screening (8 percent). The same intervention was implemented countywide, and a follow-up survey in 1996 showed significant increases in coverage. The greatest improvements were for inner-city children, whose rates increased from 55 percent in 1993 to 75 percent in 1996. These interventions have been financed by a unique collaboration between the county and state health departments that has allowed county health officials to pool money from several categorical programs. As more clients seek immunizations within their medical homes among private providers, other sources of revenue are able to finance some of the costs of the immunization program. |
Finding 5–2. Responsibility for ensuring the immunization status of selected communities or at-risk groups is currently diffused among multiple parties, including clients themselves, health care providers, health plans, health finance agencies, and public health agencies. Although the assessment of immunization coverage rates within local communities remains a fundamental responsibility of public health agencies, few local or state agencies have sufficient resources to conduct independent studies, and most must rely on data provided by others.
Finding 5–3. Needy populations are increasingly receiving care within the private health sector as Medicaid and SCHIP contract with health plans to provide benefits, including immunizations. However, the absence of reliable indicators of this shift to privately managed care has made it more difficult to monitor immunization coverage levels for the total population as well as vulnerable groups. Both private and public health care providers must be held accountable to a consistent set of measures that can be used to assess and compare their performance in adequately immunizing public program beneficiaries.
Finding 5–4. Collaborative efforts with private health plans and local providers can improve the quality of data available to support assessment studies. However, state health agencies must provide the leadership, technical expertise, and independence that are essential to the integrity of assessment efforts.
Finding 5–5. The private sector plays a significant role in offering immunization benefits and has the capability to implement prevention practices that would improve and sustain immunization coverage rates among vulnerable groups. To exercise this capability, however, the private sector requires assistance and oversight so that accurate immunization coverage rates can be established, and the causes of coverage disparities can be monitored.
Finding 5–6. If immunization assessment is to be enhanced within private provider offices, the private health sector must make behavioral changes that require more than the infusion of federal or state funds. Such efforts must involve partnerships with national, state, and local professional groups and private health plans so that common strategies can be developed and implemented at the local level. States require incentives as well as financial assistance if these public-private partnerships are to be implemented at the local level to improve the quality of local immunization services and sustain high rates of immunization coverage among vulnerable populations.
LOCAL HEALTH DEPARTMENT ROLES AND RESPONSIBILITIES
More than 3,000 public health agencies across the United States provide a broad array of programs and services staffed by technical, administrative, and support personnel within county, metropolitan, and statewide jurisdictions. As noted in an earlier IOM report, the jurisdictions and authority of local health departments overlap, and their service responsibilities and fiscal capabilities are heterogeneous (IOM, 1988). Significant variation exists in their funding sources, ranging from completely state supported to funded exclusively at the local level.
Many states rely on a county system to deliver public health services, and in recent years, many local governments have dealt directly with the federal government to obtain financial assistance in meeting the needs of vulnerable populations. The importance of using federal funds to support local initiatives is reflected in the administration of the Section 317 program within CDC. In addition to the state and other political jurisdiction grants awarded by the National Immunization Program, five metropolitan regions are eligible to receive federal immunization grants (Houston
and San Antonio, Texas; New York City, New York; Chicago, Illinois; and Philadelphia, Pennsylvania).4
The basic responsibility for public health is at the state level, but states differ in the ways in which they administer local public health programs. Some states rely entirely on state employees for local services. Others delegate their responsibilities to county or local health departments that must rely upon local revenues to supplement state resources. In some metropolitan areas, local health departments are larger than the entire public health staff of smaller or more rural states. Some states have highly centralized data collection efforts used to monitor disease outbreaks and vaccination coverage status, while others have only the results of scattered studies within local health departments that can afford to conduct them. Similarly, some states use their own or federal funds to support programs such as Women, Infants, and Children (WIC) linkages or outreach efforts to improve local coverage levels, while such initiatives are supported entirely with local funds in a limited number of jurisdictions.
Infrastructure Investments and Immunization Programs
Prior to the expansion of the Section 317 program in the early 1990s, most local health departments served primarily as providers of immunizations. Only a handful of state agencies were actively involved in data collection, coverage assessment, or partnership initiatives. With the increase in Section 317 funding in the early 1990s and legislative changes that allowed the federal government to support direct services within the states, funds became available for local immunization programs, extensive experimentation with new measurement efforts, and the formation of new public and private partnerships.
According to an informal survey conducted by the National Association of City and County Health Officials (NACCHO), in the early 1990s local health departments used Section 317 funds to develop new immunization programs in such areas as increased assessment, outreach, performance measurement, program linkages, and information management (NACCHO, 1999). Staff time and clinic hours devoted to immunization activities increased in urban areas, and health clinics were established in rural areas and isolated communities to improve access to immunization services. Evening, weekend, and satellite clinics, specialty clinics (hepatitis B and school-based clinics), and partnerships with other organizations such as WIC and Head Start were developed to target hard-to-reach populations. Local health departments also used federal funds to send staff to health fairs, strengthen advertising and public information campaigns, and improve tracking and recall systems used to survey at-risk populations. Incentive programs for patients were established, and staff training
was enhanced to keep all providers up to date on changing vaccines and schedules. More localities had the time and support necessary to become involved in the development of regional immunization registries.
These investments in broader outreach, access, and educational efforts had contributed to a significant increase in immunization coverage rates by the latter part of the decade. National childhood immunization rates increased from 74.2 to 79.2 percent for the 4:3:1:3 series between 1995 (surveying children born between February 1992 and May 1994) and 1998 (surveying children born between February 1995 and May 1997) (information provided by CDC) (see Table 1–2 in Chapter 1). Research has indicated that certain types of programs, especially in such areas as provider record audits, reminder-recall systems, and WIC linkages (see Chapter 4), contributed to the increased coverage rates reported during the past decade.
Impact of Program Cutbacks and Budget Reductions
When federal appropriations for infrastructure grants began to decline in 1996, local budgets for immunization services were substantially reduced, and in some cases eliminated entirely (programs were eliminated, for example, in Duvall County, Florida; Zanesville-Muskingum County, Ohio; Noble County, Ohio; Dakota County, Minnesota; and Hennepin County, Minnesota). In some cases, local governments used local tax dollars to subsidize immunization program activities; in other cases, money was redirected from flexible funding sources or cut from programs and services such as environmental health, home health visits, and WIC clinics (NACCHO, 1999). But few local jurisdictions had sufficient resources to support technical personnel or broad initiatives, and project cutbacks became routine.
Many cities and counties experienced up to a 50 percent reduction in immunization infrastructure funding relative to the original grant funds in the early 1990s (NACCHO, 1999). The decrease in federal funding affected each of the six roles of the immunization system with the exception of vaccine purchase, since the new VFC and SCHIP programs covered the latter costs. For example (NACCHO, 1999):
-
Cutbacks occurred in direct clinical services, resulting in reductions in clinic hours and staff, the closing of entire clinics in some areas, elimination of physician training, and reductions in update notices for private providers.
-
Resources for computer upgrading and maintenance were reduced, slowing the use of electronic records and automated tracking.
-
Community assessment activities were discontinued, diminishing the tracking of immunization coverage levels.
-
Local health departments decreased programs designed to improve immunization coverage rates among hard-to-reach populations, such as home visits and outreach activities.
-
Partnerships with organizations such as WIC and Head Start were discontinued because of the lack of staff time to assist with outreach.
-
Health departments’ capabilities to conduct community education were reduced, and local agencies had fewer resources to assist with regional immunization registries.
In addition, the reduction or elimination of many local program coordinator positions resulted in a loss of leadership that disrupted communication and assistance from state health departments. The resulting delays in obtaining information from state health departments have made it more difficult for local health departments to remain informed about changes in vaccine schedules and to address professional and public concerns in a timely manner. Record and recall systems became increasingly fragmented, and today many health departments no longer conduct full immunization audits of local providers.
In some areas, local health officials responding to the NACCHO survey reported frustration and sometimes resentment with regard to the impact of the federal cutbacks on programmatic efforts. One Western state noted: “As a result of the efforts staff supported through the immunization program, we have been able to raise our immunization rates from 56 percent to almost 90 percent. It seems tragic that funding should be cut when we are finally beginning to see some success” (NACCHO, 1999:1). Similarly, according to a Midwestern state, “It seems ironic that while immunization rates have risen slowly, we know that the last 25–30 percent will be the most difficult to reach, and now funds are cut” (NACCHO, 1999:1).
Cuts in local programs not only reduced public health services, but also decreased the emphasis placed on the importance of adhering to immunization schedules within the private sector. One health official in a Western state reported: “The greatest impact is the loss of sufficient infrastructure to sustain highly effective systems change and to sustain necessary community assessment activities that not only track coverage outcomes, but also served as a source of community opinions and knowledge, attitudes and behaviors” (NACCHO, 1999:2).
Finding 5–6. Local health departments have the capability to play important roles in working with public- and private-sector providers to assess and improve immunization coverage rates. However, they require state and federal assistance to perform these roles.
Finding 5–7. Reductions in federal assistance grants to the states have decreased and sometimes eliminated important local infrastructure efforts in areas related to data collection, technical assistance, immunization assessment, and community outreach.
STATE ROLES AND RESPONSIBILITIES
States have important responsibilities for public health services in general and immunization in particular (IOM, 1994b; IOM, 1988). In particular, they:
-
Adopt policies and practices that influence vaccine coverage and the delivery of immunization services within local jurisdictions (including the adoption of universal purchase policies in 15 states).
-
Create and enforce state mandates for the inclusion of immunization benefits in private health insurance plans.
-
Establish immunization requirements for day care and school entry, as well as long-term health care facilities.
-
Set Medicaid and SCHIP eligibility criteria and provider reimbursement levels within federal requirements, negotiate managed care terms and contracts within the limits of federal mandates, and determine the scope of services to be included in the benefits package above the federal minimum.
-
Distribute publicly purchased vaccines and administer immunizations as part of their responsibility for direct health care for indigent populations.
-
Contract with health plans for state and county employees, set health guidelines for their welfare clients (such as immunization requirements), and provide public health services for the general public.
-
Have historically borne the burden of disease surveillance; containment (initially through the use of quarantines); vaccine safety oversight; and health records management in the areas of infectious disease and, more recently, immunization coverage.
Despite this array of activities, state immunization infrastructure efforts are poorly described in the research literature. States do not track routine expenditures for assessment, assurance, or regulatory activities. The common practice is simply to divide costs between vaccine purchase budgets and program operations as general categories.
Infrastructure Investments and Immunization Programs
Immunization infrastructure encompasses the direct labor, administration, supplies, facilities and equipment, training, and overhead costs
related to each state’s overall program. Every state immunization program is concerned with vaccine purchase and service delivery, but variations exist in the scope of the population that is served and the settings in which services are delivered. In most states, the core mission and basic purpose of the state program are focused solely on children, ensuring that they receive the immunizations recommended by ACIP (Freed et al., 1999). At the same time, the state survey and eight case studies prepared for the present IOM study demonstrated significant variation in state activities that reflect differences in levels of need, resources, and local practices (see Appendixes D and E).
Section 317 Infrastructure Support. The vast majority of infrastructure support for immunization within the states comes through Section 317 grant awards administered by CDC. Following the 1989–1990 measles outbreaks, federal and state officials expressed alarm about the adequacy of existing immunization delivery systems and identified strategies designed to improve immunization coverage rates among vulnerable populations.
In the midst of turbulent health care reform and the expanded reliance on private managed care plans to deliver public health benefits to individuals eligible for federal assistance, the increased budget for Section 317 (1992–1994) and the creation of the VFC program (1994) enabled states to do more to improve immunization coverage levels. In the high-funding years of the Section 317 program, states used their grant awards primarily to expand local services (33 of 50 states) and outreach and education (33 of 50 states) (see Table 5–1). About one-third of the states developed new partnerships with WIC clinics (13 of 50 states) or initiated state or regional registries with encouragement from CDC (16 of 50 states). A few states used their federal grants to improve statewide assessment efforts (7 states), expand vaccination campaigns in general or specialized areas (5 states), or add state staff to assist with coordination and policy development (8 states). In addition to the national studies supported by CDC, 11 states conducted their own immunization coverage surveys during 1995–1997, using methods that included annual birth certificate studies, retrospective school surveys, cluster surveys, and registries (see Box 5–3).
Beyond operating their own programs, many states used their Section 317 funds to monitor and help improve immunization rates within the private sector. These efforts, such as the use of Clinic Assessment Software Application (CASA) audits5 and general management of the VFC program, represent important features of the new roles of public health agencies in assessing and ensuring the quality of private health care services financed through public funds. Yet such efforts are often the most difficult to document because they do not constitute a defined “program” in many public health agencies. The ability of health agencies to
TABLE 5–1 Main Uses of Section 317 Infrastructure Grant Funds in High-Funding Years (1994–1996) a
|
State |
Outreach and Education b |
Assessment |
WIC Linkagec |
Registryd |
Addition of State Staff |
Local Service-Delivery Expansione |
Expanded Vaccination Campaignsf |
|
AL |
✔ |
|
✔ |
|
✔ |
✔ |
|
|
AK |
✔ |
|
✔ |
|
|||
|
AZ |
|
✔ |
✔ |
||||
|
AR |
No specific information; used for activities focused on meeting immunization goals for 2-year-olds |
||||||
|
CA |
✔ |
|
✔ |
|
|||
|
CO |
✔ |
|
✔ |
|
|||
|
CT |
✔ |
✔ |
✔ |
✔ |
|
✔ |
|
|
DE |
|
✔ |
|
||||
|
DC |
✔ |
✔ |
✔ |
|
✔ |
|
|
|
FL |
✔ |
✔ |
|
✔ |
|
||
|
GA |
|
✔ |
|
||||
|
HI |
|
✔ |
|||||
|
ID |
✔ |
✔ |
✔ |
|
|||
|
IL |
✔ |
|
✔ |
|
|||
|
IN |
✔ |
|
✔ |
|
✔ |
✔ |
|
|
IA |
|
✔ |
|
||||
|
KS |
✔ |
|
✔ |
|
✔ |
|
|
|
KY |
|
✔ |
|
||||
|
LA |
✔ |
|
✔ |
|
✔ |
|
|
|
ME |
No information |
|
|||||
|
MD |
✔ |
✔ |
✔ |
✔ |
|
✔ |
|
|
MA |
✔ |
✔ |
|
✔ |
|
||
|
MI |
✔ |
|
✔ |
|
✔ |
|
|
|
MN |
|
✔ |
|
||||
|
MS |
✔ |
|
✔ |
✔ |
✔ |
✔ |
|
|
MO |
|
✔ |
|
||||
|
MT |
✔ |
|
✔ |
||||
|
NE |
✔ |
|
✔ |
|
✔ |
|
|
|
BOX 5–3 Sample of State and Local Immunization Coverage Surveys* Birth Certificate Survey Georgia Mississippi Tennessee Florida Oregon Retrospective School Survey California (this year) Minnesota (performed once “a few years ago”) New York (annual) Kansas Cluster Survey Washington (performed for several counties 2 or 3 years ago) Registry-Based Survey South Carolina Child Health Network New York City (cluster survey) Detroit (cluster survey) Colorado San Diego (random digit dialed survey) |
support management and oversight roles is challenged by programmatic restrictions within federal programs such as VFC, Medicaid, and SCHIP and the absence of general funds at the federal or state level (apart from the Section 317 grants) that can support monitoring and assessment functions. Health agencies realized that they were expected to assume new responsibilities that were difficult to justify and were unable to obtain the necessary resources to exercise this role.
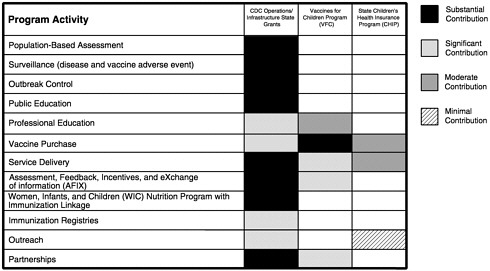
States initially had broad discretion in the use of federal funds, although CDC provided guidance each year to emphasize certain program objectives and priorities. In 1998, CDC announced a set of required activities under 18 program components to guide state programs and to provide a basis for comparison of state efforts (information provided by CDC) (see
Figure 1–5 in Chapter 1). The 18 program components, called “core functions,” are currently used by CDC to track federal and state allocations for immunization activities (information provided by CDC).
Other Federal Support. In addition to categorical grants from federal immunization programs, some states receive funding for immunization-related activities (including vaccine purchase, infrastructure support, or both) through other federal programs (Freed et al., 1999). This type of federal support is very limited, however, and is often focused on a particular program or one-time support, rather than general and ongoing infrastructure support. For example:
-
Four states receive Medicaid matching funds to support registry or outreach activities.
-
Ten states report using Maternal and Child Health (MCH/Title V) block grant funds to support immunization efforts.
-
Four states draw on Public Health Service (PHS) block grant funds for immunization programs.
-
A small number of states draw on other funding sources, including WIC (2 states), Temporary Assistance for Needy Families (TANF) (1 state), and other state/federal grants (4 states).
In a few cases, federal programs require states to carry out certain functions without federal financial support. The VFC program, for example, restricts its expenditures primarily to the purchase and distribution of vaccines. Although some funds are available to coordinate provider enrollment, the VFC program does not support the administration of vaccine products, the recruitment or training of VFC providers, or the records management of immunization coverage levels. By necessity, state public health agencies support VFC administration with other funds, and routinely draw on their Section 317 grants for this purpose.
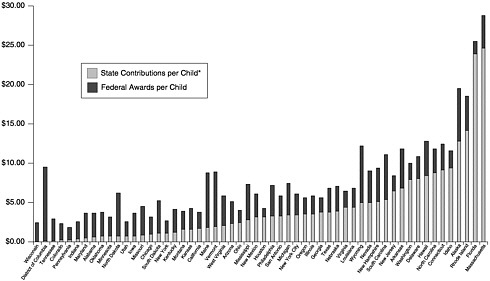
State-Level Funding. CDC first requested estimates of state-level contributions for immunization programs in the proposals for fiscal year (FY) 2000 grants. Self-reports by the states indicated that they expected to provide $109 million for vaccine purchase and $231 million for program operations to support immunization efforts in the year 2000. This figure includes funds provided by other federal agencies that are used within the state for immunization programs, along with state-level revenues and private resources. The state-level contributions are not evenly distributed: half the states (25) directly fund infrastructure support, and 4 of these states have such funding as a substantial portion (more than 40 percent) of their infrastructure budget (Freed et al., 1999) (see Figure 5–1). A few states
provide support for specific initiatives. For example, 15 states have direct or in-kind state funding for registry development (although the size and length of such funding vary).
Twenty-one states do not fund immunization infrastructure, and four recently redirected state funds from vaccine purchase to infrastructure support. More common across states is indirect support of the immunization program through intergovernmental transfers, involving other state or federal programs or services. In addition, many states provide in-kind contributions in the form of assistance from school nurses and secretaries, who conduct school-based assessments of children’s immunization status, and from local health departments (e.g., facilities and overhead, and locally funded staff who perform multiple duties, including the delivery of immunizations) (Freed et al., 1999). Five states mentioned the contributions of volunteers in conducting various immunization activities.
State Finance Practices
State vaccine purchase grants from CDC remained relatively stable during the 1990s (close to about $130 million per year in the period 1996– 1999; see Table 5–2). Although the VFC program assumed responsibility for distributing large quantities of vaccine directly to providers that immunized disadvantaged children, changes in the vaccine schedule and initial uncertainties about the reliability of the VFC program caused state health officials to stockpile surplus vaccines. Reliance on federal funds for vaccine purchase also allowed some states to use their own revenues for other, more risky investments in community assistance and registry programs. In one year (1995), a significant decrease in state vaccine expenses created a surplus of $60 million in the Section 317 vaccine purchase awards, which CDC transferred to state operations/infrastructure support with congressional approval (information provided by CDC).6
Several factors within each state influence levels of public health investment and administrative systems, including demographics (such as population size and urban/rural distribution), per capita wealth, tax revenues, the size of the uninsured populations, and health care traditions (Marquis and Long, 1997). Finance practices may also be affected by the organizational structure of state health programs. For example, in states such as Maryland and Texas, where Medicaid is located administratively or fiscally within the department of health, state agencies used vaccine purchase savings from the implementation of VFC to increase provider reimbursement fees, or to purchase additional vaccine for school health programs or other groups not covered by VFC. In states where Medicaid is not housed within the department of health, VFC savings were commonly not captured within the immunization program, and sometimes
TABLE 5–2 Annual Awards and Expenditures of Section 317 Direct Assistance (DA) Vaccine Purchase Funds (in millions of dollars)
|
Year |
New Funds |
Re-awarded Fundsa |
Total Award |
Expenditures |
Percentage of Total Award Expendedb |
|
1990 |
149.0 |
0.0 |
149.0 |
106.3 |
71% |
|
1991 |
112.9 |
37.5 |
150.3 |
102.5 |
68% |
|
1992 |
156.2 |
26.8 |
183.1 |
121.6 |
66% |
|
1993 |
171.2 |
43.9 |
215.1 |
156.2 |
77% |
|
1994 |
136.2 |
86.3 |
222.5 |
171.9 |
61% |
|
1995c |
83.1 |
74.3 |
157.4 |
96.3 |
59% |
|
1996 |
133.3 |
11.0 |
144.2 |
111.2 |
77% |
|
1997 |
124.0 |
34.7 |
158.7 |
128.4 |
81% |
|
1998d |
108.2 |
34.9 |
143.1 |
135.6 |
95% |
|
1999 |
128.0 |
8.0 |
136.0 |
NA |
NA |
|
NOTE: CDC notes that 1990 was the first year in which grants were administered centrally, instead of by regional offices. There is limited background information with which to substantiate these amounts, and as a result their accuracy is questionable. In 1994, an additional $30,672,686 in appropriated vaccine purchase funds was paid directly to the Department of the Treasury for floor stock excise taxes on behalf of all the grantees when the Vaccine Compensation Act was reauthorized. aFunds awarded in previous years but not obligated. bBased on year-end unobligated balances for 1990–1997 reported to CDC as of April 1, 1999. c$53 million rescinded from unobligated balances in fiscal year 1996 (comprising funds from 1993, 1994, and 1995). dCDC estimates for expenditures and percentage of 1998 award expended. SOURCE: Information provided by CDC. |
|||||
were not protected within the general health budget at all (Freed et al., 1999).
An additional finance issue involves differences in federal and state fiscal years. Legislatures in many states appropriate federal funds, so that expenditures cannot be made until the legislature has approved them. State legislatures do not meet every year in every state. State purchasing and hiring procedures are legal controls of major importance that can delay action in response to federal initiatives. The processes for the preparation and approval of capital budgets and general expenditure budget processes are often separate in many states and involve lengthy and detailed procedures.
States also differ in the extent to which they respond to unmet needs; CDC has reported more than a five-fold variation across states in the
proportion of the population served by health department-operated clinics. Fifteen states have adopted universal purchase policies (see Chapter 3); the remainder contribute a relatively small amount of state funds (i.e., less than 30 percent of total public vaccine purchase in the state) or nothing at all to supply vaccines to disadvantaged adults and children.
In 1994, an earlier IOM committee warned state and federal officials that “current approaches to immunizing children are not sufficient to reach the 1996 target of 90 percent coverage” (IOM, 1994b:26). This prediction was borne out: the overall immunization rate for preschool children (aged 19 to 35 months) increased to just 79.2 percent in 1998 (information provided by CDC). The committee’s report states: “To guide the development of new programs and the allocation of funding and other resources, states must have comprehensive information on children’s unmet needs for immunizations and on the factors that keep them from receiving those immunizations” (IOM, 1994b:26). Recognizing that state needs will vary, the report continues:
No single plan will lead to comprehensive immunization coverage in every state. Common themes may exist, but each state must find a solution that takes into account the specific immunization needs of its children and how its providers and organizational resources can be used to meet those needs. The committee is persuaded that solutions will require state collaboration with local health departments, private providers, state and local chapters of providers’ professional organizations, community groups, and others. States should be exploring how to strengthen primary care to meet not only children’s immunization needs but also their other important health care requirements. (IOM, 1994b:27)
In addressing the finance requirements for this enhanced set of efforts, the report notes: “States are expected to apply CDC funds previously spent on vaccine purchase to improving the infrastructure for delivering immunization services” (IOM, 1994b:22).
The present committee’s analysis of budgetary trends, conducted 5 years after that earlier IOM study, suggests that this expectation has not been realized. In many respects, state immunization programs received mixed messages during the 1990s about the delivery of immunization services. On the one hand, the Childhood Immunization Initiative and the early increases in Section 317 funding encouraged the states to rely on their public health clinics to improve access to immunizations by increasing hours of service, availability of walk-in appointments, mobile service units, immunization fairs, and other activities. Many states directed Section 317 infrastructure funds to these areas by supporting additional staff and equipment (Freed et al., 1999).
At the same time that states were encouraged to use their public clinics to expand access and foster outreach, however, the VFC program and Medicaid reforms created a counteremphasis by promoting immunizations for children in their private medical homes and encouraging greater reliance on managed care organizations to serve populations that once relied on public health clinics. In the majority of states, VFC has made strides in this area, assisted by the increasing penetration of managed care plans, the proliferation of Medicaid managed care plans, and the implementation of SCHIP. Of the 46 states that reported this information in response to the survey conducted for the present study, 40 had experienced decreases in the proportion of children receiving vaccines in the public sector, and some of these decreases were substantial (Freed et al., 1999).
Still, the need for public-sector immunization services has not disappeared. As discussed earlier, most children receive their services from private providers, but the trend toward private-sector immunization delivery is uneven (see Table 5–3). Indeed, the number of doses of vaccine provided in the public sector did not decrease appreciably during the 1990s even though the overall numbers of clients were reduced, a fact that can be attributed to the increase in the number of recommended doses for newborns and adolescents (Freed et al., 1999). Residual needs for vaccine remain in most public clinics, reflecting the realities of serving vulnerable children and adults who have urgent needs and are unable to take advantage of other health care resources. Furthermore, the clientele of public health clinics has changed; the current clientele requires more effort to maintain and improve immunization status because they are often more transient, more socially isolated within their community, and more likely to have contact with multiple health care providers in the public and private sectors.
Furthermore, recent trends in poverty measures suggest that the needs of those who depend on public programs may become more complex. While the overall proportion of children living below the poverty line has declined somewhat during recent years, the number of children in extreme poverty may be increasing (Center on Budget and Policy Priorities, 1999). These trends suggest that although fewer children may be eligible for federal and state assistance programs, those who are eligible may face more barriers, and require greater assistance, than was previously the norm. Anecdotal reports from clinical sites have confirmed this observation (Szilagyi, 1999).
State health officers in various regions of the United States have reported that managed care providers sometimes refer their patients to public clinics for vaccine services because such immunizations can then be provided without cost to the managed care plan (and the plan’s assess-
TABLE 5–3 Estimated Vaccination Coverage with 4:3:1:3a Series Among Children 19–35 Months of Age by Provider Type, Census Division, and State—United States, National Immunization Survey (NIS), 1998b
|
Division/State |
NIS Population Sizec |
Vaccinated by Public Provider (%) |
Vaccinated by Private Provider (%) |
Vaccinated by Mixed Providers (%) |
Vaccinated by Other Provider (%) |
|
National |
5,634,624 |
16.9 |
54.6 |
7.9 |
20.5 |
|
East North Central |
893,232 |
18.0 |
51.3 |
9.5 |
21.2 |
|
Illinois |
265,220 |
17.6 |
51.7 |
7.2 |
23.5 |
|
Indiana |
120,294 |
22.0 |
44.6 |
13.6 |
19.8 |
|
Michigan |
192,317 |
21.2 |
46.9 |
13.1 |
18.8 |
|
Ohio |
216,883 |
16.0 |
58.1 |
6.1 |
19.8 |
|
Wisconsin |
98,518 |
12.2 |
52.0 |
11.4 |
24.4 |
|
East South Central |
324,385 |
31.9 |
38.7 |
10.7 |
18.7 |
|
Alabama |
88,454 |
24.3 |
45.0 |
11.3 |
19.4 |
|
Kentucky |
74,893 |
32.2 |
40.9 |
10.7 |
16.2 |
|
Mississippi |
58,458 |
49.3 |
20.6 |
8.1 |
22.0 |
|
Tennessee |
102,580 |
28.2 |
42.1 |
11.7 |
18.1 |
|
Middle Atlantic |
758,284 |
7.7 |
65.9 |
4.2 |
22.2 |
|
New Jersey |
168,721 |
5.7 |
66.3 |
7.0 |
21.0 |
|
New York |
376,586 |
8.9 |
65.6 |
2.0 |
23.5 |
|
Pennsylvania |
212,976 |
7.0 |
66.1 |
5.8 |
21.0 |
|
Mountain |
369,444 |
21.6 |
46.1 |
10.4 |
21.9 |
|
Arizona |
105,862 |
17.3 |
50.1 |
4.7 |
27.9 |
|
Colorado |
77,203 |
17.1 |
52.4 |
8.9 |
21.6 |
|
Idaho |
26,666 |
28.2 |
47.9 |
14.5 |
9.3 |
|
Montana |
15,582 |
25.6 |
42.1 |
13.0 |
19.2 |
|
New Mexico |
39,573 |
19.4 |
38.1 |
14.0 |
28.5 |
|
Nevada |
40,496 |
33.3 |
40.9 |
12.5 |
13.2 |
|
Utah |
55,177 |
24.2 |
39.1 |
16.2 |
20.4 |
|
Wyoming |
8,886 |
23.7 |
48.2 |
13.4 |
14.6 |
|
New England |
249,411 |
7.2 |
72.1 |
2.4 |
18.2 |
|
Connecticut |
64,926 |
4.6 |
77.0 |
2.0 |
16.4 |
|
Massachusetts |
113,833 |
7.1 |
72.0 |
2.0 |
18.9 |
|
Maine |
21,136 |
7.5 |
68.2 |
1.9 |
22.4 |
|
New Hampshire |
21,355 |
7.5 |
68.4 |
5.7 |
18.3 |
|
Rhode Island |
18,183 |
18.2 |
67.2 |
1.1 |
13.5 |
|
Vermont |
9,976 |
5.4 |
66.8 |
6.3 |
21.5 |
|
Pacific |
1,014,554 |
11.6 |
56.2 |
7.5 |
24.7 |
|
Alaska |
14,136 |
32.1 |
30.8 |
10.6 |
26.4 |
|
California |
793,466 |
11.1 |
56.8 |
7.2 |
24.9 |
|
Hawaii |
26,902 |
6.2 |
61.7 |
4.9 |
27.2 |
|
Oregon |
64,318 |
18.0 |
50.5 |
9.9 |
21.7 |
|
Washington |
115,732 |
10.1 |
57.3 |
8.3 |
24.4 |
|
South Atlantic |
984,856 |
17.0 |
58.2 |
8.1 |
16.6 |
|
District of Columbia |
10,816 |
14.5 |
58.9 |
3.1 |
23.5 |
|
Delaware |
13,865 |
6.4 |
63.5 |
2.5 |
27.6 |
|
Division/State |
NIS Population Sizec |
Vaccinated by Public Provider (%) |
Vaccinated by Private Provider (%) |
Vaccinated by Mixed Providers (%) |
Vaccinated by Other Provider (%) |
|
Florida |
288,797 |
15.5 |
61.8 |
7.9 |
14.7 |
|
Georgia |
165,386 |
24.3 |
52.2 |
9.4 |
14.2 |
|
Maryland |
111,625 |
5.3 |
73.1 |
1.6 |
20.0 |
|
North Carolina |
151,281 |
17.4 |
51.5 |
11.9 |
19.2 |
|
South Carolina |
75,919 |
34.5 |
36.3 |
12.8 |
16.4 |
|
Virginia |
138,479 |
12.7 |
64.5 |
6.3 |
16.5 |
|
West Virginia |
28,687 |
15.5 |
59.2 |
10.1 |
15.2 |
|
West North Central |
363,354 |
19.5 |
52.4 |
8.1 |
20.1 |
|
Iowa |
52,688 |
21.8 |
48.1 |
12.4 |
17.8 |
|
Kansas |
53,968 |
30.4 |
42.1 |
10.3 |
17.3 |
|
Minnesota |
94,025 |
6.6 |
65.6 |
4.1 |
23.7 |
|
Missouri |
104,231 |
25.9 |
49.6 |
8.6 |
15.9 |
|
North Dakota |
10,748 |
29.0 |
34.8 |
11.6 |
24.6 |
|
Nebraska |
32,466 |
11.4 |
53.7 |
6.2 |
28.7 |
|
South Dakota |
15,228 |
18.5 |
50.8 |
8.9 |
21.8 |
|
West South Central |
677,104 |
25.9 |
45.9 |
9.7 |
18.5 |
|
Arkansas |
51,925 |
49.3 |
22.1 |
11.7 |
16.9 |
|
Louisiana |
89,357 |
32.6 |
42.7 |
10.5 |
14.2 |
|
Oklahoma |
66,406 |
30.7 |
36.2 |
10.3 |
22.8 |
|
Texas |
469,416 |
21.4 |
50.4 |
9.2 |
19.0 |
|
a4:3:1:3=Four or more doses of diphtheria, tetanus, and pertussis vaccine; three or more doses of poliovirus vaccine; one or more doses of a measles-containing vaccine; and three or more doses of Hemophilus influenzae type b vaccine. bChildren in this survey period were born between February 1995 and May 1997. cWeighted estimates. SOURCE: CDC, 1999e. |
|||||
ment measures will count the immunization status of the patient regardless of service-delivery setting). These reports have stimulated advisory notices by the HCFA and CDC warning that patterns of deliberate referral are subject to penalties (Richardson, 1999; Richardson and Orenstein, 1999).
Impact of State Program Cutbacks and Budget Reductions
Federal budget cutbacks in the Section 317 program during FY 1996, 1997, 1998, and 1999 were significant (see Figure 5–2). In some cases, grantees saw their infrastructure support budgets reduced by one-third
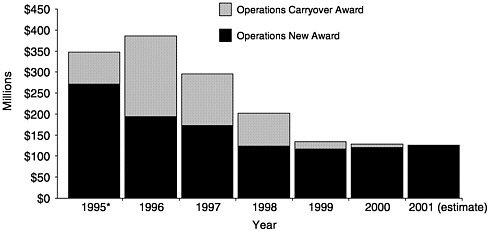
FIGURE 5–2 Section 317 grant operations funding history, 1995–2001 (dollars in millions). *In 1995, CDC transferred funds not needed for vaccine purchase to state operations. SOURCE: Information provided by CDC.
each year. As was the case with local health departments, discussed earlier, these reductions caused states to cut back many immunization efforts, including assessment, outreach, performance monitoring, program linkages, and information management (see Table 5–4)7 Two of the most common activities initiated with the original increases in Section 317 funding—outreach and education efforts and expanded service delivery— were also the most common targets of cuts (Freed et al., 1999). For example:
-
Almost all state program managers made substantial cuts in contracts with local health departments, even though they viewed local outreach activities as critical and effective.
-
Half the states reduced staffing within the immunization program by cutting staff, consolidating positions, or leaving vacancies unfilled. Eight states transferred full-time equivalents (FTEs) or activities to other programs.
-
Several states expressed concern that they do not have the workforce capacity required to investigate disease outbreaks, to work with providers, and to continue registry development. Officials in one state pointed out that it does little good to identify children who are behind on their immunizations if there is no outreach component for follow-up and subsequent vaccination.
TABLE 5–4 State Responses to Section 317 Funding Cutsa
|
|
Activities Eliminated or Reduced |
|||||||
|
State |
Outreach and Educationb |
Assessment and Surveillance |
WIC Linkage |
Registryc |
State Staffd |
Local Service-Delivery Expansione |
Expanded Vaccination Campaignsf |
Other/Notes |
|
AL |
|
No cuts because of increasing amounts of incentive funds. |
||||||
|
AK |
✔ |
|
✔ |
✔ |
|
✔ |
|
|
|
AZ |
✔ |
|
✔ |
✔ |
|
✔ |
State provided funds for registry, transferred full time equivalents (FTEs) to other program. |
|
|
AR |
|
✔ |
|
No major cuts; VFC infrastructure funds increased. |
||||
|
CA |
✔ |
|
✔ |
✔ |
|
|||
|
CO |
✔ |
|
✔ |
✔ |
|
|||
|
CT |
✔ |
|
✔ |
✔ |
✔ |
|
State provided funds to build back up. |
|
|
DE |
|
✔ |
|
VFC infrastructure funds increased. |
||||
|
DC |
|
✔ |
✔ |
✔ |
|
|||
|
FL |
✔ |
|
✔ |
|
||||
|
GA |
|
✔ |
|
✔ |
|
|||
|
HI |
|
✔ |
|
✔ |
|
✔ |
|
|
|
ID |
✔ |
✔ |
|
✔ |
Changed or increased responsibilities per FTE. |
|||
|
IL |
✔ |
|
✔ |
✔ |
✔ |
|
||
|
IN |
✔ |
|
✔ |
✔ |
✔ |
|
||
|
IA |
✔ |
|
✔ |
✔ |
✔ |
|
||
|
KS |
|
✔ |
|
|||||
|
KY |
|
Not much impact yet. |
||||||
|
LA |
✔ |
|
✔ |
|
✔ |
|
||
|
ME |
|
No information available. |
||||||
|
MD |
✔ |
✔ |
|
✔ |
✔ |
|
||
|
MA |
✔ |
|
✔ |
|
✔ |
|
Shifted some FTEs from federal to state funds. |
|
|
MI |
|
✔ |
|
State provided funds for registry. |
||||
|
MN |
✔ |
|
✔ |
✔ |
✔ |
|
VFC infrastructure funds increased; some contracts forward funded. |
|
|
MS |
✔ |
|
✔ |
✔ |
✔ |
|
Redirected some state vaccine purchase funds to registry. |
|
|
MO |
|
✔ |
|
|||||
|
MT |
|
✔ |
Received block grant funds; moved FTEs to other programs. |
|||||
|
NE |
✔ |
|
✔ |
|
||||
|
NV |
|
✔ |
|
✔ |
|
|||
|
NH |
✔ |
|
||||||
|
NJ |
✔ |
|
✔ |
✔ |
|
✔ |
|
|
|
NM |
|
✔ |
|
✔ |
|
|||
|
NY |
|
Redirected some state vaccine purchase funds; not much impact yet. |
||||||
|
NC |
✔ |
✔ |
|
✔ |
|
✔ |
✔ |
|
|
ND |
✔ |
|
✔ |
|
✔ |
|
||
|
OH |
|
✔ |
✔ |
|
Moved FTEs to other program. |
|||
|
OK |
✔ |
✔ |
|
✔ |
|
|||
|
OR |
|
✔ |
|
Received other funding sources. |
||||
|
PA |
✔ |
|
✔ |
|
✔ |
✔ |
|
|
|
RI |
✔ |
|
✔ |
|
Shared costs with other programs. |
|||
|
SC |
✔ |
✔ |
|
|||||
|
SD |
✔ |
|
✔ |
|
||||
|
TN |
✔ |
|
✔ |
✔ |
✔ |
✔ |
Shared costs with other programs at local level. |
|
|
TX |
✔ |
✔ |
✔ |
✔ |
|
✔ |
✔ |
|
|
UT |
✔ |
✔ |
|
✔ |
|
✔ |
|
Redirected some state vaccine purchase funds to support local health departments (LHDs). |
|
VT |
|
Shifted costs to other programs. |
||||||
|
VA |
|
✔ |
✔ |
✔ |
|
✔ |
|
|
|
|
Activities Eliminated or Reduced |
|||||||
|
State |
Outreach and Educationb |
Assessment and Surveillance |
WIC Linkage |
Registryc |
State Staffd |
Local Service Deliverye |
Expanded Vaccination Campaignsf |
Other/Notes |
|
WA |
✔ |
|
✔ |
|
VFC infrastructure funds increased. |
|||
|
WV |
|
✔ |
✔ |
|
✔ |
|
||
|
WI |
|
LHDs lobbied for state funds. |
||||||
|
WY |
✔ |
✔ |
|
Changed universal policy (i.e., no longer covers insured children). |
||||
|
NOTE: WIC=Special Supplemental Nutrition Program for Women, Infants, and Children. FTE=full-time equivalent. LHD=local health department. VFC=Vaccines for Children. aNot a comprehensive (or mutually exclusive) list of state responses, but rather those they chose to highlight. bOutreach and education includes such activities as work with coalitions, media campaigns, and provider education. cRegistry activities include software development and purchase of hardware and other equipment. dState staff includes staff cuts as well as vacancies that were not filled. eLocal service-delivery expansion includes contracts with LHDs, community and migrant health centers, and other partners to extend clinic hours, offer weekend clinics, add nursing staff, and so on. fExpanded vaccination campaigns include adult and adolescent campaigns, as well as campaigns focused on specific vaccines (e.g., hepatitis B). SOURCE: Freed et al., 1999. |
||||||||
-
Many states have discontinued funding for local organizations engaged in immunization outreach activities. States have reported that doing so has damaged their credibility as partners with local agencies (such as WIC clinics and community centers).
State Efforts to Adjust to Budget Declines
As federal assistance declined, many states attempted to secure from other sources, public and private, funding that would preserve essential services and alleviate the impact of the reductions. Such alternative sources included other federal funding, redirection of state vaccine purchase funds to infrastructure support, and additional state funding, among others. Only 11 states were able to replace federal funds for vaccine purchase with funds provided by their health departments and/or state legislatures. Success in procuring funds for infrastructure is generally limited to support for new vaccines, a specific immunization initiative (e.g., providing hepatitis A vaccine in Texas’ border counties), or registry development (Freed et al., 1999:22). In cases where state legislatures did support infrastructure (about 25 states), funds were sometimes appropriated directly to the local health departments. Half of the state agencies are looking for other funding sources, primarily from the state budget.
In some cases, private sources were identified to support educational or outreach efforts within the state agencies. For example, vaccine manufacturers in 31 states supported educational activities (especially provider education) and information dissemination. Statewide and/or local immunization coalitions in 19 states became significant contributors to immunization efforts, particularly outreach activities. Insurers or managed care organizations provided support in 7 states for registry efforts, vaccine purchase, or outreach and education. Most of the states obtained partial funding from other direct or indirect funding sources, including All Kids Count grants for statewide registries (12 states), county- or city-level registry efforts (11 states), and philanthropic assistance from other groups.8
Yet even with additional funding sources, as of the end of the decade almost all state immunization programs had obtained few good answers to their serious financial questions. According to one state source:
It’s a never-ending situation around here with new vaccines and all the funding issues. Immunization program managers around the country are being stretched beyond their limits. At some point, either things are going to have to be broken down differently or … I don’t know what the answer is. All of these things are important, but we’re just not able to do it all. At what point do you just say enough is enough? (Freed et al., 1999:23).
Finding 5–8. States have devised various approaches and made investments in vaccine purchase and program operations, but the level of investment is unevenly distributed across the states. Expenditures for infrastructure efforts are poorly documented, and the financial base for these efforts is not stable. State variability in caring for indigent populations has impeded the development of a national consensus about what level of care, what age groups, and what types of public health assessment, assurance, and leadership responsibilities are adequate to support a national immunization system.
Finding 5–9. Many states have attempted to maintain direct service efforts to meet residual needs, especially among young children, while also expanding their public health assessment, assurance, and policy development roles in monitoring and responding to trends within the private health sector. These enhanced efforts were undertaken without additional resources during a period when federal budgets for infrastructure support declined.
Finding 5–10. The loss of federal funds in Section 317 infrastructure grants has diminished state and local activities in such areas as immunization services, outreach, educational programs, data surveillance and measurement, and technical assistance. These reductions have impaired the ability of state health agencies to carry out effective assessment, assurance, and policy development roles. States now have less flexibility to initiate comprehensive efforts in response to new vaccines, to serve new age groups (such as adults) or selected populations, or to detect and respond quickly to sudden disease outbreaks. Their ability to meet the immunization needs of underserved communities and to encourage the uptake of new vaccines among the general population has declined.
Finding 5–11. Changes in the roles of the public- and private-sector health care system in delivering immunizations have generated uncertainty about the appropriate balance of responsibilities among public and private agencies, and between federal and state programs, in bringing expertise and resources to bear on immunization coverage concerns within local communities. This uncertainty has been exacerbated by the instability of and reductions in the funding stream for state immunization infrastructure.
Finding 5–12. The growing complexity of the vaccine schedule has increased the states’ burden of record assessment in routine procedures. Assessment studies are often reduced or eliminated when more pressing needs arise, such as vaccine purchase or service-delivery requirements.
States with large areas of concentrated poverty or populations that lack immunization as a result of underinsurance may require additional federal resources to coordinate data collection efforts, to conduct targeted assessments, and to synthesize the collection of records that are scattered across diverse health care settings.
Finding 5–13. States had provided more than $300 million to support immunization efforts as of midsummer 1999. While half the states (25) directly support infrastructure, only 4 states fund a substantial portion of their infrastructure budget (i.e., more than 40 percent). Twenty-one states currently provide no direct state support for immunization infrastructure. Four states receive such funding only by drawing on vaccine purchase funds provided by their legislatures.
Finding 5–14. Some states have identified other finance sources to support immunization services, and new private-sector sources may eventually emerge that can contribute to state programs. However, these other sources are limited in scope and are restricted to particular initiatives, such as the development of registries, education for providers, or community partnership efforts.
FEDERAL ROLES AND RESPONSIBILITIES
The National Immunization Program (NIP) within CDC is the primary agency concerned with federal policy and practices in support of state immunization efforts. NIP works with many different agencies and organizations, including other divisions within CDC, HCFA, NVAC, the Health Resources and Services Administration, and the Interagency Committee on Immunization (Rosenbaum et al., 1992; Fine, 1999; Association of Maternal and Child Health Professionals, 1999). In addition, the Departments of Agriculture, Education, and Housing and Urban Development all participate in the development and implementation of federal immunization policies and programs (Kelley et al., 1993). As one report observes: “The diversity of agencies involved is indicative of the importance of immunization to the overall well-being of children and the complexity of providing this service” (Kelley et al., 1993:1).
Although public health is commonly viewed as a primary function of the states, federal interventions have occurred frequently, beginning with the creation of public health hospitals in port cities in 1798 (DHHS, 2000). The federal government has exercised two separate but often overlapping roles in addressing immunization:
-
State assistance—The federal government has consistently sought
-
to supplement and support state efforts through policy coordination, technical assistance, and data collection. Federal grant awards also offer assistance to help states improve their ability to meet the needs of underserved populations, including the uninsured and urban poor, rural residents, immigrants and migrant workers, the elderly, and infants and children. As discussed earlier, federal immunization grants to the states expanded to include infrastructure support in the early 1990s, allowing the states to use federal funds to hire personnel and contractors for specific purposes such as outreach, data collection, and program development.
-
Federal initiatives—In addition to state assistance, the federal government has undertaken special initiatives to expedite the introduction of new vaccines or technologies into the health care system; to reduce inequities in access to immunization services; and, more recently, to address concerns about the safety and quality of vaccines. These initiatives require close collaboration with the states to ensure that federal funds are distributed according to the priorities of the federal program, rather than simply augmenting state revenues for public health.
The combination of state assistance and federal initiatives has evolved through a series of special programs and policies (see Appendix B). The result is a patchwork quilt of policy guidance that places particular emphasis on certain issues while omitting others. By using their Section 317 grant awards, states were able to stitch this quilt together in a cohesive manner that responded to local needs and circumstances. As funds were reduced, states were forced to balance responding to local conditions while also complying with federal mandates.
Infrastructure Investments and Immunization Programs
Federal investments in immunization programs in the 1990s had two basic objectives: (1) improving immunization coverage rates and sustaining high rates among hard-to-reach populations using a variety of evidence-based prevention and linkage strategies, and (2) integrating immunization services within comprehensive primary care plans and medical homes in the private health care sector. Congress has formulated specific guidance for the development of the national immunization program in a few additional areas as well:
-
In the initial buildup of the Section 317 infrastructure grants, Congress clearly intended that federal funds be used to improve access within high-risk communities by extending clinic hours and hiring staff to administer immunizations (U.S. House of Representatives, 1991; U.S. Senate, 1993, 1994).
-
Congress has directed CDC to help states target pockets of need so that federal funds can be focused on disadvantaged communities (U.S. House of Representatives, 1989; U.S. Senate, 1992, 1995, 1998).
-
Congress has supported the use of incentive grants to reward states that achieve high rates of immunization coverage (U.S. Senate, 1993, 1994, 1995, 1998).
-
Congress has guided the development of vaccine safety concerns through the creation of a federal injury compensation plan financed by a special excise tax on vaccine sales.
-
Congress has urged CDC to provide leadership in improving adult immunization coverage rates (U.S. House of Representatives, 1992).
-
Congress has urged CDC to develop the worldwide polio eradication program, drawing on carryover funds in the state infrastructure grants to support the program’s early development (U.S. House of Representatives, 1996).
Congress has not addressed the issues of state data collection or the assurance and assessment roles of public health agencies in the oversight of private-sector performance, which now represent significant aspects of immunization infrastructure. These latter areas raise fundamental concerns about the extent to which federal agencies should support and guide state practice through financial assistance and other incentives, including penalties and reporting requirements. These areas also reveal challenges that emerge when federal and state agencies attempt to guide or change professional practices within the private health care sector. Recently, legislation has been introduced that seeks to require comprehensive health insurance coverage for childhood immunization.9 But such initiatives must address the complex regulatory structure for group and individual health insurance coverage within the private sector and face the traditional political resistance to federal mandates for the private health insurance system.
Federal Finance Practices
As discussed earlier, significant increases in the federal immunization grant awards to the states occurred in the early 1990s, followed by rapid decreases in the latter part of the decade (see Figures 1–2 and 1–3 in Chapter 1). In 1990 and 1991, infrastructure grants (called Financial Assistance [FA] grants) and state expenditures were about one-fourth the level of those for vaccine purchase (called Direct Assistance [DA] grants) (see Tables 5–2 and 5–5). At mid-decade, FA levels increased substantially, rising to twice the levels for DA. New money for FA grant awards increased more than seven-fold from a total of $37 million awarded for 1990
TABLE 5–5 Annual Awards and Expenditures of Section 317 Financial Assistance (FA) Immunization Program Funds (in millions of dollars)
|
Year |
New Funds |
Re-awarded Fundsa |
Total Award |
Expenditures |
Percentage of Total Award Expendedb |
|
1990 |
36.9 |
0.0 |
36.9 |
25.8 |
70% |
|
1991 |
37.0 |
6.3 |
43.3 |
32.2 |
74% |
|
1992 |
92.3 |
5.9 |
98.2 |
43.0 |
44% |
|
1993 |
98.2 |
42.2 |
140.4 |
81.8 |
58% |
|
1994 |
227.6 |
27.3 |
254.9 |
135.4 |
53% |
|
1995 |
261.4 |
75.2 |
336.6 |
195.4 |
58% |
|
1996 |
179.7 |
191.4 |
371.1 |
247.7 |
67% |
|
1997 |
158.6 |
121.7 |
280.4 |
241.1 |
86% |
|
1998c |
115.9 |
77.8 |
193.7 |
179.5 |
93% |
|
1999d |
110.6 |
17.8 |
128.4 |
128.4 |
NAe |
|
aFunds awarded in previous years but not obligated. bBased on year-end unobligated balances for 1990–1997 reported to CDC as of December 21, 1998. cCDC estimates for 1998 expenditures and percentage of 1998 award expended. dProjected amounts for 1999. eNot available. SOURCE: Information provided by CDC. |
|||||
to $261 million for 1995. By the end of the decade, newly awarded FA grants had declined to $116 million for 1998 and $111 million for 1999 (more than a 50 percent decrease). In FY 1999, expenditures for DA and FA were roughly comparable. Four factors affected the buildup and subsequent cutbacks in the Section 317 state infrastructure grants:
-
Implementation of a pockets-of-need strategy.
-
Use of incentive grants to improve immunization rates within the states.
-
The existence of significant carryover in the early years of the state infrastructure grant awards.
-
Initiation of the global polio eradication program.
Pockets of Need. Since numerous studies have demonstrated that low socioeconomic status is strongly associated with low immunization rates, CDC employed a strategy throughout the 1990s designed to enhance efforts to identify and provide vaccination interventions to underserved populations, particularly within large urban areas. In 1991, NIP identified
23 urban areas (in addition to 5 urban grantees) as targets for new Immunization Action Plans.10 For each of the 28 target areas, an average immunization coverage rate was calculated with National Immunization Survey (NIS) data, and traditional public health providers and nontraditional community partners were encouraged to collaborate in program planning and implementation.
Several years later, the FY 1996 Senate Appropriations Committee (U.S. Senate, 1995) directed CDC to develop a strategy that would identify pockets of underimmunized children and help the states target resources to raise immunization coverage in these areas. Although NIP designated 11 major urban areas as pockets of need that would receive intensive follow-up and technical assistance, additional financial resources to support these efforts were not forthcoming in the state grant awards.11 In 1997, CDC instructed all grantees to place additional emphasis on identifying geographic subdivisions at high risk for underimmunization, measuring immunization coverage in these areas, and implementing measures designed to achieve high coverage among vulnerable groups.
CDC recommended three strategies for intensifying efforts to improve coverage rates in pockets-of-need areas: linkages between WIC and immunization services; Assessment, Feedback, Incentives, and eXchange of information (AFIX) interventions; and reminder-recall systems. State and local grantees were expected to implement these key strategies fully and to report progress in using them along with other initiatives, such as immunization registries, in areas identified as pockets of need.
The 1997 annual progress reports submitted to CDC included data provided by 58 grantees (information provided by CDC).12 About three-quarters of the respondents collected information on the key strategies recommended by CDC (WIC linkage, 79.3 percent; reminder-recall, 60.3 percent; and AFIX, 67.2 percent). However, only 11 grantees (19 percent) monitored the number of target WIC sites implementing high-risk protocols for immunization, an important strategy promoted by CDC as part of routine program management.13
In their progress reports, significant numbers of grantees indicated that they had redirected personnel (67.2 percent) or funds (55.2 percent) to work on pockets-of-need issues. The effects of these redirected efforts are not known, however. Neither CDC nor the state grantees have attempted to measure changes in coverage levels in the pockets of need against specific interventions. The prohibitive costs of small-area surveys are commonly cited as a major obstacle to such analysis.
In 1999 NVAC once again called on CDC and state and local immunization programs to focus resources on underimmunized populations. Immunization programs were encouraged to collaborate with WIC to assess each enrolled child’s immunization status, and state immunization
leaders were urged to participate in negotiating the state’s contracts for Medicaid managed care (NVAC, 1999a).
Despite these mandates, state and local immunization programs have few resources to dedicate to program coordination and leadership initiatives. As noted earlier, collaborative and partnership efforts were often the first activities to be reduced within the states when budget cutbacks occurred. The elimination of staff positions within the states, as described earlier, also resulted in multiple task assignments for remaining personnel that reduced their ability to take on new roles. While states have received additional federal assistance in the forms of SCHIP funds and VFC, the application of these resources to state immunization program needs has been constrained by the strict eligibility guidelines and limits to spending for program administration (including the costs of setting up outreach and record-keeping systems) (see Figure 5–3). These guidelines and restrictions leave little margin for collaborative program development in areas of mutual interest and common goals.
Use of Incentive Grants. In an effort to improve state performance in reaching national immunization goals, the Senate Appropriations Committee instructed CDC in 1993 (for FY 1994) to set aside approximately $32 million annually from the state infrastructure awards for incentive grants (U.S. Senate, 1993). These funds are distributed to the grantees according to their levels of immunization coverage, as reported by the NIS. Once the size of the base award has been determined for each state in response to its original request, states with higher coverage rates receive “bonus” awards from the incentive funds to reward their achievement.
In the mid-1990s, when infrastructure grants amounted to more than $300 million annually, incentive grants constituted less than 10 percent of that total. In recent years, as the total funding for infrastructure grants has diminished, the $33 million set-aside has become an increasing source of concern. Incentive grants now represent about 24 percent of the total grant awards, and grantees with low immunization coverage rates have indicated that they are being “punished” by lower total awards when they require additional assistance to meet urgent local needs.
The Carryover Problem. As noted earlier, in the aftermath of the rapid and unplanned buildup of state infrastructure grants in the early 1990s, significant amounts of carryover emerged within the state immunization budgets (see Table 5–5 and Figure 5–2). Although the states had acquired extensive experience over several decades in working with federal agencies to purchase vaccines, the large increases in infrastructure support were targeted to areas that required new personnel and new efforts (such as outreach, record assessment, performance measures, and the develop-
ment of immunization registries). Moreover, the increases occurred swiftly without adequate lead time to plan for how the funds would be used within existing state administrative and management systems.14
Although increases in Section 317 funding for infrastructure support in the early 1990s were viewed as a tremendous opportunity, states reported serious administrative impediments to reaping the full benefit of those funds (Freed et al., 1999). For example:
-
Many states had difficulty in predicting the level of funding for any given year. This made it problematic to create accurate budgets for the immunization program, engage in strategic planning, or hire full-time permanent staff.
-
Funds were awarded late in the fiscal year, often as a result of delays in congressional approval of federal health budgets. In some cases, multiple allocations were made within a given year.
-
The federal grant requirements obligated the states to spend their funds before the end of the fiscal year.
-
Statewide internal restrictions in some cases affected hiring, budgeting, or spending. Some state legislatures must allocate or approve all state agency spending, including federal grants, especially if personnel appointments are involved. States were unable to abolish personnel positions once the funding decreased; the result was administrative obligations that inhibited program development.
Two overall problems resulted from these circumstances: (1) states did not have adequate time to assess their needs and use federal funds effectively, and (2) states with cumbersome internal procedures for budgeting, spending, or hiring were unable to obligate their funds expeditiously (Freed et al., 1999). Some legislatures meet every other year, creating further delays. Both problems contributed to the buildup of carryover or unexpended funds that had been obligated by the federal government to the states, which Congress eventually viewed as excessive (U.S. Senate, 1995). The delay in expenditures during the startup period led Congress to reduce the state infrastructure grant funds in the period FY 1996–1998.15 These reductions resulted from mid-decade pressures to reduce the size of federal discretionary programs in general, making it more difficult to sustain ongoing efforts while also starting up new initiatives, such as the polio eradication program. The decreases are commonly viewed by state officials as “punishment for factors beyond their control” (Freed et al., 1999:16). Many state officials also noted that the curtailment of Section 317 carryover funds occurred precisely at the point when they believed they had made significant strides in the organization of immunization delivery, outreach, and other activities.
When Section 317 grant awards were reduced, state expenditure rates gradually increased, demonstrating the states’ growing capacity to use federal funds for immunization services. The states’ needs eventually became greater than the resources available to them. Expenditure rates of the infrastructure grants during 1997 and 1998 were in the range of 86 percent and 96 percent, respectively, and total carryover of funds is currently estimated at less than $10 million for 1998 Section 317 FA awards. CDC and state officials now report that the current level of federal funds for Section 317 infrastructure support (requested at $117 million for FY 2000) is no longer sufficient to support their efforts (Thompson, 1998).
Global Polio Eradication Initiative. Reasoning that the health and economic benefits of polio eradication would be perpetual and that extra funds would be needed for a few years only to achieve this goal, CDC launched a global polio eradication initiative in 1996, with congressional support. The initiative involved an extensive partnership (including funding and technical support) with Rotary International, the United Nations Foundation, the United Nations International Children’s Emergency Fund (UNICEF), the World Health Organization, and governments of other industrialized countries.
In the period FY 1996–1998, when budget cutbacks were common throughout DHHS, CDC received explicit guidance from both the House of Representatives and the Senate to fund the new initiative for polio eradication (as well as measles elimination) at the expense of state vaccine purchase and infrastructure development funds (U.S. House of Representatives, 1996). Recognizing that prior increases had occurred in the state infrastructure grants, and disturbed by reports of large amounts of unspent state funds from prior years, the Congress expressed strong support for the global polio eradication program and encouraged CDC to expand the effort using available resources—by reducing the state infrastructure grant awards. This decision to cut the base of the state infrastructure program to support the global polio eradication effort plays an important role in explaining the shortfall now being experienced by the states.
Impact of Budget Reductions
Reductions in state infrastructure grants have affected each of the six key roles of the national immunization system. For example:
-
Infectious disease prevention and control—At present, the NIP does not have a separate pool of funds within the Section 317 grant program to support the purchase of vaccines for outbreak control (information pro-
-
vided by CDC). Funds are likewise not available within the Section 317 program to support the training needs for outbreak control recommended by NVAC (1999a); such support may be provided by a new bioterrorism initiative financed elsewhere within CDC.
-
Surveillance and monitoring—During the 1990s, CDC maintained support for the NIS (see Chapter 4). CDC also encouraged the development of immunization registries as a key component of the future immunization surveillance system. Between 1994 and 1999, CDC allocated a total of $178.4 million in Section 317 funds within the state infrastructure awards to support immunization registries, but the size of these awards has declined in recent years (see Box 5–4) (A.Bauer, CDC, personal communication, May 21, 1999). Cutbacks in federal grants have caused several states to reduce their own surveillance and monitoring efforts, as discussed earlier. These reduced efforts represent critical omissions in the development of important baseline and benchmark coverage measures in certain key areas, such as the immunization status of Medicaid or VFC-eligible clients. The cutbacks also diminished the states’ abilities to expand surveillance for diseases such as varicella that are now vaccine-preventable while maintaining current surveillance efforts for traditional vaccine-preventable diseases. Furthermore, in areas where states are designated for special immunization initiatives (such as the ACIP recommendation that 11 states universally vaccinate children against hepatitis A), additional funds are not available to help these states with program implementation or enhanced surveillance. In such cases, states are given further program responsibilities by federal agencies without additional federal funding.
|
BOX 5–4 Total Section 317 Funds Awarded to Support Registries as of July 1, 1999 (in millions of dollars)*
|
-
Assessment and technical assistance—State immunization officials have been strongly encouraged to exercise leadership and technical assistance in a variety of areas, including the immunization of adults, the negotiation of Medicaid managed care contracts, the coordination and regulation of private insurance and VFC benefits, the auditing of private-sector immunization records, and the integration of datasets from multiple sites (NVAC, 1999a). Reductions in federal grants have severely constrained the states’ ability to exercise their current roles, much less assume enhanced responsibilities for monitoring private-sector performance, ensuring vaccine safety, and encouraging the immunization of adults. The cutbacks have also occurred at a time when negotiations regarding the distribution of government-financed vaccines have become more complex; an example is questions that have emerged about the use of VFC for clients who are covered by private (non-Medicaid) SCHIP plans. In most states, public health immunization efforts and public health insurance plans (such as Medicaid and SCHIP) are administered in separate agencies and even separate departments. Opportunities for coordination and integrated efforts are often limited. For example, state immunization programs may have technical expertise that is relevant to contract specifications for the purchase of managed care services for state beneficiaries. But those who are involved in negotiating Medicaid or SCHIP contracts may be unaware of or reluctant to involve other state employees in developing benchmark and performance standards for their contractors.
-
Programs to improve immunization coverage rates—The reductions in federal grants have had significant effects on interventions such as outreach, provider education, and service delivery, as described earlier. Efforts such as WIC linkages, reminder-recall systems, and record audit procedures, all of which have been found to be highly effective in improving immunization rates in disadvantaged communities, have been reduced routinely as a result of federal cuts that decrease resources for state and local programs.
Changes in Program Composition
Total appropriations for the Section 317 program declined by only about 5 percent in the latter part of the 1990s (decreasing from $464 million in FY 1995 to $448 million in FY 1999). Significant shifts occurred within the major components of the program during this time (see Table 5–6); for example, the program operations category (the portion of the program that is administered directly by CDC) expanded, while the state infrastructure grants were reduced. During FY 1995–1999, the program operations category increased from $104 million (23 percent of the
TABLE 5–6 Composition of CDC Immunization Appropriations, 1995– 1999, Amounts and Shares (fiscal years; dollars in thousands)
|
Type |
1995 |
1996 |
1997 |
1998 |
1999 |
|
Grants |
|||||
|
DAa: Vaccine purchase |
151,893 |
139,393 |
139,393 |
119,393 |
139,629 |
|
State operations |
23,800 |
23,800 |
23,800 |
23,800 |
23,467 |
|
Parent/patient notification |
2,900 |
2,900 |
2,900 |
2,900 |
2,859 |
|
Surveillance and response |
5,100 |
5,100 |
5,100 |
5,100 |
5,029 |
|
Infrastructure |
108,400 |
108,400 |
88,400 |
42,400 |
41,806 |
|
Program-based incentives |
33,000 |
33,000 |
33,000 |
33,000 |
32,537 |
|
Assessment activities |
3,500 |
3,500 |
3,500 |
3,500 |
3,451 |
|
Immunization information systems |
8,232 |
8,232 |
8,232 |
0 |
0 |
|
Adult/adolescent vaccination |
0 |
0 |
0 |
0 |
0 |
|
Adult immunization |
0 |
0 |
0 |
0 |
0 |
|
Other grants |
22,552 |
23,576 |
23,361 |
30,741 |
30,311 |
|
Subtotal, Section 317 grants |
359,377 |
347,901 |
327,686 |
260,834 |
279,089 |
|
Program operations |
|||||
|
Prevention activities |
38,660 |
37,917 |
37,825 |
37,825 |
38,439 |
|
Polio technical assistance |
5,727 |
11,227 |
19,277 |
19,277 |
30,874 |
|
Polio vaccine |
4,116 |
16,000 |
28,000 |
28,000 |
35,565 |
|
Measles technical assistance |
0 |
0 |
0 |
0 |
7,944 |
|
Measles vaccine |
0 |
0 |
0 |
0 |
7,944 |
|
Adult adolescent vaccination |
0 |
0 |
0 |
0 |
0 |
|
24,130 |
23,146 |
23,146 |
23,146 |
22,525 |
|
|
Vaccine safety |
4,451 |
4,451 |
4,451 |
4,451 |
4,389 |
|
National Immunization Survey |
16,000 |
16,000 |
16,000 |
16,000 |
12,472 |
|
Immunization information systems |
1,029 |
1,004 |
1,004 |
1,004 |
0 |
|
Information /education |
4,244 |
4,244 |
4,244 |
4,244 |
4,185 |
|
Interagency group research |
6,000 |
6,000 |
6,000 |
6,000 |
5,916 |
|
Subtotal, program operations |
104,357 |
119,989 |
139,947 |
139,897 |
170,253 |
|
Administrative rescission |
0 |
0 |
0 |
0 |
-1,394 |
|
Total, Section 317 program |
463,734 |
467,890 |
467,633 |
400,731 |
447,948 |
|
aDirect Assistance. bResearch and development. cAssessment and evaluation. SOURCE: Information provided by CDC. |
|||||
total NIP budget in FY 1995) to $170 million (38 percent of the total budget in FY 1999). In the same period, the grants portion of the budget (which includes state infrastructure and vaccine purchase grants, research support, and congressionally mandated studies) decreased by 20 percent (from $359 million or 77 percent of the total in FY 1995 to $279 million or 62 percent of the total in FY 1999).
The committee finds these compositional shifts troubling because they suggest an unintended reorientation of the Section 317 program that diminishes the state assistance role while expanding the federal presence. Although international polio eradication efforts are important, federal support for such efforts should not come at the expense of state immunization grant awards. It may have been reasonable during a period of national budget reductions to start up the polio eradication initiative with carryover funds from the state grants program. This finance strategy has long-term consequences, however, that require attention and merit remedial action.
Furthermore, cuts have occurred in the infrastructure grants during a time when VFC vaccine purchase funds have increased. The greater reliance on VFC and the private sector has allowed states to reduce their service-delivery role in the public health sector, but important functions remain and new roles have been added, all of which need to be supported.
Finding 5–15. Infrastructure support in the state immunization grants program lacks a strategic vision that can guide federal and state investments. Congress has not made infrastructure support within the states a priority for the national immunization program.
Finding 5–16. The federal government has traditionally assisted the states in supporting such areas as outreach and clinical services. A new emphasis is required, however, in areas that involve assurance, access, and policy development as result of the shift in the delivery of immunization services to the private sector. Administrative and staff support is needed in these areas so that local public health agencies can provide leadership and technical assistance in monitoring key indicators of quality of care and disparities in immunization coverage rates within their communities.
Finding 5–17. New federal funds for state infrastructure grants were reduced from $261 million annually (1995) to $111 million annually (1999) during a time when the health care system and immunization schedules were becoming more complicated. Resources are not available to help local communities adapt to new vaccines; monitor trends that can influence immunization rates; or implement new initiatives in the areas of assessing private-sector performance, improving coverage of adult vaccines, and conducting vaccine safety education programs.
Finding 5–18. Programs such as VFC, Medicaid, and SCHIP have administrative resources that can help states monitor vaccine coverage rates among public and private health providers. However, no coordi-
nated strategy currently exists for encouraging states to draw on these resources in building their immunization programs.
Finding 5–19. Although the federal government has traditionally supported the concept of partnership with the states to achieve national immunization goals, extensive ambiguity exists regarding the scope and forms of infrastructure that are adequate to meet national objectives while also responding to local needs. Some infrastructure services (such as providing immunizations within school health clinics or other community settings) can be undertaken by state and local health departments alone. Others require federal-state collaboration to help local agencies do more with limited resources (such as extending clinic hours). Interventions that are focused on systemic change, such as addressing missed opportunities for immunization assessment and referrals within WIC and Head Start programs, require interagency and community partnerships at the federal, state, and local levels. In implementing these interventions to serve vulnerable families, public health officials must interact with other agencies and offer resources so that high priority is given to the immunization effort.
SUMMING UP
During the past decade, the federal government assumed increasing responsibility for the immunization of vulnerable populations. The development of new vaccines, their increased costs, and the appearance of new diseases requiring immunization to protect the population have changed the nature of immunization from a niche to an increasingly integral component of the health care universe. At the same time, global travel and increased social mobility have multiplied the probabilities of dangerous infections affecting large populations throughout the United States.
As the federal government aggressively assumed a major role in the financing of vaccines, the gap between financing and delivery of primary care health services (including immunizations) expanded for large numbers of children within the United States. Many children who previously did not have access to vaccines or were immunized in public health clinics now receive vaccines in their medical homes in the private sector. Older adults (above age 65) have access to vaccines in the private sector through plans that are financed with Medicare funds. While the expanded role of the private sector in serving disadvantaged populations has served important public health objectives by increasing coverage rates, significant questions remain about the adequacy of existing services, as well as the capability of private providers and health plans to offer timely and routine vaccinations. In addition to the use of VFC funds, many commu-
nities rely on the Section 317 program for vaccines to meet residual needs among adults and children.
Recent reductions in federal grants for immunization infrastructure and shifts in the Medicaid provider base within the states have reduced the resources available to support immunization programs at the same time that the roles and responsibilities of state and local health agencies have expanded and diversified. The assurance and assessment mission and role of state health agencies require them to take on responsibilities for monitoring and improving provider behavior in the private sector, collecting and evaluating data on immunization trends within private health plans and special populations, adding new vaccines and age groups to the immunization schedule, addressing growing concerns about vaccine safety, and developing regional immunization registries and other sources of surveillance data. Although a few states have supplemented essential activities by drawing on other federal sources, shifting state budget allocations, or developing new sources of revenue (such as tobacco settlement funds), the demand on state public health agencies continues to exceed their current capacity.
Policy reforms within the private health care sector (such as the trend toward managed care, the inclusion of immunization services in private insurance benefits, and first-dollar coverage requirements for immunization services) have fostered a climate that encourages greater use of performance standards and assessment of immunization status within private practice. Yet access to reliable and timely data that accurately describe the immunization status of at-risk populations served by private plans remains elusive and uneven. Preventive services (including access to vaccines) in primary care health plans are fragmentary and unpredictable in both quality and scope. As part of their mission, public health leaders and programs bear responsibility for encouraging private providers to incorporate evidence-based strategies and new vaccines into routine primary care services, participating in regional registries, monitoring and improving immunization coverage rates in the public and private health sectors, and addressing concerns about vaccine safety.
Local and state governments have demonstrated both interest and ability with regard to developing immunization programs and services that have positive populationwide benefits, but few states have the resources needed to sustain infrastructure programs on their own. Efforts to increase and sustain coverage levels require diversified approaches, including community outreach and linkage programs, as well as systemic interventions, such as provider assessment and feedback systems and reminder-recall services.
It takes time to put new management and administrative services in place, particularly when consensus must be developed about how clients,
providers, payers, and health departments should collaborate to ensure that immunizations are provided as part of appropriate health care (IOM, 1994b). State efforts to foster public awareness of the importance of immunization coverage are particularly challenged in the current environment with the addition of new vaccines to the childhood immunization schedule, the addition of new population groups (adolescents and adults) to the immunization system, public concerns about vaccine safety, and diminished public perception of the importance of timely immunization coverage in the absence of disease outbreaks (Orenstein et al., 1999).
Recent cuts in Section 317 state grant awards have reduced the ability of the states to carry out their traditional surveillance and outreach responsibilities or improve their oversight roles. Although state and local health programs have been urged to assume new leadership and oversight roles (such as strengthening coordination with new health finance practices, monitoring immunization status within private health care plans, and developing registry initiatives), it is unlikely that such efforts can be undertaken on a national scale without federal funding committed to their support.
As new vaccines are recommended in the next few decades, health plans, health care providers, and the public will need to confront the problem of recognizing, accepting, and applying these recommendations in routine medical care. Public health interventions at both the provider and community levels are necessary to sustain quality health care services and reduce disparities in coverage that result from barriers to access or attitudes and behavior. In the absence of such interventions:
-
Efforts to track the immunization status of individuals who move across public and private health care plans will become increasingly difficult.
-
Delays may occur in the integration of new vaccines into routine medical care.
-
Further improvements in immunization coverage rates may be reduced, and significant disparities will probably occur in levels of vaccine coverage. The most severe effects are likely to be felt by those who are hard to reach and often most vulnerable to vaccine-preventable disease.
-
States may be unable to develop appropriate immunization benchmarks, impeding their efforts to use appropriate performance measures in purchasing vaccines and health care services for disadvantaged populations and monitoring quality of care within public and private health plans.
-
National and local data systems designed to monitor vaccine coverage status and disease outbreaks may become unreliable.
-
Sustaining public acceptance of vaccines may become more diffi-
-
cult as a result of decreased exposure to information on the need for immunizations, as well as the complexities involved in documenting increasing numbers of vaccines across the life span.
ENDNOTES
|
10. |
The selection criteria included coverage rates (as determined by the National Immunization Survey), population size, and the proportion of individuals from racial and ethnic minority groups residing in the core city. |
|
11. |
The 11 metropolitan areas were New York City, Philadelphia, Newark, Miami, Chicago, Detroit, Dallas, San Antonio, Houston, Phoenix, and Los Angeles. |
|
12. |
The grantee reports used different surrogate measures to identify pockets of need, such as proportion of minorities (25 grantees), population density (21), poverty level (19), provider/service shortage (17), proportion of single-parent households (13), educational status (less than 12 years of education or GED) (12), public assistance rates (10), and vaccine-preventable disease morbidity (9). One-fifth of the grantees also used geographic information systems computer software to identify and map pockets of need. The grantees described seven direct measures for identifying pockets of need: retrospective surveys (29), provider-based surveys (21), local immunization registries (20), cluster surveys (12), birth certificate-based surveys (11), statewide immunization registries (11), and random digit dialing surveys (6). In measuring and monitoring immunization coverage in the pockets of need, grantees reported on population-based methods, provider assessments, and the frequency of measurement. Retrospective school-based surveys were used by 50 percent of the grantees to measure and monitor coverage. Most respondents relied on public clinic assessments (51 of 58 grantees) to monitor coverage rates, although private provider assessments (36) and, more rarely, managed care plan assessments (17) were also used. Assessments were usually conducted annually (69 percent). |
|
13. |
Additional strategies reported by the grantees as part of their intensive efforts in pockets-of-need areas included outreach (82.8 percent), provider education (75.9 percent), and linkage with other public assistance programs (36.2 percent). Outreach efforts included public education, community awareness campaigns, coalition building, door-to-door canvassing, use of volunteers, and involvement of community-based organizations to contact families of individuals identified as undervaccinated. |
|
14. |
Between 1992 and 1995, CDC awarded nearly all carryover funds in addition to, rather than in lieu of, newly appropriated funds. This compounded the problem in grantee areas that experienced difficulty in expending their funds efficiently. CDC reports that during these years, the NIP was trying to resolve the carryover issue by encouraging states to continue to build and sustain the systems needed to raise immunization coverage levels with new funds, while using the carryover funds for one-time expenses (information provided by CDC). |
|
15. |
The amount of funds available for infrastructure services within the Section 317 grants in 1997 and 1998 was less than half of what was appropriated in 1996. See Table 5–6. |