Executive Summary
ABSTRACT Federal, state, and private-sector investments in vaccine purchases and immunization programs are lagging behind emerging opportunities to reduce the risks of vaccine-preventable diseases. Although federal assistance to the states for immunization programs and data collection efforts rapidly expanded in the early part of the 1990s, significant cutbacks have occurred in the last 5 years that have reduced the size of state grant awards by more than 50 percent from their highest point. During this same period, the vaccine delivery system for children and adults has become more complex and fragmented.
A combination of new challenges and reduced resources has led to instability in the public health infrastructure that supports the U.S. immunization system. Many states have reduced the scale of their immunization programs and currently lack adequate strength in areas such as data collection among at-risk populations, strategic planning, program coordination, and assessment of immunization status in communities that are served by multiple health care providers. If unmet immunization needs are not identified and addressed, states will have difficulty in achieving the national goal of 90 percent coverage by the year 2010 for completion of the childhood vaccination series for young children. Furthermore, state and national coverage rates, which reached record levels for vaccines in widespread use (79 percent) in 1998, can be expected to decline, and outbreaks of vaccine-preventable diseases may occur as a result, particularly among persons who are vulnerable to these diseases because of their undervaccination status.
The Institute of Medicine (IOM) Committee on Immunization Finance Policies and Practices has therefore concluded that a renewal and strengthening of the federal and state immunization partnership is necessary. The goal of this renewed partnership is to prevent infectious disease; to monitor, sustain, and improve vaccine coverage rates for child and adult populations within more numerous and increasingly diversified health care settings; and to respond to vaccine safety concerns. To achieve this renewal, states require a consistent strategy, additional funds, and a multiyear finance plan that can help expedite the delivery of new vaccines; strengthen the immunization assessment, assurance, and policy development functions in each state; and adapt childhood immunization programs to serve the needs of new age groups (especially adults with chronic diseases) in different health care environments.
The IOM committee recommends that federal and state governments adopt a national finance strategy that would allocate $1.5 billion in federal and state resources over the first 5 years to strengthen the infrastructure for child and adult immunization—an annual increase of $175 million over current spending levels. These resources would consist of $200 million per year in state infrastructure grants awarded by the Centers for Disease Control and Prevention (CDC) (the Section 317 program) and an additional $100 million per year in increased state contributions. The committee also recommends that Congress replace the current discretionary Section 317 grants with a formula approach for state immunization grant awards to improve the targeting and stability of federal immunization grants. The formula should provide a base level of support to all states, as well as additional amounts related to each state’s need, capacity, and performance. The committee further recommends that Congress introduce a state match requirement for the receipt of increased federal funds to help strengthen and stabilize the infrastructure that supports long-term public health assessment, assurance, and policy development efforts.
Along with the development of a strategic investment plan to support immunization infrastructure, the committee recommends that the federal government provide $50 million in additional funds to help states purchase pneumococcal and influenza vaccines for adults under age 65 who are not eligible for other forms of public health insurance and who have chronic illnesses such as heart and lung disease or diabetes. The committee further recommends that states increase their own vaccine purchases by $11 million annually for adults who cannot afford vaccines but are not eligible for federal assistance (the “underinsured”). Finally, the committee recommends that federal and state agencies develop a set of consistent and comparable measures to monitor the immunization status of children and adults enrolled in public and private health plans.
BACKGROUND
During the 1990s, the U.S. federal and state governments built a dynamic and flexible immunization system that has adapted to extensive changes in the science of vaccines, in demographic patterns, and in service-delivery patterns, in places ranging from remote rural counties to densely populated metropolitan areas. This highly decentralized system is shaped by local circumstances, resources, and needs, as well as by national goals and policies. Though complex and cumbersome, the federal-state immunization partnership has demonstrated an extraordinary capacity to ensure the reliable delivery of an increasing number of vaccine antigens for an expanding range of age groups, including newborns, preschool and school-aged children, adolescents, and adults in a growing number of private and public health care settings.
At present, however, the public health infrastructure that supports the national immunization system is fragile and unstable. Three trends contribute to this instability:
-
rapid acceleration in the science of vaccine research and production,
-
increasing complexity of the health care services environment of the United States (represented by trends such as the emergence of private managed care organizations as the primary health care providers for low-income populations), and
-
recent reductions in federal immunization grants to the states (reflecting congressional responses to shifting health care roles and responsibilities within the federal government, the states, and private health care providers), which followed on the heels of dramatic increases in the early 1990s.
This instability can create pressure points and service gaps that contribute to vaccine coverage disparities and may result in outbreaks of infectious disease. The resurgence of measles in 1989–1991 in the United States, which included a series of outbreaks that contributed to 43,000 cases and more than 100 deaths, primarily among children younger than 5 years of age, is a constant reminder that the presence of vaccines alone is not sufficient to protect populations against vaccine-preventable disease. Outbreaks can emerge swiftly and unexpectedly during times of complacency if vaccines are not accessible to those who are most vulnerable to infectious disease. The absence of adequate measurement tools and appropriate community assessment studies can result in reduced vigilance within the health care system if missing data foster mistaken beliefs that national or local immunization rates are up to date.
Although record levels of immunization were achieved across the
United States in the 1990s, certain problems persist within the national immunization system. These problems include the following:
-
The need to sustain and document high levels of immunization coverage for a growing number of vaccines delivered within multiple health care settings. Each day sees a new birth cohort of 11,000 infants in the United States, all of whom require routine immunizations in their first 2 years of life. An enormous effort is required in both private and public health care settings to sustain the 1998 level of 79 percent coverage of completion of the recommended immunization series for 2-year-olds across the United States. Improving coverage levels to reach the national goal of 90 percent will be increasingly difficult as new vaccines are added to the recommended schedule and as uncertainties about the benefits of vaccines increase in the absence of visible harm from infectious disease.
-
Persistent disparities in childhood levels of immunization coverage. The immunization system has successfully reduced racial and ethnic disparities in childhood immunization levels, but coverage levels in areas of concentrated poverty remain significantly lower than national and statewide levels. National surveys reveal a gap of 9 percentage points between children above and below the federal poverty level for the complete series of the most critical childhood vaccines. Significant disparities also persist in coverage rates in many metropolitan areas that have large populations of low-income residents. In some cases, childhood vaccination coverage rates are as much as 19 percent lower for metropolitan residents compared with the remainder of the state.
-
Low coverage rates and racial and ethnic disparities for adult vaccines. Immunization coverage rates for adults are well below those achieved for childhood immunizations. National immunization levels for influenza vaccines (which are needed annually) have increased to 63 percent (1997) for adults age 65 and older, but levels of pneumococcal vaccination (which is usually a one-time event) among this age group are significantly lower: only 42 percent of noninstitutionalized adults over age 65 had ever received a pneumococcal vaccination by 1997. Coverage rates for high-risk adults who suffer from chronic disease (e.g., heart or lung disease or diabetes) are especially poor (26 percent have received an influenza vaccination, while only 13 percent have received a pneumococcal vaccination). Validated coverage estimates for other adult vaccines (e.g., hepatitis A, hepatitis B, tetanus, and varicella) are severely limited or nonexistent. In addition to low coverage levels, significant racial and ethnic disparities continue to persist in adult immunization levels.
-
Mortality and morbidity from preventable infectious disease. Between 50,000 and 70,000 adults and about 300 children in the United States die annually from vaccine-preventable diseases or their complications. The
-
preventable illness and subsequent complications that result from missed vaccines carry a high and avoidable cost for individuals and society as a whole.
-
Serious gaps and inconsistencies in the coordination, support, and documentation of immunization efforts. Stress-related cracks stemming from the complexity of the nation’s immunization system show signs of deepening as shifts occur within public and private health care delivery systems. Recent controversies over the use of federally financed vaccines for children who are enrolled in stand-alone (i.e., non-Medicaid) state-sponsored insurance programs, for example, reflect inconsistencies and ambiguities in service-delivery efforts.
The collective result of the above trends is diminishing the public benefit of vaccines, especially for groups of children and adults who do not have routine access to high-quality primary care.
CHARGE TO THE COMMITTEE
Current analyses of federal and state spending for immunization services and programs reveal the absence of a strategic plan that can guide a federal-state partnership in supporting immunization efforts. The absence of a national consensus about the roles and responsibilities of federal and state agencies in fostering immunization also complicates efforts to extend the benefits of immunization to the relatively small population of high-risk children and the larger pool of adults who remain unprotected.
It is for these reasons that the U.S. Senate Appropriations Committee in 1998 asked the Institute of Medicine (IOM) to conduct a study of the Section 317 program administered by the Centers for Disease Control and Prevention (CDC).1 The study was designed to identify areas in which research-based evidence can guide federal, state, and local immunization policies and practices. The Congress formulated five key questions as the basis for the IOM study:
-
What was the extent of overall spending by all sources for immunizations in the United States during the 1990s?
-
How were new federal funds spent by the states, and to what extent did states maintain their own levels of effort over the past 5 years?
-
What are current and future funding requirements for immunization activities, and how can those requirements be met through a combination of state funding, federal Section 317 immunization grant funding, and funding available through the State Children’s Health Insurance Program (SCHIP)?
-
How should federal grant funds be distributed among the states?
-
How should funds be targeted within states to reach high-risk populations without diminishing levels of coverage among the overall population?
In addition, a sixth question was added by CDC during the negotiation of the study contract:
-
What should be the role and financing level for CDC’s current program supporting state efforts to vaccinate adults and achieve the nation’s goals for influenza and pneumococcal vaccines?
These questions reflect a need for guidance to clarify roles and help balance federal and state contributions in extending the benefits of immunization to unprotected children and adults.
SIX ROLES OF THE NATIONAL IMMUNIZATION SYSTEM
In examining current immunization policies and practices in the public and private health care sectors, the IOM committee identified six fundamental roles of the national immunization system:
-
Assure the purchase of recommended vaccines for the total population of U.S. children and adults, with particular emphasis on the protection of vulnerable groups.
-
Assure access to such vaccines within the public sector when private health care services are not adequate to meet local needs.
-
Control and prevent infectious disease.
-
Conduct population wide surveillance of immunization coverage levels, including the identification of significant disparities, gaps, and vaccine safety concerns.
-
Sustain and improve immunization coverage levels within child and adult populations, especially in vulnerable communities.
-
Use primary care and public health resources efficiently in achieving national immunization goals.
The last of these roles provides overarching support for the other five, and was the focus of the committee’s charge. Figure ES-1 displays these roles as components of the national immunization partnership.
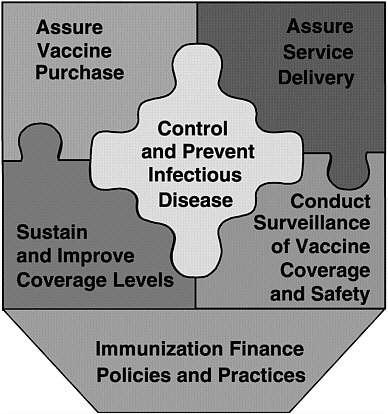
FIGURE ES-1 Six roles of the national immunization system.
A FEDERAL-STATE IMMUNIZATION PARTNERSHIP
Efforts to meet national immunization goals currently involve a set of intricate and separate financial arrangements among federal, state, and local health agencies, as well as collaborative ventures with public and private health care providers. In conducting the study, we gave particular attention to the responsibilities of federal, state, and local health agencies and the burden of effort that is required to support each of the above roles in an integrated manner. State governments are the public health stewards for disadvantaged populations within their borders, and have traditionally been responsible for meeting the health needs of residents who are not served or are underserved by the private health care sector. Each state currently invests in immunization programs through direct or in-kind support, but no state has sufficient resources to support all six of the above immunization roles. Consequently, federal assistance is required to help each state maintain the essential elements of an immunization pro-
gram, to respond to unexpected circumstances and changing conditions that require enhanced efforts, and to prevent infectious disease transmission across state borders. These arrangements are traditionally divided into two categories: vaccine purchase and infrastructure support.
Vaccine Purchase. Federal assistance for state vaccine purchases and immunization programs is provided primarily through two funding streams: Section 317 of the Public Health Service Act, administered by the National Immunization Program within CDC, and the Vaccines for Children (VFC) program, administered jointly by CDC and the Health Care Financing Administration (HCFA). Through these two efforts, the federal government awarded more than $600 million in vaccine supplies to the states in fiscal year (FY) 1999, primarily for childhood vaccines. In addition, Medicare pays for preventive adult vaccines, which are financed primarily through Medicare payments to physicians. In 1998, HCFA paid Medicare providers $114 million for influenza and pneumococcal immunizations, primarily for adults over age 65.
The vast majority of states depend primarily on federal grants for the purchase of vaccines. Only 10 states rely on state funds for 30 percent or more of the public dollars spent to purchase vaccines. In almost half the states (24), state funds account for less than 10 percent of all publicly purchased vaccines. The remaining states (16) use state funds for between 10 and 30 percent of public vaccine purchases. State-level funds enable the purchase of vaccines for many underinsured children and adults (who are not eligible for federally financed vaccines), especially those who receive vaccines in local public health clinics. Fifteen states have adopted universal purchase policies, whereby they purchase vaccines for all children served by public clinics or participating providers, regardless of their insurance status.
The number of sites administering childhood or adult vaccines purchased with government funds increased dramatically over the past decade—from about 3,000 public health clinics and several hundred Medicaid health care providers in the 1980s to more than 50,000 public and private sites in 1999. The creation of VFC has been extraordinarily successful in encouraging large numbers of private health care professionals to administer vaccines to low-income children as part of their primary health care benefits. But this success in increasing the size and diversity of the vaccine delivery system has complicated the tasks of educating providers, assessing safety, documenting coverage rates, and assuring fairness in providing access to vaccines in public and private settings.
Immunization Infrastructure. Local, state, and federal public health agencies incur significant expense in exercising their responsibilities for
monitoring infectious disease outbreaks, vaccine coverage levels, quality of care, and safety concerns. The states differ in the scope and type of public health infrastructure on which they rely to provide both immunization services for disadvantaged individuals and populationwide programs that benefit all citizens within the state.
Some states are better positioned, because of internal administrative arrangements, to use federal funds (e.g., Medicaid, VFC, Section 317 grants, or funds from the newer SCHIP) to support their public health infrastructure. But recent fluctuations in health care programs, reductions in Section 317 grants, and restrictions on the use of federal funds have significantly reduced the ability of many states to develop innovative approaches to program management, data collection, or interactions with private health care providers. Because the Section 317 grants program does not require matching state investments, fiscal incentives for states to share the costs of developing immunization programs that benefit state residents are absent.
The range of per capita contributions among the states is extremely broad: 4 states reported spending more than $10 per capita of their own funds, while the majority of states (31) reported contributions of less than $5 per capita. Only 4 states have direct state funding for a substantial portion (more than 40 percent) of their immunization program infrastructure, and almost half of the states (21) provide no direct state funding for infrastructure needs. When compared with vaccine purchase practices, these estimates indicate a limited commitment within the states to support the public health infrastructure that is required to meet local needs as well as national goals.
Private-Sector Role. The emerging role of the private sector in providing routine medical care for disadvantaged populations requires ongoing attention and oversight to determine whether vulnerable groups are up to date in their immunization coverage. Individual health care providers and health plans have traditionally not been expected to monitor patterns of vaccine coverage or disease within their communities, nor are they currently equipped to assess coverage levels in formats that can facilitate long-term populationwide studies or analysis of local or statewide health patterns.
IMMUNIZATION FINANCE POLICIES AND PRACTICES
Federal funding for state immunization programs underwent a major and rapid rise in response to the 1989–1991 measles epidemic: there was a more than seven-fold increase from $37 million in 1990 to $261 million in 1995. States faced administrative challenges in responding to these initia-
tives, however, and carried forward large amounts of unspent federal grant monies for several years. As a consequence, federal infrastructure grants declined during 1996–1998. In turn, states had to reduce efforts in such areas as clinic hours and mobile sites; immunization outreach; performance assessment; information and program management; and linkage with community-based programs, such as the Women, Infants, and Children (WIC) clinics. The annual average total of state infrastructure grant awards administered by CDC from 1994 to 1999 was $271 million, compared with an estimated total of $123 million in the year 2000 (see Table ES-1). In the past 5 years (1995–2000), Section 317 infrastructure grants to the states have decreased by more than 50 percent.
The states reported to CDC estimates of state-level annual expenditures for 2000 for vaccine purchase ($109 million) and operations ($231 million). These estimates include support from other federal programs (e.g., Maternal and Child Health grants), state revenues, and private contributions (see Table ES-1).
CONCLUSIONS
Conclusion 1: The repetitive ebb and flow cycles in the distribution of public resources for immunization programs have created instability and uncertainty that impeded project planning at the state and local levels in the late 1990s, and delayed the public benefit of advances in the development of new vaccines for both children and adults. This instability now erodes the continued success of immunization activities.
The instability of funding for state immunization programs discourages the development of strategic responses designed to foster disease prevention, improve immunization coverage levels for specific populations and age groups, reduce coverage disparities between low-income groups and the general population, and ensure vaccine safety.
Conclusion 2: Immunization policy needs to be national in scope. At the same time, the implementation of immunization policy must be flexible enough to respond to special circumstances that occur at the state and local levels.
A comprehensive strategy that clarifies the roles and responsibilities of federal and state agencies as well as private-sector providers and health plans is needed to sustain an important intergovernmental partnership in the midst of change and complexity. Consistent policies and practices at both the state and federal levels are essential to foster productive relationships and reduce overlap among multiple programs and services.
National initiatives that provide immunization coverage for larger numbers of disadvantaged families under private and public health insurance plans require state public health responsibilities to shift from direct service delivery to oversight roles concerned with assessment, assurance, and policy development. Yet certain residual immunization needs will remain that will necessitate reliable access to vaccines within the public health sector. States need flexibility and resources to adapt to these shifts, which occur unevenly across and within state borders.
Conclusion 3: Federal and state governments each have important roles in supporting not only vaccine purchase, but also infrastructure efforts that can achieve and sustain national immunization goals.
The federal government should be the senior finance partner for the national immunization system because of the central importance of vaccines in contributing to the nation’s health, and because disease outbreaks in one region can threaten the health of another without respect for political borders. However, the federal role is to supplement and support states, not replace them, in their day-to-day efforts to assure that every child and adult is properly immunized. State legislatures and governments should be expected to sustain an immunization infrastructure that reflects each state’s need, capacity, and performance. Because states are the ultimate stewards of public health, they are responsible for delivering services to those whose immunization needs are not met by the private sector. Performance monitoring, including the development of immunization registries, is important to assure that vulnerable groups have access to adequate primary health care and that public resources are used efficiently in meeting residual needs where necessary.
Conclusion 4: Private health care plans and providers have the capacity to do more in implementing immunization surveillance and preventive programs within their health practices, but such efforts require additional assistance, oversight, and incentives. At the same time, comprehensive insurance and high-quality primary care services do not replace the need for public health infrastructure.
The committee believes health plans should not have the option of providing selective coverage for vaccines once they have been recommended for widespread use, as is currently the practice in most states. For example, all health plans (public and private) that offer primary care benefits for children and adults should bear the costs of integrating all vaccines recommended for widespread use into their basic health care package. Federal mandates for insurance coverage may be necessary to
TABLE ES-1 Recommended Finance Levels for the National Immunization System (Section 317, Vaccines for Children [VFC] Program, and state-level contributions) ($ in millions)
|
|
IOM Committee Recommendation |
|||||
|
Funding Source |
Baseline Annual Avg.a (FY 1994–1999) |
FY 2000 Awarda |
Rationale for FY 2002 Appropriations |
FY 2002 Appropriation |
||
|
FEDERAL |
||||||
|
A. |
Section 317 |
|||||
|
1. |
Vaccine purchase awards |
160 |
162 |
1. |
Sustain current spending levels to meet residual needs |
160 |
|
|
Expenditures (child) |
115 |
N/A |
|||
|
|
Expenditures (adult) |
4 |
N/A |
2. |
Increase federal assistance to the states to purchase adult vaccines to improve coverage rates |
50 |
|
2. |
Infrastructure awards Expenditures |
271b 187 |
123 111 |
3. |
Increase annual award to reflect state capacity as reflected in historical expenditure levels |
200 |
|
|
4. |
Increase allocation of federal funds to states that have significant immunization needs |
|
|||
|
|
5. |
Maintain a “hold harmless” condition for existing state awards |
|
|||
|
|
Total Section 317 Awards |
431 |
285 |
|
410 |
|
|
B. |
VFC (vaccine purchase and operations) |
397 |
548 |
|
548c |
|
|
|
Total Federal Contribution (excluding Medicaid, Medicare) |
828 |
833 |
|
958 |
|
|
STATE |
||||||
|
1. |
Vaccine purchase estimates |
N/A |
109d |
6. |
Sustain and increase state vaccine purchases, especially for adults |
120 |
|
2. |
Infrastructure funds and program operations estimates |
N/A |
231 |
7. 8. |
Build support for infrastructure within each state Add state match requirement for new federal funds |
331 |
|
|
Total State Contribution |
N/A |
340 |
|
451 |
|
|
|
TOTAL (federal/state combined) |
Unknown |
1,173 |
|
1,409 |
|
|
aSource: Centers for Disease Control and Prevention (CDC), National Immunization Program. State-level data based on self-reports by the states submitted to CDC in August 1999, estimating state-level expenditures for the year 2000. bIncludes $261 million in Financial Assistance and $10 million in Direct Assistance; also includes carryover funds as well as new awards. cThis figure is likely to increase when new recommendations of the Advisory Committee on Immunization Practices are incorporated into the vaccine schedule. For example, the pneumococcal conjugate vaccine was approved in February 2000 for all infants<2 years of age and for high-risk children<5 years of age. dState report data include funds from multiple sources, including state revenues and in-kind support, local funds, other federal funds applied to immunization efforts (e.g., Title V, Preventive Health Services Block Grants), and private funds. |
||||||
reduce serious disparities between public and private health plan benefits. Public health agencies should not be expected to supplement immunization benefits within public or private health insurance plans except under short-term conditions, such as emergency outbreaks or “catch-up” conditions following the licensing of new vaccines.
In addition to vaccine coverage benefits, health plan providers can assess immunization coverage rates among their enrollees in ways that can contribute to accurate community health profiles at the state and local levels. These efforts require independent oversight, however, to assure that all groups are included in such assessments, including those populations that are not currently enrolled in public and private health plans. Public health agencies can provide important measurement and audit services, such as assessment and feedback for private providers, as an investment in the quality of community health.
RECOMMENDATIONS
The financial components of the following six recommendations are summarized in Table ES-1.
Recommendation 1: The annual federal and state budgets for the purchase of childhood vaccines for public health providers appear to be adequate, but additions to the vaccine schedule are likely to increase the burden of effort within each state. Therefore, the committee recommends that CDC be required to notify Congress each year of the estimated cost impact of new vaccines that have been added to the immunization schedule so that these figures can be considered in reviewing the vaccine purchase and infrastructure budgets for the Section 317 program.
The committee believes the annual allocation of federal funds for the purchase of vaccines through the VFC program ($505 million for FY 2000) and the Section 317 state grant program ($162 million per year for FY 2000) is sufficient to meet state requests for child vaccines within the immunization schedule recommended by ACIP as of January 2000.2 But additions to the ACIP schedule will expand the burden of preventive health care costs to state and federal health agencies as well as private health plans.
Congress should anticipate such cost increases by requiring that CDC notify Congress each year of two trends: (1) the estimated cost impact of new vaccines (including administration fees) that are scheduled for consideration as additions to the recommended immunization schedule, and
(2) the length of time that may be involved from the point at which such vaccines are recommended by the Advisory Committee on Immunization Practices (ACIP) to the establishment of a VFC contract. Federal and state vaccine purchase budgets should then be adjusted as necessary.
Recommendation 2: Additional funds are needed to purchase vaccines for uninsured and underinsured adult populations within the states. The committee recommends that Congress increase the annual Section 317 vaccine budget by $50 million per year to meet residual needs for high-risk adolescents and adults under age 65 who do not qualify for other federal assistance. The committee further recommends that state governments likewise increase their spending for adult vaccines by $11 million per year.
These estimates are based on calculations of the residual vaccine needs for uninsured at-risk populations, including adults who are younger than age 65 and suffer from chronic disease; for hepatitis B coverage among adolescents; for adults who are at risk because of sexual behavior or occupational settings; and for tetanus coverage for unprotected adults. Both federal and state vaccine purchase budgets will require annual adjustments as vaccine costs change or new vaccines or age groups are added to the adult immunization schedule. Therefore, CDC notification of the impact of such changes should be required annually, as indicated in Recommendation 1.
The improvement of adult immunization rates will require more than increased vaccine purchases. A comprehensive and coordinated adult immunization program needs to be initiated within each state, with leadership at the national, state, and local levels, to encourage the participation of private and public health care providers in offering immunizations to adults under the guidelines established in the ACIP schedule.
Recommendation 3: State immunization infrastructure programs require increased financial and administrative support to strengthen immunization capacity and reduce disparities in child and adult coverage rates. The committee recommends that states increase their immunization budgets by adding $100 million over current spending levels, supplemented by an annual federal budget of $200 million to support state infrastructure efforts.
The committee believes state immunization programs could achieve stability and carry out their roles adequately through the adoption of a
national finance strategy that involves investing a total of $1.5 billion in federal and state funds in the first 5 years to support infrastructure efforts within the states. The federal budget figure of $200 million per year is derived from three calculations: (1) annual state expenditure levels during the mid-1990s, (2) the level of spending necessary to provide additional resources to states with high levels of need without reducing current award levels for each state (known as a “hold harmless” provision), and (3) additional infrastructure requirements associated with adjusting to anticipated changes and increased complexity in the immunization schedule. The additional state contribution of $100 million per year above current spending levels is necessary to reduce current disparities in state spending practices and to address future infrastructure needs in such areas as records management, development of appropriate performance measures and immunization registries, and outreach and education for adult vaccines.
Federal reporting requirements for immunization grants should be reduced to six key areas that reflect the six fundamental roles of the national immunization system discussed in this report. Grant budgetary cycles should be extended to 2 years to give states greater discretion and flexibility to plan and implement multiyear efforts in each area.
Recommendation 4: Congress should improve the targeting and stability of Section 317 immunization grant awards to the states by replacing the current discretionary grant award mechanism with formula grant legislation.
The formula should reflect a base level as well as factors related to each state’s need, capacity, and performance. A state match requirement should be introduced so that federal and state agencies share the total costs of supporting the infrastructure required to operate a national immunization program and respond to the needs of disadvantaged populations.
Recommendation 5: CDC should initiate a dialogue with federal and state health agencies, state legislatures, state governors, and Congress immediately so that legislative and budgetary reforms can be proposed promptly when Section 317 is up for reauthorization in FY 2002.
The construction of a grant formula and the calculation of weights as recommended above is a complex analytical process that requires estimating the appropriate size of the federal base grant; determining the conditions that would facilitate redistribution of federal resources to areas of need but also maintain an adequate level of investment within each
state (the hold harmless conditions); developing an appropriate set of proxy measures that reflect need, capacity, and performance in the field of immunization; and choosing the appropriate multiyear finance mechanism for the allocation of federal funds. This work should begin immediately if its results are to be available when needed.
Recommendation 6: Federal and state agencies should develop a set of consistent and comparable immunization measures for use in monitoring the status of children and adults enrolled in private and public health plans.
Assessments of these rates should allow state and federal governments to monitor immunization levels and identify disparities in need, capacity, and performance over time and among regions, including small geographic areas and selected health plans (e.g., Medicaid, SCHIP, and private insurance). A small set of comparable measures that can harmonize the Health Plan Employer Data and Information Set and the National Immunization Survey, for example, will allow federal and state agencies to monitor state need, capacity, and performance without imposing unnecessarily burdensome reporting efforts on the states that would restrict their ability to use federal funds productively in responding to local circumstances. Such measures can also facilitate efforts by state and federal health officials to assess the quality of primary-care health services within private-sector health plans, so that public health agencies can direct appropriate resources to areas in which private-sector plans do not have sufficient capacity to meet health care needs. The use of consistent immunization measures offers benefit not only for immunization efforts, but also for other national programs that require national investments in primary health care.

















