PAPER CONTRIBUTION A
The Contribution of Social and Behavioral Research to an Understanding of the Distribution of Disease: A Multilevel Approach
George A.Kaplan, Ph.D.; Susan A.Everson, Ph.D., M.P.H.; and John W.Lynch, Ph.D., M.P.H
INTRODUCTION
The popular and scientific press are replete with articles that eagerly herald great breakthroughs in public health, medicine, and biology that will arise from our expanding knowledge in genomics, bioinformatics, and biomedicine. The coming description of the human genome married with rapid advances in biotechnology is thought by many to presage an era in which many of the major sources of disease and disabilities in world populations will be prevented, delayed, or cured. Without a doubt, the increased knowledge of the molecular basis of the pathobiology of disease portends tremendous advances in our understanding and treatment of disease. However, the premise of this paper is that these advances, in and of themselves, will not be able to accomplish these goals. Instead, we argue for a public health-based approach that incorporates knowledge across a multitude of levels, ranging from the pathobiology of disease to the social and economic policies that result in differential patterns of exposure of individuals and populations to risk factors and pathogenic environments. Central
|
Dr. Kaplan is professor and chair, Department of Epidemiology, School of Public Health, and senior research scientist, Institute for Social Research, University of Michigan; Dr. Everson is assistant research scientist, Department of Epidemiology, School of Public Health, University of Michigan; and Dr. Lynch is assistant professor, School of Public Health, and faculty associate, Institute for Social Research, University of Michigan. This paper was prepared for the symposium “Capitalizing on Social Science and Behavioral Research to Improve the Public' s Health,” the Institute of Medicine and the Commission on Behavioral and Social Sciences and Education of the National Research Council, Atlanta, Georgia, February 2–3, 2000. |
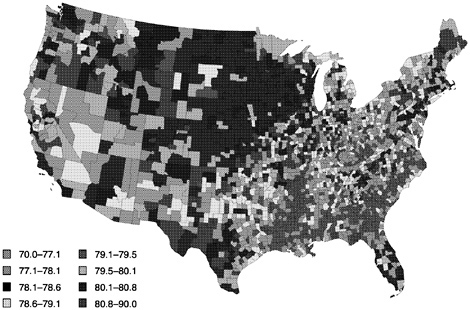
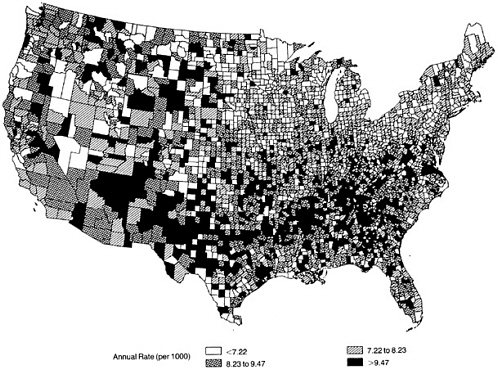
FIGURE 1 Geographic distribution of female life expectancy at birth by county and county clusters, United States, 1990.
to such a focus is an important role for economic, behavioral, and social factors, whether manifested at the individual or population level. For it is to these factors that we will largely have to look to develop a complete explanation of core epidemiologic observations concerning group and geographic differentials in the prevalence and incidence of disease and time trends in disease. In what follows we will review selected information on variations in life expectancy and the occurrence of a number of major public health problems and discuss how such a multilevel approach provides critical perspectives on the causes of these variations and on opportunities to reduce them.
Life Expectancy and Death Rates from All Causes
Overall life expectancy at birth reached 76.5 years in the United States in 1997, with almost steady increases since 1950 (NCHS, 1999). Since 1980, life expectancy at birth increased by 5.1% for males to 73.6 years, and by 2.6% for females to 79.4 years, and life expectancy at age 65 increased by 12.8% to 80.9 years, and by 4.9% to 84.2 years, for males and females, respectively. Despite these increases the United States still compares poorly to many countries—ranking twenty-fifth for males and nineteenth for females on a list of 36 countries compiled by the National Center for Health Statistics (NCHS, 1999).
Within the United States there is considerable variation in life expectancy. For example, Figure 1 presents variations in female life expectancy at birth for counties and county clusters in the United States in 1990 (Murray et al., 1998). Life expectancy at birth differs between areas by as much as 16.5 years for males and 13.3 years for females. In these analyses, the largest difference in life expectancy is between American Indian or Alaskan Native males in the cluster of Bennett, Jackson, Mellette, Shannon, Todd, and Washabaugh counties in South Dakota (56.5 years) and Asian Pacific Islander females in Bergen County in New Jersey (97.7 years). As Murray et al. (1998, p. 9) point out, this 41-year range in life expectancy within the United States is “…equal to 90 percent of the global range from the population with the lowest life expectancy, males in Sierra Leone, to the population with the highest, females in Japan.”
There also is substantial geographic variation in life expectancy at birth within race/ethnicity and sex subgroups. For example, while American Indian and Alaskan Native males have a life expectancy of 56.5 in the six-county area in South Dakota previously mentioned, this group has a life expectancy of 92.3 years in Los Angeles County. Life expectancy for white males and females also varies considerably by county—with ranges of 9.9 years and 7.6 years, respectively.
As might be expected from trends and differences in life expectancy, consideration of age-adjusted mortality rates from all causes also indicates substantial variation by gender, race/ethnicity, and time. Figure 2 (Hoyert et al., 1999)
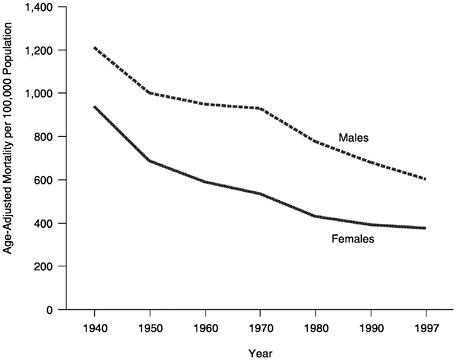
FIGURE 2 Age-adjusted, all cause mortality rates by sex, United States, 1940 – 1997.
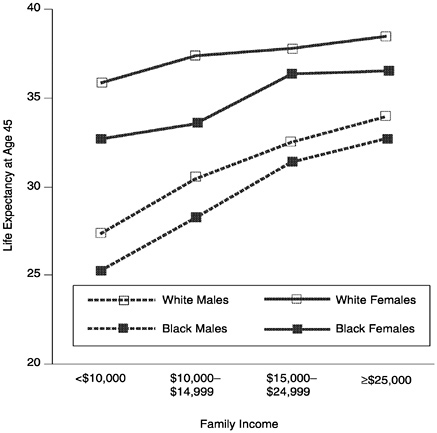
FIGURE 3 Life expectancy at age 45 by family income, race, and sex, United States, 1979–1989.
shows the decline in age-adjusted mortality rates from all causes for males and females between 1940 and 1997. During this period, rates declined by 50% for males and 60% for females. However, these declines were not experienced equally by all groups. For example, during the period from 1950 to 1997, age-adjusted mortality rates from all causes declined by 40.4% for white males, 33.6% for black males, 44.5% for white females, and 50.7% for black females. Thus, during this period, mortality differentials between white and black males increased, while for females they decreased. Detailed information for other race and ethnicity groups is not available for this period.
There is considerable variation between states in overall mortality rates. For example, in 1997, the state with the lowest age-adjusted (1990 standard) mortality rate was Hawaii (572.5 per 100,000 population), and the highest rate (exclusive of the District of Columbia) was found in West Virginia (865.1 per 100,000). This level of geographic variation in age-adjusted mortality, a difference of almost 300 deaths per 100,000 population, is very significant given that
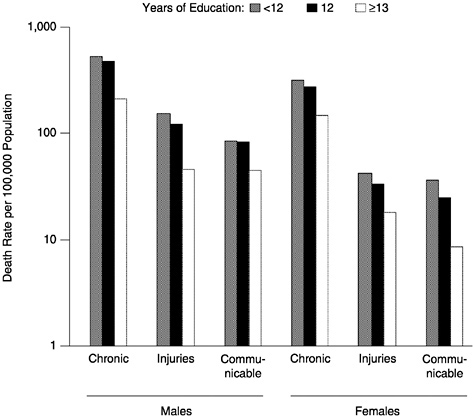
FIGURE 4 Age-Adjusted death rates among adults, age 25–65, by cause of death, sex and education, United States, 1995.
it is 40% of the overall rate for the United States (742.7 deaths per 100,000 population using the 1990 U.S. standard population).
Socioeconomic variations in mortality have been widely noted (Kaplan et al., 1987). For most diseases and health status indicators and for most measures of socioeconomic position there is an inverse relationship (Haan et al., 1987). Figure 3 shows the relationship between family income and life expectancy (1979–1989) at age 45 for white and black men and women (all ethnicities) in the United States (NCHS, 1998). The gradient between socioeconomic position and death rates is clearly seen for broad classes of causes of death, as shown in Figure 4 (NCHS, 1998).
The strong effects of socioeconomic position on mortality, coupled with substantial heterogeneity by race/ethnicity and geographic place in mortality rates and strong secular trends can lead to phenomena of major public health significance. In analyses of 1984–1993 trends in coronary heart disease (CHD) mortality in North Carolina, Barnett et al. (1999) found that declines in mortality were experienced by white men of all social classes, with the greatest benefit among those in the highest social class, while only the highest social class of
black men showed any decline at all. For example, black men in social classes III and IV (e.g., occupations such as mechanic, butcher, janitor, welder, truck driver, laborer, animal caretaker) had average annual changes in Coronary Heart Disease (CHD) mortality of +0.8% and 0.0%, respectively, whereas white men in the same social classes had average annual changes of -2.1% and -6%. Over the 10-year period, black men in the lowest social class experienced an 8.0% increase in CHD mortality, and white men in the same social class experienced a 16% decline.
UNDERSTANDING VARIATIONS IN HEALTH
These large variations in life expectancy and mortality, and similar variations in other health outcomes, present fundamental challenges to our understanding of the determinants of health in individuals and populations and of how we can reduce the burdens of disease and disability. We propose that there is no single or simple explanation for such heterogeneity, and that it is highly unlikely that the triad of genomics, bioinformatics, and biomedicine, with their focus on molecular etiologic forces located within the individual, will help explain very much of the heterogeneity in health and disease among social groups, places, and times. While such an individualistic focus can help us explain events within individuals it is unlikely to be very successful in explaining the patterning of disease by subgroups, places, or eras (Rose, 1992). However, we do not argue that we should completely dismiss such pursuits and replace them solely with a focus on macrolevel determinants of health. Such an ecologic or macrolevel focus is likely to miss many opportunities for increased understanding of disease mechanisms and intervention opportunities and suffers from its own version of tunnel vision.
Observations of the complex patterning of disease, the “lens” of epidemiology, leads instead to a new approach that attempts to bridge various levels of explanation and intervention, bringing together theory and empirical work that tie together observations of causal influence and mechanism at multiple levels. It thus represents an explanatory enterprise that does not exclusively privilege the proximal, but seeks opportunities for understanding and intervention at both upstream and downstream vantage points (Figure 5). Such a pursuit is in its infancy and represents a major challenge that will succeed only with a broad interdisciplinary vision accompanied by state-of-the-art thinking in multiple domains.
In what follows we describe some general epidemiologic and demographic features of six major public health problems: low birthweight, childhood asthma, firearm-related deaths in adolescents and young adults, coronary heart disease, breast cancer, and osteoporosis. After describing the general patterns with which these problems appear, we then sketch out some examples of the type of multilevel approach that is suggested in Figure 5.
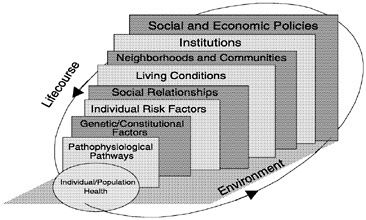
FIGURE 5 Multilevel approach to epidemiology.
THE DISTRIBUTION OF DISEASE-SOME ILLUSTRATIVE EXAMPLES
Low Birthweight
Overall
Low birthweight, defined as a live birth less than 2,500 grams, is one of the most vexing problems facing the public health community in the United States. Low birthweight can result from babies being born prematurely and/or being born too small, and it is the major underlying cause of infant mortality and early childhood morbidity. The United States has significantly higher rates of low birthweight than other comparably developed nations. For instance, the average rate of low birthweight in the United States between 1990 and 1994 was 7 births per 1,000, while in countries like Norway, Sweden, and Finland, rates were as low 4–5 per 1,000 (UNICEF, 1998). Within some U.S. population subgroups these rates of low birthweight exceed 12 per 1,000 and match the very high levels found in some Sub-Saharan African and other developing countries. Infant mortality has declined significantly over the last 30 years, in large part due to the effects of neonatal intensive care and drug therapies that have helped to increase the survival of low-birthweight infants. In stark contrast, rates of low birthweight have remained stubbornly high (NCHS, 1998). Thus, the United States has a serious and persistent problem of low birthweight, which so far seems intractable to advances in medical care and technology.
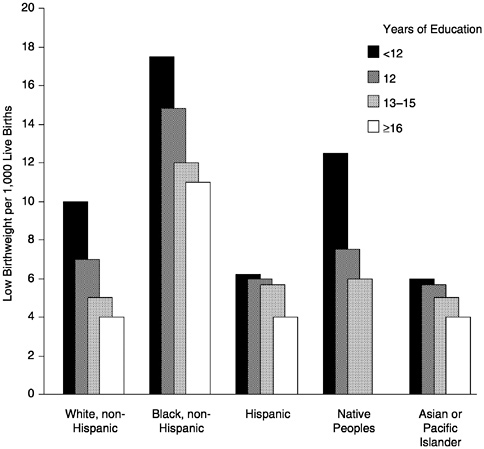
FIGURE 6 Low birthweight by education and race/ethnicity, United States, 1996.
Distribution by Race and Socioeconomic Position
As alluded to above, the problem of low birthweight is not distributed randomly across population subgroups. Figure 6 shows rates of low birthweight in 1996, according to the education and race/ethnic group of mothers aged 20 or older (NCHS, 1998). These data show both educational and race/ethnicity differences in low birthweight.
The highest levels of low birthweight, around 18 per 1,000, were among the least educated black, non-Hispanic women. The lowest rates, around 4 per 1,000, were among the most educated Hispanic, Asian Pacific Islander, and white, non-Hispanic women. While there are important educational gradients in almost every race/ethnic group, the largest differences are between race/ethnic groups (NCHS, 1998). This fact is further emphasized in a 1992 study in the New England Journal of Medicine showing that even among babies born to college-educated mothers, infant mortality was significantly higher among black babies. This difference in infant mortality was entirely attributable to the higher proportion of low birth-
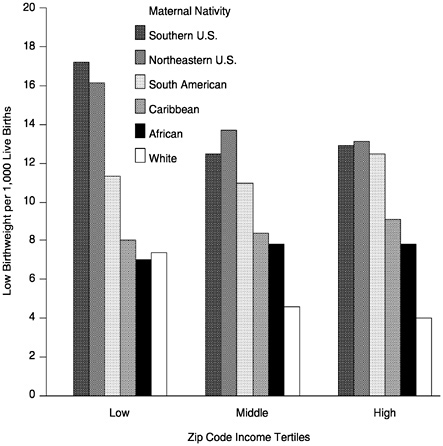
FIGURE 7 Low birthweight by zip code income tertiles and maternal nativity among “Blacks, “New York City, 1988–1994.
weight black infants (Schoendorf et al., 1992). In making any comparisonbetween race/ethnic groups in seemingly equal socioeconomic strata, such as those with a college education, it is important to remember that the social meaning and economic value of a college education may be quite different for different race/ethnic groups. Health differences between race/ethnic groups largely reflect a wide array of accumulated social exposures, so it would be naive to expect that we can capture all of these social exposures in one socioeconomic factor such as education. We must be aware of the problems of incommensurability of socioeconomic indicators in comparing across race/ethnic groups (Krieger et al., 1993; Kaufman et al., 1997). Nevertheless, the differences in low birthweight across race/ethnic groups cannot be ignored and deserve more intensive investigation. Adding to the complexity of this picture is recent research showing that birthweights of African-born black women are more closely related to those of U.S.-born white women than to U.S.-born black women (David and Collins, 1997). (See Figure 7.) Additionally, Fang et al. (1999) have shown that rates of low birthweight among
“black” women vary considerably across all income levels, according to the country of birth of the mother.
Trends
Low birthweight continues to be a stubborn public health problem, with little or no decline in rates over the last 20 years (See Figure 8.). In fact, between 1985 and 1996, New Hampshire was the only state that did not record an increase in the percentage of low-birthweight babies. For the United States, overall rates rose by an average of 9%, but in some midwestern states such as Minnesota, Iowa, Nebraska, and Indiana, low birthweight increased by as much as 20% (Annie E.Casey Foundation, 1999).
Geographic Distribution
Not unexpectedly, there also is considerable geographic variation in low birthweight across the United States. As Figure 9 shows, low birthweight is particularly concentrated in the southeastern states. These geographic differences may reflect both compositional and contextual influences on low birthweight. Compositional influences relate to characteristics of the individuals who reside
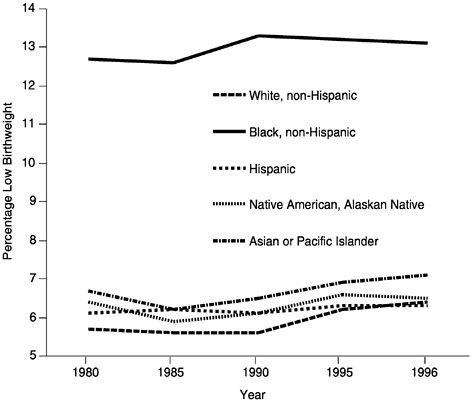
FIGURE 8 Trends in low birthweight by race/ethnicity, United States, 1980 –1996.
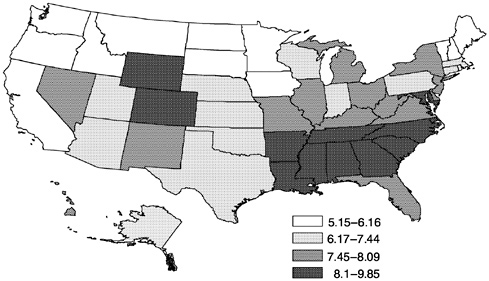
FIGURE 9 Geographic distribution of percent of live births under 2500 grams by state, United States.
in a certain area, while contextual influences refer to nonindividual aspects of the environment that also may affect rates of low birthweight. For instance, Kaplan and colleagues (1996) have shown how the extent of income inequality within a state is correlated with rates of low birthweight even after adjustment for the average incomes in the state (r = -065, p < .001). As Paneth has argued, “The effects of poverty at the level of the individual, the family and the community need all to be taken account of; the context in which pregnancy occurs is larger than the womb” (1995, p. 31).
Costs
The assessment of costs for any health problem is a complex undertaking that requires making various assumptions about what should be included and excluded from cost estimates. In the case of low birthweight, there are direct and indirect costs. The direct costs are those associated with both the immediate medical care for low-birthweight babies and the longer-term implications that low birthweight has for enduring health problems in childhood. In addition, the health complications of low birthweight place additional burdens on later child care and educational needs. Lewitt et al. (1995) estimated that in 1988, for children aged 0–15 who had been born at low birthweights, the health care, child care, and educational costs directly attributable to their birthweight were between $5.5 billion and $6 billion more than if those children had been normal weight at birth.
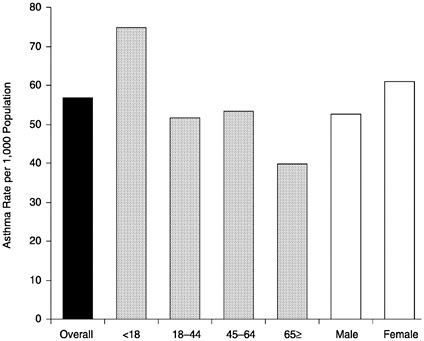
FIGURE 10 Asthma prevalence rate by age, and sex, United States, 1995.
Childhood Asthma
Overall
Asthma is one of the most common chronic health problems in the United States (See Figure 10). In 1995 it was estimated to affect almost 15 million people—almost one-third of them under age 18 (Mannino et al., 1998). Asthma prevalence has increased dramatically over the last 20 years, and what limited comparisons can be made to suggest that the increases observed in the United States may parallel increases in some other industrialized nations such as France, Britain, and Australia (Grant et al., 1999). However, the prevalence of asthma is generally lower in less industrialized countries (Cookson, 1987). The symptoms of asthma—wheezing, breathlessness, and coughing—are brought on by inflammatory processes in the airways and immunoglobulins in response to a wide variety of environmental toxins and allergens such as dust mites, cockroaches, pollens, and particular agents that reduce the overall air quality (Clark et al., 1999). The potentially greater biological vulnerability of children due to their developing immune systems may place them at heightened risk of asthmatic reactions to environmental irritants. Thus, there is a need for much more basic and applied research on asthma. As Grant et al. (1999) state, “Changes in
environmental risk factors and exposures may contribute to recent trends, but little information is available relating specific risk factors to either longitudinal asthma trends, geographic variability, or high-risk populations” (p. S1).
Distribution by Race and Socioeconomic Position
Asthma morbidity and mortality are disproportionately higher among disadvantaged children (Weiss et al., 1994). Evans (1992) estimated that asthma is 26% more prevalent among black than white children. Data on socioeconomic and race/ethnicity differences in asthma prevalence among children are limited. However, Figure 11 reveals a growing gap in asthma prevalence between blacks and whites from 1980 to 1994 when averaged across all age groups (Mannino et al., 1998).
Black children also are significantly more likely to be hospitalized for asthma (Figure 12). This is true at every level of zip code income. In fact, even black children living in zip codes where the median income was greater than $40,000 per year are much more likely to be hospitalized for asthma than white children living in the poorest income areas. Understanding what these race/ethnic and socioeconomic differences reflect is a complex task, but it is possible that residential environments for black children are poorer quality, at
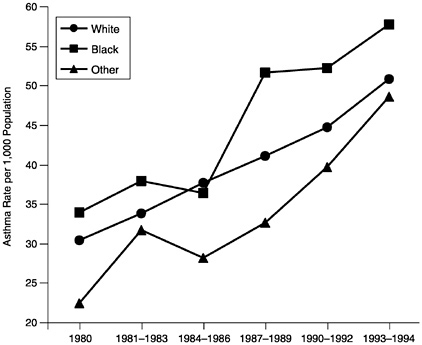
FIGURE 11 Asthma prevalence trends by year and race/ethnicity, United States, 1980–1994.
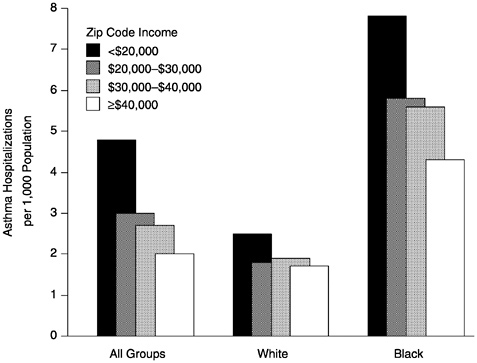
FIGURE 12 Asthma hospitalization for children, aged 1–14, by median household income according to zip code of residence, United States, 1989–1991. SOURCE: NCHS, 1998.
every level of zip code income. U.S. cities are highly segregated residentially (Massey and Denton, 1993), and important environmental differences may exist in levels of inflammatory bioallergens between the residential areas occupied by blacks and whites.
Trends
Prevalence, emergency department treatment, and mortality rates for asthma have all increased in the last 20 years (NHLBI, 1999). Disturbingly, these increases appear faster among children than adults and may reflect the greater biological vulnerability of children to the effects of bioallergens. Figure 13 shows the significantly higher prevalence of asthma among 5- to 14-year-olds in the last 10 years. The sharpest increase has been among the very young (Mannino et al., 1998). Among preschool children, asthma prevalence has increased 160% from 1980 to 1994.
Geographic Distribution
There are no large-scale United States studies assessing geographic variation in emergency department visits or hospitalizations, although self-reported prevalence estimates suggest rates are highest in the western states and lowest in the South (Collins, 1997). Smaller-scale studies also have demonstrated urban-rural differences (Malveaux et al., 1995). In a sample of children in the Bronx in New York, Crain et al. (1994) estimated that there was a cumulative prevalence of asthma of 14.3% and period prevalence of 8.6%. These estimates for inner city children were twice the national average.
Costs
In 1993 there were more than 150,000 hospitalizations for children under age 15 (CDC, 1995). The American Lung Association estimates that the direct health care costs for asthma in the United States are almost $10 billion, with inpatient hospital care being the largest single expenditure. Indirect costs related to both loss of work and missed school days may add up to more than $1 billion annually. It is estimated there are more than 10 million school days missed an-
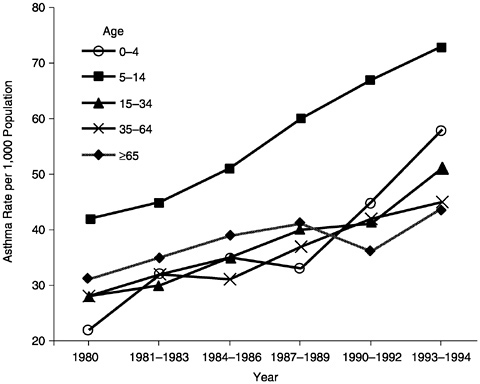
FIGURE 13 Asthma prevalence by year and age, United States, 1980–1994.
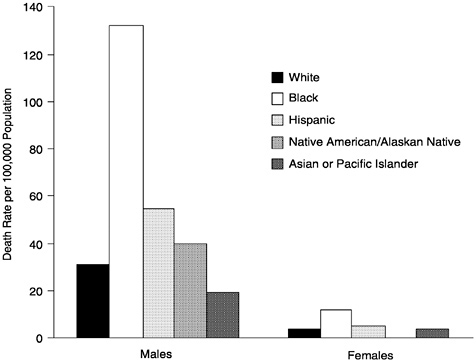
FIGURE 14 Death rates per 100,000 for firearm-related injuries among persons age 15– 24 by sex and race/ethnicity, United States, 1996.
nually due to asthma. These productivity losses through work and school are estimated to cost almost $2 billion annually (American Lung Association, 1998).
Firearm-Related Deaths Among Youth and Young Adults
Overall
Nowhere is the important contribution of injuries to the population pattern of death and disability more evident than when considering the health status of youth and young adults. Rates of death from injuries rise from 14.2 per 100,000 population for children age 10 –14 to 66.1 per 100,000 population for those age 15–19, and reach a level in the age 20- to 24-year-old group (79.9 per 100,000 population) that is not exceeded until age 75–84. Injuries, including unintentional injuries, homicide, suicide, and legal intervention, are the leading cause of death for 15- to 24-year-olds, accounting for approximately 75% of the 32,443 deaths in this age group in 1996.
Even more striking is the role of firearms in these deaths. Firearm-related injuries accounted for 25.9% of the deaths among 15- to 24-year-olds in 1997 (NCHS, 1997). In 1996, deaths from firearm-related injuries among 15- to 24-year-olds almost reached the level of those due to motor vehicle accidents (24.2
per 100,000 population versus 29.2 per 100,000 population, respectively NCHS, 1998).
Distribution by Race and Sex
The burden of these deaths is not shared equally (Figure 14). While non-Hispanic whites have the highest numbers of deaths from firearm-related injuries, males—and particularly non-Hispanic African American males—have substantially elevated rates of death from firearm-related injuries compared to females and males from other groups. Overall, the age-adjusted 1997 death rate for males from firearm-related injuries was 6.2 times higher than that for females (22.4 per 100,000 population versus 3.6 per 100,000 population) (NCHS, 1998). Among males, in 1996 the lowest rates were among Asian Pacific Islanders (19.6 per 100,000 population) and the highest rates, 6.7 times higher, were among African Americans (131.6 per 100,000 population).
Distribution by Socioeconomic Position
Given that the familiar inverse gradient between measures of socioeconomic position and health outcomes is found for homicide and suicide (Baker et al., 1992), it would not be surprising to find that it also is seen for firearm-related deaths among 15- to 24-year-olds. However, national statistics on this outcome do not generally stratify by socioeconomic position, a general deficiency that has been noted elsewhere (Krieger et al., 1997). Baker et al. (1992) provided some evidence for the association with firearm-related deaths, although not specifically for 15- to 24-year-olds, who account for 25% of all firearm-related deaths. A strong and generally consistent inverse association between per capita income of the area of residence of the decedent and rate of firearm-related deaths (1980–1986) was seen for unintentional injuries, homicide, and suicide related to firearms. For example, areas with a per capita income less than $6,000 compared to areas where it is equal to or greater than $14,000 had rates of unintentional death from firearms, homicide, and suicide that were elevated seven-, three-, and two-fold,respectively.
Trends
There have been substantial trends in firearm-related deaths among 15- to 24-year-olds over the past few decades. From 1970 to 1980 there was a 33% increase, followed by a 16% decrease in 1985, followed by steady increases totaling 158% up to 1993 and gradual declines since then through 1997. From 1993 to 1996, there was a 22% decrease in firearm-related mortality in this group. Although the general direction of these trends has been consistent, there have been variations in magnitude by race/ethnicity. For example, Figure 15
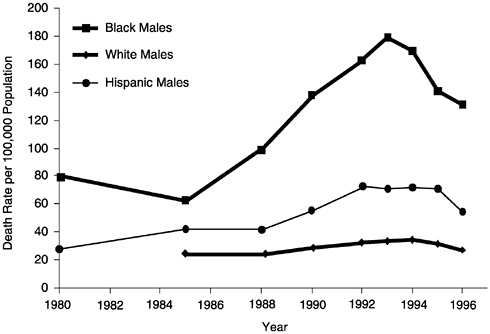
FIGURE 15 Death rates per 100,000 for firearms-related injuries among males, age 15– 24, by race/ethnicity, United States, 1980–1996.
illustrates the faster acceleration from 1985 to 1993 of firearm-related deaths among African American and Hispanic men compared to white men.
Geographic Variation
There is substantial geographic variation in the occurrence of firearm-related deaths. The general picture, across all age groups, reflects higher rates of firearm-related homicide in core metropolitan areas compared to rural areas, while there are higher rates of firearm-related unintentional injuries in rural areas (Baker et al., 1992). Fingerhut et al. (1998) analyzed 1979–1995 trends in firearm-related homicide and found similar secular trends for core metropolitan areas, fringe metropolitan areas, different size metropolitan counties, and non-metropolitan counties. Within the overall pattern of geographic differences, there is considerable unexplained heterogeneity. For example, using data available from the Centers for Disease Control and Prevention (CDC) WONDER (on-line), we examined state differences in 1996 firearm-related deaths for 15-to 24-year-old blacks and whites and found substantial variation. On average, death rates from firearm-related injuries were 7.1 (median, 5.8) times higher among blacks than for whites, but the rates of relative disadvantage ranged from 2.4-fold in Texas and 2.7-fold in North Carolina to 12.1-fold in Illinois and 14.6-fold in Massachusetts.
Costs
The calculation of costs of firearm-related injuries and deaths is complex and is hampered by a significant lack of data. Work in this area has generally not reported separate estimates for specific age groups. Nationwide, for all ages, the medical costs of gunshot injuries were recently estimated at $2.3 billion per year (Cook et al., 1999). Total annual medical care expenses, indirect costs for long-term disability, and lost productivity associated with premature death have been estimated at $20.4 billion (Max and Rice, 1993). Because long-term disability and lost productivity costs would be high for firearm-related deaths and injuries to 15- to 24-year-olds, it is likely that a substantial portion of the $20.4 billion reflects costs to children and young adults.
Cardiovascular Disease in Adults
Overall
Heart disease is the leading cause of death in the United States. In 1996, this was true for white males and females, African-American males and females, Asian-American males and females, Hispanic males and females, and American Indian males and females. Overall, deaths from heart disease accounted for 31.7% of all deaths in 1996 (NCHS, 1998) and were responsible for 15.8% of the years of potential life lost before age 75 (NCHS, 1998). Diseases of the heart account for 11.2% of the deaths among those 25–44 years of age, 27.1% among those age 45–64, and 35.7% among those 65 years or older. Coronary heart disease, which accounts for two-thirds of all heart disease deaths, alone accounted for more than 2 million hospital stays in 1995, with an average length of stay of 5.3 days, and almost 10 million physician visits (NHLBI, 1998).
Distribution by Race and Sex
There is considerable variation in rates of death from cardiovascular disease (CVD) by race, ethnicity, and sex (Figure 16). Age-adjusted rates of death for males are 82.1% higher than they are for females (NCHS, 1998). Substantial variation is seen when comparing across race and ethnicity, with the rates for Asian Pacific Islander women, for example, being one-third the rates for African American women, and the rates of death for African American men being more than 2.5-fold greater than for Asian Pacific Islander men. Generally the highest rates are for African American men and women, with the next highest rates being for non-Hispanic white men and women. Problems related to incorrect information on death certificates and census undercounts may lead to systematic biases in rates for some groups, for example, those of Hispanic ethnicity (Goff et al., 1997).
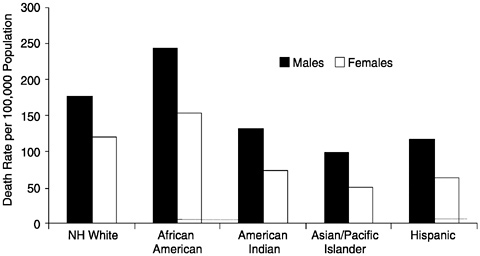
FIGURE 16 Age-adjusted death rates for diseases of the heart by race/ethnicity and sex, United States, 1996. NOTE: NH = non-Hispanic.
Distribution by Socioeconomic Position
There is substantial evidence that various measures of socioeconomic position (SEP) are importantly associated with mortality and morbidity from CVD (Kaplan and Keil, 1993; NHLBI, 1998). Figure 17 shows the inverse association between family income level and heart disease death rates for 25- to 64-year-old non-Hispanic whites and African-Americans. Those in families with incomes less than $10,000 had death rates that are 2.4- to 2.8-fold higher than those with family income greater than $15,000 in 1979–1989. A similar inverse patterning is seen when other measures of SEP, such as education and income of individuals, families, or county of residence are considered (NHLBI, 1995). Other studies have indicated that the impact of SEP on cardiovascular disease (CVD) extends to measures of CVD morbidity as well as subclinical disease (Lynch et al., 1997).
Geographic Variation
There is substantial variation in the geographic distribution of CVD. Generally speaking, death rates from CVD are highest in the southeastern portion of the United States and lowest in the western Mountain states, Alaska, and Hawaii (NHLBI, 1998). Figure 18 shows the similar variation in age-adjusted rates of death from ischemic heart disease among 25- to 74-year-olds in 1996. There also is substantial geographic variation in CVD differentials by race and ethnicity. For example, overall age-adjusted deaths rates from ischemic heart disease among those 25–74 years of age were approximately 3% higher in African-Americans in 1996 than in whites. However, the differential varied widely, from
a 20 to 51% excess in California and Nebraska, respectively, to 32 –54% lower rates for African-Americans in Washington and Minnesota.
Trends
One of the most remarkable achievements of the latter part of this century has been the substantial decline in death rates from CVD. For example, from 1900 to 1950, rates of death from CVD among those 45–54 years of age increased by 28%, but from 1950 to 1995 these rates declined by 68% (NHLBI, 1998). Given the tremendous burden from CVD in the population, these changes had major consequences. Analyses by the National Heart, Lung, and Blood Institute (NHLBI) indicate that this decline in CVD mortality rates since 1994 translates into more than one million fewer deaths from CVD during that period (NHLBI, 1998). Other analyses indicate that the decline in CVD mortality from 1965 to 1995 accounted for 70% of the 5.6-year gain in life-expectancy seen during that period (Vital Statistics of the United States, 1900 –1967; Arriaga, 1984; 1989).
There is substantial demographic and geographic variation in who has benefited from the decline in CVD (Sempos et al., 1988). For example, the average annual percentage decline in age-adjusted coronary heart disease death rates for white males and females was greater than for black males and females from 1980 to 1996. In some periods the differences were substantial—the annual percentage decline for males was 50% greater (-3.6% versus -2.4%) for whites than for blacks during 1980–1989. Analyses of these trends also indicate that areas that are better off socioeconomically have benefited more from the declines in CVD mortality (Wing et al., 1988). Barnett et al. (1999), in their analyses of 1984–1993 trends in CHD mortality in North Carolina, found that social class inequalities in coronary heart disease mortality actually widened during this period for both black and white men. Moreover, whereas declines in mortality
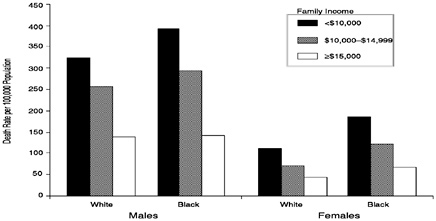
FIGURE 17 Heart disease death rate per 100,000 among persons age 25–64, by sex, race, and family income, United States, 1979–1989.
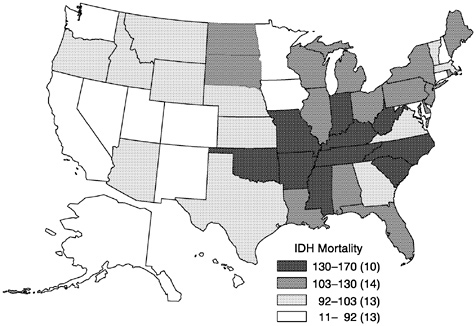
FIGURE 18 Geographic distribution of age-adjusted mortality rates from ischemic heart disease among persons age 24–75, by state, United States, 1996.
were experienced by white men of all social classes, with the greatest benefit among those in the highest social class, only the highest social class of black men showed any decline at all.
Costs
Given the high population burden of CVD, it is to be expected that CVD is associated with substantial costs. According to recent NHLBI calculations, the direct costs associated with CVD were $171 billion in 1998, and the indirect costs related to morbidity and lost productivity were $103 billion. Thus, while there have been substantial advances in reducing the health burden from CVD, it still is associated with considerable economic costs to society.
Overall Breast Cancer
Overall
Breast cancer is the most commonly diagnosed cancer in women, not counting skin cancers, accounting for one in three cancer diagnoses. Breast cancer is the leading cause of death among women aged 40 to 55 (Henderson,
TABLE 1. Age-Specific Risk of Developing Breast Cancer
|
Age |
Estimate |
|
25 |
1 in 19,608 |
|
30 |
1 in 2,525 |
|
35 |
1 in 622 |
|
40 |
1 in 217 |
|
45 |
1 in 93 |
|
50 |
1 in 50 |
|
55 |
1 in 33 |
|
60 |
1 in 24 |
|
65 |
1 in 17 |
|
70 |
1 in 14 |
|
75 |
1 in 10 |
|
85 |
1 in 9 |
|
Ever |
1 in 8 |
1995). However, lung cancer mortality rates are higher than breast cancer mortality rates in women overall (American Cancer Society, 1995), and three times as many women will experience heart disease as breast cancer in their lifetime.
Incidence of breast cancer increases greatly with age; more than three-quarters of all cases occur in women over age 50. Current estimates are that one in eight American women will develop breast cancer in her lifetime (Feuer et al., 1993). However, as noted by Feuer et al. (1993), it is important to look at age-specific probabilities because they provide a more accurate estimate of an individual's risk of breast cancer at a specific point in time, compared to lifetime probabilities (see Table 1). In other words, a 50-year-old woman who is currently cancer free has little more than a 2% risk of developing breast cancer over the next 10 years.
Breast cancer also occurs in men but is extremely rare, accounting for less than 1% of the overall incidence of and mortality due to breast cancer.
Distribution by Race and Socioeconomic Position
Breast cancer incident rates vary widely by race/ethnicity within the United States. After age 45, the incidence of breast cancer is higher in white women than in black women; however, age-specific incidence in women less than age 45 is higher in blacks (Kelsey and Bernstein, 1996; Trock, 1996).
Women of other racial or ethnic groups also experience lower incidence of breast cancer than white women. For example, compared to United States-born white women, the incidence of breast cancer is 50% lower in Asian-American women born in China or Japan and 25% lower in United States-born Asian women (Stanford et al., 1995). Figure 19 shows breast cancer incidence rates for
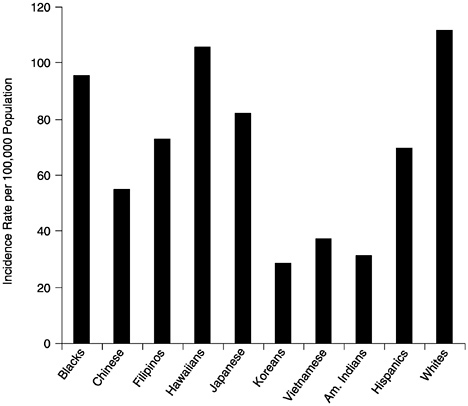
FIGURE 19 Female breast cancer incidence rates by race or ethnicity, United States, 1998–1992. SOURCE: American Cancer Society (1997).
United States women by race/ethnicity, age-adjusted to the 1970 United States population (American Cancer Society, 1995).
Mortality from breast cancer does not follow the same race/ethnicity pattern as that seen for breast cancer incidence. Breast cancer mortality rates among blacks are worse than among whites at all ages in the United States. The National Cancer Institute's (NCI's) Black/White Cancer Survival Study found that the risk of dying in the first 5 years after diagnosis was two times higher among black breast cancer patients than among white patients (Eley et al., 1994). The mortality rate among African American women over all ages is 31.2 per 100,000 population, compared to 26 per 100,000 population for white women (American Cancer Society, 1995). Mortality rates among other racial or ethnic groups, such as those shown in Figure 19, are less than 20 per 100,000 population (Perkins et al., 1995).
Unlike most chronic diseases, incidence rates of breast cancer are positively related to socioeconomic position. Reproductive factors known to increase risk for breast cancer include late age at first full-term pregnancy and low parity,
both of which vary by socioeconomic position and likely contribute to the excess risk of breast cancer observed in better-educated, higher-income women (Kelsey and Bernstein, 1996). In contrast to breast cancer incidence, mortality from breast cancer is higher among more socioeconomically disadvantaged women. Growing evidence suggests that this is partly due to a more advanced stage at diagnosis and/or tumor characteristics. For example, Gordon (1995) reported that education and income were inversely related to estrogen receptor-negative tumors, after controlling for age, race or ethnicity, and known breast cancer risk factors. Estrogen receptor-negative breast tumors are strongly associated with poorer survival and, interestingly, are more likely to be diagnosed in African American women than white women.
Trends
Breast cancer incidence increased steadily between 1940 and 1982 and then more markedly between 1982 and 1987, prompting the suggestion, especially in the popular press, that an “epidemic” of breast cancer was occurring (Lantz and Booth, 1998). However, it is clear that a higher prevalence of mammography screenings, earlier diagnoses, and related factors account for a large proportion of this increase (Forbes, 1997; Wun et al., 1995). Moreover, incidence rates in younger women increased only slightly during the same time, and since 1987, incidence rates appear to have stabilized somewhat (Kosary et al., 1995), although this trend varies slightly by race/ethnicity. It has been suggested that the observed increase in breast cancer incidence was partially due to the increased prevalence of risk factors for breast cancer, particularly reproductive factors, such as later age at first birth and smaller family sizes than in previous generations (American Cancer Society, 1995). Until relatively recently, trends in incidence of breast cancer were similar for white women and African American women. Since 1992, however, it appears that the incidence has increased somewhat among African American women while decreasing or remaining stable among whites (American Cancer Society, 1995).
For white women in the United States, the mortality rate from breast cancer was relatively stable between 1940 and 1990 but has improved markedly during the 1990s, with the greatest improvements seen in younger age groups (National Cancer Institute, 1996). In contrast, the mortality rate among African American women increased by more than 19% between 1973 and 1988 and has continued to increase during the 1990s, although this increase has slowed to less than 3% (National Cancer Institute, 1996).
Taken together, the observed trends in breast cancer incidence and mortality suggest that with improved breast cancer management more women are surviving with breast cancer than ever before. However, there is clear evidence that racial disparities in both breast cancer incidence and mortality still exist.
Geographic Variation
Breast cancer incidence varies widely by geographic location. In the United States, evidence suggests that women living in the northern states tend to have higher rates of breast cancer than women living in the southern states (Kelsey and Horn-Ross, 1996). Breast cancer incidence also varies greatly internationally, as seen in Figure 20. The San Francisco Bay area has been identified as having one of the highest rates of breast cancer among white women in the world, with rates that are more than four times greater than in Asian countries and more than 40% higher than in most European countries (Parkin et al., 1997). Recently, it was determined that regional differences in reproductive risk factors (e.g., low parity, late age at first birth), many of which are associated with a more advantaged socioeconomic position, accounted for the high incidence rates of breast cancer in the Bay area (Robbins et al., 1997). Figure 20 also shows how breast cancer incidence varies by race/ethnicity throughout the world. For example, rates among non-Jewish Israeli women are dramatically lower than the rates among Jewish Israeli women. Also, rates in Hawaii vary greatly by ethnicity. Asian women generally have some of the lowest rates of incident breast cancer among developed nations; however, rates in Asia, as well as in central European nations, have risen markedly in recent years (Kelsey and Horn-Ross, 1993). For example, breast cancer incidence in Japanese women more than doubled in the 15-year period from 1970 to 1985, although rates of breast cancer in Japanese women are still dramatically lower than rates in most American women (Kelsey and Bernstein, 1996).
Costs
Breast cancer has enormous direct and indirect costs, as well as psychosocial costs in terms of reduced quality of life, stress, and the psychological demands on the individual, family member, and friends coping with the illness. An estimated $6.6 billion is spent each year in direct medical care costs for breast cancer in the United States alone (Brown and Fintor, 1995). Median survival time for breast cancer patients is nearly a decade; consequently, the greatest proportion (approximately 45%) of medical expenditures for breast cancer is for continuing care (Brown and Fintor, 1995). Nevertheless, with more than 43,000 female breast cancer deaths per year in the United States, it has been calculated that there are more than 800,000 person-years of life lost each year or 19 person-years lost per death (Brown et al., 1993). The nonmedical, indirect, and psychosocial costs of breast cancer have not been quantified but undoubtedly increase several fold the social and economic costs of this disease.
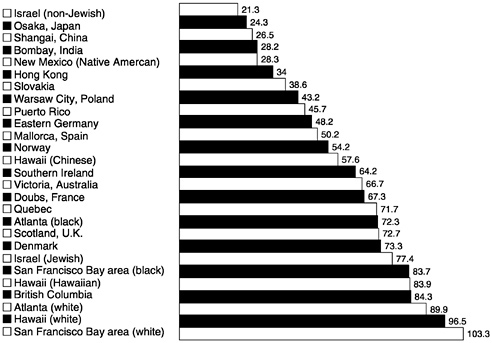
FIGURE 20 Age-adjusted incidence of breast cancer, 1988–1992, per 100,000 population. SOURCE: Adapted from Parkin et al., 1997.
Osteoporosis
Overall
It is estimated that approximately 6 million American men and women have osteoporosis and another 20 million have osteopenia (Looker et al., 1997). Prevalence is dramatically higher in women than in men (see Figure 21). Although peak bone mass is achieved in the second or third decade of life, osteoporosis is rare in individuals less than 50 years of age. In contrast, only 3% of women age 80 or older have normal bone density and 70% have evidence of osteoporosis at one or more skeletal sites (Cooper and Melton, 1996). Thus, osteoporosis can be characterized as a disorder of middle-aged and elderly adults. The greatest public health impact of osteoporosis derives from its accompanying increased risk of fractures. Osteoporotic fractures occur most frequently in the distal forearm, vertebrae, and hip (Cooper and Melton, 1996); indeed, vertebral fractures historically have been considered a defining clinical feature of osteoporosis (Albright et al., 1941). Recent estimates indicate that the age-adjusted incidence of vertebral fracture is more than twice as high as the incidence of hip fracture in women (18 per 1,000 person-years versus 6.2 per 1,000 person-years, respectively) (Melton et al., 1993); both are associated with increased morbidity and mortality in the elderly (Cooper et al. 1993; Melton, 1988).
National data on the epidemiology of osteoporosis and related fractures are somewhat limited, in part, because prior to the advent and widespread use of noninvasive bone densitometry methods such as dual energy x-ray absorptiometry (DEXA), osteoporosis was diagnosed only in the presence of a fracture. However, not all fractures, particularly vertebral fractures, are symptomatic or reach clinical attention. Presently, osteoporosis is defined by the World Health Organization (WHO) as bone mineral density more than 2.5 s.d. (standard deviation) below the young normal mean at one or more skeletal sites (WHO, 1994). Research indicates that a 1 s.d. decrease in femoral bone density is equivalent to a 14-year age increase in risk of hip fracture (Melton et al., 1993). Bone density decreases greatly with age, especially among women, making age one of the strongest risk factors for osteoporosis. However, other factors also influence bone density. For example, among women, bone loss is accelerated after natural or surgical menopause when levels of estrogen drop dramatically.
Other known or suspected risk factors for decreased bone density include tobacco use, physical inactivity, and alcohol abuse (Seeman, 1996; Snow et al., 1996). Each of these is associated with increased risk of fractures. Age-related declines in bone strength also contribute to the increased risk of fractures in elderly populations.
Distribution by Race and Sex
Rates of occurrence of osteoporosis and osteoporotic fractures vary greatly by race and ethnicity, with higher rates consistently observed in whites compared to nonwhites, particularly in North America and northern Europe (Villa and Nelson, 1996). The Third National Health and Nutrition Examination Survey (NHANES III) found a higher prevalence of osteoporosis in whites than blacks or Hispanics for both women and men (Looker et al., 1997). (See Figure 22.) One recent United States study found that age- and sex-adjusted rates of hip fracture for persons over age 50 were nearly three and a half times greater in whites than in blacks (Baron et al., 1994). Hispanics and Asians also have much lower rates of hip fracture than whites (Silverman and Madison, 1988). In addition, the age-related increase in hip fracture is observed in all populations but tends to occur at an earlier age among non-Hispanic whites than Asian, Hispanic, or black populations (Maggi et al., 1991).
Osteoporosis and related fractures occur more frequently in women than in men. NHANES III was the first nationally representative survey to assess bone mineral density using DEXA to determine the prevalence of osteoporosis in the United States adult population (Looker et al., 1995). Femoral bone density was assessed in 14,646 participants age 20 or older (63% of those eligible). Data were age adjusted to the 1980 United States census population, and prevalence of osteoporosis and low bone density or osteopenia (more than 1 but less than 2.5 s.d. below the young normal mean) were determined for women and men age 50 or older (see Figure 21). These data indicate that 15% of American
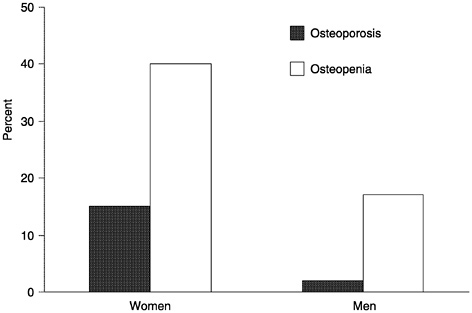
FIGURE 21 Age-adjusted prevalence of osteoporosis and osteopenia of the femur in noninstitutionalized U.S. adults, age 50 and older: NHANES III.
women age 50 or older have osteoporosis and that an additional 40% have osteopenia (Looker et al., 1997). Using the same absolute bone density cutpoint for men as for women (0.56 g/cm2 for femoral neck bone density), it was estimated that 2% of American men age 50 or over have osteoporosis and another 17% have osteopenia (Looker et al., 1997). However, extrapolating the WHO diagnostic criteria, which did not address osteoporosis or low bone density in nonwhite or male populations, so that the referent was mean bone density in non-Hispanic white men ages 20–29, produced higher estimates. With the male referent, estimates are that 4% of men age 50 or older have osteoporosis and another 33% meet criteria for osteopenia. These estimates thus show that the prevalence of osteoporosis is four to seven times greater in women than men (depending on the referent group used). Other research indicates that the estimated lifetime risk of a hip fracture, distal forearm fracture, or vertebral fracture is three times greater for women than men (39.7% for women and 13.1% for men, respectively) age 50 and older (Melton et al., 1992).
Distribution by Socioeconomic Position
Few data are available that examine osteoporosis or fracture incidence by socioeconomic position. Several of the risk factors for fracture (e.g., alcohol abuse, cigarette smoking, physical inactivity) are known to vary by socioeconomic position, with greater prevalence of these behavioral or life-style factors
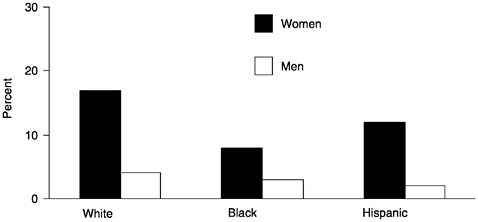
FIGURE 22 Unadjusted prevalence of osteoporosis of femoral bone by race/ethnicity among noninstitutionalized U.S. adults, age 50 years and older: NHANES III.
among poorer persons. One study reported that hip fracture incidence rates in elderly white women in the United States are higher in regions with greater poverty (Jacobsen et al., 1990). In addition, the use of postmenopausal hormone replacement therapy, which protects against bone loss, is more prevalent among socioeconomically advantaged women (Matthews et al., 1996). However, other factors that appear to protect against age-related bone loss, such as obesity, are more prevalent in lower socioeconomic strata (Sobal and Stunkard, 1989). Moreover, blacks and Hispanics, who disproportionately occupy these lower strata (especially in the United States), are known to have greater bone density and lower rates of osteoporosis and osteopenia (Looker et al., 1997). Clearly, the association between osteoporosis and associated fractures and socioeconomic position is complex, and research is needed to determine what the patterns of association are for men and women of different racial/ethnic groups.
Trends
A lack of data prevents us from knowing if there have been marked trends in the prevalence or incidence of osteoporosis in the past. However, there is evidence that the incidence of hip fractures increased fourfold between 1930 and 1980 in white men and even more dramatically in women (Melton et al., 1987), even after taking into consideration the increase in the elderly population. It has been suggested that the increasing prevalence of sedentary life-styles and greater frailty among the elderly may be contributing to this phenomenon (Cooper and Melton, 1996). Future expectations are that the prevalence of osteoporosis and related fractures will increase substantially because these are problems of the elderly. The number of individuals age 65 or older is expected to increase fivefold in the next 50 years (Cooper et al., 1992). Consequently, it is anticipated that the public health
impact of osteoporosis will increase enormously in the coming decades. For example, in 1990, there were more than 1.1 million hip fractures in women and 463,000 hip fractures in men worldwide, and it is predicted that these numbers will increase fourfold by 2050 (Cooper et al., 1992). Interestingly, because of rapidly aging populations, a greater increase in the incidence of hip fractures is expected in Latin American and Asian countries than in North American and European countries in the coming decades, making osteoporosis and related fractures a global public health challenge (Cooper and Melton, 1996).
Geographic Variation
Specific data assessing geographic variations in osteoporosis are sparse. However, there is clear evidence that the incidence of hip fracture varies by geographic region. The highest rates are in Scandinavia, followed by the United States, western Europe, Asia, and Africa (Melton et al., 1987). Rates vary markedly within regions, also. For example, there is a sevenfold difference in incidence of hip fractures within the countries of western Europe (Johnell et al., 1992). A study by Jacobsen and colleagues found interesting regional variations in hip fracture incidence in white women age 65 and older within the United States also (Jacobsen et al., 1990). Data from the Health Care Financing Administration, the Department of Veterans Affairs, the Bureau of the Census, and the Bureau of Health Professions' 1988 Area Resource file were used to examine age-adjusted rates of hip fracture by county for the 48 contiguous states. Figure 23 graphically depicts the findings, which show clear geographic variation, with higher rates in the south. Also, hip fracture incidence rates were positively related to the proportion of elderly below the poverty level and the percentage of farmland in the county, but inversely associated with water hardness and hours of January sunlight. Interestingly, however, regional variations in alcohol consumption, cigarette smoking, obesity, physical activity, or Scandinavian heritage did not account for the observed geographic patterns. The findings suggest that unobserved or unmeasured environmental characteristics and/or individual risk factors are contributing to the geographic variation in hip fracture rates. It is unknown if similar patterns are present for nonwhite populations or men.
Cost
It is difficult to determine the economic costs of osteoporosis, per se. However, the overall cost of fractures is estimated to be $20 billion annually in the United States (Praemer et al., 1992). Recent estimates suggest that hip fractures account for 300,000 hospitalizations annually, with an associated tab of $9 billion in direct medical costs (Bason, 1996). Moreover, it is estimated that hip fractures account for more than 9 years of potential life lost per 1,000 women (Eiskjaer et al., 1992). Because osteoporotic fractures disproportionately affect elderly individuals, the reductions in survival and lost wages associated with
osteoporosis are generally determined to be less than similar figures for other diseases, such as the others reviewed in this chapter. Nevertheless, it is clear that osteoporosis and related fractures are an important and growing public health problem of our aging population that have enormous economic costs in terms of increased morbidity and mortality and lost productivity.
MAKING SENSE OF THE DISTRIBUTION OF DISEASE AND ITS DETERMINANTS
The six problems described above illustrate the tremendous heterogeneity there is in the occurrence of diseases and in important public health problems. This heterogeneity by place, race/ethnic group, gender, socioeconomic position, and time ought to be the starting place for most analyses. The extent of this heterogeneity highlights the implausibility that a single set of explanatory determinants will be found or that a single set of interventions will suffice to reduce the population burden from these problems. Instead, we think the heterogeneity points to the importance of the multilevel approach presented in Figure 5. In what follows, we illustrate such an approach to the public health issues previously described. Because such an approach is in its infancy, for the most part the discussion is a mixture of empirical findings, evidence-based speculation, and arguments based on plausibility. Because it is the major focus of this report, for the most part we highlight the potential importance of domains that range from the behavioral to the social and economic.
Economic and Social Policies
Because of the clear relationships between socioeconomic position and these six problems of public health importance, it is likely that actions that have an impact on the socioeconomic position of individuals, families, and communities can potentially reduce the public health burden associated with these problems. Note that this is true even for breast cancer, for although incidence increases with SEP, mortality decreases with increasing SEP (Eley et al., 1994; American Cancer Society, 1995). At the governmental level, policies related to taxation, cash and noncash transfers, and employment may be some of the most important instruments. For example, the introduction of the earned income tax credit resulted in a reduction in the prevalence of children living in families below the poverty line (Plotnick, 1997), presumably with related health effects, and we are still awaiting the results of recent changes in welfare and entitlement policies on the financial status and health of poor families (Danziger et al., 1999). The changes in economic status of individuals and the communities they live in could conceivably lead to better health among pregnant women and women of childbearing age, thereby leading to a reduced risk of low birthweight. Increased SEP also
allows one to mitigate, or move away from, environmental exposures that might be important in the etiology and progression of childhood asthma, to live in environments with lower levels of stress and violence.
Economic policies that alter workforce participation by women may have an effect on reproductive patterns, thereby altering the risk of breast cancer. The same forces may have an impact for both men and women on levels of job strain, which may alter the risk of developing CVD or its risk factors (Schnall et al., 1994) and triggering acute events (Mittleman and Maclure, 1997). Taxation polices also can have a substantial impact on the development and maintenance of unhealthy behaviors such as smoking (Hu et al., 1995). Taxation policies that reduce funding of education also may influence the availability of physical activity at school through reduction in physical education classes (Luepker, 1999). Zoning policies and the design of living, work, and educational environments can conceivably influence the amount and patterns of leisure time and occupational physical activity.
Through mechanisms that are less well understood (Kaplan et al., 1996; Lynch et al., 2000), economic policies that alter the extent of income and wealth inequality in the population may alter disease risks independent of effects on individual incomes or wealth. In addition to being related to risk of death from all causes, increasing income inequality is associated with increased levels of CVD and other diseases (Kennedy et al., 1996; Kaplan and Lynch, 2000). The extent of variations in income inequality, presumably related to government taxation and transfer policies, on infant mortality was shown by Ross et al. (in press) who compared the association between income inequality and infant mortality in metropolitan areas in the United States and Canada. Metropolitan areas in Canada had much lower levels of income inequality than those in the United States and much less geographic variation in income inequality. This combination of decreased income inequality and restriction in the range of income inequality resulting from Canadian economic policies was associated with considerably lower rates of infant mortality in these analyses.
Social policies also can have a substantial impact. The most obvious relates to access to health insurance and state-of-the-art medical care. To the extent that there is no consensus regarding the need for universal access, then we can expect to see substantial variations by SEP and race/ethnicity in low birthweight and the diagnosis and treatment of asthma, as well as screening, treatment, and outcomes of CVD, breast cancer, and osteoporosis. Social policies regarding regulation of gun ownership, types of weapons allowed, safety devices, enforcement of regulations, and policing may all have an impact on firearm-related deaths (Wintemute, 1999). In general, social policies that have an effect on employment, or lack of it, the nature of work, community neighborhood structures, transportation, housing, schools, medical care, and other social institutions may all have an impact on the distribution of public health problems within and between populations and areas. Social policies and norms related to factors such as tobacco and alcohol use also may have a substantial impact because even changes in average consumption lev-
els may influence both the total burden of disease associated with consumption and the prevalence of heavy smoking and drinking (Rose, 1992).
Institutions
In a sense, institutions cannot be separated from the social, cultural, historical, and economic policies that create and sustain them. However, it is important to see the extent to which institutions, such as those related to the worlds of education, work, medical care, the criminal justice system, and housing, may be important determinants of public health problems and solutions. For example, it has been suggested that school and child care environments may increase the risk of childhood asthma and its complications via exposure to secondhand smoke (Bremberg, 1999) and through a lack of support for behavioral self-management strategies (Clark et al., 1999). Similarly, the school environment via promotion of poor nutritional habits through school lunch programs or on-site fast-food outlets, and reduction of school-based physical activity programs may contribute to increased risk of the development of CVD as well as decreased bone mass. The school environment also can support factors related to increased risk of later development of breast cancer, through both dietary and reproductive risk factors. School-related factors also may contribute to patterns of bullying, gang formation, and violence that may lead to firearm-related injuries.
Workplaces, through both working conditions and the physical environment, zmay increase risk. Stressful working conditions, inflexible working schedules, and afterwork effects of physically and emotionally demanding jobs may all directly contribute to increased risk of CVD (Karasek and Theorell, 1992). Indirectly, they may contribute to patterns of smoking and alcohol use and physical inactivity that increase risks of low-birthweight, breast cancer, CVD, and osteoporosis. Work schedules that make it difficult to utilize preventive or curative services could increase risk of low-birthweight deliveries, CVD, and early detection of breast cancer and osteoporosis.
The physical environment of workplaces and other institutional settings also can increase risk via exposure to tobacco smoke and other toxic substances. In addition, work environments that discourage physical activity in favor of taking elevators or discourage healthy eating via fast-food and vending machine availability also may increase risk of numerous outcomes.
Neighborhoods, Communities, and Living Conditions
A growing literature indicates that characteristics of neighborhoods and communities are associated with variations in health outcomes and individual level risk factors (Macintyre et al., 1993; Kaplan, 1996; Diez-Roux, 1998; Yen and Kaplan 1998, 1999). There are many pathways through which such area differences in health status and risk factors might be generated. Abatement of exposures to lead and other toxins, improvements in ambient air quality, and
reduction of diesel exhaust could have an impact on asthma, low birthweight, and possibly osteoporosis. Environmental restrictions on smoking and the sale and consumption of alcoholic beverages, as well as local advertising in support of smoking and drinking, may influence the rates of all six of the public health problems highlighted in this chapter. Neighborhoods differ in the availability of affordable, nutritious food (Troutt, 1993) and in access to preventive and curative services, possibly having an impact on low birthweight, asthma, cardiovascular disease, breast cancer, and osteoporosis. Lack of access to parks and opportunities for safe recreational areas may influence levels of physical activity.
Social and economic characteristics of communities also may have a great influence on public health (Haan et al., 1987; Macintyre et al., 1993; Sampson et al., 1997; Brooks-Gunn et al., 1997; Wing et al., 1988). The extent to which residents of an area feel interconnected, will help each other, and feel responsible for the “commons” is associated with lower rates of violence, much of which is firearm related (Sampson et al., 1997). Levels of social support can be influenced by neighborhood and housing design and may influence birth outcomes (Nuckolls et al., 1972), cardiovascular disease (Kaplan et al., 1988), treatment of childhood asthma (Smyth et al., 1999), and resolution of violence that can lead to firearm-related deaths.
Living conditions, reflected in the quality of housing and residential environments, may be associated with low birthweight, asthma, cardiovascular disease, and osteoporosis and the risk of hip fracture. For example, levels of allergens and exposure to environmental tobacco smoke may be associated with asthma, and conditions that increase the risk of transmission of various infectious agents may thereby lead to exacerbation of asthma (Clark et al., 1999), increased risk of low birthweight (Romero et al. 1988), and possibly, cardiovascular disease (Patel et al., 1995). Environmental hazards in the home may be associated with increased risk of hip fracture (Rubenstein et al., 1988; Grisso et al., 1996), and environmental barriers outside the home could be associated with reduction in physical activity (Kaplan, 1997).
Social Relationships
The quantity, quality, and scope of social relationships can influence the incidence and progression of a variety of health problems (Cohen and Syme, 1985). Social support and social network participation have been shown to be associated with pregnancy complications (Nuckolls et al., 1972), cardiovascular disease (Kaplan et al., 1988), breast cancer prognosis (Spiegel et al., 1989; Reynolds and Kaplan, 1990; Reynolds et al., 1994; Shrock et al., 1999), recovery from hip fracture (Cummings et al., 1988), asthma symptoms (Clark et al., 1999), and pregnancy complications (Nuckolls et al., 1972). Social groups also may influence, in both a positive and a negative direction, the adoption and maintenance of adverse behavioral risk factors such as smoking and excessive alcohol consumption. Clearly, social processes are involved in the promotion or inhibition of violence and its sequelae such as firearm-related mortality. Strain
associated with problematic relationships, or overload related to multiple social responsibilities, may increase cardiovascular risk and also may make it more difficult to access preventive or curative services.
Individual Risk Factors
There is ample evidence that the behaviors of individuals, such as tobacco and alcohol consumption, physical inactivity, and diet, are critically associated with important public health problems (McGinnis and Foege, 1993). Because this information is well known and readily available it is not reviewed in this paper. Other individual characteristics related to personality, negative affect, coping, and attitudes also are critically important. For example, considerable evidence now underscores the importance of psychological states related to negative affect and hostility in the pathogenesis and triggering of cardiovascular events and the progression of cardiovascular disease (Mittleman and Maclure, 1995; Everson et al., 1996, 1997), and there is some indication that psychological distress may exacerbate asthma symptoms (Smyth et al., 1999). These states can have indirect impacts on low birthweight, breast cancer, cardiovascular disease, and osteoporosis via their influence on access to and use of preventive and curative services, their impact on social relations, and, possibly, through the influence of psychological states on neuroendocrine and immune pathways.
CONCLUSIONS
We have briefly outlined the heterogeneity in prevalence, distribution, and trends for life expectancy and a number of important public health problems. The usual approach is to adopt either a perspective that privileges individual risk factors, which have been termed by some as the “real” causes of disease (McGinnis and Foege, 1993) or a perspective that similarly privileges an increasingly molecular understanding. Either approach, in our opinion, is likely to be extremely limited in understanding variations in disease incidence or prevalence between groups, places, or across time and consequently will generally be unsuccessful in suggesting effective intervention strategies to reduce the population burden from these problems. Instead, we have tried to argue for an integrated approach that views these problems within a multilevel framework and attempts to build bridges between levels rather than attributing primary importance to one level or another. It is likely that some success will come from efforts at specific levels, but our most complete understanding and most successful intervention attempts may very well come from a multilevel focus. In order to make progress, there is a need for considerably more information on determinants of health that lie “upstream” from individual behaviors.
In an influential book on preventive medicine, the late Geoffrey Rose declared, “The primary determinants of disease are mainly economic and social, and therefore its remedies must be economic and social ” (Rose, 1992, p. 129),
and a recent report on the “future of medicine” (Hastings Center Report, 1996) called for an effort on the scope of the Human Genome Project directed at understanding the social determinants of health. As work proceeds at a fast pace on both the behavioral and the molecular bases of disease, we need to proceed apace at accumulating knowledge of the upstream determinants of health that include social relations, neighborhoods and communities, institutions, and social and economic policies. Such an effort bridged with expanding knowledge from more “downstream” pursuits could add to the twenty-first century 's armamentarium for improving the public's health.
REFERENCES
Albright F, Smith PH, Richardson AM. Postmenopausal osteoporosis: Its clinical features. Journal of the American Medical Association 1941; 116:2465–2474.
American Cancer Society. Breast Cancer Facts and Figures, 1996. Atlanta: American Cancer Society, 1995.
American Lung Association. Trends in Asthma Morbidity and Mortality. Washington, DC: Epidemiology and Statistics Unit, 1998.
Arriaga EE. Measuring and explaining the change in life expectancies. Demography 1984;21(1):83–96.
Arriaga EE. Changing trends in mortality decline during the last decades. In: Ruzicka L, Wunsch G, Kane P, eds., Differential Mortality: Methodological Issues and Biosocial Factors. Oxford: Clarendon Press, 1989;105–129.
Baker SP, O'Neill B, Karpf RS. The Injury Fact Book, 2nd ed. New York: Oxford University Press, 1992.
Barnett E, Armstrong DL, Casper ML. Evidence of increasing coronary heart disease mortality among black men of lower social class. Annals of Epidemiology 1999; 464–471.
Baron JA, Barrett J, Malenka D, Fisher E, Kniffm W, Bubolz T, Tosteson T. Racial differences in fracture risk. Epidemiology 1994;5:42–47.
Bason WE. Secular trends in hip fracture occurrence and survival: Age and sex differences. Journal of Aging and Health 1996; 8:538–553.
Bremberg S. Evidence-Based Health Promotion for Children and Adolescents in Stock holm County. Stockholm: Stockholm County Council, 1999.
Brooks-Gunn J, Duncan GJ, Aber JL. Neighborhood Poverty: Context and Consequences for Children, Vols. 1 and 2. New York: Russell Sage, 1997.
Brown ML, Fintor L. The economic burden of cancer. In: Greenwald P, Kramer BS, Weed DL, eds., Cancer Prevention and Control. New York: Marcel Dekker, Inc., 1995; 69–81.
Brown ML, Hodgson TA, Rice DP. Economic impact of cancer in the United States. In: Schottenfeld D, Fraumeni J, eds., Cancer Epidemiology and Prevention, 2nd ed. New York: Oxford University Press, 1993; 255–266.
Annie E.Casey Foundation. Kids Count Data Book. Baltimore: The Annie E.Casey Foundation, 1999.
Centers for Disease Control and Prevention. On-line, http://wonder.cdc.gov/
Centers for Disease Control and Prevention. Vital and Health Statistics. National Hospital Discharge Survey: Annual Summary, 1993. DHHS Publication No. PHS 95–1782, 1995.
Clark NM, Brown RW, Parker E, et al. Childhood asthma. Environmental Health Perspectives 1999; (suppl 3): 421–429.
Cohen S, Syme SL, eds., Social Support and Health. Orlando, FL: Academic Press, Inc., 1985.
Collins JG. Prevalence of selected chronic conditions: United States 1990–1992. National Center for Health Statistics. Vital Health Statistics 1997; 10:194.
Cook PJ, Lawrence BA, Ludwig J, Miller TR. The medical costs of gunshot injuries in the United States. Journal of the American Medical Association 1999; 282(5):447–454.
Cookson JB. Prevalence rates of asthma in developing countries and their comparison with those in Europe and North America. Chest 1987; 91(Suppl. 6):97S–103S.
Cooper C, Atkinson EJ, Jacobsen SJ, O'Fallon WM, Melton LJ III. Population-based study of survival after osteoporotic fractures. American Journal of Epidemiology 1993; 137:1001–1005.
Cooper C, Campion G, Melton LJ III. Hip fractures in the elderly: A worldwide projection. Osteoporosis International. 1992; 2:285–289.
Cooper C, Melton LJ III. Magnitude and impact of osteoporosis and fractures. In: Marcus R, Feldman D, Kelsey J, eds., Osteoporosis. San Diego: Academic Press, 1996; 419–434.
Crain EF, Weiss KB, Bijur PE, Hersh M, Westbrook L, Stein RE. An estimate of the prevalence of asthma and wheezing among inner-city children. Pediatrics 1994; 94:356–362.
Cummings SR, Phillips SL, Wheat ME, Black D, Goosby E, Wlodarczyk D, Trafton P, Jergesen H, Winograd CH, Hulley SB. Recovery of function after hip fracture. The role of social supports . Journal of the American Geriatrics Society 1988; 36(9): 801–806.
Danziger S, Corcoran M, Danziger S, Heflin CM. Work, income and material hardship after welfare reform. Joint Center for Poverty Research Working Paper 114.0, 199–08–01, October 1999. On-line. http://www.jcpr.org/wp/Wpprofile.cfm?ID=114.0.
David RJ, Collins JW. Differing birth weight among infants of U.S.-born blacks, African-born blacks and U.S.-born whites. New England Journal of Medicine 1997; 337: 1209–1214.
Diez-Roux AV. Bringing context back into epidemiology: Variables and fallacies in multilevel analysis. American Journal of Public Health 1998; 88(2): 216–222.
Eiskjaer S, Østgård SE, Jakobsen BW, Jensen J, Lucht U. Years of potential life lost after hip fracture among postmenopausal women. Acta Orthopaedica Scandinavica. 1992; 63:293–296.
Eley JW, Hill HA, Chen VW, Austin DF, Wesley MN, Muss HB, Greenberg RS, Coates RJ, Correa P, Redmond CK, Hunter CP, Herman AA, Kurman R, Blacklow R, Shapiro Sam, and Edwards BK. Racial differences in survival from breast cancer. Results of the National Cancer Institute Black/White Cancer Survival Study. Journal of the American Medical Association 1994; 272:947–954.
Evans R. Asthma among minority children: A growing problem. Chest 1992; 101:368S– 371S.
Everson SA, Goldberg DE, Kaplan GA, Cohen RD, Pukkala E, Tuomilehto J, Salonen JT. Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosomatic Medicine 1996; 5:113–21.
Everson SA, Kaplan GA, Goldberg DE, Salonen R, Salonen JT. Hopelessness and 4-year progression of carotid atherosclerosis: The Kuopio Ishemic Heart Disease Risk Factor Study. Arteriosclerosis, Thrombosis, and Vascular Biology 1997; 17:1490–1495.
Fang J, Madhavan S, Alderman MH. Low birth weight: Race and maternal nativity—Impact of community income. Pediatrics 1999; 103(1):E5.
Feuer EJ, Wun LM, Boring CC, Flander WD, Timmel MJ, long T. The lifetime risk of developing breast cancer. Journal of the National Cancer Institute 1993; 85:892–897.
Fingerhut LA, Ingram DD, Feldman JJ. Homicide rates among U.S. teenagers and young adults: Differences by mechanism, level of urbanization, race, and sex, 1987 through 1995. Journal of the American Medical Association 1998; 280(5):423–427.
Forbes JF. The incidence of breast cancer: The global burden, public health considerations. Seminars in Oncology 1997; 24(1 Suppl 1):S1–20–S1–35.
Goff DC, Nichaman MZ, Chan W, Ramsey DJ, Labarthe DR, Ortiz C. Greater incidence of hospitalized myocardial infarction among Mexican Americans than non-Hispanic whites. The Corpus Christi Heart Project, 1988–1992. Circulation 1997; 95(6):1433–1440.
Gordon NH. Association of education and income with estrogen receptor status in primary breast cancer. American Journal of Epidemiology 1995; 142:796–803.
Grant EN, Wagner R, Weiss KB. Observations on emerging patterns of asthma in our society. Journal of Allergy and Clinical Immunology 1999; 104(2, Part 2):S1–9.
Grisso JA, Capezuti E, and Schwartz A. Falls as risk factors for fractures. In: Marcus R, Feldman D, Kelsey J, eds., Osteoporosis. San Diego: Academic Press, 1996, 599–611.
Haan M, Kaplan GA, Camacho T. Poverty and health: Prospective evidence from the Alameda County Study. American Journal of Epidemiology 1987; 125(6):989–98.
Haan MN, Kaplan GA, Syme SL. Socioeconomic status and health: Old observations and new thoughts . In: Bunker JP, Gomby DS, Kehrer BH, eds., Pathways to Health: The Role of Social Factors, Menlo Park, CA: Henry J.Kaiser Family Foundation, 1985; 76–135.
Hastings Center Report. The goals of medicine: Setting new priorities. An International Project of the Hastings Center. Hastings Center Report November-December 1996; Special Supplement: S-19.
Henderson CI. Breast cancer. In: Murphy GP, Lawrence WL, Lenhard R, eds., Clinical Oncology. Atlanta: American Cancer Society; 1995; 198–219.
Hoyert, DL, Kochanek, KD, Murphy, SL. 1999. Deaths: Final data for 1997. National Vital Statistics Reports 47:19 (http://www.cdc.gov/nchs/data/nvs47_19.pdf).
Hu TW, Sung HY, Keeler TE. Reducing cigarette consumption in California: Tobacco taxes vs an anti-smoking media campaign. American Journal of Public Health 1995; 85(9):1218–1222.
Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Regional variation in the incidence of hip fracture. Journal of the American Medical Association 1990; 264:500–502.
Johnell O, Gullberg B, Allander E, Kanis JA. MEDOS Study Group. The apparent incidence of hip fracture in Europe: A study of national register sources. Osteoporosis International 1992; 2:298–302.
Kaplan GA. People and places: Contrasting perspectives on the association between social class and health. International Journal of Health Services 1996; 26:507–519.
Kaplan GA. Behavioral, social, and socioenvironmental factors adding years to life and life to years. In: Hickey T, Speers MA, Prohaska TR, eds., Public Health and Aging. Baltimore, Johns Hopkins University Press, 1997; 37–52.
Kaplan, GA, Haan MN, Syme SL, Minkler M, Winkleby M. Socioeconomic status and health. In: Amler RW, Dull HB, eds. Closing the Gap: The Burden of Unnecessary Illness. New York: Oxford University Press, 1987; 125–129.
Kaplan GA, Salonen JT, Cohen RD, Brand RJ, Syme SL, Puska P. Social connections and mortality from all causes and from cardiovascular disease: Prospective evidence from eastern Finland. American Journal of Epidemiology 1988; 128(2):370–380.
Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation 1993; 88(4):1973–1978.
Kaplan, GA, Pamuk, E, Lynch, JW, Cohen, RD, Balfour, J. Inequality in income and mortality in the United States: Analysis of mortality and potential pathways. BMJ 1996; 312:999–1003.
Kaplan GA, Lynch JW. Socioeconomic considerations in the primordial prevention of cardiovascular disease. Preventive Medicine in press.
Karasek RA, Theorell T (contributor). Work: Stress, Productivity, and the Reconstruction of Working Life. Basic Books: New York 1992.
Kaufman, JS, Cooper, RS, McGee, DL. Socioeconomic status and health in blacks and whites: The problem of residual confounding and the resiliency of race. Epidemiology 1997; 8:621–628.
Kelsey JL, Horn-Ross PL. Breast cancer: Magnitude of the problem and descriptive epidemiology . Epidemiologic Reviews 1993; 15:7–16.
Kelsey JL, Bernstein L. Epidemiology and prevention of breast cancer. Annual Review of Public Health 1996; 17:47–67.
Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: Cross-sectional ecological study of the Robin Hood index in the United States. British Medical Journal 1996; 312(7037):100–1007.
Kosary CL, Ries LAG, Miller BA, Hankey BF, Harras A, Edwards BK. SEER Cancer Statistics Review, 1973–1992: Tables and Graphs. National Cancer Institute. NIH Publication No. 95–2789. Bethesda, MD: 1995.
Krieger N, Rowley D, Hermann AA, Avery B, Phillips MT. Racism, sexism, and social class: Implications for studies of health, disease, and well-being. American Journal of Preventive Medicine 1993; 9(Suppl 6):82–122.
Krieger N, Williams DR, Moss N. Measuring social class in U.S. public health research: Concepts, methodologies, and guidelines. Annual Review of Public Health 1997; 13:341–378.
Lantz PM, Booth KM. The social construction of the breast cancer epidemic. Social Science and Medicine. 1998;46:907–918.
Lewitt EM, Schuurman Baker L, Corman H, Shiono PH. The direct cost of low birth weight. In: The Future of Children, Vol. 5. Palo Alto, CA: The David and Lucille Packard Foundation, 1995, 35–56.
Looker AC, Johnston CC, Jr, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, and Lindsay RL. Prevalence of low femoral bone density in older U.S. women from NHANES III. Journal of Bone and Mineral Research 1995; 10:796–802.
Looker AC, Orwoll ES, Johnston CC, Jr., Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, and Heyse SP. Prevalence of low femoral bone density in older U.S. adults from NHANES III. Journal of Bone and Mineral Research 1997; 12:1761–1771.
Luepker RV. How physically active are American children and what can we do about it? International Journal of Obesity and Related Metabolic Disorders 1999; 23(Suppl 2):S12–17.
Lynch JW. Socioeconomic factors in the behavioral and psychosocial epidemiology of cardiovascular disease. In: Schneiderman N, Gentry J, da Silva JM, Speers M, Tomes H., eds., Integrating Behavioral and Social Sciences with Public Health. Washington, DC.: APA Press, (in press).
Lynch JW, Davey Smith G, Kaplan GA, House JS. Income inequality and health: A neomaterial interpretation. British Medical Journal, in press.
Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviors and psycho-social characteristics by stages of the socioeconomic lifecourse. Social Science and Medicine 1997; 44:809–819.
MacIntyre S, Maciver S, Sooman A. Area, class, and health: Should we be studying people or places? Journal of Social Policy 1993; 22:213–234.
Maggi S, Kelsey JL, Litvak J, Heyse SP. Incidence of hip fracture in the elderly: A cross-national analysis . Osteoporosis International 1991; 1:232–241.
Malveaux FJ, Fletcher-Vincent SA. Environmental risk factors of childhood asthma in urban centers. Environmental Health Perspectives 1995:103 (Suppl. 6):59–62.
Mannino DM, Homa DM, Pertowski CA et al. Surveillance for asthma—United States, 1960–1995.Atlants Centers for Disease Control and Prevention 1998; 47:S-1.
Massey D, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press, 1993.
Matthews KA, Kuller LH, Wing RR, Meilahn EN, Plantinga P. Prior to use of estrogen replacement therapy, are users healthier than nonusers? American Journal of Epidemiology 1996; 143:971–978.
Max W, Rice DP. Shooting in the dark: Estimating the cost of firearm injuries. Health Affairs 1993; 12(4):171–185.
McGinnis, JM, Foege WH. Actual causes of death in the United States. Journal of the American Medical Association 1993; 270(18):2207–2212.
Melton LJ III. Epidemiology of fractures. In: Riggs BL, Melton LJ III, eds., Osteoporosis: Etiology, Diagnosis, and Management. New York: Raven Press, 1988:133–154.
Melton LJ III, Chrischilles EA, Cooper C, Lane AW, Riggs BL. How many women have osteoporosis? Journal of Bone and Mineral Research 1992; 7:1005–1010.
Melton LJ III, Lane AW, Cooper C, Eastell R, O'Fallon WM, Riggs BL. Prevalence and incidence of vertebral deformities. Osteoporosis International 1993; 3:113–119.
Melton LJ III, O'Fallon WM, Riggs BL. Secular trends in the incidence of hip fractures. Calcified Tissue International 1987; 41:57–64.
Mittleman MA, Maclure M. Mental stress during daily life triggers myocardial ischemia (editorial; comment). Journal of the American Medical Association 1997; 277(19): 1558–1559.
Murray, CJL, Michaud, CM, McKenna, MT, Marks, JS. U.S. Patterns of Mortality by County and Race: 1965–1994, U.S. Burden of Disease and Injury Monograph Series. Cambridge, MA: Harvard Center for Population and Development Studies, 1998.
National Cancer Institute. NCI reports improvements in breast cancer death rate, 1996. On-line, http://cis.nci.nih.gov/fact/625.html.
National Center for Health Statistics. Health, United States, 1996–1997 Injury Chartbook. Hyattsville, MD: NCHS, 1997.
National Center for Health Statistics. Health, United States, 1998 with Socioeconomic Status and Health Chartbook. Hyattsville, MD: NCHS, 1998.
National Center for Health Statistics. Health, United States, 1999 with Socioeconomic Status and Health Chartbook. Hyattsville, MD: NCHS, 1999.
National Heart, Lung, and Blood Institute. Chartbook of U.S. National Data on Socioeconomic Status and Cardiovascular Health and Disease. Washington, DC: NIH, June 1995.
National Heart, Lung, and Blood Institute. Morbidity and Mortality: 1998 Chartbook on Cardiovascular, Lung, and Blood Diseases. NIH: October 1998. On-line, http://www.nhlbi.nih.gov/resources/docs/cht-book.htm
National Heart, Lung, and Blood Institute. Asthma Statistics, Data Fact Sheet. Washington, DC: NIH, 1999.
Nuckolls KB, Cassel J, Kaplan BH. Psychosocial assets, life crisis and the prognosis of pregnancy. American Journal of Epidemiology 1972; 5:431–441.
Paneth N. The problem of low birth weight, Vol. 5. In: The Future of Children. Palo Alto, CA: The David and Lucille Packard Foundation, 1995, 19–34.
Parkin DM, Whelan SL, Ferlay J, Raymond L, Young J, eds., Cancer Incidence in Five Continents, Vol. VII. Lyon, France: International Agency for Research on Cancer; IARC Scientific Publications No. 143; 1997.
Patel P, Mendall MA, Carrington D, et al. Association of Helicobacter pylori and Chlamydia pneumoniae infections with coronary heart disease and cardiovascular risk factors . British Medical Journal 1995; 311:711–714.
Perkins CL, Morris CR, Wright WE, Young JL. Cancer Incidence and Mortality in California by Detailed Race or Ethnicity, 1988–1992. Sacramento, CA: California Department of Health Services, Cancer Surveillance Section , 1995.
Plotnick RD. Child poverty can be reduced. Future of Children 1997; 7(2):72–87.
Praemer A, Furner S, and Rice DP. Musculoskeletal Conditions in the United States. ParkRidge, IL: American Academy of Orthopaedic Surgeons, 1992.
Reynolds P, Kaplan GA. Social connections and risk for cancer: Prospective evidence from the Alameda County Study. Behavioral Medicine 1990; 16:101–110.
Reynolds P, Boyd PT, Blacklow RS, Jackson JS, Greenberg RS, Austin DF, Chen VW, and Edwards BK. The relationship between social ties and survival among black and white breast cancer patients. National Cancer Institute Black/White Cancer Survival Study Group . Cancer Epidemiology, Biomarkers and Prevention 1994; 3:253–259.
Robbins AS, Brescianini S, Kelsey JL. Regional differences in known risk factors and the higher incidence of breast cancer in San Francisco. Journal of the National Cancer Institute 1997; 89:960–965.
Romero R, Mazor M, Wu YK, et al. Infection in the pathogenesis of preterm labor. Seminars in Perinatology 1988; 12:262–279.
Rose, G. The Strategy of Preventive Medicine. Oxford, UK: Oxford University Press, 1992.
Ross NA, Wolfson MC, Dunn JR, Berthelot J-M, Kaplan GA, Lynch JW. Income inequality and mortality in Canada and the United States: A cross-sectional assessment using census data and vital statistics , British Medical Journal 2000; 320:898–902.
Rubenstein LZ, Robbins AS, Schulman BL, Rosado J, Osterweil D, and Josephson KR. Falls and instability in the elderly. Journal of the American Geriatric Society 1988; 36:266–278.
Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science 1997; 277(5328):918–924.
Schnall PL, Landsbergis PA, Baker D. Job strain and cardiovascular disease (review). Annual Review of Public Health 1994; 15:381–411.
Schoendorf KC, Hogue CJ, Kleinman JC, Rowley D. Mortality among infants of black as compared to white college educated parents. New England Journal of Medicine 1992; 326:1522–1526.
Seeman E. The effects of tobacco and alcohol use on bone. In: Marcus R, Feldman D, Kelsey J, eds., Osteoporosis. San Diego: Academic Press, 1996, 577–597.
Sempos C, Cooper R, Kovar MG, McMillen M. Divergence of the recent trends in coronary mortality for the four major race-sex groups in the United States. American Journal of Public Health 1988; 78:1422–1427.
Shrock D, Palmer RF, Taylor B. Effects of a psychosocial intervention on survival among patients with stage I breast and prosta te cancer: A matched case-control study. Alternative Therapies in Health and Medicine 1999; 5:49–55.
Silverman SL, Madison RE. Decreased incidence of hip fracture in Hispanics, Asians, and blacks: California hospital discharge data. American Journal of Public Health 1988; 78:1482–1483.
Smyth JM, Soefer MH, Hurewitz A, Kliment A, Stone AA. Daily psychosocial factors predict levels and diurnal cycles of asthma symptomatology and peak flow. Journal of Behavioral Medicine 1999; 22(2):179–193.
Snow CM, Shaw JM, Matkin CC. Physical activity and risk for osteoporosis. In: Marcus R, Feldman D, Kelsey J, eds., Osteoporosis. San Diego: Academic Press, 1996; 511–528.
Sobal J, Stunkard AJ. Socioeconomic status and obesity: A review of the literature. Psychological Bulletin 1989; 105:260–275.
Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet 1989; 2:888–891.
Stanford JL, Herrinton LJ, Schwartz SM, Weiss NS. Breast cancer incidence in Asian migrants to the United States and their descendants. Epidemiology 1995; 6:181–183.
Trock BJ. Breast cancer in African American women: Epidemiology and tumor biology . Breast Cancer Research and Treatment 1996; 40:11–24.
Troutt, DD. The Thin Red Line: How the Poor Still Pay More. San Francisco: West Coast Regional Office, Consumers Union of the United States, 1993.
UNICEF. The State of the World's Children 1998. Oxford: Oxford University Press, 1998.
Villa ML, Nelson L.Race, ethnicity, and osteoporosis. In: Marcus R, Feldman D, Kelsey J, eds., Osteoporosis. San Diego, CA: Academic Press, 1996; 435–447.
Vital Statistics of the United States. Annual publications from the National Center for Health Statistics (and forerunner organization names) for data years 1900 to 1967.
Weiss KB, Sullivan SD. Socio-economic burden of asthma, allergy and other atopic illnesses . Pediatric Allergy and Immunology 1994; 5(6 suppl):7–12.
Wing S, Casper M, Riggan W, Hayes C, Tyroler HA. Socioenvironmental characteristics associated with the onset of decline of ischemic heart disease mortality in the United States. American Journal of Public Health 1988; (8):923–926.
Wintemute GJ. The future of firearm violence prevention: Building on success. Journal of the American Medical Association 1999; 282(5):475–478.
World Health Organization. Assessment of Fracture Risk and Its Application to Screening for Postmenopausal Osteoporosis. WHO Technical Report Series. Geneva: WHO, 1994.
Wun LM, Feuer EJ, Miller BA. Are increases in mammographic screening still a valid explanation for trends in breast cancer incidence in the United States? Cancer Causes and Control 1995; 6:135–144.
Yen IH, Kaplan GA. Poverty area residence and changes in physical activity level: Evidence from the Alameda County Study. American Journal of Public Health 1998; 88:1709–1712.
Yen IH, Kaplan GA. Poverty area residence and changes in depression and perceived health status: Evidence from the Alameda County Study. International Journal of Epidemiology 1999; 28:90–94.