PAPER CONTRIBUTION B
Understanding and Reducing Socioeconomic and Racial/Ethnic Disparities in Health
James S.House and David R.Williams
The initial paper by Kaplan and colleagues and the burgeoning literatures on socioeconomic and racial/ethnic disparities in health establish that such disparities are large, persistent, and even increasing in the United States and other developed countries, most notably the United Kingdom (Marmot et al., 1987; Preston and Haines, 1991; Adler et al., 1993; Pappas et al., 1993; Evans et al., 1994; Williams and Collins, 1995). Differences across socioeconomic and racial/ethnic groups or combinations thereof range up to 10 or more years in life expectancy and 20 or more years in the age at which significant limitations in functional health are first experienced (see Table 1; House et al., 1990, 1994). Both within and across countries, individuals with the most advantaged socioeconomic and racial/ethnic status are experiencing levels of health and longevity
|
Dr. House is director of the Survey Research Center in the Institute for Social Research and professor of sociology, University of Michigan, and Dr. Williams is professor of sociology and reserach scientist at the Institute for Social Research, University of Michigan. This paper was prepared for the symposium “Capitalizing on Social Science and Behavioral Research to Improve the Public's Health ,” the Institute of Medicine and the Commission on Behavioral and Social Sciences and Education of the National Research Council, Atlanta, Georgia, Februray 2–3, 2000. This work has been supported by a Robert Wood Johnson Foundation Investigation in Health Policy Research Award (Dr. House) and by grant MH-57425 from the National Institute of Mental Research and the John D. and Catherine T.MacArthur Foundation Research Network on Socioeconomic Status and Health (Dr. Williams). We are indebted to Debbie Fitch for her work in preparing the manuscript, references, figures, and table. |
TABLE 1. United States Life Expectancy, at Age 45 by Family Income (1980 dollars)a
|
Females |
Males |
|||||
|
Family Income |
White |
Black |
Diff. |
White |
Black |
Diff. |
|
Allb |
36.3 |
32.6 |
3.7 |
31.1 |
26.2 |
4.9 |
|
<$ 10,000 |
35.8 |
32.7 |
3.1 |
27.3 |
25.2 |
2.1 |
|
$10,000–$14,999 |
37.4 |
33.5 |
3.9 |
30.3 |
28.1 |
2.2 |
|
$15,000–$24,999 |
37.8 |
36.3 |
1.5 |
32.4 |
31.3 |
1.1 |
|
≥$25,000 |
38.5 |
36.5 |
2.0 |
33.9 |
32.6 |
1.3 |
|
NOTE: Diff. = difference. a1979–1989; Taken from the National Center for Health Statistics. b1989–1991; Taken from the National Center for Health Statistics. |
||||||
that increasingly approach the current biologically attainable maxima. Thus, the major opportunity for improving the health of human populations in the United States and most other societies lies in improving the longevity and health of those of below-average socioeconomic or racial/ethnic status.
Accordingly, the reduction of socioeconomic and racial/ethnic disparities in health has been identified by the U.S. Public Health Service and the National Institutes of Health as a major priority for public health practice and research in the first decade of the twenty-first century (USDHHS, 1999; Varmus, 1999). This will involve some combination of either reducing the degree to which disparities in socioeconomic and racial/ethnic status are converted into health disparities or reducing the extent of socioeconomic or racial/ethnic disparities themselves. This will further entail understanding both (1) the psychosocial and biomedical pathways that translate socioeconomic and racial/ethnic disparities into disparities in health, and (2) the broader social, cultural economic, and political processes that determine the nature and extent of socioeconomic and racial/ethnic disparities in our society, and the ways in which individuals become distributed across socioeconomic levels and defined into racial/ethnic groups.
This paper seeks to elucidate what we already know and need yet to learn about reducing socioeconomic and racial/ethnic disparities in health. We first provide a brief overview of the nature of both socioeconomic and racial/ethnic disparities in health and how they are related to each other. Second, we assess current understanding of the pathways or mechanisms by which the socioeconomic or racial/ethnic status of individuals affects their health and the implications of this understanding for reducing socioeconomic and racial/ethnic disparities in health. Third, we explore what is known about how and why communities and societies come to be stratified both socioeconomically and in terms of race/ethnicity, and how these communal and societal patterns of socioeconomic and racial/ethnic stratification affect the socioeconomic and racial/ethnic status of individuals and their health. Finally, we conclude with an assessment of what we
know and need to know about how to reduce socioeconomic and racial/ethnic disparities in health and, hence, to improve population health.
Several themes pervade our discussion. First, there are multiple indicators of socioeconomic position and hence multiple indices of socioeconomic disparities in health, and these are best comprehended in a multivariate, causal, and life course framework. Second, socioeconomic and racial/ethnic disparities in health, and the reasons for and means of reducing them, are inextricably related but also distinctive. This also can best be comprehended in a multivariate causal framework. Third, it is important to understand the pathways or mechanisms linking socioeconomic and racial/ethnic status to health. What is most striking and important here is to recognize that socioeconomic and racial/ethnic status shape and operate through a very broad range of pathways or mechanisms, including almost all known major psychosocial and behavioral risk factors for health. Thus, socioeconomic and racial/ethnic status are in the terms of Link and Phelan (1995) the “fundamental causes ” of corresponding socioeconomic and racial/ethnic disparities in risk factors and hence health and, consequently, also the fundamental levers for reducing these health disparities. Finally, existing evidence strongly suggests that the nature of the socioeconomic and racial/ethnic stratification of individuals can be changed in ways beneficial to health and, coincidentally, to a broad range of other indicators of individual and societal well-being.
THE NATURE OF SOCIOECONOMIC AND RACIAL/ETHNIC DISPARITIES AND THEIR RELATION TO HEALTH
We take the size, persistence, and even increase of socioeconomic and racial/ethnic disparities as given in Paper Contribution A. Here we seek to clarify the nature of socioeconomic and racial/ethnic status and their relations to each other and to health.
A Multivariate, Causal, and Life Course Framework
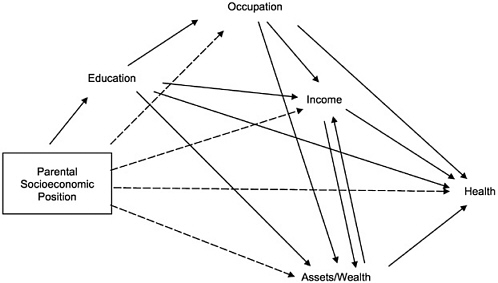
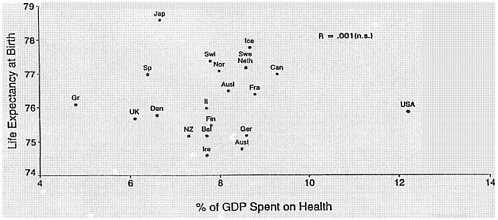
Socioeconomic status (SES) refers to individuals' position in a system of social stratification that differentially allocates the major resources enabling people to achieve health or other desired goals. These resources centrally include education, occupation, income, and assets or wealth, which are related to each other and to health in a causal framework first elucidated by Blau and Duncan (1967) and shown in its simplest form in Figure 1A. This model suggests that over the life course, individuals first acquire varying levels and types of education, which in turn help them to enter various types of occupations, which then yield income, which finally enables them to accumulate assets or wealth. Each subsequent variable in this causal chain is generally most affected by the immediately prior variable, with potential residual effects of earlier variables. This model is simple because it omits potential feedback loops other than from assets or wealth to income (e.g., a person's occupation may facilitate further educational attainment) and fails
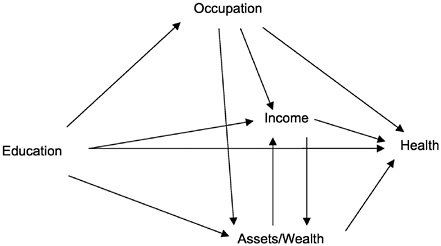
FIGURE 1A. Simple intragenerational causal model relating major indicators of socioeconomic position to each other and to health.
to incorporate variations in each of these indicators that will occur over the life course (e.g., progressions or regressions in terms of occupation or income).
Although this causal framework has been used routinely in the study of socioeconomic attainment, it has seldom been explicitly applied to the study of socioeconomic disparities. It is important, however, that it be utilized more explicitly in future research on the relation of socioeconomic status to health, and especially in thinking about how socioeconomic disparities in health have been or could be reduced. The framework helps, for example, to understand why income is perhaps the strongest and most robust predictor of health (McDonough et al., 1997; Lantz et al., 1998), because to some degree the impacts of all other variables are mediated through it. Also, some health outcomes are more strongly affected by certain socioeconomic indicators than others (education, for example, more strongly affects health behaviors, patterns of which form early in life, and the diseases or health indicators affected most by them). Overall, in the United States, education and income have proved most predictive of health, with occupation often adding little additional explanatory power and assets or wealth somewhat more. More research is needed, however, to estimate explicitly the relative effects on health of these different indicators of socioeconomic position, and how much the total effect of any given variable is spuriously produced by temporally antecedent confounding variables, mediated via temporally subsequent intervening variables, or acts more directly on health (see Sorlie et al., 1995; Lantz et al., 1998 and in press; and Robert and House, 2000 a,b).
From the point of view of reducing health disparities, we need to have such an analysis of the variance in health explained by different socioeconomic factors in order to understand or predict the health effects of planned or unplanned change in each indicator. Further, by adding other variables to Figure 1A,
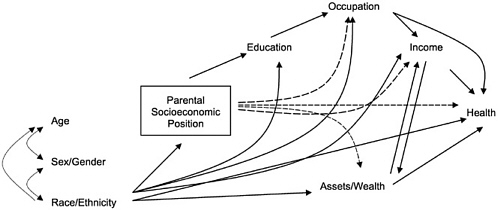
FIGURE 1C Extension of model in Figure 1B incorporating race/ethnicity, sex/gender, and age. NOTE: for clarity of presentation, no arrows are drawn from age and sex/gender to subsequent variables, but these would and should be exactly parallel to those for race/ethnicity.
we can extend our understanding of how disparities in health across these indicators of socioeconomic position may be generated by antecedent factors or mediated via subsequent factors. Several such elaborations are important in thinking about reducing other socioeconomic and racial disparities in health.
First, socioeconomic position (SEP) has to be thought of as an intergenerational as well as intragenerational phenomenon. Thus, parental socioeconomic position may importantly shape childhood well-being and hence educational and later adult socioeconomic attainment and health, as shown in Figure 1B. The work of Barker (e.g., Barker and Osmond, 1986) and others (Kaplan and Salonen, 1990; Elo and Preston, 1992; Blane et al., 1996; Kuh and Ben-Shlomo, 1997) has indicated that childhood socioeconomic position and experiences can have long-term effects on adult health (see also Paper Contribution C). This is sometimes interpreted to mean that childhood socioeconomic position is a more important determinant of health than adult socioeconomic position. However, Figure 1B suggests that most such effects are likely to be channeled through and reinforced by later socioeconomic attainment, and the unique impact of childhood SEP or its sequelae must be evaluated net of later socioeconomic or other experiences. When this is done, the unique effects of childhood SEP on adult health are often found to be small or even nonexistent relative to the effects of later adult socioeconomic attainment and experiences (e.g., Lynch et al., 1994). *Thus, although the impact of socioeconomic position on childhood health and well-being is a very important problem in its own right, it cannot and should not be viewed as a major explanation of adult socioeconomic or racial/ethnic disparities in health or hence as the major, preferred, or necessary route for reducing such adult disparities.
However, Figure 1B is also highly simplified, neglecting the changing socioeconomic position of the families of many children. Thus, the socioeconomic position of a child often changes from preschool to elementary school to secondary school and onward through adulthood. Socioeconomic advantage and disadvantage may be viewed as ebbing and flowing or cascading over a person's life course. Although recent socioeconomic position is usually the best predictor of future outcomes, sustained socioeconomic deprivation over time is likely to be even more damaging (Wolfson et al., 1993, Lynch et al., 1997), and uncertainty or variability in socioeconomic position may be deleterious even to those of generally solid middle- or higher-level SEP (McDonough et al., 1997). Thus, knowledge of the full life course of socioeconomic position is ideally desirable for understanding socioeconomic disparities in health and a target for efforts to alleviate such disparities.
Finally, Figures 1A and 1B must be further elaborated, as in Figure 1C, to take account of the impact of more ascribed and relatively fixed social
|
*Link and Phelan (in progress) have similarly showed that although cognitive ability contributes to socioeconomic attainment, its effects on health are mediated entirely through such attainments, and it in no way can explain away or make spurious the considerable impact of adult SEP on health. |
statuses—most notably for our purposes, race/ethnicity, but also age and gender. Figure 1C reveals two simple but very important truths about racial/ethnic disparities in health. First, racial/ethnic status is a major determinant of every indicator of socioeconomic position, even net of all prior variables in the model. For example, not only are African Americans disadvantaged in terms of level of education, but even given the same education, they are disadvantaged occupationally and in terms of income, and still disadvantaged in income even within the same educational and occupational levels (Featherman and Hauser, 1978). Most egregiously, their assets/wealth lag far behind other Americans of equivalent income, occupation, and education (Oliver and Shapiro, 1995; Conley, 1999). Not surprisingly, then, a great deal of racial/ethnic disparity in health is explainable in terms of the socioeconomic disadvantages associated with membership in the most historically disadvantaged racial/ethnic groups (Williams and Collins, 1995).
However, the second important truth of Figure 1C is that race/ethnicity has effects on health that are independent of socioeconomic differences between racial/ethnic groups (Williams and Collins, 1995; Williams et al., 1997). For example, African Americans generally exhibit poorer health outcomes even when compared to whites with statistically equivalent levels of socioeconomic position (see below and Table 1). Thus, race carries its own burdens for health beyond those associated with socioeconomic disadvantage. We can properly estimate and understand how race/ethnicity and socioeconomic position combine to affect health only within a multivariate framework such as Figure 1C. Further, such a framework can also reveal that race/ethnicity sometimes has salutary effects on health that may compensate in part for the deleterious effects of socioeconomic disadvantages. For example, African Americans exhibit better levels of mental health, and Latinos better levels of infant and child health, than would be expected based on their socioeconomic position. The next major section of this paper focuses on elucidating the pathways or mechanisms through which both socioeconomic position and race/ethnicity affect health, for better as well as for worse.
Due to constraints of space and desire for clarity, Figure 1C fails to represent other important issues for understanding and reducing socioeconomic disparities in health. First is the issue of reciprocal or reverse causality, especially between socioeconomic position and health. Ours and others' discussions of reducing socioeconomic and racial/ethnic disparities in health are predicated on the assumption that, by far, the predominant causal flow is from socioeconomic position and race/ethnicity to health rather than vice versa. This assumption is self-evident for a fixed attribute such as race/ethnicity and is generally borne out in empirical research on socioeconomic position, for example, by introducing baseline controls on health into the framework of Figure 1 (see House and Roberts, 2000:116–117), though clearly health events or shocks can and do affect subsequent labor force participation and income (often more in the short term than in the long term). Second, time and space prevent us from fully and systematically attending to variations by age, sex, race/ethnicity, and other factors
in the presence of size of the causal paths/effects in Figure 1, though we will on occasion note such variations (see Robert and House, 2000b:118–120 for more discussion of such issues).
Shape of the Relationship Between SES and Health
Before turning more explicitly to how we may explain and reduce socioeconomic and racial/ethnic disparities in health, it is important to clarify our understanding of the shape of the relationship between socioeconomic position and health. An intriguing finding of some research on socioeconomic inequalities in health is that it is not simply that those who are in the lowest socioeconomic groups have worse health than those in higher socioeconomic groups. Rather, a relationship between socioeconomic position and health has been observed across the socioeconomic hierarchy, with even those in relatively high-socioeconomic groups having better health than those just below them in the socioeconomic hierarchy (Adler et al., 1994; Marmot et al., 1991). Perhaps the most important implication of this finding is that it is not just the material, psychological, and social conditions associated with severe deprivation or poverty (such as lack of access to safe housing, healthy food, and adequate medical care) that explain socioeconomic inequalities in health among those already at relatively high levels of socioeconomic position.
Despite some evidence for gradient effects of socioeconomic position on health, it is also important to note the many studies indicating that the relationship of socioeconomic position, especially as indexed by income, to health is monotonic, but not a linear gradient. Although increasingly higher levels of socioeconomic position may be associated with increasingly better levels of health, there are also substantially diminishing returns of higher socioeconomic position to health. For example, studies have found diminishing and even nonexistent relationships between income and mortality (Wolfson et al., 1993; Backlund et al., 1996; Chapman and Hariharan, 1996; McDonough et al., 1997;) or morbidity (House et al., 1990, 1994; Mirowsky and Hu, 1996) at higher levels of income (e.g., above the median). This trend partially reflects a health “ceiling effect” caused by the fact that people in the upper socioeconomic strata maintain overall good health until quite late in life, leaving little opportunity for improvement in health among these groups throughout much of adulthood (House et al., 1994). Thus, it is most important to understand what accounts for socioeconomic inequalities in health across the broad lower range (e.g., lower 40–60%) of socioeconomic position, rather than focusing mainly or only on factors that might explain this relationship across the gradient or at higher levels.
PATHWAYS LINKING INDIVIDUAL SOCIOECONOMIC AND RACIAL/ETHNIC STATUS TO HEALTH
Pathways from SES to Health
We have increased understanding of how and why socioeconomic status has such strong pervasive and even increasing impacts on health. Several aspects of this deserve emphasis. First, access to and utilization of medical care play only a limited role in explaining the impact of socioeconomic factors on health, although research is needed to reassess the size of the role played by medical care. Second, there is no single or small set of factors, psychosocial or physiological, that provides the pathways linking socioeconomic position to health. Rather, what makes socioeconomic position such a powerful determinant of health is that it shapes people's experience of, and exposure to, virtually all psychosocial and environmental risk factors for health—past, present, and future—and these in turn operate through a very broad range of physiological mechanisms to influence the incidence and course of virtually all major causes of disease and health. Thus, in the end, socioeconomic position itself is a fundamental cause (Link and Phelan, 1995) of levels of individual and population health and a fundamental lever for improving health in American society.
The Limited but Insufficiently Understood Role of Medical Care
Several types of evidence point to the limited role of medical care in understanding how and why socioeconomic position affects health. First, there is evidence that modern preventive and therapeutic medical care can account for only a minor fraction of the dramatic improvements in individual and population health over the last 250 years (McKeown, 1976, 1979, 1988; McKinlay and McKinlay, 1977). Even analysts admiring of the impact of medical science on health, for example, estimate that only about 5 years of the 30-year increase in life expectancy in the United States in the twentieth century has been due to preventive or therapeutic medical care (Bunker et al., 1994). The remainder is attributable primarily to increasing socioeconomic development and associated gains in nutrition, public health and sanitation, and living conditions. Second, improvements in access to medical care occasioned by the introduction of national health insurance or service plans have, quite unexpectedly, done little or nothing to reduce socioeconomic differences in health. The rediscovery of the importance of socioeconomic disparities in health as a major public health problem was probably stimulated most by the publication in England in 1980 of the Report of the Working Group on Inequalities in Health, better known as the Black Report after the chair of the working group, Sir Douglas Black, then chief scientist of the U.K. Department of Health and subsequently president of the Royal College of Physicians. The report showed that occupational class differences in health were greater than differences by gender, race, or regional background and, most distressingly, had actually increased between 1949–1953 and
1970–1972 over the first quarter-century of existence of the British National Health Service. Nor did things improve between the early 1970s and 1980s (Marmot et al., 1987). During the 1980s and early 1990s, the British experience was replicated in other developed countries including Canada, where the introduction of national health insurance in the early 1970s had little effect on socioeconomic differences in health (Wilkins et al., 1989). Finally, adjustments for gross access to and utilization of medical care have contributed little or nothing to explaining socioeconomic and racial/ethnic differences in health in our and other data.
However, we believe that the role of medical care in socioeconomic and racial/ethnic health differences deserves renewed examination and research. First, compared to whites, racial/ethnic minorities have lower levels of access to medical care in the United States (Blendon et al. 1989; Trevino et al. 1991). Second, higher incidence rates for racial/ethnic minorities do not fully account for the higher death rates (Schwartz et al. 1990). Later initial diagnosis of disease, comorbidity, delays in medical treatment, and disparities in the quality of care also play a role. There is growing evidence of large racial/ethnic differences in the quality of medical care. Many studies have found racial/ethnic differences in the receipt of therapeutic procedures for a broad range of conditions even after adjustment for insurance status and severity of disease (e.g., Wenneker and Epstein, 1989; Harris et al. 1997). These disparities exist even in contexts where differences in economic status and insurance coverage are minimized, for example, the Veterans Administration Health System (e.g., Whittle et al., 1993) and the Medicare program (e.g., McBean and Gornick, 1994). Recent studies document that these differences in medical treatment adversely affect the health of minority group members (Peterson et al., 1997; Hannan et al., 1999). Moreover, medical care appears to play a modest role in accounting for racial differences in mortality (Woolhandler et al., 1985; Schwartz et al., 1990), and other evidence suggests that medical care has a greater impact on the health status of vulnerable racial and low-SES groups than on their more advantaged counterparts (Williams, 1990). More generally, behind declining socioeconomic and racial/ethnic disparities in gross levels of access to and utilization of medical care may lie in persisting differences in access to more continuous care from a concerned and responsive provider, associated differences in access to and utilization of important standards of preventive care (e.g., blood pressure, prostate and colorectal screening, Pap smears, mammograms, and professional advice on health behaviors), and differences in the timeliness and appropriateness of access to state-of-the-art standards of therapeutic care. Thus, socioeconomic and racial/ethnic disparities in standards and appropriateness of medical care merit increased attention in research and policy.
Psychosocial and Environmental Risk Factors
As evidence grew of the more limited impact of medical care in explaining socioeconomic and racial/ethnic disparities in health, research increasingly established a growing and even predominant role of behavioral and psychosocial risk factors in the etiology and course of human health and disease. First, and still most compelling, was the evidence of the adverse effects of cigarette smoking on mortality and morbidity, especially adult lung cancer and heart disease (e.g., USPHS, 1964). This was followed by increasing evidence of the health risks of other behaviors, including immoderate levels of eating (and hence weight) and of alcohol consumption, lack of exercise, and dietary composition, e.g., fat and fiber (Lalonde, 1975; Berkman and Breslow, 1983, USDHHS, 1990). Evidence has also accumulated on the deleterious health effects of chronic and acute stress in work and life (Theorell, 1982), hostility and depression (Scheier and Bridges, 1995), lack of social relationships and supports (House et al., 1988), and lack of control, efficacy, or mastery (Rodin, 1986), with the impact of lack of social relationships, for example, on all-cause mortality being not incomparable to that of cigarette smoking (House et al., 1988). Notably, these psychosocial factors all tend to affect a broad range of health outcomes, rather than being focused on a single outcome.
Socioeconomic Status and Psychosocial and Environmental Risk Factors
One factor (e.g., smoking) or a small set of factors (e.g., health behaviors) is sometimes seen as crucial in explaining and alleviating problems of premature morbidity and mortality more generally (e.g., USDHHS, 1990; McGinnis and Forge, 1993) and socioeconomic and racial/ethnic disparities in health in particular (Mechanic, 1989; Satel, 1996). However, increasing evidence suggests that there are few or no analogues in our current problems of public health to the necessary and sufficient microbial causes of many infectious diseases, nor are there any comparable “magic bullets” for treating, preventing, or eradicating them. Rather, the current causes of morbidity and mortality, especially from major chronic diseases, are broadly multifactorial, with no one or few decisive, but the accumulation of many being as debilitating or deadly as a virulent infectious agent (Kunitz, 1987). For example, all major health behaviors combined (i.e., cigarette smoking, immoderate weight and drinking, and lack of physical activity) appear able to explain only 10–20%, at most, of socioeconomic differences in mortality (Lantz et al., 1998). Rather, what is most striking and important about socioeconomic (and, to a lesser degree, racial/ethnic) status is the degree to which it shapes exposure to, and perhaps also the impact of, a wide range of psychosocial and environmental risk factors for health. Our data (House et al., 1992, 1994) and those of others (e.g., Marmot et al., 1991; Lynch et al., 1996) show that lower-SES individuals have a higher prevalence of almost all major psychosocial risk factors for health. That is, they manifest higher levels of
risky health behaviors such as smoking, lack of exercise, immoderate eating and drinking, and high-fat-low-fiber diets. They also experience more chronic and acute stress due to, for example, their more vulnerable economic status and the higher rates of ill health and death among friends and relatives. They generally report lower levels of social relationships and supports and of personal efficacy or control, along with higher levels of hostility and depression.
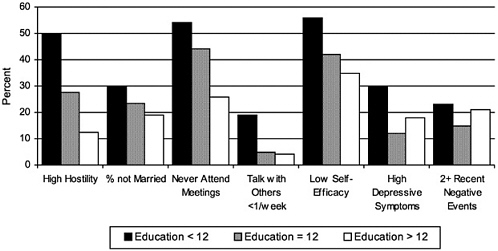
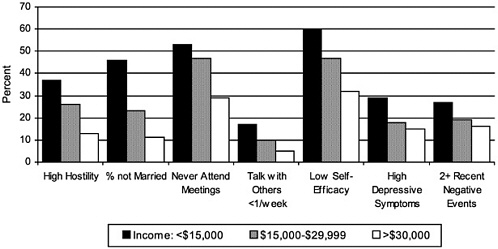
Figures 2A and 2B show, for national samples of the U.S. population, the distribution and range of these psychosocial risk factors by education and income. The prevalence of each psychosocial risk factor is always highest among those with the lowest level of education and income, with rate ratios (of the lowest- to the highest-SES groups) ranging from 1.1 to 3.8 and averaging 2.0 (see Lantz et al., 1998, for parallel data on health behaviors).
Persons of lower socioeconomic status in adulthood are also more likely to live and work in physical-chemical-biological environments that are hazardous to health. Further, they are more likely to have grown up in lower-socioeconomic environments, which may have residual adverse effects on health in adulthood that research is just beginning to examine (e.g., Power et al., 1990).
At this point we are only beginning to explore the causal pathways and complexities that link socioeconomic position to exposure to behavioral, psychosocial, and environmental risk factors and, in turn, link these risk factors to health outcomes. Our own analyses and those of others find that although any single behavioral, psychosocial, or environmental risk factor, or small set thereof, can account for only a small fraction of the association between SES and health, a set of 10–20 such risk factors can account for 50–100% of the association between a given SES indicator and health outcome. Marmot et al. (1991) and Lynch et al. (1996) have reported that adjusting for 10–20 such risk factors reduces the predictive association of SES with mortality by 50–100%. We get similar results for the cross-sectional relationship between education or income and functional status (House et al., 1994).
Potentials and Limits of Understanding and Intervening in Pathways
Better understanding of the pathways and mechanisms linking socioeconomic and racial/ethnic status to health is often and appropriately seen as crucial to reducing socioeconomic and racial/ethnic disparities in health. Once an intervening variable or mechanism is understood, efforts can be made to reduce this variable or mechanism or to weaken its impact on health, hence reducing the socioeconomic or racial/ethnic disparities in health. To the extent that we are able to decrease smoking and improve other health behaviors, lessen stress, enhance social relationships and supports, modify risky psychological dispositions or reduce exposure to environmental exposures, especially in disadvantaged socioeconomic or racial/ethnic groups, or to moderate their effects on health (e.g., develop a safe cigarette or nicotine delivery system, see Paper Contribution K), we should consequently reduce socioeconomic and racial/ethnic disparities in health. Such intervention strategies have had some beneficial effects in these regards.
However, we wish to call attention to the often insufficiently recognized limitations of such an approach and to highlight the potential, and indeed necessity, of another and complementary approach. The potential of the pathways strategy is limited in two crucial ways. First, modifying any psychosocial risk factor is a difficult process, and the impact of modifying one or a single risk factor is necessarily limited for the reasons discussed above. Second, where we have had substantial success in reducing a behavioral or psychosocial risk factor (e.g., smoking), this success is often greatest among the more advantaged due to the persistence or even accentuation (e.g., targeting of disadvantaged groups for cigarette advertising) of the causal forces giving rise to the risk factor in less advantaged groups. Thus, as overall levels of smoking have decreased in the United States, socioeconomic differences in smoking have increased (see Paper Contribution K). Finally, it is important to recognize that the mechanisms that currently link socioeconomic status to health are not the same ones that did so in the past or will in the future. Prior socioeconomic differences undoubtedly had more to do with differences in exposure to infectious agents and access to medical care than is currently the case. Indeed, many of the currently most important diseases and risk factors—such as coronary heart disease and its risk factors of smoking, lack of exercise, and high-fat diet—were at one time more characteristic of upper socioeconomic strata, but have become more incident and prevalent in lower socioeconomic strata as these diseases and risk factors have become more deleterious to health. A similar trend has characterized AIDS, which emerged first as a disease among higher socioeconomic strata but has rapidly become more prevalent in disadvantaged socioeconomic and racial/ethnic groups. Thus, whatever the major diseases (or risk factors for them) are in future years, they too are likely to be importantly determined by socioeconomic status (Link and Phelan, 1995).
In sum, as Link and Phelan (1995) have cogently argued, we need to think increasingly of disparities in socioeconomic position as the “fundamental cause” of socioeconomic disparities in health. Hence, ameliorating these socioeconomic disparities themselves may be the best strategy for reducing disparities in health. A parallel, but not identical, argument can be made regarding racial/ethnic disparities, to which we now turn, before returning to evidence that socioeconomic improvement and policy are a major form of health improvement and policy in our and other societies, arguably the most important and essential one for reducing socioeconomic disparities in health.
Understanding Racial/Ethnic Differences in Health
Race/Ethnicity and Health
National mortality data reveal that African Americans (or blacks) have an overall death rate that is more than 1.5 times higher than that of whites (NCHS, 1998). The magnitude of the racial difference in death rates varies by the specific cause of death, but a pattern of elevated death rates for blacks compared to
whites exists for almost all the leading causes of death in the United States. In contrast, all other racial/ethnic groups have an overall death rate that is lower than that of whites. However, there is considerable variability for subgroups of these populations and for specific health conditions. All nonblack minorities have considerably lower rates than whites for the two leading causes of death (heart disease and cancer) but higher rates for some conditions. Hispanics have higher mortality rates than non-Hispanic whites for tuberculosis, septicemia, HIV/AIDS, chronic liver disease and cirrhosis, diabetes, and homicide (Sorlie et al., 1993; Vega and Amaro, 1994). Subgroups of the Asian and Pacific Islander population also have elevated mortality rates for some health conditions (Lin-Fu, 1993). For example, the Native Hawaiian population has the highest death rate due to heart disease of any racial group in the United States (Chen, 1993). Similarly, American Indians who receive care from the Indian Health Service (60% of that population) have age-adjusted mortality rates higher than the national average for tuberculosis, alcoholism, diabetes, accidents, homicides, suicides, and pneumonia and influenza (NCHS, 1993).
What Is Race?
Early studies of racial variations in health viewed race as primarily reflecting biological homogeneity and racial differences in health as largely genetically determined. This view predated modern scientific theories of genetics and carefully executed genetic studies. In contrast, scientific evidence suggests that our current racial categories are more alike than different in terms of biological characteristics and genetics (Lewontin, 1972; Gould, 1977; Latter, 1980). All human beings are identical for about 75% of known genetic factors, with about 95% of human genetic variation existing within racial groups (Lewontin, 1982). Thus, there is more genetic variation within races than between them, and racial categories do not capture biological distinctiveness. Race is thus more of a social than a biological category, and racial classification schemes have been influenced by larger social and political considerations (Cooper and David, 1986; Williams, in press).
Race and SES
Although not useful as biological markers, current racial/ethnic categories capture an important part of the inequality and injustice in American society (See and Wilson, 1988). There are important power and status differences between groups. For example, in 1995 the poverty rate for Asians was almost twice that of whites, while the rate for blacks and Hispanics was more than three times that of non-Hispanic whites (NCHS, 1998). Data on poverty tell only a part of the story of economic vulnerability. In addition to persons who actually fall below the government's poverty threshold, a large number of persons are only slightly above this level. Many of these persons are at a high risk of be-
coming poor. The combination of the poor and near-poor (annual income above the poverty threshold but less than twice the poverty level) categories reveals that one in every three persons in the United States falls into this economically vulnerable category—26% of whites, 33% of Asians, 54% of blacks, and 62% of Hispanics (NCHS, 1998). Although there is a strong relationship between race and SES, they are not equivalent. For example, the rate of poverty is three times higher for blacks than for whites, but two-thirds of blacks are not poor, and two-thirds of all poor Americans are white.
Race, SES, and Health
Research reveals that SES differences between races account for much of the racial differences in health. Adjusting racial (black-white) disparities in health for SES sometimes eliminates, but always substantially reduces, these differences (Krieger et al., 1993; Williams and Collins, 1995; Lillie-Blanton et al., 1996). However, race often has an effect on health independent of SES: within levels of SES, blacks still have worse health status than whites.
Table 1 illustrates these issues with life expectancy data. At age 45, white males have a life expectancy that is almost 5 years more than black males (NCHS, 1990). Similarly, the life expectancy at age 45 for white females is 3.7 years longer than that of similarly aged black women. However, there is considerable socioeconomic variation in life expectancy within both racial groups (NCHS, 1998). When we consider the distribution of life expectancy by race and income, two important trends emerge. First, for both racial groups, income is strongly linked to health status. Consistently, persons of lower levels of income report lower life expectancy than their more economically favored peers. Black men in the highest-income group live 7.4 years longer than those in the lowest-income group. The comparable numbers for whites was 6.6 years. Thus, the SES difference within each racial group is larger than the racial difference across groups. A similar pattern is evident for women, although the SES differences are smaller. At age 45, black women in the highest-income group have a life expectancy that is 3.8 years longer than those in the lowest-income group. Among whites, the SES difference is 2.7 years. Moreover, for men and women of both racial groups, increasing levels of income are associated with longer life expectancy. The power of SES in shaping racial differences in health is clearly evident by comparing the highest-SES blacks with the lowest-SES whites, especially among males. High-income black males have a life expectancy that is 5.3 years longer than low-income white males. Thus, the disproportionate concentration of African Americans at lower SES levels is a major factor behind the overall racial differences in health.
The second pattern that clearly emerges in these data is that race is more than socioeconomic status. Consistently, there is an independent effect of race even when SES is controlled. At every level of income, for both men and women, African Americans have lower levels of life expectancy than whites. In these data, the differences are greater at the two lower levels of income than at
the two higher-economic- status categories. However, for some indicators of health status such as infant mortality, the racial gap becomes larger as SES increases (NCHS, 1998).
Role of Racism or Discrimination
The construct of racism can structure and inform our understanding of racial inequalities in health (Cooper et al., 1981; Krieger et al., 1993; Hummer, 1996; LaVeist, 1996; Williams, 1997; in press). The term racism refers to an ideology of inferiority that is used to justify the differential treatment of members of racial outgroups by both individuals and societal institutions, usually accompanied by negative attitudes and beliefs toward these groups. Racism has been a central organizing principle within American society and has played a key role in shaping major social institutions and policies (Omi and Winant, 1986; Quadagno, 1994). Historically, ideologies about racial groups were translated into policies and societal arrangements that have limited the opportunities and social mobility of stigmatized groups. The strong association between race/ethnicity and SES in the United States reflects the successful implementation of social policies that were designed to limit societal resources and rewards to socially marginalized groups.
There have been important positive changes in the racial attitudes of whites toward blacks in recent decades and broad current support for the principle of equality in most societal institutions (Schuman et al., 1997). At the same time, there is considerably less support for policies that would actually implement equal access to education, housing, jobs, and so forth (Schuman et al., 1997). Moreover, national data on stereotypes reveal that whites view blacks, Hispanics, and Asians more negatively than themselves, with blacks viewed more negatively than all other groups and Hispanics twice as negatively as Asians (Davis and Smith, 1990). Such a high level of acceptance of negative stereotypes of minority groups is an ominous harbinger of widespread societal discrimination. Psychological research indicates that the endorsement of negative racial stereotypes leads to discrimination against minority groups (Devine, 1995; Hilton and von Hippel, 1996). Moreover, well-learned stereotypes are resistant to disconfirmation (Stangnor and McMillan, 1992), and their activation is an automatic process, with individuals spontaneously becoming aware of relevant stereotypes after encountering someone to whom the stereotypes are applicable (Devine, 1989; Hilton and von Hippel, 1996).
Research reveals that considerable racial/ethnic discrimination persists in the United States in domains that affect socieconomic mobility, such as housing and employment (Kirschenman and Neckerman, 1991; Neckerman and Kirschenman, 1991; Fix and Struyk, 1993). Thus, the advent of civil rights legislation and changes in the racial attitudes of whites have not been sufficient to eradicate discrimination, and there has been remarkable stability over time on multiple dimensions of racial inequality (Economic Report of the President,
1998). For example, the median income of African Americans was 59 cents for every dollar earned by whites in 1996—identical to what it was in 1978.
Racism affects disparities in health in multiple ways. First, racism restricts and truncates socioeconomic attainment. The consequent racial differences in SES and poorer health reflect, in part, the impact of economic discrimination produced by large-scale societal structures. Residential segregation has been a primary mechanism by which racial inequality has been created and reinforced. Racial segregation has determined access to educational and employment opportunities that has importantly led to truncated socioeconomic mobility for blacks and American Indians (Jaynes and Williams, 1987; Massey and Denton, 1993). Residence in segregated neighborhoods can lead to exposure to environmental toxins, poor-quality housing, and other pathogenic living conditions, including inadequate access to a broad range of services provided by municipal authorities (Collins and Williams, 1999). These conditions importantly account for the large racial difference in homicide. The combination of concentrated poverty, male joblessness, and residential instability leads to high rates of single-parent households, and these factors together account for variation in the levels of violent crime (Sampson and Wilson, 1995). Importantly, the association between these factors and violent crime for whites was virtually identical in magnitude with the association for African Americans. Several studies have found a positive association between both adult and infant mortality and residence in segregated areas. One recent study has documented elevated mortality rates for both blacks and whites in cities high on two indices of segregation compared to cities with lower levels of segregation (Collins and Williams, 1999). This pattern suggests that beyond some threshold of segregation, the adverse conditions linked to highly segregated cities may negatively affect the health of all persons who reside there.
Moreover, because of racism, SES indicators are not commensurate across racial groups, which makes it difficult to truly adjust racial differences in health for SES (Kaufman et al., 1997). There are racial differences in the quality of education, income returns for a given level of education or occupational status, wealth or assets associated with a given level of income, the purchasing power of income, the stability of employment, and the health risks associated with occupational status (Williams and Collins, 1995; Kaufman et al., 1997).
Racial differences are especially marked for wealth. Eller (1994) shows that while white households have a median net worth of $44,408, the median net worth is $4,604 for black households and $5,345 for Hispanic ones. Moreover, racial/ethnic differences in wealth are evident at all levels of income and are greatest at the lowest income level. For persons in the lowest quintile of income in the United States, the net worth of whites is 10,000 times higher than that of blacks ($10,257 versus $1).
As noted earlier, systematic discrimination can also affect the quantity and quality of services received, including medical care. Recent research has focused on the potential health consequences of subjective experiences of discrimination. Racism in the larger society can also lead to systematic differences in exposure to
personal experiences of discrimination. These experiences of discrimination may be an important part of subjectively experienced stress that can adversely affect health. A growing body of evidence indicates that self-reported measures of discrimination are adversely related to physical and mental health in a broad range of racial/ethnic minority populations (Amaro et al., 1987; Salgado de Snyder, 1987; Krieger, 1990; Dion et al., 1992; Jackson et al., 1996; Krieger and Sidney, 1996; Kessler, et al., 1999; Noh et al., 1999). Two recent studies suggest that exposure to discrimination plays a role in explaining observed racial differences in self-reported measures of health (Williams et al., 1997; Ren, et al., 1999).
A small body of research suggests that the prevalence of negative stereotypes and cultural images of stigmatized groups can adversely affect health status. First, the widespread societal stigma of inferiority can create specific anxieties, expectations, and reactions that can affect health indirectly by having an adverse impact on socioeconomic performance and mobility (Fischer et al., 1996; Steele, 1997). There may also be more direct health effects. Researchers have long identified that one response of minority populations would be to accept the dominant society's ideology of their inferiority as accurate. A few studies have operationalized the extent to which African Americans internalize or endorse these negative cultural images. These studies have found that internalized racism is positively related to psychological distress, depressive symptoms, substance use, and chronic physical health problems (Taylor and Jackson, 1990; Taylor et al., 1991; Williams and Chung, in press).
SOCIOECONOMIC AND RACIAL/ETHNIC CHARACTERISTICS OF SOCIAL SYSTEMS AS DETERMINANTS OF INDIVIDUAL AND POPULATION HEALTH
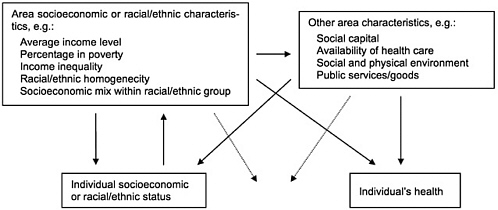
Individuals occupy particular socioeconomic positions and racial/ethnic status within broader systems of socioeconomic and racial/ethnic stratification at the level of communities, metropolitan areas, regions, nations, and even the world. Research and theory increasingly suggest the importance in at least two ways of these broader stratification systems for individual and population health. First, the nature of socioeconomic and racial/ethnic stratification at these more macrosocial levels is a major determinant of the nature and meaning of the socioeconomic and racial/ethnic status occupied by individuals. For example, the level of economic growth and development in communities, metropolitan areas, regions, nations, and the world and the relative equality or inequality in the distribution of the fruits of economic growth and development shape the absolute and relative levels of income of individuals. In particular, living in an area with lower levels of average income or higher levels of income inequality will increase the likelihood of individuals having low income levels. Similarly, as discussed in the preceding section, higher levels of racial/ethnic segregation are likely to adversely affect the socioeconomic position and other life chances of
members of disadvantaged racial/ethnic groups. Second, the socioeconomic and racial/ethnic composition of areas may have effects on individual health that are not mediated through individual socioeconomic and racial/ethnic status. Such effects may be additive or interactive, as shown in Figure 3. The socioeconomic and racial/ethnic characteristics of areas may affect individuals' (and hence population) health independently of individuals' personal socioeconomic and racial/ethnic characteristics, presumably by shaping the nature of the social and physical environment in the area in terms of variables specified in Figure 3 or other unspecified features of the environment that can affect individual health. The area-level socioeconomic, racial/ethnic, and environmental characteristics may also interact with and potentiate or buffer the impact of individual socioeconomic and racial/ethnic status on health. For example, living in a poor area may increase the impact of individual income on health because personal resources become even more consequential in the relative absence of benign environmental influences, and, conversely, living in a better-off area may soften the impact of personal economic deprivation.
Contextual Effects: Real but Limited
Effects of area characteristics on individuals are usually referred to as context effects (e.g., Hauser, 1970, 1974). Evidence of aggregate or ecological correlation between the socioeconomic and racial/ethnic characteristics of areas and the population health parameters of the areas (e.g., mortality rates) are suggestive of context effects, but do not demonstrate them because they fail to control for the characteristics of individuals, which, as shown in Figure 3, may either select people into areas or be shaped by the characteristics of the area. A small number of studies exist that test the effects of area socioeconomic and racial/ethnic characteristics net of individual-level characteristics. As in other areas of research (e.g., Jencks and Mayer, 1990), the general finding is that there are significant effects of context, but that a far greater portion of the variance in individual health outcomes is explained by the socioeconomic and racial/ethnic characteristics of individuals (see Robert, 1999 and Robert and House, 2000a, for reviews of the socioeconomic literature, and Collins and Williams, 1999, for a review of the racial/ethnic literature). However, because social contexts also exert effects on individual characteristics, they remain a potential target for interventions to preomote health.
In recent years, a particular socioeconomic characteristic of areas, income inequality, has received a great deal of attention. Interest in this topic derives from the observation at the population level (as well as at the individual level, e.g., Sorlie et al., 1995) that the relation of income to health is curvilinear, reflecting a pattern of diminishing returns, as shown in Figure 4. Across nations (and within nations over time), growth in average income per capita has had a very powerful effect on population health, presumably reflecting the associated growth both in individual incomes and in public and private social infrastruc-
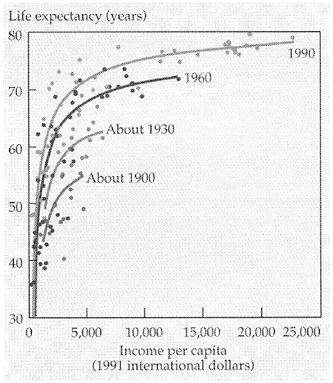
FIGURE 4 Life expectancy and income per capita for selected countries and periods. SOURCE: The World Bank, World Development Report, 1993. Reprinted in Wilkinson, 1996:34.
tures productive of health. However, at higher levels of per capita income (e.g., about $5,000 per person, 1991 international dollars), the relationship becomes much weaker. Across countries at this level, however, a number of analyses have found much stronger correlations between income inequality and health (Rodgers, 1979; Wilkinson, 1992, 1996; van Doorslaer et al., 1997). Wilkinson and others have argued that these data, and similar data comparing areas within developed countries (e.g., Ben-Shlomo et al., 1996; Kaplan et al., 1996; Kennedy et al., 1996; Kawachi et al., 1997), reflect strong effects of income inequality per se, operating through variables such as social capital, cohesion, and trust in the population. A large body of conceptual and empirical analyses suggests, on the contrary, that income inequality has its effects primarily via the underlying high level of individuals with relatively low income that necessarily characterizes areas with more unequal incomes, at least given the average levels of income in these populations (Gravelle, 1998; Deaton, 1999; Mellor and Milyo, 1999). Some evidence exists in methodologically sound studies for contextual effects of income inequality, but these are equally or more plausibly interpretable as reflecting a lower investment in public goods, especially for the
disadvantaged, in areas or political units characterized by greater income inequality (Robert and House, 2000a; Lynch et al., 2000). Again, these data still suggest that interventions that affect income inequality (or correlates of it) can be a potential means of improving individual or population health, if only or mainly by improving the incomes of more disadvantaged individuals.
In sum, the socioeconomic and, especially, racial/ethnic (due to the powerful deleterious effects of segregation on African Americans discussed at the end of the previous section) characteristics of areas are important components of understanding socioeconomic and racial/ethnic disparities. Hence, they must also be important in policies aimed at alleviating such disparities.
IMPROVING POPULATION HEALTH AND REDUCING SOCIOECONOMIC AND RACIAL/ETHNIC DISPARITIES THROUGH PLANNED SOCIAL POLICY AND UNPLANNED SOCIAL CHANGE
What has been said thus far provides powerful evidence of how social and behavioral science knowledge can contribute to societal and governmental objectives of improving population health and reducing socioeconomic and racial-ethnic disparities in health. It is these socioeconomic and racial/ethnic disparities in health that we believe largely explain why the United States has levels of population health significantly below those of peer nations such as Canada, Japan, or Sweden, and no better than those of many less developed countries (see Figure 5), despite national expenditures on health care and health research that far exceed those of any other nation. Indeed, disadvantaged portions of the U.S. population have levels of health no better than those of some of the least developed nations in the world (McCord and Freeman, 1990).
The main message we want to deliver is that socioeconomic policy and practice and racial/ethnic policy and practice are the most significant levers for reducing socioeconomic and racial/ethnic disparities and hence improving overall population health in our society, more important even than health care policy.
Interventions in Pathways or Mechanisms: Promise and Problems
One of the major reasons for understanding the pathways or mechanisms linking a health outcome to its more distal causes such as socioeconomic and racial/ethnic status is the promise that we may be able to intervene in the pathways or mechanisms, even if we cannot alter the more distal causes, and thus eliminate or mitigate the deleterious effects of the distal cause. Preventive and therapeutic pharmacological interventions via “magic bullets” epitomize this strategy for preventing disease and promoting health. Even if we cannot eradicate the bacteria, viruses, or toxins that cause infectious diseases, we can reduce or eliminate their deleterious effects via vaccination or prophylaxis. Even where
we may only partially understand, much less be able to intervene in, the ultimate causes of disease, as in hypertension, we can mitigate or eliminate its deleterious effects by acting on better-understood intervening mechanisms.
This paradigm of disease prevention and health promotion has great appeal, based on the dramatic instances of its success just alluded to. However, it remains generally more effective and efficient to approach disease promotion from a broader population or public health standpoint where feasible. This has been and may continue to be particularly true for socioeconomic and racial/ethnic disparities in health, for reasons discussed earlier. Returning to the case of cigarette smoking discussed more fully in Paper Contribution K, efforts to understand or intervene in the physiological pathway through which it operates have not yet been successful, and extensive efforts at behavioral and pharmacological interventions to stop smoking behavior at the level of individuals have been only modestly successful. Nevertheless, in the United States at least, we have made major progress in reducing levels of cigarette consumption, due in large part to broader population-wide interventions via pricing, labeling, regulation of pro-and anti-smoking advertising, and increasingly severe restrictions on where and when persons may smoke, all contributing to an increasingly strong set of social norms against smoking. Further, and paradoxically, the success of efforts to reduce smoking may have contributed, as noted above, to the perplexing pattern from which we began—overall improvements in population health but widening socioeconomic and racial/ethnic disparities in health. This is because persons of higher socioeconomic position, especially education, have been much more likely to stop or not start smoking, thus creating a growing inverse association between socioeconomic position and smoking (Moore et al., 1996).
We believe that efforts to intervene on many other psychosocial pathways linking socioeconomic and racial/ethnic status to health are likely to confront similar problems and potentially exacerbate rather than alleviate socioeconomic and racial/ethnic differences in health, unless they very carefully take account of the ways in which these pathways and mechanisms may operate differentially across socioeconomic or racial/ethnic groups. This would be true for plausibly promising interventions such as modifying other health behaviors (eating, drinking, exercise); stress management and reduction; enhancing social relationships and supports, and social capital; or modifying psychological dispositions such as anger or hostility and control or efficacy. This is primarily because such interventions generally presume that the intervening risk factor can be modified largely by individual choice and effort and hence do not alter the strong forces in our systems of socioeconomic and racial/ethnic stratification that produce differences in the first place. These forces include (1) differential access or exposure to opportunities for desirable health behaviors (e.g., areas populated by disadvantaged socioeconomic and racial/ethnic minorities tend to be long on convenience and liquor stores selling cigarettes and junk food and short on supermarkets or groceries selling fresh fruits and vegetables or on safe and supportive venues and facilities for physical activity); (2) the increased risks in disadvantaged socioeconomic groups and areas of stressful events at work or home
or of disruptions of social relationships, networks, and support by illness and death; (3) greater exposure to experiences generative of discrimination, hostility, or inefficacy; and (4) heightened exposure to social, and to physical, chemical, and biological environmental hazards. In addition, as noted above, the tendency is for new health problems (e.g., AIDS) and risk factors to arise, which may operate via quite different mechanisms and pathways and yet to become rapidly stratified by socioeconomic and racial/ethnic status.
Nevertheless, there are opportunities for intervening in pathways and mechanisms that offer promise of reducing socioeconomic and racial/ethnic disparities and hence improving overall population health. These must involve, however, sensitivity to the specific sources of risk and also of resilience in disadvantaged socioeconomic and racial/ethnic groups and areas. Let us consider two examples—medical care and sources of resilience and health promotion in disadvantaged racial/ethnic groups.
Medical Care
What we know and do not know about the role of medical care in producing and alleviating socioeconomic and racial/ethnic disparities in health is illustrative. As already noted, there can be no question that wider availability of effective therapeutic and preventive medical care has improved population health, though to a more limited degree than is often presumed. However, Preston and Haines (1991) argued that improvements in medical care may also have exacerbated socioeconomic and racial/ethnic disparities in health to the extent that differential access to care has become more consequential for health. As we have seen, the implementation of national health services or insurance has failed to reduce socioeconomic and racial/ethnic disparities in health to the degree we had hoped or expected, if at all. Growing evidence suggests, however, that gross equalization of access or utilization fails to equalize access to maximally appropriate and effective care.
Addressing three kinds of issues offers promise of reducing socioeconomic and racial/ethnic disparities in the quality and appropriateness of care and hence in health. The first is to recognize that differentials in the ways the medical care system deals with different groups can lead to problems in the delivery of care. If disadvantaged socioeconomic and racial/ethnic groups do not have access to the same type and quality of providers and the same kind of relationships and communication with them as more advantaged persons, the result is likely to be their receiving less regular, preventive, and appropriate care. Second, the focus of the medical care system on different types of care differentially affects the health of different groups. Disadvantaged groups may benefit more from improvements in basic primary and preventive care; advantaged groups, from secondary and tertiary care. Thus, relatively poor societies (e.g., China, Costa Rica, Sri Lanka, Kerala State of India) have achieved “good health at low cost” by focusing their limited resources on ensuring equal access to basic primary and preventive care (Halsted et al., 1985). Finally, as discussed above, even secon-
dary and tertiary care appears to be distributed inequitably by racial/ethnic groups and probably also by socioeconomic status. This may explain why the United States generally lags behind other developed nations in population life expectancy, but surpasses all in life expectancy at age 80, where a high technology system supports a relatively elite set of survivors in the population.
Finally, we must also give more attention in medical care to identifying the ways in which the lives of individuals are constrained by broader social, economic, and political forces. Some evidence suggests that the effectiveness of behavioral interventions varies by the degree that they attend to social situations in which individuals are embedded. Syme's (1978) study of 244 hypertensive patients clearly illustrates how addressing underlying social and economic conditions appears to enhance the management of hypertension and improve the effectiveness of antihypertensive therapy. The patients in this study were matched on age, race, gender, and blood pressure history and randomly assigned to one of three groups. The first group received routine hypertensive care from a physician. In addition to routine hypertensive care, the second group also attended 12 weekly clinic meetings providing health education with regard to hypertension by a health educator and nurse practitioner. In addition to routine hypertensive care, the third group was visited by community health workers who had been recruited from the immediate community and provided with one month of training to address the diverse social and medical needs of persons with hypertension. These outreach lay workers provided information on hypertension but also discussed family difficulties, financial strain, and employment opportunities and, as appropriate, provided support, advice, referral, and direct assistance.
After seven months of follow-up, patients in the third group were more likely to have their blood pressure controlled than patients in the other two groups. In addition, those in the third group knew twice as much about blood pressure and were more compliant with taking their hypertensive medication than patients in the other two groups, and the good compliers in the third group were twice as successful at controlling their blood pressure as good compliers in the health education intervention group. Thus, even the effectiveness of the pharmacological treatment appeared to be enhanced in the group that also addressed the underlying stressful conditions of these hypertensive persons.
A study by Buescher and colleagues (1987) further illustrates how addressing underlying economic and social issues can improve the impact of medical care. This study compared the effectiveness of two approaches to delivering prenatal care in a population of predominantly black low-SES women in Guilford County, North Carolina. One group received prenatal care at the county health department. The other group received prenatal care from private practice physicians. Women who received care from the community-based physicians were twice as likely to have a low-birthweight baby, compared to those visiting the health department. The health department's prenatal care program attempted to comprehensively address the medical and social needs of the pregnant mothers. Prenatal care was provided by nurse practitioners, instead of physicians. Time was devoted during prenatal care visits to counseling the women about
nutrition and other aspects of personal care. As appropriate, referrals were made to the Women, Infants and Children Program, which provides nutritional supplements to poor women. These referrals, as well as missed clinic appointments, were followed up aggressively. James (1993) argues that the positive cultural features of this program may have been very important. It appears that the county health department 's program offered low-income women an extended network of social support, capable of meeting their needs in much the same way that older, more knowledgeable women have traditionally guided and supported young inexperienced mothers (James, 1993).
Adaptive Attributes of Disadvantaged Groups
One of the major paradoxes in U.S. population health is that African Americans and Latinos are not as disadvantaged on some aspects of health as their socioeconomic positions would lead us to expect. Thus, although African Americans tend to have higher levels of ill health than whites for most indicators of physical health and are also disadvantaged compared to whites on indicators of subjective well-being such as life satisfaction and happiness (Hughes and Thomas, 1998), they have comparable or better health status than whites for other indicators of mental health. Community-based studies using measures of psychological distress show an inconsistent pattern of black-white differences. Some studies show that blacks have higher rates of distress compared to whites, while other studies show higher rates of psychological distress for whites compared to blacks (Dohrenwend and Dohrenwend, 1969; Neighbors, 1984; Vega and Rumbaut, 1991; Williams and Harris-Reid, 1999). However, when rates of psychiatric illness are considered, African Americans have comparable or lower rates of mental illness than whites. In the Epidemiologic Catchment Area Study (ECA), the largest study of psychiatric disorders ever conducted in the United States, there were very few differences between blacks and whites in the rates of both current and lifetime psychiatric disorders. Anxiety disorders, especially phobias, stand out as one area in which blacks had considerably higher rates than Caucasians. In the National Comorbidity Study blacks do not have higher rates of disorder than whites for any of the major classes of disorders (Kessler et al., 1994). Instead, lower rates of disorders for blacks than whites are especially pronounced for the affective disorders (depression) and the substance abuse disorders (alcohol and drug abuse).
These findings emphasize the need for renewed attention to identify the cultural strengths and health-enhancing resources within the black community. Two social institutions—the family and the church —stand out as crucial for the black population. Strong family ties and an extended family system are important resources that may reduce some of the negative effects of stress on the health of black Americans. At the same time, a recognition of the strengths of black families should not be used to romanticize them as if they were a panacea for a broad range of adverse living conditions. While these networks of mutual aid and support do facilitate survival, they are also likely to provide both stress
and support. Moreover, it is likely that cutbacks in government-provided social services in recent years have increased the burdens and demands on the support services provided by the black family. The black American church has been the most important social institution in the black community. These churches have historically been centers of spiritual, social, and political life. Black churches may promote mental health by providing a broad range of social and human services to the African-American community, serving as a conduit to the formal mental health system, providing a base for friendship networks, and facilitating collective catharsis and stress reduction through religious rituals and participation (Williams, 1998).
A second paradox is evident for Mexican Americans. In spite of high rates of poverty and comparatively low levels of access to medical care, Mexican Americans tend to have similar or better levels of health than the white population. Moreover, across a broad range of health status indicators foreign-born Hispanics have a better health profile than their counterparts born in the United States. This pattern may reflect the impact of migration. Rates of infant mortality, low birthweight, cancer, high blood pressure, adolescent pregnancy, and psychiatric disorders increase with length of stay in the United States for Hispanics (Vega and Amaro, 1994). It is likely that increasing length of stay and greater acculturation of the Hispanic and Asian population will lead to worsening health. Early studies of acculturation found that rates of heart disease among Japanese increased progressively as they moved from Japan to Hawaii to the U.S. mainland (Marmot and Syme, 1976). As groups migrate from one culture to another, immigrants often adopt the diet and behavior patterns of the new culture. Several behaviors that adversely affect health status appear to increase with acculturation. These include decreased fiber consumption, decreased breast feeding, increased use of cigarettes and alcohol—especially in young women, driving under the influence of alcohol, and use of illicit drugs (Vega and Amaro, 1994). However, the association between acculturation, length of stay in the United States, and the prevalence of disease may be complex. Migration studies of the Chinese and Japanese show that the rates of some cancers, such as prostate and colon, increase when these populations migrate to the United States, while the rates of other cancers, such as liver and cervical, decline (Jenkins and Kagawa-Singer, 1994). Research is needed to identify the extent to which there are specific aspects of culture that promote health and the strategies that may be utilized to facilitate their maintenance over time.
Social and Economic Change and Policy as Major Determinants of Health
For all the reasons discussed to this point, we believe the reduction of socioeconomic and racial/ethnic disparities in health depends most on social changes and public policies that reduce disparities in socioeconomic and racial/ethnic status, or more exactly, ensure that all citizens live under conditions
that protect against disease and promote health. We would emphasize that we do not believe that there is evidence that inequality or hierarchy per se produces large social disparities in health, though it may always be a residual difference in any situation of inequality. This is because socioeconomic and other forces of advantage have diminishing returns to health. Thus, the issue is not reducing or eliminating inequality, but reducing or eliminating the relatively severe social and economic deprivations that still characterize the broad lower range (e.g., lower 25–50%) of the U.S. population in terms of socioeconomic and/or racial/ethnic status. The history of our own and other countries suggests that the poor (and truly disadvantaged) need not always be with us, and that as their conditions of life improve so does their health and hence also overall population health.
Improvements in the status of the socioeconomically or racially/ethnically disadvantaged can be made through the provision of either private or public goods or a combination thereof. That is, we can ensure their access to education, income, and other resources that allow them to obtain in the private market housing, health care, and good living and working conditions productive of health. Alternatively we can provide many of these as public goods. Different societies at different times have chosen different mixes, but all have converged on a mix of these strategies. How good is the evidence that they work to reduce health disparities and promote population health? It is both better and worse than we might expect or like.
Macrosocial Change and Health
Not to be ignored is the evidence of history that improvements in the educational, occupational, and income levels of populations have produced massive improvements in population health that in turn improve the human capital necessary for further socioeconomic advancement (see Figure 4). This has included the reduction of health disparities by socioeconomic position, gender, and/or race/ethnicity. Not surprisingly, educational and economic development are major priorities of less developed societies, and also of the developed countries.
Social Welfare and Health
Similarly, evidence from the more developed countries strongly suggests that ensuring that the fruits of development are broadly distributed, especially to the broad lower range of the population, assists in promotion of health. The rise of Sweden and then Japan to the highest levels of population health in the world, and the clearly reduced socioeconomic disparities in the case of Sweden, must be significantly attributed to their emphasis on ensuring good conditions of life for all, albeit via different mixes of social policy and provision of private and public goods.
More Focused Social Policies
One would like to have clearer evidence, however, that specific policies that improve the social and economic status of disadvantaged groups also improve their health. Unfortunately, we have not always evaluated the effects of such policies, and rarely their health impacts, and this remains an agenda for future research. However, limited and developing evidence is at least consistent with our thesis.
At least one study from the evaluation of the negative income tax experiments of the early 1970s shows positive effects on maternal and child health. In a study of expanded income support, Kehrer and Wolin (1979) found that the birthweight of infants born to mothers in the experimental income group was higher than that of those born to mothers in the control group although neither group experienced any experimental manipulation of health services. Improved nutrition, probably a result of the income manipulation, appeared to have been the key intervening factor. Evaluation of the long-term effects of early childhood interventions, such as the Perry preschool study, also suggests long-term effects on socioeconomic factors (median income and rates of home ownership) as well as on other behavior and beliefs (e.g., staying in school, avoiding delinquency and crime, achieving better jobs) that should promote health.
Major Exogenous Income Policies
An ideal test of our thesis would be the examination of social policies that have markedly improved the economic status of all or some of the disadvantaged population. In the United States, two stand out. One is Social Security which has provided an income support program for the elder portion of the population that has, over time, lifted or kept most of them out of poverty. We (Arno and House, in progress) have undertaken to see if one can find evidence that Social Security has also improved the health of the elderly. We have sought to do so by examining the mortality experience of different adult age groups in the population over the course of the century. We hypothesized that the two largest exogenous income improvements from Social Security occurred first at its inception in the late 1930s and second when it was indexed to inflation in the late 1960s and early 1970s. Hence, we expected that one should see discontinuous improvements in the health of the elderly, but not in other age groups, after these two periods. Our initial results, shown in Figure 6, seem to us consistent with this. We recognize that there may be other compelling explanations of these two discontinuities, but we do not believe that others have or would have predicted both of them ex ante or that other explanations can explain both as well or as parsimoniously ex post. Further, these trends are consistent with the evidence that socioeconomic differences in health are markedly reduced among the elderly as compared to working-age adults (House et al., 1990, 1994). The
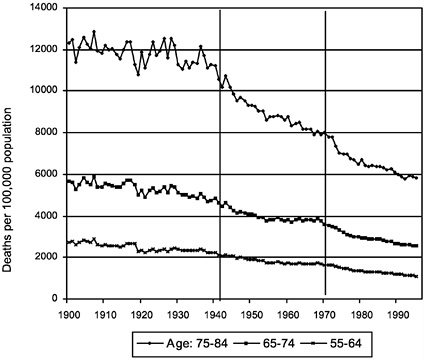
FIGURE 6 Total mortality, United States, 1900–1995.
other major income support program in our country has been the earned income tax credit, but we know of no research on its effects and would certainly see such research as a high priority for the future.
Investment in Public Goods and Infrastructure
Limited data also indicate that efforts to improve the public goods and infrastructures of communities improve the health of their residents. Some research suggests that policy changes to improve neighborhoods can importantly enhance health. Dalgard and Tambs (1997) provide findings from a 10-year follow-up study of residents in five neighborhood types in Norway. This study found that residents in a poorly functioning neighborhood that had experienced dramatic change in its social environment over time reported improved mental health 10 years later. The improvements in the neighborhoods included a new public school, playground extension, establishment of a sports arena and park, organization of activities for adolescents by the sports association of the municipality, establishment of a shopping center with restaurants and a cinema, and a subway line extension into the neighborhood. This effect was not explained by selective migration. Similarly, an intervention in England for a poorly functioning neighborhood also had dramatic effects (Halpern, 1995). Over a 2-year period this intervention refurbished housing, with a special emphasis on making it
safe and sheltered from strangers. Changes included improved traffic regulations, improved lighting and strengthening of windows, enclosure of gardens for apartments, closure of alleyways, and landscaping. In this project, residents were involved in the planning process. A 1-year follow-up study, conducted after the intervention had been in place, documented that the changes in the physical environment were associated with changes in the social environment and mental health as well. That is, the contact between neighbors had increased and neighbors reported more trust in each other. Levels of optimism and belief in the future had increased, and residents felt a stronger identification with their neighborhood. In addition, levels of anxiety and depression were significantly reduced among residents. This study reveals that improvement in the quality of life in a neighborhood can increase both the quality of social interaction or cohesion and health (see Paper Contribution I).
The Case of Racial/Ethnic Disparities
Racial/ethnic disparities in health should clearly be reduced by policies that reduce absolute and relative socioeconomic deprivation. However, they also need special approaches, obviously not aimed at changing race/ethnicity per se, but, rather, at changing the way race/ethnicity and associated racial/ethnic status are socially defined and constructed. Again, available evidence suggests there are reduced racial/ethnic disparities in health. Mullings (1989) has suggested that the civil rights movement, for example, had important positive effects on black health. By reducing occupational and educational segregation, it improved the SES of at least a segment of the black population and also influenced public policy to make health care accessible to larger numbers of people. Consistent with this hypothesis, one study found that between 1968 and 1978, blacks experienced a larger decline in mortality rates (on both a percentage and absolute basis) than whites (Cooper et al., 1981).
CONCLUSION
We hope this paper has produced an appreciation that socioeconomic and racial/ethnic disparities in health are the product of a broad and complex system of social stratification that will continue to structure the experience of and exposure to virtually all behavioral and psychosocial risk factors to health, hence producing large, persistent, and even increasing socioeconomic and racial/ethnic disparities in health. These health disparities largely explain why the United States increasingly lags behind other developed and even less developed nations in levels of population health, with the most disadvantaged portions of our population characterized by levels of population health comparable to some of the least developed nations in the world.
Socioeconomic and racial/ethnic disadvantages affect almost all forms of disease; almost all behavioral, psychosocial, and environmental risk factors pro-
ducing these diseases; and also access to the most appropriate and effective forms of medical care. These effects are persistent over time. Thus, as the major public health problems of society and the risk factors producing them change, they still will be more incident and prevalent among lower socioeconomic classes. Thus, intervening in or changing one or a few major risk factors for health (including inadequate medical care) can have only a limited effect on socioeconomic and racial/ethnic disparities in health, though this effect is clearly enhanced if interventions or changes are attentive to the broader social forces that produce these disparities.
The greatest past accomplishments and future potential for reducing socioeconomic and racial/ethnic disparities in health and improving overall population health involve improving socioeconomic status and reducing invidious racial/ethnic distinctions themselves, especially among the more disadvantaged portions of the population. Thus, economic growth and development and progress toward greater racial/ethnic equality have had and can have dramatic effects on individual and population health, especially if these changes impact the more disadvantaged socioeconomic and racial/ethnic groups in our society.
REFERENCES
Adler, N.E., Boyce, T., Chesney, M.A., Cohen, S., Folkman, S., Kahn, R.L., and Syme, S.L. ( 1994). Socioeconomic status and health: The challenge of the gradient. American Psychologist, 49(1), 15–24.
Adler, N.E., Boyce, T., Chesney, M.A., Folkman, S., and Syme, S.L. ( 1993). Socioeconomic inequalities in health: No easy solution. Journal of the American Medical Association, 269, 3140–3145.
Amaro, H., Russo, N.F., and Johnson, J. ( 1987). Family and work predictors of psychological well-being among Hispanic women professionals. Psychology of Women Quarterly, 11, 505–521.
Arno, P., and House, J.S. (in progress). Can socioeconomic policy improve population health and reduce social disparities in health: The case of Social Security.
Backlund, E., Sorlie, P.D., and Johnson, N.J. ( 1996). The shape of the relationship between income and mortality in the United States. AEP, 6, 12–20.
Barker, D.J.P., and Osmond, C. ( 1986). Infant mortality, childhood nutrition and ischaemic heart disease in England and Wales. Lancet, 1, 1077–1081.
Ben-Shlomo, Y., White, I.R., and Marmot, M. ( 1996). Does the variation in the socioeconomic characteristics of an area affect mortality? British Medical Journal, 312, 1013–1014.
Berkman, L.F., and Breslow, L. ( 1983). Health and Ways of Living. New York: Oxford University Press.
Blane, D., Hart, C.L., Smith, G.D., Gillis, C.R., Hole, D.J., and Hawthorne, V.M. ( 1996). Association of cardiovascular disease risk factors with socioeconomic position during childhood and during adulthood. British Medical Journal, 313(7070), 1434–1438.
Blau, P., and Duncan, O.D. ( 1967). The American Occupational Structure. New York: Wiley.
Blendon, R., Aiken, L., Freeman, H., and Corey, C. ( 1989). Access to medical care for black and white Americans. Journal of the American Medical Association, 261, 278–281.
Buescher, P.A., Smith, C., Holliday, J.L., and Levine, R.H. ( 1987). Source of prenatal care and infant birth weight: The case of a North Carolina county. American Journal of Obstetrics and Gynecology, 53, 204–210.
Bunker, J.P., Frazier, H.S., and Mosteller, F. ( 1994). Improving health: Measuring effects of medical care. Milbank Quarterly, 72(2), 225–258.
Chapman, K.S., and Hariharan, G. ( 1996). Do poor people have a stronger relationship between income and mortality than the rich? Implications of panel data for health-health analysis . Journal of Risk and Uncertainty, 12, 51–63.
Chen, M.S. ( 1993). A 1993 status report on the health status of Asian Pacific Islander Americans: Comparisons with Healthy People 2000 objectives. Asian American and Pacific Islander J.Health, 1, 37–55.
Collins, C.A., and Williams, D.R. ( 1999). Segregation and mortality: The deadly effects of racism? Sociological Forum, 14(3), 495–523.
Conley, D. ( 1999). Being Black, Living in the Red: Race, Wealth, and Social Policy in America. Berkeley, CA: University of California Press.
Cooper, R.S., and David, R. ( 1986). The biological concept of race and its application to public health and epidemiology. Journal of Health and Politics, Policy and Law, 11, 97–116.
Cooper, R.S., Steinhauer, M., Miller, W., David, R., and Schatzkin, A. ( 1981). Racism, society, and disease: An exploration of the social and biological mechanisms of differential mortality. International Journal of Health Services, 11(3), 389–414.
Dalgard, O.S., and Tambs, K. ( 1997). Urban environment and mental health: A longitudinal study. British Journal of Psychiatry, 171, 530–536.
Davis, J.A., and Smith, T.W. ( 1990). General Social Surveys, 1972–1990. Chicago: National Opinion Research Center.
Deaton, A. ( 1999). Inequalities in income and inequalities in health. NBER Working Paper 7141.
Devine, P.G. ( 1989). Stereotypes and prejudice: Their automatic and controlled components . Journal of Personality and Social Psychology, 56, 5–18.
Devine, P.G. ( 1995). Prejudice and out-group perception. Pp. 467–524 in A.Tesser ed., Advanced Social Psychology.
Dion, K.L., Dion, K.K., and Pak, A.W.P. ( 1992). Personality-based hardiness as a buffer for discrimination-related stress in members of Toronto's Chinese community. Canadian Journal of Behavioral Science, 24(4), 517–536.
Dohrenwend, B.P., and Dohrenwend, B.S. ( 1969). Social Status and Psychological Disorder: A Casual Inquiry. New York: Wiley.
Economic Report of the President ( 1998). Washington, DC: U.S. Government Printing Office.
Eller, T.J. ( 1994). Household Wealth and Asset Ownership: 1991. U.S. Bureau of the Census, Current Population Reports, P70–34. Washington, DC: U.S. Government Printing Office.
Elo, I.T., and Preston, S.H. ( 1992). Effects of early-life conditions on adult mortality: A review. Population Index, 58 (2), 186–212.
Evans, R.G., Barer, M.L., and Marmor, T.R. ( 1994). Why Are Some People Healthy and Others Are Not?: The Determinants of Health of Populations. New York: Aldine deGruyter.
Featherman, D.L, and Hauser, R.M. ( 1978). Opportunity and Change. New York: Academic Press.
Fischer, C.S., Hout, M., Jankowski, M.S., Lucas, S.R., Swidler, A., and Voss, K. ( 1996). Inequality by Design: Cracking the Bell Curve Myth. Princeton, NJ: Princeton University Press.
Fix, M., and Struyk, R.J. ( 1993). Clear and Convincing Evidence: Measurement of Discrimination in America. Washington, DC: Urban Institute Press.
Gornick, M.E., Eggers, P.W., Reilly, T.W., Mentnech, R.M., Fitterman, L.K., Kucken, L.E., and Vladeck, B.C. ( 1996). Effects of race and income on mortality and use of services among Medicare beneficiaries. New England Journal of Medicine, 335 (11):791–799.
Gould, S.J. ( 1977). Why we should not name human races: A biological view. Pp. 231–236in S.J.Gould (ed.), Ever Since Darwin. New York, W.W.Norton.
Gravelle, H. ( 1998). How much of the relation between population mortality and unequal distribution of income is a statistical artifact? British Medical Journal, 316, 382–385.
Halpern, D. ( 1995). Mental Health and Built Environment. London: Taylor and Francis.
Halsted, S.B., Walsh, J.A. and Warren, K.S. ( 1985) Good Health at Low Cost: Proceedings of a Conference at the Bellagio Conference Center, Bellagio, Italy, April 29–May 3. New York: Rockefeller Foundation.
Hannan, E.L., van Ryn, M., Burke, J., Stone, D., Kumar, D., Arani, D., Pierce, W., Rafii, S., Sanborn, T.A., Sharma, S., Slater, J., and DeBuono, B.A. ( 1999). Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Medical Care, 37(1), 68–77.
Harris, D.R., Andrews, R., and Elixhauser, A. ( 1997). Racial and gender differences in use of procedures for black and white hospitalized adults. Ethnicity and Disease, 7, 91–105.
Hauser, R.M. ( 1970). Context and convex: A cautionary tale. American Journal of Sociology, 75, 645–664.
Hauser, R. ( 1974). Contextual analysis revisited. Sociological Methods and Research, 2 (3), 365–375.
Hilton, J.L., and von Hippel, W. ( 1996). Stereotypes. Annual Review of Psychology, 47, 237–271.
House, J.S., Kessler, R.C., Herzog, A.R., Mero, R.P., Kinney, A.M., and Breslow, M.J. ( 1990). Age, socioeconomic status, and health. Milbank Quarterly 68(3), 383–411.
House, J.S., Kessler, R.C., Herzog, A.R., Mero, R.P., Kinney, A.M., and Breslow, M.J. ( 1992). Social stratification, age, and health. Pp. 1–32 in K.W.Schaie, D.Blazer, and J.S.House (eds.), Aging, Health Behaviors, and Health Outcomes. Hillsdale, NJ: Erlbaum.
House, J.S., Landis, K., and Umberson, D. ( 1988). Social relationships and health. Science, 241, 540–545.
House, J.S., Lepkowski, J.M., Kinney, A.M., Mero, R.P., Kessler, R.C., and Herzog, A.R. ( 1994). The social stratification of aging and health. Journal of Health and Social Behavior, 35, 213–234.
Hughes, M., and Thomas, M.E. ( 1998). The continuing significance of race revisited: A study of race, class, and quality of life in America, 1972 to 1996. American Sociological Review, 63, 785–795.
Hummer, R.A. ( 1996). Black-white differences in health and mortality: A review and conceptual model. Sociological Quarterly, 37(1), 105–125.
Jackson, J.S., Brown, T.N., Williams, D.R., Torres, M., Sellers, S.L., and Brown, K. ( 1996). Racism and the physical and mental health status of African Americans: A thirteen year national panel study. Ethnicity and Disease, 6(1,2), 132–147.
James, S.A. ( 1993). Racial and ethnic differences in infant mortality and low birth weight: A psychosocial critique. Annals of Epidemiology, 3(2), 131–136.
Jaynes, G.D., and Williams, R.M. ( 1987). A Common Destiny: Blacks and American Society. Washington, DC: National Academy Press.
Jencks, C., and Mayer, S.E. ( 1990). The social consequences of growing up in a poor neighborhood. Pp. 111–186 in L.E.Lynn, Jr., and M.G.H.McGeary (eds.), InnerCity Poverty in the United States. Washington, DC: National Academy Press.
Jenkins, C.N.H., and Kagawa-Singer, M. ( 1994). Cancer. Pp. 105–147 in N.W.S.Zane, D.T.Takeuchi, and K.N.J.Young (eds.,), Confronting Critical Health Issues of Asian and Pacific Islander Americans. Thousand Oaks, CA: Sage.
Kaplan, G.A., Pamuk, E.R., Lynch, J.W., Cohen, R.D. and Balfour, J.L. ( 1996). Inequality in income and mortality in the United States: Analysis of mortality and potential pathways. British Medical Journal, 312, 999–1003.
Kaplan, G.A., and Salonen, J.T. ( 1990). Socioeconomic conditions in childhood and ischaemic heart disease during middle age. British Medical Journal, 301, 1121–1123.
Kaufman, J.S., Cooper, R.S., and McGee, D.L. ( 1997). Socioeconomic status and health in blacks and whites: The problem of residual confounding and the resiliency of race. Epidemiology, 8, 621–628.
Kawachi, I., Kennedy, B.P., Lochner, K., and Prothrow-Stith, D. ( 1997). Social capital, income inequality, and mortality. American Journal of Public Health, 87, (9), 1491–1498.
Kehrer, B.H., and Wolin, C.M. ( 1979). Impact of income maintenance on low birth weight: Evidence from the Gary experiment. Journal of Human Resources, 14, 434–462.
Kennedy, B.P., Kawachi, I., and Prothrow-Stith, D. ( 1996). Income distribution and mortality: Cross sectional ecological study of the Robin Hood index in the United States. British Medical Journal, 312, 1004–1007.
Kessler, R.C., McGonagle, K.A., Zhao, S., Nelson, C.B., Hughes, M., Eshleman, S., Wittchen, H.-U., and Kendler, K.S. ( 1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Archives of General Psychiatry, 51, 8–19.
Kessler, R.C., Mickelson, K.D., and Williams, D.R. ( 1999). The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior, 40, 208–230.
Kirschenman, J., and Neckerman, K.M. ( 1991). “We'd love to hire them, but…”: The meaning of race for employers. Pp. 203–232 in C.Jencks, and P.E.Peterson (eds.), The Urban Underclass. Washington, DC: The Brookings Institution.
Krieger, N. ( 1990). Racial and gender discrimination: Risk factors for high blood pressure? Social Science and Medicine, 30(12), 1273–1281.
Krieger, N., Rowley, D.L., Herman, A.A., Avery, B., and Phillips, M.T. ( 1993). Racism, sexism, and social class: Implications for studies of health, disease, and well-being. American Journal of Preventive Medicine, 9(6 suppl), 82–122.
Krieger, N., and Sidney, S. ( 1996). Racial discrimination and blood pressure: The CARDIA study of young black and white adults. American Journal of Public Health, 86, 1370–1378.
Kuh, D., and Ben-Shlomo, Y. ( 1997). A Lifecourse Approach to Chronic Disease Epidemiology. Oxford: Oxford University Press.
Kunitz, S.J. ( 1987). Explanations and ideologies of mortality patterns. Population and Development Review, 13(3):379–408.
Lalonde, M. ( 1975). A New Perspective in the Health of Canadians. Ottawa: Information Canada.
Lantz, P.M, House, J.S., Lepkowski, J.M., Williams, D.R., Mero, R.P., and Chen, J. ( 1998). Socioeconomic factors, health behaviors, and mortality. Journal of the American Medical Association, 279, 1703–1708.
Lantz, P.M., Lynch, J.W., House, J.S.Lepkowski, J.M.Mero, R.P., Musick, M.A., and Williams, D.R. (in press). Socioeconomic disparities in health change in a longitudinal study of U.S. adults: The role of health risk behaviors. Social Science and Medicine.
Latter, B.D.H. ( 1980). Genetic differences within and between populations of the major human subgroups. American Naturalist, 116, 220–237.
LaVeist, T.A. ( 1996). Why we should continue to study race but do a better job: An essay on race, racism and health. Ethnicity and Disease, 6(1,2), 21–29.
Lewontin, R.C. ( 1972). The apportionment of human diversity. Pp. 381–386 in T. Dobzhansky, M.K.Hecht, and W.C.Steere (eds.), Evolutionary Biology, Vol 6. New York: Appleton-Century-Crofts.
Lewontin, R. ( 1982). Human Diversity. New York: Scientific American Books.
Lillie-Blanton, M., Parsons, P.E., Gayle, H., and Dievler, A. ( 1996). Racial differences in health: Not just black and white, but shades of gray. Annual Review of Public Health, 17, 411–448.
Lin-Fu, J.S. ( 1993). Asian and Pacific Islander Americans: An overview of demographic characteristics and health care issues. Asian and Pacific Islander Journal of Health, 1, 20–36.
Link, B.G. and Phelan, J. ( 1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, (Extra Issue): 80–94.
Lynch, J.W., Davey-Smith, G., Kaplan, G.A., and House, J.S. ( 2000). Income inequality and health: Importance to health of individual income, psychosocial environment, or material conditions. British Medical Journal, 320, 1200–1204.
Lynch, J.W., Kaplan, G.A., Cohen, R.D., Kauhanen, J., Wilson, T.W., Smith, N.L., and Salonen, J.T. ( 1994). Childhood and adult Socioeconomic status as predictors of mortality in Finland. Lancet, 343, 524–527.
Lynch, J.W., Kaplan, G.A., Cohen, R.D., Tuomilehto, J., and Salonen, J.T. ( 1996). Do cardiovascular risk factors explain the relation between Socioeconomic status, risk of all-cause mortality, cardiovascular mortality, and acute myocardial infarction? American Journal of Epidemiology, 144, 934–942.
Lynch, J.W., Kaplan, G.A., and Salonen, J.T. ( 1997). Why do poor people behave poorly? Variation in adult health behaviors and psychosocial characteristics by stages of the Socioeconomic lifecourse . Social Science and Medicine, 44 (6), 809–819.
Marmot, M.G., Davey-Smith, G., Stansfeld, S., Patel, C., North, F., Head, J., White, L. Brunner, E.G., and Feeney, A. ( 1991). Health inequalities among British civil servants: The Whitehall H Study. Lancet 337.
Marmot, M.G., Kogevinas, M., and Elston, M.A. ( 1987). Social/economic status and disease. Annual Review of Public Health, 8, 111–135.
Marmot, M.G., and Syme, S.L. ( 1976). Acculturation and coronary heart disease in Japanese-Americans. American Journal of Epidemiology, 104, 225–247.
Massey, D.S., and Denton, N.A. ( 1993). American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press.
McBean, A.M., and Gornick, M. ( 1994). Differences by race in the rates of procedures performed in hospitals for Medicare beneficiaries. Health Care Financing Review, 15(4), 77–90.
McCord C. and Freeman H.P. ( 1990). Excess mortality in Harlem. New England Journal of Medicine, 322, 173–177.
McDonough, P., Duncan, G.J., Williams, D., and House, J. ( 1997). Income dynamics and adult mortality in the United States, 1972 through 1989. American Journal of Public Health, 87 (9), 1476–1483.
McGinnis, M.J., and Forge, W.H. ( 1993). Actual causes of death in the United States. Journal of the American Medical Association, 270, 207–221.
McKeown, T.J. ( 1976). The Role of Medicine: Dream, Mirage, or Nemesis. London: Nuffield Provincial Hospitals Trust.
McKeown, T.J. ( 1979). The Role of Medicine: Dream, Mirage, or Nemesis. Princeton, NJ: Princeton University Press.
McKeown, T.J. ( 1988). The Origins of Human Disease. London: Blackwell.
McKinlay, J.B., and McKinlay, S.J. ( 1977). The questionable contribution of medical measures to the decline of mortality in the United States in the twentieth century. Milbank Memorial Fund Quarterly, 55, 405–428.
Mechanic, D. ( 1989). Socioeconomic status and health: an explanation of underlying processes . In: Bunker, J.P., Gomby, D.S., Kehrer, B.H. (eds.), Pathways to Health: The Role of Social Factors. Menlow Park, CA: Henry J.Kaiser Family Foundation.
Mellor, J., and Milyo, J. ( 1999). Income Inequality and Individual Health: Evidence from the Current Population Survey. Robert Wood Johnson Health Policy Scholars Working Paper #8. Boston University School of Management, Boston.
Mirowsky, J. and Hu, P.N. ( 1996). Physical impairment and the diminishing effects of income. Social Forces, 74(3), 1073–1096.
Moore, D.J., Williams, J.D., and Quails, W.J. ( 1996). Target marketing of tobacco and alcohol-related products to ethnic minority groups in the United States. Ethnicity and Disease, 6, 83–98.
Mullings, L. ( 1989). Inequality and African-American health status: Policies and prospects . Pp. 154–182 in W.A.VanHome, and T.V.Tonnesen (eds.), Twentieth Century Dilemmas—Twenty-First Century Prognoses. Madison, WI: University of Wisconsin Institute on Race and Ethnicity.
National Center for Health Statistics. ( 1990). Mortality Detail Files, 1990, Vol. VII. ICPSR Study #07632. Ann Arbor, MI: Inter-University Consortium for Political and Social Research.
National Center for Health Statistics. ( 1993). Trends in Indian Health—1993. Rockville, MD: U.S. Department of Health and Human Services.
National Center for Health Statistics. ( 1998). Health, United States, Socioeconomic Status and Health Chartbook. Hyattsville, MD: U.S. Department of Health and Human Services.
Neckerman, K.M., and Kirschenman, J. ( 1991). Hiring strategies, racial bias, and innercity workers. Social Problems, 38, 433–447.
Neighbors, H.W. ( 1984). The distribution of psychiatric morbidity in black Americans. Community Mental Health Journal, 20, 169–181.
Noh, S., Beiser, M., Kaspar, V., Hou, F., and Rummens, J. ( 1999). Discrimination and emotional well-being: Perceived racial discrimination, depression, and coping: A study of Southeast Asian refugees in Canada . Journal of Health and Social Behavior, 40(3), 193–207.
Oliver, ML., and Shapiro, T.M. ( 1995). Black Wealth/White Wealth: A New Perspective on Racial Inequality. New York: Routledge.
Omi, M., and Winant, H. ( 1986). Racial Formation in the United States: From the 1960s to the 1980s. New York: Routledge.
Pappas, G., Queen, S., Hadden, W., and Fisher, G. ( 1993). The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. New England Journal of Medicine 329, 103–109.
Patel, C., and Marmot, M.G. ( 1988). Efficacy versus effectiveness of relaxation therapy in hypertension . Stress Medicine, 4, 283–289.
Peterson, E.D., Shaw, L.K., DeLong, E.R., Pryor, D.B., Califf, R.M., and Mark, D.B. ( 1997). Racial variation in the use of coronary-revascularization procedures —Are the differences real? Do they matter? New England Journal of Medicine, 336(7), 480–486.
Power, C., Manor, O., Fox, A.J., and Fogelman, K. ( 1990). Health in childhood and social inequalities in young adults. Journal of the Royal Statistical Society (series A), 153, 17–28.
Preston, S.H., and Haines, M.R. ( 1991). Fatal Years. Princeton, NJ: Princeton University Press.
Quadagno, J. ( 1994). The Color of Welfare: How Racism Undermined the War on Poverty. New York: Oxford University Press.
Ren, X.S., Amick, B., and Williams, D.R. ( 1999). Racial/ethnic disparities in health: The interplay between discrimination and socioeconomic status. Ethnicity and Disease, 9(2), 151–165.
Robert, S.A. ( 1999). Socioeconomic position and health: The independent contribution of community context. Annual Review of Sociology, 25, 489–516.
Robert, S.A., and House, J.S. ( 2000a). Socioeconomic inequalities in health: Integrating individual-, community-, and societal-level theory and research. Pp. 115–135 in G. Albrecht, R.Fitzpatrick, and S.Scrimshaw (Eds.), Handbook of Social Studies in Health and Medicine. London: Sage Publishing Company.
Robert, S.A., and House, J.S. ( 2000b). Socioeconomic inequalities in health: An enduring sociological problem . Pp. 79–97 in C.Bird, P.Conrad, and A.Fremont (Eds.), Handbook of Medical Sociology. Upper Saddle River, New Jersey: Prentice Hall.
Rodgers, G.B. ( 1979). Income and inequality as determinants of mortality: An international cross-section analysis. Population Studies, 33, 343–351.
Rodin, J. ( 1986). Aging and health: Effects of the sense of control. Science 237, 143–149.
Salgado de Snyder, V.N. ( 1987). Factors associated with acculturative stress and depressive symptomatology among married Mexican immigrant women. Psychology of Women Quarterly, 11, 475–488.
Sampson, R.J., and Wilson, W.J. ( 1995). Toward a theory of race, crime, and urban inequality. Pp. 37–54 in J.Hagan, and R.D.Peterson (eds.), Crime and Inequality. Stanford, CA: Stanford University Press.
Satel, S. ( 1996). The politicization of public health. Wall Street Journal, Dec. 12, 1996; editorial section: 12.
Scheier, M.F., and Bridges, M.W. ( 1995). Person variables and health: Personality predispositions and acute psychological states as shared determinants for disease. Psychosomatic Medicine, 57, 255–268.
Schuman, H., Steeh, C., Bobo, L., and Krysan, M. ( 1997). Racial Attitudes in America: Trends and Interpretations. Cambridge, MA: Harvard University Press.
Schwartz, E., Kofie, V.Y., Rivo, M., and Tuckson, R.V. ( 1990). Black/white comparisons of deaths preventable by medical intervention: United States and the District of Columbia 1980–1986. International Journal of Epidemiology, 19, 591–598.
See, K.O., and Wilson, W.J. ( 1988). Race and ethnicity. Pp. 233–242 in N.J.Smelser (Ed.), Handbook of Sociology. Beverly Hills: Sage Publications.
Sorlie, P.D., Backlund, E., Johnson, N.J., and Rogot, E. ( 1993). Mortality by Hispanic status in the United States. Journal of the American Medical Association, 270, 2464–2468.
Sorlie, P.D., Backlund, E., and Keller, J.B. ( 1995). U.S. mortality by economic, demographic, and social characteristics: The National Longitudinal Mortality Study. American Journal of Public Health, 85 (7), 949–956.
Stangnor, C., and McMillan, D. ( 1992). Memory for expectancy-congruent and expectancy-incongruent information: A review of the social and social development literatures. Psychological Bulletin, 111, 42–61.
Steele, C.M. ( 1997). A threat in the air: How stereotypes shape intellectual identity and performance. American Psychologist, 52(6), 613–629.
Syme, S.L. ( 1978). Drug treatment of mild hypertension: Social and psychological considerations . Annals New York Academy of Science, 304, 99–106.
Taylor, J., and Jackson, B. ( 1990). Factors affecting alcohol consumption in black women, Part II. International Journal of Addictions, 25(12), 1415–1427.
Taylor, J., Henderson, D., and Jackson, B.B. ( 1991). A holistic model for understanding and predicting depression in African American women. Journal of Community Psychology, 19, 306–320.
Theorell, Töres G.T. ( 1982). Review of research on life events and cardiovascular illness. Advance Cardiology, 29, 140–147.
Trevino, F.M., Moyer, M.E., Valdez, R.B., and Stroup-Benham, C.A. ( 1991). Health insurance coverage and utilization of health services by Mexican Americans, mainland Puerto Ricans, and Cuban Americans. Journal of the American Medical Association, 265, 2233–2237.
U.S. Department of Health and Human Services ( 1990). Healthy People 2000: National Health Promotion and Disease Prevention Objectives. DHHS publication 91–50212 Washington, DC: U.S. Department of Health and Human Services.
U.S. Department of Health and Human Services. ( 1999). Healthy People 2010 Objectives: Draft for Public Comment. http://web.health.gov/healthypeople/2010Draft/object.htm
U.S. Public Health Service ( 1964). U.S. Surgeon General's Advisory Committee on Smoking and Health. Smoking and Health. U.S. Public Health Service, Washington, DC.
van Doorslaer, E., Wagstaff, A., Bleichrodt, H., Calonge, S., Gerdtham, U.-G., Gerfin, M., Geurts, J., Gross, L., Hakkinen, U., Leu, R.E., O'Donnell, O., Propper, C., Puffer, F., Rodriguez, M., Sundberg, G., and Winkelhake, O. ( 1997). Income-related inequalities in health: Some international comparisons . Journal of Health Economics, 16, 93–112.
Varmus H.E. ( 1999). Statement before the House and Senate Appropriations Subcommittees on Labor, Health and Human Services, and Education, February 23– 24. http://www.nih.gov/welcome/director/022299.htm
Vega, W.A., and Amaro, H. ( 1994). Latino outlook: Good health, uncertain prognosis. Annual Review of Public Health, 15, 39–67.
Vega, W.A., and Rumbaut, R.G. ( 1991). Ethnic minorities and mental health. Annual Review of Sociology, 17, 351–383.
Wenneker, M.B., and Epstein A.M. ( 1989). Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. Journal of the American Medical Association, 261, 253–257.
Whittle, J., Conigliaro, J., Good, C.B., and Lofgren, R.P. ( 1993). Racial differences in the use of invasive cardiovasular procedures in the Department of Veterans Affairs. New England Journal of Medicine, 329, 621–626.
Wilkins, R., Adams, O. and Brancker, A. ( 1989). Changes in mortality by income in urban Canada from 1971 to 1986. Health Reports (Statistics Canada catalogue 82–003, 1(2), 137–174.
Wilkinson, R.G. ( 1992). Income distribution and life expectancy. British Medical Journal, 301, 165–168.
Wilkinson, R.G. ( 1996). Unhealthy Societies: The Afflictions of Inequality. New York: Routledge.
Williams, D.R. ( 1990). Socioeconomic differentials in health: A review and redirection. Social Psychology Quarterly, 53(2), 81–99.
Williams, D.R. ( 1992). Black-white differences in blood pressure: The role of social factors . Ethnicity and Disease, 2, 126–141.
Williams, D.R. ( 1997). Race and health: Basic questions, emerging directions. Annals of Epidemiology, 7(5), 322–333.
Williams, D.R. ( 1998). African-American health: The role of the social environment. Journal of Urban Health: Bulletin of the New York Academy of Medicine , 75, 300– 321.
Williams, D.R. ( 1999). Race, SES and Health: The added effects of racism and discrimination . Annals of the New York Academy of Sciences, 896:173–188.
Williams, D.R. (in press). Racial variations in adult health status: Patterns, paradoxes and prospects. In N.Smelser, W.J.Wilson, and F.Mitchell (eds.), America Becoming: Racial Trends and Their Consequences. Washington, DC: National Academy Press.
Williams, D.R., and Chung, A.-M. (in press). Racism and health. In R.Gibson, and J.S. Jackson (eds.), Health in Black America. Thousand Oaks, CA: Sage Publications.
Williams, D.R., and Collins, C. ( 1995). U.S. socioeconomic and racial differences in health. Annual Review of Sociology, 21, 349–386.
Williams, D.R., and Harris-Reid, M. ( 1999). Race and mental health: Emerging patterns and promising approaches . Pp. 295–314 in A.V.Horwitz, and T.L.Scheid (eds.,), A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. New York: Cambridge University Press.
Williams, D.R., Yu, Y., Jackson, J.S., and Anderson, N.B. ( 1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2, 335–351.
Wolfson, M., Rowe, G., Gentleman, J.F., and Tomiak, M. ( 1993). Career earnings and death: A longitudinal analysis of older Canadian men. Journal of Gerontology, 48(4), S167–179.
Woolhandler, S., Himmelstein, D.U., Silber, R., Bader, M., Harnly, M., and Jones, A.A. ( 1985). Medical care and mortality: Racial differences in preventable deaths . International Journal of Health Services, 15, 1–11.