3
Allocating Resources
The Committee was charged, in part, with recommending a visionary framework for effective HIV prevention in the United States over the next 5 years. The Committee began by reviewing the HIV prevention literature. This review not only illustrated the wide variety of available social, behavioral, and technological interventions, but also highlighted the dramatic successes that have been accomplished through prevention (see Appendix B for more detail). The Committee also examined the sources and levels of federal funding for HIV prevention. We focused in particular on the Centers for Disease Control and Prevention (CDC), which plays a leading role in HIV prevention, although numerous other federal, state, and local government, and private agencies contribute substantially to these efforts (see Appendix C for a description of federal HIV prevention efforts). Further, the Committee examined the implicit strategies that appear to currently drive the investment of HIV prevention dollars, and we compared the results of those investments to the results that might have been achieved if those same resources had been allocated based on the new goal that we propose in this report, that is, preventing as many new HIV infections as possible.
The Committee’s analysis was challenging for numerous reasons, including the difficulty of determining exactly how current federal HIV funds are being spent, the absence of reliable data on HIV infection rates, and the limited data on the effectiveness and costs of many prevention
interventions.1 Nevertheless, the Committee believes that decisions regarding the allocation of public HIV prevention funds represent the single most important set of HIV prevention decisions made. Further, the Committee’s analysis indicates that a clear, consistently applied strategy of investing prevention funds in interventions that achieve the greatest potential reduction in new HIV infections could increase significantly the number of HIV infections prevented, even within current funding levels. Under this strategy, prevention funds would be allocated to the groups at highest risk and to the interventions that produce the biggest payoff for each dollar invested.
Today, very few policy makers or program administrators recognize either the enormous variation that exists in the cost-effectiveness of different types of programs or the importance of this variation in the overall impact of HIV prevention programs on the epidemic. Economic evaluation has emerged in recent years as an important tool for assisting in health policy decisions, and is increasingly being applied in the HIV prevention field (Holtgrave, 1998). Several major efforts have now examined the role of economic evaluation in public health policy decisions and have addressed methodological issues in conducting these evaluations (Phillips et al., 1998). For instance, the CDC has developed a practical guide to economic evaluation and decision analysis in public health policy decisions (Teutsch and Haddix, 1994; Haddix et al., 1996). The Panel on Cost-Effectiveness in Health and Medicine, convened by the U.S. Public Health Service in 1993, also has provided suggestions for improving the quality and comparability of cost-effectiveness analyses in health care decisions (Gold et al., 1996). In addition, collaborators from the CDC, local governments, academia, industry, and the Task Force on Community Preventive Services have established guidelines for systematic reviews of economic evaluations in community prevention (Carande-Kulis et al., 2000) and are currently examining the cost-effectiveness of HIV prevention interventions.
Still, it is unrealistic to expect that all federal prevention funds will be redirected to interventions that are shown to be the most cost-effective in
preventing new HIV infections, as resource allocation decisions are made in a highly charged environment, subject to numerous competing influences, including politics, advocacy, scientific evidence, personal values, and community norms (Holtgrave, 1998). However, a reassessment of current program investments, along with a strong commitment to direct all future increases in funding according to the principle of preventing the largest number of new infections, will yield meaningful results. The Committee recognizes the technical, social, and political barriers to immediate acceptance of this approach, but believes that the evidence argues strongly for a prevention strategy based on this principle.
In this chapter, the Committee argues the case for a data-driven strategy in support of programs that 1) demonstrate success in preventing new HIV infections and 2) do so on a cost-effective basis. Models that estimate the impact of adopting this strategy suggest that it will produce significant reductions in rates of new infections.
CURRENT ALLOCATION OF FEDERAL HIV PREVENTION FUNDS
Federal spending on HIV/AIDS is enormously complex and divided among numerous departments and agencies across the federal government. Within the Department of Health and Human Services alone, multiple agencies, including the CDC, the National Institutes of Health (NIH), the Substance Abuse and Mental Health Services Administration (SAMHSA), and the Health Resources Services Administration (HRSA), share responsibility for HIV prevention, research, and treatment efforts. State and localities also play a significant role in deciding how federal HIV prevention funds are spent. For instance, the CDC distributes a significant portion ($258 million in fiscal year 1999) of its total HIV prevention budget ($678 million in fiscal year 1999) through cooperative agreements with 65 state and local health departments (CDC, 1999). Community Planning Groups, comprised of representatives from groups of people at risk for HIV infection and of providers of HIV prevention services, advise these state and local health departments in setting their priorities and in making programmatic and resource allocation decisions (Valdiserri et al., 1995; Kaplan, 1998; Kaplan and Pollack, 1998). Similarly, SAMHSA distributes Substance Abuse Prevention and Treatment (SAPT) block grant funds to states, which decide how these funds and SAPT HIV set-aside funds2 will be used at the state and local level. Decisions regard-
ing the majority of Ryan White CARE Act funds, administered by HRSA, are also made at the state and local level (HRSA, 2000).3
Thus, there is no explicit strategy that currently guides the overall investment of federal HIV prevention funds. In some cases, individual agencies provide general criteria for prioritizing the use of federal funds. For example, the CDC directs Community Planning Groups to prioritize funds on the basis of several factors, including documented need, scientific evidence (including cost-effectiveness), consumer values and preferences, and local circumstances (CDC, 1993; Valdiserri et al., 1995). Other resource allocation decisions are subject to congressional mandates or earmarks. In many other cases, however, the criteria used to make decisions are less obvious. For instance, while Congress provides direction on the types of activities that the SAPT block grant and HIV set-aside funds can support, states have considerable discretion in how these funds are allocated. Currently, there is little information about the criteria that states use in their decisions, the types of activities that the SAPT block grant and HIV set-aside funds support, and the effectiveness or quality of programs that are funded (GAO, 2000).
Many prevention policy and funding decisions appear to be made with the tacit goal of avoiding political interference. For example, a 1994 external review suggested that CDC’s HIV prevention efforts had been limited and distorted by political pressures from the Reagan and Bush Administrations (Bayer, 1997). Fear of political reprise has been cited by some observers as a major factor in the Clinton Administration’s decision not to rescind the ban on federal funding of needle exchange programs, despite clear scientific evidence as to the value of such programs (Stolberg, 1998). Political factors also contributed to the CDC’s decision to suspend the Survey of Childbearing Women, which involved anonymous HIV testing of infants for surveillance purposes. This survey was halted just as Congress was pushing legislation to unblind the test results, a measure which would reveal the mother’s HIV status, but not necessarily the infant’s HIV status (Burr, 1997; IOM, 1999).
Indeed, the distribution of federal funds can best be described as an amalgam of administrative and legislative decisions that have been shaped in response to available data, constituency pressures, congressional mandates and earmarks, personal values, and the professional judgment of program managers. Further, the strategy that results from these cumulative decisions can best be described as “proportionality.” For the most part, federal HIV prevention funds—and CDC funds in particular—
are broadly allocated to maintain proportionality to reported AIDS cases. Thus, proportionality is the implicit strategy for allocation of federal funds. This point is illustrated by Figures 3.1–3.4. Figures 3.1 and 3.2 show how, over time, funds distributed to programs in two different CDC program categories providing services to different racial/ethnic groups approached the proportion of AIDS cases in these groups. Figures 3.3 and 3.4 show that community-planning funds distributed by the CDC to states to support HIV prevention were roughly proportional to the number of new AIDS cases reported by the states.
As a prevention strategy, proportionality has one important advantage. It begins with an objective criterion of need: observed AIDS cases. While proportionality may be useful for allocating funds for AIDS treatment, it has serious limitations, including the fact that it is an inadequate marker of need for prevention services. Further, proportionality rewards the reporting of AIDS cases rather than the prevention of new infections. This has the potential for creating two serious inefficiencies. First, proportionality reflects where the epidemic has been, rather than where it is going. Second, it rewards states and localities that use their resources ineffectively—and, as a result, have unnecessarily higher caseloads. The Committee believes that the adoption of a more sophisticated strategy
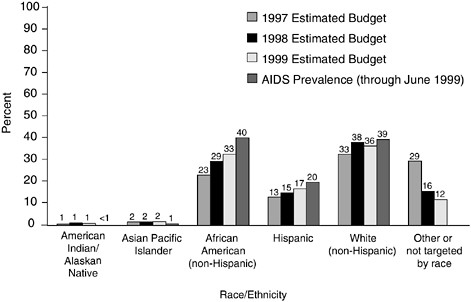
FIGURE 3.1 Counseling, testing, referral, and partner notification: FY 1997 to FY 1999 budget projections compared with AIDS prevalence by race/ethnicity. NOTE: AIDS not reported for other or not targeted by race/ethnicity. SOURCE: CDC.
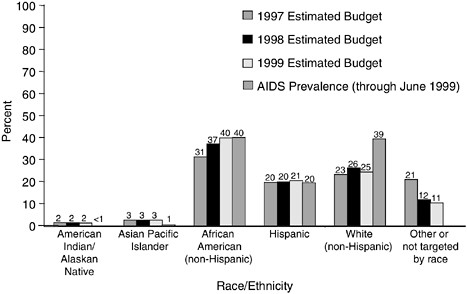
FIGURE 3.2 Health education and risk reduction: FY 1997 to FY 1999 budget projections compared with AIDS prevalence by race/ethnicity. NOTE: AIDS not reported for other or not targeted by race/ethnicity. SOURCE: CDC.
will yield larger returns. As an alternative to proportionality, the Committee recommends that prevention funds be allocated to reach populations at highest risk and to support programs that are cost-effective. Both aims are necessary to support a strategy of preventing the greatest number of new infections within budget constraints.
The Committee believes that it is now possible to start basing resource allocation decisions on cost-effectiveness principles. Cost-effectiveness is as much a way of thinking as a formal, quantitative technique for conducting policy analysis (Holtgrave, 1998). Since 1994, the CDC has endorsed the use of cost-effectiveness data as one component of its resource allocation decisions (Valdiserri et al., 1995). Even with imperfect information, adopting this framework of thinking about HIV prevention investment can set the stage for substantial improvements. While employing a framework of cost-effectiveness cannot dissolve the constraints on HIV prevention imposed by laws or the pressures of Congress, nor can it alleviate the social barriers (e.g., stigma, poverty, racism) that continue to fuel the epidemic and shape prevention policy (see Chapter 7), refocusing allocation decisions on the basis of cost-effectiveness can help elevate the discussion beyond these factors. The Committee believes that federal and state agencies, using the analytic findings to date, could make better decisions regarding their investments. Adopting a cost-effectiveness
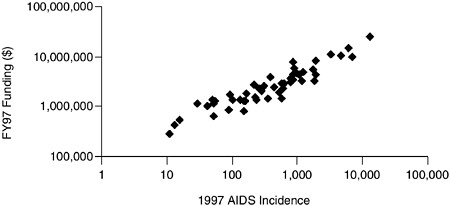
FIGURE 3.3 CDC-Allocated HIV prevention funds versus AIDS incidence by state.
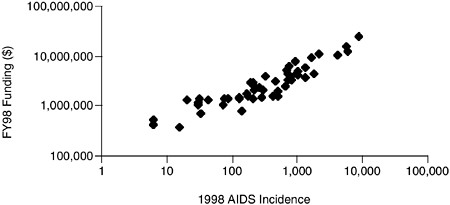
FIGURE 3.4 CDC-Allocated HIV prevention funds versus AIDS incidence by state.
framework will also point decision makers to areas where data are lacking and further research is warranted. In the absence of this framework, policy makers will continue to use the same decision rules that previously have failed in the past to maximize the number of HIV infections averted.
ASSESSING THE COST-EFFECTIVENESS OF HIV PREVENTION INTERVENTIONS
The cost-effectiveness of an intervention is a product of two factors: the cost of the intervention and the number of new infections prevented. The number of infections prevented by any particular intervention de-
pends on the baseline rate of new infections in the population that would occur in the absence of the intervention, and the fraction of those infections that the intervention can avert. Estimating the baseline rate of new infections (aggregate HIV incidence) is a problem of HIV epidemiology, while estimating program effectiveness is the fundamental challenge of program evaluation (Kaplan, 1998).
Researchers are working in both of these areas, but rarely have they converged to combine estimates for both factors.4 The Committee has attempted to combine these two areas to illustrate the value of an investment-based approach to allocation of prevention funds. Policy makers are not accustomed to making allocation decisions on the basis of cost-effectiveness. First, data have not been available to make decisions on that basis. Further, other values have dominated policy decisions about which interventions to support. The three examples below illustrate this point.
Protecting the Blood Supply
All blood donations in the United States have been screened for HIV since the deployment of the HIV antibody test in 1985, and this screening has reduced sharply the number of transfusion-related AIDS cases. However, screening is not 100 percent effective. There is a “window period” between the time of infection and the time when HIV antibodies can be detected by the screening test, and blood donated during this period may carry the AIDS virus. The window period for the recombinant HIV-1/2 combination enzyme-linked immunoassay (EIA) test is estimated at 22 days (Petersen et al., 1994; Busch et al., 1995; GAO, 1998). The p24 antigen assay, used since 1996, has reduced the window to about 16 days (Busch et al., 1995; AuBuchon et al., 1997; GAO, 1998). This six-day reduction lowered the number of infectious donations that entered the blood supply by about 27 percent. The absolute number of infections prevented, however, has been modest because the blood supply already was very safe. An estimated eight additional transfusion-related cases of HIV were pre-
vented, producing a cost-effectiveness ratio of $7.5 million per HIV infection prevented, compared to HIV antibody screening alone. Through extensive clinical trials, the Food and Drug Administration (FDA) has encouraged the development and use of a new, extremely sensitive Nucleic Acid Amplification Technology (NAT) test. This technology is designed to provide additional protection by further reducing the window period. Each additional HIV infection prevented with this new test will likely come at an even higher cost.
Preventing Perinatal Transmission of HIV
Approximately 6,000 to 7,000 HIV-infected women in the United States become pregnant each year (IOM, 1999). In the absence of treatment, between 25 percent and 30 percent of the babies born to these women will also be HIV-infected. However, the antiretroviral drug zidovudine (ZDV) has been proven effective in reducing the transmission probability to between 2 and 5 percent (IOM, 1999). The widespread use of ZDV, nevirapine, and other antiretroviral medications5 in the United States has prevented approximately 1,560 cases of perinatal HIV transmission annually. Combining the $5,700 cost of treatment for HIV-infected mothers with the HIV screening costs for all pregnant women in the United States results in a total estimated cost of $51 million, and a cost-effectiveness estimate of roughly $32,700 per HIV infection prevented.
Implementing Needle Exchange Programs
Injection drug users (IDUs) may account for an estimated 50 percent of new HIV infections (Holmberg, 1996), making them an obvious priority group for HIV prevention. Needle exchange programs that enable IDUs to trade used needles and syringes for clean equipment have proven valuable and cost-effective in HIV prevention. Many published evaluations of needle exchange programs, including separate reviews by the National Research Council, the CDC, and the U.S. General Accounting Office, have concluded that such programs reduce the spread of HIV without increasing the incidence of drug abuse in the community (GAO, 1993; NRC, 1995). Depending on the specific program model employed,
the cost-effectiveness of needle exchange is estimated to range from $3,000 to $50,000 per HIV infection prevented (Kaplan, 1995; Kahn, 1998), figures that are competitive with the cost-effectiveness of zidovudine for preventing perinatal transmission. However, needle exchange programs are not widely employed due to syringe prescription laws in some states and the prohibition against using federal funds to support such programs (See Chapter 7 for a discussion of needle exchange policies).
These examples illustrate how the federal government has promoted certain interventions and avoided others. In certain areas, large sums of money have been spent to prevent a small incremental number of infections; in other areas, federal policy prohibits federal sponsorship of certain interventions that have been proven effective in preventing a substantially larger number of infections. Together, these decisions imply a very wide range of implicit valuations regarding the monetary value of preventing an HIV infection. These decisions suggest, for example, that society implicitly values preventing a transfusion-related infection 150 times more ($7.5 million per infection averted) than preventing a drug-related infection through needle exchange ($50,000 per infection averted). While some variation in these values is to be reasonably expected,6 it is difficult to reconcile a difference of such magnitude.
USING EPIDEMIC IMPACT AS A MEASURE OF SUCCESS
In the examples above, data exist to make reasonably accurate estimates of both the impact of the intervention on new HIV infections, or the “epidemic impact,” and the cost of each new infection averted. Such clear evidence rarely is available. The Committee reviewed numerous studies evaluating HIV prevention interventions. Many of the studies conclude that “prevention works”—and, in the immediate frame of reference of the intervention, they may be correct. The great majority of such studies present comparisons of self-reported HIV risk behaviors among those participating in an HIV prevention intervention before and after the intervention was launched, and often in comparison with individuals who did
not receive the intervention. Typically, interventions are deemed successful if there are statistically significant changes in self-reported behaviors in the appropriate direction. For example, in an intervention designed to get men to use condoms during sex, if the average number of times men use condoms increases beyond what chance fluctuations would predict, then the intervention is viewed as a success. Likewise, if injection drug users participating in an intervention report that they are sharing needles less often, then this is taken as evidence that “prevention works.”
The intent here is not to review the difficulties inherent in the study of HIV risk behaviors (see NRC, 1991, for such a review). Rather, the Committee wishes to point out that, even if the reported social and behavioral data in HIV prevention studies are completely accurate, it remains difficult to decide what the results really mean in terms of HIV prevention. The basic question is: how many HIV infections can be averted through the deployment of alternative prevention interventions?
Consider the example of a prevention intervention that induces men to increase from 10 percent to 20 percent the rate at which they use condoms during receptive anal intercourse—a doubling of condom use. Assuming that the frequency with which these men practice such intercourse remains unchanged, the intervention would have doubled the number of protected acts of anal intercourse. This seems like strong evidence in favor of the intervention. However, from the standpoint of averting HIV infections, 90 percent of all acts of anal intercourse were unprotected before the intervention while, following the intervention, 80 percent of all such acts were unprotected. Basic principles of epidemiology suggest that the incidence of new HIV infections among receptive partners will be proportional to both HIV prevalence among insertive partners and the rate of unprotected anal intercourse (Anderson and May, 1991; Kahn, 1996). Since HIV prevalence would not change over a short time period, the relative reduction in HIV incidence is on the order of the relative reduction in the rate of unprotected anal intercourse, which equals 11 percent. Thus, a doubling of condom use in this example would lead only to an 11 percent reduction in HIV incidence.
This illustrates the point that, in considering the effectiveness of HIV prevention interventions for purposes of allocating funds, it is important to assess the potential benefits of prevention in terms of epidemic impact and not merely the effectiveness of the intervention in achieving its immediate objectives. A program that achieves statistically significant social and behavioral changes still may not avert large numbers of new infections. The challenge facing those who allocate prevention resources is to choose among competing interventions in different locations and to make decisions about levels of funding. Ideally, decision makers would assess
the efficacy and reach of various interventions against the background of the base rates of infection in different subpopulations. Such analysis would provide tools for predicting the results that might be expected from the many possible options for allocating HIV prevention funds. Today, decision makers virtually never have the information necessary to evaluate either the relative reach and effectiveness of competing programs or the relative risk status of various populations. Even if this information were available, there is no overall agreed upon strategy to guide decision makers’ choices.
A STRATEGIC VISION FOR HIV PREVENTION INVESTMENTS
The Committee recommends that CDC and other federal agencies supporting HIV prevention programs adopt a more strategic decision making process for allocating prevention funds. The Committee has already discussed the advantage of allocating funds on the basis of epidemic impact rather than proportionality. Executing that recommendation will require new approaches to deciding which programs to fund and at what levels. Currently, prevention interventions are evaluated based on their individual merit, within an overall allocation based on proportionality. The Committee recommends that funding decisions be made on the basis of maximizing the total number of HIV infections that can be prevented at a given expenditure level. The CDC and other federal agencies should be held accountable for facilitating and managing a funding decision-making process that is guided by that principle. Therefore, the Committee recommends:
Prevention resources should be allocated to prevent as many infections as possible. Such an allocation must take into account the cost and effectiveness of programs, in addition to estimates of HIV incidence. Evaluation should be a major component of resource allocation decision making. With better evaluation data reflecting the cost, efficacy, and reach of programs, resources could be more profitably invested in interventions that work efficiently. Interventions that do not work, or that are very expensive relative to infections prevented, could be abandoned.
While this principle may seem obvious, the Committee found that many current HIV prevention efforts are inconsistent with this goal. The remainder of this chapter describes a resource allocation strategy reflecting this vision, the advantages that would accrue from its use, and some of the problems that must be addressed prior to its implementation.
RESOURCE ALLOCATION FOR HIV PREVENTION
The primary goal of HIV prevention programs should be to prevent HIV infections. Achieving this goal requires prioritizing those combinations of HIV prevention activities that, on the basis of available evidence, are most effective in slowing the spread of disease. However, prevention programs differ in their costs as well as in their effectiveness at slowing HIV transmission. Because there always will be limited resources for HIV prevention, the basic policy and program challenge is how to use available federal funds to support the portfolio of prevention programs that will, in combination, prevent as many new infections as possible.
The Committee believes that allocation decisions regarding public HIV prevention money represent the single most important set of HIV prevention decisions made. The Committee has focused on the number of HIV infections prevented as the best metric for evaluating alternative HIV prevention resource allocation decisions.7 To the extent that there are additional benefits from these programs (e.g., decreases in drug use or in the incidence of sexually transmitted diseases), the Committee has underestimated total benefits. However, we have also underestimated total costs by focusing only on HIV prevention budgets, whereas funds used for interventions not specific to HIV prevention (e.g., interventions to reduce teen pregnancy) may also reduce HIV infection. This suggests that the resulting allocations could remain reasonable.
The Committee employed a standard model to explore the impact of different allocation decisions. The model, which is described in Appendix D, assumes a societal perspective because it deals with the use of public funds. The examples that follow, developed from the model, illustrate at both a program level and a national level the implications of alternative resource allocation decisions. This analysis assumes a unified HIV prevention budget for purposes of illustrating how different allocation deci-
sions affect the number of averted HIV infections. In reality, HIV prevention activities—such as counseling and testing, substance abuse treatment, antiretroviral therapy for pregnant women, and school-based HIV prevention education—are financed through separate funding streams, at different levels of government, and within separate organizations that have different organizational philosophies and political constituencies (See Appendix C). The fact that not all programs are funded by the same agency or budget does not invalidate the principle presented. Indeed, the following illustrations demonstrate the importance, given limited resources, of making evidence-based decisions about spending HIV prevention dollars both at the community level and at the national level.
Allocating Resources at the Community Level
As an example, assume that $300,000 will be allocated to programs providing services for injection drug users, and that the programs cost an average of $300 per client. Potentially, 1,000 of an estimated total of 1,500 IDUs in that location could be reached by such an allocation. However, if local conditions are such that only 50 percent of the total IDUs can actually be accessed by the intervention, then only 750 IDUs can be reached by the program—even if funds are available to accommodate 1,000 injectors.
Assume further that, in this location, the annual rate of new infections absent any intervention is equal to five new HIV infections per 100 IDUs per year, and that the program is able to reduce the annual rate of new infections by 20 percent. The result of spending $300,000 would be to reach 750 injectors (since that is the maximum that can be reached), and to reduce the total rate of new infections by 7.5 per year (a reduction from 37.5 to 30 total new HIV infections per year.) Note that 750 IDUs could have been reached by spending only $225,000, implying a misallocation of $75,000.
This example illustrates the problem of allocating the right amount of money to programs for one risk group in one location (Kahn, 1996). The actual challenge of allocating prevention funds across many activities in many locations is far more complex.
Allocating Resources at the National Level
In fiscal year 1999, the CDC distributed approximately $412 million through external cooperative agreements, grants, and contracts for HIV prevention programs nationwide (See Appendix C). To examine how this budget might be allocated to prevent as many infections as possible, the Committee modeled this problem using the same elements as in the previous example. The CDC allocates an HIV prevention budget across dif-
TABLE 3.1 Cost, Reach, and Efficacy of HIV Interventions
|
|
Injection Drug Users |
Men Who Have Sex with Men |
Heterosexuals |
||||||
|
Scenario |
Program Cost per Person |
Max. % of Population Reachable |
% HIV Incidence Reduction |
Program Cost per Person |
Max. % of Population Reachable |
% HIV Incidence Reduction |
Program Cost per Person |
Max. % of Population Reachable |
% HIV Incidence Reduction |
|
Optimistic |
$100 |
75% |
40% |
$50 |
75% |
55% |
$140 |
75% |
25% |
|
Base |
$300 |
50% |
20% |
$250 |
50% |
40% |
$300 |
50% |
15% |
|
Pessimistic |
$700 |
25% |
10% |
$500 |
25% |
25% |
$500 |
25% |
10% |
ferent prevention activities in varied locations. For example, the CDC allocates via the community planning process approximately $258 million to the states, territories, and those large cities hardest hit by HIV/AIDS.
As previously noted, the CDC’s HIV prevention funding now follows a pattern of proportionality to AIDS cases. Since AIDS cases appear to be used as a surrogate for HIV incidence when allocating funds, the Committee represents the agency’s current policy as proportionality to the rate of new HIV infections. Alternatively, the CDC could allocate funds on the basis of preventing as many new HIV infections as possible, within available funding levels. In Appendix D, the Committee details a mathematical model created to solve this problem, and we refer to the results as “cost-effective” allocations. In the model, HIV prevention funds are allocated toward those locations and risk groups in just the right amounts to prevent as many new HIV infections as possible in the aggregate.
The Committee’s model can be used to illustrate the improvements that might be gained if the nation invests its resources to prevent the maximum number of new infections. The Committee used this model to examine the impact of proportional policies versus cost-effective allocation policies, and to examine scenarios that assume different levels of investment according to program reach and cost-effectiveness. The model estimates the annual number of new HIV infections prevented at overall budget levels ranging up to $1 billion per year.
To illustrate our case while accounting for the considerable uncertainty in available data, the Committee developed three highly simplified scenarios that bracket the range of possibilities for HIV prevention investments. These are shown in Table 3.1. All are illustrative, as the data describing effectiveness, cost, and reach of programs are very scanty.8 The scenarios shown were developed on the basis of studies reviewed (see Appendix D for specific references) and against the background of HIV incidence data disaggregated by location and HIV risk group (Holmberg, 1996).9 The Committee believes that these scenarios provide a plausible illustration of the range of outcomes that the nation might experience under different assumptions of investment levels, program management,
|
8 |
See Appendix D for a description of how cost, efficacy, and reach estimates were derived. |
|
9 |
The analysis uses estimates of HIV incidence disaggregated by drug injectors, men who have sex with men, and high risk heterosexuals for 96 Standard Metropolitan Statistical Areas in the United States aggregated to the state level (Holmberg, 1996). |
and political will to utilize the tools available to confront the epidemic. The three scenarios are:
-
Pessimistic. Assumes that programs funded have the lowest prevention impact and high costs, and that they reach, on average, 25 percent of the relevant population.
-
Base. Assumes that programs funded have average effectiveness and average costs, and that they reach 50 percent of the relevant population.
-
Optimistic. Assumes that programs funded have the largest prevention impact and the lowest costs, and that they reach 75 percent of the relevant population (See Table 3.1).
The figures shown below illustrate that, by shifting investments towards more effective interventions and directing those interventions to the appropriate populations, more new infections can be averted. Figure 3.5 illustrates the impact of each of these scenarios assuming funding levels of up to $1 billion. For each scenario, the upper line reflects epidemic impact using the Committee’s recommendation to fund allocation on the basis of estimated HIV infection rates. The lower line illustrates the epidemic impact assuming the current proportional allocation formula. All of the curves exhibit the familiar economic property of diminishing returns to scale: as the amount of money invested in HIV prevention increases, the annual number of infections prevented also increases, but at a decreasing rate. Initial outlays on HIV prevention are thus more beneficial than later outlays.
For each of the three scenarios shown in Figure 3.5, the advantages of cost-effective over proportional allocation are considerable. For example, in the base case, allocating $412 million in proportion to HIV incidence would prevent approximately 3,000 new infections per year. Cost-effective allocation, however, would prevent roughly 3,900 new infections annually, a 30 percent increase.
Note that the proportional policy is worthwhile. Preventing 3,000 infections by spending $412 million yields an average cost of $137,333 per infection prevented, which is not at all unreasonable given that the life-time medical costs expended for treating HIV infection average near $200,000 per case (Holtgrave and Pinkerton, 1997). However, the cost-effective allocation we propose averts an additional 900 infections for the same $412 million expenditure on prevention.
Figure 3.5 also reveals the value of additional budget increases. Suppose the prevention budget could be increased by 50 percent from $412 to $618 million. In the base case, cost-effective allocation of these resources would enable preventing an additional 540 new infections per year. Com-

FIGURE 3.5 Annual infections prevented: cost-effective versus proportional allocation.
bining cost-effective allocation with a 50 percent budget increase would thus serve to increase the annual number of infections prevented by nearly 48 percent.
Figure 3.6 illustrates again the advantage to be gained from use of cost-effective rather than proportional allocation strategies. Cost-effective allocation is obviously most important when only limited funds are available; the returns from cost-effective allocations diminish as funds devoted to prevention increase. Nonetheless, in the base and pessimistic scenarios, cost-effective allocation offers at least a 30 percent increase in the number of infections that can be prevented for budgets of $500 million or less.
Against the backdrop of the previous three scenarios, Figure 3.7 shows the return on investments from more research on prevention interventions, with an emphasis on improving both the efficacy and reach of programs that might well be more expensive but that also are more effective. Figure 3.7 illustrates the “investment scenario,” whereby the efficacy
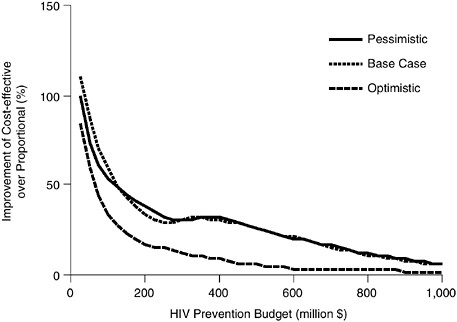
FIGURE 3.6 Cost-effective versus proportional allocation: percentage improvement.
and reach measures are those from the optimistic scenario described in Table 3.1, but costs of prevention per participant are from the pessimistic scenario.
Figure 3.7 makes it clear that investments in prevention can pay off. Assuming optimal allocation, the number of infections that can be prevented in this scenario grows to surpass the base case if at least $100 million is devoted to prevention. This scenario seems a more realistic portrait of what might be expected if investment in improved prevention programs were combined with the cost-effective allocation of prevention funds. At the Committee’s touchstone funding level of $412 million, this investment scenario would see the prevention of roughly 5,060 infections under optimal allocation (compared to 3,900 infections prevented in the base case via optimal allocation). The infections averted from proportional spending also would increase modestly from 3,000 in the base case to 3,390 in the investment scenario, again documenting the value of investing in better prevention programs.
The Committee stresses that while these calculations are illustrative, they are sufficiently robust to indicate the very substantial differences in results that could be obtained at every investment level by moving toward the recommended principles. While the Committee recommends that fed-
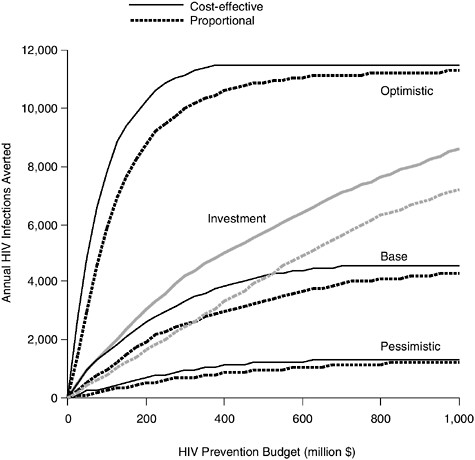
FIGURE 3.7 The impact of investing in better, more expensive programs: cost-effective versus proportional.
eral, state, and local prevention policymakers adopt a cost-effectiveness framework, the Committee is not recommending that federal, state, or local agencies replicate the exact model presented here. Improving the allocation of funds by weighing cost-effectiveness in selecting programs to be funded, and enhancing overall budget levels for prevention programs can effect very meaningful changes in the number of Americans who are infected with HIV. It is important for policy makers to understand the power of these choices and the magnitude of the changes that these choices drive.
The Committee acknowledges that other values will and should play a role in HIV prevention policy. However, it is important that the cost of those values (in terms of prevented HIV infections forgone) be understood and deliberately chosen. Two examples illustrate this point. First,
optimal allocations assume that all decisions are driven by the goal of preventing as many new HIV infections as possible, subject to resource constraints. Under certain scenarios (the base case example at $250 million funding, for example), it would not be cost-effective to fund programs aimed at women. Clearly, that would not be an ethical or socially desirable choice. A second example illustrates the cost of placing constraints on available HIV prevention programs based on values that punish socially proscribed behaviors. If needle exchange programs linked to drug treatment were allowed to enter the portfolio of federally funded HIV prevention programs, then the number of new infections prevented at the $412 million investment level is estimated to increase from 3,900 to 5,300 in the base case.10 The estimated difference of 1,400 prevented infections can be viewed as the human cost imposed by the ban on needle exchange.
SUPPORT FOR STATE AND LOCAL RESOURCE ALLOCATION
The Committee has focused on national-level resource allocation for purposes of illustrating how improved resource allocation can avert more HIV infections. The logic espoused in this chapter applies at the level of state and local governments as well. Implementing a cost-effectiveness decision-making process at the state and local levels, however, poses significant challenges. Two major barriers to conducting economic evaluations at these levels are the lack of technical expertise and the lack of funding. In addition, communities, target populations, and program staff may oppose evaluations out of fear that they will show a program is ineffective or result in a loss of funding. States and localities may also believe that evaluations conducted in other areas are not applicable to their unique needs (Weinstein and Melchreit, 1998). However, the Committee believes that these factors do not detract from the importance of developing a sound foundation for decision making, and the lack of complete information about the costs and benefits of HIV prevention efforts should not deter decision makers at all levels from adopting this framework. Using this framework can also help policy makers formulate a research agenda by pointing to areas where additional data on HIV inci-
|
10 |
This estimate follows from combining base case parameters from Table 3.1 for programs targeting men who have sex with men and heterosexuals with the optimistic estimates of program efficacy and reach, but pessimistic costs for programs targeting injection drug users (IDUs). This choice of parameters reflects what might happen if needle exchange programs linked to drug treatment programs were included in the federally funded HIV prevention portfolio. |
dence, program costs, and program effectiveness are needed to better inform future decisions.
As the nation’s lead prevention agency, the CDC has a special role to play in providing technical assistance to advisory and decision-making bodies at the state and local level on matters regarding the allocation of HIV prevention resources. The CDC’s sponsorship of cost-effectiveness workshops at recent community planning national meetings is especially welcomed in this regard. In addition, collaborations and partnerships between federal agencies (including CDC, NIH, SAMHSA, and HRSA), state health departments, community planning groups, and others will be necessary to define a research agenda, to identify and foster expertise for conducting cost-effectiveness studies, and to continue to fund research in cost-effectiveness.
REFERENCES
Anderson RM, May RM. 1991. Infectious Diseases of Humans: Dynamics and Control. Oxford, England: Oxford University Press.
AuBuchon JP, Birkmeyer JD, Busch MP. 1997. Safety of the blood supply in the United States: Opportunities and controversies. Annals of Internal Medicine 127(10):904–909.
Bayer R. 1997. Science, politics, and AIDS prevention policy. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology 14 (Suppl 2):S22–S29.
Brookmeyer R and Gail MH. 1994. AIDS Epidemiology: A Quantitative Approach. New York: Oxford University Press (Monographs in Epidemiology and Biostatistics; v. 22).
Burr C. 1997. The AIDS exception: Privacy vs. Public health. Atlantic Monthly 279(6):57–67.
Busch MP, Lee LL, Satten GA, Henrard DR, Farzadegan H, Nelson KE, Read S, Dodd RY, Petersen LR. 1995. Time course of detection of viral and serologic markers preceding human immunodeficiency virus type 1 seroconversion: Implications for screening of blood and tissue donors. Transfusion 35(2):91–97.
Carande-Kulis VG, Maciosek MV, Briss PA, Teutsch SM, Zaza S, Truman BI, Messonnier ML, Pappaioanou M, Harris JR, Fielding J. 2000. Methods for systematic reviews of economic evaluations for the Guide to Community Preventive Services. Task Force on Community Preventive Services. American Journal of Preventive Medicine 18(1 Suppl):75–91.
Centers for Disease Control and Prevention (CDC). 2000. U.S. Public Health Service Task Force Recommendations for the Use of Antiretroviral Drugs in Pregnant Women Infected with HIV-1 for Maternal Health and for Reducing Perinatal HIV-1 Transmission in the United States. Atlanta: CDC.
Centers for Disease Control and Prevention (CDC). 1999. Provisional Project List by Mission Category for FY99 CDC HIV/AIDS Budget. Atlanta: CDC.
Centers for Disease Control and Prevention (CDC). 1993. Supplemental Guidance on HIV Prevention Community Planning for Non-Competing Continuation of Cooperative Agreements for HIV Prevention Project. Atlanta: CDC.
General Accounting Office (GAO). 2000. Drug Abuse Treatment: Efforts Under Way to Determine Effectiveness of State Programs (GAO/HEHS-00-50). Washington, DC: GAO.
General Accounting Office (GAO). 1998. Blood Plasma Safety: Plasma Products Risks Are Low if Good Manufacturing Practices are Followed. (GAO/HEHS-98-205). Washington, DC: GAO.
General Accounting Office (GAO). 1993. Needle Exchange Programs: Research Suggests Promise as an AIDS Prevention Strategy. (GAO/HRD-93-60). Washington, DC: GAO.
Gold MR, Siegel JE, Russell LB, Weinstein MC (Eds.). 1996. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press.
Haddix AC, Teutsch SM, Shafer PA, Dunet DO (Eds.). 1996. Prevention Effectiveness: A Guide to Decision Analysis and Economic Evaluation. New York: Oxford University Press.
Health Resources and Services Administration. 2000. The AIDS Epidemic and the Ryan White CARE Act: Past Progress, Future Challenges. Washington, DC: HRSA.
Holmberg SD. 1996. The estimated prevalence and incidence of HIV in 96 large US metropolitan areas. American Journal of Public Health 86(5):642–654.
Holtgrave DR (Ed.). 1998. Handbook of Economic Evaluation of HIV Prevention Programs. New York: Plenum Press.
Holtgrave DR and Pinkerton SD. 1997. Updates of cost of illness and quality of life estimates for use in economic evaluations of HIV prevention programs. Journal of Acquired Immune Deficiency Syndromes 16(1):54–62.
Institute of Medicine. 1999. Reducing the Odds: Preventing Perinatal Transmission of HIV in the United States. Stoto MA, Almario DA, and McCormick MC (Eds.). Washington, DC: National Academy Press.
Janssen RS, Satten GA, Stramer SL, Rawal BD, O’Brien TR, Weiblen BJ, Hecht FM, Jack N, Cleghorn FR, Kahn JO, Chesney MA, Busch MP. 1998. New testing strategy to detect early HIV-1 infection for use in incidence estimates and for clinical and prevention purposes. Journal of the American Medical Association 280(1):42–48.
Kahn JG. 1996. The cost-effectiveness of HIV prevention targeting: How much more bang for the buck? American Journal of Public Health 86(12):1709–1712.
Kahn JG. 1998. Economic Evaluation of Primary HIV Prevention in Injection Drug Users. In Holtgrave DR (Ed.), Handbook of Economic Evaluation of HIV Prevention Programs. New York: Plenum Press. Pp. 45–62.
Kaplan EH. 1998. Economic Evaluation and HIV Prevention Community Planning—A Policy Analyst’s Perspective. In Holtgrave DR (Ed.), Handbook of Economic Evaluation of HIV Prevention Programs. New York: Plenum Press. Pp. 177–193.
Kaplan EH. 1995. Economic analysis of needle exchange. AIDS 9(10):1113–1119.
Kaplan EH and Brookmeyer R. 1999. Snapshot estimators of recent HIV incidence rates. Operations Research 47(1):29–37.
Kaplan EH and Pollack H. 1998. Allocating HIV Prevention Resources. Socio-Economic Planning Sciences 32:257–263.
National Research Council. 1991. Evaluating AIDS Prevention Programs. Coyle SL, Boruch RF, and Turner CF (Eds.). Washington, DC: National Academy Press.
National Research Council, Institute of Medicine. 1995. Preventing HIV Transmission: The Role of Sterile Needles and Bleach. Normand J, Vlahov D, and Moses LE (Eds.). Washington, DC: National Academy Press.
Petersen LR, Satten GA, Dodd R, Busch M, Kleinman S, Grindon A, Lenes B. 1994. Duration of time from onset of human immunodeficiency virus type 1 infectiousness to development of detectable antibody. The HIV Seroconversion Study Group. Transfusion 34(4):283–289.
Phillips KA, Haddix A, Holtgrave DR. 1998. An overview of economic evaluation methodologies and selected issues in methods standardization. In Holtgrave DR (Ed.). Handbook of Economic Evaluation of HIV Prevention Programs. New York: Plenum Press.
Stolberg SG. 1998. Clinton decides not to finance needle program. The New York Times:A1, April 21.
Substance Abuse and Mental Health Services Administration (SAMHSA). 2000a. HIV Strategic Plan. Washington, DC.: SAMHSA.
Substance Abuse and Mental Health Services Administration (SAMHSA). 2000b. “HIV Designated States” Fiscal Year Obligations, Substance Abuse Prevention and Treatment Block Grant. Washington, DC: SAMHSA.
Teutsch S and Haddix A, (Eds.). 1994. A Practical Guide to Prevention Effectiveness: Decision and Economic Analysis. Atlanta: Centers for Disease Control and Prevention.
Valdiserri RO, Aultman TV, Curran JW. 1995. Community planning: A national strategy to improve HIV prevention programs. Journal of Community Health 20(2):87–100.
Weinstein B and Melchreit RL. 1998. Economic Evaluation and HIV Prevention Decision Making. In Holtgrave DR (Ed.), Handbook of Economic Evaluation of HIV Prevention Programs. New York: Plenum Press.
























