5
Health Information Technology as the Engine for Learning
INTRODUCTION
Health information technology (HIT) is changing every aspect of health care, from the patient experience, to the way physicians make notes, to the dispensing of medications. Using HIT wisely is central to building a real-time knowledge engine, tools for care improvement, and a portal for practical patient involvement. For primary care physicians and patients, electronic data permit tracking of health status, outcomes, self-management, and more. At the health insurer or health system level, trends in care and outcomes can point the way to continuous quality improvement and learning. The availability of new data sources provides a broader view that can further expand quality improvement. Finally, as patients use new technology, such as cell phones, to communicate with providers, additional opportunities emerge for enhanced patient self-management, patient activation, public health messaging, and coaching.
Yet HIT has not gained a foothold with most physicians. Many have resisted purchasing electronic health record (EHR) systems because of high up-front costs and an uncertainty that EHRs will improve patient care and justify the expenditure. As the culture changes to promote “meaningful use” of patient data, new incentives are expected to drive broader adoption. Meanwhile, many physicians and patients must wrestle with the limitations of paper. It is nearly impossible to track test results, outcomes, or side effects by shuffling through a paper chart. Another challenge is that health information generated by government reports lags years behind in production. Transforming these databases into tools for learning will require new approaches.
The papers in this chapter explore the major trends toward and strategies for accelerating a nationwide HIT culture. The first paper, by David Blumenthal, formerly of Office of the National Coordinator (ONC) for Health Information Technology (now Harvard University) addresses the “meaningful use” of HIT—collecting data and disseminating them in such a way as to make science-driven care and value routine. As the concept gains traction, its meaning can broaden to include data sharing and more robust exchange.
Better types of data are also critical for success. Daniel R. Masys, Jack M. Starmer, and Jill M. Pulley of the Vanderbilt University School of Medicine describe three cases in which new classes of data support a learning health system and improved outcomes. Dashboard displays can improve the reliability of complex healthcare processes. Some electronic networks can link and use data that are scattered around the country, while others can track the experience with a particular drug after it has been approved.
Kemal Jethwani and Joseph Kvedar of Partners HealthCare report on how patients are reaping benefits as they use the Internet to connect with health systems. Notably, patients with congestive heart failure, diabetes, and high blood pressure are able to better manage their condition through electronic connectivity via cell phones, computers, and dialog with their patient team. Patients like this kind of connectedness. Also, as wireless technology grows, it offers promise for the development of many more new applications for learning.
THE MEANINGFUL USE OF HEALTH INFORMATION TECHNOLOGY
David Blumenthal, M.D., M.P.P.
Office of the National Coordinator for
Health Information Technology (former)
Harvard University
As the entity charged with coordinating efforts to implement and use advanced HIT and develop capacity for nationwide health information exchange, ONC plays a critical role in laying the groundwork for a learning health system. In its work to meet these critical short-term requirements, ONC also seeks to provide a pathway for achieving the potential of HIT to serve as an engine for continuous learning and care improvement. This paper reviews ONC’s efforts to date and some of the key technical, human, and political challenges to making available the kind of information that could be used to provide real-time and retrospective feedback to the healthcare system. Meeting all of these challenges is critical for improving health and the quality of care delivered in the United States.
HITECH Provisions and the Learning Healthcare System
Through the Health Information Technology for Economic and Clinical Health (HITECH) Act—part of the American Recovery and Reinvestment Act of 2009—Congress and the Obama Administration made investments in HIT aimed at improving health system performance and health outcomes. This act creates both the need and the requirement for ONC to lay a foundation for moving data from individual health records into some other form, as well as the need to enable solo physicians to exchange data in a way that is clinically meaningful to their patients and their practice. In so doing, the act also provides an opportunity to create capacity to support the collection and analysis of health information for addressing a variety of questions, including those involved in the study of technologies and medications or trends in public and population health. With Medicare and Medicaid funding becoming available in 2011 to reward the meaningful use of EHRs by qualified users, ONC must move quickly to meet these initial requirements.
Developing a learning health system requires that data be stored in electronic form in a way that can be translated and communicated to other sites and for other uses, and that most U.S. physicians—particularly those who work in practices of five or fewer physicians—be engaged in the capture and use of these data. But it also requires that these efforts be part of a larger national enterprise to achieve a nationwide, interoperable, private, and secure electronic health information system. ONC has several activities under way to advance progress on these near- and longer-term requirements.
State of Play: Ensuring Adoption and Effective Use of EHRs
The HITECH concept of meaningful use establishes an important link between the adoption of EHRs and their use to achieve specific health and health system performance goals. ONC’s rulemaking authority is therefore an important tool for guiding several stages of HIT infrastructure development. As part of the first stage, ONC is working to identify data elements that will meet fundamental needs for learning in the future and to enable data collection, information sharing, and reporting. As the work evolves, stages 2 and 3 will emphasize the use of EHRs to improve care processes and outcomes, respectively (Blumenthal, 2010).
Rulemaking for stage 1—defining meaningful use and certification criteria for EHRs that must be satisfied to qualify for payment—is under way. The key question driving this process is whether data specified will have almost universal value now and in the future.
ONC is also engaged in work to create robust capabilities and incentives—an ecosystem—that will permit and encourage the exchange of
health information. This capacity is essential for the extraction and analysis of data widely dispersed across the health system in individual records. ONC is working to develop the Nationwide Health Information Network, which has many of the technical features required to support such robust information exchange and the kind of inquiries necessary for metadata analysis. Cognizant of the importance of reaching clinicians where they are, ONC also seeks to provide simple, alternative methods of information exchange that may not have all the properties needed to achieve long-term aims, but will contribute to improved care for patients and providers in the short term. This simpler form of exchange will provide a pathway toward the kind of information transfer capacity needed for an ideal system.
These initial efforts to get physicians and other health professionals in small hospitals to store data electronically and to create an infrastructure that makes it possible to find and transfer data are pivotal to establishing a foundational capacity for a learning health system and are achievable within the current policy and funding provided under HITECH. ONC’s work has been substantially aided by the discussions and guidance of its committees on HIT policy and HIT standards with respect to approaches to health information exchange and requirements and data elements to include in the initial meaningful use framework. Stakeholder input on opportunities to encourage adoption and make information exchange more feasible is welcome.
Development of a National Infrastructure for Learning
If the meaningful use concept proves its value and gains durability, it may continue to be a focus of policy making. It is possible to imagine ever more demanding requirements for meaningful use, including data sharing and participation in more robust information exchange. However, ensuring the realization of the overarching vision for a national interoperable health information system that drives improvements in system performance and health depends upon leadership in Congress and the next administration, as well as public support.
Public Trust and Health Information Privacy and Security
Careful and constant attention to privacy and security issues will be essential to securing public trust and support. While people do take risks with their private information every time they go online to bank or make a purchase, there is clearly something more personal about the kinds of information stored in medical records. ONC will not be successful in creating an infrastructure for information exchange unless the public is confident—and conveys that confidence to the Congress—that those who collect and use
health data are doing so in a responsible way. The public must believe that the government is protecting its right to privacy and that the infrastructure is well protected against security breaches. To garner and maintain public trust, ONC will constantly reconsider and adapt its privacy and security frameworks, technologies, and legislative framework.
A working group of the ONC policy committee has reexamined the privacy and security needs associated with this new infrastructure and made recommendations in this area in summer 2010. Furthermore, ONC is also interested in investigating further the subject of data segmentation—the process by which sensitive data are potentially made more secure than routine health data. Technical issues exist in this area as well.
Concluding Thoughts
ONC’s goal is to enable realization of the vision of a learning health system. The problem is a technical, a human, and a political one that requires the careful balancing of, and constant attention to, a broad array of issues. Much work is required to make the needed technical infrastructure available and useful to researchers, policy makers, and the custodians of the public health. However, the potential benefits for the health and care of Americans make the success of this endeavor an imperative.
NEW CLASSES OF DATA, NEW OPPORTUNITIES TO LEARN
Daniel R. Masys, M.D., Jack M. Starmer, M.D.,
and Jill M. Pulley, M.B.A.
Vanderbilt University Medical Center
The concept of a learning health system intersects in a compelling way with the wisdom that one cannot manage what one cannot measure, or the more useful correlate that one can manage what one can measure. The society-transforming power of information technologies has been amply demonstrated by the spontaneous cultural shifts that have accompanied the global adoption of cell phones, electronic messaging of various types, and the web. The Internet is a ubiquitous set of distribution channels for digital data, and provides vivid examples of how the emergence of a new class of data results in what might be called the “leveraged creativity” of applications that dynamically use and add value to a basic infrastructure. Web “mashups”—real-time syntheses of data from multiple sources on the Internet—are typified by the many current applications that use geographic data (e.g., Google maps) and overlay hyperlinks on a seemingly endless variety of associated information, ranging from weather and traffic to shopping, as well as people joined by social networking applications. These phe-
nomena predict and are mirrored by changes in healthcare delivery—such as translational and clinical research that emerges as a result of either new classes of data with relevance for process control and/or scientific discovery or the new presentation of data that existed previously but were not available at the time and location of decision making. Three real-world examples serve to illustrate this premise.
The first is an instance of the effect of real-time presentation of data already captured in an inpatient environment, but not previously available to support quality control of a complex, team-based healthcare operation. Effective outcomes for many diseases require a multistep process, and the completion of any single step is necessary but not sufficient to achieve the desired outcome. For example, it is recommended that patients on ventilator support in intensive care units undergo a set of preventive measures to reduce risk of ventilator-associated pneumonia (VAP) (Coffin et al., 2008). These measures include prophylaxis against deep venous thrombosis, measures to reduce stress ulcers, sedation “vacations” to assess readiness to extubate, elevation of the head of the bed, mouth care, and hypopharyngeal suctioning. At Vanderbilt University Medical Center, electronic clinical decision support systems in use since 1994 provide alerts and reminders to clinicians about recommended best practices (Starmer et al., 2000). Each alert is triggered by an event monitor, a computer program that continuously reviews available data on an individual patient. The program generates a system message if a specific set of findings, such as a new laboratory value (e.g., falling serum potassium in the setting of digoxin administration) appears in the clinical data system.
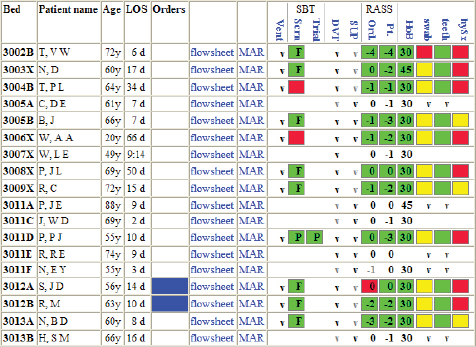
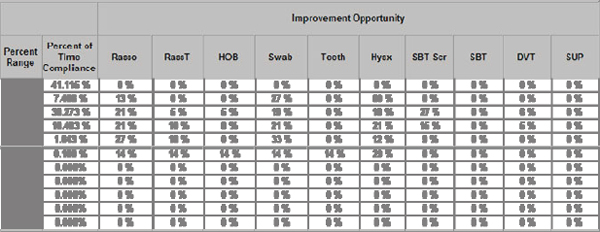
Computerized alerts were developed for the care measures needed to prevent VAP, and although compliance was high for most individual measures, the end-to-end consistency of all measures being administered for all patients was below 30 percent. A new set of displays of existing data, called “dashboards,” was created, showing all members of the care team which measures were due, done, and overdue (using simple green-yellow-red color coding, as shown in Figure 5-1). Also instituted was a set of web-based, real-time management reports of consistency of care showing “improvement opportunities” across all patients by time and location (see Figure 5-2). These changes were associated with a dramatic and sustained improvement in compliance with all measures and a reduction in the annual incidence of VAP per 1,000 patient days from 15.2 to 9.3 (Zaydfudim et al., 2009). Information technology alone was not responsible for this sustained improvement—which also required people and process—but it was a key enabling element.
A second example of new data sources catalyzing change is in the realm of personalized medicine—care tailored to known individual variability (particularly genetic variability) rather than being based on statistical
averages from large studies. In this realm, a large and growing number of studies employ genome-wide association studies (GWAS) to correlate physiologic states, such as the presence of a disease or a favorable or unfavorable response to a therapy, with individual genetic variation as represented by single nucleotide polymorphisms (SNPs), copy number variations (CNVs), and other manifestations of the genetic similarities and differences among individuals (Altshuler et al., 2008). These research efforts are made possible by high-throughput laboratory methods capable of assessing hundreds of thousands to millions of DNA molecular patterns (still representing measurement of less than 1 percent of the complete human genome) in a cost- and time-efficient manner. More than 650 such studies have been published (Hindorff et al.), based generally on an experimental model that involves finding individuals who have a condition of interest, constituting a research cohort, and performing a consistent set of research assessments to establish the phenotype. These findings are then correlated with genome-wide scans of genotype to look for statistically significant associations with SNPs, CNVs, and other types of individual genetic variation.
A National Institutes of Health-sponsored consortium named eMERGE (electronic MEdical Records and GEnomics)1 has demonstrated that phenotypes extracted from EHRs as a byproduct of health care delivered and documented for healthcare service rather than research purposes can replicate the observations drawn from carefully constituted research cohorts and also yield new observations (Ritchie et al., 2007). In addition, medical records may be regarded as reflecting the real-world experience of large collections of “experiments of nature,” thus enabling a new form of discovery that has been termed PheWAS (phenome-wide scanning) (Denny et al., 2010). In contrast to GWAS, which begin with an observable phenotype and perform a genome-wide scan, PheWAS begins with a genotype and scans all clinically documented health conditions to validate existing genetic effects, as well as to discover new, previously unanticipated relationships that can be based on specific gene effects and common molecular pathways or co-occurrences of disease states. A particularly fertile area of genomics is the evolving science of pharmacogenomics, wherein the focus is on the identification of genetic variation that affects drug absorption, metabolism, and distribution, and on the identification of biomarkers that predict unusually good or bad response to drug therapy (Ginsburg et al., 2005). As the adoption of interoperable EHRs makes clinical events available for research on a larger scale, the discovery of molecular predictors and correlates of important health states and outcomes becomes an increasingly powerful source of new classes of data for a learning health system.
A third example, with particular relevance to the themes of patient
______________
1 See http://www.gwas.net.
empowerment and patients’ ability to contribute to improved outcomes, is embodied in a prototype research application developed within Vanderbilt’s web-based patient portal, called MyHealthAtVanderbilt.2 Like patient portals at many academic and a growing number of community provider organizations, the MyHealthAtVanderbilt website provides registered users with a secure communication channel with their doctors and other providers, the ability to make appointments and renew medications, and online access to results of laboratory and imaging tests, as well as administrative functions related to billing and payment (Duncavage et al., 2007). More than 100,000 users of this portal have been enrolled, and each day more than 3,500 unique users log on to the site. This venue provides an opportunity to acquire data on types of health outcomes that are seldom if ever recorded by healthcare professionals, specifically the unanticipated positive effects of newly prescribed medications. Much attention and infrastructure are focused on identifying adverse drug effects, and surveillance for expected and unexpected adverse effects is a long-standing component of healthcare operations. Biological variability predicts that all unexpected effects are unlikely to be negative, but beyond the initial drug development process, there exists no systematic means of harvesting such serendipitous outcomes, and providers have no incentive to seek this information from patients or record it.
An institutional review board–approved pilot project undertaken within the MyHealthAtVanderbilt portal offered recipients of newly prescribed medications the opportunity to participate in an online survey of expected and unexpected drug effects. As shown in Figure 5-3, the individualized home page of a system user would display the invitation to participate if the associated pharmacy records showed that a new medication had been prescribed. Subsequently, the patient would confirm that he/she was currently taking the medication. Likert scale–like data entry would enable users to quickly describe both positive and negative reactions to medications, and unstructured text entry would enable them to describe unexpected effects (see Figure 5-4). More than 200 patients participated in the pilot feasibility study, which confirmed the expected distribution of therapeutic responses and known adverse effects and generated several “serendipity candidate” events (Pulley et al., 2010). Statistical validation of rare drug-associated events requires large populations that were not available for this pilot, but the prototype demonstrates that patient portals can be used to harness patients’ observations about their health as part of the clinical and translational research enterprise.
Each of the above examples is a data source that can be used to create a learning healthcare organization. Although quite different in the types
______________

FIGURE 5-3 Patient portal home page inviting participation in a research study regarding medication effects. The invitation is keyed on pharmacy records showing a recent new drug prescription.
of data they handle—real-time process measures in an intensive care unit, DNA variation associated with conditions recorded in EHRs, and patient-observed serendipitous drug effects—each conveys the power of new types of data to inform both research and care.
WEB 2.0 AND PATIENT ENGAGEMENT
Kamal Jethwani, M.D., M.P.H., and Joseph C. Kvedar, M.D.
Harvard Medical School and Partners HealthCare
“Connected health” is a term used to describe a model for healthcare delivery that uses technology to provide health care remotely. Technology is used to deliver patient care outside the hospital or doctor’s office, thus em-
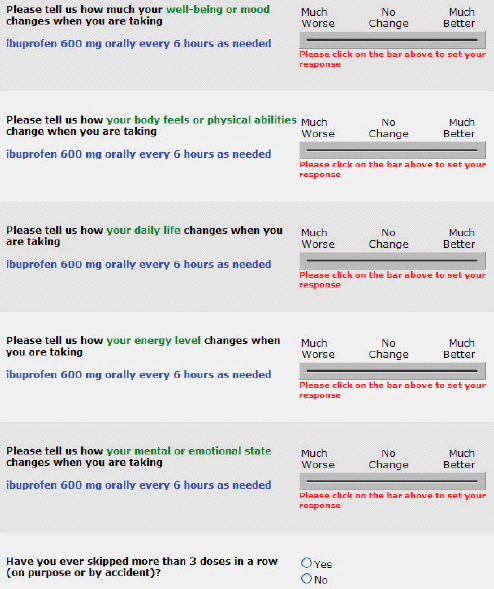
FIGURE 5-4 Sample online survey screen soliciting expected and unexpected medication effects. Patients responding “much better” or “much worse” were provided a text box for entry of their experiences.
powering patients to monitor their condition and obtain relevant feedback and coaching to achieve the best possible clinical outcomes.
The Center for Connected Health,3 a division of Partners HealthCare
______________
3 See http://www.connected-health.org (accessed October 12, 2010).
in Boston, follows these principles to deliver care for a range of high-risk patients with chronic conditions. Participants in its programs are patients and providers in Partners’ integrated delivery network throughout eastern Massachusetts. The Center has reported high rates of acceptance of its programs by patients and significant clinical improvement with a variety of patient groups, such as heart failure patients, hypertensive patients, and diabetics (Center for Connected Health).
Some forward-thinking employers in the area are also looking at such programs to help employees better manage their health. A recent example is EMC, a large data storage company that used SmartBeat, a hypertension self-management program developed by the Center for Connected Health. Such employee-based programs use characteristics that are unique to the work environment, such as competition, teamwork, and reward schemes, to motivate employees to adopt healthier behaviors.
Center for Connected Health: Overview
The Center currently offers three active programs for patients across the Partners network of hospitals: the Connected Cardiac Care Program (CCCP) for patients with chronic heart failure, Diabetes Connect for patients with type 2 diabetes mellitus, and Hypertension Connect for patients with hypertension (Table 5-1). The programs are designed to maximize opportunities for patient self-management of chronic diseases. The traditional model of care at the doctor’s office is overly episodic and minimizes the opportunity for patients to be active participants in their own care. Connected health programs change this model, bringing care directly to patients while their care provider coaches them through the process of care. The programs follow a similar structure, based on the following four cornerstones.
Accurate Physiologic and Behavioral Data
The connected health programs harness physiologic and behavioral data using technologies that obtain these data objectively, such as wireless scales and blood pressure cuffs, smart glucometers, and pulse oximeters. These objectively derived data are often more accurate and reliable than hand-entered data and are important in gaining both patient and provider engagement.
Data-Specific Feedback
Using the data transmitted to the Center’s servers, various levels of feedback are provided to users. This feedback ranges from a graphical
TABLE 5-1 Connected Health Programs Designed to Support Patient Self-Management of Chronic Disease
| Connected Cardiac Care Program (CCCP) | Diabetes Connect | Hypertension Connect | ||
| Physiologic data collected | Heart rate, blood pressure, blood oximetry, weight | Blood glucose | Blood pressure | |
| Feedback | Live feedback by tele-monitoring nurses, graphical display, and context-specific messages | Graphical display, messages from a nurse when readings out of range | Graphical display, messages from a nurse when readings out of range | |
| Coaching model | Centralized tele-monitoring nurse driven | Practice driven | Practice driven | |
| Patients enrolled as of April 1, 2010 | >1,000 | >150 | >40 | |
display of users’ data points over time, to assessment of their progress, to automatic alerts when their readings are out of a predetermined range.
Coaching
Data generated by users serve as the basis for context-specific feedback in the form of coaching. Coaching can be of two types: automatic and provider driven. Most connected health programs currently rely on coaching delivered by nurses who are working at the primary care level. These educators contact patients on a regular basis, provide feedback on their progress, and guide them to help improve control of their condition. The Center also has successfully demonstrated the use of automatic coaching by a “virtual coach.”
Interface with Physicians
The connected health approach places special emphasis on the presentation of data to clinicians. The main design principle is finding meaningful trends and exceptions and presenting them to clinicians in a concise and actionable format.
Connected Health Patients
Connected health programs use primarily the Internet to collect data, engage patients, and provide feedback on their success. Despite recent survey data from the Pew Internet Project indicating that only 62 percent of adults living with at least one chronic illness have access to the Internet, compared with 81 percent of adults with no chronic diseases (Pew Internet and American Life Project, 2010), most programs at the Center have seen almost 100 percent acceptance by users. The current challenge for connected health is to create programs that employ advanced technology in a way that is simple to use and even simpler to understand and access—hence the Center’s use of technology that connects to the Internet through simple telephone lines or Internet modems. Evidence also indicates that almost 70 percent of people with two or more chronic illnesses use mobile phones (as opposed to the 52 percent that use the Internet), underscoring the importance of mobile phones in reaching this population.
Mobile phones have proven to be an inexpensive, effective, and culturally acceptable means of keeping patients engaged with connected health programs. Mobile text messaging has been used in various programs as a tool to improve engagement. One such example is a sunscreen adherence study conducted by the Center, which demonstrated that participants who received daily text message reminders had significantly higher adherence rates (56.1 percent versus 30.0 percent, p <0.001) (Armstrong et al., 2009).
User Engagement
One commonly raised concern with connected health programs is whether patients will really use them. All programs of the Center for Connected Health are currently practice based; hence the decision regarding how active patients should be is made by the practice based on how sick the patients are, what their perceived comfort with technology is, and how far away from their goals they are.
An important observation in the Center’s ongoing program evaluation has been that patients who are not active in a program within the first 30 days of starting on the program almost never become active again. Patients who are active in the first month but not in the second likewise never become active again. Conversely, patients who remain active for the first 2 months have a 90 percent likelihood of remaining above the activity threshold throughout the program.
Another important determinant of success has been practice engagement, defined according to the number of times practitioners from a practice log on to the web portal to check their patients’ activity. Preliminary
data show that practices whose providers log on more frequently have more patients who are active and have greater clinical success.
Connected Cardiac Care Program
The CCCP is currently in its third year of operation, making it possible to study the program’s value in managing heart failure patients. Of about 3,000 eligible discharges from Partners each year, about 1,000 are enrolled in intensive monitoring using the CCCP. The program employs a weight scale, blood pressure cuff, and pulse oximeter as sensors, which upload data through a hub device given to the patient on enrollment. Three to four nurses oversee readings for 250 patients on any given day and reach out to the patients for software-flagged exceptions. Thus care can be focused on the patient, with data being uploaded every day and continuous telemonitoring being performed by the nurses. The involvement of the cardiologist is thus tailored to provide specialized care for those who need it, exactly when it is needed. Finally, the doctor is able to collaborate with patients on how their data relate to their clinical condition and affect their clinical outcomes and quality of life. As a result of this program, readmission rates have been reduced by almost half (from 0.92 annualized readmissions per person per year to 0.48) among program enrollees. Patients have reported higher awareness of how better to manage and control their clinical parameters and a greater sense of control over their disease condition.
Diabetes Connect: An Illustration of Lessons Learned
Diabetes Connect was started in February 2009 with two practices in the primary care network at Partners HealthCare that vary significantly in administration, activity, and success in the program. At the time of this analysis, the program had enrolled 75 patients divided almost equally between the two practices who were similar in age, gender, and pre-enrollment blood glucose level.
Practice 1 has a diabetes management center with dedicated staff (two registered nurses, certified diabetes educators, and a nutritionist) that supported the team of physicians. Practice 2 receives diabetes patient referrals from an endocrinologist and primary care providers in the community and is managed by one registered nurse. In the first 10 months of the program, practice 1 providers consistently logged on more often to the website (59 times/month versus 8 times/month by practice 2, p <0.001).
The overall drop in HbA1c, the main clinical outcome measure, varied by practice (–1.8 points for practice 1 and –0.9 points for practice 2, p <0.05). One explanation for this difference is how engaged the providers in charge of the application were as measured by the number of times they
logged on. Anecdotally, patients reported that they were more likely to participate in the program if they knew a provider was looking at their glucose upload data. Indeed, 78 percent of patients in practice 1 were found to be active, compared with 33 percent of patients in practice 2.
Active patients (defined as those who uploaded blood glucose readings) experienced a larger drop in HbA1c than patients who had no activity (practice 1: –1.85 vs. +0.1, p <0.001; practice 2: –1.38 vs. –0.6, p <0.05). These numbers point to a potential dose-effect relationship between patient activity and clinical success. Although the sample size is not large enough to permit definitive conclusions, the trend is convincing: those patients who uploaded their data more had better outcomes.
As already mentioned, getting patients to be engaged in the first 30 days appears to be extremely important. In this analysis, 50 patients had some activity in the first month. This number dropped to 40 in the second month. At the end of 10 months, 35 of those 40 patients were still active in the program. The 10 patients who ceased being active in the second month never became active again.
Conclusion
The recent healthcare reform legislation has opened up possibilities for changing reimbursement patterns and definitions of what is considered acceptable care. The connected health programs described in this paper show promise for helping physicians achieve clinical goals with their patients not only to meet reimbursement targets, but also to raise the standard of care provided to each patient. Early results suggest it is important to ensure and maintain both patient and provider engagement in the program.
Constant and meaningful feedback, coaching, and increased communication with providers could be useful tools to ensure patient engagement. Similarly, reimbursement patterns and improved clinical outcomes could influence provider engagement. Experience with the connected health programs shows that factors not only are individually important, but also enhance each other’s effects.
The evolving understanding of these programs will help improve the patient selection process to ensure that patients who are able to fully utilize and benefit from the programs will be enrolled. New technology, such as mobile phone applications and text messaging, provide an opportunity to simplify care provision even more and increase the range of patients that can be helped. Finally, strong organizational commitment to aligning reimbursement strategies to reflect clinical outcomes and superior patient care is essential to the successful implementation of any innovative care process, including connected health.
REFERENCES
Altshuler, D., M. Daly, and E. Lander. 2008. Genetic mapping in human disease. Science 322:881-888.
Armstrong, A. W., A. J. Watson, M. Makredes, J. E. Frangos, A. B. Kimball, and J. C. Kvedar. 2009. Text-message reminders to improve sunscreen use: A randomized, controlled trial using electronic monitoring. Archives of Dermatology 145(11):1230-1236.
Blumenthal, D. 2010. Launching HITECH. New England Journal of Medicine 262(5):382-385.
Center for Connected Health. Heart failure monitoring for homebound patients. http://www.connected-health.org/programs/cardiac-care/center-for-connected-health-models-of-care/heart-failure-monitoring-for-homebound-patients.aspx (accessed April 30, 2010).
Coffin, S. E., M. Klompas, D. Classen, K. M. Arias, K. Podgorny, D. J. Anderson, H. Burstin, D. P. Calfee, E. R. Dubberke, V. Fraser, D. N. Gerding, F. A. Griffin, P. Gross, K. S. Kaye, E. Lo, J. Marschall, L. A. Mermel, L. Nicolle, D. A. Pegues, T. M. Perl, S. Saint, C. D. Salgado, R. A. Weinstein, R. Wise, and D. S. Yokoe. 2008. Strategies to prevent ventilator-associated pneumonia in acute care hospitals. Infection Control and Hospital Epidemiology 29(S1):S31-S40.
Denny, J. C., M. D. Ritchie, M. A. Basford, J. M. Pulley, L. Bastarache, K. Brown-Gentry, D. Wang, D. R. Masys, D. M. Roden, and D. C. Crawford. 2010. PheWAS: Demonstrating the feasibility of a phenome-wide scan to discover gene-disease associations. Bioinformatics 26(9):1205-1210.
Duncavage, S., J. Mathe, J. Werner, B. Malin, A. Ledeczi, and J. Sztipanovits. 2007. A modeling environment for patient portals. American Medical Informatics Association Annual Symposium Proceedings 2007:201-205.
Ginsburg, G., R. Konstance, J. Allsbrook, and K. Schulman. 2005. Implications of pharmacogenomics for drug development and clinical practice. Archives of Internal Medicine 165:2331-2336.
Hindorff, L., H. Junkins, J. Mehta, and T. Manolio. A catalog of published genome-wide association studies. http://www.genome.gov/gwastudies (accessed June 28, 2010).
Pew Internet and American Life Project. 2010. Chronic disease and the internet. http://pewinternet.org/Reports/2010/Chronic-Disease.aspx (accessed April 30, 2010).
Pulley, J., N. Hassan, G. Bernard, J. Schildcrout, D. Robertson, D. Masys, and P. Harris. 2010. Identifying unpredicted drug benefit through query of patient experiential knowledge: A proof of concept web-based system. Clinical and Translational Science 3:98-103.
Ritchie, M. D., J. C. Denny, D. C. Crawford, A. H. Ramirez, J. B. Weiner, J. M. Pulley, M. A. Basford, K. Brown-Gentry, J. R. Balser, D. R. Masys, J. L. Haines, and D. M. Roden. 2007. Robust replication of genotype-phenotype associations across multiple diseases in an electronic medical record. American Journal of Human Genetics 86(4):560-572.
Starmer, J., D. Talbert, and R. Miller. 2000. Experience using a programmable rules engine to implement a complex medical protocol during order entry. Proceedings of the American Medical Informatics Association 2000:829-832.
Zaydfudim, V., L. A. Dossett, J. M. Starmer, P. G. Arbogast, I. D. Feurer, W. A. Ray, A. K. May, and C. W. Pinson. 2009. Implementation of a real-time compliance dashboard to help reduce ICU ventilator-associated pneumonia with the ventilator bundle. Archives of Surgery 144(7):656-662.