|
Institute of Medicine |
January 2016 |
Obesity in the Early Childhood Years: State of the Science and Implementation of Promising Solutions—Workshop in Brief
On October 6, 2015, the Roundtable on Obesity Solutions of the National Academies of Sciences, Engineering, and Medicine held a workshop titled “Obesity in the Early Childhood Years: State of the Science and Implementation of Promising Solutions.” The workshop examined what is currently known about the prevalence of obesity in young children, its trends over time, and its persistence into later childhood, adolescence, and adulthood; epigenetic factors related to risk of early childhood obesity; and the development of taste and flavor preferences in the first few years of life. The workshop explored recent developments in the science of modifiable protective and risk factors associated with obesity through age 5, including a mother’s pre-pregnancy weight and weight gain during pregnancy; smoking during pregnancy; breastfeeding; complementary feeding,1 responsive parenting; and sleep, activity, and sedentary behavior in young children.
Building on these modifiable protective and risk factors, workshop participants discussed interventions, practices, and policies (called “interventions” from here forward) that have demonstrated promise in prevention and treatment of early childhood obesity, including the role of pediatricians in obesity prevention and treatment, programs that take place in early care and education settings, and family-focused interventions. Finally, the workshop examined innovative cross-sector solutions, including multifaceted government programs at the national and local levels and partnerships involving health care systems.
This brief summary of the workshop highlights the observations made at the workshop by the speakers and during the discussion sessions. These observations represent the viewpoints of individual speakers and participants and should not be seen as conclusions or recommendations of the Institute of Medicine or of the workshop as a whole. A full summary of the workshop will be available in Spring 2016.
THE PRESENT OPPORTUNITY
Early childhood—from birth to age 5—is considered an opportune time to reverse the increase in obesity that the United States has experienced in recent years, said Mary Story, professor of global health and community and family medicine at Duke University, in her opening remarks at the workshop. As noted later in this brief, children establish eating and physical activity patterns in the early years of life that can persist throughout their lifetimes. Early childhood is also a period when parents are especially motivated to improve their own health and the health of their infants. Several workshop participants described various private- and public-sector initiatives that aim to reduce the prevalence of obesity in young children, including recent examples from New York City.
______________
1 The transition from exclusive breastfeeding to food and other liquids.
![]()
On average, children in the United States have gained weight since the early 1970s, observed Cynthia Ogden, epidemiologist at the National Center for Health Statistics at the Centers for Disease Control and Prevention (CDC). Based on growth charts prepared by the World Health Organization and CDC, Ogden described that in 2011–2012 the prevalence of high weight-for-recumbent length2 in children less than 2 years of age in the United States is between 7 and 8 percent, with a higher prevalence for girls than boys. Among children 2 to 5 years old, according to data presented by Ogden from the National Health and Nutrition Examination Survey, obesity3 has risen from approximately 5 percent in the early 1970s, when existing body mass indexes (BMIs) were used to establish a baseline for obesity, to 8.4–9.5 percent for boys and 7.2 percent for girls in 2011–2012. The percentage of 2- to 5-year-olds who are overweight4 is 14.4 percent overall, with an approximately equal distribution for boys and girls. Ogden explained that differences in these numbers between ethnic and racial groups become prominent by 2 to 5 years of age, with the numbers higher among Hispanic and African American children than among white and Asian children.
Among 2- to 19-year-olds in the United States, the prevalence of obesity has tripled—to more than 15 percent—from the 1970s to 2011–2012, Ogden reported. However, obesity trends were essentially flat over the decade before the most recent data, meaning that the increases occurred largely in the 1980s, 1990s, and the first few years of the 2000s (see Figure 1). Furthermore, for 2- to 5-year-olds, over the period from 2003–2004 to 2011–2012, the prevalence of obesity decreased from 13.9 percent to 8.4 percent, though Ogden stated that more data are needed to confirm this drop. This significant decline was seen only in this age group.
A number of studies found an association between childhood obesity and adult obesity, Ogden pointed out at the end of her presentation. These studies leave many questions unanswered about the persistence of obesity into adulthood, but suggest that it becomes more likely if the child ages at an unhealthy weight.
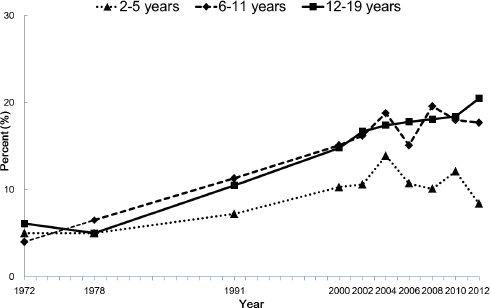
FIGURE Trends in prevalence of obesity among children and adolescents 2–19 years, by age: United States, 1971–1974 through 2011–2012.
SOURCE: Ogden presentation, October 6, 2015. Centers for Disease Control and Prevention/National Center for Health Statistics. National Health Examination Surveys II (ages 6–11), III (ages 12–17), National Health and Nutrition Examination Surveys (NHANES) I–III, and NHANES 1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, and 2011–2012.
______________
2 A weight-for-recumbent length above the 95th percentile on the CDC growth chart.
3 A BMI at or above the 95th percentile on the CDC growth chart.
4 A BMI at or above the 85th percentile and below the 95th percentile on the CDC growth chart.
Shari Barkin, William K. Warren Foundation Endowed Chair and Professor of Pediatrics at Vanderbilt University, described an intriguing new area of research that has a bearing on childhood obesity: the science of epigenetics. Epigenetics refers to how the environment may affect the expression of genes by influencing how they are expressed in different tissues and at different times. For example, maternal and paternal nutrition both affect the expression of genes in children. A mother’s high-fat diet during pregnancy can alter a child’s gene expression related to lipid metabolism, glucose metabolism, and appetite, which in turn can affect the phenotype of that child.
Further study of epigenetics could direct attention to factors in the environment that are modifiable, Barkin observed. Research on gene expression also could indicate which children are at risk, and potential mechanisms that could increase or decrease that risk.
FOOD PREFERENCES
Julie Mennella, a faculty member at the Monell Chemical Senses Center, described some of the ways in which our food preferences are shaped by our evolutionary heritage and by the foods to which we are exposed early in life. Babies are born with an attraction to the sweet taste of mother’s milk. This preference for sweet taste—our taste signal for energy—remains heightened during childhood and periods of growth. However, in the current food environment, the elegant biology that attracts children to mother’s milk and to calories makes them vulnerable to obesity.
Sensory experiences beginning early in life can modify flavor and food preferences, Mennella pointed out. With repeated tastings of a food and extended experiences with food variety, children can learn to eat healthier foods. Yet many families are not eating healthy foods, so children may have little exposure to them.
Mennella pointed to interventions before conception or the birth of a child as a time when parents are motivated to change long-established patterns of behavior as well as interventions that not only focus on the child, but also include the parents or family. Similarly, as taste and flavor preferences begin to change in adolescence, teens can be encouraged to improve their diets before they become parents themselves.
MODIFIABLE PROTECTIVE AND RISK FACTORS
Pregnancy and the early years of life offer many opportunities for understanding and addressing obesity in young children. Mothers’ pre-pregnancy BMI, weight gain during pregnancy, and smoking during pregnancy have all been associated with obesity in young children, observed Lisa Bodnar, associate professor in the Departments of Epidemiology and Obstetrics/Gynecology at the University of Pittsburgh Graduate School of Public Health and School of Medicine. For example, Bodnar reported that research has shown children of mothers who are obese or severely obese before they become pregnant have a three- to four-fold increase in risk of obesity. Children also have a substantial increase in the risk of obesity when their mothers gain more weight during pregnancy than is recommended. Finally, smoking in pregnancy is consistently associated with an increased risk of childhood obesity.
Breastfeeding is associated with childhood obesity prevention in the general population, said Rafael Pérez-Escamilla, professor of epidemiology at the Yale School of Public Health. The effect size is small, which is not surprising given the constellation of factors that influence obesity. A variety of evidence-based strategies are available to protect the ability of mothers who wish to breastfeed their babies, he noted, including facility- and community-level initiatives such as baby-friendly hospital initiatives and breastfeeding protection policies.
The dynamic eating patterns in the first few years of life offer many opportunities to change lifelong habits, noted Jose Saavedra, global chief medical officer for Nestlé Nutrition and associate professor of pediatrics at the Johns Hopkins School of Medicine. The foods and beverages a child consumes early in life can establish preferences and patterns that persist for many years. Yet, once complementary feeding is initiated, on any given day 30 to 40 percent of infants and toddlers (aged 6 months to 4 years) do not eat any vegetables, and 20 to 35 percent of children in this age group do not eat any fruit, according to Nestlé’s Feeding Infants and Toddlers Study. Campaigns that emphasize withholding solids until 4 months of age, increasing the consumption of fruits and vegetables, and decreasing the consumption of sweets and sweetened beverages could help establish healthier eating patterns, he said.
Responsive parenting, in which parents deliver prompt, developmentally appropriate responses that are contingent on a child’s behavior and needs, can reduce obesity risk, said Leann Birch, William P. Flatt Professor in the Department of Foods and Nutrition at the University of Georgia. Responsive parenting is meant to foster the development of self-regulation, including such behaviors as self-control, willpower, delay of gratification, and emotion
regulation. These behaviors related to self-regulation could be important in avoiding excessive intake in the current food environment.
Insufficient sleep in infancy and early childhood, a lack of physical activity, and sedentary behavior in early childhood are associated with a higher risk of obesity in childhood, according to Elsie Taveras, division chief of General Academic Pediatrics and director of Pediatric Population Health Management at the MassGeneral Hospital for Children, associate professor of pediatrics and population medicine at Harvard Medical School, and associate professor of nutrition at Harvard School of Public Health. Taveras also noted that these and the other risk factors identified in this session are significantly higher in some ethnic and racial groups by 2 to 5 years of age, which may partly explain the disparities in prevalence of obesity.
INTERVENTIONS THAT WORK
Interventions that begin in the first 2 years of life and continue over time have the potential to reduce childhood obesity, continued Taveras. In a review of interventions implemented in the first 2 years of life, the interventions that worked demonstrated an effect primarily by focusing on individual- or family-level behavior changes and in homes, clinical settings, or community-based settings. However, the effects of the interventions tended to be short term, suggesting that repeated interventions will be needed to sustain benefits over time.
Although there is limited study of interventions of children 2–5 years of age in the clinical setting, pediatricians have a number of advantages in reaching out to children and families, including access to children and parents or guardians and the ability to link families to information and community resources, noted Ian Paul, professor of pediatrics and public health sciences at the Pennsylvania State University College of Medicine, chief of the Division of Academic General Pediatrics, and vice chair of clinical affairs in the Department of Pediatrics at Penn State Hershey Children’s Hospital. To prevent and treat obesity, pediatricians can identify children at risk, educate families, shape the food and activity environment, and encourage self-monitoring in families. New models of care could give pediatricians more time with families and enable them to partner with other health care professionals to prevent or treat obesity in children 2–5 years of age.
Early care and education is another setting in which service providers can do more to prevent obesity in young children. The experiences children have in these settings can affect diet, physical activity, and general health outcomes, observed Dianne Ward, professor of nutrition at the University of North Carolina’s Gillings School of Global Public Health. The community context, organizational policies and practices, and interpersonal relationships with parents and care providers all can promote healthy eating and regular physical activity.
Finally, interventions in the home setting focused on healthy lifestyle behaviors (e.g., timing of introduction of solids, limiting sugar-sweetened beverages, repeated exposures to vegetables, parent diet, and physical activity modeling), parenting skills (e.g., responsive parenting, child emotion regulation), and broader family life (e.g., child school readiness, targeting child conduct disorder) can be effective in reducing BMI and have been particularly successful in working with low-income and racial and ethnic minority groups, said Kirsten Davison, associate professor of nutrition at the Harvard School of Public Health. However, as with many of the interventions discussed at the workshop, Davison stressed that results tend to be short term, and the interventions need to be reinforced in order to achieve sustained effects.
CROSS-SECTOR SOLUTIONS
The need for sustained, varied, and multifaceted interventions, involving partnerships across sectors, is evident in combating childhood obesity, noted Lisel Loy, director of the Nutrition and Physical Activity Initiative at the Bipartisan Policy Center. The workshop’s final panel examined comprehensive solutions to address childhood obesity.
The programs of the U.S. Department of Agriculture address food security and nutrition in a variety of ways, observed Kevin Concannon, the department’s undersecretary for Food, Nutrition, and Consumer Services. Programs such as the Special Supplemental Nutrition Program for Women, Infants, and Children; the Supplemental Nutrition Assistance Program; the Child and Adult Care Food Program; and the Dietary Guidelines for Americans approach the issues of obesity prevention in a variety of ways and through the involvement of a variety of partners, such as health care organizations and systems. Furthermore, these programs have the potential to do more, said Concannon, through partnerships with a wider range of state, local, and private-sector organizations.
New York City is an example of a locality that has taken decisive, multifaceted steps to address obesity, said Jeni
Clapp, director of healthy eating initiatives at the New York City Department of Health and Mental Hygiene. A range of initiatives that have focused on improving the environments in which people live, including interventions in stores, restaurants, marketing, schools, child care settings, and individual neighborhoods, has contributed to a plateauing or decline of obesity in recent years among New York City children, especially those at high risk for overweight or obesity.
The Nemours Children’s Health System is an example of a health care organization that has taken a multifaceted approach to obesity prevention and treatment, stated Allison Gertel-Rosenberg, director of national prevention and practice in the Nemours National Office of Policy and Prevention. It has sought to complement and expand the reach of clinicians using a community-based approach in which messages regarding healthy eating and physical activity extend across the lifecycle with consistent messaging from parents, early care and education providers, and physicians. In this way, the system serves as an integrator that works intentionally and systematically across sectors to improve health and well-being.
Finally, Terry Huang, professor at the City University of New York School of Public Health, offered three lessons that he has learned through his extensive cross-sectoral work on obesity prevention. First, building trust between partners takes time, resources, effort, and strategy, but it is essential for multisectoral approaches. Second, effective leadership makes it possible to leverage collaboration and competition, both of which are important in changing the outcomes of complex systems. Third, the goals of systems continually need to be reassessed and reset, which in turn will reveal new questions, new strategies, and new ways to understand and affect those systems.
CLOSING COMMENTS
The United States and other nations have reasons to fear the obesity epidemic, and especially its effects on children, said Bill Purcell,5 former mayor of Nashville, Tennessee, and chair of the Roundtable on Obesity Solutions in his closing remarks at the workshop. But the efforts of organizations to improve communication and foster cross-sector collaboration are a powerful countervailing force. All those who have authority over the lives of children have a clear responsibility. Said Purcell: “We leave this room understanding that charge and understanding that the future can and will be brighter.” ♦♦♦
______________
5 Currently of Farmer, Purcell, White, & Lassiter, PLLC.
Roundtable on Obesity Solutions
Bill Purcell III (Chair)
Farmer Purcell White & Lassiter, PLLC, Nashville, TN
Russell R. Pate (Vice Chair)
University of South Carolina, Columbia
Mary T. Story (Vice Chair)
Duke University, Durham, NC
Sharon Adams-Taylor
American Associaton of School Administrators, Alexandria, VA
Nelson G. Almeida
Kellogg Company, Battle Creek, MI
Jeanette Betancourt
Sesame Workshop, New York, NY
CAPT Heidi Michels Blanck
Centers for Disease Control and Prevention, Atlanta, GA
Don W. Bradley
Duke University, Durham, NC
Cedric X. Bryant
American Council on Exercise, San Diego, CA
Heidi F. Burke
Greater Rochester Health Foundation, Rochester, NY
Debbie I. Chang
Nemours, Newark, DE
Abbey Cofsky
Robert Wood Johnson Foundation, Princeton, NJ
Yvonne Cook
Highmark, Inc., Pittsburgh, PA
John Courtney
American Society for Nutrition, Bethesda, MD
Christina Economos
Tufts University, Boston, MA
Ihuoma Eneli
American Academy for Pediatrics, Columbus, OH
David D. Fukuzawa
The Kresge Foundation, Troy, MI
Lisa Gable
Healthy Weight Commitment Foundation, Washington, DC
Paul Grimwood
Nestlé USA, Glendale, CA
Marjorie Innocent
National Association for the Advancement of Colored People, Baltimore, MD
Scott I. Kahan
George Washington University, Washington, DC
Shiriki Kumanyika
University of Pennsylvania, Philadelphia
Catherine Kwik-Uribe
Mars, Inc., Germantown, MD
Theodore Kyle
The Obesity Society, Pittsburgh, PA
Alicia Lara
United Way Worldwide, Alexandria, VA
Matt Longjohn
YMCA of the USA, Chicago, IL
Lisel Loy
Bipartisan Policy Center, Washington, DC
Mary-Jo Makarchuk
Canadian Institutes of Health Research, Toronto, ON
Shellie Pfohl
President’s Council on Fitness, Sports, and Nutrition, Rockville, MD
Barbara Picower
The JPB Foundation, New York, NY
Nicolas P. Pronk
HealthPartners, Inc., Minneapolis, MN
Amelie G. Ramirez
Salud America!, San Antonio, TX
Olivia Roanhorse
Notah Begay III Foundation, Santa Ana Pueblo, NM
Sylvia Rowe
S.R. Strategy, LLC, Washington, DC
Jose (Pepe) M. Saavedra
Nestlé Nutrition, Switzerland
James F. Sallis
University of California, San Diego
Eduardo J. Sanchez
American Heart Association, Dallas, TX
Brian Smedley
National Collaboration for Health Equity, Washington, DC
Lawrence Soler
Partnership for a Healthier America, Washington, DC
Loel S. Solomon
Kaiser Permanente, Oakland, CA
Marion Standish
The California Endowment, Oakland, CA
Alison L. Steiber
Academy of Nutrition and Dietetics, Chicago, IL
Maha Tahiri
General Mills, Inc., Minneapolis, MN
Kathleen Tullie
Reebok, International, Canton, MA
Tish Van Dyke
Edelman, Washington, DC
Howell Wechsler
Alliance for a Healthier Generation, New York, NY
James R. Whitehead
American College of Sports Medicine, Indianapolis, IN
Tracy Wiedt
National League of Cities, Washington, DC
IOM Staff
Lynn Parker
Scholar
Leslie Sim
Senior Program Officer
Heather Del Valle Cook
Program Officer
Amanda Nguyen
Research Associate
Dara Shefska
Research Assistant
Renee Gethers
Senior Program Assistant
For additional information regarding the meeting, visit http://iom.nationalacademies.org/Activities/Nutrition/ObesitySolutions/2015-OCT-06.aspx.
DISCLAIMER: This Workshop in Brief has been prepared by Steve Olson as a factual summary of what occurred at the meeting. The statements made are those of the authors or individual meeting participants and do not necessarily represent the views of all meeting participants, the planning committee, or the National Academies.
PLANNING COMMITTEE FOR THE WORKSHOP ON OBESITY IN THE EARLY CHILDHOOD YEARS: EMERGING SCIENCE AND IMPLEMENTATION OF PROMISING SOLUTIONS* Mary T. Story (Chair), Duke University; Anne M. Dattilo, Nestlé Infant Nutrition; Allison Gertel-Rosenberg, Nemours; Jennifer MacDougall, Blue Cross and Blue Shield of North Carolina Foundation; Brent A. McBride, University of Illinois, Urbana-Champaign; Rafael Pérez-Escamilla, Yale University; Sonya Shin, Brigham and Women’s Hospital and Harvard Medical School; Elsie M. Taveras, Harvard Medical School, Harvard School of Public Health, and MassGeneral Hospital for Children; Dianne Ward, University of North Carolina, Chapel Hill
*Institute of Medicine planning committees are solely responsible for organizing the workshop, identifying topics, and choosing speakers. The responsibility for the published Workshop in Brief rests with the institution.
REVIEWERS: To ensure that it meets institutional standards for quality and objectivity, this Workshop in Brief was reviewed by Anne Dattilo, Nestlé Infant Nutrition, and Sonya Shin, Brigham and Women’s Hospital and Harvard Medical School. Chelsea Frakes, Institute of Medicine, served as the review coordinator.
SPONSORS: This workshop was partially supported by the Academy of Nutrition and Dietetics; Alliance for a Healthier Generation; American Academy of Pediatrics; American College of Sports Medicine; American Council on Exercise; American Heart Association; American Society for Nutrition; Bipartisan Policy Center; Blue Cross and Blue Shield of North Carolina; The California Endowment; ChildObesity180/Tufts University; Edelman; General Mills, Inc.; Greater Rochester Health Foundation; HealthPartners, Inc.; Healthy Weight Commitment Foundation; Highmark, Inc.; The JPB Foundation; Kaiser Permanente; Kellogg Company; The Kresge Foundation; Mars, Inc.; Nemours Foundation; Nestlé Nutrition, North America; Nestlé USA; The Obesity Society; Partnership for a Healthier America; Reebok, International; Robert Wood Johnson Foundation; Salud America!; and YMCA of the USA.
Copyright 2016 by the National Academy of Sciences.
All rights reserved.






