C
Interim Report, December 2005
At the first committee meeting, held on January 30, 2005, the Social Security Administration (SSA) asked the committee to focus its attention initially on tasks 8-10 of its charge (see Appendix B) and, if possible, to issue its findings and recommendations on those tasks as soon as possible. The committee agreed that it would address these issues in an interim letter report. However, the committee also made clear that, after completing all of its deliberations, it might refine those preliminary recommendations.
The committee issued its interim report, Improving the Social Security Disability Decision Process: Interim Report, on these three tasks on December 21, 2005. That interim report is included in this appendix. In the interim report, the committee made 13 recommendations with respect to SSA’s use of medical expertise in its disability decision-making process. Now that the committee has completed all of its deliberations, the committee adopts these recommendations as its final recommendations on these issues, subject to the following additional comments with respect to Recommendations 1-2 and 1-7 (addressing qualification requirements for physicians and psychologists who serve as medical consultants [MCs] for the state Disability Determination Services agencies and as medical experts [MEs] at administrative law judge hearings).
In recommendations 1-2 and 1-7, the committee recommended that SSA require that physicians and psychologists who serve as MCs and MEs be board certified. As the committee noted in the interim report, “board certification is rapidly becoming the standard credential for the practice of medicine or psychology.” The committee realizes that, although board cer-
tification has become the norm for physicians, relatively few psychologists are board certified. The committee therefore modified its recommendation to recommend that SSA continue the current requirements for psychologists participating as MCs or MEs but establish a long-term goal requiring that psychologists be board certified.
Improving the Social Security Disability Decision ProcessInterim Report
Committee on Improving the Disability Decision Process: SSA’s Listing of Impairments and Agency Access to Medical Expertise Medical Follow-Up Agency
INSTITUTE OF MEDICINE OF THE NATIONAL ACADEMIES
THE NATIONAL ACADEMIES PRESS
Washington, D.C.
www.nap.edu
THE NATIONAL ACADEMIES PRESS 500 Fifth Street, N.W. Washington, DC 20001
NOTICE: The project that is the subject of this report was approved by the Governing Board of the National Research Council, whose members are drawn from the councils of the National Academy of Sciences, the National Academy of Engineering, and the Institute of Medicine. The members of the committee responsible for the report were chosen for their special competences and with regard for appropriate balance.
This study was supported by Contract No. SS00-04-60083 between the National Academy of Sciences and Social Security Administration. Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the view of the organizations or agencies that provided support for this project.
Additional copies of this report are available from the National Academies Press, 500 Fifth Street, N.W., Lockbox 285, Washington, DC 20055; (800) 624-6242 or (202) 334-3313 (in the Washington metropolitan area); Internet, http://www.nap.edu.
For more information about the Institute of Medicine, visit the IOM home page at: www.iom.edu.
Copyright 2006 by the National Academy of Sciences. All rights reserved.
Printed in the United States of America.
The serpent has been a symbol of long life, healing, and knowledge among almost all cultures and religions since the beginning of recorded history. The serpent adopted as a logotype by the Institute of Medicine is a relief carving from ancient Greece, now held by the Staatliche Museen in Berlin.
THE NATIONAL ACADEMIES
Advisers to the Nation on Science, Engineering, and Medicine
The National Academy of Sciences is a private, nonprofit, self-perpetuating society of distinguished scholars engaged in scientific and engineering research, dedicated to the furtherance of science and technology and to their use for the general welfare. Upon the authority of the charter granted to it by the Congress in 1863, the Academy has a mandate that requires it to advise the federal government on scientific and technical matters. Dr. Ralph J. Cicerone is president of the National Academy of Sciences.
The National Academy of Engineering was established in 1964, under the charter of the National Academy of Sciences, as a parallel organization of outstanding engineers. It is autonomous in its administration and in the selection of its members, sharing with the National Academy of Sciences the responsibility for advising the federal government. The National Academy of Engineering also sponsors engineering programs aimed at meeting national needs, encourages education and research, and recognizes the superior achievements of engineers. Dr. Wm. A. Wulf is president of the National Academy of Engineering.
The Institute of Medicine was established in 1970 by the National Academy of Sciences to secure the services of eminent members of appropriate professions in the examination of policy matters pertaining to the health of the public. The Institute acts under the responsibility given to the National Academy of Sciences by its congressional charter to be an adviser to the federal government and, upon its own initiative, to identify issues of medical care, research, and education. Dr. Harvey V. Fineberg is president of the Institute of Medicine.
The National Research Council was organized by the National Academy of Sciences in 1916 to associate the broad community of science and technology with the Academy’s purposes of furthering knowledge and advising the federal government. Functioning in accordance with general policies determined by the Academy, the Council has become the principal operating agency of both the National Academy of Sciences and the National Academy of Engineering in providing services to the government, the public, and the scientific and engineering communities. The Council is administered jointly by both Academies and the Institute of Medicine. Dr. Ralph J. Cicerone and Dr. Wm. A. Wulf are chair and vice chair, respectively, of the National Research Council.
COMMITTEE ON IMPROVING THE DISABILITY DECISION PROCESS: SSA’S LISTING OF IMPAIRMENTS AND AGENCY ACCESS TO MEDICAL EXPERTISE
JOHN D. STOBO (Chair), President, University of Texas Medical Branch at Galveston, University of Texas
FRANK S. BLOCH (Vice Chair), Professor of Law, Vanderbilt University Law School, Nashville, TN
GUNNAR B.J. ANDERSSON, Professor and Chairman, Department of Orthopedic Surgery, Rush University Medical Center, Chicago, IL
RICHARD V. BURKHAUSER, Professor and Chairman, Department of Policy Analysis and Management, Cornell University, Ithaca, NY
DIANA D. CARDENAS, Professor and Chief, Department of Rehabilitation Medicine, University of Washington Medical Center, Seattle, WA (Dr. Cardenas became a professor at the University of Florida.)
SHEILA T. FITZGERALD, Associate Professor, Division of Occupational Health, School of Hygiene and Public Health, Johns Hopkins University School of Nursing, Baltimore, MD
ARTHUR GARSON, Dean, School of Medicine, Vice President, University of Virginia, Charlottesville, VA
KRISTOFER J. HAGGLUND, Associate Dean for Health Policy and Professor of Health Psychology, School of Health Professions, University of Missouri, Columbia, MO
ALLEN W. HEINEMANN, Professor, Department of Physical Medicine and Rehabilitation, Feinberg School of Medicine, Northwestern University, Director, Center for Rehabilitation Outcomes Research, Rehabilitation Institute of Chicago
RONALD LEOPOLD, Vice President, MetLife, Alpharetta, GA
LARRY G. MASSANARI, Former Acting Commissioner, Social Security Administration, Exton, PA
STEPHEN G. PAUKER, Professor, Tufts University School of Medicine, Vice Chairman for Clinical Affairs, Department of Medicine, Associate Physician-In-Chief, Tufts-New England Medical Center, Boston, MA
LINDA A. RANDOLPH, President and CEO, Developing Families Center, Inc., Washington, DC
BRIAN M. SCHULMAN, Private Practice in Occupational Psychiatry, Bethesda, MD
PETER W. THOMAS, Principal, Powers Pyles Sutter & Verville, PC, Washington, DC
CRAIG A. VELOZO, Professor and Associate Chair, Department of Occupational Therapy, College of Public Health and Health Professions, University of Florida; Research Health Scientist, Rehabilitation Outcomes Research Center, North Florida/South Georgia Veterans Health System
Project Staff
MICHAEL McGEARY, Study Director
MORGAN A. FORD, Program Officer
SUSAN R. McCUTCHEN, Research Associate
REINE Y. HOMAWOO, Senior Program Assistant
RICK ERDTMANN, Director, Medical Follow-up Agency
PAMELA RAMEY-McCRAY, Administrative Assistant
ANDREA COHEN, Financial Associate
DAVID K. BARNES, Consultant
Reviewers
This report has been reviewed in draft form by individuals chosen for their diverse perspectives and technical expertise, in accordance with procedures approved by the National Research Council’s Report Review Committee. The purpose of this independent review is to provide candid and critical comments that will assist the institution in making its published report as sound as possible and to ensure that the report meets institutional standards for objectivity, evidence, and responsiveness to the study charge. The review comments and draft manuscript remain confidential to protect the integrity of the deliberative process. We wish to thank the following individuals for their review of this report:
Veronica D. Feeg, George Mason University School of Nursing, Fairfax, VA
Claude Earl Fox, Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD
Linda P. Fried, Johns Hopkins University Center on Aging and Health, Baltimore, MD
Patricia M. Owens, Consultation in Health & Disability Programs, Brooklyn, NY
James M. Perrin, Massachusetts General Hospital, Boston, MA
Harold A. Pincus, University of Pittsburgh Medical Center, Pittsburgh, PA
Glenn S. Pransky, Liberty Mutual Research Institute for Safety, Hopkinton, MA
Stephen T. Wegener, Johns Hopkins University School of Medicine, Baltimore, MD
Although the reviewers listed above have provided many constructive comments and suggestions, they were not asked to endorse the conclusions or recommendations nor did they see the final draft of the report before its release. The review of this report was overseen by Joseph P. New-house, Harvard University, and Lee Goldman, University of California, San Francisco. Appointed by the National Research Council and Institute of Medicine, respectively, they were responsible for making certain that an independent examination of this report was carried out in accordance with institutional procedures and that all review comments were carefully considered. Responsibility for the final content of this report rests entirely with the authoring committee and the institution.
Preface
The Institute of Medicine (IOM) Committee on Improving the Disability Decision Process has been working since it first met in January 2005 to develop recommendations to the Social Security Administration (SSA) on how to improve the medical aspects of its disability determination process. By law, Social Security can only pay benefits to those unable to engage in substantial gainful activity because of a “medically determinable physical or mental impairment which can be expected to result in death or which has lasted or can be expected to last for a continuous period of not less than 12 months” (emphasis added). Medical and psychological expertise is critical both in developing the criteria for measuring the severity and functional impact of an impairment or impairments on an applicant’s ability to work and in applying the criteria to individual cases where the medical evidence does not clearly meet the criteria in the eyes of a nonmedical disability examiner.
The committee’s final report is due in 2006, but SSA asked the committee to focus first on the expertise issues and provide early recommendations on the qualifications of the medical and psychological experts involved in the disability decision process in a short interim report. SSA is currently in the process of revamping its disability decision process and, according to a Notice of Proposed Rulemaking (NPRM) published in the Federal Register in July 2005, plans to establish a national network of medical and psychological experts who meet qualification standards set by the Commissioner of Social Security. The NPRM did not specify the qualification standards but noted that they would be promulgated within six months of the effec-
tive date of the final rule and that the Commissioner would consider the advice of the IOM in setting the standards.
The committee is continuing to address the remaining tasks in its charge, which focus on the medical criteria for assessing if an applicant qualifies for disability benefits. In this phase of the study, the committee is assessing the overall effectiveness of the Listing of Impairments (Listings) in the disability decision process, especially the use of the Listings as a screening tool for determining disability based on medical considerations alone. The committee’s findings and recommendations concerning the screening criteria may have further implications for the expertise needed to apply the medical criteria. If so, the committee may have further recommendations about medical expertise in the final report.
In developing this interim report, the committee received input from many sources, in the form of presentations at meetings and written statements submitted for the record. Many others responded to requests for information from the committee staff. On behalf of the committee, I would like to thank those who provided information. At the first meeting on January 31-February 1, 2005, these included directors of three state Disability Determination Services (DDS) agencies—Andrew Marioni, Jr. (Delaware DDS); Tommy Warren (Alabama DDS); and Walter Roers (Minnesota DDS)—and four judges from the SSA Office of Hearings and Appeals— David B. Washington, Chief Administrative Law Judge (ALJ); Nancy Griswold, Chief ALJ, Region I, Boston; William Taylor, Executive Director, Office of Appellate Operations; and Robert Johnson, Appeals Council.
For the second meeting, in April 2005, the committee notified more than 100 organizations of the opportunity to make presentations or provide written statements at the meeting. The public forum part of the meeting was held in the Barbara Jordan Conference Center of the Kaiser Family Foundation, a very accessible facility provided for free by the Foundation. Presenters at the public forum were Eileen Sweeney, Center on Budget and Policy Priorities; Marty Ford, Disability Policy Collaboration of The Arc and United Cerebral Palsy; Ethel Zelenske, National Organization of Social Security Claimants’ Representatives; Andrew Marioni, Jr., National Council of Disability Determination Directors, and Director, Delaware Disability Determination Services; David Randolph, American Academy of Disability Evaluating Physicians; and James McCarthy, National Federation of the Blind. The National Association of Disability Examiners submitted a written statement.
At the second meeting, the committee also heard from panels of experts on training and certification requirements that might improve the level of medical expertise in the disability decision process. The panelists and their organizations were Robert Robertson, Shelia Drake, Beverly Crawford and Carol Dawn Petersen, Government Accountability Office; John
Pro, American Board of Independent Medical Examiners; Douglas Martin, American Academy of Disability Evaluation Physicians; Steve Geiringer, Wayne State University and American Academy of Physical Medicine and Rehabilitation; Elizabeth Genovese, American College of Occupational and Environmental Medicine; Sandra Hall, American Association of Occupational Health Nurses; Joanne Ebert, Association of Rehabilitation Nurses; Michael Borek, Medical Director, Delaware DDS; Joseph Aaron, Chief Medical Officer, New Jersey DDS; William Humphreys, former medical consultant, Virginia DDS; Barry Eigen, Office of Disability and Income Security Programs; Monte Hetland, Pediatric Medical Officer, Office of Medical Policy, SSA; George Jesien and Rhoda Schulzinger, Association of University Centers on Disabilities; Howard Goldman, University of Maryland School of Medicine; and Thomas Yates, Health and Disability Advocates, Chicago.
At its fourth and fifth meetings in August and October 2005, the committee heard from Christine Hartel, National Research Council (NRC); Susan Van Hemel, NRC; Kristin Johnson, Charles Sweet, and Katherine Edwards, Disability Evaluation Services, University of Massachusetts Medical School; Jo Anne Barnhart, Commissioner of Social Security; Patricia Owens, Consultation in Health and Disability Programs, Brooklyn, New York; and Ethan Balk, AHRQ Evidence-based Practice Center, Tufts-New England Medical Center.
I would like to thank the SSA officials who not only requested the study, made presentations and answered questions at committee meetings, and met with committee staff, but also contributed information, documents, and statistics and made available the directors and medical directors of state DDS agencies and administrative law judges in the Office of Hearings and Appeals who met with the committee (listed above). These officials are Jo Anne B. Barnhart, Commissioner of Social Security, who met with the committee on October 6, 2005, to describe her plans for improving the disability decision process and answer questions from committee members; Martin H. Gerry, Deputy Commissioner for Disability and Income Security Programs; Glenn Sklar, Associate Commissioner for Disability Programs; Pamela Mazerski, Associate Commissioner for Program Development and Research; and Nancy Schoenberg, Office of Disability Programs, the project officer for this study who greatly facilitated responses to the committee’s requests for information.
The staff would like to thank the following for providing information or other assistance: Bob L. Appleton, Office of Disability Programs, SSA; Barbara Barzansky, American Medical Association; Kathleen M. Bernett, American Board of Independent Medical Examiners; Howard Bradley, Office of Research, Evaluation and Statistics, SSA; Shari Bratt, National Association of Disability Examiners (NADE); Dean M. Burgess, American Association
of Occupational Health Nurses; Shanklin Cannon, Northwestern Mutual; Lenore Carlson, Office of Disability Determinations, SSA; Winthrop S. Cashdollar, America’s Health Insurance Plans; Joanne Castello, Office of Disability Programs, SSA; Thomas Charest, Jefferson Pilot Financial; Mary Chatel, Office of the Commissioner, SSA; Carol G. Cook, U.S. Office of Personnel Management; Deborah A. Cotter, American Psychological Association; Ann R. Cox, American Association of Occupational Health Nurses; Beverly Crawford, Government Accountability Office (GAO); Susan David, Office of Disability Programs, SSA; Laurence Desi, Office of Medical Policy, SSA; Anne Deutsch, Northwestern University; Terry Dodson, Office of Disability Programs, SSA; Shelia Drake, GAO; Dan Dougherty, Prudential Disability Management Services; Barry Eigen, Office of Disability Programs, SSA; Barry Eisenberg, Academy of Occupational and Environmental Medicine; Judith Feder, Georgetown University; Angela Foehl, American Psychiatric Association; Claire Green, Office of Hearings and Appeals (OHA), SSA; David Hatfield, OHA, SSA; Michael Heitz, OHA, SSA; Monte Hetland, Office of Medical Policy, SSA; Jay Himmelstein, University of Massachusetts Medical School; Deena Howell, Florida Retirement System; Sunmee Jo, OHA, SSA; Carol Jones, Office of Disability Programs, SSA; Patricia Jonas, Assistant Deputy Commissioner for Disability and Income Security Programs, SSA; Jim Julian, Office of Medical Policy, SSA; Karen Kadell, Minnesota State Retirement System; Cille Kennedy, Department of Health and Human Services; Theresa Klubertanz, NADE; Joseph LaDou, University of California Medical School-San Francisco; Susanne Lapierre, Liberty Mutual; Joni Lavery, National Academy of Social Insurance (NASI); Barry S. Levy, Tufts University; Cathy Lively, Office of Medical Policy, SSA; Jeffrey S. Lubbers, Washington College of Law, American University; Margaret Malone, Office of the Commissioner, SSA; Martha Marshall, NADE; Kathleen H. McGinley, National Association of Protection and Advocacy Systems; Paul Martin, Aetna Insurance Company; Jill F. Mocarski, Northwestern Mutual; Mark Nadel, Georgetown University; William E. Narrow, American Psychiatric Institute for Research and Education; Dorothy Nettles, Office of Disability Determinations; Paul Newacheck, University of California-San Francisco; Barbara Otto, Health & Disability Advocates, Chicago; Georgann Ozanich, Minnesota State Retirement System; Diane M. Pedulla, American Psychological Association; Carol Dawn Petersen, GAO; Clark Pickett, Office of Research, Evaluation and Statistics, SSA; Marquita Rand, Office of Medical Policy, SSA; Virginia Reno, NASI; Robert Rich, University of Illinois at Urbana-Champaign; Robert E. Robertson, GAO; John M. Rogers, The Hartford Life Insurance Companies; Gloria Barone Rosanio, CIGNA Disability Management Solutions; Jane Ross, NRC; Vince Sabatino, Office of Program Development and Research, SSA; Sandra Z. Salan, Office of Medical Policy, SSA; Stephen
Schmidt, Office of Workers’ Compensation Programs, U.S. Department of Labor; Frank Schuster, Office of Medical Policy, SSA; Art Spencer, Office of Disability Programs, SSA; Steven Sperka, Northwestern Mutual Life; Kaye Sullivan-McDevitt, UnumProvident Portland Disability Benefits Center; Lauren Swanson, CIGNA Disability Management Solutions; Patricia Thomas, MetLife Disability; Tiana Tozer, The Standard; Michael Weinrich, National Center for Medical Rehabilitation Research, National Institutes of Health; Mimi Wirtanen, NADE; Gooloo Wunderlich, NRC; Sandra Yost, American Academy of Disability Evaluating Physicians; and Barry Zevin, Tom Waddell Health Center, San Francisco Department of Public Health.
Finally, I would like to thank the staff members who have worked hard to help the committee organize its meetings and produce this interim report on a compressed time schedule. They are Michael McGeary, Study Director; Rick Erdtmann, Director, Medical Follow-up Agency; Morgan Ford, Program Officer (since October 2005); Susan McCutchen, Research Associate; Reine Homawoo, Senior Program Assistant; and David K. Barnes, Consultant.
John D. Stobo, M.D.
Chair
Figures and Tables
FIGURES
|
1 |
Processing time for disability claims in days, CY 2004, |
|||
|
2 |
Percentage of allowed claims by decision level, CY 2004, |
|||
|
3 |
Medical consultants by specialty, June 2004, |
|||
|
4 |
Comparison of MC specialty mix with initial case mix, |
|||
|
5 |
Medical experts by specialty, June 2005, |
|||
|
6 |
Number of different medical expert specialties, by region, June 2005, |
TABLES
|
1 |
Field Office Presumptive Disability Decisions, by Presumptive Disability Category, CY 2004, |
|||
|
2 |
DDS Presumptive Disability Decisions, by Impairment Code, CY 2004, |
|||
|
3 |
Approximate Costs of Presumptive Disability Cases Ultimately Disallowed, CY 2004 Data, |
|||
|
4 |
Approximate Costs of Adopting Different Allowance Rates to Determine Presumptive Disability Cases, CY 2004 Data, |
|||
|
5 |
Field Office Use of Presumptive Disability Categories for High-Allowance-Rate Impairments, CY 2004, |
ANNEX TABLES
|
1 |
DDS Medical Consultants by Specialty, June 2004, |
|||
|
2 |
Number of DDS Medical Consultants by Specialty and State, June 2004, |
|||
|
3 |
Case Mix Compared with Mix of Medical Consultant Specialties, |
|||
|
4 |
Number of Medical Experts by Specialty, June 2005, |
|||
|
5 |
Number of Medical Experts by Specialty and Federal Region, June 2005, |
|||
|
6 |
Impairment Codes of DDS Presumptive Disability Decisions with a Reversal Rate of Less Than 5 percent, CY 2004, |
|||
|
7 |
SSA Impairment Codes by Allowance Rate, from Highest to Lowest, CY 2004, |
Abbreviations and Acronyms
AAMRO American Association of Medical Review Officers
ABMS American Board of Medical Specialties
ABPP American Board of Professional Psychologists
ACUS Administrative Conference of the United States
AHC academic health center
ALJ administrative law judge
ALS amyotrophic lateral sclerosis
AMA American Medical Association
AME aviation medical examiners
AUCD Association of University Centers on Disabilities
CE consultative examination
CFR Code of Federal Regulations
CME continuing medical education
COPD chronic obstructive pulmonary disease
CPP/OAS Canada Pension Plan/Old Age Security
CPT Current Procedural Terminology, AMA
CY calendar year
DDS Disability Determination Services
DE disability examiner
DHHS U.S. Department of Health and Human Services
DOL U.S. Department of Labor
DOT U.S. Department of Transportation
Ed. Edition
eDib electronic disability process
ESRD end stage renal disease
FAA Federal Aviation Administration
FEU Federal Expert Unit
FY fiscal year
GAO Government Accountability Office
HIV human immunodeficiency virus
IME independent medical examination
IOM Institute of Medicine
MC medical consultant
M.D. doctor of medicine
ME medical expert
MRO medical review officers
NIH National Institutes of Health
NIOSH National Institute for Occupational Safety and Health
NPRM Notice of Proposed Rulemaking
OHA Office of Hearings and Appeals, SSA
OWCP Office of Workers’ Compensation Programs, DOL
PD presumptive disability
PER pre-effectuation review
Ph.D. doctor of philosophy
POMS DI Program Operations Manual System—Disability Insurance, SSA
Psy.D. doctor of psychology
QA quality assurance
QME Qualified Medical Examiner
RVU relative value unit
SDM single decision maker
SSA Social Security Administration
SSAB Social Security Advisory Board
Improving the Social Security Disability Decision Process
Interim Report
EXECUTIVE SUMMARY
Overview of Social Security Disability Programs
The Social Security Administration (SSA) provides Social Security Disability Insurance (SSDI) benefits to disabled persons of less than full retirement age and to their dependents. SSA also provides Supplemental Security Income (SSI) payments to disabled persons who are under age 65. For both programs, disability is defined as a “medically determinable physical or mental impairment” that prevents an individual from engaging in any substantial gainful activity and is expected to last at least 12 months or result in death.
As of December 2004, SSA was making disability payments to 10.8 million adults and children based on their own disability and 1.5 million dependents of disabled adults. In fiscal year (FY) 2005, SSA estimated it would process approximately 2.5 million initial claims for disability benefits, 25 percent more than in FY 2000.
Assuming that an applicant meets the nonmedical requirements for eligibility (e.g., quarters of covered employment for SSDI; income and asset limits for SSI), the file is sent to the Disability Determination Services (DDS) agency operated by the state in which he or she lives for a determination of medical eligibility. SSA reimburses the states for the full costs of the DDSs.
The DDSs apply a sequential decision process specified by SSA to make an initial decision whether a claim should be allowed or denied. If the claim is denied, the decision can be appealed through several levels of adminis-
trative and judicial review. On average, the DDSs allow 37 percent of the claims they adjudicate through the five-step process. A third of those denied decide to appeal, and three-quarters of the appeals result in allowances. Nearly 30 percent of the allowances made each year are made during the appeals process after an initial denial.
In 2003, the Commissioner of Social Security announced her intent to develop a “new approach” to disability determination. The goals of the new approach are to (1) make the correct decision as early in the claims process as possible and (2) foster return to work at all stages of the process.
IOM Study Charge
In late 2004, SSA asked the Institute of Medicine (IOM) to help in two areas related to its initiatives to improve the disability decision process.
-
Improvements in the criteria for determining the severity of impairments. Currently, SSA uses a Listing of Impairments (the Listings) to identify impairments and associated medical findings that are so severe that SSA can consider individuals with one of these impairments, or their equivalent in severity, to be disabled without additional evidence of their inability to work.
-
Improvements in the use of medical expertise in the disability decision process. Currently, each DDS has medical consultants on staff and a roster of outside medical sources it uses to conduct independent medical examinations, called consultative examinations, and each regional office of the Office of Hearings and Appeals has a roster of medical experts who have agreed to provide their opinions in cases being heard by administrative law judges. Other than state licensure, SSA does not have national qualification standards or training and certification requirements for any of these medical sources.
SSA’s request to IOM was broken down into 10 specific tasks. The first seven tasks pertain to the Listings, and the final three—tasks 8, 9, and 10—pertain to presumptive disability categories, organization of medical expertise, and training and certification of consultative examiners, respectively (see Annex). The last three tasks are addressed in this interim report.
In July 2005, SSA published a notice of proposed rulemaking (NPRM) that included establishment of a Federal Expert Unit that would set up and administer a national network of medical, psychological, and vocational experts to support the disability decision process at the initial decision point and subsequent levels of appeal. In the NPRM, SSA announced that it is looking to the IOM committee’s interim report for advice on the qualifications of the medical and psychological experts to be recruited for the national network.
The final report will address the remaining tasks, which pertain to the criteria and procedures of the disability decision process. It is possible that after further information gathering and analyses of the effectiveness of the disability decision process in identifying those who qualify for benefits and excluding those who do not, the committee may refine its recommendations concerning medical and psychological expertise in the final report.
It should be noted that, in this interim report, tasks 9 and 10 are presented before task 8. This is because, due to the NPRM, the recommendations on the qualification standards and training requirements for medical experts are of immediate importance while presumptive disability is not the subject of rulemaking at this time.
Constraints on the Disability Decision Process
The committee supports the primary goals of SSA’s new disability decision process—to make the right decision as early in the claim process as possible, and to improve the accuracy, consistency, and timeliness of disability decisions at all levels of the disability process. Because the agency has not adopted the final version of its new plan, it is too early to reach any conclusions about the new process itself. Nevertheless, the committee believes that several factors significantly limit SSA’s ability to make the correct decision early in the process and these factors contribute to error, inconsistency, and delay in decision making.
One factor is the lack of emphasis on developing a complete record at the beginning of the disability decision process, although fuller case development has been recommended in a number of reports. More complete case development at the front end of the process may not be essential for an accurate initial disability decision in every case, but overall it should reduce the impetus for appeals, reduce the number of reversals on appeal, and shorten the average length of time before reaching final adjudication. This is difficult to accomplish, however, because disability decision makers in the DDSs are subject to strong pressures from SSA to decide cases quickly and to reduce administrative costs (including medical costs) per case.
A second factor is a contrasting set of incentives for DDSs and administrative law judges, which has the effect of pushing decision outcomes in different directions at different levels of adjudication. By law, DDSs are subject to a “pre-effectuation” review by SSA regional offices of 50 percent of all decisions to allow claims in SSDI cases. Denials are not reviewed for correctness. SSA’s quality assurance system, which does look at denials as well as allowances after the fact, reviews only one percent of the cases. Although a third of the denials are appealed for review by an administrative law judge, and the majority of those appeals result in allowances, the costs of decisions reversed by the administrative law judges are not internal to the DDS. In
addition, there is no information feedback loop from the appeals process on the results of hearings, especially on the characteristics of cases allowed on appeal that were denied initially. In contrast, administrative law judges have incentives to allow claims. The chances of having an allowance decision subsequently reviewed are very small, while more than half of all denial decisions are appealed to the Appeals Council, the next level of review.
The new disability plan recently set forth by the Commissioner describes SSA’s intent to “create and operate a comprehensive and multidimensional approach to quality assurance” in order to improve quality and accountability throughout the disability process. The committee agrees that fundamental change is needed in the SSA quality review process to place equal emphasis on allowances and denials. The committee plans to address the role of balanced incentive systems in its final report.
Organization of Medical Expertise
Task 9: “Advise on how best to provide medical expertise needed to support the entire disability adjudication process. This will involve describing the type of experts needed (academic specialists; practicing specialists; practicing generalists or non-physicians); necessary credentials and where best to locate them (from university medical centers, centers of excellence for specialized care, or community practice settings).”
Claimants must have a medical basis for impairments disabling them from work to qualify for benefits. Accordingly, SSA relies on medical experts to provide medical evidence (including treating physicians and independent medical examiners), analyze the evidence, and determine if it justifies an allowance (the last two activities are performed by medical and psychological consultants in the DDSs).
DDSs collectively have more than 2,100 medical and psychological consultants (hereafter, MCs), most of them part-time contractors. In most DDSs, the MC works with a lay disability examiner to make the disability decision jointly.
The applicant’s own medical providers, called treating sources by SSA, are the primary source of medical evidence throughout the entire disability decision-making process. By regulation, DDSs must seek medical evidence and opinions from treating sources and, unless there are inconsistencies or ambiguities, give their evidence controlling weight.
Medical expertise is also provided by medical personnel who perform consultative examinations (CEs)—i.e., examinations and tests—on claimants at SSA’s request, when needed information is not available from existing medical records. Although the claimant’s own treating source is the
preferred CE provider, SSA usually uses providers that it recruits specifically to perform these examinations and tests.
For cases appealed for a hearing, administrative law judges may request the presence of a medical expert (ME) to serve as an expert witness at a hearing. MEs are private practitioners who agree to serve for a fee and are recruited by the regional offices of the Office of Hearings and Appeals (OHA).
SSA also has MCs in a federal DDS and in the regional offices, where they are involved in quality review and case consultation.
Specialization of Medical Consultants
At committee meetings, SSA staff raised concerns that not all DDSs have a full range of medical specialists among their MCs. The committee also heard from organizations representing the state DDS directors and the disability examiners and MCs that not all DDSs always have all the specialties desired. The committee also heard from administrative law judges that they are not always able to find certain specialists to serve as medical experts at hearings. According to DDSs and administrative law judges, the main reasons for lack of access to all specialties are inadequate compensation to attract higher-paid specialties and scarcity of specialists in rural areas and less populous regions of the country.
Recommendation 1-1. SSA should make arrangements to ensure that the state Disability Determination Services (DDS) agencies and the Office of Hearings and Appeals (OHA) have ready access to the full range of physician specialties and other health professionals needed to evaluate cases. These experts should be available to consult with adjudicators in the DDSs and OHA on the development and evaluation of medical and functional information needed to reach a decision.
There are several possible arrangements for ensuring DDSs access to specialists, including the establishment of a national network of experts coordinated by a Federal Expert Unit (FEU), as proposed by the July 2005 NPRM. An FEU organized as a decentralized network of medical, psychological and vocational experts could play several roles. First, network experts could serve as consultants to adjudicators at the DDSs and OHA, similar to what MEs do for OHA currently, which would provide adjudicators with access to expertise that is not otherwise available. Second, network experts could serve as MCs in the adjudication process and make the disability determination in conjunction with the disability examiner. Third, network experts could perform CEs (this is not proposed in the NPRM).
However, establishing a national network of experts who would play different roles at different points in the process (e.g., acting as agency adju-
dicators in initial decisions and providing expert opinions to administrative law judges in de novo proceedings) will require arrangements that ensure that the same medical expert does not serve as adjudicator and expert witness in the same case. Likewise, if members of the network perform CEs, they should be instructed to be impartial and not be permitted to serve in other roles in the same case.
Qualifications of Medical Consultants
Currently, DDSs rely on state licensure or, in the case of psychologists and speech-language pathologists, certain alternative qualification requirements, to ensure a minimum level of medical expertise and competence among MCs. MCs are not required to be board certified, possess any additional credentials, or have an active practice in patient care.
Board certification is rapidly becoming the standard credential for the practice of medicine and psychology. Certification also has the benefit of requiring periodic recertification to demonstrate continued competence.
Recommendation 1-2. SSA should make board certification of physicians and psychologists* mandatory. This will necessitate an increase in compensation in order to recruit and retain qualified physicians and psychologists as MCs and MEs or as members of the national network of experts, if it is established. SSA also should allow current MCs with qualified program experience who are not board certified to continue for a time period of five years.
The committee recognizes that requiring a higher level of qualification (i.e., board certification) may affect SSA’s ability to attract and retain experts. Historically, SSA has had difficulty recruiting qualified experts given the nature of the work and comparatively low reimbursement rates. Therefore, if SSA is to attract enough candidates, a requirement for higher qualifications must be accompanied by increased compensation.
Training of Medical Consultants
Board certification represents mastery of a specific body of knowledge and continuing education, but the certification process alone does not en-
sure that an individual is qualified to provide expertise in SSA’s disability programs. Currently, SSA has no standardized national training program for MCs, to ensure a reliable level of knowledge and promote consistency in decision making, although it has been working on an MC training program for several years.
Recommendation 1-3. SSA should continue to develop and implement a mandatory national training program for all MCs, including those in the national network of experts outside the DDSs. The training program should focus on how to evaluate disability and on Social Security disability policies and procedures, be competency-based, and be coupled with ongoing assessment of MC competency as part of the quality assurance process.
The training program should concentrate on the aspects of the MC role that are not usually learned in medical school or residency programs, namely, evaluation of work disability and Social Security disability program policies and procedures. The training should be ongoing, it should be competency based, and SSA should perform an ongoing assessment of MC competency as a component of its revised quality assurance program.
Better Use of Medical Expertise
Many of the Listings have a substantial functional component and at least half the adult claims are decided on the basis of the interaction of medical and vocational factors, not on severity of impairment alone. Under current procedures, MCs must be physicians, psychologists, or other “acceptable medical sources” (i.e., podiatrists, optometrists, speech-language therapists). This policy has the effect of excluding from DDSs many medical personnel who could contribute to the disability decision-making process, including personnel trained to evaluate functional limitations and their impact on ability to work (e.g., nurse practitioners, occupational therapists, physical therapists, registered nurses, psychiatric social workers).
Recommendation 1-4. SSA should expand the range of expertise available in DDSs and implement alternative methods of developing and adjudicating cases within DDSs that would make more efficient and effective use of existing sources of expertise, and SSA should require these additional types of experts to undergo the same training as MCs.
For example, DDSs could use registered nurses who are certified as nurse practitioners or case managers to help triage cases, advise disability
examiners on what is needed to complete development of the medical record, and help decide when a case should be referred to a MC for review or to a specialist.
Other Sources of Medical Expertise
Using technology (e.g., electronic case files and video hearings) to make medical experts more widely available, establishing rigorous, standardized qualification requirements for all experts, and compensating experts at a level commensurate with their expertise will help to ensure that disability adjudicators have sufficient expertise to help them address complex medical issues in most cases. However, there will still be circumstances in which SSA needs more specialized expertise than the network of experts may have. Examples include more complex or rare cases, newly developing conditions (e.g., emerging infectious diseases), or conditions for which research is rapidly changing the state of the art in clinical practice.
Recommendation 1-5. SSA should consider developing formal working relationships with specialized clinical research centers to review and evaluate the medical record in difficult cases, provide feedback on how well SSA is evaluating certain disabling conditions, and identify improvements that should be made in evaluation criteria (including the Listings) and procedures.
SSA should consider developing demonstration projects with academic clinical research centers that focus on conditions that are difficult to evaluate, similar to the demonstration project that SSA currently has with the Association of University Centers on Disabilities, even though few medical experts in academic research centers will be familiar with the SSA disability program or with evaluating the work capacities and limitations of patients. The centers would nevertheless be an excellent source of medical expertise in reviewing complex cases, a means of learning how to improve adjudicative evaluation and decision making and improving the training of disability examiners, MCs, and administrative law judges, and an input to the revision and updating of the Listings.
Involvement of Treating Physicians and Other Treating Sources
Greater participation by treating sources is an excellent means of obtaining all the relevant medical and functional information early in the disability decision process, which speeds the process, leads to more informed decisions, and saves the costs of going back to the treating physician for additional information or of having to order a CE.
Recommendation 1-6. SSA should take steps to improve the flow of medical information from treating sources, especially by asking for the specific information wanted, making it easier to furnish the information, and reimbursing for the full cost of collecting the information and for producing and transmitting the report.
Efforts should focus on making treating sources more knowledgeable about SSA rules and procedures and what is expected of them, providing protocols and forms that elicit and organize relevant information, making it easier technologically for treating sources to provide the information, and compensating them adequately for the extra practice expenses involved in providing records and a useful report.
Current rates of compensation for providing records and preparing reports significantly affect both treating source participation and report quality. Rates are generally low relative to fees paid by other disability benefit agencies, which discourages the participation of treating sources.
Qualifications of OHA Medical Experts
MEs function as independent expert witnesses in a quasi-judicial process. They have no direct adjudicative function, and they do not examine the claimant. They use their medical expertise at hearings to help the administrative law judges and other participants understand complex medical issues of the case in layman’s terms. SSA has not required specific qualification standards for MEs.
Recommendation 1-7. Medical experts (MEs) used by administrative law judges should be board certified if they are physicians or psychologists.* SSA should encourage the use of licensed medical personnel other than physicians or psychologists as MEs in appropriate cases. All MEs should be adequately compensated for the time and effort required to serve in this capacity.
Regardless of whether MEs are drawn from existing rosters, or some newly established network as is proposed in the July 2005 NPRM, SSA should establish consistent national qualification standards for MEs to ensure a level of uniformity across the country. As discussed earlier, board
certification is fast becoming the standard credential for the practice of medicine and psychology.
The fee schedule for ME services is low compared with fees paid for expert witnesses by other programs and has not been increased for some time. More adequate compensation will help increase the participation of MEs from higher-paid specialties and specialties with relatively few members.
Training and Certification of Consultative Examiners
Task 10: “Recommend needs for standardized training and certification for consultative examiners who assess claimant’s level of function based on integrated evaluation of medical impairment and functional capacity. Advise on content of a training curriculum, appropriate personnel to train, and mechanisms for the certification process.”
DDSs purchase CEs to obtain or clarify information that is missing, conflicting, or ambiguous in a claimant’s medical records. CE providers are asked to report examination and test results, a diagnosis and prognosis, and an opinion on what the claimant can do despite his or her impairment or impairments.
Each DDS is charged with recruiting and orienting medical personnel who agree to be available to perform CEs in return for a fee set by each state. CE providers are not required to be what SSA defines to be an “acceptable medical source,” if a medically determinable impairment is established and the issue at hand is the severity of the impairment and how it affects an individual’s functioning. CE providers may be what SSA calls “other sources,” who may be other medical practitioners such as nurse-practitioners, physical therapists, occupational therapists, chiropractors, and audiologists, or nonmedical sources such as teachers, day care providers, social workers, and employers.
Training and Certification Requirements for Consultative Examiners
SSA requirements for CE providers are minimal. They must be currently licensed to practice medicine in the state and have the training and experience to perform the type of examination or test being requested. They are not required to have training or certification specifically in the evaluation of disability.
Currently, each state makes its own arrangements for orienting and training CE providers. SSA furnishes CE providers with a guide, known as the Green Book, which provides general information about the Social Security disability programs and how claims are adjudicated, including the
role of CEs, how CE providers are selected, and what the DDSs look for in a report of a CE.
Recommendation 2-1. SSA should establish reasonable requirements for training and certification of consultative examination providers. The training and certification should focus on two competencies: evaluation of limitations on ability to work resulting from impairments, and evidentiary and other requirements of SSA’s disability decision-making process.
The ability to diagnose and treat diseases and injuries is fulfilled by the current requirement that CE providers be licensed or certified in their area of expertise. However, licensure and board certification do not necessarily ensure that CE providers are expert in evaluating how a person’s impairment limits his or her functioning in employment settings or that providers know how to provide medical evidence in a form useful for evaluating whether someone meets Social Security’s definition of disability. Accordingly, CE providers should be required to demonstrate competence in these subject areas, namely, functional assessment of disability and SSA disability program policies and procedures.
Adequate Reimbursement for CE Providers
A comprehensive disability examination entails much more than a standard medical examination. The clinician must assess the nature and severity of the impairment or impairments by reviewing medical records, taking a history, performing an examination, and if needed, administering a diagnostic test or tests, and then he or she must evaluate the functional consequences of the impairment or combination of impairments, determine what the claimant’s capabilities are to work (in adults) or engage in age-appropriate activities (in children), and prepare a report that helps the DDS determine the nature, severity, and duration of the impairment and the claimant’s residual functional capacity (or, in SSI children, functional limitations).
The median fee that DDSs pay for an examination and report is approximately $130. Few pay more than $165. These fees are quite low compared with the fees that other disability benefit programs pay for disability evaluations and reports, including the federal and state workers’ compensation programs and private disability insurers.
Recommendation 2-2. Reimbursement should be adequate to cover the full costs of a consultative examination, which involves more than a standard examination, whether it is focused or comprehensive in scope. This will require a substantial increase in fees over the amounts cur-
rently paid in most states. There also should be adequate compensation for time spent in orientation and training activities.
SSA should conduct market studies and studies of fees that other public programs pay for similar services to determine a national fee schedule for CEs, adjusted for geographic differences in practice costs, with several fee levels depending on how focused or comprehensive the examination is. The fee schedule should be updated annually.
Higher fees should increase the pool of medical sources willing to perform CEs, especially in harder-to-recruit specialties such as orthopedics. It should also provide the incentive for more treating physicians to be willing to perform CEs.
Requests for CEs Focused on What Is Needed in Each Case
Improving the quality of CEs depends not only on the skill and knowledge of the CE providers but also on whether they have been asked for the right information.
Recommendation 2-3. SSA should ensure that requests for consultative examinations indicate clearly what is needed in each case rather than making general requests for records and opinions.
SSA could develop templates for CE request letters for common types of cases that can be easily individualized. In addition to a checklist of standard items to consider, each request letter should contain a narrative paragraph to provide further guidance to the CE provider that describes what the disability examiner is concerned about and thinks is needed to evaluate the claim in question.
Presumptive Disability Categories
Task 8: “Review SSA’s list of presumptive disability conditions and suggest revisions, additions, and/or deletions. The committee will recommend essential criteria for establishing candidate conditions for presumptive disability and recommend the level of professional expertise needed to certify that a presumptive diagnosis is adequately established.”
An applicant for SSI based on disability or blindness may receive up to six months of payments prior to the final determination of disability or blindness if he or she is determined to be “presumptively disabled” or
“presumptively blind” (hereafter presumptive disability) and meets all other (i.e., financial) eligibility requirements. SSA field offices can make presumptive disability determinations in cases involving certain impairments specified by SSA. DDSs can make presumptive disability findings in any case in which the available evidence indicates a “strong likelihood” that the claim will be allowed after going through the regular formal determination process.
Revising the Presumptive Disability Categories with Explicit Criteria
Presumptive disability is primarily a social policy which recognizes that applicants for SSI have little or no income or assets and probably need immediate assistance with the costs of living. Therefore, the committee is unable to recommend specific categories to include or delete because the selection criteria are not solely medical.
The nonmedical criterion in selecting presumptive disability categories is the degree of risk, i.e., the reversal rate because of false positives for which SSA is willing to pay in order to reach all true positives. Early in the SSI program, SSA determined that a reversal rate of more than 10 percent over several months made a category a candidate for deletion. Only 9 of the 15 current categories meet this criterion, however. A reversal rate of 20 percent or less would bring the total to 13. At the same time, the presumptive disability categories do not include conditions that consistently have high allowance rates, which therefore on equity grounds could be considered as candidates for inclusion as presumptive disability categories. In 2004, for example, cases with 1 of 12 primary impairment codes had a 90 percent chance of approval, and only 4 of those codes corresponded closely to existing presumptive disability categories.
Recommendation 3-1. SSA should consider dropping some current presumptive disability categories, and perhaps adding some, after deciding on explicit criteria for including categories.
Calculations based on SSA allowance rates by impairment category indicate that there are a number of conditions in which the probability is high that a claimant who alleges he or she has one of the conditions will end up being allowed, which makes them good candidates to be presumptive disability categories. The question the committee cannot answer is whether that probability should be 90, 85, 80 percent, or some other number. The answer depends on the trade-off society wishes to make between helping groups of low-income persons with a given probability of being determined disabled by SSA and the cost of paying for cases that end up being disallowed.
Increasing Consistency in Presumptive Disability Decision Making
The percentage of SSI claims that are granted presumptive disability status varies widely across SSA field offices and DDSs, a situation that SSA could improve. The percentage of field office presumptive disability cases ranges from 0.1 percent to 3.5 percent of SSI claims. The range for DDSs is from 0.6 percent to 34.6 percent. The majority of field offices do not use all 15 presumptive disability categories.
Recommendation 3-2. SSA should mandate the use of the presumptive disability procedure by, and take other administrative steps to achieve more consistency among, the SSA field offices and DDSs in the implementation of the presumptive disability policy.
Currently, the use of the presumptive disability procedure is voluntary, which leads to large differences in practice from office to office that are not just the result of inherent difficulties in assessing cases. If SSA has a presumptive disability process, and it is part of national social policy, it should be applied uniformly from place to place. This is primarily a matter for administrative policy to achieve.
Learning from Terminal Illness (TERI) Procedures
Presumptive disability is a policy to expedite payments. TERI (TERminal Illness) cases involve expedited decisions. According to the SSA program operations manual, “Cases where there is an indication of a terminal illness (TERI) are to be handled in an expeditious manner because of the sensitivity involved.”
Recommendation 3-3. SSA should look at TERI procedures for lessons in making expedited decisions on cases that must meet specific medical criteria. These include uniform special procedures throughout the decision process that promote consistency as well as speed.
TERI cases are subject to special procedures through which the case is expedited through every step of the disability determination process, including the appeals process and the payment process. The issue is whether field office interviewers are able to identify TERI cases with some accuracy. This would involve determining the percentage of cases flagged as TERI cases that turn out to meet the criteria and also the percentage of cases that were not flagged that should have been. Differences between types of cases and offices could be analyzed for better understanding of TERI decision making and ways to improve it.
INTRODUCTION
Overview of Social Security Disability Programs
The Social Security Administration (SSA) provides Social Security Disability Insurance (SSDI) benefits to disabled persons of less than full retirement age and to their dependents. SSA also provides Supplemental Security Income (SSI) payments to disabled persons who are under age 65. For both programs, adult disability is defined as a “medically determinable physical or mental impairment” that prevents an individual from engaging in any substantial gainful activity and is expected to last at least 12 months or result in death. Childhood disability under SSI is defined as a physical or mental condition or combination of conditions that causes “marked and severe functional limitations” and is expected to last at least 12 months or result in death. As of December 2004, SSA was making disability payments under the SSDI and SSI programs to 9.8 million people aged 18-64 and 1.0 million children based on their own disability, as well as payments to an additional 1.5 million dependents of disabled individuals in the SSDI program (SSA, 2005c:31-33).
SSDI and SSI disability account for 22 percent of SSA’s benefits payments each year (SSA, 2005a:147). Yet, they account for 57 percent of SSA’s administrative costs, because determining disability status is much more complicated than verifying a worker’s work records to compute Social Security retirement benefits (SSA, 2005a:161).
In fiscal year (FY) 2005 SSA expected to process approximately 2.5 million initial claims for disability benefits, 1.6 million continuing disability reviews, and 600,000 appeals hearings (SSA, 2004a:4-5). The annual number of claims, which was 2.1 million in FY 2000, is expected to continue to increase as baby boomers age into their 50s and early 60s and become more prone to disabling impairments.
Claimants file applications through one of 1,300 SSA field offices, over the telephone, by mail, or on the Internet. Interviewers in the field offices apply the nonmedical eligibility criteria to determine insured status and ask claimants to provide supporting medical documentation. The case files are then sent to a state Disability Determination Services (DDS) agency, which makes the initial decision as to whether the individual is disabled based on medical and, if needed, vocational criteria provided by SSA.
The DDSs use a five-step decision process, called the sequential evaluation process by SSA, for each claim for disability benefits, whether under SSDI or SSI.1 The first decision is whether the applicant is currently engaged in substantial gainful employment, which is defined as earning more than
a certain amount per month ($830 a month in 2005 except for statutorily blind beneficiaries).2 If yes, the application is denied. Step two is to determine whether the applicant has a medically determinable impairment that is severe, i.e., significantly limits the applicant’s physical or mental ability to engage in basic work activities, and that will last 12 months or longer. If no, the claim is denied. If yes, step 3 is a determination of whether the applicant’s impairment meets or equals one of the more than 100 conditions listed in a Listing of Impairments (Listings), which are assumed to be so severe that SSA accepts that the applicant cannot work. If yes, the claim is allowed. If not, step 4 involves an assessment of the applicant’s residual functional capacity to do past work. If yes, the claim is denied. If no, step 5 looks to see if the applicant can engage in any employment in the U.S. economy. If yes, the claim is denied. If no, it is allowed. On average, the DDSs allow approximately 37 percent of the claims they adjudicate through the five-step process.
The share of claims that are allowed at step 3 by meeting or equaling the Listings has declined over the years, to about half currently. This means that a growing percentage of cases must undergo intensive medical-vocational evaluation during steps 4 and 5, which require more time and DDS staff resources to perform.
Currently, approximately 70 percent of the allowances that are eventually made are made at the initial level, a process that takes about 97 days (SSA, 2004a:Appendix A). About a third (36 percent) of the applicants whose claims are initially denied decide to file an appeal. Of those, approximately 67 percent result in allowances at some point in the multistep appeals process, which averages more than a year to complete. Ultimately, slightly more than half of the claims (52.3 percent) are approved.3
On September 25, 2003, the Commissioner of Social Security told the Subcommittee on Social Security of the House Committee on Ways and Means of her intent to develop a “new approach” to disability determination (Barnhart, 2003). The goals of the new approach are to (1) make the correct decision as early in the claims process as possible and (2) foster return to work at all stages of the process. On July 27, 2005, after consulting with a variety of groups, SSA published a notice of proposed rulemaking (NPRM) describing specific regulatory changes it plans to make to implement the Commissioner’s new approach to the disability decision-making process (SSA, 2005e). Among the initiatives proposed in the NPRM was the establishment of a Federal Expert Unit that would set up and administer a national network of medical, psychological, and vocational experts to support the disability decision process at the initial decision point and
subsequent levels of appeal. The NPRM also proposes establishment of a Quick Disability Determination Process that would use a predictive statistical model to identify cases likely to be allowed and send them to a special unit to be adjudicated within 20 days. The NPRM includes other changes that are not addressed in this report.
IOM Study Charge
SSA asked the Institute of Medicine (IOM) to help in two areas related to its initiatives to make the disability determination process more efficient and accurate. First, SSA asked IOM to recommend improvements to the Listing of Impairments, which contains impairments and associated medical findings that SSA considers so severe that individuals with them (or with conditions equal to them in severity) are considered disabled without additional evidence of their inability to work. Among other things, the IOM will look at alternative conceptual models for organizing the Listings (currently based on 14 body systems), processes for determining when the Listings require revision, and the advisability of integrating functional assessment into the Listings.
Second, SSA asked IOM to recommend ways to improve the use of medical expertise in the disability determination process, including the appeals process. Subsequently, in the July 2005 NPRM, SSA announced it is looking to the IOM for advice on the qualifications of the medical and psychological experts to be recruited for the national network.
SSA’s requests to IOM are broken down into 10 specific tasks. The first seven pertain to the Listings, and the final three—tasks 8, 9, and 10—pertain to presumptive disability categories, organization of medical expertise, and training and certification of consultative examiners, respectively (see Annex). The last three tasks are addressed in this interim report.
It should be noted that tasks 9 and 10 are presented before task 8 because, due to the NPRM, the recommendations on the qualification standards for medical experts are higher priority than those on presumptive disability, which is not the subject of rulemaking at this time.
IOM Committee
The IOM formed a committee to conduct the study. The 16 committee members are experts in clinical decision making, physical medicine and rehabilitation, orthopedic surgery, occupational medicine and nursing, psychiatry and psychology, pediatrics, public health, functional assessment, occupational rehabilitation, legal and economic aspects of disability, social security disability administration, claimant advocacy, and private disability insurance. The committee expects to issue its final report in 2006.
The committee was asked by SSA to operate under certain assumptions:
-
The existence of a national electronic disability records system that allows claims folder documents to be transmitted electronically and viewed by all employees and medical personnel, regardless of their location;
-
The existence of a national video hearing capability;
-
An unchanged statutory definition of disability; and
-
That beneficiary return-to-work, vocational rehabilitation, and work incentives for applicants are outside of the scope of the committee’s deliberations.
Interim Committee Report
SSA asked the committee to prepare preliminary recommendations, prior to the final report, addressing the three tasks that relate to medical expertise issues, with a special focus on the appropriate qualifications of medical and psychological experts involved in disability decision making. Therefore, the committee agreed to issue this interim report, which provides the committee’s initial impressions on those tasks. This report, based on preliminary information gathering and analyses, and deliberations at the committee meetings, is in some respects an interim report. After further information gathering and analyses of the effectiveness of the disability decision process in identifying those who qualify for benefits and those who do not, the committee may refine its recommendations concerning medical and psychological expertise in the final report.
The final report will address a number of issues with potential implications for the qualifications of the medical experts involved in the disability decision process. These include the extent of knowledge about differences in decision outcomes depending on the qualifications of decision makers; research on inter-rater reliability of decision criteria; comparisons of evaluations of samples of cases by different groups of SSA adjudicators or by adjudicators compared with outside medical experts; results of long-term follow-ups of applicants who were allowed and denied; evaluations of alternative decision making models, such as the single decision maker model; studies of sources of variation in allowance rates among DDSs and Office of Hearings and Appeals (OHA) hearing offices; and in-depth analyses of program statistics about the outcomes of applications for benefits at different levels of decision making. The final report will summarize what is known about how well the disability determination process serves as a screening tool to avoid false positives and false negatives and the factors that affect its sensitivity and specificity, in epidemiologic terms.4 In the absence of such
information and analysis, this report is based mostly on the judgment of the committee of the qualifications, training, and certification that should be expected of medical participants in the disability decision process.
SSA’s Proposed Disability Decision Process Changes
SSA’s requests to IOM are closely related to the agency’s plans to institute a new approach to improve the SSDI and SSI disability process. For purposes of the medical expertise issues addressed in this interim report, the relevant aspect of the plan is the intent to establish a national network of medical and psychological consultants who would be used by all adjudicators, including disability examiners in the DDSs and administrative law judges (ALJs) in the OHA. In the July 2005 NPRM, SSA proposed establishing “a Federal Expert Unit to augment and strengthen medical and vocational expertise for disability adjudicators at all levels of the disability determination process,” and creating “a national network of medical, psychological, and vocational experts who will be available to assist adjudicators throughout the country” (SSA, 2005e:43593). SSA explained that:
… [U]nder our current disability adjudication process, medical, psychological, and vocational experts are not consistently available to all adjudicators at every level or in all parts of the country.
We are therefore proposing to establish and operate a Federal Expert Unit, which we believe will help to ensure the full development of the record, enable adjudicators to make accurate determinations or decisions as early in the process as possible, and facilitate subsequent review should a case be appealed to a higher level. We propose to create a national network of medical, psychological, and vocational experts who will be available to assist adjudicators throughout the country. This national network may include experts employed by or under contract with the State agencies; however, all experts affiliated with the national network must meet qualifications prescribed by the Commissioner.
The Federal Expert Unit will organize and maintain this network comprised of medical, psychological, and vocational experts who will provide medical, psychological, and vocational expertise to State agencies, reviewing officials, administrative law judges, and the Decision Review Board. We want to ensure that the right set of medical eyes reviews medical records and answers questions about the wide variety of impairments seen in disability claims. We believe that the expert network affiliated with the Federal Expert Unit will help ensure that a medical, psychological, and vocational expert who has the qualifications required by the Commissioner
assists in adjudicating disability claims. With the assistance of the Institute of Medicine, we plan to develop standards that define the medical and psychological expertise necessary for experts to qualify for participation in the national network (SSA, 2005e:43594).
In discussions with SSA staff, the committee was asked to assume that, under the new plan, there would be a national pool of medical experts and that there would be flexibility in payment rates for expert medical advice. The committee was not to assume that the experts would necessarily be centrally located.
The plan for achieving process improvements is also predicated on successful implementation of SSA’s electronic disability system (eDib), which is currently being rolled out nationwide. SSA expects all DDSs and OHA hearing offices to be processing their workloads with electronic disability folders on a regular basis by the end of 2006 (Barnhart, 2005). Although SSA refers to eDib as an electronic disability system, it is not a true electronic medical record, in which all information would be stored as structured data. In such a system, the data could be manipulated for purposes such as policy analysis or management information. SSA’s eDib system includes a mixture of structured data and images, with the medical evidence portion of the file consisting of images of paper medical records. This will make it possible for medical experts in remote locations to review medical records, assuming that arrangements to keep claimant files secure are made.
TRENDS IN THE DISABILITY DECISION PROCESS
The Social Security disability programs have grown rapidly in recent years, and several problems have come with this growth—problems that promise to become worse as the baby boomer generation reaches the age when disability becomes more likely (the oldest baby boomers will turn 60 in 2006). These problems, which have been documented in a number of reports,5 include:
-
significant growth in applications;
-
variability in decision making at each stage in the adjudication process;
-
high rate of appeals and of reversals of initial decisions to deny benefits; and
-
long length of time to reach a final decision.
Program Growth
Historically, both the SSDI and SSI disability programs have experienced steady, although not consistent, program growth. The causes for this growth and fluctuation are complex and not fully understood, and may include the broader socioeconomic and demographic environment as well as programmatic actions and court decisions (IOM, 2002:42). Even in the context of historical program growth, recent increases in application rates have had significant workload implications for SSA. According to SSA statistics, 1,041,362 workers applied for SSDI in 1998. The number of applications grew steadily to 1,485,482 in 2004, an increase of 42.6 percent in six years (Zayatz, 2005:Table 2). Applications have also increased in the SSI program. Applications by adults for SSI disability payments increased from 1,108,957 in 1998 to 1,438,992 in 2004 (29.8 percent increase), and applications for SSI childhood disability payments went from 335,732 in 1998 to 402,218 in 2004 (20.1 percent increase) (SSA, 2005b:Appendix C).6
Variability in Disability Decisions
As noted above, the initial disability allowance rate is approximately 37 percent. However, this rate varies significantly from DDS to DDS, and from region to region. In calendar year (CY) 2004, the initial allowance rate for individual states ranged from 25.3 percent to 61.1 percent. An SSA study of initial allowance rates in the late 1990s analyzed a similar spread of about 30 percentage points across DDSs. It found that statistically controlling for economic conditions, demographic factors, prevalence of SSDI and SSI beneficiaries, health status, and other external factors explained only half of the variance across the states (Strand, 2002). This finding suggests that up to half of the variance in allowance rates among the states may be due to differences in state administrative practices (e.g., use of consultative examinations, involvement of doctors in making disability decisions, payment amounts for medical evidence of record and consultative examinations, salaries and qualifications of disability decision makers, and training practices), quality assurance practices of state agencies and SSA regional offices, and/or state program policies (e.g., requiring individuals to file for SSA disability as a condition of eligibility for state benefits).7
Allowance rates at the ALJ hearing level also vary widely from state to state. In FY 2002, the overall hearing allowance rate was about 66 percent but, at the state level, the rate varied from 35 to 86 percent (SSAB, 2001b:70).
Appeals and Allowances on Appeal
About a third of the claims denied initially by the DDSs are appealed to the ALJ hearing level, after being denied at reconsideration level. By way of comparison, 8 percent of the claims for disability compensation from the Department of Veterans Affairs (VA) are appealed to the hearing level, even though VA, like SSA, allows less than half the claims initially.8 At UnumProvident, a provider of private long-term disability insurance, 10 to 15 percent of cases initially denied are appealed (Lewin, 2001:42). In Canada, approximately 20 percent of the disability applicants denied by the Canada Pension Plan appealed for a hearing in FY 2003.9
The appeal rate of one-third contributes to the lengthy average time it takes to make a final decision. Many applicants must wait an average of more than one year from the time they are denied by a DDS until an ALJ decides their case (see next section, below, on timeliness). There also are financial implications of the high rate of appeals. According to GAO, the average cost of processing an appeal hearing ($2,157 in 2001) is much greater than the average cost of processing an initial claim ($583 in 2001) (GAO, 2004:11).
The 1,200 ALJs who hold hearings on disability cases are employees of SSA, and although they operate separately from the DDS adjudicators, they are supposed to apply the same rules and regulations. Nevertheless, ALJs allow 61 percent of the claims that are appealed to them and deny or dismiss the rest. At the VA, 22 to 26 percent of the appeals are successful, 29 to 36 percent are remanded back for reconsideration, and 40 to 42 percent of the initial decisions are upheld (Lewin, 2001:42). At UnumProvident, 7 to 12 percent are reversed (Lewin, 2001:42). About half of the denials for disability benefits from the Canada Pension Plan are reversed (CPP/OAS, 2004:Figure 8). Possible reasons for the high allowance rates by ALJs in appeals cases include (SSAB, 2001b:5-6):
-
The fact that most claimants are never seen in person by an adjudicator until they have an ALJ hearing;
-
Rules that allow claimants to introduce new evidence and allegations at each stage of the appeals process;
-
The time lag between the initial denial and the hearing, during which a claimant’s condition may worsen;
-
Administrative differences between the DDSs and hearing office, including their access to and use of medical and vocational expertise;
-
Greater involvement of attorneys and other claimant representatives at the ALJ hearing, who help claimants assemble a more complete case record;
-
Differences in the quality assurance procedures applied to initial decisions and hearings-level decisions, which may bias DDS examiners to deny claims and ALJs to allow claims; and
-
Differences in the training given to ALJs and state DDS examiners.
Decision Timeliness
In FY 2004, average processing times for disability claims at each level of the decision process were (Figure 1):
-
95 days for initial disability claims;
-
97 days for reconsiderations;
-
394 days for hearings; and
-
251 days for decisions on appeals of hearings at the Appeals Council.
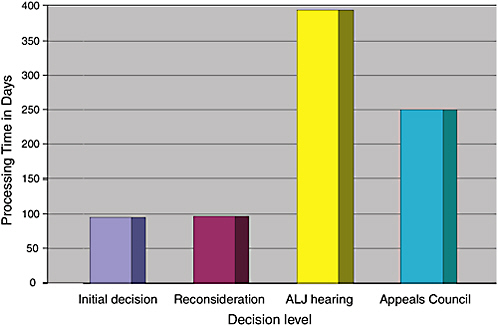
FIGURE 1 Processing time for disability claims in days, CY 2004.
SOURCE: SSA, 2005a:17.
Although the DDSs processed 2.6 million initial disability cases in FY 2004, the backlog was 625,000. ALJs issued 497,000 hearing decisions, but the number of pending hearing requests was 636,000 (SSA, 2005a:45-50).
Nevertheless, most of the disability allowance decisions in FY 2004 were made at the initial level of the decision process (Figure 2):
-
71.0 percent of the claims eventually allowed were allowed at the initial level;
-
6.2 percent of the claims eventually allowed were allowed at reconsideration;
-
22.6 percent of the claims eventually allowed were allowed at an ALJ hearing; and
-
0.2 percent of the claims eventually allowed were allowed at the Appeals Council.
Given that nearly a quarter of the claims were allowed after a hearing or an appeal of a hearing, the overall weighted average time until an allowance was made was 204 days. As noted above, appeals add substantially to the administrative costs of the program. Making the correct decision initially will require more resources at the front end of the disability
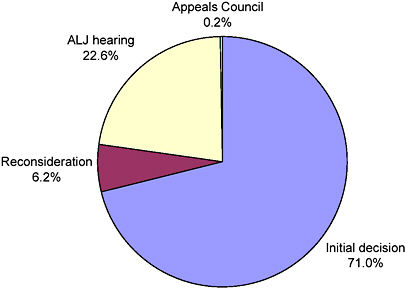
FIGURE 2 Percentage of allowed claims by decision level, CY 2004.
SOURCE: SSA, 2005d.
decision-making process, but these costs could be offset by savings from lower appeals rates.
Implications of Trends for the Interim Report
The increasing caseload makes it desirable to make the disability decision process as efficient as possible. One way to increase efficiency would be to find ways to make the Listings a more effective screening tool at step 3 of the sequential decision process, which will be addressed in the second phase of the study and the final report. A more effective screening tool could reduce the number of false negatives, i.e., cases that, although they meet the definition of social security disability, fail the screen and therefore have to undergo a more intensive and time-consuming medical-vocational analysis at steps 4 and 5 before they are allowed. The variability in allowance rates from DDS to DDS and between DDSs and OHA might be reduced if all had access to the same or equivalent expertise. If cases could be better evaluated and the medical record more fully developed at the beginning of the process, there might be fewer appeals and fewer allowances on appeal.
Equalizing access to medical expertise across decision-making units could help ameliorate the trends in case loads, processing time, appeal and reversal rates, and variability in decision making, but it is also justified on the grounds that every applicant for disability benefits should have the benefit of the expertise needed to evaluate their case regardless of where they live. Although it cannot be proven with available information, the committee finds it logical to expect that this will result in improved evaluations of complex cases, leading to more accurate decisions, which in turn will have beneficial effects by reducing the need for lengthy appeals and improving the case record for appeals that are filed. In the final report, the committee will analyze existing data and past research and identify research and experiments that SSA could sponsor to see what difference that different types and amounts of medical expertise make in decision outcomes.
The committee also notes in this interim report that several other factors are important in improving decision making. These include fuller development of cases before the initial decision and a quality assurance system with incentives that balance the need for making the right decision with the need for making decisions as quickly as possible.
CONSTRAINTS ON THE DISABILITY DECISION PROCESS
The committee supports the primary goals of SSA’s new disability plan—to make the right decision as early in the claim process as possible, and to improve the accuracy, consistency, and timeliness of disability decisions at all levels of the disability process. Because the agency has not
adopted the final version of its new plan, it is too early to reach any conclusions about the plan itself. Nevertheless, the committee believes that several factors significantly limit SSA’s ability to make the correct decision early in the process, and these factors contribute to error, inconsistency, and delay in decision making.
The development of a full record at the beginning of the disability decision process and evaluation of the record by appropriate experts, including medical experts, may not be essential for an accurate initial disability decision in every case. However, fuller case development at the front end of the process should reduce the impetus for appeals, reduce the number of allowances on appeal, and shorten the average length of time before reaching final adjudication. Full case development at the front end of the process has been recommended in a number of reports.10 This is difficult to accomplish, however, because disability claim-processing personnel, especially in DDSs, are subject to strong pressures to make decisions quickly and to reduce administrative costs (including medical costs) per case.
These time and cost pressures are reflected in SSA’s Performance and Accountability Report for FY 2004, wherein SSA identifies four strategic goals. The first goal is “To deliver high-quality, citizen-centered service.” Within each strategic goal, the report identifies specific strategic objectives. The first strategic objective under this first strategic goal is “To make the right decision in the disability process as early as possible.” To measure achievement in reaching this goal and this objective, SSA identifies six key performance indicators. Yet, despite the emphasis on high-quality service and making the right decision early in the process, none of these key performance indicators measures either the accuracy of the decisions or whether the decision was made as early in the process as possible. All six performance indicators focus on making decisions quickly and reducing the caseload (SSA, 2005a:45-51):
-
Number of initial claims processed by DDSs;
-
Number of SSA hearings processed;
-
Average processing time for initial disability claims;
-
Average processing time for hearings;
-
Number of initial claims pending; and
-
Number of hearings pending.
Within the context of these pressures to move cases quickly, DDSs and ALJs are also subject to a contrasting set of incentives that have the effect of pushing decision outcomes in different directions at different levels of adjudication.
In addition to tight time and resource constraints, DDSs are subject by law to a 50 percent “pre-effectuation” review by SSA regional offices of all decisions to allow claims in SSDI cases before payment is made. These factors create a disincentive to performing complete claim development because the chances of having a denial decision subsequently reviewed are slight. SSA’s quality assurance (QA) system reviews both SSDI and SSI cases, including allowances and denials, but the sample size is approximately 1 percent of the cases.11 About a third of the denials are appealed for review by an ALJ, but the costs of decisions reversed by the ALJ are not internal to the DDS. In addition, there is no information feedback loop from the appeals process on the results of hearings, especially on the characteristics of cases allowed on appeal that were denied initially.
In contrast, ALJs have incentives to allow claims. First, they are permitted to make use of several processing expedients that apply only to allowance cases (e.g., short-form decisions, “bench” decisions, on-the-record decisions). These make allowances easier and faster to process than denials, which require full development and a comprehensive written decision. Second, the chances of having an allowance decision subsequently reviewed are very small. On the other hand, more than half of all denial decisions are reviewed by the Appeals Council at the claimants’ requests.
The new disability plan recently set forth by the Commissioner describes SSA’s intent to “create and operate a comprehensive and multidimensional approach to quality assurance” in order to improve quality and accountability throughout the disability process. The committee agrees that fundamental change is needed in the SSA quality review process. An essential component of that change must be to promote not only quality and accountability, but consistency throughout the disability claims process. Another essential feature would be to place equal emphasis on allowances and denials. The committee will address the role of balanced incentive systems in improving the disability decision process in its final report.
ORGANIZATION OF MEDICAL EXPERTISE
Task 9: “Advise on how best to provide medical expertise needed to support the entire disability adjudication process. This will in-
volve describing the type of experts needed (academic specialists; practicing specialists; practicing generalists or non-physicians); necessary credentials and where best to locate them (from university medical centers, centers of excellence for specialized care, or community practice settings).”
Medical Expertise and the Disability Adjudication Process
Under the law, impairments cannot qualify a claimant for disability benefits unless they have a medical basis. SSA’s disability decision-making process relies on several types of medical expertise to provide medical evidence (including treating physicians and independent medical examiners), analyze the evidence, and determine if it justifies an allowance. Medical experts help to establish the medical basis of claimants’ impairments, evaluate whether they meet or equal the listings, and if not, evaluate the impact of the impairment or impairments on their functional capacity. For claim adjudication, there are four principal types of medical expertise, some internal and some external to SSA and the DDSs:
1.
Medical Consultants (MCs).
Initial disability decisions are made by personnel in state DDSs (as well as one federal DDS, operated by SSA). Every DDS has a complement of medical and psychological consultants (hereafter, MCs) who help determine whether claims meet SSA criteria. Currently, the DDSs collectively have more than 2,100 MCs, most of them part-time contractors. In most DDSs, the MC works with a trained layperson, called a disability examiner (DE), on a two-person team to make the disability decision jointly (unless there are nonmedical grounds for denial, such as a failure to undergo a consultative examination, which the DE can make alone). MCs also play an important role in assembling and interpreting the medical record that is the basis for a disability determination decision. By law, the MC must be a pediatrician (or other specialist appropriate to the child’s impairment) in child disability cases and a psychiatrist or psychologist in denials of mental disability cases. (In 10 states where SSA has been testing an alternative disability adjudication process, DEs can make the disability decision alone, unless it is a child or denial of a mental disability case.) In addition to reviewing cases, MCs may also perform other functions at a DDS, including training of DEs and other staff and developing and maintaining relationships with the medical community.
2.
Treating Medical Sources.
An applicant’s own medical providers, called treating sources by SSA, are the primary source of medical evidence throughout the entire disability
decision-making process. By regulation, DDSs must seek medical evidence and opinions from treating sources and, unless there are inconsistencies or ambiguities, give their evidence controlling weight. DDSs also must ask treating sources first to conduct a consultative examination, if one is needed, and if the treating sources meet SSA’s criteria for doing the examination.
3.
Consultative Examination (CE) Providers.
Medical expertise is also provided by medical personnel who perform examinations and tests on claimants at SSA’s request when needed information is not available from existing medical records. Although the claimant’s own treating source is the preferred source for a CE, SSA usually uses providers that it recruits specifically to perform these examinations and tests.
4.
Medical Experts (MEs).
For cases appealed to a hearing, medical expertise can come from MEs, who generally appear and testify as expert witnesses at hearings. They respond to questions from ALJs, who conduct the hearings and make the decisions, and from claimants (or their representatives). MEs are private practitioners who agree to serve for a fee. They are recruited by expert witness coordinators in the regional offices of the OHA. Currently, the regional offices have nearly 1,600 MEs on their rosters.
There are several additional sources of medical expertise for SSA, although they are not directly involved in claim adjudication:
-
Physicians and psychologists who assist in quality assurance review of claim adjudications. For cases reviewed in SSA central office, the physicians and psychologists are MCs in the federal DDS. In the regional offices, SSA relies on part-time MCs, who do not work in DDSs; and
-
Physicians, psychologists, and other medical personnel who are involved in policy development in SSA’s Office of Disability Programs.
Specialization of Medical Consultants
In meetings with the committee, SSA staff raised concerns that not all DDSs have a full range of medical specialists among their in-house MCs. They also referred to a major imbalance between alleged impairments and the areas of expertise of DDS MCs, citing, for example, a high percentage of claims involving musculoskeletal disorders, but relatively few DDS MCs who are orthopedic specialists. Most MCs are in generalist specialties such as internal medicine, pediatrics, and family medicine (35 percent) or in men-
tal health specialties (47 percent). SSA staff also expressed concern about state-to-state variation in the mix of different areas of medical expertise.
The committee also heard from organizations representing the state DDS directors and the DEs and MCs that not all DDSs had all the specialties desired.12 The main obstacles they reported were inadequate compensation to attract higher-paid specialties and lack of supply in certain regions of the country. Although the organizations testified that most cases can be adjudicated by generalists, they expressed support for arrangements enabling them to access hard-to-recruit specialists. The committee also heard from ALJs that they were not able to find certain specialists to serve as medical experts at hearings. The ALJs cited similar obstacles as DDS officials did: the low fees they can pay and the lack of certain specialists in rural areas.
Medical Consultants
In June 2004, the most prevalent specialties among medical consultants were (in descending order) psychology, internal medicine, psychiatry, pediatrics, and family practice. These five specialties account for three-quarters of the 2,136 MCs in the DDSs nationwide (Figure 3). Of these, the only specialty represented among MCs in all 52 DDSs was psychology.13
Other than 59 speech-language pathologists, no other specialty numbered more than 38 nationally. As a result, 29 DDSs had no MCs specializing in cardiology, 28 had no neurologists, and 25 had no orthopedic surgeons or orthopedic specialists. Ten DDSs had just one or two specialists other than the most prevalent five listed above. Another six only had three other kinds of specialists.
Each of the 10 regions had at least one cardiologist, neurologist, and orthopedist among its DDSs, however, and nine had at least one of the 25 ophthalmologist MCs in the country. Other scarcer specialties (and the number of regions with one or two DDSs that had them) were: endocrinology (4), gastroenterology (4), hematology (4), infectious disease (3), oncology (5), otolaryngology (2), pulmonology (6), and rheumatology (6) (Annex Table 2).
If each case had to be evaluated by a specialist in the alleged impairment, there would be a large mismatch between the mix of impairments among cases and the distribution of MCs among specialties. A recent analysis by SSA found, for example, that nearly 20 percent of decisions
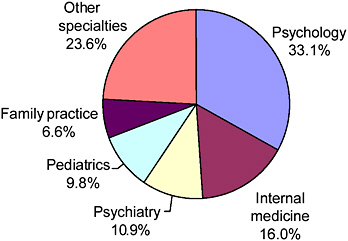
FIGURE 3 Medical consultants by specialty, June 2004.
NOTE: Each MC is classified by one primary specialty.
SOURCE: Annex Table 1.
involve musculoskeletal impairments while 2.5 percent of MCs are orthopedists (Figure 4). Nearly 4 percent of decisions are on cases involving the endocrine system, primarily diabetes mellitus, and 0.2 percent of MCs are endocrinologists. It is not known, however, how many of the decisions in these cases could have been handled by a more general specialist, such as an internist or family medicine physician, versus how many could have
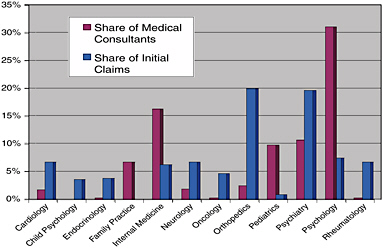
FIGURE 4 Comparison of MC specialty mix with initial case mix.
NOTE: Each MC is classified by one primary specialty.
SOURCE: Annex Table 3.
benefited from more specialized evaluation. These would be “close call” cases in which the claimant is on the boundary of “able to work” and “not able to work” or the medical evidence is complex and could be interpreted either way.
Medical Experts
In June 2005, the OHA regional offices had blanket purchase agreements with 1,575 MEs representing 1,861 specialties (some MEs were specialists in more than one field of medicine). Most of the physicians were board certified, although it is not a requirement. The most common specialties (in descending order) were clinical psychology, internal medicine, psychiatry, orthopedic surgery, and pediatrics, which accounted for two-thirds of the total (Figure 5). Physicians in these specialties were on the rosters of at least 9 of the 10 regions, along with neurology, cardiovascular diseases, ophthalmology, family practice, and rheumatology.
The number of different ME specialties varies by region (Figure 6). Some ALJs have access to a large number of specialties, for example, in the Atlanta region (41 specialties), Philadelphia region (36 specialties), and Chicago region (34 specialties). Others have access to few, such as the Denver region (12 specialties) and the Seattle region (17 specialties). Three regions lack access to MEs specializing in endocrinology (Dallas, Denver, Seattle), hematology (Atlanta, Dallas, Denver), gastroenterology (Dallas,
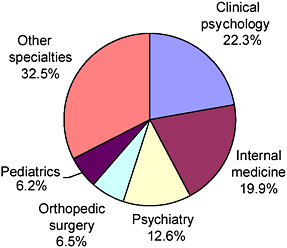
FIGURE 5 Medical experts by specialty, June 2005.
NOTE: This is the distribution of the 1,861 specialties; some MEs practice in more than one specialty and are counted more than once.
SOURCE: Annex Table 4.
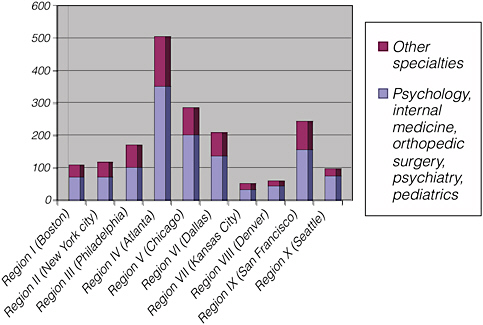
FIGURE 6 Number of different medical expert specialties, by region, June 2005.
NOTE: This is the distribution of specialist categories, not the number of MEs in each specialty.
Kansas City, and Denver), and physical medicine and rehabilitation (Boston, Denver, Seattle). For a number of specialties, there were only one or two MEs in each of a few regions. These included infectious diseases, immunology, podiatry, gynecology, speech-language therapists, and a number of pediatric subspecialties (e.g., pediatric neurology, endocrinology, allergy, and pulmonology).
DDSs need to have access to a full range of medical expertise, although the committee did not find a need for a close match between the distribution of impairments among applicants and the mix of specialties among MCs. Most people go to an internist, gynecologist, or pediatrician for medical care and are referred to more specialized experts when needed. Similarly, most private insurers take a stepped approach to medical expertise, in which only those cases needing more specialized knowledge and judgment are referred on by the claims examiners or case managers.14 Initial evaluations are often performed by a nurse, nurse practitioner, or in-house generalist physician, with relatively few cases needing to go to a specialist or subspecialist. The use of generalists to handle most situations and call on
specialists when needed allows for the most efficient use of costly specialist resources. It also helps ensure that the evaluation addresses the whole person, rather than focusing narrowly on one disorder. Such a model should also be effective for disability determinations in SSA, and it is quite similar to the way DDSs currently operate in relying on generalist specialists to evaluate the less complicated cases.
If the case record is fully developed, a trained DE should be able to make the disability determination in many cases without MC involvement, as currently occurs in SSA’s prototype process being tested in 10 states. In the prototype process, many decisions are made by DEs alone, i.e., as single decision makers (SDMs). The committee understands that SSA has evaluated the quality of SDM decisions as compared to team decisions, but the results of this evaluation were not available to the committee. Several sources told the committee that the results of the analysis showed that SDM decision quality was comparable to DE-MC team decision quality. In more complex cases, the DE could consult with a generalist MC, usually in a situation where face-to-face discussion is possible. However, only the most complex cases need to be evaluated by a specialist physician or multiple specialists. This is where the current DDS process can break down, because many DDSs have few, if any, MCs in certain specialty areas.
For cases requiring physician input, most MCs can be primary care physicians, such as internists, family practitioners, pediatricians, psychiatrists, and psychologists. These kinds of experts, who constitute three-quarters of the MCs at DDSs currently, are best equipped to handle the broad range of cases presented, including those with multiple impairments or co-morbid disorders. Additional specialist MCs, such as cardiologists, oncologists, endocrinologists, ophthalmologists, and rheumatologists, who would be appropriate for more complex cases, could be accessed through the national network if the DDS does not have an MC with the needed specialty.
Nevertheless, it is vital that all SSA adjudicators have a full range of medical expertise available. Currently, DDSs must rely on cumbersome and time-consuming ad hoc arrangements to have a case file reviewed by an MC in another state DDS, the federal DDS, the SSA regional or central office, or elsewhere, if the originating DDS does not have an MC with the appropriate expertise.
Recommendation 1-1. SSA should make arrangements to ensure that the state Disability Determination Services (DDS) agencies and the Office of Hearings and Appeals (OHA) have ready access to the full range of physician specialties and other health professionals needed to evaluate cases. These experts should be available to consult with adjudicators in the DDSs and OHA on the development and evaluation of medical and functional information needed to reach a decision.
Better availability of specialty expertise could be accomplished in several ways, which are not mutually exclusive, including:
-
formalizing and expanding the currently ad hoc cooperative arrangements among the DDSs to share experts;
-
having SSA hire or contract for the services of MCs in specialties that individual states find hard to recruit (or that are needed in low volume by any single state) and assign them to work in a few DDSs around the country but to serve all the DDSs in their region; and/or
-
having SSA establish federal regional units or national networks of medical experts in all specialties to whom complex cases could be referred for review and consultation and, perhaps, adjudication. SSA has already proposed this sort of arrangement in the Commissioner’s new disability plan (SSA, 2005e:43594-43595).
The Commissioner’s plan, as outlined in the NPRM published in the July 27, 2005 Federal Register, would establish a Federal Expert Unit (FEU). The FEU would create and maintain a national network of medical, psychological, and vocational experts15 who would be available to adjudicators through the entire disability decision process, including DEs in DDSs and the administrative judges in OHA.16 These experts would be recruited and paid by SSA at rates to be established by the Commissioner.17
The Commissioner evidently intends to recruit members of the national network of experts from practitioners in private practice, who would agree to review medical evidence in case files and either consult to MCs in the DDS and ALJs in OHA or participate as an MC in the disability determination decision, depending on the case. Assuming they are reimbursed at market rates, medical experts from specialties that DDSs and OHA have found hard to recruit would be more likely to participate and provide expertise that is not available currently. Medical and other experts could potentially be recruited from the academic health centers (AHCs). Many health profes-
sionals employed by AHCs are highly trained, salaried, and might have an interest in evaluating complex cases and earning additional income.
The July 2005 NPRM is not entirely clear on the role of the experts in the FEU network, in particular, whether they are consultants to adjudicators, including MCs in the DDSs, or are themselves MCs who participate in the adjudication decision, or both, depending on what is needed in each case. The NPRM says the experts “will be available to assist adjudicators throughout the country,” “provide medical, psychological, and vocational expertise to state agencies, reviewing officials, administrative law judges, and the Decision Review Board,” and “ensure that the right set of medical eyes reviews medical records and answers questions about the wide variety of impairments seen in disability claims.” In summary, the experts would be available to assist adjudicators by providing the medical, psychological, and vocational expertise they may need to help decide a case. This implies that the experts will act in a consulting role, advising adjudicators on what the evidence means in terms of severity and impact on function, especially in complex cases or rare conditions.
The consulting role appears to be similar to the role that MCs play in the prototype decision process being tested in 10 states, in which DEs may act as single decision makers or, if they deem it necessary to evaluate the medical evidence properly, involve an MC in the decision process. But the NPRM proposes to abolish the prototype process demonstrations. This would appear to restore the DE-MC team in the adjudication of every case nationally. If the national experts are meant to serve as consultants to adjudicators, they would be available to consult with these adjudication teams when the DDS does not have the appropriate specialist or specialists to evaluate a claim, similar to when a treating physician refers a case to a specialist for review and advice.18
At times, however, the NPRM indicates that the national experts would act as the MC in the initial decision cases whose files they are reviewing. For example, it says that the DDSs should continue to employ MCs but they would be required to meet the same qualification standards as the experts in the federal network “in order to participate in the disability adjudication process.”19 This implies that if the DDS MCs do not meet the qualifications to be part of the national network, they will not be able to act as MCs and presumably the adjudication role would be filled by non-DDS members of
the national network. The new regulatory language proposed in the NPRM says that if a DDS refers a claim to the FEU, a medical or psychological expert affiliated with the national network will evaluate the evidence to determine the medical severity of the impairment or impairments (proposed sec. 405.14). An advantage of having members of the national network act as MCs is that SSA could pay a rate high enough to attract experts in specialties that are typically paid more than internists, family doctors, and pediatricians and who DDSs find it difficult to recruit.
Members of the national network would clearly serve as consultants when acting as expert witnesses at ALJ hearings or reviewing medical records in cases before the Appeals Council (or before reviewing officials and the Decision Review Board, if they are implemented as proposed in the NPRM). In these situations, they would be providing opinion evidence requested by the adjudicator, as the MEs currently signed up the OHA regional offices do. There will be two advantages to using the national networks members as experts. First, the use of the same experts by the DDSs and OHA should increase consistency in decision making. Second, the hearing offices will have access to a greater range of specialties, especially if SSA pays the national network experts more than OHA does now. ALJs could also have medical records reviewed by anyone in the country rather than be restricted to the specialties that happen to be in the local area.
The NPRM does not address CEs, but the medical and psychological experts in the national network are obvious candidates to be CE providers, assuming that arrangements are made to ensure they act as independent evaluators when acting in the CE provider role. This topic is addressed more fully below in the discussion of Task 10.
In conclusion, an FEU organized as a decentralized network of medical, psychological and vocational experts could play several roles. First, network experts could serve as consultants to adjudicators at the DDSs and OHA, similar to what MEs do for OHA currently. In this role, they would review medical records and provide expert opinions about how to develop a case (what tests or examinations to look for or have done), interpret medical evidence (whether the diagnosis, findings, and symptoms are consistent with the severity of impairment), and provide opinions on functional limitations. This would provide adjudicators with access to expertise that is not otherwise available but that is needed to evaluate complex cases or rare diseases. A common pool of consultants with uniform training also should promote greater consistency in decision making. Network consultants could also improve the evaluation of functional capacity if membership were expanded to include additional health professionals (see “Better Use of Medical Expertise,” below).
Second, network experts could serve as MCs in the adjudication process and make the disability determination in conjunction with the DE. This
would be especially helpful in complex, difficult-to-evaluate cases requiring subspecialty expertise. There are some practical problems to overcome, however, when the DE and MC are in different locations. Communication will be an issue, as will be the resolution of conflicting opinions. Also, if the MC is highly specialized, multiple impairments or co-morbidities will require evaluation by additional experts and pose a problem of integrating the results into an overall assessment.
Third, network experts could perform CEs (this is not proposed in the NPRM).
Establishing a national network of experts who would play different roles at different points in the process (e.g., acting as agency adjudicators in initial decisions and providing expert opinions to ALJs in de novo proceedings) will require arrangements that ensure that the same medical expert does not serve as adjudicator and expert witness in the same case. Likewise, if members of the network perform CEs, they should be instructed to be impartial and not be permitted to serve in other roles in the same case.
Qualifications of Medical Consultants
Current qualification standards for MCs in SSA’s regulations require that MCs must be a:20
-
Licensed physician (medical or osteopathic doctor);
-
Licensed or certified psychologist who also meets other specific qualification standards;
-
Licensed optometrist;
-
Licensed podiatrist; or
-
Qualified speech-language pathologist.
MCs who are not physicians are limited to evaluating the specific impairments for which they are trained. Only physician MCs perform the full range of duties of an MC. Although referred to as MCs in this interim report, psychological consultants may only participate in cases involving the evaluation of mental impairments. Similarly, optometrists may only establish visual acuity and visual fields, podiatrists may only establish impairments of the foot and ankle, and speech-language pathologists may only establish speech and language impairments.
Currently, MCs are not required to be board certified, possess any additional credentials, or have an active practice in patient care.
Fully performing the MC role requires mastery of three domains of knowledge. First, MCs must be expert in their medical field (e.g., medicine,
psychology, speech-language pathology). Second, they need to understand how to evaluate disability. This is a skill not usually learned as part of standard medical education and training curriculum, which focuses on diagnosis and treatment.21 Disability evaluation, i.e., understanding how the functional limitations imposed by impairment affect ability to work, is a subject usually learned by taking additional courses or through on-the-job experience, preferably both. Third, MCs must be knowledgeable about Social Security policies and procedures for determining eligibility for disability benefits. (See “Training of Medical Consultants,” below, for additional discussion on this topic.)
Currently, DDSs rely on state licensure or, in the case of psychologists and speech-language pathologists, certain alternative qualification requirements, to ensure a minimum level of medical expertise and competence. DDSs also try to assign complex cases to MCs with more specialized expertise, although this is not required. It is also not always possible, because some specialties are not widely available. In June 2004, for example, there were 38 neurologists, 36 cardiologists, 25 ophthalmologists, and 18 orthopedic surgeons serving as MCs in DDSs nationally. Five states had none of these specialties represented among their MCs, and 25 states had between one and five.
Each DDS has a training program for its MCs to educate them on disability evaluation and Social Security program definitions and requirements. This typically includes working at first on easier cases with a more experienced MC and gradually taking on harder cases as experience is gained.
The committee finds the current qualification standards to be adequate for purposes of ensuring a minimum level of competence and qualification for speech-language pathologists, optometrists, and podiatrists. However, for physicians and psychologists, board certification is rapidly becoming the standard credential for the practice of medicine or psychology. Virtually everyone entering medical practice today is board certified. Currently, board certification is a common prerequisite for hospital privileges and other professional activities, such as participation in a provider network.
A number of studies have found a relationship between board certification of physicians and better outcomes, although other studies have not or had mixed results (Brennan et al., 2004). There is evidence that quality of physician performance (as measured by currency of knowledge, standards of practice, and patient outcomes) tends to decline with experience (as
measured by the number of years in practice or age).22 Certification boards have addressed the possibility of decline by requiring periodic recertification and are moving to a more continuous process of assessing competence (Steinbrook, 2005).
Recommendation 1-2. SSA should make board certification of physicians and psychologists* mandatory. This will necessitate an increase in compensation in order to recruit and retain qualified physicians and psychologists as MCs and MEs or as members of the national network of experts, if it is established. SSA also should allow current MCs with qualified program experience who are not board certified to continue for a time period of five years.
The basic training for a physician specialist includes four years of pre-medical education in a college or university, four years of medical school, and after receiving the M.D. degree, three to five years of residency (i.e., specialty training under supervision). After residency training, physicians are considered to be specialists and are board eligible. Approximately 30 percent elect to pursue additional training to become subspecialists. Training in a subspecialty can take another one to three years to complete. Certification boards generally require that a person seeking certification have an unrestricted state license to practice medicine to qualify to take the certification examination. Finally, a candidate for certification must pass a written and, in some cases, an oral examination. Most subspecialties require additional board exams qualifying the physician to be a board certified subspecialist. Subsequently, most boards require periodic recertification every six to 10 years, which involves continuing education, review of credentials, and further examination.
The basic training for a psychologist specialist includes a bachelor’s degree, four or more years of psychology graduate school and one year of clinical internship. After receiving the Ph.D. or Psy.D. degree, one to two additional postdoctoral fellowship years are required to be eligible for spe-
cialty certification. Additional years of clinical practice are often required to be eligible for board certification by the American Board of Professional Psychology. Board certification also requires psychologists to have an unrestricted state license to practice psychology and they must pass a written and an oral examination (ABPP, 2005).
The member boards of the American Board of Medical Specialties (ABMS) have issued more than 800,000 certificates in 36 specialties and 88 subspecialties. Approximately 30 percent were issued in the past 10 years (ABMS, 2005:Table 2). ABMS and the American Medical Association estimate that 89.2 percent of physicians with current licenses were board certified in 1999, up from 76.1 percent in 1989.23 The number certified in a subspecialty (e.g., cardiology, infectious diseases, rheumatology, child and adolescent psychiatry, pain medicine) is still small, however.
The committee recognizes that establishing a higher level of qualification (i.e., board certification) may affect SSA’s ability to attract and retain experts. SSA has historically had difficulty recruiting qualified experts given the nature of the work and comparatively low reimbursement rates. Establishing a firm requirement for higher qualifications must be accompanied by increased compensation rates if SSA is to attract enough candidates. A requirement for board certification that is not accompanied by compensation at the full market rate could have the paradoxical effect of decreasing the overall quality of the expert pool. On the one hand, it would exclude uncertified experts who are highly capable. On the other hand, it might attract only those who may be board certified but whose capabilities do not command market-rate fees.
The fact that compensation rates for current DDS MCs are set by the states may complicate the implementation of a uniform national payment system. However, given that the July 2005 NPRM indicates that SSA plans to pay DDS MCs in the national network the same as non-DDS MCs, the committee assumes that SSA has the ability to overcome this complication.
Of course, board certification only addresses physician/psychologist competence in a field of medicine (diagnosis, treatment practices, disease course). It does not ensure that they are skilled in evaluating disability or knowledgeable of Social Security disability program requirements, which is the basis for Recommendation 1-3, below. Experienced current MCs have these qualifications. Therefore, depending on the eventual structure of the medical expertise pool that is the subject of SSA’s current proposed rulemaking, SSA should establish a phase-in period or grandfathering provision for some individuals who are currently providing program medical expertise. For example, SSA could require all members of a newly organized
FEU to be board certified as of a certain date (e.g., implementation of the FEU), while still allowing current program physicians/psychologists who become members of an affiliated national network a period of five years to acquire the necessary qualifications. The committee recognizes that implementing a board certification requirement will pose practical problems but believes that it should be the standard for medical experts in SSA’s disability decision process.
In discussions with the committee, SSA staff also raised the issue of whether there should be a requirement that program physicians, psychologists, and others be currently (or recently) engaged in direct patient care. Although recognizing the advantages of current involvement in active patient care, the committee believes that such a requirement would exclude otherwise highly qualified and needed experts who do not (or no longer) engage in direct patient care for a variety of reasons, such as high malpractice insurance and other practice costs, engagement in research, and administrative duties.
Training of Medical Consultants
Board certification and recertification represent mastery of a specific body of knowledge and continuing education, but the certification process alone does not ensure that an individual is qualified to provide expertise in SSA’s disability programs. As noted above, disability evaluation expertise and program knowledge are also essential, and ongoing training is necessary to ensure competence.
Currently, SSA has no standardized national training program for MCs, which would ensure a reliable level of knowledge and promote consistency in decision making. Such a training course exists for DEs. It was developed in conjunction with the DDSs, and the DDSs are required to use it.
Many DDSs have their own programs for training MCs. A comprehensive, standardized MC training program should be based on the best of the current DDS training programs and developed with input from the DDSs. It should not only address SSA program rules, but also include a comprehensive component on disability assessment. The same program should be required for MCs in the Federal DDS and for those who review cases for PERs and QA in the regional offices.
Recommendation 1-3. SSA should continue to develop and implement a mandatory national training program for all MCs, including those in the national network of experts outside the DDSs. The training program should focus on how to evaluate disability and on Social Security disability policies and procedures, be competency-based, and
be coupled with ongoing assessment of MC competency as part of the quality assurance process.
SSA has been developing a standard training curriculum for MCs for the past several years. The curriculum was developed by a committee with representatives of the DDSs and SSA national and regional offices and is currently under review. The training program should be completed and implemented as soon as possible. It should concentrate on the aspects of the MC role that are not usually learned in medical school or residency programs, namely, evaluation of work disability and Social Security disability program policies and procedures. There also should be an ongoing training component. The training should be competency based, and SSA should perform an ongoing assessment of MC competency as a component of its revised quality assurance program.
Better Use of Medical Expertise
Under current procedures for the development and evaluation of disability claims MCs must be physicians, psychologists, or other “acceptable medical sources” (i.e., podiatrists, optometrists, speech-language therapists). This policy has the effect of excluding from DDSs many medical personnel who could support the disability decision-making process, for example, personnel trained to evaluate functional limitations and their impact on ability to work (e.g., nurse practitioners, occupational therapists, physical therapists, registered nurses, psychiatric social workers).24 Many of the Listings have a substantial functional component (e.g., mental and childhood Listings) and at least half the adult claims are decided on medical-vocational factors (i.e., an evaluation of the interaction between functional limitations and ability to work at steps 4 and 5 of the sequential evaluation process). Medical expertise in evaluating functioning is, therefore, vital to accurate claim adjudication. Currently, few if any DDSs make use of the wide range of medical expertise available beyond the currently acceptable medical sources that could both expedite case processing and improve the quality of the initial decisions.
Recommendation 1-4. SSA should expand the range of expertise available in DDSs and implement alternative methods of developing and adjudicating cases within DDSs that would make more efficient and effective use of existing sources of expertise, and SSA should require these additional types of experts to undergo the same training as MCs.
Expanding the range of expertise available in case adjudication would help DDSs implement the proposed “quick disability determination process” and make it more effective. The DDSs could triage cases more extensively, identifying not only the easy cases that can be expedited by the quick decision process, but also the hard cases that need more focused attention. In addition, it would allow DDSs to use interdisciplinary teams in appropriate cases.
For example, DDSs could use registered nurses certified as nurse practitioners or case managers to help triage cases, advise DEs on what is needed to complete development of the medical record, and help decide when a case should be referred to an MC for review and advice and/or referral to a specialist. SSA might also consider encouraging DDSs to employ nurses as DEs, as has been done in the New York DDS. If a quick decision process is developed, nurses could have the expertise, with physician backup, to identify suitable cases. This option is constrained, however, by a shortage of registered nurses in most states that is projected through at least 2020 (DHHS, 2002:Table 6).
A disability case evaluation process that makes use of a variety of expertise could look something like this:
-
Cases are initially handled by a triage unit staffed by trained personnel (similar to current DEs) who sort cases according to complexity and identify the specific expertise needed.
-
Cases are referred to one of several units, such as for:
-
Apparent simple allowances (e.g., presumptive disability, quick decision cases),
-
Uncomplicated cases that may be decided by a nonphysician professional (e.g., experienced DE, registered nurse),
-
Cases with complex medical issues requiring physician MC review,
-
Cases with complex functional issues requiring evaluation by a professional skilled in functional evaluation, or
-
Cases requiring an interdisciplinary team evaluation.
-
-
All these units have the ability to consult with experts in other units on an as-needed basis, or to transfer cases to another unit, as appropriate.
-
Expertise that is not available in the DDS (e.g., medical specialists and subspecialists) is made available via referral to:
-
Another DDS,
-
An MC in the national network, if it is established, or FEU, or
-
A specialized clinical center in a medical center (see Recommendation 1-5, below).
-
Other Sources of Medical Expertise
Using technology (such as electronic case files and video hearings) to make agency experts more widely available, establishing rigorous, standardized qualification requirements for all experts, and compensating experts at a level commensurate with their expertise will help to ensure that disability adjudicators have sufficient expertise to help them address complex medical issues in most cases. However, there will still be circumstances in which SSA needs more than a network of individual experts. Examples include more complex or rare cases or newly developing conditions (e.g., emerging infectious diseases). SSA would also benefit from having external resources that can help with program evaluation and provide analyses useful for policy development.
There are many specialized clinical research centers that focus on specific diseases and their functional consequences. The National Institute of Disability and Rehabilitation Research funds a number of specialized centers, including model programs in spinal cord injury, brain injury, and work rehabilitation, and research and training centers in a variety of disability areas. The National Institutes of Health (NIH) funds dozens of clinical research center programs, each with multiple centers (IOM, 2004). NIH-funded centers include Autoimmunity Centers of Excellence, Asthma and Allergic Diseases Centers, Comprehensive Sickle Cell Centers, Multidisciplinary Clinical Research Centers for Arthritis and Musculoskeletal and Skin Diseases, Alzheimer’s Disease Centers, Vision Research Centers, Diabetes Research and Training Centers, Autism Research Centers of Excellence, Parkinson’s Disease Research Centers of Excellence, Digestive Diseases Research Centers, a Rare Disease Clinical Research Network, and Specialized Centers of Research on various types of cancer and chronic heart and lung diseases, to name some. These centers are in academic medical centers across the country.
Recommendation 1-5. SSA should consider developing formal working relationships with specialized clinical research centers to review and evaluate the medical record in difficult cases, provide feedback on how well SSA is evaluating certain disabling conditions, and identify improvements that should be made in evaluation criteria (including the Listings) and procedures.
SSA should consider developing demonstration projects with academic clinical research centers that focus on conditions that are difficult to evaluate. Academic research centers focus on improving diagnosis and treatment and few medical experts in them will be familiar with the SSA disability
program or with evaluating the work capacities and limitations of patients. The centers would nevertheless be an excellent source of medical expertise in reviewing complex cases, a means of learning how to improve adjudicative evaluation and decision making and improving the training of DEs, MCs, and ALJs, and an input to the revision and updating of the Listings (policies and procedures for evaluating and updating the Listings will be addressed fully in the final report of this committee).
For example, SSA currently has a demonstration project with the Association of University Centers on Disabilities (AUCD) in which sets of SSI childhood cases with certain conditions (e.g., school-age children with mental retardation; children with low birth weight; adolescents with cognitive, psychiatric, or emotional impairments) are referred to AUCD centers for evaluation after they have been evaluated and a preliminary denial determination made by the DDS. This process has helped to improve the evaluation of children with mental conditions and problems with language development, and it has improved the process of gathering evidence of adaptive functioning. This project has made suggestions for improving the procedures and criteria for evaluating childhood disability, developed training for DEs, drafted national age-specific function forms, and produced an electronic database of appropriate assessment instruments for assessing children (e.g., instruments for measuring cognitive ability, adaptive behavior, speech and language skills, etc.). This arrangement is a model for similar arrangements in other areas of impairment. However, one significant limitation of the AUCD project was that it focused only on denial decisions. Any similar future projects need to look at examples of both allowances and denials.
Similar arrangements could be made with other research centers that focus on vocational rehabilitation or functional aspects of disability. This would be especially appropriate if SSA increases its efforts to return claimants to work by assessing their functional capacity earlier in the process.
Involvement of Treating Physicians and Other Treating Sources
Treating sources are an important component of SSA’s disability decision process. Under its rules, SSA develops evidence from a claimant’s own medical sources before evaluating evidence obtained on a consultative basis. It must give some deference to a treating source’s opinion and even “controlling weight” in cases where a treating source’s opinion is well supported by medically acceptable clinical and laboratory diagnostic techniques and is not inconsistent with the other substantial evidence in the case record. This deference to the treating source acknowledges that he or she has a longitudinal picture of the claimant from an on-going treatment relationship, which is desirable in documenting the severity and functional consequences of impairment or impairments.
In addition, it is SSA policy that, when a CE is required (e.g., because the evidence is incomplete or inconsistent), the treating source is the preferred source for the CE.
Despite the clear preference for treating source evidence in SSA’s rules, the committee heard testimony that treating physicians and psychologists and other medical sources who provide treatment to applicants are not used as sources of medical information as often or as well as they could be and that many treating sources who do respond to requests for medical evidence only provide copies of records, not their judgment of the patient’s functional capacities. The committee also learned that treating sources seldom perform consultative examinations, although SSA does not track this statistic. Greater participation by treating sources is an excellent means of obtaining all the relevant medical and functional information early in the disability decision process, which speeds the process, leads to more informed decisions, and saves the costs of going back to the treating physician for additional information or of having to order a CE.
Recommendation 1-6. SSA should take steps to improve the flow of medical information from treating sources, especially by asking for the specific information wanted, making it easier to furnish the information, and reimbursing for the full cost of collecting the information and for producing and transmitting the report.
Obtaining fuller and better medical evidence and opinions from treating providers, and obtaining it as early in the process as possible, would lead to more accurate and better substantiated decisions, making it possible for those who qualify for benefits to do so sooner. It would also reduce the need for costly, time-consuming, and sometimes poor quality consultative examinations.
Nevertheless, reliance on treating sources has limitations. Treating sources may unduly promote the interests of their patients, and SSA disability decision makers must take this into account in evaluating their opinions. This is why a treating source’s opinion must be well supported by the evidence. Some treating sources will be reluctant to provide more than the records, even if assured they are not making a decision affecting the wellbeing of a patient. They may fear that assessing the impairment or disability status of a patient seeking benefits may interfere with the clinician-patient relationship, especially if the patient is denied.25
Performing a proper disability evaluation or providing a complete report with a well-substantiated medical source opinion requires a great deal of time, often poorly remunerated. Evaluating patients with impairments for disability program eligibility takes more time, and therefore more practice expense, than most other types of patients (Lewin, 2005). Disability management and return-to-work issues are often present, and patients with severe impairments are often more psychologically stressed than other patients because of employment and financial concerns. In addition, clinical staff must spend additional time analyzing the medical history and records and completing a report.
Finally, treating sources may not have adequate training or experience in evaluating disability or understanding of SSA criteria and procedures to provide relevant information or opinions that squarely address DDS needs for decision making.
Ways to improve the amount and quality of input from treating sources can be identified through analysis of best practices in DDSs, which can be implemented more consistently throughout the country. Efforts should focus on making treating sources more knowledgeable about SSA rules and procedures and what is expected of them, providing protocols and forms that elicit and organize relevant information, making it easier technologically for treating sources to provide the information, and compensating them adequately for the extra practice expenses involved in providing records and a useful report. Obtaining sufficient information from treating sources at the initial level is the best way to improve the accuracy and timeliness of the decisions and to make the right decision as early in the process as possible. Examples of actions needed to be taken to improve the process include:
-
Providing higher compensation for the costs of providing records and preparing a proper report;
-
Providing materials—written, audio, and audiovisual—developed to communicate what is expected from treating sources with regard to patients who apply for social security disability benefits, similar to Understanding SSI Disability for Children, a booklet and video developed with the American Academy of Pediatrics as an educational tool for pediatricians who have patients with disabilities.26
|
26 |
The booklet and video were designed to be used for continuing education. Pediatricians who use them are eligible for up to two hours of American Medical Association Physician’s Recognition Award category 1 credit (www.pedialink.org/cme/_coursefinder/CMEdetail.cfm?aid=14720&area=liveCME). |
-
Making sure that the letters asking for medical evidence explain clearly what is needed and are specific enough that the treating physician responds with useful information;
-
Providing standard protocols or guidelines online for evaluating the most common conditions similar to the protocols developed by the SSA-AUCD Children’s SSI Project for assessing cognitive impairments, low birth weight, speech/language deficits, and other conditions in different age groups;
-
Developing standardized forms for reports that are formatted to elicit relevant information, like the Psychiatric Review Technique form (SSA-2506-BK), which was designed with the assistance of the American Psychiatric Association and other professional groups to improve the quality of evaluations of mental impairments (Pincus et al., 1991);
-
Emphasizing the need to obtain physicians’ statements about the functional aspects of the disability, in addition to the clinical information;
-
Providing standardized forms to gather information on functional limitations. Some hearing offices currently use this kind of form;
-
Making available free dictation services (as some DDSs already do) and web-based “smart” forms as well as traditional paper forms to fill out;
-
Providing flexibility for reporting physicians. For example, some physicians might prefer providing a narrative report while others may prefer checklists; and
-
Encouraging claimant participation in obtaining treating source cooperation.
Current reimbursement rates significantly affect both treating source participation and report quality. Reimbursement rates are generally low relative to market rates. For example, reimbursement for providing medical records is about $20. As will be discussed in the section on consultative examinations, below, reimbursement for performing a disability examination is also low, especially compared with comparable examinations performed for workers’ compensation and for private disability insurance carriers.27
Qualifications of OHA Medical Experts
At the hearing level of the disability claim process, ALJs are solely responsible for making the disability decision, including all medical, functional, and vocational aspects. MEs are not directly involved in the decision
making. However, they are called on to testify at hearings as expert witnesses or, occasionally, to respond to written interrogatories from ALJs.
MEs provide assessments of the medical evidence in response to specific questions from the ALJ. In FY 2001-2002, ALJs used MEs in 11 percent of cases, down from 14 percent of cases in FY 1999-2000. Judges conducting peer reviews of a sample of cases found that allowance decisions made in hearings with ME testimony were slightly better supported than those made in hearings without ME testimony (SSA, 2003:41-42).
To some extent, MEs serve a role similar to that of MCs at the initial decision step. However, there are significant differences. In most states, MCs function as decision makers (albeit on a team) and they are, for all practical purposes, employees of the DDS (even though technically most are contractors). MEs function as independent expert witnesses in a quasijudicial process. They have no direct adjudicative function, and they do not examine the claimant. They provide needed medical expertise to the proceedings to help the parties to the hearing understand complex medical issues in the case in layman’s terms. They may also be asked to provide an expert opinion on other issues, such as whether the claimant’s impairments meet or equal the severity of the Listings; the claimant’s ability to perform work-related activities; or expected impairment duration.
At the present time, SSA has not defined specific qualification standards for MEs, as it has for MCs. In addition, MEs receive no formal training from SSA, although they may receive basic program information. This is intended to ensure their independence and impartiality as expert witnesses.
Recommendation 1-7. Medical experts (MEs) used by ALJs should be board certified if they are physicians or psychologists. SSA should encourage the use of licensed medical personnel other than physicians or psychologists* as MEs in appropriate cases. All MEs should be adequately compensated for the time and effort required to serve in this capacity.
Regardless of whether MEs are drawn from existing rosters, or some newly established network as is proposed in the July 2005 NPRM, SSA should establish consistent, national qualification standards for MEs to ensure a level of uniformity across the country. As discussed earlier, board
certification is fast becoming the standard credential for the practice of medicine and psychology. Therefore, physicians and psychologists who serve as MEs should be required to be board certified. Having a high level of qualification for MEs who testify at hearings is essential to the integrity of the hearing process. In addition, given the nature of the hearing process, the committee does not believe it would be appropriate to grandfather in existing MEs who are not board certified.
Despite the absence of formal qualification standards for MEs, there appears to have been a de facto requirement that MEs be either physicians or psychologists. According to data provided by SSA, the current roster of MEs includes only a handful of “acceptable medical sources” who are not physicians or psychologists (i.e., podiatrists, optometrists, or speech and language pathologists) or other qualified health professionals. As discussed previously, there are other health professionals (e.g., occupational therapists, physical therapists, registered nurses, psychiatric social workers) who could support the disability decision-making process by providing expert assessment of impairment severity and functional limitations, including functional components of Listings. These experts would be a valuable source of information at the ALJ hearing level, as well as at the DDS level.
Although the committee has recommended additional training for DDS MCs in disability evaluation and program requirements, it does not see a similar need for MEs, given that they are not directly involved in adjudication. If the national network proposed in the NPRM is established and network experts become the pool for MEs, then MEs will receive MC training, as called for in Recommendation 1-3.
As is the case with DDS MCs, SSA has difficulty recruiting well-qualified ME candidates in certain specialties, in large part because the compensation is too low. MEs are usually paid $160 a case, $80 for reviewing the file and $80 for attending a hearing.
According to a recent survey of OHA regional offices, every region had shortages of MEs in at least some specialties (SSA, 2004b). The regional offices consistently reported that the main reason for lack of access to medical expertise was the low fees they could offer, although some said MEs were also quitting because of the recent requirements of Central Contract Registration and fingerprinting. The result is that hearings cannot be scheduled, or cases wait until enough accumulate that need the same type of specialist to make it worthwhile for the ME to appear, or MEs in other than the needed field of expertise are used. A substantial fee increase to market rates, similar to the one recommended for CEs in Recommendation 2-2, below, in conjunction with higher qualification standards, would attract more and better candidates.
TRAINING AND CERTIFICATION OF CONSULTATIVE EXAMINERS
Task 10: “Recommend needs for standardized training and certification for consultative examiners who assess claimant’s level of function based on integrated evaluation of medical impairment and functional capacity. Advise on content of a training curriculum, appropriate personnel to train, and mechanisms for the certification process.”
Each DDS purchases CEs to obtain or clarify information that is missing, conflicting, or ambiguous in claimant’s medical records. They also purchase CEs when claimants do not have a regular source of treatment and thus have fragmented records that are difficult to locate. CE providers are asked to report examination and test results, a diagnosis and prognosis, and an opinion on what the claimant can do despite his or her impairment.
Each DDS is charged with recruiting and orienting medical personnel who agree to be available to perform CEs in return for a fee set by each state. If the claimant’s treating source is qualified, equipped, and willing to perform the examination or test and generally furnishes complete and timely reports, the treating source is the preferred source for the CE, because “The individual’s treating source is often in the best position to provide detailed longitudinal information about the individual.”28 If the treating source prefers not to do the CE, there are conflicts and inconsistencies in the file that cannot be resolved by going back to the treating source, or the DDS knows from prior experience that the treating source has consistently failed to provide complete or timely reports, the DDS can obtain the CE from a nontreating source. Currently, SSA keeps track of the number and costs of CEs purchased by each DDS but does not know the percentage of cases in which a CE or CEs is ordered or the percentage that is performed by the treating source.
CE providers are not required to be what SSA defines to be an acceptable medical source,29 if a medically determinable impairment has been established and the issue at hand is the severity of the impairment and how it affects an individual’s functioning. CE providers may be what SSA calls “other sources,” who may be medical practitioners such as nurse-practitioners, physical therapists, occupational therapists, chiropractors, and audiologists, or nonmedical sources such as teachers, day care providers, social workers, and employers. The committee was told that few CEs
are purchased from sources who are not acceptable medical sources, which SSA refers to as “other sources,” although these other sources are often in a better position to provide evidence about how well their patients function than are treating physicians who may see the patients infrequently (Talmadge, 2003). Other sources will become more important if SSA changes the emphasis from proving inability to work to encouraging return to work, which will require determination of what an applicant can do, not of what they cannot do.
Training and Certification Requirements for Consultative Examiners
Current SSA requirements for CE providers are minimal. They must be currently licensed to practice medicine in the state and have the training and experience to perform the type of examination or test being requested. They are also supposed to have the facilities and equipment needed to perform the examinations or tests being requested and have a good understanding of SSA’s disability programs and their evidentiary requirements.30 CE providers are not required to have training or certification specifically in the evaluation of disability.
The DDS adjudicator is supposed to select a specialist to perform the CE when the nature or complexity of a particular impairment or impairments warrants it, although there are no guidelines for which specialist to choose. According to SSA’s program operations manual, a CE provider usually does not have to be a specialist in the medical field relevant to the individual’s impairment or impairments. For example, an internist could be asked to perform an examination involving impairments of the musculoskeletal, cardiovascular, neurological, and other body systems.31
The DDSs are required to have an ongoing program to recruit CE providers; a process for orientation, training, and review of new CE providers on the content of CE reports; and an oversight program for CE providers, with special emphasis on “key” providers (those who bill at least $100,000 for CEs annually, or have a practice directed primarily towards independent medical examinations rather than the treatment of patients, or are one of the top five CE examination providers in the state by dollar volume). These requirements were contained in the Social Security Disability Benefits Reform Act of 1984, in response to complaints about the quality of CEs, especially those performed by so-called bulk providers (Bloch, 1992:98-108). (The preference for CEs by treating sources was also mandated by this law.)
Currently, each state makes its own arrangements for orienting and training CE providers. SSA requires DDSs to submit documentation that they have conducted annual oversight visits to key providers, but data on the findings are not systematically gathered and analyzed.
SSA furnishes CE providers with a guide, known as the Green Book, which was developed to give basic information about the CE process to physicians and other health professionals (SSA, 1999). The guide, which is available online as well as on paper, provides general information about the Social Security disability programs and how claims are adjudicated, including the role of CEs, how CE providers are selected, and what the DDSs look for in a report of a CE.
Although SSA does not currently have specific training and certification requirements for CE providers, there are training and certification requirements in other federal and nonfederal medical evaluation programs. For example,
Federal Aviation Administration (FAA)
The FAA requires pilots to be medically certified to fly. This is done by Aviation Medical Examiners (AMEs). To become an AME, the FAA requires physicians to complete Medical Certification Standards and Procedures Training and a basic AME seminar and to attend a three-day AME Seminar or equivalent training at three-year intervals thereafter.
U.S. Department of Transportation (DOT)
DOT has a drug testing program for individuals in safety-sensitive positions in the transportation industry. This function is performed by Medical Review Officers (MROs). Beginning in 2001, DOT has required training and certification of MROs and 12 hours of continuing medical education (CME) related to MRO practice every three years. Rather than provide the training and certification itself, DOT recognizes training and CME courses given by the American College of Occupational and Environmental Medicine, American Society of Addiction Medicine, and American Association of Medical Review Officers (AAMRO) and the written certification examination given by AAMRO.
U.S. Department of Labor (DOL)
DOL provides benefits to workers who have contracted pneumoconiosis from coal dust or asbestosis. The pneumoconiosis must be confirmed by a radiograph. The radiograph is read first at a facility approved by the National Institute for Occupational Safety and Health (NIOSH) and con-
firmed by a physician “B Reader” engaged by NIOSH. NIOSH requires B Readers to be certified and recertified every four years. The certification examinations are held at NIOSH’s Appalachian Laboratory for Occupational Safety and Health in Morgantown, West Virginia. NIOSH suggests that applicants use NIOSH’s home self-study syllabus or attend the American College of Radiology Symposium on Radiology of the Pneumoconioses held every two years.
State Workers’ Compensation Programs
California requires those who evaluate injured workers in disputed state workers’ compensation cases to be certified as Qualified Medical Evaluators (QMEs). To be certified means passing a test for knowledge and skills in clinical assessment/evaluation; medical treatment; disability issues/vocational rehabilitation/maximum medical improvement; causation; apportionment; basic workers’ compensation laws and regulations; and report writing. The QME test was developed and is administered by CPS Human Resource Services. Eligibility to be a QME also requires completion of a 12-hour course in disability evaluation report writing approved by the state.
Several other states, for example, Texas, also require state-approved training courses and written certification examinations of physicians who evaluate impairment in workers’ compensation cases. The courses are given by the American Academy of Disability Evaluating Physicians and the written examination by the American Association of Expert Medical Evaluators.32
If not board certified, QMEs have to have completed an accredited residency program. Both California and Texas require approved continuing education courses and periodic recertification.
Recommendation 2-1. SSA should establish reasonable requirements for training and certification of consultative examination providers. The training and certification should focus on two competencies: evaluation of limitations on ability to work resulting from impairments, and evidentiary and other requirements of SSA’s disability decision-making process.
The ability to diagnose and treat diseases and injuries is fulfilled by the current requirement that they be licensed or certified in their area of medical expertise. Physicians, for example, should be licensed and, if specialists, board certified. Licensure and board certification do not necessarily ensure,
however, that CE providers are expert in evaluating how a person’s impairments limits their functioning in employment settings or that they know how to provide medical evidence in a form pertinent to evaluating whether someone meets Social Security’s definition of disability. Physicians, with the exception of those trained in occupational medicine, usually do not learn how to evaluate work disability during medical school or residency or for board certification (Scheer, 2000:121) and are often not confident about their ability to determine who is disabled (Zinn and Furutani, 1996). Accordingly, CE providers should be required to demonstrate competence in these subject areas, namely, functional assessment of disability and SSA disability program policies and procedures.
The committee realizes that such requirements increase the costs of serving as a CE provider and, all other things being equal, would reduce the availability of medical sources to perform CEs. Other programs, however, such as the California and Texas workers’ compensation programs, require training and certification of medical evaluators and have no problem recruiting. The higher compensation for CEs recommended below, if brought in line with the fees in workers’ compensation and other disability benefit programs, should offset the cost to potential CE providers of reasonable training and certification requirements.
SSA should:
-
Develop a training curriculum on disability evaluation and SSA disability policies, rules, criteria, and procedures for CE providers, including both acceptable medical sources and other providers who evaluate function, such as nurses, occupational and physical therapists, and psychiatric social workers. This curriculum should be consistent with but less in depth than the one for MCs called for in Recommendation 1-3, above.
-
Provide the training curricula as online modules with pre- and posttest questions.
-
Require CE providers to complete the appropriate training module and pass the post-test with a certain minimum score.
-
Develop continuing education modules and require CE providers to take them and pass a post-test every two years.
The training and certification requirement should be phased in over several years after the curriculum has been well tested and adequately piloted in a few locations. This must be done in conjunction with the implementation of a fee schedule commensurate with the work involved in performing CEs, to prevent CE providers from dropping out of the program in great numbers.
An additional option would be to use members of the national network of medical and psychological experts to supplement the pool of CEs, as-
suming that there are enough experts to accommodate this as well as advise DDS and OHA decision makers. The advantage of using national network experts is that they will have mastered the curriculum for MCs, which will focus on disability evaluation and on SSA program rules and practices (see Recommendation 1-3, above). There is a potential down side. SSA should be mindful that national network experts paid to serve as CE providers by SSA may not be seen as impartial as CE providers who are otherwise independent of the agency. Policies should be instituted, therefore, so that an expert who reviews the medical record in a case cannot also perform a CE in the case or serve as an expert witness if the case goes to an ALJ hearing. The national network experts should receive training that clarifies the different roles they would have as consultants to MCs, as MCs themselves, as CE providers, and as expert witnesses (MEs) at ALJ hearings. In the last case, for example, experts are involved in a de novo proceeding in which previous medical opinions are not taken for granted.
SSA should exempt treating physicians who perform CEs of their patients from these training requirements. Few if any will have more than a few patients a year needing a CE, which would not justify the time it would take to become certified. However, the longitudinal knowledge they have of a patient’s functional impairments would help offset their lack of training in disability evaluation and SSA program rules. SSA should provide guidelines to treating physicians who perform CEs and notify them that SSA will reimburse them for time spent in orientation and training activities, as called for in Recommendation 2-2, below.
Adequate Reimbursement of CE Providers
In a standard medical examination, the clinician diagnoses the problem and develops a treatment plan. In a comprehensive disability examination, the clinician not only diagnoses and assesses the nature and severity of the impairment or impairments by reviewing the medical records in the claimant’s file, taking a history, performing an examination, and if needed, administering a diagnostic test or study, he or she also:
-
Evaluates the functional consequences of the impairment or combination of impairments.
-
Determines what the claimant’s capabilities are to perform work-related activities (in adults) or to engage in age-appropriate activities, such as school, physical activities, and social activities (in children).
-
Prepares a report complete enough to help the DDS determine the nature, severity, and duration of the impairment and the claimant’s residual functional capacity and that includes the objective medical facts as well as observations and opinions.
An adequate CE examination should include the following:33
-
Review of the claimant’s medical records;
-
Taking of a medical history;
-
Examination of the patient, including the administration of any needed tests;
-
Interpretation of test results;
-
Preparation of a report detailing findings from the history, examination, and tests;
-
Diagnosis and prognosis; and
-
Medical source statement.
A medical source statement is the CE provider’s opinion of the claimant’s ability to do work-related activities, such as sitting, standing, walking, lifting, carrying, handling objects, hearing, speaking, and traveling. In cases of mental impairment or impairments, the CE provider is expected to give an opinion on the claimant’s ability to understand, carry out and remember instructions, and respond appropriately to supervision, coworkers, and work pressures in a work setting. In childhood cases, the CE provider gives an opinion on how appropriately, effectively, and independently the child can perform activities compared to the performance of other children the same age who do not have impairments.
Recommendation 2-2. Reimbursement should be adequate to cover the full costs of a consultative examination, which involves more than a standard examination, whether it is focused or comprehensive in scope. This will require a substantial increase in fees over the amounts currently paid in most states. There also should be adequate compensation for time spent in orientation and training activities.
SSA should consider adopting a standard fee schedule for DDSs to use in purchasing CEs, adjusted for geographic differences in practice costs, with several fee levels depending on how focused or comprehensive the examination is. The maximum fees should be substantially higher than Medicare’s fees for regular office visits, because of the increased time it takes to perform a disability evaluation.34 This could be done in several ways. First, SSA could mandate the use of Current Procedural Terminology
(CPT) codes in the Medicare fee schedule that are more appropriate for a disability evaluation and that have higher relative value units (RVUs) than regular office visits. Codes 99244 and 99245, for example, are for “consultations,” which are defined as “a type of service provided by a physician whose opinion or advice regarding evaluation and/or management of a specific problem is requested by another physician or other appropriate source” (AMA, 2004). Code 99244, with an RVU of 4.56, is for patients who present with problems of moderate to high severity requiring approximately 45 minutes of face-to-face time with the physician, and 99245, with an RVU of 5.90, is for patients who present with problems of moderate to high severity requiring approximately 60 minutes of face-to-face time with the physician.35 Medicare currently pays up to $173 and $224, respectively, for these services, compared with $137 and $174 for the parallel office visit codes (99204 and 99205).
Second, SSA could use a higher conversion factor than Medicare uses to multiply the RVUs for each code. Medicare’s current conversion factor is $37.89. The Federal Employee’s Compensation Act program, for example, uses a conversion factor of $50.58. This translates into maximum fees of $231 and $298, respectively, for the consultation codes mentioned above (99244 and 99245). The Texas workers’ compensation program pays 125 percent of the Medicare rate.
Alternatively, SSA could use CPT codes 99455 and 99456, which are for “work-related or medical disability evaluation services.” Medicare does not use these services and therefore has not assigned a relative value to them, but the federal Office of Workers’ Compensation Programs (OWCP) has assigned them RVUs of 6.96 and 9.16, respectively.36 This would mean fees up to $264 and $347, respectively, using the Medicare conversion factor, and up to $352 and $463 using the OWCP conversion factor.37 These fees are paid to treating physicians for an examination at the time of maximum medical improvement to assess permanent disability. OWCP pays more for second opinions from independent medical examiners (IMEs). It has competitive contracts with IME companies in each region of the coun-
try and currently pays between $600 and $685 per examination and report, depending on the region (Schmidt, 2005).
In California’s workers’ compensation program, in the event of a dispute, a QME is called on to evaluate the worker. QMEs have passed a state-administered competency based examination, take state-approved continuing education courses, and are paid through a special fee schedule.38 The fee for a basic comprehensive medical-legal evaluation, which includes record review, examination, report, and overhead expenses) is $500; the fee for a complex evaluation is $750. The Texas workers’ compensation program pays $350 for an examination and report at the time of maximum medical improvement (the fee is more if an impairment rating is performed).39
SSA should conduct market studies and studies of fees that other programs pay for similar services to determine the new national fee schedule for CEs. The fees should probably vary by specialty and geographic location. They should be updated annually.
Higher fees should increase the pool of medical sources willing to perform CEs, especially in harder-to-recruit specialties such as orthopedics. This will help ensure that the appropriate specialist or specialists can be assigned in each case. It should also provide the incentive for more treating physicians to be willing to perform CEs. Higher fees should also increase the quality of CEs, although that is based on the judgment of the committee, not hard evidence.
Focused Requests for CEs Based on What Is Needed in Each Case
Improving the quality of CEs depends not only on the skill and knowledge of the CE providers but also on whether they have been asked for the right information. DEs, in consultation with MCs, if needed, are supposed to develop a complete medical history for at least the preceding 12 months; evaluate the medical evidence to identify missing, inconsistent, or ambiguous information; and, if the treating physician does not supply the missing information or clarify inconsistencies and ambiguities, purchase a CE to obtain the information. Once a CE is indicated, the goal is to obtain needed information quickly and avoid having to ask the CE provider for additional information or order another CE.
Recommendation 2-3. SSA should ensure that requests for consultative examinations indicate clearly what is needed in each case rather than making general requests for records and opinions.
SSA could develop templates for CE request letters for common types of cases that can be easily individualized. Templates for commonly encountered disabling conditions (e.g., lower back pain, asthma, osteoarthritis, chronic pulmonary insufficiency/chronic obstructive pulmonary disease, low birth weight, loss of hearing, developmental disabilities) would contain a comprehensive list of examinations, tests, diagnostic procedures, and other questions concerning the condition in question. These would serve as a checklist to remind DEs what is typically needed in each type of case and help them identify which questions and requests need to be made in each specific case, depending on what is already in the record. The unneeded items could be deleted and the now individualized letter could be printed. However, the DE should include a narrative paragraph in the request letter describing what the DE is concerned about and thinks is needed, to provide further guidance to the CE provider.
The cooperative effort with AUCD to develop an electronic database of all appropriate assessment instruments for assessing development and functioning in children should help DEs and MCs determine what test or tests are needed in childhood cases. Similar databases could be developed of appropriate tests for other common medical conditions that are the subjects of disability claims.
Many DDSs have developed standard request letters and forms. SSA should establish a process to identify best practices currently in use among the DDSs for facilitating useful CE examinations and reports. Experienced DEs and MCs should be involved, along with outside medical experts knowledgeable about current clinical practice and research.
PRESUMPTIVE DISABILITY CATEGORIES
Task 8: “Review SSA’s list of presumptive disability conditions and suggest revisions, additions, and/or deletions. The committee will recommend essential criteria for establishing candidate conditions for presumptive disability and recommend the level of professional expertise needed to certify that a presumptive diagnosis is adequately established.”
An adult or child applying for SSI based on disability or blindness may receive up to 6 months of payments prior to the final determination of disability or blindness if he or she is determined to be “presumptively disabled” or “presumptively blind” (hereafter, presumptive disability) and meets all other (i.e., financial) eligibility requirements.
SSA field offices are authorized only to make presumptive disability determinations for certain specified impairments. DDSs can make presumptive
disability findings in any case in which the available evidence indicates a “strong likelihood” that the claim will be allowed after going through the regular formal determination process.
Initially, the list of presumptive disability categories, because it was meant for use by field office personnel with no medical training, was confined to conditions that were either (1) easily verifiable by direct observation during the claims interview (e.g., amputation) or (2) easily confirmed by a telephone call to an appropriate authority, such as the treating physician or school official (e.g., total deafness). Over time, as presumptive disability categories were added to the original three, the evidence requirements became more complex. In some categories, a document is now needed. For example, in low-birth-weight cases, a birth certificate or hospital admission summary is required. In end stage renal disease (ESRD) cases, Medicare form CMS-2728 is needed. For allegations of HIV infection, SSA developed a special check-block form for the treating source or CE provider to complete. Field office interviewers use the completed form to confirm the diagnosis and see if the checked items indicate that disease manifestations are of listing-level severity.
The impairment categories for which field offices may make presumptive disability decisions currently are:
-
Amputation of a leg at the hip.
-
Allegation of total deafness.
-
Allegation of total blindness.
-
Allegation of bed confinement or immobility without a wheelchair, walker, or crutches, allegedly due to a long-standing condition, excluding a recent accident and recent surgery.
-
Allegation of stroke (cerebral vascular accident) more than three months in the past and continued marked difficulty in walking or using a hand or arm.
-
Allegation of cerebral palsy, muscular dystrophy or muscular atrophy and marked difficulty in walking (e.g., use of braces), speaking or coordination of the hands or arms.
-
Allegation of Down syndrome.
-
Allegation of severe mental deficiency made by another individual filing on behalf of a claimant who is at least seven years of age.
-
Birth weight below 1200 grams (2 pounds, 10 ounces) for a child claimant who is less than one year old, according to the birth certificate or other evidence, such as the hospital admission summary.
-
Human immunodeficiency virus (HIV) infection confirmed by a medical source.
-
Available evidence such as the hospital admission summary which shows a gestational age at birth and a certain corresponding birth weight
-
for a child claimant who is less than one year old (e.g., 35 weeks and 1700 grams of less).
-
Confirmation from physician or hospice official that an individual is receiving hospice services for a terminal illness.
-
Allegation of spinal cord injury producing the inability to ambulate without the use of a walker or bilateral hand-held assistive devices for more than two weeks which is confirmed by an appropriate medical professional.
-
ESRD with ongoing dialysis where file contains an ESRD Medical Evidence Report-Medicare Entitlement and/or Patient Registration.
-
Allegation of amyotrophic lateral sclerosis (ALS, Lou Gehrig’s disease).
According to SSA statistics, field offices and DDSs granted presumptive disability status in 135,603 cases in CY 2004, constituting approximately 7.7 percent of the 1.76 million SSI claims made that year. Field offices accounted for 17,191 (13 percent) of the 135,603 presumptive disability decisions made in CY 2004 (the rest were made by DDSs). The field office presumptive disability cases constituted 1.0 percent of the applications for SSI benefits in 2004. The rate of presumptive disability varied from field office to field office, from 0.1 to 3.5 percent (a difference of 35 times).
Looking at field offices as a group, half of all presumptive disability decisions were in the two low-birth-weight categories (categories 9 and 11 in Table 1, column 2). Three other categories accounted for another 25 percent: category 6 (allegation of cerebral palsy, muscular dystrophy, or muscle atrophy), category 7 (allegation of Down syndrome), and category 19 (HIV infection).
Ultimately, 10.3 percent of the field office presumptive disability cases were not allowed at the initial decision level after going through the regular disability determination process (Table 1, column 3). However, some categories had very low “reversal rates,” between 1 and 2 percent (e.g., categories 7, 9, and 14), while several others had very high reversal rates, between 40 and 50 percent (categories 1 and 10).
According to SSA statistics on all title SSI disability determination decisions in CY 2004 (including concurrent SSI-DI and both presumptive disability and nonpresumptive disability cases), seven impairment codes had allowance rates of 95 percent or higher (Annex Table 7). Of these, three correspond to current presumptive categories (ALS, birth weight under 1,200 grams, and Down syndrome). The other four were cancers with high fatality rates (e.g., pancreatic and liver cancer). Another five codes had allowance rates of 90 to 94.9 percent. These included one code that corresponds to a presumptive disability category (developmental disabilities including autism). The others were cancers (e.g., lung cancer). Setting the
TABLE 1 Field Office Presumptive Disability Decisions, by Presumptive Disability Category, CY 2004
|
|
|
(1) Number of FO PD Decisions |
(2) Percentage of All FO PD Decisions |
(3) Reversal Rate |
(4) Percentage of All FO PD Reversals |
|
1. |
Amputation of a leg at the hip |
342 |
2.0% |
48.5% |
9.4% |
|
2. |
Allegation of total deafness |
479 |
2.8% |
12.1% |
3.3% |
|
3. |
Allegation of total blindness |
320 |
1.9% |
9.1% |
2.6% |
|
4. |
Allegation of bed confinement or immobility without aid |
674 |
3.9% |
9.1% |
3.5% |
|
5. |
Allegation of stroke more than 3 months in the past & continued marked difficulty… |
230 |
1.3% |
16.5% |
2.2% |
|
6. |
Allegation of cerebral palsy, muscular dystrophy or muscular atrophy & marked difficulty in… |
1,342 |
7.8% |
12.1% |
9.2% |
|
7. |
Allegation of Down syndrome |
1,863 |
10.8% |
1.3% |
1.4% |
|
8. |
Allegation of severe mental deficiency… |
717 |
4.2% |
7.1% |
2.9% |
|
9. |
Birth weight less than 1200 grams… |
5,691 |
33.1% |
1.9% |
6.2% |
|
10. |
HIV infection confirmed… |
1,235 |
7.2% |
42.1% |
29.4% |
|
11. |
Low birth weight for gestational age… |
3,092 |
18.0% |
14.8% |
26.0% |
|
12. |
Hospice services for a terminal illness confirmed… |
433 |
2.5% |
6.7% |
1.6% |
|
13. |
Allegation of spinal cord injury causing inability to ambulate without… |
266 |
1.5% |
9.4% |
1.4% |
|
14. |
ESRD with ongoing dialysis and Medicare Form… |
441 |
2.6% |
1.8% |
0.5% |
|
15. |
Allegation of ALS… |
19 |
0.1% |
5.3% |
0.1% |
|
Total |
17,191 |
100.0% |
10.3% |
100.0 |
|
|
SOURCE: Unpublished tables provided by the Office of Disability and Income Support Programs, SSA. |
|||||
cutoff at 85 percent would yield six more codes, all malignancies except chronic renal failure and childhood origin psychosis (adult).
Almost 90 percent of DDS cases granted presumptive disability status were eventually allowed after going through the regular disability determination process, but they did not achieve this rate in every type of case. The DDSs experienced allowance rates of 95 percent or more in 47 impairment codes, accounting for 38 percent of the presumptive disability cases initiated by them (Table 2). These cases included organic mental disorders, cerebral palsy, schizophrenia, leukemia, mental retardation, chronic renal
TABLE 2 DDS Presumptive Disability Decisions, by Impairment Code, CY 2004
|
Allowance Rate |
Number of Codes |
Number of Decisions |
Percentage of Decisions |
Cumulative |
|||
|
Allowance Rate |
Number of Codes |
Number of Decisions |
Percentage of Decisions |
||||
|
95-100% |
47 |
44,951 |
38.0% |
95-100% |
47 |
44,951 |
38.0% |
|
90-94.9% |
42 |
39,373 |
33.3% |
90-100% |
89 |
84,324 |
71.2% |
|
85-89.9% |
35 |
13,729 |
11.6% |
85-100% |
124 |
98,053 |
82.8% |
|
80-84.9% |
29 |
10,294 |
8.7% |
80-100% |
153 |
108,347 |
91.5% |
|
70-79.9% |
33 |
7,023 |
5.9% |
70-100% |
186 |
115,370 |
97.4% |
|
60-69.9% |
10 |
856 |
0.7% |
60-100% |
196 |
116,226 |
98.2% |
|
50-59.9% |
6 |
206 |
0.2% |
50-100% |
202 |
116,432 |
98.3% |
|
0-49.9% |
8 |
340 |
0.3% |
0-100% |
210 |
116,772 |
98.6% |
|
Unknown |
|
1,643 |
1.4% |
|
|
118,415 |
100.0% |
|
SOURCE: Unpublished tables provided by the Office of Disability and Income Support Programs, SSA. |
|||||||
failure, birth weight under 1,200 grams, lung, liver, and pancreatic cancers, cancer, and developmental disabilities including autism.40 Reversal rates were higher than 50 percent for some impairments, but they only involved a third of one percent of the cases. There were reversal rates of between 10 percent and 50 percent in 27 percent of DDS presumptive disability cases.
The annual number of presumptive disability decisions has increased greatly since 2001, when there were 60,543. The increase was entirely due to DDSs; field offices granted presumptive disability in slightly fewer cases in 2004 than in 2001, 17,191 compared with 18,862. Although the number of presumptive disability decisions more than doubled, the overall rate of reversals fell from 13 percent to 9 percent. DDSs lowered their reversal rate from 12 percent to 9 percent and the field offices from 17 percent to 10 percent. These differences seem to be due to management practices more than to medical policies.
Revising the Presumptive Disability Categories with Explicit Criteria
Presumptive disability is primarily a social policy. Congress included it in the 1972 act establishing the SSI program because it recognized that applicants for SSI have little or no income or assets and probably need immediate assistance with the costs of living. Claimants must meet the low income and assets criteria for SSI even to be considered for presumptive
|
40 |
Annex Table 6 lists all 47 impairment codes for presumptive disability decisions that had reversal rates less than 5 percent in CY 2004. |
disability. Therefore, the committee is unable to recommend specific categories to include or delete because the selection criteria are not solely medical. We can, however, analyze the impacts of setting different levels of potential reversal rates (i.e., presumptive disability cases that turn out not to meet the criteria for allowances) and suggest that SSA adopt explicit criteria and use them to revise the presumptive disability categories.
Recommendation 3-1. SSA should consider dropping some current presumptive disability categories, and perhaps adding some, after deciding on explicit criteria for including categories.
The current presumptive disability categories were created for use by nonmedical personnel in SSA field offices, which means they must have two characteristics. They must be capable of being applied by a layperson, and they must have a high probability of meeting SSA’s definition of disability. To be applied by an interviewer in a field office, the categorical condition must be either directly observable during the claims interview or quickly confirmable by contacting the treating physician or other appropriate authority. To have a high probability of meeting SSA’s definition of disability, a categorical condition must be one in which the diagnosis alone correlates highly either with inability to work for a year or more or the presence of a terminal illness.
The nonmedical criterion in selecting presumptive disability categories is the degree of risk, i.e., the reversal rate, that SSA is willing to pay for in order to increase the number of true positives. Early in the SSI program, an SSA ruling suggested that a reversal rate of more than 10 percent a month over several months made a category a candidate for deletion.41 Perhaps this is too stringent. Only nine of the 15 current categories would meet this criterion (Table 3). A reversal rate of 15 percent or less would include 12 of the current categories, and a rate of 20 percent or less would add one more, bringing the total to 13. A reversal rate of 20 percent or less would reach more needy claimants than one of 10 percent or less, but the costs of cases ultimately found to be ineligible would be higher.
At the end of 2003, the average SSI benefit for the blind and disabled under age 65 was $446.97. Taking this as the average cost of a presumptive disability decision and assuming that reversed presumptive disability cases were paid for the full six months, or $2,681.80 each, moving the reversal bar from 10 percent to 15 percent (thus adding 679 presumptive disability cases) would have cost approximately $1.8 million in 2004 (Table 3). Moving it to 20 percent (adding another 38 cases) would have cost another
TABLE 3 Approximate Costs of Presumptive Disability Cases Ultimately Disallowed, CY 2004 Data
|
PD Category Allowance Rate |
Number of PD Categories |
Number of Disallowances |
Cost of Disallowances |
Cumulative Cost of Lower Allowance Rates |
|
90% or more |
9 |
338 |
$906,447.75 |
$906,447.75 |
|
85-89.9% |
3 |
679 |
$1,820,940.90 |
$2,727,388.65 |
|
80-84.9% |
1 |
38 |
$101,908.33 |
$2,829,296.98 |
|
50-79.9% |
2 |
686 |
$1,839,713.49 |
$4,669,010.47 |
|
SOURCE: Unpublished tables provided by the Office of Disability and Income Support Programs, SSA. |
||||
$102,000. Note also that removing the two presumptive disability categories with reversal rates between 40 percent and 50 percent would have reduced costs by approximately $1.8 million.
The committee also notes that the presumptive disability categories do not include conditions that consistently have high allowance rates, which therefore on equity grounds could be considered as candidates for inclusion as presumptive disability categories. As noted in the findings section, above, title SSI claims having one of 12 primary impairment codes had a 90 percent chance of approval in CY 2004. Of the 12, four correspond closely to existing presumptive disability categories.
The other eight were types of malignancies. Currently, a claim presenting with one of the malignancy codes could only be granted presumptive disability status by a field office if the claimant were in hospice care and had less than six months to live. SSA could consider granting presumptive disability to claimants who know they have one of these cancers, and the diagnosis can be confirmed by contacting their treating physician.
Dropping the bar to impairments with 85 percent approval rates would add four more cancers, chronic renal failure and childhood-origin psychosis in adults. An 80 percent allowance rate adds nine more categories—six cancers, mental retardation, other disorders of the spinal cord, and multiple body dysfunction.
In 2004, the 12 impairment codes with 90 percent allowances rates accounted for 50,171 cases, 2.9 percent of all SSI claims made. Of these, less than 17,000 were actually granted presumptive disability. If the allowance rate cutoff were 85 percent, it would have been 18 codes and 70,486 cases, 4.0 percent of all SSI claims. Of these, 19,434 were presumptive disability cases. If the cutoff were 80 percent, the number of codes would have increased to 31 and the number of cases to 139,072, or 7.9 percent of all SSI claims. Of these, 31,045 were presumptive disability cases.
If SSA decides to adopt a uniform approval rate for presumptive disability cases, Table 3 needs to be expanded to include the costs of adding the cases with impairment codes that meet the established approval rate standard that are not now included. For example, if SSA decided to include conditions in which the approval rate averages 90 percent, the costs of presumptive disability cases in categories with lower approval rates would be eliminated, but the costs of new conditions meeting the 90 percent allowance rate criterion would be added (Table 4).
These calculations indicate that there are a number of conditions in which the probability is high that a claimant who alleges he or she has one will be allowed. The question the committee cannot answer is whether that probability should be 90, 85, 80 percent, or some other number. The answer depends on the trade-off society wishes to make between helping groups of low-income persons with given probability of being determined disabled by SSA and the cost of paying for cases that end up being disallowed.
The preceding discussion assumes that the goal of the presumptive disability policy is to identify early those who are likely to be determined disabled after the regular evaluation process and start paying them. This is consistent with congressional intent, namely, to enable claimants who have a high likelihood of being awarded benefits eventually to begin receiving benefits immediately. However, the result of the current system is that claimants with the same condition may be treated differently, depending on if they do or do not have sufficient medical evidence or an established diagnosis. And as we have discussed above, it will result in claimants with an equally severe but not explicitly categorized presumptive disability impairment being ineligible for presumptive disability status, if their impairment cannot be easily observed or verified.
TABLE 4 Approximate Costs of Adopting Different Allowance Rates to Determine Presumptive Disability Cases, CY 2004 Data
|
PD Category Allowance Rate |
Number of PD Categories |
Number of Disallowances |
Cost of Paying Disallowed Cases |
Number of Impairment Codes |
Number of Disallowances |
Cost of Paying Disallowed Cases |
|
90% or more |
9 |
338 |
$906,447 |
12 |
1,182 |
$3,169,083 |
|
85-89.9% |
3 |
679 |
$1,820,940 |
6 |
2,324 |
$6,232,503 |
|
80-84.9% |
1 |
38 |
$101,908 |
9* |
11,293 |
$30,285,567 |
|
50-79.9% |
2 |
686 |
$1,839,713 |
48 |
96,929 |
$259,944,192 |
|
*Includes mental retardation, with an allowance rate of 80.1 percent in 2004. SOURCE: Unpublished tables provided by the Office of Disability and Income Support Programs, SSA. |
||||||
Other approaches are possible. SSA could decide to grant presumptive disability in cases where the claimant’s condition is worsening and he or she has little or no funds or insurance to pay for medical treatment that might reduce the level of impairment or prevent it from worsening further. Another approach would be to stipulate that certain conditions are potentially so serious that presumptive disability is warranted, even if the award rates for those conditions are far less than 100 percent.
Increasing Consistency in the Use of Presumptive Disability
The percentage of SSI claims that are granted presumptive disability varies widely across SSA field offices and DDSs, a situation that SSA could improve. The percentage of field office presumptive disability cases ranges from 0.1 to 3.5 percent. The range for DDSs is from 0.6 to 34.6 percent. Field offices had presumptive disability cases in all 15 categories in 11 states. In two states, however, field offices used only one of the 15 categories, accounting for two cases each. Some categories with high allowance rates overall (i.e., highly likely to be allowed) were not used at all in some states, such as Down syndrome, birth weight less than 1,200 grams, ESRD, and ALS (Table 5).
Recommendation 3-2. SSA should mandate use of the presumptive disability procedure by, and take other administrative steps to achieve more consistency among, the field offices and DDSs in the implementation of the presumptive disability policy.
Currently, the use of the presumptive disability procedure is voluntary, which leads to large differences in practice from office to office that are not the result of inherent difficulties in assessing cases. If SSA has a presumpOverall Number of States without
TABLE 5 Field Office Use of Presumptive Disability Categories for High-Allowance-Rate Impairments, CY 2004
|
Impairment |
Overall Allowance Rate* |
Number of States without PD Cases in the Category |
|
Down syndrome |
97.6% |
3 |
|
Birth weight less than 1,200 grams |
98.0% |
5 |
|
Chronic renal failure (ESRD) |
88.8% |
13 |
|
ALS |
98.3% |
40 |
|
*Overall means decisions on all title SSI disability applications, PD and non-PD. SOURCE: Unpublished tables provided by the Office of Disability and Income Support Programs, SSA. |
||
tive disability process, and it is part of national social policy, it should be applied uniformly from place to place. This is primarily a matter for administrative policy to achieve.
Learning from Terminal Illness (TERI) Procedures
PD is a policy to expedite payments. TERI (TERminal Illness) cases involve expedited decisions. According to the SSA program operations manual, “Cases where there is an indication of a terminal illness (TERI) are to be handled in an expeditious manner because of the sensitivity involved.” Teleservice and field office interviewers are supposed to be on the alert for potential TERI cases in certain situations, for example, when the claimant or other person—friend, family member, or medical provider—says the illness is terminal, the claimant is receiving hospice care, the claimant has AIDS, or any other situation in which the medical condition is untreatable and expected to end in death. According to SSA’s program operations manual, examples of potential TERI conditions include claimants:
-
with a chronic dependence on a cardiopulmonary life-sustaining device;
-
awaiting a heart, heart/lung, liver or bone marrow transplant (excluding kidney and corneal transplants);
-
with chronic pulmonary or heart failure requiring continuous home oxygen and who is unable to care for personal needs;
-
with a malignant disease (e.g., cancer) who is home confined or institutionalized, unable to care for personal needs and unresponsive to therapy;
-
with diabetes and one or more of the following: multiple amputations due to diabetic gangrene; recurrent cardiovascular events (e.g., infarction or failure); or recurrent cerebrovascular events with neurological deficit;
-
with chronic liver disease (e.g., cirrhosis or hepatitis) and a history of massive gastrointestinal hemorrhage;
-
who is comatose for 30 days or more; or who is a newborn with a lethal or severe genetic or congenital defect.
Recommendation 3-3. SSA should look at TERI procedures for lessons in making expedited decisions on cases that must meet specific medical criteria. These include uniform special procedures throughout the decision process that promote consistency as well as speed.
TERI cases are subject to special procedures through which the case is expedited through every step of the disability determination process,
including the appeals process and the payment process. They are also sent immediately from the field office to the DDS for development and quick decision.
The issue is whether field office interviewers are able to identify TERI cases with some accuracy. This would involve determining the percentage of cases flagged as TERI cases that turn out to meet the criteria and, taking a sample of all cases, the percentage of cases that were not flagged that should have been. Differences between types of cases and from field office to field could be analyzed for better understanding of TERI decision making and ways to improve it, and also of ways to improve presumptive disability procedures.
AFTERWORD
This interim report has addressed 3 of the 10 tasks that the committee is charged with addressing. It focuses on one important part of improving SSA’s disability decision process: the qualifications of medical personnel participating in the decision process. It also makes recommendations for improving the implementation of the presumptive disability policy. The committee is addressing the other seven tasks in its next, and final, report, which is due in 2006. These are tasks 1 through 7 in the Annex, which focus on ways to improve other important parts of the process: the medical criteria and procedures that are used to screen applicants for eligibility.
REFERENCES
ABMS (American Board of Medical Specialties). 2005. 2005 Annual Report and Reference Handbook. Available: www.abms.org/Downloads/Publications/AnnualReport2005.pdf (accessed September 30, 2005).
ABPP (American Board of Professional Psychology). 2005. Specialty Board Certification in Professional Psychology. Available: www.abpp.org/brochures/genbrochure2005.pdf (accessed October 7, 2005).
ACUS (Administrative Conference of the United States). 1989. Improved Use of Medical Personnel in Social Security Disability Determinations. Recommendation 89-10 of the Administrative Conference of the United States. Available: www.law.fsu.edu/library/admin/acus/3058910.html (accessed October 7, 2005).
AMA (American Medical Association). 2004. CPT 2005, Standard Edition. Chicago, IL: American Medical Association.
Anfield R. 2002. Statement of Robert Anfield, M.D., Vice President and Chief Medical Officer, Customer Care Centers, UnumProvident Corporation, before the Subcommittee on Social Security, House Committee on Ways and Means, July 11. Available: waysandmeans.house.gov/legacy.asp?file=legacy/socsec/107cong/7-11-02/107-92final.htm (accessed September 16, 2005).
Barnhart JA. 2003. Statement of The Honorable Jo Anne B. Barnhart, Commissioner, Social Security Administration. Testimony before the Subcommittee on Social Security of the House Committee on Ways and Means, September 25, 2003. Available: waysandmeans.house.gov/hearings.asp?formmode=view&id=761 (accessed September 23, 2005).
Barnhart JA. 2005. Social Security’s Proposed Improvements to the Disability Determination Process. Statement of Jo Anne B. Barnhart, Commissioner of Social Security before the Subcommittee on Social Security of the House Committee on Ways and Means, September 27, 2005. Available: waysandmeans.house.gov/hearings.asp?formmode=view&id=3802 (accessed September 29, 2005).
Barzansky B. 2005. Personal communication by electronic mail on November 14. Barbara Barzansky is Associate Director, Division of Undergraduate Medical Education Policy and Standards, and Secretary, Council on Medical Education, American Medical Association, Chicago, IL.
Bloch F. 1992. Disability Determination: The Administrative Process and the Role of Medical Personnel. Westport, CT: Greenwood Press.
Bloch F, Lubbers J, Verkuil P. 2003. Introducing Nonadversarial Government Representatives to Improve the Record for Decision in Social Security Disability Decisions. Report to the Social Security Advisory Board. Available: www.ssab.gov/documents/Bloch-Lubbers-Verkuil.pdf (accessed October 7, 2005).
Brennan TA, Horwitz RI, Duffy, FD, Cassel CK, Goode LD, Lipner RS. 2004. The Role ofThe Role of Physician Specialty Board Certification Status in the Quality Movement. Journal of the American Medical Association, 292(9):1038-1043.
Canadian Parliament. 2003. Listening to Canadians: A First View of the Future of the Canada Pension Plan Disability Program. Fifth Report of the Standing Committee on Human Resources Development and the Status of Persons with Disabilities, June. Available: www.parl.gc.ca/infocomdoc/37/2/HUMA/Studies/Reports/humarp05/humarp05-e.pdf (accessed April 12, 2005).
Choudhry NK, Fletcher RH, Soumerai SB. 2005. Systematic Review: The Relationship between Clinical Experience and Quality of Health Care. Annals of Internal Medicine, 142(4):260-273.
CPP/OAS (Canada Pension Plan/Old Age Security). 2004. Review Tribunals Biennial Report: 2002-2004. Ottawa, Ontario: Office of the Commissioner of Review Tribunals, Canada Pension Plan/Old Age Security. Available: www.reviewtribunals.gc.ca/pubs/bi_rpt2004/toc_e.html (accessed April 12, 2005).
Demeter SL. 2003. Contrasting the Standard, Impairment, and Disability Examination and Report. Pp. 101-107 in Demeter SL, Andersson GBJ, eds. Disability Evaluation, 2nd Ed. St. Louis, MO: Mosby.
Demeter SL, Washington RJ. 2003. The Disability Evaluation and Report. Pp. 625-639 in De-meter SL, Andersson GBJ, eds. Disability Evaluation, 2nd Ed. St. Louis, MO: Mosby.
DHHS (Department of Health and Human Services). 2002. Projected Supply, Demand, and Shortages of Registered Nurses: 2000-2020. National Center for Health Workforce Analysis, Bureau of Health Professions, Health Resources and Services Administration, U.S. Department of Health and Human Services. Available: bhpr.hrsa.gov/healthworkforce/reports/rnproject/report.htm#chart2 (accessed November 10, 2005).
GAO (General Accountability Office). 2003. SSA Disability Decision Making: Additional Steps Needed to Ensure Accuracy and Fairness of Decisions at the Hearing Level. GAO-04-14. November 12. Available: www.gao.gov/new.items/d0414.pdf (accessed July 25, 2005).
GAO. 2004. Social Security Administration: More Effort Needed to Assess Consistency of Disability Decisions. GAO-04-656. July 2. Available: www.gao.gov/new.items/d04656.pdf (accessed July 25, 2005).
Geiringer SR. 2000. Independent Medical Evaluation. Pp. 241-256 in Rondinelli RD, Katz RT, eds. Impairment Rating and Disability Evaluation. Philadelphia: W. B. Saunders.
Himmelstein JS, Pransky GS, Sweet CP. 2000. Ability to Work and the Evaluation of Disability. Pp. 257-274 in Levy BS, Wegman DH, eds. Occupational Health: Recognizing
and Preventing Work-Related Disease and Injury, 4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins.
IOM (Institute of Medicine). 2002. The Dynamics of Disability: Measuring and Monitoring Disability for Social Security Programs. Washington, DC: National Academies Press.
IOM. 2004. NIH Extramural Center Programs: Criteria for Initiation and Evaluation. Washington, DC: National Academies Press.
Leo RJ, Del Regno P. 2001. Social Security Claims of Psychiatric Disability: Elements of Case Adjudication and the Role of Primary Care Physicians. Primary Care Companion Journal of Clinical Psychiatry, 3(6):255-262.
Lewin. 2005. A Study of the Practice Expenses Associated with the Provision of Evaluation and Management Services. May 13. Falls Church, VA: The Lewin Group.
Lewin (Lewin Group), and Pugh Ettinger McCarthy Associations. 2001. Evaluation of SSA’s Disability Quality Assurance (QA) Processes and Development of QA Options that Will Support the Ling-Term Management of the Disability Program. Prepared for the Social Security Administration. Report available: www.quintiles.com/NR/rdonlyres/ekhzi4f6bl2iwvway5ibsoerh7acjf6lpnwh3etwt6jd246bw5cdaymmastvdiojiljc7jt3cozp3nosoj56dr2k2zf/1325.pdf (accessed September 15, 2005). Appendixes available: www.quintiles.com/NR/rdonlyres/ekhzi4f6bl2iwvway5ibsoerh7acjf6lpnwh3etwt6jd246bw5cdaymmastvdiojiljc7jt3cozp3nosoj56dr2k2zf/1325.pdf (accessed September 15, 2005).
Mischoulon D. 2002. Potential Pitfalls to the Therapeutic Relationship Arising from Disability Claims. Psychiatric Annals, 32(5):299-302.
Nibali K. 2003. Social Security Disability Programs. Pp. 44-61 in Demeter SL, Andersson GBJ, eds. Disability Evaluation, 2nd Ed. St. Louis, MO: Mosby.
Pincus HA, Kennedy C, Simmens SJ, Goldman HH, Sirovatka P, Sharfstein SS. 1991. Determining Disability Due to Mental Impairment: APA’s Evaluation of Social Security Administration Guidelines. American Journal of Psychiatry, 148(8):1037-1043.
Pransky G, Katz JN, Benjamin KL, Himmelstein J. 2002. Improving the Physician’s Role in Evaluating Work Ability and Managing Disability: A Survey of Primary Care Practitioners. Disability and Rehabilitation, 24(16):867-874.
Robinson JP, Wolfe CV. 2000. Social Security Disability Insurance and Supplemental Security Income. Pp. 159-186 in Rondinelli RD, Katz RT, eds. Impairment Rating and Disability Evaluation. Philadelphia: W. B. Saunders.
Scheer SJ. 2000. Physician Assessment of Working Capacity. Pp. 121-138 in Rondinelli RD, Katz RT, eds. Impairment Rating and Disability Evaluation. Philadelphia: W. B. Saunders.
Schmidt S. 2005. Personal communication by telephone with Michael McGeary, July 19, 2005. Stephen Schmidt is in the Medical Standards and Rehabilitation Branch, Office Workers’ Compensation Programs, U.S. Department of Labor.
SSA (Social Security Administration). 1999. Consultative Examinations: A Guide for Health Professionals. SSA Pub. No. 64-025. Baltimore, MD: Office of Disability Programs, Social Security Administration. Available: www.ssa.gov/disability/professionals/greenbook/index.htm (accessed September 30, 2005).
SSA. 2003. Findings of the Disability Hearings Quality Review Process: ALJ Peer Report V. December. SSA Pub. No. 30-013. Office of Quality Assurance and Performance Assessment, Social Security Administration.
SSA. 2004a. Fiscal Year 2005 Annual Performance Plan and Revised FY 04 APP. Available: www.ssa.gov/performance/2005/ (accessed July 25, 2005).
SSA. 2004b. National Medical Expert Survey of OHA Regional Offices: Compiled Responses. Unpublished internal document furnished by SSA.
SSA. 2005a. Fiscal Year 2004 Social Security Administration Performance and Accountability Report. Washington, DC: SSA. Available: www.ssa.gov/finance/ (accessed September 28, 2005).
SSA. 2005b. 2005 Annual Report of the Supplemental Security Income Program.
Updated
SSA. 2005c. Fast Facts and Figures about Social Security, 2005. Available: www.ssa.gov/policy/docs/chartbooks/fast_facts/2005/ff2005.pdf (accessed September 28, 2005).
SSA. 2005d. Disability Determinations and Appeals, Fiscal Year 2004. Unpublished chart prepared by the Office of Disability Programs, January.
SSA. 2005e. Notice of Proposed Rulemaking: Administrative Review Process for Adjudicating Initial Disability Claims. Federal Register, 70(143):43590-43624. Available: a257.g.akamaitech.net/7/257/2422/01jan20051800/edocket.access.gpo.gov/2005/pdf/05-14845.pdf (accessed September 28, 2005).
SSAB (Social Security Advisory Board). 1998. How SSA’s Disability Programs Can Be Improved. Washington, DC: SSAB. Available: www.ssab.gov/NEW/Publications/Disability/report6.pdf (accessed July 25, 2005).
SSAB. 2001a. Charting the Future of Social Security’s Disability Programs: The Need for Fundamental Change. Washington, DC: SSAB. Available: www.ssab.gov/Publications/Disability/disabilitywhitepap.pdf (accessed July 25, 2005).
SSAB. 2001b. Disability Decision Making: Data and Materials. Washington, DC: SSAB. Available: www.ssab.gov/NEW/Publications/Disability/chartbookA.pdf (accessed July 25, 2005).
SSAB. 2003. The Social Security Definition of Disability. Washington, DC: SSAB. Available: www.ssab.gov/documents/SocialSecurityDefinitionOfDisability_000.pdf (accessed July 25, 2005).
Steinbrook R. 2005. Renewing Board Certification. New England Journal of Medicine, 353(19):1994-1997.
Strand A. 2002. Social Security Disability Programs: Assessing the Variation in Allowance Rates. ORES Working Paper No. 98. Office of Research, Evaluation, and Statistics, Social Security Administration, Washington, DC, SSA.
Talmadge JB. 2003. Resource Personnel Used in a Disability Evaluation. Pp. 640-643 in De-meter SL, Andersson GBJ, eds. Disability Evaluation, 2nd Ed. St. Louis, MO: Mosby.
Zayatz T. 2005. Social Security Disability Insurance Program Worker Experience. Actuarial Study No. 118. Social Security Administration, Office of the Chief Actuary. Available: www.socialsecurity.gov/OACT/NOTES/as118/DI-WrkerExper_Body.html#wp1057748 (accessed November 11, 2005).
Zinn W, Furutani N. 1996. Physician Perspectives on the Ethical Aspects of Disability Determination. Journal of General Internal Medicine, 11(9):525-532.
ANNEX: LIST OF STUDY TASKS
In addressing the Listings, the committee will consider:
The value and utility of the current Listings for all users (claimants, SSA, health care professionals, state offices, and officials involved in the adjudication process)
Conceptual models for organizing the Listings, beyond the current “body systems” model at 20 C.F.R. Part 404, Subpart P, Appendix I
Processes for determining when the Listings require revision and criteria upon which to add new listings or remove old ones
-
Feedback mechanisms to continuously assess and evaluate the Listings for the purpose of improving consistency in application by all adjudicators throughout the country
-
Adaptability of the Listings, including methods to account for variable access to health care services (including diagnostics and pharmaceuticals) in determining whether an individual’s condition meets or equals the Listings
-
Methods to assess and quantify the effects of multiple impairments that may not individually cross the eligibility threshold (e.g., SSA’s “equivalence” concept)
-
Advisability of and methods for integrating functional assessment into the Listings
In addressing the organization of medical expertise, the committee will:
-
Review SSA’s list of presumptive disability conditions and suggest revisions, additions, and/or deletions. The committee will recommend essential criteria for establishing candidate conditions for presumptive disability and recommend the level of professional expertise needed to certify that a presumptive diagnosis is adequately established.
-
Advise on how best to provide medical expertise needed to support the entire disability adjudication process. This will involve describing the type of experts needed (academic specialists, practicing specialists, practicing generalists or nonphysicians), necessary credentials, and where best to locate them (from university medical centers, centers of excellence for specialized care, or community practice settings).
-
Recommend needs for standardized training and certification for consultative examiners who assess claimant’s level of function based on integrated evaluation of medical impairment and functional capacity. Advise on content of a training curriculum, appropriate personnel to train, and mechanisms for the certification process.
ANNEX TABLE 1 DDS Medical Consultants by Specialty, June 2004
|
Specialty |
Number |
Percentage |
|
Psychology |
707 |
33.1 |
|
Internal medicine |
341 |
16.0 |
|
Psychiatry |
233 |
10.9 |
|
Pediatrics |
209 |
9.8 |
|
Family practice |
141 |
6.6 |
|
Speech-language pathology |
59 |
2.8 |
|
General medicine |
42 |
2.0 |
|
Neurology |
38 |
1.8 |
|
Cardiology |
36 |
1.7 |
|
Orthopedic specialist |
35 |
1.6 |
|
Surgery |
35 |
1.6 |
|
Ophthalmology |
25 |
1.2 |
|
Gynecology/obstetrics |
21 |
1.0 |
|
Anesthesiology |
21 |
1.0 |
|
Emergency medicine |
20 |
0.9 |
|
Physical medicine and rehabilitation |
19 |
0.9 |
|
Orthopedic surgery |
18 |
0.8 |
|
Osteopathy |
14 |
0.7 |
|
Occupational medicine |
13 |
0.6 |
|
All others |
122 |
5.7 |
|
Total |
2,136 |
100.0 |
|
NOTE: The percentage of specialists in each category that are board certified or board eligible is not known. SOURCE: Unpublished tables provided by the Office of Disability and Income Support Programs, SSA. |
||
ANNEX TABLE 2 Number of DDS Medical Consultants by Specialty and State, June 2004
|
State DDS |
Family Practice |
Internal Medicine |
Pediatrics |
Psychology |
Psychiatry |
Cardiology |
Neurology |
Orthopedics |
Other |
Total |
|
Connecticut |
0 |
9 |
1 |
15 |
4 |
0 |
2 |
0 |
4 |
35 |
|
Maine |
0 |
0 |
1 |
7 |
0 |
1 |
0 |
1 |
4 |
14 |
|
Massachusetts |
3 |
24 |
2 |
28 |
6 |
0 |
1 |
0 |
2 |
66 |
|
New Hampshire |
3 |
1 |
1 |
4 |
0 |
0 |
0 |
0 |
1 |
10 |
|
Rhode Island |
0 |
8 |
1 |
6 |
2 |
0 |
0 |
0 |
1 |
18 |
|
Vermont |
0 |
4 |
2 |
5 |
1 |
1 |
1 |
0 |
0 |
14 |
|
Region I Total |
6 |
46 |
8 |
65 |
13 |
2 |
4 |
1 |
12 |
157 |
|
New Jersey |
0 |
23 |
5 |
22 |
3 |
3 |
0 |
8 |
3 |
67 |
|
New York |
3 |
23 |
16 |
18 |
33 |
0 |
0 |
1 |
15 |
109 |
|
Puerto Rico |
0 |
8 |
0 |
8 |
3 |
1 |
1 |
0 |
3 |
24 |
|
Delaware |
1 |
3 |
1 |
4 |
1 |
0 |
0 |
0 |
1 |
11 |
|
District of Columbia |
0 |
3 |
3 |
2 |
0 |
0 |
0 |
0 |
0 |
8 |
|
Region II Total |
4 |
60 |
25 |
56 |
40 |
4 |
1 |
9 |
22 |
219 |
|
Maryland |
1 |
4 |
4 |
11 |
5 |
1 |
0 |
0 |
4 |
30 |
|
Pennsylvania |
5 |
7 |
4 |
45 |
2 |
0 |
1 |
3 |
12 |
79 |
|
Virginia |
6 |
6 |
8 |
20 |
2 |
2 |
0 |
2 |
9 |
55 |
|
West Virginia |
2 |
7 |
2 |
9 |
2 |
0 |
0 |
0 |
1 |
23 |
|
Region III Total |
14 |
24 |
18 |
85 |
11 |
3 |
1 |
5 |
26 |
187 |
|
Alabama |
1 |
4 |
6 |
14 |
4 |
3 |
1 |
2 |
7 |
42 |
|
Florida |
20 |
11 |
33 |
76 |
9 |
2 |
0 |
1 |
28 |
180 |
|
Georgia |
1 |
18 |
5 |
24 |
1 |
1 |
2 |
4 |
7 |
63 |
|
Kentucky |
0 |
5 |
4 |
15 |
1 |
0 |
0 |
1 |
14 |
40 |
|
Mississippi |
0 |
3 |
2 |
11 |
1 |
0 |
0 |
2 |
8 |
27 |
|
North Carolina |
9 |
5 |
4 |
19 |
4 |
0 |
1 |
1 |
6 |
49 |
|
State DDS |
Family Practice |
Internal Medicine |
Pediatrics |
Psychology |
Psychiatry |
Cardiology |
Neurology |
Orthopedics |
Other |
Total |
|
South Carolina |
2 |
4 |
4 |
21 |
1 |
0 |
1 |
1 |
11 |
45 |
|
Tennessee |
2 |
5 |
8 |
20 |
3 |
1 |
1 |
1 |
15 |
56 |
|
Region IV Total |
35 |
55 |
66 |
200 |
24 |
7 |
6 |
13 |
96 |
502 |
|
Illinois |
6 |
11 |
10 |
22 |
4 |
3 |
0 |
0 |
22 |
78 |
|
Indiana |
0 |
5 |
1 |
8 |
0 |
1 |
2 |
0 |
10 |
27 |
|
Michigan |
8 |
17 |
5 |
15 |
21 |
0 |
2 |
0 |
14 |
82 |
|
Minnesota |
0 |
6 |
2 |
12 |
1 |
0 |
0 |
5 |
2 |
28 |
|
Ohio |
12 |
11 |
5 |
41 |
1 |
0 |
0 |
2 |
16 |
88 |
|
Wisconsin |
0 |
5 |
3 |
9 |
0 |
0 |
1 |
0 |
2 |
20 |
|
Region V Total |
26 |
55 |
26 |
107 |
26 |
4 |
5 |
7 |
66 |
323 |
|
Arkansas |
0 |
1 |
5 |
3 |
2 |
1 |
1 |
3 |
2 |
18 |
|
Louisiana |
2 |
5 |
5 |
19 |
2 |
2 |
1 |
2 |
12 |
50 |
|
New Mexico |
5 |
5 |
2 |
2 |
2 |
0 |
0 |
0 |
1 |
17 |
|
Oklahoma |
2 |
5 |
1 |
10 |
1 |
0 |
0 |
0 |
1 |
20 |
|
Texas |
6 |
6 |
2 |
10 |
9 |
1 |
3 |
2 |
6 |
45 |
|
Region VI Total |
15 |
22 |
15 |
44 |
16 |
4 |
5 |
7 |
22 |
150 |
|
Iowa |
7 |
0 |
3 |
17 |
1 |
2 |
0 |
0 |
4 |
34 |
|
Kansas |
9 |
4 |
1 |
11 |
3 |
1 |
0 |
0 |
2 |
31 |
|
Missouri |
2 |
9 |
9 |
31 |
5 |
2 |
1 |
2 |
20 |
81 |
|
Nebraska |
6 |
1 |
2 |
8 |
0 |
0 |
0 |
0 |
2 |
19 |
|
Region VII Total |
24 |
14 |
15 |
67 |
9 |
5 |
1 |
2 |
28 |
165 |
|
Colorado |
0 |
5 |
2 |
3 |
5 |
2 |
2 |
2 |
4 |
25 |
|
Montana |
1 |
1 |
1 |
4 |
0 |
0 |
0 |
1 |
2 |
10 |
|
North Dakota |
0 |
3 |
0 |
4 |
1 |
1 |
0 |
1 |
1 |
11 |
|
South Dakota |
1 |
1 |
1 |
4 |
1 |
0 |
0 |
0 |
5 |
13 |
|
Utah |
0 |
1 |
1 |
6 |
5 |
0 |
1 |
0 |
4 |
18 |
|
Wyoming |
1 |
2 |
0 |
6 |
0 |
0 |
0 |
1 |
6 |
16 |
|
Region VIII Total |
3 |
13 |
5 |
27 |
12 |
3 |
3 |
5 |
22 |
93 |
|
Arizona |
1 |
6 |
2 |
7 |
9 |
1 |
4 |
1 |
13 |
44 |
|
California |
7 |
28 |
19 |
1 |
62 |
2 |
4 |
2 |
49 |
174 |
|
Hawaii |
1 |
3 |
1 |
4 |
2 |
0 |
0 |
0 |
4 |
15 |
|
Nevada |
0 |
3 |
3 |
5 |
0 |
0 |
1 |
0 |
2 |
14 |
|
Region IX Total |
9 |
40 |
25 |
17 |
73 |
3 |
9 |
3 |
68 |
247 |
|
Alaska |
0 |
1 |
1 |
0 |
2 |
0 |
2 |
0 |
2 |
8 |
|
Idaho |
0 |
1 |
1 |
2 |
0 |
0 |
0 |
1 |
1 |
6 |
|
Oregon |
1 |
3 |
1 |
7 |
0 |
0 |
0 |
0 |
4 |
16 |
|
Washington |
4 |
7 |
3 |
31 |
6 |
1 |
1 |
1 |
9 |
63 |
|
Region X Total |
5 |
12 |
6 |
40 |
8 |
1 |
3 |
2 |
16 |
93 |
|
All DDSs |
141 |
341 |
209 |
706 |
233 |
36 |
38 |
54 |
378 |
2136 |
|
NOTE: Psychiatry includes 12 child psychiatrists. Orthopedics includes 18 orthopedic surgeons, 35 orthopedic specialists, and 1 orthopedic-neurologist. SOURCE: Unpublished tables provided by the Office of Disability and Income Support Programs, SSA. |
||||||||||
ANNEX TABLE 3 Case Mix Compared with Mix of Medical Consultant Specialties
ANNEX TABLE 4 Number of Medical Experts by Specialty, June 2005
|
Specialty |
Number |
Percentage |
|
Clinical psychology |
415 |
22.3 |
|
Internal medicine |
371 |
19.9 |
|
Psychiatry |
235 |
12.6 |
|
Orthopedic surgery |
121 |
6.5 |
|
Pediatrics |
115 |
6.2 |
|
Neurology |
102 |
5.5 |
|
Cardiovascular diseases |
71 |
3.8 |
|
Ophthalmology |
57 |
3.1 |
|
Family practice |
31 |
1.7 |
|
Pulmonary diseases |
22 |
1.2 |
|
Child psychiatry |
21 |
1.1 |
|
Physical medicine and rehabilitation |
20 |
1.0 |
|
Rheumatology |
19 |
1.0 |
|
General surgery |
18 |
1.0 |
|
Occupational medicine |
18 |
0.8 |
|
Gastroenterology |
15 |
0.8 |
|
General preventive medicine |
15 |
0.8 |
|
Urological surgery |
14 |
0.7 |
|
Endocrinology |
13 |
0.6 |
|
Child psychology |
12 |
0.6 |
|
Neurological surgery |
12 |
0.6 |
|
Emergency medicine |
11 |
0.6 |
|
Medical oncology |
11 |
0.6 |
|
All others |
122 |
6.6 |
|
Total |
1,861 |
100.0 |
|
NOTE: The number of specialties is more than the number of MEs (1,575), because some practice in more than one specialty. SOURCE: Unpublished table provided by the Office of Hearings and Appeals, SSA. |
||
ANNEX TABLE 5 Number of Medical Experts by Specialty and Federal Region, June 2005
|
Federal Region |
Clinical Psychology |
Internal Medicine |
Psychiatry |
Orthopedic Surgery |
Pediatrics |
Neurology |
Cardiovascular Diseases |
Ophthalmology |
Other |
Total |
|
Region I |
18 |
23 |
16 |
10 |
6 |
9 |
4 |
5 |
18 |
109 |
|
Region II |
13 |
25 |
20 |
7 |
9 |
7 |
5 |
5 |
29 |
120 |
|
Region III |
31 |
35 |
28 |
3 |
7 |
13 |
5 |
5 |
45 |
172 |
|
Region IV |
110 |
85 |
78 |
42 |
39 |
25 |
20 |
12 |
93 |
504 |
|
Region V |
73 |
56 |
30 |
20 |
23 |
17 |
7 |
8 |
52 |
286 |
|
Region VI |
47 |
46 |
22 |
16 |
6 |
14 |
6 |
6 |
48 |
211 |
|
Region VII |
12 |
14 |
3 |
1 |
3 |
1 |
3 |
1 |
16 |
54 |
|
Region VIII |
37 |
7 |
0 |
0 |
2 |
4 |
0 |
1 |
10 |
61 |
|
Region IX |
43 |
53 |
32 |
16 |
12 |
8 |
19 |
14 |
47 |
244 |
|
Region X |
31 |
27 |
6 |
6 |
8 |
4 |
2 |
0 |
16 |
100 |
|
All regions |
415 |
371 |
235 |
121 |
115 |
102 |
71 |
57 |
374 |
1,861 |
|
SOURCE: Unpublished table provided by the Office of Hearings and Appeals, SSA. |
||||||||||
ANNEX TABLE 6 Impairment Codes of DDS Presumptive Disability Decisions with a Reversal Rate of Less Than 5 percent, CY 2004
|
SSA Impairment Code |
Number of DDS PD Decisions |
Number Reversed |
Reversal Rate (percent) |
|
4160-Chronic pulmonary heart disease |
163 |
8 |
4.9 |
|
2940-Organic mental disorders |
4,505 |
215 |
4.8 |
|
3060-Somatoform disorders |
42 |
2 |
4.8 |
|
3370-Disorders of the autonomic nervous system |
64 |
3 |
4.7 |
|
4920-Emphysema |
193 |
9 |
4.7 |
|
1830-Malignant neoplasm/ovary and other uterine adnexa |
314 |
14 |
4.5 |
|
1640-Malignant neoplasm/thymus, heart, mediastinum |
23 |
1 |
4.3 |
|
3430-Cerebral palsy |
1,835 |
78 |
4.3 |
|
4430-Peripheral vascular disease |
516 |
21 |
4.1 |
|
2950-Schizophrenic/paranoid functional disorders |
4,944 |
198 |
4.0 |
|
1920-Malignant neoplasm/other parts of the nervous system |
76 |
3 |
3.9 |
|
1900-Malignant neoplasm/eye |
31 |
1 |
3.2 |
|
1710-Malignant neoplasm/connective and other soft tissue |
99 |
3 |
3.0 |
|
1910-Malignant neoplasm/brain |
830 |
23 |
2.8 |
|
3360-Other disorders of the spinal cord |
517 |
14 |
2.7 |
|
1410-Malignant neoplasm/tongue |
192 |
5 |
2.6 |
|
7600-Multiple body dysfunction |
714 |
18 |
2.5 |
|
1510-Malignant neoplasm/stomach |
249 |
6 |
2.4 |
|
1990-Malignant neoplasm/unspecified sites |
131 |
3 |
2.3 |
|
2070-Leukemias |
1,058 |
24 |
2.3 |
|
8060-Vertebral fracture/cord lesion |
766 |
18 |
2.3 |
|
2630-Malnutrition/weight loss |
139 |
3 |
2.2 |
|
7840-Loss of voice |
983 |
20 |
2.0 |
|
2990-Childhood origin psychosis (adult) |
637 |
12 |
1.9 |
|
3180-Mental retardation |
9,643 |
185 |
1.9 |
|
1720-Malignant melanoma of skin |
179 |
3 |
1.7 |
|
5850-Chronic renal failure |
4,173 |
62 |
1.5 |
|
2990-Developmental disabilities including autism (children) |
2,558 |
36 |
1.4 |
|
1620-Malignant neoplasm/trachea, bronchus, lung |
2,606 |
35 |
1.3 |
|
1980-Malignant neoplasm/distant sites |
78 |
1 |
1.3 |
|
3320-Parkinson’s disease |
154 |
2 |
1.3 |
|
1500-Malignant neoplasm/esophagus |
367 |
4 |
1.1 |
|
1630-Malignant neoplasm/pleura |
98 |
1 |
1.0 |
|
3350-Anterior horn cell disorder (ALS) |
113 |
1 |
0.9 |
|
7580-Chromosome anomaly/Down syndrome |
1,443 |
8 |
0.6 |
|
7650-Birth weight under 1200 grams |
3,291 |
12 |
0.4 |
|
1550-Malignant neoplasm of liver and intrahepatic bile ducts |
710 |
2 |
0.3 |
|
0940-Neurosyphilis |
3 |
0 |
0.0 |
|
1560-Malignant neoplasm/gallbladder |
56 |
0 |
0.0 |
|
SSA Impairment Code |
Number of DDS PD Decisions |
Number Reversed |
Reversal Rate percent) |
|
1570-Malignant neoplasm/pancreas |
400 |
0 |
0.0 |
|
1760-Malignant Kaposi’s sarcoma |
8 |
0 |
0.0 |
|
1780-Malignant neoplasm/skeletal system |
4 |
0 |
0.0 |
|
2730-Disorders of plasma protein metabolism |
3 |
0 |
0.0 |
|
3210-Arachnoiditis |
10 |
0 |
0.0 |
|
5010-Asbestosis |
6 |
0 |
0.0 |
|
7050-Hidradenitis suppurativa |
16 |
0 |
0.0 |
|
9330-Chronic fatigue syndrome |
11 |
0 |
0.0 |
|
SOURCE: Unpublished table provided by the Office of Disability and Income Support Programs, SSA. |
|||
ANNEX TABLE 7 SSA Impairment Codes by Allowance Rate, from Highest to Lowest, CY 2004
|
SSA Impairment Code |
Number of Decisions |
Number of Allowances |
Allowance Rate (percent) |
|
All codes |
2,532,798 |
947,266 |
37.4 |
|
1550-Malignant neoplasm of liver and intrahepatic bile ducts |
4,653 |
4,616 |
99.2 |
|
1570-Malignant neoplasm/pancreas |
3,304 |
3,258 |
98.6 |
|
3350-Anterior horn cell disorder (ALS) |
1,534 |
1,506 |
98.2 |
|
7650-Birth weight under 1200 grams |
17,235 |
16,890 |
98.0 |
|
7580-Chromosome anomaly/Down syndrome |
5,242 |
5,111 |
97.5 |
|
1980-Malignant neoplasm/distant sites |
619 |
599 |
96.8 |
|
1630-Malignant neoplasm/pleura |
806 |
776 |
96.3 |
|
1560-Malignant neoplasm/gallbladder |
450 |
432 |
96.0 |
|
1620-Malignant neoplasm/trachea, bronchus, lung |
19,291 |
18,307 |
94.9 |
|
1500-Malignant neoplasm/esophagus |
2,916 |
2,744 |
94.1 |
|
2990-Developmental disabilities including autism (children) |
10,759 |
9,920 |
92.2 |
|
1910-Malignant neoplasm/brain |
6,302 |
5,754 |
91.3 |
|
1510-Malignant neoplasm/stomach |
1,966 |
1,779 |
90.5 |
|
5850-Chronic renal failure |
22,195 |
19,998 |
90.1 |
|
1780-Malignant neoplasm/skeletal system |
20 |
18 |
90.0 |
|
1720-Malignant melanoma of skin |
1,832 |
1,618 |
88.3 |
|
2070-Leukemias |
6,166 |
5,408 |
87.7 |
|
1760-Malignant Kaposi’s sarcoma |
40 |
35 |
87.5 |
|
1410-Malignant neoplasm/tongue |
1,392 |
1,197 |
86.0 |
|
2990-Childhood origin psychosis (adult) |
3,898 |
3,352 |
86.0 |
|
2030-Multiple myeloma |
2,164 |
1,859 |
85.9 |
|
1590-Malignant neoplasm/other digestive organs, peritoneum |
741 |
636 |
85.8 |
|
1990-Malignant neoplasm/unspecified sites |
552 |
471 |
85.3 |
|
1830-Malignant neoplasm/ovary and other uterine adnexa |
3,394 |
2,882 |
84.9 |
|
3180-Mental retardation |
77,102 |
65,460 |
84.9 |
|
3360-Other disorders of the spinal cord |
3,428 |
2,856 |
83.3 |
|
7600-Multiple body dysfunction |
2,555 |
2,128 |
83.3 |
|
1920-Malignant neoplasm/other parts of the nervous system |
280 |
230 |
82.1 |
|
1520-Malignant neoplasm/small intestine |
552 |
449 |
81.3 |
|
1890-Malignant neoplasm/kidney, other urinary organs |
2,740 |
2,206 |
80.5 |
|
0420-Malignant neoplasm/bone marrow or stem cell transplantation |
5 |
4 |
80.0 |
|
7400-Anencephalus/catastrophic anomaly |
569 |
453 |
79.6 |
|
2630-Malnutrition/weight loss |
1,112 |
876 |
78.8 |
|
1640-Malignant neoplasm/thymus, heart, mediastinum |
173 |
136 |
78.6 |
|
1700-Malignant neoplasm/bone and articular cartilage |
1,550 |
1,207 |
77.9 |
|
SSA Impairment Code |
Number of Decisions |
Number of Allowances |
Allowance Rate(percent) |
|
3430-Cerebral palsy |
9,864 |
7,546 |
76.5 |
|
3320-Parkinson’s disease |
3,853 |
2,894 |
75.1 |
|
1950-Malignant neoplasm/other sites |
5,399 |
4,049 |
75.0 |
|
8060-Vertebral fracture/cord lesion |
4,699 |
3,449 |
73.4 |
|
1880-Malignant neoplasm/bladder |
1,535 |
1,122 |
73.1 |
|
7840-Loss of voice |
5,162 |
3,742 |
72.5 |
|
1380-Late effects of acute poliomyelitis |
1,859 |
1,346 |
72.4 |
|
1710-Malignant neoplasm/connective and other soft tissue |
902 |
650 |
72.1 |
|
7410-Spina bifida |
1,867 |
1,344 |
72.0 |
|
1530-Malignant neoplasm/colon, rectum, anus |
11,184 |
8,019 |
71.7 |
|
2950-Schizophrenic/paranoid functional disorders |
56,218 |
40,308 |
71.7 |
|
3300-Cerebral degeneration/childhood |
616 |
439 |
71.3 |
|
3750-Cardiac transplantation |
319 |
226 |
70.8 |
|
1420-Malignant neoplasm/salivary glands |
234 |
165 |
70.5 |
|
4380-Late effects of cerebrovascular disease |
32,139 |
22,529 |
70.1 |
|
1790-Malignant neoplasm/uterus |
2,566 |
1,783 |
69.5 |
|
4430-Peripheral vascular disease |
8,979 |
6,240 |
69.5 |
|
4160-Chronic pulmonary heart disease |
2,137 |
1,481 |
69.3 |
|
2840-Aplastic anemia |
738 |
505 |
68.4 |
|
7830-Malnutrition, marasmus/growth impairment |
2,388 |
1,631 |
68.3 |
|
3590-Muscular dystrophies |
3,188 |
2,155 |
67.6 |
|
3150-Developmental/emotional disorders-infant |
4,521 |
3,034 |
67.1 |
|
0300-Leprosy |
3 |
2 |
66.7 |
|
4960-Cronic pulmonary insufficiency/COPD |
40,287 |
26,348 |
65.4 |
|
1940-Malignant neoplasm/other endocrine glands and related |
242 |
158 |
65.3 |
|
3310-Other cerebral degenerations |
3,901 |
2,536 |
65.0 |
|
2940-Organic mental disorders |
57,567 |
36,958 |
64.2 |
|
3210-Arachnoiditis |
231 |
145 |
62.8 |
|
9070-Late effects/nervous system injuries |
6,740 |
4,125 |
61.2 |
|
3690-Blindness/low vision |
24,669 |
14,752 |
59.8 |
|
4280-Heart failure |
15,865 |
9,440 |
59.5 |
|
1740-Malignant neoplasm/breast |
17,865 |
10,558 |
59.1 |
|
3620-Other retinal disorders |
3,455 |
2,038 |
59.0 |
|
3153-Speech and language delays |
32,332 |
18,914 |
58.5 |
|
4460-Periarteritis nodosa/allied condition |
296 |
171 |
57.8 |
|
1870-Malignant neoplasm/penis, male genital organs |
158 |
91 |
57.6 |
|
7500-Congenital anomalies/upper alimentary tract |
372 |
212 |
57.0 |
|
1850-Malignant neoplasm/prostate |
3,233 |
1,827 |
56.5 |
|
4920-Emphysema |
4,382 |
2,471 |
56.4 |
|
2760-Diabetic acidosis |
222 |
123 |
55.4 |
|
4540-Varicose veins/low extremities |
2,374 |
1,294 |
54.5 |
|
3570-Diabetic/peripheral neuropathy |
13,714 |
7,460 |
54.4 |
|
2020-Lymphoma |
7,075 |
3,799 |
53.7 |
|
3890-Deafness |
15,352 |
8,183 |
53.3 |
|
SSA Impairment Code |
Number of Decisions |
Number of Allowances |
Allowance Rate (percent) |
|
7460-Congenital heart anomalies |
5,542 |
2,910 |
52.5 |
|
0940-Neurosyphilis |
25 |
13 |
52.0 |
|
0430-Symptomatic HIV positive |
18,168 |
9,429 |
51.9 |
|
8540-Intracranial injury |
5,785 |
2,968 |
51.3 |
|
1900-Malignant neoplasm/eye |
194 |
99 |
51.0 |
|
2770-Disorders of metabolism/cystic fibrosis |
1,426 |
719 |
50.4 |
|
3400-Multiple sclerosis |
14,183 |
7,148 |
50.4 |
|
4250-Cardiomyopathy |
15,472 |
7,581 |
49.0 |
|
1170-Skin/mucus membrane infections |
720 |
351 |
48.7 |
|
7140-Rheumatoid & other inflammatory arthritis |
19,437 |
9,330 |
48.0 |
|
3060-Somatoform disorders |
1,425 |
681 |
47.8 |
|
1860-Malignant neoplasm/testis |
791 |
375 |
47.4 |
|
2960-Mood disorders (children) |
21,121 |
9,927 |
47.0 |
|
2390-Neoplasm/unspecified/unknown behavior |
308 |
144 |
46.8 |
|
7050-Hidradenitis suppurativa |
295 |
135 |
45.8 |
|
4410-Aortic aneurysm |
1,341 |
607 |
45.3 |
|
1730-Other malignant neoplasm of skin |
463 |
209 |
45.1 |
|
3610-Retinal detachment with retinal defects |
1,592 |
716 |
45.0 |
|
2250-Benign neoplasm/brain, nervous system |
3,049 |
1,332 |
43.7 |
|
4590-Other diseases of the circulatory system |
7,004 |
3,061 |
43.7 |
|
3370-Disorders of the autonomic nervous system |
1,408 |
614 |
43.6 |
|
1840-Malignant neoplasm/other female genital organs |
1,141 |
496 |
43.5 |
|
4140-Chronic ischemic heart disease |
44,127 |
19,195 |
43.5 |
|
4030-Hypertensive vascular/renal disease |
376 |
162 |
43.1 |
|
7200-Ankylosing/inflamnatory spondylopathies |
1,007 |
430 |
42.7 |
|
2820-Hereditary hemolytic anemias including sickle cell |
4,167 |
1,771 |
42.5 |
|
5010-Asbestosis |
289 |
122 |
42.2 |
|
7300-Osteomyelitis/other infections involving bone |
1,837 |
775 |
42.2 |
|
1930-Malignant neoplasm/thyroid gland |
782 |
327 |
41.8 |
|
5710-Chronic liver disease/cirrhosis |
30,970 |
12,853 |
41.5 |
|
7150-Osteoarthritis/allied disorders |
113,194 |
45,730 |
40.4 |
|
4480-Diseases of capillaries |
145 |
57 |
39.3 |
|
0930-Cardiovascular syphilis |
36 |
14 |
38.9 |
|
2730-Disorders of plasma protein metabolism |
93 |
36 |
38.7 |
|
3490-Other nervous system disorders |
15,534 |
5,996 |
38.6 |
|
3000-Anxiety-related disorders |
46,037 |
17,724 |
38.5 |
|
3138-Oppositional/defiant disorder |
7,776 |
2,955 |
38.0 |
|
3650-Glaucoma |
2,958 |
1,121 |
37.9 |
|
3580-Myoneural disorders |
3,118 |
1,160 |
37.2 |
|
5810-Nephrotic syndrome |
2,447 |
903 |
36.9 |
|
3120-Conduct disorder |
5,856 |
2,102 |
35.9 |
|
2960-Affective disorders (adult) |
277,560 |
99,089 |
35.7 |
|
7590-Other congenital anomalies |
3,324 |
1,160 |
34.9 |
|
2850-Other anemias |
1,864 |
641 |
34.4 |
|
SSA Impairment Code |
Number of Decisions |
Number of Allowances |
Allowance Rate (percent) |
|
3660-Cataract |
2,400 |
826 |
34.4 |
|
2790-Disorders immune mechanism (except HIV) |
1,009 |
345 |
34.2 |
|
3010-Personality disorders |
14,295 |
4,860 |
34.0 |
|
1360-Other infectious/parasitic diseases |
1,488 |
487 |
32.7 |
|
5780-Gastrointestinal hemorrhage |
979 |
311 |
31.8 |
|
9050-Late effects/musculoskeletal and connective tissue injuries |
14,412 |
4,525 |
31.4 |
|
7100-Diffuse diseases of connective tissue |
9,056 |
2,835 |
31.3 |
|
2880-Diseases of white blood cells |
145 |
45 |
31.0 |
|
3140-Attention deficit hyperactivity disorder |
94,862 |
29,312 |
30.9 |
|
3950-Diseases of aortic valve |
3,889 |
1,190 |
30.6 |
|
4100-Acute myocardial infarction |
5,254 |
1,608 |
30.6 |
|
3070-Eating and tic disorders |
349 |
106 |
30.4 |
|
2870-Purpura/other hemorrhagic conditions |
499 |
151 |
30.3 |
|
2380-Neoplasm/uncertain behavior |
204 |
60 |
29.4 |
|
5190-Other diseases of respiratory system |
8,111 |
2,385 |
29.4 |
|
1350-Sarcoidosis |
1,904 |
554 |
29.1 |
|
5300-Diseases of esophagus |
984 |
286 |
29.1 |
|
3860-Vertiginous syndromes |
2,155 |
625 |
29.0 |
|
7330-Other bone/cartilage disorders |
16,067 |
4,659 |
29.0 |
|
4940-Bronchiectasis |
674 |
193 |
28.6 |
|
7649-Birth weight between 1,200 and 2,000 grams |
6,951 |
1,981 |
28.5 |
|
2810-Deficiency anemias |
1,365 |
388 |
28.4 |
|
4020-Hypertensive vascular disease |
7,426 |
2,109 |
28.4 |
|
3980-Other rheumatic heart disease |
629 |
177 |
28.1 |
|
9490-Burns |
1,925 |
537 |
27.9 |
|
4510-Phlebitis/thrombophlebitis |
1,012 |
280 |
27.7 |
|
4240-Valvular heart diseases/other stenotic defects |
3,923 |
1,067 |
27.2 |
|
3910-Rheumatic fever/heart involvement |
169 |
45 |
26.6 |
|
4270-Cardiac dysrhythmias |
4,966 |
1,311 |
26.4 |
|
2890-Other diseases blood/blood forming organs |
1,313 |
339 |
25.8 |
|
5050-Pneumoconiosis |
240 |
61 |
25.4 |
|
5560-Idiopathic proctocolitis |
1,369 |
344 |
25.1 |
|
6940-Bullous disease |
517 |
128 |
24.8 |
|
4130-Angina pectoris |
1,761 |
426 |
24.2 |
|
2860-Coagulation defects |
826 |
199 |
24.1 |
|
2720-Hyperlipidemia |
175 |
42 |
24.0 |
|
7160-Other and unspecified arthropathies |
27,885 |
6,469 |
23.2 |
|
6960-Dermatitis |
1,951 |
451 |
23.1 |
|
2780-Obesity |
20,758 |
4,754 |
22.9 |
|
5550-Regional enteritis/granulomatous colitis |
4,723 |
1,053 |
22.3 |
|
3680-Visual disturbances |
6,158 |
1,324 |
21.5 |
|
8690-Internal injury |
506 |
108 |
21.3 |
|
8940-Lower limb open wounds |
3,117 |
664 |
21.3 |
|
3152-Learning disorder |
36,123 |
7,622 |
21.1 |
|
8270-Lower limb fractures |
34,015 |
7,075 |
20.8 |
|
SSA Impairment Code |
Number of Decisions |
Number of Allowances |
Allowance Rate (percent) |
|
2740-Gout |
1,511 |
308 |
20.4 |
|
3195-Borderline intellectual functioning |
31,621 |
6,356 |
20.1 |
|
7240-Back disorders |
311,813 |
62,674 |
20.1 |
|
0110-Pulmonary tuberculosis |
472 |
90 |
19.1 |
|
6950-Ichthyosis |
567 |
103 |
18.2 |
|
7280-Muscle, ligament, fascia disorders |
58,995 |
10,619 |
18.0 |
|
2550-Disorders of adrenal glands |
386 |
69 |
17.9 |
|
2500-Diabetes mellitus |
67,988 |
11,966 |
17.6 |
|
5690-Other disorders gastrointestinal system |
13,943 |
2,440 |
17.5 |
|
9330-Chronic fatigue syndrome |
1,974 |
342 |
17.3 |
|
2530-Disorders of pituitary gland |
441 |
75 |
17.0 |
|
7800-Sleep-related disorder |
2,371 |
403 |
17.0 |
|
7090-Other disorders skin/subcutaneous tissue |
3,399 |
557 |
16.4 |
|
5330-Peptic ulcer |
1,022 |
165 |
16.1 |
|
8390-Dislocations |
2,435 |
392 |
16.1 |
|
3460-Migraine |
8,011 |
1,282 |
16.0 |
|
3540-Carpal tunnel syndrome |
5,627 |
889 |
15.8 |
|
8840-Upper limb open wounds |
3,676 |
573 |
15.6 |
|
5530-Hernias |
3,048 |
451 |
14.8 |
|
8180-Upper limb fractures |
12,756 |
1,862 |
14.6 |
|
8290-Other fractures |
8,432 |
1,214 |
14.4 |
|
4910-Chronic bronchitis |
1,653 |
230 |
13.9 |
|
2510-Hypoglycemia |
123 |
17 |
13.8 |
|
3780-Strabismus/disorders eye movements |
557 |
76 |
13.6 |
|
3450-Epilepsy |
37,165 |
4,980 |
13.4 |
|
7370-Curvature of spine |
4,530 |
607 |
13.4 |
|
4010-Essential hypertension |
32,188 |
3,863 |
12.0 |
|
6080-Disorders of male genital organs |
434 |
49 |
11.3 |
|
5990-Other disorders of urinary tract |
3,823 |
413 |
10.8 |
|
2520-Disorders of parathyroid |
265 |
28 |
10.6 |
|
4930-Asthma |
60,855 |
6,086 |
10.0 |
|
5350-Gastritis/Duodenitis |
1,480 |
144 |
9.7 |
|
8790-Other open wounds |
432 |
42 |
9.7 |
|
3880-Other ear disorders |
3,019 |
281 |
9.3 |
|
8030-Skull fracture without intracranial injury |
460 |
35 |
7.6 |
|
8480-Sprains & strains |
19,846 |
1,111 |
5.6 |
|
2460-Disorders of thyroid |
3,592 |
198 |
5.5 |
|
6290-Disorders of female genital organs |
1,582 |
63 |
4.0 |
|
0440-Asymptomatic HIV positive |
8,438 |
262 |
3.1 |
|
3040-Substance dependence/drugs (child) |
100 |
1 |
1.0 |
|
3030-Addiction disorder/alcohol (adult) |
8,069 |
0 |
0.0 |
|
3030-Substance dependence/alcohol (child) |
39 |
0 |
0.0 |
|
3040-Addiction disorders/drugs (adult) |
7,167 |
0 |
0.0 |
|
Unknown, missing, invalid codes |
145,328 |
8,284 |
5.7 |
|
SOURCE: Unpublished table provided by the Office of Disability and Income Support Programs, SSA. |
|||



















































































































