CHAPTER ELEVEN
Public Health
Extreme heat can be fatal, and hurricanes and tornadoes cause injuries and damage infrastructure. Air pollution can be linked to respiratory illness, and drought can lead to malnutrition. These are just a few examples of how weather and climate can influence human health. Climate change has the potential to affect any health outcome that is sensitive to environmental conditions. However, the causal chain linking climate change to shifting patterns of health threats and outcomes is complicated by factors such as wealth, distribution of income, status of public health infrastructure, provision of preventive and acute medical care, and access to and appropriate use of health care information. As with many other consequences of climate change, concurrent changes in nonclimatic factors, such as combustion-related air pollution, will influence the severity of future health impacts.
Questions decision makers are asking, or will be asking, about climate change and public health include the following:
-
What climate change effects are potentially the most dangerous to human health, and who is most at risk?
-
What kinds of preventative measures and response systems can be put in place to manage these risks?
-
Are there lessons that can be learned from other threats to human health?
-
What kinds of monitoring systems are available to track the health impacts of climate change?
-
How do we help ensure that actions taken to limit or adapt to climate change do not result in unintentional adverse health impacts?
-
What actions to limit and adapt to climate change will yield public health co-benefits?
This chapter summarizes the current understanding of the health effects of climate change from stressors such as temperature, severe weather, infectious disease, and air quality. It also reviews how health may be affected—in negative or positive ways—by many of the strategies societies use to limit, prepare for, and adapt to climate change (Figure 11.1). More extensive discussions of the relationship between climate change
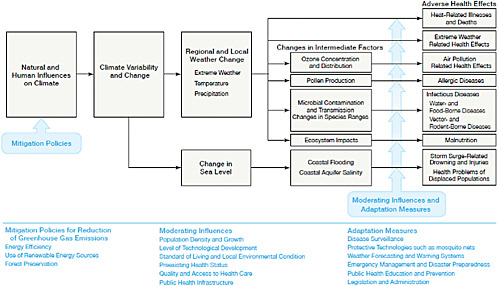
FIGURE 11.1 Simplified illustration of the mechanisms through which climate change can affect health outcomes. The blue text provides lists of policies or factors that can influence these health outcomes. Mitigation policies can potentially reduce the magnitude of climate change, while moderating influences (such as access to quality health care) or adaptation measures (such as improved public health education) could lessen the impact of adverse health effects. Mitigation and adaptation strategies will vary in the time necessary to implement them and realize their effects. SOURCE: Modified from Haines and Patz (2004).
and public health can be found in the recent synthesis of the U.S. Climate Change Science Program (CCSP, 2008a) and in other recent reports and syntheses (e.g., Confalonieri, 2007; Confalonieri et al., 2007). Additionally, this chapter identifies research needed to clarify exposure-response relationships, better quantify the impacts of climate change on human health, and identify efficient adaptation options.
EXTREME TEMPERATURES AND THERMAL STRESS
Heat waves are the leading causes of weather-related morbidity and mortality in the United States (CDC, 2006; Changnon et al., 1996). Between 1979 and 1999, some 8,015 deaths in the United States were heat related, and 3,829 of these were linked to weather conditions (Donoghue et al., 2003). As with other extreme events, the risk of heat waves is not evenly distributed across the country; for example, populations in the Midwest are at increased risk for illness and death during heat waves (CCSP, 2008a; Jones et al., 1982; Palecki et al., 2001; Semenza et al., 1996). Heat stress and heat waves are significant factors for increased morbidity and mortality in other parts of the world as well. A typical U-shaped curve (Figure 11.2) illustrates temperatures beyond which human mortality rates are observed to rise, depending on latitude.
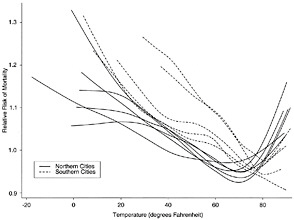
FIGURE 11.2 Temperature-mortality relative risk functions for 11 eastern U.S. cities for the period 1973 to 1994. Each city has its own line. Many northern cities (solid lines) exhibit a U-shaped curve, indicating that higher rates of mortality are exhibited at relatively cold and relatively warm temperatures. In the southern cities (dashed lines), mortality risks bear a stronger relationship with relatively cold temperatures. SOURCE: Curriero et al. (2002).
Hot days and hot nights have become more frequent in recent decades (Trenberth et al., 2007), and the frequency, intensity, and duration of heat waves are projected to increase in the decades ahead, especially under higher warming scenarios (CCSP, 2008a). By applying the magnitude of the 2003 European heat wave (see Box 12.1 in Chapter 12) to five major U.S. cities, Kalkstein et al. (2008) concluded that a heat wave of the same magnitude could increase excess heat-related deaths by more than five times the average. Projected excess deaths in New York City associated with such a heat wave, for example, would exceed the current average number of heat-related deaths nationwide each summer, with a death rate approaching that for all accidents.
There is also the potential, however, for warming temperatures to reduce exposure and health impacts associated with cold winter temperatures, although this potential is projected to vary by location (CCSP, 2008a). For example, research has shown that regions with milder winters actually have higher mortality rates during cold weather than regions with colder winters (Curriero et al., 2002; Davis et al., 2004). Seasonal variations in death rates in the United States are well documented, with more deaths occurring during winter than during summer months (Curriero et al., 2002; Macken-bach et al., 1992). However, mortality rates are influenced by a range of factors other than temperature, including housing characteristics and personal behaviors, which have not been extensively studied in the context of future climate projections. Thus, determining whether warming temperatures could alter winter temperature mortality relationships is complex and requires understanding all of the factors involved.
There have been several attempts to project future heat-related health impacts of climate change, and this is an active, albeit not large, area of current research. Figure 11.3 shows a schematic illustration of the expected impacts of warming temperatures and increased number of hot days on human health. Figure 11.4 shows a projection of total increases in heat-related deaths for a major U.S. city (Chicago) experiencing a
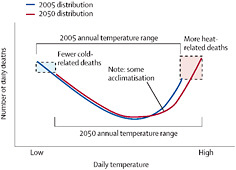
FIGURE 11.3 Schematic representation of the relationship of temperature-related deaths and daily temperature assuming no adaptation measures. The 2050 range of daily temperature (red curve) is shifted to the right of the 2005 range of daily temperature (blue curve), indicating that there could be an increase in heat-related deaths and a decrease in cold-related deaths. SOURCE: McMichael et al. (2006).
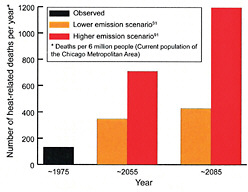
FIGURE 11.4 Potential increases in heat-related deaths in Chicago as a result of temperature increases over the 21st century. The graphs correspond to three-decade averages, centered on 1975, 2055, and 2085. Orange corresponds to climate projections with lower emissions and relatively less warming, and red corresponds to higher emissions and relatively more warming. SOURCES: USGCRP (2009a) and Hayhoe et al. (2010).
typical heat wave at three different future dates. One challenge with projecting future health impacts of heat waves is uncertainty about the extent to which people will acclimatize to higher temperatures. Uncertainty regarding adaptation strategies is also a challenge for projecting health impacts. For example, implementation of early warning systems and alteration of infrastructure to reduce urban heat islands could help minimize the impacts of heat waves by increasing adaptive capacities in communities.
SEVERE WEATHER
Deaths and physical injuries from severe weather events such as hurricanes, tornados, floods, and wildfire occur annually across the United States. Direct morbidity and mortality increase with the intensity and duration of such an event and can decrease with advance warning and preparation (CCSP, 2008a). While uncertainties remain, the general trend is that climate change will lead to an increase in the intensity of several types of severe weather events, such as flooding (see Chapter 8). Severe weather events may also lead to increases in diarrheal disease and increased incidence of respiratory symptoms, particularly in developing countries (CCSP, 2008a; Haines and Patz, 2004). Extreme events can also affect health indirectly. The mental health impacts (e.g., posttraumatic stress disorder, anxiety, and depression) of extreme events could be especially important, but they are difficult to assess (CCSP, 2008a; Haines and Patz, 2004).
INFECTIOUS DISEASES
The ranges and impacts of a number of important pathogens may change as a result of changing temperatures, precipitation, and extreme events (Confalonieri et al., 2007; Gage et al., 2008; Paaijmans et al., 2009; Pascual et al., 2006; Patz et al., 2008), resulting in greater human exposures in many parts of the world. Increasing temperatures may expand or shift the ranges of disease vectors, including mosquitoes, ticks, and rodents. Mosquito-borne diseases that may be affected by climate change include malaria, dengue fever, the West Nile virus, and the Saint Louis encephalitis virus. The West Nile and encephalitis viruses have both been associated with drought conditions brought on by extended periods of high temperatures (CCSP, 2008a; Haines and Patz, 2004). The range of the dog tick Rhipicephalus sanguineus that carries Rocky Mountain spotted fever may also expand due to increasing temperatures (Parola et al., 2008). Other tickborne diseases that may be impacted by increasing temperatures include Lyme disease and encephalitis. Rodent-borne diseases such as the hantavirus and leptospirosis may also be impacted by climate change. Aside from climate change impacts on vector-borne diseases, several pathogens that cause food- and waterborne diseases are sensitive to changes in temperature, with faster replication rates at higher temperatures. In addition, waterborne disease outbreaks (e.g., cholera outbreaks in developing countries) are also associated with heavy rainfalls and flooding (Confalonieri et al., 2007).
While vector-borne diseases will all be affected by climate-related changes in temperature, humidity, rainfall, and sea level rise, the geographical range of disease vectors depends on a variety of other factors, including population movement, land use change, public health infrastructure, and emergence of drug resistance (CCSP, 2008a; Haines and Patz, 2004). In addition, while there is wide range of vulnerability to disease within and between populations, this is also dependent on multiple, interacting factors (e.g., preexisting conditions such as malnutrition). Greater understanding of the factors contributing to the spread of infectious diseases, and the role that a changing climate will play in that spread, is needed.
AIR QUALITY
Many constituents of the atmosphere that impact public health also play a significant role in influencing climate. Of concern are aerosols, including black carbon, organic carbon, and sulfates. As discussed in Chapter 6, aerosols can have a net cooling effect on climate if they increase the Earth’s reflectivity, such as inorganic carbon released during biomass burning, or a net warming effect if they absorb outgoing infrared radi-
ation, such as the black carbon released during incomplete combustion of diesel fuel and biomass burning. Aerosols are of concern for human health due to their impacts on lung function and on respiratory and cardiac disease (Smith et al., 2009).
Tropospheric ozone is not only a greenhouse gas (GHG); it is also classified as a criteria air pollutant. Ozone is a secondary pollutant formed from the action of sunlight on ozone precursors such as carbon monoxide, nitrogen oxides, and volatile organic compounds (see Chapter 6). Human-caused emissions of ozone precursors have led to large increases in tropospheric ozone over the past century (Marenco et al., 1994; Wang and Jacob, 1998). When increased ozone events occur simultaneously with heat waves, the mortality rate can rise by as much as 175 percent (Filleul et al., 2006). Acute exposure to elevated concentrations of ozone is associated with increased hospital admissions for pneumonia, chronic obstructive pulmonary disease, asthma, allergic rhinitis, and other respiratory diseases, and also with premature mortality (e.g., Bell et al., 2005, 2006; Gryparis et al., 2004; Ito et al., 2005; Levy et al., 2005; Mudway and Kelly, 2000). A National Research Council committee concluded that “the association between short-term changes in ozone concentrations and mortality is generally linear throughout most of the concentration ranges. If there is a threshold, it is probably at a concentration below the current ambient air standard” (NRC, 2008e).
Although projected increases in temperatures across the United States in the decades ahead may raise the occurrence of high ozone concentrations (see Figure 11.5), ozone concentrations also depend on a wide range of other factors, including the rate and amount of ozone precursor emissions, human actions taken to limit ozone precursors, and meteorological factors. For example, extremely hot days tend to be associated with stagnant air circulation patterns that can concentrate ground-level ozone, exacerbating respiratory diseases and short-term reductions in lung function (USGCRP, 2001). Under one scenario of climate change for 50 U.S. cities, the increase in temperature projected to occur by the 2050s due to climate change, and a subsequent rise in tropospheric ozone, could exacerbate ozone-related health effects such as cardiovascular, respiratory, and total mortality, as well as hospital admissions for asthma, chronic obstructive pulmonary disease, and respiratory diseases of the elderly (Bell et al., 2007).
Climate change could also affect local and regional air quality through temperature-induced changes in chemical reaction rates, changes in boundary-layer heights that affect vertical mixing of pollutants, and changes in airflow patterns that govern pollutant transport. Responses to climate change can also affect air quality, most notably through changes in emissions associated with efforts to limit the magnitude of climate change. Sources of uncertainty include the degree of future climate change, future emissions of air pollutants and their precursors, and how population vulnerabil-
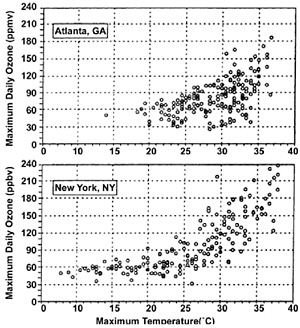
FIGURE 11.5 Ground-level ozone concentrations and temperature in Atlanta and New York City, measured between May and October, 1988 to 1990. The plots show that ozone concentrations are generally higher at warmer temperatures. SOURCE: USGCRP (2009a); based on EPA data.
ity may change in the future. When precursor emissions are held constant, projections suggest climate change will increase concentrations of tropospheric ozone across many regions, increasing morbidity and mortality (Ebi and McGregor, 2008). Increases in urban ozone pollution alone could be as much as 10 parts per billion (ppb) over the next few decades, which would make it difficult for many cities to meet air quality standards (Ebi and McGregor, 2008; Jacob and Winner, 2009). The evidence is less robust for other air pollutants, although several studies have found increased mortality associated with simultaneous rise in temperature and surface aerosols, including both particulate matter and sulfur dioxide (Hu et al., 2008; Katsouyanni et al., 1997; Smith et al., 2009). However, research is needed to understand how concentrations of these pollutants could change with climate change.
There are several examples of how the health impacts of climate change intersect with ecosystem and agricultural impacts in the context of air quality. For example, higher ozone concentrations would be detrimental not only to human health but also to crop
production. Losses in crop yields due to increasing ozone and other climate-related factors over the next two to three decades in some rapidly developing regions are expected to have a major impact on the food supply (see Chapter 10), possibly leading to malnutrition and other negative public health impacts (CCSP, 2008a; Epstein, 2005; Haines and Patz, 2004; The Royal Society, 2009). Another example is that the frequency and intensity of wildfires is enhanced in a warming climate (see Chapter 9), and this would be expected to lead to increases in the atmospheric concentration of fine particulate matter, which would have adverse health consequences (Epstein, 2005; Haines and Patz, 2004).
The potential synergies and trade-offs between climate change policies and public health policies are complex. For example, reducing some aerosols such as organic carbon or sulfates would reduce air pollution-related health impacts but increase the rate of climate change (Forster et al., 2007; see also Chapter 6). Conversely, some of the technologies and policy mechanisms that might be used to control climate change may also be complementary to measures adopted to control air pollution; for example, reducing commuter traffic by encouraging mass transit and carpooling would reduce both transportation-related GHG emissions and ozone precursors. Walking or biking for transportation would have the added benefit of increasing physical activity, potentially lowering the incidence of obesity and its related negative health outcomes. Policies designed to reduce or offset climate change may thus have a variety of intended and unintended consequences on public health, and vice versa.
OTHER HEALTH EFFECTS OF CLIMATE CHANGE
Allergies and asthma are influenced by the growth and toxicity of numerous plant species like ragweed, poison ivy, and stinging nettle; based on limited evidence, these plants increase growth and toxicity at higher temperatures and/or concentrations of CO2 (Hunt et al., 1991; Mohan et al., 2006; USGCRP, 2009a; Ziska, 2003). Drought, changes in water resources (Chapter 8), and climate impacts on agricultural production (Chapter 10) all may have consequences for human health and nutrition (CCSP, 2008a; Epstein, 2005; Haines and Patz, 2004). There could also be an increase in psychiatric disorders, such as anxiety and depression, occurring after severe weather events that cause a disruption of the home environment and economic losses (CCSP, 2008a; Haines and Patz, 2004). Shifts in migration patterns and refugee pressures may result from changes in sea level, food production, severe weather, and drought, resulting in additional human health challenges in some areas.
PROTECTNG VULNERABLE POPULATIONS
Not everyone is equally at risk from the health impacts of climate change (CCSP, 2008a; Confalonieri, 2007). For example, in the United States, cities with cooler climates generally experience more heat-related mortality than cities with warmer climates. This difference is attributed to the ability of populations to acclimatize to different levels of temperature through physiological, behavioral, and technological mechanisms (Haines and Patz, 2004). The heat island effect can result in residents of high-density urban areas being more vulnerable to heat-related health effects (CCSP, 2008a). Residents of low-lying coastal areas could be particularly vulnerable to the health impacts associated with sea level rise, coastal erosion, and more intense storms (CCSP, 2008a). Other reasons for geographic differences in vulnerability include differences in physical, ecological, and activity-related exposure to the risks within and across countries; differences in sensitivity due to the overlap with other changes and stresses in particular regions or populations; and widely varying adaptive capacities. In addition to geographic variations, certain subpopulations could also be more susceptible to the health impacts of climate change. These groups include infants and children, pregnant women, older adults, impoverished populations, people with chronic conditions, people with mobility and cognitive restraints, certain occupational groups, and recent migrants and immigrants. The specific vulnerabilities of these population groups are outlined in Table 11.1.
Responses to recent extreme weather and climate events such as Hurricane Katrina show that, even in the United States, current levels of adaptation are insufficient (US-GCRP, 2009a). Substantial inequities exist in access to public heath infrastructure, both in the United States and elsewhere (Pellow and Brulle, 2007), so health risks will be disproportionately high for the poor, elderly, and otherwise disadvantaged. Additionally, analysis has shown that, without further investment, the public health infrastructure most important for addressing the challenges of climate change could be insufficient (Ebi et al., 2009). Concerted efforts will be needed to reduce the vulnerability of populations in both this country and the world, particularly the poorest and most marginalized.
The companion report Adapting to the Impacts of Climate Change provides a summary of potential adaptation strategies for human health (NRC, 2010a). For example, public health systems need to be strengthened to enable rapid monitoring, identification of, and response to new climate change-related health risks as they arise. Other societal stresses such as poverty or economic disadvantages, chronic work-related risks or exposure to otherwise unhealthy environmental conditions, lack of access to preventive and ongoing health care, insufficient emergency preparedness, and related
TABLE 11.1 Population Groups with Specific Vulnerabilities to Climate-Sensitive Health Outcomes
|
Groups with Increased Vulnerability |
Climate-Related Exposures |
|
Infants and children |
Heat stress, ozone air pollution, water- and foodborne illnesses, psychological consequences of extreme events |
|
Pregnant women |
Heat stress, extreme weather events, water- and foodborne illnesses |
|
Older adults |
Heat stress, air pollution, extreme weather events, water-and foodborne illnesses |
|
Impoverished populations |
Heat stress, extreme weather events, air pollution, vector-borne illnesses |
|
People with chronic conditions and mobility and cognitive restraints |
Heat stress, extreme weather events, air pollution |
|
Outdoor workers |
Heat stress, ozone air pollution, vector-borne illnesses |
|
Recent migrants and immigrants |
Heat stress, vector-borne illnesses, extreme weather events |
|
SOURCE: Modified from NRC (2010a) with information from CCSP (2008a). |
|
institutional gaps or lack of effective collaboration (as was apparent in the response to Hurricane Katrina) will make effective preparation for and adaptation to climate change impacts on health more difficult. However, adaptive capacity and preparedness can be enhanced by addressing those underlying chronic problems where they persist. In addition, explicit consideration of climate change is needed within federal, state, and local programs (including nongovernmental services) and research activities to ensure that they have maximum effectiveness.
RESEARCH NEEDS
Systematically investigate current and projected health risks associated with climate change. Research is needed to develop a more complete understanding of the health effects of weather and climate events (temperature, heat waves, and severe weather) within the context of other drivers of climate-sensitive health outcomes (age, wealth, fitness, and location). This area of research has seen significant progress during the past decade but needs to be expanded more systematically in the United States and around the world. Key to this analysis is the development of reliable methods to link and quantify the relationships between climate change, and changes in food systems, water supplies, air pollution, and health outcomes.
Advance research on how air quality, heat waves, and the transmission of vector-borne diseases will change. Although several efforts have been made to project future morbidity and mortality effects of climate change-related ozone concentrations, there are currently few efforts to model the impact of climate change on other air pollutants (CCSP, 2008a). Refining projections of the frequency and occurrence of hot days and the range of disease-spreading species is necessary for effective adaptation planning and decision making. New science is needed to provide information for dealing with the impacts of climate change on public health, both nationally and internationally, keeping in mind the transboundary transport of air pollutants and disease vectors.
Characterize the differential vulnerabilities and adaptive capacity levels of particular populations to climate-related impacts, and the multiple stressors they already face or are likely to encounter in the future. The likelihood that various people and regions will suffer adverse health impacts related to climate change depends on (1) their exposure to climatic and other changes; (2) their sensitivity to these stressors, some of which are population- or person-specific (e.g., age, race) and some of which are modified (often magnified) by concurrent, nonclimatic multiple stresses; and (3) their capacity to cope, respond, and adapt to extreme events and health-related climatic changes. The latter in particular is affected by the status of and access to local public health infrastructure, including early warning systems, and human, social, and financial capital. Specific features of the local geographic and environmental situation also can affect the capacity to adapt.
Identify effective, efficient, and fair adaptation measures. Incorporating proactive adaptation into public health and health care planning would increase resilience to the health impacts of climate change. Improvements in health care interventions, access to health care, medical technologies, disease-vector surveillance systems, comprehensive heat-health warning systems, and raising awareness among health care providers are examples of such proactive measures. There are many other opportunities, however, for developing additional adaptation options. For example, seasonal and finer-scale forecasts can be used to develop early warning systems that could increase resilience to climate variability and extreme events.
Evaluate and develop effective information, education, and outreach strategies. Linking knowledge to action through partnerships with private, public, and nongovernmental organizations, and faith communities, and carefully building effective information, education, and outreach strategies that bring credible health information to potentially affected populations will be a critical element of increasing adaptive capacity and responses in the health sector. In addition, local and state
governments can be instrumental in building awareness of climate-related health impacts and adaptation options among health care providers, caregivers, and potentially affected populations. The effectiveness of various outreach efforts in affecting human behavior requires careful research and testing in place-based contexts that take advantage of local knowledge and perspectives and the particulars of social networks.














