Workshop Summary
When a nation or region prepares for public health emergencies such as a pandemic influenza, a large-scale earthquake, or any major disaster scenario in which the health system may be destroyed or stressed to its limits, it is important to describe how standards of care would change due to shortages of critical resources. Such “crisis standards of care” are the level of health and medical care capable of being delivered during a catastrophic event (whether naturally occurring or manmade). To ensure that fair and equitable care is provided to patients in a catastrophic event, nations and regions need a robust system to guide the public, health care professionals and institutions, and governmental entities at all levels.
Crisis standards of care has been the focus of several recent and ongoing Institute of Medicine (IOM) activities, including a series of workshops (IOM, 2010) and a letter report, Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations (IOM, 2009). An IOM consensus committee is currently updating the preliminary guidance issued in the 2009 letter report, and is expected to issue a full report in 2012.1
Building on these activities, the IOM Forum on Medical and Public Health Preparedness for Catastrophic Events sponsored a session at the 17th World Congress on Disaster and Emergency Medicine (WCDEM), held May 31 to June 3, 2011, in Beijing, China.2 The session, moderated
_______________________
1See http://iom.edu/Activities/PublicHealth/DisasterCareStandards.aspx for further information.
2The role of the ad hoc planning committee of the IOM Forum on Medical and Public Health Preparedness for Catastrophic Events was limited to developing this session for
by Mark Keim, senior science advisor for the Office of the Director in the National Center for Environmental Health at the Centers for Disease Control and Prevention, focused on opportunities and challenges to integrate crisis standards of care principles into international disaster response plans.
The workshop used the IOM’s Crisis Standards of Care as a means to stimulate a discussion among international stakeholders. Expert panelists discussed:
- The challenges of providing fair and equitable care in mass casualty incidents
- A potential framework for the equitable delivery of care in situations of scarce resources, and strategies for operationalizing crisis standards of care in austere environments
- Strategies for integrating crisis standards of care principles into disaster response plans
- The impact of international disaster response on changing the standard of care in the “host” country
This report summarizes the presentations and commentary by the invited panelists.
SURGE CAPACITY PLANNING AND CRISIS STANDARDS OF CARE
In the United States, catastrophic disasters have been relatively infrequent events. For the purposes of this discussion, such events have been historically considered as those in which there are around 1,000 or more human casualties, explained Dan Hanfling, special advisor for Emergency Preparedness and Response at Inova Health System. Catastrophic disasters in the late 1800s and early 1900s were generally natural disasters (e.g., flash floods, forest fires) or transportation-related incidents (e.g., sinking steamships). Excluding the 1918 influenza pandemic and casualties of war, the U.S. health care system was not faced with catastrophic disasters for most for the 20th century. However, the terrorist attacks of 2001 and the devastation from Hurricane Katrina in the Gulf Coast in 2005 have
_______________________
the WCDEM. This summary has been prepared by the rapporteurs as a factual overview of the presentations at the session. Statements, recommendations, and opinions expressed are those of individual presenters and participants, and are not necessarily endorsed or verified by the IOM or the Forum.
focused new attention on standards of care in the context of mass casualty events and associated shortages of critical resources.
The 2009 H1N1 influenza pandemic, Hanfling noted, also brought to light several specific questions to consider as part of overall surge capacity planning: Which patients and health care providers should receive limited resources, and who decides? Should professional standards of care change? What are the triggers for implementation of a potential shift in the standards under which such care is delivered? Should there be legal mechanisms to protect health care workers acting in good faith under crisis circumstances? These questions would apply to both a slow onset incident, like a pandemic, or a no-notice incident like an earthquake.
Responses to recent large-scale disasters have demonstrated problems with efficacy and optimizing the international and national relief of the medical and health teams (Benjamin et al., 2011; Burnweit and Stylianos, 2011; Morton and Levy, 2011; Tappero and Tauxe, 2011). In addition, international disaster response brings a number of additional challenges given the large and varied number of organizations involved in providing immediate and long-term care. Each organization has different responsibilities, missions, systems, and authorities. However, there often are not a set of different clearly defined responsibilities between the different organizations, which lead to challenges in response and recovery where this division is unclear or non-existent. There are numerous open and unclear aspects to these issues, and they all influence the capacity and effective response in large scale disasters, especially those related to the provision of international relief (Peleg et al., 2011).
Defining Crisis Standards of Care
To begin to address issues regarding standards of care in national planning for response to mass casualties, the U.S. Department of Health and Human Services (HHS) Agency for Healthcare Research and Quality (AHRQ) released two reports, Altered Standards of Care in Mass Casualty Events (2005) and Providing Mass Medical Care with Scarce Resources: A Community Planning Guide (2007).3 AHRQ emphasized that there will be a “spectrum of patient care delivery options” available, and there needs to be stewarding of scarce resources to deliver a standard
_______________________
3Available in the AHRQ online archive at http://archive.ahrq.gov/research/altstand/ and http://archive.ahrq.gov/research/mce/ (accessed December 1, 2011).
of care appropriate and sufficient for the situation. Incident planning and response must recognize that standards will change, and protocols for triage will need to be adaptable. The reports note that along the spectrum of care, there will be some patients who are “too well” to receive care, and some who are too sick to survive, but all will need to receive some level of health care consideration.
Building on the AHRQ reports, Hanfling highlighted several publications describing the augmentation of scarce resources in a hospital critical care setting (Rubinson et al., 2005, 2008) and, recognizing that access to ventilators may be a limiting step in the delivery of care, the triage of ventilator resources during a public health emergency (Christian et al., 2006; Hick and O’Laughlin, 2006; Powell et al., 2008). Highlighted among these efforts, Hanfling said, was the use of a scoring tool—for example, the sequential organ failure assessment (SOFA)—as a means to help discern who would be most likely to benefit from access to a ventilator.
IOM Guidance for Establishing Standards of Care for Use in Disaster Situations
In the fall of 2009, at the request of the HHS Office of the Assistant Secretary for Preparedness and Response, the IOM established the Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations. As its first task, the committee issued a letter report describing a framework for establishing crisis standards of care (IOM, 2009).4
The IOM committee defined crisis standards of care as follows:
[A] substantial change in usual healthcare operations and the level of care it is possible to deliver, which is made necessary by a pervasive (e.g., pandemic influenza) or catastrophic (e.g., earthquake, hurricane) disaster. This change in the level of care delivered is justified by specific circumstances and is formally declared by a state government, in recognition that crisis operations will be in effect for a sustained period. (IOM, 2009, p. 3)
_______________________
4As noted earlier, this committee is now engaged in a second phase of deliberations to update the preliminary guidance in the letter report. A full report is expected in the spring of 2012.
Crisis standards of care would be implemented when standard contingency plans for a surge in demand for care are insufficient (Figure 1). As discussed in the 2009 IOM report, the surge capacity following a mass casualty incident falls into three basic categories, depending on the magnitude of the event: conventional, contingency, and crisis surge capacity (Hick et al., 2009). The categories will also represent a corresponding spectrum of patient care delivered during a disaster event. As the imbalance increases between resource availability and demand, health care—emblematic of the entire health care system—maximizes conventional capacity, then moves into contingency, and, once maximized, moves finally into crisis capacity. A crisis situation may lead to an overwhelming demand for services, and result in shortages of equipment, supplies, pharmaceuticals, personnel, and other critical resources, necessitating operational adjustments (Figure 2). Hanfling noted that under conventional and contingency responses, the focus of care is the patient; however, when the response shifts to crisis mode, the focus of care becomes more
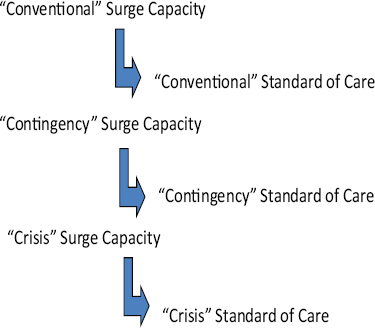
FIGURE 1 The operational flow of surge capacity planning and standards of care.
SOURCES: Hanfling presentation at WCDEM (based on Hick et al., 2009, and regional workshop presentations summarized in IOM, 2010).
of a population-based approach. As the continuum shifts to the right toward crisis care, continual efforts are made toward recovery and resupply to reestablish conventional care.
Summarizing the letter report, Hanfling noted that the committee stressed the need for fairness and equitable processes (transparency, consistency, proportionality, accountability) in decisions regarding altered standards of care. He also noted the need for stakeholder engagement and appropriate legal and regulatory authority.
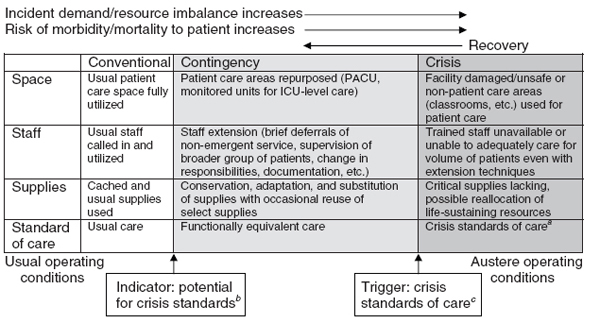
FIGURE 2 Continuum of incident care and implications for standards of care.
aUnless temporary, requires state empowerment, clinical guidance, and protection for triage decisions and authorization for alternate care sites/techniques. Once situational awareness achieved, triage decisions should be as systematic and integrated into institutional process, review, and documentation as possible.
bInstitutions consider impact on the community of resource use (consider “greatest good” versus individual patient needs—e.g., conserve resources when possible), but patient-centered decision making is still the focus.
cInstitutions (and providers) must make triage decisions balancing the availability of resources to others and the individual patient’s needs—shift to community-centered decision making.
SOURCES: Reprinted with permission from IOM (2009, p. 53). Originally adapted from Hick et al. (2009); Wynia (2009).
Principles to Guide Crisis Standards of Care
In order to ensure that patients receive the best possible care in a catastrophic event, the 2009 IOM report laid out a vision to guide the development of crisis standards of care. The report stated that the United States needs a robust system to guide the public, health care professionals and institutions, and governmental entities at all levels. To achieve such a system of just care, the committee set forth the following vision for crisis standards of care:
- Fairness—standards that are, to the highest degree possible, recognized as fair by all those affected by them (including the members of affected communities, practitioners, and provider organizations); evidence based; and responsive to specific needs of individuals and the population focused on a duty of compassion and care, a duty to steward resources, and a goal of maintaining the trust of patients and the community
- Equitable processes—processes and procedures for ensuring that decisions and implementation of standards are made equitably
![]() Transparency—in design and decision making
Transparency—in design and decision making
![]() Consistency—in application across populations and among individuals regardless of their human condition (e.g., race, age, disability, ethnicity, ability to pay, socioeconomic status, preexisting health conditions, social worth, perceived obstacles to treatment, past use of resources)
Consistency—in application across populations and among individuals regardless of their human condition (e.g., race, age, disability, ethnicity, ability to pay, socioeconomic status, preexisting health conditions, social worth, perceived obstacles to treatment, past use of resources)
![]() Proportionality—public and individual requirements must be commensurate with the scale of the emergency and degree of scarce resources
Proportionality—public and individual requirements must be commensurate with the scale of the emergency and degree of scarce resources
![]() Accountability—of individuals deciding and implementing standards, and of governments for ensuring appropriate protections and just allocation of available resources
Accountability—of individuals deciding and implementing standards, and of governments for ensuring appropriate protections and just allocation of available resources
- Community and provider engagement, education, and communication—active collaboration with the public and stakeholders for their input is essential through formalized processes
- The rule of law
![]() Authority—to empower necessary and appropriate actions and interventions in response to emergencies
Authority—to empower necessary and appropriate actions and interventions in response to emergencies
![]() Environment—to facilitate implementation through laws that support standards and create appropriate incentives
Environment—to facilitate implementation through laws that support standards and create appropriate incentives
The report also included guidance to assist state public health authorities in developing these crisis standards of care. This guidance includes criteria for determining when crisis standards of care should be implemented, key elements that should be included in the crisis standards of care protocols, and criteria for determining when these standards of care should be implemented. The five key elements that should be included in crisis standards of care protocols, along with associated components, are summarized in Table 1.
TABLE 1 Five Key Elements of Crisis Standards of Care Protocols and Associated Components
| Key Elements of Crisis Standards of Care Protocols |
Components |
| Ethical consideranons |
|
| Community and provider engagement, education, and communication |
|
| Key Elements of Crisis Standards of Care Protocols |
Components |
| Legal authority and Environment |
|
| Indicators and triggers |
Indicators for assessment and potential management
|
Triggers for action
|
|
| Key Elements of Crisis Standards of Care Protocols |
Components |
|
|
| Clinical process and operations |
Local/regional and state government processes to include
|
Clinical operations based on crisis surge response plan:
|
|
While the crisis standards of care principles discussed at the workshop and this summary are derived from a national (U.S.) perspective, it was the view of some of the participants that these principles could be at least partially extrapolated to an international
perspective. The crisis standards of care definition established by each country or response agency, while reliant on the same set of foundational principles, will need to consider the cultural values and priorities when establishing its own definition.
Crisis Standards of Care as Part of the Overall Surge Capacity Planning Framework
Hanfling reiterated that standard of care is a continuum that ranges from conventional and contingency to crisis care. He suggested that standard of care is part of an overall framework for response, incorporating planning, substituting, adapting, reusing, and reallocating resources. There must be situational awareness that a response is shifting away from a conventional response to a contingency or crisis response because of the changing availability of resources. A participant correctly noted that one variable that is changing as a crisis evolves is the provider’s scope of practice; the provider is still providing the highest level of standard of care within that evolving scope of practice or set of emerging circumstances.
Developing National/Regional Crisis Standards of Care: The Duty to Plan
Hanfling stressed that there is a moral responsibility to plan for catastrophic events. The IOM committee stated that
in an important ethical sense, entering a crisis standard of care mode is not optional—it is a forced choice, based on the emerging situation. Under such circumstances, failing to make substantive adjustments to care operations—i.e., not to adopt crisis standards of care—is very likely to result in greater death, injury, or illness. (IOM, 2009, p. 15)
Along these same lines, Yoshikura Haraguchi, formerly of the Division of Pathophysiology at National Hospital, Tokyo Disaster Medical Center, Tachikawa City, Tokyo, Japan (retired), said the aim of disaster medicine is to foster the development of a resilient society and to facilitate recovery. He noted that the prime minister of Japan has referred to a concept of working toward a “society of minimal misfortune.”
Haraguchi defined the key elements of a systematic disaster medicine approach as ethics; transparency, communication, and legal support; reliability and trust; responsibility and accountability; and public education to achieve “disaster literacy.” Comfort, compassion, dignity, fairness, equitability, and consistency are critical, especially for vulnerable populations (e.g., children, women, the elderly, the impoverished).
It must also be recognized that catastrophic response to disasters are actually long-term events, which may last weeks and months. When considering standards of care, we must consider the long-term recovery phase and capacity building, not just the acute phase response, Hanfling said, citing the work of Subbarrao and colleagues (2010). Countries have very different levels of health care and different governance structures, yet there is a need for balanced and consistent international response.
Hanfling highlighted several key components that may serve to help develop uniform crisis standards of care:
- Incorporate a crisis response framework at the very outset of the acute phase of response efforts
- Monitor use of resources to attain achievable and desirable outcomes
- Establish consistency of health care delivery strategies:
![]() Respect the sovereignty of the “host nation”
Respect the sovereignty of the “host nation”
![]() Develop consistent use of foreign medical teams (based on an opt-in classification approach)
Develop consistent use of foreign medical teams (based on an opt-in classification approach)
![]() Set goals for long-term recovery early in the response; emphasize transition of services
Set goals for long-term recovery early in the response; emphasize transition of services
![]() Understand role of palliative care in planned clinical response
Understand role of palliative care in planned clinical response
Jean Luc Poncelet, area manager in Emergency Preparedness and Disaster Relief for Latin America and the Caribbean, Pan American Health Organization/World Health Organization (WHO), noted that a challenge to developing standards and criteria is the variety of mass casualty incidents that are scattered broadly across a large geographic region and attended to by different actors at different times. The standards applicable to a plane crash, for example, may be different from those relevant to a hospital fire, which may be different again from a volcanic eruption.
Operationalizing Crisis Standards of Care in Diverse International Settings
The Japanese Experience
Haraguchi described the Japanese experience with the 2011 earthquake and subsequent nuclear crisis as a “mega-disaster,” or catastrophic health event. Such a catastrophic event can trigger a “malignant cycle” of increasing distress. For example, an earthquake may directly cause other natural disasters (e.g., landslide, tsunami, fire, flood) and building destruction, leading to general trauma and specific diseases, as well as secondary artificial and complex disasters (e.g., traffic system failure; chemical hazard from factories or traffic incidents; biological hazard; nuclear hazard). Shortages of care and supplies result, apathy sets in, and public health and mental health issues emerge, both in victims and caregivers. Downstream, there is rumor and/or demagogy, societal unrest, gradual spread of economic crisis, national crisis, and a broken medical system, all of which can have global impact far beyond the borders of the original event. Interruption at each step in the malignant cycle, through appropriate planning and implementation of plans, is essential, Haraguchi said.
Experiences from Latin America and the Caribbean
Poncelet explained that following a succession of major disasters in Peru in 1970, Nicaragua in 1972, and Guatemala in 1976, the Minister of Health for the region called for a common approach to disaster response, and thus began casualty management in Latin America and the Caribbean. The main goal was to optimize available resources to save lives, while respecting national health practice and criteria.
Poncelet highlighted some special issues of casualty management for the small islands in the Caribbean, which usually have only one health facility. Therefore, a special program has been in place now for more than 15 years to train first responders. In remote areas, the first responders are the community members who are on scene in the first minutes or hours of the response. Thus far more than 1,000 health, police, fire, defense force, and airport staff have been trained in the English-speaking Caribbean, Poncelet said, and mass casualty management plans and teams have been established in many islands. Triage, he noted, remains the responsibility of senior health professionals.
Before the January 2010 earthquake in Haiti, enough hospital beds were available for victims in most of the mass casualty incidents in Latin America and the Caribbean. The conditions and experience in Haiti, however, were completely different, Poncelet said. Under normal circumstances, the local capacity in Haiti is quickly saturated, even during a small event, and victims are generally evacuated to other countries (e.g., Guadeloupe or Martinique). There is emergency training in Haiti, but it is of limited impact as no real ambulance or emergency services exist. Following the earthquake, triage services were limited to the few very experienced non-governmental organizations (NGOs) already in the country, and to some well-prepared field hospitals and medical teams. The triage criteria were very different from one institution to another, all justifiable, Poncelet said, but with different perspectives. Poncelet also noted the tendency to forget about mass fatalities. The fatality rate in Haiti was extreme and it became impossible, he said, to fully adhere to guidelines that had been established before the earthquake for the management of dead bodies.
Barriers and Challenges to Operationalizing Crisis Standards of Care
The health community has been working on mass casualty management for many years, Poncelet said, so what is stopping us from making progress? An obvious barrier to progress is funding; this is challenging in wealthy countries, and even more so in lower-income countries. Government leadership is looking for a return on their investment, a demonstration of positive impact. But, Poncelet explained, there is no real way to demonstrate the economic return on investment in casualty management, in part because events are so rare. What is measurable, he suggested, is progress in capacity building, especially when measured against preestablished criteria and through simulation exercises.
Frederick “Skip” Burkle, senior fellow at the Harvard University Humanitarian Initiative, added that rapid urbanization compounds the challenge. Urbanization is the stronghold of the economy in most countries, but during periods of rapid urbanization, the population exceeds the existing public health infrastructure.
Participants also discussed some of the legal concerns, including the case of Anna Pou, a physician who found herself facing criminal charges for decisions she made while working in a hospital with no electricity and a large number of very ill patients in New Orleans immediately after
Hurricane Katrina. Although the criminal cases were dismissed, she is still facing civil charges. It was noted that legal mechanisms under discussion could provide some protections for health care providers operating under the most challenging conditions. This also emphasizes the importance of having a well-planned, well-articulated, proactive response plan, Hanfling said, so the need for reactive decision making is reduced. This can best be achieved through improved assessment and coordination prior to and during the initial response.
A concern was raised that in the setting of an event resulting from terrorism, the flow of information will likely not be as forthcoming as it would be in a natural disaster.
A disconnect was also noted between the international humanitarian community and national authorities. The international community makes rules, regulations, and standards for itself that are not necessarily comparable to or compatible with what is being done by the national authorities (if anything is being done at the national level).
Haraguchi stressed that ethics is the foundation of crisis standards of care. He applied classical philosophy to the question of ethics in disaster medicine, citing the concepts of utilitarianism, or “the greatest good for the greatest number of people,” proposed by Bentham and Mill, and the Maximin Principle of Rawls, which seeks justice or fairness by providing the greatest benefit to those who are the worst off.
Hanfling added that respect for the host nation or region is paramount. Response planning needs to be done in the context of the existing capabilities, with an understanding of the local strengths, weaknesses, gaps, culture, etc. The goal is to develop an ethical framework for thinking about the delivery of care in crisis. Burkle noted that the basic disaster cycle is “prevention, response, and recovery,” but Australia has added “anticipation” and “assessment” to the front end of the cycle (Rogers, 2011). Specifically, information on communities is collected at the national level to better understand the different characteristics and risks of different communities. The time for such assessment, Burkle stressed, is before a crisis so that when something happens, needs are already known.
Poncelet said that ethical standards of care can be more readily agreed to among neighboring and similar countries whose income,
technical capacity, and approach to care are similar. It is easier to be fair, Poncelet said, when everyone is operating in an environment that is limited by the same conditions and functionality. Crisis standards of care should be at least as fair as conventional standards in day-to-day operations.
The international response to the 2010 earthquake in Haiti provides several examples of the ethical dilemmas faced in trying to provide the highest level of care to the greatest number of victims in a disaster response. Hanfling cited an article on the Israeli field hospital in Haiti (Merin et al., 2010), which described their basic triage approach: how urgent is the patient’s condition, are there adequate resources to meet the patient’s needs, and can the patient’s life be saved with the interventions offered? The U.S. government (Bureau for Medicine and Surgery of the U.S. Navy and the U.S. Navy Ship Comfort), working with the Ministry of Public Health in Haiti (Ministere de la Santé Publique et de la Population), recognized the dilemma of implementing short-term solutions (i.e., amputation) and the effect these had on long-term impacts, and discouraged practitioners from offering complex medical treatments or surgical interventions that could not be sustained in Haiti after the end of the international disaster relief effort (Etienne et al., 2010). Poncelet noted that as each country assesses its mass casualty management plan or response using their own criteria, it can be very difficult to address questions of ethics. In the case of Haiti, for example, serious ethical questions persist regarding standards of care and the resulting amputee crisis.
Many difficult ethical questions need to be considered, Poncelet said. For example, should a foreign medical team work below its capacity to be fair and provide care comparable with another country’s capabilities? In other words, is the “lowest common denominator” of care an ethical solution? Should a trauma technique be implemented when the foreign team knows that they will leave before the follow-up process ends? Or, correspondingly, can a team refuse to provide some type of treatment because follow-up will not or cannot be provided by the host country?
Community and Stakeholder Engagement and Education
All participants discussed the importance of community and provider engagement and education. Any process is of little value without community support and education of professionals regarding how to
implement the process. Only through the training of nationals, and relevant national authorities, as they are the first responders and final authority, will we be able to find a long-term sustainable solution to crisis care, Poncelet said. Disaster medicine needs to solve community-level issues, Burkle agreed, and added that we have to find ways to make it more attractive to work at the community level.
Hanfling and Burkle stressed the importance vetting crisis triage processes at the community level during the planning stages, and Hanfling noted that the IOM committee is exploring the issue of community engagement in some detail as part of its current task. Keim added that a community often feels empowered by engagement in planning activities before the disaster, but is then disempowered by the multitude of national and international responders that often take over decision making.
Panelists discussed the need for, and impact of, financial and social incentives to encourage stakeholder participation. Poncelet stressed the importance of showing the community the benefit of disaster preparedness. He noted that the World Bank has decided that it is economically beneficial to be involved in disaster preparedness, and this drives their involvement.
Many participants also noted that a positive messaging approach is more effective than negative messaging. Haraguchi explained the Japanese philosophy as one that encourages learning about and preparing for disaster, so that people can work together positively to overcome disaster and continue to enjoy life.
The benefits of including diverse stakeholders at the table were also discussed. A participant pointed out that employers, unions, farm collectives, and other similar organizations should be included in planning discussions as they have vested interests in disaster preparedness, facing financial risk in the case of epidemic diseases or terrorism. In most developed countries, these entities also pay a large portion of insurance premiums for their workers. It was also noted that involving transnational corporations may help to foster a more level playing field among nations that may not cooperate naturally. If these stakeholders are not actively engaged, then they are likely not to adopt the new standards in their plans.
THE INTERNATIONAL HEALTH REGULATIONS TREATY
Burkle from Harvard described the International Health Regulations (IHR) Treaty.5 The 2003 SARS pandemic shook up the global health community, Burkle said. Up until that point, WHO had maintained a passive relationship with countries, offering expertise, but respecting the sovereignty of countries (i.e., countries can refuse WHO assistance). However, the World Health Assembly of Ministers of Health, realizing the severity of the outbreak, held an emergency session and granted WHO the authority to intervene. Thus, WHO evolved from its short-term, geographically focused capacity to having global authority with sustained long-term prevention, preparedness, and response responsibilities. This was instrumental in controlling SARS, Burkle said. The new WHO authority was formalized as the IHR Treaty, which entered into force in 2007.
A key to success of the treaty is striking the right balance between the sovereignty of individual nation-states and the common good of the international community. The treaty obligates WHO to obtain expert advice on any declared public health emergency of international concern, and provide that advice to nation-states. The treaty also encourages countries to provide each other with technical and logistical support for capacity building.
IHR will influence the establishment of crisis standards of care by emphasizing the importance of information sharing and exchange in disaster situations. The importance of situational awareness in helping to support proactive decision making cannot be overstated. With regard to standards of care capacities, the IHR treaty:
- Establishes systematic approaches to surveillance early warning systems and response (countries must establish core capacities for surveillance and response by 2012)
- Requires National Focal Points to ensure a two-way channel of communications between WHO and member states
- Requires countries to share information relevant to public health risks
- Introduced a decision instrument algorithm, Annex 2, for public health action (see Figure 3)
_______________________
5See http://www.who.int/ihr/en/index.html (accessed on December 19, 2011).
A recent survey mentioned by Burkle suggests that many nation-states still lack core capacities to detect, assess, and report risks, and may not meet the 2012 deadline. Sixty percent of the 194 nation-states responded to the survey; only 58 percent had national plans, and less than 10 percent indicated they had fully established the IHR capacities required under the Treaty.
Burkle noted that a primary barrier to achieving the goals of the Treaty is the lack of any enforceable sanctions. In the absence of legal consequences, there has instead been a system of “shame and blame” to push countries along. (Burkle noted that one of the reasons cited for not completing the survey discussed above is that countries were embarrassed that they did not yet have the required capacity.) However, the nationstates signed the Treaty, and there is an awareness that this is something larger than any individual country.
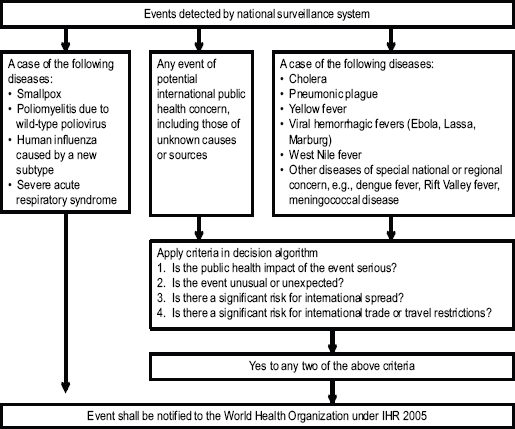
FIGURE 3 IHR Annex 2 Decision Algorithm.
SOURCE: Burkle presentation at WCDEM, adapted by Burkle from Annex 2 of the IHR.
The IHR in Practice:
The 2009 H1N1 Influenza Pandemic
The new Treaty was put to the test during the 2009 H1N1 influenza pandemic. An external review of the global response to the pandemic (WHO, 2011) found that pandemic responders were in place in 72 percent of the countries when H1N1 appeared; there was timely detection of the outbreak through the Global Influenza Surveillance network; and there was effective partnering, interagency coordination, and rapid field deployment of teams of experts that had been trained by WHO prior to the pandemic.
Nations provided samples of live influenza virus to laboratories in the developed world. A vaccine candidate was developed within 32 days, and vaccine seed strains and control reagents were available within a few weeks. To allay concerns that the vaccine would be too costly for developing countries, WHO now has a mandate to provide pandemic influenza vaccine for all those countries that cannot afford it. There is also now a provision to ensure equitable distribution of available vaccine. Early recommendations were made regarding the initial target groups for vaccination (including children, Indians in Mexico, Indians in Canada, Maori in New Zealand, Aboriginal tribes in Australia), many of whom had no prior immunizations or natural immunity to the influenza virus. Weekly analysis and reporting of the surveillance data was done, and ultimately, proper treatment courses were distributed in 72 countries.
Burkle highlighted some of the key lessons learned from implementing the Treaty in response to the 2009 pandemic H1N1 influenza. First, determining the severity of a pandemic in the early stages is difficult. A participant noted that there is some confusion regarding severity. The speed at which the outbreak spreads is the severity of the outbreak, and the phase is declared based on how many regions are affected. Another aspect, however, is the number of casualties or fatalities as a result of the outbreak. The 2009 H1N1 was widespread, but not as dangerous as expected. Another point noted by Burkle was that although the first candidate vaccine was available rapidly, the realities of vaccine development meant that no approved vaccine was available for 6 months.
The initial IHR pandemic phase structure was rather complex, and the new Annex 2 consists of a simplified phase structure: baseline, alert plan, pandemic. The need for more global health experts was also identified. In
the end, however, despite some bureaucratic “hiccups” (e.g., vaccine manufacturing issues), Burkle said this is exactly the approach needed from a global health authority.
The IHR as a Potential Framework for International Surge Planning and Crisis Standards of Care
Certain aspects of the IHR Treaty can now be considered existing standards of care (e.g., time to first candidate vaccine) governing response to a disaster (Burkle et al., 2011). The Treaty provides a historically unprecedented level of global cooperation for pandemics. This leads to the question of whether such a model for global standards of care could be applied to other large-scale disasters. (Burkle noted that the IHR covers nuclear and chemical health incidents, but have only been tested thus far in pandemics.) To accomplish this, Burkle commented, an authority must be in place to guarantee universal standards of care to prevent the type of public health emergencies that arise due to the lack of infrastructure, and/or destroy any infrastructure that did exist. A key question is who that authority might be.
Burkle recalled that the former United Nations (UN) Department of Humanitarian Affairs (DHA) had the responsibility of coordinating the humanitarian community and the UN agencies, but was stripped of all operational responsibilities in 1997 and redesignated the Office for the Coordination of Humanitarian Affairs (OCHA) to avoid being seen as a competitor with UN Field agencies. Currently, OCHA ensures coordination among UN actors and key NGO communities at the country level, and mobilizes resources on behalf of the entire UN system. Burkle opined that OCHA has the best disaster managers, but it is chronically underresourced, underfunded, and lacks needed authority. A participant countered that he did not see OCHA as being the organization that would have the capacity or the inclination to take on such a role. Burkle clarified that this was one example of the type of organization that could evolve to this role. (Furthermore, he wondered what the organization might look like today, had the original DHA operational authority not been abolished.) Some kind of global authority is needed, Burkle said, and there may be some potential for formation of an OCHA-like organization.
Burkle also noted that a framework to facilitate proactive planning is discussed in the work of Walker et al. (2010) on a “blueprint for professionalizing humanitarian assistance.”
Mass casualty preparedness pays off (e.g., prepositioned medical kits, aid agreements among countries, responders with knowledge of the local language, etc.), Poncelet said, and more preparedness is clearly needed. For large disasters, global standards should be established for mass casualty and fatality management. Hanfling cited two existing frameworks, which may serve as additional resources: the UN International Search and Rescue Guidelines classification system for international search and rescue teams and the Virtual Onsite Operational Command Center for team response registration and selection. Furthermore, models such as the IHR could serve as a potential blueprint for developing a crisis standards of care framework. There will be no global solution, however, before there are local solutions. Through this workshop, and subsequent workshop summary, the hope was expressed that a broader dialog would be initiated to stimulate additional efforts and Crisis Standards of Care concept development within the individual nation and larger international community. For example, while these issues were not discussed in detail at the workshop, it is important to address these moving forward: Is there a need for classification, criteria and standards for medical teams who arrive at the scene? What standards can be put in place for standard operating procedures, education, training, drills, equipment, response systems, international relief, and assessment?






















