Quality of Life and Community Resources
Having epilepsy is about much more than having seizures. People with epilepsy and their families typically face an array of challenges to daily living that vary with the severity and nature of the epilepsy disorder and that may change as the individual gets older. The negative effects on quality of life can be severe and involve family and social relationships, academic achievement, and opportunities for employment, housing, and the ability to function independently. Family and community support is critical across a range of services. Improvements in community services and programs are needed to ensure that they are individually centered to meet the needs of the person with epilepsy; locally focused, taking into account the full range of resources in the area; easily accessible; thoroughly evaluated; closely linked to health care providers, particularly epileptologists and epilepsy centers; and innovative and collaborative. Actions necessary to achieve these goals include identifying and disseminating best practices in the provision of epilepsy services and innovative collaborations with organizations and agencies focused on other neurological and chronic conditions or on similar service needs.
We saw four pediatric neurologists in that first year. The fourth doctor told us to stop worrying about stopping the seizures because he could not figure out her EEG [electroencephalogram]. He told us to concentrate on her quality of life. She was 4, not talking, no longer walking, and could not even smile. We were losing everything. What quality of life did she have and where was the bottom of this spiral? We did not want to find out, but we did. We now live at the bottom of the spiral looking up.
-Janna Moore and Tom Weizoerick
It is a terrifying helplessness that one feels as a parent knowing that your child’s brain is misfiring so badly that if left to continue untreated it will result in a vastly reduced life expectancy and severely reduced intellectual function.
-Jeffrey Catania
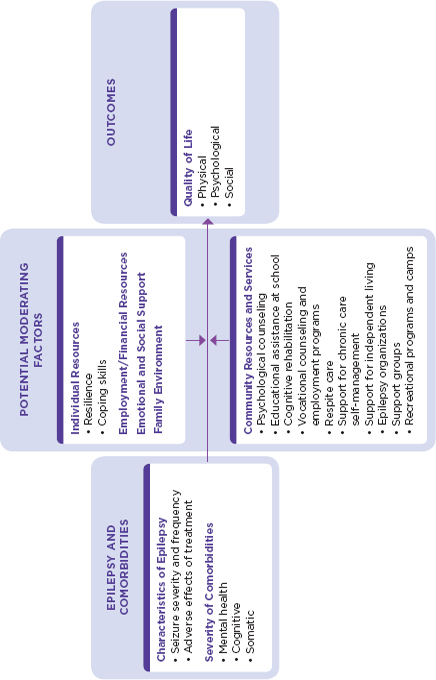
Epilepsy is much more than seizures. For people with epilepsy, the disorder is often defined in more everyday terms, such as challenges in school, uncertainties about social and employment situations, limitations on driving a car, and questions about independent living. Family members also may struggle with how to best help their loved one and maintain their family life. Because of the range of seizure types and severities and the high rate of comorbid health conditions, the types of issues that have an impact on quality of life for people with epilepsy and their families and the degree to which they are affected vary widely. As a result, the range of community services potentially needed may be extensive (Table 6-1).
This chapter aims to provide a brief introduction to the diversity of ways in which the lives of people with epilepsy are affected by the disorder and the range of community efforts that can provide support and assistance. The chapter begins with an overview of quality of life and the facets of quality of life that are particularly relevant for differing age groups. The major areas of focus for community services are then discussed—families, day care and school, sports and recreation, employment, transportation, housing, and first aid training—with each section providing the committee’s thoughts on next steps and opportunities to be explored. The chapter concludes with a discussion of navigating the broad array of community services and cross-cutting opportunities to improve services for people with epilepsy and their families.
OVERVIEW OF THE IMPACTS OF EPILEPSY ON QUALITY OF LIFE
Quality of life is a person’s subjective sense of well-being that stems from satisfaction with one’s roles, activities, goals, and opportunities, relative to that individual’s values and expectations, within the context of culture, community, and society. According to the World Health Organization (1996), “Quality of life is defined as individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (p. 5).
The term “health-related quality of life” is generally used when referring to quality of life in the context of a person’s health status (CDC, 2011a; Wilson and Cleary, 1995). Health-related quality of life is multidimensional, and for people with chronic conditions such as epilepsy, it is often related to functioning in three areas: physical, psychological, and social (Elliott and Mares, 2012; Koot, 2001; Solans et al., 2008). For the
TABLE 6-1
Spectrum of Potential Epilepsy-Related Needs and Community Services
| Types of Needs | Community Services |
| Information needs about the disorder, treatments, and health services (Chapter 7) |
• Nonprofit organization websites with general information about epilepsy (e.g., epilepsyfoundation.org; epilepsy.com) • Nonprofit organization websites with information specific to an epilepsy syndrome (e.g., dravet.org; tsalliance.org) • Federal and state websites and information resources • Health care providers, including community health workers • Case managers and social workers |
| Information needs about local community services |
• State and local Epilepsy Foundation affiliatesa • Nonprofit organizations • Social workers, case managers |
| Help in coping with the disorder and the associated comorbidities and challenges |
• Support groups • Self-management programs • Counseling |
| School-related needs |
• Cognitive testing and educational assistance • Individualized education programs (IEPs) • Teachers and school counselors who are informed about epilepsy |
| Employment-related needs |
• Vocational programs, vocational rehabilitation programs • Disability-related organizations and government agencies |
| Transportation-related needs |
• Social service organizations • Local transportation agencies • Government agencies |
| Housing-related needs |
• Social service organizations • Nonprofit organizations, including faith-based organizations • Government agencies |
| Recreation and leisure |
• Camps • Sports and recreational programs |
| Assistance for family members and caregivers |
• Respite care programs • Support groups for family members |
NOTE: As indicated throughout the report, family members, friends, caregivers, and others are key providers of social and psychosocial support.
a The Epilepsy Foundation is a nonprofit organization with a national office and more than 50 affiliates nationwide that offer varying services.
SOURCE: Adapted from IOM, 2008.
purposes of this report, the committee uses the term quality of life to incorporate health-related quality of life. Many of the physiological aspects of improving quality of life (e.g., improved treatment options, optimal care, improved access to care) are discussed in Chapter 4.
The burden of seizures and epilepsy, particularly severe forms of epilepsy or disabling comorbidities, can be overwhelming for many individuals and their families. The social and emotional toll of care (sometimes round-the-clock care) can place financial and emotional strains on marriages and families, altering roles, relationships, and lifestyles. Family members may need to take extensive leave or unexpected days off work that can disrupt careers and drain family finances. Many speakers at the committee’s workshops emphasized that epilepsy—regardless of its level of severity—creates life challenges because of the unpredictability of seizures (Box 6-1).
Studies that have examined the economic impact of epilepsy find that the indirect costs to society (productivity-related costs) generally exceed direct costs (treatment-related costs). A number of validated generic and epilepsy-specific instruments are used to assess quality of life (Chapter 2). In a systematic review of 22 cost-of-illness studies conducted around the world, among those that used reasonably comprehensive accounting for indirect cost, the indirect costs of epilepsy ranged from 12 to 85 percent of total costs (Strzelczyk et al., 2008). A study of the cost burden of epilepsy in the United States estimated a total annual cost of $12.5 billion per year, $10.8 billion in indirect costs (86.5 percent) and $1.7 billion in direct costs (13.5 percent) (Begley et al., 2000). Overall, lifetime productivity is estimated to decline 34 percent for men and 25 percent for women. Estimates of indirect costs are significantly higher for people with refractory epilepsy (Begley et al., 2000).
Children and Adolescents
In general, research comparing quality of life across different chronic conditions indicates that children and adolescents with epilepsy have a relatively high physical quality of life, but fare much worse in the psychological and social quality-of-life domains. For example, in a study comparing children with epilepsy with children with asthma, those with epilepsy had better quality of life in the physical domain but significantly lower quality of life in the psychological and social domains (Austin et al., 1994).
Many studies have focused on the psychosocial challenges faced in childhood. Recent comparison studies demonstrate that children and adolescents with epilepsy have relatively more social problems than children and youth who do not. Social problems in children and adolescents include feelings of being different, social isolation, and being subject to teasing and bullying (Elliott et al., 2005). Children with epilepsy who were 3 to 6 years
At the March workshop, Lori Towles, the mother of Max, who is 17 years old, detailed the impact of epilepsy on Max and their family. Max had brain surgery in 2010 to remove the lesion that was causing his seizures and in December 2011 celebrated 18 months of being seizure free.
$3,000 The amount I’ve paid to an advocate to secure services for Max at his current high school because of the ignorance of the school district regarding epilepsy and students with medical disabilities
19 Anti-seizure pills Max has taken per day
10 Medical and service providers that make up Max’s support team
9 Anti-seizure medications he’s tried
6:30 Pill-time—morning and night—it’s set as an alarm on everyone’s cell phone in the house
5 Number of caring and gifted teachers that have come to the house to teach math, English, and science in the last 3 years
4 Number of neurologists he sees regularly
3 Number of times Max has received the Anointing of the Sick
2 Number of additional diagnoses: ADD at age 7 and anxiety at age 10 due to the seizures
1 Years of home schooling while we tried to find a working combination of medications to control the seizures
0 Number of times he has said, "Why me”
0 Number of friends he has now
Countless
• Hours waiting in line at the pharmacy, driving to doctors’ appointments, and documenting his seizure activity
• Days missed from school due to seizures
Insulting and rude remarks made by classmates (ignorant and informed) because of his twitching, mumbling, seizing, and falling asleep in class
• Meetings, e-mails, and phone calls to his teachers and school support personnel to explain what to expect with his medical condition
• Days missed from my work to take him to doctors appointments, have meetings at school, and just be there for him
• Minutes where my daughter and I watch Max slip away into another place while his brain seizes
• Prayers from family and friends, coworkers, and neighbors
_____________
NOTE: ADD = attention deficit disorder.
old showed fewer age-appropriate social skills (Rantanen et al., 2009). Children with epilepsy ages 8 to 16 were found to have significantly lower social skills (cooperation, assertion, responsibility, and self-control) compared to healthy children; however, they did not differ significantly in social skills from children with chronic renal disease (Hamiwka et al., 2011). In a somewhat older group, youth ages 11 to 18 with epilepsy had poorer social competence, with girls having significantly less social competence than boys (Jakovljevic and Martinovic, 2006).
Having a chronic condition might help explain some of the poorer social skills described among children with epilepsy (Hamiwka et al., 2011). Beyond that possibility, Caplan and colleagues (2005) identified a number of other variables associated with social problems in children with epilepsy, including lower IQ, externalizing behavior problems, racial/ethnic minority status, and impaired social communication skills. In this study, seizure variables (e.g., age of onset, frequency, duration) were not related to social functioning. In addition, a prospective study of children and adolescents who had epilepsy surgery showed no changes in social functioning one year later, regardless of surgery outcome (Smith et al., 2004); however, improvement in social functioning was found after 2 years (Elliott et al., 2008). In childhood epilepsy, school performance and academic achievement are commonly affected, as described later in this chapter.
Compared to children with other chronic health conditions, siblings, and control groups, children with epilepsy are at increased risk for mental health conditions such as depression and attention problems (Rodenburg et al., 2005). In the 1999 nationwide British Child and Adolescent Mental Health Survey, rates of mental health comorbidities were higher in children with epilepsy (37 percent) than in children with diabetes (11 percent) or in control children (9 percent). In children with epilepsy and another type of comorbidity, such as cognitive or neurological deficits, the rate of mental health comorbidities was even higher (56 percent) (Davies et al., 2003). Children with epilepsy and intellectual disability have high rates of mental health conditions; in one study, more than 90 percent of children with epilepsy and intellectual disability could be classified as having a psychiatric diagnosis also (Steffenburg et al., 1996). A meta-analysis of 46 studies found that internalizing problems such as anxiety, depression, and social withdrawal were more common in children with epilepsy than externalizing problems such as aggression or delinquency (Rodenburg et al., 2005).
Prior to the past decade, it was generally assumed that mental health conditions and other comorbidities occurred in response to having a chronic condition, such as epilepsy. Studies of children with new-onset seizures, however, have demonstrated that mental health conditions, cognitive problems, and behavioral problems can occur very early in the disorder and in some cases precede the onset of seizures (Austin et al., 2001, 2011;
Jones et al., 2007; Oostrom et al., 2003). In addition, epidemiologic studies have shown that attention deficit hyperactivity disorder (ADHD) and other mental health conditions are risk factors for developing seizures in children (Hesdorffer et al., 2004; McAfee et al., 2007) (Chapter 3).
A number of other risk factors for mental health comorbidities have been identified. Seizure severity and frequency are associated with an increase in mental health comorbidities in some but not most studies (Austin and Caplan, 2007). Family-related psychosocial variables, such as greater family stress, fewer family resources, negative child and parent attitudes about epilepsy, poorer coping skills, and poorer family adjustment also were associated with higher rates of mental health comorbidities in children (Austin and Caplan, 2007). The authors concluded that research has not identified the causal direction of children’s mental health comorbidities and that disruptions in the family environment and mental health conditions in the child are most likely reciprocal.
Although for some individuals, epilepsy is an experience of childhood with seizures stopping during adolescence or early adulthood, for many other people seizures continue into adulthood and others live with the long-term effects that seizures have had on their cognitive or social development (Geerts et al., 2011; Kokkonen et al., 1997; Shackleton et al., 2003). For example, a 35-year prospective, population-based study in Finland found that compared to adults without epilepsy, adults who had epilepsy during childhood had poorer social outcomes in adulthood; they had less formal education, were less likely to be married or have children, and were more likely to be unemployed (Jalava et al., 1997; Sillanpää et al., 1998). Adverse lifespan outcomes have been found to be associated with histories of neurobehavioral comorbidities including early learning or cognitive and psychiatric problems (Kokkonen et al., 1997; Shackleton et al., 2003). In working to reduce the health and quality-of-life impacts of epilepsy, it is critical to address the needs of all individuals affected by the disorder.
Adults
Surveys of adults have identified risk factors for reduced quality of life for people with epilepsy, including having a greater number of seizures, longer duration of seizures, and earlier age of seizure onset (Baker et al., 1997; Jacoby and Baker, 2008; Kerr et al., 2011; Wheless, 2006). Other factors affecting quality of life include side effects of seizure medications, lack of adherence to medications, depression or anxiety, lack of social support, stigma, and concerns about employment (Aydemir et al., 2011; Baker et al., 2005; Hovinga et al., 2008; Taylor et al., 2011b). Higher rates of comorbid mental health conditions for adults with epilepsy compared to those without are described in Chapter 3, and large surveys indicate that adults
with epilepsy are relatively likely to report more mentally and physically unhealthy days per month than adults without epilepsy, with the highest rates found in those with seizures in the past 3 months (Kobau et al., 2007, 2008; Wiebe et al., 1999) (Figure 6-1).
Results from a large U.S. survey also indicated poorer social outcomes for adults with a history of epilepsy, compared to those without, including being less likely to be married and more likely to have lower levels of education, employment, and income (see Table 6-2 and discussion later in this chapter on employment and epilepsy) (Kobau et al., 2008).
Older Adults
The quality of life for older adults with epilepsy is understudied (Devinsky, 2005). A recent study by Laccheo and colleagues (2008) demonstrated that older adults with epilepsy have a significantly lower quality of life across all domains when compared with the general population.
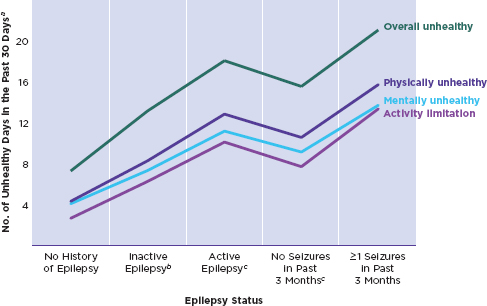
FIGURE 6-1
Health-related quality of life in adults with epilepsy.
aSelf-reported measure of health-related quality of life (Behavioral Risk Factor Surveillance System data).
bRespondents with self-reported, doctor-diagnosed seizure disorder or epilepsy who had not had a seizure in the past 3 months and were not taking medication to control epilepsy.
cRespondents with self-reported, doctor-diagnosed seizure disorder or epilepsy who were currently taking medication to control it, had one or more seizures in the past 3 months, or both.
SOURCE: CDC, 2011b; based on data from Kobau et al., 2008.
TABLE 6-2
Comparison of Adults With and Without a History of Epilepsy
| With History of Epilepsy (n = 2,207)% | Without History of Epilepsy (n = 118,638)% | |
| Marital status | ||
|
• Married or unmarried couple |
55.5 | 64.1 |
|
• Formerly married |
22.9 | 18.0 |
|
• Never married |
21.5 | 17.9 |
| Income | ||
|
• < $25,000 |
40.9 | 26.3 |
|
• $25,000 to $49,999 |
30.0 | 29.7 |
|
• ≥$50,000 |
29.2 | 43.9 |
| Employment status | ||
|
• Employed |
45.8 | 61.6 |
|
• Unemployed |
6.8 | 5.0 |
|
• Unable to work |
23.7 | 4.8 |
|
• Other (homemaker, student, or retired) |
23.7 | 28.6 |
| Could not visit doctor because of cost | ||
|
• Yes |
23.7 | 13.4 |
|
• No |
76.3 | 86.6 |
| Self-rated health | ||
|
• Good, very good, or excellent |
63.0 | 84.2 |
|
• Fair or poor |
37.0 | 15.8 |
| Life satisfaction | ||
|
• Very satisfied or satisfied |
83.4 | 94.6 |
|
• Dissatisfied or very dissatisfied |
16.6 | 5.4 |
SOURCE: Kobau et al., 2008.
Because a relatively higher percentage of epilepsy in older adults is a result of stroke, brain tumor, or dementia (Chapter 3), each with the potential to decrease quality of life, it might be anticipated that compared to other people with epilepsy, the quality of life would be lower in older populations. However, this study did not find a difference in quality-of-life scores between older adults with epilepsy and other age groups with epilepsy (Laccheo et al., 2008). The authors noted that instruments evaluating all facets of quality of life for older people with epilepsy need to be developed (Laccheo et al., 2008).
The impact of epilepsy on quality of life may reflect some differences by age and time since diagnosis. A study of three adult groups (young, middle-aged, and older) with epilepsy found that young and middle-aged adults had higher physical functioning and poorer psychological functioning than
older adults (Pugh et al., 2005). The authors propose that having epilepsy made it more difficult for middle-aged adults to accomplish the many tasks of middle age, such as providing financial and emotional support to the family, mentoring the younger generation, and providing support to aging parents. In other studies, quality of life was not found to differ between older and younger people with epilepsy, however, older adults diagnosed later in life reported more anxiety and symptoms of depression than those diagnosed earlier (Baker et al., 2001) and more concern about medication side effects (Martin et al., 2005).
My family and I took a trip to Florida once, and in the midst of my enjoyment and bliss, [my brother], who had been seizure-free for a couple months, had a relapse. [It] sent my parents into shock, my sister into tears, and me into a hurricane of resentment, fear, anger, and hatred. Why did he have to have these things at the most inopportune times? … I was afraid [my brother] would die, but I disliked that every family conversation focused on his disease. And I didn’t want to disturb the already fragile nest which was my family by inserting my own issues regarding the situation.
-Joseph Abrahams
[W]hen I was 12 years old, my mother, who had suffered a stroke at the age of 29, had begun to have seizures. ln the coming weeks she was diagnosed with epilepsy and our lives were never the same…. As an adolescent, I struggled with being my mother’s primary caretaker…. I vacillated between fear and anger, grief and bitterness, self-sacrifice and resentment. These emotions are often conveyed by parents of children with epilepsy, but l’m here to tell you that those feelings are no less intense for the children of those who suffer. lmagine being the one immediately responsible for a patient’s care—and now imagine shouldering that burden as 12- or 13-year-old.
-Carmita Vaughan
Epilepsy in one family member can negatively affect the quality of life of the entire family (Baker et al., 2008; Ellis et al., 2000; Lv et al., 2009; Taylor et al., 2011a). Epilepsy can be more disruptive to the family than many other chronic conditions because of its hidden, episodic, and unpredictable nature; potential for injury and death; frequency of comorbidities; and associated stigma. Episodic chronic health conditions are considered among the most stressful for families, because even during periods of no symptoms, the family remains on alert in anticipation of problems (Rolland, 1994). Concerns about the safety and possible death of the person with epilepsy can further increase the stress and anxiety experienced by families. Comorbidities, such as depression and cognitive deficits, present additional demands on the family’s attention. Finally, the stigma associated
with epilepsy and the possible fears that people with epilepsy and their families associate with seizures in public can curtail social and leisure activities, increasing social isolation and further reducing quality of life (Ellis et al., 2000; Fisher, 2000).
The literature contains few studies focusing on the quality of life of the family, rather than the person with epilepsy, and most family studies assess effects on the parents of children with epilepsy (Ellis et al., 2000). Studies comparing families of children with epilepsy to families of children with other chronic conditions or healthy children consistently demonstrate that families of children with epilepsy experience more dysfunction and parental anxiety, depression, and worry (Lv et al., 2009; Rodenburg et al., 2005).
Although families of adults and older adults with epilepsy have been studied much less, findings indicate that the quality of life of these families is similarly affected (Ellis et al., 2000). Research is needed to identify the impact on the quality of life and psychosocial adjustment of family members and the services that might be particularly helpful to them in learning to cope. Limitations of the literature include small sample sizes, studying only one person from each family, focusing on mothers, an underrepresentation of men and racial/ethnic minorities, and a lack of focus on families with very young children (Duffy, 2011).
The committee’s vision is for all family members of people with epilepsy to have access to resources, support, and services that would allow them to make an optimal adjustment to having a family member with epilepsy and to attain the highest possible physical, emotional, and social well-being.
The next section reviews what is known about the impact of epilepsy on the quality of life of the family, followed by how these negative effects can be reduced by improving programs and services. Three broad areas are discussed: emotional health, family social and leisure activities, and employment and role expectations.
Impact on the Emotional Health of Family Members
Epilepsy can have a negative effect on the emotional and psychological health of family members. Parents of children with epilepsy—the most studied group—had high rates of worry, stress, anxiety, and depression symptoms; this is especially true for parents of children with refractory epilepsy (Duffy, 2011; Lv et al., 2009; O’Dell et al., 2007b; Taylor et al., 2011a; Thompson and Upton, 1992; Wood et al., 2008). A common parental worry focused on the future of the child with epilepsy (Baker et al., 2008; Ramaglia et al., 2007). Some family members appear to be more at risk for a negative emotional impact. The emotional impact on parents of younger children, unmarried parents, and parents of children and adolescents who have both epilepsy and comorbidities have been shown to produce a rela-
tively poorer quality of life (Taylor et al., 2011a). In one of the few studies comparing mothers and fathers, mothers were found to bear more of the responsibility for caregiving and also to experience more anxiety and strain, as well as more worry about the stigma associated with epilepsy (Ramaglia et al., 2007). A study of caregivers determined that women caregivers over age 60 who were the only person responsible for giving medication experienced the greatest impact on their quality of life (Westphal-Guitti et al., 2007). Other factors described as contributing to increased depression were lack of emotional and practical support (Thompson and Upton, 1992), loss of sleep (Modi et al., 2009; Wood et al., 2008), and financial burden (O’Dell et al., 2007b).
All members of the family appear to be at risk for psychosocial problems (Ellis et al., 2000). Although understudied, children who watched their parents have a seizure were often confused and frightened that their parent might die. These children also experienced fear of abandonment when parents were hospitalized (Lannon, 1992). This finding is consistent with a survey reporting that parents with epilepsy worried about their children becoming upset from witnessing them have a seizure (Fisher, 2000). In a recent study, siblings expressed sadness, fear, anxiety, and worry about their brothers and sisters with epilepsy. Some siblings also reported they were worried because their parents were so exhausted, and they often felt lonely because the parents were so busy caring for their sibling with epilepsy (Hames and Appleton, 2009).
Impact on Family Social and Leisure Activities
Family social and leisure activities are often restricted because of epilepsy (Ellis et al., 2000; Taylor et al., 2011a). Parents of children with epilepsy were found to spend less time outside the home on recreational activities than controls (Modi, 2009), to rate their quality of life lower in the areas of impact on their time and on family activity (Taylor et al., 2011a), and to lack time to pursue personal interests (Lv et al., 2009). Families of adults with refractory seizures reported restricted social lives (Thompson and Upton, 1992).
Challenges that affect quality of life for families and may lead to restrictions on social and outside family activities include the need to provide caregiving, the lack of support from outside the family unit, inadequate support from extended family members, and a lack of awareness about the resources available (Ellis et al., 2000; Saburi, 2011; Thompson and Upton, 1992). Ellis and colleagues (2000) suggested that the lack of family activities might indirectly contribute to the increase in emotional difficulties experienced by family members, because participation in leisure activities can help buffer against stress and family demands.
Impact on Employment and Role Expectations
A third area in which the quality of life of family members is affected relates to employment and the disruption in meeting role expectations. Parents reported that epilepsy had a negative effect on employment, with many parents missing work due to caregiving responsibilities (Lv et al., 2009). In a survey of families from 16 countries, Baker and colleagues (2008) found that many parents needed to take time off from work because of epilepsy, and some parents gave up their jobs to care for their child. In a 12-month study of the impact of epilepsy on parents, Ramaglia and colleagues (2007) found that 33 percent of mothers and 7 percent of fathers left their jobs temporarily. One year later, all fathers were back at work; however, 16 percent of mothers were still not working. In a study of caregivers of adolescents and adults, caregivers reported that the negative impact of epilepsy (e.g., emotional challenges) was a burden that affected and interfered with their ability to work and participate in other activities. In this study, women were more likely to be caregivers and more likely to experience these burdens (Westphal-Guitti et al., 2007).
In some families, disruption of roles reduced the quality of life of family members. Lannon (1992) found that children of parents with epilepsy sometimes experienced a reversal of roles, when they felt the need or were asked to take on adult responsibilities. Siblings of children with epilepsy also reported that their activities were disrupted because of caregiving responsibilities (Hames and Appleton, 2009).
Improving Programs and Services for the Family
Many of the authors whose research is discussed above identified resources and services that could help reduce the negative impact of epilepsy on the quality of life of family members. However, family members may be unaware of available community services. Health care providers should routinely provide information about community resources and support services to all families, and state and local Epilepsy Foundation affiliates and other epilepsy-specific organizations should be an integral part of discussions with individuals with new-onset epilepsy and their families to help direct them to needed community services. Access to a 24-hour, nonmedical help line could be a valuable source of information if broadly marketed, as could in-depth websites (Chapter 7). Strategies for building social support networks could be encouraged (Rodenburg et al., 2007); for example, joining with families in similar situations for leisure and social activities. Sharing experiences through online social networks with people facing similar issues also can provide needed support (Wicks et al., 2012).
Because the negative emotional effects from epilepsy can affect family functioning and quality of life, health and community service professionals
should provide families, especially parents, with information on strategies to help reduce family stress and successfully cope with epilepsy (Rodenburg et al., 2007). For example, Hames and Appleton (2009) identified a need for materials that are specifically developed for siblings. Family members also could benefit from support groups and counseling. In the survey by Baker and colleagues (2008), 36 percent of families had consulted an epilepsy counselor.
Seeking respite care is an important strategy, particularly for families of individuals with uncontrolled seizures or serious comorbidities. These families also could benefit from the availability of respite and day care services (Thompson and Upton, 1992). These services, if available, could reduce the caregiving burden and provide opportunities for families to have time to participate in social activities or pursue personal interests. An extended family network could serve a similar function, but for unknown reasons, it appears that many families do not receive support from extended family members (Saburi, 2011). Research is needed to identify barriers to receiving support and assistance and strategies for overcoming those barriers. Public awareness campaigns may be able to disseminate information about how people with epilepsy and their families need the support of extended family members and friends. Future research that focuses on multiple members in each family would provide important information about which family members are most in need of resources and support.
[Our son] has tuberous sclerosis complex and epilepsy and he has had seizures since birth…. At age 2, Evan was placed into early intervention services in our county, and he was evaluated for special education, which included being placed on an individualized education program (IEP) when he was 3…. The IEP process empowers parents to be effective advocates for their children…. Through the IEP process [we] realized early on that many of the teaching staff were unfamiliar with epilepsy and apprehensive about caring for individuals with seizures. Included in his IEP was the request for seizure training for all staff members who would have [our son] in their care and that this training would occur prior to him entering kindergarten. We were under the impression this would involve a small meeting with … his teacher and possibly the school nurse. We walked to the library with the school principal, who was carrying a case of water, and we weren’t quite sure what we had gotten ourselves into! We learned that “staff caring for [our son]” included his teachers, the school health aide, PE and art teachers, office staff, librarians, and the list goes on. We meet with 25 to 30 staff members yearly to describe [our son’s] typical seizures and how they may affect his ability to perform in the school setting. The staff has a separate training performed by the county nurse and are required to review a seizure training video created by the
national Epilepsy Foundation…. We expect that by the time Evan exits elementary school, over 100 teachers and staff will have received extensive seizure training, and many teachers will have had annual refreshers. But this is just [one] school, and training like this needs to be expanded to all schools nationwide.
-Lisa and Robert Moss
Although most children with epilepsy do not have cognitive disabilities, as a group, children with epilepsy are at a greater risk of developing learning problems and of academic underachievement (Fastenau et al., 2008). One reason for this increase is that intellectual disability is a risk factor for developing epilepsy (Chapter 3). However, even children with epilepsy who do not have intellectual disability are at increased risk for learning and academic problems (Fastenau et al., 2008), as well as for psychosocial problems later in adolescence and adulthood (Sbarra et al., 2002). The age of onset of epilepsy is associated with effects on intelligence (Bjørnaes et al., 2001; Bulteau et al., 2000; Cormack et al., 2007; Hermann et al., 2002), learning (Fastenau et al., 2008; Sillanpää, 2004), social outcome (Lindsay et al., 1979; Sillanpää, 1983), and medical refractoriness (Berg et al., 1996; Camfield and Camfield, 2007; Casetta et al., 1999). Children who achieve seizure control relatively early in the course of epilepsy and have few cognitive impairments can attain average or above-average educational achievement. As described below, these learning, academic, and cognitive problems can result in the need for an array of support services in day care and school.
Early Childhood and Day Care
In the United States, more than 11 million children under 5 years of age are in some form of day care (professional or home) each week (NACCRRA, 2011). The paid early childhood care and education workforce in the United States is estimated at 2.2 million individuals, with approximately one-fourth caring for infants (IOM and NRC, 2011). Although little is known about the extent to which day care providers are aware of epilepsy and the range of types of epilepsy that could affect young children, there are concerns that some child care providers may refuse to accept a child with epilepsy based on their misconceptions about the disorder and about the amount of attention a child with epilepsy may need (Epilepsy Foundation, 2010).
Child care workers’ training and qualifications vary widely, with each state having its own requirements (BLS, 2009). Requirements range from less than a high school diploma to a college degree in child development or early childhood education. Requirements are generally higher for workers at child care centers compared to those for family child care providers (BLS,
2009). An increasing number of child care employers require an associate’s degree in early childhood education as a minimum requirement; however, only 12 states require training in early childhood education before leading a classroom in a child care center (BLS, 2009; NACCRRA, n.d.). As noted later in the chapter, first aid training is a requirement for many day care providers, and well-established first-aid courses (e.g., Red Cross training) provide education on how to recognize and respond to seizures. Further efforts to identify the educational needs and the knowledge and attitudes of day care staff regarding epilepsy are necessary. Such research would inform the development of guidelines and educational programs.
Additionally, parents of children with epilepsy can play an important role as advocates for training of their child’s day care providers (Epilepsy Foundation, 2010). As parents take on the role of advocate they can be supported by state and local Epilepsy Foundation affiliates and other nonprofit organizations through parent support groups; these organizations can provide written materials on epilepsy that parents can supply to their day care providers and other supporting efforts.
School
School and Academic Achievement
A major developmental task for all children is to achieve success in school. On average, school-aged children and youth spend about half of their waking hours at school. Although many children and youth with epilepsy do well in school and do not have cognitive disabilities, as a group they are relatively more likely to have learning and achievement problems, to have cognitive deficits, and to need special services. Parents report that communication and interactions with school personnel when seeking help for their children are major sources of family stress (Buelow et al., 2006).
Learning disabilities1 often are part of the school challenge for children with epilepsy. In a study of children and adolescents with epilepsy, 48 percent had a learning disability in at least one academic area using an IQ achievement discrepancy definition, and 41 to 62 percent had a learning disability using a low-achievement definition (Fastenau et al., 2008). In a recent study of special school services for children with epilepsy who had an IQ of at least 80, 45 percent used special education services, and 16 percent had been held back a year (Berg et al., 2011). In comparison studies, children with epilepsy demonstrate more cognitive deficits and academic
_______________
1Learning disabilities are defined as disorders in the basic psychological and neurological processes involved in understanding or using language, spoken or written, that may manifest themselves in an imperfect ability to listen, think, speak, read, write, spell, or use mathematical calculations.
problems than their healthy siblings (Berg et al., 2011; Dunn et al., 2010), healthy controls (Oostrom et al., 2003), and children with another chronic condition such as asthma (Austin et al., 1998, 1999). Poor achievement has generally been found in all academic areas (Austin et al., 1998; Fastenau et al., 2009; Sturniolo and Galletti, 1994).
Academic problems have been found to precede seizure onset in 15 to 24 percent of children with epilepsy (Berg et al., 2005, 2011). One of the risk factors for academic underachievement is poor cognitive functioning (Dunn et al., 2010; Fastenau et al., 2004; Schouten et al., 2002). Other risk factors include younger age of seizure onset (Dunn et al., 2010; Schoenfeld et al., 1999; Seidenberg et al., 1986), more frequent seizures or more severe seizure conditions (Austin et al., 1998, 1999; Berg et al., 2005; McNelis et al., 2007), presence of comorbidities such as ADHD (Fastenau et al., 2008), and psychosocial adjustment problems (Sturniolo and Galletti, 1994).
A supportive family environment and certain caregiver characteristics can be protective factors for children with epilepsy and can buffer the effect of poor cognitive functioning on academic achievement. For example, one study found that children with cognitive problems who lived in more supportive and organized family environments had better academic achievement than those who lived in less supportive, more disorganized homes (Fastenau et al., 2004). In a recent prospective study investigating the effect of cognitive functioning on academic achievement in children with epilepsy, Dunn and colleagues (2010) found that a higher education level of the caregiver was associated with better academic achievement and that greater caregiver anxiety was associated with lower academic achievement. These findings suggest that community support resources to help parents reduce their anxiety and create more supportive environments might also help their children in school.
The high prevalence of cognitive deficits consistently found in children with epilepsy, along with the negative impact of those deficits on academic achievement, make it imperative that children with epilepsy be screened early for cognitive problems and that early interventions be developed and applied (Fastenau et al., 2009). In addition, because children with epilepsy often have the inattentive form of ADHD (Dunn et al., 2003), which is associated with poorer academic achievement (Fastenau et al., 2008; Hermann et al., 2008), they also should be screened routinely for ADHD. Such assessments may occur as part of diagnostic testing at the time of epilepsy onset (depending on the age of the child when first diagnosed), but must be repeated regularly. Screening for cognitive problems and ADHD is important for adolescents as they transition to post–high school education and enter the workforce, so that they can identify and access programs and services to help meet their needs or seek accommodations at college
or in their work. Neuropsychological testing is a critical tool for identifying major learning impairments in children with epilepsy as well as diffuse mild cognitive impairments often missed in standardized school testing. Results and recommendations from these tests are used in developing IEPs and other educational plans and are also important in helping adolescents and young adults identify independent living needs and skills and assist in planning their future.
Unfortunately, currently there is no quick psychometric screen for assessing cognitive functioning for epilepsy, and research is needed that would enable the development of a tool to help identify children at risk for academic achievement problems. Further, the committee found few studies that tested programs that would help children with epilepsy improve their learning skills. A promising Direct Instruction2 program was piloted with children who had poor seizure control and learning difficulties in a classroom at the Hospital for Sick Children in Toronto (Humphries et al., 2005). Prior to entering a program up to 16 weeks in duration, children completed placement tests to identify their academic needs. All staff members were trained in Direct Instruction, there were no more than eight children in a classroom, and the educational program was delivered using standardized methods. Instruction was provided in a range of areas, including reading, reasoning and writing, math concepts, language, and spelling. Following the completion of the program, significant improvement was found in all academic areas except word identification in reading. The authors concluded that Direct Instruction can help children with epilepsy close gaps in learning skills that will provide a good foundation for learning. More research is needed to develop screening tools for assessing cognitive functioning in children with epilepsy, to evaluate programs to improve learning problems they experience, and to implement effective programs more widely.
School Personnel
The attitudes of teachers and other education providers (including day care providers) toward epilepsy can significantly influence students’ school performance and social skill development (Bishop and Slevin, 2004). Teachers play an important role in the health care of children with epilepsy, in that they are frequently in the best position to observe a child for possible seizures or adverse medication effects during the day. However, students
_______________
2Direct Instruction is a highly structured approach to teaching designed to facilitate learning among students with various learning problems. The method focuses on making material as clear as possible and building toward more complex ideas and skills. See, for example, http://www.promisingpractices.net/program.asp?programid=146.
with epilepsy can be at increased risk for social and academic problems if their teachers have misperceptions or a lack of information about epilepsy, or if they perpetuate the stigma often associated with the disorder (Chapter 8) (Bishop and Slevin, 2004; Dantas et al., 2001).
In several studies, teachers report little confidence in instructing students with epilepsy and acknowledge that they have limited information about the disorder, how best to work with students with epilepsy, or how to respond to seizures if they occur in the classroom (Bannon et al., 1992; Bishop and Boag, 2006; Bishop and Slevin, 2004; Wodrich et al., 2011). Further, teachers appear unlikely to actively seek information about epilepsy (Bishop and Boag, 2006). Changes may be under way in some schools as a result of a recent evaluation that found teachers who were currently teaching a child with epilepsy appeared to have more school-relevant epilepsy facts than teachers generally, and they expressed greater confidence in their ability to meet these students’ instructional, safety, and psychosocial needs (Wodrich et al., 2011).
Effective programs for educating and increasing student, teacher, school nurse, counselor, and parent awareness are critical. The Epilepsy Foundation has developed programs and resources to educate teachers and to help them increase epilepsy awareness in their classrooms. For example, the website-based program, Epilepsy Classroom, developed by UCB, Inc., in collaboration with the Epilepsy Foundation, provides lesson plans, classroom resources, and parent resources on a range of topics relevant to children with epilepsy in the school setting (Epilepsy Classroom, 2012). Several studies have shown that even brief, focused interventions in educational settings can produce improvements in epilepsy-related knowledge and attitudes among students (Fernandes et al., 2011; Martiniuk et al., 2007; Roberts and Farhana, 2010). However, teacher-focused research is limited; teacher-focused interventions need to be developed and tested; and increased education about epilepsy is needed in teacher preparation programs (Bishop and Boag, 2006) and in continuing education for school nurses, counselors, and other school personnel. Efforts are needed to design, implement, and evaluate interventions for school settings that build on techniques and methods that have been evaluated and found to be effective.
Legal Mandates
Access to special education services or other educational supports may be mandated or otherwise available for children with epilepsy as a result of the Individuals with Disabilities Education Act (IDEA) (reauthorized most recently in 2004, P.L. 108-446) and the 1973 Rehabilitation Act (P.L. 93-112) and its amendments (U.S. Department of Justice, 2005). IDEA and its
amendments mandate free and appropriate public education for all students with disabilities through age 21 or high school graduation; require that school districts identify, evaluate, and reevaluate children who need special education and related services; stipulate that education should be provided for students in the least restrictive environment and alongside of students without disabilities whenever possible; and mandate nondiscrimination in testing and evaluation services for children with disabilities. The legislation specifies the rights and processes for the development of an IEP for each student enrolled in special education and individualized transition planning to prepare special education students for post-school environments (Box 6-2). Students with disabilities who do not qualify for an IEP but have a disability and require reasonable accommodation while attending school may have an educational plan under Section 504 of the Rehabilitation Act of 1973. Section 504 regulations require a school district to provide qualified students with a disability a “free appropriate public education” regardless of the nature or severity of the disability. Further, nondiscrimination is mandated; students with disabilities must not be excluded from nonacademic activities, such as athletics, transportation, health services, recreational activities, and special interest groups or clubs. Students qualifying for protection under Section 504 include those who have been identified as having a physical or mental impairment that substantially limits one or more major life activities (U.S. Department of Education, 2011a).
Box 6-2 EDUCATIONAL PLANS FOR STUDENTS WITH DISABILITIES
Individualized education program (IEP) An IEP is a multipart written statement for the child with a disability that includes information on annual academic and functional goals, plans on how progress will be measured on those goals, details on the special education and related services to be provided to the child, and information on any appropriate individual accommodations necessary to measure the academic achievement and functional performance of the child on state- and district-wide assessments (U.S. Department of Education, 2011b). By the time the student reaches 16 years of age, the IEP must include a discussion of postsecond-ary goals and transition services needed (U.S. Department of Education, 2011c).
Section 504 educational plan Students with disabilities who do not have an IEP can have a Section 504 educational plan that outlines the educational ser-vices and accommodations necessary to ensure equal access to education (U.S. Department of Education, 2011a). Accommodations may include, for example, schedule modification, a structured learning environment, modified test instructions and test delivery, and assistive technology and medical and transportation services. Section 504 plans also allow for any necessary and related services as occupational therapy, physical therapy, and speech and language services.
The 2008 amendments to the Americans with Disabilities Act (ADA) expanded the definition of major life activities to include learning, reading, concentrating, and thinking, as well as expanding the definition to include neurological and brain functions (U.S. Access Board, 2008). The amendments also clarified that the act covers impairments, such as epilepsy, that are episodic in nature or in remission and that substantially limit a major life activity when not in remission (U.S. Access Board, 2008). Epilepsy advocates and numerous other disability advocacy groups were active in supporting and informing these changes.
Improving School and Day Care Programs
A large part of improving school and day care services for children with epilepsy revolves around enhancing teachers’ awareness about epilepsy and developing an educational plan focused on meeting students’ individual needs. Although not all children and youth with epilepsy require specialized services, these services must be available for those that do, so that all students have opportunities to reach their full potential. The committee believes that teachers, counselors, day care providers, and school personnel working with children with epilepsy have the responsibility to become informed about the disorder so that they can work effectively with parents and students to develop tailored educational plans. Additionally, the committee recognizes that parents may have to be active advocates for their children in the development and implementation of educational plans. Parents and school staff can encourage students with epilepsy to reach out to peers and teachers for help with accommodations as needed and help students become strong and informed self-advocates.
Physical activity and recreation are important components of physical and emotional well-being and quality of life for all people, and people with epilepsy are encouraged to be as physically active as possible (Epilepsy Foundation, n.d.; Howard et al., 2004). Obesity and being overweight are a concern for people with epilepsy because studies have found that children with newly diagnosed, untreated epilepsy have higher body mass index levels than children in a comparison cohort and that women with epilepsy have a higher body fat ratio than healthy controls (Daniels et al., 2009; Howard et al., 2004). A population-based study using the Canadian Community Health Surveys between 2001 and 2005 found that individuals with epilepsy were 1.4 times more likely to be physically inactive than the general population (Hinnell et al., 2010). In addition, some seizure medications have been associated with weight gain (Ben-Menachem, 2007; Biton, 2003;
Verrotti et al., 2011). Although exercise-induced seizures are rare, factors that may exacerbate seizures include hyperventilation, fatigue, altering levels of metabolism of seizure medications with exercise, psychological stress, and increased heart rate during intense activity (Dubow and Kelly, 2003; Fountain and May, 2003; Howard et al., 2004; Sahoo and Fountain, 2004).
However, research in sports and exercise suggests that regular physical activity—in addition to its well-known positive psychosocial and physiologic benefits—can reduce the frequency and severity of seizures among children and adults, including women (Arida et al., 2009, 2010; Conant et al., 2008; Eriksen et al., 1994; Nakken et al., 1990, 1997). A survey of Norwegians with epilepsy, for example, found that exercise was associated with better seizure control (Nakken, 1999). Physical activity also can improve attention, mood, and physical health and may have a role in minimizing depression in people with epilepsy (Arida et al., 2012). Although some seizure medications can affect bone density, which peaks in adolescence and has consequences in adulthood related to risks for fractures and osteoporosis (Pack, 2011; Pack and Morrell, 2004; Samaniego and Sheth, 2007), participation in regular weight-bearing activities in conjunction with adequate calcium consumption and vitamin D can mediate the process of bone loss (HHS, 2004).
A few studies have examined the extent to which people with epilepsy engage in sports and recreational activities or experience limitations in their activities. The 2003 California Health Interview Survey found that adults who have had epilepsy reported twice as many activity limitation days as those without (Kobau et al., 2007). In a study comparing siblings with and without epilepsy, no significant differences were seen for physical activity in children under 12 years, but youth ages 13 to 17 years participated less frequently in group sports and total sports activities, although participation in individual sports was similar (Wong and Wirrell, 2006).
Researchers found that Canadians ages 12 to 39 spent similar amounts of time in leisure physical activity regardless of whether they had epilepsy or not; they noted that people with epilepsy reported more walking and were less likely to be involved in ice hockey, weight training, or home exercise (Gordon et al., 2010). A study in South Korea evaluated active and inactive individuals with epilepsy to identify barriers to exercise (Han et al., 2011). Anxiety, taking multiple seizure medications, and previously experiencing a seizure during exercise were significantly associated with inactivity. In addition, fear of participation, overprotection, and discouragement from family, friends, or physicians were significant barriers. Other barriers in the study included fatigue following activities, the lack of an exercise partner, limited time, and uncertainty of how to begin and continue an exercise program.
Recommendations on participation in sports by people with epilepsy have changed over the years. The 1968 American Medical Association
Committee on Medical Aspects of Sports opposed participation in collision and contact sports by individuals with epilepsy, but by 1978 the committee had reversed that recommendation, and its 1983 statement urged full participation in physical education programs and interscholastic athletics, aided by common sense and proper supervision (Dubow and Kelly, 2003). Further research is required to understand the effects of intense exercise and the effect of exercise and sports on metabolism of seizure medications. In addition, research is needed to understand the effect of epilepsy and seizures on aerobic endurance and balance.
Selection of sports and leisure time activities for children and adults with epilepsy involves consideration of personal preferences, the nature of the sport, the risk of injury, and individual factors regarding seizure type, frequency, and severity (Drazkowski and Sirven, 2011; Dubow and Kelly, 2003; Fountain and May, 2003). Since rates and degree of injuries during participation in contact sports are similar between people with and without epilepsy, participation in contact sports is an option (Miele et al., 2006). Recommendations for athletes with epilepsy in competitive sports, contact sports, and high-risk sports include the need to receive an initial neurological evaluation to establish a baseline and another after any injuries, to adhere to prescribed medication regimens, to inform the team manager or coach about epilepsy, and to use adequate protective equipment (Dimberg and Burns, 2005). Table 6-3 provides a general categorization of sports and activities by risk.
One way to encourage exercise, skill development, and independence for children with epilepsy is through residential camps that either are specifically focused on this disorder or more broadly serve children with various serious or chronic health conditions. These types of camps offer opportunities for children to learn about self-management and interact with other children and youth who share similar experiences. Studies of health condition-specific camps found improvements in participants’ attitudes about their health condition and quality of life and reduced anxiety (Bekesi et al., 2011; Briery and Rabian, 1999). Similarly, in a 3-year study that examined adaptive coping behavior in campers at an epilepsy-specific summer camp, significant improvements were observed for return campers in communication, responsibility, and social interactions (Cushner-Weinstein et al., 2007). Many nonprofit organizations, including state and local Epilepsy Foundation affiliates, offer information on and opportunities for summer camps and other recreational activities (Epilepsy Foundation, 2011; Epilepsy.com, 2011).
Expanding participation in sports and other recreational activities will involve continued efforts to increase awareness that people with epilepsy can and should be physically active. Further, coaches, workout instructors, counselors, camp directors, and others in the physical activity and recre-
TABLE 6-3
Sporting and Recreational Activities Classified According to a Possible Risk for the ndividual with Epilepsy
| Low Risk | Moderate Risk | High Risk |
| Baseball | Basketball | Boxing |
| Bowling | Biking | Downhill skiing |
| Cross-country skiing | Boating or sailing | Gymnastics (equipment with height) |
| Golf | Football | |
| Ping-Pong | Gymnastics (floor) | Hang gliding |
| Track | Horseback riding | Hockey |
| Walking | Karate | Motor sports |
| Weight training (machines) | Skateboarding | Rock climbing |
| Yoga | Soccer | Scuba diving |
| Swimming Waterskiing | Swimming (long distance) | |
SOURCE: Adapted from Drazkowski and Sirven, 2011. Reprinted with permission from Lippincott Williams and Wilkins, http://www.lww.com.
ation fields need up-to-date information about epilepsy. Methods for most effectively providing this information need to be explored. Nonprofit organizations and the public health community can disseminate information tailored to meet this need. Individuals, parents, and caregivers should be sure that those with whom they work and who coach children and youth with epilepsy are fully aware of any specific limitations. As discussed later in the chapter, seizure first aid training is critically important.
By the time I was in high school, everybody knew I had epilepsy, and it was not really a big deal…. But then one day I decided I wanted a job…. Now, this was 1972, [and] the application looked more like a new patient intake form. It actually listed a huge long list of medical disorders, and one of them was epilepsy. I was telling everybody I had epilepsy, so I marked it. And so I took my little application up, handed it in at the window, and the person there right in front of me picks up a red pen and makes circles where I checked I had epilepsy. They did not call me for an interview. So the next day I went to another store. I saw they had a “help wanted” sign. And I filled out the application, and they did not ask for specifics, but there was a health-related question. And right there, 18 years before Congress, I enacted my own Americans with Disabilities Act. I had two qualifications. One, could I do the job and, two, if I did have a seizure, would somebody else get hurt? If I got hurt, well, couldn’t do anything about that. Since then I have never put epilepsy on the application.
-Mary Macleish
Employment is a critically important aspect of quality of life and psychosocial health, providing avenues for social participation, economic security (Bishop and Chiu, 2011), and for many people in the United States with epilepsy, access to health insurance. For some people with epilepsy, transportation to and from work poses major challenges to gaining and maintaining employment.
Although most people who have epilepsy are able to fully participate in the labor market, they consistently have higher levels of unemployment compared to the general population (Bishop, 2002; Fisher, 2000; Kobau et al., 2008; Smeets et al., 2007). Further, they are more likely to be employed in unskilled and manual jobs or underemployed (employed in a job where they have more skill, education, or training than what is required, which results in their earning capacity not being met) (Bishop and Chiu, 2011; Smeets et al., 2007). Although the lack of standard definitions makes the measurement of employment, unemployment, and underemployment a complex and inexact science (Chaplin, 2005), research using population-based samples has consistently suggested that the unemployment rate of people with epilepsy is at least twice that of the general population (Fisher, 2000) and even higher among people who seek care in tertiary care centers, which is often those individuals with more severe types of seizures (Hauser and Hesdorffer, 1990; Thorbecke and Fraser, 2008).
Available evidence underscores consistent and persistent employment problems for people with epilepsy. Responses to a community-based survey of adults with epilepsy indicated that 25 percent of eligible workers reported being unemployed at a time when the average unemployment rate in the United States was slightly more than 5 percent (Fisher et al., 2000). Data from the 2005 Behavioral Risk Factor Surveillance System (BRFSS) surveys, which included population data from 19 states, suggested that the unemployment rate was 9.8 percent for people with active epilepsy,3 8.3 percent among those with inactive epilepsy, and 5.4 percent for those with no epilepsy history (Kobau et al., 2008). Nine-state data from the 2006 BRFSS indicated that people with a lifetime prevalence of epilepsy3 were more than three times as likely to be unemployed or unable to work as people who did not have epilepsy (34 percent versus 9 percent), and people with active epilepsy were more than four times as likely to be unemployed or unable to work in a similar comparison (42 percent versus 9 percent) (Konda et al., 2009). Although estimates of the extent of employment disparities vary based on methodology and sample characteristics, relatively lower levels of employment have been consistently found for people with
_______________
3In both studies analyzing the BRFSS results, active epilepsy was defined as having 1 or more seizures in the past 3 months or taking medication for seizure control, and lifetime prevalence of epilepsy was defined as responding affirmatively to ever being told by a physician that they had a seizure disorder or epilepsy (Kobau et al., 2008; Konda et al., 2009).
epilepsy for more than three decades (Bishop, 2002). Employment disparities have continued despite improvements in clinical treatment and laws protecting the employment rights of people with disabilities (Jacoby et al., 2005).
The apparently difficult employment situation for people with epilepsy is not reducible to a single factor, such as the experience of seizures, but rather represents a complex interaction of variables (Thorbecke and Fraser, 2008). A variety of seizure-related factors (e.g., seizure frequency, type, perceived impact, felt stigma) have been shown to predict employment status, as have the age of epilepsy onset, comorbid mental health and cognitive conditions, the adverse effects of seizure medications, and various psychological factors, such as depression and anxiety (Bishop, 2004; Chaplin et al., 1998; Jacoby et al., 1996, 2005; Rätsepp et al., 2000; Yagi, 1998). Psychosocial factors relevant to unemployment rates among people with epilepsy include social isolation, social skill deficits, low self-esteem, lack of family support, and fears about negative attitudes on the part of employers (e.g., Smeets et al., 2007; Thorbecke and Fraser, 2008). External factors, such as enacted stigma and discrimination, also contribute to employment problems for people with epilepsy, and the effects of these may be more significant in times of high unemployment, when competition for jobs is heightened (Jacoby et al., 2005).
In the employment application process, deciding on the appropriateness and necessity of openness about the epilepsy diagnosis “may be influenced by legal, medical, social, and personal concerns” (Bishop and Chiu, 2011, p. 100). People with epilepsy may need to be open in acknowledging that they have epilepsy if they need work-related accommodations. If accommodations are not required and the applicant can perform the required duties of the position, then openness about the diagnosis may not be necessary (Bishop et al., 2007). In general, however, opinions vary about the advisability of disclosure. In a survey of state and local Epilepsy Foundation affiliates, none of the organizations reported that they counsel people to be open about their condition either on applications or in initial interviews, and more than half of respondents indicated that if an open discussion about the condition is necessary, they would advise that it be done after being hired (Bishop and Allen, 2001). By contrast, in a survey of employers by Jacoby and colleagues (2005), a majority of employers indicated that prospective employees with active epilepsy (defined as “currently having seizures, even if only occasionally,” p. 1981) should discuss their disorder openly, preferably early in the recruitment process, even if seizures are well controlled. As the researchers noted, “There is a clear mismatch between the position of employers, who may see non-disclosure as a breach of trust, and [people with epilepsy], many of whom opt not to disclose out of fear of enacted stigma” (Jacoby et al., 2005, p. 1984).
Employer attitudes can be a significant barrier to employment (Bishop, 2002; Bishop and Chiu, 2011; Epilepsy Foundation, 2001; Jacoby et al., 2005). Researchers have found that employers’ attitudes regarding employment of people with epilepsy include concerns about the comfort and safety of workers, worries about increased accident rates and subsequent increases in insurance rates, and questions about the need to revise work flows with possible increases in expenses for work-related accommodations (e.g., Bishop et al., 2007; Hicks and Hicks, 1991; Jacoby et al., 2005; John and McLellan, 1988). However, there is no empirical support for these concerns (Jacoby et al., 2005).
In the past several decades, survey research has found improving attitudes toward people with epilepsy (Chapter 8). However, contrasting data have been reported by researchers who used indirect survey methods that are less susceptible to socially desirable responses (Antonak and Livneh, 1995; Baumann et al., 1995; Bishop and Slevin, 2004) and by evidence that the level of unemployment for people with epilepsy and employers’ attitudes have remained fairly constant over a 30-year period (Bishop, 2002; Jacoby et al., 2005). Based on their 2005 survey of a representative random sample of UK employers, Jacoby and colleagues found that 26 percent of employers reported having employed individuals with epilepsy knowingly; 16 percent believed their company had no jobs suitable for individuals with epilepsy; 21 percent thought employing people with epilepsy would be “a major issue”; and epilepsy created high concern for around half (in part because of concerns about work-related accidents), although they said they were willing to make accommodations for people with epilepsy. Further, a U.S. study among employers and human resources personnel suggested that hiring an individual with epilepsy was less likely than hiring people with any number of other disabilities, including cancer in remission, depression, a history of heart problems, AIDS, mild intellectual disabilities, and spinal cord injury (Bishop et al., 2007).
Attitudes of employers toward hiring people with disabilities generally differ depending on the ways in which attitudes are defined and measured, as well as the size of the employer and the employer’s experience with previous hires. Positive attitudes tend to be found in studies that assessed general, as opposed to specific, attitudes and situations involving workers with disabilities. Further, although employers may have positive attitudes toward workers with disabilities, those attitudes do not always translate into active efforts to employ people with disabilities (Hernandez et al., 2000). In surveys of employers, those from large companies were more likely to have positive attitudes about workers with disabilities; to hire more workers with disabilities, including workers with epilepsy (Jacoby et al., 2005); and to have made worksite accommodations (Bruyère et al., 2003; Lee, 1996).
Larger companies were also more likely to be familiar with employment-related legislation such as the ADA (Bruyère et al., 2006).
Potential avenues for improving employment opportunities for people with epilepsy include employer education programs and awareness campaigns, vocational rehabilitation programs and career services, and enforcement of antidiscrimination and equal opportunity legislation.
Employer Education Programs
Several public education efforts have been specifically directed at employers. For example, the Epilepsy Foundation has developed and sponsored employer education and awareness campaigns and developed and disseminated other materials to promote the hiring of people with epilepsy. During Epilepsy Awareness Month, efforts have been made to educate employers about the nature of epilepsy, its successful treatment, workplace accommodations, and vocational rehabilitation for people with epilepsy. Although epilepsy education campaigns and interventions have been shown to have positive effects in promoting knowledge and attitude change in educational, health, and more general settings (e.g., Martiniuk et al., 2010; Roberts and Farhana, 2010) (Chapters 5 and 8), the number of such efforts with an employment focus has been small, and evaluations of their efficacy in the research literature are scarce.
In a study examining the impact of an epilepsy education campaign in one U.S. city that focused on the mass media, community organizations, and mailings to selected employers, Sands and Zalkind (1972) did not find differences between pre- and post-campaign attitudes. However, understanding of the techniques that increase the effectiveness of public education campaigns has evolved considerably since 1972. Further efforts are needed to design, implement, and evaluate the efficacy of focused campaigns aimed at promoting employer knowledge and attitudes.
Workplace Programs
To improve employment opportunities, research has consistently pointed to the need for effective employment training programs for people with epilepsy (Smeets et al., 2007). A two-pronged approach has been supported for epilepsy vocational rehabilitation, one focused on specialized vocational rehabilitation services and the other focused on targeted epilepsy training for staff of broader vocational rehabilitation programs (Fraser, 2011).
Specialized employment programs and resources specifically for individuals with epilepsy have proved successful. These include the now discontinued TAPS (Training Applicants for Placement Success) and Job-
Tech programs (Bishop and Allen, 2001; Thorbecke and Fraser, 2008). Ongoing employment services provided by the Epilepsy Foundation include an online career support center, the Jeannie Carpenter Legal Defense Network (whose work includes employment discrimination), and employment-related services offered by state and local Epilepsy Foundation affiliates across the country (Fraser, 2011). The Epilepsy Foundation’s website includes an employment section that is designed to assist people with employment searches; in addition, the website provides guides on job preparation and job search sites, gives suggestions on ways to discuss information about epilepsy in the workplace, and offers other resources, including a discussion forum on epilepsy and employment (Epilepsy Foundation, 2012). The Epilepsy Foundation and its affiliates also organize employer education training and employer and employee awareness and training conferences that bring employers together with supporting and enforcement agencies, such as the Equal Employment Opportunity Commission, to provide information on the rights of workers with epilepsy (Epilepsy Foundation Northwest, 2012).
General (not epilepsy-specific) employment services are available through state-federal vocational rehabilitation programs and One Stop Career Centers in each state (U.S. Department of Labor, 2012). Little research has evaluated the effectiveness of epilepsy and vocational rehabilitation programs (Smeets et al., 2007). However, programs that are focused on vocational rehabilitation for people with epilepsy appear to be more effective than general vocational rehabilitation programs (Fraser et al., 1984; Thorbecke and Fraser, 2008). For example, Fraser and colleagues (1984) reported that whereas general state vocational rehabilitation agencies achieved 9 to 21 percent placement rates among people with epilepsy, specialized vocational rehabilitation programs achieved placement for almost half of individuals, a finding reiterated in more recent research (Mount et al., 2005). These results may reflect both the focused delivery and the epilepsy knowledge of the professionals providing services. For example, the extent to which state-federal vocational rehabilitation programs hire master’s level and certified rehabilitation counselors varies by state.
Available research suggests that the most successful employment programs for people with epilepsy focus on specific skills, such as training individuals to request work accommodations, promoting self-confidence and self-efficacy in handling work-related problems, and providing training aimed at job retention (Smeets et al., 2007). Further, programs that bring employers and individuals with epilepsy into direct contact, such as through negotiated short-term work experience placements, “are likely to have more impact than educational initiatives undertaken in the abstract” (Jacoby et al., 2005, p. 1986).
The committee believes that overcoming employment barriers faced by
people with epilepsy will require the efforts of advocacy groups working with federal, state, and local vocational programs and counselors. Epilepsy-specific training provided to vocational rehabilitation counselors and other state vocational rehabilitation program personnel will improve awareness of epilepsy and allow for discussions of specific employment problems. Additionally, there is a significant need for increased longitudinal and evidence-based evaluations of the efficacy of both specialized and general vocational rehabilitation programs, in order to more specifically identify effective factors and interventions for job attainment and retention.
Employment Legislation
Employers’ awareness and knowledge about epilepsy is enhanced indirectly through the enactment and enforcement of employment and civil rights legislation. Several major laws aimed at protecting equal opportunities for people with disabilities, including the Rehabilitation Act of 1973, the Workforce Investment Act of 1998, the Ticket to Work and Work Incentive Improvement Act of 1999, and the ADA of 1990 and ADA Amendments Act of 2008 have significant potential for promoting employment opportunities for people with epilepsy (Box 6-3).
After the enactment of the ADA, several U.S. Supreme Court decisions narrowed its scope of coverage in such a way that many individuals with epilepsy were no longer protected against employment discrimination (Bishop and Chiu, 2011). However, people with epilepsy and advocates for epilepsy were among those who worked to inform policy makers of the need to expand the definition of a disability to include impairments of neurological function and episodic conditions that, when active, limit major life activities. The ADA Amendments Act incorporated these changes.
The impact of the ADA on employers’ attitudes and on rates of employment for people with disabilities generally has been mixed (Hernandez et al., 2000; Houtenville and Burkhauser, 2004). While there is evidence that employers are increasingly aware of and have more positive attitudes about general disability issues and ADA rights that they have identified as less costly to implement, they may have concerns about other ADA mandates that are perceived to be complex and costly, including accommodating workers with disabilities. At the same time, they are also concerned about the potential threat of legal actions (Hernandez et al., 2000). Roessler and Sumner (1997) found positive employer attitudes toward employees with chronic health conditions, including epilepsy. However, epilepsy was noted as one of the conditions with which employers were least familiar (Jacoby et al., 2005).
Although the ADA amendments expanded access to discrimination protection for people with epilepsy, the law’s impact is not yet evident.
Box 6-3 KEY EMPLOYMENT LEGISLATION
1973 Rehabilitation Act This act and its subsequent amendments have made significant revisions to the operation of the state-federal vocational rehabilitation programs, established funding for independent living services, and increased funding for rehabilitation and disability research through the establishment of the National Institute on Disability and Rehabilitation Research. In addition, Title V of the act served to advance the civil rights of people with disabilities, including through mandating nondiscrimination on the basis of disability in federal hiring and employment. Section 504 prohibited disability-based exclusion of otherwise qualified persons with disabilities from participation in any federal program or activity or from any program or activity that receives federal funding.
1990 Americans with Disabilities Act (ADA) The ADA ensures “equality of opportunity, full participation, independent living, and economic self-sufficiency” for individuals with disabilities. Civil rights are addressed across several domains including employment discrimination (Title 1), discrimination in public services (Title 2), and discrimination in public accommodations (Title 3). Title 1 specifically protects people with disabilities from employment discrimination in hiring, advancement, or discharge of employees, employee compensation, job training, and other terms, conditions, and privileges of employment. Titles 2 and 3 prohibit discrimination based on disability by public entities (e.g., public transportation) at all local and state levels, and they require public accommodations when needed.
2008 ADA Amendments Act As noted above, the ADA amendments clarified that the act covers impairments, such as epilepsy, that are episodic in nature or in remission and that substantially limit a major life activity when active.
Continued review and monitoring are necessary, as is ongoing research on employers’ attitudes and on the employment experiences of people with epilepsy.
Improving Employment Opportunities and Awareness About Employment Rights
People with epilepsy need to be informed and aware of their employment protections and how to invoke them. The American Epilepsy Society (AES), the Epilepsy Foundation, and Epilepsy.com of the Epilepsy Therapy Project have developed and actively promote programs and educational materials that detail the provisions of the ADA and its amendments, as well as provide information and resources relevant to employment, such as job accommodations. The extent to which these resources are accessed by employers and whether they have increased employers’ willingness to hire people with epilepsy needs to be explored.
In addition, best practices in employment programs need to be identi-
fied and widely disseminated. The committee regards this as an important area in which organizations involved with a number of chronic diseases or other neurological disorders could come together to identify and disseminate programs that work in vocational rehabilitation and to work with employers to promote the hiring of qualified people with epilepsy and other disorders.
As a practical consequence of my disorder, I have had to give up driving and to stop working…. I have had to reshape my lifestyle in order to maintain my usefulness and the esteem of those whose opinion of me matters most, as well as my own self-respect…. I have traded many duties around the house with my wife and sons so that they now do anything that requires driving, while I have taken over many more house-husband routines. To the extent that epilepsy challenged us to be a better team, we have become a stronger family. It has taken a lot of work, and that work has taken change, and change has taken courage and commitment, and all of that from all of us has taken love.
-Michael Bornemann
In the United States, the ability to drive or to be able to access reliable, affordable transportation is closely connected to employment and educational opportunities, social engagements and activities, access to health care services, and overall independence and quality of life. Seizures may limit transportation options. Challenges and fears associated with driving and transportation are frequently cited in surveys and interviews of adults with epilepsy, regardless of age or gender (Fisher et al., 2000; Gilliam et al., 1997; Martin et al., 2005; Paschal et al., 2005; Personal communication, C. A. Tubby, AES, June 28, 2011; Sare et al., 2007). In a quality-of-life study, Gilliam and colleagues (1997) found that driving, independence, and employment are the chief concerns among people with epilepsy.
Driving and Epilepsy
Driving requires a complex array of neurological functions and skills that involve vision, cognition, attention, and judgment, as well as coordination, reaction time, and motor control. Any or all of these could be impaired by epilepsy and seizures, comorbidities associated with epilepsy, or side effects of seizure medications. People with epilepsy who drive vehicles may present safety concerns for themselves, their passengers, and the public (Drazkowski, 2007a,b; Drazkowski and Sirven, 2011).
Data on the number of people with epilepsy who drive and on the
number of accidents that result from seizures are inconsistent. Surveys and interviews have indicated that approximately 20 to 30 percent of people whose epilepsy is not well controlled nevertheless drive (Bautista and Wludyka, 2006; Berg et al., 2000; Tatum et al., 2012; Webster et al., 2011). Although the number of accidents that occur as a direct result of seizures is unknown, 5 to 27 percent of people with epilepsy report that they have had a seizure that has led to an auto accident (Berg et al., 2000; Drazkowski et al., 2010; Fisher et al., 2000). Studies that analyze data on automobile accidents and deaths have mixed results as to whether risks are greater for people with epilepsy compared to the general public or to people with other health conditions (Drazkowski, 2007a; Kwon et al., 2011; Lings, 2001; Sheth et al., 2004).
Legal Considerations
Unlike other health conditions that could impair one’s ability to drive safely (e.g., cardiovascular disease, diabetes), epilepsy is explicitly addressed in driving laws in every U.S. state (Krauss et al., 2001). Although the laws and regulations vary, most states require a defined seizure-free interval, ranging from 3 to 12 months, before a person with epilepsy may legally drive. Some states have no seizure-free interval requirement at all, and others allow exceptions—for example, in cases where seizures are strictly nocturnal, there is an aura before a seizure, or when a recent seizure was the direct result of medication change (Krauss et al., 2001).
The “seizure-free interval” is a proxy for predicting which individuals are likely to remain seizure free—generally speaking, the longer the interval, the less likely is another seizure—although a definitive seizure-free interval for safe driving has not been established (Drazkowski and Sirven, 2011). Krauss and colleagues (1999) found a 93-percent lower risk of being involved in an auto accident for a person with epilepsy who had been seizure free for a year or more compared to individuals who were seizure free for a shorter period of time, whereas Drazkowski and colleagues (2003) found no significant increase in auto accidents or deaths associated with seizures when Arizona reduced its seizure-free requirement from 12 to 3 months. Sheth and colleagues (2004) also found no greater fatality rate in states with a 3-month seizure-free interval requirement, compared to states with 6- and 12-month requirements. In 1994, the American Academy of Neurology (AAN), AES, and Epilepsy Foundation developed a consensus statement that recommends a 3-month interval (AAN et al., 1994). The consensus statement also includes a list of modifiers that could alter the duration interval requirement (e.g., lack of compliance with medication regimen, a seizure that was a result of sleep deprivation or a reversible acute illness).
The role of physicians in determining driving eligibility also varies by state. For example, some states allow physicians the discretion to determine the appropriate seizure-free interval on an individual basis (Krauss et al., 2001). Similarly, reporting regulations differ by state; most states allow voluntary reporting but do not mandate it (Drazkowski et al., 2010). Six states—California, Delaware, Nevada, New Jersey, Oregon, and Pennsylvania—take a strict, and controversial, approach by requiring physicians to report people with epilepsy and active seizures who are driving (or would like to drive) to the state driving authorities (Drazkowski, 2007a; Drazkowski and Sirven, 2011). In the consensus statement noted above, the three organizations agreed that physicians should not be required to report people with epilepsy to state driving authorities (AAN et al., 1994).
Mandatory reporting requirements for physicians may affect a patient’s honesty about seizure frequency and, in turn, a clinician’s ability to provide quality care and improve management of the disorder. One survey indicated that 19 percent of patients did not accurately reveal their seizure frequency to their physician so that they could continue to drive (Elliott and Long, 2008). Moreover, a Canadian study demonstrated that a physician reporting requirement did not decrease the risk of auto accidents for drivers with epilepsy (McLachlan et al., 2007). Nor do people with epilepsy necessarily self-report their seizures to driving authorities or reply honestly to questions about their condition on driver’s license applications (Drazkowski and Sirven, 2011; Salinsky et al., 1992; Taylor et al., 1995; Tomson et al., 2004). However, the majority of drivers with epilepsy do express concerns about their safety and the safety of others and indicate they would not drive until their physician or the state driving authorities indicate it is safe to do so (Tatum et al., 2012).
There is no simple determination for when and under what circumstances a person with epilepsy can safely drive. As Krumholz notes, “no single standard satisfies all situations because of varied cultural, social, and environmental factors and risk tolerance that influence such a decision” (2003, p. 817). As new studies become available and science advances, driving laws should be reevaluated and updated. For example, one innovative study recently explored the relationship between brain activity that occurs between seizures and can be measured on EEGs, and its relationship with reaction time when driving (Krestel et al., 2011). The authors suggested that reaction-time EEGs could play a future role in evaluating individuals’ ability to drive. Additional population-based studies using innovative approaches are needed, and policy changes should be considered to ensure that driving laws are equitable, both guarding the safety of the public and preventing undue burden and diminished quality of life for people with epilepsy.
Educating People with Epilepsy and Clinicians
Due to the risks associated with having a seizure while driving, educating individuals with epilepsy about those risks and the applicable state driving laws and regulations is essential, and clinicians have an obligation to do so. The need for improved education about driving laws has been demonstrated in surveys, which indicate that many people with epilepsy (48 to 86 percent) are not aware of their state’s seizure-free interval requirements (Long et al., 2000; Tatum et al., 2012). Additionally, Long and colleagues (2000) found that almost a quarter of people with epilepsy thought that it was okay to drive “if they either ‘double-up on medication,’ are not driving alone, or are able to ‘pull over’ at the onset of a seizure” (p. 729). The proportion of individuals with epilepsy who have received counseling about driving and associated risks varies significantly—from one-tenth to three-quarters (Shareef et al., 2009; Tatum et al., 2012). Only 7 percent of patients who sought care in an emergency room following a loss of consciousness or a seizure received counseling about driving if a neurologist was not consulted; when a neurologist was involved the counseling rate was still only 34 percent (Shareef et al., 2009).
Physician knowledge of state driving laws varies by specialty; more than a third of family physicians and internists incorrectly identified whether their state required mandatory reporting, compared with approximately 19 percent of neurologists (Vogtle et al., 2007). These differences are worth noting, since many people with epilepsy seek care and management of their disorder through primary care providers (Fountain et al., 2011). Regardless of specialty, all physicians, nurses, physician assistants, and others who provide patient education for people with epilepsy need to be knowledgeable about driving laws and risks and be prepared to effectively counsel patients on these topics.
When educating and counseling patients, clinicians should recognize the links between driving, independence, and quality of life and should be prepared for an honest discussion and a potentially emotional or negative response if the patient is counseled not to drive (Drazkowski, 2007a,b). Box 6-4 provides topics for clinicians to consider in educating patients with epilepsy about driving.
Studies clearly indicate a lack of awareness in clinicians and patients about driving laws and regulations; there is a need for increased counseling and patient education. Gaps in clinician knowledge could be closed through a variety of mechanisms, including the implementation of a performance measure recommended by AAN stating that all epilepsy patients should be counseled at least once a year about “context-specific safety issues, appropriate to the patient’s age, seizure type(s) and frequency(ies), occupation and leisure activities, etc. (e.g., injury prevention, burns, appropriate driving restrictions, or bathing)” (Fountain et al., 2011, p. 96). If the per-
Box 6-4 DISCUSSION POINTS FOR EDUCATING PATIENTS ABOUT DRIVING
• Know and explain the applicable legal requirements in your jurisdiction
• Allow enough time to counsel patients and answer questions
• Be compassionate and understanding of the patient’s concerns and circumstances
• Use clear communication and be frank about the risks and consequences of driving
• Explain the risks of driving, including risks associated with seizures, and how comorbidities and side effects of seizure medications may affect driving ability
• Remind the patient of the potential consequences of driving illegally (e.g., possible prosecution or litigation following an accident and denial of insurance claims)
• Be aware of ancillary risk factors that may increase the likelihood of a person with epilepsy driving despite legal limitations and advice not to, such as having a valid driver’s license, being employed, or not having experienced a seizure-related accident
• Be aware of and discuss local transportation services (e.g., public transportation, ride sharing or carpools, transportation for people with disabilities) as alternatives to driving
• Document the discussion and advice in the patient’s health record
• When possible, provide written information on driving and advice to the patient
• Revisit the topic of driving with the patient in subsequent visits
_____________
SOURCES: Drazkowski, 2007a,b; Elliott and Long, 2008; Webster et al., 2011.
formance measure is adopted, implemented, and specific enough to include mention of driving restrictions, the potential impact could be significant if it were followed consistently: clinicians would be more likely to learn the state laws and restrictions in order to counsel their patients, the rates and regularity of patient counseling would increase significantly, patient awareness about safety issues could increase, and the topic would be revisited on an annual basis and messages about safety would be reinforced.
Transportation and Quality of Life
I thought I was well adjusted, but as I got older, living with epilepsy became more difficult. Not being able to drive because of my epilepsy has always been difficult. It seems like such a little thing, but it has been a major factor in making decisions on where we live, where I work, who will employ me, what activities my son can participate in, who goes to the grocery store, etc. I qualify for a reduced fare card for the bus, but it
limits where I go, the days I can go, and the times I can leave and arrive at a destination.
–Sabrina Cooke
Fortunately, I’ve had a great support system, but over the years, it’s been difficult to get around since I can’t drive.
–John Gambo
(lives in a rural area where public
transportation is not an option)
When people with epilepsy are not able to drive, they must rely on public transportation or family, friends, and caregivers to get where they need to go. Many U.S. cities have a public transit infrastructure, but these options are not always reliable or timely. Lack of local transportation options other than driving was cited by almost half of people with epilepsy in one study (Elliott and Long, 2008). For individuals who live in less urban areas or rural regions, access to transportation may be an even greater challenge.
Connections have been made between social support and access to transportation. For example, a survey of African American women with epilepsy indicated that those individuals with a strong social network were more likely to have access to needed transportation (Paschal et al., 2005). Approximately three-quarters of people with epilepsy believe that their family and friends would be supportive of changes to their driving patterns (when and where they drive). However, 40 percent said that they did not have family or friends available to help provide transportation (Elliott and Long, 2008).
For many people with epilepsy, the ability to drive legally is an integral part of gaining and maintaining employment, and a valid driver’s license is needed for some jobs. Additionally, getting to and from work is a challenge for many people and usually requires some form of transportation. Employment is a principal reason that people with uncontrolled epilepsy continue to drive (Bautista and Wludyka, 2006).
Driving and transportation also play a role in access to health care services, including keeping appointments with health care providers and picking up prescriptions. People with epilepsy and clinicians alike cite transportation as a significant barrier to accessing needed care (Hawley et al., 2007; Paschal et al., 2005; Personal communication, C. A. Tubby, AES, June 28, 2011). A recent study explored the connection between transportation and medication adherence—a key factor in managing epilepsy and seizure frequency (Welty et al., 2010). Approximately half of respondents who were not able to drive reported challenges with transportation as a barrier to getting medication on time. In fact, more than a fourth indicated that they believed they had had a seizure as a result of not being able to obtain their prescription in a timely manner.
Housing issues for people with epilepsy are primarily focused on meeting the needs of individuals who are physically or intellectually disabled (e.g., from injuries, from seizures suffered during brain development, or due to comorbid conditions). Another potential area of concern is housing options for older adults with epilepsy. A review of housing-related studies relevant to epilepsy found limited data on the extent and nature of housing needs (van Blarikom et al., 2006). A study of living arrangements for people with intellectual disability in Europe found that higher numbers of people with epilepsy lived in staffed residences versus unstaffed ones (Martínez-Leal et al., 2011). Van Blarikom and colleagues (2009) noted the higher staff-to-resident ratios needed by people with more severe forms of epilepsy, some of whom also had intellectual disabilities.
The Fair Housing Act as amended in 1988 prohibits housing discrimination on the basis of disability (U.S. Department of Justice, 2005). The disabilities that people have may range widely in severity and complexity, yet the law’s overall goal is for individuals to have equitable housing options that meet their needs and maximize independent living and functioning. The experience of the intellectual disability community in housing is long standing, and recent efforts have focused on implementing a range of community-based housing settings, including supportive and independent group homes (Lakin and Stancliffe, 2007; Mansell and Beadle-Brown, 2009; Wong and Stanhope, 2009).
Many nonprofit organizations help link families and individuals with appropriate housing options. For example, the Jewish Foundation for Group Homes has 22 group homes in the Washington, DC, area that provide housing for people with disabling conditions, including epilepsy (Rubin, 2011). The organization also provides a range of support services and a 1-year transitional program for individuals moving out of the school system or other programs. This transitional program focuses on self-sufficiency, community inclusion, and pre-vocational planning (Rubin, 2011).
Continuing these and other efforts to help people with epilepsy with their housing needs can improve quality of life. This is another area where the committee believes collaborative efforts of epilepsy organizations with disability organizations and other disease-specific organizations could be advantageous. Innovative housing models, including those that focus on older adults with disabilities, need to be explored and championed by nonprofit organizations, public–private collaborations, and government agencies.
Attention to first-aid training that includes seizure recognition and response is particularly important for personnel in school and day care settings, nursing home and long-term care staff, employers, and community service staff members. Although many public school teachers receive some first-aid training, the limited, and somewhat dated, research available suggests that emergency training generally, and seizure training for school staff, more specifically, may be lacking (Gagliardi et al., 1994; O’Dell et al., 2007a; Sapien and Allen, 2001). Staff of day care facilities often have training in cardiopulmonary resuscitation (CPR) and first aid, with seizure response specifically identified as a training need for some child care staff in the recent guidelines for early care and education programs published by the American Academy of Pediatrics, American Public Health Association, and National Resource Center for Health and Safety in Child Care and Early Education (AAP et al., 2011). The American Heart Association and American Red Cross Guidelines for First Aid (Markenson et al., 2010) and the National Guidelines for First Aid Training in Occupational Settings (NGFATOS, 2002) include seizure first aid.
Areas that require increased attention include more current and nationally based explorations of the extent to which teachers, day care workers, nursing home and long-term care staff, coaches, social workers, and other community service workers receive initial and refresher instruction in seizure first aid and feel confident in providing seizure care. Further explorations of the extent to which CPR and first aid training programs provide sufficient content and information on seizure recognition and appropriate response are also necessary.
IMPROVING COMMUNITY-BASED PROGRAMS
As introduced in Chapter 4, the committee supports an approach to service design and delivery that focuses on the specific health care and community service needs of the individual. Making this approach work involves changes in the organization of health care, strong links between health care and community services, and the efforts of many engaged and committed individuals and organizations. It requires familiarity with the range of available services, knowing how to access those services, and having the time and resources to make those connections or help people with epilepsy do so. Further, this approach emphasizes the importance of the family and the need to support family members and other caregivers.
Community-based programs may be epilepsy-specific or they may address needs of people with a range of health conditions. For example, many epilepsy-specific programs at the community level are affiliated with the Epilepsy Foundation. Initiatives of other epilepsy-focused organizations
are also an important part of community efforts, generally providing information and referral, individual and family support, advocacy, and education. Epilepsy-specific employment assistance, camps, and school support programs may also be offered, and many community-based organizations have strong partnerships with a range of state agencies and other nonprofit organizations.
Other community agencies offer various types of assistance (including housing, employment, transportation, counseling, and other services) to people who have a wide range of health conditions or disabilities. These agencies have the potential to help people with epilepsy; again, however, their expertise and available resources vary. The types of services are usually targeted to people who are most severely affected by epilepsy or to specific groups of individuals, such as children, older adults, people with intellectual developmental disabilities, or those with head injuries.
The needs of people with epilepsy and their families span a number of state and federal departments and agencies, and local organizations can often help identify how to obtain this assistance. A central website (www.disability.gov) serves as a guide to federal and state government resources in a variety of areas of concern to people with disabilities.
Next Steps for Community Services
Moving forward with improving and sustaining community services is vital to the well-being of people with epilepsy, particularly those with cognitive and physical disabilities. Several areas discussed below indicate where focused efforts would help improve quality of life and access to services. As discussed throughout this chapter, individual, family, and community resources can help reduce the negative effects of epilepsy and associated comorbidities on the quality of life of individuals with epilepsy and their families (Figure 6-2).
Bridging the Gaps—Making the Connections
Recognizing the complexity of the services needed by some people with epilepsy and their families, the committee urges increased attention to developing innovative approaches for navigating the myriad of resources. Both professionals and lay volunteers can bridge the gaps between people with epilepsy and community services, as well as provide links and referrals to other services. Rehabilitation counselors frequently work with adults who have epilepsy in vocational rehabilitation programs or they may be employed by hospitals and schools to help people with psychosocial adjustment and coping, as well as educational and vocational planning and services. Social workers and case managers are employed in a
number of settings—often in health care, educational, and social services settings—to give support and counseling, coordinate referrals, provide case management, and establish links with community services. Ensuring that these professionals are knowledgeable about epilepsy and aware of epilepsy-specific resources is critically important. Continuing education and training sessions offer opportunities to provide information about epilepsy, as does working with relevant counseling and social work professional organizations.
Drawing on the wealth of experiences gained in navigating the array of services is another way to help individuals or families facing a recent diagnosis of epilepsy. Patient or parent navigators are often volunteers who provide their insights and expertise and work with the newly diagnosed patient and their family over the course of weeks or months to help them become connected to needed services (Chapter 4). Community health workers or lay health educators, including promotores de salud, often develop a specialty in a particular condition, including epilepsy; speak the language of the patient and family population; and build strong ties with the health and social services sectors.
Clarifying Eligibility
While services provided by Epilepsy Foundation affiliates and other epilepsy-specific organizations are open to any person with epilepsy or seizures, eligibility for other programs may be related to level of disability (e.g., Social Security Disability Insurance, Medicare, special education), income (e.g., Medicaid and other financial assistance programs), age (e.g., Child Services, Children’s Health Insurance Program, educational assistance, older adult services), need (e.g., vocational programs, respite care, independent living, group homes), or comorbidity (e.g., mental health services, head injury services). Not all of these programs have clearly defined and detailed eligibility requirements. People with epilepsy often “fall between the cracks,” especially if they do not have a developmental disability or mental health condition that fits specific, often narrowly defined, criteria. Because epilepsy can be a hidden disorder, with unpredictable periods of disability that may or may not affect functioning every day, it may not fit the eligibility definitions or criteria for some programs. Efforts are needed to identify those programs whose eligibility requirements should be broadened or revised and to work with program officials and epilepsy policy and advocacy organizations to make the appropriate changes, taking into account the spectrum of severity of epilepsy and its comorbidities.
Building Sustainability Through Partnering
Community nonprofit programs are often transient and depend on charitable donations and volunteers to run critical programs. Although agencies that receive federal or state funding have been considered more stable than nonprofit organizations that rely solely upon charitable donations, this is changing rapidly. The ability of community services agencies of all types to sustain their activities over time and meet the needs of their constituencies must be strengthened through innovative partnerships. Epilepsy organizations are well poised to build relationships and forge advocacy partnerships with organizations whose missions are to help people with other chronic diseases, especially other neurological disorders and health conditions that are frequently comorbid with epilepsy. Finding ways to work together to strengthen existing programs and identifying innovative approaches to coordinate use of resources will be critical in responding to constrained government and charitable dollars.
Finding Innovative Approaches to Expand Access
The availability and sustainability of community resources varies across geographic regions and between urban and rural areas. For example, the lack of public transportation and inability to drive can leave rural and suburban individuals with epilepsy unable to reach appointments and access community resources. As discussed in Chapter 4, telemedicine and local clinics may help ease some of the transportation challenges. Access concerns, particularly regarding public transportation, need to be brought to the attention of state and local transportation programs and other relevant programs so that people with epilepsy have access to transportation resources.
Establishing Links with Health Care Providers
While previous chapters have stressed the role of health professionals in the care and lives of people with epilepsy, there is a critical gap in the lack of awareness of professionals about community resources. Even when health professionals know about community services, they may not have the time, expertise, or resources to connect patients and families with the appropriate agencies. As noted in Chapter 4, epilepsy centers need to develop alliances and partnerships with community agencies to establish referral mechanisms to enable patients and families to obtain the help they need. All providers would be aided by greater use of—and funding for— community health workers or professionals who can make vital connections with community resources, as described above.
Evaluating and Disseminating Community Service Programs
Applying more resources to evaluating community programs and services will allow best practices to be identified and disseminated. Evaluations typically focus on process measures (e.g., number of brochures distributed), rather than the health, quality-of-life, and economic outcomes of community services. Comparing services and programs for effectiveness may be difficult for a number of reasons, including differences in outcome measures, audience, and size. In-depth evaluations that examine impact on quality of life can be challenging and costly to conduct. Finding ways to help community service organizations and agencies evaluate programs in an effective and informative manner is a priority and can provide the accountability that is needed.
Further, once effective programs are identified, resources may be insufficient to fund and implement wide-scale outreach and dissemination of the program models. For example, as described above, research has shown significant differences in the effectiveness of various epilepsy-specific vocational program models, yet efforts to disseminate and replicate the more robust programs are often lacking.
Enhancing Support to Families and Caregivers
Efforts to improve community programs and services for families and caregivers are needed in three critical areas identified by the committee:
• Knowledge—Families and caregivers who face the challenges of caring for someone with epilepsy, especially severe types of epilepsy, need to be informed about the disorder, its comorbidities, the treatment options, the paths to obtaining high-quality health care, and available community resources (Chapter 7).
• Supportive services—Parent, sibling, and caregiver support groups help family members share their experiences and draw on the experiences of others. In addition to in-person support groups and discussions, online social networks and web connection tools can be a source of assistance. Respite care is an essential supporting service for families with significant caregiving responsibilities.
• Advocacy—Promoting the rights and needs of people with epilepsy and raising awareness about this disorder are vital to progress in preventing, treating, and curing epilepsy. People with epilepsy, their family members, and their caregivers can often be the first and most insightful source of information regarding epilepsy and can inform teachers, employers, colleagues, friends, and extended family as well as work to promote improved community services. For
example, parents can be advocates for their child to access school services and ensure that teachers are informed and competent in meeting the child’s needs. Advocacy can also take place through informing policy makers and decision makers about epilepsy and the needs facing people with it. Advocacy can be difficult, given that epilepsy is a complex, highly variable, and often misunderstood disorder. Efforts to improve the skills of people with epilepsy, their family members, and caregivers who are interested in honing their ability to be effective advocates can be integrated into self-management programs, support group training, and other educational campaigns and programs.
People with epilepsy and their families face an array of challenges to daily living that vary with the severity and nature of the epilepsy disorder and may change as the individual grows older. The negative effects on quality of life can be severe and involve family and social relationships, academic achievement, and opportunities for employment, housing, and the ability to function independently. Family and community support are critical across a range of services. As a result, the committee urges improvements in community services and programs to ensure that they are
• individually centered to meet the needs of the person with epilepsy;
• locally focused, taking into account the full range of resources in the area;
• easily accessible;
• thoroughly evaluated;
• closely linked to health care providers, particularly epileptologists and epilepsy centers; and
• innovative and collaborative in working with organizations and agencies focused on other neurological and chronic conditions or on similar service needs.
Chapter 9 provides the committee’s research priorities and recommendations for improving community services. Many epilepsy-specific and non-epilepsy organizations are involved in community services, from transportation to employment to education to recreation. Collaborations are needed that tap into the energy and dedicated efforts of individual organizations and that work to coordinate and evaluate ongoing programs and identify best practices for community services for people with epilepsy. Once best practices are identified, they need to be widely disseminated. Instilling the use of performance indicators will provide benchmarks to assess prog-
ress in community services. Of particular concern are ensuring that children with epilepsy have opportunities for early identification of academic and social problems and are provided with creative approaches to promoting academic achievement and strong social relationships. Improved collaborations with mental health services are highlighted because current U.S. health system approaches can raise disconnects between clinical and mental health services. Innovative and financially attentive approaches to community services—such as a 24-hour nonmedical help line for people with epilepsy and their families or ensuring the availability of local transportation—can build on and contribute to efforts by organizations and programs for other chronic health conditions. A strength of the epilepsy community is the depth and number of epilepsy organizations and involved individuals; building on and coordinating their work is critical to further improvements in quality of life for people with epilepsy.
AAN (American Academy of Neurology), AES (American Epilepsy Society), and Epilepsy Foundation. 1994. Consensus statements, sample statutory provisions, and model regulations regarding driver licensing and epilepsy. Epilepsia 35(3):696-705.
AAP (American Academy of Pediatrics), APHA (American Public Health Association), and NRC (National Resource Center for Health and Safety in Child Care and Early Education). 2011. Caring for our children: National health and safety performance standards; guidelines for early care and education programs. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics.
Antonak, R. F., and H. Livneh. 1995. Development, psychometric analysis, and validation of an error-choice test to measure attitudes toward persons with epilepsy. Rehabilitation Psychology 40(1):25-38.
Arida, R. M., F. A. Scorza, V. C. Terra, C. A. Scorza, A. C. de Almeida, and E. A. Cavalheiro. 2009. Physical exercise in epilepsy: What kind of stressor is it? Epilepsy and Behavior 16(3):381-387.
Arida, R. M., F. A. Scorza, and E. A. Cavalheiro. 2010. Favorable effects of physical activity for recovery in temporal lobe epilepsy. Epilepsia 51(Suppl. 3):76-79.
Arida, R. M., E. A. Cavalheiro, and F. A. Scorza. 2012. From depressive symptoms to depression in people with epilepsy: Contribution of physical exercise to improve this picture. Epilepsy Research 99(1-2):1-13.
Austin, J. K., and R. Caplan. 2007. Behavioral and psychiatric comorbidities in pediatric epilepsy: Toward an integrative model. Epilepsia 48(9):1639-1651.
Austin, J. K., M. S. Smith, M. W. Risinger, and A. M. McNelis. 1994. Childhood epilepsy and asthma: Comparison of quality of life. Epilepsia 35(3):608-615.
Austin, J. K., T. J. Huberty, G. A. Huster, and D. W. Dunn. 1998. Academic achievement in children with epilepsy or asthma. Developmental Medicine and Child Neurology 40(4):248-255.
———. 1999. Does academic achievement in children with epilepsy change over time? Developmental Medicine and Child Neurology 41(7):473-479.
Austin, J. K., J. Harezlak, D. W. Dunn, G. A. Huster, D. F. Rose, and W. T. Ambrosius. 2001. Behavior problems in children before first recognized seizures. Pediatrics 107(1):115-122.
Austin, J. K., S. M. Perkins, C. S. Johnson, P. S. Fastenau, A. W. Byars, T. J. deGrauw, and D. W. Dunn. 2011. Behavior problems in children at time of first recognized seizure and changes over the following 3 years. Epilepsy and Behavior 21(4):373-381.
Aydemir, N., C. Ozkara, P. Unsal, and R. Canbeyli. 2011. A comparative study of health related quality of life, psychological well-being, impact of illness and stigma in epilepsy and migraine. Seizure 20(9):679-685.
Baker, G. A., A. Jacoby, D. Buck, C. Stalgis, and D. Monnet. 1997. Quality of life of people with epilepsy: A European study. Epilepsia 38(3):353-362.
Baker, G. A., A. Jacoby, D. Buck, J. Brooks, P. Potts, and D. W. Chadwick. 2001. The quality of life of older people with epilepsy: Findings from a UK community study. Seizure 10(2):92-99.
Baker, G. A., A. Jacoby, J. Gorry, J. Doughty, V. Ellina, and S. Group. 2005. Quality of life of people with epilepsy in Iran, the Gulf, and Near East. Epilepsia 46(1):132-140.
Baker, G. A., E. Hargis, M. M.-S. Hsih, H. Mounfield, A. Arzimanoglou, T. Glauser, J. Pellock, S. Lund, and the International Bureau for Epilepsy. 2008. Perceived impact of epilepsy in teenagers and young adults: An international survey. Epilepsy and Behavior 12(3):395-401.
Bannon, M. J., C. Wildig, and P. W. Jones. 1992. Teachers’ perceptions of epilepsy. Archives of Disease in Childhood 67(12):1467-1471.
Baumann, R. J., J. F. Wilson, and H. J. Wiese. 1995. Kentuckians’ attitudes toward children with epilepsy. Epilepsia 36(10):1003-1008.
Bautista, R. E., and P. Wludyka. 2006. Driving prevalence and factors associated with driving among patients with epilepsy. Epilepsy and Behavior 9(4):625-631.
Begley, C. E., M. Famulari, J. F. Annegers, D. R. Lairson, T. F. Reynolds, S. Coan, S. Dubinsky, M. E. Newmark, C. Leibson, E. L. So, and W. A. Rocca. 2000. The cost of epilepsy in the United States: An estimate from population-based clinical and survey data. Epilepsia 41(3):342-351.
Bekesi, A., S. Torok, G. Kokonyei, I. Bokretas, A. Szentes, and G. Telepoczki. 2011. Health-related quality of life changes of children and adolescents with chronic disease after participation in therapeutic recreation camping program. Health and Quality of Life Outcomes 9:43.
Ben-Menachem, E. 2007. Weight issues for people with epilepsy—A review. Epilepsia 48(Suppl. 9):42-45.
Berg, A. T., S. R. Levy, E. J. Novotny, and S. Shinnar. 1996. Predictors of intractable epilepsy in childhood: A case-control study. Epilepsia 37(1):24-30.
Berg, A. T., B. G. Vickrey, M. R. Sperling, J. T. Langfitt, C. W. Bazil, S. Shinnar, T. S. Walczak, S. Pacia, and S. S. Spencer. 2000. Driving in adults with refractory localization-related epilepsy. Multi-center study of epilepsy surgery. Neurology 54(3):625-630.
Berg, A. T., S. N. Smith, D. Frobish, S. R. Levy, F. M. Testa, B. Beckerman, and S. Shinnar. 2005. Special education needs of children with newly diagnosed epilepsy. Developmental Medicine and Child Neurology 47(11):749-753.
Berg, A. T., D. C. Hesdorffer, and F. A. Zelko. 2011. Special education participation in children with epilepsy: What does it reflect? Epilepsy and Behavior 22(2):336-341.
Bishop, M. 2002. Barriers to employment among people with epilepsy: Report of a focus group. Journal of Vocational Rehabilitation 17(4):281-286.
———. 2004. Determinants of employment status among a community-based sample of people with epilepsy: Implications for rehabilitation interventions. Rehabilitation Counseling Bulletin 47(2):112-121.
Bishop, M., and C. Allen. 2001. Employment concerns of people with epilepsy and the question of disclosure: Report of a survey of the Epilepsy Foundation. Epilepsy and Behavior 2(5):490-495.
Bishop, M., and E. M. Boag. 2006. Teachers′ knowledge about epilepsy and attitudes toward students with epilepsy: Results of a national survey. Epilepsy and Behavior 8(2):397-405.
Bishop, M., and C.-Y. Chiu. 2011. Epilepsy and employment. In Society, behaviour and epilepsy, edited by J. Pinikahana and C. Walker. New York: Nova Science Publishers. Pp. 93-114.
Bishop, M., and B. Slevin. 2004. Teachers′ attitudes toward students with epilepsy: Results of a survey of elementary and middle school teachers. Epilepsy and Behavior 5(3):308-315.
Bishop, M., D. M. Stenhoff, K. D. Bradley, and C. A. Allen. 2007. The differential effect of epilepsy labels on employer perceptions: Report of a pilot study. Epilepsy and Behavior 11(3):351-356.
Biton, V. 2003. Effect of antiepileptic drugs on bodyweight: Overview and clinical implications for the treatment of epilepsy. CNS Drugs 17(11):781-791.
Bjørnaes, H., K. Stabell, O. Henriksen, and Y. Loyning. 2001. The effects of refractory epilepsy on intellectual functioning in children and adults. A longitudinal study. Seizure 10(4):250-259.
BLS (Bureau of Labor Statistics). 2009. Occupational outlook handbook, 2010-11 edition: Child care workers. http://www.bls.gov/oco/ocos170.htm (accessed January 3, 2012).
Briery, B. G., and B. Rabian. 1999. Psychosocial changes associated with participation in a pediatric summer camp. Journal of Pediatric Psychology 24(2):183-190.
Bruyère, S., W. Erickson, and J. Ferrentino. 2003. Identity and disability in the workplace. William and Mary Law Review 44(3):1173-1196.
Bruyère, S., W. Erickson, and S. VanLooy. 2006. The impact of business size on employer ADA response. Rehabilitation Counseling Bulletin 49:194-206.
Buelow, J. M., A. McNelis, C. P. Shore, and J. K. Austin. 2006. Stressors of parents of children with epilepsy and intellectual disability. Journal of Neuroscience Nursing 38(3):147-154.
Bulteau, C., I. Jambaque, D. Viguier, V. Kieffer, G. Dellatolas, and O. Dulac. 2000. Epileptic syndromes, cognitive assessment and school placement: A study of 251 children. Developmental Medicine and Child Neurology 42(5):319-327.
Camfield, C. S., and P. R. Camfield. 2007. Long-term social outcomes for children with epilepsy. Epilepsia 48(Suppl. 9):3-5.
Caplan, R., J. Sagun, P. Siddarth, S. Gurbani, S. Koh, R. Gowrinathan, and R. Sankar. 2005. Social competence in pediatric epilepsy: Insights into underlying mechanisms. Epilepsy and Behavior 6(2):218-228.
Casetta, I., E. Granieri, V. C. Monetti, G. Gilli, M. R. Tola, E. Paolino, V. Govoni, and E. Iezzi. 1999. Early predictors of intractability in childhood epilepsy: A community-based case-control study in Copparo, Italy. Acta Neurologica Scandinavica 99(6):329-333.
CDC (Centers for Disease Control and Prevention). 2011a. HRQOL concepts. http://www.cdc.gov/hrqol/concept.htm (accessed January 3, 2012).
———. 2011b. Targeting epilepsy: Improving the lives of people with one of the nation′s most common neurologicalconditions. At a glance 2011. http://www.cdc.gov/chronicdisease/resources/publications/AAG/epilepsy.htm (accessed January 3, 2012).
Chaplin, J. 2005. Vocational assessment and intervention for people with epilepsy. Epilepsia 46(Suppl. 1):55-56.
Chaplin, J. E., A. Wester, and T. Tomson. 1998. Factors associated with the employment problems of people with established epilepsy. Seizure 7(4):299-303.
Conant, K. D., A. K. Morgan, D. Muzykewicz, D. C. Clark, and E. A. Thiele. 2008. A karate program for improving self-concept and quality of life in childhood epilepsy: Results of a pilot study. Epilepsy and Behavior 12(1):61-65.
Cormack, F., J. H. Cross, E. Isaacs, W. Harkness, I. Wright, F. Vargha-Khadem, and T. Baldeweg. 2007. The development of intellectual abilities in pediatric temporal lobe epilepsy. Epilepsia 48(1):201-204.
Cushner-Weinstein, S., M. Berl, J. A. Salpekar, J. L. Johnson, P. L. Pearl, J. A. Conry, M. Kolodgie, A. Scully, W. D. Gaillard, and S. L. Weinstein. 2007. The benefits of a camp designed for children with epilepsy: Evaluating adaptive behaviors over 3 years. Epilepsy and Behavior 10(1):170-178.
Daniels, Z. S., T. G. Nick, C. Liu, A. Cassedy, and T. A. Glauser. 2009. Obesity is a common comorbidity for pediatric patients with untreated, newly diagnosed epilepsy. Neurology 73(9):658-664.
Dantas, F. G., G. A. Cariri, and A. R. Ribeiro Filho. 2001. Knowledge and attitudes toward epilepsy among primary, secondary and tertiary level teachers. Arquivos de Neuro-Psiquiatria 59(3-B):712-716.
Davies, S., I. Heyman, and R. Goodman. 2003. A population survey of mental health problems in children with epilepsy. Developmental Medicine and Child Neurology 45(5):292-295.
Devinsky, O. 2005. Quality of life in the elderly with epilepsy. Epilepsy and Behavior 6(1):1-3.
Dimberg, E. L., and T. M. Burns. 2005. Management of common neurologic conditions in sports. Clinics in Sports Medicine 24(3):637-662.
Drazkowski, J. F. 2007a. An overview of epilepsy and driving. Epilepsia 48(Suppl. 9):10-12.
———. 2007b. Driving and flying with epilepsy. Current Neurology and Neuroscience Reports 7(4):329-334.
Drazkowski, J. F., and J. I. Sirven. 2011. Driving and social issues in epilepsy. In Wyllie’s treatment of epilepsy: Principles and practice. 5th ed., edited by E. Wyllie, G. D. Cascino, B. E. Gidal, and H. P. Goodkin. Philadelphia, PA: Lippincott Williams and Wilkins. Pp. 1051-1056.
Drazkowski, J. F., R. S. Fisher, J. I. Sirven, B. M. Demaerschalk, L. Uber-Zak, J. G. Hentz, and D. Labiner. 2003. Seizure-related motor vehicle crashes in Arizona before and after reducing the driving restriction from 12 to 3 months. Mayo Clinic Proceedings 78(7):819-825.
Drazkowski, J. F., E. S. Neiman, J. I. Sirven, G. N. McAbee, and K. H. Noe. 2010. Frequency of physician counseling and attitudes toward driving motor vehicles in people with epilepsy: Comparing a mandatory-reporting with a voluntary-reporting state. Epilepsy and Behavior 19(1):52-54.
Dubow, J. S., and J. P. Kelly. 2003. Epilepsy in sports and recreation. Sports Medicine 33(7):499-516.
Duffy, L. V. 2011. Parental coping and childhood epilepsy: The need for future research. Journal of Neuroscience Nursing 43(1):29-35.
Dunn, D. W., J. K. Austin, J. Harezlak, and W. T. Ambrosius. 2003. ADHD and epilepsy in childhood. Developmental Medicine and Child Neurology 45(1):50-54.
Dunn, D. W., C. S. Johnson, S. M. Perkins, P. S. Fastenau, A. W. Byars, T. J. deGrauw, and J. K. Austin. 2010. Academic problems in children with seizures: Relationships with neuropsychological functioning and family variables during the 3 years after onset. Epilepsy and Behavior 19(3):455-461.
Elliott, I. M., L. Lach, and M. L. Smith. 2005. I just want to be normal: A qualitative study exploring how children and adolescents view the impact of intractable epilepsy on their quality of life. Epilepsy and Behavior 7(4):664-678.
Elliott, I. M., L. Lach, D. S. Kadis, and M. L. Smith. 2008. Psychosocial outcomes in children two years after epilepsy surgery: Has anything changed? Epilepsia 49(4):634-641.
Elliott, J. O., and L. Long. 2008. Perceived risk, resources, and perceptions concerning driving and epilepsy: A patient perspective. Epilepsy and Behavior 13(2):381-386.
Elliott, J. O., and A. S. Mares. 2012. Gender differences in quality of life among Canadian adults with epilepsy. Epilepsy Research 100(1-2):42-48.
Ellis, N., D. Upton, and P. Thompson. 2000. Epilepsy and the family: A review of current literature. Seizure 9(1):22-30.
Epilepsy Classroom. 2012. Epilepsy classroom. http://epilepsyclassroom.com/home/index.aspx (accessed January 3, 2012).
Epilepsy Foundation. 2001. Employment for people with epilepsy: The hardest nut. Epilepsy and Behavior 2(5):379-380.
———. 2010. Education and day care: Advocating for your child. http://www.epilepsyfoundation.org/resources/epilepsy/loader.cfm?csModule=security/getfile&PageID=21512 (accessed January 3, 2012).
———. 2011. Epilepsy USA: Summer camp issue. http://www.epilepsyfoundation.org/resources/epilepsyusa/loader.cfm?csModule=security/getfile&pageid=40425 (accessed March 10, 2012).
———. 2012. Employment topics. http://epilepsyfoundation.org/livingwithepilepsy/employmenttopics (accessed March 9, 2012).
———. n.d. Physical fitness. http://www.epilepsyfoundation.org/livingwithepilepsy/healthandwellness/staying/healthy/physicalfitness.cfm (accessed January 3, 2012).
Epilepsy Foundation Northwest. 2012. Community education and training. http://www.epilepsynw.org/programs/community-programs#efnw-conference-and-seminars (accessed March 12, 2012).
Epilepsy.com. 2011. Summer camp. http://www.epilepsy.com/EPILEPSY/plans_summer_camps (accessed December 16, 2011).
Eriksen, H. R., B. Ellertsen, H. Gronningsaeter, K. O. Nakken, Y. Loyning, and H. Ursin. 1994. Physical exercise in women with intractable epilepsy. Epilepsia 35(6):1256-1264.
Fastenau, P. S., J. Shen, D. W. Dunn, S. M. Perkins, B. P. Hermann, and J. K. Austin. 2004. Neuropsychological predictors of academic underachievement in pediatric epilepsy: Moderating roles of demographic, seizure, and psychosocial variables. Epilepsia 45(10):1261-1272.
Fastenau, P. S., J. Shen, D. W. Dunn, and J. K. Austin. 2008. Academic underachievement among children with epilepsy: Proportion exceeding psychometric criteria for learning disability and associated risk factors. Journal of Learning Disabilities 41(3):195-207.
Fastenau, P. S., C. S. Johnson, S. M. Perkins, A. W. Byars, T. J. deGrauw, J. K. Austin, and D. W. Dunn. 2009. Neuropsychological status at seizure onset in children: Risk factors for early cognitive deficits. Neurology 73(7):526-534.
Fernandes, P. T., D. A. Snape, R. G. Beran, and A. Jacoby. 2011. Epilepsy stigma: What do we know and where next? Epilepsy and Behavior 22(1):55-62.
Fisher, R. S. 2000. Epilepsy from the patient’s perspective: Review of results of a community-based survey. Epilepsy and Behavior 1(4):S9-S14.
Fisher, R. S., B. G. Vickrey, P. Gibson, B. Hermann, P. Penovich, A. Scherer, and S. Walker. 2000. The impact of epilepsy from the patient’s perspective. I: Descriptions and subjective perceptions. Epilepsy Research 41(1):39-51.
Fountain, N. B., and A. C. May. 2003. Epilepsy and athletics. Clinics in Sports Medicine 22(3):605-616, x-xi.
Fountain, N. B., P. C. V. Ness, R. Swain-Eng, S. Tonn, and C. T. Bever. 2011. Quality improvement in neurology: AAN epilepsy quality measures. Report of the Quality Measurement and Reporting Subcommittee of the American Academy of Neurology. Journal of Neurology 76(1):94-99.
Fraser, R. T. 2011. Vocational and employment services/resources. PowerPoint presented at the IOM Workshop on Public Health Dimensions of the Epilepsies, June 29. http://iom.edu/~/media/Files/Activity%20Files/Disease/Epilepsy/Panel%206%20Fraser.pdf (accessed December 19, 2011).
Fraser, R. T., W. Trejo, and W. Blanchard. 1984. Epilepsy rehabilitation: Evaluating specialized versus general agency outcome. Epilepsia 25(3):332-337.
Gagliardi, M., M. Neighbors, C. Spears, S. Byrd, and J. Snarr. 1994. Emergencies in the school setting: Are public school teachers adequately trained to respond? Prehospital and Disaster Medicine 9(4):222-225.
Geerts, A., O. Brouwer, C. van Donselaar, H. Stroink, B. Peters, E. Peeters, and W. F. Arts. 2011. Health perception and socioeconomic status following childhood-onset epilepsy: The Dutch Study of Epilepsy in Childhood. Epilepsia 52(12):2192-2202.
Gilliam, F., R. Kuzniecky, E. Faught, L. Black, G. Carpenter, and R. Schrodt. 1997. Patient-validated content of epilepsy-specific quality-of-life measurement. Epilepsia 38(2): 233-236.
Gordon, K. E., J. M. Dooley, and P. M. Brna. 2010. Epilepsy and activity—A population-based study. Epilepsia 51(11):2254-2259.
Hames, A., and R. Appleton. 2009. Living with a brother or sister with epilepsy: Siblings’ experiences. Seizure 18(10):699-701.
Hamiwka, L. D., L. A. Hamiwka, E. M. Sherman, and E. Wirrell. 2011. Social skills in children with epilepsy: How do they compare to healthy and chronic disease controls? Epilepsy and Behavior 21(3):238-241.
Han, K., S. Choi-Kwon, and S. K. Lee. 2011. Leisure time physical activity in patients with epilepsy in Seoul, South Korea. Epilepsy and Behavior 20(2):321-325.
Hauser, W. A., and D. C. Hesdorffer. 1990. Epilepsy: Frequency, causes, and consequences. Landover, MD: Epilepsy Foundation of America.
Hawley, S. R., A. M. Paschal, E. Ablah, T. St. Romain, K. Liow, and C. A. Molgaard. 2007. Initial perspectives from Midwestern neurologists: Epilepsy patients’ barriers and motivators for seeking treatment. Epilepsia 48(10):1920-1925.
Hermann, B. P., M. Seidenberg, and B. Bell. 2002. The neurodevelopmental impact of childhood onset temporal lobe epilepsy on brain structure and function and the risk of progressive cognitive effects. Progress in Brain Research 135:429-438.
Hermann, B. P., J. E. Jones, R. Sheth, M. Koehn, T. Becker, J. Fine, C. A. Allen, and M. Seidenberg. 2008. Growing up with epilepsy: A two-year investigation of cognitive development in children with new onset epilepsy. Epilepsia 49(11):1847-1858.
Hernandez, B., C. Keys, and F. Balcazar. 2000. Employer attitudes toward workers with disabilities and their ADA employment rights: A literature review. Journal of Rehabilitation 66(4):4-16.
Hesdorffer, D. C., P. Ludvigsson, E. Olafsson, G. Gudmundsson, O. Kjartansson, and W. A. Hauser. 2004. ADHD as a risk factor for incident unprovoked seizures and epilepsy in children. Archives of General Psychiatry 61(7):731-736.
HHS (U.S. Department of Health and Human Services). 2004. Bone health and osteoporosis: A report of the Surgeon General. http://www.surgeongeneral.gov/library/bonehealth/content.html (accessed March 9, 2012).
Hicks, R. A., and M. J. Hicks. 1991. Attitudes of major employers toward the employment of people with epilepsy: A 30-year study. Epilepsia 32(1):86-88.
Hinnell, C., J. Williams, A. Metcalfe, S. B. Patten, R. Parker, S. Wiebe, and N. Jetté. 2010. Health status and health-related behaviors in epilepsy compared to other chronic conditions—A national population-based study. Epilepsia 51(5):853-861.
Houtenville, A. J., and R. V. Burkhauser. 2004. Did the employment of people with disabilities decline in the 1990s, and was the ADA responsible? A replication and robustness check of Acemoglu and Angrist (2001)—Research brief. Ithaca, NY: Cornell University. http://digitalcommons.ilr.cornell.edu/edicollect/91 (accessed January 3, 2012).
Hovinga, C. A., M. R. Asato, R. Manjunath, J. W. Wheless, S. J. Phelps, R. D. Sheth, J. E. Pina-Garza, W. M. Zingaro, and L. S. Haskins. 2008. Association of non-adherence to antiepileptic drugs and seizures, quality of life, and productivity: Survey of patients with epilepsy and physicians. Epilepsy and Behavior 13(2):316-322.
Howard, G. M., M. Radloff, and T. L. Sevier. 2004. Epilepsy and sports participation. Current Sports Medicine Reports 3(1):15-19.
Humphries, T., M. Neufeld, C. Johnson, K. Engels, and R. McKay. 2005. A pilot study of the effect of direct instruction programming on the academic performance of students with intractable epilepsy. Epilepsy and Behavior 6(3):405-412.
IOM (Institute of Medicine). 2008. Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: The National Academies Press.
IOM and NRC (National Research Council). 2011. The early childhood care and education workforce: Challenges and opportunities: A workshop report. Washington, DC: The National Academies Press.
Jacoby, A., and G. A. Baker. 2008. Quality-of-life trajectories in epilepsy: A review of the literature. Epilepsy and Behavior 12(4):557-571.
Jacoby, A., G. A. Baker, N. Steen, P. Potts, and D. W. Chadwick. 1996. The clinical course of epilepsy and its psychosocial correlates: Findings from a UK community study. Epilepsia 37(2):148-161.
Jacoby, A., J. Gorry, and G. A. Baker. 2005. Employers’ attitudes to employment of people with epilepsy: Still the same old story? Epilepsia 46(12):1978-1987.
Jakovljevic, V., and Z. Martinovic. 2006. Social competence of children and adolescents with epilepsy. Seizure 15(7):528-532.
Jalava, M., M. Sillanpää, C. Camfield, and P. Camfield. 1997. Social adjustment and competence 35 years after onset of childhood epilepsy: A prospective controlled study. Epilepsia 38(6):708-715.
John, C., and D. L. McLellan. 1988. Employers’ attitudes to epilepsy. British Journal of Industrial Medicine 45(10):713-715.
Jones, J. E., R. Watson, R. Sheth, R. Caplan, M. Koehn, M. Seidenberg, and B. Hermann. 2007. Psychiatric comorbidity in children with new onset epilepsy. Developmental Medicine and Child Neurology 49(7):493-497.
Kerr, C., A. Nixon, and M. Angalakuditi. 2011. The impact of epilepsy on children and adult patients’ lives: Development of a conceptual model from qualitative literature. Seizure 20(10):764-774.
Kobau, R., H. Zahran, D. Grant, D. J. Thurman, P. H. Price, and M. M. Zack. 2007. Prevalence of active epilepsy and health-related quality of life among adults with self-reported epilepsy in California: California Health Interview Survey, 2003. Epilepsia 48(10):1904-1913.
Kobau, R., H. Zahran, D. J. Thurman, M. M. Zack, T. R. Henry, S. C. Schachter, and P. H. Price. 2008. Epilepsy surveillance among adults—19 states, Behavioral Risk Factor Surveillance System, 2005. Morbidity and Mortality Weekly Report Surveillance Summaries 57(6):1-20.
Kokkonen, J., E. R. Kokkonen, A. L. Saukkonen, and P. Pennanen. 1997. Psychosocial outcome of young adults with epilepsy in childhood. Journal of Neurology, Neurosurgery and Psychiatry 62(3):265-268.
Konda, K., E. Ablah, K. S. Konda, and K. Liow. 2009. Health behaviors and conditions of persons with epilepsy: A bivariate analysis of 2006 BRFSS data. Epilepsy and Behavior 16(1):120-127.
Koot, H. M. 2001. The study of quality of life: Concepts and methods. In Quality of life in child and adolescent illness: Concepts, methods, and findings, edited by H. M. Koot and J. L. Wallander. New York: Taylor and Frances. Pp. 3-20.
Krauss, G. L., A. Krumholz, R. C. Carter, G. Li, and P. Kaplan. 1999. Risk factors for seizure-related motor vehicle crashes in patients with epilepsy. Neurology 52(7):1324-1329.
Krauss, G. L., L. Ampaw, and A. Krumholz. 2001. Individual state driving restrictions for people with epilepsy in the U.S. Neurology 57(10):1780-1785.
Krestel, H. E., A. Nirkko, A. von Allmen, C. Liechti, J. Wettstein, A. Mosbacher, and J. Mathis. 2011. Spike-triggered reaction-time EEG as a possible assessment tool for driving ability. Epilepsia 52(10):e126-e129.
Krumholz, A. 2003. To drive or not to drive: The 3-month seizure-free interval for people with epilepsy. Mayo Clinic Proceedings 78(7):817-818.
Kwon, C., M. Liu, H. Quan, V. Thoo, S. Wiebe, and N. Jetté. 2011. Motor vehicle accidents, suicides, and assaults in epilepsy: A population-based study. Neurology:801-806.
Laccheo, I., E. Ablah, R. Heinrichs, T. Sadler, L. Baade, and K. Liow. 2008. Assessment of quality of life among the elderly with epilepsy. Epilepsy and Behavior 12(2):257-261.
Lakin, K. C., and R. J. Stancliffe. 2007. Residential supports for persons with intellectual and developmental disabilities. Mental Retardation and Developmental Disabilities Research Reviews 13(2):151-159.
Lannon, S. L. 1992. Meeting the needs of children whose parents have epilepsy. Journal of Neuroscience Nursing 24(1):14-18.
Lee, B. 1996. Legal requirements and employer responses to accommodating employees with disabilities. Human Resource Management Review 6(4):231-251.
Lindsay, J., C. Ounsted, and P. Richards. 1979. Long-term outcome in children with temporal lobe seizures. I: Social outcome and childhood factors. Developmental Medicine and Child Neurology 21(3):285-298.
Lings, S. 2001. Increased driving accident frequency in Danish patients with epilepsy. Neurology 57(3):435-439.
Long, L., A. L. Reeves, J. L. Moore, J. Roach, and C. T. Pickering. 2000. An assessment of epilepsy patients’ knowledge of their disorder. Epilepsia 41(6):727-731.
Lv, R., L. Wu, L. Jin, Q. Lu, M. Wang, Y. Qu, and H. Liu. 2009. Depression, anxiety and quality of life in parents of children with epilepsy. Acta Neurologica Scandinavica 120(5):335-341.
Mansell, J., and J. Beadle-Brown. 2009. Dispersed or clustered housing for adults with intellectual disability: A systematic review. Journal of Intellectual and Developmental Disability 34(4):313-323.
Markenson, D., J. D. Ferguson, L. Chameides, P. Cassan, K. L. Chung, J. Epstein, L. Gonzales, R. A. Herrington, J. L. Pellegrino, N. Ratcliff, and A. Singer. 2010. Part 17: First aid: 2010 American Heart Association and American Red Cross guidelines for first aid. Circulation 122(18 Suppl. 3):S934-S946.
Martin, R., L. Vogtle, F. Gilliam, and E. Faught. 2005. What are the concerns of older adults living with epilepsy? Epilepsy and Behavior 7(2):297-300.
Martínez-Leal, R., L. Salvador-Carulla, C. Linehan, P. Walsh, G. Weber, G. Van Hove, T. Määttä, B. Azema, M. Haveman, S. Buono, A. Germanavicius, H. van Schrojenstein Lantman-de Valk, J. Tossebro, A. Carmen-Câra, D. Moravec Berger, J. Perry, and M. Kerr. 2011. The impact of living arrangements and deinstitutionalisation in the health status of persons with intellectual disability in Europe. Journal of Intellectual Disability Research 55(9):858-872.
Martiniuk, A. L., K. N. Speechley, M. Secco, M. K. Campbell, and A. Donner. 2007. Evaluation of an epilepsy education program for grade 5 students: A cluster randomized trial. Epilepsy and Behavior 10(4):604-610.
Martiniuk, A. L., M. Secco, L. Yake, and K. N. Speechley. 2010. Evaluating the effect of a television public service announcement about epilepsy. Health Education Research 25(6):1050-1060.
McAfee, A. T., K. E. Chilcott, C. B. Johannes, K. Hornbuckle, W. A. Hauser, and A. M. Walker. 2007. The incidence of first provoked and unprovoked seizure in pediatric patients with and without psychiatric diagnoses. Epilepsia 48(6):1075-1082.
McLachlan, R. S., E. Starreveld, and M. A. Lee. 2007. Impact of mandatory physician reporting on accident risk in epilepsy. Epilepsia 48(8):1500-1505.
McNelis, A. M., D. W. Dunn, C. S. Johnson, J. K. Austin, and S. M. Perkins. 2007. Academic performance in children with new-onset seizures and asthma: A prospective study. Epilepsy and Behavior 10(2):311-318.
Miele, V. J., J. E. Bailes, and N. A. Martin. 2006. Participation in contact or collision sports in athletes with epilepsy, genetic risk factors, structural brain lesions, or history of cra-niotomy. Neurosurgical Focus 21(4):E9.
Modi, A. C. 2009. The impact of a new pediatric epilepsy diagnosis on parents: Parenting stress and activity patterns. Epilepsy and Behavior 14(1):237-242.
Modi, A. C., A. S. King, S. R. Monahan, J. E. Koumoutsos, D. A. Morita, and T. A. Glauser. 2009. Even a single seizure negatively impacts pediatric health-related quality of life. Epilepsia 50(9):2110-2116.
Mount, D., B. Johnstone, C. White, and A. Sherman. 2005. Vocational outcomes: VR service determinants for persons with epilepsy. Journal of Vocational Rehabilitation 23:11-20.
NACCRRA (National Association of Child Care Resource and Referral Agencies). 2011. Child care in America: 2011 state fact sheets. http://www.naccrra.org/policy/docs/ChildCareInAmericaFacts_2011_090611_reprint.pdf (accessed January 3, 2012).
———. n.d. Child care in America. http://www.naccrra.org/policy/docs/childcareinamericafactsheet.doc (accessed March 9, 2012).
Nakken, K. O. 1999. Physical exercise in outpatients with epilepsy. Epilepsia 40(5):643-651.
Nakken, K. O., P. G. Bjørholt, S. I. Johannessen, T. Løyning, and E. Lind. 1990. Effect of physical training on aerobic capacity, seizure occurrence, and serum level of antiepileptic drugs in adults with epilepsy. Epilepsia 31(1):88-94.
Nakken, K. O., A. Løyning, T. Løyning, G. Gløersen, and P. G. Larsson. 1997. Does physical exercise influence the occurrence of epileptiform EEG discharges in children? Epilepsia 38(3):279-284.
NGFATOS (National Guidelines for First Aid Training in Occupational Settings). 2002. National guidelines for first aid training in occupational settings, first aid provider core elements, course guide. 2nd edition. http://ntl.bts.gov/lib/24000/24700/24757/ngfatos.pdf (accessed January 3, 2012).
O’Dell, C., K. O’Hara, S. Kiel, and K. McCullough. 2007a. Emergency management of seizures in the school setting. Journal of School Nursing 23(3):158-165.
O’Dell, C., J. W. Wheless, and J. Cloyd. 2007b. The personal and financial impact of repetitive or prolonged seizures on the patient and family. Journal of Child Neurology 22(5 Suppl.):61S-70S.
Oostrom, K. J., A. Smeets-Schouten, C. L. Kruitwagen, A. C. Peters, and A. Jennekens-Schinkel. 2003. Not only a matter of epilepsy: Early problems of cognition and behavior in children with “epilepsy only”—A prospective, longitudinal, controlled study starting at diagnosis. Pediatrics 112(6 Pt. 1):1338-1344.
Pack, A. M. 2011. Treatment of epilepsy to optimize bone health. Current Treatment Options in Neurology 13(4):346-354.
Pack, A. M., and M. J. Morrell. 2004. Epilepsy and bone health in adults. Epilepsy and Behavior 5(Suppl. 2):S24-S29.
Paschal, A. M., E. Ablah, R. Wetta-Hall, C. A. Molgaard, and K. Liow. 2005. Stigma and safe havens: A medical sociological perspective on African-American female epilepsy patients. Epilepsy and Behavior 7(1):106-115.
Pugh, M. J., L. A. Copeland, J. E. Zeber, J. A. Cramer, M. E. Amuan, J. E. Cavazos, and L. E. Kazis. 2005. The impact of epilepsy on health status among younger and older adults. Epilepsia 46(11):1820-1827.
Ramaglia, G., A. Romeo, M. Viri, M. Lodi, S. Sacchi, and G. Cioffi. 2007. Impact of idio-pathic epilepsy on mothers and fathers: Strain, burden of care, worries and perception of vulnerability. Epilepsia 48(9):1810-1813.
Rantanen, K., S. Timonen, K. Hagstrom, P. Hamalainen, K. Eriksson, and P. Nieminen. 2009. Social competence of preschool children with epilepsy. Epilepsy and Behavior 14(2):338-343.
Rätsepp, M., A. Oun, S. Haldre, and A. E. Kaasik. 2000. Felt stigma and impact of epilepsy on employment status among Estonian people: Exploratory study. Seizure 9(6):394-401.
Roberts, R. M., and H. S. Farhana. 2010. Effectiveness of a first aid information video in reducing epilepsy-related stigma. Epilepsy and Behavior 18(4):474-480.
Rodenburg, R., G. J. Stams, A. M. Meijer, A. P. Aldenkamp, and M. Dekovic. 2005. Psychopathology in children with epilepsy: A meta-analysis. Journal of Pediatric Psychology 30(6):453-468.
Rodenburg, R., A. M. Meijer, M. Dekovic, and A. P. Aldenkamp. 2007. Parents of children with enduring epilepsy: Predictors of parenting stress and parenting. Epilepsy and Behavior 11(2):197-207.
Roessler, R. T., and G. Sumner. 1997. Employer opinions about accommodating employees with chronic illnesses. Journal of Applied Rehabilitation Counseling 28(3):29-34.
Rolland, J. S. 1994. Families, illness, and disability: An integrative treatment model. New York: Basic Books.
Rubin, R. 2011. Independent living resources for individuals with epilepsy. PowerPoint presented at the IOM Workshop on Public Health Dimensions of the Epilepsies, June 29. http://iom.edu/~/media/Files/Activity%20FilesDisease/Epilepsy/Panel%206%20Rubin.pdf (accessed December 19, 2011).
Saburi, G. 2011. Stressors of caregivers of school-age children with epilepsy and use of community resources. Journal of Neuroscience Nursing 43(3):E1-E12.
Sahoo, S. K., and N. B. Fountain. 2004. Epilepsy in football players and other land-based contact or collision sport athletes: When can they participate, and is there an increased risk? Current Sports Medicine Reports 3(5):284-288.
Salinsky, M. C., K. Wegener, and F. Sinnema. 1992. Epilepsy, driving laws, and patient disclosure to physicians. Epilepsia 33(3):469-472.
Samaniego, E. A., and R. D. Sheth. 2007. Bone consequences of epilepsy and antiepileptic medications. Seminars in Pediatric Neurology 14(4):196-200.
Sands, H., and S. S. Zalkind. 1972. Effects of an educational campaign to change employer attitudes toward hiring epileptics. Epilepsia 13(1):87-96.
Sapien, R. E., and A. Allen. 2001. Emergency preparation in schools: A snapshot of a rural state. Pediatric Emergency Care 17(5):329-333.
Sare, G., M. Rawnsley, A. Stoneman, and S. Duncan. 2007. Men with epilepsy—The lost tribe? Results of a nationwide survey of men with epilepsy living in the UK. Seizure 16(5):384-396.
Sbarra, D. A., S. E. Rimm-Kaufman, and R. C. Pianta. 2002. The behavioral and emotional correlates of epilepsy in adolescence: A 7-year follow-up study. Epilepsy and Behavior 3(4):358-367.
Schoenfeld, J., M. Seidenberg, A. Woodard, K. Hecox, C. Inglese, K. Mack, and B. Hermann. 1999. Neuropsychological and behavioral status of children with complex partial seizures. Developmental Medicine and Child Neurology 41(11):724-731.
Schouten, A., K. J. Oostrom, W. R. Pestman, A. C. Peters, and A. Jennekens-Schinkel. 2002. Learning and memory of school children with epilepsy: A prospective controlled longitudinal study. Developmental Medicine and Child Neurology 44(12):803-811.
Seidenberg, M., N. Beck, M. Geisser, B. Giordani, J. C. Sackellares, S. Berent, F. E. Dreifuss, and T. J. Boll. 1986. Academic achievement of children with epilepsy. Epilepsia 27(6): 753-759.
Shackleton, D. P., D. G. Kasteleijn-Nolst Trenite, A. J. de Craen, J. P. Vandenbroucke, and R. G. Westendorp. 2003. Living with epilepsy: Long-term prognosis and psychosocial outcomes. Neurology 61(1):64-70.
Shareef, Y. S., J. H. McKinnon, S. M. Gauthier, K. H. Noe, J. I. Sirven, and J. F. Drazkowski. 2009. Counseling for driving restrictions in epilepsy and other causes of temporary impairment of consciousness: How are we doing? Epilepsy and Behavior 14(3):550-552.
Sheth, S. G., G. Krauss, A. Krumholz, and G. Li. 2004. Mortality in epilepsy: Driving fatalities vs. other causes of death in patients with epilepsy. Neurology 63(6):1002-1007.
Sillanpää, M. 1983. Social functioning and seizure status of young adults with onset of epilepsy in childhood. An epidemiological 20-year follow-up study. Acta Neurologica Scandinavica Supplementum 96:1-81.
———. 2004. Learning disability: Occurrence and long-term consequences in childhood-onset epilepsy. Epilepsy and Behavior 5(6):937-944.
Sillanpää, M., M. Jalava, O. Kaleva, and S. Shinnar. 1998. Long-term prognosis of seizures with onset in childhood. New England Journal of Medicine 338(24):1715-1722.
Smeets, V. M., B. A. van Lierop, J. P. Vanhoutvin, A. P. Aldenkamp, and F. J. Nijhuis. 2007. Epilepsy and employment: Literature review. Epilepsy and Behavior 10(3):354-362.
Smith, M. L., I. M. Elliott, and L. Lach. 2004. Cognitive, psychosocial, and family function one year after pediatric epilepsy surgery. Epilepsia 45(6):650-660.
Solans, M., S. Pane, M. D. Estrada, V. Serra-Sutton, S. Berra, M. Herdman, J. Alonso, and L. Rajmil. 2008. Health-related quality of life measurement in children and adolescents: A systematic review of generic and disease-specific instruments. Value in Health 11(4):742-764.
Steffenburg, S., C. Gillberg, and U. Steffenburg. 1996. Psychiatric disorders in children and adolescents with mental retardation and active epilepsy. Archives of Neurology 53(9):904-912.
Strzelczyk, A., J. P. Reese, R. Dodel, and H. M. Hamer. 2008. Cost of epilepsy: A systematic review. Pharmacoeconomics 26(6):463-476.
Sturniolo, M. G., and F. Galletti. 1994. Idiopathic epilepsy and school achievement. Archives of Disease in Childhood 70(5):424-428.
Tatum, W. O., A. V. Worley, and M. L. Selenica. 2012. Disobedience and driving in patients with epilepsy. Epilepsy and Behavior 23(1):30-35.
Taylor, J., D. W. Chadwick, and T. Johnson. 1995. Accident experience and notification rates in people with recent seizures, epilepsy or undiagnosed episodes of loss of consciousness. QJM: An International Journal of Medicine 88(10):733-740.
Taylor, J., A. Jacoby, G. A. Baker, and A. G. Marson. 2011a. Self-reported and parent-reported quality of life of children and adolescents with new-onset epilepsy. Epilepsia 52(8):1489-1498.
Taylor, R. S., J. W. Sander, R. J. Taylor, and G. A. Baker. 2011b. Predictors of health-related quality of life and costs in adults with epilepsy: A systematic review. Epilepsia 52(12):2168-2180.
Thompson, P. J., and D. Upton. 1992. The impact of chronic epilepsy on the family. Seizure 1(1):43-48.
Thorbecke, R., and R. T. Fraser. 2008. The range of needs and services in vocational rehabilitation. In Epilepsy: A comprehensive textbook, second edition. Vol. 3, edited by J. J. Engel and T. A. Pedley. Philadelphia, PA: Lippincott Williams and Wilkins. Pp. 2253-2263.
Tomson, T., E. Beghi, A. Sundqvist, and S. I. Johannessen. 2004. Medical risks in epilepsy: A review with focus on physical injuries, mortality, traffic accidents and their prevention. Epilepsy Research 60(1):1-16.
U.S. Access Board. 2008. The ADA Amendments Act of 2008. http://access-board.gov/about/laws/ADA-amendments.htm (accessed December 16, 2011).
U.S. Department of Education. 2011a. Protecting students with disabilities: Frequently asked questions about Section 504 and the education of children with disabilities. http://www.2ed.gov/about/offices/list/ocr/504faq.html (accessed December 16, 2011).
———. 2011b. Sec. 300.320 definition of individualized education program. http://idea.ed.gov/explore/view/p/,root,regs,300,D,300%252E320, (accessed December 16, 2011).
———. 2011c. Individualized education program (IEP), team meetings and changes to the IEP. http://idea.ed.gov/explore/view/p/%2Croot%2Cdynamic%2CTopicalBrief%2C9%2C, (accessed March 9, 2012).
U.S. Department of Justice. 2005. A guide to disability rights laws. http://www.ada.gov/cguide.htm#anchor63409 (accessed March 9, 2012).
U.S. Department of Labor, Employment and Training Administration. 2012. CareerOneStop. hhtp://www.careeronestop.org (accessed March 12, 2012).
van Blarikom, W., I. Y. Tan, A. P. Aldenkamp, and A. T. G. van Gennep. 2006. Epilepsy, intellectual disability, and living environment: A critical review. Epilepsy and Behavior 9(1):14-18.
———. 2009. Living environment of persons with severe epilepsy and intellectual disability: A prospective study. Epilepsy and Behavior 14(3):484-490.
Verrotti, A., C. D′Egidio, A. Mohn, G. Coppola, and F. Chiarelli. 2011. Weight gain following treatment with valproic acid: Pathogenetic mechanisms and clinical implications. Obesity Reviews 12(5):e32-e43.
Vogtle, L. K., R. Martin, H. R. Foushee, and R. E. Faught. 2007. A comparison of physicians′ attitudes and beliefs regarding driving for persons with epilepsy. Epilepsy and Behavior 10(1):55-62.
Webster, N. J., P. Crawford, and F. M. Thomas. 2011. Who′s behind the wheel? Driving with medically intractable epilepsy. American Journal of Health Behavior 35(4):485-495.
Welty, T. E., S. L. Willis, and E. A. Welty. 2010. Effect of limited transportation on medication adherence in patients with epilepsy. Journal of the American Pharmacists Association 50(6):698-703.
Westphal-Guitti, A. C., N. B. Alonso, R. C. V. P. Migliorini, T. I. da Silva, A. M. Azevedo, L. O. Caboclo, A. C. Sakamoto, and E. M. Yacubian. 2007. Quality of life and burden in caregivers of patients with epilepsy. Journal of Neuroscience Nursing 39(6):354-360.
Wheless, J. W. 2006. Intractable epilepsy: A survey of patients and caregivers. Epilepsy and Behavior 8(4):756-764.
WHO (World Health Organization). 1996. WHOQOL-BREF: Introduction, administration, scoring and generic version of the assessment. Geneva, Switzerland: WHO. http://www.who.int/mental_health/media/en/76.pdf (accessed January 3, 2012).
Wicks, P., D. L. Keininger, M. P. Massagli, C. D. la Loge, C. Brownstein, J. Isojarvi, and J. Heywood. 2012. Perceived benefits of sharing health data between people with epilepsy on an online platform. Epilepsy and Behavior 23(1):16-23.
Wiebe, S., D. R. Bellhouse, C. Fallahay, and M. Eliasziw. 1999. Burden of epilepsy: The Ontario Health Survey. Canadian Journal of Neurological Sciences 26(4):263-270.
Wilson, I. B., and P. D. Cleary. 1995. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 273(1):59-65.
Wodrich, D. L., R. Jarrar, J. Buchhalter, R. Levy, and C. Gay. 2011. Knowledge about epilepsy and confidence in instructing students with epilepsy: Teachers′ responses to a new scale. Epilepsy and Behavior 20(2):360-365.
Wong, J., and E. Wirrell. 2006. Physical activity in children/teens with epilepsy compared with that in their siblings without epilepsy. Epilepsia 47(3):631-639.
Wong, I. Y. L., and V. Stanhope. 2009. Conceptualizing community: A comparison of neighborhood characteristics of supportive housing for persons with psychiatric and developmental disabilities. Social Science and Medicine 68(8):1376-1387.
Wood, L. J., E. M. S. Sherman, L. D. Hamiwka, M. A. Blackman, and E. C. Wirrell. 2008. Maternal depression: The cost of caring for a child with intractable epilepsy. Pediatric Neurology 39(6):418-422.
Yagi, K. 1998. Epilepsy: Comprehensive care, quality of life, and factors preventing people with epilepsy from being employed. Clinical Therapeutics 20(Suppl. A):A19-A29.