Key Messagesa
• According to national surveillance results, China has the second largest MDR TB burden among 27 MDR TB HBCs.
• As China has accumulated experience with MDR TB control, new models, new diagnostic methods, and new funding mechanisms have been implemented.
• Many MDR and XDR TB patients are treated at hospitals in China, and studies have shown that transmission is occurring in these settings.
• China’s capacity to conduct DST remains limited.
• HIV infection and other health problems such as diabetes contribute to the problem of MDR TB in China.
__________________
a Identified by individual speakers.
China has a population of more than 1.3 billion and a per capita gross domestic product of about $5,400. Several speakers at the workshop described the status of DR TB in China and efforts to control the disease. Participants discussed the results of a drug-resistance surveillance released in 2012, which provided crucial information that is being used to shape the country’s programmatic management of MDR TB. As they sought to explore multiple aspects and characteristics of the epidemiology of MDR
TB in China, participants also discussed the country’s MDR and XDR TB regimens, the treatment of MDR TB in hospitals, the role of HIV infection, and diabetes as a comorbidity in TB patients.
MANAGEMENT OF MDR TB IN CHINA1
Mingting Chen, Vice Director and Researcher, National Center for Tuberculosis Control and Prevention, China CDC, described survey information on China’s MDR TB prevalence and treatment and prevention approaches.
Results from the 2010 Fifth Nationwide TB Prevalence Survey in China show that all types of TB declined to 459 per 100,000 in 2010, compared with 466 per 100,000 in 2000. Smear-positive TB declined from 169 per 100,000 in 2000 to 66 per 100,000 in 2010—a “remarkable decrease” of about 61 percent, said Mingting Chen. Bacteriologically confirmed TB fell from 216 per 100,000 in 2000 to 119 per 100,000 a decade later, a decrease of 45 percent. China has 100 percent coverage of Directly Observed Treatment-Short course (DOTS), its case detection rate of new TB cases is 80 percent, and its cure rate for new TB cases is above 90 percent. More than 4.5 million smear-positive patients were cured from 2001 to 2010, and China achieved its millennium development goal for TB control 5 years ahead of schedule.
Chen laid out the steps necessary to prevent MDR and XDR TB. First, the quality of basic DOTS needs to be enhanced by consolidating a strong government commitment, improving the TB laboratory services network, and improving identification and care of TB patients in vulnerable groups. In addition, the recording and reporting system for TB needs to be strengthened, the quality of FLDs and SLDs needs to be improved, standard operating procedures in drug supply and management systems need to be implemented, and cooperation between public health institutions (such as China CDC) and hospitals needs to be intensified.
China has undertaken technical support for the treatment of MDR and XDR TB patients, providing national guidelines for the management of DR TB, issued in 2012 by China CDC; a manual for management of SLDs; guidelines for infection control; guidelines for adverse reactions to DR TB chemotherapy; and standard operating procedures for culture and DST. China also has launched a pilot project for the programmatic treatment and management of MDR and XDR TB patients (PMDRT). This initiative includes the formulation of a national framework and working plan for the PMDRT, as well as a gradual increase in the number of pilot
__________________
1 This section is based on the presentation by Mingting Chen, Vice Director and Researcher, National Center for Tuberculosis Control and Prevention, China CDC.
sites for implementation of drug resistance surveillance. The project also involves improving laboratory services at each level so they can meet the standards for MDR TB diagnostic tests, such as TB culture and DST. A projected future laboratory network for China would include various levels of laboratory services and diagnostic technologies at coverage levels ranging from the county to the entire nation (Table 4-1). Also, as part of treatment for MDR and XDR TB patients, the national drug resistance surveillance effort selected 70 counties as survey sites and enrolled more than 4,600 smear-positive patients, including 3,500 new patients and 1,100 retreatment patients. At the provincial level, 20 of China’s 30 provinces conducted drug-resistance surveys, with support from WHO, the Global Fund, and local governments. In addition, the Ministry of Health conducted a survey to determine stakeholders’ attitudes toward policies aimed at combating MDR and XDR TB to predict the cost-effectiveness of the PMDRT and to provide support for the PMDRT among policy makers.
China has established a model of cooperation between hospitals and public health centers, Mingting Chen said. Hospitals have responsibility for diagnosis, treatment, and side effects for MDR TB patients. China CDC has the responsibility for management, supervision, follow-up, detection, and drug management. Both have responsibility for reporting information to TB management information systems.
The PMDRT has received support from the Global Fund. In addition, the Bill & Melinda Gates Foundation (BMGF) has supported the development of new models, new tools, and new techniques for preventing and controlling MDR and XDR TB. This support has enabled evaluation of a number of new diagnostic technologies, including LED (light-emitting diode) microscopy, LAMP (loop-mediated isothermal amplification), the Hain test, Genechip from Boao Technical Company, and GeneXpert. In addition, China has accelerated the assessment and implementation of rapid diagnostic methods through internal initiatives and partnerships with international organizations.
These experiences have contributed to the development of an action plan for regulating the use of SLDs, building a new financing mechanism for MDR TB control, establishing MDR TB treatment and management sites at the prefecture level, fostering cooperation between TB dispensaries and other health services, enhancing human resources, and designing an appropriate case-finding strategy. High-risk populations have priority, said Chen, after which all smear-positive patients will receive screening tests for MDR TB.
The National Tuberculosis Plan, published in November 2011, calls for building up the laboratory network by 2015 so that more than 80 percent of county TB laboratories can conduct sputum culture tests, all prefecture-level laboratories can carry out DST, and all regional-level laboratories can
TABLE 4-1 Projected Future TB Laboratory Network in China
| LED Microscopy | Solid Culture and DST | Solid DST | Molecular Test | Liquid Culture and DST | Biosafety | |
| Supranational Level/National Level | Yes | Yes | Yes | Yes | Yes | P3 and P2 |
| Provincial Level | Yes | Yes | Yes | Yes | Maybe | At Least P2 |
| Prefecture Level | Yes | Yes | Yes | Yes | Maybe | P2 |
| County level | Yes | Maybe | No | Maybe | Maybe | P2 |
NOTE: DST, drug susceptibility testing; LED, light-emitting diode.
SOURCE: Mingting Chen, 2013. Presentation at the IOM workshop on the Global Crisis of Drug-Resistant Tuberculosis and the Leadership of the BRICS Countries: Challenges and Opportunities.
perform strain identification (Table 4-1). In addition, MDR TB management will be expanded so that by 2015, prefecture-based MDR TB management will have reached 50 percent, and the screening rate of patients suspected of having MDR TB will have reached 60 percent. The scale-up plan of the PMDRT for 2012 to 2015 has been designed to enhance training for TB dispensary staff and supervision for MDR TB work. The plan also calls for organizing monitoring missions to supervise the plan’s implementation, along with quarterly notification of target accomplishment status, the development of local TB control programs, and application for sustainable funding once Global Fund support ends.
Funding is critical for the future of TB and MDR TB control in China, Mingting Chen noted. Funding comes from a combination of sources, including governments, insurance, and patients. In July 2011, the Ministry of Health issued a policy on integrating MDR TB treatment into medical insurance for rural residents, with 70 percent reimbursement, 20 percent medical aid, and 10 percent self-payment. By July 2012, MDR TB had been integrated into the local National Rural Medical Care System pilots in 25 provinces, ensuring more than 70 percent compensation.
Mingting Chen added in conclusion that legislation is important to govern the isolation and travel of MDR TB patients. Also important is evaluation of China’s efforts to control and prevent MDR TB.
2007 NATIONAL SURVEY OF DRUG RESISTANCE IN CHINA2
The drug resistance surveillance effort that released its results in 2012 had several goals, said Yanlin Zhao, China CDC:
• To interpret the epidemiological status of DR TB in China.
• To analyze the risk factors for drug resistance occurrence among TB patients.
• To explore the biological characteristics of the predominant mycobacterium bacillus in China.
• To understand the micro-evolution of the prevalent strains in China.
Seventy clusters, or sites, were selected according to new smear-positive cases reported by each province relative to the total number of cases nationwide in 2004 and 2005, with all provinces having at least one cluster. Susceptibility testing was conducted for six anti-TB drugs: ethambutol, isoniazid, kanamycin, ofloxacin, rifampicin, and streptomycin. Equipment, reagents, records, and questionnaires were standardized for all the sites, and the survey workers received centralized training. The work of all the clusters was supervised, with special support for priority sites.
The survey revealed an MDR TB rate of 5.7 percent among new cases and 25.6 percent among previously treated cases, with a combined rate of 8.3 percent (Zhao et al., 2012). XDR TB rates were 0.47 percent for new cases, 2.06 percent for previously treated cases, and 0.68 percent overall. Furthermore, among new cases, 1.8 percent of patients with MDR TB were already resistant to ofloxacin or kanamycin, as were 8.5 percent of previously treated patients. According to Mingting Chen, the survey results indicate that China has the second-largest MDR TB burden among 27 HBCs.
Among the patients who completed treatment, the majority did so at China CDC facilities (Figure 4-1). The patients who did not complete treatment were more likely to have received that treatment at general hospitals or private facilities. In addition, one of the risk factors for DR TB among previously treated patients was receiving two or more treatments at TB hospitals or other medical facilities. Closer cooperation is needed between the China CDC and other medical facilities to reduce these gaps, said Yanlin Zhao.
To prevent MDR TB, new tools are needed to detect suspected cases of MDR TB and to base treatment regimes on resistance tests. Patients starting treatment in hospitals need follow-up after discharge until they complete the regimen. A better linkage between the hospital system and
__________________
2 This section is based on the presentation by Yanlin Zhao, Vice Director, National Center for Disease Control and Prevention; and Director, National Tuberculosis Reference Laboratory, China CDC.
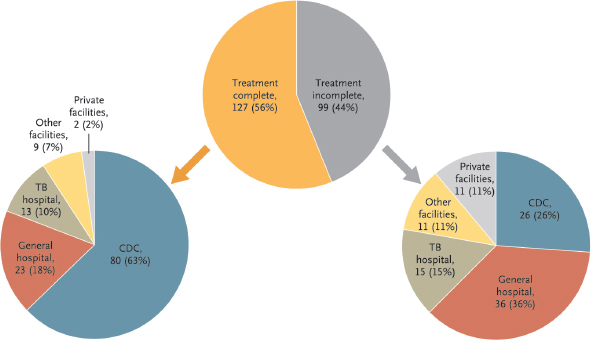
FIGURE 4-1 The majority of MDR TB patients who completed treatment did so at China CDC facilities.
SOURCE: From the New England Journal of Medicine, Zhao, Y., S. Xu, L. Wang, D. P. Chin, S. Wang, G. Jiang, H. Xia, Y. Zhou, Q. Li, X. Ou, Y. Pang, Y. Song, B. Zhao, H. Zhang, G. He, J. Guo, and Y. Wang, National survey of drug-resistant tuberculosis in China, 366(23), 2161–2170. Copyright © 2012 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
China CDC could improve the treatment provided by hospitals, strengthen infection control, and enhance follow-up after discharge. When MDR TB is detected in a patient, the patient is referred to a specialized hospital for second-line treatment. These specialized hospitals need to be strengthened and linked to the China CDC system, Yanlin Zhao said. China CDC maintains an ongoing DOTS program that uses smear microscopy for diagnosis, empirical treatment using a standardized regimen of FLDs, and community case management. Collaborations between China CDC and hospitals can improve the capability for rapid molecular diagnosis of TB and provision of diagnosis-based treatments. In addition, community-based care management can help ensure that a patient follows the treatment regimen. The use of mobile phones and medical monitors can support community case management.
Preventing DR TB among new cases requires identifying patients with no prior diagnosis of TB who were given TB drugs. They likely were suspected to have TB and started on TB drugs but did not receive a proper diagnosis. If they took TB drugs improperly for a sufficient period of time, MDR TB may have developed.
It is important to “turn off the tap” of DR TB, said Yanlin Zhao. Current factors causing drug resistance to develop will lead to the rapid loss of effectiveness of any new drug. Especially as new drugs become available, it is critical to improve systems, adopt new diagnostics, and use new drugs in a rational manner to prevent the development of drug resistance. In particular, the level of quinolone resistance has implications for the development and use of new regimens using that drug. The fact that one-third of MDR TB cases have quinolone resistance may limit the use of new regimens for MDR TB.
Yanlin Zhao is involved with an effort to collect and sequence strains of the bacterium, which makes it possible to do cluster analysis of cases. These data can be used to answer such questions as
• What is the population structure of the prevalent TB strains in China?
• What advantages do they have to become the prevalent strains?
• How do the prevalent strains interact with hosts and the environment?
• What are the risks to health care workers, and are infection control measures effective?
Finally, Yanlin Zhao briefly described plans for the next survey of drug resistance in China. The survey will continue to use the 70 clusters as sites, which will enable tracking prevalence over time. It will be possible to compare regions and genotypes to determine the effects of economic and
cultural forces and to use this information to inform individualized case management.
THE DIAGNOSIS AND TREATMENT OF MDR TB IN HOSPITALS3
When patients are diagnosed with TB in China, they receive the DOTS regimen of four drugs for 6 months, said Wenhong Zhang, Professor of Medicine, and Director, Division of Infectious Diseases, Shanghai Huashan Hospital, Fudan University. If patients have a previous history of treatment, they receive DOTS-Plus in addition to another medication for 8 months. If treatment fails, patients are transferred to a higher-level facility such as a TB hospital.
Because of these procedures, hospitals in China accumulate many DR TB cases. These cases differ from cases in other countries with a low disease burden, such as South Africa or the Americas, Wenhong Zhang emphasized. For example, the 2-month sputum conversion rate is much lower in China than in Western countries.
In a study of patients with MDR TB 4 years after standardized FLD treatment, it was found that the overall recurrence rates among new and retreatment cases were 46 percent and 66 percent, respectively; the overall death rates among new and retreatment cases were 25 percent and 46 percent, respectively; and 40 percent of the traced new cases and 24 percent of the retreatment cases were alive and without recurrent TB (He et al., 2010). These grim data highlight the importance of detecting MDR TB so that these patients are not given the standard DOTS regimen, which can augment the evolution of MDR and XDR TB, Wenhong Zhang said.
According to data from Hunan province (Deng et al., 2011), the rate of resistance to SLDs among MDR TB patients was almost 60 percent, including 53 percent to fluoroquinolones, 18 percent to amikacin, and 22 percent to capreomycin. The overall rate of XDR TB among these patients was a “very high” 18.7 percent. The high rate of fluoroquinolone resistance is especially troubling because the outcome of treatment often depends on this factor.
MDR and XDR TB can be either acquired from treatment or transmitted by other patients, but the relative importance of these two pathways in China is unknown. Citing a paper that had not yet been published at the time of the workshop, Wenhong Zhang said that he and his colleagues demonstrated the existence of XDR TB transmission in a provincial TB hospital through studies of more than 3,000 strains. They also were able to track the evolution of the strains toward greater drug resistance. These
__________________
3 This section is based on the presentation by Wenhong Zhang, Professor of Medicine, and Director, Division of Infectious Diseases, Shanghai Huashan Hospital, Fudan University.
data point toward the role of person-to-person transmission and the importance of quarantining MDR and XDR TB patients to contain the spread of disease, Wenhong Zhang said.
Wenhong Zhang and his colleagues also have examined a number of risk factors for MDR TB, including the frequency of hospital visits, age, occupation, and history of TB treatment. Two risk factors are particularly prominent: a history of TB treatment and delay in the diagnosis of TB. The results of sputum smear tests after 2 months of treatment are very important for treatment decisions as well. Wenhong Zhang also commented on the new policy in China, effective in 2010, providing that the China CDC would no longer treat patients but would provide management, supervision, and follow-up. He noted that lack of awareness that a patient should be followed up by China CDC is another MDR TB risk factor.
WHO recommends that all patients with suspected TB be tested for drug susceptibility. In treatment failure and retreatment cases, it recommends rapid DST for isoniazid and rifampicin resistance and treatment of patients empirically with second-line regimens until the test results are available. The capacity for DST in China remains limited. Most TB patients are in county hospitals, not in TB hospitals. As a result, the majority of patients cannot be tested for drug susceptibility. In 2008, China had just 52 laboratories able to conduct DST. That number has since grown to 81 and will exceed 100 in the next 2 years. Citing an article in preparation at the time of the workshop, Wenhong Zhang said that he and his colleagues have demonstrated the value of a new-generation polymerase chain reaction (PCR)-based LPA in detecting resistance to ethambutol, kanamycin, and ofloxacin. This assay could function as a supplement to traditional DST, he said, allowing for better treatment decisions in China.
Many factors affect the health outcomes of patients, Wenhong Zhang concluded, including the absence of DST for all patients, the duration of treatment, the lack of effective vaccines and high-quality drugs, the emergence and transmission of drug-resistant strains, and weak health systems in resource-poor regions. He suggested that a massive funding and political commitment is needed in China to ensure that the aims of the WHO Global Plan to Stop Tuberculosis 2006–2015 are achieved.
MDR AND XDR TB CHEMOTHERAPY IN CHINA4
According to Shou-Yong Tan, President, Guangzhou Chest Hospital, a treatment regimen for MDR or XDR TB should include pyrazinamide, a fluoroquinolone, a parenteral agent, ethionamide (or prothionamide),
__________________
4 This section is based on the presentation by Shou-Yong Tan, President, Guangzhou Chest Hospital.
and cycloserine, or PAS (para-aminosalicylic acid) if cycloserine cannot be used. It also should include at least four SLDs likely to be as effective as pyrazinamide during the intensive phase of treatment.
Strategies for treatment can be standardized, empirical, or individualized. The standardized treatment, to be given when DST is unavailable, is based on data from drug resistance surveillance in a representative patient population. The empirical treatment is based on each patient’s past history of anti-TB therapy. The individualized treatment is based on each patient’s past history of anti-TB therapy and the current results of DST.
The Guangzhou Chest Hospital TB Department has been exclusively responsible for the diagnosis and treatment of MDR TB in the Guangzhou region. All patients have been treated with the Global Fund MDR TB treatment regimen. From July 2008 through December 2012, 800 TB cases were treated, with 183 having MDR TB and 19 having XDR TB. Of all MDR TB patients who completed 24 months of standardized treatment, 30 (54.6 percent) were hospitalized, including 14 (25.5 percent) with hospital stays longer than 1 month. Among these patients, the cure rate was 63.3 percent, which was significantly higher than that in nonhospitalized patients. The failure rate in hospitalized patients was 23.3 percent, which was comparable to that for nonhospitalized patients. The dropout rate among hospitalized patients was just 6.7 percent, which was significantly lower than the overall dropout rate of 18.2 percent.
Overall mortality was 12.7 percent. The mortality in hospitalized patients was 6.7 percent, again significantly lower than for nonhospitalized patients. The overall cure rate for XDR TB patients who completed the 24-month standardized treatment was 0 percent.
According to these results, the hospitalized patients had a higher cure rate, a lower dropout rate, and lower mortality than the nonhospitalized patients. However, this regimen failed in all XDR TB patients. Irregular treatment or an unsatisfactory regimen, including unreasonable drug combinations, inadequate dosing, or a duration of treatment less than 24 months, are major factors linked to treatment failure.
Some MDR and XDR TB patients at the hospital also have undergone individualized treatments involving the use of immunomodulators, surgery, or other interventions, said Shou-Yong Tan. The cure rate, failure rate, and mortality among patients receiving such treatments were comparable to those for patients receiving the standardized treatment. Immunomodulators, surgery, or other interventional procedures showed modest impacts on treatment outcomes.
DRUG-RESISTANT TB AND HIV IN CHINA5
The Guangxi Zhuang Autonomous Region is located in the southern part of China, north of Vietnam, said Liu Feiying, Guangxi Zhuang Autonomous Region Center for Disease Control and Prevention, China. It has a population of about 50 million, 38 percent of whom are minorities, living primarily in the 70 percent of the region covered with mountains and hills.
Guangxi has a high burden of TB and HIV infection, with the second highest rate of HIV infection in China. However, the prevalence of infection with M.tb. and nontuberculous mycobacteria (NTM) in HIV-infected patients in China is unknown.
Feiying described a recent study that estimated the prevalence of M.tb. and NTM in HIV-infected patients in Guangxi province, determined the drug resistance of M.tb., and evaluated the genotypic patterns of M.tb. strains. Samples were collected from two HIV-designated hospitals in Guangxi from 2005 to 2008 and cultured using liquid and solid methods. HIV-infected patients with positive mycobacterial cultures were included. Drug resistance testing was performed by the proportion method. NTM species were identified by sequencing 16S rRNA, and the M.tb. isolates were genotyped using the VNTR (variable-number tandem-repeat) method.
From 2005 to 2008, a total of 1,233 HIV-infected patients were screened for TB infection in Guangxi. Eighteen percent—or 219—had a specimen that was culture positive for Mycobacterium species. Among these culture-positive patients, 53 percent had M.tb., and 47 percent had NTM. The majority of the isolates reflected pulmonary TB. The median CD4 count for 154 of these patients was only 35. CD4 counts were lower for patients with NTM than for M.tb. patients. Twelve NTM species were identified from the 102 NTM isolates, with M. avium complex being the most frequent.
Among the 111 M.tb. isolates with drug susceptibility test results, 27 percent were resistant to at least 1 FLD. Of these, 67 percent were new TB cases. Twelve patients had MDR TB, which was diagnosed in 8 of 20 previously treated TB cases and in 4 of 91 new TB cases. All 12 of the MDR TB patients were younger than 45 years old.
Among the 117 M.tb. isolates, 105 different genotypic patterns were identified; 97 isolates had unique genotype patterns, and 20 isolates were identified as cluster strains belonging to 8 different clusters. Beijing family strains accounted for 67 percent of M.tb. isolates, and 74 percent of isolates from patients aged less than 40 years old were of the Beijing genotype.
__________________
5 This section is based on the presentation by Liu Feiying, Guangxi Zhuang Autonomous Region Center for Disease Control and Prevention, China.
The high rate of MDR TB in previously treated HIV-infected patients in Guangxi indicates the need for effective management and treatment of patients with both TB and HIV, Feiying concluded.
Duan Hongfei, who presented a talk prepared by Chu Naihui, Beijing Chest Hospital, Capital Medical University, remarked that diabetes is a serious problem in China—there are more diabetes patients than TB patients. A 2008 national survey estimated that 90 million adults in China have diabetes, and more than 140 million adults have prediabetes (Yang et al., 2010).
In 2011, WHO and The Union launched a collaboration for the care and control of TB and diabetes (WHO and The Union, 2011). Also in 2011, dual screening of TB and diabetes was launched in some facilities in China. A study of screening of TB patients for diabetes in China was published in 2012 (Li et al., 2012). The study covered 6 facilities and 8,886 registered patients with TB. Among these TB patients, 1,090 with diabetes were identified, including 227 in whom diabetes was newly diagnosed. According to these numbers, if the screening were scaled up nationally, 124,000 additional patients with diabetes would be referred for care. Notably, the 2012 study was based on fasting blood glucose tests. A national survey in 2008 found that 47 percent of diabetes patients have normal fasting blood glucose and an abnormal oral glucose tolerance test. This means that TB cohorts might actually be found to have twice the prevalence of diabetes if they were screened using an oral glucose tolerance test.
At the same time, a study of screening of diabetes patients for TB in China was published (Lin et al., 2012). Among 11,330 diabetes patients screened, 92 had a positive TB symptom, including 7 with known TB and 48 with newly diagnosed TB. The screening was based on patient-reported data for 5 symptoms: cough for more than 2 weeks, night sweats for 4 weeks or longer, fever for 4 weeks or longer, weight loss for the previous 4 weeks, and any suspicion of active TB to account for extrapulmonary TB.
When comorbid, TB and diabetes must be treated at the same time. Physicians can choose either oral hypoglycemic agents or insulin injections to treat diabetes, though the latter is more frequently recommended. Treatment of diabetes can affect treatment for TB. For example, because the mean plasma concentration of rifampicin is lower in patients with diabetes, exposure to rifampicin is reduced by as much as 53 percent in these patients compared with nondiabetic controls (Nijland et al., 2006). Such pharma-
__________________
6 This section is based on the presentation by Duan Hongfei and Chu Naihui, Beijing Chest Hospital, Capital Medical University.
cokinetic differences may lead to easier acquisition of drug resistance and may explain the lower bacteriological response in diabetic patients with TB, Hongfei observed.
Some studies have found that TB patients with diabetes have more symptoms than those without diabetes, including cough, hemoptysis, dyspnea, fever, night sweats, and weight loss (Alisjahbana et al., 2007). There are also conflicting findings from studies evaluating whether sputum smear positivity is more frequent in diabetes than in nondiabetes. Although some studies have found a greater frequency in diabetes, Alisjahbana and colleagues (2007) found that smear positivity is nearly the same as that in nondiabetes. Hongfei suggested that the discrepancy is probably related to the frequency of cavities in the nondiabetes group, which has a close relationship with smear positivity.
Another influence of diabetes on TB is sputum conversion. Although bacillary protein may be higher at presentation in diabetic compared with nondiabetic patients, leading to modestly longer times to conversion, rates of conversion are similar in both groups by 2 to 3 months of treatment.
Finally, the combination of diabetes and TB may lead to a higher relapse rate and increased risk of death. A study from Egypt found that diabetes conferred a 3.9 times greater risk of treatment failure in patients (Morsy et al., 2003). In Indonesia, a 6-month sputum culture was positive in 22 percent of TB patients with diabetes and in 6.9 percent of controls (Alisjahbana et al., 2007). In the United States, diabetic patients with pulmonary TB have shown a sixfold increased risk of death compared with nondiabetic patients (Oursler et al., 2002). However, whether increased time to culture conversion in patients leads to a higher risk of relapse has not been adequately studied (Dooley et al., 2009).
This page intentionally left blank.














